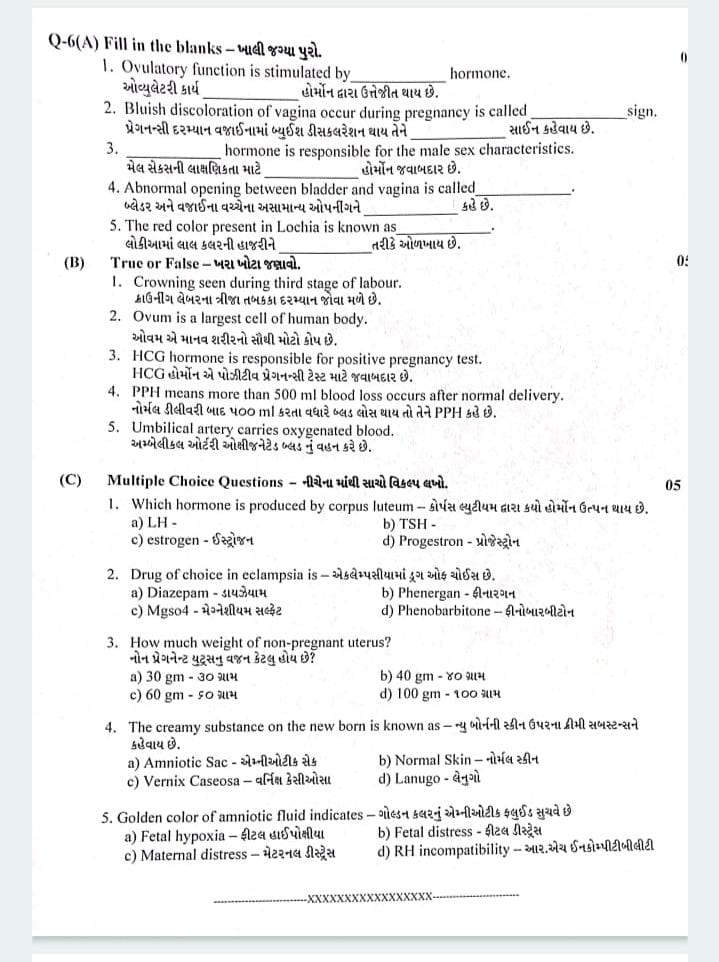
ENGLISH-MIDWIFERY & GYNECOLOGICAL NURSING-17/04/2023(UPLOAD-PAPER NO.7)-UPLOAD
ENGLISH-MIDWIFERY & GYNECOLOGICAL NURSING- PAPER NO.7 -Date: -17/04/2023
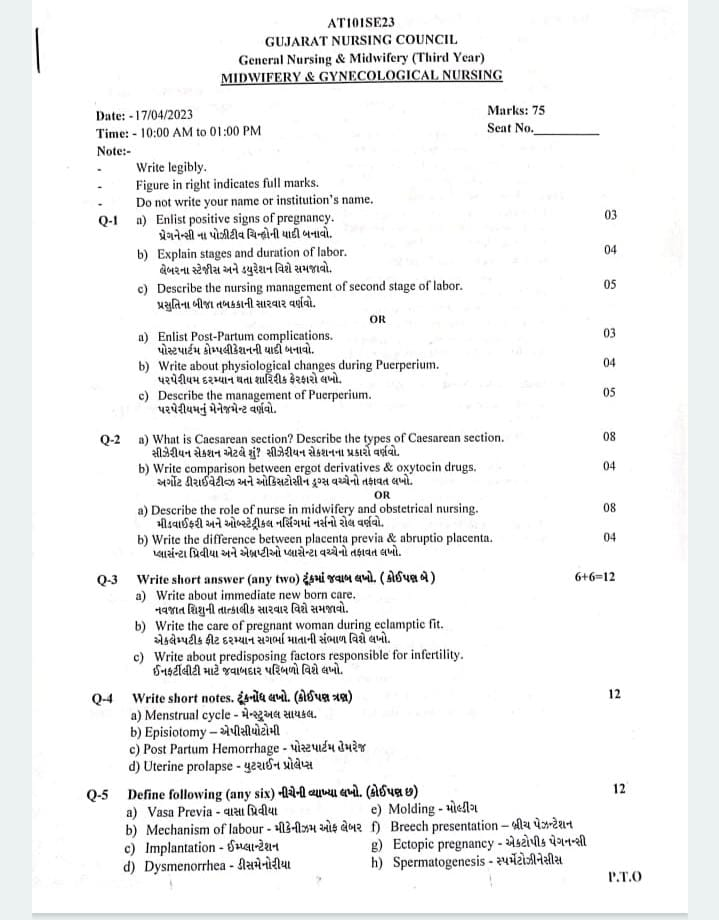
Q-1 a) Enlist positive signs of pregnancy. પ્રેગનેન્સી ના પોઝીટીવ ચિન્હોની યાદી બનાવો.
- Positive Signs of Pregnancy:
- Fetal Heart Sounds: The fetal heart beat can be heard with a Doppler or fetoscope. This heartbeat is usually heard between 10-12 weeks.
- Fetal Movements: Fetal movement is felt in the uterus by a doctor or a trained nurse. This movement is usually seen between 18-20 weeks.
- Visualization of Fetus: A clear image of the fetus is seen through ultrasound or sonography, which is a diagnostic method to confirm pregnancy.
- Palpation of Fetal Parts: The doctor Fetal organs in the uterus, such as the head, spine, or limbs, can be felt by touch.
- Fetal Cardiac Activity: Fetal cardiac activity or heartbeat can be detected by ultrasound, which usually becomes apparent between 6-8 weeks.
- All these clinical and diagnostic signs definitely confirm pregnancy, as they indicate the presence of a fetus.
b) Explain stages and duration of labor. લેબરના સ્ટેજીસ અને ડયુરેશન વિશે સમજાવો.
- Stages of Labor:
- The stages of labor are divided into four stages.
- 1) First Stage of Labor,
- 2) Second Stage of Labor,
- 3) Third Stage of Labor,
- 4) Fourth Stage of Labor
- ••>1) First Stage of Labor (Cervical Stage):
- The first stage of labor is the initial phase of childbirth. In which the cervix gradually opens (dilates) and thins (effaces). Due to which the baby can pass from the uterine cavity into the birth canal (vagina). In which regular and rhythmic uterine contractions are observed and the frequency, intensity and duration of uterine contractions gradually increase.
- The first stage of labor begins with the onset of true labor pains and lasts until the cervix is fully dilated (10 cm). This stage is also called the “cervical stage”.
- The first stage of labor is further divided into 3 stages:
- The time period of the first stage is:
Primigravida:=12-16 hours, and
Multigravida:=6-8 hours, - The first stage of labor is divided into three phases.
- 1) Latent phase,
- 2) Active phase,
- 3) Transitional phase
- 1) Latent phase,
- The latent phase is also known as “prodromal labor” or “pre-labor”.
- In this stage, cervical dilation of 1-4 cm occurs.
In this phase, contractions are repeated every 15-30 minutes and last for 15-30 seconds. - In this phase, the mother is talkative (able to talk).
2) Active phase, - The active phase is also known as the dilation phase.
In this second phase, the cervix is dilated by 5-7 centimeters. - And contractions are repeated every 3-5 minutes and last for 45-60 seconds.
- In this stage, the mother feels restless.
- 3) Transitional phase
- In the transitional phase, the dilation of the cervix is 8-10 cm.
- Contractions are repeated every 2-3 minutes and last for 60 to 90 seconds.
- Overall, the first stage of labor is a critical period in which the cervix opens, the uterus prepares for delivery by providing proper positioning of the baby in the uterine cavity. During this stage, continuous monitoring by health care providers is important to improve the condition and well-being of the mother and fetus.
- 2) Second Stage of Labor (Expulsion of Fetus): The period from full dilation of the cervix to the birth of the baby through the birth canal is called the second stage of labor.
- Its duration is:
In primigravida: 1-2 hours and in multigravida: 20-30 minutes. - The second stage of labor is further divided into two phases:
- 1) Propulsive phase,
- 2) Expulsive phase.
- 1) Propulsive phase: The propulsive phase starts from the full dilation of the cervix till the presenting part of the fetus descends to the pelvic floor (+4,+5 station).
- 2) Expulsive phase: This is the expulsive phase till the baby is completely expelled from the uterine cavity along with the mother’s bearing down efforts.
- 3) Third Stage of Labor (Expulsion of Placenta): This stage is the period from the expulsion of the baby to the expulsion of the placenta and membranes. Its time duration is 15 minutes in primigravida and multigravida
- 4) Fourth Stage of Labor (Observation Stage): After the birth of the baby, the observation stage is called the 4th stage of labor. During this stage, the general condition of the mother and the condition of the newborn and the behavior of the uterus are carefully monitored.
- Its time duration is 1 hour.
- Thus, all the four stages of total labor (1st stage + 2nd stage + 3rd stage + 4th stage)
c) Describe the nursing management of second stage of labor.પ્રસુતિના બીજા તબકકાની સારવાર વર્ણવો.
- Management of second stage of labor
- Intensity of uterine contractions increases
- Bearing down effort by the mother is seen
- Completion of dilatation of cervix occurs
- Principles:-
- Delivery of fetus should be done slowly and steadily
- Perineal injury should be prevented
- General measure:-
- Put the patient on bed rest
- Monitor the patient constantly and check the baby’s heart rate every five minutes. And check the mother’s pulse and blood pressure every 15 minutes.
- Reassure the patient and give moral support.
- Analgesic medicine should be given to relieve pain during contractions.
- Vaginal examination should be done when the second stage starts so that we can know in advance whether there is cord prolapse or not.
- Check the station and position of the fetal head.
- Preparation for Delivery:-
- Prepare the patient for delivery when clinical signs of cervical os dilatation are seen.
- Strong and frequent uterine contractions
Natural urge to bear down
Valval gaping
Anal pointing
Bulging perineum - Place the mother in lithotomy position with her head and ankles slightly raised.
- Cleaning the external genital area
- Maintain aseptic technique 3’c’ (clean hands clean surface and clean cutting and ligature the cord)
- If the mother’s bladder is full, catheterize it
- Check for membrane rupture and if there is no rupture, perform artificial rupture.
- Conduction of delivery (Delivery of head, delivery of shoulder, delivery of trunk)
Delivery of head:- When the baby’s head appears in the perineum and when contractions are present, a mediolateral type episiotomy is placed in the perineum. After delivery of the baby’s head, its mouth and oral cavity are cleaned and the eye lid is cleaned with cotton to prevent infection. And to remove the loop of the umbilical cord from the baby’s neck.
Delivery of the baby’s cord:- The baby’s cord should be delivered comfortably and easily so that the perineal area of the baby can be prevented from injury.
Delivery of the truck:- After the delivery of the cord, the baby’s axilla is placed there and the delivery is done by lateral flexion of his body.
Care of the baby after delivery:- - After delivery, the baby is stimulated to cry so that the lungs expand and the baby’s breathing pattern improves.
- If the baby does not cry properly after delivery, remove the secretion from the baby’s mouth and nose with a mucus sucker.
- Check Apgar score at birth and after five minutes to know the general condition of the baby.
- Give vitamin K intramuscularly to the baby.
- Show the baby’s sex to the mother and put an identification tag on the baby.
- Check the baby’s weight, take its footprint and give it to the mother for breast feeding within half an hour of delivery.
OR
a) Enlist Post-Partum complications. પોસ્ટપાર્ટમ કોમ્પલીકેશનની યાદી બનાવો.
- The postpartum period is the period after delivery, which usually lasts up to 6 weeks. During this period, many physiological and hormonal changes occur in the patient’s body. It is possible that some serious and life-threatening complications may arise during this period. Below is detailed information about important and clinically relevant postpartum complications:
- Hemorrhage
- (Hemorrhage is pronounced as – haemorrhage)
Postpartum hemorrhage means excessive bleeding after delivery. It is of two types: - Primary Hemorrhage: Excessive bleeding in the first 24 hours after delivery
- Secondary Hemorrhage: Bleeding after 24 hours and up to 12 days after delivery
- Main causes:
- Uterine Atony
- Trauma
- Retained Placental Tissue
- Coagulopathy
- Puerperal Infection
- Infection of the uterus or reproductive tract after delivery.
Symptoms: - Fever
- Pelvic pain
- Uterine tenderness
- Foul-smelling lochia
- Most common bacteria: Aerobic and anaerobic mixed infection
- Thromboembolism
- Blockage of a vein due to blood clots in the postpartum period.
Common types: - Deep Vein Thrombosis (DVT)
- Pulmonary Embolism (PE)
- Symptoms:
- Pain and swelling in the legs
- Difficulty breathing
- Chest pain
- Galactocele
- A benign cyst filled with breast milk that forms due to a blocked duct.
Symptoms: - Breast swelling and pain
- Milk engorgement
Treatment: - Hot fomentation
- Manual expression
- Antibiotics if infection is present
- Postpartum depression
- A psychological complication in the mother that includes pain, fatigue, sadness, and hopelessness.
Causes: - Hormonal changes
- Fatigue
- Lack of support system
- Postpartum psychosis can also develop in severe cases.
Treatment: - Psychological counseling
- Antidepressants
- Uterine inversion
- A condition where the uterus is pulled inside out. This is rare but life-threatening.
Symptoms: - Sudden collapse
- Hemorrhage
- Shock
Treatment: - Immediate replacement of uterus
- Intravenous fluids
- Surgical management if necessary
- Urinary incontinence
- Difficulty controlling urine after delivery
- Causes:
- Weakness of pelvic floor muscles
- Nerve damage
- Treatment:
- Kegel exercises
- Physiotherapy
- Controlled medical management
- Fistula
- An involuntary opening between the urethra and rectum due to trauma or prolonged labor during delivery.
Treatment: - Surgical correction
- Proper hygiene and patient care
- Breast Abscess
- (Breast abscess is pronounced as – breast abscess)
A pus-filled, purulent swelling in the breast, an infection caused by lactation - Symptoms:
- Breast redness
- Fever
- Pain and tenderness
- Treatment:
- Antibiotics
- Incision and drainage if necessary
- The postpartum period is not only a period of recovery, but also a very sensitive and risky time where proper monitoring and medical care are very important. Patients should be aware of all the signs and symptoms so that timely treatment can be given.
b) Write about physiological changes during Puerperium. પરપેરીયમ દરમ્યાન થતા શારિરીક ફેરફારો લખો.
- The postpartum period is not just a period of recovery, but a very sensitive and risky time where proper observation and medical care are very important. Patients should be aware of all the signs and symptoms so that timely treatment can be given.
- Physiological changes during the puerperium period:
- Puerperium:
The puerperium is the period of 6 weeks (42 days) after childbirth in which the tissues of the body, especially the pelvic organs, return to their pre-pregnancy stage both anatomically and physiologically. It is called puerperium. - Duration:
The onset of puerperium is from the expulsion of the placenta to about 6 weeks, during which the uterus becomes almost non-pregnant in size. The period is roughly divided as follows:
- Immediate:
Within 24 hours, - Early:
Up to 7 days, - Remote:
Up to 6 weeks
- 1) Physiological Changes in Reproductive System in the Puerperium Period:
- ( a ) Involution of Uterus:
- Involution is the process in which the bulky uterus during pregnancy progressively returns to its normal pre-pregnant state after delivery. This is called involution of uterus.
- Anatomical Considerations
- After delivery of the placenta, it heals in the endometrium of the placental site. After delivery, the uterus becomes firm and constricted with alternate hardening and softening.
- The size of the uterus during pregnancy is approximately,
Length: 20 cm, Breath: 12 cm,
Thickness: 7.5 cm - And the weight of the uterus is about 900-1000 gm.
- Which,
At the end of the puerperium period i.e. 6 weeks after childbirth, the uterus returns to its pre-pregnant state, such as, the size of the uterus during the puerperium period is
Length: 7.5 cm, Breath: 5 cm, Thickness: 2.5 cm
And the weight of the uterus is about 60 gm. - Reduction of the Size and Position of the Uterus:
- After labor, the fundus is 5 cm below the umbilicus and 12 cm above the symphysis pubis.
- After 24 hours, it is at the level of the umbilicus. The uterus descends into the pelvic cavity at a rate of 1.25 cm/hr and is not palpable abdominally above the symphysis pubis after 10 days.
- Consistency of the uterus:
- Due to frequent strong myometrial contractions, the blood flow to the uterus is controlled, making it hard. Its consistency can be felt on palpation. It should feel firm and round. If the funds are soft, it is called a boggy uterus. It indicates that the contractility is inadequate and blood loss is ongoing.
- ( b ) Involution of cervix:
- After delivery, the lower uterine segment and cervix remain loose, thin and stretched.
- They may be edematous, bruised and may contain small tears and lacerations. It takes a few weeks for the isthmus to return to its normal shape and size.
- The consistency of the first post partum day service remains normal enough to admit two fingers. Then at the end of the first week it remains soft enough to admit the tips of the fingers. The evolution of the cervix continues for 3-4 months. But the parous cervix never acquires the appearance of a non-parous cervix. The external os which initially looked like a dimple now looks like a slit.
- (C) Vaginal canal:
- It takes about 4 to 8 weeks for the distensible vagina to involute. After delivery, the vaginal canal appears swollen and smooth, gradually becoming smaller and firmer but never of its pre-pregnancy size. The introitus remains permanently large and the hymen is lacerated. It presents as nodular tags.
- (d) Perineum:
- The muscles of the perineal floor are stretched, swollen and bruised, and a scar resembling that of an episiotomy may be seen.
- (e) Broad ligaments and round ligaments:
- The broad ligaments and round ligaments take some time to recover from stretching. Initially, the ligaments are stretched, but by the end of the puerperium period, the ligaments return to their non-pregnant length.
- ( f ) Pelvic Floor and Pelvic Fascia:
- The pelvic floor and pelvic fascia take a long time to involute due to the stretching effect.
- (f) Lochia:
- The vaginal discharge that occurs during the first 15 days of the puerperium period is called lochia and comes from the uterine body, cervix and vagina.
- It contains blood vessels, decidual tissue, epithelial cells of vaginal mucus, bacteria, membrane fragments and small clots.
- Odor of lochia
- The odor (smell) of lochia is fishy.
- Types of lochia:
- There are three types of lochia.
- 1) Lokia Rubra,
2) Lokia Sirosa,
3) Lokia Alba - 1) Lokia Rubra:
- Lochia Rubra is the first phase of lochia. In which the discharge is red and bloody and lasts for 1 to 4 days after childbirth.
- In lochia rubra,
blood,
fetal membrane, decidua,
vernix caseosa and lanugo are present. - 2) Lokia Sirosa:
- Lochia Sirosa is the second phase of lochia.
- Which is seen as yellowish pale or pale brownish color.
- Lokia Sirosa lasts for 5 to 9 days.
It contains a small amount of red blood cells but a high amount of leukocytes, wound exudate, viable mucus, and microorganisms. - 3) Lochia Alba:
Lochia Alba is the third phase of lochia. It is usually seen in pale white color.
Lochia Alba is seen for 10-14 days.
In it,
a large amount of decidual cells,
leukocytes,
mucus,
cholesterol crystals,
fatty and glandular epithelial cells,
and microorganisms are seen in it. - Amount:
The average amount of lochia is about 250 ml during the first 5 to 6 days. - Normal Duration:
The normal duration of lochia is up to three weeks. If it continues even after three weeks, then there may be local lesions. - Clinical Importance of Local Discharge:
- As lochia provides information about the maternal perinatal state, it is important to assess lochia.
- Odor: May be due to offensive infection.
- Odor: Scenty or absent may be due to infection.
- Amount: Scenty or absent may be due to infection.
- Color: Continuous red color lochia may be due to subinvolution.
- Duration: If lochia persists for three weeks or more, then local lesions may be present.
- (2) Breast and Lactation:
- Breasts: Breasts develop during pregnancy due to hormonal stimulation. For a few days after delivery, both the feeding and non-feeding breasts secrete colostrum. Colostrum is the creamy yellow precursor of milk. In which the breasts are soft and non-tender.
After three days, prolactin levels increase and the breasts become firm and tender. Then milk secretion starts. Due to increased blood flow, venous and lymphatic congestion, the breasts become distended, hard and warm. This is called physiological engorgement.
It lasts for 24 to 48 hours and then resolves on its own. Milk production is stimulated by the baby’s sucking. The breasts feel firm, full and tender until they are empty. - Lactation:
Lactation is the process of breastfeeding that is based on the interplay of hormones, instinctive reflexes, and learned behaviors of the mother and newborn.
Latescence is particularly under the control of the hormones prolactin and oxytocin and is maintained by three factors: - 1) The anatomical structure of the mammary gland, development of alveoli, ducts, and nipples.
- 2) Initiation and maintenance of milk secretion.
- 3) Ejection or propulsion of milk from the alveoli to the nipple.
- Physiology of Lactation:
- Lactation
Lactation is the process of breastfeeding by which the mammary gland produces and releases milk to provide nourishment to the child. It occurs through a complex interplay of hormones. Prolactin and oxytocin are the major hormones involved in lactation.
The establishment and maintenance of lactation is generally determined by three factors:
1) The anatomical structure of the mammary gland, such as the development of the alveoli, ducts, and nipple.
2) The initiation and maintenance of milk secretion.
3) The ejection or propulsion of milk from the alveoli to the nipple. - Main two hormones responsible for lactation:
Prolactin and oxytocin work as important hormones for lactation. - 1) Prolactin:
Prolactin hormone is secreted from the anterior pituitary gland.
It is the primary hormone for the stimulation of milk production (lactogenesis).
During pregnancy, estrogen and progesterone hormones are increased, these hormones prepare the breast for milk production but inhibit lactation.
After the birth of the child, the level of estrogen and progesterone hormones decreases due to which the effect of prolactin hormone can be felt on the mammary gland and the secretion of milk increases. - 2) Oxytocin:
Oxytocin is released from the posterior pituitary gland.
The release of oxytocin is crucial for milk ejection (let-down reflex), which is usually dependent on the baby’s sucking and nipple stimulation.
Oxytocin is an important hormone for the contraction of myoepithelial cells surrounding the alveoli (milk-producing glands), which causes milk to enter the ducts from the alveoli and then from the ducts to the nipple for best fitting. - •> Lactation is divided into four phases on physiological basis.
- 1)Mammogenesis (preparation of breast),
- 2)Lactogenesis (synthesis and secretion of milk from breast alveoli),
- 3)Galactokinesis (ejection of milk),
- 4)Galactopoiesis
- (maintenance of lactation)
- 1)Mammogenesis (preparation of breast)
- During this stage, the ductal and lobuloalveolar system of the breast grow during pregnancy, in which the breast is prepared for the secretion of milk.
- 2) Lactogenesis (synthesis and secretion of milk from breast alveoli):
Some secretory activity (colostrum) occurs during pregnancy and increases after delivery.
Actually milk secretion starts on the third or fourth day postpartum. During this period, the breast feels engorged, tense, tender and warm.
Despite high prolactin levels during pregnancy, due to the effects of steroid estrogen and progesterone hormones, the breast tissue does not respond to prolactin hormone and milk secretion does not occur. However, after delivery, when estrogen and progesterone levels fall down (decrease), prolactin hormone starts its milk secretion activity in the mammary gland. Prolactin and glucocorticoid hormones are important at this stage.
Secretory activity increases directly or indirectly due to growth hormone, thyroxine and insulin. - 3) Galactokinesis (ejection of milk):
Milk is not only released by the baby’s shaking but milk is released from the alveoli through a contractile mechanism.
Oxytocin hormone is a major galactokinetic (milk ejection) hormone.
The reflex is set up during the baby’s sucking.
The impulses from the nipple and areola then pass through the thoracic sensory nerves and cause the hypothalamus to synthesize oxytocin, which then reaches the posterior pituitary gland to transport the synthesized oxytocin.
The hormone oxytocin is released from the posterior pituitary gland, which then causes the myoepithelial cells surrounding the alveoli (milk-producing glands).
This process is called “milk ejection” or “milk let-down reflex”.
The milk is forced into the ampulla of the lactiferous duct, from where it is released by the mother’s expression or the baby’s sucking.
The let-down reflex is triggered by the baby’s crying even without shaking.
The pressure of milk in the breast that increases before the baby sucks is called “draft”. It is also produced by the injection of oxytocin.
The milk ejection reflex is inhibited due to pain, breast engorgement. If the ejection reflex is inhibited for more than a few days after the start of milk secretion, breast engorgement occurs. - 4) Galactopoiesis
(Maintenance of lactation):
Prolactin is a single and important galactopoiesis hormone.
Shaking is necessary for effective and continuous lactation, not only for the release of milk from the gland but also for the release of prolactin.
Due to the pressure of milk in the breast, the rate of milk production decreases, so periodic breast feeding can reduce that pressure and maintain milk secretion.
A healthy mother produces 500-800 ml of milk to feed her baby.
Thus, the physiology of lactation is divided into 4 phases. - Milk Production:
- A healthy mother produces 500 to 800 ml of milk to feed her baby.
- (3) Cardiovascular Changes:
- Blood Volume: The blood volume that increases during pregnancy decreases and the circulatory system returns to its pre-pregnancy state.
- Cardiac Output
Excess water in the body is removed due to diuresis and diaphoresis and cardiac output comes within its normal range. - Hemoglobin and Hematocrit Level:
Due to blood loss during pregnancy, hemoglobin and hematocrit levels initially decrease but within a few weeks the blood stabilizes within its normal range. - 4) Respiratory Function: After delivery, the abdominal pressure decreases and the diaphragm descends, so lung expansion and ventilation improve but there are no noticeable changes in respiratory rate.
- (5) Endocrine Changes:
- Hormone Shift:
Pregnancy-related hormones such as estrogen, progesterone, and human chorionic gonadotropin (HCG) hormone are reduced. - Prolactin hormone levels are elevated to support breastfeeding.
- (6) Renal Changes
- Diuresis
Urine output increases, which helps the body excrete the fluid accumulated in the body during pregnancy. - Bladder Function
The bladder regains its tone and function, although some temporary issues such as urinary retention or urinary incontinence may occur. - (7) Gastro intestinal changes:
- Bowel function
Bowel function takes some time to normalize but due to its motility being reduced, a condition of constipation is seen.
Appetite in women becomes normal in some time but bowel changes are seen in some women for some time. - (8) Musculoskeletal Changes:
- Abdominal Muscles
The tone of the abdominal muscles regains in a short time while the pelvic floor muscles also return to normal in a short time, but Kegel exercises are important in strengthening the pelvic floor muscles. - (9) Psychological Changes
Hormonal fluctuations, physical recovery, and the demands of newborn care impact emotional well-being. Common experiences include mood swings such as the “baby blues”. And some women also experience postpartum depression. - Thus, these types of physiological changes are seen in women during the postpartum period.
c) Describe the management of Puerperium. પરપેરીયમનું મેનેજમેન્ટ વર્ણવો.
- Postnatal Care of Mother: Postnatal care involves systematic examination of mother and baby along with appropriate advice to mother and baby during the postnatal period.
- Aims and Objectives:
- To provide support to mother and family in the new changes.
- To provide early diagnosis and treatment to prevent any complications in mother and infant.
- To provide early referral services to mother and infant if needed such as,
- a) To support breastfeeding,
- b) To provide counseling services in nutrition, complementary feeding and immunization.
- C) To provide proper counseling about contraception.
- Principles of Normal Postpartum:
- 1) To restore the health status of the mother.
2) To prevent infection.
3) To promote lactation.
4) To motivate the mother to accept contraceptives. - In postpartum management, the following principles should be kept in mind to make the woman physically and emotionally normal, such as,
- 1) To maintain the health status of the mother.
2) To prevent infection.
3) To promote best feeding.
4) To provide care to the baby.
5) To motivate and guide for family planning.
6) To provide health education as per the need. - Management of Normal Parturition:
- Immediate Attention:
- Immediate Postnatal Care
- The period up to one hour after the expulsion of the placenta is called the fourth stage of labor in which the general condition of the patient and the behavior of the uterus are monitored.
- Observation of Woman
- In this, the vital signs of the mother such as,
temperature,
pulse,
respiration,
and blood pressure are properly monitored. If it is slightly elevated, then it is usually due to fatigue and dehydration and the vital signs are checked every 15 minutes for the next 1 to 2 hours until the patient is stable. - Then the condition of the uterus is assessed in which the uterus is firmly contracted and in the midline.
- Rest and Ambulation: It is beneficial to move the patient immediately after delivery. The benefits include a feeling of well-being, reduced bladder complications and constipation, rapid involution of the uterus due to ureteral drainage and reduced embolism. After normal delivery, the patient can do some work.
- Diet: The patient should be given a normal diet as per his/her wishes. If the patient is lactating, then a high calorie diet, adequate protein, fat, extra fluid, minerals and vitamins should be given. If the mother is non-lactating, then a diet according to the non-pregnant state should be given.
- Bladder Care: After delivery, the patient should be encouraged to pass urine as per his convenience. Sometimes, the patient’s position is not proper or the patient cannot pass urine due to pain from perineum injury. If the patient cannot pass urine, then provide proper privacy to the patient. Then, the patient should be encouraged to urinate and if the patient cannot pass urine, then catheterize properly. Keep the catheter continuously until the bladder tone returns. Properly prevent the condition of infection and cystitis through bladder care.
- Bowel Care: Early ambulation and proper diet reduce the problem of constipation. Adequate fiber food and fluid intake does not cause bowel problems and if required, mild laxatives should be provided to the patient such as mild milk of magnesia 4-6 teaspoon at bed time.
- Sleep: The patient needs both physical and mental rest, so the patient should be provided with proper work and comfortable environment. The patient gets physical and mental support by getting adequate amount of sleep. If the patient has painful piles and engorged breast, then proper analgesic medicine should be provided.
- The mother should be advised to get at least 7-8 hours of sleep at night and 1-2 hours of sleep during the day.
- Care of the Vulva and Episiotomy Wound: After delivery, clean the vulva and buttocks with saline, lotion, soap and water. Apply antiseptic ointment or lotion to the episiotomy and apply a sterile pad. Provide care after each urination and defecation. This will reduce pain.
- Many women find warm water sitz baths to be relaxing.
- Care of Breast: Wash and clean the breasts and nipples with water. Apply soap while taking a bath. Provide frequent and short fitting to prevent nipple soreness.
- Asepsis and Antiseptic: Maintain asepsis technique especially in the first week of puerperium and use local and topical antiseptic for wound dressing. Use of clean bed linen and clothing, clean surroundings, and limit number of visitors to reduce nosocomial infections.
- Immunization: If Rh negative, give Anti-D gamma globulin within 72 hours of delivery. If second dose of tetanus toxoid has not been taken during pregnancy, provide it at discharge.
- Postnatal Exercise:
- Objectives of Postnatal Exercise:
- To improve abdominal and perineal muscle tone.
- Advise the mother to do small amounts of daily routine activities.
- Attachment and Warmth (Bonding):
- After the birth of the baby, place the baby on the mother’s abdomen so that bonding with the mother occurs and proper skin-to-skin contact can occur, which leads to attachment of the mother and the baby and prevents the baby from hypothermia.
Q-2 a) What is Caesarean section? Describe the types of Caesarean section. સીઝેરીયન સેક્શન એટલે શું? સીઝેરીયન સેકશનના પ્રકારો વર્ણવો.
- Cesarean section is a surgical procedure in which an incision is made on the abdomen to deliver the baby from the uterus and the baby is delivered through it.
The types of Cesarean section are as follows. - 1.Based on the timing of delivery (according to the time of delivery):-
- Elective Cesarean section:- In this type, the Cesarean is already planned.
- Indication – Previous Cesarean section, breech presentation, placenta previa etc…
- Emergency Cesarean section:- It is unplanned. Emergency Cesarean section is done when vaginal delivery is not possible.
Indication – Fetal distress, prolonged labor, uterine rupture… - 2.Based on the uterine incision (uterine incision):-
- Lower segment cesarean section:- It is the most common type. In which a horizontal incision is made in the lower segment.
- Advantages – It reduces blood loss, the chances of uterine rupture are less and healing also comes earlier.
- Classical cesarean section:- In which a vertical incision is made in the upper segment.
- Disadvantages – The chances of uterine rupture are higher.
- 3.Based on the approach of surgery (according to the approach of surgery)
- Open cesarean section:- In which a wide incision is made on the abdomen.
It is performed in patients with emergency pregnancy or multiple previous surgeries.
Minimally-invasive cesarean section:- In this, the baby is delivered through a minimally invasive technique on the abdomen.
b) Write comparison between ergot derivatives & oxytocin drugs. અર્ગોટ ડીરાઈવેટીવ્ઝ અને ઓક્સિટોસીન ડ્રગ્સ વચ્ચેનો તફાવત લખો.
- Ergot alkaloids: – They are made from a fungus called Claviseps purpura.
- Oxytocin: – It is a naturally occurring hormone secreted by the pituitary gland. And it is also made artificially.
- *Mechanism of Action
- Ergot alkaloids: – It works on adrenergic, serotonergic and dopamine receptors and contracts muscles, causing uterine muscles to contract.
- Oxytocin: – It works on oxytocin receptors in smooth muscles, causing strengthening contractions.
- Uses
- Ergot alkaloids: – It is used to prevent and treat postpartum hemorrhage. Used as a treatment for uterine atony.
Oxytocin: – Used to induce labor. And used to prevent PPH. And given to improve breast feeding. - Duration of Action
- Ergot alkaloids: – It gives effect for a long time.
Oxytocin: – It gives effect for a short time. - Route of Administration
- Ergot alkaloids: – It is usually given intramuscularly (IM) and orally.
Oxytocin: – It is given intravenously (IV) and intramuscularly (IM). - Contraindication
- Ergot alkaloids: – Hypertension, coronary artery disease, peripheral vascular disease.
Oxytocin:- Hypertonic uterus, mechanical obstruction. - Side Effect – (Side Effect)
- Ergot alkaloids:- Nausea, vomiting, hypertension, headache, dizziness
- Oxytocin:- Uterine hyperstimulation, hyponatremia.
- Monitoring
- Ergot alkaloids:- Hypertension is seen as a side effect so it is necessary to monitor blood pressure periodically.
- Oxytocin:- It is necessary to monitor the fetus because the uterus is hyperstimulated due to oxytocin.
OR
a) Describe the role of nurse in midwifery and obstetrical nursing. મીડવાઈફરી અને ઓબ્સ્ટેટ્રીકલ નર્સિંગમાં નર્સનો રોલ વર્ણવો.
- Role of Nurse Midwifery and Gynecology Midwife is a person who provides care within the obstetric unit. She provides care to the mother during the antenatal, intranatal and postnatal periods and also provides newborn care.
- Care during the antenatal (ANC) period:-
- In the community, the midwife collects all the history of the mother through the antenatal visit. She also checks the health history, obstetric history and the physical and emotional status of the mother.
- Many laboratory investigations are also done. When the mother comes for the visit, her abdominal examination is also done.
- While caring for the mother, the midwife provides care keeping in mind the mother’s attitude and traditional beliefs.
- The duties of the midwife during prenatal care include examination, supervision and education of the pregnant mother and identification of high-risk mothers and referral for treatment.
- Care during the intranatal period:-
- This period is a crucial period. Therefore, it is necessary to take proper care of the mother.
- Assurance and comfort are given to the mother during labor.
- The midwife performs abdominal and vaginal examinations and checks the progress of labor.
- Continuous monitoring of the baby is also done.
- When a complication arises, the mother is provided with proper emergency treatment until the physician arrives.
- Research has shown that if supportive care is provided to the mother during labor, the physiology of normal labor can be enhanced and complications in the mother and child can also be prevented.
- During the postnatal period:-
- The main goal of postnatal care is to detect any health problems in the mother and baby in the early stages.
- During the postnatal period, the midwife provides health education to the mother about breast-feeding techniques, weaning period and family planning methods and finds out if the mother has any complications.
- Midwife plays the role of advocate, counselor and teacher for the mother.
- She provides teaching to the mother about reproductive health and successful motherhood.
- She also provides teaching about adolescence health promotion family life education and family planning.
- Good communication skills of midwife are her greatest contribution so that she can communicate easily with the mother and understand her problems. She is supportive. Midwife should provide health care facility when the woman needs it.
b) Write the difference between placenta previa & abruptio placenta. પ્લાસંન્ટા પ્રિવીયા અને એબ્રપ્ટીઓ પ્લાસેન્ટા વચ્ચેનો તફાવત લખો.
- Difference between placenta previa and abruptio placenta:
- 1) Clinical features
- •>Placenta previa
Nature of bleeding Painless, causeless and recurrent bleeding.
Bleeding is always visible. - Abruptio placenta
Bleeding occurs due to painful, preeclampsia or trauma. - Bleeding can be visible, invisible or mixed.
- •>Placenta previa
Character of blood Bright red blood is seen. - Abruptio placentae has dark red blood.
- •>Placenta previa
General condition and anemia Anemia is seen in proportion to visible blood loss. - Placenta previa In this, the condition of anemia is more common than the amount of visible blood loss.
- •>Placenta previa
- Features of preeclampsia Placenta previa is not associated with the condition of preeclampsia.
- In placenta previa, the features of preeclampsia are seen in 1/3 of the cases.
- 2) Abdominal examination
- •>Placenta previa The height of the uterus is found according to the gestational age.
- In placenta previa, the height of the uterus is larger than the gestational age.
- •>Placenta Previa
- Feel of Uterus In placenta previa, the uterus feels soft and relaxed.
- Abruptio placentae In placenta previa, the uterus can be tense, tender and rigid.
- •>Placenta Previa
- Malpresentation In placenta previa, malpresentation is common and the head is high-floating.
- Abruptio placentae In placenta previa, malpresentation is unrelated and the head may also be engaged.
- •>Placenta Previa
- FHS(Fetal heart sounds) Heart sounds are often present in placenta previa.
- Abruptio placentae Heart sounds are often absent in placenta previa.
- 3) Placentography (USG)
- •>Placenta previa The placenta is found in the lower segment of the uterus.
- Placenta abducta The placenta is found in the upper segment of the uterus.
- 4) Vaginal Examination
- •>Placenta previa The placenta is felt in the lower segment of the uterus.
- Placenta abducta The placenta is not felt in the lower segment of the uterus.
Q-3 Write short answer (any two) ટૂંકમાં જવાબ લખો. (કોઈપણ બે)
a) Write about immediate new born care. નવજાત શિશુની તાત્કાલીક સારવાર વિશે સમજાવો.
- Essential Newborn Care:
- Essential Newborn Care involves properly assessing and stabilizing the newborn.
- Essential Newborn Care is crucial for the fetus to transition from intrauterine life to extrauterine life.
- Goals of Essential Newborn Care
- 1) To establish, maintain, and provide support for the newborn’s respiration.
- 2) To prevent the newborn from overheating and hypothermia.
- 3) To prevent the newborn from getting infections.
- 4) To provide safety to the newborn and prevent it from injury.
- 5) To provide immediate treatment for any actual or potential problem in the newborn by early identification.
- Immediate newborn care is provided.
Essential newborn care
- 1) Establishment of respiration
When the newborn is received, immediately patent the newborn’s airway and clear the airway properly. Due to which the newborn can breathe effectively.
As soon as the newborn’s head is turned, wipe the mouth and nose and suck the mouth and nose, due to which the newborn can breathe properly. Sucking should be done first in the mouth and then in the nose, due to which secretions can be prevented from being aspirated. - 2) Initiation of Cry: Normally 99% of newborns cry immediately and spontaneously after delivery, this cry is known as a good sign for the newborn’s breathing.
- If the newborn does not cry properly, then follow the following steps:
- a) If the baby does not cry spontaneously or if the cry is weak, then lightly simulate the baby to cry.
- b) To stimulate the baby’s cry, instead of slapping his bottom, lightly rub the soles of his feet. After removing the newborn’s secretions, stimulate the baby to start his cry.
- C) Newborn’s cry is usually loud and husky and if there is any abnormal cry as follows, then the newborn should be properly monitored such as,
- •>High pitch cry: = due to hypoglycemia and increased intracranial pressure,
Weak cry: = prematurity,
Hosacry: = laryngeal strider - 3)Care of cord
- Cord care is an important immediate care of the newborn.
- The newborn’s cord should be clamped within 30 seconds of birth and then cut properly.
- After the newborn is delivered, the newborn should be placed on the mother’s abdomen.
- Then the cord should be clamped properly from two opposite sites using a cord clamp.
- The first clamp should be placed 5 cm from the umbilicus, then the second clamp should be placed 2.5 cm from the first clamp.
- Then cut the cord properly between the two clamps.
- Do not apply anything to the cord, let it dry and fall naturally.
- The cord naturally falls off within seven to ten days after birth.
- Prevent the cord from getting wet with water and urine.
- If any discharge or bleeding is present in the cord, immediately assess the cord clamp and then loosen it properly.
- If the following signs and symptoms are seen from the cord, then immediately
- report such as,
- Foul odor coming from the cord,
- No discharge,
- Redness around the cord,
- The cord is wet,
- The cord does not fall down in 7-10 days,
- Inflammation,
- Fever etc.
- 4) Maintain position of the newborn
The newborn is usually prone to choke, cough and gag during the first 12-18 hours after birth. Therefore, the newborn should be provided with a proper position. - In which the fitters should provide a proper side-lying position so that the mucus can be removed and drained.
- 5) Identification and Banding
After the baby is born, put a proper identification band on the baby so that the baby can be properly identified. - 6) Eye Care
Clean the eyes of the newborn properly from the inner canthus to the outer canthus with sterile gauze.
If necessary, apply erythromycin or tetracycline eye ointment from the lower lid of the eyes. - 7) Attachment and Warmth (Bonding)
After the baby is born, place the baby on the mother’s abdomen so that bonding with the mother occurs and proper skin to skin contact can occur so that the mother and baby can be attached and the baby can be prevented from hypothermia. - 8) APGAR Score
APGAR score is the most important part of immediate newborn care.
APGAR score is assessed 1 minute after birth and then at 5 minutes.
In APGAR score, - A:= Appearance (Skin color),
P:=Pulse (Heart rate),
G:=Grimes (Reflux irritability),
A:=Activity (Muscle tone),
R:=Respiration (Respiratory efforts) - are assessed.
The total score of APGAR score is 0-10. - APGAR score at 1 minute after birth:
- If Apgar score is 7-10 then it is considered normal i.e. no depression in which the baby is provided normal post delivery routine care.
- If the APGAR score is between 4-6, it indicates mild depression in which the child needs assistance for breathing.
- If the APGAR score is between 0-3, it indicates severe depression in which the child needs resuscitation.
- APGAR score at 5 minutes after birth:
- If the APGAR score is between 7-10, it is said to be normal, but if the Apgar score is below 7, the baby needs to be monitored for another half hour.
- 9) Vitamin K:
The intestine of a newborn is sterile for some time after birth, that is, the bacteria that are responsible for manufacturing vitamin K are not present in its intestine, due to which the newborn cannot manufacture vitamin K, that is, vitamin K is responsible for a clotting factor. If this vitamin K is not present in the body of the newborn, then there are chances of clotting in the newborn, so as a prophylactic measure, artificial injection of vitamin K is provided to the newborn baby. - Dose:=
In pre-term:=0.5 ml,
Full term:= 1 mg.
Intra muscularl
b) Write the care of pregnant woman during eclamptic fit. એકલેમ્પટીક ફીટ દરમ્યાન સગર્ભા માતાની સંભાળ વિશે લખો.
- Care of the pregnant mother during eclamptic fits
- General Management
- Hospitalization
- The mother should be hospitalized in a hospital with properly well-equipped facilities.
- Rest:- Advise the mother to take adequate rest along with advising her to stop all activities and restrict visitors.
- Positioning: Advise the mother to take rest in the proper left lateral position to reduce vena cava compression and prevent the occurrence of heel spurs.
- History Collection: Collect a complete history of the mother including the frequency and duration of the fits and any medications the mother is taking.
- Sedation and then general examination Provide the mother with a proper drug and sedate her. Ex:=phenobarbiton 15-30 mg (TDS) Or Diazepam 1.5 mg (TDS).
- After the mother is properly sedated, perform a general and abdominal examination of the mother properly and quickly.
- Vital signs Note the mother’s vital signs every half hour
- including temperature, pulse, respiration, and blood pressure.
- If there is any abnormality in the vital signs or if the vital signs are raised above their normal range, treat them immediately.
- Urinary output
- Monitor the mother’s urine output every hour.
- Nutrition: Start the mother on 10% Dextrose to maintain the mother’s fluid, nutritional and calorie levels.
- Fluid should not increase by more than 2 liters in 24 hours.
- Additionally, to maintain the mother’s calorie levels, provide the mother with 50 ml of 5% Dextrose – at an interval of 8 hours.
- Specific Management or Medical Management
- Mothers with eclampsia can be treated by providing the following medications:
- a) Anticonvulsants,
- b) Antihypertensives,
- c) Sedatives,
- d) Diuretics,
- e) Antibiotics,
- f) Other medications.
- a) Anticonvulsant
- Magnesium sulphate (MgSO4) acts as the drug of choice to treat the condition of eclampsia. As it helps in preventing eclamptic fits in the pregnant mother.
- Magnesium sulphate can be administered both IV (intravenously) and IM (intramuscularly).
- Dose and route IM (intramuscularly):
- Initial dose: Initially 4 gm IV (intravenously) bolus, administer magnesium sulphate very slowly over 3-5 minutes.
- Continuous dose: Administer 5 gm magnesium sulphate IM (intramuscularly) every four hours in alternate buttock.
- IV (Intravenously)
- Initial Dose:
- Initial dose: 4-6 gm | Magnesium sulfate should be administered IV (iv) slowly over 15-30 minutes.
- Continuous Dose:
- 1-2 gm Magnesium sulfate should be administered IV (intravenously) every hour.
- Magnesium sulfate is a toxic agent and if not provided within therapeutic levels, it can cause a condition called deep tendon reflux. The therapeutic level of Magnesium sulfate (MgSO4) is 4-7 mEq/L (milliequivalents per litre). In case of magnesium sulfate (MgSO4) overdose, calcium gluconate is used as its antidote.
- Magnesium sulfate is administered only when there is no uric acid present, urine output is increased to more than 30 ml/hr and respiratory rate is more than 12/min.
- b) Anti Hypertensive
- Antihypertensives are used to control and reduce blood pressure.
- Ex:a) Hydralazine:
- 5 to 10 mg over 2 minutes.
- b) Labetalol:
- Initial dose: 20 mg slowly over 2 minutes. Then 40-80 mg IV over 10 minutes. Total dose should not exceed 300 mg.
- c) Sedatives- (Sedatives)
- Ex:=Diazepam
- Dose = 5-10 mg IV at a rate of 2-5mg/minute.
- Maximum dose: Do not increase more than 10mg.
- d) Diuteric-(Diuretic)
- Diuretic medication should be provided only when pulmonary AD is present during pregnancy.
- Ex:=Fusemide, Mannitol.
- e) Anti Biotics:
- Antibiotics are provided as prophylactic due to which the complications of pulmonary and pleural infections can be reduced.
- Broad spectrum antibiotic medication is used in these antibiotics.
- f) Other Medication:
- i) If pulmonary ED: Provide frusemide 40 mg IV followed by 10% Mannitol.
- ii) Heart Failure:
- Ex: Use Lasix and Digitalis medication.
- iii) Hyper pyrexia:
- Antipyretic medication is used.
Nursing Management of Eclampsia - Place the pregnant woman with eclampsia in a side-lying, padded, side-railed bed.
- Place a padded tongue blade between the teeth.
- Place the mother in a lateral position to avoid aspiration.
- Maintain a patent airway during convulsions and provide adequate amounts of oxygen to the mother.
- Monitor the mother’s oxygen level properly with pulse oximetry.
- Suction the mother’s mouth properly to remove oral secretions and any vomiting.
- Note the time and duration of the mother’s convulsions.
- Provide proper and regular prenatal care to the mother with pregnancy-induced hypertension.
- Protect the mother from self-injury.
- Keep the mother in a dark room to minimize stimuli such as bright light, noise, and visitors.
- Keep the foot side of the bed slightly elevated so that secretions from the respiratory tract can drain properly.
- Assess the mother’s vital signs, including the ED, fundal height, presentation and position of the fetus, and fetal heart sound, and test the urine for protein.
- Assess the mother’s urine output properly.
- Provide intravenous infusion of glucose saline and Ringer lactate solution as prescribed to maintain the mother’s fluid and nutritional levels.
- Advise the mother to maintain personal hygiene.
- Provide the mother with properly prescribed medications.
- Assess the mother’s uterine activity, cervical status, and fetal status as membranes may rupture and delivery may occur.
- Obstetric Management:
- Most often, when a woman has convulsions, she comes for labor. If labor has not started, then artificial membrane rupture, prostaglandin gel or oxytocin is done for induction of labor or caesarean section is also done. If the baby has died, then spontaneous labor is waited for.
- Continue to start the hypertensive regimen as prescribed during the postpartum period.
- Continuously monitor the mother for any complications other than eclampsia.
- Advise the mother to have regular follow-up.
c) Write about predisposing factors responsible for infertility. ઈનફર્ટીલીટી માટે જવાબદાર પરિબળો વિશે લખો.
- Factors responsible for infertility: –
There are three main causes of infertility.
1)Fault in female,
2)Fault in male,
3)Combined factors. - A) Ovarian Factors:
- This is mainly due to ovulatory dysfunction, the three reasons for which are as follows.
- a) Anovulation/Oligoovulation:
- Anovulation/Oligoovulation is usually seen due to disturbances in the hypothalamopituitary ovarian axis.
Ovarian activity depends on gonadotrophins and the normal secretion of gonadotrophins depends on GnRH (gonadotrophin releasing hormone) released from the hypothalamus. - (b) Luteinized Unruptured Follicle (LUF)
- (Trapped Ovum):
- This is seen due to inadequate growth and function of corpus luteum.
- (C) Trapped Ovum:
- In this, the ovum is trapped inside the follicles, usually due to endometriosis or hyperprolactinemia.
- 2) Tubal Factors:
- In this, infertility is usually due to tubopathy (tubal infection) due to which tubal functions are impaired.
- Ex:= Defective ovum is picked up and then infertility is seen.
- 3) Peritoneal Factor:
- In this, one and the main factor of infertility is endometriosis.
- 4) Uterine Factors:
- These include factors that prevent the fertilized ovum from implanting in the endometrium.
- These include factors such as,
a) Endometriosis,
b) Fibroid uterus,
c) Uterine hypoplasia,
d) Congenital malformations of the uterus. - 5) Cervical Factors:
- These include second degree uterine prolapse, retroverted uterus, and changes in the composition of the cervical nucleus.
- 6) Vaginal Factors:
- These include vaginal atresia, transverse vaginal septum,
- 2) Fault in Male :-
- 1) Due to defective spermatogenesis:
This causes infertility and is usually due to the following reasons:
Orchitis, undescended testicles, testicular toxins, primary testicular failure, genetic or chromosomal disorders such as 47,XXY, endocrine factors such as thyroid dysfunction. - 2) Due to obstruction of the afferent duct system:
- This is seen in two types.
1) Congenital:
Due to absence of vas deferens.
2) Acquired:
This is usually caused by some infections, tuberculosis, gonorrhea, and surgical trauma (during herniorrhaphy).
3) Failure to deposit sperm in vagina:
This is due to failure of sperm to deposit in vagina.
This can be due to:
Impotence,
Ejaculatory failure, hypospadias, bladder neck surgery.
4) Due to error in seminal fluid:
This can be due to immotile sperm, sperm count disturbance, low fructose count. - 3) Combined factor:
This is due to combined factors of both male and female.
Q-4 Write short notes. ટૂંકનોંધ લખો. (કોઈપણ ત્રણ)
a) Menstrual cycle – મેન્સ્ટુઅલ સાયકલ.
- A) Menstrual Cycle
Definition:
Menstruation comes from the word moon. Menstruation cycle is a visible cyclic process of physiological changes in the fertile female, which occurs in the endometrium of the uterus and results in bleeding from the vagina through the interconnection of hormones. Which is due to the HPO process
(H: Hypothalamus,
P: Pituitary Gland,
O: Ovaries). - Uterine Phase:
- The uterine phase is further divided into three phases:
- 1) Bleeding Phase (4 days
- 2) Proliferative Phase (10 days)
- 3) Secretory (14 days)
- 1) Bleeding Phase (4 days):
- When the ovum is not fertilized, the increased level of progesterone hormone in the blood causes vasoconstriction of the blood vessels of the endometrium (innermost layer of the uterus). Due to this, the blood supply to the endometrial layer of the uterine cavity decreases.
- And a condition of hypoxia arises due to which necrosis and death of the cells and tissues of the endometrial layer occurs. Now due to necrosis and death of these cells and tissues, the condition of hematometra (collection of blood in the uterine cavity) arises.
Due to this condition, the nerve supply goes to the hypothalamus, which then stimulates the pituitary gland. The pituitary gland releases oxytocin, which is responsible for uterine contraction.
Due to this uterine contraction, blood flow becomes visible at the vaginal site. And menstruation starts. It contains endometrial glands, endometrial cells, blood from capillaries and unfertilized ovum. When the level of decreased progesterone reaches a critical level, another ovarian follicle is stimulated by follicle-stimulating hormone (FSH) and the proliferative phase starts. - 2) Proliferative phase (10 days):
- The proliferative phase is also called the follicular phase. In this stage, due to follicle-stimulating hormone (FSH), the ovarian follicle grows and matures and produces estrogen.
- Estrogen stimulates the proliferation of the endometrium and prepares it to receive the fertilized ovum.
Thus, the endometrium becomes thick (about 2 to 3 mm) due to rapid cell multiplication. And due to the increase in the number of follicle-secreting glands and blood capillaries, ovulation occurs at the end of this phase due to the effect of luteinizing hormone (LH) and the production of estrogen decreases. - 3) Secretory phase (14 days):
- This phase is also called the luteal phase.
- Immediately after ovulation, the lining cells of the ovarian follicle are stimulated by luteinizing hormone (LH) and its corpus luteum is formed. Now this corpus luteum produces progesterone. Due to the effect of this progesterone hormone, the endometrium of the uterine cavity secretes more mucus from the secretory glands and becomes edematous i.e. thick (5 to 6 mm) and the endometrium provides a favorable environment for the implantation of the fertilized ovum.
Thus, the menstrual cycle is explained in two phases namely ovarian phase and uterine phase.
b) Episiotomy – એપીસીયોટોમી
- A surgically planned incision is made on the perineum and posterior vaginal wall during the second stage of labor, called an “episiotomy.” An episiotomy is performed to widen the vaginal opening for spontaneous or manipulative easy and safe delivery of the fetus. An episiotomy is performed to reduce excessive stretching and rupture of the perineal muscles and fascia and to reduce stress and strain on the fetal head.
- Objectives:
- To enlarge the vaginal opening for spontaneous or manipulative easy and safe delivery of the fetus.
- To reduce excessive stretching and rupture of the perineal muscles and fascia.
To reduce stress and strain on the fetal head. - Indications:
- Episiotomy is not routinely performed but only in cases where it is considered necessary. Its indications are as follows: When the perineum is rigid: In elderly primigravida, the presenting part cannot descend or is delayed.
- When there is a possibility of perineal tear: Big baby, face to pubic delivery, breech delivery, solder dystocia.
- Operative delivery such as forceps delivery, ventouse delivery.
- Previous perineal surgery: Pelvic floor repair, perineal reconstructive surgery.
- In mild indications – when there is a risk of perineal injury in primi gravida, when the perineum is rigid, when there is occiput posterior or face delivery.
- Timing of episiotomy: Just a few moments after crowning
- The ideal time is when the head is visible for 3 – 4 cm, when the perineum is thickened during contractions. It is given after the blades are inserted in forceps delivery.
- Advantages:
- Maternal:
- It is easy for repair and healing.
- The duration of the second stage is reduced.
- Trauma to the pelvic floor muscles is reduced. Therefore, prolapse and urinary incontinence do not occur.
- Protects the perineum from lacerations, tears and hematomas.
- Fetal:
- Fetal asphyxia can be prevented.
- Intracranial injury can be reduced in prematurity babies and breech babies.
- Disadvantages:
- Blood loss – 100-200ml through the episiotomy wound. Perineal trauma increases. Vulval hematoma and infection can occur.
- Pain.
- Types of Episiotomy Episiotomy is generally of four types, namely,
- 1) Medio-lateral
- 2) Median
- 3) Lateral
- 4) ‘J’ shape
- 1) Medio-lateral: In this, an incision is made from the midpoint of the foreskin to the right or left side, downwards and outwards. It is placed 2.5 cm from the anus.
- 2) Median: In this, the incision starts from the centre of the foreskin and extends posteriorly 2.5 cm to the midline.
- 3) Lateral: In this, the incision starts from 1 cm from the centre of the foreskin and extends laterally, which may cause injury to the Bartholin gland.
- 4)’J’ SEP: In this incision starts from the centre of the foreskin and is placed 1.5 cm posterior to the midline and then downwards and outwards
- at 5 or 7 o’clock position avoiding the anal sphincter.
- Articles and Supplies for Episiotomy:
- Episiotomy and Suturing Tray/ Articles:Local Anesthetic: Xylocaine or Lignocaine 1%.
- Syringe: 10ml.
- Needle g 18 to 21 one each.
- Episiotomy Scissors: 1.
- Dissecting Forceps: Toothed: 1.
- Needle Holder: 1.
- Straight Artery Forceps: 2.
- Myo Scissors: To cut the suturing material.
- Suturing Material: Chromic Catgut with Eyelets Round Body Needle.
- Cutting Needle: 1.
- Kidney Tray.
- A Pair of Sterile Gloves.
- Linen: The perineal sheet used to conduct delivery should be removed after completion of the 3rd stage of labour, and then another perineal sheet should be used for suturing. The sheet should be approximately 90 cm x 90 cm long and should cover the lower abdomen and the edge of the table. The whole sheet should be covered, exposing the vulva and vaginal outlet.
- Cotton Swabs: Place 10 to 30 (large size) cotton swabs in the bolus. They are used to clean and wipe the episiotomy and to use during suturing.
- Perineal pad: The pad is placed in the vagina to prevent blood from dripping into the suturing site and is kept with the cord facing outward. Another pad is used during suturing and must be removed before cleaning the vagina after suturing.
c) Post Partum Hemorrhage – પોસ્ટપાર્ટમ હેમરેજ
- Postpartum Hemorrhage (PPH)
- Postpartum hemorrhage is a condition in which excessive amount of bleeding occurs from the genital tract after the birth of the baby till the end of the postpartum period (the period after birth of the baby up to 6 weeks) which adversely affects the general condition of the mother, as evidenced by an increase in pulse rate and a fall in blood pressure. So this condition is called Postpartum Hemorrhage (PPH).
- If 500 ml or more is lost after vaginal delivery,
- 1000 ml or more after cesarean section,
- and,
- If 1500 ml or more is lost after cesarean hysterectomy, then this condition is called postpartum hemorrhage (PPH).
- •>Types of postpartum hemorrhage (PPH).
- There are two main types of postpartum hemorrhage:
- 1) Primary postpartum hemorrhage,
- 2) Secondary postpartum hemorrhage.
- 1) Primary postpartum hemorrhage: Bleeding that occurs within 24 hours after the birth of the baby is called primary postpartum hemorrhage. It usually occurs in the first two hours after delivery.
- There are two other types:
- a) Third stage hemorrhage
- b) True postpartum hemorrhage
- a) Third stage hemorrhage: Third stage hemorrhage occurs before the expulsion of the placenta.
- b) True postpartum hemorrhage: True postpartum hemorrhage occurs within 24 hours after the expulsion of the placenta.
- 2) Secondary postpartum hemorrhage: Bleeding that occurs after 24 hours after the birth of the baby and during the postpartum period (up to 6 weeks) is called delayed postpartum hemorrhage, late postpartum hemorrhage or secondary postpartum hemorrhage.
- •>1) Primary Postpartum Hemorrhage: Bleeding occurring within 24 hours after the birth of the baby is called primary postpartum hemorrhage. It usually occurs in the first two hours after delivery.
It has two other types: - a)Third stage hemorrhage
- b)True postpartum hemorrhage
a)Third stage hemorrhage:
Third stage hemorrhage occurs before the expulsion of the placenta. - b)True postpartum hemorrhage:
True postpartum hemorrhage occurs within 24 hours after the expulsion of the placenta. - Etiology of Primary Postpartum Hemorrhage:
- 1) Atonic uterus,
- 2) Traumatic,
- 3) Retained tissue,
- 4) Blood coagulation disorder.
- 1) Atonic Uterus:
- About 80% of postpartum hemorrhages are caused by atonic uterus.
- In this, after the placenta separates, the uterine sinus ruptures, due to which the uterine muscles do not contract and retract properly, and the building continues, which can lead to the condition of postpartum hemorrhage.
- It is seen in the following conditions:
- Grandma multipara,
- Multiple pregnancy,
- Hydroamnios,
- Over distension of the uterus in a large baby,
- Malnutrition and anemia,
- Antepartum hemorrhage, prolonged labor,
- Anesthesia,
- Use of oxytocin for induction or augmentation of labor,
- Malformation of the uterus,
- Uterine fibroids,
- Properly managed third stage of labor,
- Retained placenta
- 2) Traumatic: About 20% of postpartum hemorrhage (PPH) is caused by trauma to the genital tract after operative delivery and includes bleeding in the cervix, vagina, Perineum, paraurethral region gets involved and uterus gets ruptured.
- 3) Retained tissue: Due to bits of placenta and blood clot remaining in uterus, condition of postpartum hemorrhage can occur.
- 4) Blood coagulation disorder: Abruptio placentae, jaundice, thrombocytopenic purpura, HELLP syndrome, intrauterine death or sepsis.
- Signs and Symptoms of Primary Postpartum Hemorrhage:
- Vaginal bleeding is most often seen externally.
- The effects of blood loss depend on the pre-delivery hemoglobin level, the degree of hypervolemia, and the rate of blood loss.
- Changes in maternal vitals, i.e. blood pressure, are seen after a blood volume loss of 20 to 25%. Rarely, rapid blood loss can cause death within minutes.
- Abdomen Uterus: Contracted in traumatic hemorrhage and flaccid and hard to massage in atonic hemorrhage.
- Management of Primary Postpartum Hemorrhage: Postpartum hemorrhage is a major cause of maternal morbidity and mortality and cannot always be prevented, but its incidence can be reduced by identifying its risk factors.
- Measures to prevent postpartum hemorrhage:
- Antenatal:
- Make efforts to improve the health status of the woman to prevent anemia.
- Delivery of high risk multipara should be done in a well equipped hospital.
- Blood group of each patient should be done.
- Placenta accreta can be detected by ultrasonography or MRI of previous cesarean delivery.
- Delivery in morbid adherent placenta should be done by a senior obstetrician.
- Intranatal:
- Active management of the third stage can reduce postpartum hemorrhage by about 60%.
- If labor has been induced or augmented with oxytocin, give oxytocin infusion for at least one hour after delivery.
- In difficult labor or instrumental delivery, observe for utero-vaginal canal trauma after delivery.
- Observe for about two hours after delivery, checking whether the uterus is hard and contracted or not, and then send to the ward only after checking.
- Give local or epidural anesthesia in forceps, ventouse or breech delivery.
- In caesarean section, spontaneous separation of placenta and delivery should be done.
- Examination of placenta and membranes after delivery.
- Antenatal management:
- Assess the health status of the patient, especially the patient’s hemoglobin level should be maintained properly.
- If the hemoglobin level is maintained properly, any complications due to blood loss can be prevented.
- Transfer the mother who is at high risk to a well-equipped hospital.
- Intranatal management:
- Administer sedative and analgesic drugs during the intrapartum period.
- Avoid hasty delivery. The baby’s head is delivered. Then its trunk takes at least 2 to 3 minutes to be delivered.
- Manage the third stage care fully in high-risk patients.
- After delivery of the placenta, assess properly whether the placenta is completely delivered or not and assess whether any bits of placenta are retained in the uterus.
- Injection oxytocin is 10 units / IM or if 20-40 units, add oxytocin to 1000 ml normal saline or Ringer lactate solution and infuse.
- Explore the uterovaginal canal and note whether there is any trauma due to difficult labor or instrumental delivery.
- Keep the patient under observation for at least two hours after delivery.
- During that time, keep noting the mother’s vital signs continuously.
- Nursing Management of Third Stage Building or True Postpartum Hemorrhage:
- Call health care personnel for extra care.
- Administer two large gauzes of intravenous cannula.
- Send blood to laboratory for blood group and cross matching.
- Administer adequate amount of intravenous fluid to mother.
- Note mother’s vital signs properly.
- If bleeding is due to atonic uterus, gently rub fundus with finger tips.
- If soft and relaxed, gently massage fundus in circular motions to remove blood clots properly.
- If bits or clots of placenta are retained in uterine cavity, remove them properly.
- Further repeat the injection of oxytocin.
- To return the uterus to its tone, administer methyl PGF2 intramuscularly or transabdominally into the myometrium and repeat as needed.
- If the uterus is still atonic, perform manual compression.
- Apply pressure to the placental side during manual compression to control bleeding.
- Tight intrauterine packing under general anesthesia to control postpartum hemorrhage.
- If the above measures fail, hysterectomy is the last option.
- General steps for management of postpartum hemorrhage:
- Initiate intravenous therapy,
- Properly catheterize the mother.
- Start blood transfusion if necessary.
- Note whether the placenta is delivered properly and if not delivered, assess whether it is separate or unseparated.
- If the placenta is not separated, remove the placenta bimanually.
- If the placenta is undelivered but separated, assess where it is present in the uterine cavity. That is, assess whether it is present in the lower segment of the uterine cavity, in the cervix, or on the vagina.
- If the placenta is present in the lower segment of the uterine cavity, remove it by controlled cord traction.
- If controlled cord traction fails, perform bimanual compression and if that also fails, perform hysterectomy as a last resort.
- If the separated placenta is on the cervix or vagina, grasp and remove it. If that fails, remove the placenta by bimanual compression and if that also fails, perform hysterectomy as a last resort.
- If the placenta is delivered, remove the retained bits of placenta in the uterine cavity properly.
- If the placental clots cannot be removed, provide injection of Syntocin 40 IU International Unit 1 Liter Intravenous Infusion. Due to which the patient’s clots can be removed.
- Then assess the mother’s complete vital signs.
- Provide the mother with a properly comfortable position and advise her to take proper rest.
- Provide the mother with proper assurance.
- 2) Secondary Postpartum Hemorrhage:
- Bleeding occurring after 24 hours after the birth of the baby and during the postpartum period (up to 6 weeks) is called delayed postpartum hemorrhage, late postpartum hemorrhage or secondary postpartum hemorrhage.
- In this, the building up can usually occur between 8 and 14 days.
- Etiology of Secondary Postpartum Hemorrhage:
- Because of bits of cotyledons or membranes remaining in the uterine cavity,
- Because of infection,
- Because of endometritis,
- Because of subinvolution of the placental site,
- Because of caesarean section wound,
- Because of estrogen therapy,
- Because of cervical carcinoma,
- Because of placental polyps,
- Because of puerperal inversion of the uterus,
- Signs and symptoms of Secondary Postpartum Hemorrhage:
- Heavy lochia discharge that is bright red in color,
- Lochia discharge offensive,
- Fever,
- High pulse rate,
- Subinvolution of the uterus
- Anemia,
- Sepsis,
- Nursing Management of Secondary Postpartum Hemorrhage:
- Properly assess the amount of blood loss.
- Properly provide blood transfusion to the patient.
- Properly identify the cause of postpartum hemorrhage.
- Administer 10 units of oxytocin IM (intramuscular) or if intravenous (IV), add 20 units of oxytocin to 500 ml of normal saline or regurgitated solution and infuse to prevent postpartum hemorrhage.
- Properly provide antibiotic medication to the patient.
- Advise the patient to take complete bed rest.
- If the patient has any retained bits of placenta, remove them properly.
- If the patient is bleeding even in a minor amount, do not ignore it as it may be an alarm signal of post partum hemorrhage.
- Remove the retained product properly by sponge holding, ovum forceps or gentle curettage.
- If the bleeding is due to trauma to the cervicovaginal canal, control it with hemostatic sutures.
- If the patient’s delivery has taken place in an unhygienic environment, administer anti-tetanus serum and anti-gas gangrene serum to the patient.
- If the patient is anaemic, provide blood transfusion.
- Monitor the patient’s vital signs properly, initially every four hours and then twice a day.
- Provide the patient with ferrous gluconate (300 mg TDS) or ferrous sulfate (200 mg TDS) orally.
- Provide the patient with folic acid (5 mg) orally.
- Provide the mother with proper care and a comfortable environment.
- Advise the mother to take proper follow-up.
d) Uterine prolapse – યુટરાઇન પ્રોલેપ્સ
- Uterine: Uterus,
Prolapse: Displacement of an organ downward from its normal place. - Uterine prolapse is also known as prolapse.
- Uterine prolapse is a condition in which the uterus, uterine tissue, or a segment of the uterus protrudes (prolapses) downward into the vaginal canal. If the uterus protrudes into the vaginal canal, the condition is called uterine prolapse. If the uterus slips from its normal position and is displaced downward to some extent, the condition is called uterine prolapse. When the muscles and ligaments of the pelvic floor are stretched and weakened, the pelvic floor muscles are unable to properly support the uterus in its normal place. Due to this condition, the uterus slips downward from its normal place, that is, protrudes, and prolapses downward through the vaginal canal.
- Etiology:
- The uterus can prolapse downward due to stretching and weakening of the pelvic floor muscles, which cannot provide proper support to the uterine cavity.
- Due to multiple pregnancies,
- During vaginal delivery, due to any injury to the vagina and its supporting structures.
- Hormonal factors (such as the reduction in the amount of estrogen after menopause).
- Overstretching of the vaginal wall.
- Heavy weight lifting.
- Premature bearing down after delivery.
- Chronic constipation.
- Forceps application during delivery.
- Genetic factors.
- Obstetric trauma.
- Applying downward pressure on the fundus of the uterus to deliver the placenta.
- Age.
- Classification of Uterine Prolapse:
- Uterine prolapse is generally classified into two types, namely,
- Incomplete uterine prolapse,
- Complete uterine prolapse
- Incomplete uterine prolapse: In this incomplete uterine prolapse, the uterus usually protrudes partially downwards from its normal place, i.e. the uterus does not completely protrude through the vaginal opening to the external side.
- Complete uterine prolapse: In this condition of complete uterine prolapse, the uterus completely protrudes outside the vagina.
- Degree of Uterine Prolapse:
- Uterine prolapse is generally divided into four degrees, namely,
- 1)1st degree,
- 2)2nd Degree,
- 3)3rd Degree,
- 4)4rth Degree,
- 1)1st degree: In this first degree, the uterus protrudes (prolapses) up to the upper half of the vagina.
- 2)2nd Degree: In this second degree, the uterus prolapses up to the vaginal opening.
- 3)3rd Degree: In this third degree, the uterus protrudes outwards through the vaginal opening.
- 4)4rth Degree: In the fourth degree, the uterus completely prolapses through the vagina to the external side.
- Symptoms and signs:
- Tissues feel like they are protruding downward from the vaginal canal.
- Back pain.
- Dragging pain in the pelvis.
- Difficulty passing urine.
- Vaginal bleeding, discharge and infection are present.
- Dyspareunia.
- Incomplete evacuation of urine.
- Difficulty passing stool.
- These symptoms are caused by obesity, prolonged standing, straining, cuffing and lifting any heavy object, which increases abdominal pressure and aggravates the symptoms.
- Diagnostic Evaluation:
- History Collection,
- Physical Examination,
- Pelvic Examination to Identify the Condition,
- Vaginal Examination.
- Management:
- The management of uterine prolapse is usually done on the basis of 5 points such as,
- 1) Treatment is provided based on the severity of the patient’s symptoms such as mild, moderate and severe symptoms.
- 2) Treatment is provided based on the severity of uterine prolapse i.e. the stage at which uterine prolapse has occurred.
- 3) Based on the age of the patient.
- 4) Treatment is based on the health status of the female.
- 5) Treatment depends on future family planning.
- Whenever uterine prolapse is treated, its management is done keeping these five points in mind.
- Management of uterine prolapse is divided into three phases such as,
- 1) Preventive management,
- 2) Conservative management,
- 3) Surgical management.
- 1) Preventive management:
- Provide effective antenatal care to the patient such as,
- 1) Provide nutritional supplements in adequate amount to the patient.
- 2) Advise the patient to maintain proper antenatal hygiene.
- 3) Advise the patient to do proper relaxation exercises.
- 4) Advise the female to have a high fiber diet and plenty of water intake to reduce constipation.
- 5) Advise the patient to avoid heavy lifting.
- Provide proper intranatal care to the patient,
- 1) To prevent the patient from prolonged labor,
- 2) To prevent premature bearing down.
- Provide adequate postnatal care to the patient, such as,
- 1) Advise the patient to avoid fundal pushing.
- 2) Advise the patient for early ambulation.
- 3) Advise women to do pelvic floor exercises and Kegel exercises as these exercises increase the strength of the muscles and also strengthen the pelvic and uterine muscles which are loose and uterine prolapse can be prevented.
- 2) Conservative Management:
- Provide proper reassurance to the patient.
- Advise the patient to improve his nutritional status.
- Advise the patient to do pelvic floor exercises to strengthen the pelvic muscles.
- Providing Pessary Treatment to the Patient This pessary is a ring made of rubber or plastic i.e. it is a ring made of latex or silicone which is used to keep the uterus in its normal place. Pessary is available in different sizes and shapes according to the weight of the female. This pessary is used to place the prolapsed uterus in its normal place.
- 3) Surgical Management:
- The following surgeries are performed to repair the weakened pelvic floor muscles in the condition of uterine prolapse such as,
- Anterior colporrhaphy,
Colpoperineorrhaphy,
Pelvic floor repair (PFR),
Fothergills operation - Which is done in the case of cystocele, enterocele, rectocele.
- Vaginal hysterectomy with PFR (pelvic floor repair) This procedure is performed if there is uterovaginal prolapse.
- Cervicopexy
Le Fort operation. (Colpoclysis)
This procedure is performed in vault prolapse.
Q-5 Define following (any six) નીચેની વ્યાખ્યા લખો. (કોઈપણ છ)12
a) Vasa Previa – વાસા પ્રિવિયા
- Vasa previa is an obstetric complication in which the fetal blood vessels pass through or near the internal orifice of the uterus and are in front of the presenting part. When the supporting membrane ruptures, these vessels are at risk of rupture because they are unsupported by the umbilical cord or placental tissue. These complications can arise during labor and delivery.
b) Mechanism of labour – મીકેનીઝમ ઓફ લેબર
The series of passive movements of the fetus as it passes through the birth canal is called the mechanism of labor. The principal movements in this are of the head. The changes in the fetal head position as the fetus passes through the birth canal are called cardinal movements. And these cardinal movements are usually seen during the second stage of labor.
c) Implantation – ઈમ્પ્લાન્ટેશન
Implantation is the process in which the zygote from the fallopian tube attaches to the endometrium of the uterine cavity to develop.
The process of implantation starts 4 to 5 days after the formation of the zygote and is completed by 11 days.
After the formation of the zygote, the zygote remains in the fallopian tube for four days and then it implants in the uterine cavity.
d) Dysmenorrhea – ડિસ્મેનોરિય
Dysmenorrhea, also known as painful periods or menstrual cramps, is a condition of pain during menstruation. Dysmenorrhea is a term describing painful menstruation, which usually includes cramps caused by uterine contractions.
Types of Dysmenorrhea:
There are generally two types of dysmenorrhea, namely:
1) Primary or Spasmodic,
2) Secondary or Congestive
1) Primary or Spasmodic:
It is a condition of painful menstruation with no identifiable pelvic pathology.
Highest levels occur in the first 2 days of menstruation.
2) Secondary or Congestive:
Painful menstruation occurs due to pelvic or uterine pathology.
e) Molding – મોલ્ડીંગ
As the fetus passes through the birth canal, the head of the fetus undergoes changes in shape due to resistance from the birth passage. This is called “molding”.
During this process, the parietal bone overlaps with adjacent bones such as the occipital bone at the back, the frontal bone at the front, and the temporal bone at the side. The right parietal bone at the vertex overrides the left parietal bone. Molding disappears within a few hours after birth.
Grading:
Grade:= 1 (The bones touch each other but do not overlap).
Grade:= 2 (The bones overlap but are easily separated).
Grade:= 3 (The bones are fixedly overlapping).
f) Breech presentation – બ્રીચ પેઝન્ટેશન
Breech presentation is the most common malpresentation of the fetus in the uterine cavity in which the lie of the fetus is longitudinal but the breech (buttocks) is the presenting part in the pelvic breech.
Attitudes/Classifications/Variety of Breech Presentation
There are mainly two types of breech presentation.
1) Complete
(Flexed Breech),
2) Incomplete
There are three other types of incomplete.
a) Breech with extended legs (Frank Breech).
b) Footling Presentation.
C) Presentation
1) Complete (flexed breech),
In it, the normal attitude of full flexion is maintained. In complete breech, the legs of the fetus are bent at the hips and the feet are bent at the knees and the feet are presented with the buttocks of the fetus.
In which the presenting parts are:
2 buttocks,
External genitalia,
And 2 feet.
2) Incomplete
In incomplete, the legs are in the podelic pole or in different degrees of extension.
There are three other types of incomplete.
a) Breech with extended legs (Frank breech).
b) Footling presentation.
C) Knee Presentation
a) Breech with Extended Legs (Frank Breech).
In this condition, the legs of the fetus are extended with the breech, i.e. the feet of the fetus are bent over the trunk of the fetus and the legs are straight from the knee. The presenting part consists of 2 buttocks and external genitalia. This condition is more common (70%) in primigravida.
b) Footling Presentation:
In footling presentation, both feet and legs are partially extended, with one or both legs being the presenting part.
C) Breech Presentation:
In breech presentation, the knee is extended but the knee is flexed, presenting in a breech position.
g) Ectopic pregnancy – એકટોપીક પેગનન્સી
When a fertilized ovum implants and develops outside the normal endometrial cavity, it is called an ectopic pregnancy.
Anatomical site of implantation of ectopic pregnancy:
Tubal pregnancy is more common, normally occurring in the right fallopian tube than in the left fallopian tube. The ampulla of the fallopian tube is the most common site of implantation of an ectopic pregnancy.
If an ectopic pregnancy occurs at the isthmus of the fallopian tube, it is considered a dangerous site, which can also lead to tubal rupture.
h) Spermatogenesis – સ્પર્મેટોઝીનેસીસ
The development of spermatids from primordial male germ cells and their subsequent differentiation into spermatozoa is called spermatogenesis. That is, the development and maturation of sperm is called spermatogenesis.
Q-6(A) Fill in the blanks – ખાલી જગ્યા પૂરો
1.Ovulatory function is stimulated by……..hormone Luteinizing hormone (LH) ઓવ્યુલેટરી કાર્ય ……હોર્મોન દ્વારા ઉત્તેજીત થાય છે. . લ્યુટિનાઈઝિંગ હોર્મોન (LH)
2.Bluish discoloration of vagina occur during pregnancy is called ……..sign. Chadwick’s sign
પ્રેગનન્સી દરમ્યાન વજાઈનામાં બ્યુઈશ ડીસકલરેશન થાય તેને…… સાઈન કહેવાય છે. ચેડવિક્સ સાઈન
3………..hormone is responsible for the male sex characteristics. Testosterone મેલ સેકસની લાક્ષણિકતા માટે…….. હોર્મોન જવાબદાર છે. ટેસ્ટોસ્ટેરોન
4.Abnormal opening between bladder and vagina is called……….. Vesicovaginal fistula (VVF) બ્લેડર અને વજાઈના વચ્ચેના અસામાન્ય ઓપનીંગને ………..કહે છે. વેસીકોવેજાઈનલ ફિસ્ટુલા (VVF)
5.The red color present in Lochia is known as……… Lochia Rubra લોકીઆમાં લાલ કલરની હાજરીને ………તરીકે ઓળખાય છે. લોકીઆ રુબ્રા
B) True or False – ખરા ખોટા જણાવો. ❌✅
1.Crowning seen during third stage of labour. ક્રાઉનીંગ લેબરના ત્રીજા તબકકા દરમ્યાન જોવા મળે છે. ❌ કારણ: Crowning occurs during the second stage of labor, when the fetal head becomes visible at the vaginal opening and does not recede.ક્રાઉનીંગ લેબરના બીજા તબકકા દરમિયાન થાય છે, જ્યારે ભ્રૂણનું માથું વજાઇનલ ઓપનિંગ પર દેખાય છે અને પાછું ખેંચાતું નથી.
2.Ovum is a largest cell of human body. ઓવમ એ માનવ શરીરનો સૌથી મોટો કોપ છે. ✅કારણ: The ovum is the largest cell in the human body, visible to the naked eye, and plays a crucial role in reproduction. ઓવમ માનવ શરીરનો સૌથી મોટો સેલ છે, જે નગ્ન આંખે દેખાઈ શકે છે અને પ્રજનન માટે મહત્વપૂર્ણ ભૂમિકા ભજવે છે.
3.HCG hormone is responsible for positive pregnancy test. HCG હોર્મોન એ પોઝીટીવ પ્રેગનન્સી ટેસ્ટ માટે જવાબદાર છે. ✅ કારણ: Human chorionic gonadotropin (HCG) is the hormone detected in urine or blood for confirming pregnancy in pregnancy tests. HCG હોર્મોન પ્રેગનન્સી પરીક્ષણમાં યુરિન અથવા રક્તમાં શોધી શકાય છે, જે પ્રેગનન્સીની પુષ્ટિ કરે છે.
4.PPH means more than 500 ml blood loss occurs after normal delivery. નોર્મલ ડીલીવરી બાદ ૫૦૦ ml કરતા વધારે બ્લડ લોસ થાય તો તેને PPH કહે છે. ✅કારણ:Postpartum hemorrhage (PPH) is defined as blood loss exceeding 500 ml following a vaginal delivery or 1000 ml after a cesarean section. – PPH નો અર્થ છે કે નોર્મલ ડિલિવરી પછી 500 ml થી વધુ અથવા સીઝેરિયન પછી 1000 ml થી વધુ રક્ત ગુમાવવું.
5.Umbilical artery carries oxygenated blood. અમ્બેલીકલ ઓર્ટરી ઓક્ષીજનેટેડ બ્લડ નું વહન કરે છે. ❌કારણ:The umbilical artery carries deoxygenated blood from the fetus to the placenta for oxygenation, while the umbilical vein carries oxygenated blood to the fetus. અમ્બેલીકલ ઓર્ટરી ડીઓકિસજનેટેડ બ્લડ ભ્રૂણથી પ્લેસેન્ટા સુધી લઈ જાય છે, જ્યારે અમ્બેલીકલ વેઇન ઓક્ષીજનેટેડ બ્લડ ભ્રૂણ સુધી લઈ જાય છે.
(C) Multiple Choice Questions નીચેના માંથી સાચો વિકલ્પ લાખો.
1.Which hormone is produced by corpus luteum – કોર્પસ લ્યુટીયમ દ્વારા કયો હોર્મોન ઉત્પન થાય છે.
a) LH-
b) TSH –
c) estrogen – ઈસ્ટ્રોજન
d) Progestron – પ્રોજેસ્ટ્રોન
કારણ: The corpus luteum produces progesterone, which supports the endometrium and maintains pregnancy.કોર્પસ લ્યુટીયમ પ્રોજેસ્ટ્રોન ઉત્પન્ન કરે છે, જે એન્ડોમેટ્રિયમને સપોર્ટ કરે છે અને ગર્ભધારણ જાળવે છે.
2.Drug of choice in eclampsia is – એકલેમ્પસીયામાં ડ્રગ ઓફ ચોઈસ છે.
a) Diazepam – ડાયઝેયામ
c) Mgso4 – મેગ્નેશીયમ સલ્ફેટ
કારણ: Magnesium sulfate is the drug of choice for preventing and treating seizures in eclampsia.-મેગ્નેશિયમ સલ્ફેટ એકલેમ્પસીયામાં દર્દીને ખંચકારા થવાનું રોકવા અને સારવાર માટે ઉપયોગી છે.
b) Phenergan – ફીનારગન
d) Phenobarbitone – ફિનોબારબિટોન
3.How much weight of non-pregnant uterus? નોન પ્રેગનેન્ટ યુટ્સનુ વજન કેટલુ હોય છે?
a) 30 gm – 30 ગ્રામ
b) 40 gm – 40 ગ્રામ
c) 60 gm – 60 ગ્રામ
કારણ: The weight of a non-pregnant uterus is approximately 60 grams, which increases significantly during pregnancy.ગર્ભાવસ્થાની પહેલાં નોન-પ્રેગ્નન્ટ યુટ્રસનું વજન આશરે 60 ગ્રામ હોય છે.
d) 100 gm – 100 ગ્રામ
4.The creamy substance on the new born is known as – ન્યુ બોર્નની સ્કીન ઉપરના ક્રીમી સબસ્ટન્સને કહેવાય છે.
a) Amniotic Sac – એમ્નીઓટીક સેક
b) Normal Skin – નોર્મલ સ્કીન
c) Vernix Caseosa – વનિર્ક્ષ કેસીઓસા
કારણ: Vernix Caseosa is a protective creamy substance covering the newborn’s skin, preventing dryness and infection.વર્નિક્સ કેસીઓસા ન્યુ બોર્નના ત્વચા પર રક્ષણાત્મક ક્રીમી પદાર્થ છે, જે ત્વચાને શોષાયી જવાથી અને ચેપથી બચાવે છે.
d) Lanugo – લેનુગો
5.Golden color of amniotic fluid indicates – ગોલ્ડન કલરનું એમનીઓટીક ફ્લૂઇડ સુચવે છે.
a) Fetal hypoxia – ફિટલ હાઈ પોક્ષિયા
b) Fetal distress – ફિટલ ડીસ્ટ્રેસ
c) Maternal distress – મેટરનલ ડીસ્ટ્રેસ
d) RH incompatibility – આર. એચ ઇનકોમ્પીટીબીલીટી
કારણ: Golden amniotic fluid suggests RH incompatibility, which may result in hemolysis and bilirubin buildup.–ગોલ્ડન એમ્નિયોટિક ફ્લૂઈડ આર.એચ. ઇનકોમ્પીટીબીલીટીને દર્શાવે છે, જે હિમોલિસિસ અને બિલીરુબિન વધારાને કારણે થાય છે.
