ENGLISH-COMMUNITY HEALTH NURSING 2 (PAPER SOLUTION GNM 3RD YEAR) 10/10/2023(Done)-uplaod-09
COMMUNITY HEALTH NURSING-2 (PAPER SOLUTION GNM 3RD YEAR) 10/10/2023(Done)-uplaod-09
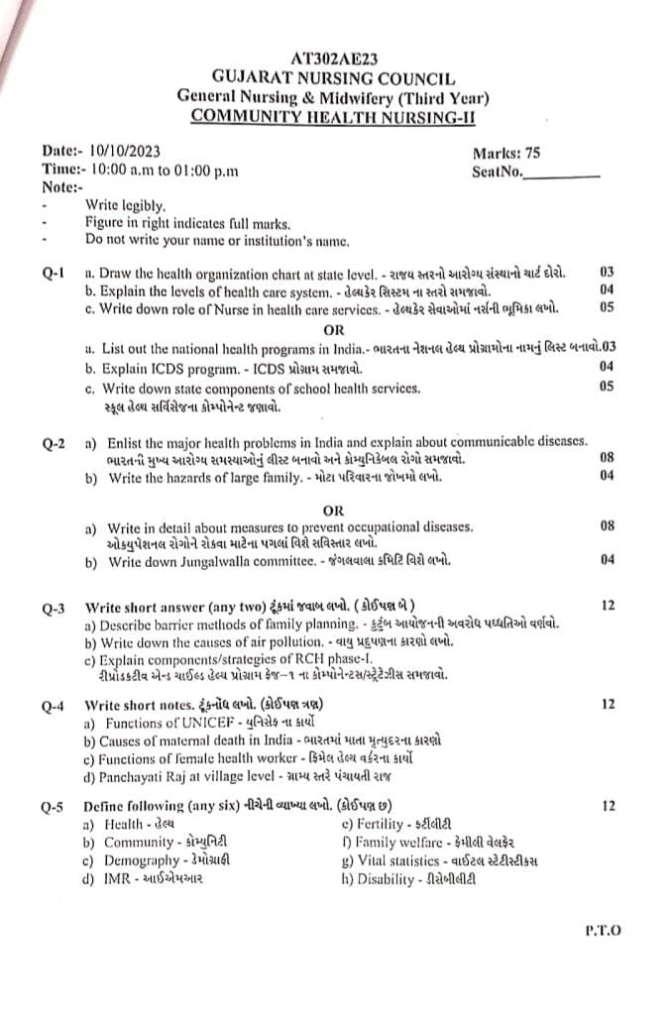
Q-1
a. Draw the health organization chart at state level. – રાજય સ્તરનો આરોગ્ય સંસ્થાનો ચાર્ટ દોરો.03
State Minister of Health in the State:
The State Minister of Health in the State is the head of the Health and Family Welfare Department and the Health Secretary and Commissioner of Health and various directors work under him. He has his own political vision and accordingly the Health Secretary and a large number of administrative staff work accordingly.
State Health Director
This is a technical wing of the State level Health and Family Welfare Department in which the Director of Health and Family Welfare is its head. Under him, the work of Public Health and Health and Family Welfare Services as well as Family Planning Services etc. comes. There is also a Deputy Director to help him and in a state like Gujarat, there is also a Regional Deputy Director. The main work of the former is for Family Planning Services and Health Education. At state level
⬇️
State ministry of health ⬇️ Headed by
Minister of health and family welfare
⬇️
Deputy minister of health and Family welfare ⬇️
Health Secretary
⬇️
Deputy secretary
⬇️ Large Administrative Staff
➡️ State health Director
⬇️
Headed by
⬇️
Director of health and family welfare
⬇️
Deputy Director
⬇️
Assistant Director of health
⬇️
Regional Activities Functional Activities
(Regional Activities) MCH
Nutrition
TB
Family Planning
Leprosy
Health Education
b. Explain the levels of health care system. – હેલ્થકેર સિસ્ટમ ના સ્તરો સમજાવો.04
Health care system is a step-wise overview, which provides services to the patient according to his health related needs. There are mainly three levels of this system — Primary Health Care, Secondary Health Care, and Tertiary Health Care. The function and importance of each level is different, and specific medical care is provided to the patient at each level.
1.Primary Health Care:
Primary health care is the first and closest contact point of the health care system for the patient. Here the patient is provided with basic health services.
Main Features:
At this level, the patient gets first contact care.
Management of common illnesses such as fever, cough, cold, headache, skin infection, hypertension, and diabetes.
Services include health education, immunization, antenatal care, nutrition counseling, and family planning.
If the patient’s condition is complex, he is sent to the next level through referral.
Health care institutions:
Sub Centre
Primary Health Centre – PHC
Health Workforce:
ANM
MPHW
Village Health Workers
2.Secondary Health Care:
Secondary health care is the level where advanced care is provided to the patient by specialist doctors. At this level, patients are usually referred from the primary level.
Main Features:
Specialist consultation and hospital-based care.
Services include pediatric, orthopedic, gynecology, ophthalmology, general surgery, and laboratory testing.
Hospitalization, emergency care, and diagnostic services are available to patients.
At this level, complicated cases are stabilized and referred to tertiary care.
Health Care Institutions:
Community Health Centre – CHC
Sub District Hospital
District Hospital
3.Tertiary Health Care:
Tertiary health care is the highest level of the health care system. Here the patient receives super-specialist care, advanced technology, and multi-disciplinary medical management.
Main Features:
Super-specialist treatment such as neurology, cardiothoracic surgery, oncology, nephrology, and gastroenterology.
Advanced investigations like MRI (MRI), CT Scan (CT scan), PET Scan (PET scan), endoscopy (endoscopy), and biopsy (biopsy) etc. are available.
Critical care units like ICU (ICU), NICU (NICU), CCU (CCU) – where ventilatory support and monitoring are provided.
Advanced medical technologies like organ transplant, cancer therapy, laparoscopic surgery are used.
Health care institutions:
Medical Colleges and Teaching Hospitals (Medical College and Teaching Hospital)
Super Specialty Hospitals (Super Specialty Hospital)
Referral System (Referral System):
Referral system is a strong link in the health care system. Through this system, the patient is referred to a higher level of care according to the nature of his illness. This three-tier structure is very important for timely and appropriate treatment of the patient.
Levels of Health Care System is a medical structure that provides care to the patient at the appropriate level according to his health status. Specific types of health care services are available at each level and connectivity is maintained at all levels through a referral system.
Through these three-tier structures, the health care system provides treatment to the patient at the right level at the right time, which is important for the effective functioning of the health sector.
c. Write down role of Nurse in health care services. હેલ્થ કેર સેવાઓમાં નર્સની ભૂમિકા લખો. 05
Role of Nurse in Health Care Services:
1.Patient Assessment:
The nurse performs a primary evaluation of the patient’s condition, which includes taking the patient’s vital signs – such as blood pressure, pulse, respiratory rate, and temperature. In addition, the patient’s symptoms, medical history, and physical examination are assessed.
2.Direct Patient Care:
The nurse provides direct care to the patient, which involves bedrest, positioning, hygiene, feeding, ambulation, etc. The nurse takes care of all the needs of the patient, especially in the absence of an attendant.
3.Medication Administration:
The nurse gives the medication at the proper dose, route, and time. The routes involved in medication include oral, intravenous, intramuscular, subcutaneous, etc. The nurse follows the Three Checks and Five Rights while administering.
4.Infection Control:
The nurse follows the methods of aseptic technique, hand hygiene, personal protection equipment, and sterilization to prevent the spread of infection in the health care setting.
5.Patient Education:
The nurse provides detailed information to the patient and his family members about the disease, treatment, side effects of medication, diet, and self-care so that the patient can manage his health properly.
6.Emotional and Psychological Support:
The nurse establishes a heartfelt connection with the patient and strengthens the patient on a mental level. If the patient experiences depression, anxiety, or stress, the nurse provides support with counseling and empathy.
7.Care Planning and Implementation:
The nurse prepares a customized care plan for the patient and implements it. The nurse also modifies the care plan according to the patient’s progress. In this process, the nurse follows the Nursing Process – Assessment, Diagnosis, Planning, Implementation and Evaluation.
8.Collaboration with Health Team:
The nurse provides holistic care to the patient through coordination with the Doctor, Physiotherapist, Nutritionist, Lab Technician and other health care professionals.
9.Documentation and Reporting:
The nurse enters all nursing observations, medication records, and response to treatment data of the patient into the nursing charts. Continuity in the patient’s treatment is maintained through proper documentation.
10.Health Promotion and Disease Prevention:
The nurse treats diseases through health education, immunization, and early detection. The nurse strengthens public health through community health services.
The nurse is an important pillar of health care services. It is not limited to just the physical care of the patient, but is also proactive in the psychological, emotional and social well-being of the patient. A skilled and dedicated nurse is the lifeblood of the health care system.
OR
a. List out the national health programs in India.- ભારતના નેશનલ હેલ્થ પ્રોગ્રામોના નામનું લિસ્ટ બનાવો.03
Below is a complete list of all the major National Health Programs in India. Each program is designed by the Government of India to improve public health facilities, disease prevention, patient management, and medical infrastructure.
1.National Health Mission (NHM)
2.National Rural Health Mission (NRHM)
3.National Urban Health Mission (NUHM)
4.Reproductive, Maternal, Newborn, Child and Adolescent Health (RMNCH+A)
5.Ayushman Bharat – Pradhan Mantri Jan Arogya Yojana (PM-JAY)
6.Universal Immunization Programme (UIP)
7.Revised National Tuberculosis Control Programme (RNTCP)
8.National Tuberculosis Elimination Programme (NTEP)
9.National Leprosy Eradication Programme (NLEP) Programme
10.National Vector Borne Disease Control Programme (NVBDCP)
11.National AIDS Control Programme (NACP)
12.National Programme for Control of Blindness and Visual Impairment (NPCBVI)
13.National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases and Stroke (NPCDCS)
14.National Mental Health Programme (NMHP)
15.National Programme for Health Care of the Elderly (NPHCE)
16.National Tobacco Control Programme (NTCP)
17.National Programme for Prevention and Control of Deafness (NPPCD) For Prevention and Control of Deafness
18.National Iodine Deficiency Disorders Control Programme (NIDDCP)
19.National Programme for Prevention and Control of Fluorosis (NPPCF)
20.Integrated Disease Surveillance Programme (IDSP)
21.Rashtriya Bal Swasthya Karyakram (RBSK)
22.Rashtriya Kishor Swasthya Karyakram (RKSK)
23.Pradhan Mantri Bhartiya Janaushadhi Pariyojana (PMBJP)
24.National Organ Transplant Programme (NOTP)
25.National Viral Hepatitis Control Programme (NVHCP)
26.National Deworming Day (NDD)
27.Pradhan Mantri Swasthya Suraksha Yojana (PMSSY)
28.National Bio-Energy Mission for Health (NBEMH)
29.National Iron Plus Initiative (NIPI)
30.Rashtriya Swasthya Bima Yojana (RSBY)
All these National Health Programs are important pillars of the public health system and strive to bring about changes in the health care delivery mechanism of India.
b. Explain ICDS program. ICDS. – ICDS પ્રોગ્રામ સમજાવો.04
ICDS (Integrated Child Development Services) is one of the most important services for child welfare.
ICDS was launched on 2 October 1975. In which there were 33 projects all over the country, in which 4 projects were involved in urban areas, 19 in rural areas, and 10 in tribal areas.
ICDS is a program in which children of 3 to 6 years of age are provided with a natural, joyful and simulating environment through Anganwadi for their growth and development.
ICDS provides basic education to the child. This service includes,
Supplementary Nutrition,
Immunization,
Health Checkup,
Medical Referral Services, Nutrition,
Health Education for Women,
Non-formal Education of Children up to 6 years,
And Pregnant and Nursing Mothers from Rural, Urban, Slum and Tribal Areas are also involved in this scheme.
Integrated Child Development Services (ICDS) Preventive and Developmental Actions are taken.
Objectives:
1) To improve the nutritional status of children in the age group of 0-6 years.
2) To ensure proper psychological, physical and social development of children.
3) To reduce child mortality rate, morbidity rate, malnutrition and school drop out rate.
4) To ensure effective coordination with different departments working for child development.
5) To enhance the capacity of the mother and the nutritional needs of the child through proper nutrition and health education.
Service Package:
1) Supplementary Nutrition,
2) Nutritional Health Education,
3) Immunization,
4) Health Checkup,
5) Pre School Non Formal Education,
6) Referral Services,
•>1) Supplementary Nutrition:
Target Group:
Children up to 0-6 years,
Pregnant Women,
Lactating Women,
Expectant Mothers.
Services Provided By:
Anganawadi Worker (AWW),
Anganawadi Helper.
In this,
Supplementary Feeding is provided.
Growth Monitoring is done.
Work is done for the prophylaxis of Vitamin – A deficiency.
Work is also done to control nutritional anemia.
A survey is conducted in the community to identify pregnant women and children.
Supplementary nutrition is provided for 300 days in a year.
Growth monitoring and nutritional surveillance are also two activities.
For this, growth charts are monitored.
This growth chart is helpful in detecting nutritional status. Weight measurement is done once a month for children below 3 years and weight and height measurement are done four times a year for children aged 3-6 years.
Severely malnourished children are provided special care and referred for better medical services.
2) Nutritional Health Education (NHED):
Target Group: Women (15-45) years. Services provided by: Anganwadi Workers (AWW), Auxiliary Nurses and Midwives (ANM), Medical Officers (MO). Nutrition and Health Education is a key element of the work of Anganwadi Workers.
Nutrition and Health Education (NHED) aims to build the capacity of women in the age group of 15 to 45 years by providing them with education on their own health development needs and child and family care.
In this, health education for nutrition is provided to every pregnant and lactating mother and the highest priority is given to nursing and expectant mothers.
3) Immunization:
Target Group
Children below the age of 6 years,
Pregnant mothers,
Lactating mothers. Services Provided by
Auxiliary Nurse and Midwife (ANM),
Medical Officer (MO) Immunization is especially given to pregnant women and children to prevent them from 6 killer diseases.
These six killer diseases include diphtheria, pertussis, tetanus, polio, hepatitis B (B) and measles. Providing the vaccine can prevent morbidity, mortality, disability, and malnutrition in children due to this major disease. Immunization of pregnant women against TT prevents the rate of maternal and neonatal tetanus.
4) Health Checkup:
Target Group
Children below six years of age,
Pregnant women,
Lactating women. Services provided by Auxiliary Nurse and Midwife (ANM),
Medical Officer (MO),
Anganwadi Worker (AWW). In this, care is provided to children below six years of age, antenatal mothers, and postnatal mothers.
In this, various health services are provided by Anganwadi Workers, PHC staff.
In this, regular health checkup,
Immunization,
Management of malnutrition,
Treatment of diarrhea,
Deworming,
Medicine distribution,
Antenatal-postnatal checkup,
Iron and folic acid supplementary medication,
Services for treating respiratory tract infections,
These types of services are provided. Along with this, services of prophylaxis against deficiency of vitamin A and anemia are also provided.
5) Pre-school Non-Formal Education:
Target group
Children between the ages of three to six years. Service provided by
Anganawadi Workers (AWW). Non-formal pre-school education is an important component. Pre-School Education (PSE) is the backbone of Integrated Child Development Services (ICDS).
These services are provided by Anganwadi Centres.
6) Referral Services:
Target Group:
Children below six years of age, Pregnant Women,
Lactating Mother Services provided by Auxiliary Nurse and Midwife (ANM),
Medical Officer (MO),
Anganawadi Worker (AWW). While conducting health check-up and growth monitoring of children, sick and malnourished children and children who need immediate medical attention are identified and referred to Primary Health Centre (PHC) and sub-centres.
Anganwadi Workers (AWWs) prepare a list of children with disabilities and create a special register for them and refer such children for further treatment.
Thus, Integrated Child Development Services (ICDS) play a crucial role in assessing maternal and child health issues, reducing malnutrition and promoting childhood development.
c. Write down state components of school health services.05
સ્કૂલ હેલ્થ સર્વિસેજના કોમ્પોનેન્ટ જણાવો 05
Aspects/Components of School Health Services:
School health programs involve various components to promote and maintain student health and well-being.
These services are essential to ensure that students have access to healthcare resources and support in the school setting.
Here, the main aspects of school health services are:
1) Health appraisal (assessment) of school children and school personnel.
2) Treatment and follow-up.
3) Prevention of communicable diseases.
4) Healthy school environment.
5) Nutritional services.
6) First aid and emergency care.
7) Mental health.
8) Dental health.
9) Eye Health.
10) Health Education.
11) Education of Handicapped Children.
12) Proper Maintenance and Use of School Health Records.
•>1) Health Appraisal (Assessment) of School Children and School Personnel:
In health appraisal (assessment), health assessment is performed not only of students but also of teachers and other school personnel.
Periodic health check-up of children, teachers and other school personnel.
First medical examination should be done when a child is admitted to school and then medical examination should be done every four years after admission and then examination should be done at the time of leaving school.
The examination includes,
Collecting a complete history of the child,
Performing a physical examination.
Taking the child’s height, weight, teeth, speech, vision, hearing tests.
Conducting laboratory tests on the child, including blood, urine, and stool examinations.
This responsibility usually falls on primary health care providers who carry out services in rural areas and are also responsible for providing treatment to children who are suffering from systemic infections, skin infections, or pediculosis.
Conducting daily checkups of children by teachers in school health services and training school teachers for this and immediately referring the child if they have any health-related complications.
In which, the following changes are observed by the school teachers:
Dull face,
Any abnormality,
Coughing, sneezing, diarrhea.
Headache, fever, or chills,
Red watery eyes,
Sleepiness,
Pain in body,
Scabies, pediculosis,
Cold, nausea and vomiting symptoms are seen.
If any such symptoms are seen, the health care personnel should be informed by the jail teacher for immediate medical service.
2) Treatment and Follow-up:
If any defect is found in the children, advice should be given about the treatment and follow-up of the children to cure them.
If any major illness is detected, inform the parents.
Provide treatment and regular follow-up to the children by the school health nurse and provide proper care to the children.
Conduct follow-up visits to maintain the health of the child.
3) Prevention of Communicable Diseases:
Communicable diseases are controlled through timely immunization. Communicable diseases in children can be prevented through properly planned immunization for the child.
Properly immunize the child as per the National Immunization Schedule.
Properly maintain the record of immunization as part of the school health record and provide it to the child during the school living time.
4) Healthy School Environment:
School building and its environment play an important role in school health.
School should be away from railway station, railway line, bus stand, market and cinema.
There should be one toilet facility for every 25 students which should be strengthened and should be arranged separately for boys and girls.
The school should have safe and separate drinking water, wash basin and school kitchen.
There should be 25% window size of the floor area.
There should be white color classrooms.
Proper lighting facility should be available.
There should be separate water source in the school.
There should be separate room for mid-day meal program (eating facility) in the school.
5) Nutritional Services:
Diet is important for school children. It is important to provide nutritious food to a child who is physically and mentally weak.
For proper development of a child, a nutritious diet should be taken, which should contain adequate amount of calories and protein.
Many children suffer from malnutrition, in which blindness and anemia are seen.
Malnutrition can be corrected through proper and adequate diet.
Properly provide a diet rich in Vitamin A
( A) in nutrition.
Mid-day meal program is necessary to improve the health of children and prevent malnutrition.
6) First Aid and Emergency Care:
A first aid box should always be available in the school. So that accidents, abdominal pain, unexpected situations like spot accidents, epileptic convulsions and diarrhea can be handled.
Teachers should be skilled in providing advice about first aid kits and drugs.
7) Mental Health:
Excessive burden of study and stress due to study leads to mental illness.
Many mental health problems like juvenile delinquency, maladjustment etc. are common problems seen in children. For this, school children are helped by vocational counselor or psychologist.
8) Dental Health: Children frequently suffer from dental diseases or defects and such children are explained about their treatment and teeth clinic.
9) Eye Health:
School is responsible for early detection of refractive error, treatment of squint, myopia eye infection etc.
Children and Vitamin (A) administration.
Provide basic eye health services in schools.
10) Health Education:
Health education is very important for school children. Through it, awareness can be created by providing health matter related information. Motivation can be developed in children and health behavior can be changed.
Attitude of the child towards health can be changed through health education.
Health education is a key element of school health services.
In health education, advice can be given about personal hygiene, environmental health, nutrition, prevention and control of communicable diseases, first and emergency care and home nursing. And health education can be given to parents about reproductive health and psychological problems.
School teachers can motivate children to practice healthy habits through demonstrations, and provide proper education to the children about maintaining high standards of cleanliness in the school, providing safe water supply, and having a good drainage system.
Education should be need wise planned and organized, and should be such that the aim and objective can be achieved.
11) Education of Handicapped Children: The main aim of providing education to handicapped children is that the child can live a normal life as much as possible and can remain independent.
12) Proper maintenance and use of school health records.
Maintain proper records of the care provided to children in school.
It records the child’s name, date of birth, names of his/her parents, etc.
The child’s record also records the child’s past history, physical examination, and screening tests.
Proper record maintenance can provide information about the child’s need for further treatment or any other health-related condition.
By addressing this aspect comprehensively, school health services play a vital role in promoting the health, safety, and academic success of students, contributing to their overall well-being and future safety.
Q-2
a) Enlist the major health problems in India and explain about communicable diseases. ભારતની મુખ્ય આરોગ્ય સમસ્યાઓનું લીસ્ટ બનાવો અને કોમ્યુનિકેબલ રોગો સમજાવો. 08
National Health Problems:
A health problem is a condition in which a person is unable to function normally.
Some of the major health problems include:
1) Communicable Diseases,
2) Non-Communicable Diseases,
3) Nutritional Problems,
4) Environmental Problems,
5) Medical Care Problems,
6) Population Problems
•>1) Communicable Diseases:
Communicable diseases are diseases that are transmitted from one person to another by infectious agents or their toxic products. This transmission can mainly occur directly or indirectly.
Its transmission can occur through contact with body fluids, through respiratory droplets, and through contact with contaminated surfaces.
Communicable diseases are a major health problem in India and 54% of deaths in India are due to communicable diseases.
Communicable diseases such as malaria, tuberculosis, diarrhea,
Acute respiratory diseases,
Filariasis,
HIV/AIDS,
Sexually transmitted diseases(STD)/Sexually transmitted infections(STI).
These communicable diseases are considered a major health problem in India.
a) Malaria:
Malaria is a major health problem in India.
Malaria is caused by the Plasmodium parasite which is transmitted through the bite of mosquitoes. There are four types of malarial parasites:
1) Plasmodium vivax,
2) Plasmodium ovale,
3) Plasmodium malariae
4) Plasmodium falciparum.
Malaria continues to be a major health problem in India. Although the total number of cases has decreased compared to previous years, the incidence of Plasmodium falciparum has increased.
According to WHO, malaria affects 36% of the world’s population, with India contributing more than 70% of the 2.5 million cases reported in South East Asia, while 2/3 of the Indian population lives in malaria zones, with the highest incidence of malaria cases occurring in the states of Madhya Pradesh, Chhattisgarh, Jharkhand, Odisha, Andhra Pradesh, Maharashtra, West Bengal and the North Eastern states.
During 2015, 1.13 million malaria cases were reported, of which P. falciparum accounted for 67% of the cases, while 287 deaths were reported.
b) Tuberculosis:
Tuberculosis is a bacterial disease caused by Mycobacterium tuberculosis. Tuberculosis bacteria affect the lungs and are spread by sneezing, coughing.
India is the country with the highest TB burden. It remains a major health problem. One-fifth of the world’s incidence of tuberculosis disease is found in India alone.
Every year, about 2.2 million people develop tuberculosis disease, of which 0.62 million are new smear-positive highly infectious cases and 0.24 million people die from tuberculosis disease every year.
According to WHO 2010, tuberculosis in India was estimated to be 249 per 100,000 population and the mortality rate due to tuberculosis disease was 23 per 100,000 population.
( C ) Leprosy:
Leprosy is another major health problem in India.
It is a bacterial disease caused by the bacteria Mycobacterium Leprae. It is transmitted by close contact with an infected person. The disease affects the skin, mucous membranes, and nervous system, causing skin discoloration and nerve damage.
Leprosy is a major health problem in India. According to the World Health Organization (WHO), India accounts for 65% of new cases of leprosy. During 2013-14, 1.27 lakh cases were detected. Of these, 9.49% were in children under 15 years of age and the deformity was grade II.
Of these, 51.48% of cases were estimated to be multibacillary. All states and union territories report cases of leprosy. However, there are significant differences not only between one state and another but also between one district and another.
India is home to 54% of the world’s leprosy.
( d ) Diarrhea:
Diarrhea is caused by bacteria, viruses and other disease conditions.
Diarrheal diseases are considered a major cause of morbidity and mortality in children under five years of age.
There are about 11.67 million cases of diarrheal diseases which occur in India due to poor environmental conditions.
In 2013, more than 100,000 children under the age of 11 months died due to diarrhea.
Diarrhea is the second leading killer disease of young children worldwide after pneumonia.
India has the highest number of diarrheal diseases. Diarrhea is a preventable and treatable disease.
It is also the leading cause of malnutrition in children under five years of age.
More than 2.3 million children die every year, of which 334,000 children die due to diarrhoeal diseases.
(e) Acute Respiratory Diseases:
Acute respiratory diseases are a major cause of morbidity and mortality in children under five years of age in India.
During 2014, 34.81 million episodes of acute respiratory diseases were reported with 2,932 deaths.
( f) Filariasis:
Filariasis is endemic in about 255 districts of 16 states and five union territories in India. About 630 million population is at risk. To achieve elimination of LF (Lymphatic Filariasis), GOI (Government of India) has started Nationwide Annual Mass Drug Administration (MDA) with annual single recommended dose of Diethylcarbamazine Citrate tablets, besides increasing home-based foot care and hydrocele operations.
National Filariasis Control Programme was started in 1955.
( G )HIV/AIDS:
HIV( Human Immunodeficiency Virus)/AIDS( Acquired Immunodeficiency Syndrome.
AIDS( Acquired Immunodeficiency Syndrome) is caused by exposure to infected blood semen(vaginal fluid).
The Indian Ministry of Health and Family Welfare estimated that the prevalence of HIV among adults (15-49 years) in 2011 was 0.27%, while the number of people living with HIV was 420,88,642, the number of new HIV infections in adults was 1,16,456 and the annual number is .
( h)STD/ STI:
More than 1 million people get sexually transmitted infections every day. Every year, about 550 million people get STIs- chlamydia, gonorrhea, syphilis and Get sick from trichomoniasis.
More than 530 million people have genital herpes. More than 290 million women have human papillomavirus infection. Most STI infections present without symptoms. This sexually transmitted infection can be transmitted from mother to child through the placenta or during delivery of the baby.
b) Write the hazards of large family. મોટા પરિવાર ના જોખમો લખો.04
Hazards of Large Family
The emotional life of a large family often brings with it many health risks and medical complications. It becomes difficult to maintain proper healthcare, nutrition, emotional support and sanitary conditions for each patient living in a large family. Below is a complete and precise description of all the possible hazards of a large family with medical terminology:
- Overcrowding:
When many family members live in the same house, overcrowding occurs in the physical space. Due to this, the patient experiences sleep disturbance, high blood pressure, and overactivity of the adrenal gland that releases stress hormones. In the long run, this causes anxiety and immune dysfunction.
2.Poor Sanitation and Hygiene
Living together with many members makes it difficult to maintain hygiene. The risk of gastroenteritis, scabies, helminthic worm infestation, and urinary tract infection increases. Infectious diseases can spread rapidly due to the inability to maintain meticulous hygienic control.
3.Nutritional Deficiencies
If family finances are limited, the patient does not get adequate nutrition. Especially, deficiency of nutrients like Iron, Vitamin D, Vitamin A, and Calcium causes conditions like Severe Anemia, Night Blindness, and Rickets in children and pregnant patients.
4.Mental Health Disorders
Due to lack of adequate emotional support from parents, patients develop Depressive Disorder, Obsessive-Compulsive Disorder, and Generalized Anxiety Disorder. Teenage Burnout Syndrome is also seen in young patients.
- Increased Risk of Communicable Diseases
Close contact is more common in large families, which leads to the rapid spread of communicable diseases such as Tuberculosis, Hepatitis A, Conjunctivitis, and Foodborne Poisoning. Pediatric patients are especially at high risk if there is no vaccination coverage.
- Financial Constraints:
Many patients find it difficult to manage their medical expenses, schooling, and nutrition-related expenses. Regular health check-ups, diagnostic testing, and medicine supply are not possible for multiple patients. This leads to a decrease in the quality of health of the patient.
7.Reproductive Health Burden
Lack of family planning leads to frequent pregnancies. Serious conditions like uterine prolapse, endometriosis, and postpartum complications are seen in female patients. Due to excessive pregnancies, nutritional storage decreases, which also increases the risk of maternal mortality.
8.Developmental Delay in Children
Lack of attention and mental stimulation leads to speech delay, autism spectrum disorder, and learning disabilities in children. If the brain development of pediatric patients is not provided with a proper environment, cognitive functions remain low.
- Educational Inequality:
It becomes difficult for all children to get a good and customized education. Due to the lack of learning support for patients with special needs, school dropout, academic failure, and confidence loss are seen.
- Delayed Medical Intervention
If there are many patients, it becomes challenging for everyone to get timely medical diagnosis and treatment. Due to this, chronic diseases such as diabetes, hypertension, and kidney disorders can develop and are detected at a late stage.
11.Parental Burnout
Constantly caring for many children and fulfilling daily responsibilities leads to Parental Burnout. This leads to chronic fatigue, muscle pain, and psychosomatic disorders in parents.
12.Sibling Rivalry and Behavioural Disorders
Rivalry for attention occurs between multiple children in the same household. This leads to anger issues, conduct disorders, and personality disorders in patients.
- Neglect of Elderly Patients:
In a large family, there is not enough focus on senior patients. Due to this, they may get Osteoarthritis, Dementia.
OR
a) Write in detail about measures to prevent occupational diseases. ઓક્યુપેશનલ રોગોને રોકવા માટેના પગલાં વિશે સવિસ્તાર લખો.08
Measures to Prevent Occupational Diseases
Occupational diseases are physical or mental diseases that occur as a result of continuous exposure of the patient to hazardous substances and unsafe work environment at the workplace. Such as silicosis, asbestosis, hearing loss, musculoskeletal disorders, dermatitis, or even psychological burnout. Such diseases severely affect the patient’s quality of life and work performance. The following are the complete and medically based measures to prevent occupational diseases:
- Workplace Risk Assessment:
First, it is necessary to identify the health hazards present to the patient in every industrial and commercial workplace. Risk assessment evaluates Pathogenic Agents, Chemical Exposure, Biomechanical Stress, and Mental Workload.
2.Use of Personal Protective Equipment:
To protect the patient from occupational hazards, the use of Personal Protective Equipment (PPE) such as respirators, earmuffs, safety gloves, goggles, and body suits should be mandatory. PPE reduces the direct exposure of the patient.
3.Engineering Controls
Health risks are reduced by making changes in the design of machines and workplaces. Such as Ventilation Systems, Sound Proofing, Automated Machines and Air Filtration Devices – all of these mechanically control the patient’s exposure.
4.Administrative Controls
Reducing working hours, implementing a rotation shift system and increasing break times. Such administrative morphology protects the patient from chronic fatigue and overexertion.
5.Medical Surveillance and Health Screening
Regular health monitoring of the patient and pre-employment medical check-up are essential. It can detect early symptoms of occupational diseases such as respiratory distress, skin rashes, hearing loss, etc.
- Vaccination Programs
Vaccinations such as Hepatitis B, Tetanus, and Influenza are essential for healthcare workers, lab technicians, or virus-exposed patients. Vaccination strengthens the patient’s immune response.
- Occupational Health Education
Making patients aware of the risks of their work is an important step. Training should focus on the correct use of PPE, recognition of health symptoms, and emergency response. Health literacy is a powerful tool for the prevention of occupational diseases.
- Ergonomic Modifications
Ergonomic design of the workplace is very important for patients who move, lift, or sit in front of a computer for long periods of time. If proper technique and position are not adopted, permanent conditions such as musculoskeletal disorders, lumbago, and cervical spondylosis can occur.
9.Psychosocial Support and Stress Management
Mental health counseling and stress relief programs are necessary for specific occupations such as healthcare, factory, or construction workers. Yoga, relaxation therapy, and monotony reduction are helpful in controlling the levels of stress hormones such as cortisol.
10.Legislative and Policy Measures
Government occupational safety and health regulations should be implemented. Such as Factories Act, Statutory Welfare Schemes, and Compensation Policy – all of which protect the rights of patients and ensure their safe work environment.
Occupational diseases can never be prevented by medical treatment alone. It requires multi-dimensional preventive strategies – including engineering controls, personal safety, health education, and periodic monitoring – all of which cannot be prevented without engaging in them.
b) Write down Jungalwalla committee. જંગલવાલા કમિટિ વિશે લખો 04
Jungalwalla Committee was an important committee set up by the Government of India in 1961, headed by Dr. N. Jungalwalla. The main objective of this committee was to bring organizational unity between Medical and Health Services in the country, make service delivery more efficient for patients and strengthen the healthcare system professionally.
This committee gave recommendations based on which the public health infrastructure, medical administration and patient care system can be reformed.
- Integration of Services
The committee said that Preventive, Promotive, Curative and Rehabilitative health services—all should be merged into one system instead of being separate. With this integration, the patient will not get fragmented care but will get comprehensive and continuous care.
- Unified Cadre
The committee proposed a unified cadre for all types of healthcare workers. That is, Medical Officers, Public Health Workers, Specialists, etc.—all under a single service structure. This would ensure that patients would receive the same level of service at every level.
- Common Seniority
Along with the unified cadre, the committee also proposed common seniority. This meant that there would be equality in terms of promotion and transfer for all categories of health workers, which is important for the quality of service to patients.
- Prohibition of Private Practice
The committee clearly recommended that all doctors on government payroll should not be allowed to practice privately. The committee advocated for only full-time government service to ensure dedicated care and ethical service to the patients.
- Equal Pay for Equal Work
The committee recommended equal pay for equal responsibilities for various medical and health personnel. This step was considered essential if there is to be no discrimination in service to the patients.
- Training and Orientation
The committee recommended regular orientation of the medical personnel, especially in Public Health, Family Welfare, Epidemiology, Health Education and Communication Skills to keep them updated. This makes it easier to provide more effective and evidence-based care to the patients.
- Code of Conduct
The committee suggested adopting clear ethical standards for all health professionals. Such as—maintaining confidentiality, taking decisions in the interest of the patient, staying away from corruption and avoiding all types of dual practice.
8.Centralized Administrative Structure
The committee suggested that there should be a central controlling authority for health services. This would ensure that the same quality of service is available to the patient at every location and accountability could be determined at the local level as well.
9.Career Structure and Motivation
There should be a clear and stable career path for health workers—including promotion, incentives and recognition. This also ensures proper care for the patient as health workers devote a long time to their field.
The Jungalwalla Committee presented a vision to bring about a fundamental change in the pattern of the Indian health system. The recommendations of this committee are still relevant today, especially as quality healthcare for patients has become a national agenda. The committee established the pillars of equity, efficiency and ethics in health services—which are considered as the basicity evidence for India’s public health system.
Q-3
Write short answer (any two) ટૂંકમાં જવાબ લખો. (કોઈપણ બે) 12
a) Describe barrier methods of family planning. – કુટુંબ આયોજનની અવરોધ પધ્ધતિઓ વર્ણવો.
Temporary methods are generally used to postpone birth and to space births. This method is mostly used by couples who do not want more children or who want to space children out.
Barrier method: Barrier method prevents the connection of sperm with the ovum. It is called barrier method. This barrier method prevents sperm from being deposited in the vagina and also prevents sperm from penetrating the cervical canal. It usually uses mechanical, chemical and combined methods.
Physical method: Includes male condom, female condom, diaphragm, vaginal sponge.
Chemical Method:
Cream: Delfen/Pharmatex
Jelly: Coromax, Volper Paste.
Foam Tablet: Aerosol Foams, Chlorimin T, Contab.
Combination: It usually uses a combination of mechanical and chemical methods.
Combination Method: It uses a combination of mechanical and chemical methods.
1) Male Condom: Male condom is a male barrier contraceptive. It comes from the Latin word “condom” and was invented by Dr. Condom. The latest condoms are available in different sizes. They are 160-180 mm in length, 49-52 mm in width and 0.04-0.07 mm in thickness. They are plain or teatwad with a tip for semen collection. They are available in different colors. Among them,
Dry type Ex: Nirodh (Government Supply) and Kohinoor,
Prelubricated type Ex: Durex, Kamasutra and or spermicidal ones Ex: Raksha etc. are available.
It is an effective and very widely used device which does not have any side effects and can also prevent pregnancy. Condoms prevent both male and female from sexually transmitted diseases (STD).
Advantages:
Cheap and has no contra-indications and side effects.
Disposable for use, simple and easy to carry.
It provides protection against sexually transmitted diseases (STD) and pelvic inflammatory disease (PID).
Reduces the incidence of tubal infertility and ectopic pregnancy.
Used when coitus is irregular and infrequent.
Prevents premature ejaculation.
Used when pills and IUCD are contraindicated.
Disadvantages:
Sleep or breaks occur during coitus.
Sexual pleasure remains insufficient. Psychological disturbances remain.
Latex allergy can occur.
2) Female condom: Female condom is a newly developed female barrier contraceptive that combines the features of a diaphragm and a condom. It is made of synthetic latex or polyurethane. It has a similar structure in which the internal ring covers the cervix and the external ring remains on the outside of the vagina. It is prelubricated with silicone and does not require spermicide.
Advantages:
It prevents STDs (sexually transmitted diseases) more effectively than male condoms because some female condoms also cover the perineum.
Since it is made of polyurethane, it does not cause allergic reactions.
Male condoms are more convenient because they require pre-coitus insertion and are less likely to break.
Disadvantages:
Expensive.
Some women have difficulty inserting.
Failure rate 5-21/100 women.
3) Vaginal diaphragm: This is an intravaginal device made of synthetic rubber, flexible metal, or plastic material. Its diameter is 5 to 10 cm. It has a flexible rim, usually made of spring or metal. A medical or paramedical person is required to measure its size. Its rim extends from the upper end of the posterior fornix in the vagina to its lower end at the back of the symphysis pubis, completely covering the cervix. It should be kept in place for a minimum of 6 hours after sexual intercourse. The failure rate is 4-12/100 women.
4) Vaginal Sponge: This combined vaginal barrier contraceptive is a sponge made of polyurethane. It contains 1gm Nonoxonal-9 spermicide. Its shape is like a mushroom cap. Its concave side covers the cervix in the upper vagina. Vaginal sponge is easy to use, it has to be moistened with water and inserted into the vagina after kneading. It remains effective for 24 hours. It releases 125 – 150 mg of Nonoxonal in 24 hours.
Chemical Method: Its other name is also spermicide because it kills sperm, thus preventing chemical contraceptive pregnancy.
Ex: Foam tablet, aerosol, cream, jelly, paste, suppository, soluble film etc. All these are inserted deep into the vagina 15 minutes before the spermicide coat.
Advantages:
It is easy to use.
It is not very expensive and increases vaginal lubrication.
Dish Advantages:
It has to be inserted deep in all the places where the form reaches and before every sexual activity. The couple may experience irritation and burning sensation.
Combined method: When a barrier method is used along with a chemical method, it is called a combined method, which usually provides double protection.
b) Write down the causes of air pollution. વાયુ પ્રદુષણ ના કારણો લખો
Causes of Air Pollution:
Air pollution is a serious health condition of today’s era, which has a negative effect on the lungs, brain, heart and overall body functions of the patient. Below is a detailed description of its main causes:
1.Vehicle Emissions
The harmful gases such as carbon monoxide, nitrogen oxides and particulate matter emitted from vehicles such as passenger cars, trucks, bikes and buses, which are widely used in today’s travel arrangements, are the main source of air pollution.
Emissions cause diseases like bronchitis, asthma and respiratory tract infection.
- Industrial Discharges
Pollutants like sulfur dioxide, carbon dioxide, lethal hydrocarbons emitted from factories, refineries, chemical plants etc. affect the environment.
These gases cause irritation in the nostrils, burning sensation in the eyes, and allergic reactions.
3.Burning of Fossil Fuels
The burning of coal, diesel, petrol and natural gas produces energy in public places but also releases harmful toxic gases. This pollution is responsible for lung damage, heart rate irregularity and cardiovascular disorders.
4.Agricultural Activities
Pesticides, herbicides and chemical fertilizers used in farms spread pollution by flying into the air.
These pollutants affect the patient’s respiratory system and can also cause kidney and liver damage in the long term.
5.Household Emissions
Indoor air pollution occurs due to smoke and fumes from biomass such as wood, sacks and condensed oils used indoors.
The carcinogenic elements arising from these cause serious disorders like lung cancer and COPD.
6.Waste Burning
Open burning of household waste, plastic materials and rubber produces toxic chemicals such as dioxins and furans.
These gases disrupt human hormonal balance and also cause neurological disturbances.
7.Construction and Demolition Activities
During construction, dust particles, cement powder and asphalt particulate matter are released into the atmosphere.
This pollution causes sinus inflammation, respiratory distress, and allergic response.
8.Natural Sources
While most sources are man-made, there are also some natural causes such as volcanic eruptions, wildfires, and dust storms, which increase air pollution.
These natural events have a serious effect on the patient’s body’s oxygen assimilation.
Air pollution is a multifactorial problem in which many harmful pollutants are present in the atmosphere as part of vehicles, industries, household appliances, farming, natural events, and construction activities.
This causes serious impact on the respiratory, cardiac, neural and organ-specific systems in the patient.
Enforcement at the policy level, technological upgradation and individual awareness are the most necessary steps for air pollution control.
c) Explain components/strategies of RCH phase-1.રીપ્રોડકટીવ એન્ડ ચાઈલ્ડ હેલ્થ પ્રોગ્રામ ફેજ-૧ ના કોમ્પોનેન્ટસ/સ્ટ્રેટેઝીસ સમજાવો
RCH (Reproductive and Child Health) Phase-1 is a national health program launched by the Government of India in the year 1997, whose main objective is to improve the health parameters of female and child and reduce the maternal and neonatal mortality rate. RCH Phase-1 includes various comprehensive health strategies.
The main components and strategies of RCH Phase-1 are explained:
- Essential Obstetric Care
Under this component, antenatal care, normal delivery services and postnatal monitoring are provided to pregnant women.
The service is provided by trained skilled birth attendants at primary health centers and community health centers to reduce maternal mortality.
- Emergency Obstetric Care
Where the patient has a complicated pregnancy or high risk delivery, facilities have been set up for emergency obstetric interventions such as cesarean section, blood transfusion and intensive monitoring.
For this, First Referral Units have been made functional.
3.Child Health Care:
Strategies like immunization, nutritional therapy, newborn resuscitation and acute respiratory infection management were implemented to reduce neonatal mortality rate to minimum.
Oral rehydration solution (ORS) and zinc therapy are used for diarrhea management.
4.Control of Reproductive Tract and Sexually Transmitted Infections (RTI/ STI Control)
Syndrome-based diagnosis for Reproductive Tract Infection (RTI) and Sexually Transmitted Infection (STI) for prevalence and treatment and RTI/STI clinics were established at major metro units.
This strategy is also very useful for HIV/AIDS prevention.
5.Birth Spacing and Family Planning
Giving women informed choice according to sexual health rights and providing services like IUCD (intrauterine contraceptive device), oral pills, condoms and sterilization for family size control.
Postpartum IUCD application has been made particularly popular.
6.Adolescent Reproductive and Sexual Health (Adolescent R.S.H.)
Includes menstrual hygiene, sex education, and counseling services for teenage patients.
Confidential advice and curative services were provided through Yuva Mitra Clinics.
7.Training of Health Personnel
Specialized training programs were implemented for ANMs, nurses, midwives and medical officers to make them capable for skilled birth and new born care.
8.Behavior Change Communication
Public awareness campaigns were conducted through IEC (Information, Education & Communication) and BCC (Behavior Change Communication) to change health related attitudes and practices.
Major maternal and child health issues were highlighted through mass media, folk drama and personal counseling.
RCH Phase-1 was an integrated approach launched to bring about improvements in maternal, newborn and reproductive health. Each component leads to holistic care of the patient and accessible services.
This program is a solid step towards the health of the future generation.
Q-4 Write short notes. ટૂંકનોંધ લખો. (કોઇપણ ત્રણ) 12
a) Functions of UNICEF – યુનિસેફ ના કાર્યો
1.child health
UNICEF provides support for vaccine production in many countries
UNICEF helps in environmental sanitation programs to improve the quality of life of people living in villages to ensure that they have access to safe drinking water and household water.
Currently, the focus is on ensuring that mothers and children have access to primary health care. This includes immunization in the fund and young children’s health, safe water and sanitation, family planning.
2.Child nutrition
UNICEF gives high priority to improving nutrition. The old SAF first helped in nutrition by supplementing child diets with the development of low-cost protein-rich food mixtures in the 1950s.
In collaboration with FAO, UNICEF began supporting the Apply Nutritional Programme through channels such as community development, agricultural extension, schools and health services, to encourage and support rural areas to grow and consume the foods needed for better child nutrition.
UNICEF also provides equipment for modern dairy farming in various parts of India
- Family and Child Welfare
UNICEF’s main objective is to improve the care of children inside and outside the home through Parent Education Day Care Centres, Child Welfare and Youth Agencies and Women’s Clubs
This programme is being implemented as part of the expansion of Health, Nutrition Education and Home Economics
- Education UNICEF, in collaboration with UNESCO, funds the training of all persons including health and sanitation workers and teachers. It emphasizes the motto that universal immunization is the best prevention. UNICEF also provides technical supplies, equipment, paper for tax books, medicine for health clinics and pipes for clean water supply in villages
It helps the government to plan, develop and expand community-based services in the areas of maternal and child health, nutrition, clean water and sanitation It helps mothers and children in natural disasters, in conflicts between two people and in epidemic diseases. It works to prevent TB, malaria, eye diseases and other diseases. UNICEF supports and helps in the implementation of various works for children and the Convention on the Rights of the Child. UNICEF covers programs that help in the survival and development of children such as immunization, nutritional habits, growth monitoring, home best management, drinking water, environment, fitting practices, sanitation and education of girls etc.
b) Causes of maternal death in India – ભારતમાં માતા મૃત્યુદરના કારણો
Causes of maternal death in India
1) Obstetric hemorrhage:
Antenatal hemorrhage (bleeding before birth) and postpartum hemorrhage (bleeding after childbirth) are the main causes of maternal mortality and are more common in places where emergency obstetric care facilities are less available or not available at all.
2) Hypertensive disorders:
Conditions such as preeclampsia and eclampsia during pregnancy, in which the mother’s blood pressure increases and the mother suffers from seizures, can also increase the maternal mortality rate.
3) Infection:
Infections such as sepsis (infection of the blood stream), postpartum infection (infection seen after childbirth), and unsafe abortion-related infections have increased the mortality rate.
4) Obstructed Labour:
When there is a condition of prolonged labour, i.e. the labour process is obstructed, uterine rupture or infection can occur, then in such a condition, when immediate emergency obstetric care is limited, maternal death can occur due to the lack of adequate health care facilities available to the mother in an area.
5) Unsafe Abortion:
In areas where abortion services are not available and are restricted, complications of unsafe abortion practices can lead to maternal death.
6) Pre-existing medical condition:
A woman who has any pre-existing health-related condition such as diabetes, heart disease, and HIV/AIDS can have complications during pregnancy and childbirth, which can increase the maternal mortality rate.
7) Lack of access to quality maternal health services:
Maternal deaths are mainly caused by limited facilities for skilled birth attendants, emergency obstetric care, essential medications, and blood transfusions, especially in rural and backward areas.
c) Functions of female health worker – ફિમેલ હેલ્થ વર્કર ના કાર્યો
“Functions of Female Health Worker” :
1.Maternal Health Services:
Female Health Worker provides (Antenatal), (Intranatal) and (Postnatal) care to pregnant patients. During this, she monitors the patient’s Hemoglobin level, blood pressure, uterine growth, fetal heart sound etc. She gives (Iron-Folic Acid) tablets and (Tetanus Toxoid) injections to the patient. If there is a high risk pregnancy, she refers it on time. She helps with aseptic technique during home delivery and observes the health of the patient and the newborn baby.
2.Child Health Services:
Female health workers provide regular (Immunization), nutritional monitoring and disease prevention for patients (children) aged zero to five years. Assess patient’s growth parameters such as weight, height and Mid Upper Arm Circumference. Provide supplementary nutrition to patients with malnutrition. Also provide (Home Based Newborn Care) for newborns.
3.Family Planning Services
Counseling the patient and his partner about family planning options such as (Oral Contraceptive Pills), (Condom), (Intrauterine Device). Explains temporary and permanent methods to maintain family size. Makes referrals for permanent methods such as (Tubectomy) and (Vasectomy). Gives demo to the patient for proper use and also informs about side effects.
4.Immunization Services
Female Health Workers provide vaccines like (BCG), (OPV), (Pentavalent Vaccine), (Measles-Rubella), (Hepatitis B) etc. under Universal Immunization Program. Monitors Adverse Events Following Immunization. Updates vaccine register and vaccination history of the patient.
5.Adolescent Health Services:
Female Health Workers supply (Iron-Folic Acid) to adolescents and girls especially. Provides (Sanitary Napkins) to them under (Menstrual Hygiene Scheme). Creates awareness about (Health and Nutrition Education), personal hygiene and sexual health through peer educator model.
6.Communicable Disease Control
Plays an active role in the identification and prevention of diseases like (Malaria), (Tuberculosis), (Dengue), (Diarrhea), (Measles). Makes (Referral) based on the symptoms of the patient. Supports (Rapid Diagnostic Test) and consults with the Medical Officer if needed. Also carries out anti-larval activities for vector borne diseases.
7.Non-Communicable Disease Screening
Screens patients for (Anemia), (Hypertension), (Diabetes), (Breast Cancer) etc. Guides the patient on diet, lifestyle modification and follow-up based on risk factors.
8.Health Education & Counseling
Provides awareness to the patient and his family on topics like Maternal Health, Child Care, Nutrition, Hygiene, Sanitation, HIV/AIDS, Drug Prohibition, Family Planning. Motivates for healthy habits through (Behavior Change Communication).
9.Home Visits & Follow-ups
Female health workers visit the home of every registered patient regularly. Especially follow-up for (Pregnant), (Postnatal), (Newborn), (Malnourished) patients. They try to provide health services at home and avoid the need to bring the patient to the health center.
10.Record Keeping & Reporting
Keeps all information like (Mother and Child Protection Card), (Eligible Couple Register), (Immunization Register), (Village Health Register) updated. Prepares reports on disease trends, vaccination coverage and health status. Submits timely monthly reports to the office.
11.Participation in National Health Programs
Female health workers actively participate in the following national programs:
(Reproductive, Maternal, Newborn, Child and Adolescent Health – RMNCH+A)
(National Tuberculosis Elimination Program)
(National Vector Borne Disease Control Program)
(National Leprosy Eradication Program)
(National Nutrition Mission)
(Janani Suraksha Yojana)
(Pradhan Mantri Matru Vandana Yojana)
Female health workers are the foundation of health services at the grassroots level. It looks after the health of patients through preventive, promotive and curative services and is vital to the functioning of the National Health System.
d) Panchayati Raj at village level – ગ્રામ્ય સ્તરે પંચાયતી રાજ
Panchayat Raj consists of the following three institutions at the village level.
1 Gram Sabha
2 Gram Panchayat
3 Nyaya Panchayat
- Gram Sabha
The Gram Sabha is a meeting of all the adults of the village who are registered voters of the village.
They meet at least twice a year and discuss important issues.
It discusses health related developmental aspects. Gram Sabha elects the members of Gram Panchayat - Gram Panchayat
A Gram Panchayat consists of 15 to 30 elected members known as Panch, which is the executive organ of Gram Sabha. Gram Panchayat covers a population of 5000 or more than 15,000. The head of Gram Panchayat is called Sarpanch. It also includes Vice President, Deputy Sarpanch and Panchayat Secretary. Members of Gram Panchayat hold office for a term of three to four years.
Functions of Gram Panchayat
The functions of Gram Panchayat are very wide and cover the entire field of civil administration. The functions are as follows
Sanitation
Public Health
Socio-Economic Development of Village
Planning and organizing health activities in the village
- Justice Panchayat
It consists of five members of the Panchayat
It provides amicable solutions to disputes between two parties or groups or individuals of the village
It solves the problem of going to the formal judicial system and creates a harmony and peace-filled environment among the members and the village
Q-5 Define following (any six) નીચેની વ્યાખ્યા લખો. (કોઇપણ છ)
a) Health-હેલ્થ
Health is a state of complete physical, mental, social and spiritual well-being and the absence of disease or infirmity.
-WHO,1948
b) Community – કોમ્યુનિટી
A community is a group of people who share a common geographic area, social structure, culture, or interest and interact with each other. In the health sector, a community is the entire population, including patients, that collectively affects their health, living conditions, lifestyle, and access to health services. Community health is essential to improving the health status of this group, including components such as promotion, prevention, care, and rehabilitation.
c) Demography – ડેમોગ્રાફી
Demos means people
Graphine means the record.
Demography
The scientific study of human population and its elements, i.e. size, composition and distribution, is called demography. Demography is the scientific study of population.
d) IMR – આઈએમઆર
IMR- I.M.R(Infant Mortality Rate)
The number of children who die within the age of 1 year out of the total number of live births in a given population of one thousand in the same year is called Infant Mortality Rate (IMR).
IMR =
Number of deaths of children less
than one year of age in a year
_ x 1000
Number of live births in the same year
e) Fertility – ફર્ટીલીટી
When there is an ability to conceive and bear children, it is called fertility. Fertility is the natural capacity to produce offspring.
f) Family welfare – ફેમીલી વેલફેર
Family Welfare is a health-focused social work that promotes the overall physical, mental and reproductive health of family members and enhances the standard of living and well-being of the family through family planning, maternal and child health, nutrition, disease prevention and health education. The main objective of Family Welfare programs is to help people achieve fertility regulation and health awareness through patient-centered and voluntary methods.
g) Vital statistics – વાઈટલ સ્ટેટીસ્ટીકસ
Vital Statistics are statistical information that is related to the basic events of life such as birth, death, marriage, divorce and population change. These statistics are important for measuring the health status of a country, social development and the effectiveness of health services. Vital Statistics form the basis for policy making, planning and resource allocation in the field of public health. Vital Statistics are regularly compiled by health departments and government agencies so that health-related activities can be monitored and evaluated.
h) Disability – ડીસેબીલીટી
Disability is a long-term impairment in a person’s intellectual, physical, mental or sensory abilities that interferes with their ability to effectively carry out their daily routines. According to the World Health Organization, disability is a complex condition that arises from the three-fold combination of impairment, activity limitation, and participation restriction. Disability is understood from medical, social and demographic perspectives and has a direct impact on a person’s quality of life.
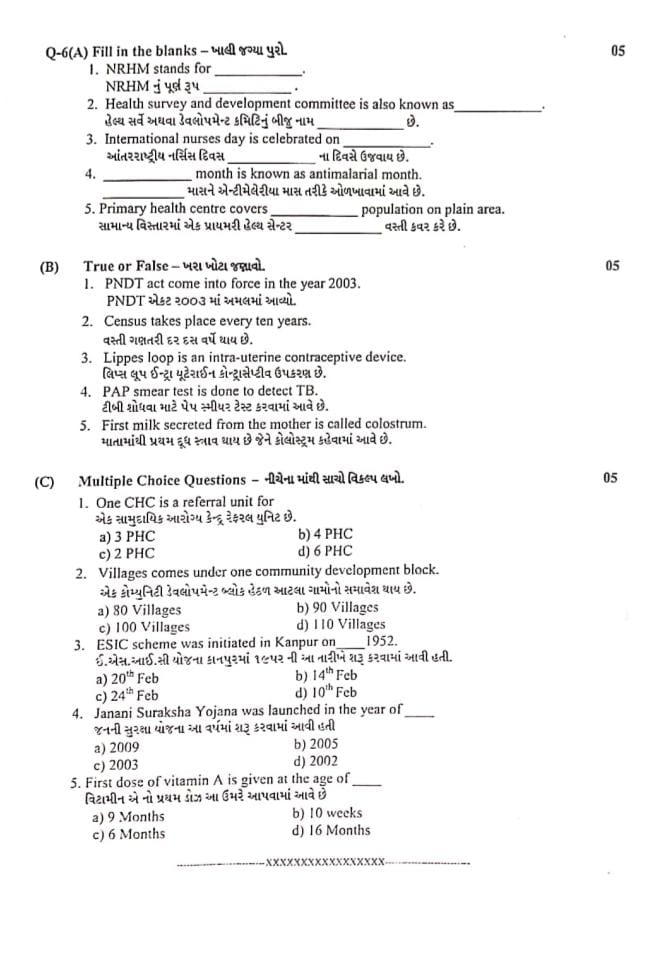
Q-6(A) Fill in the blanks – ખાલી જગ્યા પુરો 05
1.NRHM stands for…… NRHM નું પૂર્ણ રૂપ……Ans: National Rural Health Mission નેશનલ રુરલ હેલ્થ મિશન
2.Health survey and development committee is also known as…… હેલ્થ સર્વે અથવા ડેવલોપમેન્ટ કમિટિનું બીજુ નામ…… છે.Bhore Committee ભોર કમિટી
3.International nurses day is celebrated on…… આંતરરાષ્ટ્રીય નર્સિસ દિવસ…… ના દિવસે ઉજવાય છે. 12th May 12 મેના દિવસે
4……month is known as antimalarial month……માસને એન્ટીમેલેરીયા માસ તરીકે ઓળખાવામાં આવે છે. June જૂન માસ
5.Primary health centre covers……population on plain area.સામાન્ય વિસ્તારમાં એક પ્રાયમરી હેલ્થ સેન્ટર …… વસ્તી કવર કરે છે. 30,000 વસ્તી કવર કરે
B) True or False – ખરા ખોટા જણાવો.
1.PNDT act come into force in the year 2003. PNDT એકટ ૨૦૦૩ માં અમલમાં આવ્યો. Ans: False
Explanation: PNDT Act (Pre-Natal Diagnostic Techniques Act) was enacted in 1994 and amended in 2003.
2.Census takes place every ten years. વસ્તી ગણતરી દર દસ વર્ષે થાય છે . Ans: True
Explanation: In India, census is conducted every 10 years by the Office of the Registrar General and Census Commissioner.
3.Lippes loop is an intra-uterine contraceptive device. લિપ્સ લૂપ ઇન્ટ્રા યુટેરાઈન કોન્ટ્રાસેપ્ટીવ ઉપકરણ છે. Ans: True
Explanation: Lippes Loop is a type of intrauterine device (IUD) used for contraception.
4.PAP smear test is done to detect TB. ટીબી શોધવા માટે પેપ સ્મીયર ટેસ્ટ કરવામાં આવે છે. Ans: False
Explanation: PAP smear is done to detect cervical cancer, not tuberculosis.
5.First milk secreted from the mother is called colostrum. માતામાંથી પ્રથમ દૂધ સ્ત્રાવ થાય છે જેને કોલોસ્ટ્રમ કહેવામાં આવે છે. Ans: True
Explanation: Colostrum is the first thick yellow milk rich in antibodies, secreted immediately after childbirth.
(C) Multiple Choice Questions – નીચેના માંથી સાચો વિકલ્પ લખો.05
1.One CHC is a referral unit for એક સામુદાયિક આરોગ્ય કેન્દ્ર રેફરલ યુનિટ છે.
a) 3 PHC
b) 4 PHC
c) 2 PHC
d) 6 PHC
Correct Answer: b) 4 PHC
Explanation: એક CHC (Community Health Centre) સામાન્ય રીતે 4 Primary Health Centres (PHCs) માટે રેફરલ યુનિટ તરીકે કાર્ય કરે છે.
2.Villages comes under one community development block. એક કોમ્યુનિટી ડેવલોપમેન્ટ બ્લોક હેઠળ આટલા ગામોનો સમાવેશ થાય છે.
a) 80 Villages
b) 90 Villages
c) 100 Villages
d) 110 Villages
Correct Answer: c) 100 Villages
Explanation: એક Community Development Block સામાન્ય રીતે સરેરાશ 100 ગામોને આવરે છે.
3.ESIC scheme was initiated in Kanpur on 1952. ઈ.એસ.આઈ.સી યોજના કાનપુરમાં ૧૯૫ર ની આ નારીખે શરૂ કરવામાં આવી હતી.
a) 20th Feb
b) 14th Feb
c) 24th Feb
d) 10th Feb
Correct Answer: c) 24th Feb
Explanation: Employees’ State Insurance Scheme (ESIC) was inaugurated on 24th February 1952 at Kanpur.
4.Janani Suraksha Yojana was launched in the year of…..જનની સુરક્ષા યોજના આ વર્ષમાં શરૂ કરવામાં આવી હતી.
a) 2009
b) 2005
c) 2003
d) 2002
Correct Answer: b) 2005
Explanation: Janani Suraksha Yojana (JSY) was launched in the year 2005 under National Rural Health Mission.
5.First dose of vitamin A is given at the age of વિટામીન એ નો પ્રથમ ડોઝ આ ઉંમરે આપવામાં આવે છે.
a) 9 Months
b) 10 weeks
c) 6 Months
d) 16 Months
Correct Answer: a) 9 Months
Explanation: Vitamin A નો પ્રથમ ડોઝ બાળકને 9 મહિનાની ઉંમરે MR (Measles-Rubella) રસી સાથે આપવામાં આવે છે.