25/07/2018 Child health nursing (done)-UPLOAD NO.3
25/07/2018-Child health nursing-UPLOAD NO.3
Section A-38
Q-1 Long answer question (any one) 2+5+8=15
a) Define congenital heart disease.
Congenital Heart Disease (CHD) refers to structural or functional abnormalities of the heart and great vessels that are present at birth due to improper development of the heart during fetal life. These defects may affect the walls of the heart, valves, or the blood vessels near the heart.
b) Explain classification of congenital heart disease
Acyanotic Congenital Heart Diseases
These defects do not cause cyanosis, as oxygenated blood is still delivered to the body, although there is abnormal blood flow within the heart.
They usually involve left-to-right shunts or obstructive lesions.
A. Left-to-Right Shunt Lesions
Blood flows abnormally from the left (oxygenated) side of the heart to the right (deoxygenated) side, leading to increased pulmonary blood flow.
Examples:
Atrial Septal Defect (ASD) :
Atrial Septal Defect (ASD) is a congenital heart defect characterized by an abnormal opening in the interatrial septum, allowing oxygen-rich blood from the left atrium to flow into the right atrium, leading to right heart overload and increased pulmonary blood flow.
Ventricular Septal Defect (VSD) :
Ventricular Septal Defect (VSD) is a congenital heart defect where there is an abnormal opening in the interventricular septum, allowing oxygenated blood from the left ventricle to flow into the right ventricle.
Patent Ductus Arteriosus (PDA) :
Patent Ductus Arteriosus (PDA) is a congenital heart defect in which the ductus arteriosus, a fetal blood vessel connecting the pulmonary artery to the aorta, fails to close after birth, resulting in left-to-right shunting of blood.
Atrioventricular Septal Defect (AVSD) :
Atrioventricular Septal Defect (AVSD) is a congenital heart defect characterized by a combination of atrial septal defect (ASD), ventricular septal defect (VSD), and abnormal formation of the atrioventricular (AV) valves, resulting in a common AV valve and a large central heart defect
B. Obstructive Acyanotic Lesions
These involve narrowing of valves or vessels, causing obstruction of blood flow without cyanosis.
Examples :
Pulmonary Stenosis :
Pulmonary Stenosis is a congenital or acquired narrowing of the pulmonary valve or right ventricular outflow tract, which obstructs blood flow from the right ventricle to the pulmonary artery.
Aortic Stenosis :
Aortic Stenosis is a narrowing of the aortic valve opening, which obstructs blood flow from the left ventricle to the aorta, causing increased pressure in the left ventricle and decreased cardiac output.
Coarctation of Aorta :
Coarctation of the Aorta is a congenital narrowing of a segment of the aorta, typically just distal to the origin of the left subclavian artery, near the ductus arteriosus.
Cyanotic Congenital Heart Diseases
These defects result in cyanosis due to the mixing of oxygen-poor blood with oxygen-rich blood through a right-to-left shunt. As a result, deoxygenated blood enters systemic circulation, causing the skin and mucous membranes to appear bluish. It includes
Tetralogy of Fallot (TOF) :
Tetralogy of Fallot is a cyanotic congenital heart defect that consists of four anatomical abnormalities : Ventricular Septal Defect (VSD), Pulmonary Stenosis, Overriding Aorta, Right Ventricular Hypertrophy. It leads to mixing of oxygenated and deoxygenated blood, causing cyanosis in affected infants.
Transposition of the Great Arteries (TGA) :
Transposition of the Great Arteries (TGA) is a cyanotic congenital heart defect in which the aorta arises from the right ventricle and the pulmonary artery arises from the left ventricle, causing parallel circulation and severe oxygen deprivation.
Tricuspid Atresia :
Tricuspid Atresia is a cyanotic congenital heart defect in which the tricuspid valve is absent or abnormally developed, preventing blood flow from the right atrium to the right ventricle. This leads to underdevelopment (hypoplasia) of the right ventricle and mixing of oxygenated and deoxygenated blood.
Total Anomalous Pulmonary Venous Connection (TAPVC) :
TAPVC is a cyanotic congenital heart defect in which all four pulmonary veins fail to connect to the left atrium and instead connect abnormally to the right atrium or to systemic veins. This causes mixing of oxygenated and deoxygenated blood, leading to cyanosis and heart failure.
Truncus Arteriosus :
Truncus Arteriosus is a rare cyanotic congenital heart defect in which a single large artery (truncus) arises from the heart and gives rise to both the systemic and pulmonary circulation, instead of having separate aorta and pulmonary artery. It is always associated with a ventricular septal defect (VSD).
Pulmonary Atresia :
Pulmonary Atresia is a cyanotic congenital heart defect where the pulmonary valve that allows blood to flow from the right ventricle to the pulmonary artery is absent or closed, preventing blood from reaching the lungs to get oxygenated.
c) Discuss nursing care of child with ventricular septal defect in detail with nursing process
Ineffective Breathing Pattern related to pulmonary congestion, increased pulmonary blood flow as evidenced by tachypnea, dyspnea, low SpO₂
Nursing Interventions :
- Assess and record respiratory rate, rhythm, depth every 2–4 hours.
- Monitor oxygen saturation continuously or frequently.
- Place the child in a semi-Fowler’s or high Fowler’s position to reduce pressure on the lungs.
- Administer humidified oxygen as per order to improve oxygenation.
- Perform gentle chest physiotherapy if secretions are present.
- Monitor for signs of respiratory fatigue: grunting, head bobbing, cyanosis.
- Avoid overcrowded areas to reduce risk of respiratory infections.
- Keep emergency airway equipment ready if breathing worsens.
Imbalanced Nutrition Less Than Body Requirements Related to fatigue during feeding, increased metabolic demand As Evidenced by poor weight gain, irritability during feeding, weak suck reflex
Nursing Interventions
- Assess the child’s feeding behavior and tolerance to oral feeding.
- Provide high-calorie, nutrient-dense feeds (e.g., fortified formula, expressed breast milk).
- Feed in a semi-upright position to reduce aspiration risk.
- Offer frequent, small-volume feeds to prevent exhaustion.
- Use soft nipples or special feeding bottles to ease sucking.
- Consider nasogastric (NG) feeding if oral intake is insufficient.
- Monitor daily weight, intake-output, and signs of dehydration.
- Consult a pediatric dietitian for nutritional planning.
Activity Intolerance Related to decreased cardiac output and fatigue as Evidenced by irritability, dyspnea on exertion, inability to complete feeds or play
Nursing Interventions :
- Schedule rest periods between feeds and care activities.
- Limit physical stimulation and cluster nursing care to allow for uninterrupted rest.
- Support calm, quiet play and discourage overexertion.
- Monitor for tachycardia, sweating, and pallor after minimal activity.
- Encourage passive exercises to maintain circulation and tone in bed-bound infants.
- Educate parents on signs of overexertion and importance of rest.
Risk for Infection Related to increased susceptibility due to heart defect and hospital exposure
Nursing Interventions :
- Maintain strict hand hygiene before and after contact.
- Use aseptic technique during all procedures (e.g., feeding tube insertion, IV care).
- Keep the child’s immunizations up-to-date.
- Administer antibiotics prophylactically if ordered (especially before dental or surgical procedures to prevent endocarditis).
- Monitor for early signs of infection (fever, cough, irritability).
- Encourage good oral hygiene to reduce oral bacterial load.
- Educate parents about home infection prevention measures.
Anxiety (Parental) Related to unfamiliarity with child’s condition and outcome uncertainty
Nursing Interventions :
- Provide truthful and simple explanations about the child’s condition and procedures.
- Involve parents in routine care to build confidence.
- Allow time for parents to ask questions and express fears.
- Encourage rooming-in and parental bonding.
- Refer to support groups or counselors for emotional support.
- Provide written materials and encourage participation in decisions.
Deficient Knowledge (Parent/Caregiver) Related to lack of understanding of disease, treatment, and home care
Nursing Interventions :
- Explain the anatomy and pathophysiology of VSD in simple terms.
- Teach parents the importance of medications like digoxin, diuretics, and how to administer them.
- Educate on feeding methods, recognizing signs of heart failure, and importance of follow-up.
- Demonstrate pulse counting if the child is on digoxin.
- Provide return demonstration to ensure understanding.
- Offer emergency contact numbers and signs that require urgent medical help.
OR
a) Define Neonate
A neonate is a newborn infant from birth up to 28 completed days of life, regardless of gestational age at birth. This period is also known as the neonatal period and is critical for adaptation to extrauterine life, involving major physiological changes such as independent breathing, thermoregulation, and feeding.
b) Enlist characteristics of normal newborn baby.
- The average birth weight of a normal full-term newborn baby ranges from 2.5 kg to 3.5 kg, and weight loss of up to 10% in the first week is considered normal due to fluid shifts.
- The length of a healthy newborn from crown to heel is approximately 45 to 55 centimeters, with boys generally being slightly longer than girls.
- The head circumference is about 32 to 36 centimeters, usually 2 cm larger than the chest circumference, reflecting normal brain development.
- The chest circumference measures around 30 to 34 centimeters, and it should be measured at the level of the nipples when the baby is quiet.
- The heart rate ranges between 120 to 160 beats per minute at rest, but may temporarily increase during crying or decrease during deep sleep.
- The respiratory rate of a normal newborn is 30 to 60 breaths per minute, with periodic breathing (brief pauses) being common in the first days of life.
- The normal axillary temperature is between 36.5°C to 37.5°C, and temperature instability may be a sign of infection or prematurity.
- The newborn’s skin is typically pink, though acrocyanosis (bluish hands and feet) may be present temporarily in the first few hours.
- The skin may be covered with vernix caseosa (a white, cheesy coating) and lanugo (fine body hair), which are more prominent in preterm babies.
- Peeling of skin (desquamation) may occur in post-term babies and is considered normal.
- The fontanelles (soft spots on the skull) are open at birth, with the anterior fontanelle being diamond-shaped and the posterior one being smaller and triangular.
- The newborn’s reflexes include Moro, rooting, sucking, palmar grasp, plantar grasp, Babinski, and tonic neck reflex, all of which indicate normal neurological function.
- The eyes may appear swollen or have subconjunctival hemorrhage due to pressure during delivery, and transient strabismus (misalignment) is normal.
- Tear production is limited at birth; babies begin producing tears after a few weeks.
- Hearing is well developed at birth; the baby will respond to loud noises with a startle reflex.
- The baby can see large shapes and light and prefers faces or contrasting colors.
- Taste and smell are developed; the baby prefers sweet tastes and recognizes the mother’s scent shortly after birth.
- The umbilical cord is bluish-white and gelatinous at birth and contains 2 arteries and 1 vein, drying up and falling off within 7–10 days.
- A healthy newborn usually passes urine within the first 24 hours and meconium (first stool) within the first 24–48 hours of life.
- The external genitalia may appear swollen due to maternal hormones, and in girls, a small bloody vaginal discharge (pseudomenstruation) may be seen.
- The breasts of both sexes may be slightly enlarged and may even secrete a little milk (witch’s milk), due to the effect of maternal estrogen.
- A normal newborn maintains a flexed posture with arms and legs drawn towards the body, and demonstrates spontaneous movements when awake.
- Crying is loud, strong, and used as the primary mode of communication in response to discomfort or hunger.
- Sleep duration in a newborn is approximately 16 to 20 hours per day, mostly in short intervals.
- The newborn has coordinated sucking and swallowing reflexes, enabling effective breastfeeding from birth.
- The behavioral states of the newborn alternate between quiet sleep, active sleep, drowsiness, quiet alert, active alert, and crying.
- A normal newborn does not show signs of distress like grunting, nasal flaring, chest retractions, or cyanosis beyond the first minutes of life.
- There should be no signs of birth injuries or congenital anomalies such as cleft lip, club foot, or abnormal limb movement.
c) Discuss nursing management of normal new born baby
Immediate Newborn Care (First 1 Hour)
- Ensure airway patency: Clear mouth and nose using sterile bulb syringe or suction if needed.
- Dry the baby thoroughly: Stimulates breathing and prevents heat loss.
- Initiate skin-to-skin contact: Promotes bonding and thermoregulation (Kangaroo Mother Care if preterm or LBW).
- Assess Apgar score at 1 and 5 minutes.
- Clamp and cut the umbilical cord using sterile technique after cord pulsation stops.
- Prevent heat loss : Wrap baby in warm cloth; place under radiant warmer if needed.
Thermal Protection
- Maintain room temperature between 26–28°C.
- Wrap baby in warm, dry clothes and cover the head.
- Use a radiant warmer if baby is cold.
- Delay first bath until 24 hours after birth.
Breastfeeding and Nutrition
- Initiate breastfeeding within 1 hour of birth.
- Encourage exclusive breastfeeding every 2–3 hours or on demand.
- Educate the mother on proper latching technique and breastfeeding positions.
- Monitor baby’s weight gain and output.
Umbilical Cord Care
- Keep the cord stump clean and dry – expose to air.
- Do not apply powder, ghee, or antiseptic unless prescribed.
- Watch for signs of infection (redness, pus, bad smell).
- Educate mother on safe handling during diapering and dressing.
Hygiene and Skin Care
- Bathe the baby only after 24 hours, using lukewarm water.
- Use mild soap and lukewarm water for sponge bath.
- Bathe only after thermoregulation is stable.
- Change diapers frequently and clean the genital area gently.
- Avoid applying talcum powder or scented lotions.
Monitoring Vital Signs and General Health :
- Monitor respiration (30–60/min) and heart rate (120–160 bpm).
- Check temperature (36.5–37.5°C) every 4–6 hours.
- Observe for signs of distress, jaundice, poor feeding, or lethargy.
- Record daily urine and stool output.
Immunization (Birth Dose) :
- Administer BCG (intradermal), OPV-0 (oral), and Hepatitis B-0 (IM).
- Document vaccine administration on immunization card.
- Educate mother about next due doses and possible side effects.
- Observe baby for 15–30 minutes post-vaccination for any reactions.
Parental Education :
- Teach about danger signs (fast breathing, fever, convulsions, poor feeding).
- Educate on exclusive breastfeeding and demand feeding cues.
- Demonstrate safe sleeping position (supine – on the back).
- Encourage routine growth monitoring and follow-up visits.
Documentation and Identification
- Record all details : birth weight, Apgar score, temperature, feeding behavior.
- Ensure mother and baby identification tags are matched and secured.
- Maintain nursing notes for any abnormalities or interventions.
- Report any deviation from normal development immediately.
Q-2 Short Essay question (any Three) 3×5=15
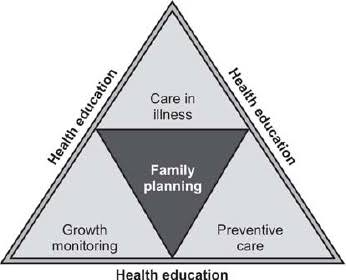
a) ICDS program
The Integrated Child Development Services (ICDS) is a comprehensive welfare program launched by the Government of India on October 2, 1975, under the Ministry of Women and Child Development. It is designed to promote the holistic development of children under 6 years of age and to support pregnant and lactating mothers, as well as adolescent girls under some extended schemes.
Objectives of ICDS
- The main aims of the ICDS program include :
- Enhancing the nutritional and health status of children below six years.
- Providing a strong foundation for proper psychological, physical, and social development.
- Reducing the incidence of malnutrition, morbidity, and mortality.
- Lowering school dropout rates by supporting pre-school education.
- Improving the capacity of mothers to look after their own health and nutrition, as well as that of their children.
Target Beneficiaries
The ICDS scheme targets :
- Children from 0 to 6 years
- Pregnant women
- Lactating mothers
- Adolescent girls in certain schemes like SABLA
Services Provided in ICDS
Supplementary Nutrition :
Nutritious meals or take-home rations are provided to combat child malnutrition and undernutrition in mothers.
Immunization :
Conducted in coordination with the Health Department, covering vaccines against common childhood diseases.
Health Check-ups :
Routine physical exams, growth monitoring, and identification of early signs of illness.
Referral Services :
Children or women who require medical attention are referred to nearby health centers.
Pre-school Education :
Non-formal education is offered to children between 3 and 6 years of age to enhance school readiness.
Nutrition and Health Education :
Mothers and women in the community are educated about child care, hygiene, feeding practices, and family planning.
Role of Anganwadi Centers (AWCs)
Anganwadi Centers are the grassroot-level delivery points for all ICDS services. They are managed by trained Anganwadi Workers (AWWs) and helpers. These centers act as a link between the community and health services, especially in rural and tribal areas.
Link with Health Services
ICDS works in collaboration with the health system to provide :
- Immunization services
- Vitamin A supplementation
- Deworming
- Growth monitoring and health referrals
Recent Developments
- Poshan Abhiyaan (National Nutrition Mission) has been launched to reduce malnutrition and promote better nutrition practices.
- Introduction of real-time digital monitoring through Common Application Software (CAS).
- Upgradation of Anganwadi centers and services.
Impact of ICDS
The ICDS program has contributed significantly to :
- Decrease in child malnutrition and mortality
- Improvement in maternal awareness
- Boost in school readiness through pre-primary education
- Promotion of community-based child care
b) Prevention of accident in children
Accidents are a leading cause of injury, disability, and death among children worldwide. Most childhood accidents occur due to lack of supervision, unsafe environments, or curiosity-driven behavior.
Supervision and Safe Environment at Home
- Always provide constant adult supervision, especially for infants and toddlers.
- Keep small objects, sharp tools, hot liquids, medicines, and chemicals out of reach.
- Use safety gates near stairs, corner guards on furniture, and non-slip mats in bathrooms.
- Cover electrical sockets and ensure that wires are tucked away.
- Avoid using walkers, as they increase the risk of falls and head injuries.
Safe Sleeping Practices for Infants
- Lay the baby on their back to sleep to prevent sudden infant death syndrome (SIDS).
- Avoid soft bedding, stuffed toys, or pillows in the crib.
- Ensure crib rails are high enough to prevent falls.
Traffic and Road Safety
- Always use child safety seats or seat belts in vehicles appropriate for age and size.
- Teach older children road-crossing rules and encourage walking on sidewalks.
- Ensure children wear helmets while riding bicycles or skateboards.
- Never leave children alone in a parked car.
Water Safety
- Never leave children unattended near bathtubs, pools, or buckets of water.
- Install fences around pools with self-locking gates.
- Teach basic swimming skills and water safety rules early.
- Store water containers covered or inverted to prevent drowning.
Burn and Fire Prevention
- Keep hot items, matches, and lighters out of reach.
- Turn pot handles inward while cooking and use back burners.
- Install smoke alarms and teach fire escape drills.
- Avoid giving children access to firecrackers or candles.
Electrical Safety
- Use socket covers, child-proof switches, and insulated wires.
- Teach children not to touch electrical items with wet hands.
- Avoid overloading plugs or using unsafe extension cords.
Toy and Play Safety
- Choose age-appropriate toys free from small detachable parts (choking risk).
- Ensure toys are non-toxic, have no sharp edges, and are properly maintained.
- Regularly inspect playgrounds for broken equipment or sharp objects.
Poisoning Prevention
- Store all medicines, cleaning agents, pesticides, and cosmetics in locked cabinets.
- Educate children not to eat unknown berries, plants, or substances.
- Keep Poison Control Center numbers handy for emergencies.
First Aid and Emergency Preparedness
- Educate caregivers and school staff on basic first aid and CPR.
- Keep a well-stocked first aid kit at home and school.
- Ensure emergency contact numbers are visible and accessible.
Parental and Community Education
- Conduct awareness programs, parenting classes, and health education in communities and schools.
- Encourage development of safe play areas, traffic rules near schools, and community vigilance.
c) Care of newborn under phototherapy
Positioning and Exposure
- Place the baby under the phototherapy unit, keeping a distance of 30–45 cm from the light source (as per guidelines).
- Ensure maximum skin exposure – remove clothing; keep only diaper and eye pads on.
- Turn the baby frequently (every 2–3 hours) for uniform light exposure.
Eye and Genital Protection
- Use soft, clean eye pads to cover the newborn’s eyes and remove during feeding.
- Genitals (especially in male infants) should be loosely covered to avoid direct light exposure.
Temperature Monitoring
- Check axillary temperature every 2–4 hours to prevent hypo- or hyperthermia.
- Maintain an appropriate room temperature or use a radiant warmer if needed.
Hydration and Nutrition
- Phototherapy increases water loss; watch for signs of dehydration (sunken fontanelle, dry lips, reduced urine).
- Encourage frequent breastfeeding or formula feeding.
- Administer IV fluids if prescribed.
Monitoring of Bilirubin Levels
- Check serum bilirubin levels regularly as advised by the doctor (e.g., every 12–24 hours).
- Discontinue phototherapy once bilirubin levels reach the safe range.
Skin and Diaper Care
- Monitor skin for rashes, peeling, or burns.
- Change diapers frequently; observe for greenish, loose stools due to bilirubin excretion.
- Apply barrier creams to prevent diaper rash.
Observation for Complications
- Watch for bronze baby syndrome (gray-brown skin discoloration).
- Assess for irritability, lethargy, or temperature instability.
Parental Education
- Educate parents on purpose of phototherapy, expected changes (e.g., green stools), and safety measures.
- Involve them in feeding, bonding, and comforting the baby during breaks.
Phototherapy Unit Maintenance
- Ensure the light source is functioning properly.
- Clean the equipment regularly to maintain infection control.
- Replace bulbs when intensity reduces as per protocol.
d) Dietary management of children with nutritional anemia
Nutritional anemia in children is most commonly caused by iron deficiency, but may also be due to folic acid, vitamin B12, and protein deficiencies. Proper dietary management is essential to correct anemia, restore hemoglobin levels, and promote healthy growth and development.
Iron-Rich Food Inclusion
- Encourage for foods rich in heme iron (better absorbed) : Liver, lean meat, fish, poultry, egg yolk
- Include non-heme iron sources : Green leafy vegetables (spinach, amaranth), pulses, jaggery, dried fruits (raisins, dates), and whole grains.
- These foods should be incorporated regularly into meals and snacks.
Enhancing Iron Absorption
- Include vitamin C-rich foods in every meal to improve iron absorption : Lemon, orange, guava, tomato, amla, papaya, sweet lime.
- Prefer cooked over raw leafy vegetables (to improve digestibility and absorption).
- Use iron utensils for cooking, which may increase iron content in food.
- For example, squeezing lemon over cooked lentils or serving fruit juice with snacks can improve iron uptake.
Avoid Iron Absorption Inhibitors
- Certain dietary substances hinder iron absorption and should be avoided during or immediately after meals
- Limit intake of tea, coffee, cola, and calcium-rich foods (milk, curd) alongside iron-rich meals.
- Avoid high-fiber, phytate-rich foods (bran, unsoaked legumes) during iron supplementation.
Meal Frequency and Balance
- Provide small, frequent, and balanced meals to maintain energy levels and prevent fatigue.
- Ensure a diet that includes proteins, carbohydrates, fats, and micronutrients to support red blood cell formation.
Infant and Toddler Feeding Practices
- Encourage exclusive breastfeeding for 6 months followed by iron-rich complementary feeding.
- After 6 months, iron-rich complementary foods should be introduced.
- Introduce fortified cereals and mashed pulses/vegetables after 6 months.
- Avoid overdependence on cow’s milk, which is low in iron and can irritate the gut lining.
- Cow’s milk should be limited before one year, as it is low in iron and can cause gut irritation leading to occult blood loss.
Use of Fortified and Supplementary Foods
- Promote iron-fortified cereals, flour, and formula milk.
- Utilize supplementary nutrition programs like ICDS and school mid-day meals, which offer iron-rich food to school-age children.
Iron and Folic Acid Supplementation (as prescribed)
- In cases of moderate to severe anemia, diet alone may not be sufficient. Oral iron and folic acid supplementation is commonly prescribed and should be administered as per the pediatrician’s recommendation.
- Ensure compliance and educate parents about duration and side effects like dark stools or mild nausea.
Nutrition Education for Family
- Counsel parents on the importance of a balanced diet, proper food combinations, and timing of meals.
- They should be informed about the importance of iron-rich foods, cooking methods, and combination of foods that improve absorption.
- Visual aids, cooking demonstrations, and dietary charts can be used to reinforce messages
- Involve the caregiver in meal planning and monitor growth and hemoglobin levels regularly.
e) Care of child with burn
1. Emergency Care (First Aid at Burn Site)
- Remove child from the source of the burn.
- Cool the burn with running tap water (not ice) for 10–20 minutes.
- Remove clothing/jewelry near the burned area, but do not peel off stuck clothes.
- Cover the burn with sterile, non-stick dressing or a clean cloth.
- Keep the child warm and calm.
- Seek immediate medical attention, especially for large or deep burns.
2. Hospital/Nursing Care
A. Airway, Breathing, Circulation (ABC) :
- Assess for airway obstruction (especially in facial burns or inhalation injury).
- Provide humidified oxygen if needed.
- Start IV fluids using Parkland formula (for >10% TBSA burns in children).
- Monitor vital signs continuously.
B. Fluid Resuscitation :
- Prevent hypovolemia using Ringer’s Lactate based on weight and surface area burned.
- Monitor urine output (goal: 1–2 mL/kg/hr in children).
C. Nutritional Support :
- High-calorie, high-protein diet.
- May require enteral feeding or NG tube in severe burns.
- Encourage oral fluids in minor burns.
D. Wound Care :
- Clean wounds daily with normal saline or mild antiseptic.
- Apply topical antibiotics (e.g., silver sulfadiazine).
- Use non-adherent dressings and change regularly.
- Monitor for infection signs (redness, swelling, pus, fever).
E. Pain Management :
- Administer prescribed analgesics like paracetamol or morphine.
- Use distraction techniques during dressing changes.
F. Infection Control :
- Strict hand hygiene and aseptic dressing techniques.
- Isolate child if needed to prevent cross-infection.
- Monitor for systemic infection or sepsis.
3. Nursing Responsibilities
- Provide emotional support to child and parents.
- Maintain accurate intake-output charting.
- Assess for signs of shock, infection, or respiratory distress.
- Educate parents on home care, wound management, and nutrition.
- Encourage early mobilization and physiotherapy to prevent contractures.
- Monitor growth and developmental delays in long-term cases.
4. Psychological Support
- Offer counseling for child and family to cope with trauma.
- Engage child in play therapy to reduce fear and anxiety.
- Promote body image acceptance in older children with visible scarring.
5. Prevention Education
- Teach burn prevention at home: keep hot objects out of reach, use safety covers, and supervise children.
- Promote fire safety, safe cooking practices, and use of child-safe devices.
Q-3 Short answer question (any four) 4×2=8
a) Define NICU
NICU stands for Neonatal Intensive Care Unit. It is a specialized hospital unit that provides intensive medical care and monitoring to critically ill, premature, or low birth weight newborns who require advanced support for survival and development. It is equipped with incubators, ventilators, monitors, and skilled neonatal staff. It Support the infants with respiratory distress, infections, birth defects, or complications during birth.
b) List down diseases caused by vitamin A’deficiency
- Night Blindness (Nyctalopia)
- Xerophthalmia
- Bitot’s Spots
- Keratomalacia
- Conjunctival and Corneal Xerosis
- Growth Retardation in Children
- Increased Susceptibility to Infections
- Follicular Hyperkeratosis
- Impaired Iron Metabolism
c) Explain degree of dehydration
Dehydration is the loss of body fluids (mainly water and electrolytes) from the body. It is classified based on the percentage of body weight lost and clinical signs, especially important in children. It includes
Mild Dehydration
- In which < 5% body weight loss
- Signs: Dry mouth, thirst, reduced urine output
Moderate Dehydration
- In which 5–10% body weight loss
- Signs : Sunken eyes, dry tongue, poor skin turgor, irritability
Severe Dehydration
- In which 10% body weight loss
- Signs : Lethargy, cold extremities, low blood pressure, sunken fontanelle (in infants), shock
d) Discuss behavioral problems in toddler
Behavioral problems in toddlers refer to challenging or disruptive behaviors that are common during early childhood (1–3 years), often due to emotional, developmental, or environmental factors. Common Behavioral Problems are Temper Tantrums, Aggression, Separation Anxiety, Thumb Sucking, Sleep and Eating Problems
e) Define cold chain
The cold chain is a temperature-controlled system used for storing and transporting vaccines and other heat-sensitive medical products within a recommended range of +2°C to +8°C to maintain their potency, safety, and effectiveness. t begins from the manufacturer and continues through transport, storage at health facilities, and finally to the point of administration. The cold chain includes the use of Ice-Lined Refrigerators (ILRs), deep freezers, cold boxes, vaccine carriers, and ice packs
Section B-37
Q-4-Long answer question (any one)
a) Define acute glomerulonephritis (2 mark)
Acute Glomerulonephritis is a sudden inflammation of the glomeruli of the kidneys, usually following a streptococcal infection, resulting in hematuria, proteinuria, edema, and hypertension due to impaired kidney filtration.
b) Explain pathophysiology and clinical manifestation of acute glomerulonephritis (5 mark)
Pathophysiology
Preceding Streptococcal Infection
- AGN commonly follows an infection, especially by Group A beta-hemolytic Streptococcus, causing pharyngitis (throat infection) or impetigo (skin infection).
- This usually occurs 1–3 weeks before the onset of renal symptoms.
Formation of Antigen-Antibody Complexes
- The immune system produces antibodies in response to streptococcal antigens.
- These antibodies combine with antigens in the circulation, forming immune complexes.
Deposition in Glomerular Capillaries
- The immune complexes get trapped in the glomerular basement membrane (GBM), which is the filter unit of the kidney.
- This activates the complement system (a part of immune defense).
Inflammatory Response in the Glomeruli
- Complement activation triggers inflammation in the glomerular capillaries.
- Inflammatory cells (neutrophils, macrophages) infiltrate the glomeruli, leading to :
- Swelling (edema) of glomerular cells
- Proliferation of mesangial and endothelial cells
- Thickening of glomerular walls
Increased Capillary Permeability
- Inflammation damages the glomerular filtration barrier, increasing its permeability.
- As a result : Red blood cells (RBCs) leak into urine → Hematuria, Proteins leak into urine → Proteinuria, Decreased Glomerular Filtration Rate (GFR)
- It occurs due to Swelling and congestion in the glomeruli, Obstruction from cellular debris and inflammatory cells
- This leads to reduced urine output (oliguria) and fluid retention.
Sodium and Water Retention
- As kidneys fail to excrete sodium and water:
- Generalized edema develops (especially around the eyes and lower limbs).
- Blood volume increases, contributing to hypertension (high BP).
Other Associated Symptoms
- Azotemia (increased blood urea and creatinine) due to impaired waste removal.
- Fatigue, headache, and irritability due to hypertension and uremia.
- Possible low-grade fever if infection or inflammation persists.
Clinical manifestation
Acute glomerulonephritis presents with sudden symptoms related to inflammation and dysfunction of the glomeruli, typically appearing 1–3 weeks after a streptococcal infection (throat or skin).
Hematuria (Blood in Urine)
- Hallmark sign of AGN.
- Urine appears cola-colored, tea-colored, or smoky due to RBC leakage into urine.
- Microscopic or gross hematuria may be present.
Oliguria (Reduced Urine Output)
- It occurs due to decreased glomerular filtration rate (GFR).
- Urine output is significantly reduced, and urine may appear dark or cloudy.
Edema
- Commonly periorbital (around the eyes), especially in the morning.
- May also involve feet, ankles, hands, or abdomen.
- Results from sodium and water retention.
Hypertension
- It Occurs due to fluid overload and activation of the renin-angiotensin system.
- It May cause headache, blurred vision, or irritability.
Headache and Lethargy
- Due to increased blood pressure or mild uremia.
- The child may be drowsy, fatigued, or irritable.
Proteinuria
- Presence of protein in urine due to glomerular membrane damage.
- Usually mild to moderate in AGN.
Anorexia and Nausea
- Poor appetite and vomiting may occur due to uremia or systemic effects.
Low-grade Fever
- May be present if AGN follows an infection.
- Fever is usually mild but should be monitored.
Flank or Abdominal Pain
- Some children may complain of pain or discomfort in the flanks due to kidney inflammation.
Signs of Underlying Streptococcal Infection
- History of recent sore throat or skin infection.
- Throat swab or ASO (anti-streptolysin O) titers may be positive.
c) Discuss medical and nursing management of child with acute glomerulonephritis (7 mark)
Medical management
Antibiotic
The first step in managing acute glomerulonephritis is the administration of appropriate antibiotics, such as penicillin or amoxicillin, to eliminate any residual streptococcal infection, although the antibiotics do not affect the kidney inflammation directly, they prevent recurrence.
Antihypertensive medications
Antihypertensive medications like nifedipine, hydralazine, or labetalol are given to control elevated blood pressure, which is a common and potentially serious complication of AGN, and blood pressure must be closely monitored during therapy.
Diuretics
Diuretics, especially furosemide, are used to promote diuresis and relieve fluid overload and edema, especially when the child presents with puffiness around the eyes, swollen limbs, or reduced urine output.
Fluid restriction
If the child shows signs of oliguria, fluid restriction is strictly followed and input-output monitoring is done regularly to prevent fluid retention and possible pulmonary edema or heart overload.
Diet management
The diet is carefully adjusted to be low in sodium to control edema and hypertension, low in potassium if hyperkalemia is present, and moderate in protein to avoid excessive nitrogen waste in case of reduced kidney function.
Fluid and electrolyte nmanagement
In cases where the child has significant electrolyte imbalances, like hyperkalemia or hyponatremia, immediate correction is done through carefully calculated IV fluids or electrolyte replacement therapy under close monitoring.
Complication management
If complications like hypertensive encephalopathy or seizures occur, anticonvulsants such as diazepam may be administered to manage neurological symptoms effectively.
In severe or unresponsive cases, where there is acute kidney failure, severe uremia, or fluid overload, the child may require emergency dialysis to restore kidney function and remove waste products.
Supportive care
It including bed rest during the acute phase, is important to reduce physical stress on the kidneys and allow healing, and gradual return to normal activity is encouraged once symptoms subside.
Nursing Management of a Child with Acute Glomerulonephritis (AGN)
Monitoring and Assessment
- Monitor vital signs, especially blood pressure frequently to detect and manage hypertension.
- Measure and record daily weight to assess fluid retention or overload.
- Monitor intake and output (I/O) carefully, noting oliguria or changes in urine color.
- Assess for signs of edema, particularly periorbital, sacral, or dependent.
- Evaluate for neurological symptoms like headache, irritability, or drowsiness (indicating hypertension or uremia).
Fluid and Electrolyte Balance
- Maintain fluid restriction as prescribed to prevent fluid overload.
- Administer IV fluids cautiously if needed and monitor for signs of fluid retention.
- Monitor serum electrolytes, especially sodium and potassium.
- Watch for signs of hyponatremia (confusion, weakness) and hyperkalemia (irregular pulse, ECG changes).
Dietary Management
- Provide a low-sodium, low-potassium, and moderate protein diet as advised.
- Restrict salty snacks, canned foods, and pickles to reduce edema and hypertension.
- If oliguria is severe, also restrict fluid and potassium intake.
Medication Administration
- Administer antihypertensives (e.g., nifedipine, hydralazine) as prescribed to control blood pressure.
- Give diuretics (e.g., furosemide) if ordered, to reduce edema and fluid overload.
- Administer antibiotics if streptococcal infection is confirmed or suspected.
- Observe for adverse drug reactions and effectiveness of therapy.
Rest and Activity
- Encourage bed rest during the acute phase to reduce cardiac and renal workload.
- Gradually increase activity as edema, hypertension, and fatigue subside.
- Provide a calm environment and encourage quiet play or books during recovery.
Infection Control
- Practice strict hand hygiene and aseptic techniques during procedures.
- Limit visitors if the child is immunocompromised.
- Monitor for any signs of secondary infection (fever, sore throat, cough).
Psychological and Emotional Support
- Reassure the child and parents about the prognosis and recovery.
- Encourage parental presence and participation in care to reduce child anxiety.
- Provide age-appropriate explanations and emotional comfort to the child.
Health Education and Discharge Teaching
- Educate parents about :
- Monitoring blood pressure at home
- Medication adherence
- Importance of follow-up visits
- Signs of relapse (e.g., reduced urine, swelling, hematuria)
- Instruct on dietary restrictions and fluid monitoring.
OR
a) Define Hirschprung’s disease (2 mark)
Hirschsprung’s disease is a congenital disorder of the intestine in which ganglion cells (nerve cells) are absent in a portion of the bowel, most commonly in the distal colon or rectum, resulting in intestinal obstruction due to the failure of peristalsis in the affected segment. It is also known as congenital aganglionic megacolon.
b) Explain clinical manifestation of Hirschprung’s disease (5 mark)
I. In Neonates (Birth to 28 Days)
Failure to pass meconium within 24–48 hours after birth
Normally, term neonates pass meconium within the first 24 hours. Failure to do so is often the first sign of Hirschsprung’s disease.
Progressive abdominal distension
Due to accumulation of gas and intestinal content proximal to the aganglionic segment. The abdomen may appear tight and shiny.
Bilious vomiting (green-colored)
Indicates obstruction distal to the ampulla of Vater. This is a serious symptom and should be immediately investigated.
Refusal to feed or poor feeding
The baby may become irritable, cry excessively, or reject breastfeeding due to bloating and discomfort.
Constipation or infrequent bowel movements
Some neonates may pass small amounts of watery stool or mucus due to overflow diarrhea, but no normal stool pattern is established.
Tight anal sphincter and empty rectum on digital rectal examination
Upon insertion of a finger into the rectum, it feels empty, but withdrawal is often followed by explosive expulsion of gas and stool (called the “squirt sign”).
II. In Infants (1–12 Months)
Chronic constipation since birth
Persistent difficulty passing stools, requiring suppositories, rectal stimulation, or enemas.
Abdominal distension and bloating
Gradually increases over time, especially after feeding. The abdomen may be asymmetrically enlarged.
Vomiting
May be non-bilious or bilious depending on severity and level of obstruction.
Feeding intolerance
The infant may suck poorly or vomit after feeds due to gut fullness.
Poor weight gain or failure to thrive
Due to chronic undernutrition and malabsorption.
Irritability and fussiness
Associated with discomfort from gas, distension, or hunger due to reduced intake.
III. In Older Children (1 year and above)
Long-standing constipation
Child may have a history of infrequent, hard stools, often not passed daily. Parents may report stooling every few days or once a week.
Abdominal distension
Chronic distension may be visible and associated with discomfort or visible peristaltic waves.
Pencil-like or ribbon-like stools
Stool passes through a narrowed segment, making it thin in appearance.
Foul-smelling, explosive stools after enemas
A classic sign that indicates blockage with backup and sudden release after intervention.
Abdominal pain and bloating
Especially after meals, due to poor gut motility.
Malnutrition and anemia
Result from inadequate digestion, absorption, and chronic illness.
Soiling or overflow incontinence
May occur due to excessive fecal loading and leakage around the impaction (not due to true sphincter weakness)
c) Discuss pre and post-operative nursing management of child with Hirschprung’s disease (7 mark)
I. Pre-operative Nursing Management
Assessment and Monitoring
- Monitor vital signs frequently and assess for early signs of enterocolitis (fever, lethargy, abdominal tenderness).
- Record abdominal girth daily to monitor distension.
- Assess for dehydration signs such as sunken eyes, dry mucosa, or poor skin turgor.
- Observe and chart bowel habits, vomiting episodes, and tolerance to feeds.
Bowel Preparation
- Administer rectal irrigations or enemas as prescribed to decompress the colon.
- Maintain strict NPO status to prevent vomiting and aspiration before surgery.
- Insert a nasogastric tube if required, for bowel decompression.
- Ensure gentle handling during rectal procedures to avoid bowel injury.
Nutritional Support
- Maintain IV fluid therapy to support hydration and electrolytes.
- Monitor electrolyte levels and report abnormalities like hyponatremia or hypokalemia.
- If malnourished, consult a dietitian for pre-op nutritional planning.
- Consider parenteral nutrition if the child cannot tolerate oral intake.
Infection Prevention
- Perform hand hygiene before and after handling the child.
- Monitor for signs of sepsis, especially in neonates with fever and poor feeding.
- Administer prophylactic antibiotics if ordered.
- Keep the perianal area clean to prevent fecal contamination and skin breakdown.
Psychological Support
- Use age-appropriate communication to reduce anxiety in the child.
- Allow parents to stay with the child to offer emotional comfort.
- Engage child in play therapy or distraction techniques if appropriate.
- Prepare the child and family using pre-op teaching tools (e.g., models, drawings).
Education to Parents
- Teach parents how to recognize signs of worsening condition, like vomiting, no stool, or fever.
- Educate about the planned surgery, possible colostomy, and hospital stay.
- Instruct on rectal irrigation technique if parents are involved in pre-op care.
- Reassure parents about prognosis and expected outcomes.
II. Post-operative Nursing Management
Monitoring Vital Signs and Pain
- Assess for hypotension, tachycardia, or fever as signs of complications.
- Use pediatric pain scales (e.g., FLACC scale) to assess pain accurately.
- Provide prescribed analgesics, monitor response, and observe for side effects.
- Watch for restlessness, crying, or guarding behavior as signs of discomfort.
Wound and Stoma Care
- Inspect surgical incision or stoma for redness, swelling, or discharge.
- Change dressing using sterile technique as per surgeon’s protocol.
- Keep the peristomal skin dry and apply protective barriers to prevent breakdown.
- Teach parents how to clean and empty colostomy bags if applicable.
Maintain Fluid and Electrolyte Balance
- Monitor intake and output every 4–6 hours.
- Check urine color and frequency as indicators of hydration.
- Administer IV fluids with electrolytes as ordered and monitor for fluid overload.
- Monitor for hypokalemia or hyponatremia, especially after diarrhea.
Gradual Reintroduction of Feeding
- Start with clear liquids, then gradually advance to breast milk or formula.
- Assess for vomiting, abdominal distension, or intolerance after each feed.
- Monitor weight gain daily to assess nutrition status.
- Encourage small frequent feeds to reduce GI burden.
Bowel Function Monitoring
- Document first bowel movement post-surgery including color, consistency, and amount.
- Watch for signs of straining, pain, or rectal bleeding.
- Alert physician if there’s no stool passed after 48 hours post-surgery.
- Monitor for recurrence of constipation or enterocolitis symptoms.
Infection Prevention
- Continue aseptic care for all invasive devices (IV lines, catheters).
- Maintain hand hygiene for staff, child, and family members.
- Watch for wound infection signs like purulent drainage or localized heat.
Emotional Support
- Provide a non-judgmental environment for parents to express concerns.
- Offer counseling services if the family shows signs of stress or anxiety.
- Encourage parent-child bonding by promoting rooming-in and participation in care.
- Reinforce positive outcomes and long-term prognosis to build confidence.
Parental education
- Administer prescribed antibiotics on time.
- Teach about medications, feeding plan, and wound/stoma care at home.
- Instruct on signs of infection, dehydration, or bowel obstruction.
- Provide written care instructions and emergency contact numbers.
- Arrange for follow-up visits and support for colostomy care or reversal surgery.
Q-5 Short Essay question (any Three)
a) Reaction of toddler to hospitalization
Hospitalization is often a stressful and frightening experience for toddlers (ages 1–3 years), as they are in the stage of developing autonomy and attachment to parents. Their understanding is limited, and changes in routine can trigger strong emotional responses.
1. Separation Anxiety (Most Prominent Reaction)
- Intense fear and distress when separated from primary caregiver.
Stages :
- Protest : Loud crying, screaming, searching for parent, rejecting contact from others.
- Despair : Quiet, withdrawn, passive behavior; appears depressed.
- Detachment : Superficial adjustment, increased interest in surroundings but emotional withdrawal from parents.
- May refuse to eat or sleep, showing loss of trust.
2. Fear of Pain and Bodily Harm
- Fear of injections, bandages, thermometers, oxygen masks, etc.
- Misinterpret procedures as punishment for something bad they did.
- Exhibit defensive behaviors like kicking, biting, screaming.
- May resist even non-painful procedures due to anticipatory fear.
3. Loss of Control and Autonomy
- Hospital environment restricts normal freedom and movement.
- Forced immobility, physical restraints (like IVs), and lack of choices lead to frustration.
- May refuse to cooperate, throw tantrums, or try to remove IVs/catheters.
4. Stranger Anxiety
- Strong fear of unfamiliar people, especially medical staff in uniforms.
- Becomes agitated or frightened during examinations or treatments.
- May cling to caregivers or hide when approached by staff.
5. Regression of Developmental Skills
- Returns to earlier behaviors like thumb sucking, bottle feeding, bedwetting, or baby talk.
- Regression is a coping mechanism in response to emotional stress.
6. Disruption in Daily Routines
- Change in eating, sleeping, and toileting routines causes irritability.
- Refuses hospital food, resists naps, or cries more at night.
- Loss of routine may lead to anxiety and confusion.
7. Sleep Disturbances
- Fear of the dark, unfamiliar surroundings, or noise from equipment may disrupt sleep.
- May develop nightmares, night terrors, or fear of sleeping alone.
8. Aggression and Hostile Behavior
- May become physically aggressive: biting, hitting, kicking nurses or parents.
- Verbal aggression: shouting, saying “go away” or “I hate you”.
- Expresses anger and helplessness through tantrums or disobedience.
9. Clinginess and Dependency
- Seeks constant reassurance and physical contact from parents.
- May cry when the caregiver tries to leave even for short periods.
- Demands attention and becomes overly attached.
10. Refusal of Food or Medication
- Toddlers may resist taking medicines or refuse food as a way to exert control.
- May associate feeding with punishment or discomfort.
11. Changes in Communication
- May become mute or less talkative.
- Use of nonverbal behaviors (pointing, nodding) increases due to fear or emotional distress.
b) Neonatal resuscitation
Definition
Neonatal resuscitation is the emergency medical management given to a newborn baby who is not breathing, gasping, or has inadequate heart rate at birth, with the goal of establishing normal breathing, heart rate, and circulation to sustain life and prevent complications.
Aims and Objectives
- To initiate and maintain effective ventilation and oxygenation
- To ensure adequate perfusion and cardiac function
- To prevent birth asphyxia-related complications like brain damage or death
- To reduce neonatal morbidity and mortality
Indications
- Resuscitation is required if the newborn:
- Is not breathing or crying
- Has gasping or irregular respiration
- Has a heart rate <100 beats/min
- Shows central cyanosis or limp muscle tone
Initial Rapid Assessment (Golden Minute)
- Within the first 60 seconds after birth, evaluate:
- Is the baby term?
- Is the baby crying or breathing?
- Does the baby have good muscle tone?
- If Yes to all → Provide routine care
- If No to any → Start resuscitation steps
Steps of Neonatal Resuscitation
1. Initial Steps (First 30 Seconds)
- Provide warmth (under radiant warmer)
- Position airway (sniffing position)
- Suction mouth and nose if needed
- Dry the baby thoroughly
- Provide tactile stimulation (back rub, foot flick)
- Reassess after 30 seconds
- If apnea or HR <100 bpm → Begin positive pressure ventilation (PPV)
2. Positive Pressure Ventilation (PPV)
- Use bag and mask ventilation (self-inflating bag or T-piece resuscitator)
- Begin with room air (21%); use oxygen if condition does not improve
- Provide breaths at 40–60/min
- Reassess chest movement and HR after 30 seconds
- If HR <60 bpm after effective PPV → Start chest compressions
3. Chest Compressions
- Use two-thumb technique over lower third of sternum
- Coordinate with ventilation in a 3:1 ratio
- 90 compressions + 30 breaths = 120 events/min
- Reassess after 60 seconds
- If HR remains <60 bpm → Administer drugs
4. Medications
- Epinephrine (0.01–0.03 mg/kg IV or via ET tube)
- Volume expanders (normal saline 10 mL/kg IV) if hypovolemia is suspected
- Administer medications after ensuring effective ventilation and compressions
Role of the Nurse in Neonatal Resuscitation
Preparation :
- Ensure all equipment is ready: warmer, oxygen, suction, bag-mask, medications
- Check functionality of resuscitation devices
Observation and Assessment :
- Monitor baby’s respiration, color, tone, and heart rate
- Assess Apgar score at 1 and 5 minutes
Assist in Resuscitation :
- Perform initial steps
- Provide bag-mask ventilation
- Assist physician in chest compressions and drug administration
Documentation :
- Time of birth
- Apgar scores
- Interventions provided
- Baby’s response
Post-Resuscitation Care :
- Transfer to NICU if required
- Monitor temperature, glucose, oxygenation
- Maintain records and inform family gently and clearly
c) Play therapy in children
Definition
Play therapy is a therapeutic approach that uses play as a medium to help children express emotions, cope with stress, improve behavioral issues, and promote emotional healing and development. It is based on the principle that play is a child’s natural language and a vital tool for understanding their inner world.
Objectives of Play Therapy
- To help children express feelings that may be difficult to verbalize
- To assist children in coping with trauma, fear, anxiety, or illness
- To enhance communication and build trust
- To develop problem-solving and coping skills
- To promote social, emotional, and cognitive development
- To relieve tension, stress, or boredom, especially during hospitalization
Types of Play Therapy
Directive Play Therapy :
- Therapist guides the session with structured activities and specific goals.
- Used for behavior modification and skill-building.
- Non-directive (Child-centered) Play Therapy:
- The child leads the session; therapist observes and supports without control.
- Encourages free expression of feelings.
Therapeutic Play :
- Used in hospital settings to help children understand procedures (e.g., using dolls to demonstrate IV insertion).
- Aims to reduce fear of medical equipment.
Medical Play :
- Helps children familiarize with healthcare tools, roles, and procedures.
Fantasy Play / Role Play :
- Children act out roles (doctor, parent, superhero) to express real-life concerns or wishes.
Materials Used in Play Therapy
- Toys: dolls, action figures, puppets
- Art supplies : crayons, paints, clay
- Sand and water trays
- Games, puzzles, building blocks
- Medical kits (for therapeutic play in hospitals)
Role of Nurse in Play Therapy
- Assess the child’s developmental level and emotional state
- Choose appropriate play materials based on age and needs
- Create a safe, friendly environment for play
- Encourage participation without pressure
- Observe behavior, verbal and non-verbal cues
- Use play to explain medical procedures and reduce anxiety
- Collaborate with child psychologists or therapists when necessary
- Educate parents about the benefits of therapeutic play
Clinical Importance of Play Therapy
- Helps hospitalized children cope with illness and separation from family
- Reduces pre-operative and procedural anxiety
- Encourages emotional resilience and positive behavior
- Aids in the diagnosis of emotional or psychological disorders
d) Nursing responsibility in oxygen therapy
Assess the Need for Oxygen Therapy
- Assess respiratory rate, depth, rhythm, and effort.
- Monitor for signs of hypoxia: restlessness, confusion, irritability, anxiety, cyanosis (bluish discoloration of lips, nail beds), tachypnea, and tachycardia.
- Measure oxygen saturation (SpO₂) using a pulse oximeter (normal range: 95–100%).
- Evaluate arterial blood gases (ABG) if ordered.
- Identify conditions requiring oxygen such as COPD, pneumonia, asthma, ARDS, cardiac failure, etcVerify Physician’s Order
- Confirm the flow rate (e.g., 2 L/min) and method of delivery (e.g., nasal cannula, face mask).
- Note any special instructions: humidification, target SpO₂, weaning plan.
- Check for patient-specific precautions, especially in CO₂ retainers like COPD patients (oxygen should be given cautiously).
- If no order is available in an emergency, begin oxygen and notify the physician immediately.
Select and Prepare Equipment
- Choose the correct delivery device based on the patient’s condition:
- Nasal cannula (low flow)
- Simple face mask, Venturi mask (fixed FiO₂)
- Non-rebreather mask, partial rebreather mask (high flow)
- Check the oxygen source (cylinder or central supply) for sufficient levels.
- Test the flowmeter, connect tubing securely.
- Attach humidifier if flow is more than 4 L/min to avoid drying of airways.
- Ensure tubing is not kinked or leaking.
Administer Oxygen Safely
- Explain the procedure to reduce anxiety and ensure cooperation.
- Place the device securely:
- Nasal prongs properly positioned.
- Masks should fit snugly without air leakage.
Maintain prescribed flow rate, typically:
- 1–6 L/min for nasal cannula
- 6–10 L/min for simple mask
- 10–15 L/min for non-rebreather mask
- Check for comfort and reposition as needed.
Monitor Patient Continuously
- Monitor vital signs, especially SpO₂, RR, HR, and BP.
Watch for signs of:
- Oxygen toxicity (e.g., coughing, chest pain, drowsiness).
- Hypoventilation in CO₂ retainers.
- Dryness or bleeding from nasal mucosa.
- Assess for skin integrity around ears, cheeks, and nose.
- Evaluate effectiveness of oxygen therapy — improvement in color, alertness, and breathing pattern.
Maintain Humidification (If Required)
- Use sterile water humidifiers with nasal cannula or mask when flow is >4 L/min.
- Check water level regularly and change humidifier daily.
- Prevent mucosal dryness, crusting, and nosebleeds.
- Educate on humidification use at home if on long-term oxygen.
Ensure Safety Measures
- Post “Oxygen in Use – No Smoking” signage near the bed.
- Keep flammable materials (oil, alcohol, aerosol sprays) away from the oxygen source.
- Ensure electrical equipment is grounded properly.
- Never use petroleum jelly or oil-based lotions near nasal prongs.
- Store oxygen cylinders upright and secure them to prevent falling.
Documentation
- Record in nurse’s notes:
- Date and time oxygen started
- Device used and flow rate
- SpO₂ values before and after initiation
- Patient’s response (improvement or complications)
- Any education provided to the patient/family
Educate the Patient and Family
- Explain the purpose and importance of oxygen therapy.
- Instruct them not to adjust the flow rate or remove the device.
- Teach safety precautions (no smoking, proper storage).
- Demonstrate proper cleaning of nasal cannula/mask at home.
- Reinforce the importance of medication compliance, hydration, and regular follow-ups.
e) National immunization schedule
The National Immunization Schedule (NIS) is a government-approved plan under the Universal Immunization Programme (UIP) that provides free vaccines to protect children, pregnant women, and infants from vaccine-preventable diseases.
For pregnant women
| Age / Timing | Vaccine | Dose | Route | Site |
|---|---|---|---|---|
| Early in pregnancy | TT1 or Td1 | 0.5 mL | IM | Upper Arm |
| 4 weeks after TT1 | TT2 or Td2 | 0.5 mL | IM | Upper Arm |
| If previously vaccinated within 3 years | Booster | 0.5 mL | IM | Upper Arm |
For Infants (Birth to 1 Year)
| Age | Vaccine | Dose | Route | Site |
|---|---|---|---|---|
| At Birth | BCG | 0.05 mL | ID | Left Upper Arm |
| Hepatitis B Birth Dose | 0.5 mL | IM | Anterolateral thigh | |
| OPV 0 (Oral Polio) | 2 drops | Oral | Oral | |
| 6 Weeks | Pentavalent-1 (DPT + Hep B + Hib) | 0.5 mL | IM | Anterolateral thigh |
| OPV-1 | 2 drops | Oral | Oral | |
| Rotavirus-1 | 5 drops | Oral | Oral | |
| PCV-1 (Pneumococcal) | 0.5 mL | IM | Anterolateral thigh | |
| 10 Weeks | Pentavalent-2 | 0.5 mL | IM | Anterolateral thigh |
| OPV-2 | 2 drops | Oral | Oral | |
| Rotavirus-2 | 5 drops | Oral | Oral | |
| 14 Weeks | Pentavalent-3 | 0.5 mL | IM | Anterolateral thigh |
| OPV-3 | 2 drops | Oral | Oral | |
| Rotavirus-3 | 5 drops | Oral | Oral | |
| PCV-2 | 0.5 mL | IM | Anterolateral thigh | |
| 9–12 Months | Measles-Rubella (MR-1) | 0.5 mL | SC | Right upper arm |
| JE-1 (in endemic areas) | 0.5 mL | SC | Left upper arm | |
| Vitamin A (1st dose) | 1 mL | Oral | Oral |
For Children (16–24 months)
| Age | Vaccine | Dose | Route | Site |
|---|---|---|---|---|
| 16–24 months | DPT Booster-1 | 0.5 mL | IM | Anterolateral thigh |
| OPV Booster | 2 drops | Oral | Oral | |
| MR-2 | 0.5 mL | SC | Right upper arm | |
| JE-2 (in endemic areas) | 0.5 mL | SC | Left upper arm | |
| Vitamin A (2nd to 9th dose) every 6 months | 2 mL | Oral | Oral |
For Children (5–6 years)
| Age | Vaccine | Dose | Route | Site |
|---|---|---|---|---|
| 5–6 years | DPT Booster-2 | 0.5 mL | IM | Upper Arm |
For Adolescents (10 & 16 years)
| Age | Vaccine | Dose | Route | Site |
|---|---|---|---|---|
| 10 years | Td | 0.5 mL | IM | Upper Arm |
| 16 years | Td | 0.5 mL | IM | Upper Arm |
Q-6-Short answer question (any four) 4×2=8
a) Define protein energy malnutrition
Protein Energy Malnutrition (PEM) is a form of undernutrition that occurs due to a deficiency of both protein and calories, commonly seen in infants and young children, leading to growth failure, muscle wasting, weight loss, and increased susceptibility to infections. It includes mainly two conditions : Kwashiorkor and Marasmus
b) Draw symbol of under-five clinic
c) Explain mode of heat loss in newborn baby
Newborns lose body heat quickly due to large surface area, thin skin, and limited fat stores. There are four main modes of heat loss:
Evaporation
Loss of heat as water evaporates from the skin surface.
Example : After birth when the baby is wet with amniotic fluid.
Conduction
Direct transfer of heat from the newborn to a cooler solid surface.
Example : Placing the baby on a cold weighing scale or mattress.
Convection
Loss of heat to surrounding air when air currents pass over the baby.
Example : Exposure to fans, open windows, or air conditioning.
Radiation
Loss of heat to nearby cooler objects without direct contact.
Example : Being near a cold wall or window
d) Define weaning
Weaning is the gradual process of introducing semi-solid and solid foods to an infant’s diet while reducing and eventually stopping breastfeeding or formula feeding. It typically begins around 6 months of age, when breast milk alone is no longer sufficient to meet the baby’s growing nutritional needs.
e) Discuss John’s criteria used for diagnosis of rheumatic heart disease
Major Criteria
- Carditis (clinical or subclinical – including valvulitis)
- Polyarthritis (migratory, large joints)
- Chorea (Sydenham’s chorea – involuntary movements)
- Erythema marginatum (non-itchy pink rings on trunk & limbs)
- Subcutaneous nodules (painless, firm swellings on extensor surfaces)
Minor Criteria
- Fever
- Arthralgia (joint pain)
- Elevated ESR/CRP (inflammatory markers)
- Prolonged PR interval on ECG
Diagnosis Requires
2 Major Criteria
OR
1 Major + 2 Minor Criteria
f) Explain concept of atraumatic care in children
Atraumatic care is a philosophy of pediatric nursing that aims to minimize or eliminate physical and psychological distress experienced by children and their families during healthcare procedures and hospitalization. It focuses on providing care that reduces pain, fear, separation anxiety, and promotes a child-friendly environment, using strategies like distraction techniques, parental presence, and age-appropriate communication.
