FON-MEDICAL SURGICAL ASEPSIS-SYNOPSIS-8-PHC
🧼✨ Terms Used in Medical & Surgical Asepsis ✨🧼
📚 Essential for Infection Control in Clinical Practice & Nursing Exams
🔹 1. Asepsis
🧴 Definition: The absence of disease-producing microorganisms.
🔍 Purpose: To prevent infection and contamination.
🌿 Types:
- Medical Asepsis (Clean technique) 🧽
- Surgical Asepsis (Sterile technique) 🧪
🔹 2. Medical Asepsis 🧼
🩺 Aims to reduce the number and spread of microorganisms.
🛡️ Examples:
- Handwashing 🤲
- Cleaning surfaces 🧹
- Wearing gloves 🧤
🔹 3. Surgical Asepsis 🛑
🧪 Complete elimination of all microorganisms, including spores.
⚠️ Used in:
- Operating Theaters 🏥
- Invasive Procedures 💉
🔹 4. Sterilization 🔥
🔥 Destruction of all forms of microbial life including spores.
🛠️ Methods:
- Autoclaving (Steam) ♨️
- Dry Heat 🔥
- Gas (Ethylene oxide) 💨
- Radiation ☢️
🔹 5. Disinfection 🧪
🧽 Elimination of most or all pathogenic microorganisms (except spores).
🧴 Agents: Phenol, Chlorine, Alcohol
🔹 6. Antiseptic 💧
🧴 Chemical used on living tissue to inhibit or kill microorganisms.
🌿 Examples: Betadine, Chlorhexidine
🔹 7. Contamination 🚫
🧫 Presence of harmful microbes on sterile items or surfaces.
🧤 Causes: Touching sterile items with unclean hands or gloves.
🔹 8. Sterile Field 🩻
🩹 Area that is kept free of microorganisms during procedures.
🧼 Must avoid:
- Touching with unsterile items ❌
- Turning your back on it ❌
🔹 9. Surgical Scrub 🧼🕐
🫧 Hand and arm washing procedure before surgery.
⏱️ Time: 5–10 minutes
🧼 Use: Antimicrobial soap (e.g., chlorhexidine/iodine)
🔹 10. Autoclave ♨️
🔬 Machine used for steam sterilization under pressure.
📦 Used for: Surgical tools, dressings, gloves.
🔹 11. Cross Infection 🔁
🦠 Infection passed from one patient to another via healthcare worker or equipment.
🚫 Prevent by: Hand hygiene, PPE, proper disinfection.
🔹 12. Carriers 🧬
👩⚕️ Persons who harbor pathogens without showing symptoms.
❗ Can still transmit disease to others.
🔹 13. Bacteriostat 🧫
🧪 Agent that inhibits bacterial growth but does not kill bacteria.
🧼 Example: Alcohol in low concentrations.
🔹 14. Personal Protective Equipment (PPE) 🧤😷
🛡️ Includes gloves, gowns, masks, face shields.
📍Used to:
- Prevent exposure to infections
- Protect both patient & nurse
🔹 15. Standard Precautions 📋
🩺 Set of guidelines used with all patients regardless of diagnosis.
⚠️ Includes:
- Hand hygiene 🤲
- PPE usage 🧤😷
- Safe injection practices 💉
🔹 16. Isolation 🚧
🚫 Separating infected patients to prevent transmission.
🛏️ Types:
- Contact
- Droplet
- Airborne
🔹 17. Nosocomial Infection 🏥🦠
🏥 Hospital-acquired infections
📈 Risk Factors: Catheters, IV lines, prolonged hospital stay
🧼 Prevented by: Aseptic technique, sterilization, hand hygiene
🌟📚 Key Exam Points 📚🌟
🔸 Hand washing is the most effective way to prevent cross infection
🔸 Surgical asepsis is used in all invasive procedures
🔸 Autoclaving = 121°C at 15 psi for 15–20 minutes
🔸 All PPE must be removed carefully to avoid contamination
🔸 Use sterile gloves for dressing open wounds
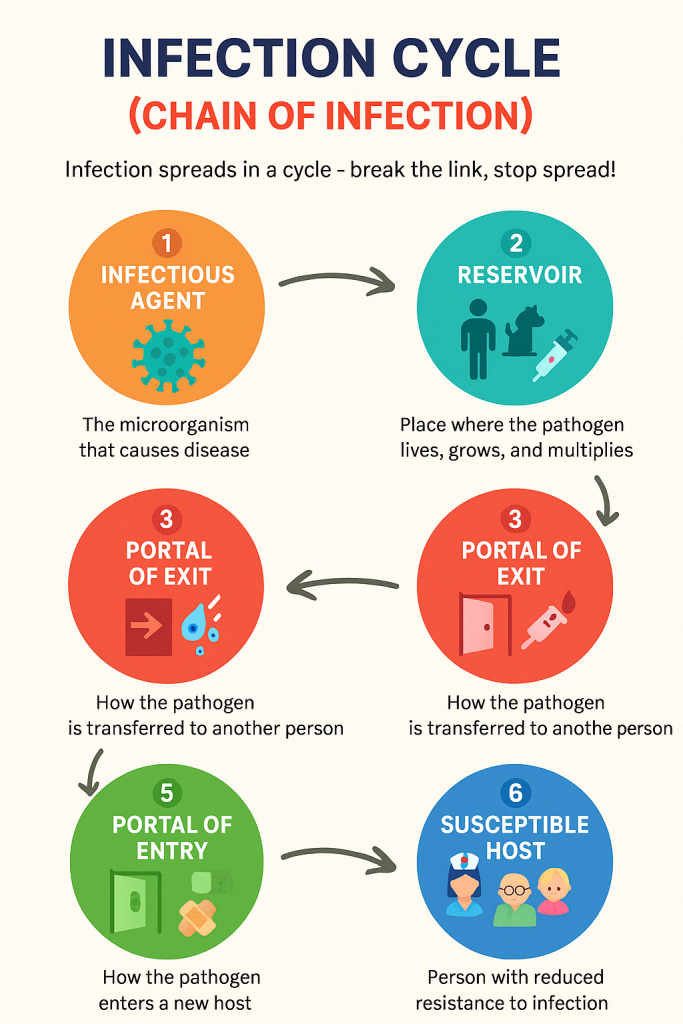
🌟 INFECTION CYCLE (CHAIN OF INFECTION) 🌟
🦠 “Infection spreads in a cycle – break the link, stop the spread!”
The Infection Cycle shows how infections develop and spread from one person to another. It has 6 essential links, and breaking any one link can prevent infection.
🔗 THE 6 LINKS IN THE CHAIN OF INFECTION
1️⃣ Infectious Agent (Pathogen) 🦠
Definition: The microorganism that causes disease
✔️ Examples:
— Bacteria (e.g., Staphylococcus)
— Viruses (e.g., Influenza, HIV)
— Fungi (e.g., Candida)
— Parasites (e.g., Plasmodium)
Control Measures:
🧼 Sterilization
💊 Antibiotics/antivirals
🧪 Rapid identification & treatment
2️⃣ Reservoir 🧍♂️🐾🌊
Definition: Place where the pathogen lives, grows, and multiplies
✔️ Examples:
— Humans (carriers or infected)
— Animals
— Water
— Soil
— Medical equipment
Control Measures:
🧽 Environmental sanitation
🛏️ Disinfection of surfaces
🚮 Proper waste disposal
🧼 Hand hygiene
3️⃣ Portal of Exit 🚪💉
Definition: How the pathogen leaves the reservoir
✔️ Examples:
— Blood 🩸
— Saliva 😮💨
— Urine & feces 🚽
— Drainage from wounds 🩹
— Coughing or sneezing 🤧
Control Measures:
😷 Covering mouth/nose
🧼 Proper disposal of body fluids
🧤 PPE (gloves, masks)
4️⃣ Mode of Transmission 🔄
Definition: How the pathogen is transferred to another person
✔️ Types:
— Direct contact (touching, kissing) 🤝
— Indirect contact (shared items) 🧻
— Droplet (sneezing, coughing) 💦
— Airborne (TB, COVID-19) 🌫️
— Vector-borne (mosquitoes, fleas) 🦟
Control Measures:
✋ Hand hygiene
🧤 PPE use
🛑 Isolation precautions
🔬 Sterile technique
5️⃣ Portal of Entry 🚪🧬
Definition: How the pathogen enters a new host
✔️ Examples:
— Broken skin 🩹
— Mucous membranes 👃👄
— Respiratory tract 🌬️
— Urinary or GI tract 🚽
— Injections/IV lines 💉
Control Measures:
🧼 Wound care
📦 Aseptic procedures
👕 Protective barriers
🚿 Catheter care
6️⃣ Susceptible Host 🧑⚕️👵👶
Definition: Person with reduced resistance to infection
✔️ Risk Factors:
— Elderly or infants
— Immunocompromised (HIV, cancer)
— Malnutrition
— Post-surgery patients
— Chronic illnesses (diabetes, heart disease)
Control Measures:
💉 Immunization
🍎 Good nutrition
💪 Regular exercise
😌 Stress reduction
📋 Treating underlying illness
🔐 BREAKING THE CHAIN – NURSE’S ROLE 👩⚕️
✅ Perform hand hygiene before and after every patient contact
✅ Use gloves, gowns, and masks (PPE)
✅ Maintain clean and sterile environments
✅ Educate patients and caregivers about infection prevention
✅ Dispose of sharps and waste safely
✅ Monitor for early signs of infection
🧩 SUMMARY: INFECTION CYCLE CHART
| 🔢 Step | 🧩 Link | 🛡️ Example Control |
|---|---|---|
| 1️⃣ | Infectious Agent | Antibiotics, sterilization |
| 2️⃣ | Reservoir | Sanitation, hygiene |
| 3️⃣ | Portal of Exit | Masks, wound care |
| 4️⃣ | Mode of Transmission | PPE, handwashing |
| 5️⃣ | Portal of Entry | Catheter care, wound dressing |
| 6️⃣ | Susceptible Host | Vaccines, nutrition |
📌 MOST ASKED EXAM QUESTIONS (MCQ STYLE)
✅ Q: What is the most effective way to break the chain of infection?
🅰️ Hand hygiene
✅ Q: Which is an example of a portal of exit?
🅰️ Sputum
✅ Q: What is a susceptible host?
🅰️ An individual with a weak immune system
✅ Q: Which part of the infection chain does PPE protect?
🅰️ Mode of transmission & portal of entry
✅ Q: What is the chain of infection in correct order?
🅰️ Agent → Reservoir → Exit → Transmission → Entry → Host
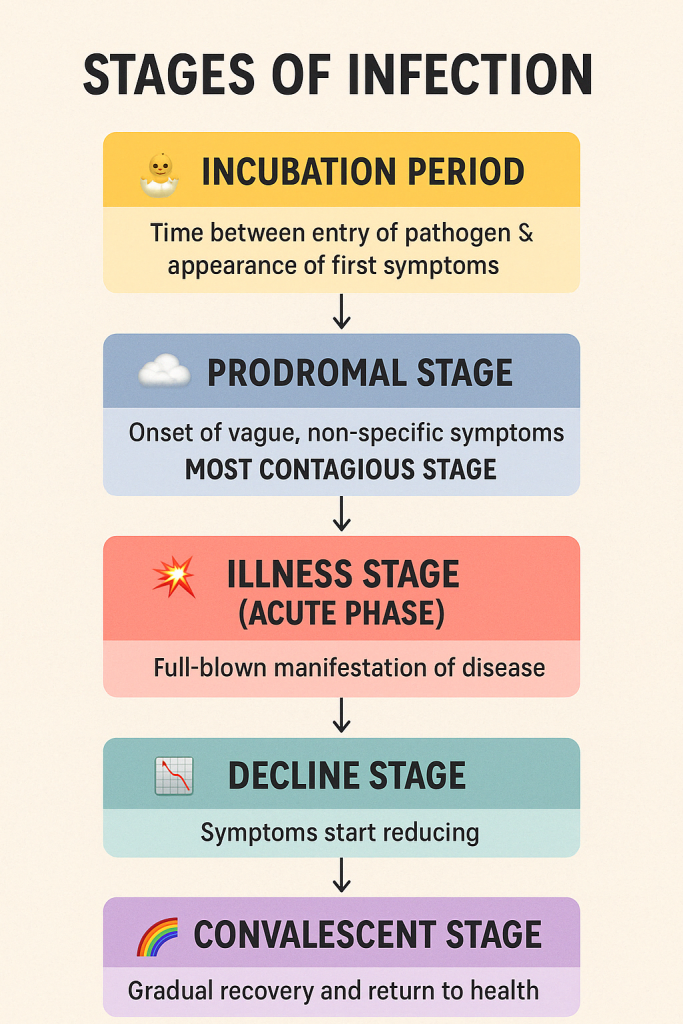
🔄 Stages of Infection (🧪Progression of Infection in the Body)
🔹 1. Incubation Period 🐣
🕰️ Time between entry of pathogen & appearance of first symptoms
📌 Key Points:
- No visible symptoms 🤐
- Microorganisms multiply silently 🧬
- Host may still be contagious! ⚠️
📝 Example:
- Chickenpox: 10–21 days
- Common cold: 1–3 days
🔹 2. Prodromal Stage 🌫️
🧠 Onset of vague, non-specific symptoms
📌 Key Symptoms:
- Fatigue 😴
- Mild fever 🌡️
- Malaise 😷
- Headache 🤕
⚠️ MOST CONTAGIOUS STAGE!
🔹 3. Illness Stage (Acute Phase) 🧨
💥 Full-blown manifestation of disease
📌 Symptoms become specific:
- High fever 🤒
- Cough/sore throat 🗣️
- Diarrhea, rashes, pain, etc.
🩺 Clinical signs easily identifiable
🔹 4. Decline Stage 📉
💊 Symptoms start reducing due to immune response or treatment
📌 Indicators:
- Fever subsides 🌡️⬇️
- Appetite returns 🍲
- Energy improves ⚡
⚠️ Patient still vulnerable to secondary infections
🔹 5. Convalescent Stage 🌈
🔁 Gradual recovery and return to health
📌 Body repairs & immunity builds
🛏️ May last days to weeks
🔬 Pathogens eliminated
✅ No more symptoms
✅ Non-contagious phase
📚📝 Most Frequently Asked MCQs (with Answers) 📘🎯
❓ Q1. Which stage of infection is considered the most contagious?
A. Incubation period
B. Prodromal stage
C. Illness stage
D. Convalescence
✅ Correct Answer: B. Prodromal stage
📌 Because the patient shows mild symptoms but is shedding the most pathogens!
❓ Q2. Which stage shows full clinical signs and symptoms?
A. Incubation
B. Decline
C. Illness stage
D. Convalescence
✅ Correct Answer: C. Illness stage
❓ Q3. What happens during the incubation period?
A. Symptoms are fully developed
B. Pathogen is eliminated
C. Pathogen enters and multiplies
D. Patient recovers
✅ Correct Answer: C. Pathogen enters and multiplies
❓ Q4. During which stage is the patient recovering but still weak?
A. Illness
B. Decline
C. Convalescence
D. Incubation
✅ Correct Answer: C. Convalescence
❓ Q5. In which stage can secondary infections occur due to lowered immunity?
A. Prodromal
B. Decline
C. Convalescence
D. Incubation
✅ Correct Answer: B. Decline
🌟 Quick Recap in Emojis 🌟
| Stage | Emoji | Meaning |
|---|---|---|
| Incubation | 🐣 | Pathogen enters, no signs |
| Prodromal | 🌫️ | Mild symptoms, most contagious |
| Illness | 💥 | Specific, full-blown symptoms |
| Decline | 📉 | Recovery starts, symptoms fade |
| Convalescence | 🌈 | Healing, body regains strength |
🌟 MODE OF TRANSMISSION 🌟
🔁 “Understand the pathway, break the chain of infection.”
Mode of transmission refers to how a pathogen moves from a reservoir to a susceptible host. There are two major categories:
✅ Direct Transmission
✅ Indirect Transmission
🧭 1️⃣ DIRECT MODE OF TRANSMISSION 🤝
➡️ Immediate transfer of infectious agents from person to person via direct contact.
🗂️ TYPES OF DIRECT TRANSMISSION:
| 🔹 Type | 📖 Description | 💡 Examples |
|---|---|---|
| 🤝 Person-to-Person Contact | Touching an infected person | Handshake, hugging, kissing |
| 💏 Sexual Contact | Intimate exposure to secretions | HIV, Gonorrhea, Syphilis |
| 💋 Mucous Membrane Contact | Contact with eyes, nose, mouth | Cold, Flu |
| 🐾 Vertical Transmission | From mother to baby | HIV, Rubella (in utero) |
| 💉 Droplet (within 3 ft) | Coughing, sneezing (large droplets >5µm) | Influenza, COVID-19, Pertussis |
✅ Prevention Strategies:
- Hand hygiene ✋
- Mask use 😷
- Avoid close contact 🤲
- Use of gloves 🧤
- Respiratory etiquette (cover cough/sneeze)
🧭 2️⃣ INDIRECT MODE OF TRANSMISSION 🧻🦟
➡️ Transfer through an intermediate object or organism.
🗂️ TYPES OF INDIRECT TRANSMISSION:
| 🔹 Type | 📖 Description | 💡 Examples |
|---|---|---|
| 🧻 Fomite Transmission | Through contaminated objects | Bed rails, thermometers, stethoscope |
| 🧪 Vehicle-Borne | Ingestion of contaminated food, water, drugs | Cholera, Hepatitis A |
| 🌫️ Airborne Transmission | Inhalation of aerosols <5 µm | TB, Measles, Varicella |
| 🦟 Vector-Borne | Insects/animals transfer pathogens | Malaria (mosquito), Plague (fleas) |
| 🏥 Nosocomial Cross-Infection | Healthcare setting infections | MRSA, VRE, Catheter-related UTIs |
✅ Prevention Strategies:
- Disinfection & sterilization 🧴
- Food safety 🥗
- Vector control 🦟
- Negative pressure rooms 🌬️
- Use of PPE 👩⚕️🧤
📊 COMPARISON CHART – DIRECT vs INDIRECT TRANSMISSION
| 🔍 Feature | 🤝 Direct | 🧻 Indirect |
|---|---|---|
| Contact | Person-to-person | Through object/vector |
| Speed | Immediate | Delayed |
| Examples | Kiss, sneeze, sex | Fomites, airborne, mosquito |
| Prevention | Hand hygiene, PPE | Sterilization, pest control |
🧠 NURSE’S ROLE IN PREVENTION
👩⚕️ Nurses are vital in breaking the transmission chain:
- 🧼 Practice hand hygiene
- 🧴 Disinfect surfaces & tools
- 😷 Wear masks, gloves, aprons
- 🗣️ Educate patients & families
- 🛑 Isolate infected individuals if required
📌 MOST ASKED EXAM QUESTIONS (MCQ STYLE)
✅ Q: Which mode involves touching an infected wound?
🅰️ Direct contact transmission
✅ Q: What is a fomite in transmission?
🅰️ Non-living object that carries pathogens
✅ Q: Which infections spread via airborne route?
🅰️ Tuberculosis, Measles
✅ Q: Mode of transmission in mosquito-borne diseases?
🅰️ Vector-borne (indirect)
✅ Q: Prevention of indirect transmission includes?
🅰️ Disinfection and sterilization
🌟 STANDARD PRECAUTIONS 🌟
🧤 “Standard Precautions = Universal Safety. Protect yourself, protect your patients.”
📘 DEFINITION
🗨️ Standard Precautions are basic infection control measures applied to the care of all patients, regardless of their diagnosis or infection status, to prevent transmission of infectious agents in healthcare settings.
✅ These are universal practices used in all patient care to ensure safety.
🎯 PURPOSE OF STANDARD PRECAUTIONS
✔️ Protect healthcare workers from exposure to infections
✔️ Prevent cross-transmission between patients
✔️ Maintain safety in clinical environments
✔️ Ensure universal application regardless of diagnosis
🧩 COMPONENTS OF STANDARD PRECAUTIONS
| 🛡️ Measure | 📖 Description | 💡 Examples |
|---|---|---|
| ✋ Hand Hygiene | Most effective method to prevent infection | Soap & water or alcohol rub before/after patient care |
| 🧤 Use of PPE | Protect against contact with body fluids | Gloves, masks, gowns, goggles |
| 😷 Respiratory Hygiene/Cough Etiquette | Reduce transmission from cough/sneeze | Covering mouth, using masks/tissues |
| 🧴 Safe Injection Practices | Prevent infections from sharps | Use sterile syringes, avoid recapping |
| 🧪 Proper Handling of Equipment | Avoid contamination from instruments | Disinfect reusable equipment |
| 🚮 Waste Disposal | Ensure safe removal of biohazard waste | Color-coded BMW bins |
| 🧽 Environmental Cleaning | Routine cleaning of surfaces | Beds, doorknobs, nursing stations |
| 🧼 Safe Handling of Soiled Linen | Prevent exposure to fluids/infectious material | Use gloves, bagging and labeling soiled linen |
🧤 PERSONAL PROTECTIVE EQUIPMENT (PPE) IN STANDARD PRECAUTIONS
| 👕 PPE | 📝 When to Use |
|---|---|
| 🧤 Gloves | When touching blood, body fluids, mucous membranes |
| 👗 Gown/Apron | If splash or spray is anticipated |
| 😷 Mask | For respiratory secretions or during procedures |
| 🥽 Eye Protection | If splash into eyes is possible (e.g., suctioning) |
🩸 APPLIED TO ALL BODY FLUIDS EXCEPT:
🚫 Sweat (if not visibly contaminated)
✅ Applied to:
Blood 🩸, urine, feces, saliva, vomitus, CSF, wound drainage, vaginal secretions, and breast milk
👩⚕️ NURSE’S ROLE IN IMPLEMENTING STANDARD PRECAUTIONS
🔹 Perform hand hygiene regularly
🔹 Use appropriate PPE for procedures
🔹 Ensure safe disposal of sharps and waste
🔹 Educate patients/families on hygiene and precautions
🔹 Maintain clean equipment and surroundings
🔹 Report and manage exposure incidents immediately
📌 MOST ASKED EXAM QUESTIONS (MCQ STYLE)
✅ Q: Which precaution is considered most important in infection prevention?
🅰️ Hand hygiene
✅ Q: Which PPE is essential for handling body fluids?
🅰️ Gloves
✅ Q: Which body fluid is NOT covered under standard precautions?
🅰️ Sweat (if not visibly soiled)
✅ Q: What is the safest method for preventing needlestick injuries?
🅰️ Avoid recapping needles and use sharps containers
✅ Q: Why are standard precautions applied to all patients?
🅰️ To prevent unrecognized transmission from asymptomatic carriers
🌟 TYPES OF ISOLATION PRECAUTIONS 🌟
🚷 “Isolate to protect — prevent the spread before it begins.”
Isolation precautions are infection control strategies used to prevent transmission of infectious diseases in healthcare settings. They are applied based on the mode of transmission.
📘 DEFINITION
🗨️ Isolation is the practice of separating infected patients to prevent direct or indirect transmission of infectious agents to others. It includes the use of PPE, environmental control, and restriction of visitors.
🧩 TYPES OF ISOLATION PRECAUTIONS
| 🛡️ Type | 📖 Purpose | 🔍 Examples of Diseases | 🧤 PPE Required |
|---|---|---|---|
| 😷 1. Standard Precautions | Applied to all patients regardless of diagnosis | All body fluids (except sweat) | Gloves, hand hygiene, mask (if needed) |
| 💦 2. Contact Precautions | For diseases spread by direct/indirect contact | MRSA, VRE, Scabies, C. difficile | Gloves, Gown |
| 💧 3. Droplet Precautions | For pathogens spread by large respiratory droplets (>5μm) | Influenza, Pertussis, COVID-19 (some cases), Mumps | Surgical Mask, Gloves |
| 🌫️ 4. Airborne Precautions | For infections spread by airborne particles (<5μm) | Tuberculosis, Measles, Chickenpox (Varicella) | N95 Respirator, Negative-pressure room, Gloves |
| 🩸 5. Protective (Reverse) Isolation | Protect immunocompromised patients from infection | Chemotherapy patients, bone marrow transplant | Mask, Gloves, Gown, HEPA-filtered air room |
🔁 COMPARISON SUMMARY CHART
| 🧪 Mode | 🧼 Room Type | 😷 Mask | 🧤 Gown/Gloves | 🛑 Special Notes |
|---|---|---|---|---|
| Standard | Shared/Private | If needed | If body fluid exposure expected | For all patients |
| Contact | Private (preferred) | No | Always | Dedicate equipment |
| Droplet | Private (preferred) | Surgical | As per contact | Maintain 3–6 ft distance |
| Airborne | Negative-pressure room | N95 | As per contact | Limit patient movement |
| Protective | Positive-pressure room | Surgical | Always | No fresh flowers, strict hygiene |
👩⚕️ NURSE’S ROLE IN ISOLATION
🔹 Explain isolation purpose to patient/family
🔹 Ensure correct PPE use (donning & doffing)
🔹 Maintain hand hygiene & room signage
🔹 Minimize patient movement
🔹 Disinfect equipment after use
🔹 Monitor for psychological effects of isolation (loneliness, anxiety)
🚨 ISOLATION COLOR CODING / SIGNAGE (varies by hospital)
| 🎨 Color | 🚷 Type |
|---|---|
| 🔴 Red | Airborne |
| 🟡 Yellow | Contact |
| 🔵 Blue | Droplet |
| 🟢 Green | Protective isolation |
📌 MOST ASKED EXAM QUESTIONS (MCQ STYLE)
✅ Q: Which isolation is used for TB?
🅰️ Airborne precautions
✅ Q: What PPE is essential in contact isolation?
🅰️ Gloves and Gown
✅ Q: Droplet precautions are required for which infection?
🅰️ Influenza
✅ Q: What kind of isolation is used for neutropenic patients?
🅰️ Protective (Reverse) Isolation
✅ Q: Which type of room is required for airborne precautions?
🅰️ Negative-pressure room
🌟 HAND HYGIENE TECHNIQUES 🌟
✋ “Clean hands save lives – the simplest and most powerful infection control tool.”
📘 DEFINITION
🗨️ Hand hygiene refers to the practice of cleansing hands using soap and water or alcohol-based hand rubs to remove dirt, microorganisms, and pathogens to prevent the spread of infection.
🎯 PURPOSE OF HAND HYGIENE
✅ To prevent cross-infection between patients, staff & environment
✅ To remove visible dirt and organic matter
✅ To reduce transient & resident flora
✅ To meet infection control and hospital standards
✋🧽 TYPES OF HAND HYGIENE
| 🔢 Type | 📖 Description | 💡 When to Use |
|---|---|---|
| 🧼 1. Handwashing (with soap & water) | Removes dirt, debris, and most pathogens | When hands are visibly soiled or after contact with body fluids |
| 🧴 2. Alcohol-based hand rub (ABHR) | Kills most pathogens on clean hands | Preferred when hands are not visibly dirty |
| 🧽 3. Surgical Hand Antisepsis | High-level hand cleaning before surgery | Before invasive procedures/surgical operations |
| 🧴 4. Antiseptic Handwash | Soap + antiseptic agents (chlorhexidine, iodine) | In high-risk areas (ICU, NICU, OR) |
🕐 WHEN TO PERFORM HAND HYGIENE (WHO “5 Moments”)
1️⃣ Before touching a patient
2️⃣ Before a clean/aseptic procedure
3️⃣ After body fluid exposure
4️⃣ After touching a patient
5️⃣ After touching patient surroundings
✅ STEP-BY-STEP TECHNIQUE – SOAP & WATER
1️⃣ Wet hands under running water
2️⃣ Apply enough soap
3️⃣ Rub hands palm to palm
4️⃣ Right palm over left dorsum & vice versa
5️⃣ Palm to palm with fingers interlaced
6️⃣ Back of fingers to opposite palms
7️⃣ Rotational rubbing of thumbs
8️⃣ Fingertips rubbed in opposite palms
9️⃣ Rinse hands with water
🔟 Dry hands with a single-use towel
💧 Turn off tap with elbow/tissue
⏱️ Duration: 40–60 seconds
✅ STEP-BY-STEP TECHNIQUE – ALCOHOL-BASED HAND RUB
1️⃣ Apply a palmful of hand rub
2️⃣ Rub hands palm to palm
3️⃣ Right palm over left dorsum & vice versa
4️⃣ Palm to palm with fingers interlaced
5️⃣ Back of fingers to opposite palms
6️⃣ Rotational rubbing of thumbs
7️⃣ Rub tips of fingers in palms
8️⃣ Allow to air dry completely
⏱️ Duration: 20–30 seconds
⚠️ COMMON MISTAKES TO AVOID
🚫 Not rubbing for enough time
🚫 Missing thumbs, fingertips, between fingers
🚫 Wearing jewelry or artificial nails
🚫 Not drying hands properly
🚫 Touching taps with clean hands
👩⚕️ NURSE’S ROLE IN HAND HYGIENE
🔹 Practice & role-model hand hygiene
🔹 Educate patients & attendants
🔹 Ensure availability of hand rub/soap dispensers
🔹 Report non-compliance
🔹 Audit & monitor hand hygiene in units
📌 MOST ASKED EXAM QUESTIONS (MCQ STYLE)
✅ Q: What is the most effective way to prevent infection transmission?
🅰️ Hand hygiene
✅ Q: How long should alcohol-based hand rub be used?
🅰️ 20–30 seconds
✅ Q: Which part is most often missed in handwashing?
🅰️ Thumbs and fingertips
✅ Q: When is hand hygiene done after removing gloves?
🅰️ Immediately after
✅ Q: Name the WHO-recommended moments for hand hygiene.
🅰️ Before patient contact, before aseptic task, after body fluid exposure, after patient contact, after patient environment contact

🌟 SURGICAL SCRUB TECHNIQUES 🌟
🖐️ “Clean hands, clean conscience – safeguard every surgery.”
📘 DEFINITION
🗨️ Surgical hand scrub is a thorough antiseptic hand and forearm cleaning process done before wearing sterile surgical gloves, aiming to eliminate transient and most resident flora.
✅ It is a critical step in maintaining aseptic conditions in the operating room (OR).
🎯 PURPOSE OF SURGICAL SCRUB
✔️ Prevent surgical site infections (SSIs)
✔️ Maintain sterility in the operating theatre
✔️ Eliminate microorganisms from hands, nails, and forearms
✔️ Protect patients and staff from cross-infection
🧴 TYPES OF SURGICAL SCRUBS
| 🔢 Type | 🧽 Description | 💡 Example Products |
|---|---|---|
| 🧼 Antiseptic Soap Scrub | Using antimicrobial soap and water | Chlorhexidine gluconate (4%), Povidone-iodine |
| 🧴 Alcohol-Based Rub | High-level disinfection without water | Ethanol/Isopropyl hand rub with emollients |
| 🧼🧴 Combined Method | Initial wash with soap + alcohol rub finish | Soap + 70% alcohol rinse |
🧠 PRINCIPLES TO REMEMBER
🔹 Scrub from clean (hands) to less clean (elbows)
🔹 Maintain sterility after scrubbing — DO NOT touch anything
🔹 Dry hands with sterile towel only
🔹 Keep hands above elbow level throughout
🔹 Use systematic sequence and time for thorough scrubbing
🪞 SURGICAL SCRUB – STEP-BY-STEP TECHNIQUE (ANTISEPTIC SOAP METHOD)
⏱️ Duration: 5 minutes (1st case), 3 minutes (subsequent)
🖐️ Step 1: Initial Wash
✔️ Remove jewelry, nail polish, and trim nails
✔️ Open sterile brush and antiseptic solution
✔️ Turn on water using elbow/foot pedal
✔️ Wet hands and arms up to elbows
🧼 Step 2: Scrubbing Procedure
🔹 Scrub each hand and forearm up to 2 inches above elbow
🔹 Use 15 strokes for each surface area:
- Fingernails
- Each finger (4 sides)
- Palms
- Back of hands
- Wrists
- Forearms
🔹 Use nail pick to clean under nails
💧 Step 3: Rinse
✔️ Rinse hands under running water fingertips downward
✔️ Do NOT let water run back toward elbows
🧻 Step 4: Drying Hands
✔️ Take a sterile towel
✔️ Dry from fingertips to elbow in a rotating motion
✔️ Use one side per arm
🧤 Step 5: Gowning and Gloving
✔️ Wear sterile gown and gloves without contaminating hands
⚠️ DOs AND DON’Ts
| ✅ DOs | ❌ DON’Ts |
|---|---|
| Use nail pick before scrubbing | Touch anything after scrubbing |
| Keep hands above elbows | Let water drip from elbow to fingers |
| Scrub systematically | Skip scrubbing between fingers |
| Use elbow to operate taps | Wear gloves with wet hands |
👩⚕️ NURSE’S ROLE IN SURGICAL SCRUBS
🔹 Teach and demonstrate correct technique
🔹 Monitor team compliance in OT
🔹 Check availability of sterile brushes, towels, and antiseptics
🔹 Prevent breaches in sterile field
🔹 Reinforce timing and sequence
📌 MOST ASKED EXAM QUESTIONS (MCQ STYLE)
✅ Q: What is the primary goal of surgical hand scrub?
🅰️ Remove transient flora and reduce resident flora
✅ Q: Which direction should you rinse hands during surgical scrub?
🅰️ From fingertips to elbows
✅ Q: What is the recommended time for the first surgical scrub of the day?
🅰️ 5 minutes
✅ Q: What is the correct level of hands during drying?
🅰️ Keep hands above elbows
✅ Q: What is used to dry hands after surgical scrub?
🅰️ Sterile towel
🌟 PHYSICAL METHODS OF STERILIZATION 🌟
🔥 “Destroy to protect — physical sterilization ensures complete microbial death.”
📘 DEFINITION
🗨️ Sterilization is the process of eliminating all forms of microorganisms, including bacteria, viruses, fungi, and spores from surfaces, instruments, or fluids.
✅ Physical methods use heat, radiation, or filtration to achieve sterilization.
🔥 TYPES OF PHYSICAL STERILIZATION METHODS
1️⃣ Moist Heat Sterilization (Autoclaving)
🌫️ Uses steam under pressure to destroy all microbes including spores.
| 🔍 Feature | 💡 Details |
|---|---|
| 🔥 Temp & Time | 121°C for 15–20 min at 15 psi pressure |
| 📦 Equipment | Autoclave machine |
| ✅ Uses | Surgical instruments, dressings, linen, culture media |
| ❗ Not for | Oils, powders, plastics |
🧪 Principle: Coagulation and denaturation of microbial proteins
2️⃣ Dry Heat Sterilization
🔥 Kills microbes through oxidation with hot air.
| 🔍 Feature | 💡 Details |
|---|---|
| 🔥 Temp & Time | 160°C for 2 hrs or 170°C for 1 hr |
| 📦 Equipment | Hot Air Oven |
| ✅ Uses | Glassware, metal instruments, powders, oils |
| ❗ Not for | Rubber, fabric, culture media |
🧪 Principle: Protein denaturation & oxidation
3️⃣ Radiation Sterilization
🌟 Uses high-energy rays to sterilize disposable items or sensitive materials.
🔸 a. Ionizing Radiation (Gamma Rays / X-rays)
| ✅ Used For | Disposable syringes, catheters, IV sets, gloves | | 🧪 Source | Cobalt-60 (gamma radiation) | | 💡 Advantage | Cold sterilization; penetrates deep |
🔸 b. Non-Ionizing Radiation (UV Rays)
| ✅ Used For | Surface sterilization of operating rooms, biosafety cabinets | | ❗ Limitation | Poor penetration, only kills surface organisms |
4️⃣ Filtration Sterilization
🧴 Removes microbes from fluids using membrane filters (not heat-based).
| 🔍 Feature | 💡 Details |
|---|---|
| ✅ Used For | Heat-sensitive fluids (e.g., antibiotics, vaccines, sera) |
| 🧪 Filter Pore Size | 0.22 µm removes bacteria |
| 🔧 Devices | Candle filters, membrane filters, HEPA filters |
| ❗ Note | Does not remove viruses or endotoxins completely |
🧪 Principle: Mechanical removal of microbes by sieving
🧠 COMPARATIVE CHART
| ⚙️ Method | 🌡️ Temp | 🕒 Time | ✅ Used For |
|---|---|---|---|
| Autoclaving | 121°C | 15–20 min | Dressings, instruments |
| Hot Air Oven | 160°C | 2 hrs | Glassware, oils |
| Gamma Rays | Room temp | Varies | Disposables |
| UV Rays | Room temp | Few minutes | Surface air sterilization |
| Filtration | Room temp | Instant | Heat-labile liquids |
👩⚕️ NURSE’S ROLE IN STERILIZATION
🔹 Ensure correct method selection based on material
🔹 Operate autoclave/dry heat equipment as per protocol
🔹 Check sterility indicators (tapes, biological indicators)
🔹 Maintain logs of sterilization cycles
🔹 Prevent contamination during storage and transport
🔹 Educate staff on aseptic techniques
📌 MOST ASKED EXAM QUESTIONS (MCQ STYLE)
✅ Q: What is the standard temperature and pressure for autoclaving?
🅰️ 121°C at 15 psi for 15–20 minutes
✅ Q: Which method is best for sterilizing glassware?
🅰️ Dry heat (Hot Air Oven)
✅ Q: Which radiation sterilization is used for disposable syringes?
🅰️ Gamma rays
✅ Q: What is the pore size of membrane filters used in filtration?
🅰️ 0.22 microns
✅ Q: Which physical method is suitable for heat-sensitive solutions?
🅰️ Filtration
🌟 CHEMICAL METHODS OF STERILIZATION 🌟
🧴 “When heat won’t do, chemicals come through — sterilize smartly.”
📘 DEFINITION
🗨️ Chemical sterilization refers to the use of liquid or gaseous chemicals to destroy all forms of microbial life, including spores, on instruments or surfaces that are heat-sensitive.
✅ It is commonly used for plastic, fiber-optic, and electronic medical equipment.
🔬 COMMONLY USED CHEMICAL AGENTS
| 🧪 Chemical | 📖 Description | 💡 Common Uses |
|---|---|---|
| 🔸 Ethylene Oxide (EtO) | Colorless gas used in special chambers | Catheters, IV sets, endoscopes, heart-lung machines |
| 🔸 Glutaraldehyde (2%) | High-level disinfectant; sporicidal in 10 hrs | Endoscopes, respiratory therapy equipment |
| 🔸 Formaldehyde | Gas or liquid; used for fumigation | Surgical instruments, hospital rooms |
| 🔸 Hydrogen Peroxide (Plasma Form) | Used in gas plasma sterilizers | Electrical instruments, implants |
| 🔸 Peracetic Acid | Rapid action (5–15 min); biodegradable | Flexible endoscopes, dialysis machines |
| 🔸 Alcohols (70%) | Not sterilizing — only disinfectant | Skin antiseptic, thermometer disinfection |
| 🔸 Phenol & Derivatives | Disinfectant, not sterilizer | Floors, walls, toilets |
🧴 ETHYLENE OXIDE (EtO) – IN DETAIL
✔️ Gas sterilizer for heat/moisture-sensitive items
✔️ Requires temperature: 37–63°C and humidity 30–60%
✔️ Aeration is mandatory post-sterilization to remove toxic residue
✔️ Toxic & flammable, needs strict safety precautions
⚠️ ADVANTAGES & DISADVANTAGES
| ✅ Advantages | ❌ Disadvantages |
|---|---|
| Suitable for heat-sensitive items | Toxic fumes (EtO, Formaldehyde) |
| Can penetrate packaging & lumens | Requires long time (EtO takes hours) |
| Effective against spores | May leave chemical residue |
| Some are biodegradable (peracetic acid) | Expensive equipment needed |
🧠 NURSE’S ROLE IN CHEMICAL STERILIZATION
👩⚕️ Nurses must:
🔹 Identify items requiring chemical sterilization
🔹 Ensure correct concentration & exposure time
🔹 Handle chemicals using PPE (gloves, mask, apron)
🔹 Label and store sterilized equipment properly
🔹 Ensure aeration is complete before use (especially for EtO)
🔹 Keep MSDS (Material Safety Data Sheets) accessible
🔹 Document sterilization logs
📋 COMPARISON: PHYSICAL vs CHEMICAL STERILIZATION
| 🔍 Feature | 🔥 Physical | 🧴 Chemical |
|---|---|---|
| Method | Heat/Radiation | Gases/Liquids |
| Example | Autoclave | EtO, Glutaraldehyde |
| Best For | Heat-stable items | Heat-sensitive items |
| Speed | Quick (15–60 mins) | Slower (hours) |
| Residue | None | May leave residue |
📌 MOST ASKED EXAM QUESTIONS (MCQ STYLE)
✅ Q: Which chemical sterilizer is used for plastic medical equipment?
🅰️ Ethylene oxide
✅ Q: Which chemical is both disinfectant and sterilant?
🅰️ Glutaraldehyde (2%)
✅ Q: What precaution is necessary after EtO sterilization?
🅰️ Aeration of items before use
✅ Q: Which chemical is best for endoscope sterilization?
🅰️ Peracetic acid or Glutaraldehyde
✅ Q: What is the main disadvantage of formaldehyde gas sterilization?
🅰️ Irritant and carcinogenic properties
🌟 STERILITY INDICATORS 🌟
🔖 “Don’t assume sterility — prove it with indicators!”
Sterility indicators are essential tools used to verify that sterilization conditions were achieved and that items are safe for use in patient care, especially in operation theaters (OT), CSSD, and wards.
📘 DEFINITION
🗨️ Sterility indicators are chemical or biological tools used to monitor, assess, and confirm that sterilization processes are effective and the instruments are free from all microorganisms, including spores.
✅ They help ensure patient safety and validate sterilization protocols.
🔍 CLASSIFICATION OF STERILITY INDICATORS
| 🔢 Type | 📖 Description | 💡 Examples |
|---|---|---|
| 🔸 1. Physical Indicators | Monitors actual sterilization parameters | Time, temperature, pressure gauges on autoclave |
| 🔸 2. Chemical Indicators | Change color when exposed to sterilization conditions | Indicator tape, sterilization pouches |
| 🔸 3. Biological Indicators (BIs) | Use spore-forming bacteria to test sterilization efficacy | Bacillus stearothermophilus for moist heat, Bacillus atrophaeus for dry heat |
🧪 1️⃣ PHYSICAL INDICATORS
🧯 Integrated into the sterilization equipment
✔️ Thermometers, pressure gauges, timers
✔️ Display actual values inside autoclave
✔️ Provide real-time monitoring
❗ Do not confirm sterilization by themselves
🎨 2️⃣ CHEMICAL INDICATORS
🧼 Color-changing markers that react to time/temp/chemical exposure
🧷 Classes of Chemical Indicators (As per ISO 11140-1):
| 🧪 Class | 🔍 Purpose | 💡 Example |
|---|---|---|
| 🟤 Class 1 | Process indicators | Autoclave tape (indicates item was processed) |
| 🟢 Class 2 | Specific test indicators | Bowie-Dick Test (for air removal in prevacuum autoclaves) |
| 🔵 Class 3-6 | Multi-variable indicators | Strips or labels that confirm time/temp/steam presence |
✔️ Used inside and outside of packs
✔️ Provide visual confirmation of exposure to sterilizing agent
🧫 3️⃣ BIOLOGICAL INDICATORS (BIs)
🦠 Gold standard for validating sterilization
✔️ Contain highly resistant bacterial spores
✔️ After sterilization, the indicator is incubated to check spore survival
✔️ No growth = successful sterilization
| 🧬 Sterilization Method | 🔬 Spore Used |
|---|---|
| Moist Heat (Autoclave) | Geobacillus stearothermophilus |
| Dry Heat / EtO Gas | Bacillus atrophaeus |
⏱️ Takes 24–48 hrs for results
✅ Most reliable — used weekly in hospitals
📋 SUMMARY CHART
| 🔖 Indicator Type | ✅ Detects | 📍 Placement |
|---|---|---|
| Physical | Time, temp, pressure | Autoclave machine panel |
| Chemical | Presence of sterilizing conditions | On/in pack |
| Biological | Actual microbial death | Test vial inside pack/load |
👩⚕️ NURSE’S ROLE IN USING STERILITY INDICATORS
🔹 Check for color change on chemical tapes/strips
🔹 Ensure biological indicator tests are done weekly
🔹 Do not use items without visible indicator confirmation
🔹 Maintain records/logbooks of sterilization cycles
🔹 Report any indicator failures to infection control immediately
📌 MOST ASKED EXAM QUESTIONS (MCQ STYLE)
✅ Q: Which is the most reliable method to confirm sterilization?
🅰️ Biological indicator
✅ Q: Which indicator tape changes color after autoclaving?
🅰️ Chemical (Class 1)
✅ Q: What does a positive biological indicator test mean?
🅰️ Sterilization failed (spores survived)
✅ Q: Which bacteria is used in biological indicators for steam sterilization?
🅰️ Geobacillus stearothermophilus
✅ Q: Which test checks air removal in autoclaves?
🅰️ Bowie-Dick Test
🌟 STERILE TECHNIQUE IN OT 🌟
🧴 “Maintain sterility – because even one microbe can be dangerous during surgery.”
📘 DEFINITION
🗨️ Sterile Technique refers to a set of precise practices and procedures used in the operation theatre (OT) to eliminate all microorganisms and maintain a sterile environment, especially during invasive procedures or surgeries.
✅ The goal is to prevent surgical site infections (SSIs) and ensure patient safety.
🎯 PURPOSE OF STERILE TECHNIQUE
✔️ Create a germ-free surgical field
✔️ Protect patient from post-op infections
✔️ Maintain OT asepsis and discipline
✔️ Ensure safety of staff and surgical team
🛠️ KEY PRINCIPLES OF STERILE TECHNIQUE
| 🔢 Rule | ✅ Principle |
|---|---|
| 1️⃣ | Only sterile items can touch other sterile items |
| 2️⃣ | If sterility is doubtful, it’s considered contaminated |
| 3️⃣ | Sterile field must be monitored and never left unattended |
| 4️⃣ | Edges of sterile fields (1 inch) are considered unsterile |
| 5️⃣ | Below waist or out of sight = unsterile |
| 6️⃣ | Airborne contamination must be minimized (limit traffic in OT) |
| 7️⃣ | Sterile team members must pass each other back-to-back |
🧤 COMPONENTS OF STERILE TECHNIQUE IN OT
1️⃣ Sterile Gowning & Gloving
👗 Gown and gloves must be sterile and worn without contamination
🧤 Closed gloving technique is used to maintain sterility
2️⃣ Creating a Sterile Field
📦 Open sterile drapes, instruments, and linen using aseptic technique
➕ Maintain sterile area above waist and in front
3️⃣ Preparation of Surgical Site
💧 Clean the patient’s skin with antiseptic solution (povidone-iodine or chlorhexidine)
🛑 Do not touch the prepared area with unsterile gloves
4️⃣ Handling Sterile Equipment
🛠️ Use sterile transfer forceps or sterile gloves
♻️ Avoid reaching over the sterile field
5️⃣ Environmental Controls in OT
🌬️ Maintain positive pressure airflow
🚷 Restrict unnecessary movement and personnel
🧹 Regular sterile cleaning of the OT
👩⚕️ NURSE’S ROLE IN MAINTAINING STERILE TECHNIQUE
🔹 Perform surgical hand scrub before entering sterile field
🔹 Set up sterile trolley using only sterile items
🔹 Observe for any breaks in sterility and report immediately
🔹 Re-glove or re-gown if contamination occurs
🔹 Monitor other team members for compliance
🔹 Maintain sterility of instruments and drapes
🔹 Label medications and solutions immediately after opening
🚨 SIGNS OF BREACH IN STERILITY
⚠️ Touching sterile items with bare hands
⚠️ Item falling below waist level
⚠️ Torn or wet sterile packages
⚠️ Turning back on sterile field
⚠️ Movement of non-sterile personnel into sterile zone
➡️ In such cases: replace item, re-scrub, or re-drape as needed
📌 MOST ASKED EXAM QUESTIONS (MCQ STYLE)
✅ Q: What is considered unsterile in a sterile field?
🅰️ The 1-inch outer edge of a sterile drape
✅ Q: Which part of the sterile gown is considered sterile?
🅰️ Front of the gown from chest to waist and sleeves to 2 inches above elbow
✅ Q: What should be done if a sterile glove is torn during surgery?
🅰️ Remove and reglove immediately
✅ Q: Which gloving technique is preferred in OT?
🅰️ Closed gloving
✅ Q: Which solution is most commonly used for surgical site skin preparation?
🅰️ Povidone-Iodine
🌟 DISINFECTION & DISINFECTANT 🌟
🧼 “If it’s not sterile — make it safe with disinfection.”
📘 DEFINITION
🧴 Disinfection
🗨️ A process that eliminates most pathogenic microorganisms, except bacterial spores, from inanimate objects and surfaces.
✅ Not the same as sterilization — disinfection reduces microbial load but may not kill all spores.
🧪 Disinfectant
🗨️ A chemical agent used on non-living objects to destroy or inhibit the growth of microorganisms.
🛑 Not safe for application on living tissues (unlike antiseptics).
🎯 PURPOSE OF DISINFECTION
✔️ Reduce the risk of infection from contaminated surfaces or instruments
✔️ Prepare equipment and areas for patient care
✔️ Maintain hospital hygiene standards
✔️ Control healthcare-associated infections (HAIs)
🧩 TYPES OF DISINFECTION
| 🔢 Type | 📖 Description | 💡 Example |
|---|---|---|
| 🔹 High-Level Disinfection (HLD) | Kills all organisms except high levels of bacterial spores | Glutaraldehyde, Peracetic acid |
| 🔹 Intermediate-Level Disinfection (ILD) | Kills mycobacteria, most viruses & bacteria | Alcohol, phenolics |
| 🔹 Low-Level Disinfection (LLD) | Kills some viruses and bacteria | Quaternary ammonium compounds, chlorine (low conc.) |
🧴 COMMONLY USED DISINFECTANTS
| 🧪 Disinfectant | ✅ Effective Against | 📍 Used On |
|---|---|---|
| Glutaraldehyde (2%) | Bacteria, viruses, spores (HLD) | Endoscopes, respiratory instruments |
| Sodium Hypochlorite (Bleach) | Bacteria, viruses (ILD-HLD) | Blood spills, surfaces, linens |
| 70% Alcohol (Ethanol/Isopropyl) | Bacteria, enveloped viruses (ILD) | Thermometers, stethoscopes, vials |
| Phenol & Derivatives | Bacteria, fungi (ILD) | Floors, toilets, walls |
| Quaternary Ammonium Compounds (QACs) | Gram-positive bacteria (LLD) | Furniture, beds, general surfaces |
| Hydrogen Peroxide (3–7%) | Bacteria, viruses, fungi | Surfaces, fogging areas |
🧪 FACTORS AFFECTING DISINFECTION
🔸 Type and number of microorganisms
🔸 Contact time ⏱️
🔸 Concentration of disinfectant
🔸 Presence of organic matter (e.g., blood, pus)
🔸 Surface type and pH
🧼 STEPS OF DISINFECTION PROCESS
1️⃣ Cleaning: Physically remove debris & organic matter
2️⃣ Rinsing: Clear surface of detergent
3️⃣ Disinfection: Apply disinfectant at proper concentration
4️⃣ Drying: Allow contact time and drying
5️⃣ Documentation: Record disinfection time, date, chemical used
👩⚕️ NURSE’S RESPONSIBILITIES
🔹 Use appropriate disinfectant based on equipment risk level
🔹 Follow correct dilution and contact time
🔹 Wear PPE (gloves, mask) when handling chemicals
🔹 Label and store chemicals properly
🔹 Educate staff on disinfection protocols
🔹 Maintain disinfection logs
📌 MOST ASKED EXAM QUESTIONS (MCQ STYLE)
✅ Q: What is the difference between disinfectant and antiseptic?
🅰️ Disinfectants are used on non-living surfaces; antiseptics on living tissues.
✅ Q: Which disinfectant is preferred for blood spills?
🅰️ Sodium hypochlorite (1%)
✅ Q: What level of disinfection is glutaraldehyde?
🅰️ High-level disinfectant
✅ Q: Which disinfectant is commonly used for thermometers?
🅰️ 70% Alcohol
✅ Q: Why is cleaning necessary before disinfection?
🅰️ To remove organic matter that can reduce disinfectant effectiveness
🌟 ASEPTIC TECHNIQUE 🌟
🧴 “Prevent the invisible threat — maintain asepsis every step of care.”
📘 DEFINITION
🗨️ Aseptic Technique refers to a set of specific practices and procedures performed under strictly sterile conditions to eliminate the introduction of pathogenic microorganisms into sterile environments.
✅ It is essential in surgical settings, dressing changes, invasive procedures, and catheter insertions.
🎯 PURPOSE OF ASEPTIC TECHNIQUE
✔️ Prevent healthcare-associated infections (HAIs)
✔️ Maintain sterility of medical equipment and procedures
✔️ Ensure patient safety during invasive care
✔️ Promote infection-free recovery
🧪 TYPES OF ASEPTIC TECHNIQUES
| 🔢 Type | 📖 Description | 💡 Examples |
|---|---|---|
| 🧼 Medical Asepsis (Clean Technique) | Reduces number & spread of microbes | Hand hygiene, PPE, clean gloves |
| 🧴 Surgical Asepsis (Sterile Technique) | Eliminates all microorganisms | OT procedures, central line insertion |
🧩 PRINCIPLES OF ASEPTIC TECHNIQUE
| ✅ Principle | 📌 Description |
|---|---|
| 1️⃣ Sterile to sterile remains sterile | Do not touch sterile items with non-sterile hands |
| 2️⃣ If in doubt, consider it contaminated | Always err on the side of caution |
| 3️⃣ Keep sterile items above waist | Below waist = non-sterile |
| 4️⃣ Avoid reaching over sterile field | Reduces contamination risk |
| 5️⃣ Maintain dry sterile fields | Moisture draws in bacteria |
| 6️⃣ Minimize air currents and traffic | Reduces airborne contamination |
🧰 EXAMPLES OF PROCEDURES REQUIRING ASEPTIC TECHNIQUE
🩺 Injections & IV therapy
💉 Wound dressing changes
👩⚕️ Urinary catheterization
🔬 Collection of sterile specimens (e.g., blood culture)
🏥 Surgical procedures
🛏️ Tracheostomy or central line care
🧤 ASEPTIC TECHNIQUE CHECKLIST
✅ Perform hand hygiene thoroughly
✅ Wear sterile gloves, mask, gown as needed
✅ Prepare a sterile field using sterile drapes
✅ Use sterile instruments and avoid touching non-sterile surfaces
✅ Avoid speaking, sneezing, or coughing over sterile field
✅ Dispose used items in biomedical waste bins appropriately
👩⚕️ NURSE’S ROLE IN ASEPTIC TECHNIQUE
🔹 Ensure compliance with aseptic guidelines
🔹 Use PPE correctly and consistently
🔹 Teach patients and caregivers about infection control
🔹 Report and correct breaks in asepsis immediately
🔹 Supervise students or junior staff in sterile procedures
🔹 Maintain records of sterile procedures
📌 MOST ASKED EXAM QUESTIONS (MCQ STYLE)
✅ Q: What is the main goal of aseptic technique?
🅰️ To prevent introduction of pathogens during procedures
✅ Q: Which area is considered unsterile in a sterile field?
🅰️ Outer 1 inch of the sterile field
✅ Q: What technique is used in catheter insertion?
🅰️ Surgical asepsis (sterile technique)
✅ Q: Which of the following breaks aseptic technique?
🅰️ Reaching over a sterile field
✅ Q: Why must sterile gloves be kept above the waist?
🅰️ Below the waist is considered contaminated
🌟 ISOLATION vs QUARANTINE 🌟
🚫 “Separate to protect — isolation and quarantine break the chain of infection.”
📘 DEFINITIONS
🚷 Isolation
🗨️ Isolation is the separation of people who are already infected with a contagious disease from those who are not infected, to prevent spread of the disease.
✅ Used when the person is symptomatic or confirmed positive.
🏠 Quarantine
🗨️ Quarantine is the restriction of movement of individuals who have been exposed to a contagious disease, to monitor if they develop symptoms.
✅ Used for asymptomatic individuals with known or suspected exposure.
🔁 COMPARISON: ISOLATION vs QUARANTINE
| 🧾 Criteria | 🚷 Isolation | 🏠 Quarantine |
|---|---|---|
| 📌 Purpose | Separate infected individuals | Restrict movement of exposed individuals |
| 🧬 Disease Status | Symptomatic or tested positive | Asymptomatic but at risk |
| 🕒 Duration | Until not infectious (per guidelines) | Incubation period (e.g., 5–14 days) |
| 🏥 Setting | Hospitals, isolation rooms | Home, quarantine facility |
| 🧤 Precautions | Strict PPE, medical supervision | Self-monitoring, hygiene, mask use |
🧪 EXAMPLES
| 🚷 Isolation | 🏠 Quarantine |
|---|---|
| COVID-19 positive patient | Close contact of COVID case |
| Active tuberculosis case | Family member of TB patient |
| Chickenpox outbreak case | Student exposed in classroom |
| Measles infection | Traveler from endemic area |
🧠 NURSE’S ROLE IN ISOLATION & QUARANTINE
👩⚕️ Nurses play a vital role in implementing, monitoring, and educating about these measures:
🔹 Identify & report cases requiring isolation/quarantine
🔹 Educate patient/family on hygiene and safety practices
🔹 Monitor vitals, symptoms, and psychological status
🔹 Ensure proper PPE use and waste disposal
🔹 Maintain infection control logs and reports
🔹 Support patients emotionally during isolation
📌 MOST ASKED EXAM QUESTIONS (MCQ STYLE)
✅ Q: Isolation is used for which type of individuals?
🅰️ Infected or symptomatic patients
✅ Q: Quarantine is applied to whom?
🅰️ People exposed but not showing symptoms
✅ Q: What is the purpose of quarantine?
🅰️ To observe if exposed individuals develop symptoms
✅ Q: What is the key difference between isolation and quarantine?
🅰️ Isolation = sick person, Quarantine = exposed person
✅ Q: What is the role of a nurse during isolation care?
🅰️ Ensure aseptic care, emotional support, and monitor infection
🌟 AUTOCLAVE 🌟
🔥 “Steam under pressure — the gold standard in sterilization.”
📘 DEFINITION
🗨️ Autoclave is a device that uses steam under pressure to sterilize surgical instruments, dressings, glassware, and other heat-resistant items by destroying all microorganisms, including spores.
✅ It’s the most commonly used method in hospitals and laboratories for moist heat sterilization.
🎯 PURPOSE OF AUTOCLAVING
✔️ Achieve complete sterilization
✔️ Eliminate bacteria, viruses, fungi, and spores
✔️ Maintain asepsis in surgical and clinical areas
✔️ Support infection control and patient safety
🔧 WORKING PRINCIPLE
🧪 Moist Heat (Steam) under Pressure
- Increases boiling point of water to achieve higher temperatures
- Kills microbes by protein denaturation & coagulation
- Pressure is used only to raise temperature, NOT to kill microbes
📊 STANDARD PARAMETERS
| 🔥 Temp | 💨 Pressure | ⏱️ Time |
|---|---|---|
| 121°C | 15 psi (pounds per square inch) | 15–20 minutes |
| 💡 OR | 134°C | 30 psi |
📦 MATERIALS THAT CAN BE AUTOCLAVED
✅ Surgical instruments
✅ Metal tools
✅ Glassware
✅ Linen packs
✅ Culture media (agar)
✅ Rubber tubing (autoclavable)
🚫 NOT suitable for: ❌ Powders
❌ Oils
❌ Heat-sensitive plastics
❌ Electronics
🧰 PARTS OF AN AUTOCLAVE
🔹 Chamber – Where items are placed
🔹 Steam Generator – Produces steam
🔹 Pressure Gauge – Monitors internal pressure
🔹 Safety Valve – Prevents overpressure
🔹 Timer & Thermostat – Sets time & temperature
🔹 Exhaust System – Releases used steam
🧪 TYPES OF AUTOCLAVES
| 🔢 Type | 📖 Description |
|---|---|
| 🔹 Gravity Displacement | Steam displaces air by gravity; common in hospitals |
| 🔹 Pre-vacuum (High-Speed) | Air removed by vacuum pump; ensures deep penetration |
| 🔹 Tabletop Autoclave | Small size, used in clinics and labs |
| 🔹 Flash Autoclave | Rapid sterilization for emergencies (higher temp, short time) |
✅ AUTOCLAVE CYCLE STEPS
1️⃣ Loading – Place dry, clean, unsealed items
2️⃣ Heating – Steam enters the chamber
3️⃣ Sterilizing – Set temp & pressure reached
4️⃣ Exhausting – Steam released, pressure drops
5️⃣ Drying – Items dry before removal
🧠 STERILIZATION MONITORING IN AUTOCLAVE
| 🔍 Type | 💡 Description |
|---|---|
| 📋 Physical Indicators | Time, temperature, pressure readings |
| 🎨 Chemical Indicators | Autoclave tape changes color when exposed |
| 🧫 Biological Indicators (BIs) | Spores used to confirm sterilization (Geobacillus stearothermophilus) |
👩⚕️ NURSE’S ROLE IN AUTOCLAVE USE
🔹 Load items correctly (avoid overloading)
🔹 Check temperature, pressure & time settings
🔹 Use and check indicator tapes & strips
🔹 Keep autoclave clean & well-maintained
🔹 Document each sterilization cycle
🔹 Ensure items are dry before removing
🔹 Report faults or failures immediately
📌 MOST ASKED EXAM QUESTIONS (MCQ STYLE)
✅ Q: What is the standard temperature and pressure used in an autoclave?
🅰️ 121°C at 15 psi for 15–20 minutes
✅ Q: What is used to test the effectiveness of autoclave sterilization?
🅰️ Biological indicator using Geobacillus stearothermophilus
✅ Q: Which items should NOT be autoclaved?
🅰️ Oils, powders, plastics
✅ Q: What principle does an autoclave use?
🅰️ Steam under pressure
✅ Q: What should be done if the autoclave tape does not change color?
🅰️ Repeat sterilization — conditions were not met
🌟 BIOMEDICAL WASTE HANDLING 🌟
🛑 “Right waste, right bin, right way — protect health and environment every day!”
📘 DEFINITION
🗨️ Biomedical Waste refers to any waste generated during diagnosis, treatment, immunization of humans or animals or in research activities related to healthcare, including sharps and laboratory waste.
✅ BMW includes infectious, hazardous, and regulated medical waste.
📜 GOVERNING GUIDELINES
📅 Biomedical Waste Management Rules, 2016 (by MoEFCC, India)
📌 Amended in 2018, 2019, and 2022 to strengthen segregation, barcoding, and occupational safety.
🗂️ CATEGORIES OF BIOMEDICAL WASTE (As per BMW Rules, 2016)
| 🔢 Category | 💉 Type of Waste | 🗑️ Bin Color | 🔥 Disposal Method |
|---|---|---|---|
| Category 1 | Human & animal anatomical waste | 🟡 Yellow | Incineration |
| Category 2 | Soiled waste (e.g., dressings, cotton) | 🟡 Yellow | Incineration/autoclaving |
| Category 3 | Expired or discarded medicines | 🟡 Yellow | Incineration/secure landfill |
| Category 4 | Chemical waste (used disinfectants) | 🟡 Yellow | Incineration/neutralization |
| Category 5 | Contaminated waste (tubes, catheters) | 🔴 Red | Autoclaving, shredding |
| Category 6 | Waste sharps (needles, blades) | ⚪ White (Puncture-proof) | Autoclave + mutilation |
| Category 7 | Glassware (bottles, slides) | 🔵 Blue | Disinfection & recycling |
🗑️ COLOR CODING SYSTEM (🆕 As per Latest Amendment)
| 🎨 Color | ✅ Used For | 💡 Example | 🔥 Treatment |
|---|---|---|---|
| 🟡 Yellow | Infectious, soiled, anatomical waste | Body parts, cotton swabs | Incineration |
| 🔴 Red | Contaminated recyclable plastic | IV sets, tubing, syringes (without needles) | Autoclave + Shred |
| ⚪ White (translucent) | Sharps waste | Needles, scalpels, lancets | Autoclave + Mutilation |
| 🔵 Blue | Glassware | Medicine bottles, broken ampoules | Disinfection & recycling |
🔄 BMW MANAGEMENT PROCESS
1️⃣ Segregation at point of generation
2️⃣ Color-coded bagging
3️⃣ Barcoding & labelling
4️⃣ Transport to storage area
5️⃣ Handover to CBMWTF (Common Biomedical Waste Treatment Facility)
6️⃣ Treatment & disposal
7️⃣ Documentation & reporting
🧤 NURSE’S ROLE IN BMW HANDLING
👩⚕️ Nurses are frontline staff in safe waste disposal:
🔹 Segregate waste as per color coding
🔹 Label bags with barcode and biohazard symbol
🔹 Wear PPE (gloves, mask, apron) while handling waste
🔹 Use needle destroyers for sharps
🔹 Avoid overfilling or leaking bags
🔹 Report accidents or needle-stick injuries immediately
🔹 Maintain waste handling records regularly
🚨 SAFETY TIPS FOR HANDLING BIOMEDICAL WASTE
✅ Do not recap needles
✅ Always close bags before disposal
✅ Never mix general and biomedical waste
✅ Follow 3 R’s: Reduce, Reuse (safely), Recycle (approved)
✅ Use biohazard symbol on bags/containers
✅ Ensure regular training and audits
📌 MOST ASKED EXAM QUESTIONS (MCQ STYLE)
✅ Q: Which color bag is used for soiled dressings?
🅰️ Yellow
✅ Q: Needle and syringe are disposed in which container?
🅰️ White puncture-proof container (needles), red bag (syringes without needles)
✅ Q: Which agency treats biomedical waste in India?
🅰️ CBMWTF (Common Biomedical Waste Treatment Facility)
✅ Q: What is the main principle of BMW management?
🅰️ Segregation at source
✅ Q: Which symbol is mandatory on biomedical waste containers?
🅰️ Biohazard symbol