AHN-2025 (done)-Juhi-UPLOAD-MCQ PENDING-PAPER SOLUTION NO.2
ADULT HEALTH NURSING-PAPER SOLUTION NO.2
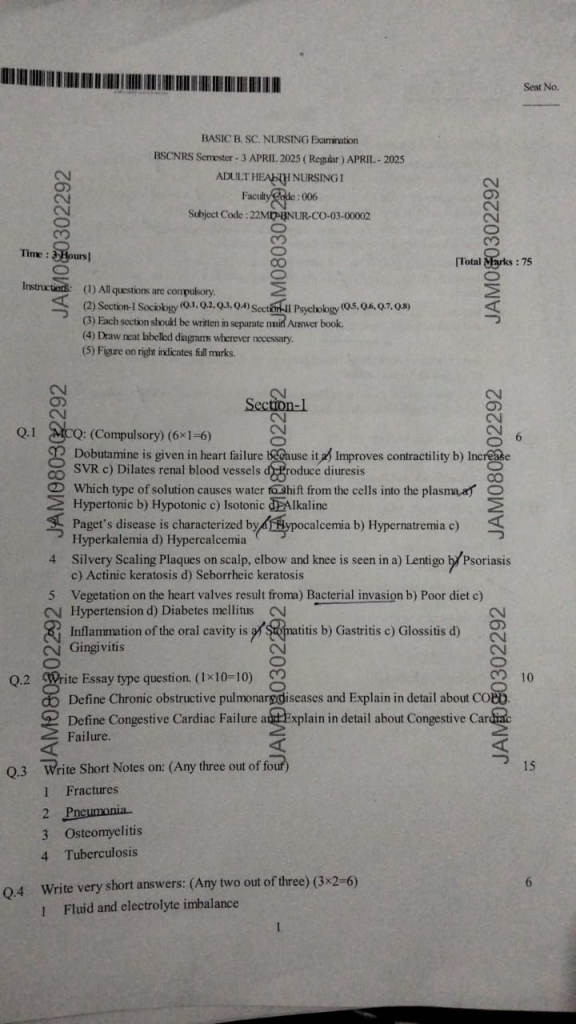
Section-1
Q:1 (Compulsory) (6×1=6)
1.Dobutamine is given in heart failure because it
a) Improves contractility
b) Increase SVR
c) Dilates renal blood vessels
d) produce diuresis
2.Which type of solution causes water shift from the cells into the plasma,
a)Hypertonic
b) Hypotonic
c) Isotonic
d) Alkaline
3.Paget’s disease is characterized by
a) Hypocalcemia
b) Hypernatremia
c) Hyperkalemia
d) Hypercalcemia
4.Silvery Scaling Plaques on scalp, elbow and knee is seen in
a) Lentigo
b) Psoriasis
c) Actinic keratosis
d) Seborrheic keratosis
5.Vegetation on the heart valves result from
a) Bacterial invasion
b) Poor diet
c) Hypertension
d) Diabetes mellitus
6. Inflammation of the oral cavity is of
a)Stomatitis
b) Gastritis
c) Glossitis
d) Gingivitis
Q.2 Write Essay type question. (1×10=10)
1.Define Chronic obstructive pulmonary diseases and Explain in detail about COPD
Definition
COPD is a progressive and irreversible lung disease characterized by chronic airflow limitation due to inflammation and structural changes in the airways and alveoli. It includes chronic bronchitis and emphysema.
Etiology
• Smoking (most common cause)
• Air pollutionOccupational dusts and chemicals
• Genetic factors (e.g., α1-antitrypsin deficiency)
• Recurrent respiratory infections
• Indoor air pollution (biomass fuel exposure)
Pathophysiology
Chronic exposure to irritants (e.g., cigarette smoke)
→ Leads to chronic inflammation in the airways and alveoli
→Causes mucus hypersecretion, airway narrowing, and fibrosis
→Destruction of alveolar walls (emphysema) and loss of elasticity
→ Results in air trapping and lung hyperinflation
→ Causes ventilation-perfusion mismatch, hypoxia, and hypercapnia
→Chronic hypoxia → pulmonary hypertension → cor pulmonale
Clinical Manifestations
• Chronic cough
• Sputum production
• Progressive dyspnea
• Wheezing
• Barrel-shaped chest (in emphysema)
• Cyanosis
• Clubbing (late stage)
• Use of accessory muscles
• Fatigue
• Weight loss
Diagnostic evaluation :
• History collection
• Physical examination
• Pulmonary function test
• Chest X-ray
• CT scan
• Alpha 1 antitrypsin level
• ABG analysis
• CBC
Medical Management
1. Bronchodilators :
Beta-agonists : Salbutamol, Formoterol
Anticholinergics : Ipratropium, Tiotropium
Methylxanthines : Theophylline
2. Corticosteroids :
Inhaled : Budesonide, Fluticasone
Oral (during exacerbation) : Prednisolone
3. Antibiotics :
During infections/exacerbations
4. Oxygen Therapy :
• Low-flow O₂ to maintain SaO₂ ~ 90%
• Avoid high O₂ in CO₂ retainers
5. Pulmonary Rehabilitation :
• Exercise training
• Breathing techniques (pursed-lip)
6. Vaccination :
Influenza and Pneumococcal vaccines
7. Smoking Cessation :
Surgical Management
• For Advanced COPD
• Lung Volume Reduction Surgery (LVRS)
• Bullectomy
• Lung Transplantation
Nursing management
Impaired Gas Exchange related to alveolar-capillary membrane changes and airflow limitation
Goal : Patient will maintain optimal gas exchange
Nursing Interventions :
• Monitor respiratory rate, depth, and SpO₂ regularly
• Administer supplemental oxygen as prescribed (low-flow if CO₂ retainer)
• Position patient in high Fowler’s or tripod position to facilitate lung expansion
• Teach pursed-lip breathing and diaphragmatic breathing
• Encourage incentive spirometry use
• Assess for cyanosis, restlessness, confusion (signs of hypoxia)
Ineffective Airway Clearance related to excessive mucus production and weak cough effort
Goal : Patient will maintain a clear airway with effective cough and normal breath sounds.
Nursing Interventions :
• Encourage fluid intake (if not contraindicated) to thin secretions
• Provide chest physiotherapy and postural drainage as indicated
• Encourage coughing and deep breathing exercisesSuction airway if necessary (esp. in acute phase)
• Administer expectorants or bronchodilators as ordered
Activity Intolerance related to imbalance between oxygen supply and demand
Goal : Patient will perform activities of daily living (ADLs) without excessive fatigue or dyspnea.
Nursing Interventions :
• Assess tolerance to activity and fatigue level
• Plan activities with rest periods
• Provide assistance with ADLs as needed
• Educate energy conservation techniques
• Administer medications like bronchodilators prior to activities
Anxiety related to breathlessness and fear of suffocation
Goal : Patient will verbalize reduced anxiety and demonstrate relaxation techniques.
Nursing Interventions :
• Stay with patient during episodes of breathlessnessUse calm, reassuring Communication
• Teach relaxation techniques (e.g., guided imagery, controlled breathing)
• Encourage expression of fears
• Avoid sudden changes in care or routine
2.Define Congestive Cardiac Failure and Explain in detail about Congestive Cardiac Failure.
Definition :
Congestive Cardiac Failure is a clinical condition in which the heart is unable to pump sufficient blood to meet the metabolic needs of the body, leading to a backup (congestion) of blood in the lungs, liver, abdomen, and lower extremities.
Causes :
Coronary Artery Disease (CAD)
Hypertension (High BP)
Myocardial Infarction (Heart Attack)
Cardiomyopathy
Valvular Heart Disease
Arrhythmias
Congenital Heart Defects
Thyroid Disorders
Severe Anemia
Infections
Pathophysiology :
→↓ Pumping efficiency of the heart
→↓ Cardiac output
→ ↓ Perfusion to tissues
→Neurohormonal activation (RAAS, SNS)
→Vasoconstriction + Fluid retention, Fluid overload
→Pulmonary & systemic congestion
→Pulmonary edema or peripheral edema depending on side involved
Clinical Manifestations :
Left-sided Failure :
• Dyspnea on exertion
• Orthopnea
• Paroxysmal nocturnal dyspnea (PND)
• Cough
• Crackles in lungs
• Fatigue
Right-sided Failure:
• Pedal edema
• Ascites
• Hepatomegaly
• Jugular vein distention (JVD)
• Weight gain
Diagnostic Evaluation :
• Blood tests: BNP, CBC, renal function, electrolytes
• ECG: To detect MI, arrhythmias
• Echocardiography: To assess EF (<40% = systolic failure)
• Chest X-ray : Pulmonary congestion, cardiomegaly
• Cardiac catheterization or stress test
Nursing management
Decreased Cardiac Output related to impaired myocardial contractility or altered heart rhythm as evidenced by hypotension, oliguria
Nursing Interventions:
• Monitor heart rate, BP, ECG, and peripheral pulses regularly
• Administer medications like digoxin, beta-blockers, and ACE inhibitors as prescribed
• Monitor for signs of decreased tissue perfusion (cold extremities, confusion)
• Keep patient in semi-Fowler’s position to reduce preload
Excess Fluid Volume related to compromised regulatory mechanism, sodium and water retention as evidenced by edema, weight gain
Nursing Interventions :
• Monitor daily weight and I/O strictly
• Assess for edema and lung sounds regularly
• Administer diuretics (e.g., furosemide) as Prescribed
• Educate on sodium/fluid restriction
Impaired Gas ExchangeRelated to: alveolar-capillary membrane changes, pulmonary congestion as evidenced by restlessness, hypoxia, dyspnea, abnormal ABGs
Nursing Interventions:
• Monitor respiratory rate, rhythm, and SpO₂
• Administer oxygen therapy as prescribed
• Position patient in high Fowler’s to enhance lung expansion
• Encourage coughing and deep breathing
Activity Intolerance related to imbalance between oxygen supply and Demand as evidenced by fatigue, dyspnea on exertion
Nursing Interventions:
• Plan rest periods between activities
• Assist with ADLs as needed
• Monitor response (pulse, BP, SpO₂) to activity
• Encourage gradual increase in physical activity
Q.3 Write Short Notes on: (Any three out of four) 15
1 Fractures
Definition :
A fracture is a break or crack in a bone. It occurs when the bone is subjected to stress greater than it can absorb, often from trauma, overuse, or conditions that weaken the bone (like osteoporosis)
Types of fracture :
Closed (simple) fracture :
The bone breaks but the skin remains intact.
Open (compound) fracture :
The broken bone pierces through the skin, increasing infection risk.
Transverse fracture :
A horizontal break across the bone.
Oblique fracture :
A diagonal break across the bone.
Spiral fracture :
A break that twists around the bone, often from a rotating force.
Comminuted fracture :
The bone is shattered into three or more pieces.
Segmental fracture :
Two fractures occur in the same bone, creating a segment between breaks.
Greenstick fracture :
Incomplete fracture where the bone bends (common in children).
Compression fracture :
Bone is crushed (often in the spine).
Avulsion fracture :
A fragment of bone is pulled off by a tendon or ligament.
Clinical manifestations:
• Sudden pain
• Swelling and bruising
• Deformity
• Inability to move or bear weight
• Crepitus (grating sound)
Diagnostic evaluation :
• History collection
• Physical examination
• X-rays (most common)
• CT scan or MRI
Treatment :
• Immobilization : Casts, splints, or braces
• Reduction : Realignment of the bone (closed or surgical)
• Surgery : For severe or displaced fractures (using plates, screws, or rods)
• Rehabilitation : Physical therapy to restore function
2 Pneumonia
Pneumonia is a serious inflammatory condition of the lung parenchyma, particularly affecting the alveoli, in which the air sacs become filled with fluid, pus, and cellular debris due to infection by bacteria, viruses, fungi, or aspiration. This leads to impaired gas exchange and difficulty in breathing.
Etiology
Infectious Causes :
Bacteria : Streptococcus pneumoniae (most common), Staphylococcus aureus, Klebsiella pneumoniae
Viruses : Influenza virus, Respiratory syncytial virus (RSV), COVID-19
Fungi : Histoplasma, Aspergillus (especially in immunocompromised)
Inhalation pneumonia
Inhalation of gastric contents, food, or vomitus, especially in unconscious or elderly patients.
Other Risk Factors :
• Smoking
• Chronic diseases (COPD, diabetes)
• Immunocompromised states (HIV/AIDS, chemotherapy)
• Advanced age
• Hospitalization or ventilator use (nosocomial pneumonia)
Clinical manifestations
• Fever and chills
• Productive cough with yellow or green sputum
• Dyspnea (shortness of breath)
• Pleuritic chest pain (pain on deep inspiration)
• Fatigue and malaise
• Crackles/rales on auscultation
• Tachypnea (rapid breathing)
• Cyanosis in severe cases
Diagnostic Evaluation :
• Chest X-ray
• Sputum culture and sensitivity
• CBC
• Pulse oximetry
• ABG analysis
• Blood culture
Medical Management :
Antibiotics :
Based on causative organism (e.g., Amoxicillin, Ceftriaxone)
Antivirals :
For viral causes (e.g., Oseltamivir for influenza)
Antifungals :
If fungal pneumonia is diagnosed (e.g., Amphotericin B)
Supportive therapy :
• Antipyretics (for fever)
• Oxygen therapy (for hypoxia)
• IV fluids (for dehydration)
• Bronchodilators (to ease breathing if bronchospasm is present)
Nursing Management :
• Monitor vital signs, oxygen saturation, and respiratory rate
• Administer medications as prescribed
• Encourage fluid intake (if not contraindicated)
• Promote rest and gradually increase activity
• Encourage deep breathing and coughing exercises
• Perform chest physiotherapy (if ordered)
• Educate patient on completing antibiotic course
• Provide emotional support
3 Osteomyelitis
Definition :
Osteomyelitis is an infection of the bone, typically caused by bacteria such as Staphylococcus aureus. The infection can reach the bone through the bloodstream, from nearby infected tissue, or directly through an open fracture or surgical procedure.
Etiology :
• Bacterial infections (e.g.Staphylococcus aureus)
• Fungal infections
• Spread from nearby infections
• Open fractures or surgical procedures
• Poor blood circulation
Clinical manifestations :
• Localized bone pain
• Swelling
• Redness and warmth over the affected area
• Fever and chills
• Fatigue
• Restricted movement of the affected limb
Types of osteomyelitis :
Acute Osteomyelitis :
Develops rapidly; more common in children.
Chronic Osteomyelitis :
Develops over time; may follow inadequate treatment of acute cases
Treatment :
• Prolonged antibiotic therapy (oral or intravenous)
• Surgical debridement to remove infected bone tissue
• Management of underlying conditions (e.g., diabetes)
• Pain management and supportive care
Nursing management :
• Monitor vital signs and signs of infection.
• Reposition the patient regularly and use supportive devices to avoid skin breakdown.
• Promote gentle exercises as tolerated to prevent joint stiffness and muscle atrophy.
• Perform regular dressing changes using aseptic techniques to prevent contamination.
• Administer prescribed antibiotics and pain medications.
• Educate the patient on medication adherence and wound care.
• Educate on symptoms that require immediate medical attention, such as increased pain or fever.
• Encourage adequate nutrition to promote healing
• Coordinate with the healthcare team for surgical interventions if necessary
4 Tuberculosis
Definition :
Tuberculosis (TB) is an infectious disease usually caused by Mycobacterium tuberculosis bacteria. It primarily affects the lungs (pulmonary TB) but can also affect other parts of the body (extrapulmonary TB)
Transmission :
Airborne droplets from coughing, sneezing, or talking by an infected person
Risk factors :
• HIV / AIDS
• Malnutrition
• Diabetes mellitus
• Smoking
• Close contact with tb patient
• Immunosuppressive therapy
Clinical manifestations :
• Persistent cough (lasting more than 2–3 weeks)
• Coughing up blood (hemoptysis)
• Chest pain, especially when breathing or coughing
• Shortness of breath
• Fatigue and weakness
• Low grade fever (especially in the evening)
• Night sweats (profuse sweating at night)
• Loss of appetite
• Weight loss
Diagnostic evaluation :
• History collection
• Physical examination
• Chest X-ray
• Mantoux test (Tuberculin skin test)
• CBNAAT / GeneXpert test
• Interferon-gamma release assay (IGRA)
• ESR, CBC, LFT as supportive
Management :
The cornerstone of TB treatment is anti-tubercular therapy (ATT), which includes a combination of drugs to prevent resistance and ensure eradication of the infection.
Intensive Phase (First 2 months) :
– Daily HRZE (Isoniazid, Rifampicin, Pyrazinamide, Ethambutol)
Continuation Phase (Next 4 months) :
– Daily HR (Isoniazid, Rifampicin)
Total Duration : 6 months (for drug-sensitive TB)
Treatment should be directly observed (DOTS) to ensure compliance.
Nursing management :
• Encourage deep breathing, coughing, and positioning (high Fowler’s)
• Administer bronchodilators/expectorants as prescribed
• Administer anti-TB drugs (RIPE regimen) as per schedule
• Monitor for side effects: hepatotoxicity, neuropathy, optic issues
• Educate about importance of adherence to full course (6–9 months)
• Supervise therapy under DOTS (Directly Observed Treatment Short-course)
• Isolate patient in a well-ventilated room
• Educate on respiratory hygiene – cough into tissues, wear masks
• Educate family on TB transmission prevention
• Encourage high-protein, high-calorie diet
• Supplement with vitamins, especially B6 with INH
• Small frequent meals and fluids
• Monitor weight regularly
Q.4 Write very short answers: (Any two out of three) (3×2=6)
1 Fluid and electrolyte imbalance
Definition :
Fluid and electrolyte imbalance refers to any disturbance in the normal levels of body fluids or electrolytes (like sodium, potassium, calcium, etc.) leading to disruption of homeostasis.
Causes :
• Vomiting
• Diarrhea
• Bleeding
• Kidney failure
• Burns
• Fever
• Diuretics
• Dehydration
• Overhydration
Types :
Fluid Imbalance :
Dehydration (hypovolemia) Overhydration (hypervolemia)
Electrolyte Imbalance :
Hyponatremia / Hypernatremia
Hypokalemia / Hyperkalemia
Hypocalcemia / Hypercalcemia
Symptoms :
• Weakness
• Fatigue
• Muscle cramps
• Confusion
• Low BP
• Irregular heartbeat
Management :
• Correct the underlying cause
• IV fluids or electrolyte replacement
• Monitor vital signs, ECG, and lab values
2 Anesthesia
Definition :
Anesthesia is a controlled, medically induced loss of sensation or awareness, used during surgical, diagnostic, or therapeutic procedures to eliminate pain and discomfort. It may involve partial or complete unconsciousness, depending on the type used.
Types of Anesthesia :
General Anesthesia
• Induces complete unconsciousness.
• Used in major surgeries.
• Agents : Propofol, Halothane.
Regional Anesthesia
• Blocks sensation in a specific region.
Examples : Spinal, Epidural, Nerve blocks.
Local Anesthesia
• Numbs a small area.
• Used in minor procedures (e.g., dental work)
• Agents : Lignocaine, Bupivacaine.
• Conscious Sedation (Moderate Sedation)
• Patient is awake but relaxed.
• Used in procedures like endoscopy.
Indications :
• During surgical operations to prevent pain
• In diagnostic procedures (e.g., colonoscopy)
• For muscle relaxation
• For anxiety relief before invasive procedures
Nursing Responsibilities :
• Preoperative assessment (NPO, allergies, consent)
• Monitoring vitals during and after anesthesia
• Ensuring airway patency
• Observing for any adverse reactions
• Patient education on pre and post-operative care
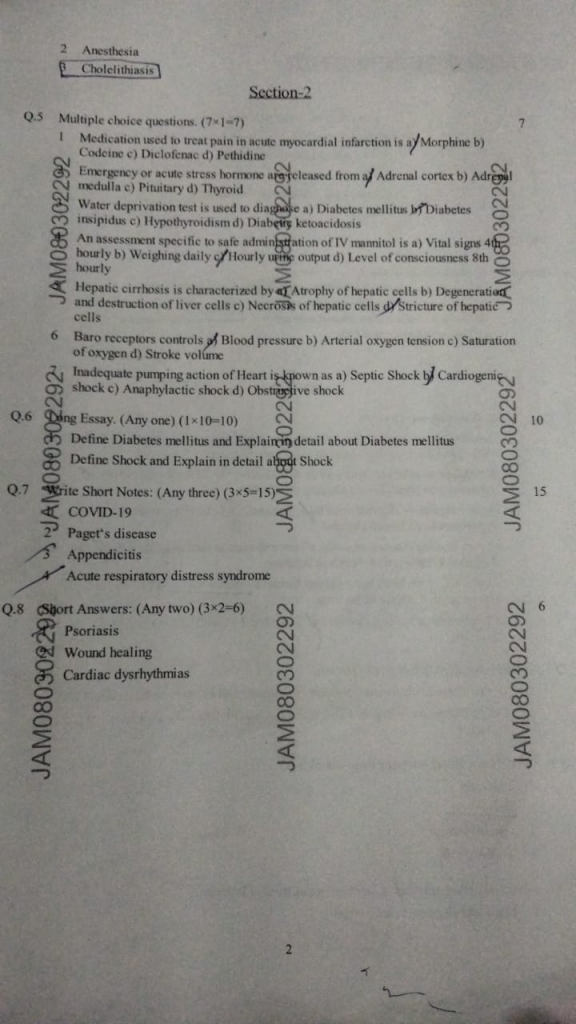
3.Cholelithiasis
Definition :
Cholelithiasis refers to the formation of gallstones in the gallbladder, which are hardened deposits of bile components like cholesterol or bilirubin.
Causes or Risk Factors :
• Female, Fat, Fertile, Forty (4 F’s)
• Obesity or rapid weight loss
• High-fat, low-fiber diet
• Diabetes
• Liver disease
• Pregnancy
• Oral contraceptives
Clinical manifestations :
• Right upper quadrant (RUQ) abdominal pain (biliary colic)
• Nausea, vomiting
• Indigestion after fatty meals
• Jaundice (if bile duct is blocked)
Diagnosis :
• Ultrasound (gold standard)
• LFTs, CBC,
• Abdominal X-ray
• CT scan
Management :
• Cholecystectomy (surgical removal of gallbladder)
• ERCP if stones are in the bile ductPain relief, dietary changes (low-fat diet)
Section-2
Q.5 Multiple choice questions. (7×1=7)
1. Medication used to treat pain in acute myocardial infarction is
a) Morphine
b) Codeine
c) Diclofenac
d) Pethidine
2. Emergency or acute stress hormone are released from
a) Adrenal cortex
b) Adrenal medulla
c) Pituitary
d) Thyroid
3.Water deprivation test is used to diagnose
a) Diabetes mellitus
b) Diabetes insipidus
c) Hypothyroidism
d) Diabętę ketoacidosis
4. An assessment specific to safe administration of IV mannitol is
a) Vital signs 4th hourly
b) Weighing daily
c) Hourly urine output
d) Level of consciousness 8th hourly
5. Hepatic cirrhosis is characterized by
a) Atrophy of hepatic cells
b) Degeneration and destruction of liver cells
c) Necrosis of hepatic cells
d) Stricture of hepatic cells
6. Baro receptors controls
a) Blood pressure
b) Arterial oxygen tension
c) Saturation of oxygen
d) Stroke volume
7.Inadequate pumping action of Heart is known as
a) Septic Shock
b) shock Cardiogenig
c) Anaphylactic shock
d) Obstructive shock
Q.6 Ding Essay. (Any one) (1×10=10)
1.Define Diabetes mellitus and Explainen detail about Diabetes mellitus
Diabetes mellitus is a chronic metabolic condition characterized by high levels of glucose (sugar) in the blood due to the body’s inability to produce enough insulin or effectively use the insulin it produces.
Types of Diabetes Mellitus
Type 1 Diabetes Mellitus (T1DM)
Also known as Insulin-Dependent Diabetes Mellitus (IDDM)
Caused by autoimmune destruction of beta cells in pancreas
Common in children and adolescents
Requires lifelong insulin therapy
Sudden onset with symptoms like polyuria, polydipsia, and weight loss
Type 2 Diabetes Mellitus (T2DM)
Also known as Non-Insulin Dependent Diabetes Mellitus (NIDDM)
Caused by insulin resistance and relative insulin deficiency
Common in adults, especially with obesity and sedentary lifestyle
Can be managed with diet, exercise, oral hypoglycemics, and sometimes insulin
Gradual onset
Gestational Diabetes Mellitus (GDM)
Diabetes occurring during pregnancy
Caused by hormonal changes leading to insulin resistance
Usually detected in 2nd or 3rd trimester
Resolves after delivery but increases risk of Type 2 DM later
Maturity-Onset Diabetes of the Young (MODY)
A rare genetic form of diabetes (monogenic)
Onset before 25 years of age
Caused by a defect in insulin production
Inherited in an autosomal dominant pattern
Secondary Diabetes Mellitus
Caused by other medical conditions or medications, such as:
Pancreatitis
Cushing’s syndrome
Steroid use
Endocrine tumors
Latent Autoimmune Diabetes in Adults (LADA)
A slow-progressing form of autoimmune diabetes
Occurs in adults (usually >30 years)
Initially appears like Type 2, but later requires insulin like Type 1
Clinical manifestation
Polyuria – Frequent urination
Polydipsia – Increased thirst
Polyphagia – Increased hunger
Unexplained weight loss (more common in type 1)
Fatigue – Feeling unusually tired
Blurred vision
Slow healing of wounds or infections
Dry skin and itchy skin
Numbness or tingling in hands or feet (neuropathy)
Diagnostic evaluation
History collection
Physical examination
Fasting blood sugar
Random blood sugar
Oral glucose tolerance test
HbA1c (glycated hemoglobin)
Urine test (glycosuria, ketonuria)
Management
Medications :
Type 1 DM :
Requires lifelong insulin therapy (short-acting, long-acting)
Type 2 DM :
Oral hypoglycemic agents (OHAs):
Metformin, Sulfonylureas, DPP-4 inhibitors, SGLT2 inhibitors
Insulin may be needed in advanced cases
Dietary Management :
Follow a diabetic diet – low in sugar and refined carbohydrates
Include high-fiber foods (whole grains, vegetables)
Maintain regular meal times to avoid glucose fluctuations
Avoid alcohol and sugary drinks
Physical Activity :
Engage in regular exercise (30–45 minutes daily)
Helps improve insulin sensitivity and control weight
Encouraged under medical guidance for Type 1 DM
Blood Glucose Monitoring :
Self-monitoring using glucometer
Monitor HbA1c every 3 months to assess long-term control
Track patterns to adjust treatment
Education & Lifestyle Modification :
Teach about signs of hypo- and hyperglycemia
Stress importance of adherence to treatment
Educate on foot care to prevent ulcers
Quit smoking and limit alcohol intake
Nursing management
Imbalanced nutrition less than body requirements related to inability to metabolize glucose as evidenced by weight loss, fatigue, polyphagia.
Goal : Patient will maintain adequate nutritional intake to meet metabolic needs.
Nursing Interventions :
Assess dietary history and daily calorie intake.
Collaborate with a dietician to formulate a diabetic diet plan.
Encourage small, frequent meals rich in complex carbohydrates and fiber.
Monitor blood glucose levels regularly before and after meals.
Educate patient on carbohydrate counting and glycemic index.
Risk for unstable blood glucose level related to inadequate insulin production or use, inappropriate diet, or physical activity pattern.
Goal : Maintain blood glucose within target range (70–130 mg/dL fasting).
Nursing Interventions :
Monitor capillary blood glucose as per schedule.
Administer insulin/oral hypoglycemics as prescribed.
Teach the patient how to self-monitor blood glucose.
Identify and avoid factors that cause hypo-/hyperglycemia.
Encourage regular physical activity and adherence to medication.
Deficient knowledge related to new diagnosis of diabetes mellitus as evidenced by frequent questions, non-adherence to diet or medication
Goal : Patient will verbalize understanding of disease process and management plan.
Nursing Interventions :
Provide individualized teaching about pathophysiology of diabetes.
Explain importance of blood glucose monitoring and insulin therapy.
Teach signs and symptoms of hypoglycemia and hyperglycemia.
Provide written materials and videos for reinforcement.
Encourage patient to participate in diabetes education classes.
Risk for infection related to hyperglycemia, impaired immune response, and poor wound healing.
Goal : Patient will remain free from infection during hospitalization.
Nursing Interventions :
Monitor for signs of infection (e.g., redness, fever, discharge).
Perform and teach proper foot care techniques.
Maintain skin hygiene and dry between toes.
Educate patient to avoid walking barefoot.
Ensure aseptic techniques during procedures and injections.
2.Define Shock and Explain in detail about Shock
Definition :
Shock is a life-threatening medical condition in which there is inadequate blood flow and oxygen delivery to the tissues and organs, resulting in cellular dysfunction, organ failure, and potentially death.
Types of Shock :
Shock can be classified into different types based on the underlying cause. The major types are :
1. Hypovolemic Shock
This occurs due to loss of blood or fluid volume from the body. It results in decreased venous return, reduced cardiac output, and inadequate tissue perfusion.
Causes : Hemorrhage, dehydration, burns, vomiting, diarrhea, or trauma.
2. Cardiogenic Shock
This type results from the failure of the heart to pump effectively, leading to reduced cardiac output and poor perfusion of tissues.
Causes : Myocardial infarction (heart attack), severe heart failure, arrhythmias, or cardiomyopathy.
3. Septic Shock
This occurs due to a severe systemic infection, usually caused by bacteria. It leads to widespread vasodilation, capillary leak, and hypotension.
Causes : Bloodstream infections, pneumonia, urinary tract infections, abdominal infections.
4. Neurogenic Shock
This type of shock is caused by loss of sympathetic tone, resulting in widespread vasodilation and pooling of blood in the periphery.
Causes : Spinal cord injury, head trauma, or spinal anesthesia.
5. Anaphylactic Shock
It is a severe allergic reaction leading to the release of histamines and other chemicals, causing vasodilation, bronchoconstriction, and hypotension.
Causes : Allergies to foods, insect stings, medications, or latex.
6. Obstructive Shock
This type occurs when there is a physical obstruction to blood flow in or out of the heart.
Causes : Pulmonary embolism, cardiac tamponade, tension pneumothorax, or aortic stenosis.
Clinical manifestations :
• Hypotension
• Tachycardia
• Weak pulse
• Tachypnea
• Shallow breathing
• Confusion
• Restlessness
• Cold, clammy, pale skin.
• Oliguria (<30 mL/hr)
• Altered temperature (high in sepsis, low in others)
Management :
Its management involves rapid identification, supporting vital functions, and treating the underlying cause.
1. Initial Assessment and Stabilization :
• Ensure Airway, Breathing, and Circulation (ABC) are maintained.
• Place the patient in Trendelenburg position (if not contraindicated) to improve perfusion.
• Provide high-flow oxygen to improve tissue oxygenation.
• Establish IV access with large-bore cannula for rapid fluid or drug administration.
• Monitor vital signs continuously (BP, HR, RR, O2 saturation, temperature).
2. Fluid Resuscitation :
• Crystalloids (e.g., Normal Saline or Ringer’s Lactate) are administered rapidly to restore intravascular volume.
• Colloids (e.g., albumin) may be used in some cases.
• Blood transfusion is needed in hypovolemic shock due to hemorrhage.
3. Medication Support :
• Vasopressors (e.g., norepinephrine, dopamine) to raise blood pressure if fluids are inadequate.
• Inotropes (e.g., dobutamine) to improve heart contractility in cardiogenic shock.
• Antibiotics (broad-spectrum) started early in septic shock after cultures.
• Epinephrine for anaphylactic shock.
• Corticosteroids in anaphylactic or septic shock if needed.
4. Oxygenation and Ventilation :
• Administer supplemental oxygen.
• Mechanical ventilation may be required if respiratory failure develops.
5. Identify and Treat Underlying Cause :
• Stop hemorrhage (surgery, pressure dressing).
• Treat infection (antibiotics, drainage of abscess).
• Remove allergen (stop drug, remove sting).
• Relieve obstruction (e.g., needle decompression for pneumothorax, thrombolysis for PE).
Nursing management :
1. Ineffective Tissue Perfusion
Goal : Improve tissue oxygenation and perfusion
Interventions :
• Monitor BP, pulse pressure
• MAP (target MAP ≥ 65 mmHg)
• Assess capillary refill, skin temperature & color
• Administer IV fluids, blood products as prescribed
• Monitor urine output hourly
• Provide oxygen therapy as needed
2. Decreased Cardiac Output
Goal : Support heart function and improve circulation
Interventions :
• Monitor ECG, HR, rhythm, and cardiac enzymes
• Administer inotropes or vasopressors (e.g., dopamine, norepinephrine)
• Maintain fluid balance (avoid overload in cardiogenic shock)
• Monitor CVP or PAP if available
3. Risk for Fluid Volume Deficit
Goal : Restore and maintain adequate fluid volume
Interventions :
• Insert 2 large-bore IVs for fluid access
• Administer crystalloids (NS, RL) and/or blood transfusionAssess for signs of fluid overload (edema, crackles)
• Document intake and output strictly
4. Impaired Gas Exchange
Goal : Maintain adequate oxygenation and ventilation
Interventions :
• Administer supplemental oxygen (nasal cannula, mask)
• Monitor SpO₂, ABG
• Position in semi-Fowler’s unless contraindicated
• Prepare for intubation and mechanical ventilation if required
5. Risk for Impaired Skin Integrity
Goal : Maintain skin integrity and prevent pressure ulcers
Interventions :
• Reposition every 2 hours
• Keep skin clean and dry
• Use pressure-relieving devices
• Assess skin regularly for breakdown or color changes
Q.7 Crite Short Notes: (Any three) (3×5=15)
1.COVID-19
Definition :
COVID-19 is an infectious disease caused by the novel coronavirus SARS-CoV-2, first identified in Wuhan, China, in December 2019.It primarily affects the respiratory system, but can also involve multiple organs including the heart, kidneys, and nervous system.
Causative Agent :
SARS-CoV-2 – a single-stranded RNA virus from the coronavirus family
Mode of Transmission :
• Droplet transmission
• Aerosol (airborne)
• Contact with contaminated surfaces
• Entry through nose, mouth, or eyes
Clinical Manifestations :
Vary from asymptomatic to severe disease.
Common Symptoms :
• Fever
• Dry cough
• Fatigue
• Loss of taste/smell
• Sore throat
• Shortness of breath
• Muscle aches
Severe Symptoms :
• Difficulty breathing
• Chest pain
• Confusion
• Cyanosis (blue lips/face)
Diagnostic Evaluation :
• RT-PCR test
• Rapid antigen test
• Antibody test
• Blood tests : CRP, D-dimer, ferritin, lymphopenia
• Chest X-ray
Medical Management :
Antiviral Therapy : Remdesivir Molnupiravir
Supportive Therapy :
• Oxygen therapy (nasal cannula, mask, ventilator if needed)
• Antipyretics (e.g., paracetamol)
• Corticosteroids (e.g., dexamethasone)
• Anticoagulants (e.g., enoxaparin)
• Monoclonal Antibodies for early-stage high-risk patients
• IV fluids
• Nutritional support
• Isolation and infection control
Nursing Management :
Assessment :
• Monitor respiratory status (RR, O₂ saturation)
• Assess for fever, cough, fatigue
Interventions :
• Oxygen administration if required
• Maintain isolation
• Encourage for intake fluids and nutrition
• Administer medications as prescribed
• Provide psychological support due to fear/anxiety
• Educate on cough hygiene, mask usage
2.Paget’s disease
Definition :
Paget’s disease is a chronic bone disorder characterized by abnormal bone remodeling, resulting in enlarged, deformed, and weakened bones due to excessive bone breakdown and disorganized repair.
Etiology :
Exact cause is unknown, but contributing factors include :
• Genetic predisposition (e.g. SQSTM1 gene mutation)
• Slow viral infection (e.g., paramyxovirus hypothesis)
• Age-related (Common after age 50)
• Family history of bone disorders
Pathophysiology :
Overactive osteoclasts
→ excessive bone resorption
→ Compensatory osteoblastic activity
→ disorganized, fibrous, and immature bone formation
→ It result in bone becomes larger, weaker, and more vascular, prone to deformities and fractures
Clinical Manifestations :
Many patients are asymptomatic early.
Bone-related :
Bone pain (dull, deep)
Bone deformities (bowed legs, skull enlargement)
Increased warmth over bones
Pathological fractures
Neurological :
Headache
Hearing loss (if skull involved)
Nerve compression
Musculoskeletal :
Arthritis in adjacent joints
Muscle weakness (if spine involved)
Diagnostic Evaluation :
Blood Tests : Serum alkaline phosphatase (ALP) Normal calcium and phosphate levels
Urine : Hydroxyproline (bone breakdown marker)
X-ray
Bone scan
CT/MRI
Medical Management :
Drug Therapy :
Bisphosphonates (first-line) : Alendronate, Risedronate, Zoledronic acid that inhibit bone resorption
• Calcitonin : Hormone that inhibits osteoclast activity
• Analgesics / NSAIDs : For pain control
• Calcium & Vitamin D : To support bone strength
• Joint replacement (arthroplasty)
Nursing Management :
Assessment :
• Monitor pain level, mobility, neurological status
• Look for bone deformities, hearing loss
Interventions :
• Administer prescribed medications
• Encourage safety measures to prevent falls/fractures
• Educate on medication adherence (especially bisphosphonates)
• Support use of walking aids, braces if needed
• Nutritional advice (calcium, vitamin D rich foods)
3.Appendicitis
Definition
Appendicitis is the inflammation of the vermiform appendix, a small, finger-like pouch attached to the cecum (beginning of the large intestine). It often results from obstruction, leading to infection and, if untreated, perforation or rupture.
Etiology
• Obstruction of the appendiceal lumen:
• Fecalith (hardened stool)
• Lymphoid hyperplasia (especially in children)
• Parasites (e.g., pinworms)
• Foreign body
• Tumors (rare)
• Infection by bacteria after obstruction
Clinical Manifestations
Early Signs
• Dull periumbilical pain → shifts to right lower quadrant (McBurney’s point)
• Anorexia, nausea, vomiting
• Low-grade fever
Later Signs:
• Guarding, rebound tenderness
• ↑ Pain with movement or coughing
• Rovsing’s sign: RLQ pain when LLQ is pressed
• Psoas & Obturator signs: pain with hip movement
Diagnostic Evaluation
• WBC count
• CRP
• Urinalysis to rule out UTI
• Ultrasound
• CT Scan (gold standard)
• X-ray
Medical Management
Preoperative Management :
• NPO
• IV fluids
• Antibiotics (e.g., ceftriaxone + metronidazole)
• Pain control with caution (so as not to mask symptoms)
Surgical Management
• Appendectomy (removal of appendix)
• Open Appendectomy
• Laparoscopic Appendectomy (preferred if uncomplicated)
• Drainage of abscess if ruptured
Nursing Management :
Preoperative Care :
• Monitor for signs of perforation (sudden pain relief → then peritonitis)
• Maintain NPO status
• Prepare for surgery (consent, shaving, IV access)
• Administer fluids, antibiotics
Postoperative Care :
• Monitor VS, wound site, signs of infection
• Early ambulation
• Pain management
• Resume fluids as per bowel sound return
• Monitor bowel movements and voiding
• Discharge teaching : wound care, signs of complications, avoid strenuous activity
4.Acute respiratory distress syndrome
Definition
ARDS is a life-threatening condition characterized by acute inflammation and increased permeability of the alveolar-capillary membrane, leading to non-cardiogenic pulmonary edema, hypoxemia, and respiratory failure.
Etiology
Direct Lung Injury :
• Pneumonia
• Aspiration of gastric contents
• Inhalation injury (smoke, toxins)
• Pulmonary contusion
• Near drowning
Indirect Lung Injury :
• Sepsis (most common)
• Severe trauma
• Pancreatitis
• Massive transfusion
• Drug overdose
• Burns
• Shock
Stages of ARDS
Exudative Phase (0–7 days): Fluid accumulation, alveolar damage.
Proliferative Phase (7–21 days): Inflammatory resolution, lung repair.
Fibrotic Phase (>21 days): Fibrosis, chronic lung damage (in some cases).
Clinical Manifestations
• Severe dyspnea, tachypnea
• Refractory hypoxemia (not improving with oxygen)
• Cyanosis
• Use of accessory muscles for breathing
• Crackles on auscultation
• Restlessness, confusion, anxiety
• Hypotension in late stages
• Respiratory alkalosis progressing to acidosis
Diagnostic Evaluation
• ABG
• CBC, cultures to detect infection
• BNP (to rule out cardiac cause)
• Chest X-ray
• CT scan
• Pulmonary function tests
• Echocardiogram
Medical Management
Respiratory Support :
• Mechanical ventilation with low tidal volume (LTVV) strategy
• PEEP (positive end-expiratory pressure) to prevent alveolar collapse
• Prone positioning for improving oxygenation
Pharmacological :
• Antibiotics if infection
• Corticosteroids (controversial; in selected cases)
• Sedatives, neuromuscular blockers
• Diuretics (if fluid overloaded)
• Vasopressors (if hypotensive)
Other Interventions :
• Treat underlying cause (e.g., sepsis, trauma)
• ECMO (Extracorporeal Membrane Oxygenation) in refractory cases
Nursing Management
Assessment :
• Continuous monitoring of ABG, vital signs, oxygen saturation
• Assess for respiratory distress and cyanosis
Interventions :
• Maintain airway and ventilation
• Administer prescribed oxygen and drugs
• Suctioning as needed
• Position: Prone or Semi-Fowler’s
• Fluid balance monitoring
• Prevent infection and pressure sores
• Provide psychological support to patient/family
Q.8 Short Answers: (Any two) (3×2=6)
1.Psoriasis
Psoriasis is a chronic, non-contagious, autoimmune skin disease characterized by rapid proliferation of keratinocytes, leading to thickened, scaly patches on the skin, often with inflammation and erythema.
Causes and Risk Factors :
• Genetic predisposition (e.g., HLA-Cw6 gene)
• Immune system dysfunction (overactivation of T-cells)
• Environmental triggers
• Infections (e.g., Streptococcal throat)
• Injury to skin (Koebner phenomenon)
• Stress
• Medications (e.g.beta-blockers, lithium)
• Cold weather
• Smoking and alcohol use
Clinical Manifestations :
• Red, raised, inflamed plaques
• Silvery-white scales
• Itching, burning or soreness
• Nail changes (pitting, onycholysis)
• Joint pain (in psoriatic arthritis)
• Symmetrical distribution: commonly seen on scalp, elbows, knees, and lower back
Diagnostic Evaluation :
• History collection
• Physical examination
• Skin biopsy
• Munro microabscesses
• KOH test
• Blood tests – ESR, CRP (elevated in inflammation)
• Psoriasis Area and Severity Index (PASI)
Management
1. Topical Treatments (for mild to moderate psoriasis) :
Corticosteroids (e.g., betamethasone) – reduce inflammation
• Vitamin D analogs (e.g., calcipotriol) – slow skin cell growth
• Coal tar & salicylic acid – reduce scaling and itching
• Topical retinoids (e.g., tazarotene) – normalize skin turnover
2. Phototherapy (for moderate psoriasis) :
• Narrow-band UVB therapy
• PUVA therapy (Psoralen + UVA)
3. Systemic Treatments (for severe cases) :
• Methotrexate, Cyclosporine, Acitretin – immunosuppressive/retinoid
• Biologics (e.g., Adalimumab, Etanercept) – target immune pathways
Nursing Management :
• Educate on correct use of topical medications
• Encourage adherence to long-term treatment plans
• Assess for side effects of systemic drugs (e.g., liver toxicity with methotrexate)
Provide psychological support (as psoriasis affects self-esteem)
• Teach stress reduction techniques (stress can worsen psoriasis)
• Monitor for signs of infection in cracked or bleeding lesions
• Encourage use of moisturizers to reduce dryness and flaking
• Educate about sun exposure: moderate sun is helpful, but avoid sunburn
• Prevent scratching to avoid Koebner phenomenon (lesion formation at trauma site)
2.Wound healing
Wound healing is the biological process by which the body repairs and regenerates damaged tissue. It typically occurs in four overlapping stages :
1. Hemostasis :
Immediately after injury, blood vessels constrict and clotting occurs to stop bleeding.
2. Inflammation :
White blood cells (mainly neutrophils and macrophages) arrive to clean the wound of debris, bacteria, and damaged tissue.
3. Proliferation :
New tissue forms through cell division, including the formation of new blood vessels (angiogenesis), collagen production, and epithelialization (new skin formation)
4. Maturation (Remodeling) :
Collagen is reorganized, and the wound fully closes. This phase can last weeks to months.
3.Cardiac dysrhythmias
Dysrhythmia (also known as arrhythmia) refers to any abnormality in the rhythm of the heartbeat. This includes heartbeats that are too fast, too slow, or irregular.
Types of Dysrhythmia :
1. Tachycardia – Heart beats too fast (over 100 beats per minute).
2. Bradycardia – Heart beats too slowly (under 60 beats per minute).
3. Atrial fibrillation – Irregular and often rapid heartbeat starting in the atria.
4. Ventricular fibrillation – Rapid, erratic heart signals in the ventricles—life-threatening.
5. Premature contractions – Early beats that disrupt the normal rhythm.
Etiology :
• Heart disease or damage (e.g.after a heart attack)
• High blood pressure
• Electrolyte imbalances (like potassium or magnesium)
• Drug or alcohol use
• Stress or anxiety
• Certain medications
Clinical manifestations :
• Palpitations (fluttering or pounding in the chest)
• Dizziness or lightheadedness
• Shortness of breath
• Chest discomfort
• Fainting (syncope)
Diagnostic evaluation :
• ECG
• Holter monitor
• Echocardiogram
• Stress tests
Treatments :
• Medications (e.g., beta-blockers)
• Pacemakers
• Ablation therapy
• Lifestyle changes
