24/01/2018-B.SC-MENTAL HEALTH-PAPER DONE
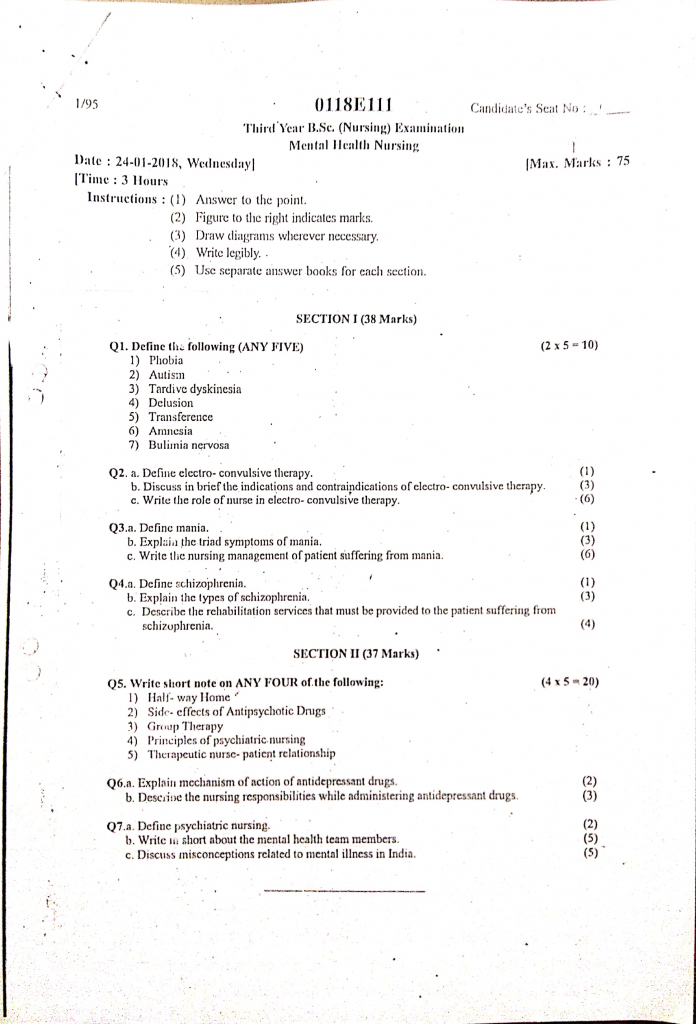
Section 1 (38 marks)
Q.1 Define the following (any five) (2×5=10)
1) Phobia
- A phobia is an intense, irrational, and persistent fear of a specific object, activity, or situation that is disproportionate to the actual danger it poses.
- It is classified as an anxiety disorder in which the individual actively avoids the feared stimulus, leading to significant distress or impairment in daily functioning.
2) Autism
- Autism, also known as Autism Spectrum Disorder (ASD), is a neurodevelopmental disorder that is characterized by persistent difficulties in social communication and social interaction, along with restricted, repetitive patterns of behavior, interests, or activities.
- It usually appears in early childhood and affects the individual’s ability to communicate, understand social cues, and adapt to new environments or changes in routine.
3) Tardive dyskinesia
- Tardive Dyskinesia (TD) is a neurological disorder characterized by involuntary, repetitive, and purposeless movements of muscles, most commonly affecting the face, lips, tongue, trunk, and limbs.
- It is most often caused by long-term use of antipsychotic medications, especially the first-generation (typical) antipsychotics, and results from dopamine receptor hypersensitivity in the brain.
4) Delusion
- A delusion is a false, fixed belief that is strongly held despite clear or obvious evidence to the contrary, and is not shared by others in the same cultural or social group.
- It is commonly seen in psychotic disorders such as schizophrenia and may involve beliefs of persecution, grandeur, reference, or control that are not based in reality.
5) Transference
- Transference is a psychological phenomenon in which a patient unconsciously redirects feelings, desires, and expectations from one person (often a significant figure from their past, such as a parent) onto the therapist or healthcare provider.
- It plays a significant role in psychotherapy, where unresolved emotions from earlier relationships are projected onto the therapist, influencing the therapeutic interaction and helping to explore the patient’s inner conflicts.
6) Amnesia
- Amnesia is a partial or total loss of memory that may be temporary or permanent, affecting a person’s ability to recall past experiences, information, or events.
- It usually results from brain injury, psychological trauma, infections, or neurological conditions, and can involve difficulty forming new memories (anterograde amnesia) or inability to recall past memories (retrograde amnesia).
7) Bulimia nervousa
- Bulimia Nervosa is an eating disorder characterized by recurrent episodes of binge eating, followed by inappropriate compensatory behaviors such as self-induced vomiting, excessive exercise, fasting, or misuse of laxatives or diuretics, in order to prevent weight gain.
- Despite often maintaining a normal body weight, individuals with bulimia nervosa experience intense fear of gaining weight and have a distorted body image, leading to significant emotional distress and physical health complications.
Q.2
a. Define electro-convulsive therapy (1)
Electroconvulsive Therapy (ECT) is a medical treatment in which a controlled electric current is passed through the brain to intentionally trigger a brief seizure, with the goal of relieving severe psychiatric symptoms, especially in conditions like major depression, schizophrenia, and bipolar disorder, when other treatments have failed.
b. Discuss in brief the indication and contraindications of electro convulsive therapy (3)
Indications of Electroconvulsive Therapy (ECT)
- Severe Depression – especially with suicidal risk or psychotic features
- Catatonia – in schizophrenia or depression
- Treatment-resistant Schizophrenia
- Acute Mania – not responding to medication
- Postpartum Psychosis
- Suicidal behavior needing urgent control
- Neuroleptic Malignant Syndrome (rare cases)
- Bipolar Depression – when drugs are ineffective
Contraindications of Electroconvulsive Therapy (ECT)
- Raised Intracranial Pressure (ICP)
- Recent Myocardial Infarction (within 3–6 months)
- Severe Heart Disease – arrhythmia, CHF
- Recent Stroke or Aneurysm
- Retinal Detachment or Eye Surgery
- High-risk Pregnancy (relative)
- Severe Pulmonary Disease (like COPD)
- Pheochromocytoma (adrenal tumor)
c. Write the role of nurse in electro convulsive therapy (6)
The nurse plays a critical role in the preparation, administration, and post-procedure care of a patient undergoing Electroconvulsive Therapy (ECT). ECT is a psychiatric procedure in which electrical stimulation is applied to the brain under controlled settings to treat severe mental disorders like major depression, mania, or catatonia, and nursing care ensures its safe and effective implementation.
✅ 1. Pre-Procedure Nursing Responsibilities
The nurse plays a crucial role in physically and psychologically preparing the patient for ECT to ensure a safe, smooth, and anxiety-free experience.
- Obtain valid written informed consent from the patient or legal guardian after confirming their understanding of the procedure, risks, and benefits.
- Ensure that the patient remains nil per oral (NPO) for at least 6–8 hours prior to the scheduled ECT session to reduce aspiration risk during anesthesia.
- Perform a pre-ECT physical and mental health assessment, including vital signs, mental status, medication history, blood sugar, ECG, and relevant investigations.
- Explain the procedure in simple and reassuring language to reduce fear, stigma, and anxiety commonly associated with ECT.
- Remove all personal belongings and medical items that could interfere or cause injury: dentures, hearing aids, jewelry, nail polish, eyeglasses, and contact lenses.
- Ensure that pre-medications ordered by the physician, such as anticholinergics (e.g., atropine), are administered on time to reduce salivation and prevent bradycardia.
- Maintain a calm, therapeutic environment and offer privacy and emotional support to the patient and family members.
- Confirm the patient’s identity, diagnosis, and scheduled ECT order, ensuring correct documentation and communication with the team.
✅ 2. Responsibilities During the ECT Procedure
During ECT, the nurse acts as a direct patient advocate and safety monitor, working alongside the psychiatrist, anesthetist, and technician.
- Position the patient in a comfortable supine position on the ECT table and ensure proper body alignment for procedure access and seizure observation.
- Assist the anesthetist in administering a short-acting general anesthetic (e.g., methohexital) and muscle relaxant (e.g., succinylcholine) as ordered.
- Ensure all monitoring equipment is functional, including ECG, pulse oximeter, blood pressure monitor, and oxygen flow.
- Apply a bite block or padded mouth guard to prevent tongue or dental injuries during the seizure.
- Provide 100% oxygen by mask before and after the procedure to compensate for respiratory suppression during anesthesia.
- Observe the duration, intensity, and quality of the induced seizure (usually 20–30 seconds); inadequate seizure may reduce therapeutic benefit.
- Maintain strict aseptic technique to prevent infections, especially if intravenous lines or airway devices are used.
- Remain calm and focused, providing continuous reassurance if the patient is semi-conscious during induction or waking.
✅ 3. Post-Procedure Nursing Responsibilities
After the ECT session, the nurse’s priority is to ensure safe recovery from anesthesia, monitor for complications, and offer supportive care.
- Gently transfer the patient to the recovery room in the lateral (side-lying) position to maintain airway patency and reduce aspiration risk.
- Monitor vital signs (pulse, BP, respiration, oxygen saturation) every 5–15 minutes until the patient is fully alert and stable.
- Observe for immediate side effects such as confusion, disorientation, nausea, muscle pain, or headache and manage them as per protocol.
- Provide a calm and quiet recovery environment, as patients may wake up confused or anxious after the seizure.
- Assist with orientation to time, place, and person, and gently reassure the patient about what has occurred.
- Offer fluids or a light snack once fully conscious, if permitted, and assess swallowing before intake.
- Document the entire procedure, including vital signs, seizure duration, medications given, patient’s response, and any adverse events.
- Educate the patient and family about aftercare instructions, possible transient memory loss, and the date of the next ECT session.
- Encourage the patient to report any persistent symptoms, such as prolonged confusion or unusual pain.
- Ensure safe transport back to the psychiatric unit or ward, and inform the attending doctor or charge nurse about the patient’s condition.
Q.3
a. Define menia (1)
Mania is mood disorder characterized by an abnormally elevated, expansive, or irritable mood, along with increased energy, hyperactivity, inflated self-esteem, reduced need for sleep, and impulsive behavior, typically lasting at least one week and interfering with social or occupational functioning.
b. Explain the triad symptoms of mania (3)
The triad of symptoms of mania refers to the three key hallmark features that are most commonly observed in individuals experiencing a manic episode, especially in bipolar disorder. These three features involve mood, thought, and behavior, and help in the early recognition and diagnosis of mania.
✅ 1. Elevated or Expansive Mood (Mood Component)
- The first and most defining feature of mania is a persistently elevated, euphoric, or irritable mood, which lasts for at least one week or more, and is present most of the day.
- The individual may appear excessively cheerful, overconfident, boastful, or unusually optimistic, even when the situation doesn’t warrant such emotions.
- In some cases, if their elevated mood is challenged, the person may quickly become irritable, angry, or hostile, showing poor frustration tolerance.
✅ 2. Increased Psychomotor Activity (Behavioral Component)
- The second element in the triad is increased energy and goal-directed activity, resulting in restlessness, hyperactivity, and excessive engagement in multiple tasks.
- The person may exhibit over-talkativeness (pressured speech), pacing, excessive phone calling, impulsive spending, or sudden travel plans.
- They may have decreased need for sleep, feeling rested with only a few hours of sleep or no sleep at all, yet remain excessively active.
- Risky behaviors like sexual indiscretions, reckless driving, or substance abuse may also be observed due to impaired judgment.
✅ 3. Flight of Ideas and Inflated Self-Esteem (Cognitive/Thought Component)
- The third feature involves cognitive disturbances, particularly racing thoughts, rapid speech, and flight of ideas, where the person jumps from one topic to another rapidly.
- The person may also show inflated self-esteem or grandiosity, believing they have special powers, talents, or a unique destiny.
- In severe cases, these thoughts may escalate into delusions of grandeur, where the individual believes they are a famous personality or have supernatural abilities.
c. Write the nursing management of patient suffering from mania (6)
1. Maintaining a Safe Environment
- The nurse must closely monitor the patient’s behavior for signs of hyperactivity, aggression, self-harm, or threats to others and intervene promptly to ensure safety.
- The environment should be structured, non-stimulating, and free from potential hazards, including sharp tools, glass, belts, or cords.
- The nurse should assign the patient to a room near the nursing station for easier observation and rapid intervention when needed.
- Use of least-restrictive alternatives such as verbal redirection, de-escalation techniques, or assigning a trusted staff member as a sitter can reduce the need for physical restraint.
- Safety protocols should be updated frequently and clearly communicated to the multidisciplinary team to ensure consistency.
2. Establishing Therapeutic Communication
- The nurse should use short, direct, and clear sentences when giving instructions, as manic patients have short attention spans and may become easily distracted.
- It is important to remain calm, non-confrontational, and consistent in tone and body language to avoid triggering defensive or aggressive responses.
- The nurse must avoid arguing or engaging in debates over delusions or grandiosity, instead gently redirecting the conversation to reality-based topics.
- Therapeutic listening should be maintained, allowing the patient to vent thoughts and emotions while ensuring that communication does not escalate agitation.
- The nurse can use therapeutic silence when appropriate to give the patient time to reflect or regain control of thought flow.
3. Controlling Stimuli and Providing a Structured Environment
- The patient should be kept in a low-stimulation room, minimizing exposure to noise, crowds, bright lights, and overstimulating social situations.
- Structured, predictable routines including meal times, rest periods, and medication administration should be followed to maintain consistency.
- The nurse should limit the patient’s access to group interactions or high-energy activities during the acute manic phase to prevent overstimulation.
- Introducing one-to-one quiet activities (e.g., puzzles, coloring, walking) helps redirect energy into safer and calming outlets.
- Visual cues like daily schedules, orientation boards, and clocks help the patient stay oriented to time and routine.
4. Promoting Rest and Sleep
- The nurse should encourage rest by offering the patient a quiet, comfortable sleeping area, reducing light, sound, and interruptions especially in the evening.
- Short rest periods during the day should be scheduled and reinforced, even if the patient does not feel tired, to prevent physical exhaustion.
- A bedtime routine (e.g., warm bath, herbal tea, calming music) should be maintained to help the body adjust to rest periods naturally.
- Sleep-promoting measures such as reducing caffeine, encouraging slow breathing, or reading calming content can be used before bedtime.
- If necessary, prescribed sedative medications should be administered on time and the patient’s response and side effects should be monitored closely.
5. Assisting with Nutrition and Fluid Intake
- The nurse should offer easy-to-eat, high-calorie finger foods such as sandwiches, boiled eggs, fruits, and juice, which allow the patient to eat while moving or pacing.
- Frequent reminders to eat and drink are necessary, as manic patients often neglect meals due to their distractibility or hyperfocus on activity.
- Keep nutritional snacks and water accessible at all times, especially after physical activity or therapy sessions.
- Monitor and document daily food and fluid intake, and consider nutritional supplements if calorie intake remains insufficient.
- If necessary, arrange for assisted feeding or intravenous fluids under medical guidance if the patient refuses food or is unable to eat independently.
6. Encouraging Hygiene and Self-Care
- The nurse should help the patient follow a simple hygiene routine with scheduled bathing, grooming, dressing, and toileting to promote self-care behavior.
- Step-by-step verbal prompts or physical guidance may be required for dressing or toothbrushing, especially if the patient is distracted or confused.
- The patient should be provided with limited, season-appropriate clothing choices to reduce impulsive or inappropriate dress.
- Reinforce personal grooming by praising small achievements, such as brushing hair or changing clothes, to boost self-esteem.
- Visual cues (e.g., mirror, hygiene checklist) may be used to reinforce self-care routines and support independence.
7. Monitoring and Administering Medications
- The nurse must ensure timely administration of mood stabilizers (e.g., Lithium, Valproate) and antipsychotics (e.g., Risperidone, Olanzapine).
- Close monitoring of vital signs, laboratory values (e.g., lithium levels), and side effects such as tremors, sedation, or gastrointestinal distress is essential.
- Patients with poor insight may refuse medications; hence, the nurse should use therapeutic techniques to encourage cooperation, like discussing benefits and addressing fears.
- Observe the patient during and after administration to ensure medication is swallowed and not cheeked or spat out.
- Documentation of effectiveness, side effects, and behavior changes is vital for medication review and adjustment by the physician.
8. Managing Social Behavior and Impulsivity
- The nurse should monitor for inappropriate behavior, including sexual disinhibition, excessive spending, or boundary violation, and intervene firmly but respectfully.
- Set clear, consistent limits on intrusive behavior and redirect the patient to safer activities that reduce overstimulation.
- The nurse should supervise peer interactions to prevent conflict or misunderstandings due to the patient’s talkativeness or attention-seeking.
- Encourage simple tasks or roles like watering plants or folding laundry, which redirect energy and promote cooperation.
- Reinforce appropriate behavior with praise or positive feedback to promote behavioral improvement.
9. Providing Emotional Support and Reality Orientation
- The nurse should provide continuous emotional support by being present, listening actively, and offering validation without encouraging unrealistic beliefs.
- Help the patient to connect with real-time events, people, and facts by using calendars, clocks, and frequent reminders.
- Delusions should not be directly challenged but gently reoriented with neutral, reality-based statements.
- Emotional support includes helping the patient understand and express underlying sadness, anxiety, or guilt, which may be masked by the manic state.
- Encouraging expression through journaling, drawing, or talking in a safe space allows emotional processing without escalation.
10. Involving Family and Educating Caregivers
- The nurse should schedule family psychoeducation sessions to discuss the symptoms, treatment, and long-term nature of bipolar disorder.
- Families should be encouraged to set firm boundaries at home, such as limiting spending and establishing sleep routines.
- Teach family members to recognize early warning signs of relapse, including reduced sleep, irritability, and overconfidence.
- Discuss the importance of medication compliance, regular follow-up, and stress management to prevent future episodes.
- Refer families to support groups or mental health NGOs where they can share experiences and access additional resources.
Q.4
a. Define schizophrenia (1)
Schizophrenia is a chronic and severe mental disorder characterized by disturbances in thought process, perception, emotions, behavior, and social functioning, in which the individual often loses touch with reality, leading to symptoms such as hallucinations, delusions, and disorganized speech or behavior.
b. Explain the types of schizophrenia (3)
Schizophrenia is categorized into different types based on the dominant symptoms the patient presents.
1️⃣ Paranoid Schizophrenia (Most Common Type)
- It is the type of schizophrenia in which the patient predominantly exhibits delusions of persecution or grandeur and auditory hallucinations.
- It is commonly seen that the person believes someone is plotting against them or spying on them, which causes extreme suspicion.
- In this type, the patient usually maintains better cognitive and emotional functioning compared to other types.
- It is commonly diagnosed in late adolescence or early adulthood and often has a better prognosis than other types.
2️⃣ Disorganized Schizophrenia (Hebephrenic Type)
- It is the type in which the patient exhibits disorganized speech, disorganized behavior, and inappropriate or flat emotional expressions.
- It is frequently observed that the person laughs or cries without any logical reason and often uses incoherent or jumbled language.
- It is commonly associated with poor grooming, social withdrawal, and child-like behavior.
- It usually begins at an early age and is linked with a poor prognosis and significant functional impairment.
3️⃣ Catatonic Schizophrenia
- It is the type of schizophrenia in which the individual shows extreme psychomotor disturbances, either in the form of motor rigidity, stupor, or excessive motor activity.
- It is commonly seen that the patient may maintain a rigid posture for hours or resist movement or instructions given by others (negativism).
- It also includes symptoms like waxy flexibility, echolalia (repeating others’ words), and echopraxia (mimicking others’ actions).
- It is a less common type now due to early diagnosis and effective antipsychotic treatment.
4️⃣ Undifferentiated Schizophrenia
- It is the type of schizophrenia in which the symptoms do not clearly fall into paranoid, catatonic, or disorganized types, but there are significant features of schizophrenia present.
- It is frequently seen that the patient displays mixed symptoms such as hallucinations, delusions, disorganized thinking, or emotional flatness.
- It is often diagnosed when the clinician cannot clearly classify the symptoms into a specific subtype.
- It may occur at any stage and has a variable prognosis depending on the severity and combination of symptoms.
5️⃣ Residual Schizophrenia
- It is the type of schizophrenia where active psychotic symptoms have reduced, but mild symptoms still remain.
- It is commonly characterized by emotional blunting, social withdrawal, and odd behavior without the presence of prominent delusions or hallucinations.
- It usually occurs after an acute episode and indicates partial recovery.
- It is important to monitor the patient as there may still be a risk of relapse into active schizophrenia.
6️⃣ Simple Schizophrenia
- It is the rare type in which there is gradual development of negative symptoms like apathy, social withdrawal, emotional dullness, and lack of motivation without prominent delusions or hallucinations.
- It is most commonly seen in early adolescence, and the progression is very slow and insidious.
- This type has a very poor prognosis because it often goes unnoticed until significant damage to the person’s social and occupational functioning occurs.
c. Described the rehabilitation services that must be provided to the patient suffering from schizophrenia (4)
1️⃣ Psychosocial Rehabilitation Services
- It is important to provide psychosocial rehabilitation to help the patient regain interpersonal and social skills.
- It includes social skill training, communication training, and interpersonal relationship development to promote independent functioning.
- It helps reduce social withdrawal, isolation, and improve community participation.
2️⃣ Vocational Rehabilitation
- It is essential to help the patient gain employment-related skills and occupational training suitable for their abilities.
- It includes job placement, vocational guidance, and on-the-job support.
- It improves patient’s self-esteem, independence, and reduces relapse risk.
3️⃣ Educational Rehabilitation
- It focuses on continuing or re-starting formal education disrupted due to illness.
- It is especially useful for young adults with early-onset schizophrenia.
- It includes remedial education, special education, and academic support.
4️⃣ Family Involvement and Psychoeducation
- It is crucial to educate the family about the illness, medication, relapse signs, and caregiving strategies.
- Family therapy helps reduce expressed emotions, which can trigger relapse.
- Supportive counseling is provided to reduce family stress and burden.
5️⃣ Half-Way Homes / Shelter Homes
- It provides transitional residential support for patients not yet ready to live independently.
- It helps the patient practice daily life skills in a semi-supervised environment.
- It prevents homelessness and provides a supportive social setting.
6️⃣ Day Care Centers
- These are structured day programs offering occupational, recreational, and therapeutic activities.
- It provides a routine and social interaction to prevent isolation.
- Helps patients who are not suitable for full-time employment.
7️⃣ Supportive Therapy & Cognitive Rehabilitation
- Regular individual counseling, CBT, and supportive psychotherapy help patients manage symptoms.
- Cognitive rehabilitation helps improve attention, memory, and problem-solving skills.
8️⃣ Community-Based Rehabilitation (CBR)
- It includes services offered within the community through mental health teams, ASHAs, and NGOs.
- It promotes home-based care, reduces stigma, and enhances community support.
Section 2 (37 marks)
Q.5 Write short notes any four of the following (4×5=20)
1) Half way home
Definition of Half-Way Home
- A Half-Way Home is a transitional, community-based rehabilitation center that provides structured residential care to individuals recovering from mental illness who no longer require hospitalization but are not yet ready to return to independent living or family settings.
- It acts as a bridge between psychiatric institutions and community life, ensuring patients learn life skills and receive therapeutic support before full reintegration into society.
- It focuses on rehabilitation, supervision, and skill-building, helping reduce relapses and long-term institutionalization.
Objectives of Half-Way Home
- It is to promote gradual social reintegration of the mentally ill into society.
- It is to help patients regain confidence and functional independence in real-life settings.
- It is to enhance coping mechanisms and manage daily stress in a semi-controlled environment.
- It is to prevent readmission by offering psychiatric monitoring and psychosocial support.
- It is to strengthen the individual’s daily living skills, including cooking, cleaning, personal care, and money management.
- It is to educate and involve families in caregiving and future rehabilitation planning.
- It is to improve vocational and occupational capabilities through skill training.
Key Services Provided in Half-Way Homes
1️⃣ Supervised Residential Facility
- Provides a safe and stable living space under the supervision of mental health professionals.
- Patients receive shelter, food, routine structure, and guidance.
- Helps in learning responsibility for personal care, time management, and tasks.
2️⃣ Medical and Psychiatric Monitoring
- Ongoing mental status assessments and physical health checkups.
- Medication management and observation for side effects or non-compliance.
- Regular visits by psychiatrists, psychologists, and psychiatric nurses.
3️⃣ Daily Living Skills Training
- Training in cooking, cleaning, laundry, money handling, grooming, hygiene.
- Encourages independence in self-care and decision-making.
- Prepares patients for solo or assisted living in the future.
4️⃣ Vocational and Occupational Rehabilitation
- Involves skills training programs like tailoring, gardening, typing, painting, computer use, etc.
- Provides job readiness and employment placement support.
- Builds economic independence and reduces burden on families.
5️⃣ Psychosocial Interventions
- Individual and group therapy sessions to address emotional, behavioral, and social issues.
- Cognitive Behavioral Therapy (CBT), relaxation techniques, and assertiveness training.
- Promotes development of healthy coping mechanisms and problem-solving skills.
6️⃣ Social Skills and Recreational Activities
- Patients are trained in social etiquette, communication, and interaction skills.
- Activities like games, music therapy, art therapy, dance, and role-play sessions are conducted.
- Helps combat social withdrawal and enhance interpersonal functioning.
7️⃣ Family Counseling and Involvement
- Families are educated on the nature of mental illness, early warning signs, and relapse prevention.
- Regular joint sessions with patient and caregivers are held.
- Aims to reduce family stress, stigma, and over-dependence.
8️⃣ Legal and Social Support Services
- Helps patients obtain identity documents, disability benefits, and social welfare support.
- Connects them to NGOs, community-based programs, and rehabilitation schemes.
9️⃣ Community Reintegration Planning
- Assists in planning for discharge to family, supported homes, or independent housing.
- Prepares the patient for challenges like stigma, job seeking, and social rejection.
- Follow-up care is arranged through outpatient mental health services or community-based teams.
Role of Nurse in Half-Way Home
The nurse plays a central role in ensuring holistic care for residents by providing medical, emotional, and psychosocial support.
1️⃣ Health Monitoring and Supervision
- Observe mental status and early signs of relapse or crisis.
- Ensure physical care, hygiene, and health check-ups.
- Monitor sleep patterns, eating habits, and medication effects.
2️⃣ Medication Administration
- Administer medications as prescribed and maintain accurate records.
- Monitor for side effects, compliance, and therapeutic response.
- Provide patient education on the importance of medication adherence.
3️⃣ Conduct Health Education
- Educate patients on self-care, diet, hygiene, sleep hygiene, and substance avoidance.
- Offer information on stress management and lifestyle changes.
4️⃣ Daily Activities & Recreation
- Organize structured daily routines, including hygiene care, group activities, and therapy sessions.
- Encourage participation in work-like settings to build confidence.
5️⃣ Emotional and Social Support
- Build trusting therapeutic relationships with patients.
- Help them verbalize feelings, manage anxiety, and improve self-worth.
- Offer crisis support, especially in emotional breakdowns or withdrawal phases.
6️⃣ Documentation and Reporting
- Maintain detailed records of patient progress, incidents, and therapy participation.
- Update mental health team and participate in care planning and discharge preparation.
7️⃣ Family Support
- Guide families in managing patient behavior, preventing relapse, and planning after discharge.
- Organize joint sessions and home visits, if needed.
2) Side effects of antipsychotic drugs
1. Extrapyramidal Symptoms (EPS)
- It includes drug-induced movement disorders such as dystonia, parkinsonism, akathisia, and tardive dyskinesia.
- These effects occur due to dopamine receptor blockade in the nigrostriatal pathway.
- Dystonia involves sudden muscle spasms (especially in the neck, face, and tongue).
- Akathisia is characterized by restlessness and an inability to stay still.
- Pseudoparkinsonism includes tremors, bradykinesia, and rigidity.
- Tardive dyskinesia causes involuntary movements, especially of the face and tongue, and can be irreversible.
2. Sedation and Drowsiness
- Many antipsychotics cause central nervous system depression, resulting in daytime sleepiness and fatigue.
- This occurs due to histamine H1 receptor antagonism.
3. Anticholinergic Effects
- Includes dry mouth, constipation, blurred vision, urinary retention, and cognitive dulling.
- These effects are more common with low-potency typical antipsychotics and some atypical agents like clozapine and olanzapine.
4. Metabolic Side Effects
- It includes weight gain, hyperglycemia, insulin resistance, and dyslipidemia.
- Atypical antipsychotics such as olanzapine and clozapine are strongly associated with metabolic syndrome.
- These side effects increase the risk of type 2 diabetes mellitus and cardiovascular disease.
5. Neuroleptic Malignant Syndrome (NMS)
- It is a rare but potentially fatal reaction characterized by hyperthermia, muscle rigidity, altered mental status, and autonomic dysfunction (e.g., high BP, tachycardia).
- It is a medical emergency and requires immediate discontinuation of the drug and supportive treatment.
6. Endocrine and Sexual Side Effects
Prolactin elevation due to dopamine blockade in the tuberoinfundibular pathway leads to:
- Galactorrhea (milk discharge),
- Gynecomastia (breast development in males),
- Amenorrhea (absence of menstruation),
- Sexual dysfunction (decreased libido, erectile dysfunction).
7. Cardiovascular Effects
- Includes orthostatic hypotension, tachycardia, and in some cases QT interval prolongation, which can lead to arrhythmias.
- Clozapine and ziprasidone are associated with cardiac conduction abnormalities.
8. Agranulocytosis (especially with Clozapine)
- Clozapine can cause severe decrease in white blood cell count (agranulocytosis), leading to life-threatening infections.
- Requires regular monitoring of WBC and absolute neutrophil count (ANC).
9. Hepatotoxicity
- Some antipsychotics may increase liver enzymes or cause drug-induced hepatitis.
- Regular liver function tests are advised during therapy.
10. Dermatological Reactions
- Rashes, photosensitivity, and pigmentation changes (especially with chlorpromazine) may occur.
- Patients should be advised to avoid excessive sun exposure.
11. Seizure Threshold Reduction
- Drugs like clozapine and chlorpromazine can lower the seizure threshold and may induce seizures, especially at high doses.
12. Hypersalivation (especially Clozapine)
- Clozapine uniquely causes excessive salivation, especially at night, which can be distressing for the patient.
13. Temperature Dysregulation
- Antipsychotics can impair the body’s ability to regulate temperature, leading to hyperthermia or hypothermia, particularly during extreme weather conditions.
3) Group therapy
Definition
- Group therapy is a form of psychotherapy in which a small number of individuals with similar emotional or psychological problems meet together under the guidance of a trained therapist.
- It is a structured therapeutic environment where patients share their experiences, learn coping skills, and gain support from both the therapist and fellow group members.
Goals of Group Therapy
- The primary goal is to help individuals explore their thoughts, emotions, and behaviors in a safe, supportive setting.
- Group therapy aims to enhance self-awareness, self-esteem, and social skills through peer feedback and therapist guidance.
- It provides emotional support, shared learning, and encouragement from others who have similar issues.
- The goal is also to help patients learn new behaviors and adaptive coping mechanisms through role-playing, discussion, and reflection.
- It is meant to facilitate change in attitudes, behaviors, and beliefs through interpersonal interaction.
Types of Group Therapy
1️⃣ Psychoeducational Group Therapy
- Psychoeducational groups are designed to educate clients about specific psychological or medical conditions, such as depression, anxiety, schizophrenia, substance use, or chronic illnesses.
- It is used to provide structured information, teach coping strategies, improve medication compliance, and enhance self-management skills.
2️⃣ Supportive Group Therapy
- Support groups are meant to offer emotional support, reassurance, and shared experience among members facing similar challenges.
- It helps patients feel less alone in their struggles, reduces stress, and promotes hope and motivation for recovery.
- Common examples include bereavement groups, cancer survivor groups, HIV support groups, and mental health peer groups.
3️⃣ Cognitive-Behavioral Therapy (CBT) Group
- CBT group therapy focuses on helping individuals recognize and change negative thought patterns, beliefs, and behaviors that contribute to emotional problems.
- This type of group therapy is goal-oriented and structured, often using homework assignments, role-play, and worksheets.
- It is especially effective in anxiety disorders, phobias, OCD, depression, and substance abuse.
4️⃣ Interpersonal Therapy (IPT) Group
- IPT group therapy focuses on improving interpersonal functioning and relationships, helping clients explore how past and current relationships affect their emotions and mental health.
- It encourages participants to develop better communication, conflict resolution, and social interaction skills.
- It is especially useful in depression, social anxiety, and personality disorders.
5️⃣ Skills Training Group Therapy
- These groups are formed to teach practical life skills, vocational abilities, and social interaction skills in a therapeutic setting.
- Common skills taught include assertiveness, stress management, time management, communication, and anger control.
- It is highly beneficial for patients with schizophrenia, developmental delays, or chronic mental illness.
6️⃣ Self-Help or Peer-Led Groups
- These groups are voluntary and typically led by members, rather than professionals, who have experience with the same condition or challenge.
- Members provide mutual support, share experiences, and promote recovery through empathy and solidarity.
- Examples include Alcoholics Anonymous (AA), Narcotics Anonymous (NA), and Depression Support Groups.
7️⃣ Expressive Therapy Groups
- These groups use creative arts such as music, dance, art, or drama as a medium for self-expression and emotional healing.
- It allows clients to express feelings non-verbally, especially when they struggle to articulate emotions.
Indications for Group Therapy
- Depression, anxiety, and stress-related disorders where patients benefit from shared experiences.
- Substance use disorders, where group settings provide peer accountability and support.
- Grief and loss, where individuals find comfort in connecting with others facing similar pain.
- Chronic medical conditions, such as cancer, diabetes, or HIV, for emotional and informational support.
- Adolescent and family issues, like school problems or parent-child conflict, are often addressed in group formats.
- Social skill deficits, especially in autism spectrum disorder or schizophrenia.
Contraindications of Group Therapy
- Patients with acute psychosis or suicidal risk who may be disruptive or unsafe for group participation.
- Individuals with severe cognitive impairment, who may not understand or benefit from discussion.
- Those with extreme social anxiety or hostility, who may struggle to engage or may harm group dynamics.
Advantages of Group Therapy
- It provides a sense of belonging and acceptance, reducing feelings of isolation.
- Group therapy offers multiple perspectives and feedback from peers.
- It is cost-effective, as one therapist can help multiple patients at once.
- It helps improve interpersonal communication and relationship-building skills.
- Patients learn by observing others and can model positive behaviors.
- It can motivate change through peer influence and role models within the group.
Disadvantages / Limitations
- Some individuals may feel shy or anxious to speak in a group setting.
- There may be conflicts or domination by certain group members, disrupting harmony.
- Confidentiality is harder to maintain, as group members must voluntarily respect others’ privacy.
Role of the Nurse in Group Therapy
- The nurse may act as a co-therapist or facilitator in psychoeducational and support groups.
- It is the nurse’s role to observe group dynamics and ensure a safe, respectful environment.
- The nurse helps in screening suitable patients for group therapy, based on psychological readiness and diagnosis.
- She must encourage participation and manage disruptive behaviors during group sessions.
- The nurse is responsible for documenting patient progress, participation, and any significant observations.
- She also provides emotional support before and after sessions, especially for patients who feel overwhelmed.
- The nurse can use group feedback to reinforce individual care plans and collaborate with other mental health professionals.
4) Principles of psychiatric nursing
✅ 1. Accept the patient as an individual
- The mental health nurse must accept the client with all his/her problems, thoughts, and behaviors without any judgment or criticism, recognizing that every individual has dignity, value, and uniqueness regardless of their mental illness.
- It is the nurse’s responsibility to develop an attitude of empathy, tolerance, and unconditional positive regard, which helps build a therapeutic relationship.
✅ 2. Maintain therapeutic nurse-patient relationship
- The mental health nurse should establish a professional, goal-directed relationship that is based on trust, empathy, honesty, and respect, helping the patient feel emotionally safe.
- It is essential to set clear boundaries, be nonjudgmental, and maintain a consistent, structured interaction with the patient.
✅ 3. Use self-understanding as a therapeutic tool
- The nurse must have self-awareness about personal emotions, attitudes, and biases, so they do not interfere with therapeutic communication or judgment.
- It is important for the nurse to understand their own mental state and behavior, as the nurse’s personality is a vital tool in mental health care.
✅ 4. Ensure patient’s safety at all times
- The nurse should take active steps to protect the patient from harming self or others, especially in cases of suicidal ideation, hallucinations, or aggressive behavior.
- It is important to provide constant observation, safe surroundings, and to remove dangerous items like sharps or cords from the patient’s environment.
✅ 5. Provide privacy and confidentiality
- It is the duty of the nurse to respect the patient’s privacy and ensure that all personal information is kept confidential, except when there is a risk to the patient’s life or others.
- Legal and ethical principles guide nurses to disclose information only with consent or as required by law.
✅ 6. Encourage self-reliance and independence
- The nurse should always promote the patient’s ability to think, decide, and act for themselves, rather than making them dependent on caregivers.
- This is done by providing support, motivation, and involvement in decision-making, which helps in boosting self-esteem and confidence.
✅ 7. Maintain reality orientation
- It is essential for the nurse to orient the patient to time, place, and person regularly, especially in those suffering from confusion, delirium, or psychosis.
- The nurse must gently correct false beliefs or delusions, without arguing, and guide the patient toward reality using calm reassurance.
✅ 8. Provide consistent and structured environment
- Patients with mental illness benefit from a predictable routine and consistent care, as it helps reduce anxiety and confusion.
- The nurse should follow ward rules strictly, avoid sudden changes, and promote regularity in daily activities (like sleep, food, and group therapy).
✅ 9. Be honest, truthful, and nonjudgmental
- Mental health nurses must be genuine and honest while interacting with patients, as trust is the foundation of the therapeutic relationship.
- The nurse should never lie or mislead the patient and must respond to all communication with empathy and professionalism.
✅ 10. Use purposeful communication and active listening
- Communication should be planned, therapeutic, and focused on helping the patient understand themselves better.
- The nurse should use open-ended questions, reflective listening, and non-verbal cues to encourage the patient to express their feelings and thoughts.
✅ 11. Avoid physical restraints unless necessary
- The nurse should always try de-escalation techniques, verbal interventions, and emotional support first, and only use restraints or seclusion when all other methods fail.
- When used, restraints must be applied with doctor’s order, safety measures, documentation, and close monitoring.
✅ 12. Promote socialization and group participation
- The nurse should encourage the patient to engage in group therapy, occupational therapy, and social interactions, which help them develop interpersonal skills and reduce isolation.
- Socialization enhances emotional expression, peer learning, and community reintegration.
✅ 13. Involve family in care process
- Mental illness affects not just the patient but also the family, so the nurse should educate, support, and involve family members in treatment planning and discharge preparation.
- Family education improves compliance, understanding, and early relapse detection.
✅ 14. Respect cultural, religious, and personal beliefs
- The nurse should understand and respect the individual’s cultural background, language, traditions, and religious practices, as they influence how the patient views illness and treatment.
- This helps in providing culturally competent and patient-centered mental health care.
✅ 15. Provide holistic care
- Mental health nursing should address not just the psychological needs, but also the physical, emotional, social, and spiritual well-being of the patient.
- This includes hygiene, nutrition, medication, therapeutic activities, and emotional counseling.
5) Therapeutic nurse patient relationship
Definition
- It is a professional, goal-directed, and time-limited interaction between a nurse and a patient, which is established to promote the patient’s well-being and recovery.
- It is based on trust, empathy, respect, confidentiality, and effective communication, and it is essential in psychiatric as well as general nursing care.
Objectives of Therapeutic Nurse-Patient Relationship
- To develop trust and build rapport between nurse and patient.
- To encourage open and honest communication.
- To support emotional, psychological, and physical healing.
- To promote patient’s independence and self-esteem.
- To help the patient express feelings and concerns freely.
- To provide a safe, empathetic, and non-judgmental environment.
- To guide the patient in identifying problems and setting goals.
- To enhance treatment compliance and coping skills.
- To maintain professional, ethical, and therapeutic boundaries.
- To educate the patient about illness and promote health awareness.
Characteristics of a Therapeutic Relationship
- It is goal-oriented, where the main focus is on the patient’s mental, emotional, physical, or social recovery.
- It is patient-centered, meaning the patient’s needs and problems guide the entire process.
- It involves clear boundaries, ensuring professional distance and emotional safety.
- It is built on trust, where the patient feels safe, understood, and accepted.
- It requires active listening and empathy, where the nurse attentively responds to the patient’s concerns and emotions.
- It promotes mutual respect and dignity, encouraging patient autonomy and participation in care.
- It involves the use of professional communication skills, including verbal and non-verbal methods.
- It is time-bound and purposeful, unlike social or personal relationships.
Phases of Therapeutic Relationship (by Hildegard Peplau)
1️⃣ Pre-Interaction Phase
- It is the phase before meeting the patient, where the nurse prepares mentally and gathers background information.
- It is the phase of self-reflection, where the nurse evaluates personal attitudes, fears, or biases.
- It involves planning for the first interaction, such as reviewing the patient’s case history or environment.
2️⃣ Orientation Phase
- It is the introductory phase, where the nurse and patient meet and start building trust.
- It involves introducing oneself, explaining the purpose of the relationship, and discussing boundaries and confidentiality.
- The nurse begins assessing the patient’s needs, problems, and goals in this phase.
- It is the phase where rapport is established, which forms the foundation of the therapeutic process.
3️⃣ Working Phase (or Exploitation Phase)
- It is the active phase of the relationship, where most therapeutic work is carried out.
- The nurse encourages the patient to express feelings, explore problems, and work towards set goals.
- It is the phase where the nurse provides support, guidance, and therapeutic interventions.
- Transference and counter-transference may occur, and must be managed appropriately by the nurse.
- It is also the phase where trust deepens, and patients start becoming more independent and cooperative.
4️⃣ Termination Phase
- It is the final phase, where the therapeutic relationship is ended in a planned and healthy manner.
- The nurse and patient review the progress made, and evaluate whether the goals were achieved.
- It involves expressing feelings about ending the relationship, both by the nurse and the patient.
- The nurse provides guidance for the future and refers the patient if needed.
- It is important for the nurse to ensure closure, avoid abrupt endings, and handle emotional responses with care.
Nursing Responsibilities in the Therapeutic Relationship
- It is the nurse’s responsibility to develop trust and maintain professional boundaries throughout the interaction.
- The nurse must respect the patient’s privacy, confidentiality, and cultural background during care.
- It is essential for the nurse to use therapeutic communication skills, such as empathy, active listening, reflection, and clarification.
- The nurse should observe non-verbal cues and respond appropriately to the patient’s verbal and emotional expressions.
- The nurse must be emotionally stable and self-aware, avoiding counter-transference or emotional dependency.
- The nurse is expected to document the progress and maintain accurate records of patient interactions.
- It is important for the nurse to encourage patient participation and support patient autonomy and decision-making.
- The nurse must be consistent and reliable, following through on promises and scheduled interactions.
- The nurse should intervene therapeutically in times of crisis, helping the patient manage anxiety, fear, or aggression.
- The nurse needs to evaluate the effectiveness of the relationship and make necessary adjustments as needed.
Q.6
a. Explain mechanism of action of antidepressants drugs (2)
- Antidepressant drugs work by increasing the levels of certain neurotransmitters in the brain, mainly serotonin, norepinephrine, and dopamine, which are often found to be low in individuals with depression.
- These medications act by blocking the reuptake or breakdown of these neurotransmitters at the synaptic cleft, thereby enhancing mood, reducing anxiety, and improving overall mental well-being.
b. Described the nursing responsibilies while administering antidepressant drugs (3)
✅ 1. Pre-Administration Responsibilities (Before Giving the Drug)
- It is the nurse’s responsibility to assess the patient’s diagnosis and mental status, including mood, suicidal ideation, sleep patterns, appetite, and energy level before starting therapy.
- The nurse must obtain a complete medical, psychiatric, and drug history to rule out contraindications like bipolar disorder, seizures, or recent use of MAOIs.
- It is important to identify the type of antidepressant prescribed, such as SSRIs, SNRIs, MAOIs, tricyclics, or atypical agents, and understand its mechanism of action, dose, and side effects.
- The nurse must ensure that MAOIs are not given with SSRIs or TCAs, as it may lead to serious drug interactions like serotonin syndrome or hypertensive crisis.
- Before giving the first dose, the nurse should monitor baseline vitals, liver and renal function tests, and electrolyte levels, especially in elderly patients.
- The nurse should educate the patient and family regarding the expected onset of action (which may take 2–4 weeks) and the importance of adherence.
✅ 2. During Administration Responsibilities
- It is the nurse’s responsibility to administer the drug at the same time every day, preferably in the morning (especially SSRIs) to avoid insomnia.
- The drug should be administered with food (if required) to reduce gastric irritation, especially with tricyclic antidepressants.
- The nurse must observe the patient for immediate side effects like dizziness, nausea, agitation, headache, or allergic reactions after the first few doses.
- Therapeutic communication should be used to assess for any suicidal ideation, especially during early stages when energy improves but mood may still be low.
- The nurse should monitor for orthostatic hypotension (especially with tricyclics and MAOIs) and advise the patient to change positions slowly.
- The nurse must document the dose given, time, route, and patient’s response in the medication record accurately.
✅ 3. Post-Administration Responsibilities
- It is the nurse’s duty to observe and document therapeutic response—such as improved mood, sleep, appetite, and reduction in suicidal thoughts—over days or weeks.
- The nurse should monitor for late-onset side effects like sexual dysfunction, weight gain, serotonin syndrome (confusion, tremor, hyperreflexia), or manic switch in bipolar patients.
- For patients on MAOIs, the nurse must educate about dietary restrictions to avoid foods high in tyramine (e.g., cheese, wine, chocolate) to prevent hypertensive crisis.
- In case of overdose or side effects like seizures, arrhythmias, or severe agitation, the nurse must inform the physician immediately and initiate emergency care.
- If the patient is non-compliant or refuses the drug, the nurse should explore the reasons non-judgmentally, offer psychoeducation, and consult with the psychiatrist.
- The nurse must continuously evaluate medication adherence, side effects, and psychological progress in collaboration with the mental health team.
✅ 4. Health Education Responsibilities
- The nurse must educate the patient and family that antidepressants are not addictive and require long-term use even after feeling better.
- Patients must be told not to stop the drug suddenly, as it may lead to withdrawal symptoms (especially SSRIs and SNRIs).
- The nurse should encourage lifestyle changes like regular sleep, nutrition, physical activity, and involvement in therapeutic activities for better results.
- The nurse should warn against alcohol or other CNS depressants, which may increase sedation or interfere with drug action.
- The nurse must educate women of childbearing age regarding pregnancy risks and the need to inform the doctor if planning a pregnancy.
Q.7
a. Define psychiatric nursing (2)
- Psychiatric Nursing is a specialized branch of nursing that focuses on the care, treatment, and rehabilitation of individuals with mental health disorders, emotional disturbances, and behavioral problems.
- It involves applying nursing principles along with psychological and therapeutic techniques to promote mental well-being, prevent mental illness, and support recovery.
b. Write in short about the mental health team members (5)
1. Psychiatrist
- A psychiatrist is a medical doctor (MBBS + MD Psychiatry) who is specially trained in the diagnosis, treatment, and prevention of mental disorders using both medications and psychotherapy.
- It is their role to conduct psychiatric evaluations, prescribe psychotropic drugs such as antidepressants or antipsychotics, and provide therapies like electroconvulsive therapy (ECT) when required.
- The psychiatrist also leads the clinical decision-making within the team and manages complex mental illnesses such as schizophrenia, bipolar disorder, and severe depression.
2. Clinical Psychologist
- A clinical psychologist is a mental health professional with a Master’s or Doctorate degree in Psychology, trained in psychological assessment and therapy.
- It is the clinical psychologist’s role to use psychological tools and standardized tests (like IQ tests, MMPI, Rorschach) for diagnosing emotional, cognitive, and behavioral issues.
- They do not prescribe medications but provide various psychotherapies such as Cognitive Behavioral Therapy (CBT), family therapy, and behavioral interventions.
3. Psychiatric Nurse / Mental Health Nurse
- A psychiatric nurse is a registered nurse (GNM/B.Sc./M.Sc. Nursing) who is specially trained in the care of mentally ill patients in both hospital and community settings.
- It is the responsibility of the psychiatric nurse to administer medications, observe patient behavior, provide psychological support, and implement therapeutic communication techniques.
- Nurses also play a key role in crisis intervention, health education, family support, and rehabilitation of psychiatric patients.
4. Psychiatric Social Worker
- A psychiatric social worker is a trained professional (usually with MSW or M.Phil in Psychiatric Social Work) who deals with the social and environmental factors affecting mental health.
- It is the role of the social worker to assess the patient’s family background, social support, living conditions, and economic status.
- They help in counseling families, arranging community resources, coordinating aftercare services, and facilitating rehabilitation.
5. Occupational Therapist (OT)
- An occupational therapist is a specialist who helps patients develop, recover, and maintain daily living and work skills.
- It is their role to assist patients with self-care activities, such as dressing, cooking, or using transport, especially for those with chronic psychiatric or developmental disorders.
- OT also works on improving motor coordination, time management, and adaptive skills needed for community reintegration.
6. Counselor / Psychotherapist
- A counselor or psychotherapist is a trained mental health professional who provides emotional support and guidance through structured counseling sessions.
- They may hold degrees like MA in Psychology, Counseling, or Mental Health Counseling, and specialize in individual, group, marital, or adolescent therapy.
- It is their responsibility to help patients cope with stress, grief, addiction, or trauma, often serving as the first point of help in schools, colleges, or NGOs.
7. Rehabilitation Therapist / Vocational Counselor
- A rehabilitation therapist works to prepare the mentally ill for returning to the community, helping them with vocational skills and social reintegration.
- They may provide job training, skill development, workplace behavior modification, and support for economic independence.
- It is their role to coordinate workshops, employment programs, or self-help groups for long-term management.
8. Support Staff (Attendants, Caregivers, Peer Support Workers)
- These individuals include trained attendants, ward staff, peer supporters, or volunteers who provide basic care and companionship.
- It is their role to help with daily activities, feeding, hygiene, and maintaining a therapeutic environment.
- Peer support workers may be recovered patients who help others by sharing their lived experiences and coping strategies.
c. Discuss misconceptions related to mental illness in India (5)
✅ 1. Mental illness is a sign of personal weakness
- Many people falsely believe that those with mental illness are weak-minded or lack the ability to face life’s problems.
- In truth, mental illness is just like physical illness — it can affect even the strongest and most intelligent individuals due to brain chemistry, trauma, or genetics.
- Seeking help is a sign of strength, not weakness, and should be encouraged to promote early recovery.
✅ 2. People with mental illness are violent or dangerous
- Movies and media often depict mentally ill people as dangerous, which spreads fear and stigma in society.
- The truth is, most individuals with mental illness are peaceful, and only a small percentage may show aggression, usually when untreated or under extreme stress.
- In fact, people with mental illness are more likely to harm themselves than to harm others.
✅ 3. Mental illnesses are rare and affect only a few people
- It is wrongly assumed that mental illness affects only a specific group of people such as the poor or uneducated.
- However, mental health conditions affect people across all socioeconomic classes, professions, and cultures, including children, elderly, and celebrities.
- According to WHO, 1 in 4 people worldwide will experience a mental health condition at some point in their lives.
✅ 4. Mental illness cannot be treated or cured
- This belief often stops people from seeking timely help, thinking it’s hopeless.
- In fact, modern psychiatric treatments have a high success rate, especially for conditions like depression, anxiety, and bipolar disorder when started early.
- Recovery is possible through a combination of medication, counseling, lifestyle changes, and family support.
✅ 5. Only “mad” people need psychiatric help
- Many people avoid going to a psychiatrist for fear of being labeled as “mad” or “crazy”.
- In truth, mental health professionals help with common issues like stress, sleep disorders, exam anxiety, trauma, and marital conflict.
- Mental healthcare is as normal and necessary as visiting a doctor for physical illness.
✅ 6. Mental illness is caused by evil spirits or supernatural forces
- In rural or less-educated areas, mental illness is still considered a punishment from God or the result of black magic.
- Such beliefs lead families to seek help from faith healers instead of doctors, delaying proper diagnosis and treatment.
- Education and awareness are essential to explain that mental illness has scientific and biological causes, not spiritual possession.
✅ 7. Mental health problems are a result of bad parenting
- This misconception blames parents, especially mothers, for the child’s mental illness, causing guilt and social stigma.
- However, conditions like autism, ADHD, or schizophrenia often result from genetic and neurochemical factors, not parenting alone.
- In many cases, even children raised in healthy families can develop mental illness due to peer pressure, bullying, or brain changes.
✅ 8. Once mentally ill, always mentally ill
- This leads to social rejection, isolation, and lack of job or marriage opportunities for people who have recovered.
- The fact is, many individuals recover completely or learn to manage their symptoms just like in diabetes or asthma.
- With early treatment and rehabilitation, many can lead independent, productive, and fulfilling lives.
✅ 9. People with mental illness cannot work or be successful
- This misconception results in denial of employment, promotion, or educational opportunities to mentally ill individuals.
- However, many people with past or ongoing mental illness have excelled as doctors, lawyers, actors, scientists, and politicians.
- All they need is reasonable support, understanding, and workplace accommodations, not exclusion.
✅ 10. Talking about mental illness makes it worse
- Families often avoid open discussions, believing that talking about depression or suicide may “put thoughts in the person’s head.”
- In reality, talking about mental health problems in a non-judgmental and supportive manner actually helps the person feel understood and encouraged.
- Open communication promotes healing, trust, and early intervention, and should always be encouraged.
✅ 11. Children and adolescents do not suffer from mental illness
- A common but false belief is that mental illness affects only adults, and that children or teenagers are too young to experience such problems.
- In reality, mental health disorders such as anxiety, depression, ADHD, and conduct disorders can begin in childhood or adolescence, and if left untreated, they may worsen with time and interfere with development, education, and relationships.
- Early identification and intervention in children is essential for better outcomes and to ensure healthy emotional and cognitive growth.