31/01/2018-B.SC-MEDICAL SURGICAL-2-UPLOAD PAPER NO.3
PAPER SOLUTION NO.3
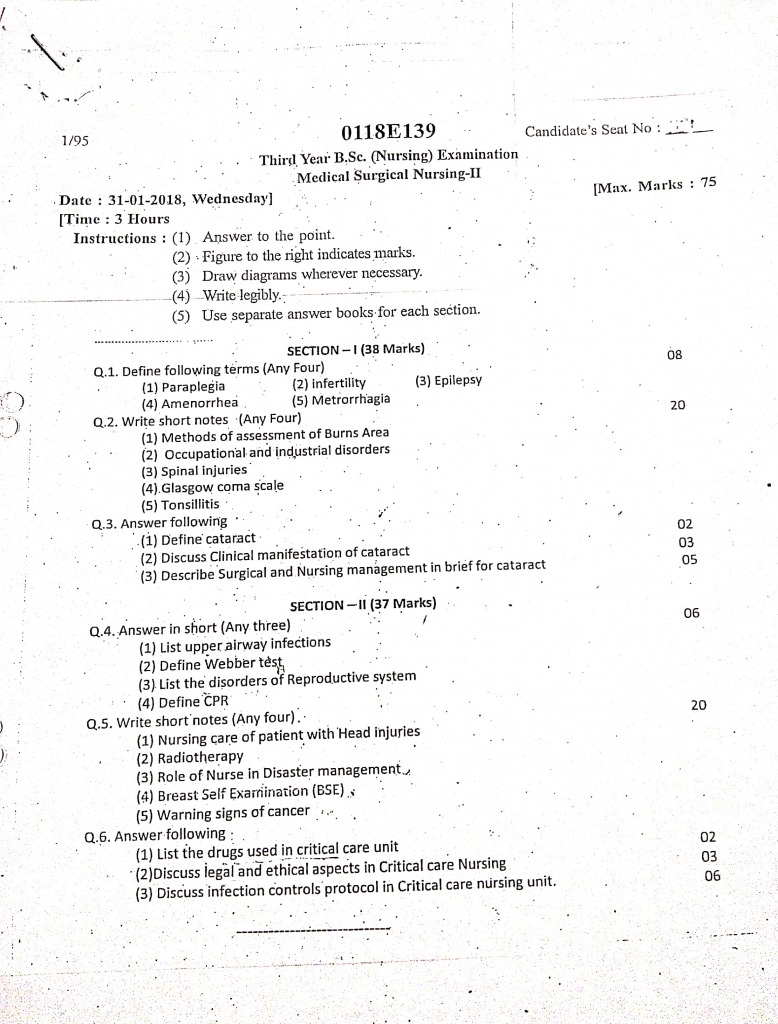
Section 1 (38 marks)
Q.1 Define following terms (Any four) (08 marks)
1. Paraplegia
- Paraplegia is defined as a type of paralysis that affects the lower half of the body, typically involving both legs and sometimes part of the lower abdomen, due to injury or disease of the spinal cord, especially in the thoracic or lumbar region.
- It results in loss of motor and/or sensory function below the level of injury and may be caused by spinal cord trauma, tumors, infections, or neurological disorders such as multiple sclerosis.
2. Infertility
Infertility is defined as the inability of a couple to conceive a child after one year of regular, unprotected sexual intercourse, or the inability to carry a pregnancy to a live birth. It can result from factors affecting the male, female, or both partners, including hormonal imbalances, anatomical problems, infections, or lifestyle factors. It is classified into :
Primary infertility : When a couple has never been able to conceive.
Secondary infertility : When a couple has conceived at least once but is now unable to conceive again.
3. Epilepsy
- Epilepsy is a chronic neurological disorder characterized by recurrent, unprovoked seizures resulting from abnormal, excessive electrical activity in the brain.
- It is diagnosed when a person has two or more unprovoked seizures occurring at least 24 hours apart, and it may lead to temporary disturbances in movement, behavior, sensation, or consciousness.
4. Amenorrhea
Amenorrhea is defined as the absence or cessation of menstruation in a woman of reproductive age for three or more consecutive menstrual cycles, or failure to begin menstruation by the age of 15 years (primary amenorrhea). It may be caused by pregnancy, hormonal disorders, stress, excessive exercise, or structural abnormalities. It is classified into :
Primary amenorrhea : When menstruation has not started by age 15.
Secondary amenorrhea : When a woman who had normal menstruation stops getting periods for 3 months or more.
5. Metrorrhagia
- Metrorrhagia is defined as uterine bleeding that occurs at irregular intervals, particularly between expected menstrual periods, and is not related to the normal menstrual cycle.
- It is non-cyclic, abnormal uterine bleeding and may be caused by hormonal imbalance, uterine fibroids, endometrial cancer, or use of oral contraceptives.
Q.2 Write short notes (any four) (20 marks)
1. Method of assessment burns area
- Assessment of burns area refers to the calculation of the percentage of Total Body Surface Area (TBSA) affected by burns.
- It helps in determining severity of burns, guiding fluid resuscitation, hospitalization needs, and treatment planning.
1. Rule of Nines (Wallace’s Rule of Nines)
- It is a quick and easy method used in emergency settings to estimate the total body surface area (TBSA) affected by burns in adults.
- The body is divided into regions that are multiples of 9%, which helps in fluid replacement calculation and burn severity assessment.
- Percentages in Adults :
1. Head and neck = 9%
2. Each arm (front and back) = 9%
3. Each leg (front and back) = 18%
4. Anterior trunk (chest + abdomen) = 18%
5. Posterior trunk (back + buttocks) = 18%
6. Perineum and genitalia = 1%
2. Lund and Browder Chart
- It is a more accurate method, especially in children and infants, because it adjusts for age-related body proportion differences.
- It provides detailed segmentation of body parts with percentage surface area based on age group.
- It considers age-specific variation in head and limb proportions.
- The chart is divided into small body segments, and the burned area is mapped for precise calculation.
- It is used in pediatric burn units or for extensive burns in adults.
- It is the gold standard for burn area assessment in clinical practice.
- Example :
- Head : 18% in infants vs 9% in adults
- Lower limb : 14% in infants vs 18% in adults
3. Lund and Browder Chart (Age-Specific Method)
- It is a more precise and accurate method for estimating Total Body Surface Area (TBSA) burned.
- This method modifies body percentage values based on the patient’s age, especially useful in infants and children, whose head and body proportions differ from adults.
- The body is divided into multiple anatomical areas, and each area has a different percentage depending on age (e.g., head accounts for more % in infants).
- A printed chart is used to shade the burned areas, and the TBSA is calculated using the age-specific values.
- Example : In a 5-year-old, the head might be considered 13%, but in an adult, it’s 9%.
- It i used in Pediatric burns, hospital settings, and documentation for surgical planning.
4. Rule of Palms (Palm Method / Hand Method)
- It is a simple method where the patient’s own palm (with fingers) is estimated to be approximately 1% of TBSA.
- It is mostly used in small, patchy, scattered, or irregular burns, or when other methods are not feasible.
- It is Quick method and useful for minor burns or first aid assessment.
- It helps first responders, community health nurses, or emergency staff estimate burn size in the field or home settings.
- Example : If the burn area is the size of 3 palms, it is about 3% TBSA burned.
5. Computerized Methods and Burn Assessment Apps (Modern Method)
- In modern hospitals, digital tools and software are used to calculate TBSA more accurately.
- These tools involve drawing burn areas on a digital body diagram, and the system automatically calculates the percentage.
- Some popular tools include BurnCase 3D, Mersey Burns App, and Smart Burn Calculator.
- These are used mainly in burn ICUs or trauma centers for detailed monitoring and surgical planning.
- It is Highly accurate, supports photographic evidence and monitoring.
- It Requires device, training, and software access.
3. Spinal injuries
Definition
- Spinal injury refers to trauma or damage to the spinal cord or vertebral column, which may result in partial or complete loss of sensory, motor, and autonomic function below the level of injury.
- Spinal injury is a medical emergency that results from trauma or disease affecting the spinal cord or vertebral column. These injuries can result in partial or complete loss of motor, sensory, and autonomic function below the level of injury. Nursing care plays a critical role in both the acute phase management and long-term rehabilitation of the patient to prevent complications and enhance recovery.
Etiology
- Road traffic accidents
- Falls from height
- Sports injuries
- Violence or gunshot wounds
- Industrial or workplace accidents
- Degenerative spinal conditions or tumors
Types of Spinal Injuries
1️⃣ Complete Spinal Cord Injury
There is a total loss of sensory and motor function below the level of injury.
Both sides of the body are equally affected.
It leads to permanent paralysis (paraplegia or quadriplegia) depending on the site of damage.
2️⃣ Incomplete Spinal Cord Injury
- There is partial preservation of motor or sensory function below the level of injury.
- Symptoms vary widely based on the extent and area of damage.
- Patients may retain some ability to move or feel.
3️⃣ Tetraplegia (Quadriplegia)
- It occurs due to injury at the cervical level of the spinal cord.
- It affects all four limbs and the trunk, including loss of bowel and bladder control.
4️⃣ Paraplegia
- It occurs due to injury at the thoracic, lumbar, or sacral level.
- It leads to loss of motor and/or sensory function in the lower limbs.
5️⃣ Brown-Séquard Syndrome
- It is a rare incomplete injury involving damage to one side of the spinal cord.
- It causes motor loss on the same side and sensory loss on the opposite side.
6️⃣ Central Cord Syndrome
- It is common in older adults with hyperextension injury.
- It affects upper limbs more than lower limbs with variable sensory loss.
Clinical Manifestations
- Loss of movement (paralysis)
- Loss of sensation (touch, pain, temperature)
- Loss of bladder or bowel control
- Breathing difficulty (if cervical spine is involved)
- Spasms or reflex activity below injury level
- Postural hypotension
Diagnostic Evaluation
- History collection
- Physical examination
- Neurological assessment
- X-ray spine
- CT scan and MRI
- Spinal cord evoked potentials
- Blood tests and ABG (in cervical injury)
Management
Initial Emergency Care
- Maintain airway, breathing, and circulation immediately at the scene.
- Immobilize the spine with cervical collars or spinal board to prevent further damage.
- Administer oxygen therapy, IV fluids, and monitor vitals closely.
Pharmacologic Treatment
- High-dose corticosteroids (e.g., methylprednisolone) may be used within 8 hours to reduce inflammation.
- Administer analgesics, muscle relaxants, and anticoagulants to prevent deep vein thrombosis.
- Treat associated complications such as hypotension, bradycardia, and infection.
Surgical Management
- Decompression laminectomy or spinal fusion is performed to stabilize the spine.
- Spinal fixation with rods, screws, or cages may be required in unstable injuries.
Rehabilitation Therapy
- Initiate physiotherapy and occupational therapy to restore function and prevent deformities.
- Focus on bladder and bowel training, skin care, and use of assistive devices.
Nursing Management
1. Respiratory Support
- Monitor respiratory rate, oxygen saturation, and ABG levels, especially in cervical injuries.
- Provide chest physiotherapy, suctioning, and positioning to prevent pneumonia.
- Prepare for mechanical ventilation if respiratory muscles are involved.
2. Neurological Assessment
- Perform regular checks of motor power, reflexes, and sensory levels.
- Monitor for changes in level of consciousness or new deficits.
- Document findings accurately in neurological charting.
3. Skin Integrity
- Turn the patient every 2 hours to prevent pressure ulcers.
- Use air mattresses, foam cushions, and inspect skin daily.
- Educate caregivers on pressure sore prevention.
4. Elimination Care
- Insert indwelling catheter or perform intermittent catheterization for urinary retention.
- Implement bowel training program using suppositories or digital stimulation.
- Maintain fluid and fiber intake to prevent constipation.
5. Nutritional Support
- Ensure high-protein, high-fiber diet to promote wound healing and prevent constipation.
- Monitor for swallowing difficulties and use feeding support if needed.
- Record daily intake and output.
6. Psychological Support
- Encourage verbal expression of emotions regarding paralysis or disability.
- Involve family and provide counseling sessions as needed.
- Refer to support groups or rehabilitation counseling.
7. Mobility and Rehabilitation
- Assist with passive and active range-of-motion exercises.
- Prevent contractures and muscle atrophy through regular physiotherapy.
- Encourage use of wheelchairs, braces, or mobility aids.
8. Health Education
- Teach patient and family about spinal precautions and signs of complications.
- Educate about home care, bowel/bladder programs, and skin care.
- Promote adherence to rehabilitation schedule and follow-ups.
4. Glassgow coma scale
Definition
- It is a standardized neurological scoring system designed to objectively measure the level of consciousness in patients with altered mental status, especially in head injury or coma.
- It was first developed in 1974 by Professors Graham Teasdale and Bryan Jennett at the University of Glasgow, hence the name Glasgow Coma Scale.
- It is a clinical tool used widely by nurses, emergency personnel, and neurologists to monitor and record the severity and progression of a coma.
Purpose of the Glasgow Coma Scale
- It is used to evaluate the neurological status and consciousness level in patients after trauma, stroke, or other brain injuries.
- It helps guide medical and nursing decisions such as whether airway protection, ICU monitoring, or neurosurgical referral is needed.
- It allows tracking of changes in consciousness over time and supports clinical judgment in both acute and chronic neurological conditions.
- It is especially useful in emergency, neuro ICU, and postoperative neurosurgical settings to detect early deterioration.
Components of GCS
1️⃣ Eye Opening Response (E) – Maximum Score: 4
| Score | Description |
|---|---|
| 4 | It is scored 4 when the patient opens eyes spontaneously without any external stimulus. |
| 3 | It is scored 3 when the patient opens eyes only when spoken to (on verbal command). |
| 2 | It is scored 2 when the patient opens eyes only in response to painful stimulus (like trapezius pinch or sternal rub). |
| 1 | It is scored 1 when the patient does not open eyes to any kind of stimulus (unresponsive). |
2️⃣ Verbal Response (V) – Maximum Score: 5
| Score | Description |
|---|---|
| 5 | It is scored 5 when the patient is alert, oriented, and speaks coherently with correct answers about name, place, and time. |
| 4 | It is scored 4 when the patient is confused but can still speak in complete sentences and respond with meaningful words. |
| 3 | It is scored 3 when the patient speaks with inappropriate words that make no contextual sense. |
| 2 | It is scored 2 when the patient makes only incomprehensible sounds like moaning or groaning without forming words. |
| 1 | It is scored 1 when the patient gives no verbal response at all. |
3️⃣ Motor Response (M) – Maximum Score: 6
| Score | Description |
|---|---|
| 6 | It is scored 6 when the patient obeys motor commands like “show me two fingers” or “move your hand.” |
| 5 | It is scored 5 when the patient purposefully localizes pain (e.g., tries to remove a painful stimulus like a nail bed pressure). |
| 4 | It is scored 4 when the patient withdraws from painful stimulus (pulls limb away reflexively). |
| 3 | It is scored 3 when the patient shows abnormal flexion to pain (decorticate posture: arms bent, legs extended). |
| 2 | It is scored 2 when the patient shows abnormal extension to pain (decerebrate posture: arms extended, wrists flexed, legs stiff). |
| 1 | It is scored 1 when there is no motor response even to painful stimuli. |
Total GCS Score = Eye (4) + Verbal (5) + Motor (6) = 3 to 15
Minimum possible score : 3 (deep coma or death-like unresponsive state).
Maximum possible score : 15 (normal, fully awake and alert state).
Interpretation of Scores
Total GCS Score Level of Brain Injury
- 13 – 15 It indicates mild brain injury or alert consciousness.
- 9 – 12 It indicates moderate brain injury and requires monitoring.
- ≤ 8 It indicates severe brain injury or coma, and immediate ICU admission or intubation may be required.
Importance in Nursing Practice
- It is essential for the nurse to accurately assess and record GCS scores at regular intervals, especially after trauma or neurosurgery.
- It is important to establish a baseline GCS and monitor for any decrease in score, which may indicate neurological worsening.
- It is necessary to use a painful stimulus like trapezius squeeze or nail bed pressure if the patient is not responding verbally.
- It is crucial for the nurse to notify the physician or neurologist immediately if GCS drops by 2 or more points.
- It is vital to recheck GCS after giving sedatives or anticonvulsants, as medications can alter the score.
- It is the nurse’s responsibility to manage airway, oxygen, and suction if GCS is ≤ 8 to prevent hypoxia.
- It is essential to use the same scale for continuity of care and documentation to avoid inter-observer variation.
- It is helpful to educate patient families about the meaning of GCS score and its implications for recovery.
5. Tonsilitis
Definition
- It is an acute or chronic inflammation and infection of the palatine tonsils, which are lymphoid tissues located on both sides of the throat.
- It is commonly caused by bacterial or viral pathogens and is most frequent in children aged 5–15 years.
Types of Tonsillitis
1️⃣ Acute Tonsillitis
- It is the sudden and rapid onset of inflammation in the tonsils.
- It usually occurs due to viral or bacterial infection and lasts for a short duration (5–10 days).
- Tonsils appear red, swollen, and may have white or yellow exudates.
- It is often associated with high fever, sore throat, and painful swallowing.
2️⃣ Chronic Tonsillitis
- It is a long-standing or frequently recurring infection of the tonsils.
- It leads to persistent throat discomfort, bad breath (halitosis), and enlarged lymph nodes.
- It may cause snoring, nasal voice, and difficulty swallowing over weeks or months.
- This type may require surgical removal (tonsillectomy) due to repeated episodes.
3️⃣ Recurrent Tonsillitis
- It refers to multiple episodes of acute tonsillitis occurring several times a year.
- Commonly seen in children with weakened immunity or chronic infections.
- The frequency is usually ≥7 episodes in 1 year, ≥5 in 2 consecutive years, or ≥3 in 3 consecutive years.
- May lead to impaired school attendance, poor sleep, and chronic fatigue.
4️⃣ Peritonsillar Abscess (Complication Type)
- Also called Quinsy, it is a pus-filled pocket that forms beside the tonsil.
- Causes severe throat pain, trismus (inability to open mouth), and uvular deviation.
- Requires urgent medical attention and drainage.
Etiology
- Caused mainly by Streptococcus pyogenes (Group A Streptococcus).
- Viral causes include adenovirus, influenza virus, Epstein-Barr virus.
- Risk factors include low immunity, poor hygiene, exposure to infections, and frequent cold/flu.
Pathophysiology of Tonsillitis
1️⃣ Entry of Pathogen
It is caused by viral or bacterial organisms entering the body through the mouth or nose, often via droplet infection.
2️⃣ Colonization
It is in this stage where microorganisms attach to the epithelial lining of the tonsils and begin multiplying.
3️⃣ Tissue Invasion
It is where pathogens invade the tonsillar crypts, triggering the local inflammatory process.
4️⃣ Immune Activation
It is through the release of cytokines and inflammatory mediators that white blood cells accumulate to fight the infection.
5️⃣ Inflammation and Swelling
It is due to vasodilation, fluid leakage, and cellular infiltration, leading to red, swollen, and painful tonsils.
6️⃣ Exudate Formation (in bacterial cases)
It is common to see pus or white patches on tonsils due to the collection of dead cells and bacteria.
7️⃣ Clinical Signs Appear
It is at this stage when fever, sore throat, dysphagia (difficulty in swallowing), and lymphadenopathy occur.
8️⃣ Recovery or Complication
It is after immune resolution that healing occurs; however, untreated cases may lead to abscess or chronic tonsillitis.
Clinical Manifestations
- Sore throat
- Pain while swallowing.
- Red and swollen tonsils with or without white patches (exudate).
- Fever
- Chills
- Malaise
- Tender, enlarged cervical lymph nodes.
- In children : vomiting or abdominal pain may occur.
Diagnosis
- History collection
- physical examination
- Throat swab for culture or rapid antigen detection test (RADT).
- Visual examination of throat using tongue depressor.
- CBC test may show elevated WBCs in bacterial infection.
Medical Management (Pharmacological)
1️⃣ Antibiotics
- It is recommended to give Penicillin V as the first-line antibiotic for streptococcal tonsillitis.
- It is suitable to use Amoxicillin-Clavulanate in penicillin-resistant cases.
- It is necessary to use Macrolides (like Azithromycin) in patients with penicillin allergy.
2️⃣ Analgesics/Antipyretics
- It is important to prescribe Paracetamol or Ibuprofen to relieve pain and reduce fever.
3️⃣ Local Treatment
- It is helpful to advise warm saline gargles or Betadine gargles to reduce throat discomfort.
Surgical Management (Tonsillectomy)
- It is indicated in recurrent tonsillitis (≥7/year) or chronic tonsillitis not responding to treatment.
- It is also required if peritonsillar abscess occurs or if there is airway obstruction due to enlarged tonsils.
- It is performed via cold knife dissection, electrocautery, or coblation techniques.
Nursing Management
1️⃣ Assessment
- It is essential to assess throat for redness, swelling, exudates, and voice changes.
- It is necessary to monitor temperature and signs of systemic infection.
- It is important to inspect for lymph node enlargement and signs of dehydration.
2️⃣ Medication Administration
- It is important to administer prescribed antibiotics (if bacterial) and antipyretics like paracetamol or ibuprofen.
- It is the nurse’s role to ensure full antibiotic course is completed.
- It is essential to observe for drug allergies or side effects during treatment.
3️⃣ Symptom Relief
- It is necessary to encourage warm saline gargles to reduce throat pain.
- It is beneficial to apply warm compresses over the neck for comfort.
- It is helpful to use humidifiers to ease throat irritation.
4️⃣ Hydration and Nutrition
- It is crucial to encourage oral fluid intake like warm soups, juices, and water.
- It is advisable to provide soft, bland, and non-irritating foods.
- It is important to monitor intake-output and prevent dehydration.
5️⃣ Rest and Recovery
- It is essential to provide bed rest during the febrile phase.
- It is necessary to ensure a calm, quiet environment to promote healing.
- It is important to limit physical activity until recovery is complete.
6️⃣ Health Education
- It is the nurse’s duty to teach proper hand hygiene and cough etiquette.
- It is important to educate parents (in pediatric cases) about signs of recurrence.
- It is advisable to inform about complications like rheumatic fever or abscess.
- It is necessary to discuss tonsillectomy indications in chronic or recurrent cases.
7️⃣ Monitoring for Complications
- It is vital to monitor for signs of airway obstruction like stridor or drooling.
- It is important to watch for signs of quinsy, high fever, and difficulty swallowing.
- Immediate referral is needed if respiratory distress or severe pain develops.
Q.3 Answer following
1. Define cataract (02)
Cataract is an ocular condition in which the natural crystalline lens of the eye becomes progressively opaque or cloudy, leading to blurred or diminished vision. It interferes with the passage of light through the lens to the retina, causing difficulty in seeing, especially in bright light. It is a painless, progressive disorder that may affect one or both eyes.
2. Discuss clinical manifestation of cataract (03)
1. Blurring of Vision
The patient experiences gradual, painless blurring or dimming of vision, which is the most common early symptom of cataract. It feels like looking through a foggy or dusty glass.
2. Increased Sensitivity to Light (Photophobia)
The individual may report discomfort or pain in bright light, sunlight, or oncoming headlights during night driving. This is especially noticeable during outdoor activities or reading under bright lamps.
3. Glare and Halos Around Lights
Patients often complain of seeing halos or bright rings around lights, particularly at night or in dim lighting. This symptom can make night driving hazardous.
4. Difficulty with Night Vision
As the cataract progresses, vision becomes worse in low-light conditions, leading to night blindness (nyctalopia).
5. Frequent Prescription Changes
There may be repeated changes in eyeglass or contact lens prescriptions that no longer provide clear vision. This is due to the progressive nature of the opacity in the lens.
6. Faded or Yellowed Colors
The person may report that colors appear dull, faded, or yellowish, making it difficult to distinguish between similar hues.
7. Double Vision in One Eye
Some patients may experience monocular double vision (diplopia), where two images appear from one eye.
8. Visible White or Grey Pupil (in advanced cases)
In mature or hypermature cataract, the pupil may appear greyish or whitish instead of black, especially under torchlight.
3. Describe surgical and nursing management in brief for cataract (05)
Surgical Management of Cataract
Surgery is the only definitive treatment for cataract, where the cloudy natural lens of the eye is removed and replaced with a clear artificial intraocular lens (IOL) to restore vision.
✅ 1. Phacoemulsification (Modern and Most Common Technique)
- Phacoemulsification is the most widely used surgical method for cataract removal and is preferred due to its minimal invasiveness and faster healing.
- A very small incision (2–3 mm) is made on the side of the cornea through which an ultrasound probe is inserted.
- The probe emits ultrasonic waves to break the cloudy lens into tiny fragments.
- The fragmented lens is then suctioned out gently, and a foldable intraocular lens (IOL) is inserted through the same small incision.
- This technique requires no sutures, causes minimal trauma, and allows rapid visual recovery.
✅ 2. Extracapsular Cataract Extraction (ECCE)
- ECCE is used for mature or hard cataracts that cannot be removed by phacoemulsification.
- A larger incision (10–12 mm) is made in the sclera or cornea.
- The entire lens nucleus is removed in one piece, leaving the posterior capsule intact to support the IOL.
- A rigid IOL is implanted into the capsular bag, and sutures are usually needed to close the incision.
- Healing takes longer compared to phaco, and there’s a slightly higher risk of postoperative inflammation.
✅ 3. Intracapsular Cataract Extraction (ICCE)
- ICCE is a rarely used, outdated method where the entire lens and its capsule are removed together.
- It requires a very large incision and is associated with higher complication risks such as retinal detachment or vitreous loss.
- The intraocular lens is placed in the anterior chamber, rather than the capsular bag.
- This method has been replaced by safer, more effective techniques like phacoemulsification.
✅ 4. Intraocular Lens (IOL) Implantation
- In all modern cataract surgeries, after removing the natural lens, a permanent artificial lens (IOL) is implanted.
- Types of IOLs include :
- Monofocal IOL – provides vision at one distance
- Multifocal IOL – helps see both near and far
- Toric IOL – used to correct astigmatism
- IOLs are made of silicone, acrylic, or PMMA, and are well tolerated with minimal rejection risk.
Nursing Management in Cataract Surgery
Nursing care is divided into three phases : Preoperative, Intraoperative, and Postoperative.
1. Preoperative Nursing Management
- The nurse should provide complete education to the patient and their family regarding the procedure, expected outcomes, risks, anesthesia, and recovery time.
- Perform baseline assessment including vital signs, visual acuity, blood sugar, blood pressure, allergy history, and pupil dilation response.
- Administer prescribed mydriatic eye drops (e.g., tropicamide, phenylephrine) to dilate the pupil.
- Instill antibiotic drops (e.g., moxifloxacin) to reduce the risk of postoperative infection.
- Ensure the patient is kept NPO (nothing by mouth) for at least 6–8 hours before surgery as per protocol.
- Confirm informed consent has been signed, and all necessary preoperative tests (blood tests, ECG) are completed.
- The surgical eye must be marked clearly, and jewelry, dentures, and contact lenses must be removed.
2. Intraoperative Nursing Management
- The nurse should assist the ophthalmic surgeon in maintaining a sterile field and ensuring aseptic technique throughout the procedure.
- Prepare all necessary instruments including phaco probe, viscoelastics, IOL, irrigation solutions, and surgical drapes.
- Monitor the patient’s vital signs, oxygen saturation, and comfort throughout the procedure.
- Offer verbal reassurance to the patient, as they are usually awake during surgery.
- Be alert for signs of anxiety, dizziness, or adverse drug reactions to anesthetics or sedatives.
- After surgery, assist in dressing the eye, applying shield or patch, and documenting intraoperative findings.
3. Postoperative Nursing Management
- Immediate Postoperative Care (Within 24 Hours) :
- Monitor the patient for any signs of complications such as sudden pain, redness, decreased vision, excessive tearing, or bleeding.
- Assess the dressing for signs of bleeding, soaking, or displacement, and reinforce or change as per protocol.
- Ensure the patient is in a semi-Fowler’s position to reduce intraocular pressure.
- Administer prescribed eye drops such as:
- Topical antibiotics to prevent infection (e.g., moxifloxacin)
- Steroids to control inflammation (e.g., prednisolone)
- NSAID drops to reduce pain and swelling
- Provide eye shield and educate the patient to avoid rubbing or pressing the operated eye.
Ongoing Postoperative Care (Days to Weeks) :
- Educate the patient to avoid bending forward, lifting heavy weights, coughing, or straining during bowel movements for at least 1–2 weeks.
- Instruct proper hand hygiene and technique of eye drop instillation, including spacing of drops if multiple are prescribed.
- Encourage the use of dark glasses or protective eyewear, especially outdoors or during sleep.
- Explain the need for regular follow-up visits, usually on Day 1, Day 7, and after 1 month for visual assessment and spectacle prescription.
- Provide a soft diet and plenty of fluids, and prevent constipation by prescribing laxatives if needed.
- Instruct the patient to report immediately if experiencing any of the following :
- Severe or sudden eye pain
- Loss of vision
- Flashes of light or floating spots
- Discharge or foul smell from eye
- Nausea or vomiting (sign of increased intraocular pressure)
4. Long-Term Nursing Education
- Educate the patient that vision may not return immediately and will improve gradually over 4–6 weeks.
- Reinforce that a final glasses prescription will be provided only after full healing.
- Counsel the patient about the importance of managing comorbidities like diabetes and hypertension, which affect ocular health.
- Provide psychological support, especially in elderly patients adjusting to new vision changes.
Section 2 (37 marks)
Q.4 Answer in short (any three) (06 marks)
1. List upper airway infections
Rhinitis
It is the inflammation of the nasal mucosa, commonly caused by viral infections such as the common cold.
Sinusitis
It is the inflammation or infection of the paranasal sinuses, leading to facial pain, nasal congestion, and headache.
Pharyngitis
It is the inflammation of the pharynx (throat), which causes sore throat, often due to viral or streptococcal infection.
Tonsillitis
It is the inflammation of the tonsils, often caused by bacteria (Streptococcus pyogenes) or viruses, leading to sore throat, fever, and swollen lymph nodes.
Laryngitis
It is the inflammation of the larynx (voice box), commonly resulting in hoarseness or loss of voice, often due to viral infection or overuse of voice.
Epiglottitis
It is a life-threatening infection of the epiglottis, mostly seen in children, usually caused by Haemophilus influenzae type B (Hib), leading to airway obstruction.
Nasopharyngitis
Commonly referred to as the common cold, it is the inflammation of the nasal passages and pharynx, caused by rhinoviruses and coronaviruses.
2. Define webber test
Weber Test is a simple clinical hearing test used to assess the type of hearing loss (i.e., conductive or sensorineural) by placing a vibrating tuning fork on the midline of the skull, usually on the forehead or the vertex of the head.
In this test, the patient is asked where the sound is heard louder—in the affected ear, unaffected ear, or equally in both ears.
It is used in conjunction with the Rinne test to differentiate unilateral hearing loss. Lateralization of sound helps determine whether the hearing loss is conductive (same ear) or sensorineural (opposite ear).
3. List the disorders of Reproductive system
Female Reproductive System Disorders
- Dysmenorrhea
- Amenorrhea
- Polycystic Ovarian Syndrome (PCOS)
- Pelvic Inflammatory Disease (PID)
- Endometriosis
- Uterine Fibroids (Leiomyomas)
- Ovarian Cysts
- Cervical Cancer
- Vaginitis
- Infertility
Male Reproductive System Disorders
- Erectile Dysfunction
- Prostatitis
- Benign Prostatic Hyperplasia (BPH)
- Prostate Cancer
- Hydrocele
- Varicocele
- Cryptorchidism
- Testicular Torsion
- Epididymitis
- Male Infertility
4. Define CPR
CPR (Cardiopulmonary Resuscitation) is a life-saving emergency procedure that combines chest compressions and rescue breaths to maintain circulation of oxygenated blood to the brain and vital organs when a person’s heart has stopped beating (cardiac arrest) or they have stopped breathing. It is intended to temporarily support circulation and breathing until advanced medical help becomes available. CPR helps in preserving brain function, preventing tissue death, and increasing survival chances in sudden cardiac arrest.
Q.5 Write short notes any four (20 marks)
1. Nursing care of patient with head injuries
Head injury refers to trauma to the scalp, skull, or brain that may be open (penetrating) or closed (non-penetrating), and can lead to serious complications including increased intracranial pressure (ICP), brain herniation, or death. It is classified as mild, moderate, or severe based on Glasgow Coma Scale (GCS) score.
✅ 1. Emergency Nursing Management (Pre-hospital or ER phase)
- The nurse must first ensure a clear and patent airway by using a head tilt-chin lift or jaw thrust maneuver (if no spinal injury is suspected).
- If spinal cord injury is suspected, the cervical spine must be stabilized using a rigid cervical collar or manual immobilization.
- The nurse should administer supplemental oxygen to maintain oxygen saturation above 95% and prevent hypoxia to brain tissue.
- It is critical to initiate cardiopulmonary resuscitation (CPR) if the patient is unresponsive with no pulse or respiration.
- Two large-bore IV lines should be secured, and isotonic fluids (like normal saline) started to manage shock.
- The nurse should assess and document Glasgow Coma Scale (GCS), pupil reaction, limb movement, bleeding, and any open wounds.
- A quick neurological assessment including verbal response, motor response, and eye-opening response is done to establish baseline.
✅ 2. Acute Phase Nursing Management (In ICU or Neuro Ward)
A. Neurological Monitoring and Assessment
- The nurse must assess level of consciousness hourly using the GCS, noting any decline which could indicate brain swelling or hemorrhage.
- Regularly check pupil size, symmetry, and reaction to light to detect early signs of increased intracranial pressure (ICP) or brain herniation.
- Monitor for abnormal posturing such as decorticate or decerebrate postures which indicate severe brain injury.
- The nurse should watch for seizure activity and have emergency anticonvulsants like lorazepam or phenytoin readily available.
B. Respiratory Support and Airway Management
- The airway must be kept clear with suctioning and humidified oxygen administration as needed.
- If the patient has GCS ≤ 8, endotracheal intubation or mechanical ventilation may be required to prevent respiratory failure.
- Maintain the head of the bed elevated at 30 degrees unless contraindicated to facilitate venous drainage from the brain.
- Avoid neck flexion, tight tracheostomy ties, or anything that could increase ICP.
C. Hemodynamic and Fluid Balance Management
- Regularly monitor blood pressure, heart rate, central venous pressure (CVP), and urine output to detect hypovolemia or shock.
- Avoid hypotension, which can worsen cerebral perfusion, by administering IV fluids and vasopressors as prescribed.
- Monitor for diabetes insipidus (excessive urine output) or SIADH (low urine output), which are endocrine complications of head trauma.
- Administer osmotic diuretics (e.g., Mannitol) or hypertonic saline as ordered to reduce cerebral edema.
D. Nutritional Support and GI Care
- Initiate enteral nutrition via nasogastric tube within 48–72 hours to maintain nutritional status.
- Monitor for abdominal distension, bowel sounds, and constipation due to immobility or medications.
- Provide proton pump inhibitors (PPIs) or H2 blockers to prevent stress ulcers or gastric bleeding.
E. Pain and Sedation Management
- Pain must be assessed and managed with analgesics like paracetamol or opioids, being cautious not to mask neurological signs.
- Use sedatives cautiously (e.g., midazolam) to calm agitated patients but avoid over-sedation.
- Apply cold compresses or dark room conditions to relieve photophobia and headaches.
F. Skin Integrity and Pressure Ulcer Prevention
- Turn and reposition the patient every 2 hours using log-roll technique to prevent spinal misalignment.
- Use pressure-relieving mattresses, heel protectors, and clean, dry linens.
- Monitor skin for redness, blisters, or pressure injuries, especially on sacrum, elbows, and heels.
G. Bowel and Bladder Care
- Monitor for urinary retention or incontinence, and maintain a sterile technique during catheter care.
- Initiate bladder training or intermittent catheterization once the patient regains consciousness.
- Provide stool softeners to prevent straining, which increases ICP.
✅ 3. Psychological and Emotional Nursing Support
- Offer empathy, reassurance, and psychological comfort to the patient and family.
- Maintain effective communication with the family, updating them on the patient’s condition and prognosis.
- Provide referral to counseling services, especially if the patient develops depression, personality changes, or PTSD.
- Encourage family involvement in care, and provide education on behavior changes that may occur post-head injury.
✅ 4. Rehabilitation Phase Nursing Care
- Collaborate with physiotherapists for early mobilization, passive and active range-of-motion exercises.
- Support speech therapy, especially in patients with aphasia, dysarthria, or dysphagia.
- Help the patient with cognitive retraining including memory exercises, reality orientation, and attention tasks.
- Educate the family on home safety modifications, such as installing handrails, removing trip hazards, and using helmets.
- Assess for community resources like home nursing, occupational therapy, and vocational rehabilitation.
✅ 5. Discharge Planning and Education
- Educate the patient and family about medication adherence, warning signs of complications (e.g., vomiting, drowsiness, seizure).
- Encourage regular follow-up with neurology, psychiatry, and rehabilitation services.
- Counsel regarding avoidance of alcohol, driving, or strenuous activities until medically cleared.
- Provide written instructions on nutrition, hygiene, and wound care if surgery was performed.
✅ 6. Documentation and Legal Aspects
- Accurately document neurological assessments, nursing interventions, and patient’s response to treatment.
- Maintain chain of evidence if head injury is due to assault or accident (medico-legal case).
- Ensure all informed consent procedures are appropriately signed and witnessed, especially before surgery or CT scans.
2. Radiotherapy
Definition
- Radiotherapy is a clinical treatment method that involves the use of controlled, high-energy ionizing radiation, such as X-rays, gamma rays, or charged particles, to kill or damage cancer cells while minimizing harm to surrounding normal tissue.
- It works by causing breaks in the DNA strands of rapidly dividing cancer cells, thereby inhibiting their ability to multiply and survive.
- Radiotherapy may be used as a curative treatment, an adjuvant therapy after surgery, a neoadjuvant therapy before surgery, or as a palliative therapy in advanced cancer to relieve symptoms such as pain, bleeding, or obstruction.
Goals and Purposes of Radiotherapy
- To destroy or shrink cancerous tumors without harming surrounding normal tissues.
- To prevent recurrence of cancer after surgery or chemotherapy.
- To relieve symptoms like pain, bleeding, or obstruction in advanced cancers (palliative radiotherapy).
- To reduce tumor size before surgery to make it operable (neoadjuvant therapy).
- To kill microscopic residual cancer cells left after surgery (adjuvant therapy).
Types of Radiotherapy
A. External Beam Radiotherapy (EBRT)
- It is the most widely used form of radiotherapy where radiation beams are delivered from a machine outside the body, such as a linear accelerator (LINAC).
- The patient lies on a treatment couch while the radiation machine rotates around them to deliver beams precisely to the tumor site from various angles.
- Techniques such as 3D-CRT (Three-Dimensional Conformal Radiation Therapy) and IMRT (Intensity-Modulated Radiation Therapy) help to shape the radiation dose to fit the tumor.
- It is usually given in daily fractions (sessions) over several weeks.
B. Internal Radiotherapy (Brachytherapy)
- In this technique, a radioactive source is placed directly into or near the tumor using applicators, needles, seeds, or catheters.
- It may be temporary (high-dose rate) or permanent (low-dose rate), depending on cancer type.
- It delivers a very high localized dose while sparing surrounding normal tissues.
- It is commonly used in gynecological cancers, prostate cancer, and oral cavity cancers.
C. Systemic Radiotherapy (Radioisotope Therapy)
- This method involves swallowing or injecting radioactive substances, such as radioiodine (I-131), strontium-89, or samarium-153, that circulate in the bloodstream and selectively target cancer cells.
- It is especially useful in thyroid cancer, bone metastases, and neuroendocrine tumors.
- This method requires isolation precautions due to systemic radioactivity.
Indications of Radiotherapy
Radiotherapy is used to treat a wide variety of malignant tumors, including :
- Breast cancer
- Cervical and uterine cancer
- Prostate cancer
- Head and neck cancers (larynx, pharynx, tongue, mouth)
- Lung cancer
- Esophageal and gastric cancer
- Brain tumors (gliomas, metastases)
- Skin cancers (basal cell, squamous cell carcinoma)
- Lymphomas (Hodgkin and non-Hodgkin)
- Pediatric cancers (e.g., medulloblastoma, rhabdomyosarcoma)
Side Effects of Radiotherapy
It may vary depending on site and dose
Local Side Effects
- Skin irritation, redness, or burns over the radiation site
- Hair loss in the treated area
- Oral ulcers, dry mouth (in head/neck radiation)
- Difficulty swallowing or sore throat (esophageal radiation)
- Diarrhea or abdominal cramps (abdominal or pelvic radiation)
- Vaginal dryness or bleeding (pelvic radiation)
Systemic Side Effects
- Fatigue
- Nausea and vomiting
- Anorexia and weight loss
- Suppression of bone marrow (in long-term or high-dose therapy)
- Risk of secondary malignancy (rare, long-term effect)
Nursing Responsibilities in Radiotherapy
A. Before Radiotherapy (Pre-procedure Nursing Care)
- The nurse must educate the patient and family about the procedure, possible outcomes, and common side effects in a compassionate manner.
- It is important to provide psychological support and reduce fear and anxiety related to the word “radiation”.
- The nurse must assess the patient’s physical baseline — weight, nutritional status, skin integrity, hydration, and vital signs.
- She ensures that any metallic objects (jewelry, implants) are noted and removed if they interfere with therapy.
- If the radiation field includes the pelvic area, patients may be instructed to empty or fill the bladder before treatment.
B. During Radiotherapy (Intra-procedure Care)
- The nurse should assist in accurate positioning of the patient on the radiation table to ensure the beam targets only the tumor site.
- She must observe for immediate adverse reactions such as dizziness, shortness of breath, or skin burning.
- The nurse should follow strict radiation safety protocols, including shielding, lead walls, and maintaining safe distance.
- During brachytherapy, the nurse should limit time spent in the radiation room, stand behind shielding, and wear a radiation dosimeter badge.
- Emotional support is important, as isolation during radiation can be psychologically distressing for many patients.
C. After Radiotherapy (Post-procedure Nursing Care)
- The nurse should inspect the radiation-exposed skin daily and report any signs of ulceration, blisters, or infection.
- It is essential to instruct the patient not to scratch, shave, or apply lotions or powders on the treated skin unless prescribed.
- Dietary counseling is required to manage nausea, mouth sores, weight loss, or bowel irregularities.
- The nurse should monitor complete blood counts (CBC) regularly if bone marrow is exposed, to assess for anemia, neutropenia, or thrombocytopenia.
- She must provide emotional and social support, especially for patients dealing with altered body image, infertility, or fatigue.
- Patient and family should be educated on long-term care, follow-up visits, and signs of complications that must be reported immediately.
Radiation Safety Guidelines for Nurses
- Follow ALARA principle (As Low As Reasonably Achievable) for exposure time.
- Maintain safe distance, use protective lead aprons or barriers, and avoid direct contact with radiation sources.
- Use a radiation badge to monitor cumulative exposure.
- Pregnant nurses should avoid assignments involving direct radiation exposure.
- Educate patients and their visitors about radiation hygiene and home precautions post-brachytherapy or systemic therapy.
3. Role of nurse in disaster management
A nurse plays a multidimensional role during all four phases of disaster management: preparedness, response, recovery, and mitigation. Nurses are the backbone of healthcare delivery in emergencies, offering clinical care, emotional support, and leadership to individuals and communities affected by disasters.
1. Role of Nurse in Disaster Preparedness Phase
- This is the pre-disaster phase where planning, training, and organization take place to reduce the impact of the disaster.
- It is the nurse’s responsibility to actively participate in hospital disaster planning committees and contribute knowledge toward making realistic and effective response strategies.
- The nurse should attend regular disaster drills and mock codes, ensuring familiarity with evacuation routes, emergency procedures, and disaster protocols.
- The nurse must educate patients, families, and communities about disaster types common to their region (e.g., earthquakes, floods, fire) and how to respond to them.
- The nurse is responsible for preparing personal and institutional emergency kits, including first aid supplies, medications, sterile dressings, gloves, IV fluids, and emergency contact lists.
- The nurse collaborates with other healthcare professionals and local authorities to assess community risks and vulnerabilities and develop action plans.
- It is also vital for the nurse to assist in creating communication flowcharts, so everyone knows whom to contact and what to do during emergencies.
- The nurse may lead public education campaigns on hygiene, disease prevention, and personal safety during disasters.
2. Role of Nurse in Disaster Response Phase
- This phase occurs during or immediately after the disaster, where the focus is on saving lives, preventing complications, and minimizing injuries.
- It is the nurse’s immediate responsibility to perform triage, which involves sorting patients based on injury severity using color-coded tags (e.g., red for urgent, yellow for delayed).
- The nurse provides life-saving emergency care, including controlling hemorrhage, managing airway, performing CPR, administering IV fluids, and stabilizing fractures.
- The nurse assists in evacuation procedures, ensuring that critically ill patients are safely transported to emergency shelters or hospitals.
- The nurse should maintain infection control measures in temporary shelters or field hospitals by ensuring proper waste disposal, hand hygiene, and use of PPE.
- The nurse maintains accurate records of victims treated, including personal details, injuries, treatments provided, and referrals.
- It is the nurse’s duty to communicate with relatives, provide updates on victim status, and offer emotional reassurance.
- In mass casualty incidents, the nurse also coordinates with ambulance services, disaster relief workers, and military personnel to streamline care delivery.
3. Role of Nurse in Disaster Recovery Phase
- This phase involves returning the affected individuals and communities back to normal life and rebuilding healthcare services.
- The nurse assists in wound care, rehabilitation, follow-up of chronic conditions, and psychological counseling for trauma victims.
- It is the nurse’s duty to identify long-term care needs, such as orthopedic rehabilitation, prosthetics for amputees, or continued treatment for burns.
- The nurse provides grief counseling and emotional support for individuals who lost loved ones, homes, or jobs.
- Nurses help in restoring healthcare infrastructure, such as setting up mobile health units or reopening damaged clinics.
- The nurse participates in health assessments and surveillance, identifying outbreaks of communicable diseases post-disaster (e.g., diarrhea, malaria, leptospirosis).
- It is the nurse’s role to conduct home visits to check on elderly, disabled, or pregnant women affected by the disaster.
- The nurse assists in government relief work, such as filling forms for compensation, housing, or ration supply.
4. Role of Nurse in Mitigation Phase
- Mitigation involves reducing the long-term risk and impact of future disasters.
- The nurse works with public health teams to educate the community about preventive actions, like securing heavy furniture in earthquake-prone zones or using mosquito nets to prevent vector-borne diseases.
- It is the nurse’s responsibility to improve community resilience by encouraging regular drills, early warning alerts, and safe construction practices.
- Nurses may engage in health mapping and environmental risk assessments to identify high-risk zones and vulnerable populations.
- The nurse provides counseling on stress management and trauma recovery, helping communities build psychological strength.
- Nurses help evaluate existing disaster plans, suggest improvements, and participate in research to identify gaps in disaster response.
5. Ethical and Professional Role of Nurse in Disasters
- It is essential that nurses practice non-discriminatory care, giving equal attention to all affected individuals regardless of age, gender, caste, or financial status.
- Nurses must maintain patient confidentiality, even in chaotic environments like emergency shelters or open field hospitals.
- The nurse should demonstrate calm, leadership behavior, helping to reduce panic and maintain order.
- The nurse advocates for vulnerable populations like children, disabled persons, pregnant women, and elderly who are often overlooked during mass relief efforts.
- It is the nurse’s ethical duty to self-monitor for fatigue or burnout and seek help if needed, to ensure optimal care delivery.
6. Communication & Coordination Role
- Nurses should maintain clear, timely, and accurate communication with physicians, disaster teams, NGOs, and local authorities.
- They may serve as a liaison between victims and rescue agencies, helping victims understand available services.
- Nurses must report outbreaks or deaths to public health authorities immediately to activate containment measures.
- They are often responsible for collaborating with media teams, when assigned, to deliver public health messages or announcements.
7. Documentation and Evaluation Role
- The nurse must record all medical care provided, resources used, number of people assisted, and any referrals made.
- Documentation helps in financial audits, legal accountability, and future disaster policy formulation.
- Nurses should assist in post-disaster evaluation reports, offering suggestions for what worked well and what needs improvement.
- These reports contribute to national disaster database systems, enhancing preparedness for future events.
4. Breast self examination
Definition
- It is a simple, non-invasive method in which a woman examines her own breasts regularly for any unusual changes in appearance or texture, in order to detect breast abnormalities such as lumps, skin dimpling, or nipple discharge, which may be an early sign of breast cancer.
- It is a procedure by which a woman systematically inspects and palpates her breasts using her own hands and eyes to detect any changes or abnormalities.
- It is considered a primary screening method for breast cancer, especially in low-resource settings.
- It is a preventive health measure recommended for women starting from 20 years of age, performed once every month.
- It helps in developing awareness of normal breast consistency, so changes can be quickly identified.
PURPOSE / OBJECTIVES OF BSE
- To detect early signs of breast cancer such as lumps, pain, or skin changes.
- To enable a woman to become familiar with the normal structure and texture of her breasts.
- To promote responsibility and self-awareness about breast health.
- To serve as a supplement to clinical breast examination (CBE) and mammography.
- To identify any visible or palpable abnormality so that medical care can be sought promptly.
IDEAL TIME FOR BSE
- In menstruating women, the best time to perform BSE is 7 to 10 days after the onset of menstruation, when breast tissue is least tender or swollen.
- In post-menopausal women, BSE should be performed on the same date every month to maintain regularity.
- Women on oral contraceptives are advised to perform BSE on a fixed day during their pill cycle.
- It should be performed monthly, as regular checks help recognize new or unusual changes more easily.
STEPS OF BREAST SELF-EXAMINATION
BSE involves visual inspection and manual palpation in both standing and lying positions.
A. VISUAL INSPECTION (Performed in front of a mirror)
- The woman should undress from the waist up and stand in front of a mirror with arms relaxed at her sides.
- She should inspect for any visible asymmetry, lumps, swelling, or skin changes such as dimpling, puckering, or redness.
- Next, she should raise both arms overhead and observe for the same changes again.
- Then she should press her hands firmly on her hips and slightly bend forward to contract the chest muscles.
- In each step, she should carefully observe both breasts for nipple changes (e.g., inversion, retraction, discharge).
B. MANUAL PALPATION (Using finger pads for touch examination)
While Standing or Bathing
- With the skin wet and soapy (which improves finger glide), she should raise her right arm.
- Using the pads of the three middle fingers of the left hand, she should palpate the right breast in small, circular motions.
- She should follow a pattern (circular, vertical strip, or wedge) to ensure full coverage of the breast tissue.
- The axillary area (underarm) should be palpated thoroughly for any enlarged lymph nodes.
- The process should be repeated for the left breast using the right hand.
While Lying Down
- She should lie on her back with a small pillow under her right shoulder and place her right arm behind her head.
- With her left hand, she should feel the right breast using gentle pressure at various depths (light for surface, medium for mid-level, and firm for deep tissue).
- She should move her fingers in a systematic manner, from the outer edge toward the nipple.
- The same steps should be repeated on the left side using the right hand.
- Lastly, she should gently squeeze each nipple to check for any discharge or fluid.
WHAT TO LOOK FOR DURING BSE
- New lump or mass in the breast or underarm area.
- Thickened areas or firm nodules that feel different from surrounding tissues.
- Changes in the shape or size of the breast.
- Skin changes like puckering, dimpling, or orange-peel texture (peau d’orange).
- Nipple abnormalities, including retraction, inversion, discharge (especially bloody or clear), or crusting.
- Persistent localized pain or tenderness in one breast or armpit.
- Swelling, warmth, or redness on the skin of the breast.
ADVANTAGES OF BSE
- It is cost-free, simple, and non-invasive.
- It empowers women to take responsibility for their own breast health.
- It helps in early detection, which improves treatment outcomes.
- It increases self-awareness and confidence in recognizing physical changes.
- It is especially useful in rural and resource-limited settings where mammography may not be available.
LIMITATIONS OF BSE
- BSE is not a substitute for clinical breast examination or mammography.
- It may lead to false alarms and unnecessary anxiety due to benign lumps.
- It may miss deep or small tumors, especially in obese women.
- Some women may lack confidence or proper technique in performing BSE correctly.
- It may cause delay in seeking medical care if symptoms are ignored or misinterpreted.
NURSING RESPONSIBILITIES IN PROMOTING BSE
✅ 1. Health Education and Awareness
- It is the nurse’s responsibility to create awareness about breast cancer and the importance of early detection through regular BSE.
- The nurse should explain that early-stage breast cancer often does not cause pain, so regular self-checks are essential.
- It is important to conduct individual or group education sessions during outpatient visits, health camps, antenatal clinics, and community health programs.
- The nurse should provide accurate, culturally sensitive information, especially in rural or less educated populations.
- Educational materials like charts, leaflets, posters, videos, or breast models should be used during teaching sessions.
✅ 2. Demonstration of Technique
- The nurse must demonstrate the correct steps of BSE practically, using breast models or visual aids.
- Each woman should be taught the systematic method of inspection and palpation, covering the entire breast and axillary area.
- The nurse must explain the importance of using finger pads, circular motion, and varying pressure for accurate palpation.
- She should teach women how to choose a fixed day each month for the examination and integrate it into their routine.
- The nurse should give clear, repeated instructions to ensure the woman learns the technique correctly.
✅ 3. Encouraging Routine Practice and Adherence
- It is the nurse’s duty to motivate and remind women to perform BSE every month consistently.
- She should help the woman overcome fear, embarrassment, or shyness, especially among adolescents or newly married women.
- The nurse can suggest using a calendar, diary, or phone alarm to remind them of their monthly BSE schedule.
- Women should be encouraged to include BSE as a regular part of their personal hygiene or self-care routine.
- Reinforcement during each follow-up visit helps to develop confidence and habit formation.
✅ 4. Assessment and Clarification
- The nurse should ask open-ended questions to assess the woman’s understanding of the BSE process.
- She must observe the woman’s demonstration, if possible, and correct any errors in hand movement, positioning, or technique.
- The nurse should evaluate whether the woman knows what signs to look for, such as lumps, nipple discharge, or skin changes.
- Misconceptions (e.g., BSE is not necessary without pain or symptoms) should be identified and corrected immediately.
✅ 5. Referral and Follow-Up Care
- If a woman finds any lump, change, or abnormality during BSE, the nurse must guide her to seek immediate medical evaluation.
- The nurse should assist in scheduling clinical breast examination, ultrasound, mammogram, or FNAC as advised.
- She must explain that not all lumps are cancerous, and further testing is necessary for accurate diagnosis.
- The nurse should provide emotional support and reduce anxiety during the waiting period for results.
- Documentation of the finding and referral must be done in the woman’s health record for future follow-up.
✅ 6. Role in Community and Public Health Settings
- Nurses working in community health centers, sub-centers, or urban health posts have a vital role in mass education about BSE.
- They can organize awareness camps during Breast Cancer Awareness Month (October) or local health events.
- Nurses should also involve ASHA, ANM, or women’s self-help groups in spreading awareness about breast self-examination.
- They can collaborate with NGOs and cancer screening programs to increase BSE practice coverage.
- Community-based teaching helps to reach underserved, tribal, and low-literacy populations.
5. Warning sign of cancer
✅ 1. C – Change in Bowel or Bladder Habits
- It is significant when a person experiences prolonged diarrhea, constipation, or alternating bowel habits for several weeks without dietary or lifestyle changes.
- It is important to observe any change in stool size, shape (ribbon-like), or presence of mucus or blood in stool.
- It is a warning sign when there is increased frequency, urgency, or pain during urination, especially in absence of UTI symptoms.
- It may also include incomplete bowel evacuation or a feeling of persistent fullness in the abdomen.
- These signs often indicate colon, rectal, prostate, or bladder cancers and should be medically evaluated.
✅ 2. A – A Sore That Does Not Heal
- It is concerning when a cut or ulcer does not heal within 2–3 weeks despite adequate care and medication.
- It may present as a crusted lesion that bleeds or oozes fluid repeatedly, especially in the oral cavity or skin.
- It is a warning sign when mouth ulcers are painless, white or red patches persist, especially in tobacco users.
- In genital areas, non-healing sores may be painless, irregular, and ulcerated, indicating possible malignancy.
- This symptom is common in oral cancer, skin cancer, cervical cancer, and penile cancer.
✅ 3. U – Unusual Bleeding or Discharge
- It includes postmenopausal vaginal bleeding, which should never be considered normal.
- There may be bleeding during or after sexual intercourse, which may suggest cervical or vaginal cancer.
- Unexplained blood in sputum, urine, or feces is a serious sign needing immediate investigation.
- Nipple discharge, especially if bloody or one-sided, may indicate breast cancer.
- Also, any unusual vaginal discharge with foul smell or mixed with blood can be a red flag for reproductive cancers.
✅ 4. T – Thickening or Lump in Breast or Elsewhere
- A hard, fixed lump in the breast or testicle, especially one that doesn’t move and is painless, is suspicious.
- Enlargement of lymph nodes in the neck, armpit, or groin without infection can suggest lymphoma or metastasis.
- Lump in soft tissues like thighs or arms, which gradually increases in size, can be sarcoma.
- Lumps associated with skin changes, nipple inversion, or dimpling raise further suspicion.
- Regular self-examinations are key to early detection of these lumps.
✅ 5. I – Indigestion or Difficulty Swallowing
- It is an alarming sign when swallowing solid foods or liquids becomes painful or feels obstructed.
- The person may also complain of heartburn, bloating, early satiety, or food regurgitation.
- There may be unexplained weight loss or vomiting after eating, indicating esophageal or gastric tumor.
- Persistent sore throat or sensation of lump in throat with no infection is another early clue.
- This sign is especially important in esophageal, stomach, or pharyngeal cancers.
✅ 6. O – Obvious Change in Wart or Mole
- Any mole showing rapid growth, irregular borders, or multiple colors (brown, black, red, white) should be assessed.
- Asymmetry in shape or elevation of a previously flat mole is considered dangerous.
- Bleeding, crusting, or itching from a mole or wart without injury may be an early sign of melanoma.
- Moles that grow larger than 6 mm in diameter and continue changing over time should be referred for biopsy.
- Skin cancer signs often appear on sun-exposed areas like face, arms, neck, or scalp.
✅ 7. N – Nagging Cough or Hoarseness
- A dry, persistent cough that lasts longer than 3–4 weeks, especially in smokers, may be the first sign of lung cancer.
- Hoarseness of voice, especially when not related to cold or allergies, can indicate laryngeal or thyroid cancer.
- Associated symptoms like chest pain, difficulty breathing, or wheezing worsen the concern.
- A cough producing bloody sputum (hemoptysis) is a very serious sign.
- Voice changes that do not resolve with usual treatment need ENT and oncological evaluation.
Additional Expanded Cancer Warning Signs
✅ 8. Unexplained Weight Loss
- A person losing more than 5% of body weight within 6 months without trying may have underlying cancer.
- It is particularly noted in pancreatic, stomach, lung, and liver cancers.
- Weight loss often accompanies loss of appetite and altered taste.
- It can also be due to cancer-induced metabolic changes or tumor-related cytokines.
✅ 9. Persistent Fatigue
- Cancer-related fatigue is not relieved by rest, unlike general tiredness.
- It may appear early in leukemia, colon cancer, or as a result of anemia caused by tumor bleeding.
- The fatigue can affect concentration, daily work, and physical stamina.
- It is commonly overlooked but is a critical symptom when associated with other cancer signs.
✅ 10. Recurrent or Chronic Pain
- Persistent back pain may indicate ovarian or pancreatic cancer.
- Bone pain, especially at night or without trauma, may indicate bone metastasis or multiple myeloma.
- Headaches not relieved by usual medication could be a sign of brain tumor.
- Any unexplained, localized, progressive pain should not be ignored.
Q.6 Answer the following
1. List the drugs used in critical care unit (2)
1. Cardiovascular Drugs
- Dopamine
- Dobutamine
- Norepinephrine (Levophed)
- Nitroglycerin
- Amiodarone
- Adenosine
2. Vasopressors & Inotropes
- Epinephrine (Adrenaline)
- Phenylephrine
- Vasopressin
3. Sedatives & Analgesics
- Midazolam
- Fentanyl
- Propofol
- Morphine
4. Neuromuscular Blocking Agents
- Succinylcholine
- Vecuronium
- Rocuronium
5. Anticonvulsants
- Lorazepam
- Diazepam
- Phenytoin
- Levetiracetam
6. Antibiotics (IV Broad Spectrum)
- Meropenem
- Piperacillin–Tazobactam
- Ceftriaxone
- Vancomycin
- Linezolid
7. Corticosteroids
- Hydrocortisone
- Dexamethasone
8. Gastrointestinal Drugs
- Pantoprazole
- Omeprazole
- Ondansetron
9. Diuretics & Electrolyte Agents
- Furosemide (Lasix)
- Potassium chloride
- Magnesium sulfate
10. Anticoagulants & Antiplatelets
- Heparin
- Enoxaparin
- Aspirin
- Clopidogrel
2. Discuss legal and ethicl aspect in critical care nursing (3)
LEGAL ASPECTS IN CRITICAL CARE NURSING
1️⃣ It is essential to obtain Informed Consent
It is the legal responsibility of the nurse to ensure that the patient or legal guardian has understood and signed consent before any major procedure like surgery, resuscitation, or dialysis.
2️⃣ It is important to follow Medical Negligence Laws
It is legally mandatory for the nurse to act with due care, and any negligence in administering medication, oxygen therapy, or patient monitoring may lead to lawsuits or license cancellation.
3️⃣ It is crucial to maintain Accurate Documentation
It is the legal duty of the nurse to maintain detailed and timely records of all medications, procedures, and observations, as these documents are considered legal evidence in case of disputes.
4️⃣ It is vital to protect Patient’s Rights under Indian Constitution and Nursing Acts
It is legally bound that patients are treated with dignity, respect, and confidentiality under laws like the Consumer Protection Act (CPA), and Indian Nursing Council (INC) Code of Ethics.
5️⃣ It is mandatory to follow Do Not Resuscitate (DNR) or Advanced Directive laws
It is the legal obligation of the nurse to honor DNR orders or living wills, if signed by the patient/family and approved by the attending physician.
6️⃣ It is necessary to report Medicolegal Cases (MLC)
It is the legal responsibility of the critical care nurse to report incidents like poisoning, suicide attempts, burns, and accidents to the police or legal authority.
ETHICAL ASPECTS IN CRITICAL CARE NURSING
1️⃣ It is ethical to respect Patient Autonomy
It is the ethical responsibility of the nurse to allow the patient or family to make decisions regarding treatment, even if the nurse or doctor disagrees with their choice.
2️⃣ It is crucial to maintain Beneficence (Do Good)
It is ethically important to act in the best interest of the patient, such as providing comfort, pain relief, and safe care in all situations.
3️⃣ It is necessary to follow Non-Maleficence (Do No Harm)
It is the ethical duty of the nurse to avoid causing harm, such as administering wrong medication or using unclean catheters.
4️⃣ It is moral to practice Justice (Fairness)
It is ethically required that all patients are given equal treatment regardless of age, religion, caste, socioeconomic status, or illness severity.
5️⃣ It is necessary to maintain Veracity (Truthfulness)
It is ethically important to provide honest information to the patient and family about the condition, procedures, and prognosis.
6️⃣ It is essential to ensure Confidentiality
It is ethically mandatory that nurses should never disclose patient details, reports, or conditions to unauthorized persons.
7️⃣ It is important to follow Ethical Dilemmas in end-of-life care
It is common in ICU for nurses to face ethical issues regarding ventilator withdrawal, life support, and organ donation, and they must act according to hospital policy and ethical frameworks.
3. Discuss infection control protocol in critical care nursing unit (6)
It is important to understand that the critical care unit (ICU/CCU/NICU/PICU) involves care of patients who are critically ill and often on life support systems, invasive monitoring, or long-term hospitalization.
Due to this, these patients are at high risk of acquiring infections, especially nosocomial infections (hospital-acquired infections). Therefore, a comprehensive infection control protocol is essential to ensure patient safety, prevent cross-contamination, and promote healing.
INFECTION CONTROL PROTOCOLS IN ICU
1️⃣ It is mandatory to practice strict Hand Hygiene at all levels
- It is the most effective and primary method of preventing the spread of microorganisms in the ICU.
- It is essential to perform handwashing with soap and water when hands are visibly soiled and to use alcohol-based hand rub when hands are not visibly dirty.
- As per WHO’s 5 Moments for Hand Hygiene, it is compulsory to clean hands :
- Before touching a patient
- Before a clean/aseptic procedure
- After body fluid exposure
- After touching a patient
- After touching patient surroundings
2️⃣ It is necessary to use Personal Protective Equipment (PPE)
- PPE includes gloves, gowns, surgical/N95 masks, face shields, shoe covers, and caps.
- It is important to use appropriate PPE based on the risk of exposure to body fluids or infectious material.
- It is mandatory to follow the correct donning (putting on) and doffing (removing) sequence to prevent self-contamination.
- PPE should be disposed of in biohazard containers after use.
3️⃣ It is critical to follow Aseptic Techniques during all invasive procedures
- In procedures like urinary catheterization, central line insertion, suctioning, tracheostomy care, wound dressing, and IV infusion, it is essential to use sterile gloves, sterile drapes, and antiseptic solution.
- It is required to maintain a no-touch technique and ensure only sterile instruments and items are used.
4️⃣ It is important to maintain Environmental Hygiene in the ICU
- It is mandatory that the surfaces, bed rails, trolleys, and equipment are cleaned and disinfected daily with 1% sodium hypochlorite.
- It is important to clean ventilators, infusion pumps, ECG machines, and monitors with alcohol wipes after each use.
- It is vital to maintain proper air ventilation using HEPA filters in ICU setup.
5️⃣ It is essential to prevent Ventilator-Associated Pneumonia (VAP)
- VAP is one of the most common infections in ventilated patients.
- Nursing actions to prevent VAP include:
- Keeping the head of the bed elevated to 30–45 degrees
- Performing oral care with chlorhexidine every 4 hours
- Using closed suction systems
- Avoiding unnecessary ventilator disconnections
- Checking and emptying ventilator tubing condensate safely
6️⃣ It is important to prevent Central Line-Associated Bloodstream Infection (CLABSI)
- Central lines can introduce organisms directly into the bloodstream.
- Prevention protocols include:
- Using full sterile barrier precautions during insertion
- Cleaning insertion site daily with chlorhexidine solution
- Changing dressings with sterile technique
- Monitoring the site for redness, pus, or swelling daily
7️⃣ It is essential to prevent Catheter-Associated Urinary Tract Infections (CAUTI)
Nurses must :
- Insert urinary catheters only when absolutely necessary
- Ensure aseptic insertion and maintenance of closed drainage system
- Perform daily perineal hygiene
- Remove catheters as early as possible to reduce risk
8️⃣ It is vital to follow Biomedical Waste Management Protocols
- It is important to dispose of all waste, including PPE, needles, dressings, etc., as per color-coded segregation rules:
- Yellow bag – Infectious waste
- Red bag – Contaminated plastic
- White container – Sharps like needles
- Blue bag – Glassware
- It is mandatory not to recap needles and to use needle destroyers or puncture-proof containers.
9️⃣ It is required to practice Isolation and Barrier Nursing Techniques
- Patients with highly contagious infections like MRSA, TB, COVID-19, C. difficile must be isolated in separate rooms.
- Nursing care involves :
- Using separate equipment for each patient
- Wearing PPE before entry and discarding before exit
- Labeling the patient room as “Infection Precaution”
- Limiting visitors and instructing them on precautions
🔟 It is important to follow Surveillance and Reporting Systems
Infection control nurses must :
- Monitor infection trends like VAP, CAUTI, CLABSI
- Report outbreaks to the hospital infection control committee
- Collect specimens for culture sensitivity and track resistance patterns
- Conduct root cause analysis for each hospital-acquired infection
1️⃣1️⃣ It is necessary to ensure Staff Education and Training
- Regular workshops, infection control audits, and training sessions must be conducted.
- Nurses must stay updated with national guidelines (e.g., CDC, WHO, NCDC India) and follow hospital protocols.
- It is encouraged to create a culture of safety and accountability in critical care areas.
