genetic-patho-unit-3-Hematological tests for the diagnosis of blood disorders
Hematological tests for the diagnosis of blood disorders
🩸 Assessment and Monitoring of Disease Conditions: Blood Tests – Hemoglobin (Hb)
🔍 What is Hemoglobin?
Hemoglobin (Hb) is a protein found in red blood cells (RBCs) responsible for carrying oxygen from the lungs to tissues and carbon dioxide back to the lungs. It is composed of heme (iron-containing pigment) and globin (protein chains).
🧪 Why Measure Hemoglobin?
Measurement of hemoglobin is a key component of a Complete Blood Count (CBC) and is used for:
- ✅ Diagnosis of anemia or polycythemia
- ✅ Monitoring response to treatment
- ✅ Preoperative screening
- ✅ Detecting chronic disease impact (e.g., renal failure, cancers, bleeding disorders)
📊 Normal Hemoglobin Ranges
| Group | Hemoglobin Range (g/dL) |
|---|---|
| Adult Male | 13.5 – 17.5 |
| Adult Female | 12.0 – 15.5 |
| Children | 11.0 – 13.5 |
| Pregnant Women | >11.0 |
(Ranges may slightly vary depending on lab standards)
🩺 Indications for Hemoglobin Test
- Suspected anemia (fatigue, pallor, breathlessness)
- Excessive bleeding (trauma, menstruation, ulcers)
- Nutritional deficiency (iron, B12, folate)
- Chronic diseases (kidney disease, cancer)
- Polycythemia symptoms (ruddy complexion, headache, dizziness)
🧠 Interpretation of Hemoglobin Levels
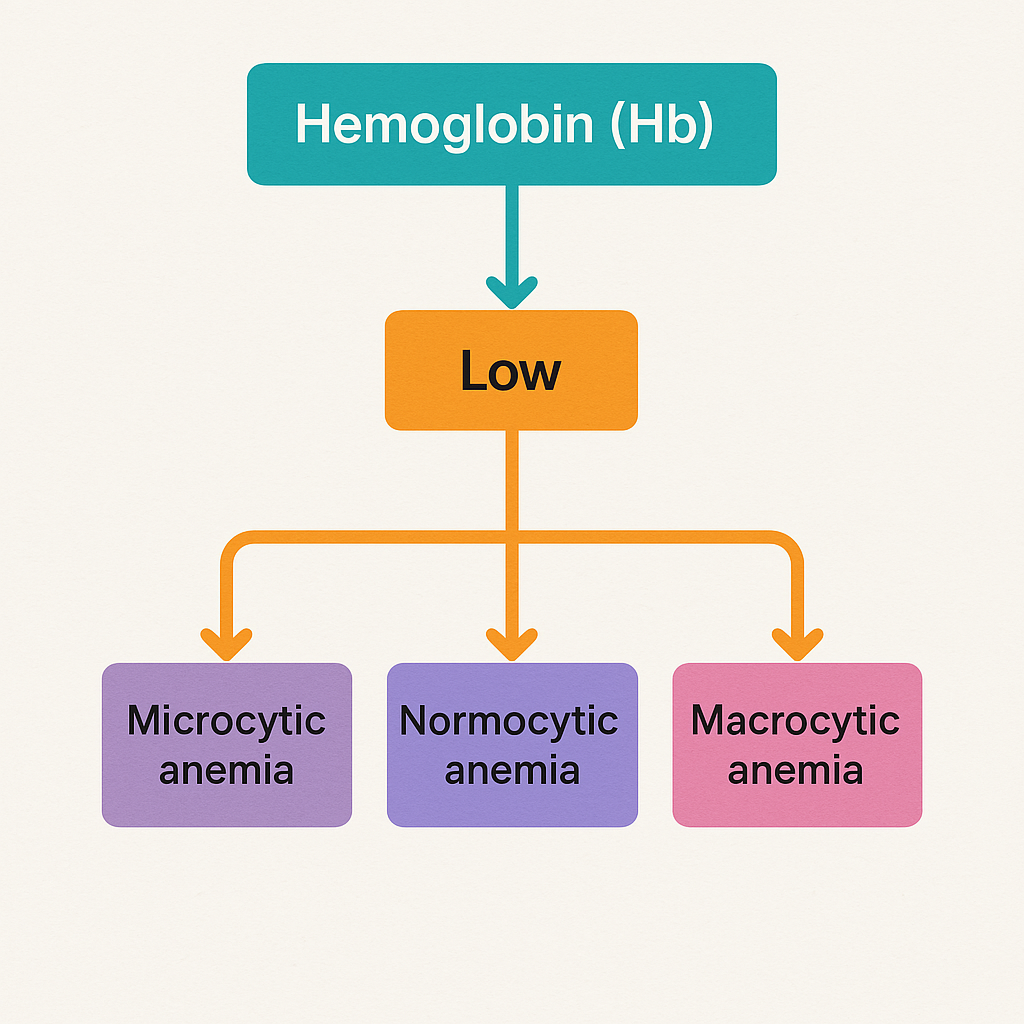
🔽 Low Hemoglobin (Anemia)
May be due to:
- 🔸 Iron deficiency (microcytic anemia)
- 🔸 Vitamin B12/Folic acid deficiency (macrocytic anemia)
- 🔸 Chronic kidney disease (reduced erythropoietin)
- 🔸 Blood loss (trauma, GI bleeding, menstruation)
- 🔸 Bone marrow suppression (aplastic anemia, cancer)
🔎 Symptoms:
- Fatigue, pale skin, shortness of breath, dizziness, cold extremities
🔼 High Hemoglobin (Polycythemia)
May be due to:
- 🔺 Polycythemia vera (bone marrow disorder)
- 🔺 Chronic hypoxia (COPD, high altitude)
- 🔺 Dehydration (relative increase)
- 🔺 Erythropoietin-secreting tumors
🔎 Symptoms:
- Headache, visual disturbances, hypertension, risk of clotting
🩹 Nurse’s Role in Hemoglobin Monitoring
✔️ Assessment:
- Observe for signs of anemia (pallor, fatigue, tachycardia)
- Monitor dietary intake (iron, folate, B12)
- Evaluate for bleeding (stool, menstrual, surgical sites)
- Track oxygen saturation and perfusion
✔️ Action/Intervention:
- Administer iron supplements or injections as prescribed
- Ensure adequate hydration and nutrition
- Monitor RBC transfusion (in severe anemia)
- Educate patient on iron-rich diet and medication compliance
✔️ Monitoring Trends:
- Baseline Hb before and after treatments
- Repeat testing in:
- Chronic illnesses
- Postoperative care
- Dialysis or chemotherapy patients
📌 Key Points Summary
- Hemoglobin is crucial for oxygen transport and clinical diagnosis.
- Anemia and polycythemia represent the two major abnormal findings.
- It is a routine and essential blood test for many systemic diseases.
- Nurses play a vital role in assessment, intervention, and patient education.
🧪 Assessment and Monitoring of Disease Conditions via Blood Tests: WBC & Platelet Count
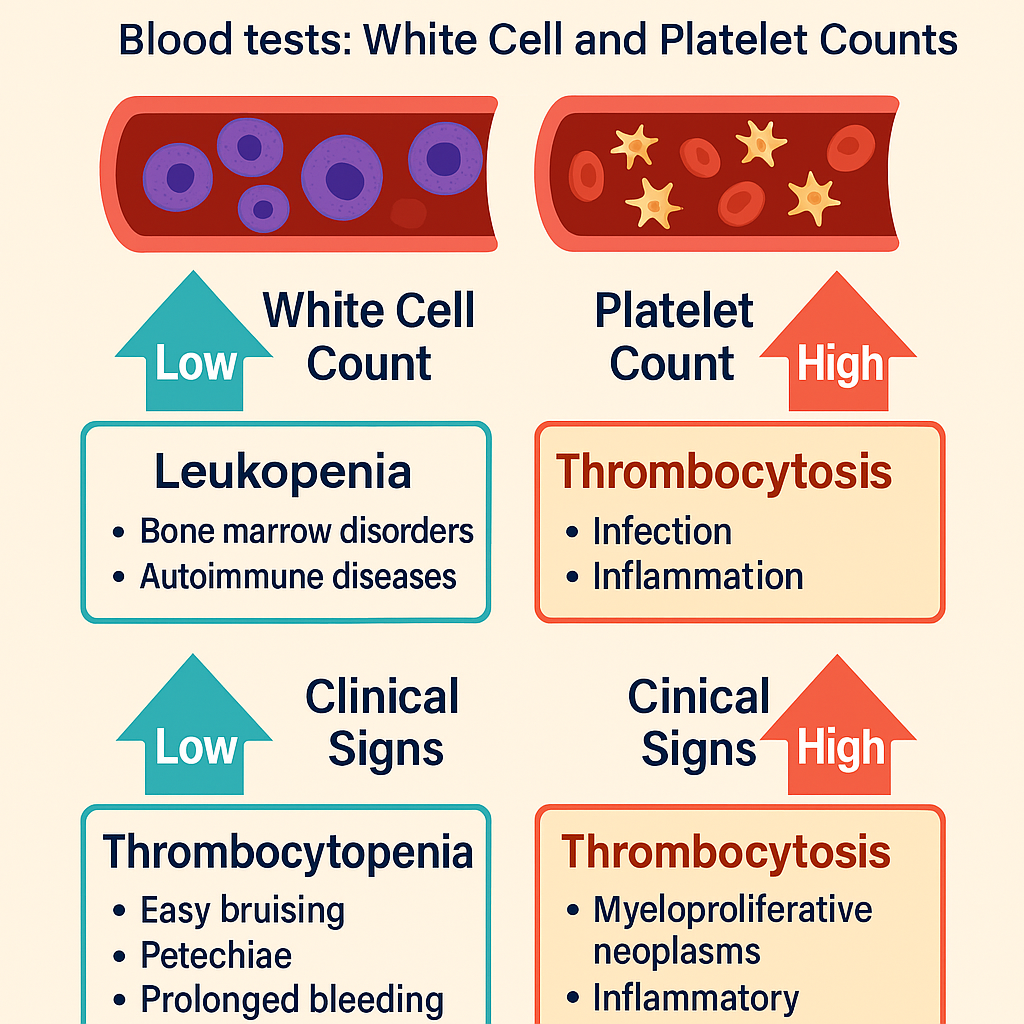
1️⃣ White Blood Cell (WBC) Count
🩸 Definition:
White blood cells are essential components of the immune system, helping the body to fight infections, inflammation, and malignancies. The WBC count evaluates the number of leukocytes per microliter of blood.
📊 Normal Range:
- Total WBC: 4,000 – 11,000 /mm³
- Differential count (percentage):
- Neutrophils: 50–70%
- Lymphocytes: 20–40%
- Monocytes: 2–8%
- Eosinophils: 1–4%
- Basophils: 0.5–1%
🔍 Uses of WBC Count in Disease Monitoring:
| Condition | WBC Findings |
|---|---|
| Bacterial infection | ↑ Neutrophils (neutrophilia) |
| Viral infection | ↑ Lymphocytes (lymphocytosis) |
| Parasitic/allergic reactions | ↑ Eosinophils (eosinophilia) |
| Bone marrow failure, aplastic anemia | ↓ WBC (leukopenia) |
| Leukemia | ↑ WBC (leukocytosis), abnormal cells |
| Sepsis or severe infection | ↑ or ↓ WBC (depending on stage) |
🩺 Nursing Assessment Points – WBC Monitoring:
- Monitor for fever, chills, and sore throat (signs of infection)
- Use protective precautions in leukopenic patients (e.g., reverse isolation)
- Monitor drug-induced changes (e.g., chemotherapy suppresses WBCs)
- Support and educate immunocompromised patients
2️⃣ Platelet Count (Thrombocyte Count)
🩸 Definition:
Platelets (thrombocytes) are cell fragments involved in blood clotting. The platelet count measures the number of platelets per microliter of blood and is vital in assessing bleeding disorders and bone marrow function.
📊 Normal Range:
- 150,000 – 400,000 /mm³
🔍 Uses of Platelet Count in Disease Monitoring:
| Condition | Platelet Findings |
|---|---|
| Thrombocytopenia (low platelets) | < 150,000/mm³ |
| Thrombocytosis (high platelets) | > 400,000/mm³ |
| Dengue fever | ↓ Platelets |
| Bone marrow suppression (e.g., chemo) | ↓ Platelets |
| ITP (Idiopathic thrombocytopenic purpura) | ↓ Platelets |
| Infections, inflammation | ↑ or ↓ Platelets |
| Myeloproliferative disorders | ↑ Platelets |
⚠️ Clinical Signs of Thrombocytopenia:
- Easy bruising
- Petechiae (tiny red skin spots)
- Prolonged bleeding from cuts
- Gum or nose bleeding
- Hematuria or blood in stools
🩺 Nursing Assessment Points – Platelet Monitoring:
- Avoid IM injections, rectal exams, or invasive procedures if platelets <50,000
- Use soft toothbrush and electric razor
- Monitor for bleeding, especially in stool, urine, gums
- Administer platelet transfusion if critically low
- Educate on bleeding precautions
🔄 Integrated Role in Monitoring Disease Conditions
| Blood Test | Purpose | Clinical Relevance |
|---|---|---|
| WBC Count | Detect infection, inflammation, bone marrow status | Aids in early diagnosis of infections and cancers |
| Platelet Count | Assess bleeding risk and clotting ability | Critical in managing dengue, ITP, chemo patients |
🩸 Assessment and Monitoring of Disease Conditions via Blood Tests: Packed Cell Volume (PCV)
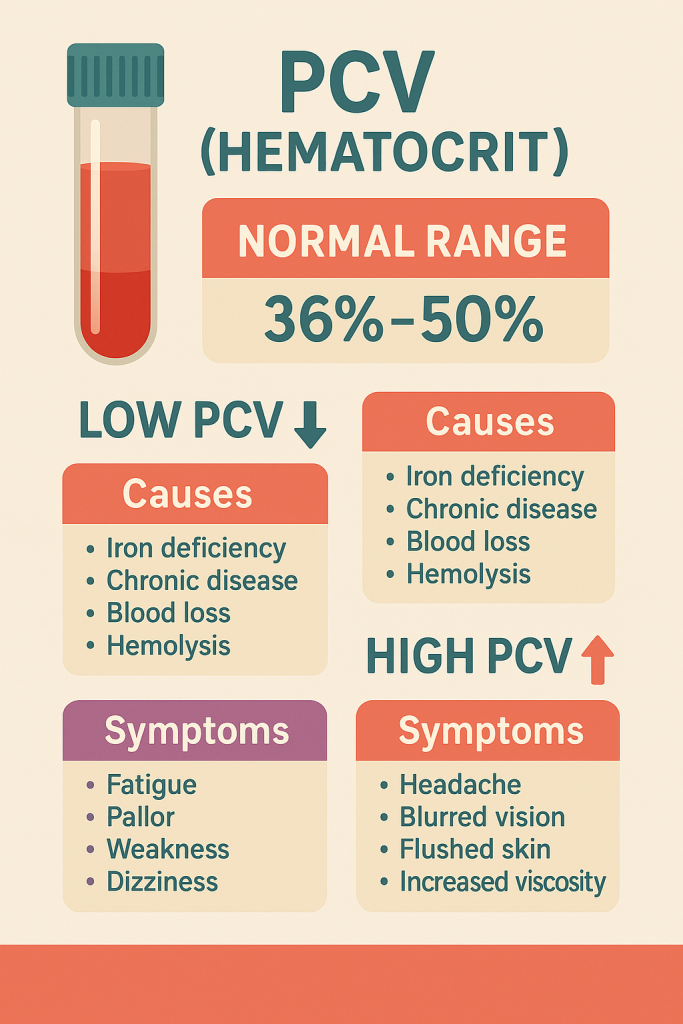
🔬 What is PCV (Packed Cell Volume)?
Packed Cell Volume (PCV) or hematocrit is the percentage of whole blood that is made up of red blood cells (RBCs). It is measured after centrifuging a blood sample and reflects the oxygen-carrying capacity of blood.
📊 Normal Reference Values:
| Group | PCV / Hematocrit (%) |
|---|---|
| Adult males | 40 – 54% |
| Adult females | 36 – 48% |
| Children | 35 – 45% |
| Newborns | 44 – 64% |
| Pregnancy | 32 – 42% |
Slight variations may occur depending on the laboratory.
🧪 Clinical Importance of PCV
PCV is used to:
- ✅ Evaluate anemia and polycythemia
- ✅ Monitor dehydration status
- ✅ Assess bleeding or hemorrhage
- ✅ Guide fluid therapy, transfusions, or treatment of chronic illnesses
🔽 Low PCV (Anemia or Hemodilution)
🩻 Causes:
- Iron, folate, or B12 deficiency
- Chronic diseases (renal failure, cancer)
- Acute blood loss
- Bone marrow suppression
- Hemolysis (autoimmune or drug-induced)
🧠 Symptoms:
- Fatigue, pallor, weakness, dizziness, breathlessness
🔼 High PCV (Polycythemia or Hemoconcentration)
🩻 Causes:
- Polycythemia vera (bone marrow overproduction)
- Dehydration (relative increase)
- Chronic hypoxia (COPD, smoking, high altitude)
- Excessive erythropoietin production (e.g., renal tumors)
🧠 Symptoms:
- Headache, blurred vision, flushed skin, increased blood viscosity, clot risk
🩺 Nursing Assessment and Monitoring Role
✔️ Before Test:
- Ensure correct sample handling in EDTA tubes
- Explain procedure and purpose to the patient
- Assess hydration and recent fluid status
✔️ Monitoring Disease Progress:
- Anemia: Track PCV alongside hemoglobin
- Dehydration: Rising PCV with clinical signs (dry tongue, low BP)
- Bleeding disorders: Sudden drop in PCV
- Renal or cardiac patients: Monitor to adjust fluid/oxygen therapy
✔️ Interventions Based on PCV:
- Low PCV:
- Iron/B12/folate supplements
- RBC transfusions
- Monitor for bleeding sources
- High PCV:
- Maintain hydration
- Administer anticoagulants if risk of thrombosis
- Monitor for signs of hypoxia or polycythemia
🧠 Clinical Integration Table
| PCV Status | Possible Conditions | Nursing Considerations |
|---|---|---|
| ↓ Low PCV | Anemia, blood loss, chronic disease | Check fatigue, bleeding, oxygen saturation |
| ↑ High PCV | Polycythemia vera, dehydration, COPD | Hydration status, clot risk, pulse, oxygen therapy |
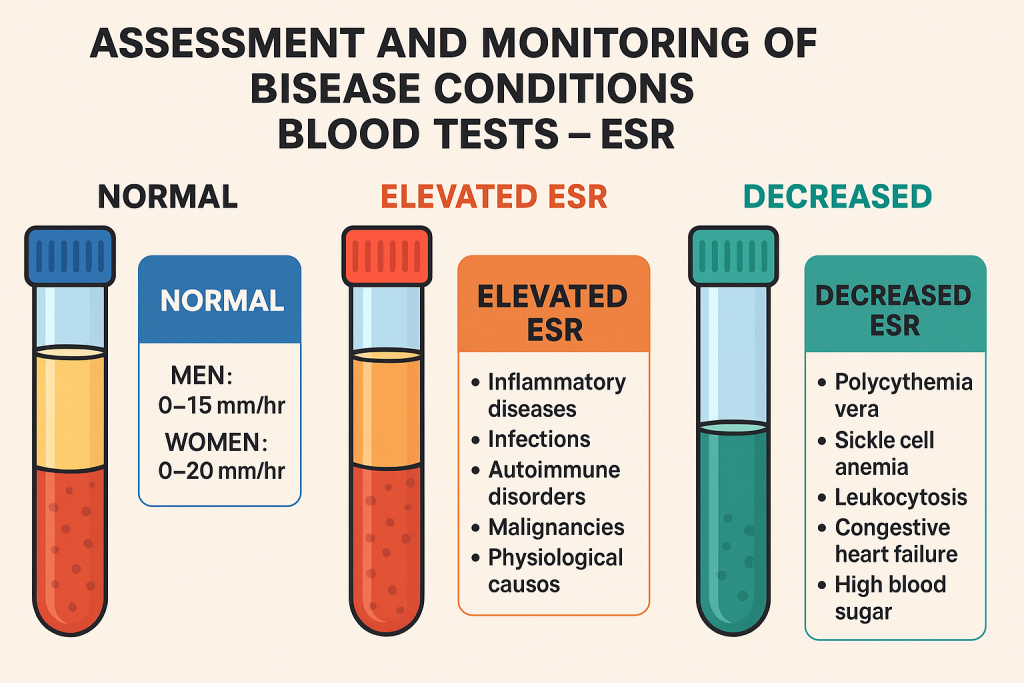
🧪 Assessment and Monitoring of Disease Conditions via Blood Tests: ESR (Erythrocyte Sedimentation Rate)
🔬 What is ESR?
Erythrocyte Sedimentation Rate (ESR) is a non-specific test that measures how quickly red blood cells (RBCs) settle at the bottom of a vertical tube in one hour. It is an indirect measure of inflammation in the body.
- When there is inflammation, certain proteins (e.g., fibrinogen) increase in the blood, causing RBCs to clump together and settle faster.
- Thus, a high ESR often reflects inflammatory or infectious processes.
📊 Normal ESR Values (Westergren method):
| Group | ESR (mm/hr) |
|---|---|
| Men | 0–15 |
| Women | 0–20 |
| Children | 0–10 |
| Elderly (both sexes) | Slightly higher acceptable range |
🩺 Clinical Utility of ESR
Though non-specific, ESR is widely used to:
- ✅ Detect inflammation, infection, or autoimmune activity
- ✅ Monitor the progression or response to treatment
- ✅ Aid in diagnosis of chronic diseases
🧪 Conditions with Elevated ESR
| System/Disorder | Examples |
|---|---|
| 🔥 Inflammatory diseases | Rheumatoid arthritis, SLE, vasculitis |
| 🦠 Infections | Tuberculosis, osteomyelitis, pelvic abscess |
| 🧬 Autoimmune disorders | Polymyalgia rheumatica, temporal arteritis |
| 💢 Malignancies | Lymphoma, multiple myeloma |
| 🚺 Physiological causes | Pregnancy, aging, menstruation |
| 📉 Anemia | Reduced RBC count allows faster sedimentation |
🔽 Conditions with Decreased ESR
- Polycythemia vera
- Sickle cell anemia
- Leukocytosis
- Congestive heart failure
- High blood sugar (severe diabetes)
🩺 Nurse’s Role in ESR Monitoring
✔️ Before Testing
- Ensure the sample is taken from a vein into an anticoagulated test tube.
- Instruct patient to avoid vigorous exercise or infection, if possible, as these can falsely elevate ESR.
✔️ Assessment & Monitoring
- Monitor ESR in chronic inflammatory diseases to assess response to treatment (e.g., RA, TB)
- Use ESR along with CRP (C-reactive protein) for better diagnostic accuracy
- Document trends rather than a single value, as ESR changes slowly
✔️ Interventions
- If ESR is elevated, assess for:
- Pain, fever, swelling, fatigue
- Suspected infection, autoimmune activity, or malignancy
- Coordinate further diagnostic tests (CBC, imaging, serology)
🧠 Summary of Clinical Correlation
| ESR Level | Clinical Implication |
|---|---|
| Normal | No active inflammation/infection |
| Moderately ↑ | Mild inflammation, early-stage infection |
| Markedly ↑ | Active chronic disease (RA, TB, SLE), malignancy |
| ↓ Decreased | May suggest polycythemia, sickle cells, microcytosis |
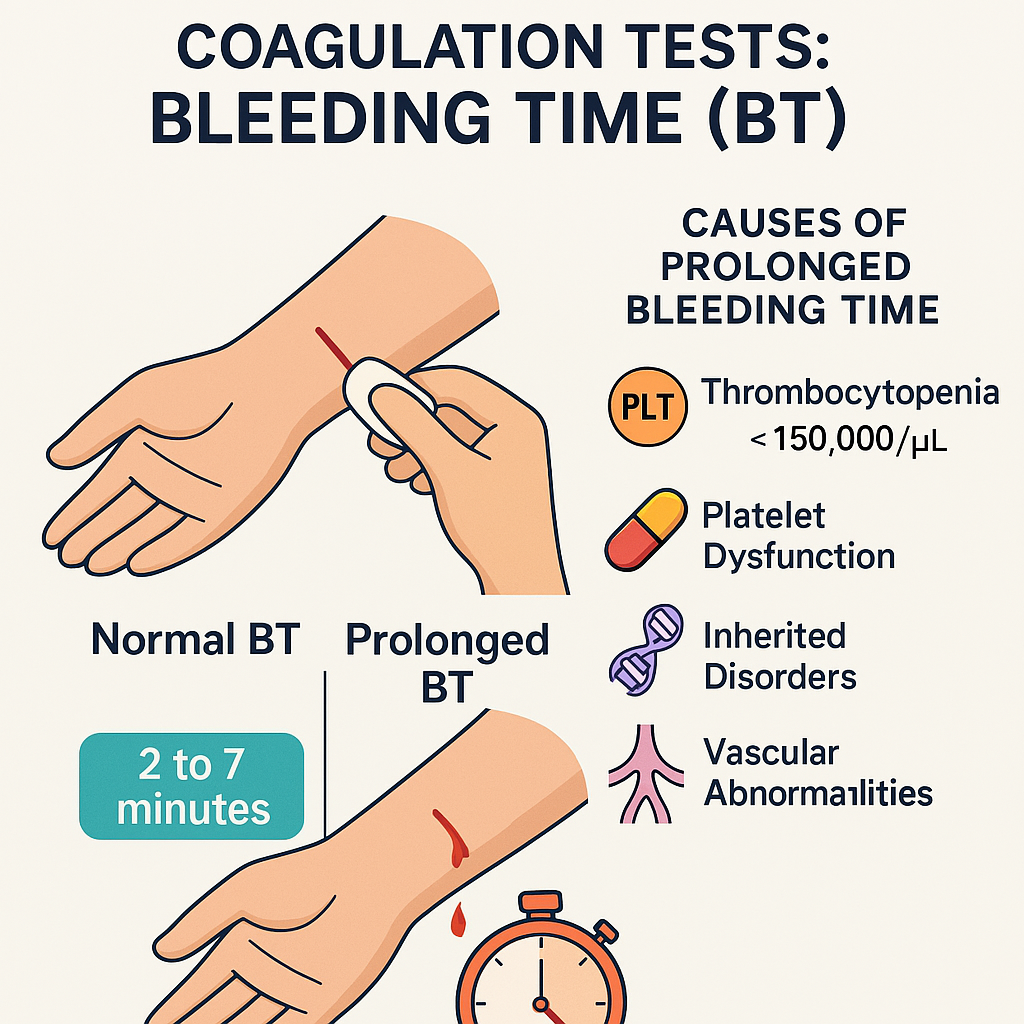
🩸 Assessment and Monitoring of Disease Conditions via Coagulation Tests: Bleeding Time (BT)
🔬 What is Bleeding Time (BT)?
Bleeding Time (BT) is a screening test that measures the duration it takes for bleeding to stop after a standardized skin incision. It is used to assess the function of platelets and capillary integrity, not the coagulation cascade directly.
🧪 Bleeding time reflects primary hemostasis – i.e., platelet adhesion, aggregation, and interaction with the vessel wall.
📊 Normal Reference Range:
- BT: 2 to 7 minutes (varies by method used)
- Ivy method: 3–7 minutes
- Duke method: 1–3 minutes
Prolonged BT indicates a defect in platelet number or function.
🔍 Clinical Indications for BT Testing
- Evaluation of unexplained bleeding or bruising
- Preoperative assessment (especially in those with bleeding history)
- Diagnosis of platelet disorders
- Monitoring antiplatelet therapy (e.g., aspirin, clopidogrel)
- Investigation of vascular disorders or von Willebrand disease
📉 Causes of Prolonged Bleeding Time
| Category | Examples |
|---|---|
| 🩺 Thrombocytopenia | Platelet count < 150,000/μL |
| ⚠️ Platelet Dysfunction | Aspirin/NSAID use, uremia, liver disease |
| 🧬 Inherited Disorders | von Willebrand disease, Bernard-Soulier syndrome |
| 🔬 Vascular Abnormalities | Ehlers-Danlos syndrome, scurvy |
✅ Bleeding Time – What It Does Not Assess
- Coagulation factor deficiencies (e.g., hemophilia A or B)
- Secondary hemostasis
- Fibrinolysis
Thus, it is not affected by clotting factor levels, and a normal BT doesn’t rule out coagulation disorders.
🩺 Nurse’s Role in BT Testing and Monitoring
✔️ Before the Test
- Explain the procedure: a small incision will be made, and bleeding is observed.
- Avoid testing in patients on aspirin, antiplatelets, or NSAIDs, unless assessing their effect.
- Do not perform in patients with very low platelets or hemophilia (risk of prolonged bleeding).
✔️ During and After the Test
- Monitor time with a stopwatch.
- Apply standardized filter paper every 30 seconds (Ivy method).
- Stop timing once bleeding ceases.
- Apply pressure dressing to the site to prevent further bleeding.
✔️ In Clinical Practice
- Use BT trends to monitor therapy effectiveness
- Report prolonged bleeding time to the physician, especially in preoperative cases
- Educate patients about signs of bleeding and when to seek care
🧠 Summary of Clinical Interpretation
| BT Result | Interpretation |
|---|---|
| Normal BT | Normal platelet function and capillary integrity |
| Prolonged BT | Thrombocytopenia, platelet dysfunction, vascular defect |
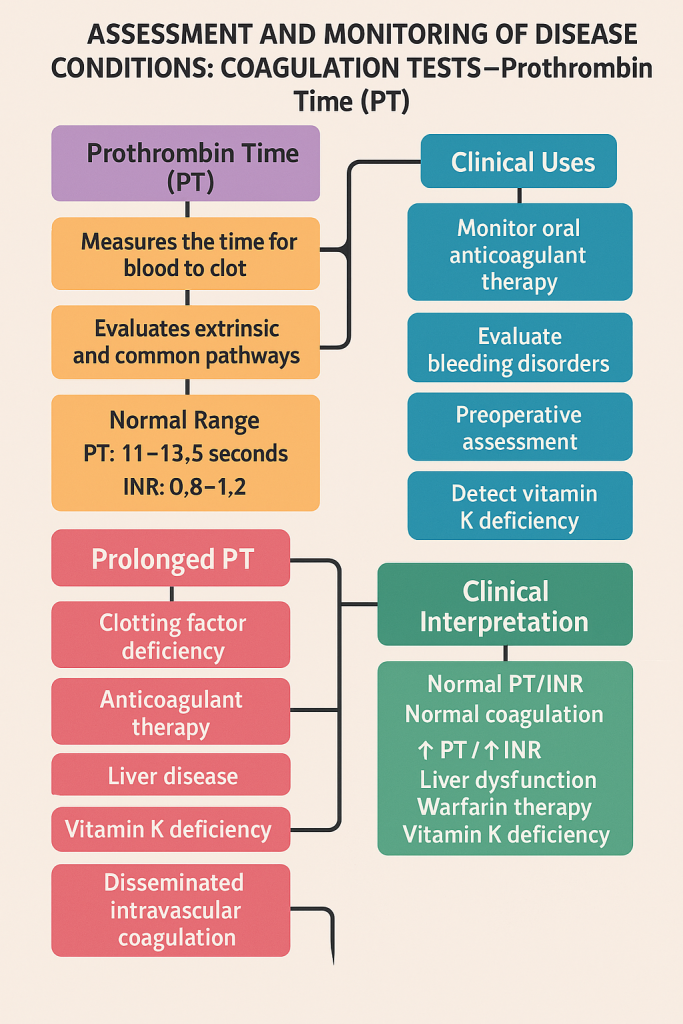
🧪 Assessment and Monitoring of Disease Conditions via Coagulation Tests: Prothrombin Time (PT)
🩸 What is Prothrombin Time (PT)?
Prothrombin Time (PT) is a laboratory test that measures the time it takes for blood plasma to clot after adding tissue factor (thromboplastin). It primarily evaluates the extrinsic and common pathways of the coagulation cascade.
PT is used to assess the function of clotting factors I (fibrinogen), II (prothrombin), V, VII, and X.
📊 Normal Reference Range:
- PT: 11 to 13.5 seconds
- INR (International Normalized Ratio): 0.8 to 1.2 (in normal individuals)
In patients on warfarin, the target INR is usually 2.0–3.0.
🔬 Clinical Uses of PT:
- ✅ Monitor oral anticoagulant therapy (e.g., warfarin)
- ✅ Evaluate bleeding disorders
- ✅ Preoperative coagulation assessment
- ✅ Assess liver function (liver synthesizes most clotting factors)
- ✅ Detect vitamin K deficiency
📉 Causes of Prolonged PT
| Category | Examples |
|---|---|
| 🧬 Clotting factor deficiency | Factor VII, X, V, II, or I deficiency |
| 💉 Anticoagulant therapy | Warfarin or coumarin therapy |
| 🧫 Liver disease | Cirrhosis, hepatitis (↓ synthesis of factors) |
| 🍀 Vitamin K deficiency | Malabsorption, antibiotics, biliary obstruction |
| 🩸 Disseminated Intravascular Coagulation (DIC) | Consumption of clotting factors |
📈 Causes of Shortened PT
- Rare and usually not clinically significant
- Can occur with:
- High fibrinogen levels
- Dehydration
- Early stages of DIC
🧠 INR (International Normalized Ratio)
- Standardizes PT results across labs
- Particularly useful for patients on warfarin therapy
- Target INR values:
- 2.0 – 3.0: Atrial fibrillation, DVT, PE
- 2.5 – 3.5: Mechanical heart valves
🩺 Nurse’s Role in PT Monitoring
✔️ Before Testing
- Collect blood sample in citrate tube
- Ensure no contamination with heparin
- Confirm if the patient is on anticoagulants or vitamin K antagonists
✔️ Monitoring
- Observe for signs of bleeding: bruising, hematuria, GI bleeding
- Track PT/INR in patients on warfarin regularly
- Notify physician if INR exceeds therapeutic range
✔️ Patient Education
- Avoid NSAIDs, alcohol, and excessive green leafy vegetables (vitamin K-rich)
- Maintain regular INR monitoring appointments
- Inform all healthcare providers about anticoagulant use
🧪 Summary of Clinical Interpretation
| PT/INR Result | Possible Condition |
|---|---|
| Normal PT/INR | Normal coagulation |
| ↑ PT / ↑ INR | Liver dysfunction, warfarin therapy, vitamin K deficiency |
| ↓ PT (rare) | High fibrinogen, early DIC (hypercoagulable) |
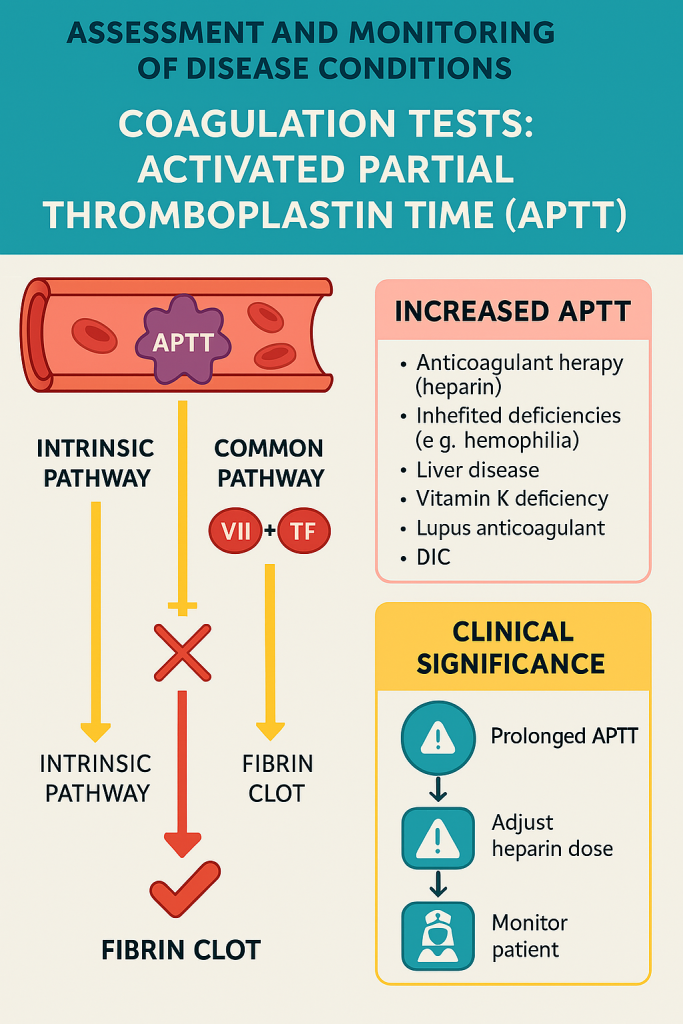
🧪 Assessment and Monitoring of Disease Conditions via Coagulation Tests: Activated Partial Thromboplastin Time (APTT)
🩸 What is APTT?
Activated Partial Thromboplastin Time (APTT) is a blood test that measures the time it takes for blood to clot by assessing the function of the intrinsic and common pathways of the coagulation cascade.
It specifically evaluates the activity of clotting factors XII, XI, IX, VIII (intrinsic) and factors X, V, II (prothrombin), and I (fibrinogen) (common pathway).
📊 Normal Reference Range:
- APTT: 25 to 35 seconds
(May vary slightly depending on laboratory methods)
- Therapeutic target range (e.g., for heparin therapy): 1.5 to 2.5 times the normal value
🔬 Clinical Uses of APTT
- ✅ Monitor unfractionated heparin therapy
- ✅ Detect clotting factor deficiencies
- ✅ Investigate unexplained bleeding or thrombosis
- ✅ Diagnose Hemophilia A and B
- ✅ Screen for lupus anticoagulant and antiphospholipid syndrome
📉 Causes of Prolonged APTT
| Category | Examples |
|---|---|
| 🧬 Inherited deficiencies | Hemophilia A (Factor VIII), Hemophilia B (Factor IX) |
| 💉 Anticoagulant therapy | Heparin overdose |
| 🧫 Liver disease | Impaired synthesis of clotting factors |
| 🍀 Vitamin K deficiency | Affects common pathway |
| 🧪 Lupus anticoagulant | Autoimmune interference with phospholipid surface |
| 🩸 DIC (Disseminated Intravascular Coagulation) | Factor consumption |
🔼 Causes of Shortened APTT (rare and less clinically significant)
- Early stages of DIC
- Extensive inflammation (increased factor VIII)
- Pregnancy or post-operative states
- Hypercoagulable states
🧠 APTT vs. PT
| Test | Pathway Measured | Main Clinical Use |
|---|---|---|
| PT | Extrinsic + Common | Warfarin monitoring |
| APTT | Intrinsic + Common | Heparin monitoring, hemophilia |
🩺 Nurse’s Role in APTT Monitoring
✔️ Before the Test
- Ensure sample is collected in a blue-top citrate tube
- Record time of last heparin administration (if applicable)
- Avoid hemolysis or contamination
✔️ During Heparin Therapy
- Monitor APTT frequently (e.g., every 6 hours)
- Adjust heparin dose based on protocol
- Watch for signs of bleeding: bruises, blood in urine/stools, bleeding gums
✔️ Patient Education
- Inform patients on anticoagulants to avoid NSAIDs, aspirin, and injury
- Teach about signs of bleeding and when to seek help
🧾 Summary of Clinical Interpretation
| APTT Result | Possible Condition |
|---|---|
| Normal APTT | Normal intrinsic pathway function |
| ↑ APTT | Heparin therapy, Hemophilia A/B, liver disease, DIC |
| ↓ APTT (rare) | Inflammation, hypercoagulability, pregnancy |
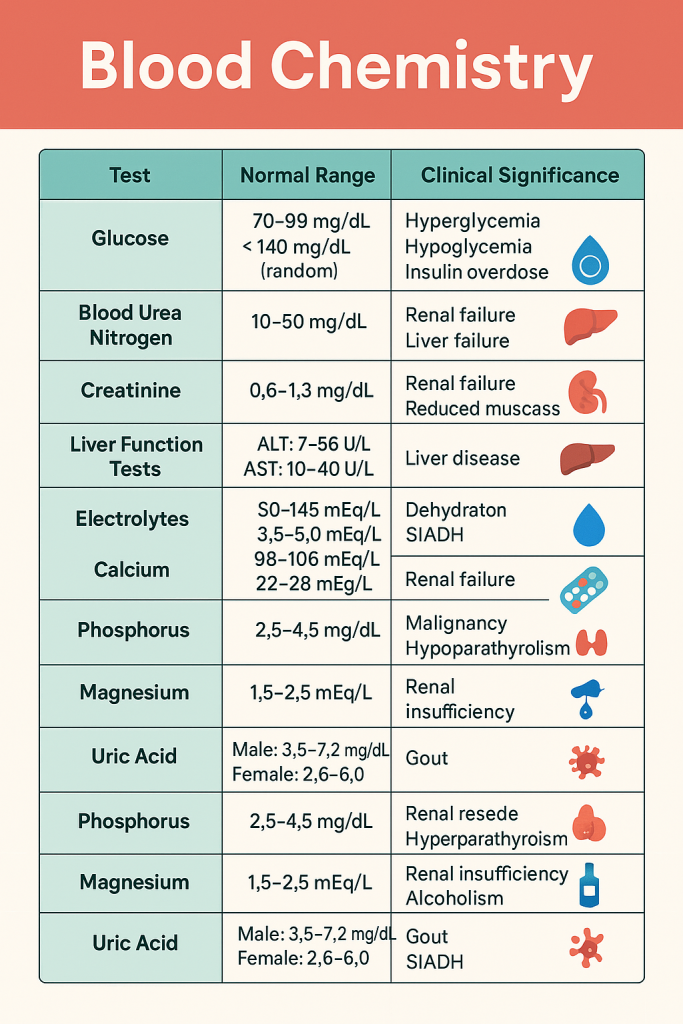
🧪 Assessment and Monitoring of Disease Conditions
🔬 Blood Chemistry – Parameters, Normal Ranges & Clinical Significance
Blood chemistry tests provide a broad overview of a patient’s metabolic, organ, electrolyte, and acid-base status. These tests are crucial for:
- 🧠 Early detection of systemic diseases
- 🩺 Monitoring chronic conditions
- 💊 Evaluating treatment effectiveness
- ⚠️ Detecting life-threatening imbalances
🧬 Key Blood Chemistry Parameters
1️⃣ Blood Glucose (Fasting & Random)
| Normal Values |
|---|
| Fasting: 70–99 mg/dL |
| Random: <140 mg/dL |
| HbA1c: <5.7% (non-diabetic) |
🔍 Clinical Interpretation:
- ↑ Hyperglycemia: Diabetes mellitus, stress, corticosteroids, Cushing’s syndrome
- ↓ Hypoglycemia: Insulin overdose, adrenal insufficiency, sepsis
2️⃣ Blood Urea Nitrogen (BUN) & Creatinine
| Normal Values |
|---|
| BUN: 10–50 mg/dL |
| Creatinine: 0.6–1.3 mg/dL |
| BUN/Creatinine ratio: ~10:1 to 20:1 |
🔍 Clinical Interpretation:
- ↑ in renal failure, dehydration, high protein diet
- ↓ in liver failure, malnutrition
3️⃣ Liver Function Tests (LFTs)
| Test | Normal Range |
|---|---|
| ALT (SGPT) | 7 – 56 U/L |
| AST (SGOT) | 10 – 40 U/L |
| ALP | 40 – 130 U/L |
| Total Bilirubin | 0.3 – 1.2 mg/dL |
| Direct Bilirubin | 0.1 – 0.4 mg/dL |
| Albumin | 3.5 – 5.0 g/dL |
| Total Protein | 6.0 – 8.0 g/dL |
🔍 Clinical Interpretation:
- ↑ ALT, AST: Hepatitis, liver damage
- ↑ ALP: Biliary obstruction, bone disease
- ↓ Albumin: Cirrhosis, nephrotic syndrome, malnutrition
- ↑ Bilirubin: Liver dysfunction, hemolysis
4️⃣ Electrolytes
| Parameter | Normal Range |
|---|---|
| Sodium (Na⁺) | 135 – 145 mEq/L |
| Potassium (K⁺) | 3.5 – 5.0 mEq/L |
| Chloride (Cl⁻) | 98 – 106 mEq/L |
| Bicarbonate (HCO₃⁻) | 22 – 28 mEq/L |
🔍 Clinical Interpretation:
- Na⁺:
- ↑: Dehydration, Cushing’s
- ↓: SIADH, diarrhea, vomiting
- K⁺:
- ↑: Renal failure, hemolysis, acidosis
- ↓: Diuretics, vomiting, insulin therapy
- Cl⁻:
- ↑: Dehydration, renal tubular acidosis
- ↓: Vomiting, metabolic alkalosis
- HCO₃⁻:
- ↑: Metabolic alkalosis
- ↓: Metabolic acidosis
5️⃣ Calcium (Ca²⁺), Phosphorus (PO₄³⁻), Magnesium (Mg²⁺)
| Parameter | Normal Range |
|---|---|
| Calcium | 8.5 – 10.5 mg/dL |
| Ionized Calcium | 4.5 – 5.6 mg/dL |
| Phosphorus | 2.5 – 4.5 mg/dL |
| Magnesium | 1.5 – 2.5 mEq/L |
🔍 Clinical Interpretation:
- Calcium:
- ↑: Hyperparathyroidism, malignancy
- ↓: Hypoparathyroidism, renal failure
- Phosphorus:
- ↑: Renal failure, hypoparathyroidism
- ↓: Malnutrition, hyperparathyroidism
- Magnesium:
- ↑: Renal failure
- ↓: Alcoholism, malabsorption, diuretics
6️⃣ Uric Acid
| Normal Range:
- Male: 3.5 – 7.2 mg/dL
- Female: 2.6 – 6.0 mg/dL
🔍 Clinical Interpretation:
- ↑: Gout, renal disease, chemotherapy, high purine diet
- ↓: Liver disease, SIADH
7️⃣ Cholesterol & Lipid Profile
| Parameter | Normal Range |
|---|---|
| Total Cholesterol | < 200 mg/dL |
| LDL (bad cholesterol) | < 100 mg/dL |
| HDL (good cholesterol) | > 40 mg/dL (male), > 50 (female) |
| Triglycerides | < 150 mg/dL |
🔍 Clinical Interpretation:
- Dyslipidemia is a major risk for atherosclerosis, stroke, CAD
🧠 Quick Reference Table – Blood Chemistry Parameters
| Test | Normal Range | Clinical Use |
|---|---|---|
| Glucose | 70–99 mg/dL (fasting) | Diabetes screening |
| Urea | 10–50 mg/dL | Renal function |
| Creatinine | 0.6–1.3 mg/dL | GFR estimation, renal health |
| ALT/AST | ALT: 7–56, AST: 10–40 | Hepatocellular injury |
| ALP | 40–130 U/L | Bone/liver diseases |
| Bilirubin | T: 0.3–1.2, D: 0.1–0.4 | Hemolysis, liver function |
| Albumin | 3.5–5.0 g/dL | Nutritional/liver status |
| Calcium | 8.5–10.5 mg/dL | Bone metabolism, clotting |
| Sodium | 135–145 mEq/L | Fluid balance |
| Potassium | 3.5–5.0 mEq/L | Cardiac and neuromuscular function |
| Bicarbonate | 22–28 mEq/L | Acid-base balance |
| Phosphorus | 2.5–4.5 mg/dL | Bone and renal health |
| Magnesium | 1.5–2.5 mEq/L | Neuromuscular, cardiac health |
| Uric Acid | 3.5–7.2 (M), 2.6–6.0 (F) | Gout, renal function |
| Lipid Profile | Varies | Cardiovascular risk |
🩺 Nurse’s Role in Blood Chemistry Monitoring
- ✅ Collect correct samples (e.g., fasting for glucose/lipids)
- ✅ Interpret abnormal trends with symptoms
- ✅ Educate patient about diet, fluid, medication adherence
- ✅ Monitor for signs of imbalance:
- Electrolyte disturbances → muscle cramps, arrhythmia
- Hypocalcemia → tetany, seizures
- Uremia → fatigue, confusion, bleeding
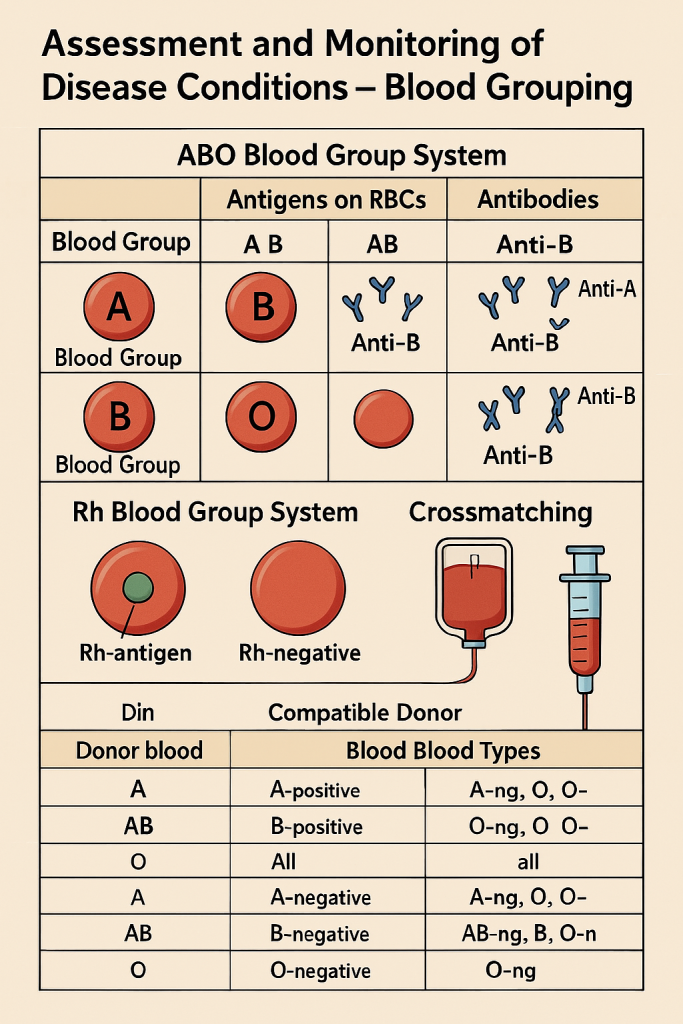
🩸 Assessment and Monitoring of Disease Conditions – Blood Grouping
🔬 What is Blood Grouping?
Blood grouping is the laboratory process of identifying a person’s blood type based on the antigens (agglutinogens) present on the surface of red blood cells and the corresponding antibodies (agglutinins) in the plasma.
The two most clinically important systems are:
- 🔹 ABO system
- 🔸 Rh (Rhesus) system
Blood grouping is vital for transfusion compatibility, organ transplantation, maternal-fetal medicine, and emergency care.
🧬 ABO Blood Group System
| Blood Group | Antigen on RBCs | Antibodies in Plasma |
|---|---|---|
| A | A | Anti-B |
| B | B | Anti-A |
| AB | A and B | None |
| O | None | Anti-A and Anti-B |
- AB is the universal recipient (no antibodies)
- O is the universal donor (no antigens)
🧬 Rh (Rhesus) System
- Based on the presence or absence of D antigen on RBCs
- Rh-positive (Rh⁺): D antigen present
- Rh-negative (Rh⁻): D antigen absent
🔍 Clinical Importance:
- Rh incompatibility in pregnancy:
- If an Rh⁻ mother carries an Rh⁺ fetus, maternal immune system may form anti-D antibodies → Hemolytic Disease of the Newborn (HDN) in subsequent pregnancies.
🩺 Why is Blood Grouping Clinically Important?
✔️ For Safe Blood Transfusion
- Prevents hemolytic transfusion reactions
- Donor and recipient blood must be compatible in ABO and Rh
✔️ In Pregnancy
- Prevents Rh isoimmunization and protects fetal health
- Anti-D immunoglobulin administered to Rh⁻ mothers after Rh⁺ delivery or miscarriage
✔️ In Organ or Tissue Transplantation
- ABO compatibility is essential to reduce rejection risk
✔️ In Emergency & Trauma
- O⁻ is used as an emergency universal donor
- Grouping is done immediately if transfusion is needed
🧪 Tests Used in Blood Grouping
- 🔹 Forward (cell) typing – RBCs tested with anti-A, anti-B, and anti-D reagents
- 🔸 Reverse (serum) typing – Serum tested against known RBCs
- 🧪 Crossmatching – Donor and recipient blood mixed to check for compatibility
- 🧬 Antibody screening – Identifies unexpected antibodies in plasma
🩺 Nursing Role in Blood Grouping Assessment
- ✔️ Confirm identity of patient before sample collection
- ✔️ Use proper anticoagulant tubes (EDTA or plain for serum)
- ✔️ Label samples correctly and send for type and crossmatch before transfusion
- ✔️ Educate patients, especially Rh⁻ mothers, about risks and anti-D injections
- ✔️ Monitor for transfusion reactions (fever, chills, hematuria, shock)
🔄 Summary Table: ABO and Rh Compatibility
| Recipient | Compatible Donor Blood Types |
|---|---|
| A⁺ | A⁺, A⁻, O⁺, O⁻ |
| B⁺ | B⁺, B⁻, O⁺, O⁻ |
| AB⁺ | All types (universal recipient) |
| O⁺ | O⁺, O⁻ |
| A⁻ | A⁻, O⁻ |
| B⁻ | B⁻, O⁻ |
| AB⁻ | AB⁻, A⁻, B⁻, O⁻ |
| O⁻ | O⁻ (universal donor) |
🧪 Assessment and Monitoring of Disease Conditions – Crossmatching (Compatibility Testing)
🧬 What is Crossmatching?
Crossmatching is a laboratory procedure performed prior to a blood transfusion to determine whether donor blood is compatible with the recipient’s blood. It is part of pre-transfusion testing and helps prevent transfusion reactions by ensuring the donor’s red blood cells will not be attacked by the recipient’s immune system.
🔍 Why Is Crossmatching Necessary?
- Ensures ABO and Rh compatibility
- Detects unexpected antibodies in the recipient’s plasma (e.g., anti-Kell, anti-Duffy)
- Prevents hemolytic transfusion reactions
- Reduces the risk of anaphylaxis, fever, and hemolysis
🧪 Types of Crossmatching Tests
🔹 1. Major Crossmatch (Most Important)
- Recipient’s serum + Donor’s RBCs
- Detects if recipient has antibodies that may react against donor’s RBCs
🔸 2. Minor Crossmatch (Less commonly done now)
- Donor’s serum + Recipient’s RBCs
- Detects if donor’s plasma contains antibodies against recipient RBCs
🔬 In modern practice, minor crossmatch is often omitted when using packed red blood cells, as plasma content is minimal.
🧪 3. Types of Crossmatch Procedures
| Method | Details |
|---|---|
| Immediate Spin | Quick, for ABO incompatibility only |
| Saline/Room Temp | Detects cold-reactive IgM antibodies |
| Indirect Antiglobulin Test (IAT) | Most sensitive – detects IgG antibodies |
| Electronic Crossmatch | Computer-verified ABO compatibility (used in some labs) |
⏱️ Time Required
- Full crossmatch: ~30–60 minutes
- Emergency transfusion (O⁻ blood): Immediate, without full crossmatch
🩸 Interpretation of Crossmatch Results
| Result | Meaning |
|---|---|
| No agglutination | ✅ Compatible – safe to transfuse |
| Agglutination/hemolysis | ❌ Incompatible – risk of reaction |
🧠 Crossmatch vs Blood Typing
| Test | Function |
|---|---|
| Blood grouping | Identifies ABO and Rh type |
| Antibody screen | Detects unexpected antibodies |
| Crossmatch | Confirms donor-recipient compatibility |
🩺 Nursing Role in Crossmatching
- ✅ Ensure proper identification of patient (name, ID band, request form)
- ✅ Collect blood sample using correct anticoagulant tube (usually plain or EDTA)
- ✅ Send sample for type and crossmatch before transfusion
- ✅ Check compatibility label on blood bag before administration
- ✅ Monitor patient closely during and after transfusion for:
- Fever, chills, rash
- Chest/back pain
- Hemoglobinuria
- Hypotension or shock
⚠️ When is Crossmatching Especially Critical?
- Multiple transfusions (antibody development risk)
- Pregnant women with Rh incompatibility history
- Organ transplantation
- Patients with autoimmune diseases or hemolytic anemia
🧾 Key Points Summary
- Major crossmatch is essential for every transfusion
- Helps avoid life-threatening hemolytic reactions
- Nurses play a key role in collection, labeling, verification, and monitoring
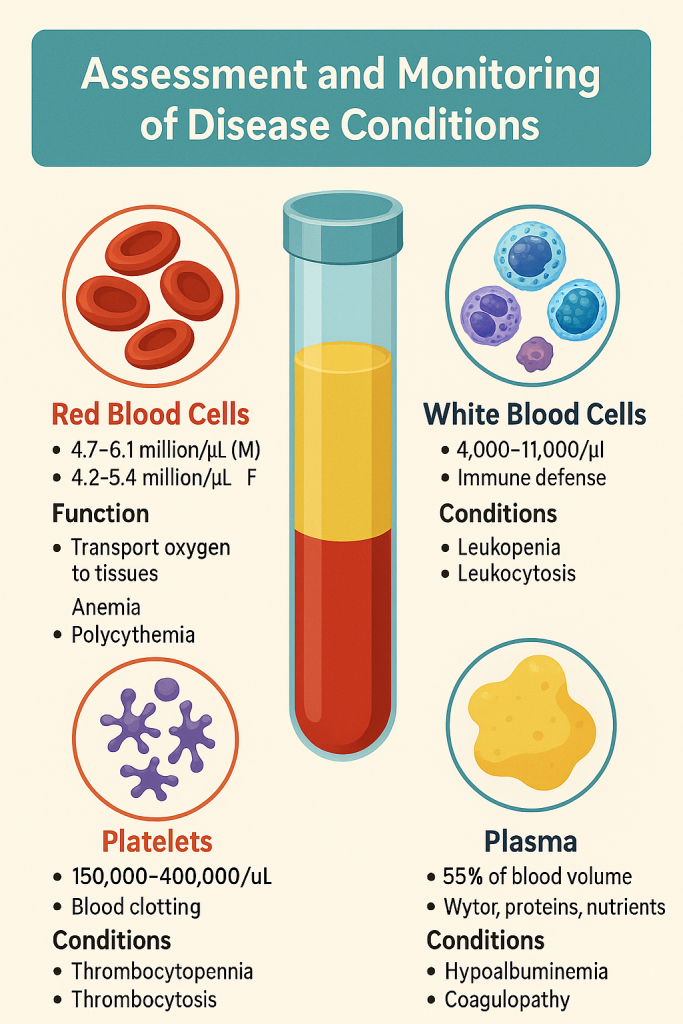
🧪 Assessment and Monitoring of Disease Conditions: Blood Components
Blood is a connective tissue composed of formed elements (cells) suspended in plasma. Evaluating its components is essential for diagnosis, monitoring treatment, and managing various systemic and hematological disorders.
🩸 Major Components of Blood
1️⃣ Red Blood Cells (RBCs) – Erythrocytes
| ✅ Normal Count |
|---|
| Males: 4.7 – 6.1 million/µL |
| Females: 4.2 – 5.4 million/µL |
🔍 Function:
- Transport oxygen (via hemoglobin) from lungs to tissues.
- Remove carbon dioxide.
🧪 Assessment:
- RBC count
- Hemoglobin (Hb): Males: 13.5–17.5 g/dL | Females: 12–15.5 g/dL
- Hematocrit (PCV): Males: 40–54% | Females: 36–48%
🩺 Clinical Relevance:
- 🔻 ↓ in anemia, blood loss, bone marrow suppression
- 🔺 ↑ in polycythemia vera, dehydration
2️⃣ White Blood Cells (WBCs) – Leukocytes
| ✅ Normal Count: 4,000 – 11,000/µL |
🔍 Function:
- Immune defense against infections.
🧪 Differential Count:
- Neutrophils: 50–70% (↑ in bacterial infection)
- Lymphocytes: 20–40% (↑ in viral infections)
- Monocytes: 2–8%
- Eosinophils: 1–4% (↑ in allergy, parasites)
- Basophils: 0.5–1%
🩺 Clinical Relevance:
- Leukocytosis: Infections, leukemia, inflammation
- Leukopenia: Chemotherapy, sepsis, HIV, bone marrow failure
3️⃣ Platelets – Thrombocytes
| ✅ Normal Count: 150,000 – 400,000/µL |
🔍 Function:
- Initiate clot formation and maintain vascular integrity.
🧪 Monitoring Tests:
- Platelet count
- Bleeding time (BT)
- Clotting time (CT)
🩺 Clinical Relevance:
- Thrombocytopenia: <150,000/µL → bleeding risk (e.g., ITP, dengue)
- Thrombocytosis: >400,000/µL → thrombotic risk (e.g., myeloproliferative disorders)
4️⃣ Plasma (55% of blood volume)
🔍 Components:
- 90% water
- 8% plasma proteins: Albumin, Globulins, Fibrinogen
- Electrolytes, glucose, hormones, enzymes, clotting factors
💧 Plasma Proteins
| Protein | Normal Value | Function |
|---|---|---|
| Albumin | 3.5 – 5.0 g/dL | Maintains osmotic pressure, transport |
| Globulins | 2.0 – 3.5 g/dL | Immune functions (antibodies) |
| Fibrinogen | 200 – 400 mg/dL | Clotting |
🩺 Clinical Relevance:
- ↓ Albumin: Liver disease, nephrotic syndrome, malnutrition
- ↓ Fibrinogen: DIC, liver failure
🩸 Other Assessments in Blood Monitoring
- ESR: Marker of inflammation
- CRP: Acute-phase response protein
- Reticulocyte count: Bone marrow activity
- Peripheral smear: Morphological examination of RBCs, WBCs, and platelets
🩺 Nurse’s Role in Blood Component Monitoring
- ✔️ Collect blood using correct technique and appropriate tubes (EDTA, citrate, plain).
- ✔️ Observe for signs and symptoms of anemia, infection, or bleeding.
- ✔️ Monitor laboratory trends and report abnormal values promptly.
- ✔️ Educate patient about tests and prepare them (e.g., fasting for lipid/glucose).
- ✔️ Administer blood transfusions or plasma components based on deficiencies.
🧠 Clinical Correlation Summary Table
| Component | Abnormality | Clinical Implication |
|---|---|---|
| RBCs | Anemia / Polycythemia | Fatigue, pallor / Risk of thrombosis |
| WBCs | Leukopenia / Leukocytosis | Infection risk / Inflammation or leukemia |
| Platelets | Thrombocytopenia / -cytosis | Bleeding / Clotting disorder |
| Plasma Proteins | Hypoalbuminemia | Edema, poor drug transport |
| Clotting Factors | Coagulopathies | Bleeding, prolonged PT/APTT |
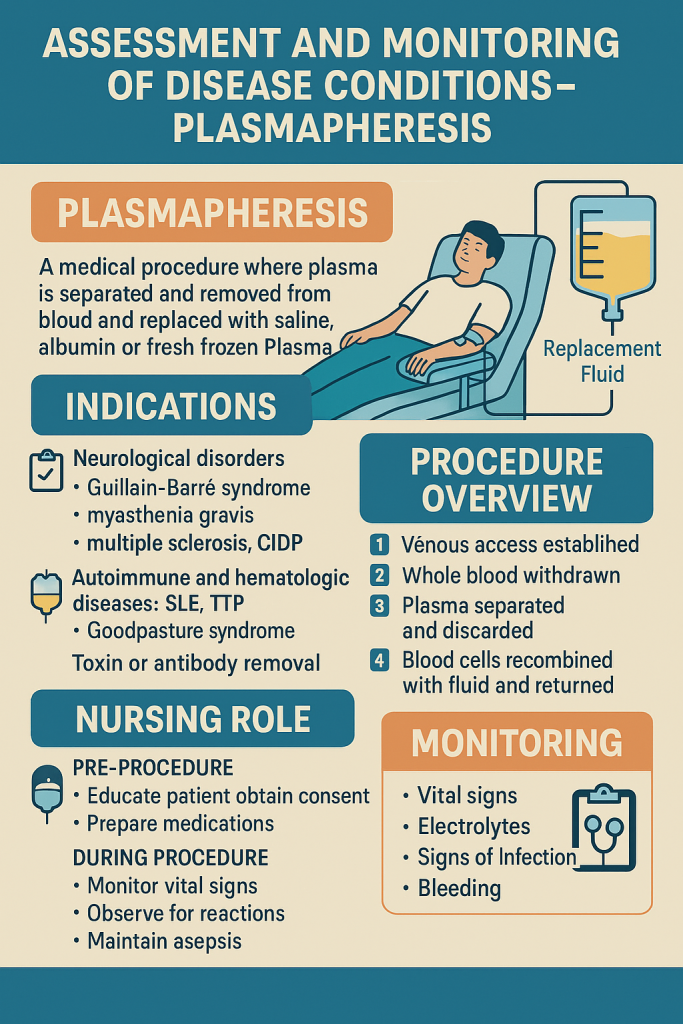
🧪 Assessment and Monitoring of Disease Conditions – Plasmapheresis
🧬 What is Plasmapheresis?
Plasmapheresis, also known as therapeutic plasma exchange (TPE), is a medical procedure in which plasma is separated and removed from the blood, and then replaced with a substitute fluid such as:
- Normal saline
- Albumin
- Fresh frozen plasma (FFP)
This process removes pathogenic substances (autoantibodies, immune complexes, toxins) circulating in plasma and is commonly used in autoimmune and neurological disorders.
🩺 Indications for Plasmapheresis
Plasmapheresis is used to treat or control diseases involving abnormal plasma constituents, particularly:
🔹 Neurological disorders
- Guillain-Barré Syndrome (GBS)
- Myasthenia Gravis (MG)
- Chronic Inflammatory Demyelinating Polyneuropathy (CIDP)
- Multiple Sclerosis (severe flares)
🔸 Autoimmune and Hematologic diseases
- Systemic Lupus Erythematosus (SLE) with nephritis
- Thrombotic Thrombocytopenic Purpura (TTP)
- Goodpasture’s syndrome
- Antibody-mediated organ transplant rejection
🧬 Toxin or antibody removal
- Wilson’s disease (copper overload)
- Hyperviscosity syndrome (in myeloma)
⚙️ Procedure Overview
- Venous access established (central line or peripheral)
- Whole blood is withdrawn
- Plasma is separated using centrifugation or filtration
- Pathogenic plasma is discarded
- Blood cells are recombined with replacement fluid and returned to the patient
🔍 Monitoring Parameters During and After Plasmapheresis
🩸 Pre-procedure Assessment:
- CBC, PT/INR, APTT
- Electrolytes (especially calcium, potassium)
- Renal and liver function tests
- Vital signs baseline
- Blood group typing (if FFP is used)
🩺 Intra-procedure Monitoring:
- Blood pressure, heart rate, oxygen saturation
- Signs of hypovolemia (dizziness, hypotension)
- Bleeding tendency (especially if FFP not used)
- Allergic or transfusion reactions (chills, rash, anaphylaxis)
🧪 Post-procedure Monitoring:
- Electrolytes (may require calcium supplementation)
- Platelet count (may transiently decrease)
- Signs of infection at catheter site
- Plasma protein levels (monitor for hypoproteinemia)
🧾 Common Side Effects & Risks
| Effect | Cause |
|---|---|
| Hypotension | Volume shifts, fluid loss |
| Hypocalcemia | Citrate anticoagulant binding Ca²⁺ |
| Bleeding | Coagulation factor removal |
| Infections | Central line catheter complications |
| Allergic reactions | Plasma protein or replacement fluid |
💉 Replacement Fluids Used
| Replacement | Indication |
|---|---|
| 5% Albumin | Most commonly used, low reaction risk |
| Fresh Frozen Plasma (FFP) | If clotting factors are needed |
| Saline or other crystalloids | Volume expansion only |
🧠 Nursing Role in Plasmapheresis
- 📋 Pre-procedure:
- Educate patient on process and expected effects
- Ensure proper consent
- Prepare emergency medications (e.g., calcium gluconate, antihistamines)
- 🩺 During the procedure:
- Continuous monitoring of vital signs
- Maintain aseptic technique with catheter
- Observe for allergic or transfusion reactions
- 📊 Post-procedure:
- Document fluid balance, vital trends
- Check for bruising, bleeding
- Monitor for electrolyte shifts or infection
🧾 Clinical Summary Table
| Aspect | Description |
|---|---|
| Purpose | Remove pathogenic substances from plasma |
| Method | Centrifugation or membrane filtration |
| Replacement | Albumin, FFP, saline |
| Indications | Autoimmune, neurological, toxin-induced diseases |
| Monitoring | Vitals, labs, bleeding, hypocalcemia |
| Nursing Role | Preparation, monitoring, documentation, education |
🩸 Assessment and Monitoring of Disease Conditions – Transfusion Reactions
🧬 What is a Transfusion Reaction?
A transfusion reaction is an adverse response of the recipient’s body to transfused blood or blood products. These reactions can be immune-mediated or non-immune, and range from mild to life-threatening.
Prompt recognition, assessment, and management are essential to prevent complications such as shock, renal failure, or death.
🔍 Classification of Transfusion Reactions
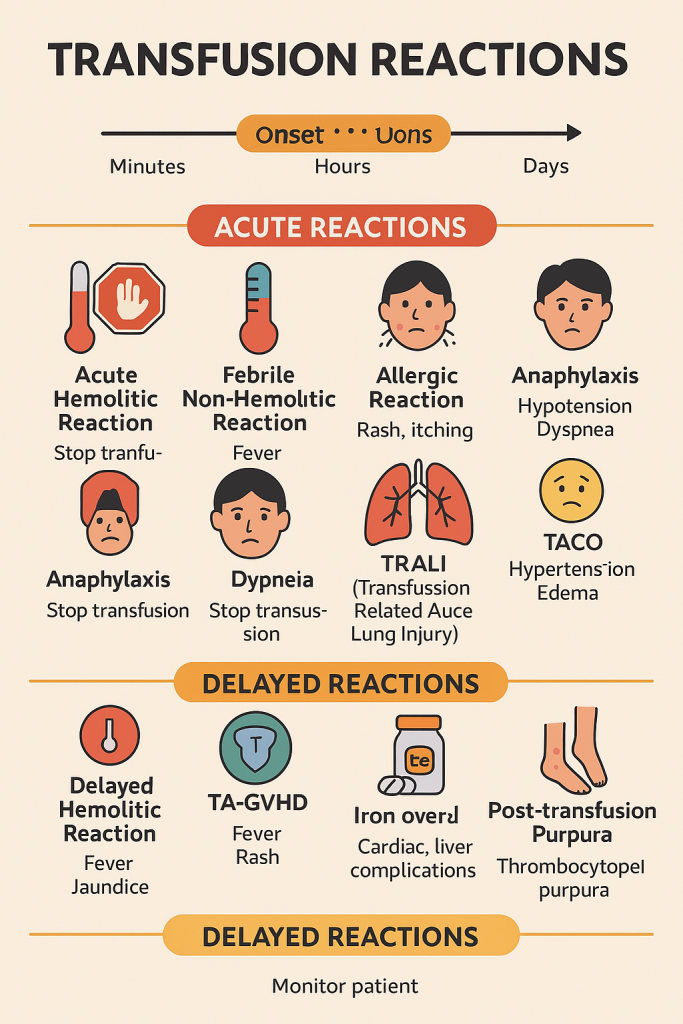
🔴 A. Acute (within 24 hours of transfusion)
| Type | Key Features |
|---|---|
| 1. Acute Hemolytic Reaction (AHTR) | 🔺 Most severe. Caused by ABO incompatibility. Hemolysis of donor RBCs due to recipient antibodies. |
| 2. Febrile Non-Hemolytic Reaction (FNHTR) | Caused by cytokines or recipient antibodies against donor WBCs. Common and mild. |
| 3. Allergic Reaction | Mild (urticaria) to severe (anaphylaxis). Caused by plasma protein hypersensitivity. |
| 4. Anaphylactic Reaction | Sudden, severe allergic reaction; common in IgA-deficient recipients. |
| 5. TRALI (Transfusion-Related Acute Lung Injury) | Non-cardiogenic pulmonary edema within 6 hrs; caused by donor anti-leukocyte antibodies. |
| 6. TACO (Transfusion-Associated Circulatory Overload) | Volume overload due to rapid infusion, especially in elderly or cardiac patients. |
🟡 B. Delayed (days to weeks after transfusion)
| Type | Key Features |
|---|---|
| 1. Delayed Hemolytic Reaction | Due to anamnestic response to minor RBC antigens. Slow hemolysis, often asymptomatic. |
| 2. Graft-versus-host disease (TA-GVHD) | Rare but fatal. Viable donor T-lymphocytes attack host tissues. |
| 3. Iron Overload (Hemosiderosis) | Seen in multiple transfusions, especially in thalassemia patients. |
| 4. Post-transfusion Purpura (PTP) | Immune destruction of platelets. Occurs ~5–10 days after transfusion. |
🩺 Clinical Assessment & Symptoms to Monitor
| Symptom | Suspected Reaction |
|---|---|
| Fever, chills, flank pain | Acute hemolytic reaction |
| Urticaria, itching | Allergic reaction |
| Hypotension, dyspnea, wheezing | Anaphylaxis or TRALI |
| Cyanosis, frothy sputum | TRALI or TACO |
| Dark urine, back pain | Hemolysis |
| Jaundice days after transfusion | Delayed hemolytic reaction |
| Petechiae, low platelet count | Post-transfusion purpura |
⏱️ Time of Onset: Clinical Differentiation
| Reaction Type | Typical Onset Time |
|---|---|
| Acute Hemolytic | Within minutes |
| FNHTR | Within 1–2 hours |
| Allergic | During or shortly after |
| TRALI | Within 6 hours |
| TACO | During/soon after transfusion |
| Delayed Hemolytic | 5–10 days post-transfusion |
| TA-GVHD | 4–30 days |
🩺 Nursing Responsibilities – Before, During, and After Transfusion
🧾 Before Transfusion
- ✅ Verify patient identity and crossmatch results
- ✅ Check ABO and Rh compatibility
- ✅ Inspect blood bag for expiry, clots, discoloration
- ✅ Record baseline vitals (T, P, R, BP)
🩺 During Transfusion
- ✅ Start slowly for first 15 minutes
- ✅ Monitor for signs: rash, chills, fever, chest pain, dyspnea
- ✅ Recheck vitals after 15 mins, then hourly
⚠️ If a Reaction Occurs
- ⛔ STOP the transfusion immediately
- 💉 Maintain IV line with normal saline
- 📢 Notify physician and blood bank
- 📦 Return blood bag and tubing for testing
- 📝 Document reaction thoroughly
- 🧪 Send samples (patient’s blood and urine) for hemolysis testing
🧠 Lab Investigations Following a Suspected Reaction
- Direct Coombs test (DAT)
- Repeat crossmatch and blood grouping
- Serum bilirubin, haptoglobin, LDH
- Urinalysis for hemoglobinuria
- Chest X-ray (in suspected TRALI or TACO)
📊 Summary Chart – Quick Comparison
| Reaction | Mechanism | Main Signs | Immediate Action |
|---|---|---|---|
| AHTR | ABO mismatch | Fever, chills, hemoglobinuria | Stop transfusion |
| FNHTR | WBC/cytokine antibodies | Fever, mild chills | Antipyretics |
| Allergic | IgE to plasma proteins | Rash, itching | Antihistamines |
| Anaphylaxis | Anti-IgA antibodies | Shock, dyspnea | Epinephrine |
| TRALI | Anti-HLA antibodies | Pulmonary edema | Stop, oxygen |
| TACO | Volume overload | Hypertension, dyspnea | Diuretics |