ENGLISH-MIDWIFERY AND GYNECOLOGICAL NURSING 10/02/2025 PAPER SOLUTION-11- (3RD YEAR) (Done)-UPLAOD
ENGLISH-MIDWIFERY AND GYNECOLOGICAL NURSING 10/02/2025 PAPER SOLUTION- NO.11
MIDWIFERY AND GYNECOLOGICAL NURSING 10/02/2025 PAPER SOLUTION NO.11
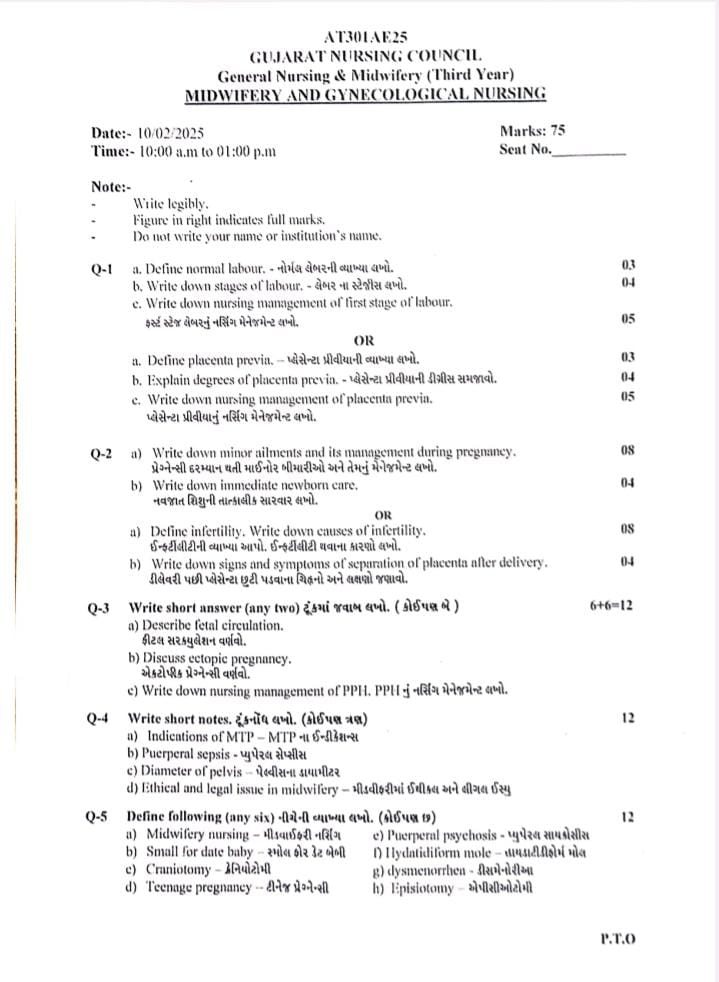
Q-1
a. Define normal labour.- નોર્મલ લેબરની વ્યાખ્યા લખો.03
- Labor:
The series of events that occur in the genital organs to bring the viable product of conception out of the uterus (womb) into the outside world through the vagina is called “labor”. - A woman who is in labor is called a “parturient”.
- And the process of giving birth is called “parturition”.
- Normal labor is also called eutoshia.
- Normal labor is said to be when the following criteria are fulfilled.
- 1) The onset of labor should be spontaneous and at term (37 to 48 weeks).
- 2) The fetus should be in vertex presentation (the occiput of the fetus’s head should be in the lower part of the uterine cavity and the fetus’s chin should be tucked against its chest).
- 3) The duration of labor should not be long (i.e. if the mother is a primary gravida, the average duration of labor should be 12 hours and if the mother is a multipara, the average duration of labor should be 6 hours)
- 4) The birth should be natural with minimal assistance.
- 5) There should be no complications that affect the health of the mother and the baby.
b. Write down stages of labour. – લેબર ના સ્ટેજીસ લખો.04
- Stages of Labor:
- The stages of labor are divided into four stages.
- 1) First Stage of Labor,
- 2) Second Stage of Labor,
- 3) Third Stage of Labor,
- 4) Fourth Stage of Labor
- 1) First Stage of Labor (Cervical Stage):
- The first stage of labor is the initial phase of childbirth. In which the cervix gradually opens (dilates) and thins (effaces). Due to which the baby can pass from the uterine cavity into the birth canal (vagina). In which regular and rhythmic uterine contractions are observed and the frequency, intensity and duration of uterine contractions gradually increase.
- The first stage of labor begins with the onset of true labor pains and lasts until the cervix is fully dilated (10 cm). This stage is also called the “cervical stage”.
- The first stage of labor is further divided into 3 stages:
- The time period of the first stage is:
Primigravida:=12-16 hours, and
Multigravida:=6-8 hours, - The first stage of labor is divided into three phases.
- 1) Latent phase,
- 2) Active phase,
- 3) Transitional phase
- 1) Latent phase,
- The latent phase is also known as “prodromal labor” or “pre-labor”.
- In this stage, cervical dilation of 1-4 cm occurs.
- In this phase, contractions are repeated every 15-30 minutes and last for 15-30 seconds.
- In this phase, the mother is talkative (able to talk).
- 2) Active phase,
The active phase is also known as the dilation phase. - In this second phase, the cervix is dilated by 5-7 cm. And contractions are repeated every 3-5 minutes and last for 45-60 seconds. In this stage, the mother feels restless.
- 3) Transitional phase
- In the transitional phase, the dilation of the cervix is 8-10 cm.
- Contractions are repeated every 2-3 minutes and last for 60 to 90 seconds.
- Overall, the first stage of labor is a critical period in which the cervix opens, the uterus prepares for delivery by providing proper positioning of the baby in the uterine cavity. During this stage, continuous monitoring by health care providers is important to improve the condition and well-being of the mother and fetus.
- 2) Second Stage of Labor (Expulsion of Fetus): The period from full dilation of the cervix to the birth of the baby through the birth canal is called the second stage of labor.
- Its duration is:
In primigravida: 1-2 hours and
In multigravida: It lasts for 20-30 minutes. - The second stage of labor is further divided into two phases:
- 1) Propulsive phase,
- 2) Expulsive phase.
- 1) Propulsive phase: The propulsive phase starts from the full dilation of the cervix until the presenting part of the fetus descends to the pelvic floor (+4, +5 stages).
- 2) Expulsive phase: This is the expulsive phase until the baby is completely expelled from the uterine cavity with the mother’s bearing down efforts.
- 3) Third stage of labor (expulsion of placenta):
- This stage is the period from the expulsion of the baby to the expulsion of the placenta and membranes.
- Its time duration is 15 minutes in primigravida and multigravida
- 4) Fourth stage of labor (observation stage):
- After the birth of the baby, the observation stage is called the 4th stage of labor. During this stage, the general condition of the mother and the condition of the newborn and the behavior of the uterus are carefully monitored.
- Its time duration is 1 hour.
- Thus, the time duration of all four stages of total labor (1st stage + 2nd stage + 3rd stage + 4th stage) is 13-15 hours in primigravida and 6-8 hours in multigravida.
c. Write down nursing management of first stage of labour.ફસ્ર્ટ સ્ટેજ લેબરનું નર્સિંગ મેનેજમેન્ટ લખો.05
- Nursing Management of First Stage of Labor:
- The first stage of labor is a critical period in which the cervix opens, the uterus prepares for delivery by providing proper positioning of the baby in the uterine cavity. During this stage, continuous monitoring by health care providers is important to improve the condition and well-being of the mother and fetus.
- Nursing management of the first stage of labor involves comprehensive care. Its aim is to support the mother physically, emotionally and educationally and to closely monitor the progress of labor.
- 1) Assessment
- Properly monitor the progress of labor, the condition of the mother and the condition of the fetus.
- Inquiry about when labor pains started.
Inquiry about any kind of leakage or leakage.
Conduct proper examination of the mother.
Conduct proper obstetric examination.
Conduct vaginal examination of the mother.
Properly check the mother’s antenatal records.
Maternal assessment
Regularly monitor the mother’s vital signs, such as,
Temperature,
Pulse,
Respiration,
And properly assess blood pressure. - Properly assess the intensity, frequency, duration, and resting tone of the pregnant woman’s uterine contractions by palpation method.
- Properly assess cervical dilation and effacement through vaginal examination.
Properly and accurately document and chart cervical dilation and effacement. - Fetal assessment
- Continuously monitor fetal heart rate through electronic fetal monitoring (EFM).
- Properly assess fetal heart rate pattern.
- Properly document fetal heart rate and properly document any abnormalities.
- 2) Support and comfort measures
- Provide the mother with a proper comfortable position that can increase the mother’s comfort level and also progress the labor process such as walking, standing, sitting, etc.
- Advise the mother on relaxation techniques such as deep breathing exercises and mind diversion therapy etc.
- Provide emotional support, reassurance and psychological support to the mother to reduce her anxiety.
- 3) Hydration and Nutrition
- Advise the mother to consume a moderate amount of fluids.
- Continuously monitor the mother’s intake output chart to properly maintain the mother’s hydration status.
- Advise the mother to consume adequate amounts of light food and fluids to maintain the mother’s nutritional status.
- Such as plain water,
- Salty lemon water,
- Soup, and fruit juice etc.
- 4) Apply antiseptic and aseptic dressings properly on the genital area to maintain cleanliness.
- 5) Education and Communication Provide education to the mother and her supporters about the mother’s condition and progress of labor.
- 6) Bowel Care Provide proper enemas to clear the mother’s bowel and increase uterine contractions.
- 7) Bladder Care Advise pregnant women to empty their bladder frequently because a full bladder inhibits contractions.
- 8) Documentation
- Assess and properly document the condition of the mother and fetus and properly maintain the partograph.
- Properly document all assessments, interventions, observations in the mother’s medical record.
- Properly record maternal vital signs, uterine contraction patterns, cervical dilation and effacement, fetal heart sounds, and labor progress.
- 9) Collaboration and Advocacy
- Collaborate with other health care personnel such as obstetricians, midwives, and nurses to ensure that decisions are made about the mother’s condition.
- Thus, by properly managing the first stage of labor, complications in the mother and fetus can be prevented and the first stage of labor can be properly maintained.
OR
a. Deline placenta previa. પ્લેસેન્ટા પ્રીવ્યાની વ્યાખ્યા લખો.03
- When the placenta partially or completely implants near or above the internal os of the lower segment of the uterus, it is called “placenta previa.” 1/3 of cases of antepartum hemorrhage are due to placenta previa.
b. Explain degrees of placenta previa. પ્લેસેન્ટા પ્રીવ્યાની ડીગ્રીસ સમજાવો.04
- Types of Placenta Previa:
There are four types of placenta previa based on the degree of extension of the placenta into the lower segment of the uterine cavity. - 1) Type I (Lateral Placenta Previa),
- 2) Type II (Marginal Placenta Previa),
- 3) Type III (Incomplete Placenta Previa),
- 4) Type IV (Complete Placenta Previa)
- 1) Type I (Lateral Placenta Previa):
- In this type, the major part of the placenta is attached to the upper segment but only the lower margin enters the lower segment but does not reach the os.
- 2) Type II (Marginal Placenta Previa):
- In this type, the placenta only reaches the margin of the internal os but does not cover it.
If the placenta is anterior, vaginal birth is possible. Blood loss is average. The risk of fetal hypoxia is higher than that of maternal shock. - 3) Type III (Incomplete Placenta Previa):
The placenta partially covers the internal os, not centrally. Bleeding occurs when the cervix begins to efface and dilate in late pregnancy, due to lower stretching. - 4) Type IV (Complete Placenta Previa):
In this, the placenta covers the internal os even when it is fully dilated. Severe hemorrhage occurs, requiring a cesarean section to save the life of the mother and baby.
C. Write down nursing management of placenta previa. પ્લેસેન્ટા પ્રીવીયાનું નર્સિંગ મેનેજમેન્ટ લખો.05
- Management of placenta previa:
- Provide adequate antenatal care to the patient to improve the health status of the mother.
- To confirm the type of placenta previa, perform an ultrasound at 20 weeks and then repeat ultrasound at 34 weeks.
- Ask the pregnant woman to take bed rest and then gently palpate the uterus for tenderness and tone.
- Properly assess the amount of blood loss.
- Color of bleeding and complete blood count (CBC) test should be done.
- Provide the patient with inj. Morphine 15 mg IM as per hospital policy and prescription.
- Properly assess the amount of blood loss in the client.
- Properly note the client’s vital signs such as temperature, pulse, respiration, blood pressure.
- Properly assess the client for anemia.
- Regularly and frequently check the fetal heart sound.
- Perform abdominal examination of the pregnant woman, then note the fetal heart sound and properly note whether there is any tenderness present in the uterus.
- Do not perform vaginal examination in the condition of placenta previa as it may increase bleeding.
- Properly monitor the pregnant woman for continuous bleeding or if it stops in between.
- If the pregnant woman needs it, arrange for further well-equipped hospital shift to a hospital with blood transfusion facility available, cesarean section facility and neonatal care unit.
- If the client has a condition of hemorrhage, start intravenous dextrose normal saline drips.
- Advise the client to avoid stress and advise him to take complete bed rest.
- When the client is admitted to the hospital, follow the following treatment such as,
- Give immediate attention,
- Then plan properly what kind of treatment is required.
- In the immediate assessment, the amount of blood loss, general condition, pallor, pulse rate and blood pressure should be properly noted.
- Blood samples should be sent to the laboratory immediately for cross-matching and assessment of hemoglobin level.
- Start infusion of normal saline to the patient.
- After cross-matching of blood, keep the blood ready to hand for transfusion.
- Perform gentle abdominal palpation to assess whether any active bleeding is present.
- Formulation of line of treatment:
- Provide proper treatment according to the condition.
- Proper estimation of hemoglobin level should be done and it should be 10 gm or more.
- Expectant treatment should be provided till 37 weeks are completed.
- Termination is performed in case of any of the following conditions such as:
Recurrent hemorrhage,
Dead fetus,
Congenital malformation of fetus,
Intrauterine growth retardation (IUGR),
In such conditions, termination is performed. - After admission to the hospital, specific treatment is started. For example,
Vaginal examination is performed in the operation theatre after proper preparation for caesarean section. - After examination, artificial rupture of membranes is done, then oxytocin is started, and then delivery is conducted as per the condition.
- If the labor process is progressing satisfactorily without any bleeding, then perform vaginal delivery.
- If bleeding is continuous, perform cesarean section on the pregnant woman.
- If the baby is malformed or dead, assess its presentation, if it is breech presentation, perform ventouse delivery, and if it is breech, perform breech delivery.
Q-2
a) Write down minor ailments and its management during pregnancy. પ્રેગ્નેન્સી દરમ્યાન થતી માઇનોર બીમારીઓ અને તેમનું મેનેજમેન્ટ લખો.08
- System:
- Nausea and Vomiting:
- Nausea and vomiting are very common in primigravida and are especially common when the woman wakes up in the morning.
- Nausea and vomiting are caused by hormones like HCG, Oestrogen, Progesterone.
- Nausea and vomiting are usually more common in primigravida and first trimester.
- Management
- Dietary Changes
- Advise the mother to eat dry toast, biscuits, salty crackers and protein-rich food when she wakes up in the morning.
- Advise the mother to eat small and frequent meals.
- Advise the mother to eat low-fat foods.
- Advise the mother to avoid fried foods and spicy foods.
- Advise the mother to take proper antiemetic medication.
- Constipation
- Constipation is the most common problem in pregnancy. Constipation is mainly seen during the second and third trimester.
- Constipation is caused by the effect of progesterone, decreased intestinal tone and mobility, decreased physical activity,
- Constipation is caused by the intake of iron supplements,
- Constipation is caused by the pressure of the gravid uterus on the colon.
- Management
- Advise the mother to take high-fiber foods.
- Advise the mother to consume adequate amounts of vegetables and fruits.
- Advise the mother to drink 6-8 glasses of water throughout the day.
- Advise the mother to drink a glass of water in the morning to activate bowel movements.
- Advise the mother to eat frequent, small, and low-fat meals.
- Advise the mother to exercise regularly.
- Advise the mother to take small amounts of milk of magnesia.
- Acidity and heartburn
- Acidity and heartburn are common during pregnancy due to relaxation of the esophageal sphincter.
- It is usually seen in mothers in greater numbers during the second and third trimesters.
- Acidity and Heartburn Acidity and heartburn are mostly seen due to increased progesterone levels, decreased intestinal size, and displacement of the stomach due to enlarged uterus.
- Management
- Advise the mother to eat in small and frequent amounts.
- Advise the mother not to overeat.
- Advise the pregnant woman not to lie down immediately after eating. Remain in a sitting upright position for at least 30 minutes after eating.
- Advise the mother to avoid fatty and spicy foods.
- Advise the mother to sleep in a reclining position with the support of five to six pillows.
- Advise the mother to perform tailor-made sitting exercises.
- Advise the mother to take antacid medication prescribed by the health care personnel.
- Bleeding from gums, glossitis and gingivitis
. Bleeding from gums can occur due to increased blood supply due to high levels of progesterone during pregnancy. - Management
- Advise the mother to use a soft toothbrush.
- Advise the mother to maintain oral hygiene.
- Advise the mother to take vitamin-B complex, green leafy vegetables, yeast, eggs and cheese.
- 2) Circulatory System
- Dizziness and Fainting
- It is mainly caused by the relaxation of the muscles of the blood vessels due to the effect of progesterone.
- It subsides due to the increase in blood volume.
- Later, the pressure of the gravid uterus on the inferior vena cava causes less blood supply to the heart.
- Management Advise the mother to sleep on her back less in the last month. And advise the mother to avoid standing for long periods.
- Dizziness
- Dizziness can also occur during pregnancy and due to this, balance can be lost and the possibility of falling is also seen more.
- It is usually caused due to cardiovascular changes during pregnancy and low blood sugar levels and anemia.
- Management
- Advise the mother to take adequate rest.
- Advise the mother to avoid standing for long periods.
- Varicose veins
- The condition of varicose veins is usually seen more during the second and third trimesters of pregnancy.
- Varicose veins mainly develop in the lower extremities and vulva during pregnancy and hemorrhoids in the rectum also occur due to obstruction of venous return by the pregnant uterus.
- Management
- Advise the mother to wear supportive shoes.
- Elastic crepe bandages and elevation of the limb while moving in varicose veins provide relief in symptoms.
- Advise the mother to avoid prolonged sitting and standing positions.
- The condition of varicocele is relieved after delivery.
- Complications like bleeding or prolapse are seen in hemorrhoids. Advise to use mild laxatives to keep the bowel soft and
- Advise to apply local hydrocortisone ointment and replacement of prolapsed piles is necessary. Avoid surgical treatment as the condition reduces after delivery.
- Ankle edema
- Ankle edema is usually seen during the second and third trimester.
- It is usually seen due to vasodilation,
- venous stasis and increased intrauterine venous pressure.
- Management
- The mother should be properly assessed for excess fluid retention or weight gain, as fluid retention can also be caused by pregnancy-induced hypertension (PIH).
- Advise the mother to keep her legs elevated at least twice a day.
- Advise the mother to wear supportive stockings.
- Advise the mother to avoid prolonged sitting or standing in one position.
- Diuretics should not be given to pregnant women as long as possible because it subsides on its own with rest and elevation of the limbs in the case of ED.
- In physiological ED or orthostatic ED, no treatment is required.
- 3) Musculoskeletal System
- Backache
- 50% of the problems during pregnancy are backache.
- Backache can occur at any stage of pregnancy but is mostly seen during the second and third trimesters of pregnancy.
- Backache is seen due to physiological changes such as joint ligament laxity (relaxin and estrogen), weight gain, hyperlordosis, pelvic anterior tilt etc.
- Other causes of backache include faulty posture, high-heeled shoes, muscular spasm, constipation, and urinary tract infections.
- Management
- Advise the mother to take proper rest.
- Advise the mother to use correct body mechanics and improve body posture.
- Advise the mother to keep the legs elevated while resting.
- Advise the mother not to wear high-heeled shoes.
- Advise the mother to perform pelvic rocking and abdominal and breathing exercises.
- A well-fitted pelvic girdle belt that corrects lumbar lordosis while walking.
- Advise the mother to sleep on a firm mattress.
- Back muscle massage, analgesics and rest can help reduce pain due to muscle spasms.
- Leg cramps
- Leg cramps usually occur during the second and third trimesters of pregnancy.
- Leg cramps can usually be caused by an altered calcium-phosphorus balance.
- And can also be caused by pressure from the uterus.
- Leg cramps are more common at night.
- Leg cramps can also be caused by calcium and vitamin B12 deficiency.
- Management
- Advise the mother to massage the legs properly.
- Advise the mother to do regular exercise, especially walking.
- Advise the mother to apply local heat to the area of pain in the leg.
- Advise the mother to take vitamin B1 and calcium orally.
- 4) Genito-urinary system
- Vaginal discharge
- Vaginal discharge is seen from the first trimester to the third trimester.
- It is usually seen due to hyperplasia of the vaginal mucosa and increased mucus production.
- Management:-
- Advise the mother to maintain proper cleansing and hygiene.
- Advise the mother to wear cotton undergarments and avoid tight undergarments.
- If there is any condition of vaginal infection, apply vaginal application of metronidazole and miconazole as per the doctor’s advice.
- Urinary urgency and frequency:-
During the 12th week of pregnancy, due to the pressure of the uterus and during the 3rd trimester of pregnancy, frequency of urination is seen due to the pressure of the fetal head, which gets relieved after delivery. - Management:-
- Advise the mother to take adequate amount of fluid intake during the day.
- Advise the mother to take limited amount of fluid intake in the evening.
- Advise the mother to void at regular intervals.
- Advise the mother to sleep in a side lying position while sleeping at night.
- Advise the mother to wear a peri-nial pad if necessary.
- Advise the mother to perform eagle exercises.
- 5) Integumentary System:-
- Itching:- Itching occurs in the body due to stria gravidarum, poor personal hygiene, heat, race, minor skin diseases.
- Management:-
- Advise the mother to bathe regularly and daily.
- Advise the mother to apply calamine lotion.
- Advise the mother to apply talcum powder to provide a soothing effect to the mother’s skin.
- Advise the mother to maintain proper hygiene conditions.
- 6) Nervous system:-
- Carpal tunnel syndrome:- Fluid retention causes pressure on the ED and median nerve, causing numbness and pins and needles sensation in the fingers and hand.
- Management:-
Advise the mother to reduce salt intake in the diet. - Advise the mother to keep her hands under the pillow.
- Insomnia and headache:- Insomnia and headache are usually seen more during the second and third trimesters.
- Management:-
Take a bath with properly warm water at night while sleeping.
Advise the mother to sleep in a cool and well ventilated room.
Advise the mother to sleep in a lateral position with the support of a pillow.
Advise the mother to share her anxiety and fear. - Thus, the minor ailments seen during pregnancy and their management are as follows.
b) Write down immediate newborn care. નવજાત શિશુની તાત્કાલીક સારવાર લખો.04
- Immediate Newborn Care:
- Immediate Newborn Care involves properly assessing and stabilizing the newborn.
- Immediate Newborn Care is crucial for the fetus to transition from intrauterine life to extrauterine life.
- Goals of Immediate Newborn Care
- 1) To establish, maintain, and provide support for the newborn’s respiration.
- 2) To prevent the newborn from overheating and hypothermia.
- 3) To prevent the newborn from getting infections.
- 4) To provide safety to the newborn and prevent it from injury.
- 5) To provide immediate treatment for any actual or potential problem in the newborn by early identification. Immediate newborn care is provided.
Immediate Newborn Care
- 1) Establishment of Respiration
When the newborn is received, immediately patent the newborn’s airway and clear the airway properly. Due to which the newborn can breathe effectively.
As soon as the newborn’s head is turned, wipe the mouth and nose and suck the mouth and nose, due to which the newborn can breathe properly. Sucking should be done first in the mouth and then in the nose, due to which secretions can be prevented from being aspirated. - 2) Initiation of Cry: Normally 99% of newborns cry immediately and spontaneously after delivery, this cry is known as a good sign for the newborn’s breathing.
- If the newborn does not cry properly, then follow the following steps:
- a) If the baby does not cry spontaneously or if the cry is weak, then lightly simulate the baby to cry.
- b) To stimulate the baby’s cry, instead of slapping his bottom, lightly rub the soles of his feet. After removing the newborn’s secretions, stimulate the baby to start his cry.
- C) Newborn’s cry is usually loud and husky and if there is any abnormal cry as follows, then the newborn should be properly monitored such as,
- •>High pitch cry: = due to hypoglycemia and increased intracranial pressure,
Weak cry: = prematurity,
Hosacry: = laryngeal strider - 3)Care of cord
- Cord care is an important immediate care of the newborn.
- The newborn’s cord should be clamped within 30 seconds of birth and then cut properly.
- After the newborn is delivered, the newborn should be placed on the mother’s abdomen.
- Then the cord should be clamped properly from two opposite sites using a cord clamp.
- The first clamp should be placed 5 cm from the umbilicus, then the second clamp should be placed 2.5 cm from the first clamp.
- Then cut the cord properly between the two clamps.
- Do not apply anything to the cord, let it dry and fall naturally.
- The cord naturally falls off within seven to ten days after birth.
- Prevent the cord from getting wet with water and urine.
- If any discharge or bleeding is present in the cord, immediately assess the cord clamp and then loosen it properly.
- If the following signs and symptoms are seen from the cord, then report it immediately, such as,
- Foul odor coming from the cord,
- No discharge,
- Redness around the cord,
- The cord is wet,
- The cord does not fall down in 7-10 days,
- Inflammation,
- Fever etc.
- 4) Maintain position of the newborn
The newborn is usually prone to choke, cough and gag during the first 12-18 hours after birth. Therefore, the newborn should be provided with a proper position. - In which, the fitters should be provided with a proper side-lying position so that the mucus can be removed and drained.
- 5) Identification and Banding
After the baby is born, put a proper identification band on the baby so that the baby can be properly identified. - 6) Eye Care
Clean the eyes of the newborn properly from the inner canthus to the outer canthus with sterile gauze.
If necessary, apply erythromycin or tetracycline eye ointment to the lower lid of the eyes. - 7) Attachment and Warmth (Bonding)
After the baby is born, place the baby on the mother’s abdomen so that bonding with the mother occurs and proper skin to skin contact can occur so that the mother and baby can be attached and the baby can be prevented from hypothermia. - 8) APGAR Score
The APGAR score is the most important part of immediate newborn care.
The APGAR score is assessed at 1 minute and then at 5 minutes after birth.
In the APGAR score, - A:= Appearance (skin color),
P:=Pulse (heart rate),
G:=Grimes (reflux irritability),
A:=Activity (muscle tone),
R:=Respiration (respiratory efforts)
are assessed.
The total score of the APGAR score is 0-10. - APGAR score at 1 minute after birth:
- If the Apgar score is 7-10, it is considered normal, i.e. no depression, in which the baby is provided with normal post-delivery routine care.
- If the APGAR score is between 4-6, it indicates mild depression, in which the child requires assistance for breathing.
- If the APGAR score is between 0-3, it indicates severe depression in which the child needs resuscitation.
- APGAR score at 5 minutes after birth:
- If the APGAR score is between 7-10, it is considered normal, but if the Apgar score is below 7, the baby needs to be monitored for another half hour.
- 9) Vitamin K:
The intestine of a newborn is sterile for some time after birth, that is, the bacteria responsible for manufacturing vitamin K are not present in its intestine, due to which the newborn cannot manufacture vitamin K, that is, vitamin K is responsible for a clotting factor. If this vitamin K is not present in the body of the newborn, then there is a possibility of clotting in the newborn, so as a prophylactic measure, artificial injection of vitamin K is provided to the newborn baby. - Dose:=
In pre-term:=0.5 ml,
Full term:= 1 mg.
Intra muscularly (IM) is provided on the vastus lateralis (lateral anterior). - Thus, essential newborn care after birth is provided as follows.
Q-3 Write short answer (any two) ટૂંકમાં જવાબ આપો (કોઈપણ બે)6+6= 12
a) Describe fetal circulation. ફીટલ સરક્યુલેશન વર્ણવો.
- Fetal Circulation
- Fetal circulation is a unique circulatory system that is present in the developing fetus. It is formed to fulfill the needs of oxygen and nutrients while the fetus is in the womb (uterus).
- A separate fetal circulation in the embryo starts during the 16th post-fertilization day.
- The fetal heart starts beating from the 21st day of fertilization. Also, the fetus in the uterus receives oxygen and nutrients from the placenta because its lungs and alimentary tract are functional. Therefore, fetal circulation is the circulation through which the fetus receives oxygen and nutrients from the placenta for its survival.
- Features of Fetal Circulation
- 1) Umbilical Cord: The umbilical cord contains two umbilical arteries and one umbilical vein.
- Umbilical Artery: The umbilical artery transfers fetal waste products and deoxygenated blood from the fetus to the placenta.
- Umbilical Vein: Transfers oxygenated blood and nutrients from the placenta to the fetus.
- 2) Placenta:
- The placenta acts as an interface between the circulatory systems of the mother and fetus.
- The placenta acts as an exchange of nutrients, oxygen, and waste products between maternal blood and fetal blood.
- As the placenta delivers oxygen and nutrients to the fetus through the umbilical vein and receives the fetus’s deoxygenated blood and waste products through the umbilical artery to the placenta.
- 3) Ductus Venosus (Vein to Vein):
- The ductus venosus is a channel through which oxygenated blood passes from the umbilical vein to the inferior vena cava bypassing the liver and digestive organs.
- Due to which oxygenated blood can reach the fetus’s brain and heart in adequate quantities.
- 4) Foramen ovale (oval opening):
- The foramen ovale is a fetal cardiac structure that is a small opening in the septum between the right atrium and the left atrium of the heart that acts as a shunt between the right atrium and the left atrium.
- This opening (shunt) allows blood in the right atrium to bypass the fetal lungs and shift to the left atrium.
- This shunt is important because the lungs of the fetus are functional during intrauterine life and are filled with fluid, due to which the fetal lungs are not able to do their work properly.
- 5) Ductus arteriosus (artery to artery):
- The ductus arteriosus is a fetal vascular connection that is a communication (sant) between the pulmonary artery and the aorta.
- Due to this ductus arteriosus, blood from the right ventricles bypasses the lungs and flows into the systemic circulation through the SANT.
- Fetal circulation:
- Oxygen diffuses from the maternal blood into the choriodecidual space (placenta), so the placental villi and vessels unite to form the umbilical vein.
- From the placenta, the umbilical vein travels through the umbilical cord to the fetus.
- The umbilical vein passes through the umbilical wall and forms two branches of the umbilical vein.
- A branch of the umbilical vein joins the portal vein of the fetus’s liver to provide nutrients and oxygen to the fetus’s liver. Blood is collected from the liver through the hepatic vein and enters the inferior vena cava.
- The 2nd branch of the umbilical vein is a major vessel called the ductus venosus. It connects directly to the inferior vena cava.
- The oxygenated blood in the umbilical vein mixes with the deoxygenated blood from the lower legs and trunk in the inferior vena cava.
- But the ductus venosus does not seriously affect the oxygen content of the blood.
- The blood now enters the right atrium through the inferior vena cava.
- Then the blood in the right atrium passes into the left atrium through the foramen ovale, a hole between the right atrium and the left atrium.
- Then the blood in the left atrium passes into the left ventricle through the mitral valve.
- Then the blood comes out of the heart through the aorta in the left ventricle.
- The coronary vessels of the aorta (coronary artery, brachiocephalic trunk (right common carotid artery, right subclavian artery, left common carotid artery, left subclavian artery)) supply blood to the branches of the heart and head.
- Blood from the head and neck enters the right atrium through the superior vena cava and crosses the inferior vena cava and enters the right ventricle through the tricuspid valve.
- Most of the blood from the right ventricle passes through the pulmonary artery, bypassing the lungs (since the lungs are inactive), and passes through the ductus arteriosus (a passage between the pulmonary artery and the aorta) into the descending aorta to supply blood to the abdominal organs and lower extremities.
- The descending aorta then forms the right and left internal iliac arteries.
- The right and left internal iliac arteries are again divided into two hypogastric arteries.
- The hypogastric artery enters the umbilical cord to form two umbilical arteries.
- These two umbilical arteries return deoxygenated blood to the placenta.
- Fetal blood circulates rapidly and is constantly renewed.
- The mean cardiac output in the fetus is 350 ml/kg/min.
b) Discuss ectopic pregnancy. એકટોપીક પ્રેગ્નેન્સી વર્ણવો.
- Definition
When a fertilized ovum implants and develops outside the normal endometrial cavity, it is called an ectopic pregnancy. Anatomical site of implantation of ectopic pregnancy: Tubal pregnancy is more common, normally occurring in the right fallopian tube than the left fallopian tube. The ampulla of the fallopian tube is the most common site of implantation of an ectopic pregnancy. If the ectopic pregnancy occurs in the isthmus of the fallopian tube, it is considered a dangerous site, which can also lead to tubal rupture. - Etiology
- Due to certain factors, the migration of the fertilized ovum into the uterine cavity is delayed.
- Due to factors that provide a favorable environment for the fertilized ovum to implant in the tubo-mucosa.
- Due to hormonal factors,
- Due to birth defects,
- Due to medical conditions.
- Risk factors
- Previous ectopic pregnancy,
- Previous surgery in the uterine tube,
- Tubal reconstructive surgery,
- Failure to use an intrauterine contraceptive device,
- Certain types of infections such as,
- Pelvic inflammatory disease,
- Chlamydia infection,
- Gonorrhea etc.,
- History of infertility,
- Assisted reproductive techniques (ART),
- Infertility treatment such as,
- In vitro fertilization (IVF),
- Maternal age above 35 years,
- Previous induced abortion,
- History of endometriosis.
- Signs and Symptoms:
- The signs and symptoms of ectopic pregnancy are classified into two types:
- 1) Acute type
- 2) Chronic type
- 1) Acute type
- In acute type of ectopic pregnancy, triad symptoms are seen such as:
- Amenorrhea,
- Sharp colicky abdominal pain,
- Vaginal bleeding
- Nausea and vomiting,
- Palence usually depends on the amount of hemorrhage.
- Signs and symptoms of shock are seen,
- such as,
- Rapid and weak pulse,
- Blood pressure fall,
- Extremities become cold and clammy.
- Abdomen feels tense, tense and tender on physical examination.
- Abdominal tenderness.
- Bowel distension.
- Tubal rupture and tubal abortion are accompanied by massive intraperitoneal hemorrhage.
- Cullen sign positive: Dark bluish peri-umbilical ecchymosis due to hemoperitoneum.
- Vaginal area appears pale during pelvic examination.
- Uterus appears to float in water.
- 2) Chronic type
- Tubal mole is common in chronic type
- It is not detected in the beginning.
- Its signs include anemia, bladder irritability, tachycardia and temperature increase.
- Amenorrhea,
- Abdominal pain,
- Vaginal bleeding that occurs shortly after the onset of abdominal pain, which may be dark in color.
- Bladder irritation, such as dysuria, frequency of urination, retention of urination.
- Body temperature increases.
- On examination, the patient appears ill,
- Pallor is observed,
- Pulse rate increases even at rest.
- Abdominal tenderness on the affected side.
- A mass-like structure is felt in the lower abdominal area, which is irregular.
- Extreme tenderness of the cervix.
- Diagnostic Evaluation:
- History Collection,
Physical Examination,
Blood Examination,
Coldocentesis (Taping of Pouch of Douglas),
Sonography,
Assessment of hCG Level,
Laparoscopy,
Laparotomy,
Dilatation and Curettage,
Transvaginal Ultrasonography (USG) - Management of Ectopic Pregnancy
- The management of ectopic pregnancy is divided into two types,
such as, - 1) Acute Ectopic Pregnancy Management,
- 2) Chronic Ectopic Pregnancy Management
- Principles of Management
- To prevent complications in the mother.
- In case of ectopic pregnancy, immediate laparotomy should be performed because the fertilized ovum cannot survive outside the uterine cavity, so the tissue is removed to prevent serious complications.
- 1) Acute ectopic pregnancy management:
- Provide anti-shock treatment to the patient and prepare for urgent laparotomy.
- Advise the patient to lie flat on the bed.
- Provide inj.morphine 15 mg (IM) to the patient.
- Start 5% dexrose drip if required.
- Arrange blood for blood transfusion.
- If blood is not available or not available and the patient is in a state of shock, it is still essential to perform laparotomy.
- The fallopian tube containing the gestational sac is removed through laparotomy and partially by surgical procedure.
- Perform salpingectomy. In which step,
- Refer the patient to the hospital,
- Advise the patient to lie down on a flat bed.
- If the patient is collapsed, raise the bed towards the foot end.
- Assess the patient’s hemoglobin level.
- If the patient needs blood transfusion, keep the blood ready.
- Administer adequate intravenous fluids to the patient until blood is available
- Ex:=Ringer lactate,
- Dexran.
- For salpingectomy, perform a quick laparotomy on the patient under general anesthesia.
- Then make an incision on the line of the intra-umbilical incision.
- Then recognize the uterus and continuously suction out the blood.
- Then both the sites of the uterus are assessed so that the gestational sac in the fallopian tube can be identified.
- Then the affected tube and ovary are observed.
- Then the clamps are applied.
- Then the gestational sac and the affected fallopian tube are removed with or without the ovary.
- The clamps are replaced by a chromic catgut ligature which should not be tightened.
- Then adequate hemostasis is ensured.
- When the patient wants to sterilize the other fallopian tube, tubectomy or salpingectomy is performed for hydrosalpinx.
- Whereas, if a blood clot is present freely in the peritoneal cavity, it should be aspirated as possible.
- Then wash the pelvic cavity properly with normal saline and close the abdomen quickly.
- In case of pregnancy in the interstitial part of the tube, only the gestational sac should be removed but sometimes for better hemostasis, quick subtotal hysterectomy is necessary.
- 2) Chronic ectopic pregnancy management:
- Admit all cases of chronic ectopic pregnancy to the emergency department.
- Keep the patient under proper observation.
- Carry out all investigations of the patient properly.
- Control bleeding quickly and effectively.
- Keep blood transfusion available.
- Provide intravenous infusion to the patient as prescribed.
- Advise the patient to perform laparotomy as early as possible.
- Prepare the patient for laparoscopy or laparotomy.
- Then advise to perform salpingectomy.
- In ectopic pregnancy, medical management includes removal of the ectopic pregnancy by making an incision on the fallopian tube or by removing a section of the tube.
- If the patient has a suppurative pelvic hematocele, provide proper antibiotics and drain the pus.
- Remove the tubal mole by laparotomy and partial incision on the fallopian tube.
- Provide proper management to the patient after surgery.
- In medical treatment, provide systemic methotrexate 50 mg IM to the patient.
- Rh antigen does not sensitize in positive Rh women. Provide Anti D gamma globulin -50 micrograms to the patient immediately after the operation to prevent isoimmunization.
- Provide care to bring the patient out of shock in acute rupture of the fallopian tube.
- Maintain the patient’s vital sign intake output chart properly.
- Provide antibiotic medication to the patient.
- Encourage the patient to move early.
- Advise the patient to take proper follow-up.
c) Write down nursing management of PPH. PPH નું નર્સીન્ગ મેનેજમેન્ટ લખો.
- Monitoring of Vital Signs of the Patient
- The most important nursing care during PPH is to regularly monitor the patient’s vital signs – such as blood pressure, pulse rate, respiratory rate and temperature. This allows an estimate of the patient’s hemodynamic status and immediate action can be taken.
- Accurate Assessment of Bleeding
- Make an accurate observation of the amount of bleeding. Blood loss should be measured by weighing the pad or using a mop. If there is excessive bleeding, it is considered as severe PPH and immediate intervention is required.
- Uterine Tone Assessment
- The main cause of PPH is atony, i.e. lack of stimulation in the uterine muscles. For this, check the uterine tone by palpating the fundus. If the uterine muscles feel soft, then uterine massage should be started immediately so that the tone increases and bleeding stops.
- Administration of Uterotonics
- Uterotonic drugs like Oxytocin, Misoprostol, Ergometrine and Carboprost should be given so that uterine contractions occur and bleeding decreases. The drug dosage and route (IV/IM/Oral) should be given as per the medical order.
- Intravenous Fluid Resuscitation
- Use crystalloid fluids such as Normal Saline or Ringer Lactate to correct blood volume loss. Shock can be prevented by giving high volume fluids at a fast rate.
- Blood Transfusion:
- Packed RBCs (Packed Red Blood Cells), Fresh Frozen Plasma (Fresh Frozen Plasma) and Platelets should be transfused wherever necessary. Monitor hemoglobin levels and keep a crossmatch unit ready.
- Patient Positioning and Oxygen Therapy
- Place the patient in a flat position or Trendelenburg position so that blood supply is more towards the brain and heart. Oxygen therapy should be given at 6-8 L/min through a face mask.
- Catheterization and Urine Output Monitoring
- Monitor the patient’s urine output through a Foley Catheter. Oliguria or anuria may be a sign of hemodynamic instability.
- Psychological Support to the Patient:
- After PPH, the patient may be fearful, anxious, or in mourning. It is very important for the nurse to explain and reassure the patient and his family.
- Communication with the Doctor and Multidisciplinary Team
- PPH is an emergency, so it is necessary to inform the doctor immediately, maintain communication with the obstetrics, anesthesia, and lab technician teams.
- Record Keeping and Documentation
- Accurate documentation of bleeding, medications, vital signs, and interventions is essential for reassessment and legal purposes.
- Thus, in cases of PPH, if nursing management is implemented quickly and appropriately, the patient’s life can be saved.
Q-4 Write short notes. ટૂંકનોંધ લખો. (કોઈપણ ત્રણ) 12
a) Indications of MTP- MTP ના ઇન્ડીકેશન્સ
- MTP stands for Medical Termination of Pregnancy, which is a medical procedure to perform a legally permissible abortion. The Government of India has allowed abortion under certain specified conditions under the MTP Act, 1971. The main purpose of this procedure is to protect the life, health and mental condition of the patient, and to prevent the birth of a child whose life may be extremely difficult or incurable.
- The following medical and legally permissible purposes (Indications) for performing MTP are very clear and important:
- Therapeutic Indication
- When abortion becomes necessary for the life of the patient or continuation of the pregnancy poses a serious risk to her physical or mental health.
- For example: Cardiac Disease, Severe Hypertension, Eclampsia, Renal Failure, Severe Mental Illness etc.
- If the patient has any serious medical condition due to which carrying the pregnancy may prove fatal.
2.Eugenic Indication
- When it is confirmed that the fetus has a serious physical or brain distortion.
- For example: Anencephaly, Down Syndrome, Spina Bifida, Hydrocephalus etc.
- In this situation, abortion can prevent the tragic consequences in the lives of both the patient and the fetus.
- Humanitarian Indication
- When the pregnancy is the result of rape or intimate relationships.
- In such cases, abortion saves the patient from mental trauma and social suffering.
- This indication is especially applicable for minor girls.
- Social Indication
- When pregnancy is not suitable for the patient’s social, economic or family situation.
- Example: The patient is very young, already has more children, does not get the support of the partner, or has serious domestic financial problems.
- In situations where it is not possible for the patient to raise more children, abortion can be a healthy option for her.
5.Failure of Contraceptive Method
- When a pregnancy occurs despite the patient and her husband using an approved contraceptive method.
- This indication is especially applicable to married women.
- The purpose of abortion in this situation is to prevent the patient from experiencing psychological and social stress due to an unwanted pregnancy.
- MTP is a scientifically, medically and legally approved method that allows the patient to have a safe abortion at the right time. The decision behind each indication is taken keeping in mind the medical suitability and the patient’s best interests. Informed consent of the patient, medical counseling and supervision of a specialist doctor are essential in this process.
b) Puerperal sepsis – પ્યુપેરીયલ સેપ્સીસ
- Puerperal Sepsis
- Puerperal sepsis is an infection of the genital tract that occurs as a complication of delivery. “Puerperal sepsis is an infection of the genital tract during the first 6 weeks of delivery or abortion.”
- Etiology:
- Endometritis,
- Endomyometritis,
- Endoparametritis,
- Or a combination of all three.
- Causative organism: Aerobic:
- Staphylococcus pyogenes,
- E. coli,
- Klebsiella,
- Pseudomonas,
- and non-hemolytic, streptococcus,
- Staphylococcus aureus,
- Anaerobes: These include:
- Anaerobes
- Bacteroides fragilis
- Clostridium welchii
- Clostridium tetani
- Predisposing factors:
- Resistance General or local conditions,
- Conditions that increase the multiplication and virulence of the organism,
- Due to the introduction of the organism from outside,
- Increasing prevalence of resistant organisms to antibiotics and chemotherapy.
- Malnutrition and anemia,
- Pre-eclampsia (antipartum factor),
- Due to premature rupture of membranes,
- Sexual intercourse during late pregnancy,
- Due to chronic debilitating illness,
- Introduction of sepsis into the upper genital tract during internal examination after rupture of membranes or during manipulative delivery.
- Dehydration and ketoacidosis during labor,
- Traumatic operative delivery,
- Hemorrhage – APH or PPH,
- Due to retained bits of placental tissue and membranes,
- Placenta previa.
- Mode of infection:
- Puerperal sepsis is specifically a wound infection. In this, the placental site, genital tract laceration or caesarean section wound can become infected in the following ways.
- Endogenous:
The organism is present in the genital tract before delivery and enters the genital organs through the bloodstream or the patient himself. - Autogenous:
Here the organisms are present elsewhere in the body and are transmitted to the genital organs through the bloodstream or droplet infection. - Streptococcus beta-haemolyticus, E-coli, C.L. Welchi and Staphylococcus migrate from septic throat, pharyngeal and skin infections.
- Exogenous:
- Exogenous infection is an infection transmitted from some other source outside the patient. The organism is introduced by attendants, usually doctors or nurses. Infection may be dust-borne or droplet-borne, during internal examinations, or through contaminated linen or blankets. Nowadays, Staphylococcus pyogenes is common.
- Symptoms and signs:
- Local infection (wound infection):
- The primary site of infection is the perineum, vagina, cervix, and uterus.
- Infection in a local wound may cause the area to become red, swollen, and pus to form.
- Mild fever, malaise, and headache may occur, and in acute infection, rigors with high fever may occur.
- Uterine Infection:
- In mild infection, temperature and pallor increase.
- Local discharge is abundant and foul smelling.
- Uterus is tender and subinvoluted.
- In advanced infection, high fever, rigors, lochia are scanty and odorless, uterus may be tender, soft and subinvoluted.
- Extrauterine:
- Pelvic tenderness (pelvic peritonitis),
- Tenderness in the phoenix (parametritis),
- Abscess in the pouch of Douglas (pelvic abscess) etc. may be seen.
- The patient may present with pelvic peritonitis (pyrexia, lower abdominal pain, tenderness, pus),
- general peritonitis,
- thrombophlebitis,
- septicemia, etc.
- Diagnostic Evaluation:
- History Collection,
- Antenatal, Intranatal and Postnatal History
- Physical Examination,
- Imaging Studies,
- Pelvic CT Scan,
- MRI (Magnetic Resonance Imaging),
- Laboratory Tests:
- Urine Examination,
- WBCs (White Blood Cell Count),
- Cervical Canal Swab,
- Intra-uterine Sampling of Uterine Cavity Discharge,
- Blood Culture.
- Management:
- Antenatal
Improve the nutritional status of the mother and eliminate any infection in the body if present. - Surgical asepsis during intranatal
delivery, screening for group B streptococcus in high risk patients,
Antibiotics - Postpartum:
Initially one week of aseptic precautions, isolation and restrict visitors. - Treatment:
- Maintain isolation in general care, provide adequate fluid, calories, antibiotics and oral iron.
- Properly maintain the patient’s intake output chart.
- Properly monitor the patient’s vital signs and maintain a local discharge chart.
- Surgical treatment: Drainage of pus and pain in perineal wound.
- Heparin IV 7-10 days in septic pelvic thrombophlebitis.
- Debridement in colpotomy in pelvic abscess, laparotomy in unresponsive peritonitis.
- Provide treatment if patient is in septic shock.
c) Diameter of pelvis પેલ્વીસ ના ડાયામીટર
- Introduction:
Pelvic diameters are of great importance in obstetrics, as they determine whether the baby can pass normally through the pelvic passage. The pelvis is divided into three main parts: Inlet, Cavity, and Outlet. Each part has different diameters that are important. - 🔴 1. Pelvic Inlet Diameters
True (Anatomical) Conjugate
➤ From sacral promontory to upper margin of pubic symphysis - 🔹 Length: 11 cm
- 🔸 Gujarati: સેક્રમના અલેટેટ પુબિક સિમ્ફિસ brim
- 🔹 Length: 13 cm
- 🔸 Gujarati: Oblique Diameter
- ➤ From one sacroiliac joint to iliopectineal eminence on opposite side
- 🔹 Length: 12 cm
- 🟡 2. Pelvic Cavity Diameters – Pelvic Cavity Diameters
- Anteroposterior Diameter (Mid-cavity)
- ➤ From midpoint of pubic symphysis to junction of 2nd and 3rd sacral vertebrae
- 🔹 Length: 12 cm
- Transverse Diameter (Bi-spinous diameter)
- ➤ Between ischial spines
- 🔹 Length: 10.5 cm
- 🟢 3. Pelvic Outlet Diameters – Pelvic Outlet Diameters
- Anteroposterior Diameter (True Conjugate of Outlet)
- ➤ From tip of coccyx to lower border of pubic symphysis
- 🔹 Length: 11.5 to 13 cm (depends on coccyx mobility)
- Transverse Diameter (Bi-ischial diameter)
- ➤ Between inner surfaces of ischial tuberosities
- 🔹 Length: 11 cm
d) Ethical and legal issue in midwifery.મીડવીફરી મા લીગલ અને ઇથીકલ ઇસ્યુસ.
- Ethical Issues of Midwifery:
- 1) Autonomy and Informed Consent:
- Respect for Autonomy: Midwives should respect women’s rights to make informed decisions about their care.
- Informed Consent: It is important to ensure that women understand their options, risks, and benefits of interventions.
- 2) Non-Malfunction (Do No Harm): Midwives should strive to avoid actions that may harm the mother or baby during childbirth.
- 3) Beneficence (Promoting Mood): Midwives have a duty to actively promote the well-being of the mother and baby during the process of pregnancy and childbirth.
- 4) Justice: All women should be provided with adequate, equitable and proper health care facilities regardless of their socioeconomic status and background.
- 5) Confidentiality: It is important to maintain the privacy and confidentiality of patient information in health care practices.
- 6) Cultural Sensitivity and Respect: Midwives should be aware of and respect the cultural, spiritual and religious beliefs of the women they care for.
- Legal Issues in Midwifery:
- 1) Problems in Medication.
- 2) Failure and Inadequate Client Monitoring.
- 3) Failure to Adequately Assess the Client.
- 4)Failure to report change in the patient.
- 5)Abortion.
- 6)Nursing care of new born.
- 1)Problem in medication: Nurse is authorized for administration of medication which has many allegations related to medication.
- Ex: Improper client identification,
Failure to monitor dosage, time and side effects of medication. - 2) Failure and Inadequate Client Monitoring:
- The nurse has to monitor the client at appropriate time intervals according to the condition of the client. During labor and delivery, they have to monitor both the mother and the baby. Monitoring them is the legal responsibility of the nurse to prevent complications in the mother and child during the prenatal, natal and postnatal periods.
- 3) Failure to Adequately Assess the Client:
- In all specialty areas, nurses should have higher level assessment skills.
- Proper assessment of the client’s health status such as prenatal assessment, fetal monitoring and assessment of labor progress is essential.
- Failure to properly assess the client can lead to missed complications and inappropriate care for the patient.
- 4) Fair to Report Changes in the Patient:
- When the nurse assesses the client’s condition and notices any changes in the client’s condition, the nurse should immediately notify the consulting physician. As a patient advocate, failure to notify the physician can delay the client’s care and may result in injury and problems for the client.
- And it can also lead to legal issues.
- 5) Abortion:
- Legal issues regarding the role of the midwife in abortion care can vary widely depending on local laws and regulations. This also involves legality, informed consent and adherence to protocol.
- The nurse has the right to refuse to assist in abortion but not the right to stop it.
- 6) Nursing Care of Newborn:
- It is important to provide immediate nursing care to the newborn, which involves assessment of the newborn, proper monitoring of the newborn, and proper stabilization of the newborn.
- There are some legal requirements to provide nursing care to the newborn, such as properly identifying the infant-mother pair through fingerprints, foot prints, and wrist bands, and taking a blood sample for phenylketonuria (PKU) testing if necessary.
- Providing a clear airway is standard of practice.
- Camping the umbilical cord.
- Applying antibiotics.
- Keeping the infant warm and minimizing stress during delivery are some of the things that need to be done.
- Resuscitation equipment should be kept in the delivery room.
- The nurse should keep records of all the events of the delivery.
- Fulfilling legal requirements through careful documentation in the delivery room.
- When standard care is not provided to the newborn, complications can arise and legal issues can also arise due to this.
Q-5 Define following (any six) – નીચેની વ્યાખ્યા લખો( કોઇ પણ છ )12
a) Midwifery nursing- મીડવાઇફરી નર્સિંગ
- Midwifery Nursing is a specialized field of nursing that is the professional and clinical care and services provided by trained midwives to care for the health of mothers and newborns during pregnancy, childbirth, and the postpartum period. This service includes components such as antenatal care, intranatal care, postnatal care, fetal monitoring, normal vaginal delivery, and occasional medical intervention. The main goal of the midwife in midwifery nursing is to provide a supportive environment for both mother and baby to deliver safely, comfortably, and naturally.
b) Small for date baby – સ્મોલ ફોર ડેટ બેબી
- A small for date baby is a newborn whose birth weight is less than the 10th percentile for gestational age. Whether a newborn is born full-term, preterm, or post-term, their weight is less than what it should be for their gestational age.
C) Craniotomy – ક્રેનીયોટોમી
- Craniotomy is a destructive surgery. The operation to expel the fetus from the uterine cavity by making a perforation in the head of the fetus, reducing the contents, and making a craniotomy is called craniotomy. This operation is performed when obstructed labor occurs due to a dead fetus in cephalic presentation.
d) Teenage pregnancy – ટીનેજ પ્રેગ્નેન્સી
- Teenage pregnancy is a pregnancy that occurs in women between the ages of 13 and 19. It usually involves young women who are still in their adult years and as a result, they may face unique social, emotional, and health challenges. Adult pregnancy can affect the mother’s educational, economic stability, and health, as well as the health and development of the child. Teenage mothers are at risk of complications such as gestational hypertension, cephalopelvic disproportion, anemia, and nutritional deficiencies. They also have a higher incidence of sexually transmitted diseases. Infants born to teenage mothers may experience complications such as prematurity, birth asphyxia, and low birth weight.
c) Puerperal psychosis – પ્યુપેરલ સાઇકોસીસ
- Puerperal psychosis or postpartum psychosis is a term that covers a group of mental illnesses in which a woman suddenly develops psychotic symptoms after childbirth. In which the woman may experience irritability, mood swings, hallucinations.
- Puerperal psychosis is a severe form of mental illness. It occurs in about 1-2 cases in 1000 women, which begins as early as the first 48 – 72 hours of delivery and most often within 2-3 weeks. It may be due to hormonal changes (such as the sudden drop in estrogen levels after birth).
d) Hydatidiform mole – હાઇડાટીડીટીફોમ મોલ
- Hydatidiform mole (H.Mole) is also called vesicular mole. It is an abnormal condition of the placenta. In which some degenerative and some proliferative changes occur in the young chorionic villi and due to this, a cluster (cluster-like shape) is formed in the cyst. And because it resembles a hydatid cyst, it is called hydatidiform mole or vesicular mole. When the chorionic villi transform into a mass of translucent vesicles, it forms a structure like a bunch of grapes, which is called hydatidiform mole.
e) dysmenorrhea – ડીસમેનોરીયા
- Painful menstruation is called dysmenorrhea. OR Dysmenorrhea is the medical term for painful menstruation, typically involving lower abdominal cramps before or during the menstrual period.
f) Episiotomy – એપીસીયોટોમી
- A surgically planned incision is made on the perineum and posterior vaginal wall during the second stage of labor, called an “episiotomy.” An episiotomy is performed to widen the vaginal opening for spontaneous or manipulative easy and safe delivery of the fetus. An episiotomy is performed to reduce excessive stretching and rupture of the perineal muscles and fascia, and to reduce stress and strain on the fetal head.
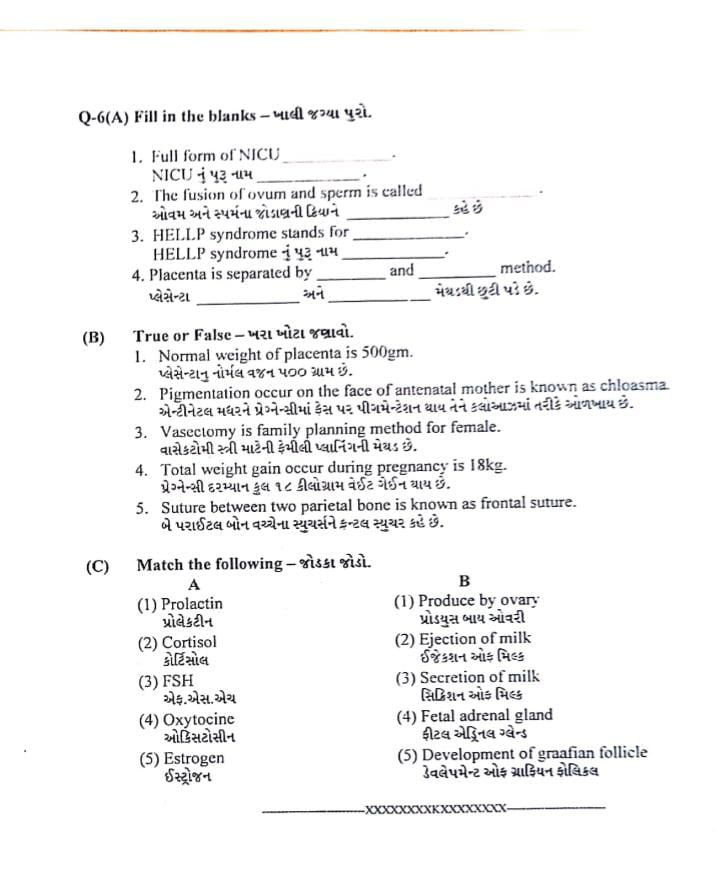
Q-6(A) Fill in the blanks – ખાલી જગ્યા પુરો.
1.Full form of NICU………
NICU નું પુરૂ નામ……… : Neonatal Intensive Care Unit
NICU નું પૂર્ણ નામ: નીઓનાટલ ઇન્ટેન્સિવ કેર યુનિટ
2.The fusion of ovum and sperm is called…….
ઓવમ અને સ્પર્મના જોડાણની ક્રિયાને………કહે છે: Fertilization
ઓવમ અને સ્પર્મના જોડાણની ક્રિયાને: ફર્ટિલાઇઝેશન કહે છે
3.HELLP syndrome stands for…………
HELLP syndrome નું પુરૂ નામ……..: Hemolysis, Elevated Liver enzymes, and Low Platelet count
HELLP Syndrome નું પૂર્ણ નામ: હીમોલિસિસ, એલિવેટેડ લિવર એન્ઝાઇમ્સ અને લોઉ પ્લેટલેટ કાઉન્ટ
4.Placenta is separated by ……..and ……..method. પ્લેસેન્ટા ……..અને ……..મેથડથી છુટી પડે છે: Schultze and Duncan method
પ્લેસેન્ટા Schultze અને Duncan પદ્ધતિથી છૂટી પડે છે
(B) True or False – ખરા ખોટા જણાવો.
1.Normal weight of placenta is 500gm. પ્લેસેન્ટાનું નોર્મલ વજન ૫૦૦ ગ્રામ છે : ✅ True (સાચું)
👉 સરેરાશ પ્લેસેન્ટાનું વજન 500 ગ્રામ જેટલું હોય છે.
2.Pigmentation occur on the face of antenatal mother is known as chloasma. એન્ટીનેટલ મધરને પ્રેગ્નેન્સીમાં ફેસ પર પીગમેન્ટેશન થાય તેને કલોઆઝમાં તરીકે ઓળખાય છે : ✅ True (સાચું)
👉 ચહેરા પર થતી ગાઢ પીગમેન્ટેશનને “Chloasma” અથવા “Mask of Pregnancy” કહે છે.
3.Vasectomy is family planning method for female. વાસેકટોમી સ્ત્રી માટેની ફેમીલી પ્લાનિંગની મેથડ છે : ❌ False (ખોટું)
👉 Vasectomy પુરુષ માટેની family planning surgery છે. સ્ત્રી માટેના વિકલ્પમાં tubectomy આવે છે.
4.Total weight gain occur during pregnancy is 18kg. પ્રેગ્નેન્સી દરમ્યાન કુલ ૧૮ કીલોગ્રામ વેઈટ ગેઈન થાય છે : ❌ False (ખોટું)
👉 સામાન્ય રીતે કુલ વેઈટ ગેઈન 11.5–16 કિલો જેટલું હોય છે (સરેરાશ 12-13 kg).
5.Suture between two parietal bone is known as frontal suture. બે પરાઈટલ બોન વચ્ચેના સ્યુચર્સને ફ્રન્ટલ સ્યુચર કહે છે : ❌ False (ખોટું)
👉 બે Parietal bones વચ્ચેનો સ્યુચર Sagittal suture કહેવાય છે. Frontal suture એ Frontal bones વચ્ચે હોય છે.
(c) Match the following – જોડકા જોડો.
A B
(1) Prolactin પ્રોલેકટીન (1) Produce by ovary પ્રોડયુસ બાય ઓવરી
(2) Cortisol કોર્ટિસોલ (2) Ejection of milk ઈજેકશન ઓફ મિલ્ક
(3) FSH એફ.એસ.એચ (3) Secretion of milk સિક્રિશન ઓફ મિલ્ક
(4) Oxytocine ઓકિસટોસીન (4) Fetal adrenal gland ફીટલ એડ્રિનલ ગ્લેન્ડ
(5) Estrogen ઈસ્ટ્રોજન (5) Development of graafian follicle ડેવલેપમેન્ટ ઓફ ગ્રાફિયન ફોલિકલ
🔶 (C) ANSWER 🔶
| A | B | Answer |
|---|---|---|
| (1) Prolactin – પ્રોલેક્ટિન | (3) Secretion of milk – દૂધ ઉત્પન્ન કરવું | ✅ (1 → 3) |
| (2) Cortisol – કોર્ટિસોલ | (4) Fetal adrenal gland – ભ્રૂણની એડ્રિનલ ગ્રંથી | ✅ (2 → 4) |
| (3) FSH – એફ.એસ.એચ | (5) Development of Graafian follicle – ગ્રાફિયન ફોલિકલનો વિકાસ | ✅ (3 → 5) |
| (4) Oxytocin – ઓક્સિટોસિન | (2) Ejection of milk – દૂધ ની બહાર નીકળવાની ક્રિયા | ✅ (4 → 2) |
| (5) Estrogen – ઈસ્ટ્રોજન | (1) Produced by ovary – અંડાશય દ્વારા ઉત્પન્ન થાય છે | ✅ (5 → 1) |
Final Matching:
1 → 3
2 → 4
3 → 5
4 → 2
5 → 1
