B.SC-MICRO-sau.uni (done-JUHI)-mcq pending-UPLOAD
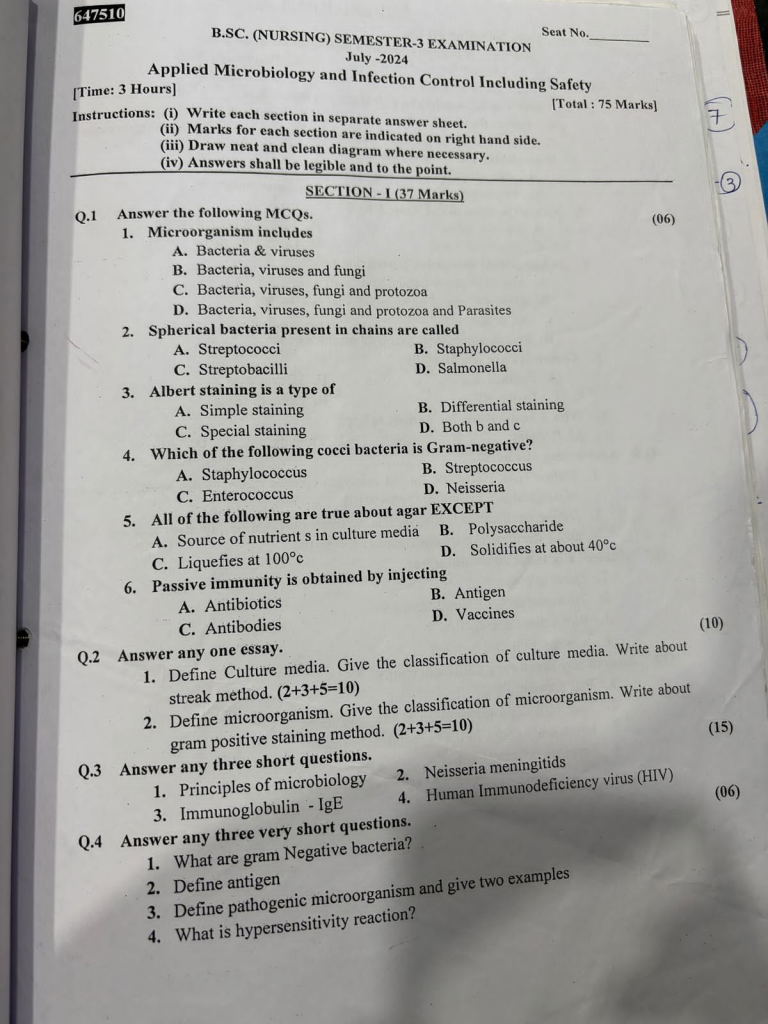
SECTION-I (37 Marks)
Q.1 Answer the following MCQs. (06)
1. Microorganism includes
A. Bacteria & viruses
B. Bacteria, viruses and fungi
C. Bacteria, viruses, fungi and protozoa
D. Bacteria, viruses, fungi and protozoa and Parasites
2. Spherical bacteria present in chains are called
A. Streptococci
B. Staphylococci
C. Streptobacilli
D. Salmonella
3. Albert staining is a type of
A. Simple staining
B. Differential staining
C. Special staining
D. Both b and c
4. Which of the following cocci bacteria is Gram-negative?
A. Staphylococcus
B. Streptococcus
C. Enterococcus
D. Neisseria
5. All of the following are true about agar EXCEPT
A. Source of nutrient s in culture media
B. Polysaccharide
C. Liquefies at 100°c
D. Solidifies at about 40°c
6. Passive immunity is obtained by injecting
A. Antibiotics
B. Antigen
C. Antibodies
D. Vaccines
Q.2 Answer any one essay.
1. Define Culture media. Give the classification of culture media. Write about streak method. (2+3+5=10)
Culture media
Culture media are nutrient preparations used in microbiology laboratories to support the growth, multiplication, and identification of microorganisms under controlled conditions.
Classification of culture media
Based on Physical State
| Type | Description | Example |
|---|---|---|
| Liquid | No solidifying agent | Nutrient broth |
| Solid | Contains agar (1.5–2%) | Nutrient agar |
| Semi-solid | Contains less agar (~0.5%) | Motility agar |
Based on Composition
| Type | Description | Example |
|---|---|---|
| Simple media | Basic nutrients for general growth | Nutrient agar |
| Complex media | Exact composition not known | Blood agar |
| Synthetic/Defined | Exact chemical composition known | Minimal media |
Based on Purpose/Function
| Type | Function | Example |
|---|---|---|
| Enriched media | Enhances growth of fastidious organisms | Blood agar, Chocolate agar |
| Selective media | Inhibits some bacteria, allows others | MacConkey agar, XLD agar |
| Differential media | Differentiates bacteria based on reaction | MacConkey agar, Blood agar |
| Transport media | Preserves sample during transport | Cary-Blair, Stuart’s media |
| Enrichment media | Increases number of desired bacteria | Selenite F broth (for Salmonella) |
Streak method
Definition
The streak method is a microbiological technique used to isolate pure colonies of bacteria from a mixed culture by mechanically thinning out the bacterial sample over the surface of a solid agar plate using a sterile loop.
Purpose
To obtain isolated colonies of bacteria
To purify a mixed culture
To study colony morphology
To prepare for biochemical and sensitivity testing
Principle
By repeatedly dragging (streaking) a microbial sample across different quadrants of the plate, the bacterial load is diluted, leading to the growth of individual, well-separated colonies.
Types of Streaking Methods
Four Quadrant Streak Method (most common)
T-Streak Method
Continuous Streak Method
Radiant Streak Method
Procedure :
Four-Quadrant Streak Method
Sterilize the inoculating loop by flaming
Dip loop in sample and streak the 1st quadrant
Re-flame loop and streak from 1st to 2nd quadrant
Repeat to make 3rd and 4th quadrants, sterilizing each time
Incubate the plate at 37°C for 24–48 hours
Result
First quadrant : Heavy growth
Second and third quadrants : Thinning out
Fourth quadrant : Well-isolated colonies
Applications
Isolation of pure cultures
Identification of bacteria
Antibiotic sensitivity testing
Colony characterization (shape, color, elevation)
2. Define microorganism. Give the classification of microorganism. Write about gram positive staining method. (2+3+5=10)
Microorganism
A microorganism is a tiny living organism that can only be seen under a microscope. It may be unicellular or multicellular and can be beneficial or harmful.
Microorganisms are microscopic organisms such as bacteria, viruses, fungi, protozoa, and algae that can live in a variety of environments and may be beneficial or harmful to other living beings.
Classification of microorganism
Microorganisms are classified based on their structure, cell type, and function. The major groups include :
Bacteria
Unicellular, prokaryotic organisms
Reproduce by binary fission
Example: Escherichia coli, Mycobacterium tuberculosis
Viruses
Acellular, non-living outside the host
Require a host cell to replicate
Example: HIV, Influenza virus
Fungi
Eukaryotic organisms, can be unicellular (yeast) or multicellular (molds)
Reproduce by spores
Example : Candida albicans, Aspergillus
Protozoa
Unicellular, eukaryotic organisms
Often motile and parasitic
Example : Plasmodium falciparum, Entamoeba histolytica
Algae
Photosynthetic, eukaryotic organisms
Mostly found in aquatic environments
Example : Chlorella, Spirogyra
Gram positive staining method
Gram staining is a differential staining technique developed by Hans Christian Gram in 1884. It is used to differentiate bacteria into Gram-positive and Gram-negative based on the composition of their cell wall
Principle
Gram-positive bacteria have a thick peptidoglycan layer in their cell wall, which retains the crystal violet stain even after alcohol decolorization.
They appear purple under the microscope.
Reagents Used
Crystal Violet – Primary stain
Gram’s Iodine – Mordant (forms crystal violet-iodine complex)
Alcohol or Acetone – Decolorizer
Safranin – Counterstain
Procedure (Step-by-Step)
Smear Preparation :
Prepare a bacterial smear on a clean glass slide and heat-fix it.
Staining with Crystal Violet (1 minute) :
Flood the smear and let it sit, then rinse with water.
Apply Gram’s Iodine (1 minute) :
Acts as a mordant to fix the dye; rinse gently with water.
Decolorize with Alcohol (10–30 seconds) :
Gently apply drops of alcohol.
Gram-positive bacteria retain the dye (remain purple).
Gram-negative bacteria lose the dye.
Counterstain with Safranin (30 seconds–1 minute) :
Stains Gram-negative bacteria pink/red; Gram-positive remain purple.
Wash and Dry :
Rinse with water and blot dry. Observe under microscope (oil immersion 100x).
Observation
Gram-positive bacteria = Purple/Violet
(due to thick peptidoglycan retaining crystal violet)
Gram-negative bacteria = Pink/Red
Examples of Gram-Positive Bacteria
Staphylococcus aureus
Streptococcus pyogenes
Bacillus anthracis
Q.3 Answer any three short questions.(15)
1.Principles of microbiology
Microbiology is the branch of science that deals with the study of microorganisms, including bacteria, viruses, fungi, protozoa, and algae. The principles of microbiology guide how these organisms are identified, classified, controlled, and studied for medical, environmental, and industrial purposes.
Principles of Microbiology
Microorganisms Are Ubiquitous
Microbes are found everywhere: in soil, water, air, on surfaces, and even in the human body.
This principle explains the importance of aseptic techniques in healthcare to prevent contamination.
Microorganisms Can Be Beneficial or Harmful
Beneficial : used in food production (e.g., curd, bread), antibiotics (e.g., penicillin), and biotechnology.
Harmful: cause diseases (e.g., TB, HIV), food spoilage, and infections.
Microorganisms Have Specific Growth Requirements
Each microorganism requires specific temperature, pH, nutrients, and oxygen conditions for optimal growth.
This helps in culturing them in laboratories and understanding infection control.
Microorganisms Can Be Cultured and Studied in the Lab
Using tools like agar media, incubators, and microscopes, microbes can be isolated and studied.
This principle supports the development of vaccines, antibiotics, and diagnostics.
Microorganisms Evolve Rapidly
They mutate and adapt quickly, leading to antibiotic resistance (e.g., MRSA, drug-resistant TB).
This principle explains the need for new drug development and rational antibiotic use.
Host-Microbe Interaction Determines Disease
Not all microbes cause disease; host immunity, microbe virulence, and environmental factors determine outcomes.
This principle helps understand pathogenesis and immunology.
2.Immunoglobulin – IgE
Definition
Immunoglobulin E (IgE) is a type of antibody produced by the immune system in response to allergens (e.g., pollen, dust, food allergens). It plays a key role in allergic reactions and defense against parasitic infections.
Structure
IgE is a monomer (single-unit) antibody
Has 2 antigen-binding sites
Present in very low concentration in normal serum
Functions of IgE
Mediates Type I Hypersensitivity (Allergy):
Triggers release of histamine and other chemicals from mast cells and basophils
Causes symptoms like itching, sneezing, bronchoconstriction, and anaphylaxis
Defense Against Parasites
Helps in identifying and destroying helminths (worms) and other large parasites
Activates eosinophils in the immune response
Clinical Importance
High levels of IgE are seen in:
Asthma
Atopic dermatitis
Allergic rhinitis
Parasitic infections
Measured using RAST test or serum IgE levels
Normal Range
< 100 IU/mL (can vary based on age and lab reference)
3.Neisseria meningitids
Neisseria meningitidis (also known as meningococcus) is a Gram-negative diplococcus bacterium that causes bacterial meningitis and meningococcemia, especially in children and young adults. It is a major public health concern due to its potential for outbreaks and rapid progression.
Morphology
Gram-negative, kidney-shaped, diplococci
Non-motile, non-spore forming
Surrounded by a polysaccharide capsule (important for virulence)
Aerobic and oxidase-positive
Epidemiology
Transmitted via respiratory droplets
Most common in crowded places (hostels, military camps)
Carrier state is common (asymptomatic nasopharyngeal carriage)
Pathogenesis
Enters the body through the nasopharynx
Crosses the blood-brain barrier
Causes inflammation of meninges (meningitis)
May enter the bloodstream causing septicemia (meningococcemia)
Clinical Manifestations
Fever, headache, nuchal rigidity (neck stiffness)
Photophobia, vomiting, altered consciousness
Purpuric rash, hypotension in meningococcemia
May lead to coma and death if untreated
Diagnosis
CSF analysis: cloudy CSF, ↑WBC, ↓glucose, ↑protein
Gram stain: Gram-negative diplococci in CSF
Culture: Grows on chocolate agar or Thayer-Martin medium
PCR and antigen detection also used
Treatment
Immediate IV antibiotics
Ceftriaxone or Penicillin G
Supportive care: fluids, oxygen, anticonvulsants (if needed)
4.Human Immunodeficiency virus (HIV)
Definition
HIV (Human Immunodeficiency Virus) is a retrovirus that attacks and gradually weakens the human immune system, especially CD4+ T lymphocytes (T-helper cells). If untreated, HIV can lead to AIDS (Acquired Immunodeficiency Syndrome).
Causative Agent
Retrovirus belonging to the Lentivirus group
Two main types
HIV-1 – more common and widespread
HIV-2 – less infectious, mostly found in West Africa
Mode of Transmission
Unprotected sexual contact with an infected person
Blood transfusion with contaminated blood
Sharing of needles/syringes (IV drug use)
Mother to child (during pregnancy, childbirth, or breastfeeding)
Organ or tissue transplantation
Pathophysiology
HIV binds to CD4 receptors on T-helper cells
Enters the cell and uses reverse transcriptase to convert its RNA to DNA
Integrates into the host genome and replicates
Gradually destroys immune cells, leading to immune suppression
Clinical Manifestations
Initially : Fever, sore throat, fatigue (acute retroviral syndrome)
Later : Weight loss, chronic diarrhea, prolonged fever
Opportunistic infections : Tuberculosis, Candidiasis, Pneumocystis pneumonia
Final stage : AIDS
Diagnosis
History collection
Physical examination
ELISA (Enzyme-Linked Immunosorbent Assay) – screening
Western Blot / PCR – confirmation
CD4 count & Viral load test – monitoring progression
Treatment
Antiretroviral Therapy (ART)
Combination of drugs such as :
Zidovudine (AZT)
Lamivudine
Efavirenz
ART doesn’t cure HIV but suppresses viral replication and boosts immunity.
Q.4 Answer any three very short questions.(06)
1. What are gram Negative bacteria?
Gram-negative bacteria are a group of bacteria that do not retain the crystal violet stain during the Gram staining process and appear pink or red under the microscope due to the safranin counterstain. It Have a thin peptidoglycan layer. It often more resistant to antibiotics than Gram-positive bacteria
Examples
Escherichia coli (E. coli) – causes urinary tract infections
Neisseria gonorrhoeae – causes gonorrhea
2. Define antigen
An antigen is any foreign substance (usually a protein or polysaccharide) that enters the body and stimulates the immune system to produce a response, especially the production of antibodies.
Examples of Antigens
Bacteria, viruses, or parts of them
Toxins, pollen, or foreign tissues (like in transplants)
3. Define pathogenic microorganism and give two examples
A pathogenic microorganism is a disease-causing microbe (such as bacteria, viruses, fungi, or parasites) that can invade the body and cause illness.
Examples
Mycobacterium tuberculosis – causes Tuberculosis
Plasmodium falciparum – causes Malaria
4. What is hypersensitivity reaction?
A hypersensitivity reaction is an abnormal and exaggerated immune response to a foreign substance (called an antigen or allergen), which can lead to tissue damage, inflammation, or other harmful effects. It occurs when the body’s immune system overreacts to substances that are normally harmless (e.g., pollen, certain drugs, food proteins).
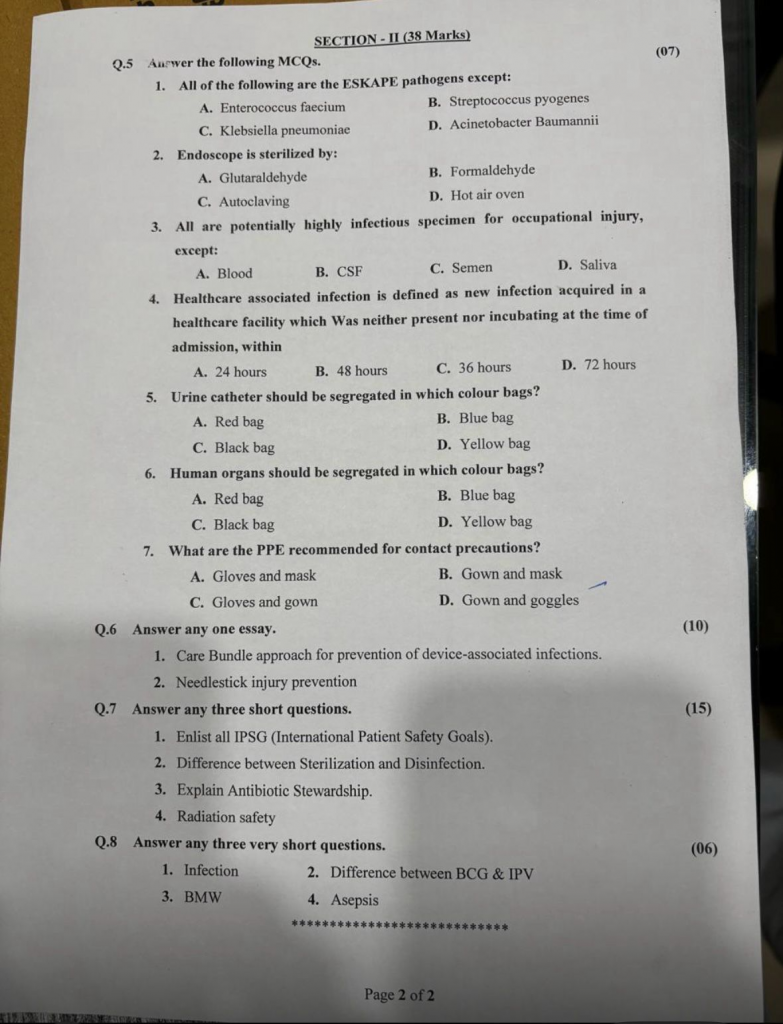
SECTION-II (38 Marks)
Q.5 Aurwer the following MCQs. (07)
1. All of the following are the ESKAPE pathogens except:
A. Enterococcus faecium
B. Streptococcus pyogenes
C. Klebsiella pneumoniae
D. Acinetobacter Baumannii
2. Endoscope is sterilized by:
A. Glutaraldehyde
B. Formaldehyde
C. Autoclaving
D. Hot air oven
3. All are potentially highly infectious specimen for occupational injury, except:
A. Blood
B. CSF
C. Semen
D. Saliva
4. Healthcare associated infection is defined as new infection acquired in a healthcare facility which Was neither present nor incubating at the time of admission, within
A. 24 hours
B. 48 hours
C. 36 hours
D. 72 hours
5. Urine catheter should be segregated in which colour bags?
A. Red bag
B. Blue bag
C. Black bag
D. Yellow bag
6. Human organs should be segregated in which colour bags?
A. Red bag
B. Blue bag
C. Black bag
D. Yellow bag
7. What are the PPE recommended for contact precautions?
A. Gloves and mask
B. Gown and mask
C. Gloves and gown
D. Gown and goggles
Q.6 Answer any one essay. (10)
1. Care Bundle approach for prevention of device-associated infections
Definition
A care bundle is a set of 3–5 evidence-based practices that, when performed collectively and consistently, lead to better outcomes than when performed individually.
Care bundles are particularly useful in preventing device-associated infections such as:
Ventilator-Associated Pneumonia (VAP)
Central Line-Associated Bloodstream Infection (CLABSI)
Catheter-Associated Urinary Tract Infection (CAUTI)
VAP Bundle (Ventilator-Associated Pneumonia Prevention)
Elements of the VAP Care Bundle
Elevate the head of bed to 30–45°
Daily sedation assessment and spontaneous breathing trial
Peptic ulcer disease (PUD) prophylaxis
Deep vein thrombosis (DVT) prophylaxis
Daily oral care with chlorhexidine
CLABSI Bundle (Central Line Infection Prevention)
Elements of the CLABSI Care Bundle
Hand hygiene before catheter insertion
Use of full-barrier precautions during insertion
Skin cleaning with 2% chlorhexidine
Avoid femoral vein site if possible
Daily review of line necessity and prompt removal
CAUTI Bundle (Catheter-Associated UTI Prevention)
Elements of the CAUTI Care Bundle
Insert catheter only when medically necessary
Use aseptic technique during insertion
Maintain a closed drainage system
Keep catheter and tubing unobstructed
Perform daily review and remove catheter promptly
Universal Principles Across All Bundles
Hand hygiene is essential before and after handling any device.
Staff training on bundle components.
Use of checklists to ensure compliance.
Regular audits and feedback to improve adherence.
Team approach involving nurses, doctors, and infection control.
Benefits of Care Bundle Approach
✔ Improves patient safety
✔ Decreases hospital-acquired infections (HAIs)
✔ Reduces hospital stay and costs
✔ Promotes standardized and quality care
✔ Encourages team-based accountability
2. Needle stick injury prevention
Definition
Needle stick injury (NSI) refers to an accidental puncture wound from a needle or other sharp object that may expose healthcare workers to bloodborne pathogens such as HIV, Hepatitis B (HBV), and Hepatitis C (HCV).
Risks of Needle Stick Injury
Exposure to infected blood or body fluids
Transmission of HIV, HBV, HCV
Physical trauma or emotional stress
Potential legal or occupational health issues
Goals of NSI Prevention
To protect healthcare workers from infection.
To ensure safe practices during handling of needles/sharps.
To promote a culture of safety in clinical settings.
Preventive Measures for Needle Stick Injury
Engineering Controls
Use of safety-engineered devices (e.g., retractable needles, needleless IV systems).
Proper sharp disposal containers (puncture-proof, labeled, easily accessible).
Work Practice Controls
Never recap needles after use. If necessary, use one-hand scoop technique.
Do not bend or break needles before disposal.
Dispose of sharps immediately after use in designated sharps container.
Avoid passing sharps hand-to-hand; use a tray.
Personal Protective Equipment (PPE)
Always wear gloves when handling blood or body fluids.
Use goggles, gowns, and face shields as needed.
Education and Training
Regular training on infection control and needle safety.
Awareness about risks, safe disposal, and post-exposure protocols.
Administrative Controls
Develop and implement needle safety policies.
Conduct needle injury surveillance and reporting.
Encourage a no-blame reporting culture.
Post-Exposure Protocol (If Injury Occurs)
Wash area immediately with soap and water.
Report the incident to infection control or supervisor.
Follow post-exposure prophylaxis (PEP) protocols for HIV, HBV, or HCV.
Document the injury and get medical evaluation.
Attend follow-up testing as advised (e.g., 6 weeks, 3 months, 6 months).
Post-Injury Action (If NSI Occurs)
Wash the site with soap and water.
Report immediately to supervisor or infection control officer.
Seek medical evaluation and start PEP if indicated.
Document the incident and monitor serology.
Q.7 Answer any three short questions. (15)
1.Enlist all IPSG (International Patient Safety Goals)
These goals are designed to promote specific improvements in patient safety in healthcare settings around the world.
List of IPSG (Total 6 Goals)
IPSG 1: Identify patients correctly
➤ Use at least two identifiers (e.g., name and date of birth) to ensure each patient receives the correct treatment.
IPSG 2: Improve effective communication
➤ Ensure correct and timely communication among caregivers, especially during handovers and reporting critical test results.
IPSG 3: Improve the safety of high-alert medications
➤ Ensure proper labeling, storage, and administration of high-risk drugs like insulin, anticoagulants, and chemotherapy agents.
IPSG 4: Ensure correct-site, correct-procedure, correct-patient surgery
➤ Use checklists, marking the surgical site, and performing a “time-out” before surgery to prevent errors.
IPSG 5: Reduce the risk of health care–associated infections
➤ Follow hand hygiene protocols, sterilization procedures, and use of infection prevention guidelines.
IPSG 6: Reduce the risk of patient harm resulting from falls
➤ Implement fall risk assessments, patient education, and safety interventions to prevent injury.
2.Difference between Sterilization and Disinfection
| Point of Comparison | Sterilization | Disinfection |
|---|---|---|
| Definition | A process that destroys or eliminates all forms of microbial life, including bacterial spores. | A process that eliminates most pathogenic microorganisms, except bacterial spores, on inanimate objects. |
| Purpose | To make an object completely free from all microorganisms. | To reduce the number of harmful microorganisms to a safe level. |
| Level of Control | High-level control – destroys all microbes. | Intermediate to low-level control – does not kill all microbes. |
| Methods Used | Autoclaving, dry heat, ethylene oxide gas, radiation, filtration. | Chemical disinfectants (phenol, alcohol, chlorine), pasteurization, boiling. |
| Used For | Surgical instruments, needles, catheters, culture media. | Floors, walls, thermometers, stethoscopes, furniture. |
| Kills Spores? | Yes | No (generally) |
3.Explain Antibiotic Stewardship
Definition
Antibiotic stewardship is a coordinated program that promotes the appropriate use of antibiotics, improves patient outcomes, reduces microbial resistance, and decreases the spread of antibiotic-resistant infections.
Objectives of Antibiotic Stewardship
Ensure right antibiotic is used for right infection.
Use antibiotics for correct duration and dose.
Prevent the overuse and misuse of antibiotics.
Reduce antimicrobial resistance (AMR).
Improve clinical outcomes and minimize side effects.
Key Components of an Antibiotic Stewardship Program (ASP)
Leadership commitment – Support from hospital administration.
Accountability – A lead physician or pharmacist is responsible for program outcomes.
Drug expertise – Involvement of clinical pharmacists.
Actions – Guidelines for prescribing and reviewing antibiotics.
Tracking – Monitor antibiotic use and resistance patterns.
Reporting – Regular feedback to prescribers.
Education – Training healthcare providers on antibiotic use and resistance.
Importance in Healthcare
Fights the global threat of antimicrobial resistance (AMR).
Protects the effectiveness of existing antibiotics.
Enhances patient safety by reducing drug toxicity and superinfections (e.g., Clostridium difficile).
Reduces hospital costs and stay duration.
4.Radiation safety
Definition
Radiation safety refers to the precautions and protective measures taken to reduce exposure to ionizing radiation, such as X-rays, gamma rays, and radioactive substances, to protect health and prevent radiation-related illnesses.
Key Principles of Radiation Safety
This principle helps in minimizing radiation risks.
Time
Reduce the time spent near radiation sources.
Less time = Less exposure.
Distance
Increase distance from the source.
Radiation intensity decreases rapidly with distance.
Shielding
Use protective materials (e.g., lead aprons, lead shields, walls).
Prevents or reduces radiation from reaching the body.
Radiation Safety Measures in Healthcare Settings
Use lowest effective dose of radiation.
Use personal dosimeters to monitor exposure.
Limit unnecessary staff and patient exposure.
Post warning signs in radiation zones.
Maintain and calibrate radiation equipment regularly.
Train staff in radiation protection protocols.
Use PPE like lead aprons, thyroid shields, and gloves.
Regulatory Guidelines
Follow national bodies like AERB (Atomic Energy Regulatory Board).
Adhere to international standards from IAEA or ICRP.
Importance
Prevents radiation-induced conditions : Skin burns, cancer, infertility, fetal defects, etc.
Ensures patient and healthcare worker safety.
Q.8 Answer any three very short questions (6) marks
1.Infection
Infection is the invasion and multiplication of pathogenic microorganisms such as bacteria, viruses, fungi, or parasites in the body tissues, which may lead to local or systemic illness.
Infection is the invasion, multiplication, and survival of pathogenic microorganisms such as bacteria, viruses, fungi, or parasites within the body, which may cause local or systemic tissue damage and disease.
2. BMW
Biomedical Waste (BMW) is any waste that is generated during the diagnosis, treatment, or immunization of human beings or animals, or during research activities or production of biologicals. It includes infectious materials, sharps, body parts, blood-soaked items, and laboratory waste.
Example : Used syringes, soiled dressings, human tissues, etc.
3. Difference between BCG & IPV
| Point | BCG Vaccine | IPV Vaccine |
|---|---|---|
| Full Form | Bacillus Calmette–Guérin | Inactivated Poliovirus Vaccine |
| Prevents | Tuberculosis (TB) | Poliomyelitis (Polio) |
| Type of Vaccine | Live attenuated bacterial vaccine | Inactivated (killed) viral vaccine |
| Route of Administration | Intradermal (usually left upper arm) | Intramuscular or subcutaneous injection |
| Given At | Birth (within 24 hours) | 6, 10, 14 weeks (as part of immunization) |
4. Asepsis
Asepsis is the absence of pathogenic microorganisms in a given environment, especially during medical or surgical procedures, to prevent infection. It refers to practices and procedures used to maintain sterility and avoid contamination by harmful microbes.
Example : Sterilization of surgical instruments, hand hygiene, wearing gloves and masks.