APPLIED ANATOMY & PHYSIO.B.SC. SEMESTER-1-BKNMU-MCQ-MAY-2025
APPLIED ANATOMY & PHYSIOLOGY-2025
SECTION-I
Q.1 Select correct answer for Following MCQs. (06)
1.Which of the following is the functional unit of the kidney?
A. Glomerulus
B. Nephron
C. Bowman’s capsule
D. Loop of Henle
2.Left Atrioventricular valve is also called as valve
A. Aortic
C. Tricuspid
B. Bicuspid
D. Mitral
3.The arrangement of grey matter in spinal cord resembles the shape of letter
A. M
B. Q
C. W
D. H
4.Which of the following is a cranial nerve?
A. Sciatic nerve
B. Median nerve
C. Vagus nerve
D. Brachial nerve
5.The type of joint found between the atias and axis vertebrae is:
A. Ball-and-socket joint
B. Hinge joint
C. Pivot joint
D. Saddle joint
6.Which layer of the skin contains blood vessels, nerves, and glands?
A. Epidermis
B. Dermis
C Hypodermis
D. Stratum corneum
Q.2 Long Essay. (Any One) (10)
1.Describe gross structure of Liver in detail with diagram
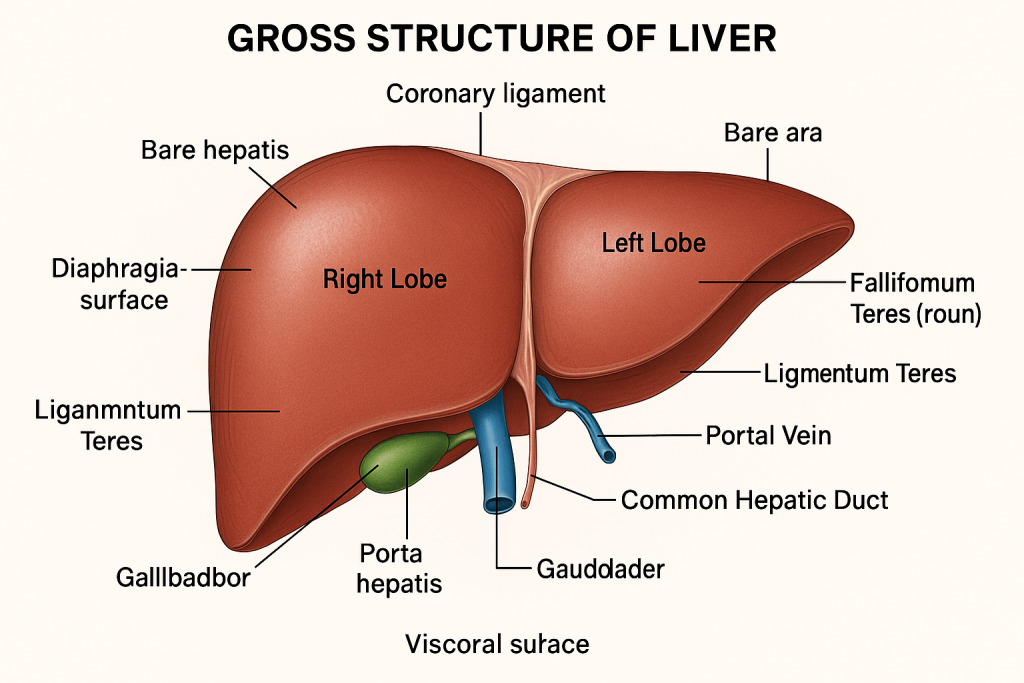
The liver is the largest internal organ and the largest gland in the human body. It plays a crucial role in metabolism, detoxification, storage, synthesis of bile, and regulation of blood components. The liver weighs around 1200–1500 grams in adults and is a highly vascular organ situated in the right upper quadrant of the abdomen, just beneath the diaphragm.
Gross Anatomy of the Liver
🔹 1. Position and Location
- Intraperitoneal organ, occupying the right hypochondrium, part of the epigastrium, and extending slightly into the left hypochondrium.
- Lies beneath the diaphragm, above the stomach, right kidney, and duodenum.
- Fixed in position by peritoneal ligaments and pressure from surrounding organs.
🔹 2. Shape, Color, and Consistency
- Shape: Wedge-shaped or triangular when viewed anteriorly; convex above and concave below.
- Color: Dark reddish-brown due to its rich blood supply.
- Consistency: Soft, friable, but dense organ enclosed in a fibrous capsule (Glisson’s capsule).
🔹 3. Surfaces of the Liver
🟦 A. Diaphragmatic Surface
- Convex, smooth, and dome-shaped.
- Lies against the undersurface of the diaphragm.
- Covered by visceral peritoneum except at the bare area.
- Divided into anterior, superior, and posterior surfaces.
- Forms the costodiaphragmatic recess above the right dome.
🟩 B. Visceral Surface
- Concave, irregular, and directed downwards, backward, and to the left.
- Impressions from neighboring organs:
- Gastric impression (stomach)
- Duodenal impression
- Renal impression (right kidney)
- Colic impression (hepatic flexure of colon)
- Gallbladder fossa
- Includes the porta hepatis (gateway of liver)
🔹 4. Borders of the Liver
- Anterior border: Sharp and thin; visible under costal margin.
- Posterior border: Blunt, rounded, and lies against the diaphragm.
- Inferior border: Separates diaphragmatic from visceral surface; palpable in hepatomegaly.
🔹 5. Lobes of the Liver
The liver is divided into four anatomical lobes, based on surface landmarks:
🟥 A. Right Lobe
- Largest lobe.
- Occupies most of the right hypochondrium.
- Contains:
- Gallbladder fossa
- Right hepatic vein
- Segment V to VIII (in surgical classification)
🟨 B. Left Lobe
- Flatter and smaller.
- Lies in epigastrium and left hypochondrium.
- Contains segments II and III, and part of IV.
🟧 C. Caudate Lobe
- Lies on posterior aspect, between inferior vena cava and ligamentum venosum.
- Functions independently in terms of blood supply and drainage.
🟫 D. Quadrate Lobe
- Lies between gallbladder fossa and ligamentum teres.
- Below porta hepatis.
🔹 6. Ligaments of the Liver
These are folds of peritoneum that suspend and support the liver:
🔸 A. Falciform Ligament
- Connects liver to anterior abdominal wall.
- Contains ligamentum teres (remnant of umbilical vein).
🔸 B. Coronary Ligament
- Attaches superior liver surface to diaphragm.
- Forms the boundary of the bare area.
🔸 C. Triangular Ligaments (Right & Left)
- Extensions of the coronary ligament.
- Help in anchoring liver laterally.
🔸 D. Lesser Omentum
- Extends from liver to lesser curvature of the stomach and first part of duodenum.
- Contains hepatic artery, portal vein, and bile duct (in hepatoduodenal ligament).
🔹 7. Porta Hepatis (Transverse Fissure)
- A deep horizontal fissure on the visceral surface.
- Acts as a gateway for structures entering and exiting the liver.
- Contains:
- Portal vein
- Hepatic artery
- Common hepatic duct
- Lymphatics and nerves
🔹 8. Bare Area of the Liver
- A non-peritoneal area on the posterior surface.
- In direct contact with the diaphragm.
- Surrounded by coronary ligaments.
🔹 9. Segmental Anatomy (Functional Classification)
- According to Couinaud’s classification, the liver is divided into 8 functional segments, each with its own blood supply and biliary drainage.
- Important in surgical resections (e.g., segmentectomy or lobectomy).
- Segments I to VIII arranged clockwise:
- Segment I = Caudate lobe (independent)
- Segment IV = Quadrate lobe
🔹 10. Blood Supply of Liver
The liver receives dual blood supply:
✅ A. Hepatic Artery (25%)
- Branch from celiac trunk
- Supplies oxygenated blood to hepatocytes.
✅ B. Portal Vein (75%)
- Formed by union of superior mesenteric vein and splenic vein.
- Carries nutrient-rich, deoxygenated blood from GIT to liver for processing.
🔹 11. Venous Drainage
- Blood drains from liver via 3 major hepatic veins (right, middle, left).
- These veins drain directly into the inferior vena cava.
🔹 12. Lymphatic Drainage
- Lymph from liver drains into:
- Hepatic lymph nodes
- Celiac nodes
- Mediastinal nodes
🔹 13. Nerve Supply
- Sympathetic fibers: from celiac plexus (vasomotor)
- Parasympathetic fibers: from vagus nerve
- Liver has no pain receptors on the surface (capsule may cause pain when stretched)
🔹 14. Coverings of the Liver
- Covered by:
- Glisson’s capsule (fibrous tissue)
- Visceral peritoneum (except at bare area, porta hepatis, and gallbladder fossa)
The liver’s gross structure reflects its functional complexity and clinical importance. Divided anatomically and functionally into distinct lobes and segments, and having dual blood supply, it plays a key role in digestion, detoxification, storage, metabolism, and immune regulation. A clear understanding of liver anatomy is essential for surgical, pathological, and nursing practices in healthcare.
2.Describe the different types of Synovial joints in detail with diagram
Types of Synovial Joints
Synovial joints are classified based on the shape of the articulating surfaces and the type of movement they permit. There are six major types, each allowing specific types of movement depending on its anatomical structure.
1. Plane Joints
Plane joints, also known as gliding joints, have flat or slightly curved articular surfaces that allow bones to slide over one another. These joints permit limited movement, typically in a single plane and are non-axial. Examples include the intercarpal joints of the wrist and intertarsal joints of the foot. Although the movement is minimal, it plays a critical role in fine-tuning positioning and absorbing forces.
2. Hinge Joints
Hinge joints operate similarly to the hinge of a door, allowing movement predominantly in one axis — flexion and extension. One bone has a convex surface that fits into the concave surface of another bone. This uniaxial joint permits powerful and controlled movement, as seen in the elbow joint (between the humerus and ulna), knee joint (a modified hinge), and the interphalangeal joints of the fingers and toes. The stability of hinge joints is enhanced by strong collateral ligaments.
3. Pivot Joints
Pivot joints allow rotational movement around a single axis. These uniaxial joints consist of a rounded bony process that rotates within a ring formed by bone and ligament. An excellent example is the atlantoaxial joint between the first and second cervical vertebrae, which allows the head to rotate side-to-side (“no” motion). Another example is the proximal radioulnar joint, which enables pronation and supination of the forearm.
4. Condyloid Joints
Also called ellipsoid joints, condyloid joints feature an oval convex surface of one bone fitting into a complementary concave surface of another. These are biaxial joints, allowing movement in two planes: flexion-extension and abduction-adduction, along with circumduction. Examples include the radiocarpal (wrist) joint and metacarpophalangeal (knuckle) joints. These joints are involved in movements requiring precision and control.
5. Saddle Joints
Saddle joints have articular surfaces that are reciprocally concave and convex, resembling a rider sitting on a saddle. These joints are also biaxial but allow a slightly greater range of motion than condyloid joints. The most prominent example is the carpometacarpal joint of the thumb (between the trapezium and the first metacarpal), which allows flexion, extension, abduction, adduction, and opposition. This joint provides the thumb with remarkable dexterity essential for grasping and manipulating objects.
6. Ball-and-Socket Joints
These are the most mobile type of synovial joint, allowing movement in multiple axes and planes — making them multiaxial. One bone has a spherical head that fits into a rounded cup-like socket of another bone. This configuration permits a full range of movement: flexion, extension, abduction, adduction, rotation, and circumduction. The shoulder (glenohumeral joint) and hip (acetabulofemoral joint) are classic examples. While the shoulder allows greater mobility, the hip joint is more stable due to deeper socket engagement
Q.3 Write Short notes. (Any Three)(15)
1 Structure of Pancreas
The pancreas is a soft, elongated, retroperitoneal gland located in the upper abdomen. It serves both exocrine and endocrine functions. Structurally, it is part of the digestive system and endocrine system and plays a vital role in digestion and glucose regulation. Its anatomical placement and unique histological organization make it a critical organ in maintaining metabolic homeostasis.
📌 Anatomical Location and Position
The pancreas is located in the epigastric and left hypochondriac regions, lying transversely across the posterior abdominal wall behind the stomach. It extends from the duodenum on the right to the spleen on the left and lies at the level of the L1 and L2 vertebrae.
It is considered a retroperitoneal organ, except for its tail, which is intraperitoneal. The pancreas is closely related to several structures including the duodenum, stomach, spleen, left kidney, and major blood vessels such as the aorta and inferior vena cava.
🧠 Gross Structure of the Pancreas
The pancreas is divided into four main parts, each with distinct anatomical features:
🔹 1. Head
- The head is the broadest part, situated within the C-shaped curve of the duodenum.
- A small projection called the uncinate process extends from the lower part of the head and lies behind the superior mesenteric vessels.
🔹 2. Neck
- The neck is a short, flattened portion between the head and body.
- It lies anterior to the superior mesenteric vessels and overlies the portal vein, which is formed behind the neck.
🔹 3. Body
- The body is elongated and triangular in cross-section.
- It passes obliquely to the left across the vertebral column and lies posterior to the stomach.
- The splenic vein runs along its posterior surface, and it is related to the left kidney and left adrenal gland.
🔹 4. Tail
- The tail is the narrowest and left-most part of the pancreas.
- It lies within the splenorenal ligament, close to the hilum of the spleen.
- It is the only part of the pancreas that is intraperitoneal.
🩸 Duct System of the Pancreas
✅ Main Pancreatic Duct (Duct of Wirsung):
- Runs the length of the pancreas.
- Joins with the common bile duct to form the hepatopancreatic ampulla (ampulla of Vater), which opens into the second part of the duodenum through the major duodenal papilla.
✅ Accessory Pancreatic Duct (Duct of Santorini):
- Sometimes present.
- Opens into the duodenum above the major papilla, via the minor duodenal papilla.
🔬 Microscopic (Histological) Structure
The pancreas has both exocrine and endocrine components:
🧪 1. Exocrine Part (Majority of the Pancreas – ~98%)
- Composed of serous acini that secrete digestive enzymes.
- Acinar cells produce enzymes like amylase, lipase, trypsinogen, and chymotrypsinogen.
- These secretions are drained by ductules into the main pancreatic duct and then into the duodenum.
🧬 2. Endocrine Part (Islets of Langerhans)
- Scattered throughout the pancreas, especially in the tail region.
- Made of hormone-secreting cells:
- Alpha cells – secrete glucagon
- Beta cells – secrete insulin
- Delta cells – secrete somatostatin
- PP cells – secrete pancreatic polypeptide
These hormones are secreted directly into the bloodstream and help regulate blood glucose levels.
🩺 Blood Supply
- Arterial supply:
- Branches of the splenic artery (for body and tail)
- Superior pancreaticoduodenal artery (from gastroduodenal artery)
- Inferior pancreaticoduodenal artery (from superior mesenteric artery)
- Venous drainage:
- Via pancreatic veins into splenic vein, superior mesenteric vein, and finally into the portal vein.
⚙️ Nerve Supply
- Sympathetic fibers from the celiac plexus.
- Parasympathetic fibers from the vagus nerve.
- These regulate both endocrine and exocrine functions.
2 Structure of Eye
The eye is a complex, spherical sensory organ responsible for the sense of vision. It is often referred to as the “camera of the body” as it captures light rays and converts them into electrical impulses interpreted by the brain. The human eye is protected, nourished, and supported by multiple layers and structures, making it a highly specialized organ. Understanding its structure is essential for studying visual physiology and related disorders.
👁️ External Features of the Eye
The human eye is almost spherical, about 2.5 cm in diameter, and lies in the orbit, protected by the eyelids, eyelashes, and lacrimal apparatus. Only the anterior part (cornea) is visible externally.
Anatomical Structure of the Eyeball
The eyeball consists of three concentric layers (tunics) and internal components such as chambers, lens, and fluids. The three main layers from outer to inner are:
🔵 1. Outer Fibrous Layer (Protective Layer)
This is the outermost layer that provides protection and shape to the eyeball. It consists of:
🟣 A. Sclera
- The white, opaque part of the eye that covers the posterior 5/6 of the eyeball.
- It is made of dense connective tissue.
- Provides protection, maintains shape, and gives attachment to extraocular muscles.
🔵 B. Cornea
- The transparent, avascular part in the anterior 1/6 of the eyeball.
- It allows light to enter the eye and contributes to refraction.
- Extremely sensitive to touch and pain due to dense innervation.
🟠 2. Middle Vascular Layer (Uveal Tract)
This is the middle pigmented and vascular layer that provides nutrients and regulates light entry. It includes:
🟢 A. Choroid
- A highly vascular, pigmented membrane lining the inner surface of the sclera.
- Supplies oxygen and nutrients to the retina.
- Pigment prevents internal reflection of light.
🟡 B. Ciliary Body
- A ring-shaped structure composed of ciliary muscles and processes.
- Controls the shape of the lens (accommodation) via suspensory ligaments.
- Produces aqueous humor.
🔴 C. Iris
- The colored part of the eye with a central opening called the pupil.
- Regulates light entry by constriction (via sphincter pupillae) and dilation (via dilator pupillae).
- Contains smooth muscle and pigment cells.
🔴 3. Inner Nervous Layer (Retina)
The innermost layer of the eye is the retina, responsible for converting light into nerve impulses.
🔵 A. Pigmented Layer
- Outer layer containing melanin; absorbs stray light.
🔴 B. Neural Layer
- Contains photoreceptor cells (rods and cones), bipolar cells, and ganglion cells.
- Rods: Responsible for vision in dim light (night vision).
- Cones: Responsible for color vision and sharpness (day vision).
- The retina also contains:
- Optic disc (blind spot): Where the optic nerve exits, no photoreceptors.
- Macula lutea and fovea centralis: Area of sharpest vision, dense with cones.
⚪ Internal Structures of the Eye
🟡 Lens
- A transparent, biconvex, elastic structure located behind the iris.
- Helps in fine focusing of light rays on the retina (accommodation).
- Held in place by suspensory ligaments from the ciliary body.
🔵 Aqueous Humor
- A clear fluid secreted by the ciliary body.
- Found in anterior and posterior chambers of the eye (in front of the lens).
- Maintains intraocular pressure, nourishes cornea and lens.
🔴 Vitreous Humor
- A gel-like transparent substance filling the posterior segment (behind the lens).
- Maintains shape of the eyeball and holds the retina in place.
👁️ Accessory Structures of the Eye
✅ Eyelids (Palpebrae)
- Protect the eye from injury and light.
- Spread tears during blinking.
✅ Conjunctiva
- Thin, transparent mucous membrane lining the inside of eyelids and anterior sclera.
✅ Lacrimal Apparatus
- Composed of lacrimal gland, ducts, sac, and nasolacrimal duct.
- Produces and drains tears that moisten and protect the eye.
✅ Extraocular Muscles
- Six muscles (superior, inferior, medial, lateral rectus and two obliques) control eye movements.
3 Structure of Stomach
The stomach is a muscular, hollow, J-shaped organ of the digestive system that lies between the esophagus and small intestine (duodenum). It acts as a reservoir for food, mechanically and chemically breaking it down with the help of gastric secretions. It plays a vital role in digestion, secretion, absorption, and protection. Structurally, the stomach is anatomically and histologically specialized to carry out these functions efficiently.
📌 Location and Position
The stomach is located in the upper left quadrant of the abdominal cavity, primarily in the epigastric, umbilical, and left hypochondriac regions. It lies beneath the diaphragm and partly under the left costal margin. Its position varies with posture, fullness, and body type. In a well-fed state, it extends from the left of the midline to just below the xiphoid process.
📐 External Gross Anatomy of the Stomach
The stomach has two curvatures, two surfaces, and is divided into four main anatomical parts:
🔷 1. Curvatures
- Greater curvature: Long convex border on the left side, gives attachment to the greater omentum.
- Lesser curvature: Shorter concave border on the right side, gives attachment to the lesser omentum.
🔶 2. Surfaces
- Anterior surface: Related to the liver, diaphragm, and anterior abdominal wall.
- Posterior surface: Related to the pancreas, spleen, left kidney, adrenal gland, and transverse mesocolon – collectively forming the stomach bed.
🔷 3. Parts of the Stomach
The stomach is divided into four anatomical regions:
🟣 A. Cardia
- The part where the esophagus opens into the stomach.
- Lies just below the cardiac orifice.
- Contains the cardiac sphincter, which prevents reflux of food into the esophagus.
🔵 B. Fundus
- The dome-shaped superior portion above the level of the esophageal opening.
- Lies beneath the diaphragm and may contain air (visible on X-rays).
🟠 C. Body (Corpus)
- The main central portion of the stomach.
- Responsible for mixing and temporary storage of food.
- Contains numerous gastric glands secreting enzymes and acid.
🔴 D. Pyloric Part
- Located near the duodenum and includes:
- Pyloric antrum: Wider proximal part
- Pyloric canal: Narrow distal part leading to the pyloric sphincter
- The pyloric sphincter regulates the passage of chyme into the small intestine.
🧪 Histological (Microscopic) Structure of the Stomach Wall
The wall of the stomach is made up of four concentric layers, from outer to inner:
✅ 1. Serosa (Outer Layer)
- The outermost covering, made of visceral peritoneum.
- Reduces friction as the stomach moves.
✅ 2. Muscularis Externa
- Consists of three layers of smooth muscle:
- Outer longitudinal layer
- Middle circular layer
- Inner oblique layer (unique to stomach)
- These muscle layers help in churning, mixing, and propelling food during digestion.
✅ 3. Submucosa
- Contains blood vessels, lymphatics, and nerves (Meissner’s plexus).
- Supports mucosa and provides elasticity.
✅ 4. Mucosa (Innermost Layer)
- Lined by simple columnar epithelium.
- Contains gastric pits and glands:
- Chief cells: Secrete pepsinogen
- Parietal cells: Secrete HCl and intrinsic factor
- Mucous cells: Secrete protective mucus
- G cells: Secrete gastrin hormone
The mucosa forms rugae (folds) when the stomach is empty, which help it expand when food enters.
🔬 Blood Supply of the Stomach
🩸 Arterial supply
- From branches of the celiac trunk:
- Left gastric artery
- Right gastric artery
- Left and right gastroepiploic arteries
- Short gastric arteries
🩸 Venous drainage
- Veins drain into the portal vein via:
- Left and right gastric veins
- Gastroepiploic veins
- Short gastric veins
🧠 Nerve Supply
- Parasympathetic supply: Via vagus nerve, stimulates gastric secretions and motility.
- Sympathetic supply: From celiac plexus, inhibits gastric activity and constricts blood vessels.
🧬 Lymphatic Drainage
Lymph from the stomach drains into:
- Gastric lymph nodes
- Pancreaticosplenic nodes
- Celiac lymph nodes
4.Structure of Pharynx
The pharynx is a muscular, funnel-shaped tube that serves as a common passage for both the respiratory and digestive systems. It extends from the base of the skull to the level of the sixth cervical vertebra, where it continues as the esophagus. The pharynx plays a vital role in breathing, swallowing (deglutition), and phonation. It acts as a crossroad where food and air share a common pathway, but are directed into different systems through coordinated muscular actions.
📌 Location and Extent
The pharynx is located behind the nasal cavities, oral cavity, and larynx. It extends from the base of the skull (body of sphenoid and basilar part of occipital bone) down to the level of C6 vertebra, where it becomes continuous with the esophagus.
🧠 Divisions of the Pharynx
Anatomically, the pharynx is divided into three regions based on the structures it lies behind:
🔹 1. Nasopharynx
- Location: Lies behind the nasal cavity and above the soft palate.
- Lining: Pseudostratified ciliated columnar epithelium (respiratory epithelium).
- Openings:
- Internal nares (choanae) open into it anteriorly.
- Pharyngeal opening of the auditory (Eustachian) tube on each lateral wall.
- Tonsils: Contains the pharyngeal tonsil (adenoids) on its roof.
- Function: Passage of air from the nasal cavity to the oropharynx.
🔸 2. Oropharynx
- Location: Lies behind the oral cavity, extending from the soft palate to the upper border of the epiglottis.
- Lining: Stratified squamous epithelium (to resist friction).
- Openings:
- Communicates with the oral cavity via the fauces (oropharyngeal isthmus).
- Tonsils: Contains the palatine tonsils between the palatoglossal and palatopharyngeal arches.
- Function: Conveys food and air; active in swallowing and speech.
🔻 3. Laryngopharynx (Hypopharynx)
- Location: Lies behind the larynx, extending from the upper border of the epiglottis to the lower border of the cricoid cartilage (level of C6).
- Lining: Stratified squamous epithelium.
- Openings:
- Anteriorly opens into the larynx via the laryngeal inlet.
- Structures:
- Contains piriform fossae (recesses) on each side of the laryngeal inlet.
- Function: Directs food toward the esophagus and air toward the larynx.
🧬 Layers of the Pharyngeal Wall
The wall of the pharynx is composed of the following four concentric layers, from inner to outer:
✅ 1. Mucosa
- Innermost layer.
- Lined by either respiratory epithelium (nasopharynx) or stratified squamous epithelium (oro- and laryngopharynx).
✅ 2. Submucosa
- Connective tissue layer containing blood vessels, lymphatics, and nerves.
✅ 3. Muscular Layer
- Outer circular muscles: Form constrictors (superior, middle, and inferior constrictor muscles) that help in swallowing by pushing the bolus downward.
- Inner longitudinal muscles: Include stylopharyngeus, salpingopharyngeus, and palatopharyngeus; help elevate the pharynx during swallowing and speaking.
✅ 4. Buccopharyngeal Fascia
- Outermost connective tissue layer.
- Contains the pharyngeal plexus of nerves and blends with adjacent fascial layers.
🩸 Blood Supply
- Arterial supply:
- Branches from external carotid artery, including:
- Ascending pharyngeal artery
- Facial artery
- Maxillary artery
- Lingual artery
- Branches from external carotid artery, including:
- Venous drainage:
- Drains into the pharyngeal venous plexus, then into internal jugular vein.
🧠 Nerve Supply
- The pharynx is innervated by the pharyngeal plexus formed by:
- Motor fibers: From the vagus nerve (cranial nerve X).
- Sensory fibers: From glossopharyngeal nerve (cranial nerve IX).
- Sympathetic fibers: From the superior cervical ganglion.
- Note: Stylopharyngeus muscle is innervated directly by CN IX, not via the plexus.
🧫 Lymphatic Drainage
- Drains into deep cervical lymph nodes, especially:
- Jugulodigastric node (important in tonsillar infections).
- Retropharyngeal and parapharyngeal nodes.
Q.4 Write Very Short notes. (Any Three)(06)
1.Name the branches of coronary artery
🔵 1. Right Coronary Artery (RCA)
Originates from the right aortic sinus.
✳️ Main Branches of RCA:
- Conus branch – to the infundibulum (right ventricular outflow tract)
- Right marginal artery – supplies the right ventricle
- Posterior interventricular artery (Posterior descending artery/PDA) – runs in posterior interventricular groove, supplies posterior 1/3rd of interventricular septum
- Sinoatrial (SA) nodal branch – supplies the SA node (in ~60% of people)
- Atrioventricular (AV) nodal branch – supplies the AV node
✅ Area Supplied:
- Right atrium
- Most of right ventricle
- Part of left ventricle (inferior surface)
- Posterior 1/3 of interventricular septum
- SA and AV nodes (in majority)
🔴 2. Left Coronary Artery (LCA)
Originates from the left aortic sinus. It is short and bifurcates into two major branches:
✳️ Main Branches of LCA:
- Left anterior descending (LAD) artery:
- Runs in anterior interventricular groove
- Gives diagonal branches to left ventricle
- Gives septal branches to anterior 2/3 of interventricular septum
- Left circumflex artery (LCx):
- Runs in the left atrioventricular (coronary) sulcus
- Gives left marginal artery to the lateral wall of left ventricle
- May give SA nodal branch (in ~40% of people)
2.Mention the types of bone
🔹 1. Long Bones
- Description: Longer than they are wide, with a shaft and two ends.
- Structure: Composed of compact bone with a central marrow cavity.
- Function: Support weight and facilitate movement.
- Examples:
- Femur (thigh bone)
- Humerus (upper arm bone)
- Radius, Ulna, Tibia, Fibula
🔸 2. Short Bones
- Description: Approximately equal in length, width, and thickness (cube-shaped).
- Structure: Mostly spongy bone with a thin outer layer of compact bone.
- Function: Provide stability and limited motion.
- Examples:
- Carpals (wrist bones)
- Tarsals (ankle bones)
🔹 3. Flat Bones
- Description: Thin, flattened, and usually curved.
- Structure: Two thin layers of compact bone with spongy bone in between.
- Function: Protect internal organs and provide surface for muscle attachment.
- Examples:
- Skull bones (e.g., frontal, parietal)
- Sternum
- Ribs
- Scapula
🔸 4. Irregular Bones
- Description: Complex shapes that do not fit other categories.
- Structure: Mostly spongy bone enclosed by thin compact bone.
- Function: Protect nervous tissue and support structures.
- Examples:
- Vertebrae
- Hip bones (pelvis)
- Facial bones
🔹 5. Sesamoid Bones
- Description: Small, round bones embedded in tendons.
- Function: Reduce friction and modify pressure at joints.
- Examples:
- Patella (kneecap) – largest sesamoid bone
- Sesamoid bones in hands and feet
3.Enumerate the muscles of buttocks
🔹 1. Superficial Muscles (Gluteal Group)
These muscles are large and responsible for movement of the thigh (extension, abduction, and rotation).
✅ a) Gluteus Maximus
- Largest and most superficial muscle
- Action: Extends and laterally rotates the thigh
✅ b) Gluteus Medius
- Located beneath gluteus maximus
- Action: Abducts and medially rotates the thigh
✅ c) Gluteus Minimus
- Deepest of the three gluteal muscles
- Action: Abducts and medially rotates the thigh
✅ d) Tensor Fasciae Latae
- Located on the lateral side of the thigh
- Action: Tenses the fascia lata and assists in thigh abduction
🔸 2. Deep Muscles (Lateral Rotators of Hip)
These smaller muscles lie beneath the gluteus minimus and are mainly involved in lateral rotation of the thigh.
✅ a) Piriformis
✅ b) Superior Gemellus
✅ c) Obturator Internus
✅ d) Inferior Gemellus
✅ e) Quadratus Femoris
4.Name the layers of uterus
🔹 1. Perimetrium (Serosal Layer)
- The outermost layer.
- It is part of the visceral peritoneum.
- Covers the fundus and part of the body of the uterus.
- Provides protection and reduces friction with other organs.
🔸 2. Myometrium
- The middle and thickest layer.
- Composed of smooth muscle fibers arranged in longitudinal, circular, and oblique layers.
- Responsible for uterine contractions during menstruation and childbirth.
🔹 3. Endometrium
- The innermost mucosal lining of the uterus.
- Rich in blood vessels and glands.
- Divided into:
- Stratum functionalis – sheds during menstruation
- Stratum basalis – regenerates the functionalis layer
- Site of implantation for fertilized egg and supports fetal development.
SECTION-II (38 Marks)
Q.5 Select correct answer for Following MCQs. (07)
1.Which hormone regulates the sleep-wake cycle?
A. Serotonin
B. Melatonin
C. Adrenaline
D. Cortisol
2.Which cell structure act as power house of cell
A Mitochondria
B. Spleen
C. Golgi body
D. Liver
3.What is the normal pH of blood in humans?
A. 6.8-7.0
B. 7.35-7.45
C. 7.8-8.0
D. 8.5-9.0
4.Pepsin is responsible for the digestion of
A. Protein
B. Carbohydrate
C. Fat
D. Minerals
5.Which organ is the main regulator of water balance in the body?
A. Liver
B Kidneys
C. Lungs
D. Heart
6.During muscle contraction, calcium ions bind to:
A. Myosin
B. Troponin
C. Actin
D. Tropomyosin
7.The main function of platelets is to:
A. Transport oxygen
B. Initiate blood clotting
C. Fight infections
D. Regulate blood pressure
Q.6 Long Essay. (Any One) (10)
1.Discuss in detail the various stages of erythropoiesis and functions of blood
✨ Part I: Stages of Erythropoiesis
Erythropoiesis is the biological process by which erythrocytes (red blood cells or RBCs) are produced in the red bone marrow from multipotent stem cells. It ensures continuous replacement of aging and destroyed RBCs and is essential for oxygen transport and tissue oxygenation.
📍 Site of Erythropoiesis
- In the embryo:
- Yolk sac (2–3 weeks of gestation)
- Liver and spleen (2nd–7th month)
- In the fetus:
- Primarily liver and spleen
- In adults:
- Red bone marrow of flat bones (sternum, ribs, vertebrae, skull, pelvis) and proximal ends of humerus and femur
🔄 Sequential Stages of Erythropoiesis
- 🔹 Hematopoietic Stem Cell (HSC)
- Pluripotent stem cell that differentiates into common myeloid progenitor.
- It gives rise to erythroid, megakaryocyte, myeloid, and mast cell lineages.
- 🔹 Proerythroblast (Pronormoblast)
- First committed erythroid precursor.
- Large cell with round nucleus, basophilic cytoplasm due to ribosomes.
- Nucleoli are prominent.
- 🔹 Basophilic Erythroblast
- Smaller in size, intense basophilic cytoplasm.
- Begins active hemoglobin synthesis.
- Nucleus starts to condense.
- 🔹 Polychromatic Erythroblast
- Cytoplasm is grayish due to presence of both ribosomes (blue) and hemoglobin (pink).
- Nucleus becomes smaller, more condensed.
- Significant hemoglobin production occurs here.
- 🔹 Orthochromatic Erythroblast (Normoblast)
- Cytoplasm is mostly acidophilic (pink) due to high hemoglobin content.
- Nucleus becomes pyknotic (dense) and is eventually expelled from the cell.
- 🔹 Reticulocyte
- Anucleated immature RBC.
- Contains remnants of RNA and organelles visible with supravital stains (e.g., methylene blue).
- Enters bloodstream and matures into RBC within 24–48 hours.
- 🔹 Mature Erythrocyte
- Biconcave, flexible, enucleated disc.
- Diameter: ~7.2 micrometers.
- Life span: ~120 days.
- Function: Oxygen and carbon dioxide transport using hemoglobin.
- Controlled mainly by Erythropoietin (EPO), a glycoprotein hormone.
- EPO is secreted by the peritubular capillary lining cells of the kidney in response to hypoxia.
- Other essential factors:
- Iron – essential for heme synthesis.
- Vitamin B12 & Folic Acid – required for DNA replication.
- Amino acids – necessary for globin chain formation.
- Hormones – androgens, thyroxine, and corticosteroids enhance erythropoiesis.
- ❤️ Part II: Functions of Blood
Blood is a vital fluid connective tissue that accounts for approximately 7–8% of total body weight (~5–6 liters in an average adult). It is composed of plasma (55%) and formed elements (45%), including RBCs, WBCs, and platelets.
🔴 1. Transport Functions
- Oxygen transport:
- Carried by hemoglobin in RBCs from lungs to body tissues.
- Carbon dioxide transport:
- As bicarbonate (70%), carbaminohemoglobin (20–25%), and dissolved CO₂ (5–10%).
- Nutrient transport:
- Glucose, amino acids, lipids, vitamins absorbed from GIT to cells.
- Hormones and enzymes:
- Endocrine secretions are transported to target organs.
- Metabolic waste transport:
- Urea, uric acid, and creatinine are transported to kidneys for excretion.
🟢 2. Regulatory Functions
- Acid–base balance:
- Maintained by buffer systems (bicarbonate, phosphate, hemoglobin).
- Thermoregulation:
- Blood distributes heat generated by muscle and organ activity throughout the body.
- Fluid–electrolyte balance:
- Regulated through plasma proteins and ions (Na⁺, K⁺, Ca²⁺, Cl⁻).
⚪ 3. Protective Functions
- Immunological defense:
- WBCs (neutrophils, monocytes, lymphocytes) fight infections and produce antibodies.
- Clotting mechanism:
- Platelets, fibrinogen, and clotting factors form clots to prevent blood loss.
- Inflammation and phagocytosis:
- Neutrophils and macrophages ingest pathogens and damaged cells.
🔵 4. Homeostatic Functions
- Maintains tissue perfusion and pressure.
- Circulating antibodies and immune cells help in long-term immune regulation.
- Removes toxic substances from tissues.
- Blood tests help diagnose:
- Anemia, infection, diabetes, leukemia, clotting disorders, blood group compatibility.
- Blood typing: Essential for transfusions and organ transplantation.
- CBC (Complete Blood Count): Assesses health and detects a wide range of disorders.
2.Describe cardiac Conduction system and cardiac cycle in detail
The cardiac conduction system is a specialized network of excitable myocardial cells that generate and transmit electrical impulses across the heart. These impulses ensure that the atria and ventricles contract in a coordinated, rhythmic, and timely manner, resulting in effective pumping of blood. Unlike skeletal muscle, the heart contracts involuntarily and rhythmically due to this intrinsic conduction system.
🔋 Main Components of the Cardiac Conduction System
🔹 1. Sinoatrial (SA) Node – Primary Pacemaker of the Heart
- Location: In the wall of the right atrium, near the superior vena cava opening.
- Function: Generates spontaneous electrical impulses at a rate of 70–100 beats per minute under normal physiological conditions.
- These impulses spread through the atrial myocardium, causing atrial contraction.
- The rate is influenced by autonomic nervous system:
- Sympathetic stimulation increases rate.
- Parasympathetic (vagal) stimulation decreases rate.
🔹 2. Atrioventricular (AV) Node
- Location: In the interatrial septum, near the tricuspid valve.
- Function: Receives impulses from the SA node and delays conduction by ~0.1 sec.
- This delay allows for complete ventricular filling before ventricular contraction.
- Acts as a backup pacemaker if SA node fails (rate: ~40–60 bpm).
🔹 3. Bundle of His (Atrioventricular Bundle)
- Arises from the AV node and passes through the fibrous skeleton of the heart.
- Acts as the only electrical connection between atria and ventricles.
- Divides into right and left bundle branches.
🔹 4. Right and Left Bundle Branches
- Travel along the interventricular septum toward the heart’s apex.
- Conduct impulses to respective ventricles:
- Right bundle → right ventricle
- Left bundle → left ventricle (further divides into anterior and posterior fascicles)
🔹 5. Purkinje Fibers
- Network of specialized fibers arising from bundle branches.
- Spread throughout the ventricular myocardium.
- Initiate rapid and coordinated ventricular contraction starting from the apex to the base, aiding efficient blood ejection.
The cardiac cycle is the sequence of mechanical and electrical events in the heart during one heartbeat. It includes:
- Systole – Contraction phase (pumping)
- Diastole – Relaxation phase (filling)
Each cycle ensures the heart chambers contract and relax in a synchronized manner to maintain continuous blood flow.
⏱️ Duration of the Cardiac Cycle
- At a normal heart rate of 75 bpm, one cardiac cycle lasts about 0.8 seconds.
🔄 Phases of the Cardiac Cycle
The cardiac cycle includes three major phases, each having critical subphases:
🔸 1. Atrial Systole (Duration: ~0.1 seconds)
- Triggered by the SA node.
- Both atria contract, pushing blood into the relaxed ventricles.
- AV valves (mitral and tricuspid) remain open, while semilunar valves are closed.
- Contributes approximately 20–30% of ventricular filling (“atrial kick”).
🔸 2. Ventricular Systole (Duration: ~0.3 seconds)
✅ A. Isovolumetric Contraction
- Ventricles begin to contract after impulse from Purkinje fibers.
- AV valves close (first heart sound – S1).
- Semilunar valves remain closed.
- Pressure builds without a change in volume.
✅ B. Ejection Phase
- When ventricular pressure exceeds that in aorta/pulmonary artery:
- Semilunar valves open.
- Blood is ejected into systemic and pulmonary circulations.
- End-systolic volume remains in ventricles (~50 mL).
🔸 3. Ventricular Diastole (Duration: ~0.4 seconds)
✅ A. Isovolumetric Relaxation
- Ventricles begin to relax after ejection.
- Semilunar valves close (second heart sound – S2).
- All valves remain closed briefly.
- Ventricular pressure drops rapidly.
✅ B. Passive Filling
- Once ventricular pressure falls below atrial pressure:
- AV valves open.
- Blood flows passively from atria into ventricles (~70–80%).
🩺 Heart Sounds During Cardiac Cycle
- S1 (“Lub”) – Closure of AV valves (start of ventricular systole).
- S2 (“Dub”) – Closure of semilunar valves (start of diastole).
- S3 – Heard in early diastole in children/athletes (may indicate heart failure in adults).
- S4 – Heard just before S1, associated with stiff ventricles.
Q.7 Write Short notes. (Any Three) (15)
1.Functions of Cerebellum
1. Coordination of Voluntary Movements
- Acts as the “comparator” — it compares motor commands from the cerebral cortex with sensory feedback from muscles.
- Ensures smooth, accurate, and purposeful movements.
- Coordinates both gross motor skills (walking, posture) and fine motor skills (writing, instrument playing).
🔹 2. Maintenance of Balance and Equilibrium
- Integrates signals from the vestibular system, proprioceptors, and visual input.
- Maintains static posture (standing still) and dynamic balance (walking or turning).
- Adjusts trunk and limb position during movement.
🔹 3. Regulation of Muscle Tone
- Regulates the baseline tension in muscles through interaction with the reticular formation and spinal motor neurons.
- Helps prevent hypotonia (decreased tone) or hypertonia (increased tone).
🔹 4. Motor Learning and Skill Acquisition
- Important in learning and refining new motor activities (e.g., riding a bicycle, playing a musical instrument).
- Stores motor memory through repeated practice.
- Adjusts incorrect or imprecise movements (error correction).
🔹 5. Timing and Rhythm of Movements
- Coordinates the timing and sequencing of muscle activity.
- Especially important in movements requiring rhythm and pace — e.g., speaking, dancing, clapping in time.
🔹 6. Cognitive and Emotional Roles (Recent Discoveries)
- The lateral cerebellar hemisphere is involved in attention, language, and executive function.
- Regulates emotional processing, anticipatory planning, and motor imagery through connections with the prefrontal cortex.
2 Physiology of Respiration
🔹 1. Pulmonary Ventilation (Breathing)
This is the movement of air into and out of the lungs.
✅ A. Inspiration (Inhalation)
- Active process involving contraction of:
- Diaphragm (flattens and descends)
- External intercostal muscles (lift rib cage)
- Thoracic cavity volume increases → Intrapulmonary pressure drops → Air enters lungs.
✅ B. Expiration (Exhalation)
- Passive process during quiet breathing:
- Diaphragm and intercostal muscles relax.
- Thoracic volume decreases → Intrapulmonary pressure rises → Air is expelled.
- Active expiration (e.g., during exercise) involves:
- Internal intercostals and abdominal muscles.
🔹 2. Pulmonary Gas Exchange (External Respiration)
- Occurs in the alveoli of the lungs.
- Oxygen diffuses from alveolar air (high O₂) into capillary blood (low O₂).
- Carbon dioxide diffuses from blood (high CO₂) into alveoli (low CO₂).
- Driven by partial pressure gradients (Dalton’s Law).
✅ Factors Affecting Gas Exchange:
- Surface area of alveoli
- Thickness of respiratory membrane
- Partial pressure difference
- Ventilation-perfusion (V/Q) matching
🔹 3. Transport of Gases in Blood
✅ A. Oxygen Transport
- 98.5% is carried by hemoglobin as oxyhemoglobin (HbO₂).
- 1.5% is dissolved in plasma.
✅ B. Carbon Dioxide Transport
- 7–10% dissolved in plasma
- 20–23% bound to hemoglobin as carbaminohemoglobin (HbCO₂)
- 70% transported as bicarbonate ions (HCO₃⁻) (via carbonic anhydrase reaction)
🔹 4. Internal Respiration (Tissue Gas Exchange)
- Occurs at the capillary-tissue interface.
- Oxygen diffuses from blood (high pO₂) to tissues (low pO₂).
- Carbon dioxide diffuses from tissues (high pCO₂) to blood (low pCO₂).
🧠 Regulation of Respiration
Respiration is controlled both neuronally and chemically:
🔸 A. Neural Control
Controlled by respiratory centers in the medulla oblongata and pons:
✅ Medullary Centers:
- Inspiratory center: Initiates normal rhythmic breathing.
- Expiratory center: Active during forced expiration.
✅ Pontine Centers:
- Apneustic center: Promotes inspiration.
- Pneumotaxic center: Inhibits inspiration to regulate rhythm and depth.
🔸 B. Chemical Regulation
Chemoreceptors detect changes in:
- pCO₂, pO₂, and pH.
✅ Central Chemoreceptors:
- Located in medulla oblongata.
- Respond mainly to increased pCO₂ and H⁺ concentration in CSF.
✅ Peripheral Chemoreceptors:
- Located in carotid bodies and aortic bodies.
- Respond to low pO₂, high pCO₂, and low pH.
3.Physiology of Muscles Contraction
🔄 Excitation-Contraction Coupling: Sequence of Events in Muscle Contraction
The physiology of skeletal muscle contraction involves electrical, chemical, and mechanical events, coordinated in a stepwise fashion:
✅ 1. Nerve Impulse and Neuromuscular Transmission
- An action potential (electrical signal) is generated in a motor neuron.
- The nerve impulse reaches the neuromuscular junction (NMJ).
- This causes the release of acetylcholine (ACh) into the synaptic cleft.
- ACh binds to nicotinic receptors on the sarcolemma of the muscle fiber.
- This leads to depolarization of the sarcolemma, initiating an action potential in the muscle.
✅ 2. Action Potential Propagation
- The muscle action potential travels along the sarcolemma and down the T-tubules (transverse tubules).
- It reaches the sarcoplasmic reticulum (SR) and triggers the release of calcium ions (Ca²⁺) into the sarcoplasm.
✅ 3. Calcium Binding and Exposure of Binding Sites
- Ca²⁺ binds to the troponin-C subunit on the thin (actin) filament.
- This causes tropomyosin to move away, exposing myosin-binding sites on actin.
✅ 4. Cross-Bridge Formation (Actin-Myosin Interaction)
- Energized myosin heads (with ADP + Pi) attach to the exposed sites on actin → forming a cross-bridge.
✅ 5. Power Stroke
- ADP and Pi are released → Myosin head pivots and pulls the actin filament toward the center of the sarcomere → muscle shortens.
✅ 6. Detachment of Myosin Head
- A new ATP molecule binds to the myosin head → Cross-bridge breaks → Myosin detaches from actin.
✅ 7. Reactivation of Myosin Head
- ATP is hydrolyzed into ADP + Pi → Myosin head is “re-cocked” and ready for the next cycle.
✅ 8. Termination of Contraction
- Acetylcholinesterase breaks down ACh → Ends muscle excitation.
- Ca²⁺ is actively pumped back into the sarcoplasmic reticulum by calcium ATPase.
- Tropomyosin re-covers the myosin-binding sites → Muscle relaxes.
4.Functions of Stomach
The stomach is a muscular, J-shaped organ of the digestive system, located in the upper left quadrant of the abdominal cavity, between the esophagus and the duodenum. It acts as both a temporary storage organ and a site for chemical and mechanical digestion, especially of proteins. Its functions are mediated by gastric glands, muscle layers, nervous system, and hormonal control, making it a dynamic organ essential for nutrient processing and body defense.
✅ Major Functions of the Stomach
🔹 1. Temporary Storage of Ingested Food
- The rugae (folds) of the stomach wall allow expansion to hold up to 1.5–2 liters of food and liquid.
- Storage allows time for controlled release into the small intestine.
- Prevents sudden overload of the duodenum, ensuring proper enzymatic digestion downstream.
🔹 2. Mechanical Digestion (Churning & Mixing)
- Peristaltic contractions of the muscularis externa (with three layers: longitudinal, circular, oblique) mix food with gastric juice.
- Converts solid food into a semi-liquid mass called chyme.
- Facilitates homogenization of food, enhancing enzyme access and digestion.
🔹 3. Chemical Digestion of Proteins
- Chief cells in gastric glands secrete pepsinogen, an inactive enzyme.
- Parietal cells secrete hydrochloric acid (HCl) which:
- Converts pepsinogen → pepsin (active form)
- Denatures ingested proteins
- Provides acidic pH (1.5–3.5) optimal for enzyme activity
- Pepsin begins protein hydrolysis into peptides.
🔹 4. Secretion of Gastric Juice
- Average daily secretion: 2 to 3 liters.
- Gastric juice contains:
- HCl: Acidic environment for digestion, antimicrobial action
- Pepsinogen: Protein-digesting enzyme precursor
- Intrinsic Factor: Essential for vitamin B₁₂ absorption
- Mucus: Protective alkaline layer
- Water and electrolytes
🔹 5. Secretion of Intrinsic Factor
- Intrinsic factor, secreted by parietal cells, is vital for:
- Binding vitamin B₁₂ in the stomach
- Enabling its absorption in the ileum
- Deficiency leads to pernicious anemia – a megaloblastic anemia.
🔹 6. Controlled Gastric Emptying
- Pyloric sphincter regulates the release of chyme into the duodenum.
- Prevents sudden acid surge in the small intestine.
- Gastric motility is influenced by:
- Gastrin (stimulates emptying)
- Enterogastric reflex, CCK, and secretin (inhibit emptying)
🔹 7. Limited Absorption
Though most absorption occurs in the small intestine, the stomach absorbs:
- Water (especially when dehydrated)
- Alcohol
- Certain lipid-soluble drugs (e.g., aspirin, NSAIDs)
- Caffeine and other stimulants
🔹 8. Secretion of Protective Mucus
- Mucous neck cells produce thick, alkaline mucus.
- Forms a protective barrier between the epithelium and acidic gastric contents.
- Prevents self-digestion (gastric ulceration).
- Maintained by prostaglandins, which are inhibited by NSAIDs (leading to ulcers).
🔹 9. Hormonal and Neuroendocrine Functions
- Enteroendocrine (G) cells secrete gastrin:
- Stimulates HCl and pepsinogen secretion
- Promotes gastric motility
- Other gastric hormones:
- Histamine: Stimulates parietal cells via H₂ receptors
- Somatostatin: Inhibits gastric secretion
- Ghrelin: Appetite-stimulating hormone, secreted by gastric mucosa during fasting
🔹 10. Defense Against Infections
- HCl inactivates and kills ingested pathogens.
- Acts as a first line of defense in the gastrointestinal tract.
- Maintains gut flora balance by inhibiting harmful bacterial overgrowth.
Q.8 Write Very Short notes. (Any Three)(06 Marks)
1.List out the hormones secreted by Pituitary gland
🔵 1. Anterior Pituitary (Adenohypophysis)
Major hormones:
- Growth Hormone (GH)
- Stimulates body growth, especially bones and muscles.
- Thyroid-Stimulating Hormone (TSH)
- Stimulates the thyroid gland to produce T₃ and T₄.
- Adrenocorticotropic Hormone (ACTH)
- Stimulates the adrenal cortex to release cortisol.
- Follicle-Stimulating Hormone (FSH)
- Stimulates follicle development in ovaries and spermatogenesis in testes.
- Luteinizing Hormone (LH)
- Triggers ovulation and progesterone secretion in females; testosterone production in males.
- Prolactin (PRL)
- Stimulates milk production in lactating females.
- Melanocyte-Stimulating Hormone (MSH)(in some species and infants)
- Influences skin pigmentation.
🔴 2. Posterior Pituitary (Neurohypophysis)
These hormones are synthesized in the hypothalamus and stored/released by the posterior pituitary:
- Antidiuretic Hormone (ADH or Vasopressin)
- Promotes water reabsorption in kidneys; regulates blood pressure.
- Oxytocin
- Stimulates uterine contractions during labor and milk ejection during breastfeeding.
2.Define reflex action
A reflex action is a rapid, automatic, and involuntary response of the body to a specific stimulus that occurs without conscious effort. It is an essential protective mechanism that helps the body respond quickly to harmful or sudden changes in the environment.
Reflex actions are carried out through a neural pathway called the reflex arc, which allows the body to bypass the brain and produce an immediate response via the spinal cord or brainstem.
They are:
- Fast (usually completed in milliseconds)
- Involuntary (does not require thought)
- Predictable (same stimulus → same response)
- Protective in function (prevent injury or maintain homeostasis)
3.Process of micturition
🔁 Phases of Micturition:
✅ 1. Storage Phase (Filling Phase):
- Urine formed by kidneys is transported to the urinary bladder via the ureters.
- The bladder fills gradually and expands due to detrusor muscle relaxation (smooth muscle in bladder wall).
- The internal urethral sphincter remains contracted (involuntary control).
- The external urethral sphincter remains contracted voluntarily (skeletal muscle).
- Controlled by the sympathetic nervous system (T11–L2):
- Inhibits detrusor contraction
- Promotes sphincter contraction (urine retained)
✅ 2. Voiding Phase (Emptying Phase or Micturition Reflex):
- As bladder fills (~300–500 mL), stretch receptors in the bladder wall are activated.
- Signals sent via pelvic nerves (parasympathetic S2–S4) to spinal cord and brain.
- Parasympathetic response triggers:
- Contraction of detrusor muscle
- Relaxation of internal sphincter
- If the external urethral sphincter is voluntarily relaxed, urination occurs.
- Micturition center in the pons (brainstem) coordinates voluntary control.
4.Write two functions of gall bladder.
✅ 1. Storage of Bile
- The gall bladder stores bile produced by the liver.
- It can hold about 30–50 mL of concentrated bile.
- Bile is stored here until it is needed for digestion.
✅ 2. Concentration and Release of Bile
- The gall bladder concentrates bile by removing water and electrolytes.
- When fatty food enters the small intestine, the hormone cholecystokinin (CCK) stimulates the gall bladder to contract and release bile into the duodenum.
- Bile helps in the digestion and absorption of fats.
