ENGLISH-COMMUNITY HEALTH NURSING 2 (PAPER SOLUTION GNM 3RD YEAR) 11/02/2025(Done)-uplaod no-10
COMMUNITY HEALTH NURSING 2 (PAPER SOLUTION-10-GNM 3RD YEAR) 11/02/2025
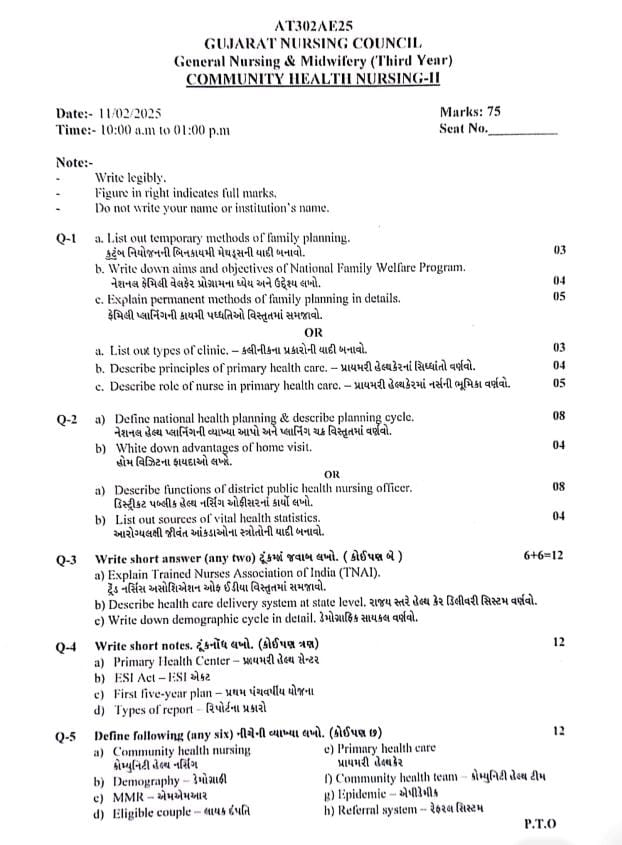
Q-1
a. List out temporary methods of family planning. કુટુંબ નિયોજનની બિનકાયમી મેથડ્સની યાદી બનાવો.03
TEMPORARY METHOD OF FAMILY PLANNING:
Temporary method is a reversible and time-limited contraceptive technique for family planning whose main aim is to prevent unwanted pregnancy. This method prevents the natural work of fertilization or implantation without causing permanent effects on the reproductive function of the patient. Each method should be selected according to the patient’s age, hormonal balance, co-morbid conditions and family planning goals.
Barrier Method:
In the barrier method, the entry of sperm into the female reproductive tract is physically obstructed so that it does not reach the egg.
- Male Condom
- Female Condom
- Diaphragm
- Cervical Cap
- Spermicides
- Hormonal Method:
Hormonal methods cause immediate changes in the hormonal mechanism of the patient and work by suppressing ovulation or making the endometrium unfavorable for pregnancy. - Combined Oral Contraceptive Pills (Pills) Progestin-Only Pills (Progestin-Only Pills)
- Contraceptive Patch (Contraceptive Vaginal Ring)
- Emergency Contraceptive Pills (Emergency Contraceptive Pills)
- Intrauterine Contraceptive Device – IUCD:
- This is a small flexible plastic device that is inserted inside the uterus and mechanically and biochemically obstructs the work of sperm and prevents implantation.
- Copper T IUCD
- Hormonal IUCD
- Multiload IUCD
Injectable Contraceptive:
Injectables are hormonal drugs that are administered into the patient’s body via the intramuscular route and inhibit ovulation for a long time.
DMPA (Depo-medroxyprogesterone acetate)
NET-EN (Net-EN: Norethisterone enanthate)
Implants:
- An implant is a subdermal rubbery rod that is inserted under the skin in the patient’s arm. It slowly releases hormones that provide a long-lasting contraceptive effect.
- Norplant
- Implanon
- Nexplanon
- Natural Method:
- The natural method is based on observing the patient’s menstrual cycle and fertile period. It does not use any medical devices or drugs.
- Calendar Method
- Cervical Mucus Method
- Basal Body Temperature Method
- Coitus Interruptus
- Lactational Amenorrhea Method
- Emergency Contraception:
- Emergency contraception is an option for patients that is taken immediately after unprotected sexual activity and works to obstruct ovulation or implantation.
- Levonorgestrel
- Ulipristal Acetate
- Copper T IUCD insertion
- Temporary methods are safe and reversible options for the patient and should be chosen based on the patient’s reproductive rights, health status, and family planning desires. Appropriate counseling and informed choice are essential for each method.
b. Write down aims and objectives of National Family Welfare Program. નેશનલ ફેમિલી વેલફેર પ્રોગ્રામના ધ્યેય અને ઉદ્દેશ્ય લખો.04
India is the first country in the world to implement a family welfare program on a national basis through the government. Family welfare is also known as the family planning program. This family planning program was included as an official program since 1952.
Aim:
The main aim of the National Family Welfare Program is to control the population growth of the country, improve reproductive health, maternal health and child health and make quality healthcare services easily available to the patients.
Objectives:
The objectives of family welfare include improving the overall health and well-being of the family.
The objectives of family welfare are as follows:
1) Promoting reproductive health:
To ensure that families have access to reproductive health-related services, including family planning, maternal and child health care, and prevention and management of reproductive tract infections. Their involvement is ensured.
2) Reduce maternal mortality rate:
Maternal death and complications can be reduced by providing skilled care to the mother during pregnancy, during childbirth, and during the postpartum period.
3) Reduce infant and child mortality:
Morbidity and mortality rates in children can be reduced by providing proper nutrition, immunization, and proper health care services to infants and children.
4) Promoting family planning:
Encouraging individuals or couples to use contraceptive methods to space their pregnancies and plan pregnancies according to their choice.
5) Ensuring safe motherhood:
Promoting safe childbirth practices, prenatal care and postnatal care to improve maternal health outcomes.
6) Improving nutrition and hygiene:
Assessing malnutrition and promoting hygienic practices to improve the overall health and well-being of families.
7) Preventing and management of communicable diseases:
Identifying and treating infections that affect reproductive health, such as sexually transmitted and other communicable diseases.
8) Social support:
Social support includes providing a social support system to families and vulnerable populations, such as single-parent households, low-income families, and families with disabilities and chronic illnesses. This support involves financial assistance, counseling services, and community-based support.
9) Promotion of small family norm:
To encourage families to voluntarily choose small family sizes to improve maternal and child health outcomes and overall family well-being.
10) Promotion of spacing method:
To provide advice on the use of contraceptives to space pregnancies. Due to which healthier outcomes for the mother and her child can be promoted.
11) Ensuring access to contraceptives:
To ensure that adequate contraceptives reach all eligible couples to properly adopt family planning.
12) Prevention of unwanted birth:
Provide information and services to prevent unintended pregnancy, which can lead to better maternal health and improved socio-economic outcomes for families.
13) Promotion of planned pregnancy:
Encourage couples to plan and prepare for pregnancy in order to promote the health of both mother and child.
14) Promotion of birth spacing:
Advise families to maintain adequate space between pregnancies to maintain the overall well-being of the mother and child and reduce complications due to close pregnancies.
15) Age appropriate child bearing:
Advise families to plan age appropriate pregnancies to reduce complications due to early or late pregnancies.
These objectives collectively aim to empower individuals and families to make informed choices about their reproductive health and family planning, thereby improving overall health outcomes and enhancing the quality of life for families.
c. Explain permanent methods of family planning in details.ફેમિલી પ્લાનિંગની કાયમી પધ્ધતિઓ વિસ્તૃતમાં સમજાવો.05
Sterilization/ Permanent Contraception:
Permanent surgical contraception, also known as voluntary sterilization, is a surgical method in which the reproductive function of an individual male or female is purposefully and permanently destroyed. Such as,
1) Male Sterilization: Vasectomy,
2) Female Sterilization: Tubectomy
1) Male Sterilization: Vasectomy:
Vasectomy is a permanent sterilization operation performed on males in which both sides of the vas deferens are resected and its ends are cut and ligated.
Advantages:
It has simple operation technique and less complications.
It can be performed as an outdoor procedure in camps and villages.
The failure rate is 0.15% and the success rate of reversal anastomosis operation is 50%.
Equipment, hospital stay, doctor training are all less expensive.
Disadvantages:
Additional contraception is required for 2-3 months after the operation until the semen becomes sperm free.
Frigidity or impotence may occur, which is mostly psychological.
Non Scalpel Vasectomy (NSV):
This operation is performed under local anesthesia in which the vas is caught with specially designed forceps, then the stretched skin over the vas is punctured with the sharp point of the forceps without using a scalpel and then the vas is dissected. Sutures are not required and the time is also less. There is a fast recovery but the skill of the surgeon is required to a greater extent.
Female Sterilization/ Tubectomy:
Tubectomy is a method of permanent sterilization performed in females. In this, the fallopian tubes are cut to block the passage of the ovum and then they are ligated.
Time of Operation:
Postpartum Sterilization:
If the patient is healthy, tubectomy can be done 24-48 hours after delivery.
Internal Sterilization:
When the operation is performed at a time other than childbirth and abortion, it is called internal sterilization.
Traditional tubectomy:
This method is also known as abdominal tubectomy. This method is usually performed under general anesthesia or spinal anesthesia in which an incision is made in the lower abdominal area and then the fallopian tube is cut and tied or clamped. After that, the layers of the abdomen are closed. This usually works as a permanent contraceptive that blocks the path of the ovum. It usually requires hospitalization for five to six days and the sutures can be removed after the 5th day after the operation.
Post-operative Advice:
Heavy weights should not be lifted for 6 weeks.
Heavy work should be avoided for three months.
Sexual activity can be resumed after 4 weeks of the operation.
Minilap Operation:
This is a minor form of abdominal tubectomy which is usually performed under local anesthesia in which a 2.5 to 3 cm incision is made in the lower abdominal area and then parts of the fallopian tube are cut and clamped and then the abdominal layer is sutured again. This method is a very safe and effective method. This procedure can usually be performed at the Primary Health Center (PHC) level and also in the community. This procedure acts as a good technique for postpartum sterilization.
Advantage:
This technique is usually suitable for postpartum sterilization.
This procedure is generally less traumatic than an abdominal tubectomy.
It also generally has fewer complications.
Laparoscopic Sterilization:
This laparoscopic sterilization technique is a very popular procedure of female sterilization in which the fallopian tubes are blocked or a rubber ring is placed in the fallopian tubes due to which the ovum cannot reach the uterus. Before inserting the laparoscope, the abdomen is expanded with carbon dioxide, nitrous oxide or air. Then the laparoscope is inserted through the abdomen and the tubes are visualized. Then, when the tubes are visualized, a fallopian ring is placed in the fallopian tube or a clip is applied due to which the tubes are blocked. Then the laparoscope is removed and the layers of the abdomen are sutured and closed.
Advantage:
The incision is very small and the scar is also small.
It requires less time for the operation.
It is a less expensive procedure.
Complications are minimal.
Hospital stay is short, usually up to 48 hours.
Disadvantages:
It is not usually performed in post-partum patients.
It is not suitable for patients who have medical disorders such as heart disease, respiratory disease, diabetes and hypertension.
Complication:
Pain,
Stretching,
Irregular menstrual cycle,
Local infection.
OR
a. List out types of clinic. – કલીનીકના પ્રકારોની યાદી બનાવો.03
“Clinic” is a healthcare organization where preventive, diagnostic, and therapeutic services are provided to patients. Different types of clinics deliver health services to patients with a specific objective. Below is a list of different types of clinics and their descriptions.
- General Clinic:
This clinic provides health services to patients at the OPD level for general health problems. For common ailments like fever, headache, cold, indigestion, a general practitioner provides services.
- Specialty Clinic:
This clinic is working for a specific medical branch. For example, Cardiology, Neurology, Dermatology, Gynecology, etc. Here, specialist doctors provide diagnosis and treatment.
- Antenatal Clinic:
This clinic works for the health of the patient during pregnancy. It provides services like blood pressure, hemoglobin level, fetal growth and nutrition testing and tetanus injection.
- Postnatal Clinic:
This clinic works for the health care of the mother and newborn baby in the period after childbirth. In which breastfeeding guidance, maternal health assessment and contraceptive advice are provided.
- Immunization Clinic:
This clinic provides vaccination services to the patient. Especially for children and pregnant women, vaccines like BCG, OPV, Pentavalent, MR are given.
6.Family Planning Clinic:
This clinic provides contraceptive devices such as condoms, oral pills, injectables and IUCD (Intrauterine Contraceptive Device) to the patients. Also, advice is given on permanent methods such as sterilization.
7.T.B. Clinic:
This clinic provides diagnosis, DOTS therapy (Directly Observed Treatment, Short-course) and follow-up services for Tuberculosis patients.
8.STI / RTI Clinic:
This clinic provides treatment and counseling to patients for Sexually Transmitted Infections and Reproductive Tract Infections.
9.Mental Health Clinic:
This clinic works for the mental health of the patient. It provides psychological assessment and therapeutic intervention for conditions like depression, anxiety, psychosis.
18.Pediatric Clinic:
This clinic works exclusively for children. It provides vaccinations, growth chart checks, treatment for common diseases and nutritional advice.
11.Nutrition Clinic:
This clinic works for nutritional problems. Such as anemia, PEM (Protein Energy Malnutrition), obesity etc. The patient is given diet plan, supplements and counseling.
12.HIV/ART Clinic:
This clinic provides diagnosis, counseling and ART (Antiretroviral Therapy) treatment for HIV positive patients. Regular monitoring is done according to the patient’s immune status.
13.Rehabilitation Clinic:
This clinic works for the complete recovery of the patient after chronic diseases. Services like physiotherapy, occupational therapy and speech therapy are available.
In community health nursing, various types of clinics provide services to the patients according to their specific needs. Each clinic has a specific purpose and area of service. These clinics make the healthcare system more effective, specialized and patient-centric.
b. Describe principles of primary health care.-પ્રાયમરી હેલ્થકેરનાં સિધ્ધાંતો વર્ણવો.04
There are 5 main principles of primary health care.
1) Equitable Distribution,
2) Community Participation,
3) Appropriate Technology,
4) Focus on Prevention,
5) Intersectoral Coordination
1) Equitable Distribution:
Health services and resources should be distributed equally in the community. Primary health care should be available to all without any discrimination of caste, creed and gender, religion, rich, poor, urban or rural. According to this principle, primary health care should be available to every individual, family and community. It is based on social justice. People living in rural areas are the main target of primary health care.
2) Community Participation:
It is difficult to achieve the goal of primary health care without the involvement of the community.
Continuous efforts should be made to get the involvement of the community in the planning, implementation, and maintenance of health services.
Local health workers of villages like village health guides, anganwadi workers, ASHAs, train-aids provide health services by overcoming any communication barriers and culture.
This is done in such a way that it becomes acceptable to the community.
3) Appropriate Technology:
The technology used in primary health care should be scientifically sound, safe, socially acceptable, appropriate to local requirements and financially viable and should be available at the local level.
Ex: Use of ORS is an example for the treatment of diarrhea.
4) Focus on Prevention:
The main focus of primary health care is not to treat disease but to prevent disease and promote health. Primary health care emphasizes health education.
5) Intersectoral Coordination:
For the successful implementation of primary health care, coordination of other sectors is necessary such as agriculture, sanitation, housing, nutrition, public workers, communication and education etc.
Thus, primary health care mainly involves 5 principles.
c. Describe role of nurse in primary health care.-પ્રાયમરી હેલ્થકેરમાં નર્સની ભૂમિકા વર્ણવો.05
Introduction:
Primary healthcare is the first and most fundamental link of healthcare for the patient. Preventive, Promotive, Curative and Rehabilitative Care is provided here. Nurses play an important role in primary healthcare and work to maintain, restore and improve the health of the patient. The role of nurses is described in detail in various aspects below.
1.Health Educator:
Nurses provide information to patients and community members about nutrition, hygiene, vaccination, reproductive health, family planning, and communicable diseases. Nurses motivate people for health-related behavior through IEC (Information, Education and Communication) programs.
2.Care Provider:
The nurse provides immediate first aid to the patient which includes monitoring vital signs, dressing, administering injections or oral medication and assessing the patient.
3.Immunization Coordinator:
The nurse is responsible for administering vaccines like BCG, OPV, DPT, Pentavalent, MR under vaccination programs. The nurse maintains the cold chain and takes immediate action for AEFI (Adverse Events Following Immunization).
4.Community Surveyor:
The nurse assesses the health status of the patient through home visits. She prepares records like Eligible Couple Register, MCH Register and Immunization Register.
5.Disease Identifier and Referral Agent:
The nurse makes primary identification of diseases like TB, Leprosy, Malaria, Diabetes, Hypertension and provides high level referral to the patient as per the requirement.
6.Maternal and Child Health Provider:
The nurse provides services for Antenatal Care, Intranatal Care and Postnatal Care. She provides guidance for Breastfeeding, Growth Monitoring, Weaning and Immunization.
7.Family Planning Counselor:
The nurse provides guidance to the patient for contraceptive methods like IUCD, Oral Contraceptive Pills, Condoms, Injectables. Also provides counseling for Sterilization.
8.Communicable Disease Controller:
The nurse is responsible for surveillance, awareness, and prevention in epidemic situations like Cholera, Dengue, Measles etc.
9.Health Record Keeper and Reporter:
The nurse records all the health records related to the patient, such as Immunization Card, ANC Card, Referral Slip etc. The nurse sends this information as a report to the local health office.
10.Program Implementer:
The nurse implements various national health programs like NRHM, RCH, UIP, NACP RMNCH+A at the grassroots level.
In primary health care, the nurse is the first point of contact for the patient. She plays an important role not only in treatment but also in health maintenance, disease prevention, medical service delivery and patient satisfaction. Nurses are the cornerstone of the health system, ensuring the best and most comprehensive healthcare to patients at the primary level.
Q-2
a) Define national health planning & describe planning cycle. નેશનલ હેલ્થ પ્લાનિંગની વ્યાખ્યા આપો અને પ્લાનિંગ ચક્ર વિસ્તૃતમાં વર્ણવો.08
National Health Planning is a process in which evidence-based decisions are made at the national level, considering the health needs of the population, so that maximum health benefits can be achieved using limited resources.
It involves collecting data, formulating health policies, setting priorities, setting objectives and goals, and developing strategies and programs to implement them systematically.
Objectives of National Health Planning:
- To meet the health service needs of the country.
- To ensure equitable distribution of health resources.
- To ensure equity and accessibility.
- To reduce morbidity and mortality.
- Improve the quality of care.
- Strengthen the health system.
- Improve the health outcomes of the population.
- Planning Cycle:
The Planning Cycle is a structured and systematic process of national health planning, which includes the following steps:
Step 1: Analysis of Health Situation:
Identify the strengths and weaknesses of the current health system.
Obtain information on morbidity, mortality, demographics and health service utilization.
Understand the needs of patients, health workers and the community and make an evidence-based analysis.
Step 2: Setting Goals and Objectives:
Set clear and measurable goals to improve health at the national level.
Set targets for each health problem that will help in tracking progress.
Step 3: Assessing Resources:
Analyze manpower, finance, equipment, facilities and other available resources.
Take necessary steps for resource optimization.
Step 4: Prioritization of Health Problems:
Categorize health problems based on their seriousness, frequency, impact and resource availability.
Step 5: Plan Formulation:
Prepare a detailed action plan keeping in mind the objectives.
Determine the timeframe, activities, resource allocation and responsibilities.
Step 6: Implementation of Plan:
Run the programs and services as per the plan in a planned manner.
Integrate health staff, community and stakeholders.
Step 7: Monitoring and Supervision:
Monitor activities and outputs regularly.
Check whether the work is being done as per the plan.
Step 8: Evaluation:
Evaluate the extent to which the objectives and goals of the plan have been achieved.
Study outcomes and impact.
Use lessons learned for future planning.
4.Importance of Planning Cycle in Community Health Nursing:
To make health service delivery at community level effective.
To provide guidance for systematic implementation of health programs.
To address the health needs of patients and population strategically.
To ensure comprehensive and appropriate utilization of available resources for public benefit.
National Health Planning is an important process to meet the health needs of patients and population of the country on a scientific and practical basis. Planning Cycle provides a structured and directive method for this plan. By following it, it becomes possible to make the health care system more effective, equitable and robust.
b) Write down advantages of home visit. હોમ વિઝિટના ફાયદાઓ લખો.04
Home Visit is a specific, planned and systematic health service in which a trained health worker visits an individual patient’s home to provide observation, treatment, guidance or support. This service is provided in the patient’s familiar and natural environment – that is, the home environment.
Key Advantages of Home Visit:
- Better Understanding of Environment
The health worker can better understand the social, economic and cultural context of the patient’s home.
This helps in creating a personalized care plan.
2.Continuity of Care:
Home visits enable continuous follow-up, monitoring and rehabilitation for the patient.
Home visits maintain continuity of health care when the patient is unable to go to the hospital.
3.Builds Trust and Rapport:
Two-way communication and a trusting relationship are developed between the health worker and the patient and his family, which increases patient compliance.
4.Promotion of Health Education:
During home visits, the patient and family are informed about health education, diet, hygiene, immunization and first aid.
5.Early Detection of Health Problems:
During home visits, health workers can identify health problems of patients living in slums, rural areas or remote low-socioeconomic groups.
6.Cost-effective Method:
Home visits are a great way to save the patient the cost of going to the hospital or clinic.
Home-based treatment saves time, money and energy.
7.Improves Compliance to Treatment:
When patients receive treatment plans, medicines and guidance at home, they are more willing and regular to follow the treatment.
8.Suitable for High-risk Groups:
Home visits are very effective for patients with chronic conditions such as elderly patients, paralyzed patients, post-operative patients or patients with cancer.
9.Encourages Family Involvement:
During home visits, health workers can train family members for patient care.
This ensures family-centered care.
10.Strengthens Community Participation:
Home visits increase people’s positive approach and sense of responsibility, which is essential for the successful implementation of health programs at the community level.
Home Visit is a patient-centered and community-oriented service that provides patients with quality health care in the comfortable, familiar, and safe environment of their home.
OR
a) Describe functions of district public health nursing officer. ડિસ્ટ્રીક્ટ પબ્લીક હેલ્થ નર્સિંગ ઓફીસરનાં કાર્યો લખો.08
District Public Health Nursing Officer:
The District Public Health Nursing Officer is a senior level health nursing professional responsible for the health administration of the district, who plans, organizes, implements, supervises and evaluates all public health nursing activities.
Functions of District Public Health Nursing Officer:
1.Planning and Implementation of Health Programs:
The District Public Health Nursing Officer is responsible for planning and implementing various national health programs. He develops strategies to deliver public health nursing services to the people and supervises their implementation.
2.Supervision and Monitoring:
They supervise and monitor the work of health workers, ANMs, nurses and other paramedical staff working at the talati level. They see whether the quality is maintained in the standards of service delivery or not.
3.Training and Capacity Building:
The officer organizes regular training for health workers and nursing staff. The capacity of the staff is built on the basis of skill development, updated clinical practices and new knowledge so that the patients can get quality care.
4.Data Collection and Reporting:
Collection of data related to health-related outcomes, immunization, maternal health, child health and contraceptive use and regular reporting to the government on the basis of this.
5.Infection Control and Public Health Safety:
The officer ensures follow-up of standard protocols of infection control. He monitors the maintenance of hygienic conditions in health centers, sterilization and waste management processes.
6.Community Participation and Awareness:
The officer organizes awareness campaigns at the local level such as on maternal care, nutrition, hygiene, vaccination, etc. They coordinate with local bodies and non-governmental organizations to increase involvement in community health.
- Emergency and Disaster Management:
The officer plans for rapid response in conditions like health emergencies or natural disasters at the district level. He coordinates patient care, rehabilitation and resource movement.
- Coordination with Other Departments:
The officer plays a role in advancing integrated health activities in collaboration with education, women and child development, public distribution system and other departments.
9.Budgeting and Resource Allocation:
The officer is responsible for the proper allocation and utilization of funds for health services. He makes available material, manpower and equipment as per the requirement.
10.Ensuring Quality of Care:
He is responsible for ensuring that quality and ethical standards are maintained in the healthcare services provided to the patients. He ensures adherence to clinical guidelines and nursing ethics.
The District Public Health Nursing Officer plays a key role in the health sector. He advises the frontline workforce, ensures implementation of public health policies and holds a key position for patient-centred quality healthcare delivery across the district.
b) List out sources of vital health statistics. આરોગ્યલક્ષી જીવંત આંકડાઓના સ્ત્રોતોની યાદી બનાવો.04
Vital Health Statistics:
Vital health statistics are factual figures that provide complete information about the health status of a population, morbidity, mortality, birth rate, death rate, life expectancy, etc. These figures are very important for making various health policies, planning, evaluation, and health service delivery.
Sources of vital statistics:
1.Civil Registration System (CRS):
Civil Registration System is a continuous, permanent and compulsory recording of the occurrence and characteristics of vital events (birth, death, marriage, etc.).
Authority: Administered by the Registrar General of India under the Ministry of Health.
Importance: Provides primary data for birth and death rates, which are crucial for planning and policy making.
- Sample Registration System (SRS):
Conducts large-scale demographic surveys for reliable annual estimates of birth rates, death rates and other fertility and mortality indicators.
Authority: Conducted by the Office of the Registrar General of India and the Census Commissioner.
Importance: Supplements CRS (Sample Registration Systems) data and provides more accurate and timely estimates.
- Census:
Conducted every ten years, the Census of India collects comprehensive data on the population. It collects information on age, caste and marital status.
Authority: Conducted by the Office of the Registrar General of India and the Census Commissioner.
Importance: Provides detailed demographic information that supports various statistical analyses and socio-economic planning.
- National Family Health Survey (NFHS):
A large-scale, multi-round survey conducted on a representative sample of households across India.
Authority: Conducted by the Ministry of Health and Family Welfare in coordination with the International Institute for Population Sciences (IIPS).
Significance: Provides data on population, health and nutrition, as well as fertility rates, maternal and child health.
- Health Management Information System (HMIS):
Is an online portal that collects data from health facilities across India.
Authority: Managed by the Minister of Health and Family Welfare.
Significance: Provides data on health indicators, service delivery and performance of health programmes.
6) Annual Health Survey (AHS):
Provides district-level estimates of key indicators, such as fertility and mortality rates.
Authority: Conducted by the Office of the Registrar General and Census Commissioner of India.
Importance: Helps in evaluating the impact of health programmes and policies at a more localized level.
7) Demography and Health Survey (DHS):
Conducted periodically to collect data on population, health and nutrition.
Authority: Coordinated by various institutions and often in partnership with international agencies.
Importance: Provides internationally comparable data for monitoring and evaluation.
8) Medical Certification of Cause of Death (MCCD):
A system of recording the cause of death by medical practitioners using a standardized format.
Authority: Managed by the Office of the Registrar General of India.
Importance: Provides accurate data on mortality patterns and causes of death, which is essential for public health planning.
9) Health Survey and Research:
Various surveys and research studies are conducted by government agencies, academic institutions and international organizations.
Examples: National Sample Survey (NSS), India Human Development Survey etc.
Importance: These surveys provide additional data on various health and demographic parameters, which helps in comprehensive analysis and policy formulation.
Vital statistics in India, obtained from multiple sources, play a crucial role in providing accurate and comprehensive data on the health and demographic characteristics of each population. These statistics are essential for the effective planning, implementation and monitoring of health and social programs.
Q-3 Write short answer (any two) ટૂંકમાં જવાબ લખો. (કોઈપણ બે)6+6=12
a) Explain Trained Nurses Association of India (TNAI).ટ્રેઇન્ડ નર્સિંસ અસોશિએશન ઓફ ઇન્ડિયાવિસ્તૃતમાં સમજાવો.
Trained Nurses Association of India:
Trained Nurses Association of India is the oldest and most prominent nursing association in the country. This organization works to raise the literacy, professional standards and quality of patient care of the nursing profession. TNAI protects the interests of the nursing profession and represents it at various levels.
Establishment:
TNAI was established in the year 1908, when its original name was “Association of Nursing Superintendents”. Later in 1922, its new form was introduced as “Trained Nurses Association of India”. In 1909, it gained membership of the International Council of Nurses (ICN).
Objectives:
The main objectives of TNAI are as follows:
To maintain high standards of education and practice in the nursing profession.
To promote ethical standards of nurses.
To create opportunities for professional growth and development for nurses.
To improve the quality of patient care.
To protect the interests of nurses and to raise their voice for their rights.
To cooperate with the National Health Policy from a nursing perspective.
Functions:
The main functions of TNAI include:
To formulate guidelines for nursing education.
To promote research and development.
To conduct Continuing Professional Development programs for nurses.
To collaborate with national and international nursing organizations.
To enhance the importance of nurses in the public health care system.
Membership:
There are four types of membership in TNAI:
1.Student Membership
2.General Membership
3.Associate Membership
4.Life Membership
Various activities, training and seminars are organized for each member so that their professional skills are improved.
Publications:
TNAI publishes “The Nursing Journal of India”, which is important for nursing research, theories and studies. Apart from this, various educational materials and guidelines are also published.
Affiliations:
TNAI has affiliations with the following international bodies:
1.International Council of Nurses
2.Commonwealth Nurses and Midwives Federation
3.Indian Nursing Council
4.World Health Organization
The collaboration with all these organizations helps TNAI in raising nursing standards at the global level. Trained Nurses Association of India acts as a strong pillar for the nursing profession. It not only looks after the interests of nurses, but also contributes greatly to the healthcare system of the country. TNAI is a platform that empowers nurses for professional ethics, standards and patient care.
b) Describe health care delivery system at state level. રાજય સ્તરે હેલ્થ કેર ડિલીવરી સિસ્ટમ વર્ણવો.
- Introduction:
The health care delivery system at the state level is an organized system responsible for planning, implementation, and supervision of health services, which is run by the state government. It works for the management of all health programs, public health initiatives, and medical institutions. - Major Components:
A. State Health Directorate:
Works under the state health department.
Managed by senior officials like Director of Health Services, Director of Medical Education etc.
Responsible for making health policy, implementing programs, monitoring and evaluation.
B. State Ministry of Health:
Receives guidance from the Health Minister and Secretary.
Responsible for all state level funds, policies and public health matters.
- Three-Tier Health Care Delivery Structure at State Level:
A. Primary Level:
Facilities: Sub-centres, Primary Health Centres (PHCs).
Targets mainly rural and underserved population.
Services include immunization, maternal and child health (MCH), health education, dietetic counselling etc.
B. Secondary Level:
Facilities: Community Health Centres (CHCs),
Taluk/District Hospitals.
Specialty Services: Obstetrics, Pediatrics, General Surgery, Medicine.
Operates for referral care.
C. Tertiary Level:
Facilities: Medical College Hospitals, Research Institutes, High Specialty Hospitals.
Provides advanced care and super-specialty services.
Acts as a referral point for complex cases.
- State-Level Health Institutions:
Medical Colleges and Hospitals
State TB Training and Demonstration Centres
Health and Family Welfare Training Centres
State Nursing Councils
State Referral Laboratories
- Supporting Systems and Manpower:
Multipurpose Health Workers, Nurses, Lab Technicians, Medical Officers, Specialists.
Mission Directorates like NRHM (National Rural Health Mission), NUHM (National Urban Health Mission) also provide support.
IT-enabled monitoring and Health Management Information System (HMIS).
- Key Responsibilities of State Health System:
Health Infrastructure Development
Human Resource Management
Formulation of Public Health Policy
Implementation of Health Insurance Schemes
Emergency Medical Response Planning
Health Surveillance and Risk Management
- Challenges at State Level:
Insufficient Manpower and Funds
Access to Health Services in Rural Areas
Weakness of Referral Mechanism
Deficiencies in Data Management System
- Coordination with Central Health System:
At the state level, Central Government Missions and Schemes like NHM (National Health Mission), Ayushman Bharat are also implemented for health care delivery. The state government keeps it operational by integrating it with its own health infrastructure and policies.
The health care delivery system at the state level is an infrastructure that works to deliver services to the people from primary to tertiary level as a whole. It ensures patient-centric care through policy, implementation, monitoring and coordination. Technology, manpower and coordination are important for more effective health care
c) Write down demographic cycle in detail. ડેમોગ્રાફીક સાઇકલ વર્ણવો.
Demographic Cycle:
Demos means people
Graphine means the record.
Demography
The scientific study of human population and its elements i.e. size, composition and distribution is called demography. Demography means the scientific study of population.
Concept of Demography
Demography is a branch of science that studies human population and focuses on only three elements.
1) Any changes in the size of the population i.e. increase or decrease in size.
2) Structure of the population (basic of age and size).
3) Geographical distribution on the basis of state or region.
There are mainly 5 stages of demographic cycle.
1) First Stage = High Stationary Stage,
2) Second Stage = Early Expanding,
3) Third Stage = Late Expanding,
4) Fourth Stage = Low Stationary,
5) Fifth Stage = Decline Stage
1) First Stage = High Stationary Stage: In the high stationary stage, there are no changes in the size and composition of the population.
Birth Rate: ↑High
Death Rate: ↑High
Because in it, the high birth rate and high death rate, i.e. both cancel each other and due to which the population remains stationary (stable).
Till the middle of the 17th century, the world’s population was in this stage and India was in this stage till 1920.
Ex: India in 1920
2)Second Stage= Early Expanding: In the second stage, the death rate decreases in the early expanding stage because health conditions improve and the birth rate remains unchanged.
Birth rate: ↑Unchanged
Death rate: ↓Decline
In the early expanding stage, the birth rate does not change but the death rate decreases due to which there is a slight increase in the size of the population.
The world’s population was in this stage from the middle of the 17th century to the middle of the 19th century. India was in this stage from 1921 to 1950
Ex: South Asia, Africa
3)Third stage = Late expanding: In the third stage late expanding stage, the death rate declines a little more and the birth rate declines a little
Birth rate: ↓slide (slightly) decline
Death rate: ↓further decline
In the late expanding stage, the birth rate declines a little while the death rate declines a little more but since the birth rate is slightly higher than the death rate, population growth is seen in it.
Ex: china,Singapore and india
4) Fourth stage= Low Stationary: In the fourth stage low stationary stage, birth rate becomes low and death rate also becomes low due to which population is seen stationary (stable).
Birth rate: ↓low
Death rate: ↓low
Due to low birth rate and death rate in this stage, population is seen to be stable and this is generally seen mainly in developed and industrialized countries.
Zero population growth is recorded in Australia during 1980-1985.
Ex:=Australia in 1980-1985.
5) Fifth stage=Decline stage: In the fifth stage decline stage, birth rate becomes further low while death rate remains unchanged due to which population is seen to decrease.
Birth Rate: ↓Further Low
Death Rate: ↓Unchange
Thus, in this decline stage, there is a decrease in population due to the decrease in birth rate and while there is a death rate, this stage is usually seen in Germany and Hungary.
Ex:= Germany and Hungary.
Demographic cycles help to explain how populations evolve and transition through different stages of development, affected by socio-economic factors, technological advancement and cultural changes.
Q.4 Write short notes. ટૂંકનોધ લખો. (કોઇપણ ત્રણ)12
a) Primary Health Center – પ્રાઇમરી હેલ્થ સેન્ટર
Introduction:
Primary Health Center (PHC) is the first point of contact in the health care delivery system, a well-organized health institution designed especially for rural and remote areas. This center provides comprehensive, integrated, and community oriented health care services to the patient.
- Objectives of PHC:
To provide primary health care to the patients
To provide preventive, promotive, curative and rehabilitative services
To implement national health programmes
To provide health education and behaviour change communication
To achieve specific objectives for maternal and child health
- Location and Population Coverage:
Each PHC is usually designed for a population of 30,000 in rural areas and 20,000 in tribal and hilly areas.
It is set up in areas where other health care resources are not readily available.
- Services Offered:
Outdoor Patient Services (OPD): Treatment of common diseases
Maternal and Child Health (MCH): Antenatal, intrapartum, postnatal care and minimum newborn care
Immunization: All necessary vaccinations under the Universal Immunization Program
Family Planning: Counseling and contraceptive services
Disease Control Programs: Health programs for TB, Leprosy, Malaria, HIV/AIDS etc.
Basic Laboratory Services (laboratory)
Referral Services (referral): Referral to CHC or Tertiary Care Center for complicated cases
- Staffing Pattern:
A PHC has a fixed manpower of:
1 Medical Officer (officer)
1 Pharmacist
1 Lab Technician (technician)
3 Staff Nurses
1 Health Assistant – Male
1 Health Assistant – Female
Other Class IV Staff
- Infrastructure:
OPD Department
Mini Operation Theatre
Laboratory
Maternity Room
6 Bed Inpatient Facility
Store and Drug Depot
Consultation Room and Waiting Area
- Role in National Health Programs
PHC is one of the key locations for implementation of various National Health Programs, such as:
National Tuberculosis Elimination Program (NTEP)
National Leprosy Eradication Program (NLEP)
National Vector Borne Disease Control Program (NVBDCP)
Reproductive and Child Health Program (RCH)
Universal Immunization Program (UIP)
Conversion as Health & Wellness Center under Ayushman Bharat Yojana
- Importance of PHC in Community Health
The patient is provided with immediate treatment and Guidance
Health Awareness and Education
Moral support to protect people from diseases
Multisectoral approach helps in achieving public health targets
- Challenges:
Manpower shortage
Infrastructure and system limitations
Lack of referral mechanism
Inadequate monitoring and evaluation system
Primary Health Center is the foundation of the health care system. Its function is not only to provide treatment but also to improve the health indicators of the entire community by providing preventive and promotive health services to the patients. With proper management, manpower and infrastructure, it provides an accessible, effective and affordable health care platform for the people.
b) ESI Act-ESI એક્ટ
ESI: Employees State Insurance (ESI) Act
The Employees State Insurance (ESI) Act, was passed in 1948. This Act is a comprehensive social security Act in the country. This Act is an important measure to provide social services and health insurance in the country.
Which provides employees (employees) with certain benefits such as case and medical benefits in the event of illness, maternity, disability and death due to employment injury.
Applicability:
The ESI Act is applicable to factories and certain notified establishments where 10 or more persons are employed. It covers both the organized and unorganized sectors of the economy.
This Act provides Rs. It is applicable to employees earning up to Rs. 21,000 per month. However, the Central Government can increase the salary limit by notification.
Coverage:
Employees covered under the ESI Act are entitled to various benefits provided under the scheme.
The Act provides compulsory coverage for eligible employees and employers.
Administration:
The ESI Scheme is administered by the Employees’ State Insurance Corporation (ESIC), a statutory body under the Ministry of Labour and Employment, Government of India.
ESIC manages the funds collected through contributions and ensures the effective implementation of the scheme.
Contribution:
Contributions to the ESI scheme are made by both employees and employers.
The current contribution rate is 1.75% of the salary for employees and 4.75% for employers, which is 6.5% of the total salary.
Inspection and Enforcement:
The scheme inspects the establishments covered to ensure that its provisions are being followed.
Non-compliance with the provisions of the ESI Act can lead to penalties and legal action.
Adjudication and Appeal:
The ESI Act provides for the adjudication of disputes relating to the implementation of the Act.
Employees and employers have the right to appeal against the decisions of the ESIC authorities.
Objective:
The primary objective of the ESI Act is to protect employees and their families from financial hardship in times of medical emergencies and to provide them with quality medical care and social security benefits.
Its objective is to promote health and welfare among industrial workers covered under the scheme.
Benefits of ESI Act:
1) Medical Benefit,
2) Sickness Benefit,
3) Maternity Benefit,
4) Disability Benefit,
5) Dependent Benefit,
6) Funeral Benefit,
7) Rehabilitation Benefit.
1) Medical Benefit:
Medical benefit includes full medical care during hospitalization.
Comprehensive medical care is provided to the insured person and their dependents through a network of ESI hospitals, dispensaries and tie-up hospitals. Which are as follows:
OPD care,
Provision of drugs and dressings,
All types of specialty medical services,
Free drugs,
Pathological and radiological investigation,
Immunization and family planning services,
Domiciliary services,
Antenatal and postnatal services,
Emergency services,
Ambulance services,
Health education in patient treatment.
Medical services like etc. are provided,
and along with
In complicated cases where specialized treatment is required, the patient is sent for institutional treatment outside the state at the expense of ESI Corporation.
Other Medical Benefits:
Dentures,
Artificial Limbs,
Spectacles (Prostheses),
Hearing Aid,
Hernia Belt,
Walking Caliper,
Jacket, etc. are also provided when required.
2) Sickness Benefit:
If the sickness is certified by the Insured Medical Officer or the Insurance Medical Practitioner, then the insured person is entitled to sickness benefits.
Sickness benefit is payable on a case-by-case basis for a maximum of 91 days in any continuous period of 365 days. The rate of payment in a case is 50% of the daily wage.
A person receiving sickness benefit has to undergo medical treatment as provided under the Act.
Extended Sickness Benefit:
If the insured person is suffering from a long-term disease, then as per the Act, he is entitled to extended sickness benefit for a maximum of two years in addition to the 91 days of sickness benefit. There are 34 diseases for which extended benefits can be paid to a person who has been in continuous employment for two years.
Enhanced Sickness Benefit:
An enhanced sickness benefit of 14 days is provided to an assured woman after tubectomy and 7 days to an assured male after vasectomy.
3) Maternity Benefit:
In maternity benefit, an employee who is pregnant gets a leave of 120 to 180 days.
Night work is not provided to such pregnant women from 7.00 pm to 06.00 am.
If there is a medical termination of pregnancy (MTP), then 15 days of leave is given for it.
If there is an abortion in any case, then the woman is given a leave of 6 weeks or 45 days.
Paternity leave is provided for up to 15 days.
Excessive weight-bearing work is not provided to pregnant women under this act.
Pregnant women are also provided with free antenatal, intranatal and postnatal services.
4) Disability Benefit:
In case of temporary or permanent disability due to employment injury, case benefit is provided.
The amount of benefit changes based on the disability.
Temporary Disability Benefit (TDB) is payable from the first day of entry into ineligible employment and any contribution is paid in case of employment injury at the rate of 90% of the salary as long as the disability continues.
Permanent Disability Benefit:
Permanent disability benefits are paid at the rate of 90% of the salary in the form of monthly payments based on the extent of loss of earning capacity as certified by the Medical Board.
In case of total disability, they are given life pension.
5) Dependent Benefit:
In cases where death or injury occurs due to employment injury or occupational hazards, dependents of the deceased or injured person are paid 90% of their wages in the form of monthly payments.
6) Funeral Benefit:
Funeral Benefit provides a cash payment of ₹10,000/- towards the funeral expenses of the insured person on his death.
7) Rehabilitation Benefit:
- The insured person and his family members can continue to receive medical treatment even after permanent disability or retirement.
- The insured worker is provided with an artificial limb when required along with artificial and sickness benefits as per the rate of the case till the artificial limb is replaced.
- Overall, the Employees’ State Insurance Act, 1948, stands as a crucial pillar of social security in India, which improves the welfare of employees and their dependents covered by various benefits with the aim of providing financial assistance and medical care in times of need.
c) First five-year plan પ્રથમ પંચવર્ષીય યોજના
- Introduction:
The First Five-Year Plan (plan) was the first plan implemented in India from 1951 to 1956 for health, agriculture, industrial, and economic development. This plan was specially designed keeping in mind patient and community welfare. It was the first historical attempt to strengthen the foundation of the health sector. - Time Period:
The plan was operational from April 1, 1951 to March 31, 1956. - Objective of the Plan:
- To provide basic needs like nutrition, health and shelter to all citizens of the country
- To boost primary health care and public health services
- To establish health institutions for rural patients
- To start health manpower training programs like multipurpose health workers and midwives
- To reduce maternal mortality and infant mortality rates
- To invest more in vaccination, sanitation and pure water supply
- Allocation for Health Sector:
Total expenditure: ₹2069 crore
Approximately ₹140 crore has been allocated for health and family welfare
A major portion of this is for health infrastructure development and public health was for programs
- Major Health Initiatives:
- Establishment of Primary Health Centers (PHCs) started
- Start of Community Development Programme (programme)
- National Malaria Control Programme (NMCP)
- National Tuberculosis Control Programme (NTCP)
- Leprosy Control Programme (LCP)
- Referral system developed to reach health care to patients
- Special allowance for nursing and midwifery training
- Health Infrastructure Development:
- For the first time, planning of infrastructure for health institutions like PHCs, MCH centres, and State Health Directorates
- Planning of technical manpower to provide accessible health care facilities to patients
- Middle management training programmes to strengthen health administration at state and district levels
- Impact on Community Health Impact):
- Timely treatment, preventive and promotive services started to be available to patients
- Official efforts were started to reduce epidemics and reduce morbidity-mortality
- Direction was set to improve rural health care through trained health workforce
- Effective services were delivered to the target population through national health programmes
- Limitations of the Plan:
- Required manpower and infrastructure were still inadequate
- Public awareness to deliver services to patients was still low
- Funds were not available as per requirement for health and sanitation
- Technical supervision and evaluation mechanisms were not yet developed
- The First Five-Year Plan provided a strong foundation for India’s health policy. Due to the success of this plan, all subsequent plans gave more priority to the health sector. This scheme became a turning point for India in the field of primary health care, disease control programs, patient-centric approach, and health institutional development. It laid the foundation for a structured, sustainable, and people-oriented health care system in India.
d) Types of report – રિપોર્ટ ના પ્રકારો
- Introduction:
A report is a document that presents analytical information, statistics, and observations related to specific health issues. A report is used as an important document in medical, public health, research, and administrative work. A properly prepared report provides guidance on the health status, trends, and preventive measures of a patient or population. - Classification of Reports:
Reports can be categorized according to various criteria, such as use, frequency, source, and purpose. The main types are as follows:
A. Based on Frequency:
- Daily Report:
Information about daily operations, patient visits, medication administration, case registration, etc.
Example: OPD report, immunization record.
- Weekly Report:
Summary of weekly activities
Example: Epidemic Control Report, Sanitation Inspection Report.
- Monthly Report:
Overall overview of health services provided during a month.
Example: Maternal Mortality Rate (MMR), Infant Mortality Rate (IMR).
- Annual Report:
Detailed record of health activities and results carried out during the entire year.
Example: State Health Performance Report, Hospital Annual Report.
B. Based on Purpose:
- Informative Report:
Only intended to provide information.
Example: Report on Patient Demographics.
- Analytical Report:
Includes analysis along with information.
Example: Report on Disease Trends.
- Investigative Report:
A report prepared to investigate a problem or epidemic.
Example: Outbreak of Diarrhea in an Old Age Home.
C. Based on Nature:
- Verbal Report:
Information or report given verbally, such as at shift handover.
Valid for a short period of time.
- Written Report:
In written form. Has official and legal validity.
Example: Nursing Care Report, Death Report, Birth Report.
D. Based on Source:
- Internal Report:
Prepared for use within the organization/hospital.
Example: Staff Duty Report, Inventory Status.
- External Report:
A report sent to an external agency or government.
Example: Report to District Health Office, National Reporting.
E. Special Reports:
- Case Study Report:
A report that provides a detailed health history and care plan for an individual patient.
- Incident Report:
A record of a specific incident or accident that occurred in a nursing or hospital setting.
- Evaluation Report:
A report that provides an evaluation of a program or service.
Q-5 Define following (any six) નીચેની વ્યાખ્યા લખો. (કોઇપણ છ)12
a) Community health nursing કોમ્યુનિટી હેલ્થ નર્સિંગ
Community Health Nursing (nursing) is a systematic and professional nursing practice that is carried out for the health management of individuals, families and groups of the community. It includes aspects of health promotion, disease prevention, patient care, rehabilitation and health education. Community health nursing is an integral part of public health nursing and the primary health care system, which works for the physical, mental, and social well-being of patients. This nursing method works on the basis of nursing science, public health principles and social sciences and adopts a population-oriented and evidence-based approach. The main objective of Community Health Nursing (nursing) is to provide comprehensive, continuous, and quality health care to the patient within their own environment and social context.
b) Demography – ડેમોગ્રાફી
Demography The scientific study of human population and its elements i.e. size, composition and distribution is called demography. Demography is the scientific study of population.
Concept of Demography
Demography is a branch of science that studies human population and focuses on only three elements.
1) Any changes in the size of the population i.e. increase or decrease in size.
2) Structure of the population (basic of age and size).
3) Geographical distribution on the basis of state or region.
C) MMR – એમ એમ આર
Maternal Mortality Rate (MMR) is the number of maternal deaths per 100,000 live births during a given period, usually a year.
Maternal mortality rate(M.M.R) =
Total number of female deaths due to complications within 42 days of childbirth or delivery during a given year
—————- × 100,000
Total number of live births in the same year.
d) Eligible couple – લાયક દંપતિ
An Eligible Couple (couple) is a legally married couple of husband and wife, the wife being in the reproductive age group of 15 to 49 years, and the husband and wife should have a sexual relationship so that there is full potential for pregnancy. An Eligible Couple (couple) is known as the most basic and target unit for family welfare services and family planning programs. By identifying such couples, national population policy, community surveillance, and reproductive health services can be successfully implemented. Identification of the Eligible Couple (couple) is essential for every health worker so that they can provide services such as contraceptive method facilitation, counseling, and maternal-child health care in a timely and appropriate manner.
e) Primary health care – પ્રાયમરી હેલ્થકેર
Primary health care is an essential (necessary) health care that is made universally accessible to everyone and acceptable to everyone through full participation in it and primary health care should be affordable to the community and the country.
f) community health team – કોમ્યુનિટી હેલ્થ ટીમ
A Community Health Team (team) is an organized group of multi-specialty health care professionals responsible for delivering comprehensive, continuous, and coordinated health care services to patients at the community level. This team typically includes members such as nurses, medical officers, health assistants, multipurpose health workers, lab technicians, pharmacists, and auxiliary nurse midwives. The Community Health Team (team) performs functions such as implementing health policies, screening patients, counseling, referrals, follow-up care, and health education. The main goal of this team is to ensure health promotion, disease prevention, and rehabilitative care in the community so that the overall health outcomes of the patient can be improved.
g) Epidemic – એપીડેમીક
An epidemic is a condition in which the spread of a specific disease affects a much larger number of patients than usual in a defined geographical area and over a defined period of time. When the incidence rate of a disease increases rapidly and has a serious impact on the health of the population, it is described as an epidemic. This condition is usually seen in infectious diseases such as cholera, dengue, influenza, chikungunya, or diseases like COVID-19. An epidemic is a matter of significant public health concern because it poses an increased risk of morbidity and mortality of the patient. In such a situation, it becomes imperative to adopt immediate surveillance, reporting, quarantine, treatment, and prevention measures.
h) Refferal System – રેફરલ સિસ્ટમ
Referral System is a health care system in which a patient is referred from a Primary Healthcare Provider to a more specialized specialist or higher level of care when the patient requires more specialized treatment or complex medical intervention. This system ensures that the patient receives the right health care services at the right level at the right time, which helps improve the health outcomes of the patient. Referral System involves different levels such as primary healthcare, secondary healthcare, and tertiary healthcare, where each level provides services according to the health needs of the patient. This system plays an important role in increasing coordination between health institutions, optimizing resources, and providing patient-centered care.
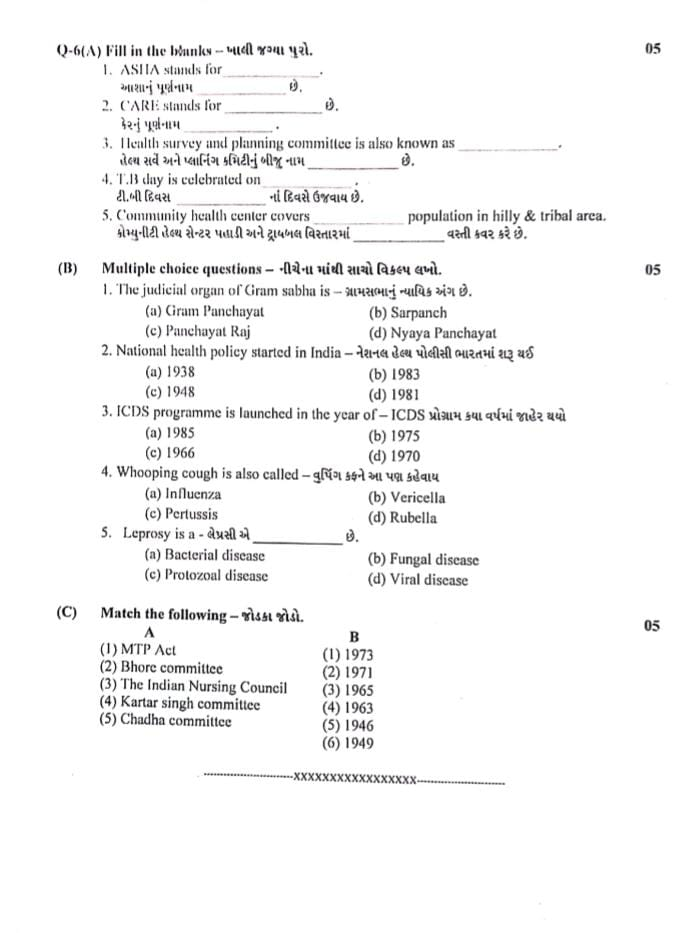
Q-6(A) Fill in the blanks ખાલી જગ્યાઓ પૂરો.05
1.ASHA stands for……
આશાનું પૂર્ણનામ……છે: Accredited Social Health Activist
2.CARE stands for
કેરનું પૂર્ણનામ……: Cooperative for Assistance and Relief Everywhere
3.Health survey and planning committee is also known as…… હેલ્થ સર્વે અને પ્લાનિંગ કમિટીનું બીજુ નામ…… છે : Bhore Committee
4.T.B day is celebrated on……
ટી.બી દિવસ…… નાં દિવસે ઉજવાય છે : 24th March
5.Community health center covers…… population in hilly & tribal area. વસ્તી કવર કરે છે. કોમ્યુનીટી હેલ્થ સેન્ટર પહાડી અને ટ્રાયબલ વિસ્તારમાં……વસ્તી કવર કરે છે: 80,000
(B) Multiple choice questions – નીચેના માંથી સાચો વિકલ્પ લખો.05
1.The judicial organ of Gram sabha is…… ગ્રામસભા નું ન્યાયિક અંગ છે.
(a) Gram Panchayat
(b) Sarpanch
(c) Panchayat Raj
(d) Nyaya Panchayat
2.National health policy started in India……નેશનલ હેલ્થ પોલીસી ભારતમાં શરૂ થઇ.
(a) 1938
(b) 1983
(c) 1948
(d) 1981
3.ICDS programme is launched in the year of …… ICDS પ્રોગ્રામ કયા વર્ષમાં જાહેર થયો.
(a) 1985
(b) 1975
(c) 1966
(d) 1970
4.Whooping cough is also called …… વુપિંગ કફને આ પણ કહેવાય.
(a) Influenza
(b) Vericella
(c) Pertussis
(d) Rubella
5.Leprosy is a……
લેપ્રસી એ……છે.
(a) Bacterial disease
(b) Fungal disease
(c) Protozoal disease
(d) Viral disease
(C) Match the following – જોડકા જોડો.
A B
(1) MTP Act (1) 1973
(2) Bhore committee (2) 1971
(3) The Indian Nursing Council (3) 1965
(4) Kartar singh committee (4) 1963
(5) Chadha committee (5) 1946
(6) 1949
(C) Answer :
| A | B | ✅ Correct Match |
|---|---|---|
| (1) MTP Act | 1971 | (1 → 1971) |
| (2) Bhore Committee | 1946 | (2 → 1946) |
| (3) The Indian Nursing Council | 1947 | (3 → 1947) |
| (4) Kartar Singh Committee | 1973 | (4 → 1973) |
| (5) Chadha Committee | 1963 | (5 → 1963) |
✅ Answer :
- (1) MTP Act → 1971
- (2) Bhore Committee → 1946
- (3) The Indian Nursing Council → 1947
- (4) Kartar Singh Committee → 1973
- (5) Chadha Committee → 1963
