BSC SEM 4 UNIT 1 ADULT HEALTH NURSING 2
UNIT 1 Nursing management of patient with disorders of Ear, Nose and Throat
ANATOMY AND PHYSIOLOGY OF THE EAR
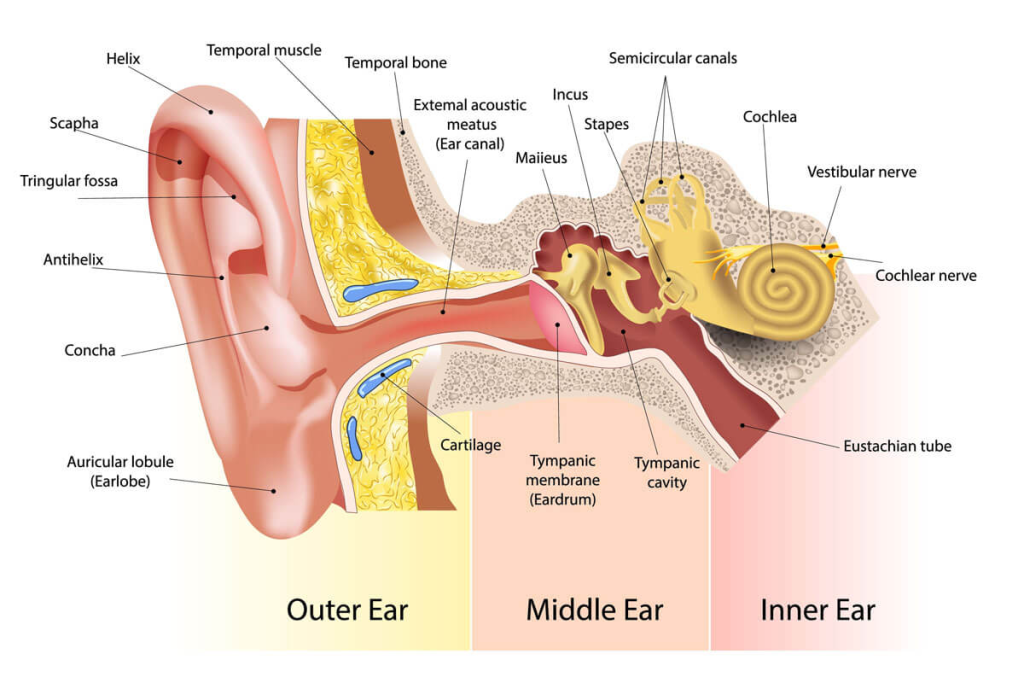
The ear has 2 main roles:
Hearing (auditory function)
Balance (equilibrium function)
It is divided into three main parts:
1. External Ear (Outer Ear)
🔸 Parts:
- 👂 Pinna (Auricle) – Cartilage covered by skin; collects sound waves.
- 🌀 External Auditory Canal (Meatus) – A tube (~2.5 cm) leading to the eardrum; lined with hairs & ceruminous glands that secrete earwax.
- 🥁 Tympanic Membrane (Eardrum) – Thin membrane that vibrates in response to sound waves.
🔸 Functions:
✅ Collects & funnels sound waves to the middle ear.
✅ Protects inner structures with wax and hairs.
2. Middle Ear (Tympanic Cavity)
🔸 Parts:
- 🦴 Ossicles (3 small bones):
- Malleus (Hammer) – Connected to eardrum.
- Incus (Anvil) – Connects malleus to stapes.
- Stapes (Stirrup) – Presses on oval window of cochlea.
- 🌬️ Eustachian Tube – Connects middle ear to the nasopharynx; equalizes pressure.
- 🪟 Oval Window & Round Window – Membrane-covered openings into inner ear.
🔸 Functions:
✅ Amplifies vibrations from the eardrum to the inner ear.
✅ Equalizes air pressure via Eustachian tube.
3. Inner Ear (Labyrinth)
🧠 Made of bony labyrinth (filled with perilymph) & membranous labyrinth (filled with endolymph)
A. Cochlea – For Hearing
- Structure: Snail-shaped organ with 3 fluid-filled chambers:
🌀 Scala vestibuli,
🌀 Scala media (cochlear duct),
🌀 Scala tympani - Organ of Corti – Contains hair cells (mechanoreceptors) that convert vibrations into nerve signals.
B. Vestibule – For Balance
- Contains:
🟡 Utricle & Saccule – Detect linear movements & head position.
🧭 Uses otoliths (tiny crystals) that move with gravity.
C. Semicircular Canals – For Balance
- Three canals (anterior, posterior, lateral) oriented in 3 planes.
- Detect rotational movements of the head.
🔸 Functions of Inner Ear:
✅ Cochlea: Converts mechanical sound to electrical impulses → Auditory Nerve (CN VIII) → Brain
✅ Vestibular Apparatus: Maintains body balance & spatial orientation
PHYSIOLOGY OF HEARING
Sound Transmission Pathway:
- Sound waves → collected by pinna
- Travel via auditory canal → vibrate the tympanic membrane
- Vibrations transmitted by ossicles (malleus → incus → stapes)
- Stapes creates wave in perilymph via the oval window
- Pressure wave → moves basilar membrane in cochlea
- Hair cells in Organ of Corti bend → generate nerve impulse
- Impulse sent to auditory cortex of temporal lobe via Cranial Nerve VIII (Vestibulocochlear nerve)
PHYSIOLOGY OF BALANCE
Static Equilibrium:
- Controlled by utricle & saccule
- Detect head tilt and linear acceleration (e.g., moving forward)
Dynamic Equilibrium:
- Controlled by semicircular canals
- Detect angular/rotational movements (e.g., spinning)
Both send signals to brainstem & cerebellum to adjust muscle tone and posture.
NERVE SUPPLY
- CN VIII (Vestibulocochlear Nerve):
- Cochlear branch → hearing
- Vestibular branch → balance
KEY POINTS FOR NURSING STUDENTS
🔸 Ear infections may involve the external, middle, or inner ear.
🔸 Otitis media affects the middle ear—often post-URTI in children.
🔸 Blocked Eustachian tube affects pressure and hearing.
🔸 Balance disorders (e.g., vertigo) often involve semicircular canals.
🔸 Safe ear care is essential—avoid inserting objects that may damage the canal or eardrum.
🔸 Audiometry and tuning fork tests (Rinne, Weber) help assess hearing loss type.
ANATOMY & PHYSIOLOGY OF THE NOSE
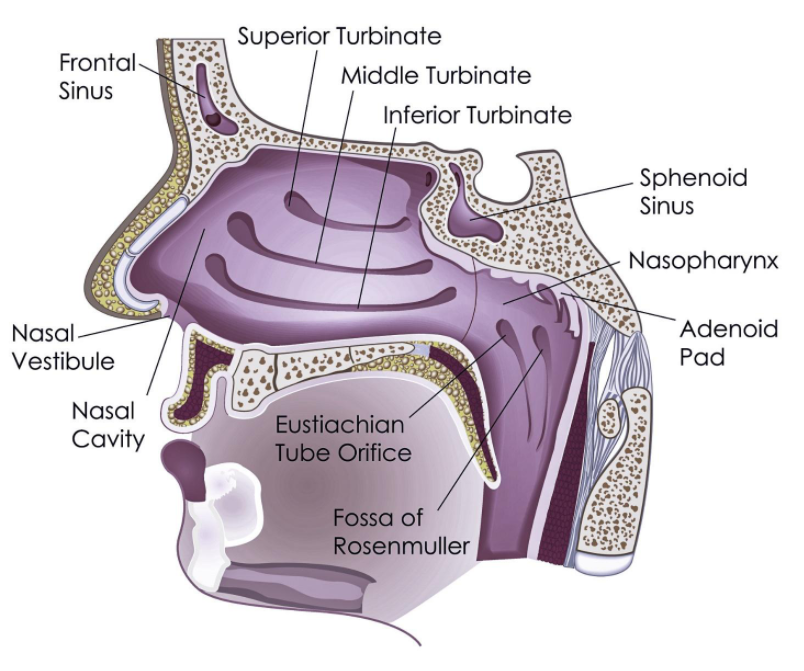
The nose is the primary organ for smell (olfaction) and an important part of the respiratory system. It serves both respiratory and sensory functions.
PARTS OF THE NOSE
The nose is divided into two major regions:
1. External Nose (Visible Part)
🔸 Features:
- 👃 Nasal bones (bridge of nose)
- Cartilages (lateral, alar)
- Nostrils (nares) – openings for air intake
- Covered by skin & lined with sebaceous glands
🔸 Functions:
✅ Intake of air
✅ Protection via hairs (vibrissae) that trap dust
2. Internal Nose (Nasal Cavity)
📍 Located behind the external nose and divided by the nasal septum (made of cartilage & bone)
🔸 A. Nasal Septum
- Divides nasal cavity into right and left halves
- Composed of:
🔹 Vomer bone
🔹 Perpendicular plate of ethmoid
🔹 Cartilage
🔸 B. Nasal Conchae (Turbinates)
There are 3 bony projections on each side:
- 🔸 Superior
- 🔸 Middle
- 🔸 Inferior
🌀 Function: Increase surface area and create turbulence to warm, moisten, and filter air.
🔸 C. Meatuses
- Grooves under each concha: superior, middle, and inferior meatus
- Drains sinuses and lacrimal fluid
🌀 LINING OF NASAL CAVITY
The nasal cavity is lined with mucous membrane containing:
- Ciliated columnar epithelium
- Goblet cells (produce mucus)
💡 Function: Mucus traps dust/pathogens; cilia sweep mucus to throat for swallowing.
🔶 PARANASAL SINUSES
Air-filled cavities in skull bones that open into the nasal cavity:
🔸 Frontal sinus
🔸 Maxillary sinus
🔸 Ethmoid sinus
🔸 Sphenoid sinus
🌀 Functions:
✅ Lighten skull weight
✅ Produce mucus
✅ Act as resonating chambers for voice
🧠 OLFACTORY REGION (ROOF OF NASAL CAVITY)
🔹 Contains olfactory epithelium:
- Specialized olfactory receptor neurons
- Supported by sustentacular cells
- Connected to olfactory bulb → olfactory nerve (CN I)
🔹 Function: Smell detection via volatile odorant molecules
🫁 PHYSIOLOGY OF THE NOSE
1. Respiratory Function
✅ Air enters via nostrils
✅ Is filtered (hairs, mucus)
✅ Warmed (rich blood supply)
✅ Moistened (mucous glands)
✅ Sent to pharynx → trachea → lungs
2. Olfactory Function (Smell)
✅ Odorant molecules dissolve in mucus
✅ Stimulate olfactory receptors
✅ Signal travels via CN I (Olfactory nerve)
✅ Reaches olfactory cortex in the temporal lobe of brain
3. Protective Function
✅ Sneeze reflex (removal of irritants)
✅ Mucus traps pathogens
✅ Enzymes (like lysozyme) fight bacteria
🧬 BLOOD SUPPLY
Rich vascular supply from:
🔸 Sphenopalatine artery
🔸 Facial artery
🔸 Ophthalmic artery
🔸 Kiesselbach’s plexus (anterior nosebleeds site)
🧠 NERVE SUPPLY
🔸 Olfactory Nerve (CN I) – smell
🔸 Trigeminal Nerve (CN V) – general sensation
🔸 Autonomic nerves – control glands & blood vessels
🩺 KEY POINTS FOR NURSING STUDENTS
✅ Nasal congestion may indicate allergy, infection, or obstruction
✅ Deviated nasal septum can cause breathing difficulty
✅ Epistaxis (nosebleed) commonly originates from Kiesselbach’s plexus
✅ Sinusitis causes facial pain & pressure
✅ Smell loss (anosmia) can occur in COVID-19, trauma, or neurological disorders
✅ Regular nasal hygiene and humidification reduce risk of infections
👄👅🗣️ ANATOMY & PHYSIOLOGY OF THE THROAT (PHARYNX + ASSOCIATED STRUCTURES)
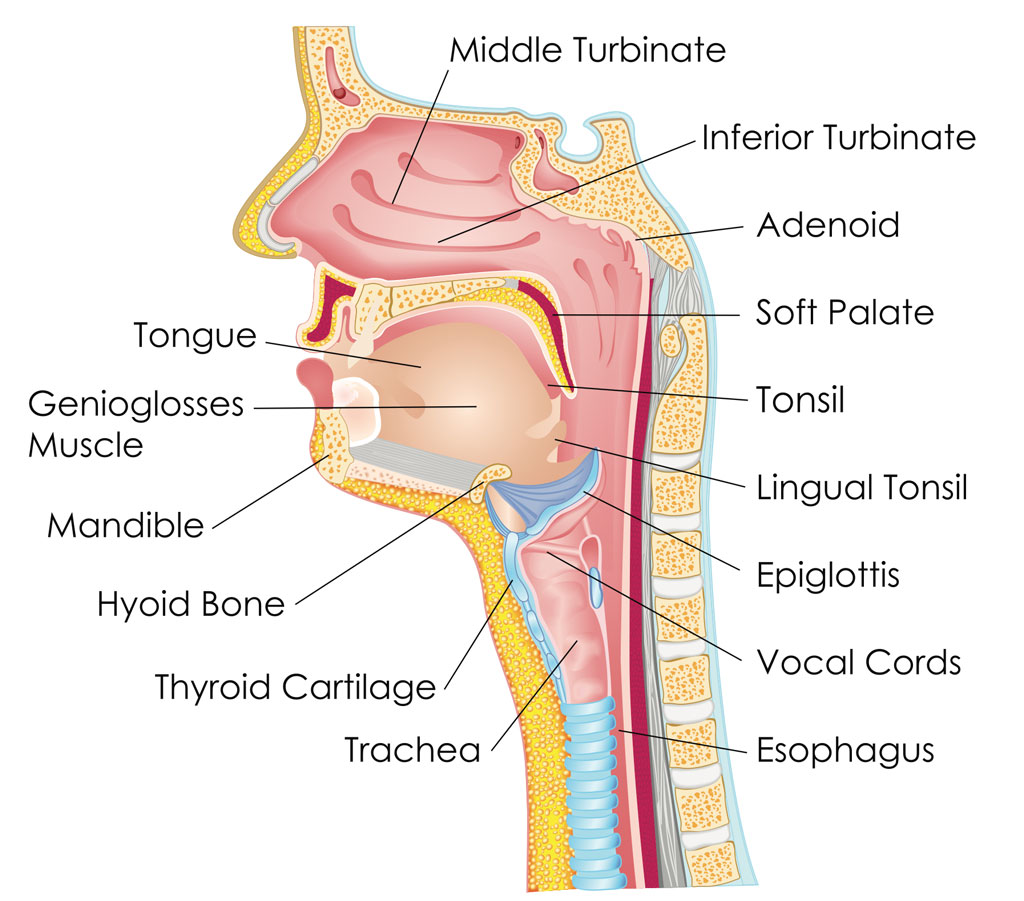
The throat, medically known as the pharynx, is a muscular tube that serves as a shared passage for both the respiratory and digestive systems.
🔷 MAIN DIVISIONS OF THE THROAT
The pharynx is divided into three anatomical regions:
🔹 1. Nasopharynx
📍 Location: Behind the nasal cavity, above the soft palate
🔸 Lined with: Pseudostratified ciliated epithelium
🔸 Contains:
- 🌀 Openings of the Eustachian (auditory) tubes
- 🛡️ Pharyngeal tonsil (Adenoids)
✅ Function:
- Passageway for air
- Equalizes ear pressure via Eustachian tubes
- Traps pathogens via adenoids
🔹 2. Oropharynx
📍 Location: Behind the oral cavity, from soft palate to epiglottis
🔸 Lined with: Stratified squamous epithelium (resists food friction)
🔸 Contains:
- 👅 Base of tongue
- 🛡️ Palatine & lingual tonsils
✅ Function:
- Common pathway for air and food
- Involved in swallowing and immune defense
🔹 3. Laryngopharynx (Hypopharynx)
📍 Location: From epiglottis to cricoid cartilage
🔸 Opens into:
- 🫁 Larynx (anteriorly) – air passage
- 🍽️ Esophagus (posteriorly) – food passage
✅ Function:
- Directs air → larynx and food → esophagus
- Part of swallowing mechanism
🧠 ASSOCIATED STRUCTURES OF THE THROAT
🔸 A. Epiglottis
🪶 Flap of cartilage that closes over the trachea during swallowing to prevent aspiration
🔸 B. Larynx (Voice Box)
🗣️ Contains vocal cords and is involved in sound production
🔸 C. Tonsils (Lymphoid tissue)
🛡️ First line of defense; trap microbes
🧬 PHYSIOLOGY OF THE THROAT
🔹 1. Swallowing (Deglutition)
Occurs in 3 phases:
➤ Phase 1: Oral Phase (Voluntary)
- Tongue pushes food to oropharynx
➤ Phase 2: Pharyngeal Phase (Involuntary)
- Soft palate elevates → closes nasopharynx
- Epiglottis folds → closes larynx
- Food directed to esophagus
➤ Phase 3: Esophageal Phase (Involuntary)
- Peristaltic movement pushes bolus down
🔹 2. Respiratory Function
- Air passes from nasal/oral cavity → pharynx → larynx → trachea → lungs
🛑 Swallowing reflex temporarily halts breathing to protect airway.
🔹 3. Voice Production
- Air from lungs passes through larynx
- Vibrates vocal cords
- Tension & length of cords determine pitch and volume
💉 BLOOD SUPPLY OF THE THROAT
Supplied by branches of:
🔸 External carotid artery
🔸 Facial artery
🔸 Ascending pharyngeal artery
🧠 NERVE SUPPLY
- Glossopharyngeal nerve (CN IX) – sensory to pharynx
- Vagus nerve (CN X) – motor to pharyngeal muscles
- Hypoglossal nerve (CN XII) – motor to tongue
🩺 KEY POINTS FOR NURSING STUDENTS
✅ Pharyngitis – Common throat infection; may be viral or bacterial
✅ Tonsillitis – Inflammation of palatine tonsils
✅ Dysphagia – Difficulty swallowing (common in stroke, neuromuscular issues)
✅ Airway obstruction can occur if the epiglottis fails to function (epiglottitis)
✅ Throat swab – used to diagnose streptococcal infections
✅ Tracheostomy care – May be needed if upper airway is obstructed
✅ Maintain oral hygiene to prevent infections in immunocompromised patients
HISTORY-RELATED MANAGEMENT OF PATIENTS WITH EAR, NOSE, AND THROAT (ENT) DISORDERS
I. IMPORTANCE OF HISTORY TAKING IN ENT DISORDERS
- History-taking is the first step in identifying, diagnosing, and managing ENT conditions.
- ENT symptoms often overlap (e.g., pain, discharge, congestion, bleeding), so a targeted history is essential for clinical differentiation.
II. GENERAL PRINCIPLES OF ENT HISTORY TAKING
When a patient presents with an ENT complaint, the nurse or clinician must systematically assess:
Chief Complaint (CC)
🟡 Ask: “What brought you here today?”
➤ Common complaints:
- Ear: Earache, hearing loss, tinnitus, discharge, dizziness
- Nose: Congestion, discharge, bleeding, loss of smell
- Throat: Sore throat, hoarseness, difficulty swallowing, cough
History of Present Illness (HPI)
✅ Details about the chief complaint:
- 🔹 Onset: Sudden or gradual?
- 🔹 Duration: How long has it lasted?
- 🔹 Progression: Better, worse, or same?
- 🔹 Nature of symptoms: Sharp pain? Pulsatile? Blocked sensation?
- 🔹 Associated symptoms: Fever, headache, facial pain, etc.
- 🔹 Aggravating/Relieving factors: Position, eating, noise, etc.
- 🔹 Treatment taken: Home remedies or medications?
🧠 This step helps differentiate between infective, allergic, traumatic, or neoplastic causes.
Past Medical & Surgical History
- Previous ENT infections (otitis media, sinusitis, tonsillitis)
- Chronic illnesses (e.g., diabetes, allergies, GERD)
- Previous surgeries: Ear tubes, tonsillectomy, septoplasty
Medication History
- Any ototoxic drugs (e.g., aminoglycosides)?
- Nasal sprays, decongestants, antihistamines
- Steroids or antibiotics used recently?
Family History
- History of genetic hearing loss
- Allergic rhinitis, sinus disorders, or ENT malignancies in family
Social & Environmental History
- Occupation (e.g., noise exposure in factories → hearing loss)
- Smoking & alcohol (risk for pharyngeal/laryngeal cancer)
- Use of earphones, swimming (external ear infections)
- Exposure to allergens or pollution
Voice Use History (especially in throat complaints)
- Is the patient a teacher, singer, speaker?
- Overuse of voice can cause nodules, hoarseness, or vocal strain.
Review of Systems
- General symptoms: Fever, fatigue
- Neurological symptoms: Dizziness, facial weakness
- Respiratory/GI symptoms: Postnasal drip, reflux
III. CLINICAL MANAGEMENT BASED ON HISTORY
Once detailed history is taken, management includes:
A. Ear Disorders
🦻 Example: Otitis Media
- History: Earache, fever, hearing loss, recent URTI
- Management:
- Warm compress
- Antibiotics if bacterial
- Analgesics
- Myringotomy if pus accumulation
🦻 Hearing Loss
- History of noise exposure or drug use
- Refer for audiometry
- Consider hearing aids or ENT referral
B. Nose Disorders
👃 Example: Allergic Rhinitis
- History: Seasonal triggers, sneezing, nasal congestion
- Management:
- Allergen avoidance
- Antihistamines, nasal corticosteroids
- Saline nasal rinse
👃 Example: Epistaxis (Nosebleed)
- History: Bleeding episodes, trauma, hypertension
- Management:
- Anterior nasal packing
- BP control
- Cauterization if bleeding site visible
C. Throat Disorders
🗣️ Example: Pharyngitis or Tonsillitis
- History: Sore throat, fever, painful swallowing, white patches
- Management:
- Warm saline gargles
- Analgesics & antibiotics
- Hydration & rest
- Tonsillectomy in chronic cases
🗣️ Example: Hoarseness
- History: Duration, voice misuse, smoking
- Management:
- Voice rest
- ENT evaluation (laryngoscopy)
- Speech therapy or surgery if nodules
NURSE’S ROLE IN HISTORY-RELATED MANAGEMENT
✅ Collect comprehensive and confidential history
✅ Observe non-verbal signs: Facial pain, hearing difficulty
✅ Maintain comfort and privacy
✅ Document findings accurately
✅ Educate patient on symptom reporting
✅ Support emotional and psychological needs (e.g., hearing loss, chronic throat cancer)
CONCLUSION
📌 History is the foundation of ENT diagnosis.
📌 A well-taken history guides investigations, reduces unnecessary tests, and tailors appropriate treatment.
📌 Nurses play a vital role in history elicitation, symptom monitoring, and patient education.
PHYSICAL ASSESSMENT OF PATIENT WITH EAR, NOSE, AND THROAT (ENT) DISORDERS
Physical assessment in ENT helps confirm findings from history and guides the need for further evaluation or referrals.
GENERAL STEPS BEFORE STARTING
🔹 Wash hands and gather equipment
🔹 Ensure good lighting and privacy
🔹 Explain the procedure to the patient
🔹 Position patient comfortably (usually seated)
🔹 Use inspection, palpation, percussion, and otoscopy/oroscopy techniques as needed
I. EAR ASSESSMENT
1. Inspection & Palpation of External Ear
- 🔸 Shape, size, and symmetry of auricles
- 🔸 Redness, swelling, lesions, or discharge
- 🔸 Press on tragus and mastoid process for tenderness
📍 Pain = External otitis or mastoiditis
2. Otoscopic Examination
Use an otoscope to view the external auditory canal and tympanic membrane (eardrum)
🔍 Check for:
- Wax, foreign bodies, inflammation, edema
- Color and integrity of tympanic membrane:
- Normal: Pearly gray and translucent
- Bulging: Middle ear infection
- Retraction: Eustachian tube dysfunction
- Perforation: Hole or scar
✅ 3. Hearing Assessment
- Whisper Test: From behind the patient at ~2 feet
- Rinne Test (Tuning fork at 512 Hz):
- Compares air vs. bone conduction
- Normal: AC > BC
- Weber Test: Fork placed on forehead
- Normal: Sound heard equally in both ears
- Lateralization = conductive or sensorineural loss
🔷 II. NOSE ASSESSMENT
✅ 1. Inspection of External Nose
- 🔸 Alignment, deformities, swelling, trauma
- 🔸 Nasal flaring (sign of respiratory distress)
✅ 2. Palpation
- Gently palpate the bridge and soft tissues of nose for tenderness, crepitus
✅ 3. Internal Examination (Use Penlight or Nasal Speculum)
🔍 Check for:
- Septal deviation or perforation
- Mucosal color (pink = normal; pale = allergy; red = infection)
- Presence of discharge (color, consistency)
- Polyps or foreign bodies
- Bleeding points (e.g., Kiesselbach’s plexus)
✅ 4. Sinus Palpation & Percussion
- Frontal Sinus: Press above eyebrows
- Maxillary Sinus: Press below cheekbones
📍 Tenderness = Sinusitis
📍 Percussion (tapping) can also elicit pain if infected
🔷 III. THROAT ASSESSMENT 👄🗣️
✅ 1. Inspection of Oral Cavity & Oropharynx
Use a tongue depressor and penlight
🔍 Check:
- Lips: Cracks, lesions
- Teeth: Cavities, missing teeth
- Gums: Inflammation, bleeding
- Tongue: Coating, mobility, ulcers
- Hard & soft palate: Color, lesions
- Uvula: Midline or deviated
- Tonsils: Enlargement (graded I to IV), exudate, redness
- Pharyngeal wall: Redness, postnasal drip
✅ 2. Voice Quality
- Note hoarseness, nasal tone, or stridor
- Persistent hoarseness may indicate vocal cord pathology or cancer
✅ 3. Swallowing Assessment
- Ask patient to swallow water
- Observe for coughing, choking, or delayed swallow
✅ 4. Neck Palpation (Lymph Nodes & Thyroid)
- Palpate cervical lymph nodes for:
- Enlargement
- Tenderness
- Fixation (suggests malignancy)
- Assess thyroid gland for goiter or nodules (related to voice/swallowing)
🧠 DOCUMENTATION & NURSING IMPLICATIONS
📝 Document:
- Objective findings
- Laterality (Right/Left)
- Patient’s response to touch and tuning fork tests
- Size and grade of tonsils
- Type and color of discharge
- Pain or tenderness areas
- Any obstruction or deviation noted
🧑⚕️ Nurse’s role:
- Monitor for airway obstruction (e.g., swelling or bleeding in throat)
- Prepare patient for ENT specialist referral if needed
- Educate on proper hygiene (ear care, sinus irrigation)
- Advise on voice rest, saltwater gargles, or allergen avoidance
🧪🔬 DIAGNOSTIC TESTS FOR ENT DISORDERS
(Ear 👂, Nose 👃, and Throat 🗣️)
These tests help confirm diagnosis, assess severity, and plan treatment in ENT conditions.
🔷 I. EAR-RELATED DIAGNOSTIC TESTS 👂
1️⃣ Otoscopy
🔍 Purpose: Visual examination of the external auditory canal and tympanic membrane (eardrum)
✅ Detects:
- Otitis externa, otitis media
- Tympanic membrane perforation or bulging
- Wax impaction, foreign body
2️⃣ Tuning Fork Tests (Rinne & Weber Tests)
🔊 Purpose: Differentiate between conductive and sensorineural hearing loss
✅ Rinne Test:
- Normal: Air conduction > Bone conduction
✅ Weber Test: - Sound lateralizes to affected side = Conductive loss
- Sound lateralizes to healthy side = Sensorineural loss
3️⃣ Pure Tone Audiometry (PTA)
🎧 Purpose: Assess hearing sensitivity using tones at different frequencies and intensities
✅ Identifies type & degree of hearing loss
4️⃣ Tympanometry
🌀 Purpose: Measures middle ear pressure and mobility of tympanic membrane
✅ Detects:
- Eustachian tube dysfunction
- Otitis media with effusion
- Perforation of the eardrum
5️⃣ Auditory Brainstem Response (ABR)
🧠 Purpose: Evaluates electrical activity in the auditory nerve and brainstem
✅ Used for:
- Infants or uncooperative patients
- Diagnosing acoustic neuroma
- Neurological causes of hearing loss
6️⃣ Otoacoustic Emissions (OAE) Test
🎧 Purpose: Measures sounds generated by the cochlea in response to auditory stimuli
✅ Common in newborn hearing screening
7️⃣ CT / MRI of Temporal Bone
🧠 Purpose: Detailed imaging of inner and middle ear
✅ Useful for:
- Tumors (acoustic neuroma)
- Cholesteatoma
- Mastoiditis
🔷 II. NOSE-RELATED DIAGNOSTIC TESTS 👃
1️⃣ Anterior Rhinoscopy / Nasal Endoscopy
🔦 Purpose: Visualize nasal cavity, septum, turbinates using a nasal speculum or endoscope
✅ Detects:
- Polyps, deviated septum
- Inflammation, tumors
- Foreign body or bleeding source
2️⃣ X-ray of Paranasal Sinuses (PNS View)
🦴 Purpose: Detect sinusitis, fluid levels, bone abnormalities
✅ Used to assess frontal, maxillary, ethmoid, sphenoid sinuses
3️⃣ CT Scan of Nose & Sinuses
🧠 More accurate than X-ray for:
- Chronic sinusitis
- Nasal polyps
- Tumors
- Sinus wall erosion
4️⃣ Nasal Smear / Culture & Sensitivity (C/S)
🧫 Purpose: Identify bacterial, viral, or fungal infections
✅ Helps in selecting appropriate antibiotics
5️⃣ Allergy Testing (Skin Prick Test / IgE Blood Test)
🧪 Purpose: Identify allergens in allergic rhinitis
✅ Common allergens: pollen, dust, mites, animal dander
6️⃣ Olfactory Testing
👃 Purpose: Assesses ability to smell
✅ Useful in sinusitis, COVID-19, and neurological disorders
🔷 III. THROAT-RELATED DIAGNOSTIC TESTS 🗣️
1️⃣ Throat Examination / Laryngoscopy
🔬 Indirect (mirror) or direct (flexible fiberoptic) laryngoscopy
✅ Used to evaluate:
- Vocal cord movement
- Laryngeal cancer
- Foreign bodies
- Hoarseness, dysphagia
2️⃣ Throat Swab Culture
🧫 Purpose: Identify pathogens causing tonsillitis, pharyngitis
✅ Group A Streptococcus → rapid strep test or culture
3️⃣ Barium Swallow Test (for Dysphagia)
🩻 Purpose: X-ray of pharynx and esophagus after swallowing barium
✅ Detects structural or motility disorders
4️⃣ Fine Needle Aspiration Cytology (FNAC)
💉 Purpose: Sample of lymph node or neck mass
✅ Detects:
- Malignancy
- Tuberculosis lymphadenitis
- Reactive lymph nodes
5️⃣ Voice Analysis / Stroboscopy
🗣️ Purpose: Analyze vocal cord vibration and quality
✅ Useful in:
- Chronic hoarseness
- Vocal nodules
- Speech therapy evaluation
6️⃣ MRI/CT of Neck
🧠 For deeper throat pathologies:
✅ Tumors, abscesses, structural abnormalities of larynx/pharynx
🧑⚕️ ROLE OF NURSE IN DIAGNOSTIC TESTS
✔️ Prepare and educate the patient before test
✔️ Maintain infection control and sterility
✔️ Support during invasive procedures
✔️ Monitor for adverse reactions (contrast allergy, bleeding)
✔️ Record findings and communicate to the medical team
✔️ Emotional reassurance and post-test care
✅ CONCLUSION
📌 ENT diagnostic tests range from basic bedside exams to advanced imaging and audiological testing.
📌 Choosing the right test is guided by symptoms, history, and physical findings.
📌 Nurses are integral to preparing, assisting, and monitoring patients throughout the diagnostic process.
OTALGIA (EAR PAIN)
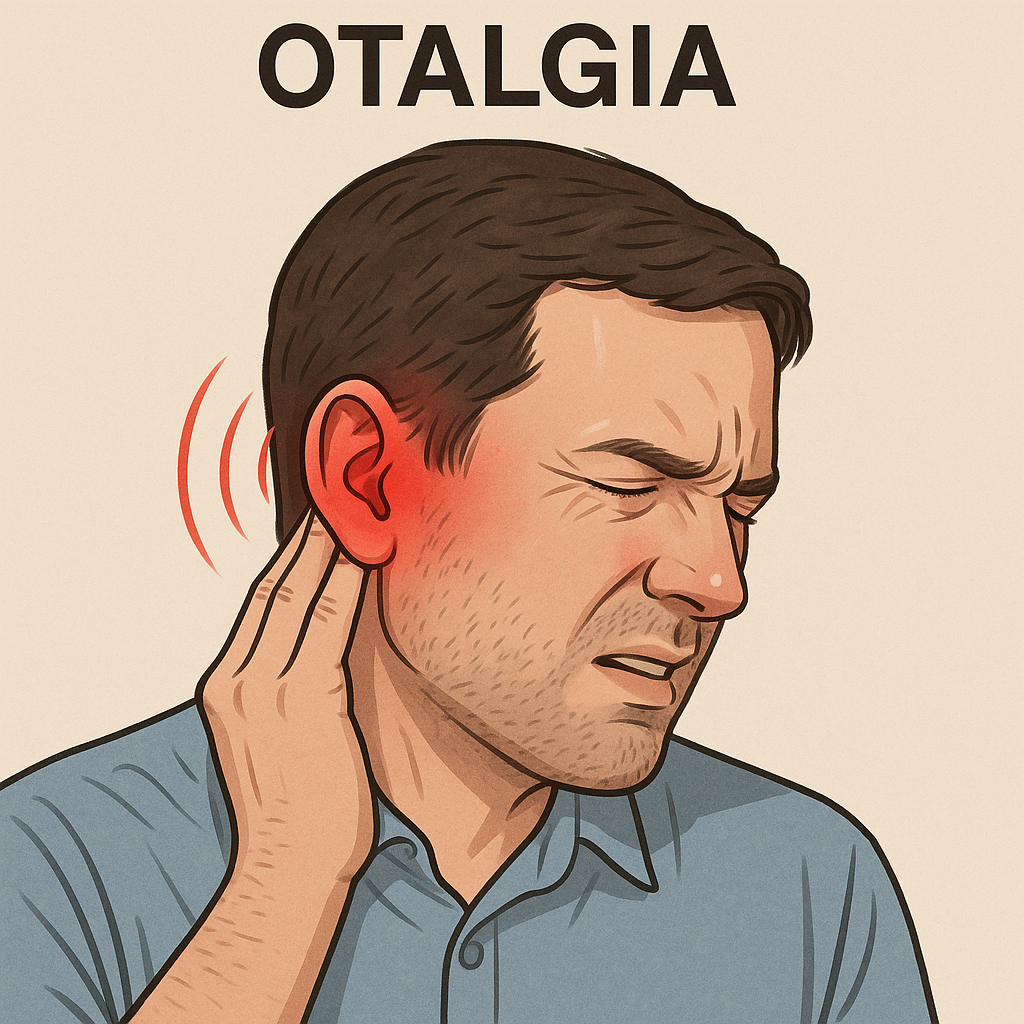
DEFINITION
Otalgia refers to pain in the ear, either due to primary pathology of the ear itself or secondary (referred) causes from adjacent structures (teeth, throat, sinuses, etc.).
CAUSES OF OTALGIA
A. Primary Otalgia (Originating from the Ear)
- Otitis externa (infection of external ear canal)
- Otitis media (middle ear infection)
- Impacted cerumen (earwax)
- Foreign body in the ear canal
- Eustachian tube dysfunction
- Barotrauma
- Trauma (e.g., slap, blunt injury)
- Mastoiditis
B. Referred (Secondary) Otalgia
- Tonsillitis or pharyngitis
- Temporomandibular joint (TMJ) disorders
- Dental caries or impacted molars
- Cervical spine pathology
- Parotitis or parotid gland tumor
- Laryngeal or hypopharyngeal malignancy
TYPES OF OTALGIA
| Type | Description |
|---|---|
| ✅ Primary | Pain originates from ear pathology |
| 🔁 Referred | Pain is referred from nearby non-ear structures |
PATHOPHYSIOLOGY
🔸 Pain in the ear occurs due to stimulation of cranial nerves:
- CN V (Trigeminal) – TMJ, sinus, dental pain
- CN VII (Facial) – External ear
- CN IX (Glossopharyngeal) – Pharynx, tonsils
- CN X (Vagus) – Larynx
🔸 In infections, inflammation leads to fluid accumulation, pressure buildup → stimulates pain receptors
🔸 In referred otalgia, nerve convergence in the brainstem results in misperception of pain location
SIGNS & SYMPTOMS
- Ear pain (dull, sharp, throbbing)
- Fullness or blocked sensation
- Discharge (in infections)
- Fever (in otitis)
- Reduced hearing
- Itching (otitis externa)
- Jaw pain (if TMJ/dental related)
- Sore throat or difficulty swallowing (if referred from pharynx)
DIAGNOSIS
✅ History & Physical Examination
- Location, onset, duration, nature of pain
- Associated symptoms (fever, discharge, sore throat, dental issues)
✅ Otoscopic Examination
- Tympanic membrane inspection
- Look for inflammation, perforation, fluid
✅ Tuning Fork Tests (Weber, Rinne)
✅ Audiometry (if hearing loss suspected)
✅ Throat, Dental, Sinus, and Neck Examination
✅ X-ray PNS / CT scan / MRI (for deeper infections or tumors)
✅ Culture of ear discharge (if present)
MEDICAL MANAGEMENT
🔹 Analgesics: Paracetamol, Ibuprofen for pain relief
🔹 Antibiotics:
- Otitis externa → topical drops (e.g., ciprofloxacin, gentamicin)
- Otitis media → systemic antibiotics (e.g., amoxicillin-clavulanate)
🔹 Ear drops: With anti-inflammatory and antiseptic agents
🔹 Antihistamines/Decongestants: For allergic or Eustachian tube dysfunction
🔹 Steroids: Topical or systemic in severe inflammation
🔹 Warm compresses to relieve pain
🔹 Treatment of secondary cause (e.g., dental care, throat infection)
SURGICAL MANAGEMENT
🔸 Myringotomy: Incision of tympanic membrane to drain middle ear fluid
🔸 Tympanostomy Tube Insertion: For recurrent otitis media
🔸 Tonsillectomy or Adenoidectomy: If tonsillar disease causes recurrent otalgia
🔸 TMJ Surgery: If temporomandibular joint disorder is severe
🔸 Mastoidectomy: In chronic mastoiditis or abscess
🔸 Excision of tumor: If referred pain from ENT cancers
NURSING MANAGEMENT
✅ Assessment:
- Location, severity, and character of pain
- Ear discharge: note color, odor, consistency
- Check for systemic signs like fever
✅ Interventions:
- Administer prescribed medications
- Apply warm compresses to relieve pain
- Assist with ear drops (ensure correct technique)
- Maintain ear hygiene & keep ear dry
- Educate patient not to use sharp objects in ear
- Elevate head during rest to reduce pressure
- Monitor for complications like perforation or hearing loss
✅ Emotional Support: Especially in children or elderly patients
NUTRITIONAL CONSIDERATIONS
- Ensure hydration – especially during fever
- Soft, easy-to-swallow foods if pain is referred from throat or jaw
- Avoid very cold or spicy foods if associated with pharyngitis
- Promote immunity with vitamin C-rich foods (oranges, lemon, amla)
- Encourage balanced diet to aid healing
COMPLICATIONS
- Tympanic membrane perforation
- Hearing loss (conductive or sensorineural)
- Mastoiditis
- Intracranial spread of infection (rare)
- Facial nerve paralysis
- Recurrent ear infections
- Abscess formation (ear canal or mastoid)
KEY POINTS TO REMEMBER
✅ Always differentiate between primary and referred otalgia
✅ A thorough ENT and general exam is crucial
✅ Otitis media is most common in children
✅ Avoid inserting foreign objects or cotton buds in ears
✅ Pain persisting >1 week despite treatment → needs further investigation
✅ Nurses play a crucial role in symptom relief, medication administration, and patient education
FOREIGN BODIES IN THE EAR
DEFINITION
A foreign body in the ear refers to any object that is not naturally present in the external auditory canal, introduced accidentally (mostly in children) or intentionally (rarely in adults with psychiatric conditions).
COMMON IN
✅ Children aged 2–8 years
✅ Also seen in adults (especially with psychiatric illness or trauma)
TYPES OF FOREIGN BODIES
1️⃣ Inanimate Objects
- 💡 Beads, buttons, chalk, erasers
- 🧱 Pebbles, paper, plastic parts
- 🍬 Food materials (peas, beans, seeds)
2️⃣ Animate (Living) Objects
- 🪳 Insects (ants, cockroaches, flies)
- 🕷️ Spiders
- 🐛 Larvae (rare)
3️⃣ Medical Objects
- 🧴 Cotton swabs, broken hearing aid pieces
ETIOLOGY / CAUSES
🔸 Accidental insertion (children playing)
🔸 Self-cleaning attempts
🔸 Insects entering during sleep
🔸 Psychiatric behavior or intoxication
🔸 Assault or trauma
PATHOPHYSIOLOGY
- Foreign object → mechanical blockage or irritation
- Animate objects → movement causes intense pain, inflammation
- If left untreated → can lead to infection, trauma, and hearing loss
SIGNS AND SYMPTOMS
| Symptom | Description |
|---|---|
| 👂 Ear pain (otalgia) | Sudden, sharp, or persistent |
| 🔊 Hearing loss | Conductive (due to blockage) |
| 🤕 Fullness sensation | Feeling of pressure in ear |
| 🐜 Movement sensation | In case of live insects |
| 🤢 Discharge | Foul-smelling, pus or blood-tinged |
| 🔊 Tinnitus | Ringing or buzzing sounds |
| 🧒 Irritability or crying | In young children |
DIAGNOSIS
✅ Clinical History:
- Sudden symptoms in a previously normal ear
- Witnessed insertion (common in kids)
✅ Physical Examination:
- Otoscopy: Visualization of the foreign body, surrounding inflammation, or discharge
- Examine both ears, nose, and throat (check for other FBs)
✅ Imaging (if needed):
- X-ray: If object is metallic
- CT scan: If deep insertion, trauma, or complications suspected
💊 MEDICAL MANAGEMENT
🔹 General Principles
✅ Do not irrigate if the object is:
- Organic (e.g., seeds – may swell)
- Battery or hygroscopic (absorbs moisture)
- Sharp or pointed
🔧 METHODS OF REMOVAL
1️⃣ Manual Extraction
- With ear forceps, hook, or suction catheter under otoscope/microscope
- Child may need restraint or sedation
2️⃣ Irrigation (Ear Syringing)
- Only for non-organic, non-swelling, blunt objects
3️⃣ Suction
- For smooth or soft objects
4️⃣ Alcohol or Oil Instillation
- For live insects: To immobilize before removal
5️⃣ General Anesthesia (GA)
- Required in uncooperative children or deeply impacted objects
🏥 SURGICAL MANAGEMENT
🔸 Tympanotomy / Canalotomy:
- If object has migrated deep and caused perforation, abscess, or cannot be removed non-invasively
🔸 Treatment of Complications:
- Perforation repair, infection drainage, etc.
🧑⚕️ NURSING MANAGEMENT
✅ Assessment:
- Observe for pain, discharge, and hearing changes
- Check mental status (if psychiatric cause suspected)
✅ Preparation:
- Calm the patient (especially child)
- Prepare tray with forceps, otoscope, suction, torch, antiseptics
- Monitor vitals if sedation is used
✅ Post-Procedure Care:
- Observe for pain, bleeding, dizziness
- Administer prescribed analgesics or antibiotics
- Educate parents/patients about not inserting objects into ears
✅ Documentation:
- Object type, side, removal technique, patient response
🍽️ NUTRITIONAL CONSIDERATIONS
🟡 Not directly applicable unless:
- Systemic infection with fever → encourage hydration
- Pain or infection affects eating → provide soft, lukewarm diet
⚠️ COMPLICATIONS
- Ear canal laceration
- Tympanic membrane perforation
- Otitis externa or media
- Hearing loss
- Chronic infection
- Foreign body aspiration (if object dislodges into airway)
🧠 KEY POINTS TO REMEMBER
✅ Do NOT try home removal methods (matchsticks, pins)
✅ Refer urgently if:
- Child is uncooperative
- FB is metallic, organic, or a battery
✅ Always re-check after removal to confirm nothing is left behind
✅ In case of live insects, immobilize before removing
✅ Prevention through parent education is critical!
🎗️👂 TUMORS IN THE EXTERNAL EAR
📘 DEFINITION
Tumors of the external ear refer to abnormal growths (benign or malignant) that arise from the skin, cartilage, or soft tissue of the auricle (pinna) or external auditory canal (EAC).
🧪 CAUSES / RISK FACTORS
1️⃣ Chronic sun exposure (UV radiation – major cause for pinna tumors)
2️⃣ Chronic ear infections or trauma
3️⃣ Radiation exposure
4️⃣ Genetic mutations or syndromes (e.g., basal cell nevus syndrome)
5️⃣ Immunosuppression
6️⃣ Occupational hazards (welders, farmers)
7️⃣ Old age and male gender (higher risk)
8️⃣ Poor hygiene in the ear canal (especially in neglected infections)
🔍 TYPES OF EXTERNAL EAR TUMORS
🔹 A. Benign Tumors
- Sebaceous cysts
- Lipoma
- Chondroma (cartilage tumor)
- Exostosis or Osteoma (bony growths in canal)
- Papilloma (wart-like lesion)
🔹 B. Malignant Tumors
- Basal Cell Carcinoma (BCC) – Most common on pinna
- Squamous Cell Carcinoma (SCC) – Aggressive; affects canal and surrounding skin
- Melanoma – Pigmented lesion with high metastatic risk
- Adenocarcinoma – Arises from ceruminous glands
- Sarcoma – Rare, aggressive connective tissue tumors
🔬 PATHOPHYSIOLOGY
- Exposure to carcinogens (like UV light or chronic inflammation) → DNA mutations
- Abnormal proliferation of skin or glandular cells
- In benign tumors – growth remains localized
- In malignant tumors – local tissue invasion, perineural spread, possible metastasis
- External auditory canal tumors can erode into temporal bone or middle ear
🚨 SIGNS AND SYMPTOMS
| 🔹 Symptom | 🔹 Description |
|---|---|
| Painless or painful lump | On pinna or inside ear canal |
| Ulcer or crusted lesion | Non-healing, may bleed |
| Discharge from the ear | Foul-smelling or blood-stained |
| Itching / irritation | Common in early benign tumors |
| Hearing loss | Due to canal obstruction |
| Tinnitus or ear fullness | In canal or deep tissue involvement |
| Facial nerve palsy | In advanced malignant tumors |
| Enlarged lymph nodes | Indicates spread |
🧪 DIAGNOSTIC TESTS
✅ History and Physical Examination
✅ Otoscopy / Otomicroscopy – View lesion
✅ Biopsy (Excisional / Incisional) – CONFIRMS diagnosis
✅ CT scan / MRI of temporal bone – For bony involvement or deep spread
✅ FNAC of lymph nodes (if palpable)
✅ Audiometry – Assess hearing loss
✅ Chest X-ray / PET scan – For metastatic work-up
💊 MEDICAL MANAGEMENT
🔹 For benign tumors:
- May need no treatment if small and asymptomatic
- Topical or systemic antibiotics for infected cysts
- Steroids for inflammatory lesions
🔹 For malignant tumors:
- Radiotherapy – Used in early superficial SCC or post-surgery
- Chemotherapy – Reserved for unresectable, advanced, or metastatic cancers
- Topical imiquimod for superficial BCC (in select cases)
🏥 SURGICAL MANAGEMENT
🔧 Benign Tumors:
- Excision under local anesthesia (e.g., cyst, papilloma, osteoma)
🔧 Malignant Tumors:
- Wide local excision with margin clearance
- Partial/total auriculectomy (removal of pinna if involved)
- Lateral temporal bone resection – If deep spread to canal
- Neck dissection – If lymph nodes involved
- Reconstructive surgery (skin grafts or flaps)
🧑⚕️ NURSING MANAGEMENT
✅ Preoperative Care:
- Psychological support (especially if cosmetic disfigurement expected)
- Consent and education about surgery, chemo, or radiation
- Ensure skin hygiene around lesion
✅ Postoperative Care:
- Monitor for bleeding, wound infection, swelling
- Pain management and dressing care
- Monitor facial nerve function if deep surgery done
- Support for body image disturbances
- Maintain ear dryness & hygiene
✅ Patient Education:
- Sun protection (hats, sunscreen)
- Avoid self-cleaning of ear
- Follow-up for recurrence surveillance
🥦 NUTRITIONAL CONSIDERATIONS
- High-protein, vitamin-rich diet to promote healing
- Adequate fluids to maintain hydration
- Soft diet if surgery affects facial nerve/mouth function
- Avoid alcohol and smoking (risk of recurrence/metastasis)
⚠️ COMPLICATIONS
- Local recurrence of tumor
- Facial nerve damage
- Cosmetic deformity
- Temporal bone erosion
- Hearing loss
- Lymph node and distant metastasis (in SCC or melanoma)
- Psychological trauma / body image issues
🧠 KEY POINTS TO REMEMBER
✅ Tumors of the external ear may be benign or malignant
✅ Sun exposure is a major risk factor for pinna tumors
✅ SCC of the external auditory canal is aggressive and requires early intervention
✅ Biopsy is essential for diagnosis
✅ Surgical removal with margin clearance is the mainstay of treatment
✅ Nurses play a vital role in post-op care, wound healing, and patient education
✅ Prevention includes sun protection, avoiding trauma, and early consultation
👂🟤 IMPACTED WAX
(Cerumen Impaction)
📘 DEFINITION
Impacted wax refers to the accumulation of cerumen (earwax) in the external auditory canal that blocks the canal partially or completely, leading to symptoms like hearing loss, discomfort, and sometimes pain or infection.
🧪 CAUSES / RISK FACTORS
🔹 Natural overproduction of cerumen
🔹 Narrow or tortuous ear canal
🔹 Use of cotton swabs, pins, or matchsticks pushing wax deeper
🔹 Ageing – wax becomes harder and drier in elderly
🔹 Use of hearing aids or earbuds (block natural migration)
🔹 Skin conditions – eczema, psoriasis affecting the ear canal
🔹 Lack of regular ear hygiene or excessive cleaning attempts
🔍 TYPES OF EAR WAX
| Type of Wax | Description |
|---|---|
| 🟠 Soft Wax | Yellow, moist, easy to remove |
| 🟤 Hard Wax | Dark, dry, impacted deeply |
| ⚫ Mixed Type | Sticky with solid chunks; variable |
🔬 PATHOPHYSIOLOGY
- Cerumen is normally secreted by ceruminous and sebaceous glands in the outer third of the ear canal.
- Normally it moves outward with jaw motion and dries up/flakes out.
- If this natural migration is disturbed, or if wax is pushed back by objects, it accumulates.
- As more wax builds up → blocks the canal, hardens over time, and may press against the tympanic membrane, causing conductive hearing loss or pain.
🚨 SIGNS AND SYMPTOMS
| Symptom | Description |
|---|---|
| 🔇 Hearing loss | Conductive, usually gradual and unilateral |
| 🤕 Earache (otalgia) | Especially with hard wax pressing the canal |
| 🌀 Ear fullness or pressure | Sensation of blockage or discomfort |
| 🔔 Tinnitus | Ringing or buzzing sound |
| 💧 Ear discharge | If infected or moist wax |
| 🤢 Dizziness or vertigo | In rare severe impactions |
| 😠 Irritability (in children) | Crying, tugging ears, feeding refusal |
🧪 DIAGNOSIS
✅ History
- Gradual hearing loss, blockage sensation, use of cotton swabs
✅ Otoscopy
- Direct visualization of yellow/brown/black wax occluding canal
- Can assess whether wax is soft or hard, partial or complete blockage
✅ Tuning Fork Tests (if needed)
- May show conductive hearing loss (Rinne negative, Weber lateralizes to blocked ear)
✅ No need for imaging unless suspecting underlying perforation, cholesteatoma, or tumor
💊 MEDICAL MANAGEMENT
1️⃣ Wax Softening Agents (Cerumenolytics)
Used 3–5 days before removal to soften wax:
| Agent | Mode of Action |
|---|---|
| 💧 Warm saline | Moistens and softens wax |
| 🟢 Hydrogen peroxide (3%) | Releases oxygen, breaks down wax |
| 🧴 Glycerin or baby oil | Lubricates and softens |
| 🧴 Carbamide peroxide | Breaks down hard wax chemically |
2️⃣ Aural Syringing (Ear Irrigation)
- Performed using lukewarm saline or water with a bulb syringe or irrigator
- Fluid directed along the canal wall, not directly at eardrum
- Avoid if:
❌ Tympanic membrane is perforated
❌ History of ear surgery
❌ Active ear infection
3️⃣ Manual Removal (Curettage / Suction)
- With Jobson Horne probe, curette, or suction
- Done under otoscopic or microscopic guidance
- Preferred for:
🔸 Hardened wax
🔸 Elderly or children
🔸 Failed irrigation
🏥 SURGICAL MANAGEMENT
🔸 Rarely required unless:
- Impacted wax causes complications (e.g., otitis externa, tympanic membrane perforation)
- Deep-seated wax needs removal under general anesthesia in uncooperative patients (especially children)
🔸 Surgical intervention may involve:
- Microsuction under microscope
- Meatoplasty (widening of ear canal) in repeated impactions due to anatomical defect
🧠 KEY POINTS TO REMEMBER
✅ Impacted wax is preventable – avoid inserting objects in ear
✅ Cerumen is protective, not dirty – cleaning too much is harmful
✅ Always check for ear drum integrity before irrigation
✅ Nurses play a vital role in wax removal, patient education, and ear care
👩⚕️🩺 NURSING MANAGEMENT OF IMPACTED EAR WAX
🎯 NURSING OBJECTIVES
✅ Relieve discomfort and restore hearing
✅ Safely remove wax or assist with removal
✅ Prevent complications like infection or perforation
✅ Educate the patient about proper ear hygiene
✅ Provide emotional comfort and reduce anxiety
🔷 I. ASSESSMENT
📝 The nurse should gather the following data:
- 🟢 Subjective Data:
- Patient’s complaint (hearing loss, pain, fullness)
- Duration and severity of symptoms
- History of ear trauma or self-cleaning habits
- Any prior ear surgery or chronic infections
- 🔵 Objective Data:
- Inspect and palpate the outer ear for swelling, tenderness, or redness
- Otoscopic examination (if trained): Observe cerumen blockage
- Monitor for discharge, odor, or signs of inflammation
- Assess hearing by whisper test or tuning fork (if needed)
🔷 II. PLANNING & GOALS
- Patient will report relief from discomfort
- Cerumen will be safely removed without trauma or pain
- Patient will maintain proper ear hygiene to prevent recurrence
- No complications such as ear infection or tympanic membrane damage will occur
🔷 III. NURSING INTERVENTIONS
1️⃣ Prepare for Wax Removal
- Gather sterile instruments if removal is to be performed
- Prepare warm saline or prescribed cerumenolytic drops
- Position patient comfortably – usually sitting with head tilted to affected side
- Place towel and kidney tray to protect clothing
- Explain procedure to reduce anxiety
2️⃣ Assist with or Perform Ear Irrigation (if nurse-trained & authorized)
- Use body-temperature water (~37°C) to prevent vertigo
- Gently irrigate along canal wall, not directly on eardrum
- Monitor for dizziness, nausea, or pain during procedure
- Discontinue if bleeding or severe discomfort occurs
- Dry the ear gently with sterile gauze or cotton wick post-irrigation
3️⃣ Apply Cerumenolytic Drops (if ordered)
- Instruct the patient to lie on the opposite side
- Instill drops gently and ask to stay in position for 5–10 minutes
- Cotton plug may be used loosely at the canal opening
- Usually done twice daily for 3–5 days before wax removal
4️⃣ Post-Procedure Care
- Assess for improvement in hearing and symptoms
- Observe for any signs of infection or complications
- Document the amount, color, and consistency of removed wax
- Ensure the ear canal is dry
5️⃣ Health Education to Prevent Recurrence
🟢 Do’s:
- Clean outer ear only, gently with a washcloth
- Use prescribed cerumenolytic drops periodically if prone to wax
- Visit healthcare provider for regular ear checks if recurrent issue
🔴 Don’ts:
- Avoid using cotton buds, matchsticks, pins in the ear
- Avoid water entry if there’s an open canal or perforation
- Do not self-irrigate with force or if unsure of condition
🔷 IV. EVALUATION
✔️ Relief of ear discomfort and pain
✔️ Wax successfully removed without complications
✔️ Hearing improved or restored
✔️ Patient demonstrates understanding of ear hygiene
✔️ No signs of infection post-removal
🧠 KEY NURSING POINTS
✅ Always rule out eardrum perforation before irrigation
✅ In children or uncooperative adults, sedation or ENT referral may be needed
✅ Document everything: symptoms, procedure steps, patient response
✅ Nurses can play a major role in screening, early detection, and safe wax removal in primary care.
🍽️ NUTRITIONAL CONSIDERATIONS
Although impacted wax is not directly a nutritional disorder, certain general nutritional aspects support ear health and prevent infections, especially in recurrent cases.
✅ Recommended Nutritional Considerations:
1️⃣ Hydration
💧 Adequate water intake helps maintain moisture in secretions, including cerumen.
🔸 Dry cerumen is more likely to become impacted.
2️⃣ Vitamin A
🥕 Found in carrots, sweet potatoes, spinach
✅ Maintains healthy epithelial tissue in the ear canal
3️⃣ Vitamin C & Zinc
🍊 Citrus fruits, nuts, seeds
✅ Boosts immune defense and tissue repair in case of infections
4️⃣ Vitamin D
☀️ Sunlight exposure and fortified foods
✅ Deficiency linked to higher infection risk
5️⃣ Avoid excess sugar and processed food
❌ May reduce immune efficiency and promote inflammation
🔔 Special dietary attention may be needed post-ear surgery or infection for tissue healing and immune support
⚠️ COMPLICATIONS OF IMPACTED WAX
If not treated promptly, impacted wax can lead to several problems:
| Complication | Description |
|---|---|
| 🔊 Conductive hearing loss | Common if canal is fully blocked |
| 🤕 Otalgia (ear pain) | Due to pressure against ear canal or eardrum |
| 💧 Otitis externa | Wax traps moisture → bacterial or fungal infection |
| 🧠 Vertigo or imbalance | Especially if wax touches tympanic membrane |
| ⚡ Tinnitus | Ringing or buzzing sensation |
| 🧪 Difficulty in ear examination | Can mask other pathologies like infections or perforations |
| 🧯 Tympanic membrane injury | Improper removal techniques can lead to perforation |
🧠 KEY POINTS FOR NURSING STUDENTS & CLINICIANS
✅ Cerumen is protective – It lubricates, cleans, and prevents microbial growth
✅ Impacted wax = pathological only when it causes symptoms or occlusion
✅ Always assess for tympanic membrane integrity before any irrigation
✅ Avoid inserting sharp or long objects into ears – primary cause of wax impaction
✅ Use cerumenolytics first to soften hard wax before removal
✅ Never irrigate the ear in cases of perforation, past ear surgery, or severe otitis externa
✅ Educate patients on safe ear hygiene and the risks of self-cleaning
✅ Referral to ENT is essential for impacted wax with complications or uncooperative patients,
🥁👂 TYMPANIC MEMBRANE PERFORATION
📘 DEFINITION
Tympanic Membrane Perforation refers to a tear or hole in the tympanic membrane (eardrum) — the thin tissue that separates the external ear canal from the middle ear. It can lead to hearing loss, pain, or middle ear infection.
🔍 ANATOMY REMINDER
🧠 The tympanic membrane is a delicate, semitransparent membrane that:
- Vibrates in response to sound waves
- Transmits sound to the ossicles (middle ear bones)
- Protects the middle and inner ear from external pathogens and debris
⚠️ CAUSES OF TYMPANIC MEMBRANE PERFORATION
🔹 1. Infective Causes
- Acute otitis media (AOM): Pressure from pus/fluid buildup can rupture the membrane
- Chronic otitis media: Long-standing infection with intermittent rupture
🔹 2. Traumatic Causes
- Direct trauma: Insertion of foreign objects (cotton buds, hairpins)
- Slap to the ear (boxing, domestic abuse) → pressure wave rupture
- Skull fracture involving the temporal bone
- Blast injuries (e.g., explosion or gunshot near the ear)
🔹 3. Barotrauma
- Sudden changes in atmospheric pressure (e.g., flying, scuba diving, hyperbaric chambers)
- Eustachian tube dysfunction increases susceptibility
🔹 4. Iatrogenic (Medical Procedure–related)
- Improper ear syringing
- Trauma during ear surgery
- Perforation during foreign body removal
🧬 TYPES OF TYMPANIC MEMBRANE PERFORATION
Tympanic membrane perforations are classified based on their location, size, cause, and duration:
🔸 A. Based on Location
| Type | Description |
|---|---|
| 🟠 Central perforation | Perforation within the pars tensa, surrounded by membrane margin — most common and usually less severe |
| 🔴 Marginal perforation | Edge of the membrane; higher risk of complications and cholesteatoma |
| 🟡 Attic perforation | In the pars flaccida (superior part); often associated with chronic infections and cholesteatoma risk |
🔸 B. Based on Size
| Type | Description |
|---|---|
| ⬤ Small | Pinpoint-sized or <25% of TM |
| ⬤ Moderate | Involves 25–50% of TM |
| ⬤ Large/Subtotal | >50% or almost entire membrane |
| ⬤ Total | Complete absence of membrane |
🔸 C. Based on Duration
| Type | Description |
|---|---|
| 🕒 Acute | Recent onset (within days to 2 weeks); often heals spontaneously |
| 🕐 Chronic | Lasts >3 months; often associated with repeated infections or cholesteatoma |
🔬 PATHOPHYSIOLOGY OF TYMPANIC MEMBRANE PERFORATION
1️⃣ Triggering Event (infection, trauma, barotrauma) →
2️⃣ Sudden or progressive increase in pressure inside the middle ear
⮕ Caused by pus, fluid, or external mechanical force
3️⃣ The tympanic membrane (TM), being thin and delicate, ruptures due to:
- Pressure overload from behind (e.g., AOM)
- Sudden negative pressure (e.g., slap, blast injury)
- Direct penetration (e.g., sharp object)
4️⃣ Once perforated:
- Middle ear becomes open to the external environment
- Pathogens can easily enter, leading to otitis media or externa
- Sound transmission is disrupted, causing conductive hearing loss
5️⃣ If untreated or recurrent:
- Chronic infection may occur
- Tympanic membrane fails to heal → forms chronic suppurative otitis media (CSOM)
- Risk of cholesteatoma and ossicular damage
🚨 SIGNS & SYMPTOMS OF TYMPANIC MEMBRANE PERFORATION
| Symptom | Description |
|---|---|
| 🔇 Hearing loss | Usually conductive, varies with size/location of perforation |
| 💧 Ear discharge (otorrhea) | Clear, purulent, or blood-tinged; often foul-smelling |
| 🤕 Ear pain (otalgia) | Usually present in acute or traumatic perforations |
| 🔊 Tinnitus | Ringing or buzzing sound in the affected ear |
| 🌀 Vertigo or dizziness | May occur if inner ear is involved or due to sudden trauma |
| 💥 Bleeding from ear | Seen in traumatic or barotrauma-related perforations |
| 😷 Associated symptoms | Fever, sore throat, nasal congestion (if due to infection) |
🔔 Many small perforations may be asymptomatic, especially in chronic cases.
🧪 DIAGNOSIS OF TYMPANIC MEMBRANE PERFORATION
✅ 1. History Collection
- Sudden pain, trauma, slap, infection, ear manipulation
- Hearing loss or discharge
- Travel, diving, or air pressure exposure
✅ 2. Physical Examination
- Inspection of the auricle and external ear
- Presence of swelling, tenderness, discharge
✅ 3. Otoscopy / Pneumatic Otoscopy
- Visualization of a tear, hole, or absence of tympanic membrane
- May show:
- Central/marginal perforation
- Active discharge
- Erythema, bulging (infection)
✅ 4. Tuning Fork Tests
| Test | Expected Finding (Conductive Loss) |
|---|---|
| 🔔 Rinne Test | Bone conduction > air conduction (negative) |
| 🎧 Weber Test | Sound lateralizes to the affected ear |
✅ 5. Audiometry (Pure Tone)
- Confirms degree and type of hearing loss
- Mostly shows conductive hearing loss
- Sensorineural loss possible in severe trauma
✅ 6. Tympanometry
- Type B (flat curve) indicating middle ear fluid or perforation
- Helps assess TM mobility and Eustachian tube function
✅ 7. Imaging (in complicated cases)
- CT scan of Temporal Bone: If chronic ear disease, cholesteatoma, or bone erosion is suspected
- MRI: To assess soft tissue involvement or intracranial spread
💊🩺 MEDICAL MANAGEMENT OF TYMPANIC MEMBRANE PERFORATION
Medical treatment aims to control infection, relieve symptoms, and promote natural healing, especially in acute or small perforations.
🔷 1️⃣ Acute Tympanic Membrane Perforation
✅ Conservative Management (especially in traumatic or AOM-induced perforations):
- 🔸 Keep ear dry: Avoid water entry during bathing or cleaning
➤ Use cotton ball coated with petroleum jelly during showers - 🔸 Analgesics:
- Paracetamol or ibuprofen for pain relief
- 🔸 Antibiotic Ear Drops (if discharge present):
- Ciprofloxacin or Ofloxacin drops
➤ Avoid aminoglycoside drops (e.g., gentamicin) if there’s a risk of inner ear toxicity
- Ciprofloxacin or Ofloxacin drops
- 🔸 Oral Antibiotics (if secondary bacterial infection or active discharge):
- Amoxicillin-clavulanate
- Cefuroxime or azithromycin (based on culture, if taken)
- 🔸 Decongestants/Nasal sprays:
- To improve Eustachian tube function and reduce middle ear pressure
- Eg: Xylometazoline (nasal spray)
- 🔸 Steroids (rarely used):
- Only in inflammation or allergic cases under ENT supervision
🔷 2️⃣ Chronic Perforation or CSOM (Chronic Suppurative Otitis Media)
- Long-term management includes:
- Aural toilet (gentle cleaning under microscope)
- Topical antibiotics/steroids based on discharge and infection
- Treatment of underlying causes (e.g., sinusitis, allergy)
🏥🔧 SURGICAL MANAGEMENT OF TYMPANIC MEMBRANE PERFORATION
Surgery is indicated if the perforation:
✅ Does not heal within 6–8 weeks
✅ Is large or subtotal
✅ Is associated with recurrent infections or cholesteatoma
✅ Causes significant hearing loss
🔧 1️⃣ Myringoplasty
➤ Repair of tympanic membrane alone, without middle ear exploration
- Graft material:
- Temporalis fascia (most common)
- Tragal cartilage, perichondrium
- Approach:
- Postaural (behind ear) or endaural
- Outcome:
- High success rate if no active infection
- Improved hearing and dry ear
🔧 2️⃣ Tympanoplasty
➤ Repair of TM + ossicular chain reconstruction (if damaged)
- Types (I to V) based on extent of middle ear reconstruction
- Includes ossiculoplasty if ossicles are eroded
- Restores both structure and hearing function
🔧 3️⃣ Mastoidectomy (in complicated cases)
➤ Indicated if there’s cholesteatoma, mastoid abscess, or chronic mastoiditis
- Involves removal of infected mastoid air cells
- Combined with tympanoplasty often
🧑⚕️ Postoperative Care Includes:
- Ear kept dry
- Avoid nose blowing
- Antibiotics and analgesics
- Follow-up for graft inspection
- Hearing test after healing
👩⚕️🩺 NURSING MANAGEMENT OF TYMPANIC MEMBRANE PERFORATION
🎯 OBJECTIVES
✅ Relieve discomfort and prevent complications
✅ Promote healing of the tympanic membrane
✅ Maintain hygiene and dryness of the affected ear
✅ Educate the patient on ear care and follow-up
✅ Support pre- and post-operative recovery (if surgery is done)
🔷 I. NURSING ASSESSMENT
- 📋 Collect subjective data:
- Onset and duration of ear pain, discharge, or hearing loss
- History of trauma, infection, ear manipulation, or barotrauma
- 👂 Physical observation:
- Assess for ear discharge, odor, and color
- Inspect for signs of infection (swelling, redness, fever)
- Check hearing using whisper test or tuning fork (if trained)
🔷 II. NURSING DIAGNOSES
1️⃣ Acute pain related to tympanic membrane injury
2️⃣ Risk for infection related to open tympanic barrier
3️⃣ Impaired sensory perception (hearing) related to perforation
4️⃣ Knowledge deficit related to ear care and prevention
5️⃣ Risk for disturbed body image (post-surgery cases)
🔷 III. NURSING INTERVENTIONS
✅ 1. Pain & Symptom Management
- Administer prescribed analgesics (paracetamol, ibuprofen)
- Apply warm dry compresses (if advised by physician)
- Encourage rest and quiet environment to reduce discomfort
✅ 2. Infection Prevention & Ear Care
- Instruct patient to keep ear dry (use cotton plug while bathing)
- Clean discharge gently with sterile gauze
- Do not insert ear buds or any object into the ear
- Administer prescribed ear drops carefully:
- Pull pinna up and back for adults
- Maintain correct positioning after instillation for a few minutes
✅ 3. Monitoring and Reporting
- Monitor for:
- Fever, purulent discharge, or increased pain
- Signs of vertigo or worsening hearing loss
- Report any signs of complications like bleeding, persistent discharge, or facial weakness
✅ 4. Preoperative & Postoperative Care (if surgery is planned)
Preoperative:
- Provide psychological support and reduce anxiety
- Educate about myringoplasty or tympanoplasty procedures
- Explain NPO status and pre-surgical hygiene
Postoperative:
- Position the patient with the operated ear facing upward
- Instruct patient to avoid sneezing with closed mouth
- Avoid blowing nose forcefully
- Administer antibiotics and monitor for post-op pain, dizziness, or drainage
- Educate about follow-up appointments and hearing evaluation
✅ 5. Health Education
- Avoid inserting any object into ears
- Avoid swimming or diving until healing is confirmed
- Report immediately if hearing worsens, discharge increases, or fever develops
- Use protective earplugs if exposed to loud sounds or pressure changes
- Encourage regular ENT checkups for recurrent infections
🔷 IV. EVALUATION
✔️ Patient reports relief from pain and discharge
✔️ Tympanic membrane heals without complications
✔️ Hearing function maintained or improved
✔️ Patient demonstrates knowledge of ear care and precautions
✔️ No further infection or reinjury occurs.
🍽️ NUTRITIONAL CONSIDERATIONS
Although tympanic membrane perforation is not directly linked to nutrition, proper dietary support plays a key role in:
🔹 Promoting healing
🔹 Preventing infection
🔹 Supporting immune response, especially in post-operative or chronic cases
✅ Recommended Nutritional Guidelines:
1️⃣ High-Protein Diet
- Essential for tissue repair and regeneration
- Sources: Eggs, milk, pulses, meat, paneer, soy
2️⃣ Vitamin C
- Supports collagen formation and boosts immunity
- Sources: Citrus fruits (orange, lemon), guava, amla, bell peppers
3️⃣ Vitamin A
- Maintains healthy epithelial tissues (including the tympanic membrane lining)
- Sources: Carrots, spinach, pumpkin, mangoes
4️⃣ Zinc & Iron
- Support immune function and oxygen transport for healing
- Sources: Nuts, seeds, legumes, green leafy vegetables
5️⃣ Hydration
- Keeps mucous membranes moist and prevents further infection
- Encourage plenty of fluids, especially in febrile or infective conditions
⚠️ If the patient has infection with fever, increase fluid and vitamin intake accordingly.
⚠️ COMPLICATIONS OF TYMPANIC MEMBRANE PERFORATION
If untreated or poorly managed, the following complications may arise:
🔹 Acute Complications
| 🩺 Complication | Description |
|---|---|
| 🔊 Conductive hearing loss | Due to impaired vibration of TM |
| 💧 Chronic ear discharge | Indicates chronic suppurative otitis media |
| 🦠 Otitis media or externa | Recurrent or persistent infections |
| 🌀 Vertigo or imbalance | Especially if middle or inner ear involved |
🔹 Chronic/Severe Complications
| 🧠 Complication | Description |
|---|---|
| ❌ Tympanosclerosis | Scarring and thickening of the eardrum |
| 🧫 Cholesteatoma | Growth of skin cells in the middle ear → bone erosion |
| 🔇 Permanent hearing loss | Due to ossicle damage or chronic infection |
| 🧠 Intracranial spread | Meningitis, brain abscess (rare but serious) |
🧠 KEY POINTS TO REMEMBER
✅ Tympanic membrane perforation is commonly caused by infection, trauma, or barotrauma
✅ Most acute small perforations heal spontaneously with conservative care
✅ Avoid inserting objects or water into the ear during recovery
✅ Diagnosis is confirmed by otoscopy and audiometry
✅ Myringoplasty or tympanoplasty may be required for large, non-healing, or chronic perforations
✅ Nurses play a key role in:
- Pain relief
- Ear care
- Medication administration
- Health education for recurrence prevention
✅ Encourage balanced nutrition to support healing and prevent infections
✅ Refer promptly if:
- Hearing loss worsens
- Discharge persists
- Vertigo or severe symptoms occur
👂🦠 OTITIS MEDIA
📘 DEFINITION
Otitis media is defined as the inflammation or infection of the middle ear — the air-filled space located behind the tympanic membrane (eardrum) that contains the ossicles (malleus, incus, stapes).
It may be:
- Acute (sudden onset, short duration)
- Chronic (persistent or recurring with discharge)
- With or without effusion (fluid accumulation)
🔬 ANATOMICAL REFERENCE
🧠 The middle ear connects to the nasopharynx via the Eustachian tube, which helps in pressure equalization and drainage.
When this tube is blocked or dysfunctional, it leads to fluid accumulation, infection, and inflammation — resulting in otitis media.
🔎 CAUSES OF OTITIS MEDIA
🔹 I. Infectious Causes
- Bacterial Infections (most common in acute cases):
- Streptococcus pneumoniae
- Haemophilus influenzae
- Moraxella catarrhalis
- Staphylococcus aureus (especially in chronic cases)
- Viral Infections (especially in children):
- Respiratory syncytial virus (RSV)
- Influenza virus
- Adenovirus
- Rhinovirus
Viral URTI often precedes bacterial otitis media.
🔹 II. Obstruction or Dysfunction of Eustachian Tube
- Allergies (e.g., allergic rhinitis)
- Adenoid hypertrophy
- Cleft palate
- Enlarged tonsils
- Sinusitis
- Nasal polyps
🔹 III. Predisposing Factors
| Factor | Explanation |
|---|---|
| 🧒 Age (6 months – 2 years) | Eustachian tube is shorter and more horizontal |
| 🧫 URTI history | Infection spreads from throat to ear |
| 🌬️ Sudden atmospheric changes | Airplane descent, diving → barotrauma |
| 🚬 Passive smoking | Damages mucociliary function |
| 🍼 Bottle feeding in lying position | Allows milk to enter Eustachian tube |
| 🧬 Genetic/family history | Recurrent ear infections seen in families |
| 🏘️ Daycare attendance | Higher risk of infections in children |
🧾 TYPES OF OTITIS MEDIA
Otitis Media (OM) is classified based on onset, duration, presence of fluid, and recurrence. The main types are:
🔷 1️⃣ Acute Otitis Media (AOM)
🔹 Definition:
A sudden-onset infection of the middle ear, often caused by bacteria or viruses, and commonly follows an upper respiratory infection (URI).
🔹 Features:
- Rapid onset of ear pain, fever, irritability
- Bulging and inflamed tympanic membrane
- May have middle ear effusion (fluid) with or without perforation
🔹 Common in: Infants and young children (6 months – 3 years)
🔷 2️⃣ Otitis Media with Effusion (OME)
(Also called Serous Otitis Media or Glue Ear)
🔹 Definition:
Presence of non-infected fluid (effusion) in the middle ear without signs of acute infection.
🔹 Features:
- No pain or fever
- Feeling of fullness or mild hearing loss
- Tympanic membrane appears retracted or dull, with visible fluid level
🔹 Cause:
- Eustachian tube dysfunction post-infection or allergy
🔹 Common in: Children with recent AOM, allergic rhinitis, or adenoid hypertrophy
🔷 3️⃣ Chronic Suppurative Otitis Media (CSOM)
🔹 Definition:
Persistent or recurrent ear discharge through a perforated tympanic membrane, lasting more than 6–12 weeks.
🔹 Features:
- Continuous or intermittent purulent, foul-smelling discharge
- Conductive hearing loss
- May be painless
- High risk of cholesteatoma, ossicular damage, and intracranial complications
🔹 Causes:
- Poorly treated AOM
- Repeated infections
- Trauma or surgery
🔷 4️⃣ Recurrent Acute Otitis Media (RAOM)
🔹 Definition:
≥3 episodes of acute otitis media within 6 months or ≥4 episodes in 1 year, with resolution between episodes.
🔹 Risk Factors:
- Young age
- Bottle feeding
- Daycare attendance
- Passive smoking
- Immature immune system
🔷 5️⃣ Adhesive Otitis Media
🔹 Definition:
Chronic condition in which the tympanic membrane becomes tightly adherent to the middle ear structures due to prolonged negative pressure.
🔹 Features:
- Thin, retracted TM
- Hearing loss
- Often asymptomatic until advanced
🔷 6️⃣ Tympanosclerosis / Otitis Media with Sequelae
🔹 Definition:
Scarring and calcification of the tympanic membrane or middle ear structures after repeated episodes of OM.
🔹 Features:
- White patches on TM
- Reduced mobility of the membrane
- Conductive hearing loss
🧬🔬 PATHOPHYSIOLOGY OF OTITIS MEDIA
Otitis media involves inflammation and/or infection of the middle ear, typically following Eustachian tube dysfunction. The exact mechanisms vary slightly between Acute Otitis Media (AOM), Otitis Media with Effusion (OME), and Chronic Suppurative Otitis Media (CSOM).
🔷 1️⃣ ACUTE OTITIS MEDIA (AOM)
🔁 Step-by-Step Pathophysiological Process:
- Precipitating factor (e.g., viral upper respiratory infection, allergy)
⮕ Causes Eustachian tube dysfunction (ETD) - ETD leads to impaired ventilation and drainage of the middle ear
- Resulting in negative pressure in the middle ear cavity
⮕ Promotes fluid accumulation (effusion) - The stagnant fluid becomes secondarily infected by bacteria or viruses
🔹 Common pathogens: Streptococcus pneumoniae, Haemophilus influenzae, Moraxella catarrhalis - Inflammatory response leads to:
- Redness and bulging of the tympanic membrane
- Increased vascular permeability
- Pus formation in the middle ear cavity
- If pressure builds up excessively, it may result in:
- Rupture of the tympanic membrane
- Otorrhea (ear discharge)
- Temporary conductive hearing loss
🔷 2️⃣ OTITIS MEDIA WITH EFFUSION (OME)
🔁 Mechanism:
- Following an AOM episode or due to allergic inflammation
- Eustachian tube remains blocked, but no active infection
- Sterile fluid (serous or mucoid) collects in the middle ear
- Fluid is thick and sticky, interfering with sound conduction
- Chronic presence of fluid may affect speech and learning in children
🔷 3️⃣ CHRONIC SUPPURATIVE OTITIS MEDIA (CSOM)
🔁 Mechanism:
- Repeated episodes of AOM or untreated ear infections
- Leads to persistent perforation of the tympanic membrane
- Chronic bacterial colonization and continuous inflammatory response
- Granulation tissue and polyp formation may occur
- Continuous or intermittent purulent discharge from middle ear
- Over time, there may be:
- Ossicular damage
- Cholesteatoma formation
- Bone erosion (e.g., mastoid, temporal bone)
- Risk of intracranial complications
🧠 Summary of Key Processes Involved:
| 🔍 Event | 🧠 Consequence |
|---|---|
| Eustachian tube dysfunction | Negative middle ear pressure |
| Fluid accumulation | Impaired hearing, infection risk |
| Bacterial/viral infection | Inflammatory response, pus formation |
| Tympanic membrane rupture | Relief of pressure, discharge |
| Chronic inflammation | Permanent structural damage & hearing loss |
🚨 SIGNS AND SYMPTOMS OF OTITIS MEDIA
The presentation of Otitis Media varies depending on its type and stage. Below is a breakdown:
🔷 1️⃣ Acute Otitis Media (AOM)
| Symptom | Description |
|---|---|
| 🤕 Ear pain (otalgia) | Sudden, severe, often worse at night |
| 🌡️ Fever | Mild to high-grade, especially in children |
| 💧 Ear discharge | If tympanic membrane ruptures (serous/purulent) |
| 🔇 Hearing loss | Conductive, temporary |
| 🔊 Tinnitus | Ringing or buzzing (occasionally present) |
| 🧒 Irritability / Crying | In infants and toddlers |
| 🛌 Restlessness / Poor sleep | Discomfort during lying down |
| 🤢 Nausea or vomiting | Associated with inner ear irritation |
🔷 2️⃣ Otitis Media with Effusion (OME)
(Also known as Serous Otitis Media)
| Symptom | Description |
|---|---|
| 🔇 Mild hearing loss | Often the only symptom |
| 🌀 Ear fullness or popping | Due to fluid behind tympanic membrane |
| 💬 Speech delay in children | Especially in chronic or bilateral cases |
| ❌ No fever or pain | Unlike acute otitis media |
🔷 3️⃣ Chronic Suppurative Otitis Media (CSOM)
| Symptom | Description |
|---|---|
| 💧 Persistent ear discharge | Foul-smelling, purulent, may be intermittent |
| 🔇 Conductive hearing loss | Progressive, due to ossicle damage |
| ❌ No pain usually | Unless secondary infection is present |
| 🧫 Granulation/polyps | May be visible in external canal |
| 🧠 Vertigo/headache | If inner ear or intracranial involvement |
🧪 DIAGNOSIS OF OTITIS MEDIA
Diagnosis involves a combination of clinical history, physical examination, and investigations.
🔷 A. Clinical History
✅ Key questions to ask:
- Recent cold or upper respiratory infection
- Any ear pain, discharge, or hearing changes
- History of recurrent episodes or trauma
- Family history, feeding habits, daycare exposure (in children)
🔷 B. Physical Examination
👂 Otoscopy / Pneumatic Otoscopy
Gold standard for visual diagnosis
| Otoscopic Findings | Interpretation |
|---|---|
| 🔴 Red, bulging TM | Acute Otitis Media (AOM) |
| 💧 Fluid level behind TM | Otitis Media with Effusion (OME) |
| ⬛ Perforated TM | Suggests CSOM or ruptured AOM |
| ⚪ White plaques on TM | Tympanosclerosis (chronic sequelae) |
| ❌ Immobile TM on pneumatic otoscopy | Suggests middle ear effusion |
🔷 C. Hearing Tests
🎧 Tuning Fork Tests
- Rinne Test: Negative (BC > AC) in conductive loss
- Weber Test: Lateralizes to affected ear
🩺 Pure Tone Audiometry
- Shows conductive hearing loss
- Helps measure degree of impairment
🔷 D. Tympanometry
- Type B curve: Indicates fluid in middle ear or perforation
- Type C: Suggests Eustachian tube dysfunction
🔷 E. Laboratory Investigations (if needed)
- 💉 Culture and Sensitivity: Of ear discharge (in CSOM)
- 🧫 CBC: May show elevated WBCs in infection
- 🧠 CT Scan / MRI: For suspected complications (mastoiditis, cholesteatoma, brain abscess)
💊🩺 MEDICAL MANAGEMENT OF OTITIS MEDIA
Management depends on the type, severity, and duration of the condition.
🔷 1️⃣ ACUTE OTITIS MEDIA (AOM)
🎯 Goals:
- Control infection
- Relieve pain and fever
- Prevent complications (e.g., perforation, mastoiditis)
✅ Pharmacological Management
| Drug Class | Examples | Purpose |
|---|---|---|
| 💊 Analgesics / Antipyretics | Paracetamol, Ibuprofen | Reduce ear pain and fever |
| 💊 Antibiotics | Amoxicillin (1st line), Amoxicillin-Clavulanate, Cefuroxime | Treat bacterial infection (7–10 days) |
| 💧 Ear drops (only after perforation) | Ciprofloxacin or Ofloxacin drops | For purulent discharge post-perforation |
| 🧴 Nasal decongestants | Xylometazoline nasal drops/spray | Relieve Eustachian tube blockage |
🔔 Observation Approach may be used in mild cases (especially in children >2 years) for 48–72 hrs, with symptom-based care before initiating antibiotics.
🔷 2️⃣ OTITIS MEDIA WITH EFFUSION (OME)
🎯 Goals:
- Promote natural drainage
- Restore Eustachian tube function
- Monitor for hearing impairment in children
✅ Pharmacological Measures
- Nasal decongestants – Short term use for congestion
- Antihistamines (e.g., cetirizine) – In allergic children
- Nasal corticosteroids (e.g., mometasone) – For adenoid-related blockage
🚫 Routine use of systemic antibiotics is not recommended unless secondarily infected.
🔄 Observation & Monitoring:
🔷 3️⃣ CHRONIC SUPPURATIVE OTITIS MEDIA (CSOM)
🎯 Goals:
- Control chronic infection
- Prevent further hearing loss
- Prepare ear for possible surgical repair
✅ Medical Management
| Measure | Details |
|---|---|
| 💧 Topical antibiotics | Ciprofloxacin/Ofloxacin ear drops (with or without steroids) |
| 🧴 Aural toilet | Cleaning of discharge and debris using suction or gauze |
| 💊 Oral antibiotics | For acute exacerbations (based on culture if possible) |
| ❌ Avoid water entry | Keep ears dry — use cotton with petroleum jelly while bathing |
| 🚫 Avoid ototoxic drops | Especially if TM is perforated (e.g., gentamicin drops) |
🧠 Special Considerations:
- Evaluate for cholesteatoma or mastoiditis if discharge is persistent, foul-smelling, or associated with granulation tissue.
🏥🔧 SURGICAL MANAGEMENT OF OTITIS MEDIA
Surgical intervention is considered when medical management fails, or in complicated and chronic cases of otitis media to prevent or treat hearing loss, recurrent infections, or structural damage.
🔷 1️⃣ ACUTE OTITIS MEDIA (AOM)
🔸 Surgery is rarely required, but may be necessary in complications such as:
✅ Myringotomy
- A small incision made in the tympanic membrane to drain pus/fluid from the middle ear
- Relieves pressure and pain
- Indicated in severe AOM with bulging TM or failed antibiotic response
🔸 Tympanostomy Tube Insertion (Grommets)
- A small ventilation tube is placed through the myringotomy incision
- Allows continuous middle ear aeration and prevents fluid re-accumulation
🔷 2️⃣ OTITIS MEDIA WITH EFFUSION (OME)
🔸 Surgery is indicated if effusion persists for more than 3 months with:
- Hearing loss
- Speech delay
- Recurrent AOM
- Anatomical defects (e.g., cleft palate)
✅ Myringotomy with Grommet Insertion
- Helps ventilate middle ear and drain sterile fluid
- Grommets usually fall out spontaneously in 6–12 months
✅ Adenoidectomy
- Removal of enlarged adenoids (if contributing to Eustachian tube blockage)
🔷 3️⃣ CHRONIC SUPPURATIVE OTITIS MEDIA (CSOM)
🔸 Surgical treatment is often definitive and curative
✅ Tympanoplasty
- Surgical repair of the tympanic membrane and ossicular reconstruction (if needed)
- Indicated in chronic perforation with or without hearing loss
✅ Mastoidectomy
- Removal of infected mastoid air cells in the mastoid bone
- Indicated in:
- Cholesteatoma
- Recurrent mastoiditis
- Extensive middle ear disease
Types:
- Cortical (simple) mastoidectomy
- Modified radical mastoidectomy
- Radical mastoidectomy
✅ Myringoplasty
- Repair of tympanic membrane only without ossicle involvement
- Graft materials: temporalis fascia, tragal cartilage
⚠️ COMBINED PROCEDURES
Often performed together:
- Tympanoplasty + Mastoidectomy
- Grommet insertion + Adenoidectomy
🧠 Postoperative Care Includes:
- Keep ear dry
- Administer prescribed antibiotics and analgesics
- Avoid nose blowing, sneezing with mouth closed
- Regular follow-up and audiometry
- Wound care and monitoring for discharge, fever, dizziness
👩⚕️🩺 NURSING MANAGEMENT OF OTITIS MEDIA
🎯 OBJECTIVES OF NURSING CARE
✅ Relieve pain and discomfort
✅ Prevent complications (e.g., hearing loss, mastoiditis)
✅ Administer prescribed medications correctly
✅ Maintain ear hygiene
✅ Educate the patient and family
✅ Support pre- and post-operative recovery (if surgery is done)
🔷 I. NURSING ASSESSMENT
1️⃣ Subjective Data
- Complaints of ear pain, fullness, or discharge
- History of URI, allergies, or ear trauma
- Changes in hearing, irritability (in children), or sleep disturbances
2️⃣ Objective Data
- Vital signs: Check for fever
- Observe ear canal for discharge or odor
- Assess for hearing changes
- Check facial symmetry (rule out complications affecting cranial nerve VII)
🔷 II. NURSING DIAGNOSES
| Nursing Diagnosis | Related to |
|---|---|
| 🩺 Acute pain | Inflammation of middle ear |
| 🛌 Disturbed sleep pattern | Due to ear pain |
| 🔇 Impaired sensory perception (hearing) | Fluid or infection in the middle ear |
| 🧫 Risk for infection spread | Middle ear infection |
| ❌ Deficient knowledge | Lack of awareness about ear hygiene, medication |
| 😓 Anxiety (in child/parent) | Illness, pain, possible surgery |
🔷 III. NURSING INTERVENTIONS
✅ 1. Pain and Symptom Management
- Administer analgesics and antipyretics (e.g., paracetamol, ibuprofen) as prescribed
- Apply warm compress to the affected ear (if not draining) for relief
- Encourage rest and reduced noise exposure
✅ 2. Medication Administration
- Instill ear drops correctly:
- Warm to body temperature before use
- Pull pinna up and back for adults, down and back for children
- Keep patient in position for 5 minutes post-instillation
- Administer antibiotics (oral or topical) as per schedule
- Monitor for side effects or allergic reactions
✅ 3. Preventing Infection and Complications
- Keep the ear dry – Use a cotton ball with petroleum jelly during bathing
- Clean external discharge gently with sterile gauze
- Do not insert objects like cotton buds or fingers into the ear
- Educate parents to avoid feeding infants in a lying position
✅ 4. Preoperative and Postoperative Care (if surgery is planned)
Pre-op:
- Prepare patient and family for tympanoplasty or myringotomy
- Ensure informed consent, pre-op instructions, and NPO status
- Provide psychological support, especially in children
Post-op:
- Position patient with the operated ear facing upward
- Avoid coughing, sneezing, or blowing nose forcefully
- Maintain aseptic dressing care
- Monitor for dizziness, discharge, fever, or hearing loss
✅ 5. Health Education
- Instruct on completing the full course of antibiotics
- Emphasize follow-up audiometry in chronic/recurrent cases
- Counsel parents about speech delay monitoring in children
- Teach safe ear cleaning practices
🔷 IV. EVALUATION
✔️ Pain relieved within 24–48 hours
✔️ Ear discharge reduced or resolved
✔️ Hearing returns to baseline (if temporary loss)
✔️ No signs of complications (e.g., vertigo, facial palsy)
✔️ Patient or caregiver demonstrates understanding of care
🍽️ NUTRITIONAL CONSIDERATIONS IN OTITIS MEDIA
While otitis media is not directly a nutritional disorder, proper nutrition plays a crucial supportive role in:
✅ Boosting immune response
✅ Aiding recovery
✅ Preventing recurrent infections, especially in children
✅ Recommended Nutritional Guidelines:
1️⃣ High-Protein Diet
- Helps in tissue repair and immune function
- Sources: Eggs, milk, pulses, tofu, fish
2️⃣ Vitamin C
- Boosts immunity and reduces infection severity
- Sources: Citrus fruits (oranges, lemon), guava, berries
3️⃣ Vitamin A
- Essential for maintaining healthy mucosal linings (including Eustachian tube and middle ear)
- Sources: Carrots, spinach, mangoes, sweet potatoes
4️⃣ Zinc & Iron
- Aid in wound healing and infection resistance
- Sources: Nuts, seeds, legumes, green leafy vegetables
5️⃣ Hydration
- Keeps mucosal tissues moist and helps in clearing infection
- Encourage fluids, especially in febrile or antibiotic-treated patients
⚠️ COMPLICATIONS OF OTITIS MEDIA
If left untreated or recurrent, otitis media may lead to serious local, regional, or systemic complications.
🔹 Local Complications
| Complication | Description |
|---|---|
| 🔇 Conductive hearing loss | Due to fluid, perforation, or ossicle damage |
| 🧫 Tympanic membrane perforation | May become chronic and affect hearing |
| 💧 Otorrhea | Persistent discharge |
| ⚪ Tympanosclerosis | Scarring of the eardrum |
🔹 Regional Complications
| Complication | Description |
|---|---|
| 🦴 Mastoiditis | Infection of mastoid bone; may need surgery |
| 🧠 Facial nerve palsy | Inflammation affects cranial nerve VII |
| 🧠 Labyrinthitis | Inner ear infection; causes vertigo |
🔹 Intracranial Complications (Rare but life-threatening)
| Complication | Description |
|---|---|
| 🧠 Meningitis | Infection spreads to meninges |
| 🧠 Brain abscess | Pus collection due to advanced infection |
| 💉 Lateral sinus thrombosis | Venous sinus clot due to ear infection |
🧠 KEY POINTS TO REMEMBER
✅ Otitis media is most common in infants and children due to short, horizontal Eustachian tubes
✅ Acute cases may resolve with observation or antibiotics
✅ OME (Serous Otitis) often follows AOM and may cause speech delay in children
✅ CSOM (Chronic) requires prolonged medical care or surgery
✅ Early treatment helps prevent hearing loss and complications
✅ Nurses must focus on:
- Pain relief
- Ear care
- Medication adherence
- Parental education
- Early referral for persistent/recurrent cases
✅ A balanced diet, hydration, and good hygiene support recovery
🎗️👂 MIDDLE EAR TUMORS
📘 DEFINITION
Middle ear tumors are abnormal growths (benign or malignant) that originate in the middle ear cavity, including the tympanic cavity, ossicles, and surrounding structures. They may arise from skin, vascular tissue, bone, or glands and may affect hearing, balance, or cranial nerves
🧪 CAUSES / RISK FACTORS
- Chronic suppurative otitis media (CSOM)
- Radiation exposure (e.g., previous cancer treatment)
- Genetic mutations or familial syndromes (e.g., paraganglioma syndrome)
- Chronic inflammation or recurrent middle ear infections
- Viral oncogenes (in rare cases)
- Environmental toxins or occupational exposure
- Age > 40 years (higher risk for malignancy)
🔍 TYPES OF MIDDLE EAR TUMORS
🔹 Benign Tumors
- Glomus tumor (Paraganglioma) – Most common
- Cholesteatoma – Benign but locally aggressive
- Osteoma – Arises from bony tissue
- Hemangioma – Vascular tumor
- Schwannoma – From nerve sheath of cranial nerves
🔹 Malignant Tumors
- Squamous cell carcinoma – Most common primary malignancy
- Adenocarcinoma – From glandular tissue
- Rhabdomyosarcoma – Rare, in children
- Basal cell carcinoma – Rare in middle ear, more common in outer ear
- Metastatic tumors – Rare (from breast, kidney, or lung)
🧬 PATHOPHYSIOLOGY
- Tumor cells arise from vascular, glandular, squamous, or neural tissues in the middle ear
- Benign tumors (e.g., glomus) are highly vascular and slowly progressive
- Malignant tumors invade locally (ossicles, cochlea, facial nerve, dura)
- Tumor may obstruct Eustachian tube → causes fluid accumulation or secondary infection
- In advanced cases, tumors may erode bone, enter inner ear or brain, or cause cranial nerve dysfunction
🚨 SIGNS AND SYMPTOMS
| Symptom | Description |
|---|---|
| 🔇 Hearing loss | Conductive, sensorineural, or mixed |
| 💧 Persistent ear discharge | May be foul-smelling or blood-stained |
| 🔊 Pulsatile tinnitus | Especially in glomus tumors |
| 🌀 Vertigo or imbalance | Tumor encroaching on inner ear |
| 🧠 Headache | From pressure or intracranial involvement |
| 🤢 Facial nerve weakness | Due to nerve invasion (e.g., facial palsy) |
| 🩸 Bleeding from ear | Spontaneous or on manipulation |
| 💥 Fullness or pressure | Non-specific but common |
🧪 DIAGNOSIS
✅ 1. Clinical Examination
- Otoscopic findings: red/blue mass, polyp, bleeding
- Cranial nerve examination
✅ 2. Audiological Tests
- Pure Tone Audiometry (PTA) – Type and degree of hearing loss
- Tympanometry – Reduced mobility or Type B/C curve
✅ 3. Imaging Studies
- HRCT Temporal Bone – Bony erosion, tumor extent
- MRI with contrast – Soft tissue invasion, cranial nerve or brain involvement
- Angiography (for glomus tumors) – Vascular nature of lesion
✅ 4. Biopsy
- Incisional or excisional (with caution for vascular tumors)
- Histopathology confirms type and grade
💊 MEDICAL MANAGEMENT
🔹 Benign Tumors (e.g., glomus):
- Pre-op embolization of feeding vessels to reduce bleeding
- Steroids for edema or nerve inflammation
- Antibiotics if secondary infection present
- Observation in small, asymptomatic cases (especially elderly or unfit for surgery)
🔹 Malignant Tumors:
- Radiotherapy – For residual or inoperable tumors
- Chemotherapy – Often used in rhabdomyosarcoma or advanced SCC
- Pain control, antiemetics, and supportive medications as needed
🏥 SURGICAL MANAGEMENT
🔧 Primary Treatment for Most Tumors
| Procedure | Indications |
|---|---|
| 🩺 Tympanomastoidectomy | Tumor removal involving mastoid + middle ear |
| 🩺 Lateral temporal bone resection | Extensive tumors with bony invasion |
| 🩺 Facial nerve decompression | If facial palsy present |
| 🩺 Ossiculoplasty | To reconstruct ossicles post-tumor removal |
| 🧠 Craniotomy (neuro-otology cases) | For intracranial extension |
| 🩸 Pre-op embolization (glomus) | Reduces intraoperative bleeding |
Multidisciplinary approach (ENT + oncology + neurosurgery) may be required for advanced cases.
👩⚕️ NURSING MANAGEMENT
✅ Preoperative Care
- Assess hearing, balance, neurological signs
- Explain procedure, risks, and possible facial nerve involvement
- Educate about postoperative expectations (hearing loss, discharge)
- Ensure NPO, consent, and skin preparation
✅ Postoperative Care
- Monitor vital signs, bleeding, and dressing
- Assess for facial nerve function
- Position with operated side upward
- Administer analgesics, antibiotics, antiemetics
- Keep ear dry and clean
- Educate on avoidance of nose blowing, water entry, and heavy lifting
✅ Health Education
- Importance of follow-up and radiotherapy (if needed)
- Signs of recurrence: discharge, bleeding, new neurological signs
- Support for body image disturbances (especially if facial paralysis)
🍽️ NUTRITIONAL CONSIDERATIONS
- High-protein diet: Supports healing and tissue repair
- Iron and vitamin-rich foods: Combat anemia and boost immunity
- Soft foods: If facial weakness affects chewing/swallowing
- Hydration: Maintain mucosal health
- Supplements: Zinc, Vitamin C for wound healing
⚠️ COMPLICATIONS
| Complication | Description |
|---|---|
| 🔇 Permanent hearing loss | Post-surgery or tumor-induced |
| 🧠 Facial nerve palsy | Due to tumor invasion or surgical damage |
| 🧠 Intracranial spread | In malignancies |
| 🧫 Recurrence of tumor | Especially if margins were not clear |
| 💉 Post-op bleeding or CSF leak | Rare but serious |
| 💢 Psychological distress | Due to cosmetic deformity or hearing loss |
🧠 KEY POINTS TO REMEMBER
✅ Middle ear tumors are rare but potentially dangerous
✅ Glomus tumors are the most common benign vascular tumors
✅ Early signs: pulsatile tinnitus, hearing loss, discharge
✅ Imaging and biopsy are essential for diagnosis
✅ Surgery is the primary treatment; radiation/chemo for advanced cases
✅ Nurses play a key role in monitoring, infection prevention, and emotional support
✅ Multidisciplinary follow-up is essential for complete recovery and recurrence prevention
👂🌀 MÉNIÈRE’S DISEASE
📘 DEFINITION
Ménière’s disease is a chronic disorder of the inner ear that affects both hearing and balance. It is characterized by recurrent episodes of vertigo, fluctuating sensorineural hearing loss, tinnitus, and a feeling of aural fullness (ear pressure).
It results from an abnormal accumulation of endolymphatic fluid in the inner ear (labyrinth) — a condition called endolymphatic hydrops.
🔍 CAUSES / RISK FACTORS
The exact cause of Ménière’s disease is not fully understood, but several contributing factors and theories have been identified:
🔹 1. Endolymphatic Hydrops
- Overproduction or impaired absorption of endolymph (fluid in the inner ear)
- Leads to distention of the membranous labyrinth → affects cochlea and vestibular system
🔹 2. Autoimmune Reactions
- Immune-mediated damage to inner ear structures
🔹 3. Genetic Predisposition
- Family history in some cases (autosomal dominant pattern seen in a few)
🔹 4. Viral Infections
- Past viral labyrinthitis or vestibular neuritis may trigger inflammation and fluid imbalance
🔹 5. Allergies
- Allergic responses may disrupt inner ear fluid dynamics
🔹 6. Vascular Insufficiency
- Reduced blood flow to the cochlea or inner ear
🔹 7. Head Injury or Trauma
- May damage the endolymphatic sac or ducts
🔹 8. Migraine-Associated Vertigo
- Some cases overlap with vestibular migraine
🧠 Risk Factors Include:
- Age 20–50 years (peak incidence)
- Female gender (slightly more common)
- Stress or fatigue
- High salt intake or poor fluid regulation
- Caffeine, alcohol, smoking (may trigger or worsen episodes)
🔷 TYPES OF MÉNIÈRE’S DISEASE
Ménière’s disease can be classified based on its clinical presentation, extent of inner ear involvement, and laterality (one or both ears affected).
🔹 1️⃣ Classic (Typical) Ménière’s Disease
- Involves all four hallmark symptoms:
✅ Recurrent vertigo
✅ Fluctuating sensorineural hearing loss
✅ Tinnitus
✅ Aural fullness - Vertigo episodes last 20 minutes to several hours
- Hearing loss is initially reversible, but may become permanent over time
🔹 2️⃣ Cochlear Ménière’s Disease (“Lermoyez Syndrome”)
- Predominantly auditory symptoms without significant vertigo
- Hearing loss
- Tinnitus
- Aural fullness
- May progress later to include vestibular symptoms (vertigo)
🔹 3️⃣ Vestibular Ménière’s Disease
- Dominated by recurrent episodes of vertigo
- Minimal or no hearing loss initially
- Tinnitus and aural fullness may be absent or mild
- May later develop into typical Ménière’s disease with hearing involvement
🔹 4️⃣ Bilateral Ménière’s Disease
- Affects both ears, either simultaneously or sequentially
- More severe impact on balance and hearing
- Higher risk of permanent disability
🔹 5️⃣ Secondary Ménière’s Disease
- Occurs secondary to another identifiable cause, such as:
- Autoimmune inner ear disease
- Syphilis
- Head trauma
- Viral infection (labyrinthitis)
- Treatment often targets the underlying condition in addition to symptomatic relief
🧬 PATHOPHYSIOLOGY OF MÉNIÈRE’S DISEASE
🔁 Underlying Mechanism: Endolymphatic Hydrops
1️⃣ The inner ear contains two types of fluid:
- Endolymph (in the membranous labyrinth)
- Perilymph (in the bony labyrinth)
2️⃣ In Ménière’s disease, there is an abnormal increase in the volume or pressure of endolymph due to:
- Overproduction of endolymph
- Impaired absorption in the endolymphatic sac
- Obstruction of endolymphatic ducts
3️⃣ This leads to distention of the membranous labyrinth, affecting both:
- Cochlear structures (hearing loss, tinnitus)
- Vestibular structures (vertigo, imbalance)
4️⃣ As the condition progresses:
- Repeated episodes damage hair cells in the cochlea and semicircular canals
- Results in permanent hearing loss and chronic imbalance
🚨 SIGNS AND SYMPTOMS OF MÉNIÈRE’S DISEASE
Ménière’s disease is characterized by intermittent attacks involving both auditory and vestibular symptoms:
| Symptom | Description |
|---|---|
| 🌀 Vertigo | Sudden, spinning sensation lasting 20 minutes to several hours; may cause nausea, vomiting |
| 🔇 Fluctuating sensorineural hearing loss | Initially reversible; worsens over time, usually affects low frequencies first |
| 🔊 Tinnitus | Ringing, buzzing, or roaring sound in the affected ear |
| 💥 Aural fullness | Sensation of pressure, congestion, or heaviness in the ear |
| 🤢 Nausea & vomiting | Associated with severe vertigo |
| 🧍 Imbalance | Feeling of unsteadiness between attacks |
| 😓 Fatigue | Due to repeated episodes and post-attack weakness |
🔔 Symptoms are usually unilateral initially, but may become bilateral in 30–50% of cases over time.
🧪 DIAGNOSIS OF MÉNIÈRE’S DISEASE
Diagnosis is primarily clinical, supported by audiometric and vestibular tests.
🔷 A. History & Clinical Criteria (AAO-HNS Guidelines)
A definite diagnosis requires:
- ≥2 episodes of vertigo lasting ≥20 minutes
- Fluctuating hearing loss (documented audiometrically)
- Tinnitus or aural fullness
- Exclusion of other causes (e.g., vestibular migraine, tumors)
🔷 B. Audiometry (Pure Tone Audiogram – PTA)
- Shows sensorineural hearing loss, typically in low frequencies
- Hearing may fluctuate in early stages
- Progressive hearing deterioration in chronic disease
🔷 C. Vestibular Function Tests
| Test | Finding in Ménière’s Disease |
|---|---|
| 🔄 Caloric test | Reduced vestibular response on affected side |
| ⚖️ VNG (Videonystagmography) | Shows spontaneous or positional nystagmus |
| 🌀 Rotary chair test | Abnormal vestibular function response |
🔷 D. Electrocochleography (ECoG)
- Measures electrical potentials from cochlea
- Increased summating potential/action potential (SP/AP) ratio indicates endolymphatic hydrops
🔷 E. MRI of Internal Auditory Canal / Brain
- Done to rule out other conditions like:
- Acoustic neuroma (vestibular schwannoma)
- Multiple sclerosis
- Brainstem infarcts or tumors
💊🩺 MEDICAL MANAGEMENT OF MÉNIÈRE’S DISEASE
The goal of medical treatment is to:
✅ Control acute attacks of vertigo
✅ Reduce frequency and severity of future episodes
✅ Preserve hearing as much as possible
✅ Improve quality of life
🔷 1️⃣ MANAGEMENT DURING ACUTE ATTACK
During an episode of vertigo, the patient may require bed rest and medications to reduce nausea, vomiting, and dizziness.
✅ Symptomatic Medications:
| Drug Class | Examples | Purpose |
|---|---|---|
| 🚫 Antiemetics | Promethazine, Ondansetron | Control nausea and vomiting |
| 🌀 Vestibular suppressants | Meclizine, Betahistine, Diazepam | Reduce vertigo and dizziness |
| 💊 Antihistamines | Dimenhydrinate, Cinnarizine | Help reduce vestibular symptoms |
🛌 Bed rest is recommended during severe attacks.
🔷 2️⃣ LONG-TERM MANAGEMENT / PREVENTION
These medications help prevent future attacks and manage chronic symptoms.
✅ Preventive Medications:
| Drug Class | Examples | Purpose |
|---|---|---|
| 🔄 Diuretics | Hydrochlorothiazide, Acetazolamide | Reduce endolymphatic pressure (fluid) |
| 🌀 Vestibular modulator | Betahistine (commonly used) | Improves microcirculation in inner ear |
| 💊 Vasodilators | Nicergoline, Pentoxifylline | Improve blood flow to the cochlea |
| 🚫 Antihistamines | Cinnarizine, Meclizine | Long-term vertigo control |
| 🧠 Anti-anxiety agents | Diazepam, Lorazepam | Used when anxiety worsens symptoms |
| 💉 Corticosteroids (intra-tympanic) | Dexamethasone injection | Reduces inflammation in inner ear |
🔷 3️⃣ DIETARY AND LIFESTYLE CHANGES (Supportive Therapy)
These are essential parts of medical management:
- Low sodium diet (<1500 mg/day) → Helps reduce fluid retention in inner ear
- Avoid caffeine, alcohol, and tobacco
- Limit sugar and MSG intake
- Stay well hydrated
- Stress reduction techniques (yoga, meditation)
- Regular sleep and avoidance of fatigue
🔷 4️⃣ FOLLOW-UP AND MONITORING
- Audiometry: Repeated every few months to assess hearing changes
- Balance rehabilitation therapy (vestibular physiotherapy)
- Psychological support: For anxiety, depression due to chronic nature of illness
🏥🔧 SURGICAL MANAGEMENT OF MÉNIÈRE’S DISEASE
Surgery is considered when:
✅ Medical therapy fails
✅ Vertigo is severe, disabling, and frequent
✅ Hearing is severely affected or already lost
✅ The patient’s quality of life is impaired
🎯 The primary goal is to relieve vertigo — hearing preservation is attempted when possible.
🔷 TYPES OF SURGICAL MANAGEMENT
1️⃣ Endolymphatic Sac Decompression or Shunt Surgery
🧠 Purpose: To relieve pressure from endolymphatic hydrops
- A small part of the mastoid bone is removed to expose and decompress the endolymphatic sac
- A shunt tube may be inserted to allow drainage of excess fluid
✅ Advantages:
- Preserves hearing
- Reduces vertigo frequency in 70–90% of cases
- Minimally invasive
❌ Limitations:
- May not stop progression of hearing loss
- May need revision surgery
2️⃣ Vestibular Nerve Section (Vestibular Neurectomy)
🧠 Purpose: To cut off the nerve that carries balance signals from inner ear to brain
- Involves cutting the vestibular branch of the 8th cranial nerve while preserving the cochlear branch
- Done via retrosigmoid or middle cranial fossa approach
✅ Advantages:
- Excellent vertigo control (up to 95%)
- Hearing preservation possible
❌ Risks:
- Intracranial surgery
- Facial nerve damage
- CSF leak or infection
3️⃣ Labyrinthectomy
🧠 Purpose: Destruction or removal of the balance portion of the inner ear (labyrinth)
- Complete elimination of vestibular function on the affected side
- Indicated only when hearing is already severely impaired or lost
✅ Advantages:
- Very effective in vertigo control
- Simple and effective in advanced disease
❌ Disadvantages:
- Complete, irreversible hearing loss in that ear
- May require balance rehabilitation
4️⃣ Intratympanic Therapy (Minimally Invasive Options)
A. Intratympanic Gentamicin Injection
- Ototoxic antibiotic injected into middle ear
- Selectively destroys vestibular hair cells, reducing vertigo
- Given in controlled doses to minimize cochlear damage
✅ Benefits:
- Outpatient, minimally invasive
- Effective vertigo control
❌ Risks:
- May cause progressive hearing loss
B. Intratympanic Dexamethasone Injection
- Anti-inflammatory steroid
- Used when vertigo is not severe but persistent
- Hearing-sparing alternative
🧠 SUMMARY COMPARISON:
| Procedure | Vertigo Control | Hearing Preservation | Invasiveness |
|---|---|---|---|
| Endolymphatic sac surgery | Moderate-High | Usually preserved | Low |
| Vestibular nerve section | High | Usually preserved | High |
| Labyrinthectomy | Very high | Lost | Moderate |
| Intratympanic gentamicin | High | May be lost | Low |
| Intratympanic steroids | Moderate | Preserved | Very low |
👩⚕️🩺 NURSING MANAGEMENT OF MÉNIÈRE’S DISEASE
🎯 NURSING OBJECTIVES
✅ Relieve vertigo and associated discomfort
✅ Prevent injury during attacks (due to falls or imbalance)
✅ Promote comfort, rest, and hearing conservation
✅ Support patient emotionally
✅ Provide education for long-term lifestyle and dietary modifications
✅ Assist in pre- and post-operative care (if surgery is done)
🔷 I. NURSING ASSESSMENT
1️⃣ Subjective Data:
- Patient’s report of vertigo episodes (duration, frequency)
- History of hearing loss, tinnitus, and fullness in the ear
- Impact on daily life, emotional status, stress levels
2️⃣ Objective Data:
- Observation of gait imbalance or unsteadiness
- Monitoring vital signs during acute episodes
- Assess for nausea, vomiting, eye movement (nystagmus)
- Hearing ability using whisper test or audiometry records
🔷 II. NURSING DIAGNOSES
| Diagnosis | Related Factors |
|---|---|
| 🌀 Risk for injury | Due to vertigo and loss of balance |
| 😰 Anxiety | Unpredictable attacks, hearing loss |
| 🛌 Disturbed sleep pattern | Recurrent nighttime vertigo |
| 🔇 Impaired sensory perception (auditory) | Fluctuating hearing loss |
| 🍽️ Imbalanced nutrition (less than body needs) | Nausea, vomiting, dietary restrictions |
| 🧠 Knowledge deficit | About disease, management, and prevention |
🔷 III. NURSING INTERVENTIONS
✅ 1. During Acute Attack
- Place patient in quiet, dark room
- Position on bed with head slightly elevated
- Instruct to lie still; sudden movements worsen vertigo
- Maintain side rails up for fall prevention
- Administer prescribed medications:
- Antiemetics (e.g., promethazine)
- Vestibular suppressants (e.g., meclizine)
- Sedatives (e.g., diazepam)
✅ 2. Post-Attack Care
- Assist with ambulation; assess for postural instability
- Encourage fluids and small frequent meals to reduce nausea
- Monitor for hearing changes or neurological signs
✅ 3. Injury Prevention
- Educate on home safety:
- Use of grab bars, non-slip rugs, and adequate lighting
- Avoid walking in crowded or uneven areas alone
- Encourage use of walking aid if necessary
- Encourage rest between episodes
✅ 4. Psychosocial Support
- Provide emotional reassurance: chronic conditions often lead to depression
- Refer to support groups or vestibular rehabilitation therapists
- Help manage anxiety and fear of attacks
✅ 5. Health Education
- Avoid triggers: caffeine, alcohol, smoking, excess salt
- Teach low sodium diet (<1500 mg/day)
- Advise compliance with prescribed medications
- Stress the importance of regular ENT/audiology follow-ups
- Instruct to avoid:
- Sudden head movements
- Driving or operating machinery during or after episodes
✅ 6. Pre- and Post-Operative Care (if surgery is done)
- Pre-op:
- Explain procedure, reduce fear
- Ensure NPO status, consent, hygiene, baseline vitals
- Post-op:
- Monitor for bleeding, facial nerve function, hearing changes
- Maintain head elevation, provide wound care
- Assist with vestibular rehab if balance is affected
🔷 IV. EVALUATION
✔️ Patient reports relief from vertigo symptoms
✔️ No falls or injuries during hospitalization
✔️ Patient demonstrates understanding of medication and diet
✔️ Patient verbalizes reduced anxiety
✔️ Hearing is preserved or managed with assistive devices
🥗🍵 NUTRITIONAL CONSIDERATIONS IN MÉNIÈRE’S DISEASE
Diet plays an important role in controlling fluid balance, reducing endolymphatic pressure, and preventing vertigo attacks.
✅ Recommended Dietary Modifications
| Nutritional Element | Recommendations |
|---|---|
| 🧂 Sodium (Salt) | Low-sodium diet (<1500 mg/day) to reduce fluid retention in the inner ear |
| ☕ Caffeine | Avoid coffee, tea, cola → may trigger vertigo |
| 🍷 Alcohol | Avoid alcohol → affects inner ear circulation |
| 🚬 Nicotine | No smoking → vasoconstriction affects cochlear blood flow |
| 💦 Fluid intake | Maintain adequate hydration, but distribute fluids evenly throughout the day |
| 🍲 Balanced meals | Eat regular, small meals – may stabilize inner ear pressure |
| 🧃 Avoid MSG (Monosodium glutamate) | May exacerbate symptoms in sensitive individuals |
⚠️ COMPLICATIONS OF MÉNIÈRE’S DISEASE
Untreated or poorly managed Ménière’s disease may lead to:
🔹 Auditory Complications
- 🔇 Progressive sensorineural hearing loss (often permanent over time)
- 🔊 Tinnitus worsening
- ❌ Speech discrimination decline
🔹 Vestibular Complications
- 🌀 Frequent falls or balance-related injuries
- 🧠 Chronic dizziness and instability
- 🧍 Disabling vertigo episodes interfering with daily life
🔹 Psychological Complications
- 😞 Depression and anxiety due to unpredictability of attacks
- 🧠 Social withdrawal or isolation
- 😓 Fear of going out alone or driving
🔹 Post-Surgical Complications
- 🔇 Complete hearing loss (if labyrinthectomy is performed)
- 🧠 Facial nerve injury
- 💧 CSF leak, infection, or dizziness after vestibular neurectomy
🧠 KEY POINTS TO REMEMBER
✅ Ménière’s disease is a chronic inner ear disorder causing vertigo, tinnitus, fluctuating hearing loss, and aural fullness
✅ Caused by endolymphatic hydrops (fluid accumulation in the inner ear)
✅ Vertigo attacks can last minutes to hours and are often disabling
✅ Diagnosis is clinical, supported by audiometry and vestibular tests
✅ Medical treatment includes vestibular suppressants, diuretics, and diet control
✅ Surgery is considered when medical therapy fails (e.g., labyrinthectomy, neurectomy)
✅ Nurses play a key role in symptom relief, injury prevention, medication compliance, and education
✅ A low-sodium diet, stress control, and lifestyle changes are crucial in long-term management
✅ Regular follow-up with ENT and audiology services is essential
🌀👂 BENIGN PAROXYSMAL POSITIONAL VERTIGO (BPPV)
📘 DEFINITION
Benign Paroxysmal Positional Vertigo (BPPV) is a common vestibular disorder characterized by brief episodes of vertigo (a false sense of spinning) triggered by changes in head position. It is caused by displaced otoliths (calcium crystals) in the semicircular canals of the inner ear.
🔍 CAUSES / RISK FACTORS
| Cause / Risk Factor | Description |
|---|---|
| 🧠 Head injury or trauma | Displaces otoconia into semicircular canals |
| 👵 Aging | Degeneration of otolith membrane in elderly |
| 🧬 Idiopathic (unknown) | Most common cause (no identifiable factor) |
| 🧫 Inner ear infection (labyrinthitis) | Inflammatory damage to vestibular system |
| 🧠 Post-surgical | Especially after ear, dental, or head surgeries |
| 🧬 Migraine | Increases risk of vestibular sensitivity |
| ⚙️ Prolonged bed rest or inactivity | Disuse causes crystal dislodgement |
🔢 TYPES OF BPPV
BPPV is categorized based on the semicircular canal involved:
| Type | Description |
|---|---|
| 🔄 Posterior canal BPPV | Most common; vertigo when looking up/down |
| ➡️ Horizontal canal BPPV | Triggers vertigo when turning in bed |
| ⬆️ Anterior canal BPPV | Rare; vertigo when bending forward |
| 🔁 Unilateral or Bilateral | One or both ears affected |
🧬 PATHOPHYSIOLOGY
1️⃣ Otoliths (calcium carbonate crystals) normally rest in the utricle (a vestibular organ)
2️⃣ Due to trauma, aging, or other causes, otoliths dislodge and migrate into a semicircular canal (usually the posterior canal)
3️⃣ When the head moves in certain directions:
- The displaced otoliths stimulate hair cells abnormally in the canal
- This sends false signals to the brain about head movement
4️⃣ Brain receives conflicting messages from eyes, muscles, and ears
⮕ Results in vertigo, nystagmus, and imbalance
🚨 SIGNS AND SYMPTOMS
| Symptom | Description |
|---|---|
| 🌀 Brief episodes of vertigo | Spinning sensation lasting <1 minute |
| 🤕 Triggered by position change | Sitting up, lying down, rolling in bed |
| 😖 Nausea or vomiting | May accompany severe vertigo |
| 👁️ Nystagmus (eye flickering) | Observed during attacks |
| 🧍 Unsteadiness | Mild imbalance post-attack |
| ❌ No hearing loss or tinnitus | Unlike Ménière’s or labyrinthitis |
🧪 DIAGNOSIS
| Diagnostic Tool | Purpose |
|---|---|
| 🔎 Dix-Hallpike Maneuver | Provokes vertigo and nystagmus in posterior BPPV |
| 🧪 Roll Test (Supine Head Turn) | Used for horizontal canal BPPV |
| 🎧 Audiometry | Normal hearing confirms BPPV vs Ménière’s |
| 🧠 MRI/CT (if needed) | Rule out CNS pathology if atypical symptoms |
💊 MEDICAL MANAGEMENT
| Approach | Description |
|---|---|
| 🔄 Canalith repositioning maneuvers | Epley (posterior), Barbecue roll (horizontal) – gold standard |
| 💊 Vestibular suppressants | Meclizine, Betahistine – for short-term relief of symptoms |
| 💊 Antiemetics | Ondansetron, Promethazine for nausea/vomiting |
| 🛌 Activity modifications | Avoid triggers; sleep with head elevated initially |
❌ Long-term medication is not recommended — physical repositioning is curative.
🏥 SURGICAL MANAGEMENT
Only for intractable, recurrent, and disabling BPPV not responding to maneuvers.
| Surgery | Purpose |
|---|---|
| 🔧 Posterior Canal Plugging | Blocks affected canal from abnormal signals |
| 🔧 Vestibular nerve section | Reserved for very severe, disabling cases |
Surgery is rarely needed — <5% of patients
👩⚕️ NURSING MANAGEMENT
✅ During Vertigo Attacks:
- Assist patient to lie down safely
- Keep surroundings calm and quiet
- Provide cool air and emesis basin
- Reassure the patient – vertigo is short-lived
- Administer antiemetics and vestibular suppressants as prescribed
- Educate on head positioning to avoid symptom triggers
✅ Between Attacks:
- Teach and demonstrate canalith repositioning exercises
- Instruct on safe ambulation, use of assistive devices if needed
- Encourage hydration and rest
- Prepare patient for referral to ENT or vestibular physiotherapy
🥗 NUTRITIONAL CONSIDERATIONS
- No specific dietary restrictions for BPPV
However, general recommendations include:
| Dietary Guidance | Rationale |
|---|---|
| 💦 Stay well hydrated | Supports inner ear fluid balance |
| ☕ Limit caffeine/alcohol | Reduce central vestibular irritability |
| 🍋 Include Vitamin D (if deficient) | Linked to higher BPPV recurrence if low |
| 🍲 Eat small, regular meals | Prevent postural hypotension-related imbalance |
⚠️ COMPLICATIONS
| Complication | Description |
|---|---|
| 🤢 Falls or injury | From sudden vertigo or unsteadiness |
| 🔁 Recurrence | BPPV may recur in 30–50% within 1 year |
| 😟 Anxiety, fear of movement | May limit daily activity or cause phobia |
| ❌ Misdiagnosis | If confused with stroke, migraine, or tumor |
🧠 KEY POINTS TO REMEMBER
✅ BPPV is the most common cause of positional vertigo
✅ It is benign and self-limiting, but may recur
✅ Caused by displaced otoliths in semicircular canals
✅ Diagnosis is made clinically using Dix-Hallpike and Roll tests
✅ Repositioning maneuvers are the mainstay of treatment
✅ Surgery is rare, used only in refractory cases
✅ Nurses must ensure fall prevention, symptom management, and patient education
🧠👂 LABYRINTHITIS
📘 DEFINITION
Labyrinthitis is an inflammatory disorder of the inner ear (labyrinth) that affects both the cochlear (hearing) and vestibular (balance) systems. It results in sudden onset of vertigo, hearing loss, and tinnitus, often accompanied by nausea and unsteadiness.
It is usually caused by viral or bacterial infections, and may be associated with respiratory tract infections, ear infections, or systemic illness.
🔍 CAUSES OF LABYRINTHITIS
Labyrinthitis may be triggered by several infectious and non-infectious conditions:
🔹 1️⃣ Viral Infections (Most Common)
| Virus | Related Illness |
|---|---|
| Influenza virus | Flu |
| Herpes simplex virus | Cold sores |
| Varicella-zoster virus | Shingles |
| Mumps or measles virus | Pediatric viral illnesses |
| Cytomegalovirus | In immunocompromised patients |
| COVID-19 (SARS-CoV-2) | Recent reports of vestibular involvement |
🔹 2️⃣ Bacterial Infections
- Otitis media (middle ear infection) spreading to the inner ear
- Meningitis (via cerebrospinal fluid or hematogenous spread)
- Chronic suppurative otitis media (CSOM) with inner ear extension
- Mastoiditis leading to labyrinthine involvement
🔹 3️⃣ Autoimmune or Post-inflammatory Reaction
- Seen in autoimmune inner ear disease
- May follow upper respiratory tract infections as a post-viral inflammation
🔹 4️⃣ Other Causes
- Head trauma involving the temporal bone
- Ototoxic medications (e.g., aminoglycosides)
- Allergic responses
🔢 TYPES OF LABYRINTHITIS
Labyrinthitis can be classified based on etiology or extent of involvement:
🔷 A. Based on Cause
| Type | Description |
|---|---|
| 🦠 Viral Labyrinthitis | Most common; follows cold/flu; self-limiting |
| 🧫 Bacterial Labyrinthitis | More severe; often with purulent discharge; may cause permanent damage |
| 🤧 Autoimmune/Inflammatory | Due to immune system reaction; often recurrent |
🔷 B. Based on Involvement
| Type | Features |
|---|---|
| 🎧 Serous (Toxic) Labyrinthitis | Inflammation without direct infection; toxins or inflammatory mediators from nearby structures (e.g., otitis media) |
| 💉 Suppurative (Purulent) Labyrinthitis | Direct infection of inner ear; more destructive; often bacterial |
| 🔁 Localized vs. Generalized | May affect only part (e.g., vestibule) or entire labyrinth |
🧬 PATHOPHYSIOLOGY OF LABYRINTHITIS
🔁 Underlying Mechanism: Inflammation of the Inner Ear (Labyrinth)
1️⃣ The labyrinth is a part of the inner ear that includes:
- Cochlea (for hearing)
- Vestibular apparatus (for balance and spatial orientation)
2️⃣ In labyrinthitis, this structure becomes inflamed, typically due to:
- Viral infections (most common)
- Bacterial invasion from middle ear or meninges
- Toxic substances (e.g., inflammatory mediators, bacterial toxins)
3️⃣ Inflammation leads to:
- Dysfunction of vestibular receptors → Vertigo and imbalance
- Disruption of cochlear hair cells → Hearing loss and tinnitus
4️⃣ In severe cases, inflammation may:
- Damage nerve endings (vestibulocochlear nerve)
- Result in permanent sensorineural hearing loss
🚨 SIGNS AND SYMPTOMS OF LABYRINTHITIS
The presentation depends on whether the cause is viral (usually milder) or bacterial (more severe and rapid-onset):
🔷 General Symptoms:
| Symptom | Description |
|---|---|
| 🌀 Vertigo | Sudden onset, intense spinning lasting hours–days |
| 💫 Dizziness | Feeling of imbalance or unsteadiness |
| 🤢 Nausea & Vomiting | Common due to severe vestibular disturbance |
| 🔇 Hearing Loss | Usually unilateral, sensorineural in nature |
| 🔊 Tinnitus | Ringing, buzzing, or roaring sound in the ear |
| 🧍 Gait Disturbance | Wobbling or veering while walking |
| 👂 Ear fullness or pressure | Sometimes present |
| ❌ No pain in viral type | Unlike otitis media |
🔷 In Bacterial Labyrinthitis (Suppurative Type):
- Symptoms are more severe and rapidly progressive
- Often associated with ear discharge, fever, and facial weakness
🧪 DIAGNOSIS OF LABYRINTHITIS
Diagnosis is clinical, but supported by ENT, neurological, and audiological tests:
🔷 1. Clinical History & Physical Examination
- Sudden onset of vertigo + hearing loss
- Recent viral illness or ear infection
- No central nervous system signs (to rule out stroke)
🔷 2. Neurological and Vestibular Tests
| Test | Findings in Labyrinthitis |
|---|---|
| 🌀 Head thrust test | Positive – eyes fail to fixate when head is turned toward affected side |
| 👁️ Nystagmus | Horizontal or rotary, beating away from affected ear |
| 🧠 Romberg’s test | Unsteadiness when eyes are closed |
| 👣 Tandem walking | Impaired |
🔷 3. Audiometric Tests
- Pure Tone Audiometry (PTA):
- Shows sensorineural hearing loss (often unilateral)
- Speech discrimination may be reduced in affected ear
🔷 4. Imaging (If needed)
| Imaging | Purpose |
|---|---|
| 🧠 MRI with gadolinium | Rule out acoustic neuroma, infarcts, MS |
| 🩻 CT scan of temporal bone | Detects bony erosion or complications from otitis media/mastoiditis |
🔷 5. Lab Tests (in bacterial suspicion)
- CBC: Elevated WBC count
- CRP/ESR: Elevated
- Ear swab for culture and sensitivity (if discharge present)
💊🩺 MEDICAL MANAGEMENT OF LABYRINTHITIS
The goal of medical treatment is to:
✅ Control infection (if bacterial)
✅ Relieve vertigo, nausea, and other distressing symptoms
✅ Prevent complications such as hearing loss or spread to CNS
✅ Support full recovery of vestibular and auditory function
🔷 1️⃣ General Symptomatic Management
| Drug Category | Examples | Purpose |
|---|---|---|
| 🌀 Vestibular suppressants | Meclizine, Cinnarizine, Diazepam | Reduce vertigo and balance symptoms |
| 🤢 Antiemetics | Promethazine, Ondansetron | Control nausea and vomiting |
| 💊 Antihistamines | Dimenhydrinate | Used in viral cases for mild vertigo |
| 💊 Analgesics / Antipyretics | Paracetamol, Ibuprofen | Pain and fever management |
🔷 2️⃣ Treatment Based on Etiology
✅ Viral Labyrinthitis (Most Common)
- Supportive treatment with rest, hydration, vestibular suppressants, and antiemetics
- Corticosteroids (Prednisolone) may be used to reduce inflammation and preserve hearing (early phase)
- Recovery is usually complete within 1–3 weeks
✅ Bacterial Labyrinthitis (Suppurative / Severe)
- Requires hospitalization in most cases
- Intravenous broad-spectrum antibiotics (e.g., Ceftriaxone, Ampicillin, Vancomycin)
- If middle ear or mastoid infection is source → address primary infection
- Corticosteroids may be added in severe inflammation
- May require myringotomy for drainage if middle ear effusion is present
🔷 3️⃣ Vestibular Rehabilitation Therapy (VRT)
- Indicated after acute symptoms resolve to aid central compensation
- Includes balance exercises, gaze stabilization, and habituation therapy
- Helps reduce long-term dizziness and improves function
🏥🔧 SURGICAL MANAGEMENT OF LABYRINTHITIS
Surgery is rarely required and reserved for complications or chronic progression.
🔹 Indications for Surgery:
- Persistent or progressive bacterial infection not responding to medical therapy
- Intracranial complications (e.g., meningitis, brain abscess)
- Cholesteatoma or mastoiditis as source of infection
- Perilymphatic fistula due to labyrinth rupture
🔹 Surgical Procedures
| Procedure | Purpose |
|---|---|
| 🛠️ Myringotomy with tube | Drain middle ear fluid; relieve pressure |
| 🛠️ Mastoidectomy | Removes infected mastoid air cells (CSOM cases) |
| 🛠️ Labyrinthectomy | Destruction of diseased labyrinth in non-hearing ear (last resort) |
| 🛠️ Drainage of abscess | If CNS infection or petrositis develops |
⚠️ Surgical options are used only when life-threatening or ear-threatening complications occur.
👩⚕️🩺 NURSING MANAGEMENT OF LABYRINTHITIS
🎯 OBJECTIVES OF NURSING CARE
✅ Relieve vertigo and associated discomfort
✅ Prevent injury and falls
✅ Promote rest and healing
✅ Administer medications safely and monitor effectiveness
✅ Provide psychological and emotional support
✅ Educate the patient about treatment, precautions, and prevention of recurrence
🔷 I. NURSING ASSESSMENT
1️⃣ Subjective Data:
- Complaints of sudden vertigo, nausea, hearing loss
- History of recent upper respiratory tract infection or ear infection
- Presence of ear fullness, tinnitus, or visual disturbances
2️⃣ Objective Data:
- Observe for gait instability, nystagmus, or difficulty in balance
- Monitor vital signs, especially if febrile (suggests bacterial cause)
- Evaluate fluid intake/output if vomiting is severe
- Assess hearing status and ear discharge if present
🔷 II. NURSING DIAGNOSES
| Diagnosis | Related to |
|---|---|
| 🌀 Risk for injury | Due to vertigo and unsteady gait |
| 🤢 Imbalanced nutrition (less than body needs) | Due to vomiting and nausea |
| 😷 Acute discomfort | Inner ear inflammation, vertigo, and headache |
| 🔇 Impaired sensory perception (hearing) | Due to inner ear inflammation |
| ❌ Deficient knowledge | About disease, medications, and prevention |
| 😨 Anxiety | Uncertainty about symptoms and recurrence |
🔷 III. NURSING INTERVENTIONS
✅ 1. Symptom Relief and Comfort
- Place the patient in a quiet, darkened room during acute vertigo
- Position head elevated and still to reduce stimulation
- Encourage bed rest during acute phase
- Limit environmental stimuli (light, noise)
- Avoid sudden movements or quick head turns
✅ 2. Medication Administration
- Administer:
- Vestibular suppressants (e.g., meclizine, diazepam)
- Antiemetics (e.g., promethazine, ondansetron)
- Antibiotics (if bacterial labyrinthitis suspected)
- Corticosteroids (as ordered)
- Monitor drug effectiveness and side effects
- Maintain hydration, especially in patients with vomiting
✅ 3. Fall and Injury Prevention
- Use side rails, call bell, and bedside commode if needed
- Assist with ambulation during acute or post-attack phase
- Advise patient to avoid walking alone until dizziness subsides
- Encourage slow position changes
✅ 4. Psychosocial Support
- Reassure patient about the temporary nature of symptoms (in viral cases)
- Educate about realistic recovery expectations
- Provide support in case of hearing concerns or anxiety
✅ 5. Health Education
- Teach the patient:
- Importance of completing full course of medications
- To report signs of worsening (severe headache, high fever, confusion – may suggest CNS spread)
- Use of home safety precautions (non-slip rugs, grab bars, avoid driving)
- Need for follow-up audiometry or ENT consultation
🔷 IV. EVALUATION
✔️ Patient reports reduced vertigo and nausea
✔️ Maintains hydration and nutrition despite symptoms
✔️ No falls or injuries during hospitalization
✔️ Verbalizes understanding of disease and management
✔️ Demonstrates improved gait and balance during ambulation
🥗💧 NUTRITIONAL CONSIDERATIONS IN LABYRINTHITIS
Although Labyrinthitis itself is not a nutritional disorder, proper nutrition plays a supportive role in symptom control, hydration, and healing — especially during acute episodes.
✅ Key Dietary Guidelines:
| Recommendation | Rationale |
|---|---|
| 💧 Adequate hydration | Prevents dehydration caused by vomiting |
| 🍲 Small, frequent meals | Helps reduce nausea and maintain energy |
| 🧂 Low-sodium diet (in recurrent or Ménière’s-like cases) | Helps regulate inner ear fluid balance |
| ☕ Avoid caffeine and alcohol | May worsen dizziness and irritability |
| 🥗 Vitamin-rich foods (A, C, B12) | Support nerve health and immune system |
| 🧃 Ginger tea or mint | Natural antiemetic effects, soothes nausea |
⚠️ COMPLICATIONS OF LABYRINTHITIS
If not diagnosed or managed early, Labyrinthitis may lead to several ear and neurological complications:
🔹 Ear-Related Complications
| Complication | Description |
|---|---|
| 🔇 Permanent sensorineural hearing loss | Especially in bacterial labyrinthitis |
| 🧠 Vestibular hypofunction | Chronic imbalance or motion intolerance |
| 🔁 Recurrent vertigo or dizziness | May become disabling if central compensation fails |
🔹 Neurological Complications (in bacterial or untreated cases)
| Complication | Description |
|---|---|
| 🧠 Meningitis | Infection may spread to meninges |
| 🧠 Brain abscess | Rare but severe consequence of suppurative spread |
| 💀 Petrositis or mastoiditis | Infection spreads to adjacent skull bones |
| 🧠 Cranial nerve palsies | Especially facial nerve if inflammation spreads |
🧠 KEY POINTS TO REMEMBER
✅ Labyrinthitis is inflammation of the inner ear (labyrinth)
✅ It affects both hearing and balance, unlike BPPV which only affects balance
✅ Viral labyrinthitis is more common and usually self-limiting
✅ Bacterial labyrinthitis is more dangerous and may lead to hearing loss or CNS infection
✅ Main symptoms include vertigo, nausea, hearing loss, tinnitus, and gait disturbance
✅ Diagnosis is clinical, confirmed by vestibular tests and audiometry
✅ Vestibular suppressants, antiemetics, and antibiotics (in bacterial cases) are key treatments
✅ Vestibular rehab and patient education are essential for recovery
✅ Nurses play a vital role in symptom management, fall prevention, and patient counseling
✅ Early treatment reduces risk of complications like permanent deafness or meningitis.
👂💊🎗️ OTOTOXICITY TUMORS
📘 DEFINITION
Ototoxicity tumors refer to either:
🔹 Tumors that cause ototoxic effects (hearing loss, balance disturbances) by compressing auditory or vestibular structures
🔹 Or, tumors treated with ototoxic drugs (e.g., cisplatin), which result in inner ear damage
They involve both direct mechanical disruption (tumor compression) and indirect chemical damage (via ototoxic chemotherapy).
🧪 CAUSES / RISK FACTORS
🔷 1. Primary Tumors Causing Ototoxicity-like Symptoms
- Vestibular Schwannoma (Acoustic Neuroma)
- Meningioma (cerebellopontine angle)
- Cholesteatoma (middle ear tumor)
- Glomus tumors (paragangliomas)
- Brainstem tumors affecting auditory pathways
🔷 2. Cancers Treated with Ototoxic Drugs
| Tumor Type | Ototoxic Drug Used |
|---|---|
| Testicular cancer | Cisplatin |
| Ovarian cancer | Carboplatin |
| Head & neck cancers | Cisplatin, radiation |
| Brain tumors (gliomas, medulloblastoma) | Cisplatin or methotrexate |
| Lung cancer | Platinum-based chemotherapy |
🔢 TYPES OF OTOTOXICITY TUMORS
🔹 Based on Tumor Origin
| Type | Description |
|---|---|
| 🧠 Vestibular Schwannoma | Benign tumor of CN VIII, causes gradual hearing loss |
| 🧠 Meningioma | Compresses CN VIII at the cerebellopontine angle |
| 🧠 Cholesteatoma | Middle ear mass eroding ossicles; can cause secondary inner ear damage |
| 💉 Cisplatin-induced ototoxicity | Seen in solid tumors treated with chemotherapy |
🧬 PATHOPHYSIOLOGY
1️⃣ Tumor Mass Effect:
Tumors like vestibular schwannoma or meningioma compress CN VIII or cochlear nuclei, leading to impaired neural transmission of sound or balance signals.
2️⃣ Chemical-Induced Ototoxicity:
Cisplatin and similar drugs damage cochlear hair cells, stria vascularis, and spiral ganglion neurons via free radical formation and apoptosis, especially in the basal turn of the cochlea.
3️⃣ Combined Mechanism:
In some cancer patients, tumor pressure + chemotherapy both contribute to hearing loss, tinnitus, vertigo.
🚨 SIGN AND SYMPTOMS
| Symptom | Description |
|---|---|
| 🔇 Sensorineural hearing loss | Usually progressive, may be sudden in tumor-related cases |
| 🔊 Tinnitus | Ringing, buzzing, or roaring in the ears |
| 🌀 Vertigo / dizziness | Due to vestibular nerve involvement |
| 🧍 Gait imbalance | Seen with vestibular dysfunction |
| ❌ Facial numbness or weakness | If adjacent cranial nerves (CN V, VII) are compressed |
| 🧠 Headache or visual changes | With large tumors or raised intracranial pressure |
🧪 DIAGNOSIS
🔷 Clinical History & Otologic Exam
- Progressive unilateral hearing loss
- Tinnitus, vertigo, chemotherapy history
- Neurological signs (facial weakness, nystagmus)
🔷 Audiologic Tests
- Pure Tone Audiometry (PTA) – Shows sensorineural loss
- Speech discrimination tests – Often disproportionately reduced in tumors
- Auditory Brainstem Response (ABR) – May show prolonged wave latencies
🔷 Imaging
- MRI with gadolinium: Gold standard for tumor visualization
- CT scan: Helpful in middle ear tumors or bony erosion (e.g., cholesteatoma)
🔷 Blood & Lab Tests
- Kidney function tests – If on ototoxic chemotherapy
- Tumor markers – In systemic malignancy
💊 MEDICAL MANAGEMENT
| Approach | Description |
|---|---|
| 💉 Steroids (short-term) | Reduce inflammation and edema around nerve |
| 💊 Vestibular suppressants | Meclizine or diazepam for vertigo management |
| 💊 Antioxidants (NAC, Vitamin E) | Experimental use to reduce cisplatin ototoxicity |
| 🔄 Chemotherapy dose adjustment | To minimize cochlear damage |
| 💊 Diuretics (with caution) | May enhance cisplatin toxicity if used with it |
🏥 SURGICAL MANAGEMENT
| Surgery Type | Indication |
|---|---|
| 🧠 Microsurgical tumor removal | Vestibular schwannoma, meningioma |
| 👂 Tympanomastoidectomy | Cholesteatoma or glomus tumor |
| 🧠 Cochlear nerve decompression | Rarely, to relieve pressure |
| 🎧 Cochlear implant | In profound hearing loss after tumor removal or chemo |
| 🔬 Intraoperative monitoring | Facial and auditory nerve monitoring |
👩⚕️ NURSING MANAGEMENT
✅ Preoperative / Chemotherapy Phase:
- Baseline audiometry and vestibular assessment
- Monitor for early symptoms of ototoxicity
- Educate about reporting tinnitus, dizziness, or hearing changes
✅ Postoperative / Post-Chemotherapy Care:
- Monitor wound site, facial nerve function, balance
- Encourage safe ambulation (fall prevention)
- Provide emotional support if hearing loss occurs
- Educate about hearing aids, cochlear implants, or assistive devices
- Coordinate with speech/audiology rehabilitation
🥗 NUTRITIONAL CONSIDERATIONS
| Nutritional Focus | Reason |
|---|---|
| 🧃 Hydration maintenance | Supports renal clearance of ototoxic drugs |
| 🍊 Vitamin-rich diet (A, C, E) | Antioxidants may help reduce ototoxicity risk |
| 🥩 Protein-rich foods | Aids in tissue repair post-surgery |
| 🚫 Limit salt, caffeine | May worsen inner ear fluid imbalance or tinnitus |
⚠️ COMPLICATIONS
| Complication | Description |
|---|---|
| 🔇 Permanent hearing loss | Due to nerve destruction or drug toxicity |
| 🧠 Facial nerve palsy | Post-surgical or tumor invasion |
| 🧠 Cerebellar symptoms | Large tumors may affect balance and coordination |
| 🧠 CSF leak or infection | Postoperative risks |
| 😞 Depression, social withdrawal | Due to sensory disability |
🧠 KEY POINTS TO REMEMBER
✅ Ototoxicity tumors involve either tumor-induced nerve compression or chemotherapy-induced cochlear damage
✅ Most commonly associated tumors: vestibular schwannoma, meningioma, and cholesteatoma
✅ Cisplatin is a major ototoxic drug used in solid tumor treatment
✅ Early signs include tinnitus, vertigo, unilateral hearing loss
✅ Diagnosis relies on audiometry, ABR, and MRI
✅ Treatment includes tumor resection, dose modification, cochlear implant
✅ Nurses play a key role in early detection, patient safety, emotional support, and rehabilitation coordination.
🌸👃 RHINITIS
📘 DEFINITION
Rhinitis is defined as the inflammation or irritation of the nasal mucosa, characterized by sneezing, nasal congestion, rhinorrhea (runny nose), itching, and postnasal drip. It can be acute or chronic, and either infectious, allergic, or non-allergic in origin.
🔍 CAUSES OF RHINITIS
Rhinitis can result from various environmental, infectious, allergic, or physiological factors:
🔹 Infectious Causes
- Viral infections (most common) – e.g., rhinovirus, coronavirus, influenza
- Bacterial infections – may follow viral illness
- Fungal infections (in immunocompromised individuals)
🔹 Allergic Causes
- Seasonal allergens: Pollen, grass, trees (hay fever)
- Perennial allergens: Dust mites, animal dander, mold
- Occupational allergens: Latex, chemical fumes
🔹 Non-Allergic / Irritant-Induced Causes
- Cold air, smoke, perfumes, strong odors
- Hormonal changes (e.g., pregnancy rhinitis)
- Certain medications (e.g., ACE inhibitors, aspirin)
- Food-induced (gustatory rhinitis)
🔹 Other Causes
- Structural abnormalities: Deviated nasal septum, polyps
- Chronic sinusitis
- Atrophic changes in elderly (atrophic rhinitis)
🔢 TYPES OF RHINITIS
1️⃣ Allergic Rhinitis
🔸 Immune-mediated response to allergens
🔸 Divided into seasonal and perennial
2️⃣ Infectious Rhinitis (Acute Viral Rhinitis / Common Cold)
🔸 Short-term, contagious, caused by viruses
🔸 Self-limiting in 7–10 days
3️⃣ Non-Allergic Rhinitis (NAR)
🔸 No IgE involvement
🔸 Triggered by smoke, weather, food, or medication
4️⃣ Occupational Rhinitis
🔸 Exposure to workplace allergens or irritants
5️⃣ Hormonal Rhinitis
🔸 Seen in pregnancy, menstruation, hypothyroidism
6️⃣ Drug-Induced Rhinitis (Rhinitis Medicamentosa)
🔸 Rebound nasal congestion due to overuse of nasal decongestants (e.g., oxymetazoline)
7️⃣ Atrophic Rhinitis
🔸 Chronic condition seen in the elderly with mucosal atrophy and crusting
🧬 PATHOPHYSIOLOGY OF RHINITIS
A. Allergic Rhinitis Pathophysiology
1️⃣ Allergen exposure → activates immune system
2️⃣ IgE antibodies are produced against the allergen
3️⃣ Re-exposure → allergen binds to IgE on mast cells
4️⃣ Mast cells release histamine, leukotrienes, prostaglandins
5️⃣ Causes:
- Vasodilation → nasal congestion
- Increased glandular secretion → runny nose
- Nerve stimulation → sneezing and itching
B. Infectious Rhinitis Pathophysiology
1️⃣ Viral entry via inhalation or hand contact
2️⃣ Virus infects nasal epithelial cells
3️⃣ Triggers inflammatory response with cytokines
4️⃣ Results in:
- Swelling of mucosa → congestion
- Mucous gland stimulation → rhinorrhea
- Possible secondary bacterial infection
🚨 SIGNS AND SYMPTOMS
| Symptom | Description |
|---|---|
| 🤧 Sneezing | Common in allergic and viral types |
| 💧 Rhinorrhea | Watery or mucoid nasal discharge |
| 🌫️ Nasal congestion | Due to mucosal swelling |
| 👃 Nasal itching | Prominent in allergic rhinitis |
| 🧠 Headache or facial pressure | Due to sinus congestion |
| 👁️ Watery eyes | Often seen in allergic rhinitis |
| 😮 Postnasal drip | Mucus draining into the throat |
| 😷 Cough or throat irritation | Especially with chronic or postnasal rhinitis |
| 🌡️ Low-grade fever | In viral/bacterial rhinitis |
🧪 DIAGNOSIS OF RHINITIS
1️⃣ History and Physical Examination
- Type, duration, and pattern of symptoms
- Family or personal history of allergies, asthma, eczema
- Nasal mucosa examination (pale in allergic, red/swollen in infectious)
2️⃣ Allergy Testing (if allergic rhinitis is suspected)
- Skin prick test
- Serum IgE testing (RAST)
3️⃣ Nasal Smear
- Eosinophils → allergic rhinitis
- Neutrophils → infectious rhinitis
4️⃣ Imaging (if complications or chronic rhinitis suspected)
- X-ray or CT scan of paranasal sinuses
- Rule out polyps, sinusitis, or structural anomalies
💊🩺 MEDICAL MANAGEMENT OF RHINITIS
Medical treatment depends on the type of rhinitis (allergic, infectious, non-allergic, etc.) and focuses on relieving symptoms, reducing inflammation, and preventing recurrence.
🔷 1️⃣ ALLERGIC RHINITIS
| Medication Type | Examples | Purpose |
|---|---|---|
| 💊 Antihistamines (oral/nasal) | Cetirizine, Loratadine, Fexofenadine, Azelastine | Reduce sneezing, itching, runny nose |
| 💊 Nasal corticosteroids | Fluticasone, Budesonide, Mometasone | Reduce mucosal inflammation & congestion |
| 💊 Decongestants (short-term) | Oxymetazoline (nasal), Pseudoephedrine | Relieve nasal stuffiness (max 5–7 days) |
| 💊 Leukotriene receptor antagonists | Montelukast | Adjunct therapy, especially with asthma |
| 💊 Mast cell stabilizers | Cromolyn sodium | Preventative (use before allergen exposure) |
| 💉 Allergen immunotherapy | Allergy shots (SCIT) or sublingual tablets | Desensitize immune response (long-term) |
🔷 2️⃣ INFECTIOUS RHINITIS (ACUTE VIRAL RHINITIS – COMMON COLD)
| Treatment | Purpose |
|---|---|
| 💊 Antipyretics & analgesics | Paracetamol, Ibuprofen – for fever, headache |
| 💧 Nasal saline irrigation | Clears mucus, soothes mucosa |
| 💊 Antihistamines (1st gen) | Chlorpheniramine – relieve sneezing, rhinorrhea |
| 💊 Decongestants | Oral/nasal for short-term relief |
| ❌ Antibiotics | Not indicated for viral infections |
🔷 3️⃣ CHRONIC / NON-ALLERGIC RHINITIS
| Medication | Purpose |
|---|---|
| 💊 Intranasal anticholinergics | Ipratropium bromide – reduces rhinorrhea |
| 💊 Nasal corticosteroids | Reduce inflammation and edema |
| ⚠️ Avoid irritants | E.g., perfumes, smoke, cold air |
⚠️ Note on Rhinitis Medicamentosa (rebound congestion):
- Caused by overuse of topical decongestants (>5–7 days)
- Treatment: Stop the spray, start nasal steroids and saline rinse
🏥🔧 SURGICAL MANAGEMENT OF RHINITIS
Surgery is considered for chronic or structural causes of rhinitis not responding to medical therapy, or when complications (like nasal obstruction, polyps) arise.
✅ Indications for Surgery:
- Structural abnormalities (e.g., deviated nasal septum)
- Nasal polyps causing obstruction
- Chronic hypertrophic turbinates
- Chronic sinusitis unresponsive to medication
- Refractory allergic rhinitis affecting quality of life
🔷 Surgical Procedures:
| Procedure | Purpose/Indication |
|---|---|
| 🔧 Septoplasty | Correction of deviated nasal septum |
| 🔧 Turbinate reduction | Radiofrequency or partial resection to relieve obstruction |
| 🔧 Polypectomy | Removal of nasal polyps |
| 🔧 Functional Endoscopic Sinus Surgery (FESS) | Improves sinus drainage in chronic sinusitis or recurrent infections |
| 🔧 Vidian neurectomy | Rarely used; severs parasympathetic nerve to reduce nasal secretion |
| 🔧 Cryotherapy / Laser therapy | Used for vasomotor or non-allergic rhinitis when conservative measures fail |
🧑⚕️ Postoperative Considerations:
- Nasal packing or splints may be placed temporarily
- Avoid blowing nose or sneezing forcefully
- Saline rinses encouraged after initial healing
- Follow-up for nasal endoscopy and recovery checks
👩⚕️🩺 NURSING MANAGEMENT OF RHINITIS
🎯 NURSING OBJECTIVES
✅ Relieve discomfort caused by nasal congestion, discharge, and sneezing
✅ Prevent secondary infections or complications (e.g., sinusitis, ear infection)
✅ Educate the patient on self-care and allergy management
✅ Monitor response to medications and ensure proper administration
✅ Support recovery and improve quality of life
🔷 I. NURSING ASSESSMENT
| Category | Details |
|---|---|
| 📋 Subjective Data | Complaints of sneezing, congestion, nasal discharge, itching, headache |
| 👁️ Objective Data | Observe for watery eyes, swollen nasal mucosa, nasal voice, mouth breathing |
| 🧾 History Taking | Allergies, recent infections, exposure to irritants, seasonal symptoms, drug use (decongestants) |
🔷 II. NURSING DIAGNOSES
| Nursing Diagnosis | Related To |
|---|---|
| 🤧 Ineffective airway clearance | Nasal congestion and mucosal edema |
| 🌡️ Acute discomfort | Nasal inflammation, pressure, itching |
| 🔍 Deficient knowledge | About triggers, medications, and prevention |
| 😞 Disturbed sleep pattern | Nocturnal nasal congestion or coughing |
| 🤒 Risk for infection | Bacterial superinfection of nasal sinuses |
🔷 III. NURSING INTERVENTIONS
✅ 1. Relieve Nasal Congestion and Discomfort
- Encourage nasal saline irrigation (normal saline sprays or neti pot)
- Apply warm compress to sinuses if facial pressure is present
- Provide humidified air or advise use of a humidifier
- Encourage adequate hydration to thin secretions
- Instruct on safe use of decongestants (limit topical use to ≤5 days)
✅ 2. Administer and Monitor Medications
- Administer as prescribed:
- Antihistamines (oral or nasal)
- Nasal corticosteroids (e.g., fluticasone)
- Decongestants (pseudoephedrine, oxymetazoline)
- Educate about:
- Correct nasal spray technique
- Potential side effects (dryness, rebound congestion)
- Avoiding overuse of decongestants (rhinitis medicamentosa)
✅ 3. Environmental Control and Allergen Avoidance
- Identify and eliminate exposure to:
- Pollen, dust mites, pet dander, mold, smoke
- Educate on:
- Using air purifiers, dust-proof covers, frequent cleaning
- Keeping windows closed during high pollen seasons
- Wearing masks in dusty or polluted environments
✅ 4. Promote Rest and Comfort
- Advise patient to sleep with head elevated to reduce postnasal drip
- Provide tissues and encourage gentle nose blowing
- Use non-sedating antihistamines in daytime to avoid drowsiness
✅ 5. Patient Education
- Teach patient about:
- Chronic vs acute rhinitis
- Long-term control strategies (especially in allergic rhinitis)
- When to seek medical help (e.g., fever, sinus pain, ear pressure)
- Encourage follow-up for allergy testing or ENT referral if needed
🔷 IV. EVALUATION
✔️ Patient experiences relief from congestion, sneezing, and itching
✔️ Maintains a clear airway and normal breathing pattern
✔️ Identifies allergens or irritants and avoids triggers
✔️ Demonstrates correct use of nasal sprays and other medications
✔️ Maintains good sleep hygiene and fluid intake.
🥗💧 NUTRITIONAL CONSIDERATIONS IN RHINITIS
Though not a nutritional disorder, dietary choices can help boost immunity, reduce inflammation, and support recovery — especially in allergic or chronic rhinitis.
✅ Recommended Nutritional Guidelines:
| Dietary Element | Purpose / Benefit |
|---|---|
| 💧 Hydration (fluids, warm soups) | Thins mucus secretions, eases nasal congestion |
| 🍊 Vitamin C-rich foods | Boosts immune defense and reduces histamine release |
| 🧄 Anti-inflammatory foods | Garlic, turmeric, ginger – natural antihistamines |
| 🥬 High-fiber fruits & vegetables | Support immunity and mucosal health |
| 🐟 Omega-3 fatty acids | Found in fish, flaxseeds – help reduce allergic inflammation |
| 🚫 Avoid allergenic foods | Such as nuts, dairy, eggs if patient has known food sensitivities |
| 🚫 Avoid cold or sugary drinks | May increase mucus production or throat irritation |
⚠️ COMPLICATIONS OF RHINITIS
If left untreated or poorly managed, rhinitis — especially chronic or allergic types — can lead to multiple complications:
🔹 Respiratory & ENT Complications
| Complication | Description |
|---|---|
| 🤧 Chronic sinusitis | Blocked sinuses from long-term mucosal inflammation |
| 👂 Otitis media (middle ear infection) | Due to Eustachian tube blockage, especially in children |
| 🫁 Bronchial asthma exacerbation | Especially in patients with allergic rhinitis |
| 👃 Nasal polyps | From chronic inflammation in allergic rhinitis |
| 😴 Obstructive sleep disturbances | Snoring, mouth breathing, sleep apnea from nasal blockage |
🔹 Medication-Related Complications
- Rhinitis medicamentosa from prolonged decongestant use
- Steroid-induced mucosal dryness with long-term nasal corticosteroids
🧠 KEY POINTS TO REMEMBER
✅ Rhinitis is inflammation of the nasal mucosa, and may be allergic, infectious, or non-allergic
✅ Main symptoms: Sneezing, nasal congestion, rhinorrhea, and itching
✅ Allergic rhinitis involves an IgE-mediated immune response
✅ Diagnosis includes history, nasal exam, allergy tests, and imaging if needed
✅ Management involves:
- Antihistamines, nasal steroids, decongestants, and allergen avoidance
- Saline rinses and supportive care in infectious rhinitis
✅ Surgical correction may be required for structural or chronic cases
✅ Nurses play a vital role in symptom control, education, and monitoring
✅ Encourage hydration, immunity-boosting nutrition, and environmental hygiene
👃🦠 SINUSITIS
(Also called: Rhinosinusitis)
📘 DEFINITION
Sinusitis is the inflammation or infection of one or more of the paranasal sinuses, resulting from obstruction of normal sinus drainage pathways. It may be acute, subacute, or chronic, and can be caused by infections, allergens, or anatomical abnormalities.
The paranasal sinuses are air-filled cavities in the skull:
- Maxillary sinuses (cheek)
- Frontal sinuses (forehead)
- Ethmoid sinuses (between the eyes)
- Sphenoid sinuses (deep behind the nose)
🔍 CAUSES OF SINUSITIS
| Category | Common Causes |
|---|---|
| 🦠 Infectious | Viral (most common), Bacterial (e.g., Streptococcus pneumoniae, H. influenzae), Fungal (in immunocompromised) |
| 🤧 Allergic | Allergic rhinitis, hay fever, environmental allergens |
| 🧱 Structural | Deviated nasal septum, nasal polyps, enlarged turbinates |
| 🧪 Chemical/Irritants | Smoke, dust, pollution, strong odors |
| 👃 Foreign bodies | Especially in children causing unilateral sinus infection |
| 🦷 Dental origin | Infected upper teeth roots penetrating maxillary sinuses |
| 😷 Others | Cystic fibrosis, immunodeficiency, frequent URTIs |
🔢 TYPES OF SINUSITIS
🔷 A. Based on Duration
| Type | Duration |
|---|---|
| ⏳ Acute sinusitis | < 4 weeks (usually viral) |
| ⏳ Subacute sinusitis | 4 to 12 weeks |
| ⏳ Chronic sinusitis | > 12 weeks, persistent inflammation |
| 🔁 Recurrent acute sinusitis | ≥ 4 episodes/year with symptom-free intervals |
🔷 B. Based on Affected Sinus
| Type | Involved Sinus |
|---|---|
| 👃 Maxillary sinusitis | Pain in cheeks, upper teeth, jaw |
| 🧠 Frontal sinusitis | Forehead pain, worse in the morning |
| 👀 Ethmoid sinusitis | Pain between eyes, eyelid swelling |
| 🌀 Sphenoid sinusitis | Deep head pain, behind eyes or vertex |
| 🔁 Pansinusitis | Inflammation of all sinuses |
🧬 PATHOPHYSIOLOGY OF SINUSITIS
1️⃣ Trigger (infection, allergen, irritant) leads to:
➡️ Mucosal inflammation of the sinus lining
2️⃣ Inflammation causes:
➡️ Edema and blockage of the sinus ostia (drainage openings)
3️⃣ Mucus and secretions accumulate in the sinus cavities →
➡️ Stagnation provides a fertile environment for bacterial or fungal overgrowth
4️⃣ Trapped secretions → increased pressure, pain, and possible complications (e.g., abscess, orbital cellulitis)
🚨 SIGNS AND SYMPTOMS OF SINUSITIS
| Symptom | Description |
|---|---|
| 🤧 Nasal congestion | Blocked nasal passages, mouth breathing |
| 💧 Thick nasal discharge | Yellow-green, purulent, often unilateral |
| 🤕 Facial pain or pressure | Over cheeks, forehead, eyes, increases on bending |
| 🌡️ Fever | Often in bacterial sinusitis |
| 👃 Loss/reduction of smell | Due to mucosal swelling |
| 😷 Postnasal drip | Mucus drainage into throat |
| 😴 Fatigue / malaise | General discomfort |
| 🧠 Headache | Especially in frontal or sphenoid sinusitis |
| 🦷 Toothache (maxillary) | Referred pain from maxillary sinus |
| 👁️ Swelling around eyes | In severe or ethmoid sinusitis |
🧪 DIAGNOSIS OF SINUSITIS
🔷 1️⃣ Clinical Assessment
- History of duration, pattern, severity of symptoms
- Facial tenderness on palpation
- Transillumination of sinuses (dimmed light in affected sinus)
🔷 2️⃣ Nasal Endoscopy
- Allows direct visualization of:
- Mucosal edema
- Purulent drainage
- Polyp formation or structural obstruction
🔷 3️⃣ Imaging
| Imaging Modality | Purpose |
|---|---|
| 🩻 X-ray (Water’s view) | May show opacity in maxillary sinuses |
| 🧠 CT scan (gold standard) | Best for evaluating extent, chronicity, or planning surgery |
| 🧠 MRI | Used to assess soft tissue spread or complications (e.g., abscess) |
🔷 4️⃣ Culture & Sensitivity (C&S)
- In chronic or recurrent sinusitis to guide antibiotic therapy
💊🩺 MEDICAL MANAGEMENT OF SINUSITIS
The goal of medical treatment is to: ✅ Relieve symptoms
✅ Eliminate infection (if present)
✅ Restore sinus drainage
✅ Prevent complications and recurrence
🔷 1️⃣ Acute Sinusitis (Mostly Viral)
| Treatment Component | Examples | Purpose |
|---|---|---|
| 💧 Saline nasal irrigation | Isotonic or hypertonic saline rinses | Clear mucus, reduce inflammation |
| 💊 Decongestants | Oxymetazoline (nasal spray), Pseudoephedrine | Reduce nasal/sinus swelling (short-term use only) |
| 💊 Analgesics / Antipyretics | Paracetamol, Ibuprofen | Relieve pain and fever |
| 💊 Antihistamines (if allergic) | Cetirizine, Loratadine | Reduce allergy-related inflammation |
| 💊 Nasal corticosteroids | Fluticasone, Mometasone | Decrease mucosal swelling |
🚫 Antibiotics not recommended for viral sinusitis (most cases resolve within 7–10 days)
🔷 2️⃣ Bacterial Sinusitis (Moderate to Severe)
✅ Indications for antibiotics:
- Symptoms >10 days without improvement
- Severe symptoms: high fever, purulent discharge, facial pain
- Worsening after initial improvement (“double sickening”)
| Antibiotics (First-line) | Duration |
|---|---|
| 💊 Amoxicillin-clavulanate | 5–7 days (adults), 10–14 days (children) |
| 💊 Doxycycline | For penicillin-allergic patients |
| 💊 Cefixime or Cefuroxime | In resistant or complicated cases |
| 💊 Clindamycin + Cephalosporin | For anaerobic coverage (especially in dental origin) |
🔷 3️⃣ Chronic Sinusitis Management
| Treatment | Purpose |
|---|---|
| 💊 Long-term nasal steroids | Reduce chronic inflammation |
| 💧 Regular saline irrigation | Maintain drainage and clear secretions |
| 💊 Antibiotics (3–6 weeks) | Based on culture sensitivity |
| 💊 Antifungal therapy (if needed) | In fungal sinusitis (esp. in immunocompromised) |
| 💊 Allergy control | With antihistamines or immunotherapy |
🏥🔧 SURGICAL MANAGEMENT OF SINUSITIS
Surgery is indicated when: ✅ Medical therapy fails (especially in chronic or recurrent sinusitis)
✅ There’s an anatomical obstruction (e.g., deviated septum, polyps)
✅ There are complications (e.g., orbital cellulitis, abscess, meningitis)
🔧 Types of Surgical Procedures
| Procedure | Indication / Purpose |
|---|---|
| 🔬 Functional Endoscopic Sinus Surgery (FESS) | Most common; opens natural sinus drainage pathways using an endoscope |
| 👃 Septoplasty | Corrects deviated nasal septum that blocks drainage |
| 🌀 Polypectomy | Removes nasal polyps causing obstruction |
| 🔍 Turbinate reduction | Shrinks enlarged turbinates |
| 🧠 Caldwell-Luc operation | Accesses maxillary sinus via upper gum; used less now |
| 💉 Drainage of abscess | If complications arise (e.g., subperiosteal, orbital abscess) |
| 🧠 Image-guided sinus surgery | Advanced FESS guided by CT scans for precise navigation |
🧑⚕️ Postoperative Care:
- Nasal packing (if done) is removed after 24–48 hours
- Avoid nose blowing, heavy lifting, hot drinks for a few days
- Continue saline irrigation and prescribed medications
- Monitor for complications: bleeding, infection, CSF leak
👩⚕️🩺 NURSING MANAGEMENT OF SINUSITIS
🎯 Nursing Objectives
✅ Relieve nasal and facial discomfort
✅ Promote sinus drainage and prevent complications
✅ Administer medications safely and effectively
✅ Educate the patient on treatment, self-care, and prevention
✅ Support surgical recovery if performed
🔷 I. NURSING ASSESSMENT
| Component | Details |
|---|---|
| 📋 Subjective data | Headache, facial pain/pressure, congestion, nasal discharge, reduced smell |
| 👁️ Objective data | Swollen nasal mucosa, mouth breathing, fever, tenderness over sinuses |
| 🩺 Medical history | Allergies, recurrent colds, recent URTI, dental infections, past surgeries |
🔷 II. NURSING DIAGNOSES
| Nursing Diagnosis | Related To |
|---|---|
| 🤕 Acute pain | Inflammation and sinus pressure |
| 🌬️ Ineffective airway clearance | Nasal obstruction due to mucosal swelling |
| 🔁 Risk for infection progression | Unresolved infection or poor drainage |
| ❌ Deficient knowledge | Misunderstanding of medication use or self-care |
| 😴 Disturbed sleep pattern | Due to nasal blockage and breathing difficulty |
🔷 III. NURSING INTERVENTIONS
✅ 1. Relieve Pain and Nasal Pressure
- Apply warm moist compresses over affected sinuses to promote drainage
- Elevate the head of the bed to facilitate sinus drainage
- Encourage gentle nose blowing (one nostril at a time)
- Administer analgesics/antipyretics (e.g., Paracetamol, Ibuprofen)
✅ 2. Promote Airway Clearance and Drainage
- Instruct on steam inhalation or nebulization
- Encourage saline nasal sprays or irrigation (e.g., neti pot)
- Monitor nasal discharge for color, odor (suggestive of infection)
- Educate on avoiding nasal decongestants beyond 3–5 days (to prevent rebound congestion)
✅ 3. Administer Medications as Prescribed
- Antibiotics (if bacterial) – ensure full course is completed
- Antihistamines – especially if allergic component suspected
- Nasal corticosteroids – for chronic inflammation
- Monitor for side effects or allergic reactions
✅ 4. Postoperative Care (if sinus surgery done)
- Monitor for bleeding, CSF leak, or infection signs
- Instruct patient to avoid nose blowing, straining, or bending over
- Ensure sterile dressing changes if needed
- Encourage routine saline irrigation post-surgery for healing
✅ 5. Health Education
- Teach to identify early signs of complications:
- Increased facial swelling
- High fever
- Visual changes (suggesting orbital cellulitis)
- Encourage hydration and rest
- Stress the importance of avoiding allergens, dust, and cold air
- Recommend using air humidifiers during dry seasons
🔷 IV. EVALUATION
✔️ Pain and pressure are relieved or significantly reduced
✔️ Patient maintains patent airway and reports improved breathing
✔️ Patient adheres to medication and nasal hygiene regimen
✔️ Prevents recurrence by avoiding allergens/irritants
✔️ Understands when to seek medical help.
🥗💧 NUTRITIONAL CONSIDERATIONS IN SINUSITIS
While sinusitis is not primarily a nutritional disorder, appropriate dietary measures can support immune function, reduce inflammation, and relieve symptoms.
✅ Recommended Nutritional Guidelines:
| Nutritional Element | Purpose / Benefit |
|---|---|
| 💧 Increase fluid intake | Helps thin mucus and promote sinus drainage |
| 🍋 Vitamin C-rich foods | Boosts immunity and reduces duration of infections (e.g., citrus fruits, amla, guava) |
| 🧄 Anti-inflammatory foods | Garlic, turmeric, and ginger reduce nasal inflammation |
| 🥬 Leafy greens and vegetables | Provide antioxidants and vitamins for tissue healing |
| 🐟 Omega-3 fatty acids | Found in fish, walnuts – help modulate inflammation |
| 🚫 Avoid dairy (if sensitive) | May thicken mucus in some individuals |
| 🥵 Avoid cold foods and drinks | Cold items can worsen symptoms in acute sinusitis |
| ☕ Limit caffeine and alcohol | Can cause dehydration and worsen sinus dryness |
⚠️ COMPLICATIONS OF SINUSITIS
If untreated or poorly managed, sinusitis can lead to serious ENT or intracranial complications, especially in chronic or bacterial forms.
🔷 ENT Complications
| Complication | Description |
|---|---|
| 👁️ Orbital cellulitis | Infection spreads to the eye socket; causes swelling, pain, visual changes |
| 🧠 Osteomyelitis | Infection of facial bones (e.g., frontal bone) |
| 🔁 Recurrent sinusitis | Multiple episodes per year |
| 👃 Nasal polyps | Chronic inflammation leads to mucosal overgrowth |
| 🦷 Dental pain | From maxillary sinus involvement |
🔷 Intracranial Complications (Rare but severe)
| Complication | Description |
|---|---|
| 🧠 Meningitis | Infection spreads to meninges |
| 🧠 Brain abscess | Due to extension of ethmoid or frontal sinus infection |
| 🧠 Cavernous sinus thrombosis | Blood clot in venous system from sinus infection |
🧠 KEY POINTS TO REMEMBER
✅ Sinusitis is the inflammation of one or more paranasal sinuses, often following a cold or allergy
✅ Most acute cases are viral and resolve without antibiotics
✅ Chronic sinusitis lasts more than 12 weeks and may require imaging and long-term therapy
✅ Symptoms include nasal congestion, facial pain/pressure, purulent discharge, and headache
✅ Medical treatment includes analgesics, decongestants, nasal corticosteroids, saline rinses, and antibiotics if bacterial
✅ Functional Endoscopic Sinus Surgery (FESS) is the most common surgical option for chronic/refractory sinusitis
✅ Nurses play a key role in symptom relief, medication education, fall prevention, and surgical care
✅ Diet and hydration help thin mucus and reduce inflammation
✅ Prevent recurrence by avoiding triggers like smoke, dust, allergens, and cold air.
TONSILLITIS
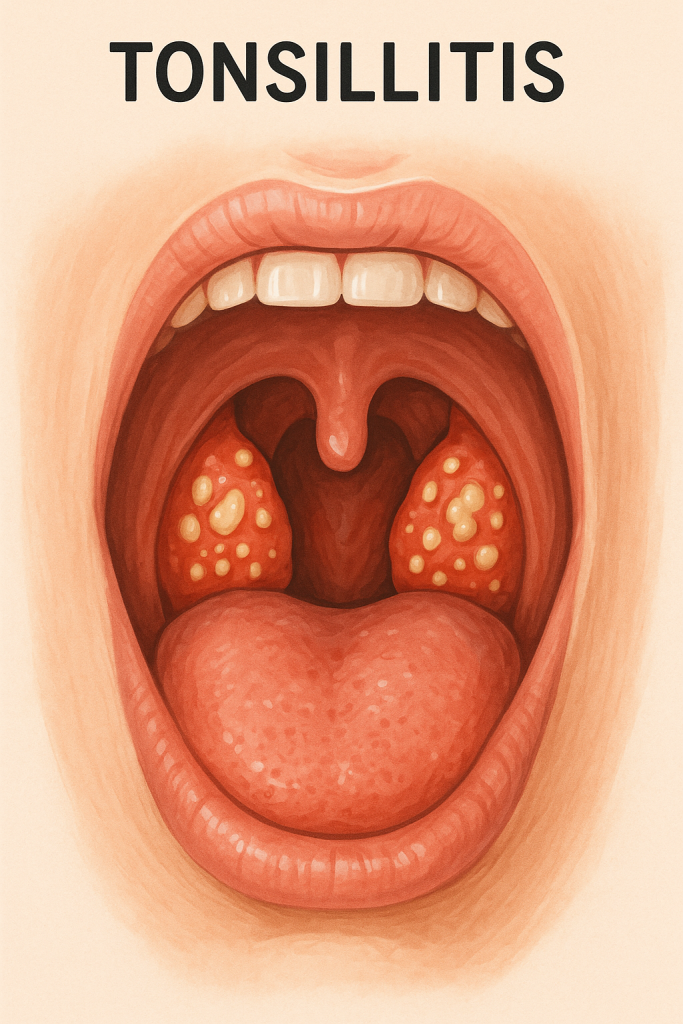
DEFINITION
Tonsillitis is defined as the inflammation and infection of the palatine tonsils, which are lymphoid tissues located on either side at the back of the throat. It is characterized by sore throat, difficulty swallowing, fever, and swollen tonsils, and may be acute or chronic in nature.
Tonsils play a role in immune defense, especially in childhood.
CAUSES OF TONSILLITIS
Tonsillitis can be caused by a variety of infectious agents:
1. Viral Causes (most common)
- Adenovirus
- Influenza virus
- Epstein–Barr virus (mononucleosis)
- Coronavirus
- Rhinovirus
- Herpes simplex virus
2. Bacterial Causes
- Group A β-hemolytic Streptococcus pyogenes (most common bacterial cause)
- Staphylococcus aureus
- Haemophilus influenzae
- Neisseria gonorrhoeae (rare)
- Mycoplasma pneumoniae (atypical presentation)
Risk Factors
- Age (common in children aged 5–15 years)
- Repeated exposure to infections (e.g., school settings)
- Poor oral hygiene
- Low immunity
- Environmental irritants (e.g., smoking exposure)
TYPES OF TONSILLITIS
A. Based on Duration
| Type | Description |
|---|---|
| ⏱ Acute Tonsillitis | Sudden onset; lasts for <10 days |
| 🔁 Recurrent Tonsillitis | Multiple episodes per year (≥5–7 per year) |
| 🕒 Chronic Tonsillitis | Persistent mild inflammation for months |
| ⚠️ Peritonsillar Abscess (Quinsy) | Complication of untreated acute tonsillitis |
B. Based on Cause
| Type | Cause |
|---|---|
| 🦠 Bacterial Tonsillitis | Commonly due to Streptococcus pyogenes |
| 🧫 Viral Tonsillitis | Caused by adenovirus, EBV, etc. |
PATHOPHYSIOLOGY OF TONSILLITIS
1️⃣ Pathogens (virus or bacteria) enter the body via airborne droplets or contact.
2️⃣ These microbes invade the epithelial lining of the tonsils, initiating an inflammatory immune response.
3️⃣ The tonsillar crypts (deep folds) trap bacteria/virus → triggers:
- Leukocyte infiltration
- Tissue swelling
- Exudate formation
4️⃣ Result:
- Enlarged tonsils with white/yellow patches, erythema, and pain
- Immune response may cause fever, lymph node swelling, and sore throat
SIGNS AND SYMPTOMS OF TONSILLITIS
| Symptom | Description |
|---|---|
| 🤒 Fever and chills | Especially in bacterial tonsillitis |
| 😫 Sore throat | Most common complaint; can radiate to ears |
| 🗣️ Dysphagia (painful swallowing) | Due to swollen, inflamed tonsils |
| 👅 Enlarged red tonsils | With or without white patches/exudates |
| 👃 Foul breath (halitosis) | Due to bacterial overgrowth |
| 🧠 Headache, malaise | Common in systemic viral/bacterial infections |
| 💬 Muffled or hoarse voice | Due to throat inflammation |
| 🦠 Cervical lymphadenopathy | Tender, enlarged lymph nodes near the jaw/neck |
| 🚫 Trismus or drooling | In severe cases or abscess |
DIAGNOSIS OF TONSILLITIS
1️⃣ History and Physical Examination
- Ask about:
- Duration and frequency of sore throat
- Associated fever, voice change, or difficulty swallowing
- Examine:
- Tonsillar enlargement (grade 1–4)
- Presence of exudates, redness, crypts, or ulcers
2️⃣ Throat Swab / Culture
- Gold standard for confirming bacterial tonsillitis
- Detects Group A Streptococcus or other organisms
3️⃣ Rapid Antigen Detection Test (RADT)
- For Group A Streptococcus
- Quick results, used in clinics
4️⃣ Complete Blood Count (CBC)
- Viral: ↑ lymphocytes
- Bacterial: ↑ neutrophils, ↑ WBC
5️⃣ Monospot Test (for EBV)
- If infectious mononucleosis is suspected (especially in adolescents)
💊🩺 MEDICAL MANAGEMENT OF TONSILLITIS
🎯 Objectives:
✅ Eliminate the infection (if bacterial)
✅ Relieve pain and fever
✅ Prevent complications
✅ Improve oral intake and comfort
🔷 1️⃣ Supportive/Symptomatic Treatment (For viral or mild bacterial cases)
| Treatment | Purpose |
|---|---|
| 💊 Analgesics/Antipyretics | Paracetamol or Ibuprofen – relieve pain and fever |
| 💧 Warm salt water gargles | Reduce throat inflammation and discomfort |
| 🧊 Cold fluids or popsicles | Soothe throat and reduce swelling |
| 💊 Local anesthetic lozenges | Temporary pain relief |
| 💦 Adequate fluid intake | Prevent dehydration, especially in children |
| 🍲 Soft, bland diet | Minimize throat irritation |
| 🛌 Rest and isolation | Especially in infectious (viral or strep) cases |
🔷 2️⃣ Antibiotic Therapy (For confirmed or strongly suspected bacterial tonsillitis)
| Antibiotic | Duration | Notes |
|---|---|---|
| 💊 Penicillin V (oral) | 10 days | First-line for Group A Streptococcus |
| 💉 Penicillin G (IM) | Single dose | Used for poor oral compliance |
| 💊 Amoxicillin | 10 days | Effective and well-tolerated |
| 💊 Azithromycin | 3–5 days | Alternative for penicillin allergy |
| 💊 Clindamycin | For recurrent or resistant cases |
⚠️ Important: Complete the full antibiotic course to prevent rheumatic fever or glomerulonephritis
🔷 3️⃣ Antiviral Management
Only indicated if the cause is confirmed viral like EBV (Epstein-Barr Virus):
- Symptomatic treatment is mainstay
- Corticosteroids (short course) may be used in severe airway obstruction
🏥🔧 SURGICAL MANAGEMENT OF TONSILLITIS
🔷 Indications for Tonsillectomy
Tonsillectomy (surgical removal of tonsils) is considered when:
✅ Recurrent Tonsillitis (e.g., ≥7 episodes in 1 year, ≥5/year for 2 years)
✅ Chronic Tonsillitis with persistent bad breath, pain, or abscess
✅ Peritonsillar Abscess (especially if recurrent)
✅ Airway obstruction due to enlarged tonsils (e.g., sleep apnea, mouth breathing)
✅ Tonsillar hypertrophy with dysphagia or speech problems
✅ Suspicion of tonsillar tumor or neoplasia
🔧 Surgical Procedures
| Procedure | Description |
|---|---|
| 🛠️ Conventional tonsillectomy | Performed under general anesthesia with scalpel or electrocautery |
| 🔥 Coblation tonsillectomy | Uses radiofrequency with less thermal damage |
| 🔥 Laser tonsillectomy | Less bleeding; often for adults or outpatient |
| 💉 Tonsillotomy | Partial removal (not common in infection cases) |
🧑⚕️ Postoperative Care Highlights
- Monitor for bleeding, especially in first 24 hours and after 7 days
- Maintain hydration and soft/cold diet
- Avoid hot/spicy foods, gargling, coughing, or strenuous activity
- Manage pain with prescribed analgesics
- Observe for signs of infection or secondary hemorrhage
👩⚕️🩺 NURSING MANAGEMENT OF TONSILLITIS
🎯 Nursing Objectives
✅ Relieve throat discomfort and fever
✅ Ensure adequate hydration and nutrition
✅ Prevent complications (e.g., abscess, airway obstruction)
✅ Support recovery and promote compliance with treatment
✅ Provide postoperative care if tonsillectomy is performed
🔷 I. NURSING ASSESSMENT
| Component | Observation/Action |
|---|---|
| 📋 Subjective data | Sore throat, difficulty swallowing, headache, malaise |
| 👁️ Objective data | Swollen/red tonsils, fever, lymph node enlargement, voice change |
| 🩺 History taking | Recent URTI, frequency of infections, allergy to medications |
| 💧 Hydration status | Check oral intake, signs of dehydration (dry lips, low output) |
🔷 II. NURSING DIAGNOSES
| Diagnosis | Related To |
|---|---|
| 🔥 Acute pain | Inflammation and swelling of tonsils |
| 🌬️ Ineffective airway clearance | Tonsillar hypertrophy and secretions |
| 🍽️ Imbalanced nutrition (less than body needs) | Painful swallowing, poor intake |
| 🌡️ Hyperthermia | Infection-related fever |
| ❌ Deficient knowledge | About disease, medication use, and prevention |
🔷 III. NURSING INTERVENTIONS
✅ 1. Pain and Fever Management
- Administer analgesics/antipyretics as prescribed (e.g., paracetamol, ibuprofen)
- Encourage warm saline gargles (if age-appropriate)
- Use cool compresses on forehead and neck if febrile
- Provide comfort measures like warm fluids and quiet environment
✅ 2. Maintain Airway and Promote Breathing
- Encourage upright or semi-Fowler’s position to reduce throat swelling
- Monitor for stridor, drooling, or difficulty breathing (signs of obstruction)
- Perform gentle suctioning if excessive secretions are present (in children)
✅ 3. Promote Hydration and Nutrition
- Offer cold fluids, ice chips, popsicles, or milkshakes
- Provide soft, bland foods (e.g., mashed potatoes, soup, pudding)
- Monitor oral intake, urine output, and signs of dehydration
- Avoid hot, spicy, or acidic foods that irritate the throat
✅ 4. Administer and Educate About Medications
- Ensure correct antibiotic schedule and complete course
- Watch for allergic reactions or side effects
- Explain importance of avoiding self-medication and overuse of antibiotics
- Teach correct technique if throat sprays or lozenges are used
✅ 5. Post-Tonsillectomy Care (if applicable)
- Monitor for postoperative bleeding (especially 1st and 7th day post-op)
- Instruct to avoid nose blowing, coughing, and clearing throat forcefully
- Maintain hydration and cold liquid intake
- Encourage quiet activities and adequate rest
- Assess for pain, administer prescribed analgesics
- Instruct to report:
- Bright red bleeding from mouth/nose
- Signs of infection (fever, foul breath)
🔷 IV. EVALUATION
✔️ Pain and fever reduced with medication and comfort measures
✔️ Adequate oral intake maintained
✔️ Tonsils reducing in size or healed post-surgery
✔️ No signs of complications like abscess or airway distress
✔️ Patient and/or caregiver demonstrate understanding of home care, medications, and follow-up needs,
🥗🍲 NUTRITIONAL CONSIDERATIONS IN TONSILLITIS
Nutrition is essential in supporting recovery, especially when painful swallowing, fever, or post-tonsillectomy healing interfere with food intake.
✅ Nutritional Goals:
- Ensure adequate hydration
- Provide calorie-dense, soft-texture foods to support healing
- Avoid irritants and promote tissue recovery
🍴 Recommended Diet:
| Dietary Advice | Rationale |
|---|---|
| 💧 Encourage fluids (water, juice, broth) | Prevent dehydration, ease throat dryness |
| 🍦 Cold or cool liquids (milkshakes, ice cream, smoothies) | Soothe throat inflammation and reduce swelling |
| 🥣 Soft foods (porridge, mashed potato, custard) | Minimize discomfort during swallowing |
| 🍊 Vitamin C-rich foods (if tolerated) | Support immunity and tissue repair |
| 🍗 Protein-rich items (blended dal, curd, eggs) | Help with tissue healing and energy needs |
⚠️ Foods to Avoid:
- 🌶️ Spicy or acidic foods (may irritate throat)
- 🍟 Fried or hard/crunchy foods (can cause discomfort or bleeding post-op)
- 🥤 Carbonated or very hot beverages
⚠️ COMPLICATIONS OF TONSILLITIS
If untreated or improperly managed, tonsillitis may lead to local and systemic complications, especially in bacterial cases.
🔹 Local Complications:
| Complication | Description |
|---|---|
| 💥 Peritonsillar abscess (Quinsy) | Pus-filled swelling near tonsils causing trismus, severe pain |
| 😮 Airway obstruction | Due to massively swollen tonsils (especially in children) |
| 🦠 Otitis media | Infection spreads via Eustachian tube |
| 🦷 Dental malocclusion | Chronic hypertrophy may affect jaw in children |
🔹 Systemic Complications (esp. from Streptococcal infection):
| Complication | Description |
|---|---|
| 💓 Rheumatic fever | Autoimmune response affecting heart, joints |
| 🩺 Post-streptococcal glomerulonephritis | Kidney inflammation leading to hematuria, edema |
| 🌡️ Sepsis | Rare; generalized bloodstream infection |
🧠 KEY POINTS TO REMEMBER
✅ Tonsillitis is inflammation of the tonsils, often due to viral or bacterial infection
✅ Group A Streptococcus (GAS) is the most common bacterial cause
✅ Presents with sore throat, fever, dysphagia, swollen tonsils, and lymphadenopathy
✅ Diagnosis includes clinical examination, throat swab, and rapid antigen tests
✅ Antibiotics (penicillin) are given if bacterial; supportive care for viral types
✅ Tonsillectomy is considered in recurrent, chronic, or complicated cases
✅ Nurses play a vital role in pain relief, hydration support, education, and monitoring
✅ Ensure complete antibiotic course to prevent rheumatic complications
✅ Proper nutrition, hydration, and rest are essential for recovery
✅ Monitor for signs of peritonsillar abscess or bleeding post-tonsillectomy.
LARYNGITIS
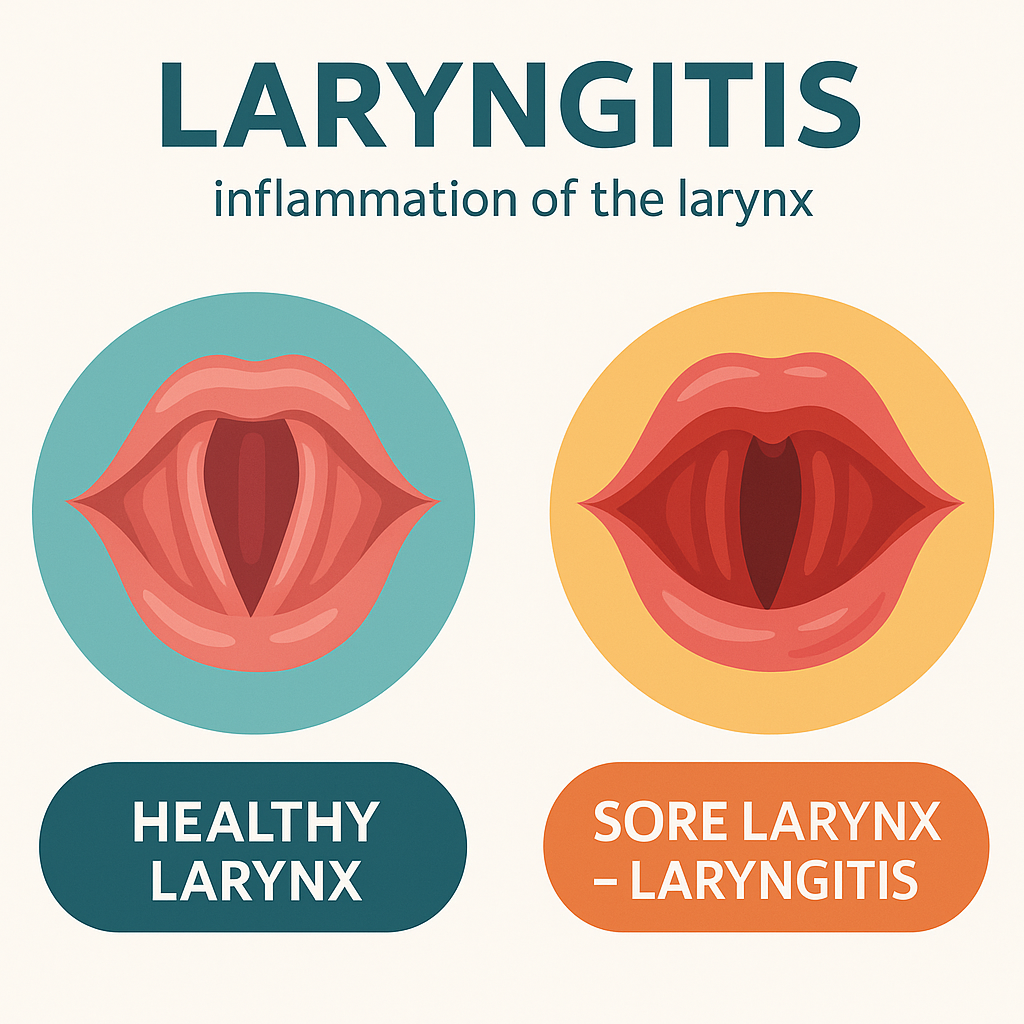
DEFINITION
Laryngitis is the inflammation of the larynx (voice box), typically involving the vocal cords, resulting in hoarseness, voice loss, sore throat, and dry cough. It may be acute or chronic, and is often caused by infections, vocal strain, allergens, or irritants.
🔍 The larynx is located in the upper part of the trachea and contains the vocal cords, which vibrate to produce sound.
CAUSES OF LARYNGITIS
1️⃣ Infectious Causes
- Viral (most common): Rhinovirus, Influenza, Parainfluenza, Adenovirus
- Bacterial: Group A Streptococcus, Haemophilus influenzae (rare)
- Fungal: Candida species (in immunocompromised or steroid inhaler users)
- Tuberculosis or Syphilitic laryngitis (rare, chronic cases)
2️⃣ Non-Infectious / Irritant Causes
- Excessive voice use: shouting, singing, teaching
- Smoking, alcohol abuse
- GERD (acid reflux irritates the larynx)
- Inhalation of dust, chemicals, fumes
- Allergies or postnasal drip
- Trauma (e.g., endotracheal intubation)
- Radiation therapy to neck
TYPES OF LARYNGITIS
Based on Duration:
| Type | Description |
|---|---|
| ⏱ Acute Laryngitis | Sudden onset, lasts < 3 weeks (viral or overuse) |
| ⏳ Chronic Laryngitis | Persists > 3 weeks due to long-term irritants |
Based on Cause:
| Type | Cause |
|---|---|
| 🦠 Infectious laryngitis | Viral, bacterial, fungal |
| 😷 Reflux laryngitis | Due to gastroesophageal reflux (GERD) |
| 🗣️ Vocal strain laryngitis | Overuse of voice |
| 💨 Irritant-induced laryngitis | From smoking, fumes, allergens |
| 🧫 Chronic hypertrophic or atrophic | Thickened or thinned vocal cords (seen in smokers or elderly) |
PATHOPHYSIOLOGY OF LARYNGITIS
1️⃣ Trigger (infection, irritant, overuse) causes inflammation of the laryngeal mucosa and vocal cords
2️⃣ Inflammation leads to:
- Edema (swelling) of the vocal cords
- Redness and possible mucous exudate
- Impaired vibration of cords → hoarseness or aphonia (voice loss)
- Coughing due to laryngeal irritation
- Reflex muscle spasms in chronic cases
3️⃣ If chronic, the repeated insult may lead to:
- Fibrosis or thickening of vocal cords
- Granulomas or polyps in severe cases
SIGNS AND SYMPTOMS OF LARYNGITIS
| Symptom | Description |
|---|---|
| 🔇 Hoarseness of voice | Most common symptom – may progress to voice loss |
| 🗣️ Weak, breathy, or raspy voice | Due to improper vocal cord vibration |
| 😷 Dry or sore throat | Especially in acute viral laryngitis |
| 🗯️ Dry cough | Non-productive, frequent |
| 🌡️ Low-grade fever | Occasionally present in viral/bacterial cases |
| 🫁 Feeling of a lump in throat | Especially in chronic laryngitis |
| 😮 Throat clearing | Recurrent due to irritation or postnasal drip |
| ❌ Pain with speaking or swallowing | In moderate to severe inflammation |
⚠️ Emergency signs (rare but serious):
- Stridor (noisy breathing)
- Difficulty breathing or swallowing
- Drooling (may suggest epiglottitis in children)
DIAGNOSIS OF LARYNGITIS
1️⃣ Clinical History and Physical Exam
- Hoarseness, voice change, sore throat, cough
- History of voice overuse, GERD, smoking, or infection
- Inspection of oropharynx (may be normal or show redness)
2️⃣ Indirect or Direct Laryngoscopy
- Visualizes inflammation, swelling, redness, ulcers, or polyps
- Flexible fiberoptic laryngoscopy preferred in persistent or chronic cases
3️⃣ Throat Swab and Culture
- Rule out bacterial or fungal causes in suspected infection
4️⃣ Other Investigations (if chronic):
- Voice assessment by speech therapist
- Biopsy if suspicious of neoplastic lesion
- pH monitoring if GERD-related laryngitis suspected
MEDICAL MANAGEMENT OF LARYNGITIS
The management depends on the cause (viral, bacterial, allergic, irritant, or chronic). Most cases are self-limiting and respond to conservative treatment.
1️⃣ General Supportive Measures (for all types)
| Management | Purpose |
|---|---|
| 🔇 Voice rest | Prevents further trauma to inflamed vocal cords |
| 💧 Hydration | Keeps mucosa moist and promotes healing |
| 🌬️ Humidified air/steam inhalation | Soothes laryngeal mucosa |
| 🍵 Warm saline gargles | Eases throat irritation |
| 🛌 Rest and avoid smoking/alcohol | Essential in acute and chronic cases |
2️⃣ Acute Viral Laryngitis (most common)
| Treatment | Notes |
|---|---|
| ❌ No antibiotics | Viruses are the cause; use supportive care |
| 💊 Analgesics | Paracetamol or Ibuprofen for pain/fever |
| 🌿 Herbal lozenges | Temporary soothing effect |
3️⃣ Bacterial Laryngitis (rare)
| Antibiotics (if indicated) | Duration | Used when… |
|---|---|---|
| 💊 Amoxicillin-clavulanate | 5–7 days | Purulent sputum, fever, systemic signs |
| 💊 Clarithromycin / Azithromycin | For penicillin-allergic patients |
4️⃣ Fungal Laryngitis
- Often due to Candida, especially in steroid inhaler users or immunocompromised
- Treated with:
- 💊 Nystatin oral suspension
- 💊 Fluconazole (in systemic cases)
- Educate about rinsing mouth after steroid inhaler use
5️⃣ Chronic/Reflux Laryngitis
| Management | Notes |
|---|---|
| 💊 Proton pump inhibitors (PPIs) | Omeprazole, Pantoprazole – reduce acid reflux |
| 💊 H2 blockers | Ranitidine – alternative option |
| 🔄 Lifestyle changes | Weight loss, elevate head, avoid caffeine/alcohol |
| ❌ Avoid spicy, acidic food | To prevent laryngeal irritation |
6️⃣ Antihistamines and Antiallergics
- Used if postnasal drip or allergies are contributing
- Examples: Cetirizine, Loratadine
SURGICAL MANAGEMENT OF LARYNGITIS
Surgery is rarely required and reserved for chronic or complicated cases:
Indications for Surgery:
- Chronic laryngitis not responding to medication
- Suspicion of neoplastic lesion or vocal cord polyp
- Vocal cord nodules, granulomas, cysts
- Laryngeal stenosis or structural abnormalities
Surgical Procedures
| Procedure | Purpose |
|---|---|
| 🔬 Microlaryngoscopy with biopsy | Diagnostic; confirms chronic changes or malignancy |
| 🗣️ Vocal cord polypectomy | Removal of benign vocal cord lesions |
| 🔥 Laser laryngeal surgery | Precise excision of nodules/granulomas with minimal damage |
| 🔄 Vocal cord stripping | For severe chronic inflammation or hyperkeratosis |
| 💉 Injection laryngoplasty | For vocal cord paralysis (voice restoration) |
| 🛠️ Tracheostomy (rare/emergency) | If airway obstruction is severe (e.g., epiglottitis, abscess) |
NURSING MANAGEMENT OF LARYNGITIS
Objectives of Nursing Care
✅ Relieve throat discomfort and promote vocal cord healing
✅ Maintain effective airway and prevent respiratory distress
✅ Ensure hydration and nutrition
✅ Educate the patient regarding voice rest, lifestyle changes, and medication compliance
✅ Prevent complications and support recovery
I. NURSING ASSESSMENT
| Area | Nursing Focus |
|---|---|
| 📋 History taking | Recent URI, voice overuse, smoking, GERD, allergens |
| 🗣️ Voice assessment | Hoarseness, aphonia, duration of voice loss |
| 👃 Airway check | Observe for signs of airway obstruction (stridor, retractions) |
| 🌡️ Vital signs monitoring | Especially temperature, respiratory rate, and oxygen saturation |
| 👄 Hydration and intake | Check oral intake, dry mucosa, or signs of dehydration |
| 😷 Throat and nasal exam | For associated pharyngitis, postnasal drip |
II. NURSING DIAGNOSES
| Nursing Diagnosis | Related To |
|---|---|
| 🔇 Impaired verbal communication | Inflammation/swelling of vocal cords |
| 🌬️ Ineffective airway clearance | Swelling of laryngeal structures or mucus |
| 🔥 Acute pain (throat) | Inflammation and mucosal irritation |
| 💧 Risk for fluid volume deficit | Reduced intake due to pain or fever |
| 📚 Deficient knowledge | About disease process, treatment, and voice hygiene |
III. NURSING INTERVENTIONS
1. Voice Care and Comfort Measures
- Encourage complete voice rest or minimal speaking
- Educate on avoiding whispering (puts more strain on cords)
- Provide pen and paper or communication board for non-verbal communication
- Use humidifier or steam inhalation to reduce dryness and soothe irritation
- Administer warm fluids (if tolerated) and throat lozenges
2. Monitor and Maintain Airway Patency
- Observe for hoarseness with difficulty breathing or stridor (signs of airway compromise)
- Keep patient in upright position to promote easier breathing
- Suction gently if thick secretions are present (especially in postnasal drip)
3. Medication Administration and Monitoring
- Administer prescribed:
- Analgesics/antipyretics
- Antibiotics (if bacterial)
- PPIs or antacids (for reflux-induced laryngitis)
- Antihistamines (if allergic cause)
- Monitor for side effects and allergic reactions
4. Hydration and Nutrition Support
- Encourage increased fluid intake (water, broth, non-citrus juices)
- Provide soft, non-irritating foods (avoid spicy or acidic items)
- Monitor for dehydration: low urine output, dry lips, poor skin turgor
5. Patient and Family Education
- Teach:
- Voice rest importance
- Avoid smoking, alcohol, and air pollutants
- Proper inhaler technique if on steroid sprays
- Use mouth rinsing after inhalers to prevent fungal laryngitis
- How to recognize warning signs (e.g., severe hoarseness >2 weeks, stridor)
IV. EVALUATION
✔️ Patient experiences relief from hoarseness and throat pain
✔️ Maintains hydration and adequate nutrition
✔️ Demonstrates understanding of voice hygiene and medication use
✔️ Avoids airway obstruction and other complications
✔️ Verbal communication improves or returns to baseline.
NUTRITIONAL CONSIDERATIONS IN LARYNGITIS
Nutritional care in laryngitis focuses on:
✅ Maintaining hydration
✅ Preventing throat irritation
✅ Supporting immune recovery
✅ Minimizing voice strain during swallowing
Recommended Nutritional Practices:
| Nutritional Element | Purpose / Benefit |
|---|---|
| 💧 Increased fluid intake | Keeps throat moist, soothes mucosa, and thins secretions |
| 🍲 Warm fluids | Soups, herbal teas, broths ease inflammation and pain |
| 🍦 Cold items | Ice chips, popsicles may relieve acute pain in some cases |
| 🥣 Soft-textured foods | Mashed vegetables, porridge, smoothies — easy to swallow |
| 🍯 Honey (if not contraindicated) | Natural anti-inflammatory and throat soother |
| 🧂 Avoid spicy/salty foods | Prevent additional mucosal irritation |
| 🍋 Avoid acidic drinks | Citrus juices, carbonated beverages can worsen irritation |
| 🧃 Avoid dairy (if mucus-producing) | May increase throat secretions in some individuals |
COMPLICATIONS OF LARYNGITIS
Most cases resolve with conservative management, but untreated or chronic cases may result in:
Acute Complications:
| Complication | Description |
|---|---|
| 🚨 Airway obstruction | Due to severe laryngeal swelling (esp. in children) |
| 🦠 Secondary infection | Bacterial superinfection of inflamed mucosa |
| 🔊 Severe voice loss (aphonia) | In prolonged vocal cord inflammation |
Chronic Complications:
| Complication | Description |
|---|---|
| 🗣️ Vocal cord nodules or polyps | Due to persistent overuse or irritation |
| ⚠️ Chronic hoarseness | From unresolved or repeated inflammation |
| 🔥 Laryngeal granuloma or cyst | Long-term irritation, GERD-related or post-intubation |
| 🧫 Laryngeal carcinoma (rare) | Especially in chronic smokers with hoarseness >3 weeks |
KEY POINTS TO REMEMBER
✅ Laryngitis is inflammation of the larynx/vocal cords, most commonly viral or due to vocal overuse
✅ Main symptom is hoarseness, often with sore throat, dry cough, and weak voice
✅ Viral laryngitis is self-limiting; antibiotics are not routinely required
✅ Management includes:
- Voice rest, hydration, humidification, and pain relief
- Treat underlying cause (infection, reflux, allergens, smoking)
✅ Chronic hoarseness (>3 weeks) must be evaluated for structural lesions or malignancy
✅ Nurses play a key role in:
- Symptom management
- Monitoring airway
- Educating on voice hygiene
- Preventing complications
EPISTAXIS
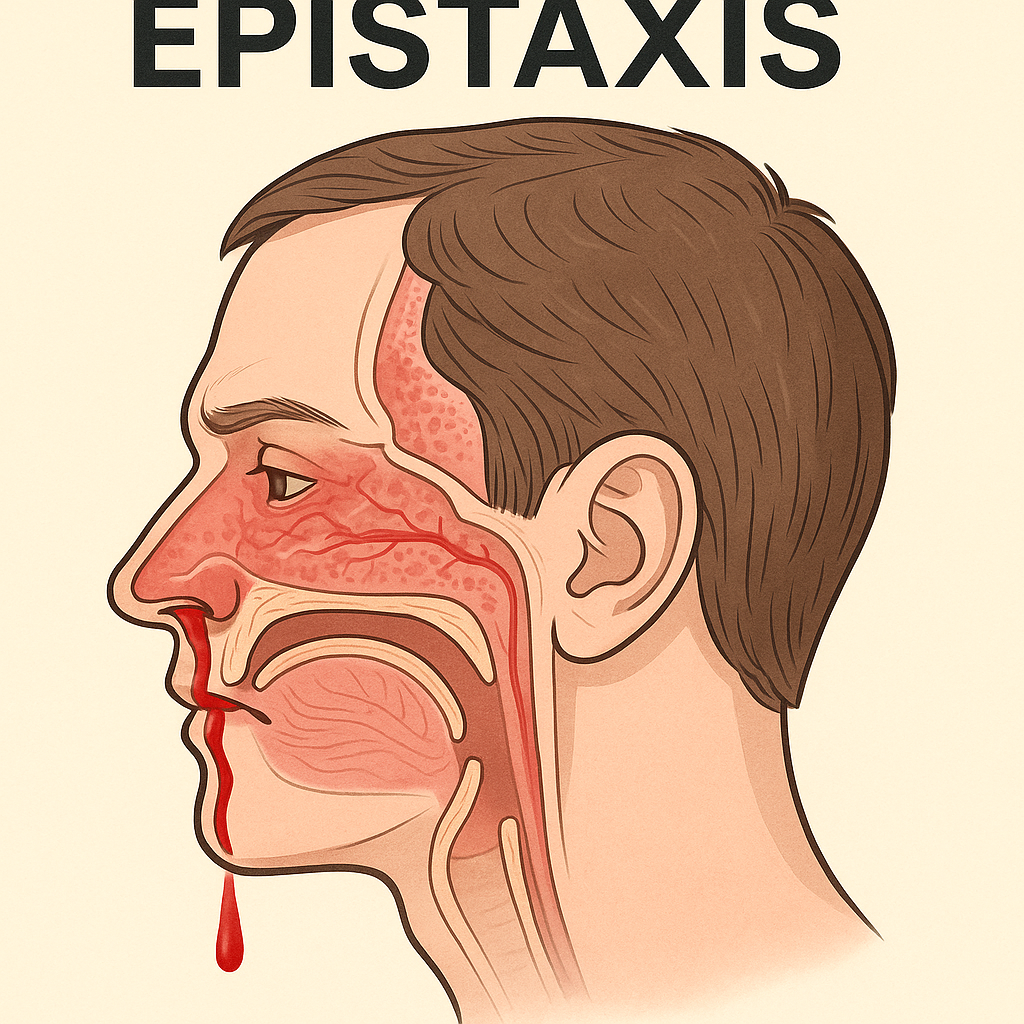
(Nosebleed)
📘 DEFINITION
Epistaxis is defined as bleeding from the nasal cavity, usually from the nasal septum or lateral nasal wall, due to rupture or erosion of blood vessels in the nasal mucosa. It is a common ENT emergency and may be spontaneous or traumatic, mild or severe, and anterior or posterior in origin.
🔍 CAUSES OF EPISTAXIS
Epistaxis may result from local, systemic, environmental, or iatrogenic factors.
🔷 1️⃣ Local Causes
- Trauma (nose picking, blow to nose)
- Deviated nasal septum
- Nasal infections (rhinitis, sinusitis)
- Tumors (benign or malignant)
- Nasal surgery or foreign body
- Dry air exposure or irritants
🔷 2️⃣ Systemic Causes
- Hypertension
- Blood disorders: Hemophilia, leukemia, thrombocytopenia
- Liver disease (affects clotting factors)
- Vitamin C or K deficiency
- Use of anticoagulants (aspirin, warfarin, heparin)
🔷 3️⃣ Environmental / Others
- High altitude (low humidity and oxygen)
- Sudden temperature changes
- Drug abuse (e.g., cocaine sniffing)
- Pregnancy (due to increased blood flow)
🔢 TYPES OF EPISTAXIS
🔹 Based on Site of Bleeding:
| Type | Characteristics |
|---|---|
| 🔺 Anterior Epistaxis | Most common (~90%), from Kiesselbach’s plexus, easily visible and managed |
| 🔻 Posterior Epistaxis | Less common, from Woodruff’s plexus or branches of sphenopalatine artery; may be profuse and hard to locate |
🔹 Based on Duration or Pattern:
- Acute Epistaxis: Single, sudden episode
- Recurrent Epistaxis: Frequent nosebleeds, often due to underlying disorder
- Chronic Epistaxis: Common in older adults or systemic diseases
🧬 PATHOPHYSIOLOGY OF EPISTAXIS
1️⃣ The nasal mucosa is highly vascular, supplied by branches from both internal and external carotid arteries.
2️⃣ Factors such as trauma, inflammation, dryness, hypertension, or clotting defects can rupture superficial vessels.
3️⃣ Anterior bleeding usually originates from the Kiesselbach’s plexus — a vascular network at the anterior septum.
4️⃣ Posterior bleeding arises from deeper arteries like the sphenopalatine or posterior ethmoidal, making it more difficult to control.
5️⃣ Continued bleeding may lead to hypovolemia, airway obstruction, or aspiration if severe.
🚨 SIGNS AND SYMPTOMS OF EPISTAXIS
| Symptom | Description |
|---|---|
| 👃 Bleeding from one or both nostrils | Sudden, bright red bleeding (anterior) |
| 🤢 Blood in throat or mouth | Common in posterior epistaxis |
| 😰 Anxiety, palpitations | From blood loss or distress |
| 💨 Breathing difficulty | If bleeding obstructs nasal airflow |
| 😵 Dizziness, weakness, fainting | Signs of hypovolemia in severe cases |
| 🩸 Recurrent episodes | Indicates underlying pathology or coagulopathy |
🧪 DIAGNOSIS OF EPISTAXIS
🔷 1️⃣ Clinical Assessment
- Time, duration, and frequency of nosebleeds
- Any trauma, surgery, nasal irritation
- History of hypertension, bleeding disorders, medications
🔷 2️⃣ Physical Examination
- Anterior rhinoscopy with nasal speculum and light
- Posterior nasal exam (if anterior bleeding not found)
- Vital signs to assess shock in severe cases
🔷 3️⃣ Laboratory Tests
- 🩸 CBC – to assess hemoglobin, platelet count
- 🧪 Bleeding time, clotting time, INR – for coagulation status
- 🧬 LFTs, RFTs – if systemic illness suspected
- 💊 Medication history (anticoagulants, NSAIDs)
🔷 4️⃣ Imaging (if needed)
- X-ray or CT scan of sinuses – if tumor, trauma, or foreign body suspected
- Nasal endoscopy – for difficult or posterior bleeds
💊 MEDICAL MANAGEMENT OF EPISTAXIS
✅ Initial First Aid (Nurse-led / Emergency)
| Steps | Purpose |
|---|---|
| Sit the patient upright, leaning forward | Prevent blood aspiration and airway obstruction |
| Pinch nostrils for 10–15 minutes | Direct pressure to stop bleeding |
| Apply ice pack to bridge of nose | Causes vasoconstriction |
| Ask patient to breathe through mouth | To avoid sniffing or swallowing blood |
✅ Pharmacological Management
| Medication Type | Purpose |
|---|---|
| 💉 Topical vasoconstrictors | Oxymetazoline, phenylephrine – constrict vessels |
| 💊 Antibiotics (if packing used) | Prevent sinus or nasal infections |
| 💊 Tranexamic acid (topical/systemic) | Promotes clot stability |
| 💊 Antihypertensives (if needed) | Control blood pressure |
| ❌ Avoid NSAIDs, aspirin | As they increase bleeding tendency |
✅ Nasal Packing (if bleeding persists)
- Anterior nasal packing: Gauze with antibiotic ointment or special nasal tampon
- Posterior nasal packing: For posterior bleeds; often requires admission and monitoring
🏥🔧 SURGICAL MANAGEMENT OF EPISTAXIS
Used when medical and conservative methods fail, or when recurrent/severe bleeding persists.
🔧 Common Surgical Options:
| Procedure | Indication / Notes |
|---|---|
| 🧠 Cauterization (chemical or electric) | Silver nitrate or electrocautery for visible bleeding points |
| 🩺 Ligation of arteries | Sphenopalatine or ethmoidal artery ligation in resistant cases |
| 🔬 Endoscopic nasal surgery | For recurrent posterior bleeds or vascular lesions |
| 🛠️ Septoplasty | If bleeding is due to septal deviation or trauma |
| 🧬 Embolization | Performed by interventional radiology – occludes bleeding vessel via catheter (for high-risk cases) |
👩⚕️🩺 NURSING MANAGEMENT OF EPISTAXIS
🎯 Objectives of Nursing Care
✅ Control active bleeding
✅ Maintain airway patency
✅ Prevent aspiration or recurrence
✅ Monitor for complications (e.g., shock, infection)
✅ Provide patient education on prevention and home care
🔷 I. NURSING ASSESSMENT
| Assessment Area | Focus |
|---|---|
| 📋 History taking | Recent trauma, nose-picking, hypertension, medications (e.g., aspirin, warfarin), bleeding disorders |
| 👃 Bleeding site & severity | Duration, flow rate, side, color (bright red = arterial) |
| 🧠 Vital signs | BP, HR, RR – assess for hypovolemia or hypertension |
| 💨 Airway & breathing | Check for nasal obstruction, mouth breathing, stridor |
| 🩸 Signs of anemia | Dizziness, pallor, fatigue in case of prolonged bleeding |
| 💊 Medication review | Identify any anticoagulants or NSAIDs use |
🔷 II. NURSING DIAGNOSES
| Diagnosis | Related To |
|---|---|
| 🩸 Risk for bleeding | Ruptured nasal vessels, coagulation disorders |
| 💨 Ineffective airway clearance | Due to nasal obstruction or posterior bleeding |
| 😵 Risk for aspiration | Blood flowing backward into oropharynx |
| 😰 Anxiety | Related to sudden bleeding and distress |
| 📚 Deficient knowledge | Regarding causes, triggers, and self-care |
🔷 III. NURSING INTERVENTIONS
✅ 1. During Active Bleeding (Initial Emergency Care)
- Place the patient in a sitting position, leaning slightly forward
- Ask the patient to pinch the soft part of the nose firmly for 10–15 minutes
- Apply ice pack or cold compress over the nose and nape of neck
- Instruct to breathe through the mouth and avoid talking
- Keep emesis basin nearby if blood is swallowed
- Monitor airway closely, especially in posterior bleeds
- Do not let the patient lie flat or tilt head backward (increases aspiration risk)
✅ 2. After Bleeding Stops
- Assess hemodynamic status (pulse, BP, pallor)
- Inspect for rebleeding or clots in nasal passages
- Provide calm environment to reduce anxiety or BP spikes
- Educate to avoid nose blowing, sneezing with mouth closed, and strenuous activity for 24–48 hours
- Keep nasal mucosa moist (humidified air, saline spray)
✅ 3. If Nasal Packing is Done
- Monitor for:
- Discomfort, difficulty breathing
- Signs of infection (fever, foul odor)
- Pressure ulceration inside nasal cavity
- Ensure packing remains in place and is removed as scheduled
- Administer antibiotics and analgesics as prescribed
- Educate patient to report any new bleeding or increased pain
✅ 4. Airway and Aspiration Precautions
- In posterior epistaxis with pack or risk of aspiration:
- Keep suction equipment nearby
- Observe for gagging, choking, restlessness
- Position in semi-Fowler’s or side-lying position
✅ 5. Patient & Family Education
- Teach:
- Avoid nose picking, trauma, smoking, alcohol
- Keep nails trimmed (especially in children)
- Manage underlying hypertension or bleeding disorders
- Use humidifier during dry seasons
- Avoid spicy food, hot drinks, and bending forward after bleeding episode
- Seek help if:
- Bleeding lasts >20 minutes
- Recurrent or spontaneous bleeding occurs
- Bleeding follows trauma or is associated with headache/vision changes
🔷 IV. EVALUATION
✔️ Bleeding successfully controlled
✔️ Airway maintained without compromise
✔️ Patient remains stable (vital signs normal)
✔️ No signs of aspiration or infection
✔️ Patient verbalizes understanding of preventive and emergency home care
🥗 NUTRITIONAL CONSIDERATIONS IN EPISTAXIS
While epistaxis is not directly caused by diet, proper nutrition plays a role in:
✅ Supporting blood vessel health
✅ Preventing mucosal dryness
✅ Promoting healing in recurrent or chronic cases
✅ Supporting clotting function in coagulopathies
✅ Recommended Nutritional Guidelines:
| Nutrient/Food Item | Purpose and Benefit |
|---|---|
| 💧 Adequate water intake | Prevents dryness of nasal mucosa, especially in dry climates |
| 🍊 Vitamin C-rich foods | Strengthens capillaries, reduces mucosal fragility (e.g., oranges, amla, guava) |
| 🥬 Iron-rich foods | Replenish blood loss if anemia develops (e.g., spinach, jaggery, meats) |
| 🐟 Vitamin K-rich foods | Supports coagulation (e.g., green leafy vegetables, broccoli) |
| 🚫 Avoid spicy/hot foods | Can dilate nasal blood vessels and trigger rebleeding |
| 🚭 Avoid caffeine and alcohol | These may dry out mucosa and increase BP in hypertensives |
⚠️ COMPLICATIONS OF EPISTAXIS
Though usually benign, untreated or recurrent epistaxis can lead to:
🔹 Local Complications:
| Complication | Description |
|---|---|
| 🔁 Recurrent nosebleeds | Due to uncorrected cause or nasal mucosal trauma |
| 🦠 Infection (sinusitis, rhinitis) | From prolonged nasal packing or mucosal injury |
| 🧱 Septal perforation | From repeated cauterization or trauma |
| 🧫 Foreign body retention | Particularly in children or mentally impaired patients |
| 🔄 Rhinitis medicamentosa | Rebound congestion and bleeding from overuse of nasal decongestants |
🔹 Systemic Complications:
| Complication | Description |
|---|---|
| 🩸 Anemia | In cases of prolonged or repeated blood loss |
| 🫁 Aspiration of blood | Can lead to coughing, choking, or pneumonia |
| ⚠️ Hypovolemic shock (rare) | In severe, uncontrolled posterior bleeding |
| ⛑️ Airway obstruction | Due to posterior clot or pooling blood |
🧠 KEY POINTS TO REMEMBER
✅ Epistaxis is a common ENT emergency, often from Kiesselbach’s plexus in the anterior septum
✅ Most cases are anterior, mild, and self-limiting; posterior bleeds are rare but dangerous
✅ Causes include trauma, hypertension, coagulopathies, infections, dry air, and irritants
✅ Initial care includes pinching nostrils, leaning forward, and cold compress
✅ Treatment may involve nasal packing, cauterization, or artery ligation
✅ Nurses must monitor for airway patency, bleeding control, and signs of shock or aspiration
✅ Teach patients to avoid nose picking, trauma, spicy food, and dry environments
✅ Ensure proper hydration, vitamin C, and iron intake if anemia or recurrent bleeding occurs
✅ Seek emergency care if bleeding is prolonged (>20 mins), recurrent, or severe
NASAL OBSTRUCTION

DEFINITION
Nasal obstruction refers to a partial or complete blockage of one or both nasal passages that impairs airflow through the nose. It can be acute or chronic, intermittent or constant, and significantly affects breathing, sleep, voice, and quality of life.
CAUSES OF NASAL OBSTRUCTION
Nasal obstruction can result from a variety of local or systemic conditions, including:
1️⃣ Structural Causes
- Deviated nasal septum (most common)
- Nasal polyps
- Enlarged inferior turbinates
- Adenoid hypertrophy (common in children)
- Nasal tumors (benign or malignant)
- Choanal atresia (congenital blockage)
2️⃣ Inflammatory/Infectious Causes
- Allergic rhinitis
- Acute or chronic sinusitis
- Viral or bacterial rhinitis
3️⃣ Foreign Bodies
- Especially in children (beads, toys, food)
4️⃣ Traumatic Causes
- Nasal fracture
- Post-surgical swelling
5️⃣ Iatrogenic/Drug-Related
- Rhinitis medicamentosa (rebound swelling from overuse of nasal decongestants)
TYPES OF NASAL OBSTRUCTION
| Type | Description |
|---|---|
| 🔁 Unilateral | Often caused by foreign body, tumor, or septal deviation |
| 🔁 Bilateral | Seen in polyps, allergic rhinitis, adenoid hypertrophy |
| ⏱ Acute | Sudden onset – usually due to infection or trauma |
| 🕒 Chronic | Lasts >12 weeks – often related to structural or allergic causes |
PATHOPHYSIOLOGY
1️⃣ Nasal obstruction results from physical narrowing or blockage of the nasal cavity.
2️⃣ Structural issues (e.g., deviated septum, polyps) reduce the cross-sectional area of the airway.
3️⃣ Inflammatory processes cause:
- Mucosal edema,
- Increased secretions,
- Narrowed airflow pathways
4️⃣ In rhinitis medicamentosa, prolonged decongestant use leads to rebound congestion, worsening obstruction.
5️⃣ Reduced airflow through the nasal passages results in:
- Mouth breathing
- Altered speech
- Snoring or sleep apnea in severe cases
SIGNS AND SYMPTOMS
| Symptom | Description |
|---|---|
| 🔴 Nasal congestion | Sensation of blocked nose, worse on one or both sides |
| 🗣️ Mouth breathing | Especially during sleep or exercise |
| 🤧 Postnasal drip | Common in allergic or infectious causes |
| 🗯️ Snoring or noisy breathing | Due to reduced airflow during sleep |
| 😴 Sleep disturbances | Restlessness, daytime fatigue |
| 🧠 Headache or facial pressure | From sinus involvement |
| 🦻 Reduced sense of smell | Due to obstruction of olfactory passage |
| 💨 Shortness of breath (rare) | Seen in severe bilateral obstruction |
DIAGNOSIS OF NASAL OBSTRUCTION
1️⃣ Clinical Evaluation
- History: Duration, severity, laterality, associated symptoms
- Physical exam: Visual inspection of nose and nasal mucosa
2️⃣ Anterior Rhinoscopy
- Visualizes septal deviation, turbinate hypertrophy, polyps, foreign body
3️⃣ Nasal Endoscopy
- Allows deeper visualization of posterior nasal cavity, nasopharynx, and sinus drainage areas
4️⃣ Imaging Studies
- X-ray of paranasal sinuses: For sinusitis
- CT scan of sinuses: For chronic sinusitis, polyps, tumors, or surgical planning
- MRI: In suspected tumors or soft tissue lesions
5️⃣ Allergy Testing
- Skin prick test or serum IgE: If allergic rhinitis is suspected
MEDICAL MANAGEMENT
Treatment is aimed at relieving symptoms and treating the underlying cause.
✅ For Inflammatory/Infectious Causes:
| Medication | Purpose |
|---|---|
| 💊 Nasal corticosteroids | Fluticasone, mometasone – reduce inflammation (esp. in allergic rhinitis and polyps) |
| 💊 Antihistamines | Cetirizine, loratadine – for allergic triggers |
| 💊 Decongestants (short-term) | Oxymetazoline nasal spray – avoid >5 days |
| 💊 Saline nasal irrigation | Soothes and clears nasal passages |
| 💊 Antibiotics (if infection) | For bacterial sinusitis |
| 💊 Anticholinergics | Ipratropium bromide – reduces secretions |
✅ For Rebound Congestion (Rhinitis Medicamentosa):
- Discontinue nasal decongestants
- Start nasal steroids and saline rinses
- Gradual tapering may be necessary
🏥 SURGICAL MANAGEMENT
Surgery is considered for persistent nasal obstruction not responsive to medical therapy or in structural causes.
🔧 Common Surgical Procedures:
| Procedure | Indications |
|---|---|
| 🔧 Septoplasty | For deviated nasal septum |
| 🔧 Turbinate reduction (turbinoplasty) | For hypertrophied inferior turbinates |
| 🔧 Polypectomy / FESS | For nasal polyps or chronic sinusitis |
| 🔧 Adenoidectomy | In children with adenoid hypertrophy |
| 🔧 Endoscopic sinus surgery | To open blocked sinus passages |
| 🔧 Removal of foreign body/tumor | If identified as cause |
👩⚕️🩺 NURSING MANAGEMENT OF NASAL OBSTRUCTION
🎯 Nursing Objectives
✅ Maintain airway patency
✅ Relieve nasal congestion and associated discomfort
✅ Monitor for complications (e.g., sinusitis, sleep disturbances, infections)
✅ Provide pre- and post-operative care (if surgery done)
✅ Educate the patient on treatment adherence and prevention
🔷 I. NURSING ASSESSMENT
| Assessment Focus | Key Observations |
|---|---|
| 👃 Nasal breathing | Degree of obstruction (unilateral/bilateral), mouth breathing |
| 🗣️ Voice changes | Hyponasal voice due to poor nasal resonance |
| 💤 Sleep disturbances | Snoring, restlessness, daytime fatigue |
| 🌡️ Signs of infection | Fever, nasal discharge, facial pressure |
| 💬 History taking | Allergy, trauma, recurrent colds, previous surgery |
| 🫁 Respiratory assessment | Oxygen saturation and rate in severe bilateral cases |
🔷 II. NURSING DIAGNOSES
| Diagnosis | Related To |
|---|---|
| 💨 Ineffective airway clearance | Nasal blockage from structural or inflammatory causes |
| 🤧 Impaired comfort | Congestion, postnasal drip, mouth breathing |
| 🔂 Disturbed sleep pattern | Noisy breathing, mouth breathing |
| 📚 Deficient knowledge | About causes, treatments, medication use |
| ❌ Risk for infection | Due to retained secretions or nasal packing |
III. NURSING INTERVENTIONS
1. Relieving Nasal Obstruction and Promoting Comfort
- Elevate the head of the bed to ease breathing
- Encourage use of saline nasal sprays or rinses
- Apply warm compresses to sinuses in cases of sinus pressure
- Ensure proper room humidification to prevent drying of mucosa
- Avoid exposure to allergens, dust, strong perfumes, or smoke
2. Administering and Monitoring Medications
- Administer nasal corticosteroids, antihistamines, or decongestants as prescribed
- Educate on correct nasal spray technique
- Monitor for rebound congestion (rhinitis medicamentosa)
- Ensure compliance with antibiotics in infectious causes
- Observe for side effects like nasal dryness or epistaxis
3. Postoperative Nursing Care (if surgery performed)
| Postoperative Focus | Nursing Actions |
|---|---|
| 🛌 Positioning | Keep head elevated to reduce edema and bleeding risk |
| 🩸 Bleeding monitoring | Check nasal dressings, observe for active bleeding |
| 😷 Airway care | Encourage mouth breathing initially; provide oral care |
| 💧 Hydration & nutrition | Encourage soft foods and fluids; prevent dehydration |
| 💊 Pain control | Administer analgesics as prescribed |
| 📚 Discharge teaching | Avoid nose blowing, strenuous activity, hot drinks |
4. Health Education & Prevention
- Teach:
- Avoidance of triggers (dust, pollen, smoke)
- Proper inhaler and nasal spray use
- Importance of hydration and air humidification
- Avoid overuse of decongestant sprays
- Reinforce follow-up appointments, especially in:
- Allergic rhinitis
- Post-surgical care
- Chronic nasal obstruction
IV. EVALUATION
✔️ Airway remains patent with improved breathing pattern
✔️ Reduction in nasal congestion, discharge, or discomfort
✔️ Patient verbalizes understanding of home care and medication use
✔️ Sleep and oral intake return to normal
✔️ No signs of infection, bleeding, or recurrence.
NUTRITIONAL CONSIDERATIONS IN NASAL OBSTRUCTION
Nutrition plays an indirect but important role in managing and recovering from nasal obstruction, especially when caused by allergic, infectious, or chronic inflammatory conditions.
Dietary Recommendations:
| Nutritional Focus | Purpose / Benefit |
|---|---|
| 💧 Encourage fluid intake | Helps to thin mucus and ease nasal drainage |
| 🍲 Warm soups & herbal teas | Soothe irritated nasal passages, aid in breathing comfort |
| 🍊 Vitamin C-rich foods | Boost immunity and reduce inflammation (e.g., citrus, amla, kiwi) |
| 🥬 Iron-rich foods | Prevent fatigue in chronic cases causing poor sleep |
| 🐟 Omega-3 fatty acids | Anti-inflammatory properties (e.g., fish, flaxseed) |
| 🌶️ Avoid spicy or very hot foods | May increase mucus secretion or irritate nasal lining |
| 🥛 Dairy products (moderate) | May increase nasal secretions in sensitive individuals |
| 🚫 Avoid alcohol & caffeine | Can dehydrate and dry nasal mucosa |
COMPLICATIONS OF NASAL OBSTRUCTION
Untreated or persistent nasal obstruction can lead to local, systemic, or quality-of-life-related complications:
Local Complications
| Complication | Description |
|---|---|
| 😷 Chronic sinusitis | Due to blocked sinus drainage pathways |
| 🦠 Recurrent respiratory infections | Poor nasal filtration of pathogens |
| 🦻 Eustachian tube dysfunction | May lead to otitis media, especially in children |
| 🗣️ Speech alterations | Especially in children with chronic mouth breathing |
| 💤 Mouth breathing & bad breath | Due to ongoing nasal obstruction |
Systemic / Long-term Complications
| Complication | Description |
|---|---|
| 😴 Obstructive Sleep Apnea (OSA) | Can result from bilateral obstruction during sleep |
| 😵 Cognitive fatigue | Due to poor oxygenation and sleep disturbances |
| 🧠 Impaired quality of life | Decreased productivity, concentration, and confidence |
| 💀 In rare cases: hypoxia | If prolonged severe obstruction without treatment |
KEY POINTS TO REMEMBER
✅ Nasal obstruction is a common complaint that may arise from structural, inflammatory, infectious, or allergic causes
✅ It leads to mouth breathing, snoring, poor sleep, altered voice, and reduced quality of life
✅ Anterior rhinoscopy, nasal endoscopy, and imaging (CT scan) are key to diagnosis
✅ Medical treatment includes:
- Nasal corticosteroids
- Antihistamines
- Decongestants (short-term)
- Saline irrigations
✅ Surgical options like septoplasty, polypectomy, FESS, or adenoidectomy are used in structural or chronic cases
✅ Nurses play a vital role in:
- Monitoring airway
- Medication education
- Postoperative care
- Teaching prevention strategies
✅ Proper hydration, immunity-boosting nutrition, allergen avoidance, and medication adherence improve outcomes
✅ Chronic or recurrent nasal obstruction must be evaluated to prevent long-term complications.
LARYNGEAL OBSTRUCTION

DEFINITION
Laryngeal obstruction is a partial or complete blockage of the laryngeal airway, preventing normal airflow into the lungs. It is a medical emergency when severe, as it may lead to acute respiratory distress or death without prompt intervention.
The larynx is responsible for voice production and acts as a protective airway gate. Obstruction compromises both breathing and phonation.
CAUSES OF LARYNGEAL OBSTRUCTION
Causes can be inflammatory, traumatic, neoplastic, neurologic, or congenital:
1️⃣ Infectious / Inflammatory
- Acute laryngitis
- Epiglottitis (especially in children)
- Laryngeal edema from allergy, infection, or burns
2️⃣ Trauma
- Direct blow to the neck
- Strangulation
- Endotracheal intubation injury
- Inhalation of hot gases or chemicals
3️⃣ Neoplastic
- Laryngeal tumors (benign or malignant)
- Vocal cord papillomas
- Subglottic stenosis
4️⃣ Neurologic / Functional
- Vocal cord paralysis
- Laryngospasm due to reflux, anesthesia, or psychogenic causes
5️⃣ Foreign Body Aspiration
- Common in children
- Sudden onset choking and cyanosis
6️⃣ Allergic / Anaphylactic Reaction
- Angioedema involving the larynx
- Medical emergency with rapid swelling
TYPES OF LARYNGEAL OBSTRUCTION
| Type | Description |
|---|---|
| 🌀 Partial obstruction | Some airflow present, may have stridor or voice changes |
| 🚫 Complete obstruction | No air movement; respiratory arrest imminent |
| ⬆️ Supraglottic | Above the vocal cords (epiglottis, aryepiglottic folds) |
| ⬇️ Subglottic / Glottic | At or below the vocal cords |
| 🔁 Acute or Chronic | Sudden or progressive onset depending on the cause |
PATHOPHYSIOLOGY
1️⃣ Obstruction of the larynx impedes airflow to the lungs, leading to:
- Hypoxia (low oxygen levels)
- Hypercapnia (CO₂ retention)
- Respiratory acidosis
2️⃣ If unresolved, this results in:
- Air hunger
- Increased work of breathing
- Respiratory failure
3️⃣ Protective reflexes (e.g., laryngospasm) may worsen the condition
4️⃣ In chronic cases, fibrosis, stenosis, or tumor growth leads to progressive airway narrowing
SIGNS AND SYMPTOMS
| Symptom | Description |
|---|---|
| 😰 Dyspnea | Difficulty breathing, especially on inspiration |
| 🗣️ Hoarseness or voice loss | Indicates involvement of vocal cords |
| 🌬️ Stridor (inspiratory) | High-pitched noise from turbulent airflow |
| 🫁 Tachypnea | Rapid breathing |
| 😵 Restlessness, cyanosis | Indicate hypoxia |
| 🧠 Confusion or drowsiness | Signs of worsening respiratory distress |
| ❌ Choking / No breath sounds | Seen in complete obstruction |
| 💬 Inability to speak | Red flag for total airway blockage |
DIAGNOSIS
1️⃣ Clinical Examination
- Observe for stridor, use of accessory muscles, cyanosis
- Assess speech, air entry, and neck movement
2️⃣ Flexible Fiberoptic Laryngoscopy
- Direct visualization of laryngeal structures
- Identify edema, mass, foreign body, vocal cord motion
3️⃣ Imaging Studies
- X-ray soft tissue neck: May show soft tissue swelling or foreign body
- CT scan / MRI: For tumors or deep soft tissue involvement
4️⃣ Blood Gas Analysis
- Check for hypoxemia and hypercapnia
5️⃣ Allergy Testing (if anaphylaxis suspected)
MEDICAL MANAGEMENT
Management depends on severity:
In Mild or Early Cases:
| Therapy | Indication |
|---|---|
| 💊 Corticosteroids | Reduce airway inflammation and edema |
| 💊 Nebulized adrenaline | For acute laryngeal edema or croup |
| 💊 Antihistamines | In allergic laryngeal swelling |
| 💊 Bronchodilators | If coexisting asthma component |
| 💉 IV fluids and oxygen | Supportive care to maintain oxygenation |
| ❌ Avoid sedatives | May worsen hypoventilation |
In Emergency Cases:
- Secure airway immediately:
- High-flow oxygen
- Prepare for intubation or tracheostomy
SURGICAL MANAGEMENT
Surgical intervention is life-saving in many cases of severe laryngeal obstruction.
Surgical Options:
| Procedure | Indication |
|---|---|
| 🛠️ Endotracheal intubation | Temporarily relieves obstruction |
| 🔪 Emergency tracheostomy | For complete obstruction unrelieved by intubation |
| 🧬 Cricothyrotomy (emergency) | Emergency airway if tracheostomy/intubation fails |
| 🔍 Laryngoscopic foreign body removal | If obstruction is due to foreign body |
| 🔥 Laser debulking of tumor | For obstructive laryngeal tumors |
| 🔁 Laryngeal reconstruction / stenting | In chronic stenosis or trauma cases |
NURSING MANAGEMENT OF LARYNGEAL OBSTRUCTION
Nursing Objectives
✅ Maintain airway patency and adequate oxygenation
✅ Identify early signs of airway compromise
✅ Provide emergency care when obstruction becomes severe
✅ Assist in diagnostic and surgical interventions
✅ Educate the patient and family for prevention and follow-up care
I. NURSING ASSESSMENT
| Assessment Area | Key Observations |
|---|---|
| 💨 Respiratory status | Stridor, tachypnea, use of accessory muscles, cyanosis |
| 🗣️ Voice quality | Hoarseness, aphonia (inability to speak), muffled voice |
| 📋 History collection | Allergies, recent URTI, trauma, foreign body, medications |
| 💊 Medication history | Use of NSAIDs, antibiotics, or known allergen exposure |
| 🧠 Mental status | Restlessness, anxiety, confusion (early signs of hypoxia) |
II. NURSING DIAGNOSES
| Nursing Diagnosis | Related To |
|---|---|
| 💨 Ineffective airway clearance | Laryngeal swelling, secretions, or obstruction |
| ⛔ Impaired gas exchange | Due to restricted airflow |
| 🚨 Risk for aspiration | Especially in unconscious or partially obstructed airway |
| 😰 Anxiety | Caused by difficulty breathing |
| 📚 Deficient knowledge | Regarding emergency signs, causes, and prevention |
III. NURSING INTERVENTIONS
1. Maintain and Monitor Airway Patency
- Position patient in high-Fowler’s or semi-Fowler’s to ease breathing
- Monitor oxygen saturation continuously (SpO₂)
- Keep suction equipment and emergency airway tools at bedside
- Administer humidified oxygen as prescribed
- Prepare for intubation or tracheostomy if needed
- Stay with the patient during respiratory distress episodes
2. Administer Medications as Prescribed
| Medication Type | Nursing Action |
|---|---|
| 💊 Corticosteroids | Monitor for relief of swelling, observe side effects |
| 💊 Antihistamines | Especially in allergic cases (e.g., diphenhydramine) |
| 💨 Nebulized epinephrine | Observe response to relieve airway edema |
| 💉 Bronchodilators / oxygen therapy | Monitor breathing and lung sounds |
3. Emergency Response for Acute Obstruction
- Activate emergency team/code blue
- Provide bag-valve-mask ventilation if apneic
- Be ready to assist physician in cricothyrotomy or tracheostomy
- Do not leave the patient alone
4. Postoperative or Post-Procedure Care (if surgery done)
| Intervention | Purpose |
|---|---|
| 🩹 Tracheostomy care | Prevent infection and ensure tube patency |
| 🧼 Wound monitoring | Check for bleeding, swelling, or surgical site issues |
| 🧃 Hydration and nutrition | Provide IV fluids or enteral feeding if needed |
| 🧑⚕️ Speech therapy referral | For voice recovery in post-laryngectomy patients |
5. Health Teaching and Psychological Support
- Educate about early warning signs: stridor, voice changes, dyspnea
- Avoid known allergens or irritants
- Instruct on safe swallowing, especially in neurogenic obstruction
- Support emotional needs: voice loss or airway device anxiety
- Provide family education on emergency management and follow-up
IV. EVALUATION
✔️ Airway is patent and oxygenation is adequate
✔️ Emergency medications and procedures implemented promptly if needed
✔️ Patient demonstrates reduced anxiety and better breathing pattern
✔️ Postoperative or rehabilitative needs are met
✔️ Patient/family verbalize understanding of condition and prevention
.
NUTRITIONAL CONSIDERATIONS IN LARYNGEAL OBSTRUCTION
Nutritional care depends on the severity, cause, and treatment approach (medical vs surgical). Patients with airway compromise, post-intubation, or post-surgical interventions (like tracheostomy or laryngectomy) may require modified nutrition strategies.
Key Nutritional Guidelines:
| Nutritional Strategy | Purpose & Relevance |
|---|---|
| 💧 Adequate fluid intake | Prevents dehydration and keeps mucosa moist |
| 🥣 Soft or semi-liquid diet | Minimizes swallowing effort in mild cases |
| 🚫 Avoid spicy/hot/acidic foods | Reduces irritation of inflamed laryngeal tissues |
| ❌ Avoid oral intake if high aspiration risk | In case of severe obstruction or poor airway protection |
| 🥤 Enteral feeding (NG/PEG) | For patients with prolonged obstruction, tracheostomy, or post-surgery inability to swallow |
| 🥬 High-protein, high-calorie foods | Promote tissue repair and maintain strength |
| 👄 Oral hygiene (post-feeding) | Especially important in tracheostomy or tube-fed patients |
COMPLICATIONS OF LARYNGEAL OBSTRUCTION
Untreated or improperly managed laryngeal obstruction can be life-threatening:
Immediate Complications
| Complication | Description |
|---|---|
| 🚨 Acute respiratory distress | Life-threatening airway compromise |
| 🫁 Hypoxia and hypercapnia | Due to poor air exchange |
| ❌ Cardiac arrest | If complete airway blockage is not relieved |
| 🧠 Brain damage | From prolonged oxygen deprivation |
| 😵 Loss of consciousness | Due to CO₂ retention or oxygen loss |
Long-term / Post-treatment Complications
| Complication | Description |
|---|---|
| 🗣️ Voice changes / hoarseness | Due to vocal cord damage or laryngeal trauma |
| 💬 Loss of speech | Post-laryngectomy or vocal cord paralysis |
| 🩺 Aspiration pneumonia | From impaired laryngeal closure during swallowing |
| 🧫 Infection (tracheostomy site or larynx) | Post-procedure complication |
| 🔁 Recurrent obstruction | Due to tumor regrowth, stenosis, or edema |
KEY POINTS TO REMEMBER
✅ Laryngeal obstruction is a medical emergency that can rapidly lead to death if not managed
✅ Causes include: trauma, tumors, infections, allergic reactions, foreign bodies, or laryngeal edema
✅ Clinical signs: stridor, hoarseness, dyspnea, cyanosis, anxiety, and inability to speak
✅ Diagnosis is mainly clinical, supported by laryngoscopy, imaging, and blood gases
✅ Medical management includes:
- Oxygen therapy
- Corticosteroids
- Nebulized adrenaline
- Antihistamines (if allergic origin)
✅ Surgical interventions:
- Tracheostomy, cricothyrotomy, foreign body removal, tumor excision, laryngeal stenting
✅ Nurses play a critical role in:
- Airway monitoring
- Emergency preparedness
- Post-op care and infection prevention
- Nutrition and aspiration precautions
- Patient and family education
✅ Early intervention saves lives — recognize stridor, sudden hoarseness, or difficulty breathing as red flags!.
DEAFNESS (HEARING LOSS)

DEFINITION
Deafness (or hearing loss) is defined as the partial or complete inability to hear sound in one or both ears. It may be temporary or permanent, congenital or acquired, and can significantly affect communication, language development, and quality of life.
WHO defines disabling hearing loss as:
- >40 dB loss in the better hearing ear in adults
- >30 dB in children
CAUSES OF DEAFNESS
Hearing loss can result from damage or dysfunction in the outer ear, middle ear, inner ear, auditory nerve, or auditory cortex.
1️⃣ Conductive Causes (Outer or middle ear)
- Impacted wax
- Otitis media (acute/chronic)
- Tympanic membrane perforation
- Otosclerosis (ossicle fixation)
- Eustachian tube dysfunction
- Foreign body in ear canal
2️⃣ Sensorineural Causes (Inner ear/cochlea or auditory nerve)
- Presbycusis (age-related)
- Noise-induced hearing loss
- Viral infections (e.g., mumps, measles)
- Meniere’s disease
- Ototoxic drugs (aminoglycosides, furosemide)
- Acoustic neuroma (vestibular schwannoma)
3️⃣ Mixed Causes
- Combination of both conductive and sensorineural (e.g., chronic otitis media with cochlear damage)
4️⃣ Central Causes
- Tumors, strokes, or trauma affecting auditory brain pathways
TYPES OF DEAFNESS
| Type | Description |
|---|---|
| 🔉 Conductive hearing loss | Sound is blocked from reaching the inner ear (outer/middle ear problem) |
| 🔊 Sensorineural hearing loss | Damage to cochlea or auditory nerve |
| 🔄 Mixed hearing loss | Combination of conductive and sensorineural components |
| 👶 Congenital hearing loss | Present at birth; due to genetic factors, TORCH infections, birth injury |
| 🧠 Central auditory processing disorder | Brain cannot interpret sound signals properly |
PATHOPHYSIOLOGY
The normal hearing process involves sound waves passing through:
1️⃣ Outer ear → collected and directed to the tympanic membrane
2️⃣ Middle ear → ossicles (malleus, incus, stapes) amplify vibrations
3️⃣ Inner ear (cochlea) → converts vibrations into electrical impulses
4️⃣ Auditory nerve → carries impulses to the brain for interpretation
In conductive deafness:
- Sound fails to reach the cochlea due to blockage or mechanical disruption
In sensorineural deafness:
- Damage to hair cells of the cochlea or auditory nerve fibers
SIGNS AND SYMPTOMS
| Symptom | Description |
|---|---|
| 🔇 Reduced ability to hear sounds | Especially soft or distant speech |
| 🗣️ Speech difficulties | In children, delayed language development |
| 📢 Asking for repetition | Frequently asking others to speak louder/again |
| 📺 Increasing volume of TV/radio | Common behavioral sign in adults |
| ❌ Not responding to sounds | Especially in infants and toddlers |
| 🤷 Difficulty in noisy environments | Due to poor sound discrimination |
| 🧏 Lip reading or sign use | In profound or long-term hearing loss |
| 🧠 Tinnitus or vertigo | Often present in inner ear disorders (e.g., Meniere’s) |
DIAGNOSIS OF DEAFNESS
1️⃣ History and Physical Examination
- Onset, duration, family history, exposure to noise/drugs
2️⃣ Tuning Fork Tests
Simple bedside tests to differentiate type:
| Test | Purpose |
|---|---|
| 🎵 Rinne Test | Compares air vs bone conduction |
| 🎵 Weber Test | Lateralization to affected side (conductive) or unaffected side (sensorineural) |
3️⃣ Audiometry
- Measures hearing thresholds in decibels
- Pure tone audiometry (PTA) identifies the degree and type of loss
4️⃣ Tympanometry
- Assesses middle ear pressure and mobility of tympanic membrane
5️⃣ Otoacoustic Emissions (OAE)
- Tests cochlear (outer hair cell) function – useful in newborn screening
6️⃣ Brainstem Evoked Response Audiometry (BERA)
- Evaluates auditory nerve and brainstem function – especially in infants/unconscious
MEDICAL MANAGEMENT
For Conductive Hearing Loss:
| Treatment | Example/Use |
|---|---|
| 👂 Earwax removal | Cerumenolytics, irrigation |
| 💊 Antibiotics | Otitis media, otitis externa |
| 💧 Decongestants / Antihistamines | Eustachian tube dysfunction |
| 🧴 Topical steroid drops | In allergic or inflammatory ear conditions |
For Sensorineural Hearing Loss:
| Treatment | Notes |
|---|---|
| 💊 Corticosteroids | For sudden sensorineural hearing loss |
| 🧬 Antivirals | If viral infection suspected |
| 🚫 Avoid ototoxic drugs | Substitute with safer alternatives |
| 🔊 Hearing aids | For mild to moderate permanent loss |
| 🧏 Speech therapy | Especially for children |
SURGICAL MANAGEMENT
Surgical Options Based on Cause:
| Procedure | Indication |
|---|---|
| 🔩 Myringotomy with grommet | Chronic otitis media with effusion |
| 🔧 Tympanoplasty | Perforated eardrum |
| 🔧 Ossiculoplasty | Reconstruction of ossicles |
| 🔧 Stapedectomy | Otosclerosis (replaces stapes with prosthesis) |
| 🦻 Cochlear implant | Profound bilateral sensorineural loss not helped by hearing aids |
| 🧠 Tumor removal (e.g., neuroma) | Acoustic neuroma pressing on auditory nerve |
NURSING MANAGEMENT OF DEAFNESS (HEARING LOSS)
Nursing Objectives
✅ Promote effective communication
✅ Support psychosocial adaptation to hearing loss
✅ Prevent further hearing impairment
✅ Assist in rehabilitation (hearing aids, implants)
✅ Educate patient and family for coping and communication strategies
I. NURSING ASSESSMENT
| Assessment Area | Focus Points |
|---|---|
| 📋 History | Onset, duration, progression, noise exposure, ototoxic drugs |
| 🧏 Hearing function | Observation of speech response, lip reading, hearing aid use |
| 🗣️ Communication ability | Verbal responses, lip reading, use of sign language |
| 🧠 Cognitive/emotional state | Frustration, isolation, depression, anxiety |
| 🦻 Assistive device use | Hearing aid, cochlear implant — condition and compliance |
II. NURSING DIAGNOSES
| Nursing Diagnosis | Related To |
|---|---|
| 🧏♂️ Impaired verbal communication | Hearing loss affecting speech understanding |
| 😞 Social isolation | Inability to engage in verbal communication |
| 🤯 Disturbed sensory perception (auditory) | Altered hearing threshold |
| ❌ Risk for injury | Due to inability to hear alarms or warnings |
| 📚 Deficient knowledge | About assistive devices or rehabilitation |
III. NURSING INTERVENTIONS
1. Enhance Communication
| Intervention | Rationale |
|---|---|
| ✅ Face the patient while speaking | Enhances lip-reading and visual cues |
| ✅ Speak slowly and clearly (normal tone) | Avoids shouting which distorts sound |
| ✅ Use gestures, facial expressions | Supports non-verbal communication |
| ✅ Provide writing material or communication boards | For profound or sudden hearing loss |
| ✅ Minimize background noise | Helps in understanding speech clearly |
| ✅ Rephrase if misunderstood | More effective than repeating the same words |
2. Assist with Hearing Devices
- Ensure hearing aids are working properly
- Teach correct usage, cleaning, and storage
- Replace batteries or troubleshoot issues as needed
- Encourage regular follow-up with audiologist
- Support patients with cochlear implants in adapting to sounds
3. Environmental Safety Measures
- Place patient in safe, quiet, well-lit environment
- Install visual alarms (e.g., flashing fire alarms, doorbells)
- Use hand signals or gentle touch to get attention
- Educate family to alert patient before touching or entering room
4. Patient and Family Education
- Explain the type and cause of deafness in simple language
- Encourage early use of hearing aids or assistive technology
- Offer referrals to:
- Audiologists
- ENT specialists
- Speech-language therapists
- Sign language training
- Promote hearing conservation:
- Avoid loud noise
- Use ear protection
- Monitor ototoxic drug use
5.Psychological support
- Acknowledge emotional impact of hearing loss
- Encourage group therapy or peer support groups
- Promote positive self-esteem and independence
IV. EVALUATION
✔️ Patient uses appropriate communication strategies effectively
✔️ Maintains social interaction and safety in the environment
✔️ Demonstrates proper use and care of assistive devices
✔️ Verbalizes understanding of preventive and rehabilitative strategies
✔️ Shows improved psychological adjustment to hearing loss.
NUTRITIONAL CONSIDERATIONS IN DEAFNESS
While deafness is not primarily a nutritional disorder, certain nutrients support auditory health, nerve function, and may help prevent or slow progression of hearing loss — especially in sensorineural and age-related deafness.
Nutritional Recommendations:
| Nutrient/Food | Function / Benefit |
|---|---|
| 🍊 Vitamin C, E (antioxidants) | Protect hair cells of the inner ear from oxidative stress (e.g., oranges, spinach, nuts) |
| 🐟 Omega-3 fatty acids | Support cochlear circulation and nerve health (e.g., fish, flaxseeds) |
| 🥬 Folate (Vitamin B9) | Improves blood flow to the cochlea (e.g., leafy greens, legumes) |
| 🥚 Vitamin B12 | Deficiency associated with sensorineural hearing loss (e.g., eggs, dairy, fortified cereals) |
| 🧂 Low sodium diet | In Meniere’s disease, reduces fluid retention in the inner ear |
| 🚫 Avoid caffeine/alcohol/smoking | Can impair cochlear blood flow and worsen hearing loss |
🧃 Hydration is important for maintaining electrolyte balance in cochlear fluids.
COMPLICATIONS OF DEAFNESS
Deafness can lead to medical, social, emotional, and developmental issues if left untreated or unsupported:
In Adults
| Complication | Description |
|---|---|
| 😔 Social isolation & depression | Due to communication difficulties |
| 🧠 Cognitive decline | Associated with untreated hearing loss |
| ❌ Occupational limitations | Safety and communication risks in the workplace |
| 🚨 Injury risk | Inability to hear alarms, traffic, or warnings |
In Children
| Complication | Description |
|---|---|
| 🗣️ Speech and language delay | Especially in undiagnosed congenital cases |
| 🧠 Learning difficulties | Poor classroom performance, attention issues |
| 👨👩👧 Behavioral problems | Frustration, aggression, or withdrawal |
| 👁️ Overdependence on visual cues | May affect overall communication development |
KEY POINTS TO REMEMBER
✅ Deafness (hearing loss) is a partial or total inability to hear, caused by conductive, sensorineural, or mixed mechanisms
✅ Early identification, especially in infants and children, is critical to prevent speech and cognitive delays
✅ Causes range from wax impaction, infections, and tumors to genetic and ototoxic drug exposure
✅ Diagnosed via tuning fork tests, audiometry, tympanometry, and BERA
✅ Medical treatment includes:
- Wax removal, antibiotics, corticosteroids, hearing aids
✅ Surgical treatment includes:
- Tympanoplasty, ossiculoplasty, cochlear implants, tumor removal
✅ Nurses play a vital role in:
- Enhancing communication
- Teaching use of assistive devices
- Providing emotional support
- Ensuring safety and environment adaptation
✅ Nutrients like vitamin B12, folate, omega-3, and antioxidants support hearing health
✅ Untreated deafness can lead to social, emotional, and cognitive decline.
FOR UNLOCK 🔓 FULL COURSE NOW. MORE DETAILS CALL US OR WATSAPP ON- 8485976407
