ENGLISH-MIDWIFERY AND GYNECOLOGICAL NURSING 30/07/2018 PAPER SOLUTION NO.10- (3RD YEAR) (Done)-UPLOAD
ENGLISH-MIDWIFERY AND GYNECOLOGICAL NURSING 30/07/2018 PAPER SOLUTION NO.10

MIDWIFERY AND GYNECOLOGICAL NURSING 30/07/2018 PAPER SOLUTION NO.10
Q-1
a. Define true labour pain. ટ્રુ લેબર પેઇનની વ્યાખ્યા આપો.03
- True labor pains are rhythmic, progressive, and involuntary contractions in the uterus of the patient, leading to dilation and effacement of the cervix, paving the way for the actual delivery of the fetus.
- This pain usually begins in the lower back and radiates to the lower abdomen. These contractions are regular, their duration increases, and their intensity gradually increases.
- True labor pains do not subside with changing positions or resting. They are caused by the natural release of the hormone oxytocin and the contraction of the myometrium.
- During true labor pain, microscopic changes are seen in the patient’s cervix, such as dilation, effacement, and bloody mucus discharge from the cervix – called a bloody show.
- This pain is physically and mentally challenging for the patient, but it is a sign that the patient is now about to enter active labor.
b. Write signs of true labour pain. ટ્રુ લેબર પેઇનના ચિન્હો લખો.04
- Signs of True Labor Pain:
- 1) Painful uterine contraction
- 2) Shaw
- 3) Progressive dilatation and effacement of cervix
- 4) Formation of “bag of water”
- 1) Painful uterine contraction:
- Throughout pregnancy, painless Braxton Hicks contractions occur with simultaneous hardening of the uterus. The character of these contractions changes, becoming more powerful, intermittent, and associated with more pain.
- The pain is usually felt in the front of the abdomen and radiates to the back. Contractions are the first sign of labor pain. Initially, a woman experiences one or two contractions per hour which increase in frequency (initially these are tolerable).
- Contractions may become more intense over a period of 6-8 hours. After that, the active phase of labor begins. In this, contractions become more severe and occur every 2-3 minutes and last for 45 to 60 seconds. During this period, it is very difficult for a woman to relax because the intense nature of the pain is accompanied by rapid dilation of the cervix.
- Furthermore, contractions do not occur very often but are more intense. Eventually, a woman experiences intense contractions between 60-90 seconds. And more regularly, they occur every 2-3 minutes. This is the stage of labor called hard labor where the cervix dilates up to 10 cm.
- 2) Shaw:
- In pregnancy, the operculum (cervical mucus plug) forms and comes out as a bloodstained mucoid discharge a few hours before or with labor, called “Shaw”.
- Rupture of the capillary vessels of the cervix and stretching of the lower uterine segment cause blood to ooze from the raw decidual surface.
- 3) Progressive dilatation and effacement of cervix:
- The effective force of the first stage is painful uterine contractions. Due to these painful uterine contractions, the cervix progressively dilates and effaces.
- The cervix dilates to about 10 cm.
- The muscle fibers surrounding the internal os are pulled upward by the retracted upper segment, thereby shortening the cervix and then merging with the lower uterine segment and becoming part of it, and gradually effacement of the cervix occurs.
- 4) Formation of “bag of water”:
- Due to dilatation of the lower uterine segment, the chorion detaches. The loose part of this fluid bulges into the dilating internal os. The amniotic fluid in front of the head is fixed in the cervix which is called fore water. Fore water helps in effacement of the cervix and early dilatation of the os. Fore water maintains a uniform pressure in the uterus during uterine contractions, thus providing some protection to the fetus and placenta. In this way, the pressure during contractions does not come on fore water which is called general fluid pressure.
- For example: When the membranes are intact, the pressure of uterine contraction comes on the fluid and remains uniform throughout the uterus.
c. Write management of first stage of labour. ફસ્ટ સ્ટેજ ઓફ લેબરનું મેનેજમેન્ટ લખો. 05
- Nursing Management of First Stage of Labor: The first stage of labor is a critical period in which the cervix opens, the uterus prepares for delivery by providing proper positioning of the baby in the uterine cavity. During this stage, continuous monitoring by health care providers is important to improve the condition and well-being of the mother and fetus.
- Nursing management of the first stage of labor involves comprehensive care. Its aim is to support the mother physically, emotionally and educationally and to closely monitor the progress of labor.
- 1) Assessment
Properly monitor the progress of labor, the condition of the mother and the condition of the fetus. - Inquiry about when labor pains started.
Inquiry about any kind of leakage or leakage.
Conduct proper examination of the mother.
Conduct proper obstetric examination.
Conduct vaginal examination of the mother.
Properly check the mother’s antenatal records.
Maternal assessment
Regularly monitor the mother’s vital signs, such as,
Temperature,
Pulse,
Respiration,
And properly assess blood pressure. - Properly assess the intensity, frequency, duration, and resting tone of the pregnant woman’s uterine contractions by palpation method.
- Properly assess cervical dilation and effacement through vaginal examination.
Properly and accurately document and chart cervical dilation and effacement. - Fetal assessment
Continuously monitor fetal heart rate through electronic fetal monitoring (EFM).
Properly assess fetal heart rate pattern.
Properly document fetal heart rate and properly document any abnormalities. - 2) Support and comfort measures
Provide the mother with a proper comfortable position that can increase the mother’s comfort level and progress the labor process, such as walking, standing, sitting, etc.
Advise the mother on relaxation techniques such as deep breathing exercises and mind diversion therapy etc.
Provide emotional support, reassurance and psychological support to the mother to reduce her anxiety. - 3) Hydration and Nutrition
Advise the mother to consume a moderate amount of fluids.
Continuously monitor the mother’s intake output chart to properly maintain the mother’s hydration status.
Advise the mother to consume adequate amounts of light food and fluids to maintain the mother’s nutritional status.
Such as plain water,
salty lemon water,
soup, and fruit juice etc. - 4) Antiseptic and aseptic
Apply antiseptic dressings properly to the genital area to maintain cleanliness. - 5) Education and communication
Provide education to the mother and her supporters about the mother’s condition and progress of labor. - 6) Bowel care
Properly provide enemas to the mother to clear the mother’s bowels and increase uterine contractions. - 7) Bladder care
Advise pregnant women to empty their bladder frequently because a full bladder inhibits contractions. - 8) Documentation
Assess and properly document the condition of the mother and fetus and properly maintain the partograph.
Properly document all assessments, interventions, observations in the mother’s medical record.
Properly record maternal vital signs, uterine contraction patterns, cervical dilation and effacement, fetal heart sounds and labor progress. - 9) Collaboration and Advocacy
Collaborate with other health care personnel such as obstetricians, midwives and nurses to make informed decisions about the mother’s condition.
Thus, by properly managing the first stage of labor, complications in the mother and fetus can be prevented and the first stage of labor can be properly maintained.
OR
a. Define spermatogenesis સ્પરમેટોજીનેસીસની વ્યાખ્યા આપો.03
“The development of spermatids from primordial male germ cells and their subsequent differentiation into spermatozoa is called spermatogenesis. That is, the development and maturation of sperm is called spermatogenesis.“
b. Describe development of Placenta. પ્લેસેન્ટાના ડેવલપમેન્ટનું વર્ણન કરો. 04
- Introduction:
The placenta is an important temporary organ that performs important functions such as nutrition, gaseous exchange, vitamins, and waste product removal between the fetus and the mother. The placenta develops early in pregnancy and is fully developed by full term. - Developmental Stages of Placenta:
- Formation of Trophoblast:
- After fertilization, a blastocyst is formed, from which the trophoblast develops from the outer cell mass.
- The trophoblast divides into two levels:
- Cytotrophoblast: The inner layer, in which cell division occurs at a high rate.
- Syncytiotrophoblast: The outer layer, which is responsible for implantation in the maternal endometrium.
- Development of Chorionic Villi:
- Chorionic Villi are formed from the trophoblast.
- Initially, Primary Villi are formed, followed by Secondary Villi and then Tertiary Villi.
- These villi act as the functional unit of the placenta.
- Formation of Intervillous Space:
- Syncytiotrophoblast affects the maternal blood vessels and forms Lacunae.
- This lamina later transforms into the intervillous space, in which the mother’s blood flows.
- Maternal and Fetal Circulation Establishment:
- The mother’s blood enters the intervillous space through the uterine arteries.
- Two umbilical arteries and one umbilical vein enter the placenta for the fetal blood.
- Gas, nutrient and metabolic exchange takes place through the placental membrane.
- Final Maturation:
- By the 12th week, the placenta is fully developed.
- By full term, the placenta weighs about 500-600 grams and its diameter is about 15-20 cm.
- Functions of Placenta:
- Nutrition Transfer
- Gaseous Exchange
- Endocrine Function (Hormone Secretion) – such as Human Chorionic Gonadotrophin (hCG), Human Placental Lactogen (hPL), Estrogen and Progesterone
- Metabolic Waste Removal
- Immunological Protection
C. Write about circulation through the placenta. પ્લેસેન્ટા દ્વારા થતા સરકયુલેશન વિશે લખો 05
- Introduction:
The placenta is an important organ for the exchange of nutrition, oxygen, carbon dioxide, hormones and waste products between the mother and the fetus. Placental circulation ensures selective exchange of essential elements between the mother and the fetus by preventing direct contact between their blood. - There are two main divisions of Placental Circulation:
- Maternal Circulation:
The blood filled with oxygen and nutrients from the patient’s uterine arteries reaches the intervillous space of the placenta.
Here, exchange takes place between the patient’s blood and fetal blood through the placental membrane.
After use, the patient’s blood returns back through the uterine veins.
- Fetal Circulation:
- Deoxygenated blood is carried from the fetal heart to the chorionic villi of the placenta through two umbilical arteries.
- Here, after receiving oxygen and nutrients through the placental membrane, the oxygenated blood returns to the fetus through the umbilical vein.
- Circulation Process:
- Entry of Maternal Blood:
- Blood reaches the intervillous space of the placenta through the patient’s uterine arteries.
- Exchange of Substances:
- The placental membrane acts as a selective barrier where oxygen, glucose, amino acids, vitamins, and minerals are transferred to the fetal blood.
- Carbon dioxide, urea, creatinine, and other metabolic wastes are transferred back to the patient’s blood.
- Return of Fetal Blood:
- Oxygenated blood returns to the fetal heart through the umbilical vein.
- Importance of Placental Membrane:
- This membrane consists of four layers:
- Syncytiotrophoblast
- Cytotrophoblast
- Connective Tissue
- Fetal Capillary Endothelium
- The placental membrane maintains selective permeability by forming a barrier between the fetal blood and the patient’s blood.
- Functions of Placental Circulation:
- Respiratory Function:
- Supplies oxygen to the fetus and removes carbon dioxide.
- Nutritive Function:
- Delivers nutrients such as glucose, amino acids, vitamins, and minerals to the fetus.
- Excretory Function:
- Transfers metabolic waste into the patient’s blood and removes it.
- Endocrine Function:
- Secrets hormones such as hCG (Human Chorionic Gonadotropin), hPL (Human Placental Lactogen), Estrogen, and Progesterone.
- Immunological Function:
- Provides passive immunity by transferring patient’s antibodies to the fetus.
- Conclusion:
Placental circulation is essential for the overall development of the fetus. If the placenta does not function properly, serious conditions such as fetal growth retardation, hypoxia, and still birth arise. Therefore, proper antenatal care and monitoring of placental function are essential for the patient.
Q.2
a. Write difference (any two) તફાવત લખો (ગમે તે બે) 08
1.Institutional delivery and home delivery. ઇન્સ્ટિટ્યુશનલ ડીલીવરી અને હોમ ડીલીવરી. 08
- Institutional Delivery:
- Delivery is done safely in a health facility such as a hospital or health center by trained health professionals.
- Home Delivery:
- Delivery is done at the patient’s home in the presence of a midwife or unknowing family member.
| Order | Points of Difference | Institutional Delivery | Home Delivery |
|---|---|---|---|
| 1 | Place | Health Institution (Hospital/Health Center) | Home |
| 2 | Care givers | Trained Health Professionals (Doctors/Nurses) | Midwives or Family Members |
| 3 | Health Services | Operation Theatre, Oxygen Support, Emergency Management | Health facilities not available |
| 4 | Risk | Low for patient and newborn | High for patient and newborn |
| 5 | Transmission Risk | Low (Aseptic Conditions) | High (Risk of Infections) |
| 6 | Expenses | Low or free (under government schemes) | Low but health risk high |
| 7 | Complication management | Immediate Management Available | Immediate treatment not available |
| 8 | Effect on health | Mother and child health is better | Health problems and nutritional problems increase |
2.Monozygotic and Dizygotic twins. મોનોઝાયગોટીક અને ડાયઝાયગોટીક ટવીન્સ. 04
- Monozygotic Twins:
- Monozygotic twins are children that are formed by the division of a single unfertilized ovum (zygote) by mitosis. These twins are completely genetically identical and usually both are the same sex. These types of twins have the same width, height, facial structure and DNA pattern.
- Dizygotic Twins:
- Dizygotic twins are children that are formed by the fertilization of two different ovums and two different sperms. These twins have less genetic similarity and can be of the same or different sex. These types of twins have different body types, clothing, DNA, and completely different physical characteristics.
| Order | Points of Difference | Monozygotic Twins | Dizygotic Twins |
|---|---|---|---|
| 1 | Source of origin | Formed from one zygote | Formed from two different zygotes |
| 2 | Fertilization | One ovum and one sperm | Two different ovums and two different Sperm |
| 3 | Sex | Sex is always the same | Sex can be the same or different |
| 4 | DNA | Identical DNA | Non-identical DNA |
| 5 | Placenta | Usually one placenta | Two separate placentas |
| 6 | Blood supply | Shared blood supply | Can have separate blood supplies |
| 7 | Physical similarity | Very similar appearance and features | There is a lot of physical variation |
| 8 | Frequency | Low Incidence | Common Incidence |
3.Physiological & Pathological Jaundice ફીઝીયોલોજીકલ જોન્ડિસ અને પેથોલોજીકલ જોન્ડિસ.
- Physiological Jaundice:
- Physiological jaundice is the normal jaundice in a newborn patient, usually due to liver immaturity and incompetence of bilirubin metabolism. This condition is usually harmless and appears in the first 2-3 days of life. This jaundice disappears naturally in 7-10 days as the liver develops sufficiently.
- Pathological Jaundice:
- Pathological jaundice is when the cause of jaundice is a pathological condition, such as hemolytic disorder, liver disease, sepsis or glucuronyl transferase deficiency. This jaundice is more serious and requires immediate treatment.
| Order | Points of Difference | Physiological Jaundice | Pathological Jaundice |
|---|---|---|---|
| 1 | Start time | 2-3 days after birth | At birth or within 24 hours |
| 2 | Bilirubin level | Usually low (Mild) | Higher levels (Severe) |
| 3 | Cause | Liver Immaturity, slow bilirubin metabolism | Hemolysis, infection, liver disease |
| 4 | Symptoms | Light yellow discoloration, patient usually stable | Severe yellow discoloration, lethargy, severe loss of appetite |
| 5 | Severity of disease | Usually harmless | Can be a serious condition |
| 6 | Treatment | No special treatment usually required | Phototherapy, Exchange transfusion may be necessary |
| 7 | Risk | Low Risk, resolves spontaneously | High risk of kernicterus, neurological damage |
| 8 | Daily bilirubin increase | Less than 5 mg/dL | Rapidly increases above 5 mg/dL |
| 9 | Duration | Usually resolves in 7-10 days | May persist for a long time |
b. Nursing care of patient with Pelvic inflammatory disease,
પેલ્વીક ઇન્ફલામેટ્રી ડિસીઝનાં પેશન્ટ ની નર્સિંગ કેર.
- Nursing Care of a Patient with Pelvic Inflammatory Disease:
- Pelvic inflammatory disease is the medical term used for infection and inflammation in the reproductive organs of a female patient such as the uterus, fallopian tubes, and ovaries. This condition is mainly caused by the spread of sexually transmitted infections or bacterial infections. If not treated properly and on time, serious complications such as infertility and ectopic pregnancy can occur.
- Nursing Care for the Patient:
- Assessment:
- A complete history should be taken of the patient, including information about pelvic pain, vaginal discharge, dysuria, and menstrual irregularity.
- Vital signs such as body temperature, pulse, and blood pressure should be assessed.
- Pain Management:
- The patient should be given analgesics and anti-inflammatory drugs for pelvic pain.
- Pain relief should be provided with hot fomentation or heat therapy.
- Infection Control:
- The patient should be encouraged to take regular and complete doses of antibiotic therapy.
- Guidance should be given to maintain personal hygiene.
- Sexual partners should also be referred for appropriate treatment.
- Monitoring for Complications:
- The patient should be monitored for complications such as pelvic abscess, septicemia, ectopic pregnancy and infertility.
- Psychological Support:
- Provide counseling for anxiety, depression and guilt feelings in the patient.
- Provide appropriate information about the disease to the patient and their family members and guide them for future prevention.
- Nutritional Care:
- Provide the patient with a diet rich in high protein and vitamin C, which improves immunity.
- Maintain adequate hydration.
- Health Education:
- Guidance to the patient about safe sex practices to avoid sexually transmitted infections.
- Encourage the patient to take medications regularly and get complete rest for complete recovery without recurrence of the disease.
- Discharge Planning:
- Advise the patient for follow-up visits for health check-ups.
- Guidance to maintain pelvic exercises and hygiene.
OR
1.Describe the role of nurse in midwifery and obstetrical nursing. મીડવાઇકરી અને ઓબસ્ટ્રેટીકલ નર્સિંગમાં નર્સનો રોલ વર્ણવો.08
- Introduction:
- Midwifery and Obstetrical Nursing are important fields related to the health care of female patients during pregnancy, delivery, postnatal period, and newborn. Nurses in this field provide physical, mental, and emotional support to the patient and ensure holistic care at all levels.
- Antenatal Care:
- To conduct a complete antenatal assessment of the patient and work towards the diagnosis and prevention of diseases.
- To encourage the patient to take iron, folic acid, and other necessary supplements.
- To monitor for diseases such as gestational diabetes and hypertension.
- To guide the patient about Prenatal Exercises and Safe Diet.
- To give timely advice for Tetanus Toxoid and other necessary immunization.
- Intranatal Care:
- To ensure comprehensive care for the patient in the labor room.
- To monitor the partograph for labor progress.
- To provide breathing technique and relaxation therapy for pain management.
- To assist in delivery through sterile technique.
- To continuously monitor the fetal heart sound and contraction pattern.
- Postnatal Care:
- Monitoring the mother during the puerperium period for complications such as weakness, hemorrhage, infection.
- Encouraging the patient for breast feeding and guiding her for positioning.
- Explaining about high calorie and high protein diet to provide nutrition.
- Providing psychological counseling for the mother’s mental state.
- Explaining to the patient to monitor uterine involution and lochia.
- Newborn Care:
- Monitoring the vital signs and Apgar score of the newborn.
- Observe the newborn for diseases like Hypothermia, Hypoglycemia and Pathological Jaundice.
- Encourage the mother and family for exclusive breast feeding.
- Explain the vaccination schedule for the newborn.
- Family Planning and Counseling:
- Guidance to the patient and his partner for contraception and family planning.
- Provide complete information about programs such as birth control.
- Conclusion:
In midwifery and obstetric nursing, the nurse not only provides physical care to the patient, but also provides complete support and guidance for his mental, social and economic needs. The nurse’s job is to ensure the health and safety of both the mother and the newborn and to provide patient-centric care.
2. Write causes of maternal morbidity and mortality in India. ભારતમાં મેટરનલ મોર્ટાલીટી અને મોર્બીડીટીના કારણો લખો.04
- Introduction:
- Maternal Morbidity and Maternal Mortality are serious public health problems in India. Maternal morbidity refers to health-related illnesses or diseases that occur in a patient during pregnancy, delivery or the postpartum period, while maternal mortality refers to the death of a patient during that period.
Major Causes:
- Hemorrhage:
- Postpartum hemorrhage is the most common cause of maternal mortality.
- Conditions such as uterine atony, placenta previa and placental abruption are responsible for hemorrhage in a patient.
- Hypertensive Disorders of Pregnancy:
- Pre-Eclampsia and Eclampsia are serious conditions in which the patient experiences high blood pressure, headaches, visual disturbances, and convulsions.
- HELLP Syndrome can also be fatal.
- Sepsis:
- Puerperal Sepsis is caused by unhygienic delivery care and the use of unhygienic instruments.
- The patient presents with symptoms such as high fever, body pain, and shock.
- Obstructed Labor:
- Labor is obstructed due to causes such as pelvic disproportion, malpresentation and fetal macrosomia, which can be fatal for the patient.
- Unsafe Abortions:
- Abortions performed without knowledge or qualification, which pose risks such as infection, hemorrhage and uterine perforation.
- Anemia:
- The patient has very low hemoglobin levels due to deficiency of iron, folic acid and vitamin B12, which increases the risk of heart failure and mortality.
- Malnutrition:
- Nutrient Deficiency in the patient such as protein, iron, calcium and vitamins weakens the health and reduces the immune system.
- Delayed and Inadequate Medical Care:
- Lack of antenatal check-up and late stage hospitalization cause the patient to reach the hospital in critical condition, where it becomes difficult to provide treatment.
- Socio-economic Factors:
- Poverty, illiteracy, lack of health services and negative attitude of the family towards female patients are also responsible for maternal morbidity and mortality.
- Early Marriage and Frequent Pregnancies:
- Teenage pregnancy and frequent pregnancies at short intervals put more stress on the patient’s body and lead to poor health.
- Conclusion:
- To reduce maternal morbidity and mortality, it is essential to provide timely antenatal care, nutritional support, safe delivery and appropriate medical care to the patient. Along with this, nursing staff and health workers should focus more on patient-centric care and health education.
Q.4 Write Shortnotes (ANY THREE) ટૂંક નોંધ લખો (કોઇપણ ત્રણ)3×4 = 12
1.Hormonal replacement therapy.હોર્મોનલ રિપ્લેસમેન્ટ થેરાપી.
- Hormonal Replacement Therapy (HRT)
- Introduction:
- Hormonal Replacement Therapy is a medical therapy in which hormones are given from an external source to replace the deficiency in the patient’s body when there is a deficiency in the level of hormones. Especially in females, after menopause or after hysterectomy, when there is a deficiency of female hormones such as Estrogen and Progesterone, HRT is given.
- When is Hormonal Replacement Therapy given? (Indications for HRT):
- 1.Menopause – When the menstrual cycle in females stops completely and the level of estrogen in the body decreases.
- 2.Premature Ovarian Insufficiency – In cases where estrogen levels drop before the age of 40.
- 3.Post-hysterectomy – When the patient’s uterus and sometimes ovaries are removed.
- 4.Hypogonadism – When the patient’s body has low hormone production.
- 5.Transgender Hormone Therapy – Hormone therapy for gender reassignment for transgender patients.
- Types of HRT:
- 1.Estrogen-only Therapy – Only estrogen is given, which is considered safe only for patients who do not have a uterus.
- 2.Combined Estrogen and Progesterone Therapy – If the uterus is still present, it is necessary to give progesterone along with estrogen to reduce the chances of endometrial hyperplasia.
- 3.Local (Vaginal) Estrogen Therapy – Mainly useful for local symptoms like vaginal dryness, itching or pain.
- Routes of Administration:
- 1.Oral Tablets
- 2.Transdermal Patches
- 3.Gels and Creams
- 4.Vaginal Rings or Tablets
- 5.Injectables
- Benefits of HRT:
- Relieves Vasomotor Symptoms such as hot flashes, night sweats.
- Relieves problems affecting the vagina such as dryness and pain.
- Reduces the risk of osteoporosis.
- Helps with mood swings and sleep problems.
- Risks and Precautions:
- Long-term use of HRT may increase the risk of Breast Cancer, Deep Vein Thrombosis, Stroke, and Heart Disease.
- A complete medical evaluation is necessary before starting HRT.
- Regular follow-up of the patient, Mammography, and Pelvic Examination are mandatory.
- Contraindications:
- Patients with a history of breast cancer or endometrial cancer.
- Liver disease, irregular uterine bleeding.
- History of thrombosis or stroke.
- Hormonal Replacement Therapy is a tool that proves to be very beneficial if used correctly and in the right patient. It improves the patient’s quality of life, but it should be used only under the advice and supervision of a doctor. HRT must be personalized for each patient to be safe and effective.
2.Functions of amniotic fluid-એમ્બીયોટીક ફલ્યુઇડના કાર્યો
- The main function of amniotic fluid is to provide protection to the fetus.
- During pregnancy:
- 1) Amniotic fluid acts as a shock absorber and protects the fetus from external injuries.
- 2) It also works to maintain temperature.
- 3) Amniotic fluid distends the amniotic sac. Thus, it provides space for growth and free movements of the fetus. It also prevents adhesion between the fetal parts and the amniotic sac.
- 4) The nutritional value is negligible but provides adequate water supply to the fetus.
- During labor:
- Helps in dilation of the cervix. Prevents obstruction of the placenta circulation during uterine contractions.
- Works to protect the placenta and fetus during uterine contractions.
- Flushes the birth canal during the end of the first stage of labor and protects the fetus with its aseptic and bactericidal action. Also prevents ascending infection in the uterine cavity.
- Clinical Importance
- The study of amniotic fluid provides information about the well-being and maternity of the fetus. Intra-amniotic instillation is used as an abortion method using chemicals.
- Helps in the assessment of fetal malformations, i.e. during 16-18 weeks, cell culture of amniotic fluid obtained by amniocentesis can identify chromosomally defective babies, e.g. Down syndrome. Enzyme deficiencies are cultured. And amniotic fluid can identify metabolic errors in the fetus.
- Amniotic fluid with high levels of alphafetoprotein (AFP) can identify a fetus with an open neural tube defect (anencephaly).
- Amniotic fluid index (AFI) is assessed for low or high volume.
- Draining the fluid by rupturing the membranes also helps in the induction of labor.
3.PNDT act પી.એન.ડી.ટી. એક્ટ
- Objective of the Act:
- The main objective of the PNDT Act is to prevent sex-based foeticide. The main reason for the increasing male to female ratio in India is female foeticide. This Act prohibits the use of diagnostic techniques to determine the sex of a patient’s future child and for this purpose, the use of diagnostic techniques has been banned except in certain specified cases.
- Establishment and Amendments of the Act:
- This Act came into force in the year 1994 and was made stricter in 2003. Initially, this Act was applicable only to pre-natal tests but later it was extended to the pre-conception stage as well.
- Important Definitions:
- Pre-natal Diagnostic Techniques: Techniques that involve tests that can identify the sex of the fetus such as Ultrasound, Amniocentesis, Chorionic Villus Sampling, etc.
- Sex Selection: When a pregnancy or abortion is performed based on the sex of the child.
- Sex Determination: The process of determining the sex of a patient’s fetus.
- Key Provisions of the Act:
- It is a criminal offence for any medical professional to perform or cause sex determination.
- Registration of every Genetic Counseling Centre, Genetic Laboratory, and Genetic Clinic is mandatory.
- Registration of all Ultrasound Machines is mandatory.
- It is mandatory to keep a correct and complete record of each patient by filling Form F.
- The form must contain the patient’s details, purpose of the test and the doctor’s signature.
- What if the law is not implemented? (Penalties for Violation):
- Imprisonment up to three years and a fine of Rs. 10,000 for the first time if the crime is proven.
- Imprisonment up to five years and a fine of Rs. 50,000 for the second time.
- License for Medical Practitioner may be suspended or revoked.
- Technical Terminology and its Role:
- Ultrasound: Useful for checking the development and health of the fetus of the patient but it can be misused for gender determination.
- Amniocentesis: Amniotic fluid is taken for testing which can also determine gender.
- Chorionic Villus Sampling: Testing of cells of the placenta can also be useful for gender determination.
- Radiologist: A specialist who performs imaging tests who is responsible under this law.
- Social Importance of the Law:
- PNDT Act is not only a legal but also a revolutionary step in social terms. This law is a tool to advance gender equality in Indian society. The policy goal of the law is to protect patients from gender-based discrimination and prevent female foeticide.
4.Threatened Abortion-થ્રેટેન્ડ એબોર્સૅન
- Threatened abortion:
- In threatened abortion, the process of abortion starts but the abortion does not reach the condition where recovery is impossible, that is, if proper care is taken, recovery can occur. And the pregnancy can continue.
- Signs and Symptoms:
- Vaginal erection,
- Mild abdominal pain and cramping,
- Light bleeding,
- Blood color bright red,
- Mild abdominal pain,
- Bleeding painless,
- Mild back pain,
- Dull pain in the lower abdominal area,
- No fresh lump or expulsion,
- Cervix closed,
- Discharge.
- Signs:
- Abdominally: Gravit uterus feels soft and enlarges like a period of menorrhagia.
- Speculum examination or vaginal palpation: The cervix is closed and stained discharge is present.
- Investigation:
- Blood investigation including,
HB, ABO and Rh grouping.
Urine test,
Bimanual palpation,
Pelvic ultrasonography,
Transvaginal ultrasonography. - Management of Threatened Abortion
- Proper assessment and monitoring of the pregnant woman in the nursing management of threatened abortion. Provide proper supportive care to the woman.
- 1) Assessment
- Vital signs
Continuously monitor the vital signs of the mother. Such as,
Pulse,
Blood pressure,
Temperature,
Respiration etc. - Bleeding Assessment
Assess the color, amount, intensity and consistency of vaginal bleeding. - History Collection
Collect proper history of the mother including complete history of previous pregnancy and abortion. - 2) Monitoring and Observation
Continuously observe the mother and assess her for any signs and symptoms of shock (hypotension, tachycardia, pallor). - Conduct proper investigations of the mother including routine hemoglobin, hematocrit, ultrasonography, ABO & Rh grouping.
- 3) Bedrest and Physical Activity
Advise the mother to take complete bed rest.
Advise the mother to limit physical activity.
Advise the mother not to do household work for a month. - 4) Emotional Support
Provide emotional support and reassurance to the mother and her family.
Properly clear the doubts and queries of the mother and her family members.
Do not give false reactions to the mother and her family members. - 5) Education
Provide education to the mother about the signs and symptoms of abortion such as increased bleeding, severe pain etc. and advise her to seek immediate medical treatment if any such signs and symptoms are observed.
Provide education to the mother to take proper follow-up. - 6) Hydration and Nutrition
Advise the mother to have adequate fluid intake.
Continuously monitor the mother’s intake output chart.
Advise the mother to have a properly balanced diet.
Advise the mother to have a high fiber diet to prevent constipation.
Provide supplements to the mother with good fitting.
Ex:= Ferrous sulfate 200 mg( BD. ),
Folic acid 5 mg/ day( TDS ).
Provide the mother with a high protein and vitamin E rich diet. - 7) Medication Administration
Provide the mother with prescribed medication.
Provide medication to control bleeding and relieve pain.
Provide education to the mother about the dosage, direction and side effects of the medication.
If the mother has problems of sleep and anxiety, then provide Tab.Diazepam, ( 5-10 mg before night meal ),
Or Tab.Calmpose, ( 5-10 mg before night meal ),
Or Tab.valium ( 5-10 mg before night meal ), to relieve it. - Provide mild amount of laxative to the mother at bed time for good bowel activity.
Ex:= Milk of Magnesia. - Do not provide enema to the mother because enema is responsible for stimulating uterine contractions in the mother.
Provide mild laxatives or suppositories to relieve constipation, if present, within 48 hours of the mother experiencing signs and symptoms of threatened abortion. - 8) Consultation and Referral
Properly collaborate with other health care personnel for care.
Provide timely referral services to the mother, if needed. - 9) Documentation
Timely document the mother’s assessment findings, interventions provided, and any changes in the mother’s condition. - 10) Follow-up
Advise regular follow-up for mother’s progress and reassessment. - Nursing management of threatened abortion is usually provided to provide proper comprehensive care to the mother and to bring about improvement in the mother’s condition.
5.Oligohydramnias ઓલીગોહાઇડ્રોમ્નીઅસ
- Definition: Oligo: Reduce
Hydroamnios: Amniotic Fluid - When the amount of amniotic fluid (amniotic fluid) at term is less than 200 ml, it is called oligohydroamnios. Oligohydroamnios is a medical condition in which the amount of amniotic fluid around the fetus during pregnancy is less than its normal amount. Amniotic fluid is important for cushioning the fetus and facilitating normal development. Oligohydroamnios may be associated with various complications, such as fetal distress, preterm birth, or fetal development problems.
- Etiology:
- The exact cause is unknown. It is related to the following conditions:
- Postpartum gestation,
- Renal dysfunction,
- Obstetrical trauma,
- Failure to secrete amniotic fluid by the amniotic cells covering the placenta.
- Absent kidney.
- Reduced fetal urine formation.
- Symptoms and signs:
- Smaller uterine size for gestational age.
- Reduced fetal movement.
- Breech presentation is common.
- Fetal growth retardation or deformity.
- Low amniotic fluid makes the uterus appear full of feces.
- Thick meconium is passed during labor.
- Complications:
- Maternal: Prolonged labor, operative interference,
Maternal morbidity. - Management:
- If the fetus has congenital malformations, then delivery should be done regardless of the gestational age.
- Vaginal delivery is favorable.
- If the fetus is normal with third trimester, conservative management should be done and advice should be given for increased fluid intake along with amnio infusion in meconium lye.
Q.5 Define following (Any Six) વ્યાખ્યા આપો (કોઇપણ છ) 6×2=12
1.Denominator ડીનોમીનેટર
- The denominator is the bony part of the fetus that is the presenting part in relation to the various quadrants of the maternal pelvis.
- For example,
- In vertex/cephalic presentation, the denominator is the occiput.
- In face presentation, the denominator is the mantum (chin).
- In brow presentation, the denominator is the frontal eminence.
- In breech presentation, the denominator is the sacrum.
- In solder presentation, the denominator is the acromion process of the scapula of the solder.
2.Lie – લાઇ
- The relationship of the long axis of the fetus to the long axis of the maternal spine is called “lie”.
- Lie is usually longitudinal but can also be transverse and oblique.
- 1) Longitudinal:
- In this, the long axis of the fetus is parallel to the long axis of the maternal spine. This means that the fetus is in either a head-down (cephalic) or feet-down (breech) position. This is the most optimal fetal position for delivery.
- 2) Transverse:
- In obstetrics, a transverse lie involves a position of the fetus where the fetus is positioned horizontally across the mother’s uterus, rather than parallel to the mother’s spine. In this position, the fetus’s head is on one side of the uterus and its buttocks or legs are on the opposite side. This position is not conducive to delivery through the vaginal canal and often requires a cesarean section.
- 3) Oblique:
- In obstetrics, an oblique lie occurs when the fetus is positioned at an angle in the uterine cavity, with both the fetus’s head and buttocks tilted toward one side of the mother. This position is neither longitudinal nor transverse but instead is at a diagonal angle. This type of lie is not ideal for vaginal delivery.
3.Mastitis – માસ્ટાઇટીસ
- The condition of infection and inflammation in the breast tissue is called mastitis. One of the complications of mastitis is the condition of a breast abscess.
4.Naegele’s Formula – નીગેલ્સ ફોર્મ્યુલા’
- Naegele’s Formula is a validated and standardized method used to calculate the Estimated Date of Delivery (EDD). According to this formula, 9 months are added to the date of the Last Menstrual Period (LMP) and 7 days are added. For example, if the LMP is January 10, then according to Naegele’s Formula, the EDD will be October 17. This method provides the highest accuracy for a woman’s regular 28-day menstrual cycle and is widely used in Obstetrics.
5.Sub involution – સબ ઇનવોલ્યુશન
- Subinvolution is a condition in which the involution of the uterus, i.e. the process of returning to its original shape and position, after delivery is not completed within the normal period or is delayed. In this condition, the uterus remains larger than normal and Lochial discharge continues for a long time. The main causes of subinvolution include retained placental fragments, infection, and inadequate uterine tone. Its symptoms include prolonged bleeding, pelvic pain, and enlarged uterus. Immediate diagnosis and appropriate treatment of subinvolution are important to avoid postnatal complications.
6.Decapitation – ડીકેપીટેશન
- In this destructive surgery, the fetal head is cut from the trunk and the delivery is completed with extraction of the trunk. This operation is performed in dead fetuses with neglected breech presentation and interlocking heads of twins.
7.Obstructed labour- ઓબસ્ટ્રક્ટેડ લેબર
- Obstructed labor is a condition in which the presenting part of the fetus, which is progressively descending despite good (proper) uterine contractions, is arrested due to a mechanical obstruction. This is called “obstructed labor”. In obstructed labor, the fetus may also die due to the fetus not getting an adequate amount of oxygen.
8.Caput succedaneum કેપટ સકકસીડેનીયમ
- The accumulation of serosanguinous fluid in the layers of the scalp causes edematous swelling, which is called caput succedaneum. It is caused by pressure from the girdle of contact. It is sometimes the bony pelvis, dilating cervix or vulval ring. Due to reduced venous return, swelling and lymphatic drainage are seen. Caput succedaneum is also seen at the time of birth. It is indented when pressed. The swelling is boggy. It crosses the suture line and disappears within 24-36 hours. It is mostly seen after rupture of membranes.
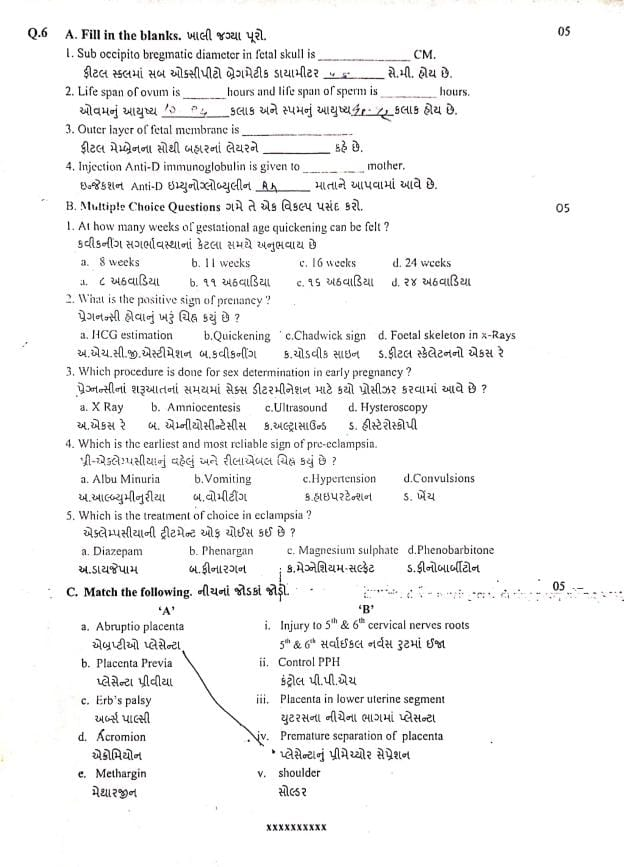
Q.6 A. Fill in the blanks. ખાલી જગ્યાઓ પૂરો.05
1.Sub occipito bregmatic diameter in fetal skull is…….CM.
ફીટલ સ્કલમાં સબ ઓકસીપીટો બ્રેગમેટીક ડાયામીટર…..સે.મી. હોય છે ✅ Answer:9.5 cm
2.Life span of ovum is….hours and life span of sperm is …… Hours. ઓવમનું આયુષ્ય……કલાક અને સ્પમ નું આયુષ્ય…… કલાક હોય છે ✅ Answer:
Ovum: 12 to 24 hours
Sperm: 48 to 72 hours
3.Outer layer of fetal membrane is……. ફીટલ મેમ્બ્રેનના સૌથી બહારનાં લેયરને …….કહે છે. ✅ Answer: Chorion (કોરિયન)
4.Injection Anti-D immunoglobulin is given to……mother. ઇન્જેકશન Anti-D ઇમ્યુનોગ્લોબ્યુલીન……માતાને આપવામાં આવે છે. ✅ Answer: Rh-negative mother
B. Multiple Choice Questions ગમે તે એક વિકલ્પ પસંદ કરો.
1.At how many weeks of gestational age quickening can be felt? ક્વીકનીગ સગર્ભાવસ્થાનાં કેટલા સમયે અનુભવાય છે.
a) 8 week- અ. ૮ અઠવાડિયા
b) 11 weeks – બ. ૧૧ અઠવાડિયા
✅ c) 16 weeks – ૧૬ અઠવાડિયા
d) 24 weeks – ડ. ૨૪ અઠવાડિયા
2.What is the positive sign of prenancy? પ્રેગનન્સી હોવાનું ખરું ચિહ્ન કયું છે ?
a. HCG estimation અ.એચ.સી.જી.એસ્ટીમેશન
b.Quickening.
બ.કવીકનીંગ
c.Chadwick sign
ક.ચોડવીક સાઇન
✅ d) Foetal skeleton in X-ray એક્સ-રેમાં ફીટલ સ્કેલેટન
3.Which procedure is done for sex determination in early pregnancy?
પ્રેગ્નન્સીનાં શરૂઆતનાં સમયમાં સેક્સ ડીટરમીનેશન માટે કયો પ્રોસીઝર કરવામાં આવે છે ?
a. X Ray અ.એકસ રે
✅b. Amniocentesis
બ. એમ્નીયોસીન્ટેસીસ
c.Ultrasound
ક.અલ્ટ્રાસાઉન્ડ
d. Hysteroscopy
ડ. હીસ્ટેરોસ્કોપી
4.Which is the earliest and most reliable sign of pre-eclampsia. પ્રી-એક્લેમ્પસીયાનું વહેલું અને રીલાએબલ ચિહ્ન કયું છે ?
a. AlbuMinuria
અ.આબ્લ્યુમીનુરીયા
b. Vomiting
બ.વોમીટીંગ
✅ c. Hypertension ક.હાઇપરટેન્શન
d.Convulsions
ડ.ખેંચ
5.Which is the treatment of choice in eclampsia? એક્લેમ્પસીયાની ટ્રીટમેન્ટ ઓફ ચોઈસ કઈ છે ?
a. Diazepam
અ.ડાયજેપામ
b. Phenargan
બ.ફીનારગન
✅ C. Magnesium sulphate
ક. મેગ્નેશિયમ સલ્ફેટ
d.Phenobarbitone
ડ. ફીનોબાર્બીટોન
C. Match the following. નીચનાં જોડકાં જોડો.05
A B
a. Abruptio placenta i. Injury to 5th & 6th cervical nerves roots 5 & એબ્રપ્ટીઓ પ્લેસેન્ટા 6th સર્વાઈકલ નર્વસ રુટમાં ઈજા b. Placenta Previa પ્લેસેન્ટા પ્રીવીયા ii. Control PPH કંટ્રોલ પી.પી.એચ
c. Erb’s palsy અર્બ્સ પાલ્સી iii. Placenta in lower uterine segment
d. Acromionએક્રોમિયોન યુટરસના નીચેના ભાગમાં પ્લેસન્ટા
e. Methargin મેથાર્જીન iv. Premature separation of placenta
પ્લેસેન્ટાનું પ્રીમેચ્યોર સેપ્રેશન
v. shoulder સોલ્ડર
🔶 CORRECT ANSWER (05) 🔶
| A | B | ✅ Correct Matching |
|---|---|---|
| a. Abruptio placenta | iv. Premature separation of placenta | ✅ a → iv |
| b. Placenta Previa | iii. Placenta in lower uterine segment | ✅ b → iii |
| c. Erb’s palsy | i. Injury to 5th & 6th cervical nerve roots | ✅ c → i |
| d. Acromion | v. Shoulder | ✅ d → v |
| e. Methargin | ii. Control PPH | ✅ e → ii |
Final Answers :
a → iv
b → iii
c → i
d → v
e → ii
