29/08/2017-B.SC-NURSING FOUNDATION PAPER SOLUTION NO.6
PAPER SOLUTION NO.6 – 29/08/2017
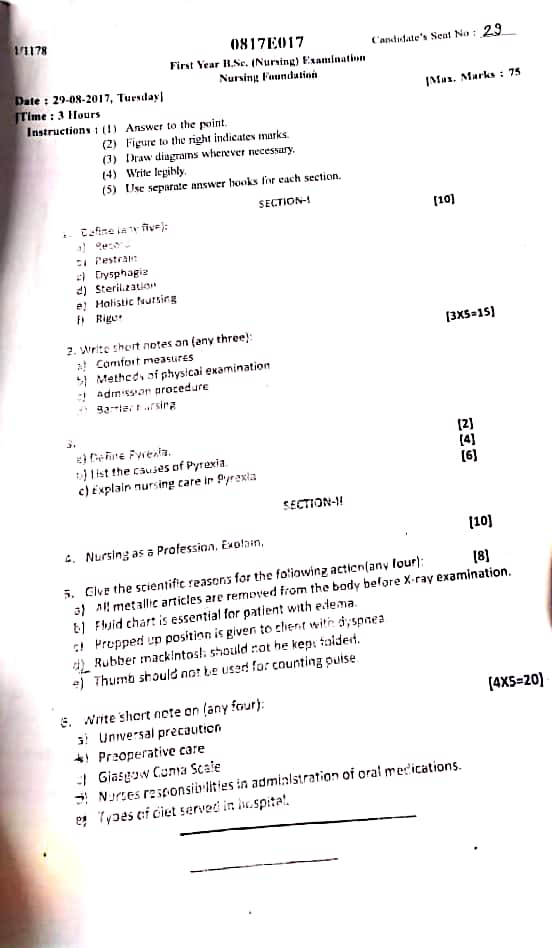
Section 1
Q.1 Define following (any five) (10 mark)
a) Record
- A record is a written or electronic document that systematically captures, stores, and preserves important information, observations, or events for future reference, communication, evaluation, or legal purposes in the healthcare setting.
- In nursing, records are essential for documenting patient care, treatments, progress, and communication among healthcare professionals.
b) Restraint
- Restraint is any method, device, material, or equipment used to limit a person’s movement, physical activity, or access to their own body to protect the patient or others from harm.
- Restraints can be physical (such as belts, straps, or side rails), chemical (medications used to sedate or control behavior), or environmental (like seclusion rooms).
- The use of restraints should always follow strict guidelines, be ethically justified, and used only when necessary, as they can affect a person’s dignity and autonomy
c) Dysphagia
- Dysphagia is a medical term that refers to difficulty or discomfort in swallowing.
- It can occur during the swallowing of solids, liquids, or both, and may result from problems in the mouth, throat (pharynx), or esophagus.
- Causes may include neurological disorders (like stroke), structural abnormalities, or muscular disorders.
d) Sterilization
- Sterilization is a process used to destroy or eliminate all forms of microbial life, including bacteria, viruses, fungi, and bacterial spores, from instruments, equipment, or surfaces. It is a critical step in infection control to prevent the transmission of infectious agents.
- Sterilization methods can be physical (such as heat—autoclaving, dry heat), chemical (using agents like ethylene oxide or glutaraldehyde), or mechanical (filtration).
e) Holistic nursing
- Holistic nursing is a practice that considers the whole person—body, mind, emotions, spirit, and environment—in the care and treatment of patients.
- It focuses on promoting healing and well-being by addressing physical, psychological, social, cultural, and spiritual needs, rather than just treating symptoms or diseases.
f) Rigor
- Rigor is a sudden, intense episode of shivering accompanied by shaking of the whole body due to rapid, involuntary muscle contractions.
- It usually occurs when the body temperature rises quickly, commonly seen in infections like malaria or septicemia.
- Rigor indicates a rapid increase in the hypothalamic set point for temperature, causing the body to generate heat through muscle activity.
Q.2 Write short notes (any three) (3×5=15)
a) Comfort measures
Definition of Comfort Measures
- Comfort measures are the actions taken by the nurse to enhance the comfort, reduce suffering, and promote rest and relaxation of patients across all age groups and health conditions.
- These measures are both physical (like relieving pain or positioning) and psychosocial (like listening or supporting emotionally) in nature.
Objectives of Comfort Measures
- It is to promote rest, relaxation, and peaceful environment for recovery or palliative care.
- It is to prevent bedsores, fatigue, pain, or anxiety in the hospitalized patient.
- It is to enhance the patient’s sense of dignity, privacy, and psychological stability.
- It is to support a better healing process by reducing physical and emotional stress.
Types of Comfort Measures
A. Physical Comfort Measures
- It includes positioning the patient properly in bed, such as semi-Fowler’s or lateral position to prevent pressure sores and promote breathing.
- It is providing a clean, dry, and wrinkle-free bed, which prevents skin irritation and improves sleep.
- It is ensuring pain management using prescribed medications or non-pharmacological interventions like massage or cold/hot compress.
- It is maintaining body hygiene through sponge baths, oral care, hair brushing, and nail care to make the patient feel fresh.
- It is regulating room temperature, lighting, and noise levels to create a peaceful environment.
- It involves meeting elimination needs by timely offering of bedpan, urinal, or helping to the toilet.
- It is giving adequate nutrition and hydration as per the patient’s condition.
B. Psychological Comfort Measures
- It includes providing emotional support through listening, talking, or simply being present during distress.
- It is reassuring the patient about their treatment, progress, and clarifying doubts.
- It is encouraging family visits or interaction as per hospital policy to promote a sense of connection.
- It is offering privacy during procedures and rest, using curtains and soft tone of voice.
- It is respecting cultural, spiritual, and personal values of the patient to foster dignity and trust.
C. Spiritual Comfort Measures
- It is providing access to religious books, prayer items, or spiritual personnel if the patient desires.
- It is ensuring a peaceful and respectful environment for patients in terminal or palliative care.
- It is giving time and space for silent meditation, prayer, or spiritual expression.
Nurse’s Role in Providing Comfort Measures
- It is the nurse’s role to continuously assess the patient’s physical condition and level of discomfort by using pain rating scales, verbal cues, or non-verbal signs such as grimacing, restlessness, or withdrawal.
- The nurse should ensure proper positioning and alignment of the patient’s body, using pillows, supports, and footboards to prevent pressure sores, joint contractures, and respiratory issues.
- It is the nurse’s duty to promote personal hygiene and grooming, including oral care, bed baths, skin care, perineal care, and clean linen, which help restore patient dignity and reduce infection risk.
- The nurse must adjust the environment to ensure comfort by managing room temperature, turning off bright lights, reducing noise, and ensuring proper ventilation and cleanliness.
- It is the nurse’s responsibility to provide prescribed analgesics, antipyretics, or sedatives safely and monitor their effectiveness for managing pain or anxiety.
- The nurse should communicate empathetically and offer psychological comfort by active listening, addressing fears, clarifying doubts, and reassuring patients about their treatment.
- The nurse must encourage mobility or gentle range-of-motion exercises as appropriate to prevent stiffness, promote circulation, and enhance comfort in bed-ridden patients.
- It is important for the nurse to assist with elimination needs like offering a bedpan, urinal, or helping to the toilet, and ensuring perineal hygiene to avoid skin breakdown or infection.
- The nurse should also facilitate family involvement or spiritual support, if desired by the patient, to promote emotional and cultural comfort, especially in terminal or long-term care settings.
- It is essential for the nurse to document all comfort measures provided, assess their outcomes, and communicate with the healthcare team if discomfort persists or worsens.
- The nurse should provide small diversional activities like music therapy, allowing personal items at bedside, reading material, or light conversation to distract from pain and loneliness.
- The nurse must ensure respect for the patient’s preferences and dignity, including preferences for food, routine, and cultural or spiritual practices, which greatly enhance the feeling of comfort.
b) Method of physical examination
It is a systematic process used by healthcare professionals to collect objective data about the patient’s body through direct observation, palpation, percussion, and auscultation in order to assess health status and detect any abnormalities.
1. Inspection (Visual Observation)
- It is the first and most basic technique of physical examination in which the nurse uses the eyes to carefully observe every area of the patient’s body for signs of health or disease.
- It is used to evaluate general appearance, skin conditions, color changes, body symmetry, gait, and behavior.
- It must be performed in a well-lit environment, preferably using both natural and artificial light for accurate observation.
- It is also useful to observe involuntary movements, facial expressions, mood, hygiene, and visible scars or deformities.
- The nurse should inspect from multiple angles, sometimes using tools like a penlight or magnifier to examine details like pupils or lesions.
- It should be done before touching the patient, to avoid altering the natural appearance of the skin or structures.
2. Palpation (Touch)
- It is the method in which the nurse uses the pads of the fingers or whole hand to feel body parts, to assess abnormalities not visible during inspection.
- It helps in identifying tenderness, texture, temperature, shape, swelling, and pulsations of organs or tissues.
- The nurse may perform light palpation (about 1 cm depth) for surface structures and deep palpation (4–5 cm) to assess organs like liver or spleen.
- The dorsal surface of the hand is more sensitive to temperature, while the palmar surface is better for assessing texture and moisture.
- It is important to warm the hands before palpation to ensure patient comfort.
- Palpation should be done gently and gradually, starting with non-tender areas and moving towards tender zones to avoid causing unnecessary pain.
3. Percussion (Tapping)
- It is a technique where the examiner taps gently on the surface of the body using fingers to evaluate the condition of underlying structures based on the sound produced.
- It is commonly used to assess organs such as the lungs, abdomen, and liver to determine if they are air-filled, fluid-filled, or solid.
- The sounds produced during percussion are classified as resonance, hyperresonance, dullness, flatness, and tympany, each indicating different tissue characteristics.
- The technique includes direct percussion (tapping directly on the body) and indirect percussion (tapping on a finger placed on the body).
- It is useful in identifying fluid in pleural spaces (pleural effusion), enlarged organs, or bowel obstruction.
- Percussion also helps in measuring the size and position of organs like liver and spleen, especially in medical-surgical settings.
4. Auscultation (Listening with Stethoscope)
- It is a method in which the nurse uses a stethoscope to listen to internal body sounds produced by organs such as the lungs, heart, intestines, and blood vessels.
- It is essential to assess heart rate, rhythm, murmurs, lung sounds (e.g., crackles, wheezes), and bowel activity.
- Auscultation should be performed in a quiet room, with the stethoscope placed directly on the skin (not over clothes) for accurate sounds.
- The nurse should be familiar with normal and abnormal sounds, such as S1 and S2 heart sounds, bronchial and vesicular breath sounds, and bowel gurgles.
- The diaphragm of the stethoscope is used for high-pitched sounds (breath, bowel, normal heart sounds), while the bell is used for low-pitched sounds (murmurs, bruits).
- It should be done after percussion and palpation, except during abdominal exams, where auscultation comes first to avoid altering bowel sounds.
5. Olfaction (Use of Smell)
- It is the process in which the nurse uses their sense of smell to identify abnormal body odors that may indicate underlying health problems.
- It helps in detecting foul-smelling wound discharge (infection), fruity breath (diabetic ketoacidosis), alcohol odor (alcohol intoxication), or uremic breath (renal failure).
- Though often overlooked, it can provide quick diagnostic clues even before other tests are performed.
- It is especially useful in neurology, dermatology, wound care, and metabolic disorders.
- The nurse should always maintain professional distance while using this method to ensure dignity and privacy of the patient.
- Proper hygiene must be followed after assessment, especially when dealing with infectious discharges or secretions.
Nursing Considerations During Physical Examination
- The nurse must ensure adequate lighting, privacy, and draping during the procedure.
- Each step should be clearly explained to the patient to gain trust and cooperation.
- All equipment such as gloves, stethoscope, penlight, and tongue depressor must be clean and ready.
- Infection control measures like handwashing and disinfecting tools must be practiced.
- The head-to-toe approach should be followed systematically to avoid missing any body part.
c) Admission procedure
It is a systematic process through which a patient is formally accepted and registered into the healthcare facility to receive medical or nursing care, and includes administrative, medical, and nursing steps.
Definition
It is the process of receiving a patient into the hospital for the purpose of diagnosis, treatment, observation, and care either on a temporary or permanent basis.
Objectives of Admission Procedure
- It is to establish the patient’s identity, condition, and reason for hospitalization.
- It is to ensure continuity of care by documenting vital information and medical history.
- It is to provide comfort and orientation to the patient and reduce anxiety.
- It is to initiate therapeutic interventions and plan for individualized care.
Types of Admission
a. Emergency Admission
- It is an admission that occurs without prior appointment, often due to sudden illness, trauma, or accident.
- It is mostly handled through the emergency department and requires immediate care.
- It includes critical cases like accidents, strokes, poisoning, burns, etc.
b. Routine/Planned Admission
- It is an admission arranged in advance for planned procedures like surgery, investigations, or treatment.
- It allows proper pre-admission preparation and briefing to the patient and family.
- It is scheduled and handled during normal working hours.
c. Direct Admission
- It is a type of admission where the patient is directly admitted into a ward or room without going through the outpatient department.
- It is usually initiated by a consultant or physician known to the patient.
d. Transfer Admission
- It occurs when the patient is transferred from another hospital or healthcare facility for further or specialized care.
- It includes cases like cardiac referral or neurology care.
e. Daycare Admission
- It is when a patient is admitted for short procedures and discharged on the same day.
- Examples include cataract surgery or chemotherapy.
Steps in Admission Procedure
Step 1: Reception and Initial Identification
- It is when the patient arrives and is received by the front office or nurse.
- The patient’s name, age, gender, address, and emergency contact are confirmed.
- The admission slip is checked or generated.
Step 2: Registration and Documentation
- It involves completing admission forms, medical history forms, and consent documents.
- The patient is assigned a unique hospital identification number and admission number.
- Financial details or insurance documents are collected.
Step 3: Medical Assessment
- It is when the doctor or admitting officer performs an initial examination.
- Vitals, chief complaints, medical and surgical history are recorded.
- Provisional diagnosis and treatment orders are noted.
Step 4: Ward Assignment and Transportation
- Based on the patient’s condition, a suitable ward/room is selected (e.g., ICU, private, semi-private).
- The patient is transported to the ward using wheelchair or stretcher as per need.
Step 5: Nursing Admission and Initial Care
- It is the first nursing interaction, where the nurse completes the admission checklist.
- Vitals, weight, height, allergies, personal belongings, and hygiene needs are assessed.
- The patient is oriented to the room, call bell, bathroom, and visiting hours.
Nurse’s Responsibilities During Admission
- Nurses play a vital role in the admission process by ensuring the patient is physically and emotionally comfortable, all data is accurately recorded, and that care begins promptly after admission.
- It is the nurse’s responsibility to receive the patient with warmth, courtesy, and a calm attitude, helping reduce fear and anxiety associated with hospitalization.
- It is essential for the nurse to verify the identity of the patient using name, age, and date of birth, and to apply a properly labeled identification band on the wrist.
- The nurse should assist the patient in settling into the assigned bed or room, helping with positioning, unpacking belongings, and ensuring the surroundings are clean and safe.
- It is the nurse’s duty to perform baseline assessments, including vital signs (temperature, pulse, respiration, blood pressure), weight, height, oxygen saturation, and consciousness level.
- The nurse must record a detailed nursing history, including personal, medical, surgical, allergy, medication, and family background.
- It is crucial to document all personal belongings such as clothes, ornaments, glasses, dentures, and mobility aids, and ensure their safe storage or handover to relatives.
- The nurse should explain hospital policies and routines, including meal timings, visiting hours, medication schedules, and emergency procedures.
- It is necessary for the nurse to initiate the nursing care plan based on assessment findings, and to prioritize care if the patient has urgent needs.
- The nurse must ensure communication and coordination with the healthcare team, especially informing the attending physician about the patient’s arrival and any critical findings.
- The nurse should assist in obtaining laboratory samples or performing investigations ordered immediately after admission (e.g., blood test, ECG, X-ray).
- It is part of the nurse’s role to ensure patient safety, including checking side rails, call bell functionality, bed height adjustment, and orientation to emergency exits.
- The nurse should educate the patient and family members about their condition, treatments planned, and clarify any doubts they have in simple and reassuring language.
- It is also the nurse’s responsibility to provide psychological support, especially in pediatric, elderly, or critically ill patients who may be fearful or disoriented.
- The nurse should check for previous hospital records or medication charts, and integrate them into the current care process if needed.
d) Barrier nursing
Definition of Barrier Nursing
- Barrier nursing is a strict infection control technique used to prevent the spread of infectious diseases from a patient to others, including healthcare workers, visitors, and other patients by using physical, chemical, and procedural barriers.
- It involves isolating the patient, using personal protective equipment (PPE), and following standard precautions like handwashing, disinfection, and safe disposal of materials. This practice is especially important in cases of highly communicable diseases such as tuberculosis, COVID-19, Ebola, and MRSA.
Objectives / Purpose of Barrier Nursing
- It is used to prevent the transmission of pathogens from infected patients to others.
- It is designed to protect healthcare workers from acquiring infections during patient care.
- It helps in isolating the infection source, thereby preventing nosocomial (hospital-acquired) infections.
- It is applied to protect immunocompromised patients through reverse barrier techniques.
- It maintains infection-free hospital environments during outbreaks or epidemics.
Types of Barrier Nursing
1. Strict Barrier Nursing (Source Isolation):
- It is used for patients with contagious diseases like COVID-19, tuberculosis, cholera, MRSA, or measles.
- The aim is to protect others from being infected by the patient.
- Strict isolation, PPE, separate equipment, and restricted access are applied.
2. Protective or Reverse Barrier Nursing:
- It is used to protect immunocompromised patients from acquiring infections from the environment or staff.
- Applied in patients with low immunity, such as those undergoing chemotherapy, transplant recipients, or burn patients.
- Sterile equipment, filtered air, hand hygiene, and no outside food or visitors are common protocols.
Key Principles of Barrier Nursing
Isolation of the Patient:
- Patient must be kept in a separate isolation room with proper ventilation.
Use of PPE (Personal Protective Equipment):
- Includes gowns, gloves, masks, face shields, shoe covers, and caps.
Dedicated Equipment:
- Use separate thermometers, BP cuffs, stethoscopes for each patient.
Hand Hygiene:
- Wash hands thoroughly before and after patient contact using soap or alcohol-based hand rub.
Signage and Restricted Entry:
- Post signs like “Infection Control – Do Not Enter Without PPE” outside isolation rooms.
Environmental Cleaning:
- Disinfect surfaces, equipment, and floors daily using proper disinfectants.
Proper Waste Disposal:
- Dispose of biomedical waste (gloves, masks, dressings) as per color-coded waste segregation guidelines.
Safe Linen Handling:
- Soiled linen must be bagged in red bags and disinfected separately.
Airborne Precaution (if needed):
- Use N95 masks, negative pressure rooms, and restricted movement for airborne diseases like TB.
Education and Communication:
- Teach visitors and family about barrier procedures and use of PPE.
Nursing Responsibilities in Barrier Nursing
Assessment and Monitoring
- Monitor patient for signs of infection, vital signs, and response to treatment.
- Watch for psychological effects of isolation like anxiety or depression.
Maintaining Aseptic Technique
- Perform dressing changes, IV infusions, and procedures using strict aseptic technique.
Supervision of Isolation Practices
- Ensure all staff follow standard and transmission-based precautions consistently.
Use of PPE
- Don and doff PPE according to protocol to avoid contamination.
Documentation
- Record all nursing care, PPE usage, infection control measures, and patient progress.
Patient Education
- Instruct patient and family on the importance of isolation, PPE, and hygiene.
Psychosocial Support
- Provide emotional support and allow safe communication with family members.
Coordination with Infection Control Team
- Collaborate with infection control nurse and report any breach or exposure.
Environmental Hygiene
- Ensure proper disinfection and monitor cleaning personnel adherence.
Waste Management
- Follow biomedical waste protocols strictly to prevent cross-contamination.
Diseases Requiring Barrier Nursing
- Tuberculosis (Airborne)
- COVID-19 (Droplet & Airborne)
- Ebola Virus Disease (Contact)
- MRSA (Contact)
- Hepatitis A and E
- Measles and Chickenpox (Airborne)
- Severe diarrhea like Cholera
- Dengue Hemorrhagic Fever (with bleeding precautions)
Importance of Barrier Nursing
- It is crucial for infection control in hospitals and health centers.
- It protects both patients and healthcare workers from infectious diseases.
- It helps in reducing hospital-acquired infections (HAIs).
- It is essential in the management of outbreaks and pandemics.
- It builds confidence among patients, staff, and public in safe care practices
Q.3
a) Define pyrexia (2)
Pyrexia is defined as a temporary elevation of body temperature above the normal range due to an increase in the body’s thermoregulatory set point, usually in response to infection, inflammation, or illness. In which oral temperature > 37.5°C (99.5°F) and Rectal temperature > 38°C (100.4°F).
b) List the causes of pyrexia (4)
- Bacterial infections
- Viral infections
- Parasitic infections
- Fungal infections
- Autoimmune diseases (e.g., SLE, rheumatoid arthritis)
- Inflammatory conditions (e.g., IBD, trauma, burns)
- Cancers (e.g., leukemia, lymphoma)
- Drug reactions (e.g., antibiotics, antiepileptics)
- Blood transfusion reactions
- Post-vaccination response
- Brain disorders (e.g., meningitis, encephalitis, stroke)
- Seizures and post-ictal states
- Hyperthyroidism / Thyroid storm
- Pheochromocytoma
- Adrenal insufficiency / crisis
- Diabetic ketoacidosis
- Heat stroke / sunstroke
- Excessive physical exertion in heat
- Pyrexia of unknown origin (PUO)
c) Explain nursing care in pyrexia (6)
Nursing care in pyrexia focuses on continuous assessment, symptomatic relief, hydration, comfort, and preventing complications by addressing both medical and emotional needs of the patient.
1. Assessment and Monitoring Responsibilities
- It is the nurse’s responsibility to monitor the temperature using the same site (oral/axillary/rectal) for consistency.
- It is essential to document temperature readings on a temperature chart or graph to visualize fever patterns.
- It is necessary to observe for chills, rigors, or profuse sweating, which can help identify fever stages.
- It is also important to check capillary refill time and oxygen saturation if fever is associated with infection.
- It is the duty of the nurse to assess the patient’s level of consciousness regularly if the fever is very high or the patient is elderly/pediatric.
2. Temperature Reduction Measures
- It is the nurse’s duty to start cooling measures only when the fever crosses 101°F (38.3°C) or based on doctor’s orders.
- It is essential to use ice packs or cooling blankets cautiously to prevent shivering or rebound hyperthermia.
- It is important to avoid alcohol rubs or extreme cold methods, as they may cause vasoconstriction and discomfort.
- It is also necessary to assess for signs of hypothermia during cooling in vulnerable patients.
- It is helpful to ask the patient about comfort level during non-pharmacological methods like sponge bath.
3. Hydration and Nutritional Support
- It is important to encourage frequent small sips of water if the patient cannot tolerate full glass intake at once.
- It is the nurse’s role to include ORS, fruit juices, and clear soups to maintain electrolyte balance.
- It is necessary to monitor for signs of fluid overload when giving IV fluids, especially in cardiac or renal patients.
- It is helpful to offer nutrient-rich, soft foods like khichdi, porridge, or mashed fruits.
- It is also essential to observe for nausea or vomiting, and modify diet as needed.
4. Rest, Comfort, and Hygiene Measures
- It is essential to ensure minimum disturbance during fever, providing a quiet environment to support rest.
- It is important to maintain positioning for comfort, such as elevating the head to ease breathing or side-lying for unconscious patients.
- It is the nurse’s responsibility to provide sponge bath and change of clothes to reduce discomfort due to sweating.
- It is helpful to check for signs of pressure ulcers in long-term bed rest cases.
- It is necessary to offer back care and mouth care frequently to maintain hygiene and improve comfort.
5. Medication Administration and Observation
- It is essential to administer antipyretics only at safe intervals, avoiding overdosage (e.g., paracetamol max 4g/day).
- It is the nurse’s duty to check for history of drug allergy before giving antibiotics or NSAIDs.
- It is important to observe therapeutic response after 30–60 minutes of medication administration.
- It is necessary to prepare emergency drugs like antihistamines or epinephrine in case of anaphylaxis.
- It is helpful to observe stools, urine, and general appearance, especially in cases of systemic infections like typhoid.
6. Reporting and Documentation
- It is necessary to report any spike over 103°F (39.4°C) or febrile seizures immediately to the physician.
- It is important to document time and type of all interventions, including physical cooling and drug administration.
- It is the nurse’s duty to record symptoms such as rash, pallor, confusion, or rigors with time and action taken.
- It is helpful to document intake/output chart and calculate fluid balance for evaluation.
- It is also necessary to ensure communication with the infection control team if infection is suspected to be contagious.
7. Health Education and Psychological Support
- It is the nurse’s role to educate the patient and family on importance of continuing medications even after fever reduces.
- It is important to reassure the patient that fever is often a natural body response to infection, reducing unnecessary panic.
- It is necessary to instruct caregivers to observe and report any unusual symptoms at home if the patient is discharged.
- It is helpful to guide on home management of fever such as cold compress, tepid sponge, and fluid intake.
- It is also important to respect cultural and personal beliefs related to fever and healing, while educating scientifically.
Section 2
Q.4 Nursing as a profession explain (10)
Nursing is not just a job but a recognized, scientific, and ethical profession that focuses on the care of individuals, families, and communities to achieve, maintain, or recover optimal health and quality of life. It is a noble calling rooted in compassion, knowledge, skills, and lifelong service to humanity. The foundation of nursing is built on professional education, scientific knowledge, ethical standards, clinical skills, and interpersonal relationships.
✅ 1. It is a Humanitarian and Caring Profession
- It emphasizes compassionate care, respecting the dignity and rights of every individual.
- It is built on the principles of empathy, patience, and human connection.
- It serves vulnerable populations such as the elderly, terminally ill, and mentally challenged with dedicated support.
- Nurses provide emotional and spiritual comfort alongside physical care.
- It helps promote healing through presence, listening, and empathy.
✅ 2. It Requires Formal Education and Scientific Knowledge
- Nursing education includes both theoretical instruction and practical training in clinical settings.
- The curriculum follows standards set by Indian Nursing Council (INC) and includes community health, mental health, medical-surgical, and pediatric nursing.
- Advanced degrees such as M.Sc. Nursing, Nurse Practitioner (NP), and PhD provide opportunities for specialization.
- Continuous in-service education ensures updated knowledge on diseases, technology, and treatment protocols.
- Digital learning and simulations are being integrated into modern nursing education.
✅ 3. It Has a Well-defined Body of Knowledge and Theory
- Nursing knowledge is derived from nursing theories, research, and health sciences.
- Theories such as Orem’s Self-Care Model, Roy’s Adaptation Model, and Nightingale’s Environment Theory guide nursing care.
- Evidence-based practice bridges research with real-world care delivery.
- Nursing knowledge also integrates psychosocial, cultural, and spiritual dimensions of health.
- This scientific foundation ensures critical thinking and effective decision-making in practice.
✅ 4. It is Governed by Code of Ethics and Legal Responsibility
- Nurses must follow ethical principles such as autonomy, justice, beneficence, and fidelity.
- The INC Code of Ethics ensures protection of patients’ rights and professional conduct.
- Nurses must maintain confidentiality, informed consent, and accurate documentation.
- Violation of ethical/legal standards may lead to disciplinary action or cancellation of license.
- Ethical dilemmas are common (e.g., end-of-life care, DNR), requiring nurses to apply ethical reasoning.
✅ 5. It Involves Critical Thinking and Clinical Judgement
- Nurses assess, diagnose, plan, implement, and evaluate care using the nursing process.
- They interpret data, prioritize needs, and modify interventions based on patient response.
- In emergencies, nurses make life-saving decisions (e.g., during CPR, stroke, seizures).
- Clinical judgement helps reduce errors, improves outcomes, and enhances safety.
- Nurses use technology (monitors, ventilators, EHR) along with judgment to plan care effectively.
✅ 6. It Provides Autonomy and Independent Practice
- Nurses perform independent functions like health assessment, patient teaching, and wound care.
- In primary health centers or rural settings, nurses may act as first contact healthcare providers.
- In ICU, OR, and emergency settings, nurses independently monitor and intervene based on protocols.
- Advanced practice nurses and Nurse Practitioners (NPs) in some countries prescribe medications and conduct procedures.
- Nurses advocate for patient rights and participate in policy-making through nursing councils.
✅ 7. It Encourages Lifelong Learning and Professional Growth
- Nurses are required to attend Continuing Nursing Education (CNE) sessions to maintain license renewal.
- They can specialize in critical care, oncology, psychiatry, neonatal, or community health.
- Professional bodies like TNAI (Trained Nurses Association of India) support growth and leadership.
- They contribute to nursing literature through research, journals, and case studies.
- Opportunities exist in teaching, administration, and international career pathways.
✅ 8. It is Interdisciplinary and Team-Oriented
- Nurses collaborate with physicians, therapists, pharmacists, social workers, and more.
- Effective teamwork improves patient care coordination, safety, and satisfaction.
- Nurses also supervise and mentor junior staff and students within clinical units.
- They play a leadership role in interdisciplinary rounds, care planning, and discharge coordination.
- They ensure communication flow between departments, patients, and families.
✅ 9. It Plays a Vital Role in Health Promotion and Community Service
- Nurses conduct health education on hygiene, breastfeeding, nutrition, and sanitation.
- They lead immunization drives, screening programs, and manage epidemic outbreaks.
- In school health programs, they provide vision checks, growth monitoring, and health talks.
- Community Health Nurses (CHNs) promote maternal and child care, family planning, and home-based care.
- They often serve as the only accessible health resource in remote areas.
✅ 10. It Offers Diverse Career Opportunities and Global Recognition
- Nurses can work in government hospitals, private hospitals, NGOs, armed forces, disaster teams, and abroad.
- Special roles include forensic nurse, legal nurse consultant, nurse informaticist, and flight nurse.
- Indian nurses are highly sought after globally for their discipline, skill, and patient care ethics.
- They are eligible to appear for exams like NCLEX (USA), HAAD (UAE), Prometric (Qatar, Saudi), and CRNE (Canada).
- Nursing also opens doors to leadership roles in hospital administration and healthcare policymaking.
Q.5 Give the scietific reason for the following actions (any four) (8 mark)
a) All metallic articles removed from the body before x ray examination
All metallic articles are removed from the body before an X-ray examination because metal can obstruct X-ray beams, leading to artifacts or shadows on the image. This can distort the results and interfere with accurate diagnosis by obscuring internal structures.
b) Fluid chart is essential for patient with edema.
A fluid chart is essential for a patient with edema because it helps monitor and manage fluid balance. Edema results from excess fluid accumulating in the tissues; by recording fluid intake and output, healthcare providers can detect positive fluid balance, indicating fluid retention, and adjust treatment accordingly to prevent worsening edema and related complications.
c) Propped up position is given to client with dyspnoea.
Propped-up position is given to a client with dyspnoea because it helps ease breathing by allowing the lungs to expand more fully. This position reduces pressure on the diaphragm, improves oxygen intake, and decreases the effort needed to breathe, providing comfort and relief from breathlessness.
d) Rubber Mackintosh should not be kept folded.
Rubber Mackintosh should not be kept folded because folding can cause cracks or permanent creases in the material. This damages the waterproof surface, reduces its durability, and may lead to leakage. Instead, it should be stored flat or rolled to maintain its flexibility and prolong its life.
e) Thumb should not be used for counting pulse.
The thumb should not be used to count pulse because it has its own strong pulse from the digital artery. When used to check someone else’s pulse, you might feel your own pulse instead of the other person’s, leading to an incorrect reading. To avoid this, the index and middle fingers should be used for accurate pulse detection.
Q.6 Write short notes (any four) (4×5=20)
a) Universal precautions
Universal precautions refer to a set of infection control practices used by healthcare workers to prevent transmission of blood-borne pathogens (such as HIV, HBV, HCV) during patient care.
These precautions assume that all blood and body fluids may be potentially infectious, regardless of the patient’s known diagnosis.
1. Use of Personal Protective Equipment (PPE)
- It is essential for healthcare workers to wear gloves, gowns, masks, goggles or face shields whenever contact with blood or body fluids is anticipated.
- It helps in creating a barrier between the healthcare provider and the infectious material.
2. Hand Hygiene
- It is necessary for nurses to wash hands thoroughly with soap and water or use alcohol-based hand rub before and after patient contact.
- Hand hygiene must be performed before wearing and after removing gloves to prevent cross-infection.
3. Safe Handling and Disposal of Needles & Sharps
- It is important to never recap used needles and always dispose them in puncture-proof, labeled sharps containers.
- It is the nurse’s responsibility to ensure safe disposal of all sharp instruments to avoid needle-stick injuries.
4. Proper Handling of Blood and Body Fluids
- It is necessary to treat all blood, semen, vaginal secretions, CSF, pleural, pericardial, peritoneal, and amniotic fluids as potentially infectious.
- It is important to avoid direct contact with these fluids through broken skin or mucous membranes.
5. Environmental Cleaning and Surface Disinfection
- It is essential to disinfect all contaminated surfaces and equipment with appropriate solutions such as 1% sodium hypochlorite.
- It helps in preventing indirect transmission from inanimate objects.
6. Linen and Laundry Handling
- It is the nurse’s duty to handle soiled linen with gloves, and transport it in leak-proof bags to avoid contamination.
- It is important to never shake or agitate dirty linen, which could release infectious particles into the air.
7. Wound Care and Exposure Precautions
- It is important to cover cuts, wounds, and abrasions on hands or arms with waterproof dressings before attending patients.
- It prevents the entry of infectious agents through broken skin.
8. Biomedical Waste Management
- It is the nurse’s responsibility to ensure that all medical waste is segregated at the source and disposed of as per biomedical waste rules.
- Color-coded bins and proper labeling must be followed.
9. Education and Training of Healthcare Workers
- It is essential for the nurse to undergo regular training programs on standard precautions and infection control measures.
- It helps in updating knowledge and reducing occupational risks.
10. Reporting of Exposure Incidents
- It is important to immediately report any needle-stick injury or exposure to blood/body fluids to the infection control team.
- Post-exposure prophylaxis (PEP) must be initiated as per protocol.
11. Application in All Settings
- It is the duty of the nurse to follow universal precautions with every patient, regardless of diagnosis or infection status.
- It emphasizes the principle of universal application to protect both healthcare workers and patients.
b) Preoperative care
Preoperative care refers to the nursing and medical care given before a surgical procedure to prepare the patient physically, emotionally, and mentally for surgery. It includes assessment, education, physical preparation, and psychological support to reduce surgical risks and enhance recovery.
1. Physical Preparation of the Patient
- It is necessary to ensure the patient has completed fasting (NPO) status as per doctor’s instruction (usually 6–8 hours before surgery).
- It is important to clean the surgical area by shaving or clipping hair and giving antiseptic bath if required.
- It is the nurse’s responsibility to remove dentures, nail polish, jewelry, spectacles, contact lenses, and makeup to prevent complications.
- It is essential to check and record vital signs (BP, pulse, temperature, respiration) as baseline data before shifting to OT.
- It is required to ensure the bowel and bladder are emptied prior to surgery (e.g., enema or catheterization as prescribed).
- It is also necessary to administer preoperative medications such as sedatives, antibiotics, or antiemetics as per doctor’s orders.
- It is important to confirm that the patient is wearing identification tag and allergy band before sending to the operating room.
2. Psychological Preparation of the Patient
- It is the nurse’s role to assess the patient’s emotional status, anxiety, or fear related to surgery.
- It is important to provide reassurance and clear explanations regarding the surgical procedure, anesthesia, and postoperative care.
- It is necessary to encourage the patient to ask questions and clarify doubts to reduce stress.
- It is helpful to allow family presence before surgery to provide emotional comfort and reduce apprehension.
- It is essential to build trust and confidence by maintaining a calm, supportive, and professional demeanor.
3. Legal and Ethical Preparation
- It is the nurse’s responsibility to ensure that the informed written consent has been obtained and signed before surgery.
- It is important to verify patient identity and surgical site as per hospital safety protocols (e.g., surgical site marking).
- It is necessary to review medical and surgical history, allergies, previous reactions to anesthesia, and current medications.
- It is essential to record any prosthesis, pacemakers, or implants present in the patient’s body.
4. Nutritional and Metabolic Considerations
- It is required to assess the nutritional status and hydration level of the patient before surgery.
- It is important to provide IV fluids if oral intake is restricted for long duration.
- It is necessary to monitor blood glucose levels in diabetic patients and ensure insulin or hypoglycemic medications are adjusted.
- It is the nurse’s role to inform the surgeon and anesthetist if there is dehydration, anemia, or electrolyte imbalance.
5. Teaching and Education Before Surgery
- It is the nurse’s responsibility to educate the patient about breathing exercises, coughing technique, and early ambulation.
- It is important to teach the patient about postoperative pain management and use of devices like PCA pumps.
- It is essential to explain the use of surgical drains, catheters, oxygen therapy, or IV lines that may be used after surgery.
- It is helpful to inform the patient about expected length of hospital stay and recovery process.
6. Nursing Responsibilities Before Surgery
- It is important to check for completed preoperative investigations like CBC, blood group, chest X-ray, ECG, etc.
- It is the nurse’s duty to communicate any abnormal findings to the surgeon or anesthetist immediately.
- It is necessary to maintain privacy and confidentiality during preoperative assessments.
- It is the nurse’s duty to ensure that the patient chart, consent form, investigation reports, and ID tags are complete before sending to OT.
c) Glasgow coma scale
Definition
- It is a standardized neurological scoring system designed to objectively measure the level of consciousness in patients with altered mental status, especially in head injury or coma.
- It was first developed in 1974 by Professors Graham Teasdale and Bryan Jennett at the University of Glasgow, hence the name Glasgow Coma Scale.
- It is a clinical tool used widely by nurses, emergency personnel, and neurologists to monitor and record the severity and progression of a coma.
Purpose of the Glasgow Coma Scale
- It is used to evaluate the neurological status and consciousness level in patients after trauma, stroke, or other brain injuries.
- It helps guide medical and nursing decisions such as whether airway protection, ICU monitoring, or neurosurgical referral is needed.
- It allows tracking of changes in consciousness over time and supports clinical judgment in both acute and chronic neurological conditions.
- It is especially useful in emergency, neuro ICU, and postoperative neurosurgical settings to detect early deterioration.
Components of GCS
1️⃣ Eye Opening Response (E) – Maximum Score: 4
| Score | Description |
|---|---|
| 4 | It is scored 4 when the patient opens eyes spontaneously without any external stimulus. |
| 3 | It is scored 3 when the patient opens eyes only when spoken to (on verbal command). |
| 2 | It is scored 2 when the patient opens eyes only in response to painful stimulus (like trapezius pinch or sternal rub). |
| 1 | It is scored 1 when the patient does not open eyes to any kind of stimulus (unresponsive). |
2️⃣ Verbal Response (V) – Maximum Score: 5
| Score | Description |
|---|---|
| 5 | It is scored 5 when the patient is alert, oriented, and speaks coherently with correct answers about name, place, and time. |
| 4 | It is scored 4 when the patient is confused but can still speak in complete sentences and respond with meaningful words. |
| 3 | It is scored 3 when the patient speaks with inappropriate words that make no contextual sense. |
| 2 | It is scored 2 when the patient makes only incomprehensible sounds like moaning or groaning without forming words. |
| 1 | It is scored 1 when the patient gives no verbal response at all. |
3️⃣ Motor Response (M) – Maximum Score: 6
| Score | Description |
|---|---|
| 6 | It is scored 6 when the patient obeys motor commands like “show me two fingers” or “move your hand.” |
| 5 | It is scored 5 when the patient purposefully localizes pain (e.g., tries to remove a painful stimulus like a nail bed pressure). |
| 4 | It is scored 4 when the patient withdraws from painful stimulus (pulls limb away reflexively). |
| 3 | It is scored 3 when the patient shows abnormal flexion to pain (decorticate posture: arms bent, legs extended). |
| 2 | It is scored 2 when the patient shows abnormal extension to pain (decerebrate posture: arms extended, wrists flexed, legs stiff). |
| 1 | It is scored 1 when there is no motor response even to painful stimuli. |
Total GCS Score = Eye (4) + Verbal (5) + Motor (6) = 3 to 15
Minimum possible score : 3 (deep coma or death-like unresponsive state).
Maximum possible score : 15 (normal, fully awake and alert state).
Interpretation of Scores
Total GCS Score Level of Brain Injury
- 13 – 15 It indicates mild brain injury or alert consciousness.
- 9 – 12 It indicates moderate brain injury and requires monitoring.
- ≤ 8 It indicates severe brain injury or coma, and immediate ICU admission or intubation may be required.
Importance in Nursing Practice
- It is essential for the nurse to accurately assess and record GCS scores at regular intervals, especially after trauma or neurosurgery.
- It is important to establish a baseline GCS and monitor for any decrease in score, which may indicate neurological worsening.
- It is necessary to use a painful stimulus like trapezius squeeze or nail bed pressure if the patient is not responding verbally.
- It is crucial for the nurse to notify the physician or neurologist immediately if GCS drops by 2 or more points.
- It is vital to recheck GCS after giving sedatives or anticonvulsants, as medications can alter the score.
- It is the nurse’s responsibility to manage airway, oxygen, and suction if GCS is ≤ 8 to prevent hypoxia.
- It is essential to use the same scale for continuity of care and documentation to avoid inter-observer variation.
- It is helpful to educate patient families about the meaning of GCS score and its implications for recovery.
d) Nurses responsibility in administration of oral medicine
Oral route is the most common and safest method of drug administration. The nurse plays a vital role in ensuring safe, accurate, and effective administration of oral medicines. The responsibilities are grouped as before, during, and after administration.
1. Responsibilities Before Administration
- It is the nurse’s responsibility to verify the physician’s order for the right drug, dose, route, time, and patient.
- It is essential for the nurse to check the “Five Rights” of medication administration: right patient, right drug, right dose, right time, and right route.
- It is the duty of the nurse to identify the patient properly using two identifiers like name and hospital ID band.
- It is important to check the patient’s allergy history and ensure that the drug is not contraindicated.
- It is necessary to assess the patient’s ability to swallow safely and check for nausea, vomiting, or reduced consciousness.
- It is required for the nurse to prepare the correct dose using a clean medication cup or spoon and avoid touching pills with bare hands.
- It is important to wash hands and maintain aseptic technique to prevent contamination.
- It is also necessary to check the expiration date and integrity of the medication packaging before use.
2. Responsibilities During Administration
- It is the nurse’s duty to explain the medication name, purpose, and side effects to the patient before giving the drug.
- It is important to offer the drug with a glass of water, unless otherwise restricted (e.g., NPO or fluid restrictions).
- It is essential to remain with the patient until the medication is swallowed completely.
- It is the nurse’s responsibility to never leave medications unattended or at the patient’s bedside.
- It is crucial to observe the patient’s willingness and understanding, especially in pediatric or elderly patients.
3. Responsibilities After Administration
- It is the nurse’s duty to document the time, dose, and name of the drug administered in the patient’s medication record.
- It is essential to monitor the patient for therapeutic effect and any adverse reaction after drug administration.
- It is required to report and record any side effects, allergic reaction, or refusal of medicine immediately.
- It is important for the nurse to educate the patient about any specific instructions, such as taking the drug before meals, avoiding alcohol, or drug-food interactions.
- It is the nurse’s role to ensure safe disposal of empty wrappers, medicine cups, or spoons used during administration.
e) Types of diet served in the hospital
Hospital diets are specially planned to meet the nutritional needs of patients based on their medical condition, ability to digest and absorb nutrients, and therapeutic requirements. These diets are classified as follows:
Regular/Normal Diet
- It is a balanced diet that contains all essential nutrients in adequate quantity.
- It is served to patients who do not have any specific dietary restrictions.
- It includes all food groups such as cereals, pulses, vegetables, fruits, dairy, and meats.
- It is useful for maintaining health and meeting general nutritional needs during recovery.
Clear Liquid Diet
- It is composed of transparent fluids that leave no residue in the intestine.
- It includes clear soups, tea, black coffee, apple juice, gelatin, and glucose water.
- It is given to patients before and after surgery or during acute gastrointestinal illness.
- It helps to maintain hydration and provide minimal energy without stressing the digestive system.
Full Liquid Diet
- It includes both clear liquids and opaque fluids such as milk, custards, and strained soups.
- It is suitable for patients who cannot chew or digest solid food.
- It helps in transitioning from clear liquid to soft diet in post-operative or oral/throat surgery cases.
- It provides more nutrients than a clear liquid diet and is easy to digest.
Soft Diet
- It includes soft-textured, easily digestible foods like porridge, mashed potatoes, eggs, cooked vegetables, and soft fruits.
- It is prescribed for patients with dental issues, GI problems, or post-operative recovery.
- It avoids foods that are hard, spicy, fried, or high in fiber.
- It helps in gradual progression from liquid to normal food while reducing digestive strain.
Bland Diet
- It includes non-irritating, low-fat, low-spice, and low-fiber foods.
- It is recommended for patients with ulcers, gastritis, or peptic acid disorders.
- It includes white rice, milk, boiled potatoes, and bananas.
- It minimizes gastric stimulation and aids healing of the digestive tract.
High-Protein Diet
- It includes protein-rich foods such as eggs, milk, pulses, meat, and protein supplements.
- It is given to patients with burns, trauma, infection, post-surgery, or protein deficiency.
- It promotes wound healing, tissue repair, and immune function.
- It is essential for patients with muscle wasting or malnutrition.
Low-Protein Diet
- It limits intake of protein-rich foods like meat, eggs, and dairy.
- It is prescribed for patients with renal failure or severe liver disease.
- It reduces the formation of nitrogenous waste products.
- It helps in reducing the workload on kidneys and prevents complications.
Low-Fat/Cholesterol Diet
- It restricts foods high in saturated fats and cholesterol like fried foods, butter, and red meat.
- It is indicated in patients with heart disease, obesity, or gallbladder disorders.
- It focuses on lean protein, fruits, vegetables, and whole grains.
- It helps in weight control and cardiovascular health.
Diabetic Diet
- It is planned to control blood sugar levels by limiting refined carbs and sugars.
- It includes complex carbohydrates, fiber-rich foods, and controlled fat intake.
- It involves frequent small meals with portion control.
- It is essential for diabetic patients to manage insulin and blood glucose levels.
Renal Diet
- It restricts sodium, potassium, phosphorus, and protein depending on kidney function.
- It includes special guidelines for fluid intake and food selection.
- It is important for patients on dialysis or with chronic kidney disease.
- It prevents fluid overload, hyperkalemia, and metabolic complications.
Low-Sodium Diet
- It avoids added salt and high-sodium processed foods.
- It is given to patients with hypertension, edema, or cardiac and renal diseases.
- It helps in controlling blood pressure and reducing fluid retention.
- It uses herbs and natural flavoring instead of salt.
High-Calorie Diet
- It provides extra calories through carbohydrate and fat-rich foods.
- It is indicated for patients with malnutrition, TB, cancer, and chronic infections.
- It includes frequent, energy-dense meals and snacks.
- It supports weight gain and provides energy for recovery.
Low-Calorie Diet
- It is used for weight loss and management of obesity and metabolic syndrome.
- It limits intake of sugars, fats, and high-calorie foods.
- It is balanced with adequate nutrients but lower total caloric intake.
- It supports healthy weight control and reduces disease risks.
Fiber-Rich Diet
- It is rich in dietary fiber from whole grains, fruits, vegetables, and legumes.
- It is beneficial in constipation, irritable bowel syndrome, and lowering cholesterol.
- It improves bowel movement and digestive health.
- It helps in maintaining satiety and glucose control.
Fiber-Restricted Diet
- It limits raw fruits, vegetables, seeds, and whole grains.
- It is used in conditions like inflammatory bowel disease, diarrhea, or post-GI surgery.
- It reduces irritation in the intestines and aids healing.
- It includes soft, cooked, and low-residue foods.
