29/01/2018 child health nursing (done)-UPLOAD NO.4
29/01/2018 child health nursing (done)-UPLOAD NO.4
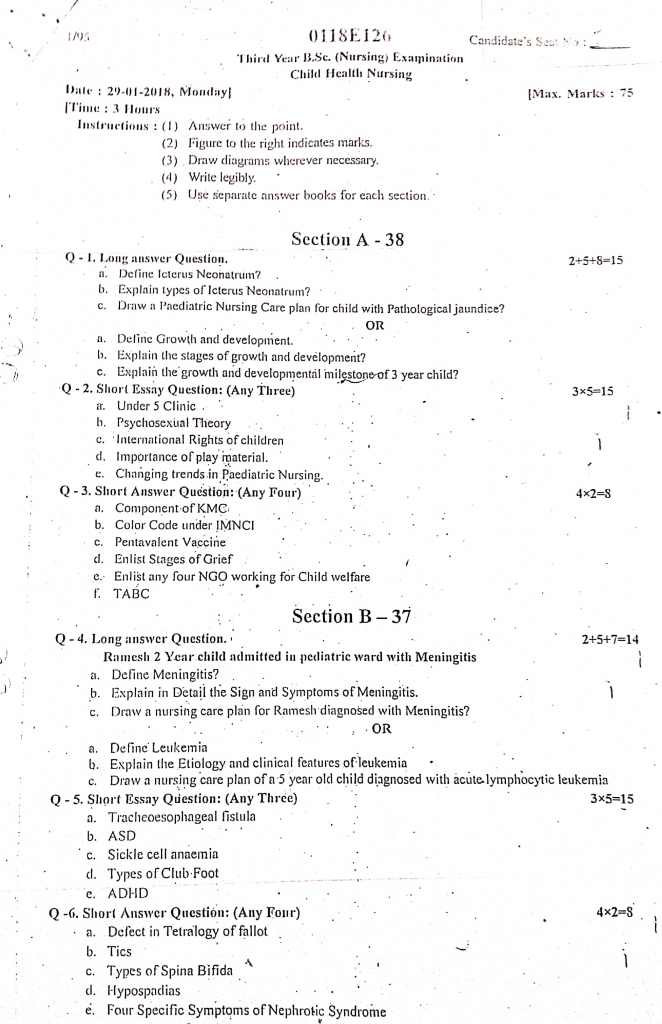
Section A-38
Q1. Long answer Question. 2+5+8=15
a. Define Icterus Neonatrum?
Icterus Neonatorum refers to the yellowish discoloration of the skin, sclera, and mucous membranes in a newborn baby due to elevated levels of bilirubin in the blood. It is commonly seen in the first week of life and is caused by the immature liver’s inability to process and excrete bilirubin efficiently. It is also known as Neonatal Jaundice.
b. Explain types of Icterus Neonatrum?
Neonatal jaundice is broadly classified into two categories :
- 1. Physiological jaundice
- 2. Pathological jaundice
1️⃣ Physiological Jaundice :
- It is the most common type of neonatal jaundice seen in healthy term and preterm newborns.
- It usually appears after 24 hours of birth and peaks around the 3rd to 5th day.
- It is caused by the immature liver’s inability to conjugate bilirubin effectively due to insufficient glucuronyl transferase enzyme activity.
- It is characterized by mild bilirubin elevation that generally does not exceed 12–15 mg/dL.
- It resolves spontaneously within 7–10 days in term infants and 2–3 weeks in preterm infants.
- It does not require treatment, only regular monitoring is necessary.
2️⃣ Pathological Jaundice :
- It is a serious form of jaundice that indicates an underlying pathological condition.
- It usually appears within the first 24 hours of life.
- It is caused by excessive hemolysis, blood group incompatibility (Rh or ABO), infections, or metabolic disorders.
- It is identified by a rapid rise in bilirubin (>5 mg/dL/day) or total levels exceeding 15 mg/dL in term infants.
- It requires immediate medical attention to prevent complications like kernicterus or acute bilirubin encephalopathy.
- It is managed with phototherapy, exchange transfusion, or treatment of the underlying cause.
3️⃣ Breastfeeding Jaundice :
- It is a type of jaundice that occurs in the first week of life, typically between day 2 and day 5.
- It is caused by insufficient intake of breast milk, leading to dehydration and reduced bilirubin elimination.
- It is associated with poor latch, infrequent feeding, and delayed milk production.
- It usually resolves once the baby starts feeding more frequently and effectively.
- It is managed by promoting regular and adequate breastfeeding.
4️⃣ Breast Milk Jaundice :
- It is a prolonged form of jaundice seen in healthy breastfed babies.
- It usually appears after the first week of life (typically between days 7–14) and may persist up to 12 weeks.
- It is caused by certain substances in breast milk, such as beta-glucuronidase, which interfere with bilirubin conjugation.
- It is not harmful, and the infant remains alert, feeding well, and gaining weight.
- It does not require discontinuation of breastfeeding.
- It usually resolves spontaneously over time.
5️⃣ Hemolytic Jaundice (Hemolytic Disease of Newborn) :
- It is a pathological type of jaundice caused by the destruction of red blood cells.
- It usually appears within 12–24 hours of birth.
- It is most commonly caused by Rh incompatibility (Rh-negative mother and Rh-positive baby) or ABO incompatibility.
- It is characterized by high bilirubin levels and signs of anemia in the newborn.
- It may lead to complications like kernicterus or hydrops fetalis if untreated.
- It is treated by phototherapy, intravenous immunoglobulin (IVIG), or exchange transfusion.
6️⃣ Jaundice in Preterm Infants (Prematurity Jaundice) :
- It is more common and more severe in preterm babies due to immature liver enzyme systems.
- It usually appears within the first few days of life and may last longer than in term babies.
- It is caused by decreased hepatic uptake, conjugation, and excretion of bilirubin.
- It increases the risk of bilirubin crossing the blood-brain barrier and causing neurological damage.
- It is managed by close bilirubin monitoring and early initiation of phototherapy.
7️⃣ Infective Jaundice (Sepsis-Induced Jaundice) :
- It is a form of jaundice caused by neonatal infections, including sepsis and TORCH infections.
- It may appear at any time during the neonatal period depending on the onset of infection.
- It is caused by liver dysfunction due to infection or cholestasis resulting in conjugated or mixed hyperbilirubinemia.
- It is associated with symptoms like fever, lethargy, vomiting, poor feeding, or abdominal distension.
- It is managed with intravenous antibiotics and supportive care.
8️⃣ Crigler-Najjar Syndrome (Genetic Type) :
- It is a rare inherited form of unconjugated hyperbilirubinemia.
- It is caused by a deficiency or absence of the enzyme UDP-glucuronyl transferase, responsible for bilirubin conjugation.
- It appears shortly after birth and may result in persistently high bilirubin levels.
It is classified as :
- Type I (severe) : No enzyme activity – requires liver transplant.
- Type II (mild) : Partial activity – may respond to phenobarbital.
- It is a lifelong condition and requires ongoing management.
c. Draw a pediatric Nursing Care plan for child with Pathological jaundice?
Assessment Data (Subjective and Objective)
Subjective Data :
- Mother complains child is sleepy and not feeding well.
- Caregivers notice yellowish discoloration of the skin and eyes.
Objective Data :
- Yellowish discoloration of sclera and skin (icterus).
- Serum bilirubin level : 18 mg/dL.
- Poor feeding, lethargy, high-pitched cry.
- Enlarged liver or spleen (in some cases).
- Diagnosed with Rh incompatibility or G6PD deficiency.
Nursing Diagnoses
- Impaired skin integrity related to bilirubin deposition in the skin.
- Imbalanced nutrition: Less than body requirement related to poor feeding and lethargy.
- Risk for neurological injury related to high serum bilirubin (kernicterus).
- Deficient knowledge of parents related to disease condition and home care.
- Fluid volume deficit related to decreased intake and increased insensible loss.
Goals and Expected Outcomes
- The child’s bilirubin levels will reduce to normal range.
- Child will show improved feeding pattern and weight gain.
- No signs of kernicterus or neurological damage will occur.
- Parents will verbalize understanding of jaundice, treatment, and phototherapy precautions.
- Skin and mucous membranes will remain intact and hydrated.
Nursing Interventions with Rationales
Diagnosis 1: Impaired Skin Integrity
Interventions :
- Monitor skin for redness, blisters, or dryness, especially under phototherapy – It is important to detect skin complications early.
- Ensure the use of eye shields and genital covering during phototherapy – It protects eyes and sensitive organs from ultraviolet damage.
- Turn the child every 2 hours – It helps prevent pressure injuries and enhances light exposure uniformly.
- Apply non-sensitizing moisturizers as prescribed – It helps maintain skin moisture without interfering with treatment.
- Maintain hygiene and change diapers frequently – It prevents skin irritation due to moisture and bilirubin excretion.
Diagnosis 2 : Imbalanced Nutrition: Less than Body Requirements
Interventions :
- Assess feeding patterns and weight daily – It helps evaluate nutritional status and progress.
- Encourage frequent breastfeeding every 2–3 hours – It promotes bilirubin excretion through stool.
- Support expressed breast milk or formula feeding if direct breastfeeding is inadequate – It ensures calorie needs are met.
- Record intake-output chart and calorie count – It ensures accurate nutritional tracking.
- Teach the mother proper latching and feeding techniques – It enhances effective feeding and bonding.
Diagnosis 3 : Risk for Neurological Injury (Kernicterus)
Interventions :
- Monitor serum bilirubin and neurological signs (e.g., lethargy, seizures, high-pitched cry) – It helps in early identification of complications.
- Ensure continuous phototherapy as per protocol – It reduces bilirubin levels rapidly and prevents accumulation.
- Provide hydration orally or via IV as ordered – It promotes elimination of bilirubin through kidneys and bowel.
- Monitor for apnea, poor muscle tone, or decreased reflexes – It is necessary to detect early signs of bilirubin encephalopathy.
- Report any signs of kernicterus immediately to physician – Early intervention can prevent permanent brain damage.
Diagnosis 4 : Deficient Knowledge of Parents
Interventions :
- Assess parent’s knowledge about jaundice and phototherapy – It helps identify educational needs.
- Explain the causes, signs, and dangers of pathological jaundice in simple terms – It promotes understanding and compliance.
- Teach the importance of regular feeding and follow-up bilirubin checks – It ensures continuity of care.
- Inform parents about eye protection, skin care, and duration of phototherapy – It involves them in safe home and hospital care.
- Provide written materials or demonstrations for reinforcement – It strengthens learning.
Diagnosis 5 : Fluid Volume Deficit
Interventions :
- Monitor hydration status: fontanelle, skin turgor, mucous membranes – It is vital to detect early signs of dehydration.
- Encourage breastfeeding every 2–3 hours or offer expressed milk – It ensures optimal fluid intake.
- Monitor urine output (number of wet diapers) and stool frequency – It assesses hydration and bilirubin excretion.
- Administer IV fluids if prescribed in severe cases – It supports physiological stability.
- Maintain room temperature to reduce insensible fluid loss – It helps preserve hydration.
Evaluation
- Child’s bilirubin reduced from 18 mg/dL to <10 mg/dL.
- Child started feeding every 2 hours and showed gradual weight gain.
- No signs of kernicterus or neurological damage observed.
- Parents verbalized proper understanding of home care and phototherapy.
- Skin integrity remained intact; child was adequately hydrated.
OR
a. Deline Growth and development.
Growth
Growth is a quantitative increase in the size, height, weight, or mass of the body or any of its parts. It refers to physical changes and can be measured in units (like centimeters or kilograms). Example : Increase in height or weight of a child.
Development
Development is a qualitative improvement in the functioning or capabilities of the individual. It refers to the maturation of physical, emotional, intellectual, and social abilities. Example : A child learning to speak, walk, or develop social skills.
b. Explain the stages of growth and development?
1️⃣ Prenatal Stage (Conception to Birth)
- It is the initial stage of life, beginning at conception and lasting until birth.
- It is divided into :
- Germinal Stage (0–2 weeks) : Fertilization and implantation.
- Embryonic Stage (2–8 weeks): Major organ systems begin to form.
- Fetal Stage (9 weeks to birth): Growth and maturation of systems.
- It is critical due to high vulnerability to teratogens, infections, and nutritional deficiencies.
2️⃣ Infancy (Birth to 1 year)
- It is a rapid growth period both physically and neurologically.
- Physical development: Birth weight doubles by 5–6 months, triples by 1 year; teeth eruption begins.
- Motor development: Rolling over (4–6 months), sitting (6–8 months), standing with support (9–10 months), walking (by 12 months).
- Cognitive development: Sensorimotor stage (as per Piaget) – learning through senses and movement.
- Emotional development: Stranger anxiety, attachment to caregivers.
- It is marked by immunizations, breastfeeding, and early stimulation.
3️⃣ Toddler Stage (1 to 3 years)
- It is the stage of autonomy, curiosity, and language explosion.
- Physical development: Slower growth rate, improved coordination, 12–16 teeth appear.
- Motor skills : Walking independently, climbing, beginning toilet training.
- Cognitive development : Symbolic thought begins, object permanence strengthens.
- Language : Vocabulary increases from a few words to over 100.
- Behavioral traits : Temper tantrums, negativism, separation anxiety.
- It is important to provide a safe environment and positive reinforcement.
4️⃣ Preschool Stage (3 to 6 years)
- It is the stage of imaginative play and beginning of social interaction.
- Physical development : Steady growth in height and weight.
- Motor development : Ability to hop, draw, use scissors, dress self.
- Cognitive development : Preoperational stage – egocentric thinking, magical beliefs.
- Social development : Making friends, learning gender roles, playing in groups.
- Language : Sentences become more complex; asking many questions.
- It is essential to encourage independence and prepare for school.
5️⃣ School-Age Stage (6 to 12 years)
- It is the stage of industry, learning, and social skill development.
- Physical growth : Slower but steady; strength and stamina improve.
- Cognitive development : Concrete operational stage – logical thinking, conservation, classification.
- Social skills : Peer influence increases; cooperation and teamwork develop.
- Emotional development : Developing self-esteem, understanding right and wrong.
- It is crucial to support education, moral development, and healthy self-concept.
6️⃣ Adolescence (12 to 18 years)
- It is the stage of identity formation, puberty, and independence.
- Physical changes : Secondary sexual characteristics, growth spurts, menarche in girls.
- Cognitive development : Formal operational stage – abstract thinking, decision making.
- Emotional development : Mood swings, peer pressure, identity crisis.
- Social development : Friendships, attraction to opposite sex, risk-taking behavior.
- It is important to provide emotional support, sex education, and guidance.
7️⃣ Early Adulthood (18 to 40 years)
- It is the stage of intimacy, career development, and life stability.
- Physical health is at its peak, but lifestyle habits start to influence future well-being.
- Emotional development : Intimate relationships, marriage, and family planning.
- Cognitive skills : Mature problem solving, ethical thinking.
- It is a time to achieve economic independence and social responsibilities.
8️⃣ Middle Adulthood (40 to 65 years)
- It is the stage of productivity and evaluation of life’s achievements.
- Physical changes : Wrinkles, menopause in women, graying hair, reduced stamina.
- Cognitive development : Peak of career and wisdom.
- Social roles : Parenting teenagers, becoming grandparents, community involvement.
- Emotional issues : Mid-life crisis, empty nest syndrome.
- It is essential to focus on health screenings and stress management.
9️⃣ Late Adulthood (65 years and above)
- It is the stage of reflection, retirement, and physical decline.
- Physical changes : Decreased mobility, vision/hearing loss, chronic illnesses.
- Cognitive changes : Memory issues, risk of dementia or Alzheimer’s in some.
- Social aspects : Retirement, isolation, loss of spouse or friends.
- Emotional development : Coping with aging, life review, satisfaction or despair.
- It is important to promote dignity, support systems, and mental well-being.
c. Explain the growth and developmental milestone of 3 year child?
- Growth and developmental milestones are age-specific functional skills or tasks most children can do at a certain age.
- The 3-year-old child is in the toddler to early preschool stage, marked by refined motor skills, language explosion, and social independence.
- It is a crucial phase in the child’s development because it lays the foundation for future learning, behavior, and health.
✅ 1. Physical Growth Milestones
- It is a period of slow and steady growth after the rapid growth seen in infancy.
- Average weight : Around 13 to 14 kg, which is about quadruple the birth weight.
- Average height : About 90–96 cm, increasing by approximately 6–8 cm per year.
- Head circumference : Reaches around 49–50 cm, with a proportionate body structure.
- Chest circumference equals or slightly exceeds head circumference.
- Fat distribution decreases, and the child appears leaner and more muscular than a toddler.
- All 20 primary (deciduous) teeth are usually present.
- Appetite may decrease, a normal phenomenon known as physiological anorexia.
✅ 2. Gross Motor Development
- It is marked by enhanced balance, posture, and mobility.
- Walks and runs with improved coordination and without falling.
- Climbs stairs using alternate feet while going up and may still use both feet while descending.
- Stands on one foot momentarily and begins to hop on one foot.
- Jumps in place and forward, begins to gallop.
- Can kick a large ball forward without falling.
- Begins to ride a tricycle with ease.
- Catches a ball with stiff arms.
- Throws objects overhead without losing balance.
- It is the stage where active outdoor play significantly improves neuromuscular coordination.
✅ 3. Fine Motor Development
- It is the stage of growing hand-eye coordination and finger dexterity.
- Builds a tower of 8–10 cubes.
- Copies a circle and vertical line.
- Turns book pages one at a time, can open doors with handles.
- Holds a crayon with fingers instead of a fist (tripod grasp begins).
- Begins to cut paper with blunt scissors under supervision.
- Strings large beads, completes simple puzzles (3–4 pieces).
- Can draw a person with 2–4 body parts (e.g., head and legs).
- Feeds self well with spoon and begins to use a fork.
- Starts dressing self, though needs help with buttons/zippers.
✅ 4. Language Development
- It is a time of explosive language qacquisition and clearer speech.
- Vocabulary expands to 900–1000 words or more.
- Forms 3–5 word sentences, often with correct grammar.
- Identifies self by full name, age, and sometimes gender.
- Repeats rhymes, sings songs, and uses plurals and pronouns (“I”, “me”, “you”).
- Understands prepositions like “in”, “on”, “under”.
- Carries out 2–3 step commands (e.g., “Pick up your toy and give it to me”).
- Frequently asks “why?” and “how?”, reflecting cognitive growth.
- Speech is understandable to strangers about 75% of the time.
- Begins to talk to toys, demonstrating imagination and role-play through language.
✅ 5. Cognitive Development (Piaget’s Preoperational Stage
- It is the stage of symbolic thinking, fantasy play, and egocentrism.
- Engages in pretend or imaginative play (“playing house”, “doctor”).
- Can identify and name 2–4 colors, basic shapes.
- Understands the concepts of “big vs small”, “long vs short”.
- Can follow simple stories and answer simple questions about them.
- Understands past and present but has difficulty grasping future time.
- Begins to solve simple puzzles and match similar objects.
- Displays magical thinking – believes in fairies, monsters, etc.
- Has limited understanding of cause and effect – may believe thoughts can cause events.
✅ 6. Emotional and Social Development
- It is a sensitive stage for emotional regulation and social adaptation.
- Demonstrates increased independence: wants to do things “by myself”.
- Shows attachment to parents/caregivers, but enjoys playing with peers.
- Begins to understand sharing and turn-taking, though may still be possessive.
- Exhibits a variety of emotions – pride, jealousy, fear, embarrassment.
- Has occasional tantrums when frustrated.
- Shows fear of imaginary creatures, the dark, or separation.
- Develops imaginary friends, which are normal at this age.
- Begins to show empathy – may offer comfort when someone is sad.
✅ 7. Self-Care and Personal-Social Skills
- It is the stage of emerging independence in daily activities.
- Can undress and put on simple clothes with little help.
- Completes toilet training during daytime, though occasional accidents may happen.
- Washes and dries hands with supervision.
- Begins brushing teeth with help.
- Can help in tidying up toys or setting the table.
- May help feed pets or perform small household tasks under supervision.
- Follows simple safety instructions like holding hands while crossing the street.
✅ 8. Play Patterns and Behavior
- It is the age of associative and imaginative play.
- Prefers group play, although may not fully cooperate in shared goals.
- Likes to imitate adult roles, such as cooking, driving, teaching.
- Enjoys simple board games, puzzles, stacking blocks, and dolls.
- Likes repetition – may enjoy the same story, game, or song repeatedly.
- Uses play to express feelings, relieve anxiety, and process experiences.
- Engages in parallel play, gradually moving toward interactive play.
Q-2. Short Essay Question: (Any Three)3+5=15
A. Under 5 Clinic
Definition
An Under-Five Clinic is a comprehensive child health service unit that provides preventive, promotive, curative, and educational services to children from birth up to five years of age. It plays a vital role in reducing child morbidity and mortality and promoting optimal growth and development.
Objectives of Under-Five Clinic
- To reduce infant and under-five mortality through timely immunization, early diagnosis, and treatment.
- To monitor and promote growth and development using growth charts and health check-ups.
- To detect and manage malnutrition and common childhood illnesses like ARI, diarrhea, anemia, etc.
- To educate and empower mothers and caregivers about child care, hygiene, nutrition, and family planning.
- To provide immunization services according to the National Immunization Schedule.
- To offer referral services for children with complications or developmental delays.
Components / Services of Under-Five Clinic
✅ Growth Monitoring
Growth monitoring involves regularly measuring and recording the child’s weight and height, plotting them on standardized growth charts to assess physical development and detect signs of malnutrition or abnormal growth patterns early.
✅ Nutritional Surveillance
Nutritional surveillance includes periodic assessment of the child’s dietary intake, anthropometric measurements, and clinical signs to identify nutritional deficiencies such as protein-energy malnutrition, anemia, and vitamin A deficiency, followed by appropriate dietary counseling and supplementation.
✅ Immunization
Immunization services are provided according to the National Immunization Schedule, ensuring timely administration of vaccines like BCG, OPV, DPT, Hepatitis B, Pentavalent, Measles-Rubella, and others to protect children against preventable infectious diseases.
✅ Treatment of Minor Ailments
The clinic offers early diagnosis and treatment of common childhood illnesses such as diarrhea, acute respiratory infections, fever, skin diseases, and worm infestations, using standardized protocols including ORS, zinc tablets, and deworming medications.
✅ Vitamin A Supplementation and Deworming
Children aged 9 months to 5 years receive periodic Vitamin A syrup every six months to prevent xerophthalmia and improve immunity, along with deworming tablets every six months to control intestinal worm infestations.
✅ Health Education and Counseling
Mothers and caregivers are educated on topics like exclusive breastfeeding, timely complementary feeding, personal hygiene, sanitation, prevention of communicable diseases, recognition of danger signs, and the importance of full immunization and regular health checkups.
✅ Referral Services
Children showing signs of severe illness, developmental delay, congenital defects, or failure to thrive are promptly referred to higher-level healthcare facilities for specialized evaluation and management to ensure timely intervention and care.
Role of the Nurse in Under-Five Clinic
✅ Growth Monitoring and Charting
The nurse is responsible for regularly weighing and measuring the height of under-five children, plotting these on WHO growth charts, and identifying any deviations such as underweight, stunting, or wasting.
✅ Immunization Services
The nurse administers vaccines as per the National Immunization Schedule, ensures correct technique, observes for adverse reactions, maintains cold chain, and keeps accurate immunization records.
✅ Nutritional Assessment and Counseling
The nurse assesses dietary history, identifies signs of nutritional deficiencies like anemia or protein-energy malnutrition, and provides counseling to mothers on breastfeeding, complementary feeding, and balanced nutrition.
✅ Management of Minor Illnesses
Nurses assess and treat minor ailments such as diarrhea, respiratory infections, and skin conditions using standing orders, and dispense appropriate medications like ORS, zinc, and deworming tablets.
✅ Vitamin A and Deworming Administration
The nurse ensures the timely administration of Vitamin A syrup and deworming tablets to children according to government guidelines.
✅ Health Education to Mothers and Caregivers
The nurse plays a crucial role in educating mothers about child care practices, hygiene, sanitation, home remedies, feeding techniques, immunization importance, and recognizing danger signs.
✅ Screening for Developmental Delays
Nurses observe for developmental milestones and assess early signs of delays or disabilities, making appropriate referrals for further evaluation and intervention.
✅ Record Keeping and Reporting
The nurse maintains individual child health cards, registers all services provided, compiles data, and submits reports to health authorities for program evaluation.
✅ Referral Services
Children requiring further medical attention due to complications, growth failure, or congenital issues are referred by the nurse to Primary Health Centres (PHCs) or hospitals for advanced care.
✅ Follow-Up and Home Visits
Nurses follow up on children who miss clinic visits, especially those with growth faltering or immunization default, often conducting home visits to ensure continuity of care.
b. Psychosexual Theory
Introduction
- The Psychosexual Theory was proposed by Sigmund Freud, an Austrian neurologist and the founder of psychoanalysis.
- It is based on the belief that human personality develops through a series of childhood stages, in which the pleasure-seeking energies of the id (called libido) become focused on certain erogenous areas.
- It is important because Freud believed that early childhood experiences play a critical role in shaping adult personality and behavior.
- In this theory, failure to resolve conflicts at any stage may lead to fixation, which results in psychological problems later in life.
Stages of Psychosexual Development
Oral Stage (0 to 1 year)
- It is the first stage of psychosexual development, in which the mouth is the primary source of pleasure.
- In this stage, the child gains pleasure through sucking, biting, breastfeeding, and exploring objects with the mouth.
- It is a crucial period for developing trust and attachment.
- If fixation occurs (e.g., due to early weaning), the child may develop oral personality traits like smoking, nail-biting, overeating in adulthood.
- Nursing Importance: Nurses should ensure proper breastfeeding, comfort feeding, and support bonding between infant and mother during this stage.
Anal Stage (1 to 3 years)
- It is the stage where the child’s focus shifts to the anus, and pleasure is derived from controlling bowel movements.
- In which the child is learning toilet training, and this stage is associated with autonomy and control.
- A supportive toilet training process helps the child develop a sense of independence and accomplishment.
- Fixation can result in anal-retentive personality (overly neat, rigid) or anal-expulsive personality (messy, disorganized).
- Nursing Importance : Nurses can assist parents in positive reinforcement techniques during toilet training and guide them on normal bowel habits.
Phallic Stage (3 to 6 years)
- It is the stage in which the genitals become the focus of pleasure, and the child becomes curious about the differences between sexes.
- In which Freud introduced concepts like the Oedipus complex (in boys) and Electra complex (in girls), involving unconscious desires for the opposite-sex parent.
- Resolution of these complexes leads to gender identity formation and internalization of moral values.
- If unresolved, fixation may result in relationship problems, guilt, or sexual identity issues in adulthood.
- Nursing Importance : Nurses should encourage healthy curiosity, avoid shaming of body parts, and support age-appropriate education on body image and privacy.
Latency Stage (6 to 12 years)
- It is the stage where sexual energy is dormant (latent), and the child focuses on school, friendships, hobbies, and skill-building.
- In which intellectual and social development takes priority, and the libido is channeled into social interactions and peer relationships.
- This stage helps the child build self-confidence, discipline, and teamwork.
- Fixation is less likely here but may result in lack of social skills or low self-esteem if the child is isolated.
- Nursing Importance: Pediatric nurses and school health nurses should promote peer bonding, group activities, and positive self-image.
Genital Stage (12 years and above)
- It is the final stage, in which the sexual impulses reawaken with puberty, and the individual seeks mature, adult sexual relationships.
- In which emotional attachment, intimacy, and sense of identity are strengthened.
- Successful navigation of this stage leads to balanced personality, healthy sexual identity, and strong interpersonal relationships.
- Fixation can cause relationship difficulties, identity confusion, or sexual dysfunction.
- Nursing Importance : Nurses must support adolescents through puberty education, counseling, and mental health guidance, especially in school and community settings.
Nursing Implications of Psychosexual Theory
✅ 1. Understanding Child Behavior Based on Developmental Stage
- It is important for nurses to understand and interpret behaviors such as thumb-sucking, temper tantrums, or toilet resistance based on the child’s psychosexual stage.
- In which behaviors like oral fixation in infants or anal control in toddlers can be viewed not as misbehavior but as normal developmental expressions.
- It helps the nurse to avoid mislabeling or punishing developmentally appropriate actions, thereby providing age-appropriate emotional support.
✅ 2. Planning Age-Appropriate Nursing Interventions
- It is essential for nurses to plan interventions based on the child’s psychosexual needs and stage of conflict.
- In which an oral-stage child should be comforted with pacifiers, oral medication syringes, and frequent cuddling, whereas an anal-stage child may benefit from praise during toilet training.
- It also allows for play therapy, storytelling, and therapeutic communication methods appropriate to the emotional maturity of the child.
✅ 3. Providing Holistic and Developmentally Appropriate Care
- It is the nurse’s responsibility to provide care that matches the psychosocial and psychosexual maturity of the child.
- In which the nurse must respect the child’s need for autonomy during anal stage, or privacy and body image during phallic and genital stages.
- It also includes ensuring that procedures are explained using age-appropriate language, so the child feels safe and understood.
✅ 4. Supporting Parent Education and Counseling
- It is essential for pediatric and community health nurses to educate parents about normal psychosexual development and reassure them about common behaviors like genital curiosity or toilet regression.
- In which counseling can help prevent negative reinforcement, such as shame or punishment, that may lead to fixation or later maladjustment.
- It also involves guiding parents on setting healthy boundaries without using fear or guilt in early developmental years.
✅ 5. Identifying Maladaptive Behaviors and Emotional Regression
- It is useful for nurses to observe for signs of fixation or regression, such as thumb-sucking in an older child, excessive neatness, or aggression.
- In which unresolved conflicts at any stage can manifest as maladaptive coping behaviors during stress, illness, or hospitalization.
- It helps the nurse to report psychological issues early and refer the child for mental health evaluation or play therapy, if needed.
✅ 6. Enhancing Therapeutic Communication with the Child
- It is important for the nurse to adjust communication style based on the child’s developmental and emotional age as per Freud’s stages.
- In which children in the latency stage may be more responsive to group play and peer support, while oral-stage infants need more touch and comfort.
- It helps to create a trusting and healing environment, especially in clinical or hospital settings.
✅ 7. Promoting Healthy Sexual Development and Education
- It is the nurse’s duty, especially in school and adolescent health settings, to offer accurate, age-appropriate sexual health education.
- In which genital-stage adolescents should be given guidance on body image, menstruation, safe practices, and emotional changes.
- It supports the prevention of guilt, misinformation, and risk behaviors related to poor sexual development.
✅ 8. Reducing Hospital Anxiety Through Developmental Support
- It is crucial in pediatric wards where hospitalization can trigger regression to earlier stages, like bedwetting or attachment behavior.
- In which the nurse can use comfort items, routines, familiar toys, or family presence to help the child feel secure.
- It also helps reduce emotional trauma and supports faster psychological recovery.
c. International Rights of children
The United Nations Convention on the Rights of the Child (UNCRC) is a legally binding international agreement adopted in 1989 to protect and promote the rights of children worldwide. These rights ensure that children live with dignity, freedom, protection, and access to essential services for healthy growth and development.
1. Right to Survival
- Every child has the inherent right to life and survival from birth.
- Governments must ensure policies that support child health and nutrition programs.
- Access to safe drinking water, sanitation, and hygienic living conditions must be guaranteed.
- Measures to prevent malnutrition and communicable diseases should be prioritized.
- Emergency healthcare services should be accessible during disasters or epidemics.
2. Right to Development
- Right to free and compulsory primary education for every child.
- Opportunities for skill development, vocational training, and higher education should be available.
- Promotion of cultural and recreational activities to support mental and emotional growth.
- Access to early childhood development programs to support brain development in formative years.
- Special provisions for children belonging to marginalized and minority communities to ensure equal development.
3. Right to Protection
- Protection from economic exploitation and hazardous work environments.
- Laws must prevent recruitment of children in armed forces or conflict zones.
- Strict measures against child trafficking, child pornography, and online exploitation.
- Immediate rehabilitation and reintegration programs for rescued children.
- Establishment of child helplines and child protection committees at community levels.
4. Right to Participation
- Children’s views must be considered in matters related to education, health policies, and community decisions.
- Platforms should be created for children’s councils and youth parliaments.
- Right to freedom of expression through media, writing, art, and peaceful assembly.
- Encouragement to participate in cultural heritage preservation and environmental initiatives.
- Special attention to including children with disabilities in participatory activities.
5. Right to Non-Discrimination
- Equal rights must be ensured regardless of race, color, sex, language, religion, political opinion, national or social origin.
- Protection against discriminatory practices in education, healthcare, and legal systems.
- Policies should promote gender equality and inclusion of LGBTQ+ children.
- Special attention to children affected by migration, refugee status, or statelessness.
- Accessible infrastructure and communication methods for children with disabilities.
6. Right to Health and Nutrition
- Immunization programs should be universally available and accessible.
- Provision of adolescent health services, including reproductive and mental health counseling.
- Implementation of school health programs for early detection of health issues.
- Access to affordable and nutritious food under government welfare schemes.
- Regular monitoring of growth and development indicators through healthcare services.
7. Right to Family Environment
- Priority placement with biological families whenever possible, ensuring a safe environment.
- In cases of parental separation, the child’s best interest must be prioritized regarding custody.
- Availability of adoption services following ethical and legal procedures.
- Protection of children from domestic violence and neglect.
- Community-based child care and family strengthening programs should be implemented.
8. Right to Identity
- Every child should receive birth registration immediately after birth.
- Legal identity ensures access to essential services like education, healthcare, and social welfare programs.
- Protection of the child’s name, nationality, and cultural identity, especially for indigenous and tribal communities.
- Governments must prevent statelessness by ensuring nationality rights to children born on their soil.
9. Special Rights for Children with Disabilities
- Ensure accessibility in public spaces, schools, transportation, and communication technologies.
- Provision of inclusive education programs and special education facilities when needed.
- Availability of assistive devices and rehabilitation services.
- Protection against stigma, neglect, and abuse in institutions or care homes.
- Promotion of their independence, dignity, and full participation in society.
d. Importance of play material.
It promotes physical development
- It is important because physical play materials like balls, climbing ropes, tricycles, and jumping tools help in the development of gross motor skills, which are essential for strength, balance, and coordination.
- In which fine motor materials such as blocks, threading beads, crayons, and clay improve hand-eye coordination, finger dexterity, and grip control.
- It helps children, especially toddlers and preschoolers, to develop body awareness, posture control, and spatial orientation, all of which are crucial for their future physical tasks like writing or sports.
It stimulates cognitive and intellectual growth
- It is important because play materials like shape sorters, number blocks, alphabet boards, and puzzles stimulate thinking ability, concentration, and memory in children.
- In which educational toys, musical toys, and activity cubes support problem-solving, decision-making, and language development, laying the foundation for school readiness.
- It helps enhance the child’s learning through exploration, which fosters curiosity, logical thinking, and analytical abilities from early childhood.
It enhances emotional and social development
- It is essential because role-playing materials like dolls, kitchen sets, costumes, and doctor kits allow children to express emotions, rehearse social roles, and understand family dynamics.
- In which shared play with peers using toys promotes teamwork, empathy, sharing, negotiation, and patience, helping children become socially responsible.
- It helps children cope with separation anxiety, shyness, or trauma by providing a safe outlet to express their feelings and feel in control of their world.
It supports therapeutic communication and hospital play
- It is very useful in pediatric nursing because hospitalized children often face fear, pain, and emotional distress, and play materials help in reducing anxiety and provide emotional comfort.
- In which tools like puppets, soft toys, storytelling kits, drawing boards, and musical instruments are used by nurses for therapeutic play, where children are guided to express their thoughts.
- It helps nurses to build rapport with the child, gain their trust, and even assess their developmental delays, psychological needs, or understanding of their illness.
It aids in age-appropriate developmental stimulation
- It is significant because each age group has specific developmental needs, and appropriate play materials stimulate correct physical, mental, and emotional growth.
- In which infants benefit from soft rattles, mirrors, and mobiles; toddlers enjoy building blocks and musical toys; preschoolers need pretend play and creative kits; and school-age children enjoy educational board games and sports kits.
- It helps in early identification of developmental delays when a child does not respond to age-appropriate toys, thus aiding in early intervention and referral.
It provides educational value and learning opportunities
- It is beneficial because toys like educational laptops, talking books, number games, and flashcards introduce children to basic academic concepts in a fun and interactive way.
- In which learning through play develops counting, colors, shapes, vocabulary, and general knowledge, making it easier for children to adjust to school environments.
- It helps to make learning enjoyable and effective, especially for children with learning disabilities or attention difficulties.
It encourages creativity and imagination
- It is crucial because toys like drawing kits, craft materials, building blocks, and role-play costumes encourage imaginative thinking and creativity, which is vital for mental flexibility.
- In which open-ended play material (like LEGO, sand, water play) gives children the freedom to create, build, and pretend, which fosters original thinking and decision-making.
- It helps in improving storytelling skills, abstract thinking, and the ability to visualize, which are key for brain development.
It helps in behavioral observation and nursing assessment
- It is important in pediatric nursing because the way a child interacts with play materials provides clues about behavioral, cognitive, and emotional health.
- In which nurses can assess issues like aggression, withdrawal, fear, regression, or trauma by observing the type and pattern of play.
- It helps nurses to tailor individual care plans and report abnormal findings to physicians or psychologists for timely management.
e. Changing trends in Paediatric Nursing.
Pediatric nursing is a specialized area of nursing that focuses on the care of infants, children, and adolescents. Over the years, several changes have taken place in pediatric nursing due to advancements in healthcare, technology, and family dynamics.
Below are the major changing trends in pediatric nursing :
✅ 1. Family-Centered Care Approach
- It is an approach that recognizes the importance of family in a child’s recovery and involves them actively in planning and decision-making.
- In which parents are encouraged to stay with the child during hospitalization and provide emotional as well as physical care.
- It is focused on building trust and partnership between nurse, child, and family by respecting their culture, preferences, and knowledge of the child.
✅ 2. Evidence-Based Practice (EBP) in Pediatric Nursing
- It is the integration of clinical expertise with the best available research evidence to deliver quality pediatric care.
- In which guidelines are developed for managing common childhood illnesses like pneumonia, diarrhea, and neonatal sepsis based on updated clinical studies.
- It allows pediatric nurses to provide care that is current, safe, and validated by research, reducing variation in practice.
✅ 3. Use of Advanced Technology in Child Health
- It includes using pediatric-specific equipment such as neonatal ventilators, infusion pumps, and digital monitoring devices.
- In which telehealth and remote consultation are used for follow-up care and parent education in rural and underserved areas.
- It is helpful in early detection of complications through technologies like continuous vital sign monitoring and automated alerts.
✅ 4. Emphasis on Preventive and Promotive Care
- It is the shift from treatment to prevention, focusing on immunization, growth monitoring, and early detection of developmental delays.
- In which pediatric nurses participate in community health programs such as IMNCI, RBSK, and Vitamin A supplementation drives.
- It includes educating caregivers about hand hygiene, safe weaning practices, exclusive breastfeeding, and hygiene during complementary feeding.
✅ 5. Holistic and Developmental Approach
- It is an approach that considers the child’s physical, emotional, cognitive, and social development as part of health care.
- In which care is planned based on developmental milestones and age-specific needs such as speech, mobility, and social interaction.
- It emphasizes the importance of emotional bonding, play, and school performance as part of overall child health evaluation.
✅ 6. Play Therapy and Therapeutic Communication
- It is used to reduce fear, anxiety, and emotional distress in hospitalized children by engaging them in developmentally appropriate activities.
- In which tools like puppets, drawing, storytelling, and role play help children express feelings and understand treatments.
- It helps nurses build rapport and trust, especially with toddlers and preschoolers, who may be non-verbal or fearful.
✅ 7. Rights of the Child and Legal Framework
- It is based on the UN Convention on the Rights of the Child, which emphasizes protection, participation, and provision for all children.
- In which pediatric nurses are legally bound to report suspected abuse or neglect to child welfare authorities.
- It ensures informed consent (or assent in older children), privacy during procedures, and the right to respectful communication.
✅ 8. Role of Pediatric Nurse Practitioner (PNP) and Specialization
- It includes advanced practice roles like Neonatal Nurse Specialist, Pediatric ICU Nurse, and Pediatric Oncology Nurse.
- In which pediatric nurses can prescribe medications, perform procedures, and manage long-term conditions independently in some countries.
- It supports early diagnosis, specialized care, and better continuity of care in complex and chronic pediatric illnesses.
✅ 9. Home-Based and Community-Based Pediatric Care
- It is the trend where chronic or rehabilitative care is extended to the child’s home and school setting to reduce hospital stays.
- In which pediatric nurses visit homes to provide care for children with disabilities, cerebral palsy, or on long-term oxygen therapy.
- It also includes coordination with Anganwadi workers, ASHAs, and school nurses to monitor child development and nutrition.
✅ 10. Increased Focus on Adolescent Health
- It is the recognition that adolescents (10–19 years) have unique health needs like mental health, sexual health, and substance abuse prevention.
- In which programs like Rashtriya Kishor Swasthya Karyakram (RKSK), WIFS, and menstrual hygiene programs are implemented by pediatric and community nurses.
- It also includes adolescent counseling, school-based health education, and promotion of safe behaviors and decision-making.
Q-3. Short Answer Question: (Any Four) 4×2=8
a. Component of KMC
Skin-to-Skin Contact :
Continuous and prolonged direct skin contact between the mother (or caregiver) and the baby, promoting warmth, bonding, and breastfeeding.
Exclusive Breastfeeding :
Encourage and support exclusive breastfeeding to provide optimal nutrition and immunity.
Early Discharge and Proper Follow-Up :
Discharge the baby early from the hospital when stable and ensure regular follow-up visits for growth monitoring and support.
b. Color Code under IMNCI
Pink Color Code – Urgent Referral or Admission :
Indicates severe illness requiring immediate hospital referral or inpatient care.
Yellow Color Code – Specific Treatment at Health Facility :
Indicates moderate illness requiring specific treatments like antibiotics or oral medications at the health center but not immediate referral.
Green Color Code – Home Care Advice :
Indicates the child is not seriously ill and can be managed safely at home with advice on care and when to return if the condition worsens.
c. Pentavalent Vaccine
Pentavalent vaccine is a combined vaccine that protects children against five life-threatening diseases in a single shot, which are Diphtheria, Pertussis (Whooping Cough), Tetanus, Hepatitis B, and Haemophilus influenzae type B (Hib). It is administered at: 6 weeks, 10 weeks, and 14 weeks of age as part of the Universal Immunization Programme (UIP).
d. Enlist Stages of Grief
Denial :
Refusing to accept the reality of the loss or situation.
Anger :
Expressing frustration and blaming self or others for the loss.
Bargaining :
Attempting to negotiate or make promises to reverse or delay the loss.
Depression :
Feeling deep sadness, hopelessness, and withdrawal from normal activities.
Acceptance :
Gradual adjustment to the loss and finding a way to move forward.
e. Enlist any four NGO working for Child welfare
UNICEF (United Nations International Children’s Emergency Fund)
Save the Children
CRY (Child Rights and You)
Smile Foundation
f. TABC
TABC is an approach used in emergency care and resuscitation, particularly for trauma patients.
T – Temperature Control
Maintain normal body temperature to prevent hypothermia, which can worsen shock and bleeding.
A – Airway Management
Ensure the patient’s airway is clear and protected to maintain effective breathing.
B – Breathing Support
Assess and support breathing through oxygen administration or mechanical ventilation if needed.
C – Circulation Support
Manage circulation and control bleeding to ensure adequate blood flow and prevent shock.
Section B-37
Q-4. Long answer Question..2+5+7=14
Ramesh 2 Year child admitted in pediatric ward with Meningitis
a. Define Meningitis?
Meningitis is an inflammatory condition of the meninges, which are the protective membranes covering the brain and spinal cord. It is commonly caused by bacterial, viral, fungal, or parasitic infections, but can also result from chemical irritation or malignancy. This condition is a medical emergency, especially in cases of bacterial meningitis, and requires prompt diagnosis and treatment to prevent severe complications like brain damage, hearing loss, or death.
b. Explain in Detail the Sign and Symptoms of Meningitis.
✅ General Signs and Symptoms (Seen in Most Patients)
1. Fever :
- It is one of the first and most common symptoms.
- Typically high-grade, with or without chills.
- It indicates the systemic inflammatory response.
2. Severe Headache :
- A constant and intense headache that is not relieved by normal painkillers.
- Occurs due to meningeal irritation and raised intracranial pressure (ICP).
3. Neck Stiffness (Nuchal Rigidity) :
- Resistance and pain during neck flexion.
- A classic sign of meningeal irritation.
- Present in both adults and older children.
4. Photophobia :
- Sensitivity to light due to irritation of optic nerve and brain meninges.
- Patients may prefer dark or dim-lit environments.
5. Nausea and Vomiting :
- Commonly associated with raised intracranial pressure.
- Vomiting is often projectile and not related to food intake.
6. Altered Level of Consciousness :
- Ranges from drowsiness to confusion, disorientation, or even coma.
- Occurs due to cerebral edema, increased ICP, or infection.
7. Seizures (Convulsions) :
- May occur due to inflammation or irritation of the cerebral cortex.
- Seen in both children and adults; can be focal or generalized.
8. Cold Hands and Feet / Shock-like Symptoms :
- Seen in advanced bacterial meningitis.
- Indicates septic shock or systemic involvement.
✅ Specific Signs of Meningeal Irritation (Classic Neurological Signs)
1. Kernig’s Sign :
- Positive when pain or resistance is felt on extension of the knee while the hip is flexed at 90°.
- Indicates stiffness of the hamstring muscles due to meningeal irritation.
2. Brudzinski’s Sign :
- Positive when passive neck flexion causes involuntary flexion of hips and knees.
- Also due to meningeal irritation.
✅ Skin and Systemic Signs (Mainly in Bacterial Meningitis)
1. Petechial or Purpuric Rash:
- Seen in meningococcal meningitis.
- Indicates sepsis with disseminated intravascular coagulation (DIC).
2. Hypotension and Tachycardia
- Part of septic shock picture.
- Requires immediate intervention.
✅ Signs and Symptoms in Infants and Young Children
(Note: Classic signs like headache or neck stiffness may be absent in this age group)
- High-pitched cry or irritability
- Bulging fontanelle (soft spot on head)
- Poor feeding or refusal to eat
- Lethargy or excessive sleepiness
- Fever or hypothermia
- Vomiting and convulsions
- Arching of back (opisthotonos)
- Seizures without clear cause
c. Draw a nursing care plan for Ramesh diagnosed with Meningitis?
1. Assessment Data (Subjective and Objective)
Subjective Data :
- Complaints of severe headache and neck stiffness
- Nausea and photophobia (sensitivity to light)
- Irritability, confusion, and sometimes drowsiness reported by the caregiver
Objective Data :
- Positive Kernig’s and Brudzinski’s signs
- High-grade fever (above 38.5°C)
- Vomiting and signs of increased intracranial pressure (e.g., altered consciousness)
- Seizures or involuntary movements
- CSF examination shows increased WBC count and protein, decreased glucose (in bacterial type)
2. Nursing Diagnoses (Problem List)
- Acute pain related to meningeal irritation and inflammation.
- Hyperthermia related to infectious process affecting central nervous system.
- Disturbed sensory perception related to CNS irritation and increased intracranial pressure.
- Risk for injury (seizures) related to cerebral irritation and fever.
- Deficient knowledge related to disease condition, treatment plan, and prognosis.
3. Goals and Expected Outcomes
- Patient will report a reduction in headache and pain.
- Patient will maintain normal body temperature within 24–48 hours.
- Patient will respond appropriately to verbal stimuli and remain oriented.
- Patient will not experience seizures or fall-related injuries during the care period.
- Patient/family will demonstrate understanding of illness, medication, and preventive measures.
4. Nursing Interventions and Rationales
1. Nursing Diagnosis : Acute Pain related to meningeal irritation and inflammation
Nursing Interventions:
- Assess the location, intensity, duration, and character of headache using appropriate pain assessment tools – It helps guide targeted pain management.
- Maintain the patient in a quiet, dimly lit, and calm environment – to reduce sensory stimulation which aggravates headache.
- Position the patient in semi-Fowler’s position with head midline – to promote venous drainage and reduce intracranial pressure (ICP).
- Apply cold compresses or cool cloth to the forehead – to provide soothing effect and vasoconstriction.
- Administer prescribed analgesics such as acetaminophen or NSAIDs – to relieve pain.
- Avoid sudden movements or jarring of the bed – to minimize pain caused by meningeal irritation.
- Encourage relaxation techniques such as deep breathing and guided imagery – to reduce perception of pain.
- Monitor for worsening signs of ICP (e.g., projectile vomiting, altered LOC) – as headache could signal complications.
2. Nursing Diagnosis : Hyperthermia related to infectious process
Nursing Interventions :
- Monitor body temperature every 2 to 4 hours – to detect fever spikes and assess effectiveness of antipyretics.
- Administer antipyretic medications (e.g., paracetamol, ibuprofen) as prescribed – to reduce fever and discomfort.
- Provide tepid sponge baths and encourage use of light clothing – to aid in evaporative cooling.
- Ensure adequate hydration orally or via IV – to prevent dehydration and assist thermoregulation.
- Encourage intake of cool, clear fluids like coconut water, fruit juice – to promote fluid balance.
- Monitor for signs of chills, rigors, and dehydration – to adjust care plan accordingly.
- Use cooling blankets or fans if temperature exceeds 39.5°C – under supervision.
- Educate family to avoid overbundling or covering the child during fever episodes.
3. Nursing Diagnosis : Disturbed Sensory Perception related to CNS irritation
Nursing Interventions :
- Assess level of consciousness regularly using Glasgow Coma Scale (GCS) – to detect any deterioration.
- Reduce environmental stimuli (lights, noise, loud talking) – to promote rest and reduce agitation.
- Orient the patient to person, place, and time frequently – to assist in maintaining cognitive functioning.
- Provide calm, simple explanations before procedures – to decrease anxiety and confusion.
- Use bed alarms or call bells to prevent wandering or falls in confused patients.
- Ensure eye care and lip moisturization if the patient is unresponsive – to prevent dryness and injury.
- Encourage family members to talk to the patient in familiar tone – to provide reassurance and orientation.
- Evaluate for visual/auditory disturbances, photophobia, hallucinations – and report promptly.
4. Nursing Diagnosis : Risk for Injury related to seizures or increased intracranial pressure
Nursing Interventions :
- Keep bed in lowest position, use padded side rails, and maintain seizure precautions – to prevent falls.
- Ensure suction equipment and oxygen are at bedside – to maintain airway during a seizure.
- Monitor for aura, pupil changes, or involuntary movements – which may precede seizures.
- Administer anticonvulsants as prescribed (e.g., phenytoin, levetiracetam) – to prevent or control seizures.
- Do not insert any object into the mouth during seizure activity – to prevent oral trauma.
- After seizure, turn the patient to side-lying position – to prevent aspiration.
- Document duration, type, and recovery phase of seizures – to assist physician evaluation.
- Maintain a calm and reassuring environment post-seizure – to support patient’s emotional recovery.
5. Nursing Diagnosis : Deficient Knowledge related to disease condition, treatment, and prevention
Nursing Interventions :
- Assess patient’s and family’s current knowledge and misconceptions – to plan teaching accordingly.
- Explain the nature of meningitis, its cause, mode of transmission, and treatment in simple language – to increase awareness.
- Educate on the importance of completing full course of antibiotics or antivirals – to ensure recovery.
- Provide written and verbal information about follow-up visits, signs of recurrence, and medication adherence.
- Encourage vaccination against meningitis pathogens (Hib, meningococcal, pneumococcal) – to prevent future episodes.
- Instruct caregivers on hygiene measures (handwashing, not sharing utensils) – to avoid spread.
- Encourage fluid and nutritional intake, adequate rest, and hygiene at home – to promote recovery.
- Reinforce the importance of neurological follow-up, especially in children – to detect long-term complications early.
5. Evaluation
- Patient reported reduced pain and headache after interventions.
- Body temperature returned to normal within 48 hours of treatment.
- Patient remained oriented and responsive.
- No seizure activity or fall occurred during the hospital stay.
- Patient and caregiver verbalized understanding of disease and treatment plan.
OR
a. Define Leukemia
Leukemia is a malignant cancer of the blood-forming tissues, primarily affecting the bone marrow and lymphatic system, characterized by the uncontrolled and excessive production of abnormal white blood cells (leukocytes) which interfere with the normal function of blood cells.
b. Explain the Etiology and clinical features of leukemia
Etiology of Leukemia (Causes of Leukemia)
Leukemia has multifactorial causes, including genetic, environmental, and immunological factors:
1. Genetic Factors
- It is associated with chromosomal abnormalities like Philadelphia chromosome (t(9;22)) seen in chronic myeloid leukemia (CML).
- Family history of leukemia increases the risk.
- Genetic disorders such as Down syndrome, Fanconi anemia, and Bloom syndrome may predispose to leukemia.
2. Radiation Exposure
- Exposure to high-dose ionizing radiation, such as from atomic bomb or radiotherapy, increases leukemia risk.
- Radiation during prenatal or early childhood period is particularly dangerous.
3. Chemical Exposure
- Benzene (used in chemicals, paints, and fuels) is a known carcinogen.
- Chemotherapeutic agents, especially alkylating agents, may lead to secondary leukemia.
4. Viral Infections
- Some viral infections, especially Human T-cell leukemia virus type 1 (HTLV-1), are linked to adult T-cell leukemia.
5. Weakened Immune System
- Individuals with immunodeficiency disorders or on long-term immunosuppressive therapy are at increased risk.
6. Smoking and Lifestyle Factors
- Cigarette smoking increases the risk of acute myeloid leukemia (AML).
- Poor diet, low immunity, and lack of antioxidants also contribute.
Clinical Features of Leukemia (Signs and Symptoms)
Symptoms of leukemia are related to bone marrow failure and organ infiltration by abnormal WBCs.
A. General Symptoms
- Fever with or without infection – due to low immunity.
- Fatigue and weakness – due to anemia.
- Loss of appetite and weight loss.
- Night sweats or excessive sweating.
B. Hematological Symptoms
- Anemia – pallor, shortness of breath, weakness.
- Increased bleeding or bruising – due to low platelet count (thrombocytopenia).
- Frequent nosebleeds, bleeding gums, or petechiae (tiny red spots on skin).
C. Infectious Symptoms
- Frequent or persistent infections – due to abnormal or low-functioning white blood cells.
- Sore throat, oral ulcers, and recurring respiratory infections.
D. Organ Infiltration Symptoms
- Bone and joint pain – due to marrow expansion.
- Enlarged lymph nodes (lymphadenopathy) – neck, armpit, groin.
- Hepatosplenomegaly – enlarged liver and spleen, leading to abdominal discomfort or fullness.
- Central nervous system symptoms (in acute leukemia) – headache, vomiting, blurred vision, seizures.
c. Draw a nursing care plan of a 5 year old child diagnosed with acute lymphocytic leukemia
1. Assessment Data (Subjective and Objective)
Subjective Data :
- Mother reports that the child is excessively tired and weak.
- Complains of body pain and loss of appetite.
- Parents state the child has frequent episodes of fever.
Objective Data :
- Pallor, bruising, and petechiae observed on skin.
- Weight loss noted.
- Fever of 38.8°C recorded.
- Blood test reports show decreased RBCs, WBCs, and platelets.
- Child appears lethargic and irritable.
2. Nursing Diagnoses (Problem List)
- Risk for infection related to immunosuppression due to leukemia and chemotherapy.
- Imbalanced nutrition: Less than body requirements related to decreased appetite, nausea, and vomiting.
- Fatigue related to decreased oxygen-carrying capacity and disease process.
- Risk for bleeding related to thrombocytopenia and bone marrow suppression.
- Anxiety (Child and Parent) related to hospitalization, unfamiliar environment, and diagnosis.
Goals and Expected Outcomes
- Child will remain free from infection as evidenced by normal temperature and absence of signs of sepsis.
- Child will consume adequate nutrition for age and weight.
- Child will verbalize feeling less tired and demonstrate improved activity tolerance.
- No signs of bleeding such as petechiae, epistaxis, or hematuria will be observed.
- Child and parents will express reduced anxiety and demonstrate coping strategies.
Nursing Interventions and Rationales
Diagnosis 1 : Risk for Infection
Interventions :
- Monitor child’s temperature every 4 hourly and note any spike – as it helps detect infections early, especially in neutropenic children.
- Strictly implement hand hygiene and aseptic techniques – it is essential in breaking the chain of infection.
- Institute neutropenic precautions (e.g., avoid live plants, fresh fruits, raw vegetables) – to protect from external pathogens.
- Inspect IV sites, oral cavity, and perineal area daily for infection signs – these are common portals of entry for microorganisms.
- Encourage fluid intake to maintain hydration – to support immune function and flush toxins.
- Administer prescribed prophylactic antibiotics, antifungals, or antivirals – to prevent opportunistic infections.
- Avoid contact with individuals who have respiratory or contagious illnesses – to minimize exposure.
- Ensure child’s toys and environment are sanitized daily – to maintain a clean environment for immune-compromised child.
Diagnosis 2 : Imbalanced Nutrition Less than Body Requirements
Interventions :
- Monitor daily weight, intake-output chart, and BMI percentile – to evaluate nutritional status and energy balance.
- Offer small, frequent, calorie-dense meals and snacks – it enhances tolerance and nutrient intake.
- Provide oral care before and after meals, especially if mucositis is present – to reduce pain and promote intake.
- Use distraction methods like storytelling or music during mealtime – to encourage eating in young children.
- Give antiemetics 30 minutes before meals as prescribed – to reduce nausea caused by chemotherapy.
- Assess for signs of oral ulcers or thrush – which can interfere with oral intake.
- Consult a pediatric dietician to individualize the child’s meal plan – ensuring balance and palatability.
- Involve parents in meal preparation if allowed – as familiar food may increase acceptance.
Diagnosis 3 : Fatigue
Interventions :
- Assess fatigue levels using age-appropriate fatigue scales – to quantify and document progression.
- Encourage rest periods between activities and procedures – to avoid exhaustion.
- Promote uninterrupted nighttime sleep – essential for tissue recovery and immune support.
- Provide favorite quiet activities (coloring, puzzles, books) – to keep child engaged without exhausting energy.
- Encourage family involvement in recreational care – to support emotional energy and bonding.
- Cluster nursing care to minimize unnecessary movement – and reduce physiological stress.
- Monitor hemoglobin and hematocrit levels – as anemia contributes directly to fatigue.
Diagnosis 4 : Risk for Bleeding
Interventions :
- Monitor skin, gums, stool, and urine for any bleeding or bruising – to detect early signs of internal or external bleeding.
- Avoid intramuscular injections and rectal temperatures – as these can induce trauma and bleeding.
- Apply gentle pressure after venipuncture or injection – to prevent hematoma formation.
- Use soft-bristled toothbrush and avoid flossing – to reduce gum trauma.
- Provide a safe play environment (no sharp toys, padded corners) – to prevent accidental injury.
- Monitor platelet counts and report if <50,000/mm³ – to initiate preventive action.
- Teach caregivers to identify and report signs of bleeding at home – like epistaxis or black stools.
- Administer platelet transfusion as prescribed during severe thrombocytopenia – to restore hemostasis.
Diagnosis 5 : Anxiety (Child and Parents)
Interventions :
- Assess child and parental anxiety level using verbal and non-verbal cues – to plan tailored emotional support.
- Encourage expression of fears, questions, and concerns – to validate feelings and reduce emotional load.
- Use therapeutic play (dolls, drawing) to help child express emotions – which is vital in pediatric coping.
- Explain procedures step-by-step in child-friendly language – to prepare the child and avoid fear of the unknown.
- Involve parents in care and decisions – to give them a sense of control and participation.
- Provide continuity of nursing staff as much as possible – to build rapport and familiarity.
- Encourage presence of favorite items (toys, blankets) with the child – to reduce fear and promote comfort.
- Refer to counselor or child-life specialist if anxiety persists – to provide professional psychological support.
Evaluation
- Child maintained normal temperature and had no signs of infection.
- Nutritional intake improved; child gained 0.5 kg during stay.
- Episodes of fatigue decreased with improved rest pattern.
- No new bruising or bleeding noted.
- Parents verbalized understanding of treatment and appeared less anxious.
Q-5. Short Essay Question: (Any Three)3×5-15
a. Tracheoesophageal fistula
Tracheoesophageal Fistula (TEF) is a congenital abnormal connection between the trachea and the esophagus, leading to the passage of food or fluids into the respiratory tract and resulting in serious respiratory complications if untreated.
Causes of TEF
- Congenital Malformation during 4th–6th week of embryonic life.
- Associated with VACTERL anomalies.
- Chromosomal disorders like Trisomy 13, 18, and 21 (Down Syndrome).
- Maternal polyhydramnios during pregnancy.
- Exposure to teratogenic drugs or environmental toxins.
- Rarely, acquired causes like trauma, foreign body ingestion, or prolonged intubation.
Types of Tracheoesophageal Fistula (TEF)
✅ 1. Type C (Most Common Type) – EA with Distal TEF
- The upper esophagus ends in a blind pouch (atresia), and the lower esophagus connects to the trachea.
- It occurs in about 85% of cases.
- Clinical Features: Excessive drooling, coughing, choking during feeds, and abdominal distension due to air in the stomach.
✅ 2. Type A – Isolated Esophageal Atresia (No TEF)
- The esophagus is interrupted with no connection to the trachea.
- Accounts for about 8% of cases.
- Clinical Features: Drooling of saliva, inability to pass a feeding tube, no gas in the abdomen.
✅ 3. Type E (H-Type Fistula) – TEF without Esophageal Atresia
- There is a direct fistula between the trachea and esophagus, but the esophagus is continuous.
- Accounts for about 4% of cases.
- Clinical Features: Recurrent pneumonia, coughing during feeding, but normal swallowing.
- Difficult to diagnose early because symptoms may be subtle.
✅ 4. Type B – EA with Proximal TEF (Rare)
- The upper esophagus connects to the trachea; the lower esophagus ends in a blind pouch.
- Extremely rare (about 1% of cases).
- Clinical Features: Choking and aspiration immediately after birth; abdomen remains flat due to no gas entry.
✅ 5. Type D – EA with Both Proximal and Distal TEF (Very Rare)
- Both ends of the esophagus are connected to the trachea via fistulas.
- Accounts for less than 1% of cases.
- Clinical Features: Severe respiratory distress, recurrent aspiration, and early onset of symptoms after birth.
Clinical Manifestations
- Excessive frothy saliva and drooling immediately after birth.
- Coughing and choking during feeding episodes.
- Cyanosis (bluish discoloration), especially while feeding or crying.
- Respiratory distress and noisy breathing due to aspiration.
- Recurrent aspiration pneumonia from swallowed milk or secretions entering the lungs.
- Abdominal distension due to air entering the stomach through the fistula.
- Inability to pass a nasogastric tube into the stomach (diagnostic clue).
Diagnostic Evaluation
- History collection
- Physical examination
- NG tube test
- X-ray
- Contrast study
- Echocardiography
- Ultrasound
Management
✅ 1. Immediate Preoperative Management
Prevent Aspiration :
- Keep the baby nil per oral (NPO) (no oral feeds).
- Insert a Replogle tube (double-lumen tube) into the upper esophageal pouch to continuously suction secretions and prevent aspiration.
- Keep the infant in a semi-upright (head elevated) position to minimize reflux of secretions into the airway.
Maintain Airway and Oxygenation :
- Administer humidified oxygen if signs of respiratory distress are present.
- Monitor oxygen saturation (SpO₂) and provide ventilatory support if needed.
Hydration and Electrolyte Balance :
- Initiate intravenous fluids (IVF) to maintain hydration and correct electrolyte imbalances.
Antibiotic Therapy :
- Start broad-spectrum antibiotics to prevent or treat aspiration pneumonia.
✅ 2. Surgical Management (Definitive Treatment)
Timing of Surgery :
- Surgery is typically performed as soon as the infant is stabilized.
- In stable cases, immediate surgery is planned; in critically ill infants, surgery may be delayed after initial stabilization.
Surgical Procedure :
- Ligation of the fistula to close the abnormal connection between the trachea and esophagus.
- Primary anastomosis to reconnect the two ends of the esophagus if possible.
- In cases with long-gap atresia, staged repair or esophageal replacement procedures may be necessary.
✅ 3. Postoperative Management
Airway and Breathing :
- Closely monitor for respiratory distress and ensure airway patency.
- Provide oxygen support or mechanical ventilation if required.
Feeding Management :
- Start gastrostomy feeding if oral feeding is not possible initially.
- Gradually introduce oral feeds after confirming the integrity of esophageal repair (contrast study may be done before initiating oral feeds).
Monitor for Complications :
- Watch for signs of anastomotic leak, strictures, tracheomalacia, or recurrent fistula.
- Assess for signs of infection or sepsis.
Parental Counseling :
- Educate parents regarding postoperative care, feeding techniques, and recognizing complications.
- Explain the importance of follow-up visits for long-term monitoring.
b. ASD
Definition of ASD
- Atrial Septal Defect (ASD) is a congenital heart defect in which there is an abnormal opening in the atrial septum, i.e., the wall (septum) that separates the right and left atria of the heart.
- It allows oxygen-rich blood from the left atrium to mix with oxygen-poor blood in the right atrium, resulting in left-to-right shunting.
- It is one of the most common congenital heart defects, and may be asymptomatic in childhood.
Types of Atrial Septal Defect (ASD)
1. Ostium Secundum (Most common type)
- It is located at the fossa ovalis in the center of the atrial septum.
- This type accounts for about 70% of ASDs.
- It is often isolated and commonly seen in both children and adults.
2. Ostium Primum
- It is a low-positioned defect located near the atrioventricular (AV) valves.
- Often associated with endocardial cushion defects, and seen in Down syndrome.
- May involve mitral valve abnormalities (e.g., cleft mitral valve).
3. Sinus Venosus ASD
- Located near the entry of the superior or inferior vena cava into the right atrium.
- Often associated with anomalous pulmonary venous return (abnormal drainage of pulmonary veins into right atrium).
4. Coronary Sinus ASD (Rare)
- Involves unroofing of the coronary sinus, allowing communication between the left atrium and coronary sinus.
- Often associated with persistent left superior vena cava.
Etiology / Causes of ASD
- Genetic mutations (e.g., Down syndrome, Ellis-van Creveld syndrome)
- Maternal factors during pregnancy (e.g., alcohol consumption, rubella infection, diabetes)
- Familial congenital heart diseases
- Chromosomal abnormalities (e.g., Trisomy 21, 18)
Pathophysiology of ASD
- Blood flows from left atrium (high pressure) to right atrium (low pressure) due to the defect.
- This causes volume overload in the right atrium, right ventricle, and pulmonary circulation.
- Over time, this leads to right heart enlargement, pulmonary hypertension, and possible right-sided heart failure.
- In long-standing cases, Eisenmenger’s syndrome may occur, reversing the shunt (right-to-left).
Clinical Manifestations ASD
- May be asymptomatic in early life.
- Fatigue and exercise intolerance
- Shortness of breath (dyspnea) on exertion
- Frequent respiratory infections in children
- Heart murmur (soft systolic murmur due to increased flow across pulmonary valve)
- Palpitations or arrhythmias in older children or adults
- Cyanosis (in severe or reversed shunt cases)
- Failure to thrive in infants (if associated with other heart defects)
Diagnostic Evaluation
- Echocardiography (2D/Color Doppler) – primary tool to visualize the septal defect.
- Electrocardiogram (ECG) – may show right axis deviation, right atrial enlargement.
- Chest X-ray – shows cardiomegaly and increased pulmonary vascular markings.
- Cardiac catheterization – for measuring pressures and confirming diagnosis.
- MRI/CT scan – may be used in complex cases or before surgical planning.
Management of ASD
Medical Management :
- Observation in small, asymptomatic ASDs (especially <5 mm in infants).
- Diuretics for managing symptoms of volume overload.
- Antibiotics prophylaxis may be indicated before dental/surgical procedures in some patients.
- Antiarrhythmics if atrial arrhythmias present.
Surgical Management :
- Open heart surgery to close the defect with sutures or a patch (for large or complex ASDs).
- Indicated if significant left-to-right shunt or symptoms present.
Catheter-based (Device Closure) :
- Minimally invasive transcatheter closure using a septal occluder device (e.g., Amplatzer).
- Preferred for secundum ASDs with adequate septal rims.
Complications of Untreated ASD
- Right-sided heart failure
- Pulmonary hypertension
- Atrial arrhythmias (e.g., atrial fibrillation)
- Stroke (due to paradoxical embolism if shunt reverses)
- Eisenmenger’s syndrome (irreversible pulmonary hypertension with cyanosis)
- Reduced exercise capacity and growth retardation in children
Nursing Management of Atrial Septal Defect (ASD)
1. Assessment
Assess vital signs like heart rate, respiratory rate, oxygen saturation regularly.
Observe for signs of cyanosis, fatigue, poor feeding, and recurrent respiratory infections.
Monitor growth parameters to identify failure to thrive.
2. Maintain Oxygenation
- Provide humidified oxygen therapy as prescribed.
- Keep child in semi-Fowler’s position to ease breathing.
- Encourage breathing exercises or incentive spirometry in older children.
3. Nutrition and Fluids
- Offer small, frequent, high-calorie feeds to reduce fatigue.
- Monitor intake-output chart to prevent fluid overload.
- Administer diuretics if prescribed, and monitor electrolytes.
4. Medication Care
- Administer diuretics, digoxin, and antibiotics as prescribed.
- Monitor for drug side effects, especially for digoxin (bradycardia, vomiting).
- Ensure medication adherence and parental education.
5. Preoperative Care
- Prepare child and parents emotionally and physically for surgery.
- Keep child NPO before procedure, and monitor for anxiety.
- Complete required investigations (ECG, echo, labs).
6. Postoperative Care
- Monitor vitals, surgical site, and signs of complications (arrhythmias, bleeding).
- Provide pain relief, ensure rest, and early mobilization.
- Encourage gentle activity and lung expansion techniques post-surgery.
7. Infection Prevention
- Maintain aseptic techniques during all procedures.
- Educate parents about oral hygiene to prevent endocarditis.
- Ensure immunization schedule is followed.
8. Discharge Education
- Instruct parents to watch for symptoms like breathing difficulty, cyanosis, poor feeding.
- Emphasize importance of regular follow-up and medication adherence.
- Encourage normal growth and development with age-appropriate activities.
9. Emotional and Family Support
- Provide psychological reassurance to parents and allow involvement in care.
- Offer support group references if available
c. Sickle cell anemia
Definition
Sickle Cell Anemia is a genetic blood disorder characterized by the production of abnormal hemoglobin called Hemoglobin S (HbS). This abnormal hemoglobin causes red blood cells (RBCs) to become rigid, sticky, and crescent or sickle-shaped, which leads to blockages in small blood vessels, reduced oxygen delivery, and various complications. It is an autosomal recessive inherited disorder.
Causes of Sickle Cell Anemia
Genetic Mutation :
Caused by a mutation in the HBB gene on chromosome 11, leading to abnormal Hemoglobin S production.
Autosomal Recessive Inheritance :
Occurs when a person inherits two sickle cell genes, one from each parent.
Ethnic Predisposition :
Common in people of African, Middle Eastern, Indian, and Mediterranean origin, due to historical malaria prevalence.
Pathophysiology of Sickle Cell Anemia
Genetic Mutation :
Sickle cell anemia is caused by a mutation in the HBB gene, which leads to the production of abnormal Hemoglobin S (HbS) instead of normal Hemoglobin A.
Sickling of Red Blood Cells :
Under low oxygen conditions, HbS polymerizes and forms stiff rods inside red blood cells (RBCs), causing them to become rigid and sickle-shaped.
Reduced Oxygen Carrying and Blockage :
These sickle-shaped RBCs cannot pass smoothly through small blood vessels, leading to vascular blockages (vaso-occlusion) and decreased oxygen delivery to tissues.
Hemolysis (Breakdown of RBCs) :
Sickle cells are fragile and have a shorter lifespan (10–20 days instead of 120 days), leading to chronic anemia due to the continuous breakdown of RBCs.
Tissue Hypoxia and Organ Damage :
Blockage of blood flow and reduced oxygen supply lead to pain crises, ischemia, and long-term damage to organs such as the spleen, kidneys, heart, and brain.
Increased Risk of Infections :
Due to repeated damage and functional loss of the spleen (autosplenectomy), patients have a weakened immune system and are prone to frequent infections.
Clinical feature
- Fatigue and Weakness due to anemia.
- Pain Crises (sudden severe pain in bones, joints, chest).
- Swelling of Hands and Feet (Dactylitis).
- Jaundice (yellowish skin and eyes).
- Frequent Infections due to spleen dysfunction.
- Delayed Growth and Puberty in children.
- Vision Problems (retinopathy).
- Serious Complications like stroke and acute chest syndrome.
Diagnostic evaluation
- History collection
- Physical examination
- CBC
- Peripheral Blood Smear
- Hemoglobin Electrophoresis
- Sickling Test
- HPLC Test
- Newborn Screening
- Genetic Testing
Management
📌 1. Preventive Management :
- Hydration : Ensure the patient drinks plenty of fluids to keep blood diluted and reduce the risk of sickling crises.
- Avoidance of Triggers : Advise avoiding exposure to cold temperatures, high altitudes, stress, and strenuous physical activity.
- Infection Prevention : Administer routine vaccinations (Pneumococcal, Meningococcal, and Influenza vaccines). Provide prophylactic antibiotics like Penicillin, especially in children under 5 years, to prevent infections.
📌 2. Pharmacological Management :
Hydroxyurea :
- Increases the production of fetal hemoglobin (HbF), which reduces the frequency of sickling and painful crises.
- Also helps decrease the need for blood transfusions.
Folic Acid Supplementation :
- Supports red blood cell production to counter chronic anemia.
Pain Management :
- Mild pain : Use NSAIDs like Ibuprofen.
- Severe pain : Administer opioids like Morphine during vaso-occlusive crises.
Antibiotics :
- Start early treatment of any infections as these can trigger sickling crises.
📌 3. Blood Transfusion Therapy :
- Used in cases of severe anemia, stroke prevention, acute chest syndrome, or prior to surgery.
- Exchange transfusions may be performed in severe or life-threatening situations to quickly reduce the number of sickled cells.
📌 4. Advanced Treatment Options :
Bone Marrow or Stem Cell Transplantation :
- Currently the only potential curative treatment, mainly for young patients with severe disease and matched donors.
Gene Therapy (Emerging Treatment) :
- Research is ongoing to correct the genetic defect responsible for sickle cell anemia.
📌 5. Supportive and Nursing Care :
- Monitor for Complications : Watch for signs of stroke, acute chest syndrome, severe anemia, and infections.
- Nutritional Support : Provide a diet rich in iron, folic acid, and high-protein foods to support red blood cell production.
- Psychosocial Support : Offer counseling to help the patient and family cope with the chronic nature of the disease.
- Patient and Family Education : Teach about recognizing early signs of a sickling crisis and the importance of medication adherence, hydration, and regular follow-up care.
Nursing Management
Pain Management
- Administer prescribed analgesics, such as NSAIDs or opioids (e.g., morphine), especially during a sickle cell crisis.
- Use non-pharmacological methods like warm compresses and distraction techniques.
- Encourage bed rest during painful episodes.
Hydration Therapy
- Provide adequate oral and IV fluids to reduce blood viscosity and promote circulation.
- Monitor intake and output and ensure the patient is not dehydrated.
Oxygen Administration
- Administer humidified oxygen in cases of breathlessness or low oxygen saturation.
- Monitor SpO₂ (oxygen saturation) regularly.
Infection Prevention
- Follow strict hand hygiene and maintain a clean environment.
- Administer routine vaccinations and prophylactic antibiotics if ordered.
- Monitor for early signs of infection, such as fever or respiratory symptoms.
Nutritional Support
- Provide a high-protein, high-calorie diet with folic acid supplementation to support red blood cell production.
- Encourage iron-rich foods only if iron deficiency exists, as excess iron may be harmful.
Psychosocial Support and Education
- Offer emotional support and allow expression of feelings.
- Educate the patient and caregivers about trigger avoidance (cold exposure, dehydration, high altitudes, infections).
- Teach about importance of regular follow-ups, hydration, and medication adherence.
d. Types of Club Foot
Club foot is classified into four main types based on foot posture and cause. Each type is described in detail below:
A. Talipes Equinovarus (TEV) :
- It is the most common type of club foot and is often referred to simply as “clubfoot”.
- In this condition, the foot is pointed downward (equinus) and turned inward (varus).
- It is a congenital condition, meaning it is present at birth.
- It affects bones, tendons, and muscles, leading to a rigid and twisted foot shape.
It is characterized by :
- Inversion of the heel.
- Plantar flexion of the ankle (equinus).
- Adduction and inversion of the forefoot.
- Medial rotation of the entire foot.
B. Talipes Calcaneovalgus
- In this type, the foot is dorsiflexed (upward) and everted (outward).
- The heel is down (calcaneo) and the forefoot is bent upward and outward (valgus).
- It is usually caused by intrauterine crowding and is often flexible and self-limiting.
- This is commonly observed in newborns but typically improves without surgery.
It is characterized by :
- Dorsiflexion of the ankle.
- Eversion and abduction of the foot.
- Flattened foot arch.
- Often associated with breech presentation.
C. Talipes Calcaneovarus
- In this condition, the foot is dorsiflexed (upward) and turned inward (varus).
- The heel is down (calcaneo) and the forefoot turns toward the midline.
- It is rare and can be associated with neurological disorders like cerebral palsy.
It is characterized by :
- Dorsiflexed ankle joint.
- Inverted and adducted forefoot.
- Commonly results in difficulty wearing shoes.
D. Talipes Equinovalgus :
- In this condition, the foot is plantarflexed (downward) and everted (outward).
- The heel is lifted (equinus) and the forefoot is turned outward (valgus).
- It is a rare deformity and can be acquired due to neuromuscular diseases.
It is characterized by :
- Plantar flexion of the ankle.
- Outward deviation of the heel.
- Often associated with muscle weakness or imbalance.
Additional Classifications of Club Foot
These classifications are based on cause, rigidity, and associated conditions, which help guide the treatment approach.
A. Congenital Club Foot (Idiopathic Club Foot)
- It is the most commonly observed form of club foot and it is present at birth without any known external cause.
- It is typically bilateral in about 50% of cases, and more common in male children than females.
- It is called idiopathic because no neuromuscular or syndromic cause is identified in the majority of cases.
- The deformity is often rigid and structural, meaning bones, muscles, tendons, and ligaments are abnormally developed.
- It requires early orthopedic intervention, usually with Ponseti casting technique, followed by bracing.
B. Positional Club Foot (Flexible or Postural Club Foot)
- It occurs due to intrauterine crowding or poor fetal positioning, especially in twin or breech pregnancies.
- The structure of the foot is normal, but the position is temporarily distorted.
- The deformity is flexible and can be corrected with gentle stretching, exercises, and physiotherapy.
- It is not associated with any bony abnormality or congenital malformation.
- Usually resolves spontaneously or with non-surgical conservative management.
C. Teratologic Club Foot (Syndromic Club Foot)
- This type is associated with neuromuscular disorders or genetic syndromes, such as:
- Arthrogryposis multiplex congenita
- Spina bifida
- Myelomeningocele
- Larsen syndrome
- It is usually severe and rigid, making it difficult to correct with conservative measures alone.
- It often requires extensive surgical correction in addition to casting and therapy.
- Prognosis depends on the severity of the underlying syndrome and may involve long-term disability.
- Early multidisciplinary care is essential including orthopedics, neurology, and physiotherapy.
D. Acquired Club Foot
- It is not present at birth, but develops later in life due to secondary causes such as :
- Poliomyelitis
- Cerebral palsy
- Trauma or burns
- Infections like tuberculosis or osteomyelitis
- The deformity is often asymmetric and can be progressive.
- It involves muscle imbalance, joint contractures, and sometimes joint destruction.
- Treatment may require orthotic support, surgery, or corrective splints, depending on cause and severity.
- Nursing care includes mobility support, physiotherapy, and skin care especially for affected children.
E. Recurrent Club Foot
- This occurs when a previously treated club foot returns or relapses, especially if bracing is not continued as advised.
- The most common cause of recurrence is non-compliance with orthotic bracing (foot abduction brace) after casting.
- It may present as mild deformity or return to original rigid shape.
- Management includes repeat serial casting, and in severe cases, minor surgical corrections.
- Nurses must emphasize parental education and follow-up care to prevent relapse.
F. Atypical Club Foot
- This is a rare form where the midfoot is severely abducted and foot has a bean-shaped appearance.
- It may occur due to incorrect casting techniques or underlying genetic disorders.
- The deformity is more rigid than typical idiopathic clubfoot.
- Requires modified Ponseti technique or surgery for correction.
- Early diagnosis and proper orthopedic referral are crucial to avoid long-term disability.
e. ADHD
Definition
Attention Deficit Hyperactivity Disorder (ADHD) is a neurodevelopmental disorder characterized by a persistent pattern of inattention, hyperactivity, and impulsivity, which is inconsistent with the child’s developmental level. These symptoms interfere with academic, social, and emotional functioning and are usually noticed before the age of 12 years.
Causes and Risk Factors
Genetic Factors : Strong familial tendency; first-degree relatives often affected.
Neurobiological Factors : Abnormalities in brain structure and function, especially in areas regulating attention and impulse control (prefrontal cortex).
Environmental Factors : Prenatal exposure to alcohol, tobacco, or drugs; low birth weight; lead exposure.
Psychosocial Factors : Chaotic family environment, poor parenting, or neglect may aggravate symptoms.
Types of ADHD
📌 1. Predominantly Inattentive Type (ADHD-PI) :
This type is mainly characterized by the child’s inability to maintain attention and focus, leading to frequent daydreaming, forgetfulness, difficulty following instructions, and losing necessary items, while hyperactive behaviors are usually not present.
📌 2. Predominantly Hyperactive-Impulsive Type (ADHD-PHI) :
In this type, the child shows excessive physical activity, constant fidgeting, inability to stay seated, and impulsive behaviors like interrupting conversations or acting without thinking, while problems with inattention are minimal.
📌 3. Combined Type (Most Common) :
This is the most common form where the child exhibits both inattention and hyperactive-impulsive behaviors, resulting in difficulties with focusing, staying still, controlling impulses, and completing tasks effectively.
Clinical Features:
1. Inattention Symptoms
- Difficulty sustaining attention during tasks or play.
- Often does not seem to listen when spoken to directly.
- Easily distracted by irrelevant stimuli.
- Frequently loses things necessary for activities (toys, books, pencils).
- Avoids tasks requiring prolonged mental effort.
2. Hyperactivity Symptoms
- Constantly fidgeting or squirming in seat.
- Runs or climbs excessively in inappropriate situations.
- Talks excessively and finds it difficult to engage quietly in activities.
3. Impulsivity Symptoms
- Blurts out answers before questions are completed.
- Has difficulty waiting for their turn.
- Frequently interrupts conversations or games.
Management of ADHD
Behavioral Therapy :
- Parent training and behavior modification programs.
- Use of positive reinforcement, structured routines, and reward systems.
- Social skills training to improve peer interactions.
Educational Interventions :
- Classroom modifications such as seating arrangements away from distractions, frequent breaks, and simplified instructions.
- Use of individualized education programs (IEPs) when needed.
Pharmacological Treatment :
Stimulant Medications :
- Methylphenidate (Ritalin) and Amphetamines are most effective in improving focus and reducing hyperactivity.
Non-Stimulant Medications :
- Atomoxetine (Strattera) – useful when stimulants are contraindicated.
- Clonidine and Guanfacine may help control hyperactivity and impulsivity.
Psychological Support :
- Cognitive Behavioral Therapy (CBT) to improve self-control and problem-solving skills.
- Family counseling and support groups.
Nursing management
✅ 1. Behavioral Management :
- Establish a structured and consistent daily routine.
- Use clear and simple instructions for tasks.
- Apply positive reinforcement and reward systems for appropriate behavior (sticker charts, small rewards).
- Implement time-out strategies to manage impulsive or aggressive behavior.
✅ 2. Educational Support :
- Collaborate with teachers to provide an Individualized Education Plan (IEP) if needed.
- Minimize distractions in the learning environment.
- Encourage the use of visual aids and task breakdown into small steps.
- Provide frequent breaks during tasks to prevent frustration.
✅ 3. Medication Management :
- Administer prescribed medications such as Methylphenidate or Atomoxetine as per the doctor’s order.
- Monitor for side effects like insomnia, decreased appetite, or increased irritability.
- Educate parents and caregivers about proper medication timing and adherence.
✅ 4. Safety Promotion :
- Supervise during high-risk activities to prevent injuries.
- Ensure the home and school environments are free from hazardous objects.
- Teach the child about safety rules in a simple and repetitive manner.
✅ 5. Social and Emotional Support :
- Encourage participation in group activities and structured play to enhance social skills.
- Provide emotional support to improve self-confidence and reduce frustration.
- Help the child develop coping skills to manage impulses and anger.
✅ 6. Family Education and Counseling :
- Educate parents about ADHD, its management, and the importance of consistent discipline techniques.
- Encourage parents to attend behavioral therapy programs.
- Provide resources for support groups and community services.
Q-6. Short Answer Question: (Any Four) 4×2=8
a. Defect in Tetralogy of fallot
Tetralogy of Fallot is a congenital heart defect characterized by the presence of four structural abnormalities in the heart:
Ventricular Septal Defect (VSD) :
A hole between the right and left ventricles allowing mixing of oxygenated and deoxygenated blood.
Pulmonary Stenosis :
Narrowing of the pulmonary valve or artery, reducing blood flow to the lungs.
Overriding of Aorta :
The aorta is displaced over the VSD, receiving blood from both ventricles.
Right Ventricular Hypertrophy :
Thickening of the right ventricular wall due to increased workload.
b. Tics
Tics are sudden, rapid, repetitive, and involuntary movements or vocal sounds that occur repeatedly and are often difficult to control. They can involve motor tics (such as eye blinking, head jerking) or vocal tics (such as throat clearing, grunting, or repeating words). Tics are commonly seen in conditions like Tourette’s syndrome and may increase with stress or anxiety but often decrease during focused activities.
c. Types of Spina Bifida
Spina Bifida Occulta :
- Mildest form; hidden defect in vertebrae.
- No protrusion of spinal cord or meninges.
- Usually asymptomatic; may have a skin dimple or hair tuft.
Meningocele :
- Meninges protrude through the spinal defect forming a fluid-filled sac.
- Spinal cord remains in place.
- Minimal neurological issues; surgical correction required.
Myelomeningocele (Meningomyelocele) :
- Most severe form; meninges and spinal cord protrude through the defect.
- Causes paralysis, bladder/bowel incontinence, and hydrocephalus.
- Requires immediate surgery and long-term care.
d. Hypospadias
Hypospadias is a congenital abnormality of the male urethra in which the urethral opening is located on the underside (ventral surface) of the penis, rather than at the tip of the glans penis. This condition can vary in severity, with the opening located anywhere from just below the glans to the perineum, and is often associated with a downward curvature of the penis (chordee).
e. Four Specific Symptoms of Nephrotic Syndrome
Generalized Edema (Swelling) :
Painless, soft, and pitting edema, starting from the face (periorbital edema), progressing to the abdomen (ascites), legs, and whole body (anasarca).
Proteinuria :
Excessive loss of protein in urine, usually greater than 3.5 grams per day, leading to frothy or foamy urine.
Hypoalbuminemia :
Low levels of serum albumin (< 2.5 g/dL) due to protein loss in urine, contributing to edema formation.
Hyperlipidemia :
Elevated blood cholesterol and triglyceride levels as the liver tries to compensate for protein loss by producing more lipoproteins.