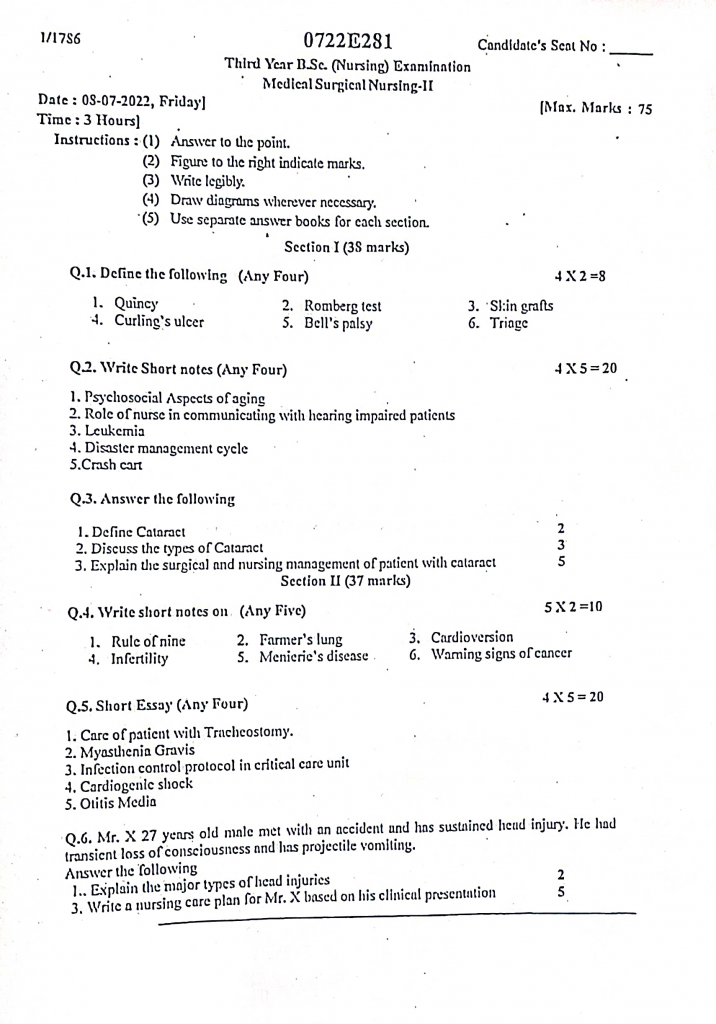
08/07/2022-B.SC-MEDICAL SURGICAL-2-PAPER DONE-UPLOAD NO.1-AHN-II
08/07/2022-B.SC-MEDICAL SURGICAL-2-PAPER DONE-UPLOAD NO.1-AHN-II
kindly send your University paper’s Image watsapp us on 8485976407. we upload its solution immediately
Section 1
Q.1 Define the following (any four) [8]
1. Quincy
- Quinsy, also known as peritonsillar abscess, is a localized collection of pus that forms in the tissues surrounding the tonsils, specifically between the tonsillar capsule and the pharyngeal muscles.
- It is usually a complication of acute tonsillitis and commonly affects young adults. It is caused by bacterial infection, most often Group A Streptococcus, and results in severe throat pain, swelling, and difficulty in swallowing.
2. Romberg test
- Romberg Test is a neurological examination used to assess a person’s sense of proprioception (the ability to sense the position and movement of the body parts).
- It is performed by asking the patient to stand upright with feet together, arms at the sides, and eyes closed.
- It is considered positive if the patient starts to sway or loses balance, indicating sensory ataxia or impaired proprioception, often associated with conditions like posterior column disorders or peripheral neuropathy.
3. Skin grafts
- Skin grafts are surgical procedures in which a piece of healthy skin is removed from one part of the body (donor site) and transplanted to cover a damaged or missing area of skin (recipient site).
- It is commonly used in the treatment of burns, extensive wounds, skin loss due to infection, surgery, or trauma. It helps in promoting healing, preventing infection, and restoring skin integrity and function.
4. Curling ulcer
- Curling ulcer is a type of acute peptic ulcer that occurs in the duodenum as a result of severe burns or extensive trauma.
- It is commonly seen in patients with major burns, especially when more than 30% of the total body surface area is affected.
- It develops due to reduced plasma volume, which leads to ischemia of the gastrointestinal mucosa, resulting in ulceration and potential bleeding.
5. Bells palsy
- Bell’s Palsy is a form of sudden, temporary, unilateral facial paralysis that results from inflammation or compression of the 7th cranial nerve (Facial nerve).
- It is characterized by sudden weakness or paralysis of the muscles on one side of the face, leading to a drooping appearance, inability to close the eye, and loss of facial expressions on the affected side.
- It is often linked to viral infections such as herpes simplex virus (HSV), and usually resolves on its own within weeks to months, though some cases may need medical treatment like steroids or physiotherapy.
6. Traige
- Triage is the process of prioritizing patients based on the severity of their condition in order to ensure that the most critically ill or injured individuals receive immediate medical care.
- It is commonly used in emergency departments, disaster sites, and mass casualty situations, where resources such as staff and equipment may be limited.
- It helps in improving patient outcomes by organizing care delivery according to urgency, often using color-coded tags or categories like immediate, delayed, minimal, and expectant.
Q.2 Write short notes (any four) [20]
1. Psychosocial aspect of aging
- The psychosocial aspects of aging refer to the emotional, social, behavioral, and mental changes that occur as a person grows older.
- These aspects affect how elderly people interact with society, cope with loss, adjust to retirement, and maintain emotional health.
1️⃣ Social Isolation and Loneliness
- It is commonly experienced by older adults due to loss of spouse, friends, or children moving away, leading to emotional emptiness.
- It is often made worse by physical limitations such as hearing loss, poor vision, or reduced mobility, which restrict social engagement.
- Elderly people living alone or in rural and urban slum areas face higher levels of isolation due to environmental or financial barriers.
- Long-term loneliness can lead to depression, cognitive decline, substance abuse, and increased mortality risk.
- They may feel forgotten or unwanted, particularly in digital societies where younger people engage online.
- It is important to promote community involvement, elder-friendly programs, and peer interaction to reduce isolation.
2️⃣ Role Changes and Retirement Adjustment
- Aging leads to transition from active work life to retired life, which results in a loss of identity, role, and structured routine.
- Many elderly people struggle with the feeling of being unproductive or useless, especially after a high-status or professional career.
- Role reversal within the family — from caregiver to dependent — can be psychologically distressing.
- Without new interests or meaningful activities, retired individuals may face boredom, frustration, and emotional decline.
- The financial impact of retirement may contribute to stress, insecurity, or over-dependence on family members.
- Nurses should promote lifelong learning, part-time volunteering, hobbies, and encourage involvement in community or religious groups.
3️⃣ Bereavement and Grief
- Aging is accompanied by multiple losses such as death of a spouse, siblings, close friends, or pets.
- Grief in elderly people can be silent and prolonged, and often goes unrecognized by family or caregivers.
- It may manifest as irritability, poor appetite, sadness, or apathy rather than open crying or despair.
- Bereavement can worsen existing health conditions or lead to depression, sleep disorders, or suicidal ideation.
- Many avoid discussing their grief due to cultural beliefs, stigma, or a desire not to “burden” family.
- Nurses should offer emotional support, group therapy, listening sessions, and refer to bereavement counselors when needed.
4️⃣ Fear of Dependence and Loss of Autonomy
- Older adults commonly fear becoming dependent on others for personal care, finances, and mobility, especially after illness or disability.
- They may resist help even when needed, due to shame, pride, or fear of losing control.
- Being placed in institutions or old-age homes without consent can result in anxiety, withdrawal, or aggression.
- Overprotective families may inadvertently restrict independence, contributing to frustration and helplessness.
- Dependency may also result in emotional abuse, neglect, or loss of dignity, particularly in crowded or resource-limited settings.
- Promoting independence through assistive devices, shared decision-making, and respect for choices enhances quality of life.
5️⃣ Body Image and Self-Esteem Issues
- Aging brings physical changes like wrinkles, sagging skin, hair loss, or mobility challenges, which affect self-perception.
- Chronic illnesses and use of medical aids like catheters, hearing aids, or walkers can create embarrassment or inferiority.
- Elderly people may feel unattractive or undesirable, especially if widowed or facing sexual health concerns.
- Social withdrawal may result from shame about incontinence, tremors, or altered physical appearance.
- Media portrayal of youthfulness often excludes aging populations, causing low self-worth and age-related stigma.
- Nurses should encourage grooming, self-care, personal dressing, and positive reinforcement to build confidence.
6️⃣ Depression and Anxiety in Old Age
- Depression is common in elderly people but often underdiagnosed, as symptoms are mistaken for fatigue or aging.
- Causes include loneliness, multiple losses, chronic illness, financial burden, and fear of death.
- Anxiety may arise from worry about dependence, safety, illness, or inability to contribute to the family.
- They may display non-verbal signs like refusal to eat, excessive sleep, irritability, or loss of interest in surroundings.
- Due to stigma, many elderly are hesitant to seek psychiatric help or counseling.
- Nurses should assess using tools like GDS (Geriatric Depression Scale) and provide empathetic counseling, family education, and referrals.
7️⃣ Cognitive Changes and Dementia
- Normal aging causes slight memory decline, but progressive conditions like Alzheimer’s and dementia severely impair brain function.
- Affected individuals show signs of forgetfulness, confusion, disorientation, and behavioral changes.
- Dementia leads to loss of self-care ability, increasing dependency and caregiver stress.
- It also causes emotional disturbances, including paranoia, agitation, and personality shifts.
- Lack of cognitive stimulation and isolation may accelerate mental decline.
- Nurses should ensure structured routines, memory aids, caregiver support, and safety measures to reduce complications.
8️⃣ Family Dynamics and Generational Gap
- Elderly individuals may feel excluded or devalued in modern family settings where younger members dominate decision-making.
- Cultural differences, digital illiteracy, and changing family roles create emotional disconnects between generations.
- Verbal or financial abuse by family members may occur, especially in resource-scarce or high-stress households.
- Lack of open communication leads to conflicts, mistrust, and isolation within families.
- When respected and involved, elders often provide wisdom, child care support, and moral guidance.
- Nurses must educate families on intergenerational respect, shared caregiving roles, and the emotional value of elders.
9️⃣ Spiritual and Existential Concerns
- Elderly individuals often reflect on life’s purpose, accomplishments, regrets, and seek closure before death.
- Fear of dying, spiritual guilt, or lack of meaning may cause emotional suffering or existential crisis.
- Many turn to prayer, meditation, spiritual rituals, or scripture for comfort and peace.
- Some may struggle with loss of religious practice due to disability or institutional living.
- Life review therapy helps them reconnect with meaningful experiences, family memories, and legacies.
- Nurses should respect spiritual beliefs, offer access to chaplains or religious leaders, and promote dignified end-of-life care.
2. Role of nurse in communicating with hearing impaired patient
1️⃣ Preparing the Environment for Communication
- It is the nurse’s responsibility to create a calm, quiet setting with minimal background noise for optimal focus and understanding.
- It is essential to ensure good lighting on the nurse’s face so the patient can clearly observe lip movements and facial cues.
- The nurse should turn off radios, TVs, and other noisy devices during conversation to reduce sensory distractions.
- It is helpful to seat the patient in a position where they can see the speaker directly without glare or obstruction.
- The nurse must avoid communicating from behind, across rooms, or while multitasking, as visual contact is critical.
- Ensuring a comfortable and safe physical environment supports longer and clearer communication without fatigue.
2️⃣ Use of Verbal and Nonverbal Techniques
- The nurse should speak clearly, slowly, and in a normal tone, avoiding shouting or exaggerated mouth movements.
- It is necessary to use simple, short, and familiar words in a calm, conversational style for easy comprehension.
- Facial expressions, hand gestures, and appropriate body language should be used to reinforce the message.
- It is helpful to pause between key sentences, allowing the patient to process or lip-read effectively.
- Maintaining direct eye contact shows respect, keeps the patient engaged, and improves mutual understanding.
- If the patient looks confused, the nurse should repeat or rephrase the message, not just speak louder.
3️⃣ Using Written Communication and Visual Aids
- The nurse should be ready to write down important instructions on paper, whiteboard, or note pad for clarity.
- It is important to use drawings, diagrams, or printed materials when explaining complex procedures or medications.
- Providing pre-printed communication cards or flashcards with common phrases helps in quick interaction.
- The nurse can ask the patient to write back questions or concerns, encouraging two-way written dialogue.
- All written information should be in large font, simple language, and preferably in the patient’s preferred language.
- Use of smartphone text apps or digital display tools is helpful if the patient is comfortable with technology.
4️⃣ Supporting Use of Hearing Aids and Assistive Devices
- The nurse should ensure the patient is wearing their hearing aid correctly and that it is functioning well.
- It is important to check for battery power, device fitting, and report any issues to the audiologist.
- The nurse may assist the patient in cleaning, inserting, or adjusting the volume of the hearing aid when requested.
- Patients using cochlear implants or amplified headsets must be positioned properly to receive sound effectively.
- If the patient has forgotten or lost their device, the nurse should adapt communication using writing or signs.
- The nurse should be aware of and utilize hospital-based assistive tools, like vibrating pagers, flashing alarms, or text-enabled devices.
5️⃣ Involving Interpreters and Alternative Communication
- If the patient uses sign language, the nurse should arrange for a certified interpreter for clear medical communication.
- In case of emergencies, the nurse may use basic sign gestures or visual cues until professional help arrives.
- Relying on family members or children to interpret should be avoided, especially for sensitive or legal discussions.
- The nurse should document the patient’s preferred communication method, such as ASL, lip reading, or writing.
- The nurse should advocate for the patient’s right to equal and accessible communication as per hospital policy.
- It is helpful for nurses to learn basic fingerspelling or common signs to build trust and rapport with hearing-impaired patients.
6️⃣ Emotional Support and Patient Empowerment
- The nurse should maintain a respectful, non-patronizing attitude to prevent the patient from feeling ignored or inferior.
- The nurse should validate the patient’s concerns, offering empathy and reassurance during every interaction.
- It is important to allow the patient extra time to respond, avoiding rushing or interrupting their communication.
- The nurse should involve the patient actively in care decisions by ensuring comprehension through repeat-back methods.
- Encouraging the use of self-advocacy tools, like communication cards or preference badges, promotes independence.
- The nurse should assess for emotional distress or withdrawal, and refer to counseling or support groups if needed.
3. Leukemia
Definition of Leukemia
- It is a malignant cancer of the blood-forming tissues, including bone marrow and lymphatic system, characterized by uncontrolled proliferation of abnormal white blood cells (leukocytes).
- It is a hematologic cancer in which the immature or abnormal WBCs crowd out normal blood cells, impairing the body’s ability to fight infections, control bleeding, and carry oxygen.
- It is classified into acute or chronic types and can involve lymphoid or myeloid cell lines.
Types of Leukemia
1️⃣ Acute Lymphoblastic Leukemia (ALL)
- It is a rapidly progressing leukemia of lymphoid precursor cells.
- It is most common in children, especially aged 2–5 years.
- It is marked by the overproduction of immature lymphoblasts in bone marrow and blood.
2️⃣ Acute Myeloid Leukemia (AML)
- It is a fast-growing leukemia affecting myeloid stem cells.
- It occurs mainly in adults over 40 years.
- It results in accumulation of immature myeloblasts, reducing normal RBCs, WBCs, and platelets.
3️⃣ Chronic Lymphocytic Leukemia (CLL)
- It is a slow-growing leukemia involving mature-looking but non-functional lymphocytes.
- It is most common in elderly adults, especially males.
- It may be asymptomatic for years but eventually leads to immunosuppression and anemia.
4️⃣ Chronic Myeloid Leukemia (CML)
- It is a gradual onset leukemia involving granulocytic precursors.
- It is strongly associated with the Philadelphia chromosome (t(9;22) translocation).
- It progresses through chronic phase, accelerated phase, and finally blast crisis if untreated.
Etiology
- Genetic mutations
- Ionizing radiation exposure
- Chemical exposure (e.g., benzene)
- Chemotherapy history
- Down syndrome or genetic disorders
- Smoking
- Viral infections (e.g., HTLV-1)
- Family history of leukemia
Pathophysiology of Leukemia
1️⃣ Mutation of Stem Cells
It is the genetic alteration of hematopoietic stem cells, causing them to proliferate abnormally.
2️⃣ Overproduction of Immature Cells
It is due to the transformation of stem cells into immature leukemic cells, which do not function normally.
3️⃣ Suppression of Normal Blood Cell Production
It is due to bone marrow overcrowding by leukemic cells, which inhibits production of RBCs, WBCs, and platelets.
4️⃣ Infiltration into Organs
It is where abnormal leukemic cells infiltrate liver, spleen, lymph nodes, and central nervous system, causing organ enlargement and dysfunction.
5️⃣ Immunosuppression and Bleeding
It is due to lack of normal WBCs and low platelet count, leading to frequent infections and hemorrhage.
Clinical Manifestations
- Fever and recurrent infections
- Pale skin (anemia)
- Fatigue and weakness
- Easy bruising and bleeding
- Petechiae and purpura
- Bone and joint pain
- Enlarged spleen/liver
- Lymphadenopathy
- Weight loss and night sweats
Diagnostic Evaluation
- History collection
- Physical examination
- CBC: Increased WBCs, low RBCs/platelets
- Peripheral blood smear
- Bone marrow aspiration and biopsy
- Cytogenetic studies (e.g., Philadelphia chromosome)
- Flow cytometry
- Lumbar puncture (in ALL for CNS involvement)
Management
1️⃣ Chemotherapy
- It is the primary treatment for all types of leukemia.
- It includes induction, consolidation, and maintenance phases, especially in acute leukemias.
2️⃣ Targeted Therapy
- It is used in CML with tyrosine kinase inhibitors like Imatinib, targeting the Philadelphia chromosome.
3️⃣ Radiation Therapy
- It is used in specific situations like CNS involvement or bone pain management.
4️⃣ Bone Marrow / Stem Cell Transplantation
- It is considered in relapsed or high-risk leukemia cases, especially AML and ALL.
- It requires HLA-matched donors and is often preceded by high-dose chemotherapy.
5️⃣ Supportive Treatment
- It includes transfusions of RBCs or platelets, antibiotics, antifungals, and growth factors (e.g., G-CSF).
Nursing Management
1️⃣ Assessment
- It is necessary to assess for signs of infection, bleeding, fatigue, and vital signs regularly.
- It is important to monitor lab reports (CBC, ANC, platelets) and document any abnormal signs.
2️⃣ Infection Control
- It is crucial to maintain neutropenic precautions, such as hand hygiene, isolation, and sterile techniques.
- It is essential to avoid raw foods, flowers, and crowded places for immunocompromised patients.
3️⃣ Bleeding Precautions
- It is important to avoid invasive procedures, soft toothbrushes, and monitor for bruising or bleeding.
- It is advised to avoid intramuscular injections and use pressure post venipuncture.
4️⃣ Medication and Chemotherapy Care
- It is essential to administer chemotherapeutic drugs as per protocol and monitor for side effects like nausea, mucositis, alopecia.
- It is the nurse’s responsibility to ensure hydration and monitor renal function during treatment.
5️⃣ Nutritional and Fluid Support
- It is necessary to provide high-protein, high-calorie soft foods, especially in mucositis.
- It is advised to monitor fluid intake and output and correct electrolyte imbalances.
6️⃣ Psychological Support
- It is helpful to offer emotional counseling, address body image issues, and reduce anxiety.
- It is essential to support the family, especially in pediatric cases.
7️⃣ Health Education
- It is important to educate about completing chemotherapy, infection warning signs, and follow-up care.
- It is advisable to teach about oral care, nutritional hygiene, and reporting early signs of relapse.
4. Disaster management cycle
Definition
- The disaster management cycle refers to the ongoing process of planning, organizing, responding to, recovering from, and mitigating the effects of disasters, whether natural or man-made.
- It is divided into four main phases: Mitigation, Preparedness, Response, and Recovery, each with specific objectives and actions.
Phases of Disaster Management Cycle
1️⃣ Mitigation Phase
- It includes actions that aim to reduce the loss of life and property before a disaster occurs.
- It involves identifying potential risks and hazards through risk mapping and vulnerability assessments.
- It includes implementing building codes, zoning laws, and environmental regulations to minimize damage.
- It emphasizes public awareness programs and education to promote disaster-resilient behaviors.
- It includes structural mitigation, such as flood barriers, earthquake-resistant buildings, and firebreaks.
- It focuses on insurance schemes and financial planning to reduce post-disaster economic burdens.
- Nurses play a role in community education about disaster risks, hygiene, disease prevention, and preparedness.
2️⃣ Preparedness Phase
- It includes activities that help individuals, communities, and governments get ready before a disaster strikes.
- It involves developing disaster response plans, communication systems, and evacuation routes.
- It includes training first responders, healthcare teams, and volunteers through mock drills and simulations.
- It includes stockpiling emergency supplies, such as food, water, medicines, and rescue tools.
- It ensures the establishment of emergency shelters and identifying safe zones for evacuation.
- It involves community-level disaster education to improve knowledge on how to act during different types of disasters.
- Nurses contribute by participating in disaster drills, organizing first aid training, and creating hospital disaster plans.
3️⃣ Response Phase
- It includes immediate actions taken during and right after the disaster to save lives and reduce impact.
- It involves search and rescue operations, providing emergency medical care, and evacuating affected populations.
- It includes distributing relief materials such as food, clean water, clothing, and shelter.
- It requires activation of emergency health services, including triage, stabilization, and transport of injured victims.
- It involves coordinating between police, fire services, military, and NGOs to ensure an organized response.
- It includes psychosocial support for victims and families suffering trauma or loss.
- Nurses are frontline responders, providing first aid, triage services, immunization, and preventing disease outbreaks.
4️⃣ Recovery Phase
- It focuses on restoring normalcy and rebuilding the affected community post-disaster.
- It involves reconstruction of infrastructure—homes, hospitals, schools, and roads.
- It includes rehabilitation of displaced people, restoring employment, education, and healthcare access.
- It provides mental health support and counseling for victims, survivors, and responders.
- It includes evaluation of the disaster response, identifying strengths, gaps, and areas for improvement.
- It ensures long-term health monitoring, management of chronic illnesses, and nutritional support.
- Nurses play a vital role in community outreach, health education, and follow-up care for affected individuals.
5. Crash cart
Definition
- A crash cart is an emergency trolley or cabinet used in hospitals to provide immediate access to life-saving equipment and drugs during medical emergencies such as cardiac arrest.
- A crash cart is a specially organized mobile trolley that holds resuscitation equipment, emergency drugs, and monitoring tools used during sudden life-threatening conditions such as cardiac arrest, respiratory failure, anaphylaxis, or shock.
- It is also known as a code cart or emergency cart and is commonly placed in ICUs, emergency rooms, operation theatres, and wards.
Purpose of Crash Cart
- It is used to store and transport emergency equipment and medications efficiently to the patient’s bedside.
- It provides a standardized and organized system for delivering immediate resuscitative care during emergencies.
- It helps reduce response time during Code Blue or cardiac arrest situations by offering all essential items in one place.
- It ensures that emergency protocols such as BLS (Basic Life Support) and ACLS (Advanced Cardiac Life Support) are followed without delays.
- It is designed to improve team coordination during high-pressure emergency situations.
- It also ensures safety, accountability, and preparedness by encouraging regular checks and inventory management.
Contents of a Crash Cart (Detailed & Categorized)
A crash cart is organized drawer-wise, with different types of items grouped for easy access.
A. Airway Management Equipment
- Bag-Valve-Mask (BVM) (Ambu bag) for manual ventilation support.
- Endotracheal tubes of various sizes for airway intubation.
- Laryngoscope with curved and straight blades + spare batteries and bulbs.
- Oropharyngeal (Guedel) airways and nasopharyngeal airways to maintain airway patency.
- Oxygen masks, nasal cannulae, and non-rebreather masks for oxygen delivery.
- Portable suction machine with suction catheters and Yankauer suction tip to clear secretions.
B. Circulation and IV Access Supplies
- IV cannulas (16G, 18G, 20G, 22G), butterfly needles, and infusion sets.
- IV fluids like normal saline, Ringer’s lactate, and Dextrose 5% for rapid fluid replacement.
- Syringes (2 mL, 5 mL, 10 mL, 20 mL) and needles of various gauges.
- Tourniquet, alcohol swabs, cotton balls, and micropore tape for IV insertion.
- Blood pressure apparatus, stethoscope, pulse oximeter, and thermometer for vital monitoring.
- Sharps disposal box and kidney trays for safe handling of used items.
C. Emergency Medications (Core Drugs)
- Adrenaline (Epinephrine) – 1:10,000 or 1:1000 for cardiac arrest and anaphylaxis.
- Atropine – for bradycardia (slow heart rate).
- Amiodarone – for life-threatening arrhythmias (ventricular fibrillation or tachycardia).
- Lidocaine, Magnesium sulfate, Calcium gluconate, and Dopamine – for cardiac stabilization.
- Sodium bicarbonate – for acidosis correction during prolonged resuscitation.
- Other emergency drugs: Naloxone (for opioid overdose), Dextrose 50% (for hypoglycemia), Nitroglycerin (for chest pain), Hydrocortisone (for allergic reactions).
D. Defibrillator and Monitoring Equipment
- Defibrillator (manual or AED) with paddles and gel pads for cardiac shock.
- Cardiac monitor with ECG leads for rhythm observation.
- Pulse oximeter, glucometer, and thermometer to assess patient condition.
- ECG electrodes, ECG paper, and blood pressure monitor.
- Gel for ECG and defibrillation to ensure proper conductivity.
- Battery backup and self-test features must be checked daily for readiness.
E. Miscellaneous and Documentation Supplies
- Sterile gloves, disposable aprons, face masks, and protective eyewear for safety.
- Scissors, artery forceps, IV stand, kidney tray, waste bags, and gauze.
- Code blue documentation forms, resuscitation record sheets, and emergency medication logs.
- CPR algorithms (BLS and ACLS) printed and laminated for quick reference.
- Inventory checklist for daily inspection of the crash cart.
- Flashlight or pen torch for neurological checks (pupil response).
Nursing Responsibilities Regarding Crash Cart
- It is the nurse’s responsibility to inspect the crash cart daily and after every use to ensure full readiness.
- The nurse must check the expiry dates of drugs, verify the quantity of supplies, and report missing or expired items immediately.
- The nurse should ensure the defibrillator is plugged in, charged, and performs a self-check regularly.
- The crash cart must be well-labeled, organized drawer-wise, and easily accessible at all times.
- The nurse must document all medications and items used during an emergency in the logbook.
- It is the nurse’s role to participate in mock codes, CPR training, and remain familiar with the location and function of all crash cart contents.
Placement and Accessibility
- Crash carts must be located in ICU, emergency room, post-op units, labor room, and high-dependency wards.
- They should be placed near nurses’ stations or where response time needs to be minimal.
- Only authorized personnel should handle and check the cart.
- All staff should be trained and updated about the layout and organization of the crash cart.
Q.3 Answer the following
1. Define cataract (2 mark)
Cataract is an ocular condition in which the natural crystalline lens of the eye becomes progressively opaque or cloudy, leading to blurred or diminished vision. It interferes with the passage of light through the lens to the retina, causing difficulty in seeing, especially in bright light. It is a painless, progressive disorder that may affect one or both eyes.
2. Discuss the types of cataract (3 mark)
1️⃣ Nuclear Cataract
- It is a type of cataract in which the central part (nucleus) of the lens gradually becomes hardened and yellowed or brown due to aging.
- It is most commonly seen in elderly individuals and progresses slowly over many years.
- It is associated with symptoms such as difficulty in distance vision, especially in bright sunlight or night driving (glare, halos).
- It may initially improve near vision temporarily, a phenomenon called “second sight.”
2️⃣ Cortical Cataract
- It is a cataract that affects the outer layer (cortex) of the lens, and it begins as wedge-shaped opacities (spoke-like) at the periphery.
- It gradually progresses toward the center of the lens, interfering with vision.
- It is commonly associated with diabetes mellitus, trauma, and aging.
- Patients may complain of glare, hazy vision, and seeing halos around lights, especially at night.
3️⃣ Posterior Subcapsular Cataract (PSC)
- It is a type of cataract that occurs at the back surface of the lens capsule, just in front of the posterior capsule.
- It affects younger individuals more commonly, especially those with prolonged steroid use, radiation exposure, or diabetes.
- It causes blurred vision while reading, trouble seeing in bright light, and increased glare or haloes.
- This type of cataract progresses more rapidly compared to other types.
4️⃣ Congenital Cataract
- It is a present-at-birth or early-childhood-onset cataract that results from genetic factors, intrauterine infections (e.g., rubella), or metabolic disorders.
- It may affect one or both eyes and can be visually significant, requiring early detection and surgery.
- If not treated early, it may result in amblyopia (lazy eye) or permanent visual impairment.
- Signs include white pupil (leukocoria) or failure to follow objects visually.
5️⃣ Traumatic Cataract
- It occurs due to direct or penetrating injury to the eye, chemical burns, or radiation exposure.
- The lens capsule may rupture, and lens proteins become opaque, causing cataract formation.
- Symptoms depend on the extent of damage, and surgical intervention is often required.
6️⃣ Secondary Cataract (After-Cataract)
- It is not a true cataract but refers to clouding of the posterior lens capsule after cataract surgery.
- It usually occurs months or years after successful cataract extraction.
- It is treated using YAG laser capsulotomy to restore clear vision.
3. Explain the surgical and nursing management of patient with cataract
Surgical Management of Cataract
Surgery is the only definitive treatment for cataract, where the cloudy natural lens of the eye is removed and replaced with a clear artificial intraocular lens (IOL) to restore vision.
✅ 1. Phacoemulsification (Modern and Most Common Technique)
- Phacoemulsification is the most widely used surgical method for cataract removal and is preferred due to its minimal invasiveness and faster healing.
- A very small incision (2–3 mm) is made on the side of the cornea through which an ultrasound probe is inserted.
- The probe emits ultrasonic waves to break the cloudy lens into tiny fragments.
- The fragmented lens is then suctioned out gently, and a foldable intraocular lens (IOL) is inserted through the same small incision.
- This technique requires no sutures, causes minimal trauma, and allows rapid visual recovery.
✅ 2. Extracapsular Cataract Extraction (ECCE)
- ECCE is used for mature or hard cataracts that cannot be removed by phacoemulsification.
- A larger incision (10–12 mm) is made in the sclera or cornea.
- The entire lens nucleus is removed in one piece, leaving the posterior capsule intact to support the IOL.
- A rigid IOL is implanted into the capsular bag, and sutures are usually needed to close the incision.
- Healing takes longer compared to phaco, and there’s a slightly higher risk of postoperative inflammation.
✅ 3. Intracapsular Cataract Extraction (ICCE)
- ICCE is a rarely used, outdated method where the entire lens and its capsule are removed together.
- It requires a very large incision and is associated with higher complication risks such as retinal detachment or vitreous loss.
- The intraocular lens is placed in the anterior chamber, rather than the capsular bag.
- This method has been replaced by safer, more effective techniques like phacoemulsification.
✅ 4. Intraocular Lens (IOL) Implantation
- In all modern cataract surgeries, after removing the natural lens, a permanent artificial lens (IOL) is implanted.
- Types of IOLs include :
- Monofocal IOL – provides vision at one distance
- Multifocal IOL – helps see both near and far
- Toric IOL – used to correct astigmatism
- IOLs are made of silicone, acrylic, or PMMA, and are well tolerated with minimal rejection risk.
Nursing Management in Cataract Surgery
Nursing care is divided into three phases : Preoperative, Intraoperative, and Postoperative.
1. Preoperative Nursing Management
- The nurse should provide complete education to the patient and their family regarding the procedure, expected outcomes, risks, anesthesia, and recovery time.
- Perform baseline assessment including vital signs, visual acuity, blood sugar, blood pressure, allergy history, and pupil dilation response.
- Administer prescribed mydriatic eye drops (e.g., tropicamide, phenylephrine) to dilate the pupil.
- Instill antibiotic drops (e.g., moxifloxacin) to reduce the risk of postoperative infection.
- Ensure the patient is kept NPO (nothing by mouth) for at least 6–8 hours before surgery as per protocol.
- Confirm informed consent has been signed, and all necessary preoperative tests (blood tests, ECG) are completed.
- The surgical eye must be marked clearly, and jewelry, dentures, and contact lenses must be removed.
2. Intraoperative Nursing Management
- The nurse should assist the ophthalmic surgeon in maintaining a sterile field and ensuring aseptic technique throughout the procedure.
- Prepare all necessary instruments including phaco probe, viscoelastics, IOL, irrigation solutions, and surgical drapes.
- Monitor the patient’s vital signs, oxygen saturation, and comfort throughout the procedure.
- Offer verbal reassurance to the patient, as they are usually awake during surgery.
- Be alert for signs of anxiety, dizziness, or adverse drug reactions to anesthetics or sedatives.
- After surgery, assist in dressing the eye, applying shield or patch, and documenting intraoperative findings.
3. Postoperative Nursing Management
- Immediate Postoperative Care (Within 24 Hours) :
- Monitor the patient for any signs of complications such as sudden pain, redness, decreased vision, excessive tearing, or bleeding.
- Assess the dressing for signs of bleeding, soaking, or displacement, and reinforce or change as per protocol.
- Ensure the patient is in a semi-Fowler’s position to reduce intraocular pressure.
- Administer prescribed eye drops such as:
- Topical antibiotics to prevent infection (e.g., moxifloxacin)
- Steroids to control inflammation (e.g., prednisolone)
- NSAID drops to reduce pain and swelling
- Provide eye shield and educate the patient to avoid rubbing or pressing the operated eye.
Ongoing Postoperative Care (Days to Weeks) :
- Educate the patient to avoid bending forward, lifting heavy weights, coughing, or straining during bowel movements for at least 1–2 weeks.
- Instruct proper hand hygiene and technique of eye drop instillation, including spacing of drops if multiple are prescribed.
- Encourage the use of dark glasses or protective eyewear, especially outdoors or during sleep.
- Explain the need for regular follow-up visits, usually on Day 1, Day 7, and after 1 month for visual assessment and spectacle prescription.
- Provide a soft diet and plenty of fluids, and prevent constipation by prescribing laxatives if needed.
- Instruct the patient to report immediately if experiencing any of the following :
- Severe or sudden eye pain
- Loss of vision
- Flashes of light or floating spots
- Discharge or foul smell from eye
- Nausea or vomiting (sign of increased intraocular pressure)
4. Long-Term Nursing Education
- Educate the patient that vision may not return immediately and will improve gradually over 4–6 weeks.
- Reinforce that a final glasses prescription will be provided only after full healing.
- Counsel the patient about the importance of managing comorbidities like diabetes and hypertension, which affect ocular health.
- Provide psychological support, especially in elderly patients adjusting to new vision changes.
Section 2
Q.4 Write short notes on (any five) [10]
1. Rule of nine
The Rule of Nines is a clinical tool used to estimate the percentage of total body surface area (TBSA) that has been burned in a patient with burn injuries. It helps in guiding fluid resuscitation, determining severity of burns, and planning medical or surgical management.
Adult Body Surface Area (BSA) Estimation – Rule of 9%:
Head and Neck – 9%
Each Upper Limb – 9% (4.5% front + 4.5% back)
Each Lower Limb – 18% (9% front + 9% back)
Front of the Trunk – 18%
Back of the Trunk – 18%
Perineum (Genital area) – 1%
2. Farmers lung
- Farmer’s Lung is a type of hypersensitivity pneumonitis, which is an inflammatory lung disease caused by repeated inhalation of organic dust, especially from moldy hay, straw, grain, or compost.
- It is an occupational lung disorder commonly seen in farmers, agricultural workers, and people working with crops and livestock.
- It results from the body’s immune reaction to inhaled fungal spores, especially Micropolyspora faeni and Thermoactinomyces vulgaris, leading to chronic lung inflammation, cough, breathlessness, and fever.
3. Cardioversion
- Cardioversion is a medical procedure used to restore a normal heart rhythm in individuals who have certain types of abnormal heartbeats (arrhythmias) such as atrial fibrillation, atrial flutter, or supraventricular tachycardia.
- It is performed either by delivering a controlled electric shock to the heart (electrical cardioversion) or by giving anti-arrhythmic medications (pharmacologic cardioversion) under medical supervision.
- It helps in re-establishing a normal sinus rhythm and preventing complications like stroke, heart failure, and sudden cardiac arrest.
4. Infertility
- Infertility is defined as the inability of a couple to conceive a child after one year of regular, unprotected sexual intercourse, despite trying to become pregnant. It may be classified as:
- Primary infertility – when a couple has never conceived.
- Secondary infertility – when a couple has conceived before but is now unable to do so.
- It can result from male factors (like low sperm count), female factors (like ovulation problems or blocked fallopian tubes), or unexplained causes.
5. Menieres disease
Meniere’s Disease is a chronic disorder of the inner ear that affects hearing and balance, caused by an abnormal accumulation of endolymphatic fluid in the inner ear (labyrinth).
It is characterized by recurrent episodes of :
- Vertigo (a spinning sensation)
- Tinnitus (ringing in the ears)
- Hearing loss
- A feeling of fullness or pressure in the affected ear
It usually affects one ear, and symptoms may come and go, but over time may lead to permanent hearing loss.
6. Warning sign of cancer
Warning signs of cancer are the early physical or symptomatic indicators that may suggest the presence of cancerous changes in the body and require prompt medical evaluation. These signs help in the early detection of cancer, improving chances of successful treatment.
Mnemonic – “CAUTION” (By American Cancer Society) :
C – Change in bowel or bladder habits
A – A sore that does not heal
U – Unusual bleeding or discharge
T – Thickening or lump in the breast or elsewhere
I – Indigestion or difficulty in swallowing
O – Obvious change in a wart or mole
N – Nagging cough or hoarseness
Q.5 Short essay (any four) [20]
1. Care of patient with tracheostomy
1️⃣ Airway Maintenance and Assessment
- It is important to assess the airway patency regularly by observing for signs of obstruction, such as gurgling breath sounds or visible mucus plug.
- It is necessary to check the position of the tracheostomy tube and ties to prevent accidental dislodgement or pressure injuries.
- It is essential to monitor respiratory rate, rhythm, depth, and oxygen saturation using a pulse oximeter every 2–4 hours or as needed.
- It is required to inspect for bilateral chest expansion and signs of labored breathing.
- It is helpful to assess for signs of early hypoxia such as restlessness, confusion, and tachycardia.
- It is important to document breathing effort, color of lips/nails, and consciousness level regularly for clinical evaluation.
2️⃣ Suctioning Care
- It is vital to perform sterile suctioning when the patient shows signs of secretion accumulation like cough, desaturation, or audible secretions.
- It is necessary to pre-oxygenate the patient for 30–60 seconds before suctioning to prevent desaturation.
- It is important to limit suction duration to under 15 seconds, and repeat only if absolutely necessary.
- It is required to observe for complications such as bradycardia, vagal response, and hypoxia during and after suctioning.
- It is recommended to use appropriate suction catheter size (not more than 1/2 the internal diameter of the trach tube).
- It is essential to check and record the amount, color, and consistency of secretions after suctioning.
3️⃣ Tracheostomy Site and Tube Care
- It is important to perform daily site care using sterile technique, clean with saline, and apply sterile gauze around the stoma.
- It is necessary to change the inner cannula once or twice daily, or sooner if visibly blocked with secretions.
- It is crucial to inspect the site for signs of infection like redness, swelling, foul odor, or purulent discharge.
- It is helpful to rotate the tube gently (if advised) to prevent tissue adherence or ulcer formation.
- It is important to ensure tracheostomy ties are not too tight, allowing one finger to slide underneath.
- It is advised to change the trach dressing when moist, soiled, or at least once daily to avoid infection.
4️⃣ Oxygenation and Humidification
- It is essential to administer humidified oxygen or air using a trach collar or T-piece to keep secretions thin.
- It is necessary to monitor oxygen saturation (SpO₂) continuously, especially during repositioning or suctioning.
- It is advised to change the humidifier water daily and use sterile water to prevent contamination.
- It is important to avoid dry gases, which can lead to crusting and blockage of the tube.
- It is also required to monitor for signs of oxygen toxicity in long-term oxygen therapy patients.
- It is helpful to ensure that oxygen delivery devices are clean and well-fitted around the trach tube.
5️⃣ Emergency Preparedness
- It is critical to keep a tracheostomy emergency kit at the bedside, including spare trach tubes (same and one size smaller), obturator, suction catheter, and ambu bag.
- It is essential to be trained and ready to respond to accidental decannulation by inserting the spare tube with the obturator.
- It is necessary to monitor for signs of airway blockage such as silent chest, labored breathing, or rising CO₂ levels.
- It is important to educate the team and family to immediately report dislodgement or difficulty in breathing.
- It is recommended to keep oxygen and suction equipment functional and within reach at all times.
- It is advised to avoid changing tracheostomy tubes alone, especially in the first 72 hours post-insertion.
6️⃣ Patient Comfort and Communication
- It is important to assist with non-verbal communication like writing boards, picture charts, or communication apps.
- It is helpful to encourage the use of speaking valves (e.g., Passy-Muir) if the airway above the trach is intact and medically approved.
- It is necessary to maintain the patient in a semi-Fowler’s or Fowler’s position to promote easier breathing and drainage.
- It is advised to offer oral and lip care regularly, especially if the patient is NPO (nil per os).
- It is essential to reduce environmental stress and reassure the patient through eye contact and gentle touch.
- It is also necessary to involve family members in communication support and emotional care.
7️⃣ Patient and Family Education
- It is necessary to teach family/caregivers the signs of infection, bleeding, blockage, or dislodgement.
- It is important to demonstrate step-by-step suctioning, cleaning, and dressing change techniques using sterile technique.
- It is required to educate them on how to humidify air and use oxygen equipment safely at home.
- It is essential to provide written instructions and visual aids for better understanding of tracheostomy care.
- It is advised to teach caregivers what to do in emergencies like accidental tube removal or difficulty breathing.
- It is also important to reinforce hand hygiene and daily cleaning of equipment to prevent infection.
2. Myasthenia gravis
Definition of Myasthenia Gravis
- It is a chronic autoimmune neuromuscular disorder in which the body produces antibodies against acetylcholine receptors (AChR) at the neuromuscular junction.
- It results in impaired transmission of nerve impulses to muscles, leading to weakness and fatigue of voluntary skeletal muscles.
- It most commonly affects ocular, bulbar, facial, and respiratory muscles and may fluctuate in severity throughout the day.
Types of Myasthenia Gravis
1️⃣ Ocular Myasthenia Gravis
- Affects only extraocular muscles, causing ptosis and diplopia.
- Often the initial presentation before generalization in some patients.
- May remain limited to the eyes in 10–20% of cases.
2️⃣ Generalized Myasthenia Gravis
- It Involves skeletal muscles beyond the eyes — such as bulbar, limb, and respiratory muscles.
- Symptoms may fluctuate throughout the day, worsening with exertion.
- It is Most common form of MG diagnosed in adults.
3️⃣ Neonatal Myasthenia Gravis
- Occurs in newborns due to transplacental transfer of maternal anti-AChR antibodies.
- It Leads to hypotonia, weak cry, poor sucking, and respiratory difficulty.
- Typically self-limiting, resolving within 2 to 3 weeks postpartum.
4️⃣ Congenital Myasthenic Syndrome (CMS)
- Inherited (genetic), not autoimmune — due to mutations affecting acetylcholine release or receptors.
- Symptoms present in infancy or childhood with generalized weakness and delayed milestones.
- Does not respond to immunosuppressants, but may benefit from specific drug therapies like ephedrine.
5️⃣ Drug-Induced Myasthenia-like Syndrome
- Certain drugs (e.g., penicillamine, aminoglycosides, beta blockers) can worsen or mimic MG symptoms.
- Symptoms usually resolve once the causative drug is discontinued.
Etiology
- Autoimmune antibody formation against AChR
- Thymus gland hyperplasia or tumor (thymoma)
- Genetic predisposition
- Viral or bacterial triggers
- Drug-induced (e.g., aminoglycosides, beta blockers)
Pathophysiology of Myasthenia Gravis
1️⃣ Autoantibody Formation
It is the immune system that produces autoantibodies against acetylcholine receptors (AChR) on the motor endplate.
2️⃣ Receptor Blockade
It is these antibodies that block or destroy ACh receptors, preventing acetylcholine from binding.
3️⃣ Impaired Neuromuscular Transmission
It is due to this blockade that nerve signals fail to stimulate muscle contraction effectively.
4️⃣ Progressive Muscle Weakness
It leads to fluctuating muscle weakness, especially after repeated use, due to reduced synaptic transmission.
5️⃣ Fatigability
It is the hallmark where muscle strength worsens with activity and improves with rest.
Clinical Manifestations
- Ptosis (drooping eyelids)
- Diplopia (double vision)
- Facial muscle weakness
- Difficulty chewing or swallowing
- Slurred speech
- Weakness in arms and legs
- Respiratory muscle weakness (myasthenic crisis)
- Symptoms worsen with activity, improve with rest
Diagnostic Evaluation
- History and neurological exam
- Edrophonium (Tensilon) test
- Anti-AChR antibody blood test
- Repetitive nerve stimulation (RNS) test
- Single fiber electromyography (SFEMG)
- Chest CT/MRI for thymoma
- Pulmonary function tests (PFTs)
Management
1️⃣ Anticholinesterase Medications
- Pyridostigmine (Mestinon) is the first-line treatment, increasing acetylcholine at neuromuscular junctions.
- May also include Neostigmine, especially in severe or hospital settings.
- Dosing is individualized and adjusted based on symptom control and side effects.
2️⃣ Immunosuppressive Therapy
- Prednisone (oral corticosteroid) is commonly used in moderate-to-severe MG.
- Steroid-sparing agents like Azathioprine, Mycophenolate mofetil, Cyclosporine may be added for long-term control.
- Rituximab, a monoclonal antibody, may be used in refractory or MuSK-antibody positive MG.
3️⃣ Plasmapheresis (Plasma Exchange)
- In which Removes circulating pathogenic autoantibodies from the bloodstream.
- It is Indicated in myasthenic crisis, preoperative preparation, or severe relapse.
- Typically provides short-term relief, often combined with other therapies.
4️⃣ Intravenous Immunoglobulin (IVIG)
- Competes with autoantibodies and modulates immune response.
- Used in acute exacerbations, pregnant women, and non-responders to other therapies.
- Onset is faster than immunosuppressants but temporary.
5️⃣ Thymectomy
- It is Recommended especially in younger patients (<60 years) and those with thymic tumors (thymoma).
- It Can result in long-term remission or reduced medication need.
- Performed via open surgery or minimally invasive techniques (VATS).
6️⃣ Respiratory and Supportive Management
- Ventilatory support in case of myasthenic crisis due to respiratory muscle weakness.
- Nutritional support (e.g., feeding tube) may be needed in cases of severe bulbar dysfunction.
- Speech therapy and physical rehabilitation improve quality of life and reduce fatigue.
Nursing Management
1️⃣ Assessment
- It is important to assess muscle strength, especially in the eyes, face, and limbs.
- It is necessary to monitor for respiratory function and signs of myasthenic or cholinergic crisis.
- It is essential to evaluate swallowing ability, speech clarity, and fatigue level during daily activities.
2️⃣ Medication Administration
- It is vital to administer anticholinesterase drugs on time, especially before meals to improve chewing.
- It is essential to monitor for cholinergic side effects like bradycardia, diarrhea, or excess saliva.
- It is necessary to educate the patient on lifelong medication adherence.
3️⃣ Prevent Aspiration and Respiratory Compromise
- It is crucial to offer soft food or thickened liquids and upright positioning during meals.
- It is necessary to suction secretions when needed and monitor oxygen saturation.
- It is vital to prepare for ventilatory support during a crisis.
4️⃣ Energy Conservation and Fatigue Prevention
- It is essential to plan short, frequent rest periods and schedule activities in the morning.
- It is helpful to assist with ADLs (Activities of Daily Living) during fatigue periods.
- It is important to prevent emotional or physical stress which may worsen symptoms.
5️⃣ Health Education
- It is the nurse’s responsibility to educate about medication timing, crisis warning signs, and infection prevention.
- It is necessary to inform about avoiding medications that may exacerbate MG (e.g., aminoglycosides, beta blockers).
- It is advisable to provide emotional support and information about support groups or neurology follow-up.
3. Infection control protocal in critical care unit
It is important to understand that the critical care unit (ICU/CCU/NICU/PICU) involves care of patients who are critically ill and often on life support systems, invasive monitoring, or long-term hospitalization.
Due to this, these patients are at high risk of acquiring infections, especially nosocomial infections (hospital-acquired infections). Therefore, a comprehensive infection control protocol is essential to ensure patient safety, prevent cross-contamination, and promote healing.
INFECTION CONTROL PROTOCOLS IN ICU
1️⃣ It is mandatory to practice strict Hand Hygiene at all levels
- It is the most effective and primary method of preventing the spread of microorganisms in the ICU.
- It is essential to perform handwashing with soap and water when hands are visibly soiled and to use alcohol-based hand rub when hands are not visibly dirty.
- As per WHO’s 5 Moments for Hand Hygiene, it is compulsory to clean hands :
- Before touching a patient
- Before a clean/aseptic procedure
- After body fluid exposure
- After touching a patient
- After touching patient surroundings
2️⃣ It is necessary to use Personal Protective Equipment (PPE)
- PPE includes gloves, gowns, surgical/N95 masks, face shields, shoe covers, and caps.
- It is important to use appropriate PPE based on the risk of exposure to body fluids or infectious material.
- It is mandatory to follow the correct donning (putting on) and doffing (removing) sequence to prevent self-contamination.
- PPE should be disposed of in biohazard containers after use.
3️⃣ It is critical to follow Aseptic Techniques during all invasive procedures
- In procedures like urinary catheterization, central line insertion, suctioning, tracheostomy care, wound dressing, and IV infusion, it is essential to use sterile gloves, sterile drapes, and antiseptic solution.
- It is required to maintain a no-touch technique and ensure only sterile instruments and items are used.
4️⃣ It is important to maintain Environmental Hygiene in the ICU
- It is mandatory that the surfaces, bed rails, trolleys, and equipment are cleaned and disinfected daily with 1% sodium hypochlorite.
- It is important to clean ventilators, infusion pumps, ECG machines, and monitors with alcohol wipes after each use.
- It is vital to maintain proper air ventilation using HEPA filters in ICU setup.
5️⃣ It is essential to prevent Ventilator-Associated Pneumonia (VAP)
- VAP is one of the most common infections in ventilated patients.
- Nursing actions to prevent VAP include:
- Keeping the head of the bed elevated to 30–45 degrees
- Performing oral care with chlorhexidine every 4 hours
- Using closed suction systems
- Avoiding unnecessary ventilator disconnections
- Checking and emptying ventilator tubing condensate safely
6️⃣ It is important to prevent Central Line-Associated Bloodstream Infection (CLABSI)
- Central lines can introduce organisms directly into the bloodstream.
- Prevention protocols include:
- Using full sterile barrier precautions during insertion
- Cleaning insertion site daily with chlorhexidine solution
- Changing dressings with sterile technique
- Monitoring the site for redness, pus, or swelling daily
7️⃣ It is essential to prevent Catheter-Associated Urinary Tract Infections (CAUTI)
Nurses must :
- Insert urinary catheters only when absolutely necessary
- Ensure aseptic insertion and maintenance of closed drainage system
- Perform daily perineal hygiene
- Remove catheters as early as possible to reduce risk
8️⃣ It is vital to follow Biomedical Waste Management Protocols
- It is important to dispose of all waste, including PPE, needles, dressings, etc., as per color-coded segregation rules:
- Yellow bag – Infectious waste
- Red bag – Contaminated plastic
- White container – Sharps like needles
- Blue bag – Glassware
- It is mandatory not to recap needles and to use needle destroyers or puncture-proof containers.
9️⃣ It is required to practice Isolation and Barrier Nursing Techniques
- Patients with highly contagious infections like MRSA, TB, COVID-19, C. difficile must be isolated in separate rooms.
- Nursing care involves :
- Using separate equipment for each patient
- Wearing PPE before entry and discarding before exit
- Labeling the patient room as “Infection Precaution”
- Limiting visitors and instructing them on precautions
🔟 It is important to follow Surveillance and Reporting Systems
Infection control nurses must :
- Monitor infection trends like VAP, CAUTI, CLABSI
- Report outbreaks to the hospital infection control committee
- Collect specimens for culture sensitivity and track resistance patterns
- Conduct root cause analysis for each hospital-acquired infection
1️⃣1️⃣ It is necessary to ensure Staff Education and Training
- Regular workshops, infection control audits, and training sessions must be conducted.
- Nurses must stay updated with national guidelines (e.g., CDC, WHO, NCDC India) and follow hospital protocols.
- It is encouraged to create a culture of safety and accountability in critical care areas.
4. Cardiogeneic shock
Definition of Cardiogenic Shock
- It is a life-threatening condition in which the heart suddenly fails to pump enough blood to meet the body’s needs, despite having adequate intravascular volume.
- It is most often a complication of severe myocardial infarction (MI) or advanced heart failure.
- It is classified under distributive or low-output shock and results in decreased cardiac output, hypotension, tissue hypoperfusion, and multi-organ failure if not promptly treated.
Types of Cardiogenic Shock
1️⃣ Ischemic Cardiogenic Shock
- It is caused by acute myocardial infarction (MI) leading to significant loss of contractile myocardium.
- It is the most common type, especially in elderly and high-risk cardiac patients.
- It is associated with STEMI, left ventricular failure, or right ventricular infarction.
- It may present with sudden hypotension, cool extremities, and pulmonary edema.
2️⃣ Mechanical Cardiogenic Shock
- It is due to structural cardiac damage such as papillary muscle rupture, ventricular septal defect, or free wall rupture after MI.
- It includes valvular disorders (acute mitral or aortic regurgitation) and cardiac tamponade.
- It usually requires surgical correction and intensive hemodynamic support.
3️⃣ Arrhythmic Cardiogenic Shock
- It results from severe bradyarrhythmias (e.g., complete heart block) or tachyarrhythmias (e.g., ventricular tachycardia/fibrillation).
- It causes abrupt reduction in cardiac output and may lead to cardiac arrest.
- It is treated with antiarrhythmic drugs, cardioversion, or pacing.
4️⃣ Fulminant Myocarditis-related Shock
- It occurs due to acute inflammation of the myocardium, often viral in origin (e.g., Coxsackie virus).
- It is common in younger individuals and may mimic acute MI.
- It can cause rapid deterioration and often requires ECMO or transplant consideration.
5️⃣ Drug-induced or Toxin-related Cardiogenic Shock
- It may occur due to cardiotoxic drugs (e.g., beta-blockers, calcium channel blockers, digoxin overdose).
- It can also result from poisoning or illicit drug use (e.g., cocaine, amphetamines).
- It requires specific antidotes, activated charcoal, and advanced cardiac life support (ACLS) measures.
Etiology
- Acute myocardial infarction (MI)
- Severe left ventricular failure
- Cardiomyopathy
- Valvular heart diseases (e.g., stenosis, regurgitation)
- Cardiac tamponade
- Life-threatening arrhythmias (VT, VF, bradycardia)
- Myocarditis
Pathophysiology of Cardiogenic Shock
1️⃣ Myocardial Injury or Dysfunction
It is due to ischemia, infarction, or inflammation that leads to reduced contractility of the ventricles.
2️⃣ Decreased Cardiac Output
It results in inadequate perfusion of vital organs like brain, kidney, and lungs.
3️⃣ Compensatory Mechanisms Activated
It is the sympathetic nervous system and RAAS that become activated to raise heart rate and vasoconstriction, but they also increase myocardial oxygen demand.
4️⃣ Increased Afterload and Worsening Hypoperfusion
It is due to vasoconstriction, leading to increased systemic vascular resistance, which further burdens the failing heart.
5️⃣ Multi-organ Dysfunction
It is caused by sustained hypoperfusion, leading to acute renal failure, liver injury, and metabolic acidosis.
Clinical Manifestations
- Hypotension (SBP < 90 mmHg)
- Cold, clammy skin
- Weak, rapid pulse
- Chest pain
- Shortness of breath
- Pulmonary crackles
- Confusion or altered LOC
- Decreased urine output
- Jugular venous distension (JVD)
Diagnostic Evaluation
- History collection
- Physical examination
- ECG (to detect MI or arrhythmia)
- Echocardiogram (to assess ejection fraction, valve function)
- Cardiac enzymes (troponin, CK-MB)
- Chest X-ray (pulmonary congestion)
- Blood gases (metabolic acidosis, hypoxia)
- Hemodynamic monitoring (CVP, pulmonary artery pressure)
- Serum lactate (tissue hypoperfusion marker)
Management
1️⃣ Oxygenation and Ventilation Support
- It is essential to provide high-flow oxygen or mechanical ventilation to maintain tissue oxygenation.
- It may require endotracheal intubation if respiratory failure occurs.
2️⃣ Hemodynamic Stabilization
- It includes fluid resuscitation cautiously, especially if there is no pulmonary edema.
- It is important to maintain mean arterial pressure (MAP) and organ perfusion.
3️⃣ Inotropic Support
- It involves drugs like Dobutamine and Dopamine to increase myocardial contractility and cardiac output.
- Norepinephrine may be used to support blood pressure in hypotensive patients.
4️⃣ Revascularization (If MI-related)
- It is necessary to restore coronary perfusion through PCI (angioplasty) or thrombolytic therapy.
- It is often combined with antiplatelet and anticoagulant therapy.
5️⃣ Mechanical Circulatory Support Devices
- It may include Intra-aortic Balloon Pump (IABP) to reduce afterload and improve coronary perfusion.
- Left Ventricular Assist Devices (LVADs) or ECMO may be used in severe cases.
6️⃣ Treatment of Underlying Cause
- It is necessary to repair valve dysfunction, treat arrhythmias, or drain tamponade if present.
- It is essential to manage comorbid conditions such as diabetes, hypertension, or sepsis if contributing.
Nursing Management
1️⃣ Assessment and Monitoring
- It is necessary to frequently assess vital signs, urine output, oxygen saturation, and level of consciousness.
- It is important to monitor cardiac rhythm, ECG changes, and central line pressures (if present).
- It is essential to document any signs of worsening shock, like mottling or decreasing urine.
2️⃣ Oxygen and Respiratory Support
- It is important to administer oxygen as ordered and assist with ventilator care if intubated.
- It is crucial to assess for respiratory distress, cyanosis, and auscultate lungs regularly.
3️⃣ Medication Administration
- It is the nurse’s responsibility to administer inotropes, vasopressors, and analgesics as prescribed.
- It is important to monitor drug side effects like tachycardia, arrhythmia, or infiltration of IV lines.
- It is vital to ensure patency of central lines and accurate pump settings.
4️⃣ Fluid and Electrolyte Management
- It is essential to track fluid input/output, daily weight, and monitor for edema or dehydration.
- It is necessary to correct electrolyte imbalances that may cause arrhythmias (e.g., K⁺, Mg²⁺).
5️⃣ Psychosocial and Family Support
- It is crucial to provide emotional reassurance, reduce anxiety, and explain procedures in simple terms.
- It is necessary to involve family members in decision-making and emergency consent when required.
6️⃣ Health Education (Post-Recovery)
- It is important to teach about cardiac rehab, dietary salt/fluid restriction, smoking cessation, and medication adherence.
- It is advisable to educate on recognizing early signs of heart failure or MI recurrence.
5. Otitis media
Definition of Otitis Media
- It is an inflammation or infection of the middle ear cavity, which is located between the tympanic membrane (eardrum) and the inner ear.
- It commonly occurs due to blockage of the Eustachian tube, resulting in fluid build-up and infection.
- It is most frequent in infants and young children, but it can affect adults as well.
- It can be acute, chronic, or with effusion (fluid without active infection).
Types of Otitis Media
1️⃣ Acute Otitis Media (AOM)
- It is a sudden onset middle ear infection, usually following an upper respiratory tract infection.
- It is characterized by ear pain, fever, and bulging of the tympanic membrane.
- It may include fluid and pus accumulation in the middle ear.
2️⃣ Otitis Media with Effusion (OME)
- It is the presence of fluid in the middle ear without signs of active infection.
- It often follows AOM or occurs with Eustachian tube dysfunction.
- It may lead to hearing loss or a sense of fullness in the ear.
3️⃣ Chronic Suppurative Otitis Media (CSOM)
- It is a long-term infection of the middle ear with persistent ear discharge (otorrhea) through a perforated tympanic membrane.
- It may result in hearing loss, and sometimes cholesteatoma formation (abnormal skin growth in the ear).
Etiology
- Bacterial infection (e.g., Streptococcus pneumoniae, Haemophilus influenzae)
- Viral respiratory infections
- Eustachian tube dysfunction
- Exposure to smoke/allergens
- Bottle feeding in supine position
- Immature immunity in children
- History of upper respiratory tract infection (URTI)
Pathophysiology of Otitis Media
1️⃣ Eustachian Tube Dysfunction
It is commonly due to inflammation or blockage from a respiratory infection or allergy, impairing ventilation of the middle ear.
2️⃣ Negative Pressure and Fluid Accumulation
It is from blocked drainage that fluid builds up in the middle ear cavity, creating a medium for microbial growth.
3️⃣ Microbial Invasion
It is the bacteria or viruses that enter from the nasopharynx into the middle ear, initiating inflammation.
4️⃣ Inflammation and Exudate Formation
It leads to mucosal swelling, pus formation, and pressure on the eardrum, causing pain and potential rupture.
5️⃣ Chronic Infection (If Untreated)
It results in perforation, persistent discharge, and may cause ossicle damage and hearing impairment.
Clinical Manifestations
- Ear pain (otalgia)
- Fever
- Hearing loss or fullness in ear
- Irritability (in children)
- Tugging/pulling at the ear
- Purulent ear discharge (if perforated)
- Tinnitus or vertigo (sometimes)
Diagnostic Evaluation
- History collection
- Physical examination
- Otoscopic examination
- Tympanometry
- Hearing tests (audiometry)
- Culture of ear discharge (if present)
- CBC (to detect infection)
Management
1️⃣ Antibiotic Therapy
- It is common to prescribe Amoxicillin (first-line) or Amoxicillin-Clavulanate in bacterial cases.
- It is essential to complete the full antibiotic course to prevent complications.
- Macrolides (e.g., Azithromycin) may be used in penicillin-allergic patients.
2️⃣ Analgesics and Antipyretics
- It is important to manage pain and fever using Paracetamol or Ibuprofen.
- It improves comfort and feeding in children.
3️⃣ Decongestants and Antihistamines
- It may be used to relieve nasal congestion and improve Eustachian tube function, especially in allergic cases.
4️⃣ Myringotomy (Surgical Drainage)
- It is a minor surgical procedure to create an opening in the tympanic membrane to drain fluid.
- It is often done when there is persistent effusion or hearing loss.
5️⃣ Tympanostomy Tube Insertion
- It is the placement of ventilation tubes into the ear to prevent fluid build-up and recurrence of infection.
- It is considered for recurrent otitis media or chronic effusion lasting over 3 months.
6️⃣ Treatment of Chronic Suppurative Otitis Media (CSOM)
- It may require aural toilet (cleaning of ear discharge), topical antibiotics, and surgery like tympanoplasty or mastoidectomy in complicated cases.
Nursing Management
1️⃣ Assessment
- It is necessary to monitor ear pain, discharge, and hearing ability.
- It is important to assess temperature, signs of systemic infection, and behavioral cues in children.
2️⃣ Medication Administration
- It is the nurse’s role to administer antibiotics, antipyretics, and ear drops as prescribed.
- It is important to ensure adherence to the full antibiotic course.
- It is essential to monitor for adverse effects or allergy to medications.
3️⃣ Ear Care and Hygiene
- It is advised to keep the ear dry, especially in CSOM or post-myringotomy cases.
- It is essential to teach safe ear cleaning — no cotton buds or objects inside the ear.
- It is helpful to gently clean external discharge with sterile cotton.
4️⃣ Supportive and Comfort Care
- It is useful to apply warm compresses to reduce pain.
- It is necessary to ensure the child gets adequate fluids, rest, and comfort.
- It is important to prevent exposure to smoke, allergens, and cold air.
5️⃣ Health Education
- It is crucial to teach parents about early recognition of symptoms and when to seek care.
- It is important to discourage bottle feeding in lying down position.
- It is advisable to complete vaccinations (e.g., pneumococcal, influenza) to prevent AOM.
- It is necessary to explain the importance of follow-up for recurrent or chronic cases.
Q.6 Mr.X 27 years old male met with an accident and has sustained head injury. He had transient loss of consciousness and has projectile vomiting. Answer the following
1. Explain the major types of head injuries (2 mark)
1️⃣ Concussion
It is a mild traumatic brain injury caused by a sudden blow or jolt to the head.
It leads to temporary loss of brain function like confusion, dizziness, or brief unconsciousness.
2️⃣ Contusion
It is a bruise on the brain tissue due to direct impact.
It causes localized swelling, bleeding, and neurological symptoms.
3️⃣ Skull Fracture
It is a break in the cranial bone caused by trauma.
Types include linear, depressed, basilar, and compound fractures.
4️⃣ Epidural Hematoma
It is bleeding between the skull and dura mater, usually from arterial rupture.
It is a medical emergency requiring immediate intervention.
5️⃣ Subdural Hematoma
It is bleeding between the dura and arachnoid layer, usually from venous rupture.
It may be acute or chronic.
6️⃣ Intracerebral Hemorrhage
It is bleeding within the brain tissue itself.
Common in high-velocity injuries or hypertension-related trauma.
2. Write a nursing care plan for Mr. X based on his clinical presentation (5 mark)
Altered level of consciousness related to cerebral trauma as evidenced by transient unconsciousness
✅ Goal :
It is to maintain optimal level of consciousness and prevent further neurological deterioration.
✅ Nursing Interventions :
- It is important to assess the Glasgow Coma Scale (GCS) every 1–2 hours to monitor neurological status and detect early signs of deterioration.
- It is essential to maintain airway patency by positioning the patient in lateral or semi-Fowler’s position to prevent aspiration in unconscious state.
- It is crucial to monitor vital signs regularly (BP, HR, RR, SpO2, temperature) to detect signs of increased intracranial pressure or shock.
- It is required to keep emergency resuscitation equipment ready at bedside (oxygen, suction, crash cart) to manage sudden decline.
- It is advisable to limit stimuli in the environment, such as noise or light, to reduce ICP elevation.
- It is necessary to administer medications such as mannitol (osmotic diuretic), antiepileptics, or sedatives as prescribed.
- It is important to provide psychological support to family members, explaining the condition and plan of care.
Risk for aspiration related to projectile vomiting and altered mental status
✅ Goal :
It is to prevent aspiration and maintain a clear airway during episodes of vomiting.
✅ Nursing Interventions :
- It is essential to position the patient in lateral (side-lying) position or elevate head-end at 30–45° to prevent aspiration.
- It is necessary to keep suction apparatus readily available to clear vomitus from airway immediately.
- It is advised to monitor for signs of aspiration such as cough, cyanosis, abnormal breath sounds or respiratory distress.
- It is important to administer antiemetics (e.g., ondansetron, metoclopramide) as prescribed to control vomiting.
- It is advised to provide NPO (nothing by mouth) status during acute phase to reduce risk of aspiration.
- It is recommended to monitor oxygen saturation (SpO2) continuously and provide oxygen if needed.
Disturbed sensory perception (visual/auditory) related to cerebral trauma as evidenced by disorientation and possible sensory changes
✅ Goal :
It is to maintain orientation and prevent complications related to sensory misinterpretation or hallucinations.
✅ Nursing Interventions :
- It is important to frequently reorient the patient to time, place, and person using clear and simple language to minimize confusion.
- It is necessary to observe for signs of sensory disturbances such as photophobia, blurry vision, hearing changes, or hallucinations.
- It is essential to keep familiar items such as clocks, calendars, or personal belongings near the patient to promote awareness.
- It is advised to provide adequate lighting in the room to reduce disorientation during nighttime.
- It is recommended to limit overstimulation by reducing noise, avoiding too many visitors, or unnecessary alarms.
- It is required to consult a neurologist or specialist if the patient complains of persistent visual or auditory changes.
- It is vital to provide a safe environment by removing clutter, using side rails, and ensuring call bell access to prevent injury due to sensory confusion.
Risk for increased intracranial pressure related to cerebral edema or hemorrhage
✅ Goal :
It is to prevent further increase in intracranial pressure and reduce the risk of brain herniation.
✅ Nursing Interventions :
- It is advised to maintain the head in midline position and avoid neck flexion to promote venous drainage.
- It is important to avoid activities that increase ICP like coughing, straining, or frequent suctioning.
- It is necessary to monitor neurological signs such as pupil size, limb strength, and response to stimuli.
- It is crucial to administer mannitol or hypertonic saline as per prescription to reduce cerebral edema.
- It is required to assess input/output balance and monitor electrolytes, especially sodium.
- It is essential to maintain a quiet and dark room environment to prevent ICP triggers.
Anxiety of family members related to critical condition of patient and lack of knowledge
✅ Goal :
It is to reduce anxiety and promote understanding of the condition and treatment plan.
✅ Nursing Interventions :
- It is necessary to provide clear and frequent information about patient’s condition and progress.
- It is advised to allow family members to visit and stay informed to reduce emotional distress.
- It is beneficial to involve family in care decisions as appropriate to build trust.
- It is important to refer them to counseling services or spiritual support as per their beliefs.