ENGLISH-MIDWIFERY AND GYNECOLOGICAL NURSING-2023 (PAPER NO.6 UPLOAD)
ENGLISH-MIDWIFERY AND GYNECOLOGICAL NURSING-2023-PAPER NO.6

09/10/2023
Q-1-
a. Define Involution of uterus – ઇન્વોલ્યુશન ઓફ યુટ્રસ ની વ્યાખ્યા આપો.
- After delivery, the uterus appears soft and hard. Involution is a process in which the reproductive organs, especially the uterus, return to their normal pre-pregnancy state.
- The rate of involution of the uterus is assessed by the fundal height. While taking the fundal height, the mother is asked to empty the bowel and bladder, so that the fundal height does not increase.
- Rate of involution:– There is no change in the height of the uterus in the first 24 hours after delivery, from the 2nd to the 11th day the fundus descends by 1.25 and on the 11th day it becomes a pelvic organ.
b.Enlist Post-Partum complications પોસ્ટપાર્ટમ કોમ્પ્લીકેશનન્સની યાદી બનાવો.
- The following complications are seen during the postpartum period.
- 1.Puerperial pyrexia:– In this condition, the mother’s body temperature is 100.4 °F or higher.
- 2.Puerperial sepsis:– A postpartum complication in which there is an infection within the genital tract.
- 3.Breast engorgement:– It is a condition in which the breasts become painfully full due to overfilling of milk. Which is caused by an imbalance between milk supply and infant demand.
- 4.Mastitis:– This is a condition in which there is an infection within the breast tissue.
- 5.Urinary tract infection:– Microorganism reserve occurs due to urine stasis during pregnancy and urinary tract infection is seen during the postpartum period due to inadequate hygiene.
- 6.Thrombosis:– Thrombosis is a common and important complication seen in postpartum period, and it is commonly seen in leg veins and pelvic veins.
- 7.Post partum hemorrhage:– When blood loss is more than 500ml during normal vaginal delivery and more than 1000 ml during cesarean section, the condition is called PPH.
- PPH is the most common cause of maternal mortality.
- 8.Subinvolution of uterus:– When the process of involution of uterus is impaired or retarded, it is called sub involution of uterus.
- 9.Post partum blues: – It is generally seen during the first three to seven days of postpartum, in which the mother feels irritable, sad, cries more easily, confused.
- 10.Post partum Depression: – When the symptoms of postpartum blues are seen for more than six weeks, then it converts into depression and suicidal tendencies increase in the mother.
c. List out latest trends in midwifery practice. મીડવીફરી પ્રેકટીસના લેટેસ્ટ ટ્રેન્ડસની યાદી બનાવો.
- 1.Technological advances:– Nowadays, the use of sophisticated computers has increased and nursing personnel are using it, due to which new technology has been established. Due to advanced technology, knowledge in nursing personnel has also increased. High technology is a challenge for future nurses.
- 2.Increased cost of high tech care:– Due to high and sophisticated technology, the cost has also increased. A good amount has to be paid for obstetric procedures. Slowly obstetric care is becoming a business for care providers.
- 3.Changing patterns of child birth:– Nowadays, early marriage practice continues, due to which younger mothers become pregnant, due to which complications like preterm labor and low birth weight etc. are seen during pregnancy. Due to which a change is seen in the birth pattern of the child.
- 4.Perinatal risk factors:– 30 to 40% of low birth weight babies are seen in developing countries and other perinatal risk factors include factors like mother’s age, medical history, past pregnancy, socioeconomic status and prenatal care.
- 5.Family centered care:– Maternity care has been enhanced. Due to family centered care, the emotional bonding between mother and baby increases and the over-anxiety of mother and father and their family is reduced.
- 6.Rising cesarean birth rates:- As the rate of fetal monitoring and prenatal monitoring ultrasound has increased, the cesarean birth rate has also increased.
- 7.Increasing the number of intensive care units: – Emphasis has also been placed on the care of infants and children. Intensive care units have also been increased for many infants and children who are low birth weight or ill and need critical care.
- 8.Increasing use of alternative treatment modalities: – Health care providers are making the public aware about alternative treatment modalities such as meditation, exercise, herbal therapy, etc.
- 9.Early discharge: – If no complications are found in the mother and baby after delivery, then they are discharged early, so that other infections can be prevented.
- 10.Role of fathers: – Fathers are explained about parental bonding, so that the emotional bonding between the child and the father improves.
Or.
A.Define P.P.H- પી.પી.એચ. ની વ્યાખ્યા આપો.
- When blood loss exceeds 500ml during normal delivery and exceeds 1000ml during cesarean section, the condition is called postpartum hemorrhage.
- If PPH occurs within 24 hours of delivery, it is called primary PPH. And when it occurs after 24 hours and up to 6 weeks, it is called secondary PPH.
- Postpartum hemorrhage is the most common cause of maternal mortality.
b. Write down cause of primary P.P.H -પ્રાયમરી પી.પી.એચ ના કારણો લખો.
- When PPH occurs within 24 hours after delivery, it is primary PPH.
- The causes of primary PPH are as follows.
- Tone:- Severe hemorrhage and hypovolemic shock are seen due to uterine atony and contraction and refraction failure of myometrial muscle fibers.
The causes of uterine atony are as follows,
Multiple pregnancy
Fetal macrosomia
Polyhydroamnios
Terrain structure abnormality - Tissue:- Incomplete detachment and expulsion do not occur due to which the tissue of the placenta remains retained there, due to which bleeding is seen due to continuous contraction and retraction. The causes of retained placenta are as follows.
Succenturiate placenta
Abnormal placenta
Plasta accreta
- 3.Trauma:- When trauma occurs inside the genital tract during delivery, it is also a cause of PPH. The causes of trauma are as follows.
- Prolonged labor
- Cephalopelvic disproportion
- Forceps delivery
- Vacuum delivery
- Extension of episiotomy
- 4.Thrombosis:- Due to bleeding disorder, platelets fail to form a clot against bleeding and bleeding is seen due to continuous contraction and retraction. And blood vessel thrombosis does not occur due to which PPH is seen.
c. Write down management of primary PPH-પ્રાયમરી પી.પી.એચ નું મેનેજમેન્ટ લખો.
- Management of Postpartum Hemorrhage (PPH):
- Postpartum hemorrhage is a condition in which excessive amount of bleeding occurs from the genital tract after the birth of the baby till the end of the postpartum period (period up to 6 weeks after birth of the baby) which adversely affects the general condition of the mother, as evidenced by increased pulse rate and fall in blood pressure. This condition is called Postpartum Hemorrhage (PPH).
- If there is excessive bleeding of 500 ml or more after vaginal delivery,
1000 ml or more after cesarean section, then it is called Postpartum Hemorrhage. - Management of Postpartum Hemorrhage:
- Postpartum hemorrhage is a major cause of maternal morbidity and mortality, hence proper and effective management of postpartum hemorrhage is important to prevent complications.
- Management of postpartum hemorrhage involves a systemic approach which involves controlling bleeding, stabilizing the mother, and identifying the cause of postpartum hemorrhage.
- 1) Immediate Action:
- Early Recognition Early identification of signs and symptoms of postpartum hemorrhage such as excessive bleeding (more than 500 ml if vaginal delivery and more than 1000 ml if cesarean section), tachycardia, hypotension, pallor and signs of shock.
- Call for help Notify senior obstetrician, anesthesiologist and other necessary health care personnel to assist in the management of postpartum hemorrhage.
- Assessment Quantity of Blood Loss Proper assessment of the amount of blood loss.
- Clinical Assessment Perform a focused clinical examination to assess uterine tone, size, and any signs of trauma and to assess whether retained product is present.
- Establish Intravenous (IV) Access Establish large-sized intravenous (IV) access for rapid fluid administration and medication administration in women with postpartum hemorrhage.
- Oxygen Administration Provide supplemental oxygen to maintain tissue oxygenation.
- 2) Pharmacological Management
- Uterotonic Medication Administer uterotonic agents to stimulate uterine contractions and control bleeding.
- Oxytocin Oxytocin is the first-line agent in which a bolus dose of 10 to 40 units in 1 liter of crystalloid solution should be given as an infusion over 10 to 30 minutes.
- Followed by infusion of 40 units in 1 liter of IV fluid over 4-6 hours.
- See Misoprostol If oxytocin is not available, administer 800 mcg rectally and 600 orally.
- 3) Non-pharmacological management:
- Uterine massage Gently massage the uterine fundus to enhance uterine contractions and control bleeding.
- Balloon Tamponade In postpartum hemorrhage, if bleeding continues even after administration of uterotonic drugs and uterine massage, balloon tamponade (Bakery balloon and Follis catheter) should be used to apply pressure against the uterine wall to achieve hemostasis and control bleeding.
- 4) Surgical Intervention
- Manual Removal of Placenta If placental tissue is suspected to be present in the uterine cavity, the placenta should be removed manually under anesthesia.
- Compression Sutures To mechanically compress the uterus and to control bleeding, uterine compression sutures should be applied.
- Uterine Artery Ligation Uterine artery ligation is performed as a surgical option in some cases to reduce blood flow to the uterus. Hysterectomy Hysterectomy is performed as an emergency measure when bleeding cannot be controlled by other measures and the patient’s condition is deteriorating.
- 5) Supportive Care and Monitoring:
- Fluid Administration
Administer adequate intravenous fluids to improve the patient’s tissue perfusion, such as:
Normal saline
Or Ringer lactate solution. - Blood Transfusion When excessive bleeding occurs, provide blood transfusions as needed.
- Monitoring
Continuously monitor the patient’s vital signs, urine output, and level of consciousness. - Repeat hematological and biochemical tests to assess response to treatment.
- Psychological Support Postpartum hemorrhage (PPH) is a traumatic condition, so proper psychological support should be provided to the patient and her family members.
- 6) Prevention
- Antenatal Care Early identification of risk factors for postpartum hemorrhage during the antenatal period so that early management can be done and complications can be prevented.
- Active management of third stage of labor Use of prophylactic uterotonic medication to prevent postpartum hemorrhage and reduce the risk of uterine atony.
- Skilled birth attendance Trained personnel should be available to immediately recognize and manage obstetric emergencies.
- 7) Follow-up and Documentation:
- Advise the patient for proper follow-up after post-partum care so that recovery can be monitored and if the patient has an anemic condition, it can also be assessed.
- Properly document the event, the interventions performed for it, and the patient’s response to treatment, etc.
- Thus, proper management of postpartum hemorrhage is important to prevent complications due to conditions such as postpartum hemorrhage in women after childbirth.
Q-2
a. Write down signs of onset of labour .લેબર શરૂ થવાના ચિહ્નનો લખો
- Signs of Onset of Labor:
- 1) Painful Uterine Contractions (Labor Pain)
- 2) Show
- 3) Progressive Dilatation and Effacement of Cervix
- 4) Formation of “Bag of Water”
- 1) Painful Uterine Contractions (Labor Pain):
- Throughout pregnancy, painless Braxton Hicks contractions occur with simultaneous hardening of the uterus. The character of these contractions changes, becoming more powerful, intermittent, and associated with more pain. The pain is usually felt in the front of the abdomen and radiates to the back. Contractions are the first sign of labor pain. Initially, the woman experiences one or two contractions per hour which increase in frequency (initially these are tolerable).
- The contractions may become more intense over a period of 6-8 hours. After that, the active phase of labor begins. In this, the contractions become more severe and occur every 2-3 minutes and last for 45 to 60 seconds. During this period, it is very difficult for the woman to relax because the intense nature of the pain is accompanied by rapid dilation of the cervix. Furthermore, the contractions do not occur very often but are more intense. Finally, the woman experiences intense contractions between 60-90 seconds. And more regularly occur at intervals of every 2-3 minutes. This is the stage of labor called hard labor where the cervix dilates up to 10 cm.
- 2) Show:
- In pregnancy, the operculum (cervical mucus plug) forms and comes out as a bloodstained mucoid discharge a few hours before or with labor, which is called “show”.
- Rupture of the capillary vessels of the cervix and stretching of the lower uterine segment cause blood to ooze from the raw decidual surface.
- 3) Progressive dilatation and effacement of cervix:
- The effective force of the first stage is painful uterine contractions. Due to these painful uterine contractions, the cervix progressively dilates and effaces.
- The cervix dilates to about 10 cm.
- The muscle fibers around the internal os are pulled upwards by the retracted upper segment, thus the cervix shortens and then merges with the lower uterine segment and becomes part of it and gradually effacement of the cervix occurs.
- 4) Formation of “bag of water”:
- Dilatation of the lower uterine segment causes the chorion to detach. The loose part of this fluid bulges into the dilating internal os. The amniotic fluid in front of the head is fixed in the cervix which is called fore water. Fore water helps in effacement of the cervix and early dilation of the os. The hind water maintains a uniform pressure in the uterus during uterine contractions, thus providing some protection to the fetus and placenta. In this way, the pressure during contractions does not come on the fore water which is called general fluid pressure.
- For example: When the membranes are intact, the pressure of uterine contractions comes on the fluid and remains uniform throughout the uterus.
b. Define third stage of labour and write down active management of third stage of labour (AMTLS) થર્ડ સ્ટેજ ઓફ લેબરની વ્યાખ્યા આપો તથા લેબરના થર્ડ સ્ટેજનું એકટીવ મેનેજમેન્ટ લખો.
- The third stage of labour is the period after the birth of the baby, where the placenta and membranes are completely expelled. This stage is very important for the health of the mother and usually lasts for 5 to 30 minutes.
- Management of the third stage of labour:
- The management of the third stage is the most crucial because it involves the separation and expulsion of the placenta from the uterine cavity, and the third stage aims to prevent complications of postpartum haemorrhage.
- The management of the third stage requires strict vigilance of the placenta, due to which complications of postpartum haemorrhage can be prevented.
- Stages of management Currently, two methods are used in the management of the third stage.
- 1) Expectant (Watchful) Management
- 2) Active Management
- 1) Expectant (Watchful) Management
- In this management, the separation of the placenta and its descent into the vagina are allowed to occur spontaneously.
- For this management, minimal assistance is given for placental expulsion.
- In this stage, the mother is constantly watched, i.e. the mother is not left alone even for a short time.
- If the mother is in a lateral position, then she is given a dorsal position, due to which the signs of placental separation and the amount of blood loss can be properly observed.
- In this management, only the separation, descent and expulsion of the placenta are properly observed.
- One hand is placed on the fundus so that,
- a) the separation of the placenta can be observed.
- b) The state of uterine activity i.e. contraction and relaxation can be understood.
- Separation of placenta
- The placenta starts separating from the uterine wall within a few minutes after the birth of the baby, so wait for 15 to 20 minutes for the placenta to separate on its own.
- No touch technique is used in this.
- In this, there is a “no touch policy” i.e. the placenta is expelled due to gravity in 15-20 minutes i.e. no massage on the fundus.
- Do not use any type of uterotonic and do not use any manual method for expulsion of the placenta.
- Expulsion of Placenta
When the placenta is expelled, the following points should be followed: Advise the patient to apply a downward forceps when the uterus is hard.
Raised intra-abdominal pressure is important for expulsion of the placenta.
And the placenta can be expelled spontaneously. - 2) Active Management
- 1) Use of uterotonics Oxytocin is the drug of choice in the management of the third stage of labor.
- Provide 10 units of oxytocin IM (intramuscularly) in the management of the third stage.
- Oxytocin helps in expulsion of the placenta by enhancing uterine contractions.
- 2) CCT (Control Cord Traction) Controlled cord traction uses a manual method in which the umbilical cord is tracked and pulled downward and backward gently, due to which the placenta separates from the uterine wall and can then be expelled. However, controlled cord traction is performed when uterine contractions are present by placing the hand on the suprapubic area.
- 3) Delayed cord cutting Wait for one to three minutes after delivery of the fetus and then cut the umbilical cord. This technique is more useful in term newborns. Because the newborn can receive adequate amount of blood from the placenta, due to which the condition of anemia can be prevented.
- But in preterm babies, the liver is immature and there is a high rate of breakdown of red blood cells and if the cord cutting is done late, then due to this, the condition of hyperbilirubinemia (jaundice) can arise in the newborn.
- 4) Postpartum vigilance After the delivery of the placenta, the placenta should be properly inspected, including the cotyledons, lobes and maternal and fetal sites, and then fundal massage should be done after the delivery of the placenta, due to which the continuity of uterine contractions can be maintained and if there are retained bits of placenta, they can be properly expelled.
OR
a.Describe nursing responsibility during administration of oxytocin drugs. ઓક્સિટોસીન ડ્રગ્સ આપતી વખતે નર્સની જવાબદારીઓ લખો.
- Responsibilities of the nurse while administering injectable oxytocin during labor:
- Administering injectable oxytocin during labor is a critical responsibility for the nurse. Although oxytocin plays an important role in facilitating labor and managing labor progression, the nursing responsibilities for oxytocin administration are as follows.
- 1) Assessment and Preparation
- Before administering injectable oxytocin, the nurse should properly assess the pregnant woman’s labor progression, fetal heart rate, and uterine contractions, and maternal vital signs. Due to which the medication can be properly initiated and continued.
- Preparation Prepare oxytocin solution properly as per hospital protocols and as prescribed by health care personnel.
- 2) Monitoring
- Uterine Contraction Continuously monitor uterine contractions by palpation method and assess whether uterine contractions are occurring regularly and properly.
- Fetal Heart Rate Continuously monitor fetal heart rate and assess whether there are any signs and symptoms of fetal distress.
- 3) Administration
- Initiation and Adjustment
- Properly administer medication as prescribed by health care provider.
- Keep infusion rate low initially and then increase infusion based on uterine contractions and labor progression.
- 4) Patient Education
- Explanation Provide an explanation to the mother and her support person about the purpose of oxytocin infusion, its side effects, and continuous monitoring.
- Expectations Provide an explanation to the mother and her support person about what to expect after giving oxytocin, such as an increase in the intensity and frequency of uterine contractions.
- 5) Documentation
- Charting Document the administration of oxytocin, including starting time, infusion rate, maternal vital signs, uterine contraction patterns, and continuous charting of fetal heart rate.
- Response to Treatment
After oxytocin infusion, monitor uterine contractions properly to assess the effectiveness of oxytocin and assess how progressive labor is.
And assess whether there are any side effects of oxytocin. - 6) Communication: Communicate with other healthcare personnel for oxytocin administration, such as,
Collaborate with obstetricians, midwives, and other nurses. - Patient Updates Provide ongoing patient updates to the mother and her support person, including information on labor progress, fetal well-being, and any changes after oxytocin administration.
- 7) Emergency Response: If any side effects are observed during the administration of oxytocin and other symptoms such as uterine hyperstimulation are observed, oxytocin should be discontinued immediately and supportive care should be provided.
- Thus, there is a need to perform such nursing responsibilities while providing injectable oxytocin.
b. What is contracted pelvis describe the management of contracted pelvis કોન્ટ્રાકટેડ પેલ્વીસ એટલે શું? કોન્ટ્રાકટેક પેલ્વીસનું મેનેજમેન્ટ વર્ણવો.
- Management of Contracted Pelvis:
- Management of contracted pelvis, which refers to a pelvis that is abnormally small and has an abnormal shape that can make the birth of the child difficult, requires careful assessment and intervention to ensure the safety of both the mother and the child during labor and delivery.
- Management of contracted pelvis:
- 1) Diagnosis and assessment:
- Pelvimetry
- Pelvimetry involves measuring the pelvis to assess the dimensions and shape of the pelvis.
- This measurement can be done clinically (external measurement) or radiologically (X-ray, MRI).
- Take a complete history of the mother Take a complete history of the mother to assess whether any difficulties have arisen in the mother previously during delivery or cesarean delivery.
- Clinical Evaluation Complete physical examination of the mother, mostly pelvic measurements, so that the condition of the contracted pelvis can be properly assessed.
- 2) Antenatal Care:
- Early Detection Early identification of the contracted pelvis through routine antenatal checkups or ultrasound examinations during the early period of pregnancy.
- Consultation If the woman has a high-risk pregnancy, she should be referred to an obstetrician specialist and to a perinatologist for their comprehensive management.
- 3) Labor Management:
- Continuous Monitoring Closely monitoring maternal and fetal conditions during labor, including proper monitoring of fetal heart rate and proper assessment of maternal vital signs.
- Labor Progress Continuously assessing the labor process. If labor is slow or arrested, it indicates a condition of cephalopelvic disproportion.
- Positioning Provide the mother with proper position that provides optimal pelvic dimensions for labor progress.
- 4) Intervention During Labor:
- Artificial Rupture of Membranes If the membranes are intact and labor is progressing slowly, artificial rupture of membranes can be performed to improve the progress of labor.
- Oxytocin Infusion To improve contractions, provide oxytocin infusion and continuously monitor fetus and uterine contractions.
- Instrumental Delivery: If the baby is in distress and vaginal delivery is possible, vacuum extraction or forceps delivery can be performed.
- 5) Cesarean Section:
- Indications Cesarean section is performed when vaginal delivery is impossible, due to which any complications to the fetus and the mother can be prevented.
- Timing When vaginal delivery is impossible, it is important to make a timely decision to perform a cesarean section to prevent complications for the fetus and the mother.
- 6) Postpartum Care:
- Maternal Monitoring Closely monitoring the mother during the postpartum period to prevent any complications such as postpartum hemorrhage.
- Neonatal Care Immediate newborn care should be provided to the newborn after birth, especially in cases where any complicated labor condition has arisen, to ensure that the newborn is properly well.
- 7) Counseling and Education:
- Education: To educate the mother and her family members by providing them with complete information about the mother’s condition and the causes and interventions that may lead to it.
- Future Pregnancy Planning: To discuss the effect of a contracted pelvis on future pregnancies and delivery options.
- 8) Multidisciplinary Approach:
- Team Collaboration: When the condition is too complicated, all these specialists like obstetricians, midwives, anesthetists, neonatologists should be available.
- 9) Psychological Support:
- The condition of contracted pelvis is stressful and emotionally challenging for a woman, so proper psychological support should be provided to the mother and family members.
Q-3 Write short notes any two ટુંક માં જવાબ લાખો (કોય પણ બે)
a. Write down the functions of amniotic fluid એમ્નીઓટીક ફલ્યુઈડના કાર્યો લખો.
- During Pregnancy:
Functions: - The main function is to provide protection to the fetus.
- During Pregnancy:
- 1) Amniotic fluid acts as a shock absorber and protects the fetus from external injuries.
- 2) It also works to maintain temperature.
- 3) Amniotic fluid distends the amniotic sac. Thus, it provides space for growth and free movements of the fetus. It also prevents adhesion between the fetal parts and the amniotic sac.
- 4) The nutritional value is negligible but provides adequate water supply to the fetus.
- During Labor:
- Helps in dilation of the cervix.
- Prevents obstruction of the placenta circulation during uterine contractions.
- Works to protect the placenta and fetus during uterine contractions.
- Flushes the birth canal during the end of the first stage of labor and protects the fetus with its aseptic and bactericidal action. Also prevents ascending infection in the uterine cavity.
- Clinical Importance
- 1) Amniotic fluid acts as a shock absorber and protects the fetus from external injuries.
- 2) It also works to maintain temperature.
- 3) Amniotic fluid distends the amniotic sac. Thus providing space for growth and free movements of the fetus. Also prevents adhesion between fetal parts and amniotic sac.
- 4) The nutritional value is negligible but provides adequate water supply to the fetus.
b. Write down the causes of obstructed labour ઓન્સ્ટ્રેકટેડ લેબરના કારણો લખો.
- Etiology
1)Fault in passage (birth canal),
2)Fault in passenger (fits)
1)Fault in passage (birth canal): - ( a ) Bony,
- ( b ) Soft tissue obstruction
- ( a ) Bony :
- Contracted pelvis,
- Cephalopelvic disproportion (CPD),
- Abnormal pelvis (Ex: android, anthropoid)
- ( b ) Soft tissue obstruction:
- Due to cervical dystocia due to prolapse or previous operative scarring,
- Cervical or broad ligament fibroid, impacted ovarian tumor,
- Due to tumor in rectum, bladder and pelvic bone.
- Due to biconcave uterus.
- Due to abnormality in uterus.
- Due to vaginal stenosis.
- Due to vaginal septum.
- Due to rigid perineum.
- 2) Fault in passenger (fits):
- Transverse lie, brow presentation
c. Write down the treatment of morality of infertility. ઈનફર્ટીલીટીની સારવાર પધ્ધતિઓ લખો.
- Treatment modalities of infertility:
- Treatment modalities of infertility vary and generally depend on the cause of infertility.
- 1) Lifestyle modifications:
- Weight management: Achieving a healthy body mass index (BMI) through adequate diet and regular exercise can improve fertility.
- Smoking and alcohol cessation:
Smoking and alcohol consumption in excessive amounts both negatively impact fertility. Hence, they should be avoided. - Stress reduction:
Yoga, meditation, and counseling techniques help in reducing stress and its effect on fertility. - 2) Medical Treatment:
- Ovulation induction
Women who have an ovulatory disorder (polycystic ovary syndrome) are given medications such as clomiphene citrate, letrozole, or gonadotrophins that stimulate ovulation. - Hormonal therapy
Correcting hormonal imbalances that affect fertility, such as thyroid disorders and hyperprolactinemia. - Treatment of infection
If there is a condition such as pelvic inflammatory disease (PID), the patient is given adequate antibiotic medication to treat the infection that is affecting fertility. - 3) Surgical Intervention:
- Laparoscopic surgery
is used to treat conditions that affect fertility, such as endometriosis, pelvic adhesions, and fibroids. - Tubal surgery
Tubal surgery involves repairing blocked or damaged fallopian tubes that prevent sperm from reaching the egg. - 4) Assisted Reproductive Technologies (ART):
- Intrauterine Insemination (IUI):
Intrauterine Insemination is a process to improve fertilization in which sperm is inserted directly into the uterine cavity at the time of ovulation. - In Vitro Fertilization (IVF)
In the in vitro fertilization process, ovum and sperm are fertilized outside the body, i.e. in a laboratory.
In which step, - Ovarian stimulation
A medication is used that stimulates the ovaries to produce multiple eggs. - Egg retrieval
A surgical procedure to collect eggs from the ovaries. - Fertilization
The eggs and sperm are mixed in a laboratory dish and then the embryos are cultured. - Embryo transfer
Now more than one embryo is transferred into the uterine cavity. - Intra Cytoplasmic Injection
In this procedure, sperm is directly introduced into the egg to improve fertilization. - 5) Donor Gametes:
- Couples who have severe fertility issues and whose infertility is genetic can use donor eggs or donor sperm for fertility.
- Donor Egg
Donor eggs are fertilized with the sperm of the partner or donor through IVF. - Donor sperm
It is used when there is severe infertility in the male. And also because of the genetic risk in the male, donor sperm is used. - 6) Surrogacy: In surrogacy, another female (surrogate) carries and delivers a child for individuals or couples who are unable to conceive or carry a pregnancy to term:
- Gestational surrogacy
In gestational surrogacy, both the desired woman’s eggs and the desired male’s sperm (surrogate gametes) are collected, in vitro fertilized in a laboratory, and transmitted to the surrogate mother. - 7) Psychological support
Infertility is emotionally challenging. Counseling, support groups, and therapy are important for individuals and couples to cope with the condition of infertility. - Thus, treatment for infertility depends on the different causes in each individual. In which reproductive endocrinologists, urologists, surgeons, and mental health professionals provide adequate treatment to each infertile couple according to their cause and according to their needs.
Q-4 ટુંક નોધલાખો (કોયપણ ત્રણ)
a. difference between contraction ring and retraction ring કોન્ટ્રાશન રીંગ અને રીટ્રેશન રીંગ વચ્ચેનો તફાવત
- Constriction Ring/ Retraction Ring:
- Constriction Ring
- 1.Nature: Constriction ring is caused by localized incoordinate uterine contractions.
- 2.Cause: Irritability in the uterus.
- 3.Situation. Any location but usually above and after the junction of the upper and lower segments without changing position.
- 4.Uterus: Abnormal polarity is seen.
- 5.Abdominal Examination:
- Uterus: Normal,
- F.H.S. Present,
- Fetal part: Easily palpated,
- Ring: Not felt.
- Round ligament: Not felt.
- 6.Vaginal examination: Lower segment is not compressed by the presenting part.
- The ring is filled over the head.
- Features of obstructed labor are absent.
- 7.Result: Maternal exhaustion and fetal anoxia are late features and the uterus does not rupture.
- Treatment: Relax the ring and deliver or cut the ring if necessary by cesarean delivery.
- Retraction ring/ Bandles ring:
- 1 Nature Retraction ring is the end result of tonic uterine contractions and retraction.
- 2.Cause: Obstructed labor occurs.
- The situation always starts at the junction of the upper and lower segments and then gradually moves upwards.
- Utes. Normal polarity is seen.
- Abdominal examination:
Utes: Tense and tender.
F.H.S.. Mostly absent.
Fetal part is not easily palpated.
Ring: Feels rough on the groove.
Round ligament: Stiff and tender.
Vaginal examination Lower segment is compressed by the presenting part.
Ring is not felt vaginally.
Features of obstructed labor are present.
Result: Maternal exudation, sepsis, fetal anoxia are seen. Uterine rupture usually occurs in multigravida.
Treatment: If there is no rupture, perform a cesarean delivery.
b. Care of preet mature baby પ્રિમેચ્યોર બેબીની કેર
- After the birth of the child, the cord should be clamped immediately so that the condition of hypervolemia can be treated. Then the condition of hyperbilirubinemia can be corrected.
- If there is a condition of hyperbilirubinemia and exchange transfusion is required, then the length of the cord should be kept long.
- Clear the child’s mouth and nose properly with a mucus sucker.
- Provide oxygen using a mask and nasal catheter properly.
- Wrap the baby properly in a sterile towel.
- Keep the child in a head-down position on a proper cot.
- To prevent the child from hemorrhagic condition, inj. Vitamin. K 1 mg I/M should be provided.
- Handle the baby with extreme gentleness.
- Advise the baby to avoid bathing.
- Keep the child’s body temperature properly stable.
- Prevent the child from developing atelectasis.
- Prevent the child from developing infection.
- Provide the child with proper nursing care.
- Preterm babies are functionally immature, so they need special care.
c. Lochia લોકીઆ
- The vaginal discharge that occurs during the first 15 days of the puerperium period is called lochia and comes from the uterine body, cervix and vagina.
- It contains blood vessels, decidual tissue, epithelial cells of vaginal mucus, bacteria, membrane fragments and small clots.
- Odor of lochia
- The odor (smell) of lochia is fishy.
- Types of lochia:
- There are three types of lochia.
- 1) Lochia rubra,
- 2) Lochia seroosa,
- 3) Lochia alba
- 1) Lochia rubra: Lochia rubra is the first phase of lochia. In which the discharge is red and bloody and lasts for 1 to 4 days after childbirth.
- Lochia rubra contains blood, fetal membrane, decidua, vernix caseosa and lanugo.
- 2) Lochia seroosa: Lochia seroosa is the second phase of lochia.
Which appears yellowish pale or pale brownish in color. - Lochia seroosa lasts for 5 to 9 days.
It contains a small amount of red blood cells but a high amount of leukocytes,
Wound exudate,
Surviving mucus,
and microorganisms. - 3) Lochia alba: Lochia alba is the third phase of lochia. It usually appears pale white in color.
Lochia alba lasts for 10-14 days.
In it,
a large amount of decidual cells,
leukocytes,
mucus,
cholesterol crystals,
fatty and glandular epithelial cells,
and microorganisms are found in it. - Amount:
The average amount of lochia is about 250 ml during the first 5 to 6 days. - Normal Duration:
The normal duration of lochia is up to three weeks. If it continues even after three weeks, then there may be local lesions. - Clinical Importance of Local Discharge:
- Lochia provides information about the maternal perinatal state, so it is important to assess lochia.
- Odor: May be due to offensive infection.
- Odor:
Scenty or absent may be due to infection. - Amount:
Scenty or absent may be due to infection. - Color:
Continuous red color lochia may be due to subinvolution. - Duration:
If lochia persists for three weeks or longer, it may be a local lesion.
d. Partograph પાર્ટોગ્રાફ
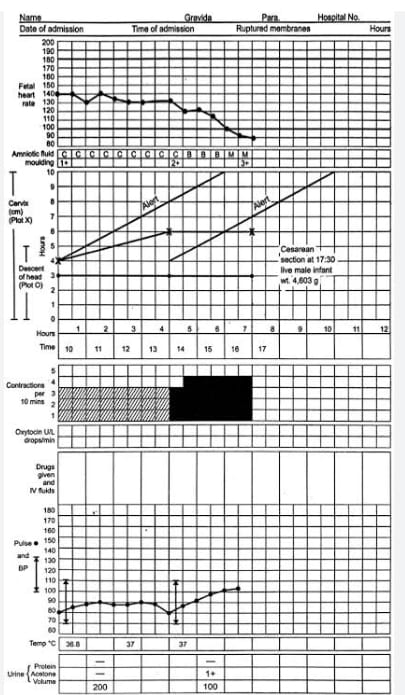
- Definition:
Partograph is a graphic recording and tool for cervical dilation, fetal head descent and labor progress and the condition of the mother and fetus. Immediate and relevant information about the condition of the mother and fetus can be obtained through partograph.
It recognizes the need to take action at the appropriate time and for timely referral. Morbidity and mortality rates of the mother and fetus can also be improved through partograph. - Objectives or Advantages:
- 1) To make proper observations and record during labor.
- 2) To understand the latent and active phases of labor.
- 3) To interpret the partograph and identify any deviation from normal and take appropriate action.
- 4) To know the progress of labor and take action at the right time and refer.
- 5) To see the record at a glance in a single sitting and to hand over easily.
- 6) To avoid having to record labor events repeatedly.
- 7) To reduce the rate of prolonged labor and education.
- Observation Charted on Partograph:
- 1) Pregnant Woman Information:
- A) Name,
- B) GTPAL Score
- G: Gravida,
- T:=Tomb Birth,
- P:=Par,
- A:=Abortion,
- L:=Living Children.
- C) Name of the hospital,
D) Hospital registration number,
E) Date and time of admission,
F) Time of membrane rupture,
G) Period of gestation,
H) Date and time of onset of labour. - 2) Fetal condition:
A) Fetal heart rate,
B) Amniotic fluid,
C) Molding. - 3) Progress of labour
A) Cervical dilation,
B) Descent of head,
C) Uterine contractions. - 4) Maternal condition
A) Oxytocin, drugs and I.v. fluid administration
B) Pulse,
C) Blood pressure,
D) Temperature,
E) Urine volume, acetone and protein. - All this information is filled in the partograph.
- Points to keep in mind while filling the partograph:
- 1) When the woman reaches the active phase of labor, the partograph should be maintained and the pregnant woman should not be left alone.
- 2) Fetal heart rate should be counted and recorded every half hour,
Fetal heart sounds should be counted for a full 1 minute and should be counted immediately after the uterine contractions are completed. - 3) When the dilation of the cervix is 4 cm or more, the frequency, intensity, duration, pulse, fetal heart rate of uterine contractions should be monitored every 30 minutes.
- 4) Blood pressure and cervical dilation (in cm) should be monitored every two hours.
- 5) Descent of head and temperature should be monitored every four hours.
- Partograph
- 1) Patient identification data
This includes the woman’s name, age, GTPAL score, date and time of admission, registration number, time of membrane rupture and time and date of onset of labor. - 2) Fetal condition
Fetal heart rate should be counted and recorded every half hour.
Fetal heart rate should be counted for a full 1 minute.
Fetal heart rate should be counted immediately after uterine contractions are detected.
If fetal heart sound (FHS) is < 120/Minutes or if (FHS) is > 160/Minutes, it indicates fetal distress. If there is a condition of fetal distress, immediate action should be taken.
The vertical column in each small box shows the interval of half an hour. - 2) Condition of Membrane
Along with the fetal condition, the condition of the amniotic membrane and the color of the amniotic fluid should also be recorded every 30 minutes. - A) If the amniotic membrane is intact: = I (Intect),
- B) If the liker is clear: = C (Clear),
- C) If the liker is absent: = A (Absent),
- D) If the amniotic membrane is ruptured: = R (Rupture),
- E) If the liker is meconium stained: = M (meconium),
- F) If blood is present in the liker: B (Blood)
- Thus, the condition of the amniotic membrane and amniotic fluid should be marked as follows in the partograph.
- 3) Molding (The bones of the fetal head are separated by sutures and fontanelles, but when it passes through the birth canal, the bones of the fetal head overlap each other and the shape of the head changes for a while, due to which the fetal head can pass easily through the birth canal. This condition is called molding.)
Molding is recorded by grade. - A) 0 -> If the bones are separated and the sutures are easily felt.
- B) + -> When the bones just touch each other.
- C) ++ -> When the bones overlap but easily separate.
- D) +++ -> When the bones are severely fixed and overlapping.
- 4) Progress of Labor
- Start plotting labor progression on the partograph only after the woman is in active labor.
Active labor is when the cervical dilation is 4 cm or more and at least two good contractions occur in every 10 minutes.
Record cervical dilation in cm every four hours.
Record the onset of cervical dilation starting from the left alert line (when the mother is in active labor). Normally the graph line remains continuously above the left alert line, indicating the proper time each time.
If the alert line is crossed, i.e. if the graph moves to the right of the alert line, it indicates prolonged labor. Hence, the midwife is immediately alerted that there is something abnormal in labor. Note the time when the alert line is crossed and immediately start taking measures for immediate treatment or referral.
When the graph crosses the action line i.e. if it goes to the right side of the action line, immediately start treatment or refer the mother to the appropriate medical service.
The difference between the alert and action lines is 4 hours. - 5) Uterine contractions
Uterine contractions should be recorded every half hour. Contractions occurring twice in ten minutes indicate good uterine contractions. - Mark them in the box of the partograph as follows.
- -> Mild uterine contractions < 20 seconds,
- -> Moderate uterine contractions 20 – 40 seconds,
- -> Strong uterine contractions > 40 seconds.
- 6) Cervical Dilation and Descent of Fetal Head
- The descent of the fetal head down through the out labor process occurs simultaneously with cervical dilation.
- Until the cervix is 7 centimeters dilated, the assessment of the fetal head descent is done by abdominal palpation, which assesses the fifth (5) digit of the fetal head above the pelvic brim.
- In the partograph, cervical dilation is plotted by (x) while the descent of the fetal head is plotted by (O).
- 7) Maternal Condition
The maternal pulse is recorded on the partograph every half hour
and is plotted on the partograph by a dot (•). - Maternal blood pressure is recorded every 4 hours, both systolic blood pressure and diastolic blood pressure are indicated by vertical arrows (↕) where the upper end of the arrow indicates systolic BP. While the lower end of the arrow indicates diastolic blood pressure.
Maternal temperature should be recorded every four hours on the partograph.
Maternal urine volume, urine acetone and protein levels should be recorded properly on the partograph.
If any drug or oxytocin medication is given to the mother during the labor process, its dose, route and time of administration should be recorded properly. - Thus, early, quick and relevant information about the labor progress and the condition of the mother and fetus can be obtained through the partograph.
Q-5 Define following નીચેની વ્યાખ્યા લાખો (કોય પણ છ )
a. Quickning કવીકનીંગ
- Quickening is the first time the mother feels the movement of the fetus in the uterus. Quickening occurs between the 17th and 20th weeks of pregnancy.
b. Prolonged labour પ્રોલોન્ગડ લેબર
- Prolonged labor is an excessively prolonged period of labor, where the delivery process takes longer than normal. This condition poses a risk to both the mother and the fetus.
- Definition by health organizations:
- WHO (World Health Organization):
- When the first stage or second stage of labor is longer than the expected time.
- Typically:
- First labor: more than 20 hours.
- Subsequent labor: more than 14 hours.
c. Lightning લાઈટનીંગ
- Lightening occurs a few weeks before labor begins. During the third trimester of pregnancy, the baby descends into the mother’s pelvis and prepares the pelvis for birth. Lightening is also called engagement.
d. Photo therapy ફોટોથેરાપી
- Phototherapy is a medical treatment that exposes a baby’s skin to fluorescent light to reduce the amount of unconjugated bilirubin and treat conditions such as jaundice. During phototherapy, the baby’s eyes and genitals are covered.
e. Cephelohaemetoma સેફેલોહીમેટોમા
- Cephalohematoma is a collection of blood within the scalp. It appears a few hours after birth. In cephalohematoma, the swelling is limited and does not cross the scalp suture.
f.Chloasma કલોઆઝમા
- Chloasma is a condition in which brown pigmentation of the skin is seen on the face and forehead. Chloasma is seen during the second or third trimester of pregnancy.
g. Antipartum hemorrhage એન્ટીપાર્ટમ હેમરેજ
- It is a condition in which bleeding is seen from or within the genital tract, which occurs after 24 weeks of pregnancy and before the birth of the baby.
h. Vasico vaginal fistula વેસીકો-વજાઈનલ ફીસ્યુલા
- Vesico-vaginal fistula is an abnormal connection or opening between the bladder and the vagina. Vesico-vaginal fistula can be diagnosed with x-rays and CT scans.
Q-6 (A) ખાલી જગ્યા પૂરો .
1.Photograph can be started at the……cm dilatation of service 4 cm ……..સે.મી સવાઈકલ ડાયલેટેશન હોય ત્યારે પાર્ટોગ્રાફ ભરવાનો શરૂ કરી શકાય છે. 4 સે.મી.
2.Precipitate labour completed within ……….hours 3 hours પેસીપીટેટ લેબર……. કલાકમાં પુરૂ થાય છે. 3 કલાકમાં
3.Daily requirement of folic acid during pregnancy is…… Microgram 600 micrograms પ્રેગન-ન્સી દરમ્યાન ફોલીક એસિડની દૈનિક જરૂરીયાન………. માઈક્રોગ્રામ છે. 600 માઈક્રોગ્રામ
4……….. Sutures are located between two paritle bone. Sagittal બે પેરાઈટલ બાનની વચ્ચે ……,સુચર આવેલા છે. સેજિટલ
5.inj……….. prevent RH incompatibility Anti-D (Rh Immunoglobulin) ઈન્જેક્શન ………..આર એચ ઇનકોમ્પીટીબીલીટીને પ્રીવેન્ટ કરે છે. એન્ટી-ડી (આર એચ ઈમ્યુનોગ્લોબ્યુલિન)
Q.6 (B) ખરા ખોટા જણાવો ✅❌
1.Bundl’s ring is a sign of normal labour. બેન્ડલ્સ રીંગ એ નોર્મલ લેબરની નિશાની છે. ❌ કારણ:Bandl’s ring is a pathological sign, often associated with obstructed labor and uterine rupture, not normal labor.- બેન્ડલ્સ રીંગ એ પેથોલોજીકલ લક્ષણ છે, જે સામાન્ય રીતે ઓબ્સ્ટુકટેડ લેબર અને યુટ્રસ રપ્ચર સાથે જોડાયેલું હોય છે, નોર્મલ લેબર સાથે નહીં.
2.Tab misoprostol can not be administered safely by midwife
ટેબલેટ મીસોપ્રોસ્ટોલ મીડવાઈફ દ્વારા સેફલી આપી શકાય નહિ. ❌કારણ: Misoprostol can be safely administered by trained midwives under proper guidelines for purposes like labor induction and postpartum hemorrhage management.-મીસોપ્રોસ્ટોલ પ્રમાણભૂત માર્ગદર્શિકાઓ હેઠળ અને યોગ્ય તાલીમ ધરાવતી મીડવાઈફ દ્વારા સુરક્ષિત રીતે આપવામાં આવે છે, ખાસ કરીને લેબર ઇન્ડક્શન અને પોસ્ટપાર્ટમ હેમોરેજ માટે.
3.Crowing seen during third stage of labour
કાઉનીંગ લેબરના થર્ડ સ્ટેજમાં જોવા મળે છે.❌કારણ: Crowning occurs during the second stage of labor when the fetal head becomes visible at the vaginal opening and does not recede.-કાઉનીંગ લેબરના સેકન્ડ સ્ટેજ દરમિયાન થાય છે, જ્યારે ભ્રૂણનું માથું વજાઈનલ ઓપનિંગ પર દેખાય છે અને પાછું ખેંચાતું નથી.
4.Syphilis is a systemie disease caused by treponema pallidum,
સીફીલીસ સીસ્ટેમીક ડીસીઝ છે જે ટ્રેપોનેમા પેલીડમથી થાય છે ✅કારણ: Syphilis is a sexually transmitted systemic infection caused by the bacterium Treponema pallidum, affecting multiple organs if untreated.-સીફીલીસ એ ટ્રેપોનેમા પેલીડમ બેક્ટેરિયા દ્વારા થતી સેક્સ્યુઅલી ટ્રાન્સમિટેડ સીસ્ટેમીક ઇન્ફેકશન છે, જે સારવાર ન કરવાથી અનેક અંગોને અસર કરે છે.
5.Oum is a largest cell of human body.
ઓવમ હયુમન બોડીનાં મોટામાં મોટો સેલ છે. ✅કારણ: The ovum is the largest cell in the human body, visible to the naked eye, and plays a critical role in reproduction.-ઓવમ એ માનવ શરીરનો સૌથી મોટો સેલ છે, જે નગ્ન આંખે દેખાઈ શકે છે અને પ્રજનન માટે મહત્વપૂર્ણ ભૂમિકા ભજવે છે.
Q.6 (C) Multiple Choice Questions નીચેના માંથી સાચો વિકલ્પ લખો.
1.Umbilical artery carries…..blood. અમ્બીબીકલ આર્ટરી …….બ્લડનું વહન કરે છે
a) Deoxygenated ડીઓકિસજનેટેડ
કારણ: The umbilical arteries carry deoxygenated blood from the fetus to the placenta for oxygenation-અમ્બીબીકલ આર્ટરી ભ્રૂણમાંથી ડીઓકિસજનેટેડ બ્લડને પ્લેસેન્ટા તરફ ઓક્સિજનેશન માટે લઈ જાય છે.
b) Oxygenated – ઓકિસજનેટેડ
c) Mixed –
d) Less oxygenated –
2.The most important hormone required for milk production is મિલ્ક પ્રોડકશન માટે જરૂરી મહત્વનો હોર્મોન છે.
a) Oxytocin – ઓફિસટોસીન
b) Prolactin – પ્રોલેકટીન
કારણ: Prolactin stimulates the mammary glands to produce milk postpartum, while oxytocin aids in milk ejection.-પ્રોલેકટીન ડિલિવરી પછી સ્તનગૃંથિઓને દૂધનું ઉત્પાદન કરવા માટે પ્રોત્સાહન આપે છે, જ્યારે ઑક્સીટોસિન દૂધને બહાર કઢવામાં મદદ કરે છે.
C) H.C.G – એચ. સી. જી
d) HPL.-એચ.પી.એલ
3.Commonest cause of rapture of uterus is રપ્ચર ઓફ યુટ્રટ્સનું સામાન્ય કારણ છે
a) Obstructed labour ઓબ્સ્ટુકટેડ લેબર
કારણ: Prolonged obstructed labor increases uterine pressure, leading to rupture if not managed timely.–લાંબા સમય સુધી ઓબ્સ્ટુકટેડ લેબર હોવાથી યુટ્રસના દબાણમાં વધારો થાય છે, જે સમયસર સંભાળ ન લેવાય તો રપ્ચર તરફ દોરી જાય છે.
b) Post-ceasarean section પૉસ્ટ સીઝીરીયન સેક્શન
c) Shoulder presentation – સોલ્ડર પ્રેઝેન્ટેશન
d) None of above – એક પણ નહિ
4.Bishop scoring is based on all except બીટાપ સ્કોર આ સિવાયના બધા પર આધારિત છે.
a) Dilatation of cervix – સર્વીકસનું ડાયલેટેશન
b) Ellacement of cervix – સવીકસનં ઈકંસમેન્ટ
c) Uterine contraction યુટ્રઈન કોન્ટ્રાકશન
કારણ: Bishop scoring evaluates the readiness of the cervix for labor, including factors like dilatation, effacement, station of the head, and consistency of the cervix. Uterine contractions are not part of the scoring system.-બીટાપ સ્કોરિંગ લેબર માટે સર્વિક્સની તૈયારીને આંકે છે, જેમાં ડાયલેટેશન, ઇકંસમેન્ટ, હેડ સ્ટેશન અને સર્વિક્સની કન્સિસ્ટન્સીનો સમાવેશ થાય છે. યુટ્રિન કોન્ટ્રાકશનનો સમાવેશ થતો નથી.
(d) Station of head – સ્ટેશન ઓફ હેડ
5.Involution of uterus completed by ઈન્ડોલ્યુશન ઓફ યુટ્રટ્સ કમ્પલીટ થાય છે.
A) Six weeks છ અઠવાડિયે
કારણ:Involution is the process of the uterus returning to its pre-pregnancy size and shape, which usually takes about six weeks postpartum.-ઇન્ડોલ્યુશન એ યુટ્રસને તેની ગર્ભાવસ્થા પૂર્વની આકાર અને કદ પર પાછું લાવવાની પ્રક્રિયા છે, જે સામાન્ય રીતે ડિલિવરી પછી લગભગ છ અઠવાડિયામાં પૂર્ણ થાય છે.
b) Two weeks – બે અઠવાડીયે
C) Four weeks – ચાર 1) Six weeks
b) Two weeks – બે અઠવાડીયે
