24/07/2013 (Pharmacology, Pathology and Genetics)-JUHI DONE-UPLOAD NO.3
Pharmacology, Pathology and Genetics – PAPER SOLUTION NO.03
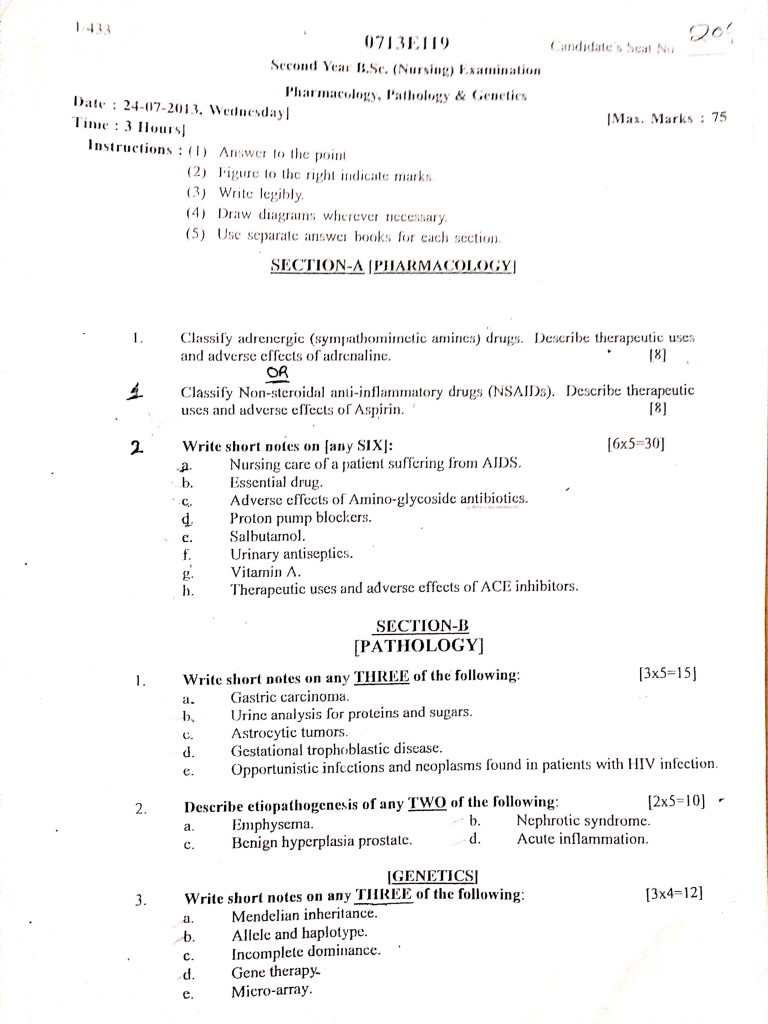
Section – A (Pharmacology)
Q.1 Claasify adrenergic (sympathomimetic amines) drugs. Described therapeutic uses and adverse effects of adrenalin [8 mark]
Classification of Adrenergic (Sympathomimetic) Drugs
Adrenergic drugs are also called sympathomimetics because they mimic the action of sympathetic nervous system neurotransmitters like adrenaline and noradrenaline. These drugs stimulate alpha and/or beta adrenergic receptors.
✅I. Based on Chemical Structure
1️⃣ Catecholamines
- These are naturally occurring or synthetic compounds that contain a catechol nucleus (a benzene ring with two hydroxyl groups) and an amine group.
- Examples: Adrenaline (Epinephrine), Noradrenaline (Norepinephrine), Dopamine, Dobutamine, Isoprenaline.
- These drugs act directly on adrenergic receptors and are rapidly metabolized by MAO and COMT, so they have a short duration of action.
- They are not effective orally because they are degraded in the gastrointestinal tract.
- Catecholamines are typically used in emergency conditions like cardiac arrest, anaphylaxis, and shock.
2️⃣ Non-Catecholamines
- These are synthetic adrenergic agonists that do not contain a catechol group, hence more resistant to degradation.
- Examples: Phenylephrine, Salbutamol, Ephedrine, Amphetamine, Terbutaline.
- These drugs have longer duration of action and can be given orally.
- They can cross the blood-brain barrier and often show CNS effects (e.g., euphoria, alertness).
- These drugs are used in nasal decongestion, asthma, hypotension, and attention-deficit disorders.
✅ II. Based on Mode of Action
1️⃣ Direct-Acting Adrenergic Agonists
- These drugs act directly by binding to alpha or beta adrenergic receptors.
- Examples: Adrenaline, Noradrenaline, Phenylephrine, Isoprenaline, Salbutamol.
- Their effect depends on the receptor subtype they stimulate (e.g., beta-2 agonists cause bronchodilation).
- These are used in clinical settings like bronchial asthma, bradycardia, hypotension, and shock.
- They act rapidly and predictably, with dose-dependent effects.
2️⃣ Indirect-Acting Adrenergic Agonists
- These drugs do not act directly on receptors, but increase the release of endogenous norepinephrine from nerve terminals.
- Examples: Amphetamine, Tyramine.
- These drugs produce CNS stimulation (alertness, decreased fatigue) and peripheral vasoconstriction.
- They are useful in narcolepsy, ADHD, and appetite suppression (limited use due to side effects).
- Tolerance and dependency can develop due to chronic use.
3️⃣ Mixed-Acting Adrenergic Agonists
- These drugs act both directly on receptors and indirectly by releasing norepinephrine.
- Examples: Ephedrine, Pseudoephedrine.
- They have dual action, making them effective in treating nasal congestion, asthma, and hypotension.
- These drugs have a moderate duration of action and can be administered orally.
- Over-the-counter use is regulated because of abuse potential and side effects like hypertension.
✅ III. Based on Receptor Selectivity
1️⃣ Alpha-1 Agonists
- These selectively stimulate alpha-1 receptors located on vascular smooth muscle.
- Examples: Phenylephrine, Midodrine, Methoxamine.
- They cause vasoconstriction, increasing blood pressure and reducing nasal congestion.
- Useful in treating hypotension, nasal congestion, and to prolong local anesthetic action.
- May cause reflex bradycardia and hypertension as side effects.
2️⃣ Alpha-2 Agonists
- These act on presynaptic alpha-2 receptors, leading to inhibition of norepinephrine release.
- Examples: Clonidine, Methyldopa, Brimonidine.
- Used in hypertension, withdrawal symptoms, and glaucoma.
- They cause central inhibition of sympathetic outflow, resulting in decreased blood pressure.
- May cause dry mouth, sedation, and rebound hypertension on sudden withdrawal.
3️⃣ Beta-1 Agonists
- These selectively stimulate beta-1 receptors mainly found in the heart.
- Examples: Dobutamine.
- Used in acute heart failure and cardiogenic shock to increase cardiac output.
- They increase heart rate, myocardial contractility, and cardiac conduction.
- Can lead to tachycardia or arrhythmias at high doses.
4️⃣ Beta-2 Agonists
- These act on beta-2 receptors, causing bronchodilation and vasodilation.
- Examples: Salbutamol, Terbutaline, Salmeterol, Formoterol.
- Widely used in asthma and chronic obstructive pulmonary disease (COPD).
- Also used to delay preterm labor due to uterine relaxation.
- Side effects include tremor, tachycardia, and hypokalemia.
5️⃣ Non-Selective Beta Agonists
- These stimulate both beta-1 and beta-2 receptors.
- Examples: Isoprenaline.
- Used in heart block and bronchospasm, though use is limited due to cardiac side effects.
- Cause increased heart rate and bronchodilation.
- Should be avoided in patients with ischemic heart disease.
Therapeutic Uses of Adrenaline (Epinephrine)
Adrenaline is a potent, non-selective adrenergic agonist that stimulates α1, α2, β1, and β2 receptors. It is used in multiple emergency and routine medical situations due to its wide-ranging physiological effects.
1. Management of Anaphylactic Shock
- It is the drug of choice in the treatment of anaphylaxis, a severe allergic reaction that can cause airway obstruction, hypotension, and circulatory collapse.
- It acts by relaxing bronchial smooth muscles (β2), raising blood pressure (α1), and increasing heart rate (β1).
- It is given intramuscularly for rapid systemic absorption.
2. Use in Advanced Cardiac Life Support (ACLS)
- It is used in Advanced Cardiac Life Support (ACLS) protocols during cardiopulmonary resuscitation (CPR) to restore spontaneous circulation.
- It acts by stimulating β1 receptors in the heart, thereby increasing myocardial contractility and heart rate.
- It is given intravenously or intraosseously in emergency settings.
3. Treatment of Acute Bronchial Asthma
- It is used during acute severe bronchospasm or status asthmaticus when other bronchodilators fail.
- It causes rapid bronchodilation by acting on β2 adrenergic receptors in bronchial smooth muscle.
- It is usually administered subcutaneously in emergency asthma cases.
4. Vasoconstrictor in Local Anesthesia
- It is added to local anesthetic solutions (e.g., lignocaine) to cause local vasoconstriction (α1 receptor-mediated).
- This helps to prolong the duration of anesthesia, reduce systemic absorption, and minimize local bleeding.
5. Control of Superficial Bleeding
- It is applied topically or injected locally to control capillary bleeding during minor surgeries such as nasal, oral, or dental procedures.
- Its vasoconstrictive effect (α1 stimulation) helps reduce blood loss and improve visibility during the procedure.
6. Management of Hypotension During Spinal or Anesthetic Shock
- It is used to restore falling blood pressure due to spinal anesthesia or intraoperative hypotension.
- It increases peripheral vascular resistance (α1 action) and improves cardiac output (β1 action).
7. Emergency Use in Glaucoma (Open-Angle Type)
- Adrenaline helps reduce intraocular pressure by increasing aqueous humor outflow via β2 stimulation.
- Although now replaced by newer agents, it was previously used as topical eye drops for open-angle glaucoma.
8. Prolonging Duration of Spinal or Epidural Anesthesia
- When combined with regional anesthetics, adrenaline causes localized vasoconstriction, reducing drug absorption into the bloodstream.
- This results in prolonged anesthesia and reduced risk of systemic toxicity.
9. Emergency Use in Croup or Upper Airway Obstruction
- Nebulized adrenaline is used in children with croup to reduce laryngeal edema and improve airflow.
- Its α1-mediated vasoconstriction in the airway mucosa helps relieve stridor and respiratory distress.
10. Diagnostic Use in Pupil Dilation (Mydriasis)
- Adrenaline or its analogues may be used topically in the eye to induce pupil dilation, especially in cases requiring fundoscopic examination.
- It causes mydriasis by stimulating α1 receptors in the radial muscle of the iris.
Adverse Effects of Adrenaline (Epinephrine)
Adrenaline is a potent non-selective adrenergic agonist that stimulates α1, α2, β1, and β2 receptors. Though life-saving in many emergencies, it can also cause serious systemic side effects, especially if used in excess or without monitoring.
1. Cardiovascular Adverse Effects
- It may cause tachycardia, which is an abnormally rapid heart rate, due to β1 receptor stimulation on the heart.
- It may result in cardiac arrhythmias, including ventricular fibrillation, especially in patients with pre-existing heart conditions.
- It may cause severe hypertension due to α1-mediated vasoconstriction, which can lead to intracranial hemorrhage or stroke in rare cases.
- It may cause anginal pain or myocardial infarction in patients with coronary artery disease, due to increased myocardial oxygen demand.
2. Central Nervous System (CNS) Effects
- It may produce restlessness and anxiety, due to central stimulation of adrenergic pathways.
- It may lead to tremors, especially in hands, due to β2 receptor stimulation in skeletal muscles.
- It may cause headache and dizziness, likely due to abrupt elevation of blood pressure.
3. Respiratory Effects
- In some sensitive individuals, paradoxically, it may cause pulmonary edema, especially in overdose or during cardiogenic shock, by increasing venous return and capillary pressure.
- It may also cause shortness of breath or chest tightness, especially if used in rapid intravenous injection.
4. Metabolic and Endocrine Effects
- It may lead to hyperglycemia, due to β2 receptor-mediated glycogenolysis and gluconeogenesis in the liver.
- It may result in lactic acidosis, especially in prolonged use, by increasing anaerobic metabolism.
5. Local Adverse Effects (at injection site)
- When injected locally in high concentration, it may cause ischemia and tissue necrosis, due to intense vasoconstriction by α1 receptors.
- Inadvertent intravenous injection of a high dose may lead to instantaneous cardiovascular collapse.
6. Allergic or Hypersensitivity Reactions
- Although rare, hypersensitivity to preservatives (e.g., sodium metabisulfite) used in adrenaline injections may cause allergic symptoms like rash, wheezing, or bronchospasm.
7. Rebound Effects
- Sudden withdrawal or cessation after continuous use may cause rebound hypotension or bronchospasm.
- Tolerance (tachyphylaxis) may develop with repeated use, reducing its effectiveness over time.
Or
Q.1 Classify non steroidal anti inflammatory drugs (NSAID). Described therapeutic uses and adverse effects of aspirin [8 mark]
Classification of NSAIDs (Non-Steroidal Anti-Inflammatory Drugs)
NSAIDs are classified based on chemical structure, COX selectivity, and duration of action. Below are long, point-wise details for each type.
✅ A. Based on Chemical Structure
1️⃣ Salicylates
- It includes drugs that are chemically related to salicylic acid and exhibit anti-inflammatory, analgesic, and antipyretic properties.
- Examples: Aspirin, Sodium salicylate, Diflunisal.
- It is commonly used in cardiovascular prophylaxis due to its irreversible platelet inhibition.
- It can cause Reye’s syndrome in children when used during viral infections.
- Salicylates are also useful in treating mild musculoskeletal pain and fever.
2️⃣ Propionic Acid Derivatives
- These are widely used NSAIDs that provide effective relief from pain and inflammation.
- Examples: Ibuprofen, Naproxen, Ketoprofen, Flurbiprofen.
- These drugs are better tolerated in the gastrointestinal system compared to aspirin.
- Ibuprofen is also available in pediatric formulations and is safe in fever management in children.
- Naproxen has a longer duration of action and is preferred in chronic inflammatory diseases like arthritis.
3️⃣ Acetic Acid Derivatives
- These NSAIDs are structurally derived from acetic acid and have strong anti-inflammatory actions.
- Examples: Diclofenac, Indomethacin, Sulindac, Etodolac.
- Diclofenac is commonly used for postoperative pain, arthritis, and sports injuries.
- Indomethacin is particularly useful in gout and closure of patent ductus arteriosus in neonates.
- These drugs may cause significant GI and CNS side effects, including headache and dizziness.
4️⃣ Enolic Acid Derivatives (Oxicams)
- These NSAIDs belong to the oxicam family and are primarily used for long-term chronic pain management.
- Examples: Piroxicam, Meloxicam, Tenoxicam.
- These drugs have a very long half-life, allowing once-daily dosing for patient convenience.
- They are widely used in osteoarthritis and rheumatoid arthritis.
- These drugs carry a higher risk of gastric ulceration if not used with food or gastric protection.
5️⃣ Fenamates (Anthranilic acid derivatives)
- These drugs are effective for treating menstrual pain, muscle cramps, and mild-to-moderate pain.
- Examples: Mefenamic acid, Meclofenamate.
- Mefenamic acid is commonly prescribed in dysmenorrhea due to its strong analgesic effect on uterine contractions.
- It can cause diarrhea, GI upset, and nephrotoxicity in long-term use.
- This group is rarely used in chronic conditions due to safety concerns.
6️⃣ Pyrazolone Derivatives
- These are older NSAIDs with strong analgesic effects but are less commonly used now.
- Examples: Phenylbutazone, Oxyphenbutazone, Metamizole.
- Phenylbutazone is effective in acute gout but may cause bone marrow suppression.
- These drugs have high toxicity potential, including agranulocytosis and aplastic anemia.
- Due to their adverse effects, they are banned or restricted in many countries.
7️⃣ Selective COX-2 Inhibitors (Coxibs)
- These drugs selectively inhibit COX-2 enzyme and have minimal gastric irritation.
- Examples: Celecoxib, Etoricoxib, Valdecoxib, Parecoxib.
- They are especially useful in rheumatoid arthritis and osteoarthritis without GI bleeding risk.
- These drugs are not antiplatelet, so they do not interfere with bleeding time.
- However, they may increase cardiovascular risks, such as hypertension and thrombosis.
✅B. Based on COX Enzyme Selectivity
1️⃣ Non-Selective COX Inhibitors
- These inhibit both COX-1 and COX-2, leading to pain relief and inflammation control, but with gastric side effects.
- Examples: Aspirin, Ibuprofen, Diclofenac.
- They reduce prostaglandin synthesis in both stomach and inflamed tissues, hence effective but ulcerogenic.
- Long-term use may cause gastritis, peptic ulcer, or GI bleeding.
- They are contraindicated in patients with a history of gastric ulcer or bleeding disorders.
2️⃣ Preferential COX-2 Inhibitors
- These mainly inhibit COX-2, with lesser inhibition of COX-1, offering a balance between efficacy and safety.
- Examples: Nimesulide, Meloxicam, Etodolac.
- These are commonly used for musculoskeletal pain and post-operative pain.
- Nimesulide has hepatotoxic potential and should be avoided in liver disease patients.
- Etodolac offers fewer GI symptoms, especially when given short-term.
3️⃣ Selective COX-2 Inhibitors (Coxibs)
- These target only COX-2, thereby preserving gastric mucosa and platelet function.
- Examples: Celecoxib, Etoricoxib.
- Ideal in patients with GI risk or those requiring long-term NSAID use.
- They are not suitable for cardiac patients due to increased thrombotic events.
- Monitoring of blood pressure and renal function is necessary during long-term therapy.
✅ C. Based on Duration of Action
1️⃣ Short-Acting NSAIDs (Half-life <6 hrs)
- These are rapidly acting drugs with short duration, suitable for acute pain.
- Examples: Ibuprofen, Diclofenac, Indomethacin.
- They provide quick relief but require frequent dosing (2–3 times/day).
- Useful in acute dental pain, injury, or headache.
- Risk of rebound pain is higher if doses are skipped.
2️⃣ Long-Acting NSAIDs (Half-life >10 hrs)
- These are slow-releasing or long-duration NSAIDs ideal for chronic inflammatory conditions.
- Examples: Piroxicam, Meloxicam, Naproxen.
- Allow once or twice daily dosing, improving compliance in elderly or chronic patients.
- Effective in ankylosing spondylitis, osteoarthritis, and chronic back pain.
- Long-acting drugs may accumulate and cause renal toxicity in patients with impaired kidney function.
Therapeutic Uses of Aspirin
Aspirin (acetylsalicylic acid) is a widely used non-steroidal anti-inflammatory drug (NSAID) that possesses analgesic, antipyretic, anti-inflammatory, and antiplatelet properties. Its uses depend on dose and clinical condition.
1. As an Analgesic (Pain Reliever)
- It is used in the treatment of mild to moderate pain, such as headache, dental pain, musculoskeletal pain, and dysmenorrhea (painful menstruation).
- It works by inhibiting cyclooxygenase enzymes (COX-1 and COX-2), thereby reducing prostaglandin synthesis, which is responsible for pain sensation.
2. As an Antipyretic (Fever Reducer)
- Aspirin is used to reduce elevated body temperature in patients suffering from fever due to infections or inflammatory diseases.
- It helps by acting on the hypothalamic heat-regulating center, promoting heat loss through vasodilation and sweating.
3. As an Anti-inflammatory Agent
- It is effective in treating inflammatory conditions, such as rheumatoid arthritis, osteoarthritis, bursitis, and tendonitis.
- It works by blocking prostaglandin-mediated inflammation, thereby reducing swelling, redness, and joint stiffness.
4. As an Antiplatelet Agent (Low Dose Therapy)
- Low-dose aspirin (usually 75–150 mg/day) is commonly prescribed for prevention of heart attack, stroke, and other thrombotic events in patients at risk.
- It works by irreversibly inhibiting COX-1 enzyme in platelets, thus inhibiting thromboxane A2 production, which is responsible for platelet aggregation and vasoconstriction.
5. Used in Acute Myocardial Infarction (Heart Attack)
- In acute heart attack, aspirin is given immediately to prevent further clot formation and reduce mortality.
- It is often used in combination with other drugs like clopidogrel, statins, and beta-blockers.
6. Use in Stroke Prevention
- Aspirin is used in ischemic stroke or transient ischemic attack (TIA) to prevent recurrence by reducing clot formation in cerebral vessels.
7. Used in Kawasaki Disease (in children)
- Aspirin is used as part of the treatment to reduce inflammation in blood vessels, and prevent coronary artery complications.
8. Use in Post-surgical Conditions (Cardiovascular surgeries)
- Aspirin is often continued after stent placement or bypass surgery to prevent thromboembolic complications.
9. Used in Colorectal Cancer Prevention (in high-risk patients)
- Long-term low-dose aspirin may reduce the risk of colorectal carcinoma, especially in patients with familial adenomatous polyposis (FAP), although this is under ongoing clinical evaluation.
Adverse Effects of Aspirin
While aspirin is therapeutically valuable, it can produce significant side effects, especially when used in high doses or over long durations.
1. Gastrointestinal Adverse Effects
- It may cause gastritis, gastric irritation, nausea, vomiting, and epigastric pain.
- It increases the risk of peptic ulcer and gastrointestinal bleeding due to inhibition of protective prostaglandins in the gastric mucosa.
2. Bleeding Tendency
- Aspirin causes prolonged bleeding time by inhibiting platelet aggregation, even at low doses.
- It may lead to internal bleeding, easy bruising, nosebleeds, and post-surgical bleeding.
3. Allergic Reactions
- It may cause skin rash, itching, nasal polyps, bronchospasm, or even anaphylaxis in sensitive individuals.
- This is known as aspirin sensitivity or aspirin-induced asthma, especially in patients with pre-existing asthma.
4. Reye’s Syndrome (in Children)
- Aspirin should not be given to children under 12 years with viral infections (like influenza or chickenpox), as it may cause Reye’s syndrome, a potentially fatal condition involving brain and liver damage.
5. Renal Impairment
- Chronic use may lead to reduced renal perfusion, fluid retention, and in long-term cases, chronic kidney disease.
6. Salicylism (Aspirin Toxicity)
High doses can lead to a toxic syndrome called salicylism, which includes symptoms like :
- Tinnitus (ringing in ears)
- Vertigo
- Nausea and vomiting
- Hyperventilation
- Metabolic acidosis
- Confusion or seizures in severe cases
7. Hepatotoxicity (in rare cases)
- In some cases, elevated liver enzymes or hepatic injury may be observed, especially with prolonged use.
8. Drug Interactions and Contraindications
- Aspirin may interact with warfarin, steroids, NSAIDs, and antihypertensives, leading to increased side effects.
- It is contraindicated in peptic ulcer, bleeding disorders, asthma, and renal failure.
Q.2 Write short notes on (any six) [30 marks]
1. Nursing care of a patient suffering from AIDS
Comprehensive Assessment :
- Perform full physical examination including skin, mucosa, lymph nodes, neurological status.
- Monitor vital signs, body weight, temperature, and fluid input-output.
- Assess for signs of opportunistic infections (fever, cough, diarrhea, oral ulcers, night sweats).
- Monitor mental status (depression, confusion, memory loss).
- Assess socioeconomic background, support system, and level of knowledge about HIV.
Infection Prevention and Control:
- Strict use of standard precautions (hand hygiene, gloves, PPE).
- Educate the patient and family on hygiene, food safety, and wound care.
- Isolate patient (if needed) in case of active tuberculosis or other communicable OIs.
- Ensure proper disposal of bodily fluids, linen, and sharps.
- Encourage respiratory hygiene to prevent airborne transmission.
Nutritional Management:
- Provide high-protein, high-calorie diet rich in micronutrients.
- Manage appetite loss, oral thrush, nausea, or diarrhea with appropriate diet adjustments.
- Encourage hydration and avoid raw or undercooked food.
- Collaborate with a dietician for personalized nutritional planning.
Symptom Management and Medication Adherence:
- Administer ART (antiretroviral therapy) as prescribed and ensure strict adherence.
- Treat opportunistic infections with antimicrobials, antifungals, antivirals.
- Control symptoms like fever, pain, diarrhea, cough, vomiting, fatigue.
- Watch for drug side effects (hepatotoxicity, neuropathy, anemia).
- Encourage the use of pill organizers or reminders for adherence.
Hygiene and Skin Care:
- Perform daily oral care to prevent thrush or mucosal ulcers.
- Provide gentle skin care to prevent infections, pressure ulcers, and Kaposi’s lesions.
- Maintain perineal hygiene in case of diarrhea or incontinence.
- Prevent bedsores through regular repositioning and skin inspection.
Psychological and Emotional Support:
- Create a non-judgmental, empathetic environment.
- Allow expression of feelings, fear, guilt, or denial.
- Provide stress management techniques like relaxation, spiritual support.
- Offer referral to counselors, psychologists, or peer support groups.
- Involve the patient in decision-making to promote autonomy.
Health Education and Lifestyle Modification:
- Teach about the nature of HIV/AIDS, transmission, and prevention.
- Instruct on safe sexual practices (use of condoms).
- Promote smoking cessation, alcohol avoidance, and adequate sleep and exercise.
- Emphasize routine medical follow-up and CD4 count/viral load monitoring.
- Educate about vaccinations (influenza, pneumococcal, HPV, hepatitis B).
Social and Family Support:
- Involve family/caregivers in care and emotional support.
- Address stigma, discrimination, and social isolation.
- Help access government schemes, NGOs, or financial aid.
- Support in maintaining employment, relationships, or education if possible.
Rehabilitation and Vocational Counseling:
- Encourage gradual return to work or suitable activities if condition stabilizes.
- Refer to occupational therapy or vocational training programs.
- Promote independent living skills in stable patients.
Palliative and End-of-Life Care (if terminal):
- Focus on symptom relief, dignity, and comfort in the final stages.
- Provide spiritual care, pain control, and emotional presence.
- Support family during bereavement and help with legal and social issues.
- Respect advance directives or living wills if discussed.
2. Essential drug
Definition
- It is defined as those drugs that satisfy the health care needs of the majority of the population and should therefore be available at all times in adequate amounts, appropriate dosage forms, with assured quality and at an affordable cost.
- The concept of essential drugs was introduced by the World Health Organization (WHO) in 1977 as a core component of health policy to improve access to medicines.
Objectives of Essential Drug Concept
- It is to ensure equitable availability and accessibility of necessary medications for all age groups and all disease conditions.
- It is to promote the rational use of drugs among health care providers and the public.
- It is to optimize health care resources by prioritizing cost-effective and evidence-based medicines.
Criteria for Selection of Essential Drugs
- It should be selected based on prevalence of disease, evidence on efficacy and safety, and comparative cost-effectiveness.
- It should meet the needs of priority health problems of the community.
- It should be suitable for use in different levels of health care, from primary to tertiary levels.
- It should have proven efficacy and safety profile through scientific evidence and clinical trials.
- It should be stable in local storage and climatic conditions.
Examples of Essential Drugs (WHO Model List)
Antibiotics – Amoxicillin, Ciprofloxacin, Metronidazole
Antimalarials – Artemisinin-based combination therapy (ACT), Chloroquine
Analgesics & Antipyretics – Paracetamol, Ibuprofen
Antihypertensives – Amlodipine, Enalapril
Antidiabetics – Metformin, Insulin
Anti-tubercular drugs – Rifampicin, Isoniazid
Vaccines – BCG, DPT, Hepatitis B
Oral Rehydration Salts (ORS) and Zinc for diarrheal disease
Iron and Folic Acid tablets for anemia
Advantages of Essential Drug List (EDL)
- It promotes rational prescription and avoids polypharmacy (unnecessary multiple drugs).
- It helps in cost containment in health care and reduces wastage of medicines.
- It improves quality of patient care through standardized treatment protocols.
- It guides procurement and drug inventory management at all levels of health care.
- It facilitates training and education of health care workers on evidence-based pharmacotherapy.
Essential Drugs in India
- India follows the National List of Essential Medicines (NLEM) which is periodically updated (latest update: 2022).
- The NLEM includes 384 drugs across various therapeutic categories essential for public health.
- It is managed by the Ministry of Health and Family Welfare and plays a key role in drug price control under the Drug Price Control Order (DPCO).
Nursing Responsibilities Regarding Essential Drugs
- It is the nurse’s responsibility to ensure the correct administration of essential drugs as per physician’s orders.
- It is essential for the nurse to check drug expiry dates, correct dosages, and proper storage conditions to maintain drug efficacy.
- The nurse should provide proper health education to patients regarding the importance, dose, and duration of essential drugs.
- The nurse should participate in monitoring of side effects and adverse drug reactions and report them to the medical officer.
- The nurse must follow infection control measures while handling injectable essential drugs and dispose of medical waste properly.
3. Adverse effect of amino glycoside antibodies
❗ 1. Nephrotoxicity (Toxic Effect on Kidneys)
- It is the most important adverse effect in which the aminoglycoside drug gets accumulated in the proximal convoluted tubules, causing acute tubular necrosis and leading to elevated serum creatinine and urea levels.
- It is more commonly seen in elderly patients, neonates, and patients with existing renal impairment, as they have reduced drug clearance.
- It is also enhanced by dehydration, high doses, or prolonged therapy beyond 7 days, especially when used with other nephrotoxic agents like vancomycin or NSAIDs.
- It can lead to oliguria (low urine output) or even acute kidney injury (AKI) if not monitored and dose-adjusted properly.
❗ 2. Ototoxicity (Damage to Ear – Hearing and Balance)
- It is a serious adverse effect in which aminoglycosides accumulate in the endolymph and perilymph of the inner ear, damaging the hair cells of cochlea and vestibular system, resulting in tinnitus, vertigo, and irreversible sensorineural hearing loss.
- It is usually bilateral and permanent, and patients may not show symptoms until significant damage has occurred.
- Ototoxicity is more common with genetic susceptibility, especially those with mitochondrial mutations (e.g., A1555G mutation).
- Hearing tests such as audiometry and vestibular assessments should be regularly done in high-risk patients.
❗ 3. Neuromuscular Blockade
- Aminoglycosides can interfere with acetylcholine release at neuromuscular junction, resulting in progressive muscle weakness and respiratory muscle paralysis, which may require ventilatory support.
- It is especially dangerous in patients with Myasthenia Gravis, or when used with other neuromuscular blockers during surgery or ICU care.
- This effect may be reversed by IV calcium gluconate or neostigmine in emergency settings.
- Early signs include difficulty in breathing, swallowing, and limb weakness, which should be reported immediately.
❗ 4. Hypersensitivity and Allergic Reactions
- Some patients may develop rash, itching (pruritus), fever, or urticaria after receiving aminoglycosides, particularly topical forms like neomycin.
- Anaphylaxis, though rare, may occur especially with repeated parenteral doses or previous sensitization.
- Skin testing is not usually predictive, so caution is advised, particularly in patients with known drug allergies.
- Reactions may also include serum sickness–like syndrome characterized by fever, rash, and joint pain.
❗ 5. Teratogenicity (Harm to Developing Fetus)
- Aminoglycosides can cross the placenta and may accumulate in fetal tissues, especially in the inner ear, leading to congenital hearing loss or vestibular dysfunction.
- Streptomycin is most commonly associated with fetal ototoxicity among all aminoglycosides.
- They are classified as Pregnancy Category D, meaning risk exists, but benefit may outweigh risk in life-threatening infections.
- Use during first trimester is especially risky, so aminoglycosides should only be given under strict medical supervision if alternatives are not available.
❗ 6. Superinfections
- Prolonged use of aminoglycosides may kill normal flora, allowing overgrowth of resistant organisms such as Clostridium difficile, Candida albicans, etc.
- It may result in oral thrush, vaginal candidiasis, or pseudomembranous colitis (watery diarrhea with abdominal cramps).
- Patients on broad-spectrum antibiotics must be monitored for signs of new infections, which could indicate superinfection.
- Probiotics and antifungal cover may be considered in patients on long-term therapy.
❗ 7. Local Reactions (Injection Site or Administration-Related)
- Intramuscular injections can cause pain, induration, or muscle fibrosis at the site of administration, especially with repeated injections.
- Intravenous infusions may lead to phlebitis, redness, and thrombosis of vein if given too rapidly or in high concentration.
- Topical use (especially in ear or skin creams) may cause contact dermatitis or allergic rash, particularly with neomycin.
- Proper dilution, rotation of injection sites, and use of central lines for long-term therapy help prevent such complications.
4. Proton pump inhibitors
Definition
- Proton pump inhibitors (PPIs) are a class of drugs that irreversibly inhibit the H⁺/K⁺ ATPase enzyme system (proton pump) in the gastric parietal cells of the stomach.
- It is responsible for suppressing the final step of acid production, thus reducing gastric acid secretion effectively and for a prolonged period.
Examples of PPIs (Generic names)
- Omeprazole
- Pantoprazole
- Esomeprazole
- Lansoprazole
- Rabeprazole
- Dexlansoprazole
3. Mechanism of Action
- It acts by irreversibly binding to and inactivating the H⁺/K⁺ ATPase enzyme system (also called the gastric proton pump) located on the parietal cells of the stomach.
- This enzyme is responsible for the final stage of gastric acid secretion into the stomach lumen.
- Once the enzyme is blocked, acid secretion is reduced, even if stimulation continues from histamine, gastrin, or acetylcholine
- PPIs are prodrugs that are activated in the acidic environment of the parietal cell canaliculi.
- It leads to a long duration of action (up to 24 hours), making once-daily dosing effective in most cases.
Indication
- It is used in the treatment of Gastroesophageal Reflux Disease (GERD).
- It is indicated for Peptic Ulcer Disease (gastric and duodenal ulcers).
- It is used for Helicobacter pylori eradication therapy (with antibiotics).
- It is given for Zollinger-Ellison Syndrome (gastrinoma with excessive acid).
- It is used in NSAID-induced gastritis and ulcers.
- It is also prescribed for stress ulcer prophylaxis in ICU patients.
Adverse Effects
- It may cause headache, dizziness, nausea, and abdominal discomfort.
- It may lead to diarrhea or constipation.
- Long-term use may result in vitamin B12 deficiency due to malabsorption.
- It may lead to hypomagnesemia (low magnesium levels).
- Chronic use is associated with increased risk of bone fractures.
- It may increase risk of Clostridium difficile infections in the intestine.
- Rarely, it can cause acute interstitial nephritis or skin rashes.
Contraindications
- It is contraindicated in patients with known hypersensitivity or allergy to PPIs.
- It should be avoided in patients with severe hepatic impairment without dose adjustment.
- Caution should be taken in patients with osteoporosis or electrolyte imbalances.
- It is not recommended for long-term unsupervised use.
Nursing Responsibilities
- The nurse must administer the PPI drug before meals, preferably in the morning, to enhance absorption and effectiveness.
- The nurse should educate the patient that PPIs are not for immediate relief of heartburn, and effects may take 1–4 days to be fully felt.
- The nurse should monitor the patient for gastrointestinal side effects such as diarrhea or constipation and report if they persist.
- The nurse must assess for signs of vitamin B12 or magnesium deficiency, especially in long-term users, such as fatigue, numbness, or cramps.
- The nurse should instruct the patient to avoid alcohol, smoking, and spicy foods which may worsen gastritis or acid reflux symptoms.
- The nurse must be vigilant in long-term users and alert for signs of osteoporosis or bone pain, recommending calcium/vitamin D if necessary.
- The nurse must review the patient’s medication chart to prevent drug interactions, especially with antiretrovirals, antifungals, and warfarin.
- The nurse should educate the patient to swallow the tablet whole and not to crush or chew enteric-coated capsules or tablets.
5. Salbutamol
Introduction
- Salbutamol is a short-acting β2-adrenergic receptor agonist (SABA) that is commonly used to provide quick relief from bronchospasm in diseases like asthma and COPD (Chronic Obstructive Pulmonary Disease).
- It is also called Albuterol. It is a works as bronchodilator.
- It is available in various forms such as inhalers, tablets, syrups, and nebulizer solutions.
Mechanism of Action (MOA)
- It is a selective β2-adrenergic receptor agonist, meaning it specifically binds to β2 receptors present in bronchial smooth muscles.
- It activates adenyl cyclase, an enzyme that increases the levels of cyclic AMP (cAMP) inside the cell.
- This elevated cAMP relaxes bronchial smooth muscles, resulting in bronchodilation and relief from bronchospasm.
- It also reduces airway resistance and facilitates airflow, making breathing easier during an acute asthma attack.
- At higher doses or in sensitive individuals, it may also stimulate β1 receptors, leading to mild cardiac effects such as increased heart rate.
Indications (Therapeutic Uses)
- It is primarily indicated for the treatment of acute bronchospasm in patients with bronchial asthma.
- It is used for the prevention of exercise-induced asthma when administered prior to physical exertion.
- It is useful in patients with COPD, especially during acute exacerbations.
- It is given via nebulizer or inhaler during emergency situations, such as status asthmaticus (severe asthma attack).
- Oral forms of Salbutamol may be used in pediatric patients who cannot use inhalers effectively.
Adverse Effects (Side Effects)
- It often causes tremors of hands, which is dose-dependent and more common in systemic (oral) use.
- It may cause palpitations and tachycardia, especially at higher doses or when β1 receptors are stimulated.
- It is known to cause nervousness, restlessness, and headache, particularly in children and elderly.
- Hypokalemia (low potassium levels) can occur with frequent or high-dose usage.
- It may cause throat irritation or dry mouth when used as an inhaler.
- Rarely, it can cause paradoxical bronchospasm, which worsens breathing instead of relieving it.
Contraindications
- It is contraindicated in patients with known hypersensitivity to Salbutamol or similar adrenergic agents.
- It should be used cautiously in patients with cardiovascular diseases, such as ischemic heart disease, arrhythmias, and hypertension.
- It is avoided in patients with hyperthyroidism, as it may increase sympathetic activity.
- It is used with caution in diabetic patients, as it may cause hyperglycemia.
- High doses should be avoided during pregnancy unless clearly needed, especially in the first trimester.
Nursing Responsibilities
1. Drug Administration
- It is the nurse’s responsibility to check the correct dose, route (inhaler, nebulizer, oral), and frequency of administration.
- It is important to shake the inhaler well and instruct the patient on correct inhalation technique, including breath-holding after inhalation.
- In nebulizer use, the nurse must ensure that the patient is seated upright and breathes slowly and deeply.
2. Monitoring and Assessment
- It is necessary to monitor the patient’s respiratory rate, oxygen saturation, and lung sounds before and after administration.
- The nurse should observe for any improvement in wheezing, dyspnea, or chest tightness after drug use.
- It is also important to monitor for side effects like tremors, palpitations, or nervousness.
3. Patient Education
- The nurse must instruct the patient not to overuse the inhaler and to use it only as prescribed.
- The patient should be advised to rinse the mouth after each inhalation to prevent throat irritation or infection.
- Patients must be taught to carry their rescue inhaler (Salbutamol) at all times, especially during exercise or travel.
4. Prevention of Complications
- The nurse must ensure that the patient is aware of the signs of drug overdose, such as chest pain, fast heartbeat, and severe tremors.
- It is the nurse’s duty to educate the patient about proper storage of the inhaler away from heat and moisture.
5. Coordination with Healthcare Team
- It is important to report inadequate response to the physician, especially in cases of frequent attacks or need for repeated doses.
- The nurse should coordinate with the doctor for adjusting maintenance medications like corticosteroids or leukotriene inhibitors if Salbutamol is overused.
6. Urinary antiseptics
Definition
- It is defined as a group of antimicrobial agents that exert their effect specifically within the urinary tract, without achieving significant systemic antibacterial levels.
- It is important to understand that these agents concentrate in urine and act locally to suppress or eliminate urinary tract pathogens.
- Unlike systemic antibiotics, urinary antiseptics are not meant to treat infections outside the urinary tract.
Common Urinary Antiseptics Include
- Nitrofurantoin
- Methenamine
- Nalidixic acid
- Ciprofloxacin (in low dose for prophylaxis)
- Norfloxacin
- Trimethoprim
- Fosfomycin trometamol
- Phenazopyridine (symptomatic urinary analgesic, not an antimicrobial)
Mechanism of Action
1. Nitrofurantoin
- It is known that Nitrofurantoin gets reduced by bacterial flavoproteins to reactive intermediates, which then attack bacterial ribosomal proteins and DNA, disrupting protein synthesis and DNA replication.
- Its action is bactericidal at high concentrations, and it primarily affects Gram-negative bacilli like E. coli and some Gram-positive cocci.
2. Methenamine
- It is a prodrug that requires acidic urine (pH <5.5) to decompose into formaldehyde, which is a potent bactericidal agent.
- It is important to remember that formaldehyde acts non-specifically, damaging microbial proteins and DNA.
3. Fosfomycin Trometamol
- It works by irreversibly inhibiting the enzyme MurA, which is essential in the first step of bacterial cell wall synthesis, particularly peptidoglycan formation.
- It is effective against multi-drug resistant strains, including ESBL-producing E. coli.
4. Nalidixic Acid
- It is the first quinolone and works by inhibiting DNA gyrase and topoisomerase II, thereby preventing bacterial DNA supercoiling and replication.
- It is more effective against Gram-negative organisms in the urinary tract.
Spectrum of Activity
Nitrofurantoin: Effective against E. coli, Enterococcus, Staphylococcus saprophyticus, but not effective against Proteus or Pseudomonas.
Methenamine: Broad-spectrum due to formaldehyde release, but effectiveness depends on urine acidity.
Fosfomycin: Active against E. coli, Klebsiella, Enterococcus, including many drug-resistant strains.
Nalidixic Acid: Active mostly against E. coli and Proteus, with limited Gram-positive activity.
Indications (Therapeutic Uses)
- It is used for the treatment of uncomplicated lower urinary tract infections, such as acute cystitis, urethritis, and asymptomatic bacteriuria in women.
- It is indicated as a prophylactic agent in patients with recurrent UTIs, especially Nitrofurantoin in low doses at night.
- Methenamine is used as a long-term suppressive agent in chronic urinary infections, especially when anatomical or neurological abnormalities predispose to infection.
- Fosfomycin is used as a single-dose therapy for uncomplicated cystitis in women.
- These drugs are also recommended for urinary infection prevention during or after urological procedures, such as catheterization or cystoscopy.
Adverse Effects
1. Nitrofurantoin
- It commonly causes nausea, vomiting, and anorexia, especially on an empty stomach.
- Long-term use may lead to chronic pulmonary reactions, including interstitial lung disease or fibrosis.
- Peripheral neuropathy and hepatic injury may also occur in elderly or renal-impaired patients.
- It can cause urine discoloration (brownish), which is harmless but may alarm patients.
2. Methenamine
- It may cause bladder irritation, manifested by dysuria and frequency.
- Crystalluria and hematuria can occur if urine is not adequately acidic.
- It may cause gastrointestinal disturbances like nausea and vomiting.
3. Fosfomycin
- It is generally well tolerated but may cause diarrhea, headache, or vaginitis.
- Rarely, allergic reactions such as rash or angioedema can occur.
4. Nalidixic Acid
- It may cause CNS disturbances, especially in children or the elderly—such as headache, dizziness, and seizures.
- Gastrointestinal symptoms like nausea, vomiting, and photosensitivity reactions may occur.
Contraindications
- Nitrofurantoin is contraindicated in renal failure patients, as ineffective urine levels and systemic toxicity may occur.
- It is avoided in the last trimester of pregnancy, due to the risk of hemolytic anemia in the newborn (G6PD deficiency).
- Methenamine should not be used in hepatic insufficiency, due to risk of ammonia retention.
- Nalidixic acid is contraindicated in infants under 3 months, due to risk of intracranial hypertension.
- It is contraindicated in patients with known hypersensitivity to any of these agents.
Nursing Management / Responsibilities
1. Assessment and Monitoring
- It is the nurse’s responsibility to monitor renal function before and during therapy (especially with Nitrofurantoin and Methenamine).
- It is necessary to monitor for therapeutic response, such as relief from dysuria, fever, and urinary frequency.
- It is essential to check urine pH if the patient is on Methenamine, and ensure it remains acidic for optimal drug effect.
2. Patient Education
- The nurse should instruct the patient to take Nitrofurantoin with food or milk to minimize gastric upset.
- It is important to inform the patient that urine may turn brownish, which is harmless.
- The patient should be advised to complete the full course of therapy even if symptoms improve early.
- The nurse must educate the patient to increase fluid intake, unless contraindicated, to aid urinary flushing.
3. Drug Interaction and Compliance
- The nurse should avoid co-administration of antacids containing magnesium or aluminum with Nitrofurantoin, as they reduce absorption.
- It is essential to review patient’s medication history to avoid drug interactions.
- The nurse should reinforce the importance of adherence to dose timing to maintain consistent urinary concentration of the drug.
4. Observation of Side Effects
- The nurse should observe for signs of pulmonary toxicity, such as dry cough or dyspnea, especially in patients on long-term Nitrofurantoin.
- The patient should be assessed for peripheral neuropathy symptoms like numbness or tingling.
- In elderly patients, watch for CNS effects if using Nalidixic acid.
5. Urinary Hygiene Counseling
- The nurse should advise the patient on proper perineal hygiene, especially in females to prevent reinfection.
- It is important to suggest voiding after sexual intercourse, particularly in recurrent UTIs.
7. Vitamin A
Vitamin A is a fat-soluble vitamin that plays a crucial role in maintaining normal vision, immune function, growth and development, and the health of epithelial tissues.
Forms of Vitamin A
- It is found in two major forms: Preformed Vitamin A (Retinol) from animal sources and Provitamin A (Beta-Carotene) from plant sources.
- Retinol is the active form that is stored in the liver, whereas beta-carotene is a precursor that the body converts into retinol.
Sources of Vitamin A
Animal Sources (Retinol)
- It is richly found in liver, fish liver oils (like cod liver oil), egg yolk, butter, ghee, and fortified milk.
- These are highly bioavailable sources and directly provide ready-to-use vitamin A in the form of retinol.
Plant Sources (Beta-Carotene)
- Green leafy vegetables such as spinach, amaranth, fenugreek leaves are rich in beta-carotene.
- Orange and yellow fruits and vegetables like carrots, mangoes, papaya, pumpkin, and sweet potatoes are excellent sources of provitamin A.
Functions of Vitamin A
- It is essential for the synthesis of rhodopsin in retina which is required for normal vision, especially night vision.
- It maintains the integrity and function of epithelial tissues in the skin, respiratory tract, gastrointestinal tract, and genitourinary tract.
- It plays an important role in boosting immunity by supporting white blood cell function.
- It promotes normal growth and development, especially in children, by helping in cell differentiation.
- It contributes to healthy hair, nails, and skin through its epithelial maintenance role.
- It has antioxidant properties (especially beta-carotene), which protect cells from oxidative damage.
Deficiency of Vitamin A
- It causes night blindness (nyctalopia), which is an early symptom of deficiency.
- Severe deficiency may lead to xerophthalmia, characterized by dryness of the conjunctiva and cornea.
- If untreated, it can cause Bitot’s spots, corneal ulcers, and eventually keratomalacia and blindness.
- It reduces immune response, making the body more susceptible to infections like measles, pneumonia, and diarrhea, especially in children.
- In children, deficiency may lead to growth retardation and delayed development.
Toxicity of Vitamin A (Hypervitaminosis A)
- Excess intake, especially of preformed vitamin A, can lead to toxicity symptoms such as nausea, vomiting, headache, dizziness, blurred vision.
- Chronic toxicity may cause liver damage, bone pain, and intracranial hypertension.
- In pregnancy, excess vitamin A intake may cause teratogenic effects leading to birth defects.
Recommended Dietary Allowance (RDA)
- Adult women : 600 mcg/day Retinol Equivalent (RE)
- Adult men : 700 mcg/day Retinol Equivalent (RE)
- Children : 300–400 mcg/day RE, depending on age.
- Pregnant and lactating women: 800–950 mcg/day RE, due to increased needs.
Nursing Responsibilities Related to Vitamin A
- Nurse must assess for clinical signs of deficiency such as night blindness, dry eyes, Bitot’s spots in at-risk populations like children and pregnant women.
- Nurse plays a key role in educating patients and caregivers about dietary sources of vitamin A and the importance of consuming a balanced diet.
- Nurse must ensure timely administration of prophylactic Vitamin A supplements, especially during national programs for child health (like at 9, 18, 24 months etc.).
- Nurse should observe for signs of toxicity if high-dose supplements are given, especially in pediatric and antenatal care.
- Nurse may be involved in nutrition surveillance programs, school health checkups, and growth monitoring where vitamin A deficiency is screened.
8. Therapeutic uses and adverse effect of ACE inhibitors
Therapeutic Uses of ACE Inhibitors
(Angiotensin-Converting Enzyme Inhibitors like Enalapril, Ramipril, Lisinopril, Captopril)
1️⃣ Treatment of Hypertension (High Blood Pressure)
It is widely used in the management of mild to moderate hypertension because it blocks the formation of angiotensin II, resulting in vasodilation and decreased systemic vascular resistance, thereby lowering blood pressure effectively.
2️⃣ Management of Congestive Heart Failure (CHF)
It is commonly indicated in patients with heart failure, as it reduces both preload and afterload on the heart, thereby improving cardiac output, reducing symptoms like dyspnea and fatigue, and enhancing exercise tolerance.
3️⃣ Post-Myocardial Infarction Care
It is used in patients after myocardial infarction (heart attack) to reduce ventricular remodeling, prevent progression to heart failure, and improve survival rate by reducing mortality risk.
4️⃣ Treatment of Diabetic Nephropathy
It is beneficial in preventing and slowing progression of diabetic kidney disease by reducing glomerular filtration pressure and lowering proteinuria (protein in urine), especially in patients with type 1 or type 2 diabetes.
5️⃣ Chronic Kidney Disease (CKD)
It is used to preserve renal function in non-diabetic CKD patients, especially those with proteinuria, because of its ability to decrease intraglomerular pressure and slow down kidney damage.
6️⃣ Left Ventricular Dysfunction (Symptomatic or Asymptomatic)
It is effective in patients with asymptomatic left ventricular systolic dysfunction, because it delays the development of overt heart failure and improves long-term cardiac function and prognosis.
7️⃣ Prevention of Cardiovascular Events in High-Risk Patients
It is used in patients with multiple cardiovascular risk factors such as diabetes, stroke history, or coronary artery disease to prevent future events like heart attacks and strokes by reducing overall cardiovascular load.
8️⃣ Treatment of Scleroderma Renal Crisis
It is considered the drug of choice for scleroderma renal crisis, a rare and serious complication of systemic sclerosis, due to its strong renal protective and blood pressure lowering effects.
9️⃣ Treatment of Proteinuric Glomerulonephritis
It is used in patients with glomerular diseases associated with proteinuria, such as IgA nephropathy or focal segmental glomerulosclerosis, to reduce protein loss and preserve kidney function.
Adverse Effects of ACE Inhibitors
(Angiotensin-Converting Enzyme Inhibitors such as Enalapril, Ramipril, Captopril)
1️⃣ Dry and Persistent Cough
It is one of the most common adverse effects of ACE inhibitors and it occurs due to the accumulation of bradykinin in the lungs, which leads to a non-productive, irritating cough that may require discontinuation of therapy.
2️⃣ First-Dose Hypotension
It may cause a sudden and significant drop in blood pressure after the first dose, especially in patients who are salt-depleted or on diuretics, leading to symptoms like dizziness, fainting, and weakness.
3️⃣ Hyperkalemia (High Potassium Levels)
It can lead to increased potassium levels in the blood, because ACE inhibitors reduce aldosterone secretion, thereby decreasing renal excretion of potassium, which may cause cardiac arrhythmias if severe.
4️⃣ Angioedema (Severe Swelling)
It may cause angioedema, a rare but serious allergic reaction characterized by swelling of the face, lips, tongue, and throat, which can lead to airway obstruction and may be life-threatening.
5️⃣ Elevated Serum Creatinine and Renal Impairment
It may lead to reduced kidney function and increased serum creatinine, especially in patients with bilateral renal artery stenosis, due to decreased glomerular filtration pressure.
6️⃣ Contraindicated in Pregnancy
It is strictly contraindicated during pregnancy (especially 2nd and 3rd trimesters) because it can cause fetal renal dysfunction, growth retardation, and congenital malformations, making it unsafe for pregnant women.
7️⃣ Dizziness, Fatigue, and Headache
It may cause dizziness, general tiredness, and headaches, particularly during the early phase of treatment, due to sudden reduction in blood pressure and cerebral perfusion.
8️⃣ Hematological Reactions
It may rarely cause neutropenia or agranulocytosis, which are serious blood disorders marked by decrease in white blood cells, especially in patients with renal dysfunction or autoimmune diseases.
9️⃣ Skin Rash and Metallic Taste
It may cause minor allergic reactions such as skin rashes, pruritus (itching), and a metallic or altered taste sensation in the mouth, particularly with older ACE inhibitors like captopril.
🔟 Gastrointestinal Symptoms
It may lead to mild gastrointestinal disturbances such as nausea, vomiting, abdominal pain, and diarrhea, which usually resolve on their own or with supportive care.
Section B (Pathology)
Q.1 Write short notes on (any three) [15 marks]
1. Gastric carcinoma
Definition
- Gastric carcinoma is a malignant tumor originating from the epithelial lining of the stomach, most commonly arising from the glandular epithelium.
- It is a slow-growing adenocarcinoma and often diagnosed at an advanced stage due to nonspecific early symptoms.
Etiology
- Helicobacter pylori infection
- Diet rich in smoked/salted/nitrosamine foods
- Chronic atrophic gastritis
- Genetic factors and family history
- Smoking and alcohol consumption
- Previous gastric surgery
- Pernicious anemia
Pathophysiology
- Chronic irritation of gastric mucosa (by H. pylori or chemical agents) causes metaplasia and dysplasia of epithelial cells.
- These dysplastic changes may progress to carcinoma in situ and then to invasive cancer.
- The tumor may involve any part of the stomach, commonly the antrum and lesser curvature.
- It may grow infiltratively (linitis plastica) or form ulcerative masses.
- It can spread by direct invasion, lymphatic spread, or hematogenous metastasis to liver, lungs, peritoneum, and ovaries (Krukenberg tumor).
Clinical Manifestations
- Loss of appetite
- Weight loss
- Abdominal pain/discomfort
- Early satiety (feeling full quickly)
- Fatigue and weakness
- Black stool (melena)
- Anemia symptoms
Diagnostic Evaluation
- Upper GI endoscopy with biopsy
- Barium meal X-ray
- CT scan/MRI for staging
- Complete blood count (CBC)
- Tumor marker (CEA)
- PET scan or laparoscopy (in advanced cases)
Medical and Surgical Management
- Surgical resection (subtotal or total gastrectomy) is the primary treatment for localized tumors.
- Lymph node dissection is done during surgery to reduce spread.
- Chemotherapy (e.g., 5-FU, cisplatin) may be used before (neoadjuvant) or after (adjuvant) surgery.
- Radiation therapy may be combined with chemotherapy in advanced cases.
- Palliative care is provided in unresectable tumors to manage symptoms and improve quality of life.
Nursing Management
1. Nutritional Support
- The nurse should assess the patient’s nutritional status and appetite and plan for small, frequent, high-protein, high-calorie meals.
- If oral intake is poor, enteral or parenteral nutrition may be required.
- Monitor for dumping syndrome post-gastrectomy and educate on dietary modifications.
2. Preoperative and Postoperative Care
- Preoperatively, the nurse should explain the procedure, obtain consent, and prepare the patient physically and emotionally.
- Postoperatively, monitor vital signs, drain output, and signs of infection.
- Provide pain management, assist in early ambulation, and monitor for complications like anastomotic leak or peritonitis.
3. Education and Psychosocial Support
- The nurse must explain the importance of early symptom reporting, diet adherence, and follow-up care.
- Provide emotional support and counseling, as cancer diagnosis may lead to anxiety, fear, or depression.
- Refer to support groups or cancer counseling services as needed.
4. Chemotherapy/Radiotherapy Care
- Monitor for side effects of chemotherapy, such as nausea, vomiting, mucositis, and bone marrow suppression.
- Educate about infection prevention measures and ensure hydration and oral care.
2. Urine analysis for protein and sugar
Purpose of Urine Analysis
1️⃣ It is done to detect the presence of abnormal substances such as protein (albumin) and sugar (glucose) in the urine, which can indicate underlying kidney or metabolic disorders.
2️⃣ It is used as a screening tool in routine health check-ups, and also during the monitoring of known conditions like diabetes mellitus and renal disease.
3️⃣ It helps in early detection of nephropathy in hypertensive or diabetic patients, even before clinical symptoms appear.
Urine Test for Protein (Albuminuria)
Principle
1️⃣ It is based on the precipitation of proteins in acidic conditions or chemical reactions with specific reagents like sulfosalicylic acid or heat.
2️⃣ When heat or chemical reagent is added to urine containing protein, it forms a visible white turbidity or precipitate, indicating a positive result.
Procedure (Common Methods)
1. Heat and Acetic Acid Test
- A clean test tube is filled two-thirds with urine.
- The upper part is gently heated over a flame.
- A few drops of 3% acetic acid are added to rule out phosphate precipitation.
- If turbidity remains after acid, it indicates the presence of protein.
2. Sulfosalicylic Acid Test
- To 5 mL of clear urine, 3 drops of sulfosalicylic acid (3%) are added.
- Formation of turbidity or precipitate indicates presence of protein.
- Degree of turbidity may be graded from trace to ++++.
Clinical Significance of Protein in Urine
1️⃣ It indicates kidney damage or increased glomerular permeability, commonly seen in conditions like nephrotic syndrome, glomerulonephritis, or diabetic nephropathy.
2️⃣ It may be present in infections of urinary tract, where inflammation damages the renal tubules or glomeruli.
3️⃣ Temporary proteinuria may occur due to fever, strenuous exercise, stress, or dehydration, which usually resolves spontaneously.
Urine Test for Sugar (Glycosuria)
Principle
1️⃣ It is based on the reduction of copper ions in Benedict’s reagent by reducing sugars like glucose, which leads to a color change depending on sugar concentration.
2️⃣ The test detects glucose levels above the renal threshold (usually >180 mg/dL), which are excreted in urine when blood glucose is very high.
Procedure (Benedict’s Test)
- 5 mL of Benedict’s reagent is taken in a test tube.
- 8 drops of urine are added to the reagent.
- The mixture is boiled gently for 2–3 minutes.
- After cooling, the color is observed.
Color Interpretation
- Blue = No sugar
- Green = Trace
- Yellow = + (low sugar)
- Orange = ++ (moderate sugar)
- Brick Red = +++ (high sugar)
Clinical Significance of Sugar in Urine
1️⃣ It is commonly found in uncontrolled diabetes mellitus, where blood glucose exceeds the renal threshold and spills into the urine.
2️⃣ It may also occur in pregnancy (gestational glycosuria) or in renal glycosuria, a condition where glucose is excreted despite normal blood glucose.
3️⃣ Persistent glycosuria can lead to increased risk of urinary tract infections (UTIs) and should be monitored regularly in diabetic patients.
Nursing Responsibilities in Urine Testing
1️⃣ It is the nurse’s responsibility to collect a clean-catch midstream urine sample in a sterile container to avoid contamination.
2️⃣ It is important to label the sample with the patient’s name, date, and time of collection before sending it to the laboratory or performing bedside testing.
3️⃣ The nurse must observe color changes carefully and interpret results accurately based on standardized color scales or reagent strips.
4️⃣ The nurse should report any abnormal findings to the physician promptly and record them in the patient’s chart for diagnosis and further management.
5️⃣ The nurse must educate patients with proteinuria or glycosuria about the importance of follow-up, diet control, and adherence to medication.
3. Astrocytic tumors
Definition
- It is defined as a type of brain tumor that arises from astrocytes, which are star-shaped glial cells responsible for supporting neurons and maintaining the blood-brain barrier.
- These tumors are classified under gliomas, and they can range from slow-growing benign forms to aggressive and highly malignant types.
Etiology (Causes)
- Unknown in most cases
- Genetic mutations (e.g., p53, IDH1)
- Ionizing radiation exposure
- Neurofibromatosis type 1 (NF1)
- Family history of gliomas
Types of Astrocytic Tumors
1️⃣ Pilocytic Astrocytoma (Grade I)
- It is a slow-growing benign tumor, commonly seen in children and young adults, usually located in the cerebellum or optic pathway.
2️⃣ Diffuse Astrocytoma (Grade II)
- It is an infiltrative, slow-growing tumor with potential to transform into higher grades over time.
3️⃣ Anaplastic Astrocytoma (Grade III)
- It is a malignant tumor with increased cellularity and mitotic activity, typically found in adults.
4️⃣ Glioblastoma Multiforme (Grade IV)
- It is the most aggressive and malignant form, characterized by rapid growth, necrosis, and poor prognosis.
Pathophysiology
- It begins when astrocytes undergo genetic mutations, leading to abnormal proliferation and loss of cell cycle control.
- The tumor mass invades surrounding brain tissue, disrupting normal neural function and increasing intracranial pressure.
- As the tumor grows, it can cause edema, necrosis, hemorrhage, and compression of vital brain structures.
- High-grade astrocytomas often show vascular proliferation and resistance to therapy, contributing to rapid progression and recurrence.
Clinical Manifestations
- Headache (worse in morning)
- Seizures
- Nausea and vomiting
- Weakness or numbness
- Behavioral or personality changes
- Blurred or double vision
Diagnostic Evaluation
- MRI Brain with contrast (best tool)
- CT Scan
- Biopsy (histological grading)
- Neurological examination
- Molecular testing (IDH mutation, MGMT promoter status)
Medical Management
1️⃣ Surgical Removal
Whenever feasible, surgical resection of the tumor is performed to reduce mass effect and confirm diagnosis by histopathology.
2️⃣ Radiotherapy
It is used post-operatively or in inoperable tumors, especially in high-grade astrocytomas, to destroy residual tumor cells.
3️⃣ Chemotherapy
Temozolomide is commonly used for glioblastoma, along with other agents like nitrosoureas.
4️⃣ Targeted Therapy
In some cases, agents targeting molecular mutations (e.g., IDH1) may be used in clinical trials or specific tumor types.
5️⃣ Corticosteroids
Dexamethasone is often prescribed to reduce cerebral edema and intracranial pressure, thereby relieving symptoms like headache and nausea.
Nursing Management
Neurological Monitoring
- It is the nurse’s responsibility to frequently assess the patient’s level of consciousness, orientation, pupil response, and motor strength to detect early signs of increased intracranial pressure or neurological deterioration.
Medication Administration and Monitoring
- The nurse must administer corticosteroids and antiepileptic drugs as prescribed and closely monitor for adverse effects such as hyperglycemia, infection, or sedation.
Postoperative Care
- It is important to provide post-surgical care including wound assessment, drainage monitoring, and prevention of complications such as infection, CSF leak, or seizures.
Psychological Support
- The nurse should offer emotional support to both the patient and family, as astrocytic tumors, especially malignant ones, carry a poor prognosis that can cause anxiety, depression, and fear.
Nutritional and Functional Support
- It is essential to encourage adequate nutrition, assist with feeding if needed, and promote mobility and physical therapy to prevent muscle wasting and pressure sores, especially in bedridden patients.
Complications
- Increased intracranial pressure
- Seizures
- Brain herniation
- Neurological deficits (e.g., hemiparesis, aphasia)
- Tumor recurrence or progression
- Cognitive and personality changes
4. Gestational trophoblastic disease
Definition
- Gestational Trophoblastic Disease refers to a group of rare tumors that arise from abnormal proliferation of trophoblastic cells of the placenta during or after pregnancy.
- It includes both benign and malignant forms, such as Hydatidiform Mole (complete and partial), Invasive mole, Choriocarcinoma, and Placental Site Trophoblastic Tumor (PSTT).
Types of Gestational Trophoblastic Disease (GTD)
1️⃣ Hydatidiform Mole
- Most common type; also called molar pregnancy.
- Abnormal growth of chorionic villi forming grape-like vesicles.
- Subtypes: Complete (no fetus) and Partial (some fetal tissue present).
2️⃣ Invasive Mole
- A hydatidiform mole that invades the myometrium (uterine muscle).
- Can cause uterine perforation and bleeding.
- Usually follows a complete mole.
3️⃣ Choriocarcinoma
- A highly malignant tumor of trophoblastic tissue.
- Can metastasize rapidly to lungs, liver, brain.
- Requires aggressive chemotherapy (e.g., methotrexate).
4️⃣ Placental Site Trophoblastic Tumor (PSTT)
- Rare tumor at the placental implantation site.
- Slow-growing but may become chemotherapy-resistant.
- Often treated with surgery (e.g., hysterectomy).
Etiology
- Abnormal fertilization of ovum
- Maternal age <20 or >40 years
- History of previous molar pregnancy
- Nutritional deficiencies (low carotene, folic acid)
- Ovular genetic defects (empty egg or double sperm)
Clinical Manifestations
- Vaginal bleeding (usually dark brown or prune-colored)
- Excessive nausea and vomiting (hyperemesis gravidarum)
- Uterus larger than gestational age
- Absence of fetal heart sounds
- Passage of grape-like vesicles
- High beta-hCG levels
- Early onset preeclampsia (<20 weeks)
Diagnostic Evaluation
- Serum β-hCG levels (markedly elevated)
- Transvaginal ultrasound (“snowstorm” or “cluster of grapes” pattern)
- Chest X-ray (to check for metastasis)
- Histopathological exam (after evacuation)
- CBC, liver & renal function tests for pre-op assessment
Medical and Surgical Management
1. Uterine Evacuation
- Suction curettage is the treatment of choice for molar pregnancy.
- Oxytocic agents are used post-evacuation to contract the uterus.
2. Chemotherapy
- Methotrexate or Actinomycin-D is used for malignant forms like choriocarcinoma or persistent trophoblastic disease.
- Chemotherapy is continued until three consecutive negative β-hCG levels.
3. Follow-up
- Monitor β-hCG levels weekly until normal, then monthly for 6–12 months.
- Avoid pregnancy for at least one year during follow-up.
Nursing Management
1. Monitoring and Diagnosis
- The nurse should monitor vaginal bleeding, uterine size, and signs of infection during and after evacuation.
- Assist in ultrasound, serum hCG testing, and prepare the patient for procedures like suction D&C.
2. Postoperative Care
- Monitor vital signs, intake/output, and signs of complications like perforation or hemorrhage.
- Administer prescribed oxytocics, antibiotics, and analgesics as required.
3. Emotional and Psychological Support
- The nurse must offer emotional reassurance due to loss of pregnancy and risk of cancer.
- Provide grief counseling and family support if needed.
4. Follow-up and Education
- Educate the patient about the importance of regular follow-up β-hCG tests.
- Advise to use reliable contraception and avoid pregnancy for at least one year post-treatment.
- Encourage adherence to chemotherapy schedules if prescribed.
Complications
- Hemorrhage
- Uterine perforation
- Progression to choriocarcinoma
- Infertility (rare)
- Metastasis (lungs, liver, brain)
5. Opportunistic infections and neoplasm found in patient with HIV infection
- Human Immunodeficiency Virus (HIV) primarily attacks the immune system, especially CD4+ T lymphocytes, making the patient highly vulnerable to infections and cancers that would not typically cause illness in healthy individuals.
- These infections and tumors are called opportunistic because they take advantage of the weakened immune system, especially when the CD4 count falls below 200 cells/mm³.
Opportunistic Infections in HIV Patients
1️⃣ Fungal Infections
🔹 Candidiasis
It is one of the most common fungal infections, affecting the oral cavity (thrush), esophagus, and vagina, causing white patches, pain, and difficulty swallowing.
🔹 Cryptococcal Meningitis
It is a life-threatening infection of the meninges caused by Cryptococcus neoformans, presenting with headache, fever, neck stiffness, and altered mental status.
🔹 Pneumocystis jirovecii pneumonia (PCP)
It is a severe fungal lung infection, causing dry cough, hypoxia, and respiratory distress, especially in patients with CD4 <200.
🔹 Histoplasmosis
It is a disseminated fungal infection affecting lungs, liver, and bone marrow, causing fever, cough, and hepatosplenomegaly.
2️⃣ Viral Infections
🔹 Cytomegalovirus (CMV)
It can cause retinitis leading to blindness, as well as colitis and pneumonitis in patients with severe immunosuppression.
🔹 Herpes Simplex Virus (HSV)
It may cause recurrent, painful genital and oral ulcers, and may involve the esophagus or lungs in advanced cases.
🔹 Varicella Zoster Virus (VZV)
It causes herpes zoster (shingles), with painful skin rashes and blisters, which can become disseminated in HIV patients.
🔹 JC Virus (John Cunningham virus)
It leads to progressive multifocal leukoencephalopathy (PML), a fatal brain disease causing weakness, visual disturbances, and altered behavior.
3️⃣ Bacterial Infections
🔹 Mycobacterium tuberculosis (TB)
It is a common co-infection with HIV, affecting lungs and other organs, with symptoms like chronic cough, weight loss, fever, and night sweats.
🔹 Mycobacterium avium complex (MAC)
It causes disseminated infection in patients with CD4 count <50 cells/mm³, presenting with fever, diarrhea, and anemia.
🔹 Salmonella species
They may cause recurrent septicemia (blood infections) with symptoms like fever and diarrhea.
🔹 Bacterial pneumonias
Caused by Streptococcus pneumoniae, Haemophilus influenzae, often recurring and severe in HIV-infected persons.
4️⃣ Parasitic Infections
🔹 Toxoplasmosis
Caused by Toxoplasma gondii, it leads to brain abscesses, seizures, and neurological symptoms, particularly when CD4 count is below 100.
🔹 Cryptosporidiosis
It is a parasitic infection of the intestines causing chronic watery diarrhea, weight loss, and electrolyte imbalance.
🔹 Isosporiasis
It also causes prolonged diarrhea, mainly seen in tropical countries and immunocompromised patients.
Neoplasms (Cancers) in HIV Patients
1️⃣ Kaposi’s Sarcoma
It is the most common AIDS-related malignancy, caused by Human Herpesvirus 8 (HHV-8), presenting as purple or brown skin lesions, and may involve internal organs like lungs and GI tract.
2️⃣ Non-Hodgkin’s Lymphoma (NHL)
It includes aggressive B-cell lymphomas such as primary CNS lymphoma, which presents with headaches, seizures, and focal neurological deficits.
3️⃣ Cervical Cancer
It is caused by persistent HPV (Human Papillomavirus) infection, and HIV-positive women are at higher risk of developing invasive cervical carcinoma.
4️⃣ Anal Cancer
It is also associated with HPV infection, and risk is increased in men who have sex with men (MSM) and immunocompromised individuals.
5️⃣ Hodgkin’s Lymphoma
Though less common than NHL, it can occur in HIV-positive persons, often with more advanced disease and poorer prognosis.
Nursing Responsibilities
1️⃣Infection Prevention
It is the nurse’s responsibility to educate HIV patients on maintaining hygiene, using safe food and water, and avoiding exposure to infectious environments, especially when CD4 counts are low.
2️⃣ Early Symptom Identification
The nurse must monitor for signs of opportunistic infections such as fever, cough, weight loss, seizures, or diarrhea, and report to the physician for timely intervention.
3️⃣ Medication Adherence Support
The nurse should ensure that patients adhere strictly to ART (antiretroviral therapy) and prophylactic medications to prevent opportunistic infections like PCP or toxoplasmosis.
4️⃣ Emotional and Psychological Support
It is important for the nurse to provide counseling and mental health support to patients dealing with cancer diagnosis or chronic infections, which may affect their self-esteem and emotional wellbeing.
5️⃣ Nutritional and Hydration Support
The nurse should encourage high-protein, calorie-dense diet and adequate fluid intake, especially in patients with weight loss, chronic diarrhea, or cancer-related cachexia.
Q.2 Describe etiopathogenesis (any two) [10 mark]
1. Emphysema
Etiology of Emphysema
1. Cigarette Smoking (Primary Cause)
- It is the most common and preventable cause of emphysema due to chronic inhalation of smoke, which damages alveolar walls and reduces lung elasticity.
2. Alpha-1 Antitrypsin Deficiency (Genetic Cause)
- It is a rare inherited condition that leads to early-onset emphysema, especially in non-smokers, by allowing unchecked destruction of alveolar tissue by enzymes.
3. Long-term Air Pollution Exposure
- Continuous exposure to industrial pollutants, vehicular fumes, and biomass fuels can cause chronic irritation and alveolar damage.
4. Repeated Respiratory Infections
- Frequent lung infections in childhood or adulthood can damage the airways and alveoli, contributing to emphysematous changes.
🔸 5. Occupational Exposure
→ Working in environments with chronic exposure to chemical fumes, coal dust, or asbestos increases the risk of emphysema.
6. Aging and Natural Lung Degeneration
- With increasing age, there is gradual loss of lung tissue elasticity and recoil, which can mimic or worsen emphysematous changes.
7. Passive Smoking (Secondhand Smoke)
- Prolonged exposure to environmental tobacco smoke can also lead to chronic inflammation and alveolar wall destruction.
8. Poor Nutrition and Low Antioxidant Levels
- Deficiency of vitamin C, E, or other antioxidants may impair lung repair mechanisms, making lungs more prone to damage.
Pathogenesis of Emphysema
Exposure to Irritants
- It begins with long-term exposure to harmful substances such as cigarette smoke, air pollution, or chemical fumes, which irritate and damage the airway epithelium.
Inflammatory Cell Infiltration
- Irritation leads to the recruitment of neutrophils, macrophages, and lymphocytes into the alveolar spaces, triggering an inflammatory response.
Protease Release and Tissue Damage
- These inflammatory cells release proteolytic enzymes (especially elastase), which begin to break down elastin and collagen present in the alveolar walls.
Antiprotease Imbalance
- In healthy lungs, alpha-1 antitrypsin neutralizes proteases.
- In emphysema (especially in genetic forms), there is a deficiency or inactivation of alpha-1 antitrypsin, causing an imbalance between proteases and antiproteases.
Destruction of Alveolar Walls (Septal Damage)
- Due to unchecked proteolytic activity, alveolar septa are destroyed, resulting in loss of alveolar wall integrity and merging of alveoli into larger, less efficient air spaces.
Loss of Elastic Recoil
- Destruction of elastin fibers reduces the lung’s ability to recoil during expiration, leading to air trapping and hyperinflation of the lungs.
Formation of Bullae
- The destruction leads to enlarged air spaces (bullae) which do not contribute to gas exchange and further reduce lung function.
Pulmonary Capillary Bed Loss
- Along with alveolar damage, the surrounding capillary networks are also destroyed, reducing pulmonary perfusion and impairing gas exchange.
Airflow Limitation
- Due to narrowed bronchioles and collapse of alveolar walls during exhalation, there is difficulty in air expulsion, causing progressive airflow obstruction.
Ventilation-Perfusion (V/Q) Mismatch
- The mismatch between ventilation and perfusion develops, leading to hypoxemia and in later stages, hypercapnia.
Chronic Lung Hyperinflation
- Continuous air trapping results in barrel-shaped chest, flattened diaphragm, and increased work of breathing, especially during exertion.
2. Nephrotic syndrome
Etiology of Nephrotic Syndrome
1. Primary (Idiopathic) Glomerular Diseases
- It includes kidney-specific conditions where no systemic cause is identified:
- Minimal Change Disease (MCD) – most common in children
- Focal Segmental Glomerulosclerosis (FSGS)
- Membranous Nephropathy
2. Secondary Causes (Systemic Diseases)
- It occurs as a result of systemic conditions affecting kidneys:
- Diabetes mellitus (Diabetic nephropathy)
- Systemic Lupus Erythematosus (SLE)
- Amyloidosis
- HIV infection
- Hepatitis B and C
3. Infections (Post-Infectious Glomerulonephritis)
- Certain infections can trigger nephrotic syndrome:
- Streptococcal infections
- Malaria
- Syphilis
- Schistosomiasis
4. Allergic Reactions and Toxins
- It may be induced by insect stings, bee venom, or toxins that alter glomerular permeability.
5. Drugs and Medications
- Some drugs can cause nephrotic syndrome through hypersensitivity or toxic effects:
- NSAIDs (e.g., ibuprofen)
- Penicillamine
- Gold compounds
- Interferons
6. Malignancies (Paraneoplastic Syndromes)
- Certain cancers are associated with nephrotic syndrome:
- Lymphomas (especially Hodgkin’s)
- Leukemia
- Carcinomas of lung, colon, and stomach
7. Hereditary and Congenital Causes
- Genetic disorders affecting glomerular structure can lead to early-onset nephrotic syndrome:
- Congenital nephrotic syndrome (Finnish type)
- Alport syndrome
8. Autoimmune Disorders
- Autoimmune diseases causing immune complex deposition in glomeruli may result in nephrotic syndrome:
- SLE
- IgA nephropathy
- Goodpasture’s syndrome
Pathogenesis of Nephrotic Syndrome
Initial Glomerular Injury
- The pathogenesis begins with damage to the glomerular filtration barrier, which includes the glomerular endothelium, basement membrane, and podocytes (epithelial cells).
- This injury may be caused by immune-mediated damage, toxins, infections, or genetic mutations (e.g., minimal change disease or focal segmental glomerulosclerosis).
Alteration in Podocyte Function and Structure
- The podocytes, which normally maintain the slit diaphragm for selective filtration, become effaced, fused, or detached from the basement membrane.
- This causes loss of integrity of the filtration barrier, especially the size and charge-selective properties.
Increased Glomerular Permeability
- Due to podocyte damage and disruption of the basement membrane, there is increased permeability to plasma proteins, especially albumin and other low molecular weight proteins.
- Protein molecules escape into the urine, resulting in massive proteinuria (>3.5g/day).
Hypoalbuminemia and Reduced Plasma Oncotic Pressure
- As albumin is lost in large quantities through urine, the serum albumin levels decrease, leading to hypoalbuminemia.
- This reduces the plasma oncotic (colloid osmotic) pressure, causing fluid to shift from the intravascular space to the interstitial space.
Generalized Edema Formation
- The fluid shift results in interstitial fluid accumulation, leading to periorbital, pedal, and generalized edema (anasarca).
- In response, renal sodium and water retention worsen the edema due to activation of the renin-angiotensin-aldosterone system (RAAS) and antidiuretic hormone (ADH) secretion.
Hyperlipidemia and Lipiduria
- The liver compensates for hypoalbuminemia by increasing lipoprotein synthesis, leading to hypercholesterolemia and elevated triglycerides.
- Lipids also appear in the urine due to glomerular damage, leading to lipiduria with the presence of fatty casts (oval fat bodies) in urine.
Increased Risk of Thrombosis and Infection
- Loss of antithrombin III and other regulatory proteins in urine predisposes the patient to hypercoagulability, leading to renal vein thrombosis or pulmonary embolism.
- Simultaneously, loss of immunoglobulins and complement proteins through urine causes immunosuppression, increasing the risk of bacterial infections like peritonitis or cellulitis.
3. Benign hyperplasia prostate
Etiology of Benign Prostatic Hyperplasia (BPH)
1. Aging (Most Common Factor)
- It is the primary risk factor for BPH, as prostate enlargement naturally occurs with advancing age, especially after the age of 50 years.
2. Hormonal Imbalance
- There is an increase in dihydrotestosterone (DHT), a potent derivative of testosterone, which stimulates prostate cell growth.
- Estrogen levels may also increase with age and may enhance DHT sensitivity in the prostate.
3. Genetic Factors
- BPH risk is higher in men with a family history of prostate enlargement, especially if diagnosed before the age of 60.
4. Lifestyle and Dietary Factors
- Sedentary lifestyle, obesity, high-fat diet, and low fiber intake may contribute to hormonal changes that promote prostatic hyperplasia.
5. Chronic Inflammation
- Long-standing prostatitis or inflammation may lead to cellular proliferation and glandular hyperplasia in the prostate.
6. Metabolic Syndrome
- Conditions such as insulin resistance, hypertension, and dyslipidemia are associated with increased risk of BPH due to hormonal and inflammatory mechanisms.
7. Testicular Function
- Men who undergo bilateral orchiectomy (removal of testes) at an early age do not develop BPH, indicating the role of androgens in its development.
8. Ethnicity
- Some studies show that BPH prevalence may vary among different ethnic groups, with African-American men having a higher risk.
Pathogenesis of Benign Prostatic Hyperplasia (BPH)
Hormonal Influence and Aging
- With advancing age, there is a decrease in active testosterone and a relative increase in estrogen levels in males.
- This hormonal imbalance stimulates the prostate stromal and epithelial cells to multiply abnormally.
- The enzyme 5-alpha reductase converts testosterone into dihydrotestosterone (DHT), which is the primary stimulator of prostate growth.
Increased DHT Activity
- DHT binds to androgen receptors in prostate cells and stimulates DNA synthesis, cell growth, and inhibition of cell death (apoptosis).
- This leads to accumulation of cells in the periurethral (transitional) zone of the prostate gland, resulting in prostate enlargement.
Hyperplasia of Stromal and Epithelial Tissues
- There is non-cancerous overgrowth of both stromal cells (connective tissue) and glandular epithelial cells of the prostate.
- These growing nodules compress the urethra and alter the normal shape and function of the urinary tract.
Compression of the Urethra
- As the enlarged prostate compresses the prostatic urethra, there is increased resistance to urinary flow.
- This leads to obstructive symptoms such as hesitancy, weak stream, straining, and incomplete emptying of the bladder.
Bladder Muscle Compensation and Fatigue
- To overcome the resistance, the detrusor muscle (bladder wall) undergoes hypertrophy and contracts more forcefully.
- Over time, the muscle becomes fatigued and dysfunctional, leading to residual urine, urinary retention, and overflow incontinence.
Development of Secondary Changes
- Prolonged obstruction may cause bladder wall thickening, formation of diverticula, urinary tract infections, hydronephrosis, and potentially renal failure if untreated.
4. Acute inflammation
Etiology of Acute Inflammation
1. Infectious Agents
- It may be caused by bacteria, viruses, fungi, or parasites that invade tissues and trigger an immune-inflammatory response.
2. Physical Agents
- It can result from trauma, cuts, abrasions, burns, radiation, or extreme temperatures (heat or cold).
3. Chemical Agents
- Exposure to toxins, acids, alkalis, or irritants like chemical burns and foreign bodies can initiate inflammation.
4. Immunological Reactions
- It may arise from hypersensitivity reactions (e.g., allergies) or autoimmune diseases where the body attacks its own tissues.
5. Tissue Necrosis / Ischemia
- It can be triggered by cell death due to lack of blood supply (e.g., in myocardial infarction, stroke) causing release of inflammatory signals.
6. Foreign Bodies
- Entry of splinters, sutures, or dust particles may induce a localized acute inflammatory reaction.
Pathogenesis of Acute Inflammation
1. Tissue Injury or Insult
- The process of acute inflammation begins with an injury to body tissues due to infectious agents (bacteria, viruses, fungi), physical trauma, chemical irritants, thermal injury (burns/frostbite), or ischemia (lack of oxygen supply).
- This injury causes cell membrane disruption, leading to the release of intracellular contents, triggering the inflammatory response.
2. Release of Inflammatory Chemical Mediators
- Damaged tissues and activated immune cells such as mast cells, macrophages, and endothelial cells release inflammatory mediators, including:
- Histamine from mast cells
- Bradykinin from plasma proteins
- Prostaglandins from arachidonic acid metabolism
- Leukotrienes from leukocytes
- Cytokines like Interleukin-1 (IL-1) and Tumor Necrosis Factor-alpha (TNF-α)
→ These mediators initiate and regulate the vascular and cellular responses during inflammation.
3. Vasodilation (Increased Blood Flow)
- Histamine and prostaglandins induce arteriolar vasodilation, which increases blood flow to the affected site.
- This results in erythema (redness) and localized heat, classic signs of inflammation (rubor and calor).
4. Increased Vascular Permeability
- Chemical mediators cause endothelial cell retraction, forming intercellular gaps in the capillary walls.
- This allows plasma proteins, antibodies, and leukocytes to leak into the interstitial space, forming protein-rich exudate.
- The accumulation of fluid in tissue causes edema (tumor) and contributes to pain (dolor) due to pressure on nerve endings.
5. Leukocyte Recruitment (WBC Migration)
- Chemotactic substances (e.g., IL-8, C5a, leukotriene B4) attract neutrophils to the inflammation site.
- The leukocyte recruitment involves:
- Margination – WBCs move to the edge of blood vessels
- Rolling and Adhesion – Temporary then firm attachment to endothelium via selectins and integrins
- Diapedesis (Transmigration) – Neutrophils migrate through endothelial gaps into the tissue
6. Phagocytosis and Microbial Killing
- At the site, neutrophils and macrophages engulf pathogens and debris through phagocytosis.
- Inside the phagocyte, lysosomal enzymes, reactive oxygen species (ROS), and nitric oxide (NO) are released to kill and digest the microbes.
- This step is essential for clearing the cause of inflammation and initiating tissue repair.
7. Resolution or Chronic Progression
- If the injurious agent is neutralized, anti-inflammatory mediators like IL-10 and transforming growth factor-beta (TGF-β) promote healing and resolution.
- If the insult persists or damage is extensive, the process may transition into chronic inflammation, abscess formation, or fibrosis (scar tissue).
Genetics
Q.3 Write short notes on (any three) [12 mark]
1. Mendelian inheritance
Introduction to Mendelian Inheritance
- It is known as the classical genetic theory that explains how characteristics are passed from parents to offspring through genes.
- It is based on the experiments conducted by Gregor Johann Mendel, who is known as the Father of Genetics, during the years 1856 to 1863.
- It describes the basic principles by which hereditary traits are transmitted in living organisms, especially using pea plants (Pisum sativum).
- It is the foundation for understanding patterns of inheritance and the behavior of genes during reproduction.
- It focuses on how alleles (alternative forms of genes) influence the genotype (genetic makeup) and phenotype (observable characteristics) of organisms.
Mendel’s Experiments on Pea Plants
- It is important to note that Mendel selected pea plants because they have easily distinguishable traits, are self-pollinating, and have a short generation time.
- He selected seven contrasting traits such as tall/dwarf plants, round/wrinkled seeds, green/yellow pods, etc.
- He performed monohybrid crosses (single trait) and dihybrid crosses (two traits) and recorded the inheritance patterns over multiple generations.
- His results were based on quantitative analysis, where he applied mathematics and probability to interpret the data.
- From his observations, he proposed three fundamental laws of inheritance that became the basis of classical genetics.
3. Mendel’s Three Laws of Inheritance
1️⃣ Law of Dominance
- It states that when two alleles are different, one allele (dominant) masks the effect of the other (recessive) in the heterozygous condition.
- It was observed in the F₁ generation, where all offspring from a cross between tall (TT) and dwarf (tt) plants were tall (Tt).
- It shows that dominant traits are expressed even when only one copy of the gene is present.
- For example, if T = Tall and t = dwarf, the genotype Tt results in a tall phenotype due to dominance of T.
2️⃣ Law of Segregation (Purity of Gametes)
- It states that alleles for each trait separate during gamete formation, so each gamete carries only one allele for each gene.
- It means that the two members of a gene pair (one from each parent) are segregated independently during meiosis.
- This law explains why traits may reappear in the F₂ generation even if they are absent in the F₁ generation.
- For example, crossing two heterozygous plants (Tt × Tt) results in a 3:1 ratio (Tall : Dwarf) in the F₂ generation.
3️⃣ Law of Independent Assortment
- It states that genes for different traits assort independently of one another during gamete formation.
- This means that the inheritance of one trait is not affected by the inheritance of another trait.
- It is applicable in dihybrid crosses where two traits are studied at once, such as seed shape and seed color.
- In a cross of RRYY × rryy (Round Yellow × Wrinkled Green), the F₂ generation shows a 9:3:3:1 phenotypic ratio.
Examples of Mendelian Traits in Humans
- Tongue rolling – The ability to roll the tongue is dominant.
- Earlobe attachment – Free earlobes are dominant; attached earlobes are recessive.
- Dimples on cheeks – Presence of dimples is a dominant trait.
- Freckles on the face – Presence of freckles is a dominant trait.
- Hitchhiker’s thumb – Straight thumb is dominant; bent thumb is recessive.
- Color blindness – A recessive trait often carried on the X chromosome (sex-linked).
Importance in Nursing and Clinical Genetics
- It helps nurses understand how hereditary diseases like cystic fibrosis, hemophilia, and thalassemia are passed on.
- It allows the nurse to educate families about genetic risks and patterns of inheritance in counseling sessions.
- It supports nurses in recognizing carrier states in parents, especially for autosomal recessive conditions.
- It plays a role in prenatal diagnosis and screening, helping detect abnormalities like Down syndrome or Tay-Sachs.
- It helps nurses provide emotional and informational support to clients at risk for genetic diseases.
- It aids in the application of ethical principles when dealing with family history and genetic testing results.
2. Allele and haplotype
ALLELE
Definition of Allele
- It is defined as an alternative or variant form of a gene that is located at the same position (locus) on homologous chromosomes.
- Alleles control specific traits, and they occur in pairs in diploid organisms — one inherited from the mother and one from the father.
- Every individual has two alleles for each gene, and the combination of these alleles determines the individual’s observable traits (phenotype).
Key Features of Allele
- Alleles exist in different forms – dominant, recessive, co-dominant, or incomplete dominant – and each type influences how a trait appears.
- Alleles control inherited characteristics like eye color, blood type, hair texture, and genetic disorders.
- Alleles can be identical (homozygous, e.g., AA or aa) or different (heterozygous, e.g., Aa) in an individual.
- Alleles can mutate over generations, leading to genetic diversity, disease susceptibility, or resistance.
Types of Alleles
- Dominant allele – It expresses the trait in both homozygous and heterozygous conditions. (Example: A for tallness in pea plants)
- Recessive allele – It expresses the trait only when present in homozygous form. (Example: a for dwarfness in pea plants)
- Co-dominant allele – Both alleles are expressed equally in the heterozygous state. (Example: IA and IB in AB blood group)
- Multiple alleles – More than two alleles exist for a single gene in the population. (Example: ABO blood group system – IA, IB, i)
- Mutant allele – A changed allele due to mutation that may lead to diseases like sickle cell anemia or cystic fibrosis.
Examples of Alleles
- Blood Group – IA, IB, i (A, B, AB, and O blood groups)
- Eye Color – Brown (dominant), blue (recessive)
- Sickle Cell Anemia – HbA (normal) and HbS (mutated) alleles
- Cystic Fibrosis – CFTR gene mutations lead to disease
- Pea Plant Height – T (tall), t (dwarf)
HAPLOTYPE
Definition of Haplotype
- A haplotype is defined as a group of genes or DNA variations (alleles, markers, or SNPs) that are inherited together from a single parent, because they are located close together on the same chromosome.
- The term “haplotype” is short for haploid genotype, and it describes a segment of DNA where genes are transmitted as a block.
- Haplotypes are especially important in genetic linkage studies, organ transplant matching, and disease research.
Key Features of Haplotype
- A haplotype represents a specific combination of genetic markers or alleles, inherited without recombination.
- It helps in studying population genetics, tracing inheritance patterns, and understanding genetic predisposition to diseases.
- Haplotypes are crucial in HLA typing for organ transplantation, where compatibility is essential for graft survival.
- Haplotypes are identified using genome sequencing and SNP analysis, which can uncover inherited risk factors for diseases.
Examples of Haplotype
- HLA Haplotype – A combination of HLA-A, HLA-B, and HLA-DR genes inherited together from one parent.
- SNP Haplotype Block – A set of closely linked SNPs (Single Nucleotide Polymorphisms) passed together during inheritance.
- Y-chromosome haplotypes – Used in tracing paternal lineage in genetics
3. Incomplete dominance
Definition
- Incomplete dominance is defined as a type of non-Mendelian inheritance where neither of the two alleles is completely dominant over the other, resulting in a heterozygous phenotype that is a blend or intermediate of the two homozygous phenotypes.
- It is a condition where both alleles in a gene pair partially express themselves, and the resultant trait is not like either parent but is an intermediate of both.
Scientific Basis / Mechanism
1️⃣ In incomplete dominance, each allele contributes to the expression of the phenotype, but neither is strong enough to fully express itself alone in the presence of the other.
2️⃣ The heterozygous individual has both alleles active, and the proteins or enzymes produced by both alleles combine to form an intermediate expression.
3️⃣ This pattern contrasts with complete dominance, where one dominant allele completely masks the effect of a recessive allele.
4️⃣ The concept of incomplete dominance follows Mendel’s law of segregation (alleles segregate independently) but violates his principle of dominance.
Phenotypic and Genotypic Ratio (In F2 Generation)
✅ Phenotypic ratio – 1:2:1 (distinct from Mendelian 3:1)
✅ Genotypic ratio – 1:2:1 (same as phenotype)
Example
RR (Red flower) × WW (White flower) → All RW (Pink flowers)
RW × RW → 1 RR (Red) : 2 RW (Pink) : 1 WW (White)
Classic Examples of Incomplete Dominance
1. Mirabilis Jalapa (Four O’Clock Plant)
- This is the most commonly cited botanical example.
- When a plant with red flowers (RR) is crossed with a plant with white flowers (WW), all F1 offspring produce pink flowers (RW).
- In F2 generation, self-cross of pink plants gives red, pink, and white flowers in 1:2:1 ratio.
- The pink flower phenotype is intermediate, showing incomplete dominance.
2. Andalusian Fowl (Birds)
- When a black-feathered bird (BB) is crossed with a white-feathered bird (WW), the offspring have blue-grey feathers (BW).
- This intermediate color is a result of partial expression of both black and white alleles.
3. Human Example – Tay-Sachs Disease (Biochemical Level)
- In Tay-Sachs disease, the homozygous recessive individual (tt) suffers from complete enzyme deficiency, leading to fatal neurodegeneration.
- Heterozygous individuals (Tt) have only half the normal amount of enzyme and may show mild or no symptoms, thus expressing an intermediate phenotype.
Key Characteristics of Incomplete Dominance
1️⃣ It occurs when neither allele is completely dominant or recessive over the other.
2️⃣ The heterozygous phenotype is intermediate between the two homozygous phenotypes.
3️⃣ It leads to a blending of parental traits, but the original traits reappear in F2 generation.
4️⃣ The phenotypic and genotypic ratios are the same in F2: 1 homozygous dominant : 2 heterozygous : 1 homozygous recessive.
5️⃣ It is a type of non-Mendelian inheritance, commonly seen in plants, birds, and in some biochemical traits in humans.
Importance in Nursing and Genetics
1️⃣ Understanding incomplete dominance is useful in genetic counseling, especially when explaining carrier states and risk probabilities to patients and families.
2️⃣ It helps in predicting phenotypic outcomes in cases of autosomal diseases or traits that don’t follow typical dominant-recessive patterns.
3️⃣ It is foundational knowledge for interpreting genetic disorders, especially in fields like pediatric nursing, community health, and prenatal care.
4. Gene therapy
Definition of Gene Therapy
- Gene therapy is a technique in which defective or missing genes are replaced, removed, or altered to treat or prevent disease.
- It is mainly used to treat genetic disorders, some cancers, and certain viral infections by introducing functional genes into a patient’s cells.
- It is a part of genomic medicine, aimed at correcting genetic abnormalities at their root cause.
Principle of Gene Therapy
- It works on the concept of delivering a normal functional gene to cells that are affected by defective or missing genes.
- This gene is inserted using a vector, commonly a virus modified to carry human genetic material without causing disease.
- Once inside the body, the gene expresses a therapeutic protein to correct the disorder.
Types of Gene Therapy
1️⃣ Somatic Gene Therapy
- It involves inserting genes into somatic (body) cells such as liver, muscle, or blood cells.
- It affects only the treated individual and is not passed on to offspring.
2️⃣ Germline Gene Therapy
- It involves modifying genes in sperm, eggs, or embryos.
- Changes are heritable and passed on to future generations.
- It is ethically controversial and not allowed in many countries.
3️⃣ In Vivo Gene Therapy
- Gene is directly delivered into the patient’s body.
4️⃣ Ex Vivo Gene Therapy
- Cells are taken from the patient, genetically modified in the lab, and then re-injected into the patient.
Steps in Gene Therapy Procedure
- Identification of faulty gene causing the disease.
- Designing or choosing a healthy gene that can compensate for the defect.
- Selecting a vector (e.g., adenovirus, lentivirus, liposome).
- Delivery of the gene into the target cell or tissue.
- Monitoring for effectiveness and side effects.
Applications of Gene Therapy
- Genetic Disorders – Cystic fibrosis, Hemophilia, Thalassemia, SCID (Severe Combined Immunodeficiency).
- Cancer Therapy – Altering genes in cancer cells to suppress tumors.
- Viral Infections – Research in HIV/AIDS gene therapy.
- Neurodegenerative Diseases – Parkinson’s disease and Huntington’s disease.
- Ophthalmologic Diseases – Leber’s congenital amaurosis (vision restoration).
Challenges & Limitations
- Possible immune response to vectors.
- Risk of insertional mutagenesis (gene inserted in the wrong place).
- High cost and complex procedures.
- Ethical concerns, especially in germline therapy.
Nursing Responsibilities in Gene Therapy
- It is essential for the nurse to educate the patient and family about the procedure, risks, and benefits of gene therapy.
- The nurse should ensure informed consent is obtained, especially because gene therapy is often experimental.
- It is necessary to monitor the patient closely for any adverse reactions like fever, allergic reaction, or inflammation post gene therapy.
- The nurse should be vigilant in administering supportive care, especially if viral vectors are used.
- The nurse may assist in sample collection, follow-up investigations, and psychological support to the patient.
- It is important to maintain ethical sensitivity and confidentiality when dealing with genetic information.
- The nurse should keep updated knowledge about new gene therapies to provide accurate and current information to the patient.
5. Micro array
Definition
- It is a molecular biology technique used to detect the expression of thousands of genes simultaneously in a single experiment by using a small solid support such as a glass slide or silicon chip.
- It is also called a DNA microarray, gene chip, or biochip, and it allows scientists to analyze gene expression patterns, mutations, or genetic differences.
- It plays an important role in genomics, oncology, genetic testing, and personalized medicine.
Principle
- The basic principle of microarray involves the hybridization of labeled DNA or RNA molecules (from a patient or sample) to complementary DNA probes that are fixed in a specific grid pattern on the chip.
- Each spot on the chip contains known DNA sequences (probes) representing specific genes.
- When the sample’s DNA or RNA binds to the complementary probes, it produces a fluorescent signal, which is detected using a scanner.
- The intensity of fluorescence at each spot represents the level of gene expression or mutation presence.
Steps Involved in Microarray Procedure
1️⃣ Sample Collection
- RNA is isolated from the cells or tissues of the test subject, often from diseased and healthy samples for comparison.
- This step is critical for accurate gene expression analysis.
2️⃣ Reverse Transcription and Labeling
- The isolated RNA is reverse transcribed into complementary DNA (cDNA) using reverse transcriptase.
- During this process, the cDNA is labeled with fluorescent dyes such as Cy3 (green) for control and Cy5 (red) for test samples.
3️⃣ Hybridization
- The labeled cDNA is added to the microarray chip, which contains thousands of fixed probes.
- Under controlled temperature and conditions, the labeled cDNA binds (hybridizes) to the complementary DNA probes.
4️⃣ Washing
- The chip is washed to remove unbound or non-specific molecules to prevent false results.
5️⃣ Scanning and Detection
- The chip is scanned using a laser scanner that detects the fluorescent signals.
- The location and intensity of fluorescence indicate which genes are expressed and to what extent.
6️⃣ Data Analysis
- Specialized software translates the scanned image into digital data showing gene expression profiles, mutation mapping, or comparative expression between two samples.
Types of Microarrays
1️⃣ DNA Microarray
- It is used to study the expression levels of thousands of genes simultaneously.
- It helps in identifying which genes are active or inactive in a particular cell or tissue.
- Commonly used in cancer research to compare healthy and diseased tissue.
2️⃣ SNP Microarray (Single Nucleotide Polymorphism)
- It detects small genetic variations (mutations) at a single DNA base.
- It is helpful in genetic disease diagnosis and studying hereditary conditions.
- Used in prenatal testing and neurological disorders.
3️⃣ Comparative Genomic Hybridization (CGH) Microarray
- It compares tumor DNA with normal DNA to find chromosomal changes.
- It detects deletions or duplications in chromosomes (copy number variations).
- Commonly used in cancer diagnosis.
4️⃣ Protein Microarray
- It analyzes protein-protein interactions and antibody-antigen binding.
- Useful in vaccine research, autoimmune diseases, and diagnosing infections.
5️⃣ Tissue Microarray
- Combines multiple tissue samples on a single slide for analysis.
- Mostly used in histopathology and cancer studies for rapid testing.
Applications in Nursing and Medical Fields
1. Diagnosis of Genetic Disorders
- It is used to detect gene mutations related to Down syndrome, cystic fibrosis, sickle cell anemia, etc.
2. Cancer Research and Oncology
- It helps in detecting gene expression profiles in tumors like breast cancer, leukemia, and lung cancer.
- It identifies oncogenes and tumor suppressor genes for targeted therapy.
3. Prenatal and Neonatal Testing
- Microarrays are used in prenatal screening to detect congenital anomalies in fetuses.
4. Pharmacogenomics
- It helps in understanding individual drug responses, and guides the use of personalized medications to avoid adverse effects.
5. Infectious Disease Diagnosis
- Identifies microbial pathogens and their genetic resistance patterns.
6. Research and Drug Development
- Supports identification of drug targets and biomarker discovery for therapeutic innovations.
Advantages of Microarray
- It allows simultaneous analysis of thousands of genes in one experiment.
- It requires very small amounts of sample, making it minimally invasive.
- It provides rapid results compared to conventional methods.
- It helps in early diagnosis, prognosis, and monitoring treatment responses.
- It supports personalized treatment planning, which is highly beneficial in nursing care planning.
Limitations of Microarray
- It is technically complex and requires advanced laboratory infrastructure.
- The cost of performing microarray is high and not feasible for all hospitals.
- It can detect only known gene sequences, not novel mutations.
- Risk of cross-hybridization or non-specific binding which can cause false results.
- Requires bioinformatics expertise for data interpretation, which may not be available in all clinical settings.
