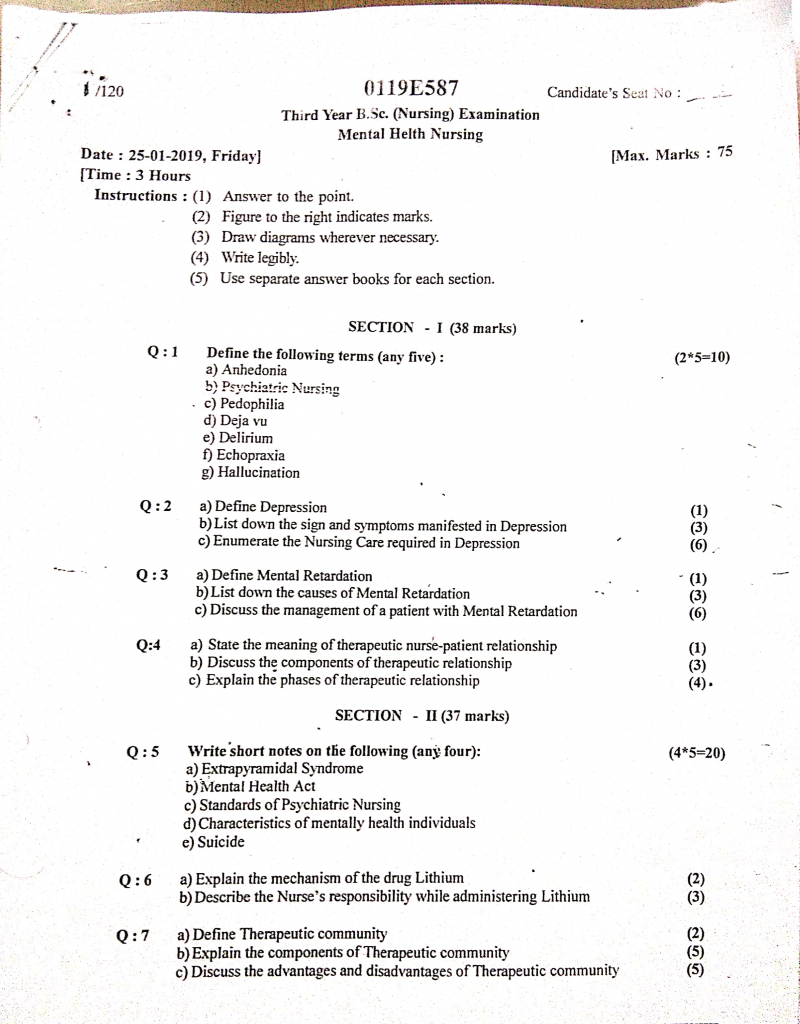
25/01/2019-B.SC-MENTAL HEALTH-PAPER DONE
Section 1 (38 marks)
Q.1 Define the following terms (any five) (2×5=10)
a) Anhedonia
- Anhedonia is a core symptom of depression and other mental health disorders, defined as the inability to experience pleasure or interest in activities that were once considered enjoyable or satisfying.
- It affects both social and physical aspects of life, such as loss of interest in hobbies, relationships, eating, or sexual activity, and reflects a dysfunction in the brain’s reward system, especially involving dopamine pathways.
b) Psychiatric nursing
- Psychiatric Nursing, also known as Mental Health Nursing, is a specialized field of nursing that focuses on the care, treatment, and rehabilitation of individuals with mental health disorders, emotional disturbances, and behavioral problems.
- It involves using therapeutic communication, psychosocial interventions, medication administration, and a holistic approach to help patients achieve optimal mental well-being, while also working closely with families and mental health teams to promote recovery and prevent relapse.
c) Pedophilia
- Pedophilia is a psychiatric disorder characterized by a persistent and intense sexual attraction or fantasies involving prepubescent children, typically under the age of 13 years.
- According to the DSM-5 (Diagnostic and Statistical Manual of Mental Disorders, 5th Edition), this condition is diagnosed when such thoughts, urges, or behaviors last for at least 6 months, and cause distress or impairment in social, occupational, or other important areas of functioning.
- It is considered a paraphilic disorder and poses serious ethical, legal, and psychological consequences, requiring professional psychiatric intervention.
d) Deja vu
- Déjà Vu is a psychological phenomenon in which an individual has the strong and uncanny feeling that they have already experienced a present situation, event, or environment, even though it is happening for the first time.
- It is a type of memory illusion and is commonly experienced in healthy individuals, but may also be associated with neurological conditions such as temporal lobe epilepsy.
- The term “déjà vu” is French for “already seen”, and it usually lasts only for a few seconds.
e) Delirium
- Delirium is an acute, sudden-onset, and fluctuating disturbance of consciousness that is characterized by impaired attention, confusion, disorganized thinking, and altered level of awareness of the environment.
- It is usually caused by an underlying medical condition, substance intoxication or withdrawal, infection, or metabolic imbalance, and it often occurs in elderly or critically ill patients.
- Delirium is considered a medical emergency and requires prompt assessment and treatment to prevent complications.
f) Echoprexia
- Echopraxia is a neurological and psychiatric symptom in which an individual involuntarily imitates or mimics the movements, gestures, or actions of another person.
- It is commonly associated with schizophrenia, autism spectrum disorders, Tourette’s syndrome, and certain neurological conditions, and is considered a form of automatic, non-purposeful behavior.
- Echopraxia reflects an impairment in the control of voluntary actions and may indicate underlying frontal lobe dysfunction or loss of inhibition in the brain.
g) Hallucination
- Hallucination is a false sensory perception that occurs without any external stimulus, meaning the person perceives something that is not actually present in the environment.
- It can involve any of the five senses, including:
- Auditory hallucinations (hearing voices or sounds) – most common in psychiatric disorders like schizophrenia
- Visual hallucinations (seeing things that are not there)
- Olfactory, gustatory, or tactile hallucinations (smelling, tasting, or feeling sensations without cause)
Q.2
a) Define depression (1)
Depression is a common mood disorder characterized by persistent sadness, loss of interest or pleasure in daily activities, along with emotional, cognitive, behavioral, and physical symptoms, that interfere with a person’s normal functioning and last for at least two weeks or more.
b) List down the sign and symptoms manifested in depression (3)
Depression is a mood disorder that presents with a wide range of emotional, cognitive, behavioral, and physical symptoms, which persist for more than two weeks and impair social, occupational, and personal functioning.
1️⃣ Persistent Low Mood or Sadness
The patient often experiences a continuous feeling of sadness, emptiness, or hopelessness, even without a clear reason.
2️⃣ Loss of Interest or Pleasure (Anhedonia)
There is a noticeable lack of interest or enjoyment in activities that were previously pleasurable, such as hobbies, work, or social interaction.
3️⃣ Fatigue or Loss of Energy
The individual frequently complains of feeling tired, weak, or physically drained, even after adequate rest or without much activity.
4️⃣ Sleep Disturbances
Patients may have insomnia (difficulty falling or staying asleep) or hypersomnia (excessive sleepiness or sleeping too much).
5️⃣ Appetite and Weight Changes
There is either a significant decrease or increase in appetite, which may lead to unexplained weight loss or gain.
6️⃣ Feelings of Worthlessness or Excessive Guilt
The person often expresses inappropriate guilt, low self-worth, or feelings of being a burden to others.
7️⃣ Difficulty in Concentration or Decision-Making
Patients frequently report poor memory, reduced attention span, or inability to think clearly or make decisions.
8️⃣ Psychomotor Changes
There may be psychomotor retardation (slowed movement, speech, and thinking) or psychomotor agitation (restlessness, fidgeting, pacing).
9️⃣ Recurrent Thoughts of Death or Suicide
The person may talk about wanting to die, express suicidal ideation, or may have made suicide attempts.
🔟 Social Withdrawal and Isolation
The patient often avoids social interactions, isolates themselves, and becomes disconnected from friends or family.
c) Enumerate the nursing care required in depression (6)
Depression is a serious mood disorder that requires comprehensive nursing care focused on promoting safety, emotional support, therapeutic communication, and medication adherence. The nurse plays a crucial role in observing behavioral changes, preventing self-harm, and helping the patient regain self-worth and functioning.
1️⃣ Establishing a Therapeutic Nurse–Patient Relationship
- The nurse should develop a warm, empathetic, honest, and non-judgmental relationship with the patient to promote trust and emotional security, which are essential for therapeutic progress.
- The nurse must demonstrate genuineness and active listening, validating the patient’s feelings without giving false reassurance.
- Regular presence, maintaining eye contact, and using open-ended and supportive communication techniques are key in encouraging the patient to express feelings of sadness, guilt, or worthlessness.
- This phase may take time, as depressed patients may initially show resistance, lack of interest, or apathy, but consistent and patient-centered communication builds rapport.
2️⃣ Ensuring Safety and Suicide Prevention
- The nurse must continuously assess the patient for suicidal thoughts, behaviors, or verbal cues such as “I want to die” or “My family would be better off without me.”
- If suicidal ideation is present, the nurse must implement suicide precautions, including close observation (1:1 if needed), removal of sharp objects, belts, cords, and toxic substances.
- The environment should be kept safe, low-stimulus, and calm, and the nurse should document any verbal or behavioral warning signs.
- The nurse must immediately report any active suicide plans to the physician or mental health team and collaborate on emergency interventions.
3️⃣ Promoting Daily Routine and Self-Care Activities
- Depressed patients often neglect basic hygiene, grooming, and eating due to lack of motivation and psychomotor retardation, so the nurse should provide gentle reminders, encouragement, and physical assistance when needed.
- Assist the patient with bathing, brushing teeth, dressing appropriately, combing hair, and gradually encourage independence as mood improves.
- Reinforce participation in basic chores, walking, recreational tasks, or occupational therapy, to re-establish a sense of purpose and structure.
- The nurse should celebrate small achievements, like brushing teeth without prompting, to boost confidence.
4️⃣ Monitoring Nutrition and Fluid Balance
- Depression often leads to loss of appetite, anorexia, or overeating, so the nurse should monitor daily food intake, weight changes, and hydration status.
- Offer nutritious, easy-to-digest meals in small, frequent portions, and encourage the patient to eat in a group or supervised setting to avoid isolation.
- In patients with severe weight loss or risk of malnutrition, consult with a dietitian, and initiate nutritional supplements or tube feeding as ordered.
5️⃣ Medication Administration and Monitoring
- The nurse must ensure the correct administration of prescribed antidepressants (e.g., SSRIs, TCAs, SNRIs) and explain their purpose, dosage, and possible side effects.
- The nurse should observe for early side effects such as nausea, drowsiness, headache, or increased anxiety, and monitor for serious risks like serotonin syndrome or suicidal ideation during early therapy.
- Educate the patient and family that antidepressants may take 2–4 weeks to show effects and should not be stopped abruptly without medical advice.
- The nurse must reinforce medication adherence, even if the patient feels better, to prevent relapse.
6️⃣ Encouraging Emotional Expression and Ventilation
- The nurse should create a non-threatening and confidential environment where the patient feels safe to talk about sadness, grief, guilt, anger, or fear.
- Use communication strategies like reflection, summarizing, paraphrasing, and silence to facilitate open expression.
- Avoid giving false assurance like “Everything will be fine,” instead use empathetic responses such as “It sounds like you’re feeling very overwhelmed.”
7️⃣ Involving in Social and Therapeutic Activities
- The nurse should encourage the patient to participate in group therapy, recreational therapy, occupational therapy, or mild physical activities based on their interest and energy levels.
- Involvement in creative tasks like painting, music, or gardening provides emotional relief and distracts from negative thinking.
- Group therapy helps reduce feelings of loneliness and enhances peer support and interaction skills.
8️⃣ Enhancing Self-Esteem and Positive Thinking
- Depression is often associated with feelings of worthlessness, guilt, and low self-image, so the nurse should help the patient recognize positive qualities, small achievements, and past strengths.
- Help the patient set realistic, achievable goals, and praise each step of progress, no matter how small.
- Encourage use of affirmations, self-monitoring of mood, and practice of relaxation or mindfulness techniques.
9️⃣ Providing Psychoeducation to Patient and Family
- The nurse must educate the patient and family about the nature of depression, course of illness, available treatments, and relapse prevention strategies.
- Address common misconceptions like “depression is a sign of weakness” or “medicines are addictive,” using scientific, respectful explanations.
- Family members should be taught to observe mood patterns, respond calmly to emotional crises, and encourage treatment adherence.
🔟 Planning for Discharge and Community Support
- The nurse must ensure that discharge planning includes follow-up appointments, therapy schedules, and community mental health referrals.
- Encourage the patient and family to connect with support groups, helplines, or NGOs offering counseling and rehabilitation.
- Educate about warning signs of relapse, such as social withdrawal, sleep disturbances, or suicidal thoughts, and guide on when to seek help.
Q.3
a) Define mental retardation (1)
Mental retardation (currently referred to as Intellectual Disability) is a neurodevelopmental disorder characterized by significantly below-average intellectual functioning (IQ below 70) accompanied by deficits in adaptive behavior, such as communication, self-care, social skills, and daily living activities, which begin during the developmental period, usually before the age of 18 years. It affects the individual’s ability to learn, reason, and function independently, requiring ongoing support and care.
b) List down the causes of mental retardation (3)
Mental retardation, or intellectual disability, can result from a wide range of biological, genetic, environmental, prenatal, perinatal, and postnatal factors. These factors interfere with normal brain development, leading to impaired intellectual and adaptive functioning.
1️⃣ Genetic and Chromosomal Causes
- It includes conditions caused by abnormalities in genes or chromosomes, such as:
- Down syndrome (Trisomy 21)
- Fragile X syndrome
- Phenylketonuria (PKU)
- Tuberous sclerosis
- Rett syndrome
- These disorders are either inherited or result from spontaneous genetic mutations during fetal development.
2️⃣ Prenatal Causes (Before Birth)
- These causes affect brain development while the baby is still in the womb, including:
- Maternal infections such as rubella, toxoplasmosis, syphilis, cytomegalovirus (CMV)
- Exposure to harmful substances like alcohol (Fetal Alcohol Syndrome), drugs, or toxins
- Severe malnutrition or iodine deficiency during pregnancy
- Uncontrolled maternal diabetes or hypertension
- Radiation or trauma during pregnancy
3️⃣ Perinatal Causes (During Birth)
- These include complications that occur around the time of delivery, such as:
- Birth asphyxia (lack of oxygen during delivery)
- Prolonged or obstructed labor
- Low birth weight or prematurity
- Intracranial hemorrhage
- Neonatal jaundice (kernicterus) leading to brain damage
4️⃣ Postnatal Causes (After Birth)
- Factors affecting brain development after birth may include:
- Severe head injury or brain trauma
- Central nervous system infections like meningitis or encephalitis
- Seizure disorders (e.g., epilepsy)
- Severe protein-energy malnutrition (PEM)
- Environmental deprivation, such as extreme neglect or lack of stimulation
5️⃣ Psychosocial and Environmental Causes
- These include non-biological factors such as:
- Extreme poverty, poor parenting, or emotional neglect
- Lack of early educational exposure or social interaction
- Institutionalization without adequate mental stimulation
c) Discuss the management of a patient with mental retardation (6)
1️⃣ Medical Management
- The first step in management is to conduct a comprehensive medical evaluation, including neurological assessment, IQ testing, genetic testing (e.g., karyotyping), and metabolic screening to determine the severity and possible cause of intellectual disability.
- If the disability is due to a treatable condition like hypothyroidism, phenylketonuria, or hydrocephalus, appropriate treatment such as thyroxine therapy, dietary modification, or neurosurgical intervention must be initiated early to prevent further intellectual decline.
- The physician must evaluate for co-existing physical illnesses such as vision or hearing impairments, seizures, or physical disabilities, which may worsen the level of disability if unaddressed.
- For patients showing behavioral problems like hyperactivity, aggression, self-injury, or sleep disturbances, psychotropic medications such as antipsychotics (e.g., risperidone), mood stabilizers (e.g., valproate), or sedatives may be used cautiously with regular monitoring for side effects.
- Regular follow-ups are necessary to monitor growth, development, medication effects, and to modify care plans as the child grows.
2️⃣ Psychological and Behavioral Management
- Behavior modification techniques such as positive reinforcement, modeling, shaping, token economy, and time-out strategies are used to improve behavior, reduce aggression, and develop attention span.
- If the patient has mild or moderate disability, they may benefit from structured cognitive-behavioral therapy (CBT), where they are trained to identify feelings, respond to triggers, and build coping skills.
- Patients with emotional problems such as low self-esteem, frustration, anxiety, or withdrawal must receive individual or group counseling from a trained clinical psychologist.
- Play therapy and art therapy can be useful for children with limited verbal abilities, helping them express emotions and interact meaningfully.
- Family members should also be given psychological counseling to help them adjust emotionally, develop positive attitudes, and understand realistic expectations.
3️⃣ Educational and Special Education Management
- Children should be enrolled in special education centers or inclusive schools where learning is tailored to their cognitive level, attention span, and physical abilities.
- Individualized Education Plans (IEPs) must be designed for each child, specifying their learning objectives, skill training, behavior goals, and monitoring criteria.
- Education should include basic literacy, numeracy, personal hygiene training, money handling, community safety, and social communication skills.
- Speech therapy is necessary for those with delayed language development or speech defects, while occupational therapy supports improvement in motor skills and daily living activities.
- Sensory stimulation techniques and visual learning tools like picture cards, apps, and colored charts are especially effective for children with limited attention or verbal skills.
4️⃣ Vocational Training and Social Rehabilitation
- For adolescents and adults, vocational rehabilitation is essential to prepare them for independent or semi-supported living. Training should be based on their strengths, such as gardening, cooking, simple packing, laundry, carpentry, or assembling tasks.
- Pre-vocational training teaches time management, basic discipline, workplace hygiene, and safety awareness, which are essential to function in any job.
- Based on the person’s ability, they may be placed in sheltered workshops, group employment centers, or open employment with supervision.
- Social rehabilitation must include training in communication, public behavior, use of public transport, community participation, and conflict resolution.
- Patients should be encouraged to participate in community outings, special Olympics, cultural programs, and recreational activities to build confidence and social integration.
5️⃣ Family Counseling and Parental Training
- Parents must be helped to accept the child’s condition without guilt, blame, or frustration, and educated about the nature, causes, and prognosis of intellectual disability.
- They should be trained to provide structured routines at home, use positive reinforcement at home, and encourage skill development in daily living.
- Family counseling helps to prevent emotional burnout, neglect, or abuse, which may sometimes happen in households with limited support.
- Sibling counseling is also important to prevent jealousy, resentment, or neglect among other children.
- Support groups and parent associations like PARIVAAR, Special Olympics Bharat, and local NGOs provide emotional, legal, financial, and community support.
6️⃣ Nursing Management
- The nurse must begin with a thorough assessment of the patient’s mental status, developmental level, physical health, emotional needs, and family background.
- Daily nursing care includes assisting in feeding, bathing, grooming, toileting, dressing, and ensuring personal hygiene and safety, especially for moderate to profound disability.
- The nurse should create a structured, predictable, and low-stress environment, which reduces anxiety and behavioral problems.
- Nurses play a vital role in monitoring drug therapy, educating caregivers on side effects and adherence, and reporting unusual behaviors or deterioration.
- The nurse must use simple language, visual cues, repetition, and reward systems when communicating with the patient.
- During hospitalization, the nurse ensures safety protocols, prevents elopement or self-injury, and promotes participation in recreational or therapy activities.
- The nurse educates the family about home-based care, community resources, legal rights, and the importance of early intervention and long-term planning.
Q.4
a) State the meaning of therapeutic nurse patient relationship (1)
- The therapeutic nurse–patient relationship is a professional, purposeful, and goal-oriented interaction between a nurse and a patient that is designed to promote the patient’s mental, emotional, and physical well-being.
- It is based on trust, empathy, respect, confidentiality, and professional boundaries, and helps the patient to cope with illness, express emotions, modify behavior, and work toward recovery through therapeutic communication and mutual collaboration.
b) Discuss the components of therapeutic relationship (3)
1️⃣ Trust
- Trust is the foundation of a therapeutic relationship, where the patient believes that the nurse will act in their best interest, maintain confidentiality, and provide safe, competent care.
- It is established through consistency, honesty, reliability, empathy, and non-judgmental behavior from the nurse.
- Without trust, patients may withhold information, resist treatment, or show non-cooperation.
2️⃣ Respect (Unconditional Positive Regard)
- Respect refers to the nurse’s ability to accept the patient as a unique individual with dignity, regardless of their condition, background, or behavior.
- The nurse demonstrates respect by listening attentively, addressing the patient politely, maintaining privacy, and avoiding labeling or judgment.
- Respect builds the patient’s self-esteem and emotional safety, essential for open communication.
3️⃣ Empathy
- Empathy is the ability to understand and feel what the patient is experiencing emotionally, without becoming emotionally overwhelmed.
- Unlike sympathy (feeling sorry), empathy helps the nurse to connect with the patient’s emotional world and respond with compassion and understanding.
- It promotes trust, emotional expression, and healing in the patient.
4️⃣ Genuineness (Authenticity)
- Genuineness means the nurse must be honest, transparent, and emotionally present in their interaction with the patient.
- A genuine nurse expresses real concern, avoids false reassurance, and does not hide behind a professional mask.
- This creates a safe and authentic space where the patient feels valued and heard.
5️⃣ Professional Boundaries
- Maintaining boundaries ensures that the relationship remains therapeutic, ethical, and professional, not personal or exploitative.
- Boundaries help the nurse to avoid dual relationships, favoritism, dependency, or inappropriate behavior.
- The nurse must always remember that the relationship exists to benefit the patient, not to meet the nurse’s emotional or social needs.
6️⃣ Confidentiality
- Confidentiality refers to the nurse’s responsibility to protect the patient’s private information and not disclose it without proper consent or legal requirement.
- It builds trust and emotional safety, and helps patients to speak freely about their thoughts and feelings.
- Exceptions to confidentiality include situations involving risk of harm to self or others.
7️⃣ Therapeutic Communication
- Therapeutic communication involves the use of active listening, open-ended questions, silence, reflection, and clarification to help the patient express themselves.
- The nurse must use verbal and non-verbal techniques that promote trust, insight, and emotional release.
- It is goal-oriented, non-judgmental, and focused on the patient’s healing and well-being.
8️⃣ Mutual Goal Setting
- In a therapeutic relationship, both nurse and patient must collaboratively identify goals of care, such as reducing anxiety, improving coping skills, or increasing social interaction.
- Mutual goal setting increases the patient’s involvement, motivation, and accountability in the healing process.
- Goals must be realistic, measurable, and individualized.
9️⃣ Rapport
- Rapport is the emotional connection and mutual understanding between nurse and patient that creates a comfortable and trusting environment.
- It is built through attentive listening, empathy, patience, and consistent presence.
- Strong rapport helps patients to open up and participate actively in the therapeutic process.
c) Explain the phases of therapeutic relationship (4)
The therapeutic nurse–patient relationship is a planned, goal-directed, and professional interaction between a nurse and a patient, especially in mental health settings, aimed at promoting emotional healing, trust, and behavior change. This relationship is based on empathy, respect, confidentiality, and professional boundaries and evolves through four main phases.
1️⃣ Pre-Interaction Phase (Preparation Phase)
- This is the phase that occurs before the nurse meets the patient face-to-face, and it involves self-reflection, preparation, and planning by the nurse.
- The nurse reviews the patient’s medical history, diagnosis, and background, and prepares emotionally and mentally to meet the patient.
- The nurse also identifies potential biases or anxieties and sets clear goals and boundaries for the upcoming interaction.
- It is important in this phase that the nurse develops awareness about maintaining confidentiality, professionalism, and empathy.
2️⃣ Orientation Phase (Introductory Phase)
- This is the phase when the nurse first meets the patient and establishes the foundation of the therapeutic relationship.
- The nurse introduces herself and explains her role, purpose of the relationship, and duration of interaction, creating clarity and safety for the patient.
- The nurse begins to build trust and rapport through active listening, open communication, and non-judgmental behavior.
- During this phase, assessment is performed, goals of therapy are set, and the patient’s needs and concerns are explored.
- Confidentiality, boundaries, and the patient’s rights are also discussed to ensure mutual understanding and respect.
3️⃣ Working Phase (Therapeutic Phase)
- This is the longest and most active phase where therapeutic work is done and the nurse helps the patient explore feelings, thoughts, behaviors, and problems.
- The nurse encourages expression of emotions, identification of coping mechanisms, and helps the patient develop new skills, behaviors, and insight.
- The nurse uses various therapeutic techniques such as active listening, empathy, confrontation, clarification, and behavior modification.
- This phase may involve emotional resistance, transference, or regression, which the nurse must handle professionally.
- The focus remains on goal-directed action and patient participation, helping them move towards recovery or adjustment.
4️⃣ Termination Phase (Resolution Phase)
- This is the final phase where the therapeutic relationship comes to an end due to discharge, goal completion, or transfer.
- The nurse helps the patient reflect on progress, reinforces positive coping mechanisms, and prepares them for independence or community reintegration.
- It is common for patients to feel sadness, fear, or dependence, which the nurse must address sensitively.
- The nurse must also evaluate the effectiveness of the interventions, provide follow-up instructions, and ensure continuity of care.
- Termination should be done ethically and respectfully, emphasizing the patient’s growth and autonomy.
Section 2 (37 marks)
Q.5 Write short notes on the following (any four) (4×5=20)
a) Extrapyramidal syndrome
Definition of EPS
- Extrapyramidal symptoms (EPS) are drug-induced movement disorders that result from interference with the extrapyramidal system—the part of the brain responsible for involuntary movements, posture, and coordination.
- EPS typically occurs as a side effect of antipsychotic (especially typical/first-generation) medications like haloperidol or chlorpromazine.
Types of Extrapyramidal Symptoms
1️⃣ Acute Dystonia
- It is a sudden onset of involuntary muscle contractions, often affecting the face, neck, eyes, and tongue.
- It is commonly seen within hours to days of starting or increasing the dose of antipsychotics.
- Symptoms include torticollis (twisting of neck), oculogyric crisis (upward deviation of eyes), and jaw spasms.
2️⃣ Parkinsonism (Drug-induced Parkinsonism)
- It is a condition resembling Parkinson’s disease and typically appears within days to weeks of treatment.
- Symptoms include tremors, rigidity, bradykinesia (slowness of movement), shuffling gait, and mask-like facial expression.
3️⃣ Akathisia
- It is a feeling of inner restlessness with an urge to move constantly, such as pacing, fidgeting, or inability to sit still.
- It usually appears within a few days to weeks after initiating treatment.
- Patients may feel anxious or irritable due to the compulsion to move.
4️⃣ Tardive Dyskinesia (TD)
- It is a late-onset, often irreversible movement disorder that appears after months or years of antipsychotic use.
- Symptoms include involuntary, repetitive movements of the face, tongue (like lip-smacking, tongue thrusting), limbs, or trunk.
- Risk increases with long-term use of typical antipsychotics, especially in older adults.
5️⃣ Tardive Dystonia & Tardive Akathisia
- These are chronic and more severe forms of dystonia and akathisia that develop after long-term use of antipsychotic medications.
- They may persist even after discontinuing the drug.
Causes and Risk Factors
- Use of typical (first-generation) antipsychotics like haloperidol, fluphenazine, chlorpromazine.
- High doses or rapid dose escalation of antipsychotic medication.
- Long-term use of antipsychotics.
- Elderly patients, females, and those with brain injury are more susceptible.
- Genetic predisposition may also play a role.
Pathophysiology
- EPS result from dopamine D2 receptor blockade in the nigrostriatal pathway of the brain.
- This leads to dopamine deficiency, which disrupts the normal balance between dopamine and acetylcholine in the basal ganglia, causing abnormal involuntary movements.
Clinical Features
- Muscle stiffness, tremor
- Facial grimacing, jaw clenching
- Uncontrolled tongue movement
- Inner restlessness (akathisia)
- Abnormal posture or gait
- Drooling or rigidity
- Anxiety and distress due to movement difficulty
Diagnosis
- Primarily clinical diagnosis based on history of antipsychotic drug use and observed symptoms.
- Use of rating scales like AIMS (Abnormal Involuntary Movement Scale) for tardive dyskinesia.
- Differential diagnosis to rule out neurological conditions like Parkinson’s disease.
Medical Management
- Anticholinergic drugs like benztropine or trihexyphenidyl are used for dystonia and Parkinsonism.
- Beta-blockers (like propranolol) or benzodiazepines (like lorazepam) are used for akathisia.
- Switching to atypical (second-generation) antipsychotics like clozapine or quetiapine may reduce EPS.
- Tetrabenazine or valbenazine may be used for tardive dyskinesia.
- Dose reduction or discontinuation of the offending drug is considered if EPS is severe.
Nursing Management
✅ 1. Early identification and monitoring:
The nurse must closely monitor the patient for any signs of involuntary movements, restlessness, or stiffness, especially during the first few weeks of treatment.
✅ 2. Medication administration and education:
The nurse should administer antiparkinsonian agents as prescribed and teach the patient about the importance of medication adherence.
✅ 3. Emotional support:
The nurse should provide reassurance and emotional support to reduce anxiety and improve coping with distressing symptoms.
✅ 4. Patient safety measures:
Ensure a safe environment by assisting the patient during ambulation or in case of postural instability due to Parkinsonism or dystonia.
✅ 5. Reporting and collaboration:
The nurse must promptly report any EPS symptoms to the physician and collaborate for medication review or dose adjustment.
✅ 6. Health teaching:
Educate the patient and family members about the signs of EPS and the importance of timely reporting.
✅ 7. Encourage fluid intake and nutrition:
Monitor for weight loss or difficulty in chewing/swallowing (especially in tardive dyskinesia) and support with dietary modifications as needed.
b) Mental health act
The Mental Healthcare Act, 2017 is a comprehensive and rights-based legislation enacted by the Government of India, which aims to provide accessible, affordable, and quality mental healthcare services while protecting the dignity, rights, and autonomy of persons with mental illness.
It came into effect on July 7, 2018, and replaced the outdated Mental Health Act, 1987. It brings Indian mental health legislation in alignment with the United Nations Convention on the Rights of Persons with Disabilities (UNCRPD), to which India is a signatory.
Main Objectives of the Act
- It ensures that every person has the right to access mental health services without discrimination based on gender, caste, religion, or socioeconomic status.
- It guarantees the protection and promotion of the rights of persons with mental illness, including their right to dignity, autonomy, and participation in decision-making.
- It emphasizes the decriminalization of suicide, considering it as a symptom of mental illness requiring care, not punishment.
- It promotes the availability of community-based mental health services, rehabilitation, and social inclusion for mentally ill persons.
- It establishes legal frameworks for advance directives and nominated representatives, allowing patients to make future treatment decisions in advance.
Salient Features of the Mental Healthcare Act, 2017
✅ 1. Right to Access Mental Healthcare (Section 18)
- Every citizen has the right to receive affordable and quality mental healthcare services provided by government institutions, free of cost.
- This includes outpatient and inpatient care, emergency services, medications, rehabilitation, and supported housing.
- The government is legally obligated to make these services available in every district of the country.
✅ 2. Right to Live with Dignity (Section 20)
- All persons with mental illness have the right to live a life of dignity, free from discrimination, abuse, and neglect, whether in hospitals, homes, or public settings.
- It also ensures that no one can be chained, isolated unnecessarily, or treated inhumanely in psychiatric institutions.
✅ 3. Right to Confidentiality (Section 23)
- Patients have the right to privacy and confidentiality regarding their diagnosis, treatment, and hospital records.
- Professionals are legally bound to not disclose any information without the patient’s consent, except in legally justified cases.
✅ 4. Right to Informed Consent and Participation (Section 22)
- All treatment must be done with the patient’s free and informed consent, where they are educated about diagnosis, treatment options, benefits, and risks.
- The patient has the right to accept or refuse treatment, and participate in care planning.
✅ 5. Advance Directive (Section 5–13)
- Any person can write an Advance Directive, stating their treatment preferences, refusal of certain interventions, or preferred hospital in case of future mental illness.
- The person can also appoint a Nominated Representative to make healthcare decisions on their behalf when they are unable to do so.
✅ 6. Decriminalization of Suicide (Section 115)
- The Act recognizes that suicide is often the result of mental distress, and declares that any person attempting suicide shall be presumed to be suffering from mental illness.
- Therefore, such individuals must be offered medical care, counseling, and rehabilitation, not legal punishment under Section 309 of IPC.
✅ 7. Rights During Admission and Treatment (Section 19, 86–91)
- The Act distinguishes between voluntary and involuntary admission of patients into mental health establishments.
- It ensures that involuntary admission must be reviewed by a Mental Health Review Board and must comply with strict legal safeguards.
- Patients have the right to appeal against wrongful admission or discharge.
✅ 8. Registration of Mental Health Establishments (Section 65–77)
- Every mental health hospital, clinic, or institution must be registered under the Act to ensure quality standards, qualified staff, ethical treatment, and clean infrastructure.
- Regular inspections and audits are required to prevent human rights violations in institutions.
✅ 9. Mental Health Review Board (MHRB)
- A quasi-judicial authority is established in each state and district to review patient complaints, protect rights, approve advance directives, and oversee involuntary admissions.
- The board consists of a judicial officer, psychiatrist, mental health professionals, and social worker or advocate.
✅ 1️⃣0. Promotion of Community-Based Mental Healthcare
- The Act promotes the decentralization of mental health services, encouraging day-care centers, halfway homes, rehabilitation centers, and support groups.
- It aims to rehabilitate mentally ill persons in the community, reducing the stigma of institutionalization.
Role of Nurse under the Mental Healthcare Act, 2017
- The nurse must respect and protect the legal rights of psychiatric patients, including informed consent, confidentiality, and dignity.
- Nurses should be aware of the types of admission (voluntary/involuntary) and assist in ensuring that legal protocols are followed.
- The nurse must help patients understand and execute advance directives, and communicate with the nominated representative.
- They are responsible for reporting abuse, negligence, or unethical practices to the Mental Health Review Board.
- Nurses play a vital role in educating patients and families about their rights under the Act, treatment options, and rehabilitation services.
- Psychiatric nurses also support the Act by documenting care properly, advocating for patients, and participating in policy and quality improvement in psychiatric settings.
c) Standards of Psychiatric nursing
- The standards of psychiatric nursing are professionally accepted guidelines that define the quality, ethics, scope, and responsibilities of a psychiatric nurse. These standards ensure that the nurse provides safe, ethical, patient-centered, and evidence-based care to individuals suffering from mental health disorders.
- They serve as a framework for clinical practice, guide nursing actions, and promote professional accountability. They are based on principles laid down by authorities like the Indian Nursing Council (INC), American Nurses Association (ANA), and WHO.
1️⃣ Standard I: Assessment
- The psychiatric nurse is responsible for conducting a comprehensive and continuous assessment of the client’s physical, psychological, emotional, spiritual, and social condition.
- This includes techniques like mental status examination (MSE), psychiatric history taking, risk assessment, behavioral observation, and family interviews.
- The nurse must assess the impact of environmental factors, substance use, trauma history, support system, and level of functioning in daily life.
- The assessment must be systematic, culturally sensitive, and individualized for each patient.
2️⃣ Standard II: Nursing Diagnosis
- After the assessment, the nurse must analyze the data to identify specific psychiatric nursing diagnoses using standardized language such as NANDA (North American Nursing Diagnosis Association).
- The diagnosis may include risk for self-harm, disturbed thought process, impaired social interaction, ineffective coping, sleep pattern disturbances, etc.
- These nursing diagnoses help to prioritize care needs and form the foundation for planning effective interventions.
3️⃣ Standard III: Outcome Identification
- The psychiatric nurse must identify short-term and long-term outcomes/goals in collaboration with the patient, family, and health team.
- Outcomes must be specific, measurable, achievable, relevant, and time-bound (SMART) and should reflect improvement in behavior, emotional regulation, safety, and functioning.
- Examples include: “Patient will verbalize feelings within 2 days” or “Patient will remain free from self-injury during hospitalization.”
4️⃣ Standard IV: Planning
- Based on the nursing diagnosis and expected outcomes, the nurse must formulate an individualized nursing care plan, addressing physical, emotional, social, and spiritual needs.
- Planning involves selecting evidence-based interventions, therapeutic strategies, safety measures, medication adherence plans, and discharge planning.
- The nurse also plans family involvement, psychoeducation, and referral services as needed.
5️⃣ Standard V: Implementation
- This includes executing the planned interventions, such as administering psychiatric medications, conducting counseling sessions, leading group therapy, managing crises, or using behavioral therapies.
- The nurse must also ensure safety measures, maintain a therapeutic milieu, and promote healthy coping mechanisms in patients.
- Implementation also involves health education, family guidance, documentation, and coordinating with the multidisciplinary team.
6️⃣ Standard VI: Evaluation
- The psychiatric nurse must evaluate the patient’s response to each intervention and compare it with the previously identified goals or outcomes.
- Evaluation must be continuous, reflective, and documented, and must involve feedback from the patient and family.
- Based on the results, the care plan must be modified, continued, or terminated appropriately to ensure progress.
7️⃣ Standard VII: Ethics and Legal Practice
- The psychiatric nurse must uphold ethical principles such as autonomy, non-maleficence, beneficence, confidentiality, informed consent, and justice.
- The nurse should also be aware of and follow mental health legislation such as the Mental Healthcare Act (India, 2017) regarding rights of patients, legal admission procedures, use of restraints, and discharge policies.
- The nurse must respect the dignity and human rights of all patients, regardless of diagnosis.
8️⃣ Standard VIII: Professional Development and Competence
- Nurses should regularly update their knowledge and skills through continuing education programs, seminars, workshops, conferences, and self-study.
- They must maintain competence in therapeutic communication, new psychiatric drugs, behavior modification techniques, and emerging trends in mental health.
- Professional development promotes career growth, job satisfaction, and high-quality patient care.
9️⃣ Standard IX: Collaboration and Interdisciplinary Approach
- The psychiatric nurse must work in close collaboration with psychiatrists, psychologists, social workers, occupational therapists, and other mental health professionals.
- This team approach ensures holistic and coordinated care, addressing all aspects of the patient’s recovery.
- Effective communication and mutual respect among team members are essential for the success of interdisciplinary care plans.
🔟 Standard X: Documentation
- The nurse must ensure timely, accurate, and clear documentation of all assessments, interventions, patient responses, behavioral observations, medication administration, and progress notes.
- Proper documentation serves as legal evidence, enhances continuity of care, and facilitates communication among care providers.
- It is a vital part of professional accountability and protects the nurse and institution from legal issues.
d) Characteristics of mentally health individuals
A mentally healthy individual is someone who has the ability to maintain a harmonious balance between thoughts, emotions, and behavior, and effectively adapt to life’s challenges. Mental health is not merely the absence of psychiatric illness, but the presence of psychological well-being, emotional resilience, personal satisfaction, and social efficiency.
1️⃣ Positive Self-Awareness and Realistic Self-Concept
- A mentally healthy individual possesses a clear understanding of their own identity, emotions, motives, strengths, and weaknesses without being overly self-critical or self-obsessed.
- They demonstrate self-acceptance, meaning they can live peacefully with their imperfections and have a realistic level of self-esteem.
2️⃣ Effective Stress Management and Coping Ability
- Mentally healthy individuals are able to tolerate stress, anxiety, and frustration without emotional breakdown or self-harming behavior.
- They exhibit healthy coping mechanisms such as seeking support, engaging in problem-solving, using relaxation techniques, or physical activities rather than resorting to escape, addiction, or violence.
- They can face difficult circumstances, disappointments, or loss with strength and resilience.
3️⃣ Stable and Balanced Emotions
- A mentally healthy person is able to express emotions appropriately, meaning their emotional responses are in proportion to the situation and not impulsive or suppressed.
- They can feel happiness, sadness, anger, or love without losing control and are able to regain emotional equilibrium after stress or trauma.
- They demonstrate emotional maturity, avoiding unnecessary conflicts and mood extremes.
4️⃣ Healthy Interpersonal Relationships
- Such individuals maintain positive, supportive, and respectful relationships with family members, friends, co-workers, and society at large.
- They show empathy, trust, tolerance, cooperation, and effective communication in social interactions.
- They are not overly dependent on others, yet they are open to seeking help and giving support when needed.
5️⃣ Rational Thinking and Sound Judgment
- Mentally healthy individuals possess the ability to think clearly, logically, and make decisions based on facts and reason, not on fear, bias, or emotion alone.
- They are able to analyze situations, foresee consequences, and choose appropriate responses.
- They have control over impulsive behaviors and avoid irrational fears or magical thinking.
6️⃣ Self-Motivation and Productive Living
- A mentally healthy person is goal-oriented, self-driven, and motivated to achieve personal and professional success.
- They engage in meaningful activities like work, education, volunteering, or hobbies, and maintain a sense of usefulness and fulfillment.
- They take responsibility for their life and work towards personal growth and improvement.
7️⃣ Adaptability and Flexibility
- Mentally healthy individuals can adjust to new environments, roles, and life transitions such as changes in job, relationships, or lifestyle.
- They are open to feedback and able to modify their thoughts or actions when needed, without becoming rigid or defensive.
- They embrace change with positivity and learn from past mistakes.
8️⃣ Social and Moral Responsibility
- They demonstrate a strong sense of ethics and responsibility towards society and uphold moral values and social norms.
- A mentally healthy person behaves with honesty, integrity, compassion, and respect for others’ rights and beliefs.
- They actively contribute to the well-being of others and maintain civic responsibility, such as obeying laws and participating in community service.
9️⃣ Self-Control and Discipline
- Such individuals maintain control over their impulses, desires, and emotions, avoiding harmful behaviors such as aggression, substance abuse, or reckless actions.
- They are capable of delaying gratification, maintaining focus, and following routines or long-term goals with discipline.
🔟 Sense of Inner Peace and Spiritual Well-being
- Many mentally healthy individuals possess a sense of spiritual grounding or inner peace, which may be rooted in religion, faith, nature, or personal values.
- They often practice self-reflection, meditation, or mindfulness, which helps them stay calm, hopeful, and centered during difficulties.
- This spiritual outlook contributes to their resilience, forgiveness, and purpose in life.
e) Suicide
Definition of Suicide
Suicide is defined as the act of intentionally causing one’s own death, usually as a result of severe psychological distress, mental illness, or crisis.
It is considered a psychiatric emergency and a major public health issue globally.
Types of Suicide (According to Durkheim’s Sociological Classification)
1️⃣ Egoistic Suicide
- It occurs in individuals who feel isolated or not integrated into society or a social group.
- Common in people with depression or loneliness.
2️⃣ Altruistic Suicide
- Occurs when an individual sacrifices their life for the group or society.
- Seen in soldiers, religious martyrs, or people in tightly bonded groups.
3️⃣ Anomic Suicide
- Happens due to sudden breakdown in social norms such as during economic crisis, divorce, or natural disaster.
- The person may feel hopeless or directionless.
4️⃣ Fatalistic Suicide
- Due to excessive regulation or oppression in life (e.g., prisoners, abused individuals).
- The person may feel life is unbearable and escape is impossible.
Causes / Risk Factors of Suicide
1️⃣ Psychiatric Illness
Depression, bipolar disorder, schizophrenia, substance abuse, and borderline personality disorder are major risk factors.
2️⃣ Psychological Factors
Hopelessness, impulsivity, low self-esteem, emotional distress, or childhood trauma.
3️⃣ Social and Cultural Factors
Social isolation, financial issues, family conflict, relationship breakups, academic failure.
4️⃣ Biological Factors
Low serotonin levels in the brain are linked to increased suicidal behavior.
5️⃣ Medical Illness
Chronic pain, cancer, or debilitating illnesses often contribute to suicidal ideation.
6️⃣ Past Suicide Attempts or Family History
Previous attempts or suicide in the family increase the risk.
7️⃣ Access to Means
Easy access to firearms, poisons, or medications facilitates suicide.
Warning Signs of Suicide (Verbal and Behavioral Cues)
- Talking about death, suicide, or expressing hopelessness.
- Giving away prized possessions or making a will.
- Withdrawing from family, friends, and social life.
- Sudden calmness after a depressive period.
- Saying things like “I want to die” or “They’ll be better off without me.”
Methods of Suicide (Means)
- Ingestion of poison or drugs
- Self-injury (cutting veins, stabbing)
- Jumping from heights
- Firearm use
- Drowning
- Burning
- Electrocution
- Jumping in front of a vehicle
Suicide Prevention Strategies
✅ Primary Prevention
- Mental health awareness campaigns
- School and college counseling programs
- Stress management and life skills education
✅ Secondary Prevention
- Early diagnosis and treatment of depression and mental illness
- Crisis helplines and suicide hotlines
- Psychological first aid during disasters
✅ Tertiary Prevention
- Support and follow-up for suicide survivors
- Support groups for families of suicide victims
- Long-term therapy and rehabilitation
Nursing Management in Suicidal Patients
1️⃣ Establish Therapeutic Relationship
- Build trust with empathy and non-judgmental communication.
- Maintain consistent, calm, and genuine presence.
2️⃣ Suicide Risk Assessment
- Assess for suicidal thoughts, plans, means, and history of attempts.
- Ask direct but sensitive questions like “Are you thinking about hurting yourself?”
3️⃣ Ensure Safety
- Place patient under close supervision (1:1 observation if needed).
- Remove harmful items like sharp objects, belts, cords, and toxic substances.
- Maintain a safe, low-stimulus environment.
4️⃣ Document Findings
- Keep clear records of assessments, verbal threats, behavior, and interventions.
5️⃣ Medication Administration
- Administer antidepressants or antipsychotics as prescribed and observe for side effects.
- Ensure medication compliance and prevent hoarding.
6️⃣ Family and Peer Involvement
- Educate family about warning signs and provide emotional support.
- Involve social workers or support groups if needed.
7️⃣ Crisis Intervention Techniques
- Use active listening, ventilation of feelings, problem-solving assistance, and reality orientation.
8️⃣ Referral and Follow-up
- Refer to psychiatric services, psychotherapy, or crisis centers.
- Ensure long-term follow-up to prevent recurrence.
Q.6
a) Explain the mechanism of the drug lithium (2)
1️⃣ Modulation of Neurotransmitters
- It is believed that lithium exerts its mood-stabilizing effects by modulating the levels of neurotransmitters, particularly by inhibiting dopamine and glutamate, which are associated with manic symptoms, and enhancing the action of GABA and serotonin, which produce calming effects.
- This balance helps reduce excessive excitatory transmission in mania and improves emotional regulation in depression.
2️⃣ Inhibition of Inositol Monophosphatase (IMPase)
- Lithium inhibits the enzyme inositol monophosphatase, which leads to the depletion of inositol triphosphate (IP3) and diacylglycerol (DAG)—both of which are important secondary messengers in cell signaling pathways.
- By disrupting this phosphatidylinositol signaling cascade, lithium dampens hyperactive neuronal responses, especially those associated with mania and agitation.
3️⃣ Neuroprotective and Neuroplastic Effects
- It has been shown that lithium enhances neurogenesis and increases levels of brain-derived neurotrophic factor (BDNF), which helps in protecting neurons from damage and promoting neural repair.
- This neuroprotective mechanism may contribute to long-term stabilization of mood and cognitive function in bipolar patients.
4️⃣ Regulation of Ion Transport:
- Lithium can alter the movement of sodium (Na⁺) and potassium (K⁺) ions across cell membranes, particularly in neurons.
- It competes with sodium ions and affects membrane potential and neuronal excitability, thereby reducing abnormal electrical activity associated with mood swings.
5️⃣ Inhibition of Glycogen Synthase Kinase-3 (GSK-3):
- Lithium inhibits the enzyme GSK-3, which is involved in numerous cellular processes including circadian rhythm, neuronal survival, and gene expression.
- Inhibiting GSK-3 is believed to contribute to mood stabilization and anti-suicidal effects.
b) Describe the nurses responsibility while administering lithium (3)
1️⃣ Assessment Before Administration
- The nurse should assess the patient’s history of renal, thyroid, and cardiovascular disease, as lithium can adversely affect these systems.
- It is important to check baseline serum lithium levels, renal function tests (creatinine, BUN), thyroid function (TSH), and electrolyte levels (especially sodium) before initiating therapy.
- The nurse should verify that the patient is not dehydrated or on a low-sodium diet, as both increase the risk of lithium toxicity.
2️⃣ Correct Administration
- The nurse must ensure lithium is given with food or after meals to minimize gastrointestinal irritation.
- The prescribed dose and schedule should be strictly followed, as lithium must be taken consistently at the same time each day.
- The nurse should avoid crushing or chewing extended-release tablets and ensure the patient swallows them whole.
3️⃣ Monitoring During Treatment
- The nurse should monitor serum lithium levels regularly (initially every 5–7 days, then every 2–3 months) to maintain therapeutic levels (0.6–1.2 mEq/L).
- The nurse should observe for signs of lithium toxicity, such as nausea, vomiting, diarrhea, tremors, confusion, muscle weakness, and blurred vision.
- Continuous monitoring of urine output, hydration status, weight, and blood pressure is essential during therapy.
4️⃣ Patient Education
- The nurse should educate the patient to maintain a consistent intake of dietary sodium and fluids (2–3 liters/day) to prevent fluctuations in lithium levels.
- The patient must be informed to report early signs of toxicity and not to take NSAIDs, diuretics, or ACE inhibitors without consulting the physician, as these can increase lithium levels.
- The nurse should counsel the patient about avoiding sudden lifestyle changes, like extreme dieting, fasting, or dehydration (e.g., during fever, vomiting, or sweating).
5️⃣ Documentation and Communication
- The nurse must document the administered dose, time, lithium level results, patient symptoms, and any side effects observed.
- Any abnormal findings or potential signs of toxicity should be immediately reported to the physician for further evaluation.
- Nurses must also coordinate with lab personnel to ensure timely collection and processing of blood samples for lithium monitoring.
6️⃣ Managing Side Effects and Emergencies
- The nurse should be prepared to withhold the dose and notify the physician if signs of toxicity are present.
- In case of severe toxicity, the nurse may assist in initiating emergency interventions such as gastric lavage, IV fluids, or dialysis if prescribed.
- The nurse should provide emotional support to the patient and family, especially during the adjustment period when side effects like tremors or mild GI discomfort may occur.
Q.7
a) Define therapeutic community (2)
- A Therapeutic Community (TC) is a structured, participative, and group-based psychiatric treatment environment where patients and healthcare professionals live, interact, and work together, using the community itself as the main tool for therapeutic change and rehabilitation.
- It is designed to help patients develop social skills, emotional insight, responsibility, and independence through shared decision-making, open communication, and mutual support in a democratic setting.
b) Explain the components of therapeutic community (5)
1️⃣ Democratic Participation
- It is the component where every member of the therapeutic community—staff and patients—has a voice in the operation and management of the community, ensuring equality and shared authority.
- It encourages collective problem-solving, which develops decision-making abilities and prepares patients for social reintegration.
- It allows patients to develop leadership skills and experience accountability, which strengthens their self-esteem and sense of social identity.
2️⃣ Shared Responsibility
- It refers to dividing roles and responsibilities among all members of the community so that each person contributes meaningfully to daily activities like cleaning, cooking, organizing programs, or supporting peers.
- It helps individuals rebuild a sense of purpose and structure, especially those who have experienced long-term dependence or isolation.
- Shared responsibility builds a culture of cooperation, where each member learns the value of teamwork and collective growth.
3️⃣ Group Therapy and Community Meetings
- It involves regularly scheduled sessions where patients share their feelings, receive feedback, and learn social skills, guided by trained professionals.
- It helps in the ventilation of suppressed emotions, development of insight, and recognition of maladaptive patterns of thinking and behavior.
- These meetings provide a platform for conflict resolution, fostering negotiation skills and emotional maturity in a safe setting.
4️⃣ Open Communication
- It emphasizes the need for honest, respectful, and emotionally expressive interaction among patients and staff in both formal and informal settings.
- Open communication reduces the fear of rejection or punishment, allowing patients to express vulnerabilities and seek support.
- It helps build trust, transparency, and a supportive atmosphere, which are essential for therapeutic growth and self-discovery.
5️⃣ Reality Confrontation
- This component involves constructively challenging each other’s inappropriate behavior or irrational thoughts, helping patients face the consequences of their actions.
- It encourages peer accountability and personal reflection, which helps individuals correct their behavior without feeling attacked.
- It strengthens the patient’s ability to cope with criticism and feedback, which is vital for real-world functioning after discharge.
6️⃣ Social Learning
- It is the process by which patients observe, imitate, and model positive behaviors and social interactions within the community.
- It allows for experiential learning, where patients understand acceptable behavior by seeing its effect on others and on themselves.
- Social learning fosters interpersonal sensitivity, empathy, and adaptive behavior, which are important for maintaining relationships outside the hospital.
7️⃣ Structure and Routine
- It involves designing a well-regulated schedule of therapeutic, occupational, recreational, and communal activities, reducing aimlessness and providing purpose.
- A consistent daily routine reduces anxiety and builds discipline, which is crucial for patients who have previously lived in disorganized or chaotic environments.
- It gives patients a sense of time orientation, stability, and control, which are necessary for psychological healing and recovery.
8️⃣ Staff as Role Models
- Staff members demonstrate healthy coping strategies, respectful communication, emotional regulation, and ethical behavior, which patients can observe and emulate.
- Their behavior sets the tone for the environment and helps develop therapeutic boundaries and trust.
- Staff act as emotional anchors, offering support while guiding patients through personal growth and social adjustment.
c) Discuss the advantages and disadvantages of therapeutic community (5)
Advantages of Therapeutic Community
1️⃣ It promotes active participation of patients in their own treatment, which enhances self-confidence, responsibility, and independence.
2️⃣ It encourages open communication and emotional expression through group activities, which helps patients develop healthy interpersonal skills and trust.
3️⃣ It creates a supportive environment where patients help each other, which reduces isolation, increases social skills, and fosters empathy.
4️⃣ It provides a democratic setup, where all members (patients and staff) are involved in decision-making, leading to a sense of empowerment and equality.
5️⃣ It helps patients observe and correct their own behavior through peer feedback, which enhances insight and motivation for change.
6️⃣ It allows round-the-clock therapeutic interaction, not limited to therapy sessions alone, making treatment more holistic and continuous.
7️⃣ It reduces dependence on medication, as behavioral and social interventions become central to care, improving long-term coping.
8️⃣ It prepares patients for re-entry into society, as the structured routine, responsibilities, and interactions simulate real-life environments.
9️⃣ It is especially helpful for patients with chronic mental illness, substance abuse disorders, and personality disorders, where long-term behavior modification is essential.
Disadvantages of Therapeutic Community
1️⃣ It may not be suitable for acutely ill or highly psychotic patients, as they may not be able to participate meaningfully in group decisions and activities.
2️⃣ It requires long-term commitment and patience, which may not be feasible for all patients due to personal, financial, or social reasons.
3️⃣ There is a risk of peer pressure or group conflict, which may negatively affect vulnerable patients if not properly supervised.
4️⃣ Staff need special training in group dynamics, therapeutic communication, and crisis handling, which may not always be available.
5️⃣ Some patients may resist structure or rules, making them non-cooperative or disruptive in the community setting.
6️⃣ It may be emotionally intense, as patients are encouraged to confront their behaviors and emotions openly, which some may find overwhelming.
7️⃣ Resources, time, and space requirements are high, as therapeutic communities need proper housing, group facilities, and staff availability.
8️⃣ Confidentiality concerns may arise, especially when personal issues are shared in group settings, requiring strict ethical guidelines.