30/08/2018-B.SC-NUTRI & BIOCHEM PAPER-UPLOAD NO.08
PAPER SOLUTION NO.08-30/08/2018
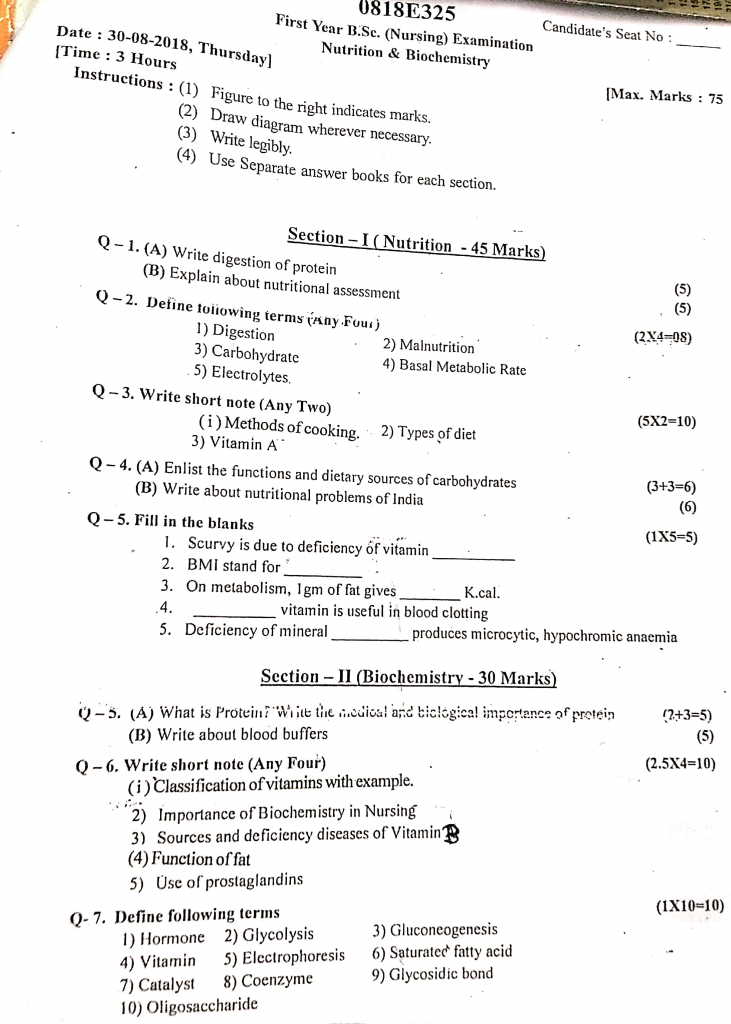
Section 1 (Nutrition 45 marks)
Q.1
A) Write the digestion of protein (5)
Protein digestion is a complex biochemical process in which dietary proteins are broken down into smaller peptides and amino acids by the action of specific enzymes in the gastrointestinal tract. These end products are then absorbed and utilized by the body for tissue repair, growth, hormone synthesis, and enzyme production.
1️⃣ Digestion Begins in the Stomach (Gastric Phase)
- Protein digestion does not begin in the mouth, as there are no proteolytic enzymes in saliva.
- In the stomach, the acidic environment (pH 1.5–3.5) created by hydrochloric acid (HCl) plays a crucial role in denaturing the protein structure, making it more accessible to enzymes.
- HCl also converts the inactive enzyme pepsinogen (secreted by chief cells) into its active form, pepsin.
- Pepsin is the main enzyme that begins breaking down large protein molecules into smaller polypeptides and proteoses through hydrolysis of peptide bonds.
- The stomach churning action helps to mechanically mix the food with gastric juice, forming a semi-liquid mass called chyme, which is then pushed into the small intestine for further digestion.
2️⃣ Digestion in the Small Intestine (Intestinal and Pancreatic Phase)
- When chyme enters the duodenum, the acidic environment stimulates the release of secretin and cholecystokinin (CCK) hormones from the intestinal mucosa.
- These hormones trigger the pancreas to release pancreatic juice, which contains several inactive proteolytic enzymes including trypsinogen, chymotrypsinogen, and procarboxypeptidase.
- The enzyme enterokinase (or enteropeptidase), present in the duodenal lining, activates trypsinogen to trypsin, which then activates chymotrypsin and carboxypeptidase.
- Trypsin and chymotrypsin further hydrolyze polypeptides into tripeptides, dipeptides, and small peptides.
- Carboxypeptidase breaks the peptide bonds at the carboxyl end of the protein chain, releasing individual amino acids.
- The partially digested proteins continue to move through the jejunum and ileum, where digestion completes.
3️⃣ Final Digestion at the Intestinal Wall (Brush Border Phase)
- The intestinal mucosal cells of the small intestine (brush border) secrete additional enzymes such as aminopeptidase and dipeptidase.
- Aminopeptidase cleaves peptide bonds from the amino terminal end, releasing more amino acids.
- Dipeptidase acts specifically on dipeptides, breaking them into two free amino acids.
- This final enzymatic breakdown ensures that proteins are fully converted into absorbable units (free amino acids, dipeptides, tripeptides).
4️⃣ Absorption of Amino Acids
- The resulting amino acids, dipeptides, and tripeptides are absorbed through the epithelial lining of the small intestine, primarily in the jejunum.
- Active transport mechanisms, aided by sodium-dependent carriers, are responsible for moving amino acids into the intestinal mucosal cells.
- Inside the enterocytes, dipeptides and tripeptides are further broken down into individual amino acids, which then enter the portal vein and are transported to the liver.
- The liver acts as the primary center for amino acid metabolism, where they are either stored, used for protein synthesis, or converted to other compounds like glucose or urea.
5️⃣ Role of Protein After Digestion
- The absorbed amino acids are utilized in the body for tissue repair, muscle growth, enzyme formation, hormone synthesis, antibody production, and maintaining nitrogen balance.
- Excess amino acids are not stored; instead, they are deaminated in the liver and their nitrogen is excreted as urea via the kidneys.
- The carbon skeletons may be used for energy production or converted into glucose or fat, depending on body needs.
B) Explain about nutritional assessment (5)
Definition
- Nutritional assessment is a systematic and scientific approach used to evaluate the nutritional status of an individual or population by analyzing data related to diet, body measurements, biochemical markers, and clinical signs.
- It is also a process used in clinical and community settings to detect malnutrition, plan dietary interventions, and monitor nutritional improvements.
Objectives of Nutritional Assessment
- It is conducted to identify the presence of nutrient deficiencies or excesses and their impact on health status.
- It is done to screen individuals or groups who are at nutritional risk, such as low-birth-weight babies, elderly, or hospitalized patients.
- It helps to plan and implement individualized nutrition care plans based on scientific evaluation.
- It serves as a tool to evaluate the success of dietary or therapeutic interventions over time.
- It helps to create baseline data for public health nutrition programs and disease prevention policies.
- It is also useful for educating patients and caregivers about proper nutrition, diet, and health behavior changes.
Types of Nutritional Assessment (ABCD + E)
🅰️ A – Anthropometric Measurements
- It includes physical measurements such as weight, height, BMI, waist-hip ratio, and MUAC to assess growth and body composition.
- These measurements are compared with standard growth charts or WHO reference values to detect undernutrition, overnutrition, or stunting.
- It is useful for monitoring growth trends in children and tracking weight loss or gain in adults during treatment.
- It also helps in classifying malnutrition types such as wasting, stunting, and obesity.
🅱️ B – Biochemical Assessment
- It includes laboratory evaluation of nutrients or metabolites in blood, urine, saliva, or stool samples.
- It helps to assess micronutrient levels such as Vitamin D, B12, folate, iron, calcium, and electrolyte balance.
- It is especially useful in diagnosing subclinical or hidden deficiencies, where no physical symptoms are visible.
- It supports medical diagnosis of anemia, protein deficiency, metabolic disorders, and renal or liver dysfunction.
🅲️ C – Clinical Assessment
- It involves systematic examination of the body to identify signs and symptoms of nutrient deficiencies or health conditions related to poor nutrition.
- Common signs include pale skin, hair loss, bleeding gums, cracked lips, swollen tongue, edema, or spoon-shaped nails.
- It is quick, non-invasive, and often used in rural and community settings by health workers for screening.
- It is also important for identifying secondary signs of systemic diseases such as protein-energy malnutrition or scurvy.
🅳️ D – Dietary Assessment
- It includes evaluation of daily food intake, nutrient patterns, food preferences, meal frequency, and portion sizes.
- Common tools include 24-hour dietary recall, 3-day food record, food frequency questionnaire, and diet history interview.
- It helps to assess the adequacy, balance, and diversity of an individual’s diet in relation to nutritional requirements.
- It identifies barriers to healthy eating, such as low income, poor appetite, cultural restrictions, or lack of nutrition knowledge.
🅴️ E – Environmental and Socioeconomic Assessment
- It considers the influence of income, education, occupation, food availability, sanitation, and housing conditions on nutrition.
- It helps to understand why malnutrition exists despite dietary adequacy due to poor hygiene, unsafe water, or economic challenges.
- It is essential for planning community-based nutritional interventions and welfare programs like ICDS or PDS.
- It also identifies at-risk populations like slum dwellers, migrants, or tribal communities who require targeted nutritional support.
Nursing Responsibilities in Nutritional Assessment
- The nurse is responsible for measuring and recording accurate anthropometric data using standardized equipment like weighing scales and measuring tapes.
- Nurse plays a key role in detecting early signs of malnutrition or nutrient deficiencies during clinical rounds or health camps.
- Nurse is trained to collect dietary information through structured interviews, recall techniques, or food diaries.
- Nurse must educate the patient and family on the importance of balanced diet, food hygiene, and timely supplementation.
- Nurse participates in screening programs for child growth, maternal nutrition, elderly care, and chronic illness like diabetes or renal disorders.
- Nurse also assists in follow-up and documentation of patient nutritional status and responses to dietary interventions.
Q.2 Define following terms (any four) (2×4=8)
1) Digestion
Digestion is the complex physiological process in which large, insoluble food molecules are broken down into smaller, soluble molecules with the help of enzymes, mechanical movements, and digestive juices, so that they can be absorbed and utilized by the body for energy, growth, and repair.
2) Malnutrition
Malnutrition is a condition that results from an imbalance between the body’s nutritional needs and the intake, absorption, or utilization of nutrients, leading to undernutrition, overnutrition, or nutrient deficiencies, which adversely affect health, growth, and bodily functions.
3) Carbohydrate
Carbohydrates are organic compounds made up of carbon, hydrogen, and oxygen, which serve as the body’s primary and most immediate source of energy, providing 4 kilocalories per gram, and are found mainly in plant-based foods such as cereals, fruits, vegetables, and sugars.
4) Basal metabolic rate
Basal Metabolic Rate (BMR) is the minimum amount of energy required by the body to carry out essential physiological functions such as breathing, circulation, cell metabolism, and temperature regulation while at complete physical and mental rest, in a post-absorptive state, and in a thermoneutral environment.
5) Electrolytes
Electrolytes are chemical substances that, when dissolved in water or body fluids, dissociate into electrically charged particles called ions, which help in maintaining fluid balance, acid-base equilibrium, nerve impulse transmission, and muscle contraction.
Q.3 Write short notes (any two) (5×2=10)
1) Method of cooking
Cooking is the process by which food is prepared using various forms of heat. Each cooking method affects the taste, texture, digestibility, and nutritional value of food. The methods are broadly divided into Moist Heat, Dry Heat, Frying, and Microwave or Modern methods.
1️⃣ MOIST HEAT METHODS
(These involve cooking food using water, steam, or other liquids.)
✅ Boiling
- It is a method in which food is completely immersed in water and heated to its boiling point (100°C), allowing it to cook until soft or tender.
- It is one of the simplest and oldest cooking methods, suitable for rice, lentils, eggs, vegetables, and pasta.
- It helps in destroying most pathogenic organisms, thus making food safe for consumption.
- It is often used in therapeutic and bland diets, especially in patients with gastrointestinal conditions.
- However, it may lead to loss of water-soluble nutrients like Vitamin C and B-complex unless the cooking water is reused.
- Overboiling can make food mushy and less appealing, and it should be avoided.
- Boiling is also helpful in softening fibrous food materials, making them digestible for infants and elderly.
✅ Simmering
- It is a gentle cooking method where food is cooked just below boiling point (85–95°C) for an extended time.
- It produces small, gentle bubbles that allow slow and even cooking, ideal for broths, dals, meat stews, and soups.
- Simmering helps in better flavor extraction, especially when cooking meat or bones for broth.
- It maintains the structural integrity of food, unlike boiling, which may break it down.
- It is widely used in hospital diets for preparing light, nourishing meals.
- It ensures thorough cooking of complex ingredients without overcooking delicate ones.
✅ Steaming
- Steaming is a process in which food is cooked by the heat of steam rather than by water itself, preserving most nutrients.
- It is considered the healthiest cooking method, as it does not require oil or direct heat.
- It is ideal for preparing idli, dhokla, vegetables, momos, and fish, especially in therapeutic diets.
- Steaming helps in preserving color, taste, and texture, especially of green vegetables and fruits.
- It reduces the risk of nutrient loss, particularly water-soluble vitamins, which are easily leached during boiling.
- It is highly suitable for dietary modifications in hypertension, diabetes, and cardiovascular diseases.
- Steam cookers, pressure cookers, or bamboo baskets may be used for this purpose.
✅ Poaching
- Poaching involves cooking food gently in liquid at temperatures ranging from 70°C to 80°C, below boiling point.
- This method is ideal for eggs, fish, pears, and apples, which are delicate and can break with vigorous boiling.
- It is a preferred cooking method in renal and cardiac diets, as it allows food to retain moisture without added fats.
- Poaching retains natural flavors and helps keep the food soft, moist, and nutrient-rich.
- It is often used with flavored liquids (like broth, milk, or fruit juice) to enhance the final dish.
- It ensures food is cooked without the formation of a crust, which is beneficial in texture-sensitive patients.
2️⃣ DRY HEAT METHODS
(These methods cook food without the use of water, using hot air or direct heat.)
✅ Roasting
- Roasting is a method of cooking food using dry heat, either in an oven or over an open flame.
- It is widely used for nuts, root vegetables, meats, paneer, and eggplant to enhance taste and aroma.
- Roasting helps develop a brown crust and smoky flavor, which enhances palatability.
- It results in moisture reduction, making the food crispy and shelf-stable.
- Frequent turning and temperature control are necessary to prevent burning or uneven roasting.
- It is particularly useful in reducing fat content by allowing excess oil to drip off.
- However, excessive roasting may lead to nutrient degradation, especially of sensitive vitamins.
✅ Baking
- Baking involves cooking food in dry, hot air inside a closed oven, generally at temperatures between 160–250°C.
- It is used for bread, cakes, cookies, pies, lasagna, and baked snacks.
- Baking is suitable for low-oil or oil-free diets, making it heart-healthy.
- It creates uniform cooking with a golden crust while keeping the inside soft and moist.
- It is important to preheat the oven and avoid overbaking, which may dry out the food.
- Baking is used in clinical nutrition to prepare special diet foods for diabetics, cardiac patients, or obese individuals.
✅ Grilling
- Grilling is a method of cooking food over direct heat, usually from below (as in charcoal or electric grills).
- It is widely used for vegetables, meats, kebabs, fish, and paneer.
- It creates a charred and crispy outer layer while retaining juices inside.
- Grilled food has a distinct smoky flavor, and it requires minimal oil, making it healthy.
- It is necessary to marinate food beforehand to enhance taste and retain moisture during high-heat exposure.
- Prolonged or high-temperature grilling may lead to charring, which can produce harmful compounds if not controlled.
✅ Toasting
- Toasting involves browning food items using dry heat without oil, typically applied to bread, nuts, and spices.
- It is done using toasters, ovens, or open flame.
- Toasting helps remove moisture, making food crispy and improving shelf life.
- It is widely used in breakfast items and for preparing bases for sandwiches or croutons.
- Care must be taken to avoid over-toasting, which may lead to bitterness or burning.
3️⃣ FRYING METHODS
(These methods cook food by immersing or contacting it with hot oil.)
✅ Deep Frying
- Deep frying involves completely submerging food in hot oil at 170–190°C until it becomes golden and crispy.
- It is used for making pakoras, puris, samosas, cutlets, and snacks.
- It enhances taste, texture, and color, making food attractive and palatable.
- However, it is a high-calorie method and unsuitable for therapeutic diets.
- Frequent reuse of oil can lead to oxidation and toxin formation, so oil must be used judiciously.
- Deep-fried food should be drained well on tissue or mesh to reduce excess oil before serving.
✅ Shallow Frying
- Shallow frying uses a small amount of oil in a flat pan to cook food on both sides.
- It is suitable for parathas, dosas, cutlets, omelets, and fish fillets.
- This method requires medium heat and frequent turning for even cooking.
- It uses less oil compared to deep frying and is more suitable for regular diets.
- However, nutrient loss and calorie addition still occur if not carefully monitored.
✅ Sauteing
- Sauteing is a quick cooking method where small pieces of food are stirred or tossed in a small amount of fat over high heat.
- It is widely used for vegetables, paneer, chicken cubes, onions, and spices at the beginning of many dishes.
- It retains crunch, color, and nutrients while enhancing flavor due to caramelization.
- Sauteing is commonly used in Indian curries and continental side dishes.
- It requires constant movement to prevent sticking or burning.
4️⃣ COMBINATION METHOD
✅ Braising
- Braising combines both dry and moist heat methods, where food is first browned by dry heat and then cooked in a small amount of liquid.
- It is used for tough cuts of meat, root vegetables, and stuffed dishes that need slow, gentle cooking.
- The initial browning adds rich color and flavor, while the later liquid phase makes it tender and moist.
- It is ideal for hospital bulk cooking or nutritional meals that must be soft and wholesome.
- It is a time-consuming method but yields rich, concentrated flavors.
5️⃣ MICROWAVE COOKING
- Microwave cooking uses electromagnetic waves to generate heat by vibrating water molecules within food.
- It is a modern, fast, and energy-efficient method suitable for reheating or cooking soft-textured food.
- It is used for vegetables, fish, reheated chapatis, porridges, or baby food.
- Microwaving helps retain most nutrients because of short cooking time and minimal water use.
- It is not ideal for frying, browning, or dry crisp textures, which need conventional ovens or grilling.
2) Types of diet
- A diet refers to the sum of food consumed by a person regularly, and it can be modified depending on the person’s age, activity level, health status, medical condition, and therapeutic needs.
- In hospital and clinical settings, diets are prescribed by doctors and dietitians to promote recovery, support nutritional status, and prevent complications.
Types of Diet (Based on Purpose and Consistency)
1️⃣ Regular or Normal Diet
- It is a well-balanced diet that provides all essential nutrients in appropriate quantities to maintain health.
- It is given to healthy individuals without any specific dietary restrictions.
- Includes carbohydrates, proteins, fats, vitamins, and minerals from all food groups.
- Suitable for general hospital patients who do not require dietary modifications.
2️⃣ Soft Diet
- This diet includes easily digestible, soft-textured, and lightly seasoned foods, often given after surgery or to patients with chewing difficulties.
- Foods are usually boiled, steamed, mashed, or pureed.
- It excludes spicy, fried, and fibrous foods.
- Used in conditions such as gastrointestinal disturbances, dental issues, or post-operative recovery.
3️⃣ Clear Liquid Diet
- Consists of transparent, liquid foods that leave no residue in the intestinal tract.
- Includes clear broth, plain tea, apple juice, gelatin, glucose water, and coconut water.
- It is prescribed for acute illness, vomiting, diarrhea, or before diagnostic tests like endoscopy.
- It is usually given for short durations (24–48 hours).
4️⃣ Full Liquid Diet
- This diet includes both clear and opaque liquids, such as milk, custard, cream soups, yogurt, fruit juices without pulp, and eggnog.
- It is used for patients who cannot chew or swallow solid food, such as those with oral surgery, severe weakness, or throat disorders.
- It provides more calories and nutrients than a clear liquid diet.
5️⃣ Bland Diet
- Composed of foods that are soft, low in fiber, mildly seasoned, and non-irritating to the digestive tract.
- Avoids spicy, acidic, fried, or high-fiber foods.
- Indicated in gastritis, ulcers, heartburn, or GI inflammation.
- Examples include porridge, mashed potatoes, boiled vegetables, milk, and white bread.
6️⃣ Therapeutic Diet
- Specifically planned to treat or manage medical conditions like diabetes, hypertension, kidney disease, and liver disorders.
- These diets are modified in nutrients (e.g., low salt, low fat, high protein) and must be prescribed by a physician or dietitian.
- Examples include low sodium diet for hypertension, renal diet for kidney disease, diabetic diet, etc.
7️⃣ High Protein Diet
- Designed to meet increased protein needs in burns, wounds, malnutrition, infections, or post-surgery recovery.
- Includes milk, eggs, meat, legumes, cheese, and protein supplements.
8️⃣ Low Calorie Diet
- Prescribed to promote weight loss in obese or overweight individuals.
- Includes foods that are low in fat and sugar, such as fruits, vegetables, lean meats, and whole grains.
- Often accompanied by exercise and lifestyle changes.
9️⃣ High Calorie Diet
- Recommended for malnourished individuals, cancer patients, tuberculosis patients, or those with increased metabolic needs.
- Includes energy-rich foods like butter, ghee, full cream milk, nuts, and sugary drinks.
1️⃣0️⃣ Low Fat Diet
- Contains reduced fat content, especially saturated fats and cholesterol.
- Prescribed in heart diseases, gallbladder problems, pancreatitis, and obesity.
- Encourages consumption of grilled or baked foods, and avoids fried, oily, and creamy items.
1️⃣1️⃣ Fibre-Rich Diet
- It Includes whole grains, fruits, vegetables, legumes, and bran to improve bowel movement and prevent constipation.
- It is Used in constipation, hemorrhoids, irritable bowel syndrome (IBS), and weight management.
3) Vitamin A
Vitamin A is a fat-soluble vitamin that plays a crucial role in maintaining normal vision, immune function, growth and development, and the health of epithelial tissues.
Forms of Vitamin A
- It is found in two major forms: Preformed Vitamin A (Retinol) from animal sources and Provitamin A (Beta-Carotene) from plant sources.
- Retinol is the active form that is stored in the liver, whereas beta-carotene is a precursor that the body converts into retinol.
Sources of Vitamin A
Animal Sources (Retinol)
- It is richly found in liver, fish liver oils (like cod liver oil), egg yolk, butter, ghee, and fortified milk.
- These are highly bioavailable sources and directly provide ready-to-use vitamin A in the form of retinol.
Plant Sources (Beta-Carotene)
- Green leafy vegetables such as spinach, amaranth, fenugreek leaves are rich in beta-carotene.
- Orange and yellow fruits and vegetables like carrots, mangoes, papaya, pumpkin, and sweet potatoes are excellent sources of provitamin A.
Functions of Vitamin A
- It is essential for the synthesis of rhodopsin in retina which is required for normal vision, especially night vision.
- It maintains the integrity and function of epithelial tissues in the skin, respiratory tract, gastrointestinal tract, and genitourinary tract.
- It plays an important role in boosting immunity by supporting white blood cell function.
- It promotes normal growth and development, especially in children, by helping in cell differentiation.
- It contributes to healthy hair, nails, and skin through its epithelial maintenance role.
- It has antioxidant properties (especially beta-carotene), which protect cells from oxidative damage.
Deficiency of Vitamin A
- It causes night blindness (nyctalopia), which is an early symptom of deficiency.
- Severe deficiency may lead to xerophthalmia, characterized by dryness of the conjunctiva and cornea.
- If untreated, it can cause Bitot’s spots, corneal ulcers, and eventually keratomalacia and blindness.
- It reduces immune response, making the body more susceptible to infections like measles, pneumonia, and diarrhea, especially in children.
- In children, deficiency may lead to growth retardation and delayed development.
Toxicity of Vitamin A (Hypervitaminosis A)
- Excess intake, especially of preformed vitamin A, can lead to toxicity symptoms such as nausea, vomiting, headache, dizziness, blurred vision.
- Chronic toxicity may cause liver damage, bone pain, and intracranial hypertension.
- In pregnancy, excess vitamin A intake may cause teratogenic effects leading to birth defects.
Recommended Dietary Allowance (RDA)
Adult women : 600 mcg/day Retinol Equivalent (RE)
Adult men : 700 mcg/day Retinol Equivalent (RE)
Children : 300–400 mcg/day RE, depending on age.
Pregnant and lactating women: 800–950 mcg/day RE, due to increased needs.
Nursing Responsibilities Related to Vitamin A
- Nurse must assess for clinical signs of deficiency such as night blindness, dry eyes, Bitot’s spots in at-risk populations like children and pregnant women.
- Nurse plays a key role in educating patients and caregivers about dietary sources of vitamin A and the importance of consuming a balanced diet.
- Nurse must ensure timely administration of prophylactic Vitamin A supplements, especially during national programs for child health (like at 9, 18, 24 months etc.).
- Nurse should observe for signs of toxicity if high-dose supplements are given, especially in pediatric and antenatal care.
- Nurse may be involved in nutrition surveillance programs, school health checkups, and growth monitoring where vitamin A deficiency is screened.
Q.4
A) Enlist the functions and dietary souuces of carbohydrates (3+3=6)
Functions of Carbohydrates
1️⃣ Carbohydrates serve as the primary and most immediate source of energy for all body cells, providing 4 kilocalories per gram, which supports muscle contraction, brain function, and body metabolism.
2️⃣ Carbohydrates help in protein sparing, which means that when the body gets enough carbohydrates, it does not break down proteins for energy, allowing proteins to be used for growth, repair, and enzyme production.
3️⃣ They regulate fat metabolism by ensuring that fats are burned efficiently; in the absence of carbohydrates, incomplete fat breakdown occurs, leading to the formation of harmful ketone bodies.
4️⃣ They maintain blood glucose levels by supplying glucose through digestion and absorption, which is especially important for the proper functioning of the brain and central nervous system, which rely primarily on glucose.
5️⃣ Carbohydrates contribute to dietary fiber, especially from sources like whole grains, fruits, and vegetables; fiber aids in digestion, prevents constipation, and promotes a healthy gut.
6️⃣ Carbohydrates help in synthesis of nucleic acids (DNA and RNA) by providing ribose and deoxyribose sugars, which are essential structural components of genetic material.
7️⃣ They enhance palatability and taste of food, as sugars and starches improve flavor, aroma, and texture of meals, increasing appetite and food enjoyment.
8️⃣ Carbohydrates play a role in cell recognition and immune function, as glycoproteins and glycolipids on cell surfaces are made from sugar molecules involved in immune responses and cellular communication.
Dietary Sources of Carbohydrates
1️⃣ Cereals such as rice, wheat, maize, barley, and oats are the richest sources of complex carbohydrates like starch, which provide sustained energy to the body.
2️⃣ Pulses and legumes including lentils, chickpeas, and beans contain moderate amounts of carbohydrates along with dietary fiber and protein, making them highly nutritious.
3️⃣ Root vegetables like potatoes, sweet potatoes, and yams are excellent sources of starch, which is a major form of carbohydrate stored in plants.
4️⃣ Fruits such as bananas, mangoes, grapes, apples, and papaya provide simple sugars like fructose and glucose, which are easily absorbed and quickly utilized by the body for energy.
5️⃣ Sugary foods such as table sugar (sucrose), jaggery, honey, and glucose powder provide concentrated forms of carbohydrates, but should be consumed in moderation to avoid health issues.
6️⃣ Milk and dairy products contain lactose, which is a natural milk sugar that provides a small but important portion of daily carbohydrate intake.
7️⃣ Vegetables like carrots, beets, corn, and peas also contribute to carbohydrate intake, especially in the form of starch and dietary fiber.
8️⃣ Bakery items, noodles, pasta, and other processed foods made from flour and cereals are major sources of refined carbohydrates in modern diets.
B) Write about the nutritional problem of india (6)
1️⃣ India is a country with diverse population and socioeconomic backgrounds, where despite agricultural richness, a large portion of the population still suffers from malnutrition and micronutrient deficiencies.
2️⃣ The nutritional problems in India are mainly due to poverty, food insecurity, lack of health education, unhygienic practices, and limited access to health services, especially in rural and tribal areas.
3️⃣ These problems affect all age groups, especially children under 5 years, adolescent girls, pregnant and lactating women, and elderly people.
4️⃣ Nutritional problems in India include both under-nutrition (deficiency disorders) and over-nutrition (obesity and lifestyle disorders).
Major Nutritional Problems in India
1️⃣ Protein-Energy Malnutrition (PEM)
- It is the most common nutritional disorder seen in children below 5 years, especially in rural and low-income families.
- It includes conditions like Marasmus and Kwashiorkor, which result from deficiency of protein and energy-rich food.
- It causes growth retardation, muscle wasting, edema, and increased susceptibility to infections.
- PEM leads to high infant mortality rate and poor cognitive development.
2️⃣ Iron Deficiency Anemia
- It is one of the most widespread nutritional problems in India, particularly among adolescent girls, pregnant women, and children.
- It occurs due to inadequate intake of iron-rich foods, frequent infections, poor absorption, and blood loss during menstruation or pregnancy.
- It results in fatigue, pallor, low hemoglobin, reduced work capacity, and poor academic performance in students.
- It also increases the risk of maternal and child mortality during childbirth.
3️⃣ Vitamin A Deficiency
- It is common among young children, especially those who are not breastfed properly or have frequent infections.
- It leads to night blindness, xerophthalmia, Bitot’s spots, and in severe cases, corneal ulceration and blindness.
- Vitamin A is crucial for immunity, skin health, and eye development, and its deficiency weakens resistance to infections.
4️⃣ Iodine Deficiency Disorders (IDD)
- Iodine deficiency leads to goiter, cretinism, mental retardation, and growth abnormalities.
- It is a public health concern in mountainous and river basin regions with iodine-deficient soil.
- Despite the Universal Salt Iodization Programme, some regions still face this deficiency due to lack of awareness and poor-quality iodized salt.
5️⃣ Vitamin D and Calcium Deficiency
- Lack of exposure to sunlight and calcium-rich food leads to rickets in children and osteomalacia or osteoporosis in adults.
- Urban sedentary lifestyle and inadequate dietary habits are major contributing factors.
- These deficiencies lead to bone deformities, pain, fractures, and stunted growth.
6️⃣ Folate and Vitamin B12 Deficiency
- These are particularly common among vegetarians and pregnant women, leading to megaloblastic anemia and neural tube defects in newborns.
- Folate is important for DNA synthesis, and its deficiency affects cell division and fetal development.
7️⃣ Overnutrition and Obesity
- With urbanization and sedentary lifestyles, India is also facing rising cases of obesity, type 2 diabetes, hypertension, and cardiovascular diseases.
- Overnutrition is seen more in urban populations, middle-income groups, and school children.
- It is caused by excessive consumption of processed food, sugar, and fats, and lack of physical activity.
8️⃣ Hidden Hunger (Micronutrient Malnutrition)
- This refers to subclinical deficiency of essential vitamins and minerals, even if calorie intake is sufficient.
- It includes zinc, vitamin C, selenium, magnesium, and essential fatty acid deficiencies, which impair immunity, healing, and development.
Contributing Factors to Nutritional Problems in India
1️⃣ Poverty and unemployment limit the ability to purchase nutritious food.
2️⃣ Poor maternal health and low birth weight babies contribute to a cycle of undernutrition.
3️⃣ Lack of nutrition education leads to poor feeding and weaning practices.
4️⃣ Infectious diseases (e.g., diarrhea, worm infestation) worsen nutritional status.
5️⃣ Social inequalities and gender bias cause girls and women to receive less food.
6️⃣ Poor sanitation and hygiene increase the risk of gastrointestinal infections.
7️⃣ Food insecurity due to droughts, inflation, or lack of food storage.
8️⃣ Cultural and food taboos restrict intake of essential nutrients.
Role of Nurse in Addressing Nutritional Problems
1️⃣ It is the nurse’s duty to identify malnourished individuals, especially children and pregnant women, during community visits or clinics.
2️⃣ It is important to provide nutrition counseling and educate families on balanced diets, breastfeeding, and weaning practices.
3️⃣ The nurse must participate in growth monitoring and surveillance programs.
4️⃣ It is necessary to ensure distribution of iron, folic acid, vitamin A supplements, and deworming medications.
5️⃣ The nurse should collaborate with ICDS, Anganwadi, and public health programs like Mid-Day Meal, POSHAN Abhiyaan, and Anemia Mukt Bharat.
6️⃣ It is essential to refer severely malnourished cases to Nutritional Rehabilitation Centres (NRCs) and monitor follow-up.
Q.5 Fill in the blanks (1×5=5)
1) Scurvy is the deficiency of vitamin …….
Vitamin C (Ascorbic Acid)
2) BMI stands for …….
Body Mass Index
3) On metabolism, 1 gm of fat gives …….. Kcal
9 Kcal
4) ……. Vitamin is useful in blood clotting
Vitamin K
5) Deficiency of mineral ……. Produces microcytic, hypochromic anemia
Iron
Section 2 (Biochemistry-30 marks)
Q.5
A) What is protein ? Write the medical and biological importance of protein (2+3=5)
Protein is a complex organic compound made up of carbon, hydrogen, oxygen, nitrogen, and sometimes sulfur, composed of long chains of amino acids linked together by peptide bonds.
Proteins are essential macromolecules found in every cell and tissue of the body and are required for growth, repair, enzyme action, hormone production, immune function, and many more vital processes.
BIOLOGICAL IMPORTANCE OF PROTEINS
1️⃣ It is the primary structural component of all cells and tissues such as skin, muscles, cartilage, bones, and hair, helping in maintaining the structural integrity of the body.
2️⃣ It is essential for the synthesis of enzymes, which are proteins that catalyze and regulate all biochemical reactions in the body including digestion, respiration, and metabolism.
3️⃣ It is necessary for the formation of hormones, especially peptide hormones like insulin, glucagon, and growth hormone, which regulate various physiological processes.
4️⃣ It helps in the formation of antibodies (immunoglobulins), which are protein molecules that defend the body against infections, forming the basis of the immune system.
5️⃣ It plays a vital role in transportation within the body, as seen in hemoglobin (a protein that carries oxygen in the blood) and albumin (which maintains oncotic pressure and transports drugs/hormones).
6️⃣ It is responsible for muscle contraction and movement, as seen in actin and myosin proteins in skeletal and cardiac muscles.
7️⃣ It is crucial in maintaining osmotic balance and acid-base balance, helping to regulate fluid distribution between blood and tissues.
8️⃣ It acts as a buffer system to maintain pH balance and prevent harmful shifts in acidity and alkalinity.
9️⃣ It serves as a secondary energy source during starvation or inadequate carbohydrate intake, providing 4 kcal of energy per gram.
🔟 It supports tissue growth and repair, especially after injury, illness, or surgery, making protein crucial for healing and recovery.
MEDICAL IMPORTANCE OF PROTEINS
1️⃣ It is essential in wound healing and post-surgical recovery, as increased protein intake accelerates tissue repair and collagen formation.
2️⃣ It is used in the dietary management of malnutrition, such as in kwashiorkor and marasmus, which are protein deficiency diseases seen in children.
3️⃣ It is vital in managing hypoalbuminemia, where low protein levels in blood cause edema and require protein-rich diets or albumin infusions.
4️⃣ It is helpful in maintaining immunity, especially in immunocompromised patients or those undergoing chemotherapy, where protein-rich diets help rebuild immune defense.
5️⃣ It is used in managing liver and kidney diseases, where the type and amount of protein need to be adjusted according to metabolic capacity.
6️⃣ It plays a key role in sports medicine and physiotherapy, aiding in muscle building and post-exercise recovery among athletes and patients in rehabilitation.
7️⃣ It is necessary in protein-based therapies, such as monoclonal antibodies used for autoimmune diseases and cancers.
B) Write about the blood buffers (5)
- Blood buffers refer to a group of physiological chemical systems present in the blood, whose primary function is to maintain the normal pH of blood within a narrow range of 7.35 to 7.45, despite continuous production of acids and bases during metabolism.
- These buffer systems act by neutralizing excess hydrogen ions (H⁺) or hydroxide ions (OH⁻), thereby preventing significant pH fluctuations which could otherwise disrupt enzymatic activity and cellular functions.
- It is essential to understand that slight changes in blood pH can severely affect the function of organs like the brain, heart, and kidneys, hence buffer systems are the body’s first line of defense against acid-base disturbances.
Purpose and Importance of Blood Buffers
- It is to protect the body from acidosis (when pH falls below 7.35) and alkalosis (when pH rises above 7.45), both of which can be life-threatening if left untreated.
- It is to maintain a stable internal environment (homeostasis) which is essential for the proper functioning of enzymes, hormones, and cellular metabolism.
- It is to work in coordination with the respiratory system (lungs) and renal system (kidneys) to excrete excess acids or bases and maintain pH balance.
- It is to act immediately (within seconds), providing a quick buffering response before other regulatory systems are activated.
Types of Blood Buffer Systems
1️⃣ Bicarbonate Buffer System (H₂CO₃ / HCO₃⁻)
- This is the most important and abundant extracellular buffer system in the blood.
- It consists of a weak acid (carbonic acid – H₂CO₃) and its conjugate base (bicarbonate ion – HCO₃⁻).
- When there is excess acid (H⁺), the bicarbonate reacts with it to form carbonic acid, which is then converted to carbon dioxide (CO₂) and water (H₂O) and exhaled through the lungs.
- When there is excess base (OH⁻), carbonic acid neutralizes it to form bicarbonate and water, preventing alkalosis.
- Reaction : H⁺ + HCO₃⁻ ⇌ H₂CO₃ ⇌ CO₂ + H₂O
- The lungs help regulate CO₂ (hence pH) through respiration, and the kidneys help control HCO₃⁻ levels through excretion or reabsorption.
2️⃣ Phosphate Buffer System (H₂PO₄⁻ / HPO₄²⁻)
- This system operates mainly in the intracellular fluid and renal tubules where phosphate concentrations are higher.
- It includes dihydrogen phosphate (H₂PO₄⁻), which acts as a weak acid, and monohydrogen phosphate (HPO₄²⁻), which acts as a weak base.
- It buffers strong acids and bases by converting them into weaker, less harmful substances.
- Reaction : H₂PO₄⁻ ⇌ H⁺ + HPO₄²⁻
- It plays a significant role in maintaining pH of urine and contributes to the excretion of hydrogen ions (H⁺) by the kidneys.
3️⃣ Protein Buffer System (e.g., Hemoglobin, Albumin)
- This is the most important intracellular buffer system, especially inside red blood cells.
- Proteins contain amino acids, some of which have functional groups that can act as acid (donate H⁺) or base (accept H⁺) depending on the pH.
- Hemoglobin in red blood cells acts as a buffer by binding to hydrogen ions produced when carbon dioxide is converted into carbonic acid.
- Reaction : HHb ⇌ H⁺ + Hb⁻
- Plasma proteins like albumin also help buffer blood by accepting or donating H⁺ ions depending on the situation.
4️⃣ Hemoglobin Buffer System
- Hemoglobin is not only involved in oxygen transport but also acts as a buffer for acid generated during CO₂ transport.
- When carbon dioxide diffuses into red blood cells, it reacts with water to form carbonic acid, which then dissociates into H⁺ and HCO₃⁻.
- Hemoglobin binds the H⁺ ion, thus preventing pH drop inside the cell.
- This system works in close relation with the bicarbonate buffer system and is vital for maintaining blood pH in tissues and lungs.
Organs Involved in Buffer Regulation
- Lungs help regulate pH by controlling the rate of CO₂ exhalation, which directly affects carbonic acid concentration.
- Kidneys assist by excreting hydrogen ions (H⁺) and reabsorbing bicarbonate ions (HCO₃⁻), thus providing long-term pH regulation.
- The combined action of lungs, kidneys, and blood buffers ensures that blood pH remains stable even during metabolic or respiratory imbalances.
Clinical Relevance of Blood Buffers
- In metabolic acidosis (e.g., diabetic ketoacidosis), the bicarbonate buffer system tries to neutralize excess H⁺ ions, and respiration increases to remove CO₂.
- In respiratory alkalosis (e.g., hyperventilation), the body reduces respiratory rate to retain CO₂ and shift the buffer reaction toward acid production.
- ABG (Arterial Blood Gas) analysis is commonly used to evaluate acid-base balance and assess the function of buffer systems.
- Buffer systems are vital in critically ill patients, where acid-base disturbances are common and require immediate correction.
Q.6 Write short notes (any four) (2.5×4=10)
1) Classification of vitamins with example
1. Fat-Soluble Vitamins
These vitamins are soluble in fat, stored in the liver and adipose tissues, and not excreted easily.
✅ Vitamin A – Example: Carrot, liver, milk
✅ Vitamin D – Example: Sunlight, fish oil, egg yolk
✅ Vitamin E – Example: Nuts, seeds, vegetable oils
✅ Vitamin K – Example: Green leafy vegetables, broccoli
2. Water-Soluble Vitamins
These vitamins are soluble in water, not stored in large amounts, and excess is excreted in urine.
✅ Vitamin B Complex:
- B1 (Thiamine) – Whole grains, pulses
- B2 (Riboflavin) – Milk, eggs
- B3 (Niacin) – Meat, peanuts
- B6 (Pyridoxine) – Banana, fish
- B9 (Folic acid) – Green leafy vegetables
- B12 (Cobalamin) – Liver, dairy, fish
✅ Vitamin C (Ascorbic acid) – Example: Citrus fruits, amla, guava
2) Importance of biochemistry in nursing
1️⃣ It helps nurses understand the structure and function of biomolecules such as carbohydrates, proteins, lipids, vitamins, and enzymes, which are vital for maintaining normal body functions.
2️⃣ It is essential in understanding metabolic processes like glycolysis, gluconeogenesis, protein synthesis, and fat metabolism, which assist in assessing a patient’s nutritional and metabolic status.
3️⃣ It enables nurses to interpret biochemical laboratory results, such as blood glucose levels, urea, creatinine, cholesterol, liver function tests, and electrolytes, which are important for clinical decision-making.
4️⃣ It aids in understanding the biochemical basis of diseases like diabetes mellitus, liver disorders, renal failure, acid-base imbalance, and electrolyte disturbances.
5️⃣ It provides a foundation for drug metabolism and pharmacokinetics, helping nurses to understand how drugs are absorbed, distributed, metabolized, and excreted by the body.
6️⃣ It supports the nurse in nutritional planning by giving insights into the role of vitamins, minerals, and essential fatty acids in health and disease prevention.
7️⃣ It is important in managing fluid and electrolyte balance, especially in critical care and post-operative patients, where biochemical monitoring is vital.
8️⃣ It helps in understanding genetic disorders and molecular medicine, which is increasingly important in modern nursing, especially in pediatric and oncology care.
9️⃣ It enhances the nurse’s role in health education and counseling, by giving scientific knowledge about diet, exercise, diabetes control, cholesterol management, and prevention of nutritional deficiencies.
🔟 It strengthens evidence-based practice, allowing nurses to integrate biochemical data into holistic patient care and clinical research.
3) Sources and deficiency disease of vitamin B
Sources of Vitamin B Complex
1️⃣ Whole grains (wheat, rice, oats)
2️⃣ Milk, curd, paneer
3️⃣ Eggs, liver, meat, fish
4️⃣ Pulses, legumes, soybeans
5️⃣ Green leafy vegetables (spinach, cabbage)
6️⃣ Nuts and seeds
7️⃣ Bananas, avocado
8️⃣ Fortified cereals and fermented foods
Deficiency Diseases of Vitamin B
1️⃣ B1 (Thiamine): Beriberi – nerve damage, muscle weakness
2️⃣ B2 (Riboflavin): Cheilitis, sore tongue, red eyes
3️⃣ B3 (Niacin): Pellagra – dermatitis, diarrhea, dementia
4️⃣ B6 (Pyridoxine): Anemia, irritability, neuropathy
5️⃣ B9 (Folic Acid): Megaloblastic anemia, fetal neural defects
6️⃣ B12 (Cobalamin): Pernicious anemia, nerve damage
4) Function of fat
1️⃣ Fat is a concentrated source of energy, providing 9 kilocalories per gram, which is more than double the energy provided by carbohydrates and proteins.
2️⃣ Fat serves as an energy reserve, as excess fat is stored in adipose tissues, which can be utilized by the body during periods of fasting, illness, or starvation.
3️⃣ Fat helps in the absorption of fat-soluble vitamins such as vitamin A, D, E, and K, which are essential for vision, bone health, immunity, and blood clotting.
4️⃣ Fat provides insulation and regulates body temperature, as the subcutaneous fat layer helps retain heat and protect internal organs from temperature changes.
5️⃣ Fat cushions and protects vital organs, such as the kidneys, heart, and liver, by forming a protective layer around them.
6️⃣ Fats are essential for the synthesis of hormones and cell membranes, especially cholesterol and essential fatty acids (omega-3 and omega-6), which are involved in hormone regulation and brain function.
7️⃣ Fat adds taste, texture, and satiety to food, making meals more palatable and helping to delay the feeling of hunger after eating.
8️⃣ Essential fatty acids (EFAs) present in fat are necessary for growth, skin health, immune function, and inflammatory regulation.
5) Use of prostaglandin
1️⃣ It is used for the induction of labor in pregnant women, especially when there is a medical need to deliver the baby before natural labor begins (e.g., PGE2 or misoprostol).
2️⃣ It is useful in the termination of pregnancy (medical abortion) during early gestation by promoting uterine contractions (e.g., misoprostol with mifepristone).
3️⃣ It is administered to maintain the patency of ductus arteriosus in neonates with congenital heart defects (e.g., PGE1 – alprostadil) until surgical correction is possible.
4️⃣ It is prescribed in the treatment of peptic ulcer disease, particularly for preventing NSAID-induced gastric ulcers by promoting mucus secretion and reducing acid (e.g., misoprostol).
5️⃣ It is used in the treatment of glaucoma and ocular hypertension by increasing the outflow of aqueous humor (e.g., latanoprost, travoprost – PGF2α analogs).
6️⃣ It is employed to control postpartum hemorrhage (PPH) by inducing strong uterine contractions and reducing blood loss (e.g., carboprost – PGF2α).
7️⃣ It is used for cervical ripening before surgical procedures like D&C or IUD insertion by softening and dilating the cervix (e.g., dinoprostone).
8️⃣ It is utilized in erectile dysfunction treatment, where PGE1 analog (alprostadil) is injected intracavernosally to promote penile erection through vasodilation.
9️⃣ It is used to induce abortion in molar pregnancy or fetal demise by initiating uterine evacuation.
🔟 It is used in assisted reproductive technologies (ART) to prepare the endometrium for embryo implantation.
Q.7 Define following terms (1×10=10)
1) Hormone
A hormone is a chemical messenger that is secreted by endocrine glands directly into the bloodstream and carried to distant target organs or tissues where it regulates specific physiological processes such as growth, metabolism, reproduction, mood, and homeostasis.
2) Glycolysis
Glycolysis is a biochemical process in which one molecule of glucose (a 6-carbon sugar) is broken down into two molecules of pyruvate (a 3-carbon compound), releasing energy in the form of ATP and NADH, and occurring in the cytoplasm of the cell.
3) Glucogenesis
Gluconeogenesis is a metabolic process in which glucose is synthesized from non-carbohydrate sources, such as amino acids, lactate, glycerol, and pyruvate, especially during periods of fasting, starvation, or intense exercise.
4) Vitamin
Vitamins are organic compounds that are essential for normal growth, metabolism, and overall health, and are required in small quantities in the diet because the body either cannot synthesize them at all or not in sufficient amounts.
5) Electrophoresis
Electrophoresis is a laboratory technique used to separate charged particles such as proteins, DNA, or RNA based on their size, charge, and shape by applying an electric field through a medium like agarose or polyacrylamide gel.
6) Saturated fatty acids
Saturated fatty acids are a type of fatty acid that contain no double bonds between the carbon atoms in their hydrocarbon chain. This means all carbon atoms are fully “saturated” with hydrogen atoms, making the chain straight and able to pack tightly.
7) Catalyst
A catalyst is a substance that increases the speed of a chemical reaction without itself undergoing any permanent change or being consumed in the reaction. It lowers the activation energy, allowing the reaction to proceed faster or under milder conditions.
8) Coenzyme
A coenzyme is an organic, non-protein molecule that binds with an enzyme and helps it catalyze a biochemical reaction. It acts as a cofactor, meaning it is necessary for the enzyme’s activity, but it is not consumed permanently in the reaction. Coenzymes often act as carriers of electrons, atoms, or functional groups during the reaction and are usually derived from vitamins.
9) Glycosidic bond
A glycosidic bond is a type of covalent bond that joins a carbohydrate (sugar molecule) to another group, which can be another carbohydrate or a different molecule (like alcohol, protein, or nucleic acid). This bond is formed between the anomeric carbon of one monosaccharide and a hydroxyl group (–OH) of another molecule.
10) Oligosaccharide
Oligosaccharides are carbohydrates composed of 2 to 10 monosaccharide units that are chemically bonded together by glycosidic bonds. They are intermediate in size between simple sugars (monosaccharides and disaccharides) and complex carbohydrates (polysaccharides).
