Physio-Unit-8-Musculoskeletal system
🦴 Bones – Physiology and Functions
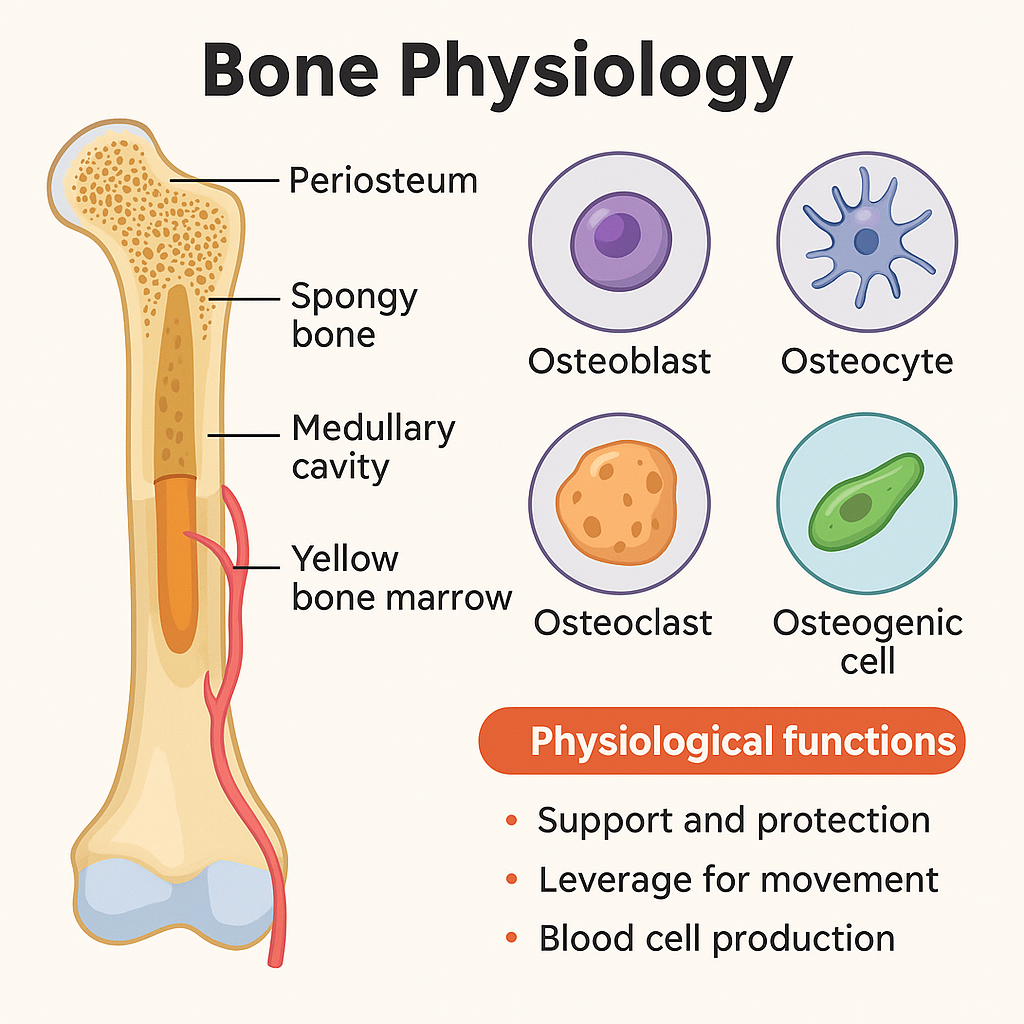
The human skeletal system comprises 206 bones, each serving as a vital component of a dynamic organ system. Bone is a specialized connective tissue that is continuously remodeled and responsive to metabolic, mechanical, and hormonal stimuli.
🧬 I. Composition of Bone Tissue
Bone is composed of:
- Cells: osteoblasts, osteocytes, osteoclasts
- Extracellular matrix: collagen fibers (mostly type I) and ground substance
- Mineral content: primarily calcium phosphate in the form of hydroxyapatite [Ca₁₀(PO₄)₆(OH)₂]
🔹 Bone Cell Types:
| Cell | Function |
|---|---|
| Osteoblasts | Bone-forming cells that secrete osteoid |
| Osteocytes | Mature osteoblasts embedded in bone matrix |
| Osteoclasts | Bone-resorbing cells that degrade bone tissue |
| Osteoprogenitor | Stem cells that differentiate into osteoblasts |
📚 II. Key Functions of Bones
1. Support
- Provides a rigid framework that supports the body and cradles soft organs.
- The axial skeleton holds the central axis; the appendicular skeleton anchors limbs.
2. Protection
- Encases and shields vital structures:
- Skull protects the brain
- Vertebrae protect the spinal cord
- Ribs protect the heart and lungs
3. Movement
- Bones act as levers for muscle contraction.
- Joints between bones allow controlled movement.
- Muscle attachment sites (tendons) anchor to bones.
4. Mineral Storage
- Major reservoir for calcium and phosphorus.
- Maintains serum calcium through hormonal regulation:
- Parathyroid hormone (PTH) increases bone resorption.
- Calcitonin inhibits resorption.
- Vitamin D promotes calcium absorption and mineralization.
5. Hematopoiesis
- Occurs in red bone marrow (found in flat bones and ends of long bones).
- Produces:
- Red blood cells (RBCs)
- White blood cells (WBCs)
- Platelets
6. Fat Storage
- Yellow bone marrow stores triglycerides, which serve as an energy source.
- Found in the medullary cavity of long bones.
7. Endocrine Function
- Bones produce osteocalcin, a hormone that:
- Stimulates insulin secretion
- Enhances sensitivity to insulin
- Regulates fat deposition
🔁 III. Bone Remodeling and Physiology
Bone is not static—it undergoes constant remodeling through a balance of:
- Bone deposition by osteoblasts
- Bone resorption by osteoclasts
Phases of Remodeling:
- Activation – Pre-osteoclast recruitment
- Resorption – Osteoclasts break down bone matrix
- Reversal – Mononuclear cells prepare bone surface
- Formation – Osteoblasts build new bone
- Quiescence – Bone returns to resting state
Influencing Factors:
- Hormones: PTH, estrogen, testosterone, calcitonin, vitamin D
- Mechanical stress: Weight-bearing activities stimulate bone formation
- Nutritional factors: Calcium, phosphorus, and vitamin D are critical
🧾 IV. Summary Table – Major Functions of Bones
| Function | Description |
|---|---|
| Support | Framework for body shape and posture |
| Protection | Shields internal organs from mechanical injury |
| Movement | Acts as levers for muscles; enables locomotion |
| Mineral storage | Stores Ca²⁺ and PO₄³⁻; regulates blood mineral levels |
| Hematopoiesis | Produces blood cells in red marrow |
| Fat storage | Stores lipids in yellow marrow |
| Endocrine function | Produces osteocalcin for glucose metabolism and hormone regulation |
🩺 V. Clinical Relevance in Nursing and Medicine
| Condition | Relevance |
|---|---|
| Osteoporosis | Bone resorption exceeds formation → fracture risk |
| Fractures | Impaired structural integrity; requires immobilization |
| Rickets/Osteomalacia | Vitamin D deficiency affects mineralization |
| Paget’s Disease | Disorganized bone remodeling |
| Bone cancer | Can arise from or spread to bone tissue |
| Hyperparathyroidism | Causes bone resorption and calcium release |
Bones are multifunctional, living tissues that provide mechanical strength, mineral homeostasis, hematopoietic support, and endocrine signaling. Understanding their physiology is essential for clinical assessments, orthopedic care, and holistic nursing interventions.
🧠 Movements of Bones – Physiology of Axial and Appendicular Skeleton
The human skeleton is divided into two main parts:
- Axial Skeleton: Skull, vertebral column, ribs, and sternum
- Appendicular Skeleton: Limbs and girdles (shoulder and pelvic girdles)
These components work together through joints and muscular attachments to facilitate a wide range of body movements, support posture, and maintain balance.
🦴 I. Movements of the Axial Skeleton
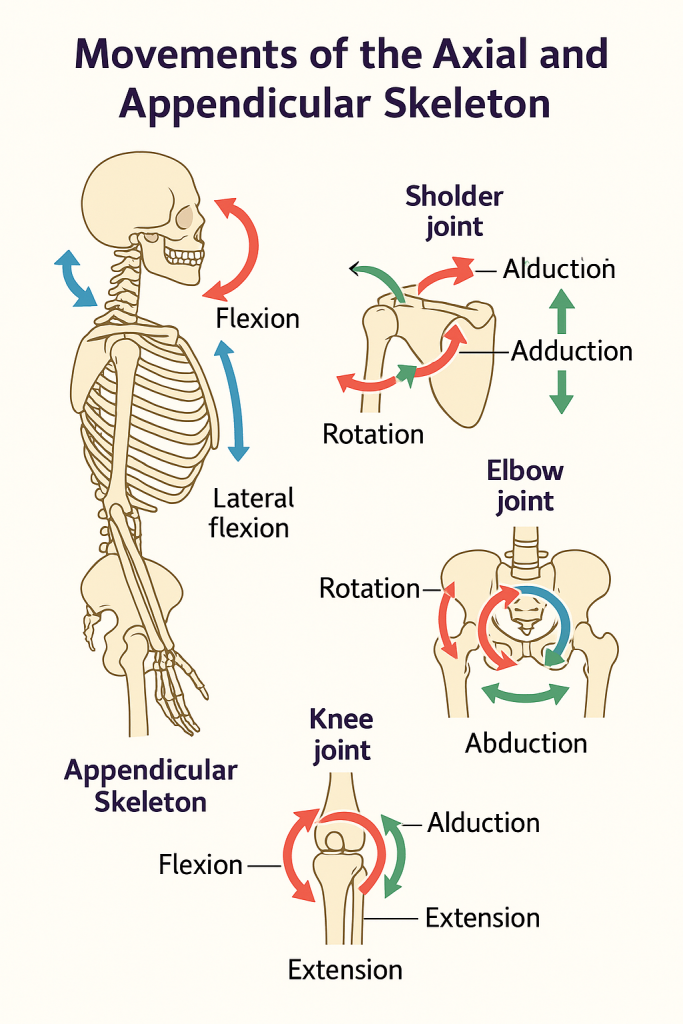
The axial skeleton provides support and protection while enabling limited but essential movements—mainly flexion, extension, rotation, and lateral bending.
🔹 1. Skull
- Mostly immobile, except:
- Temporomandibular joint (TMJ): allows jaw elevation, depression, protrusion, retraction, and side-to-side movement.
🔹 2. Vertebral Column (Spine)
| Region | Movements |
|---|---|
| Cervical | Flexion, extension, lateral flexion, rotation (highly mobile) |
| Thoracic | Rotation and lateral flexion (limited due to rib attachment) |
| Lumbar | Flexion, extension, lateral flexion (no rotation) |
| Sacrum/Coccyx | Fused; minimal movement |
Intervertebral discs, facet joints, and ligaments support spinal movement.
🔹 3. Thoracic Cage (Ribs and Sternum)
- Allows expansion and contraction during respiration.
- Movements:
- Pump handle motion (elevation of upper ribs)
- Bucket handle motion (lateral expansion of lower ribs)
🦿 II. Movements of the Appendicular Skeleton
The appendicular skeleton is primarily responsible for locomotion and manipulation of the environment. Movements are classified by the type of synovial joints involved and their anatomical planes.
🔸 1. Shoulder Joint (Glenohumeral Joint)
- Ball-and-socket joint; most mobile joint
- Movements:
- Flexion / Extension
- Abduction / Adduction
- Medial / Lateral rotation
- Circumduction
🔸 2. Elbow Joint
- Hinge joint
- Movements:
- Flexion / Extension
- Pronation / Supination (at radioulnar joint)
🔸 3. Wrist and Hand
- Wrist (radiocarpal joint): Flexion, extension, radial/ulnar deviation
- Metacarpophalangeal (MCP): Flexion, extension, abduction, adduction
- Interphalangeal (IP): Flexion, extension
🔸 4. Hip Joint
- Ball-and-socket joint
- Movements:
- Flexion / Extension
- Abduction / Adduction
- Medial / Lateral rotation
- Circumduction
🔸 5. Knee Joint
- Modified hinge joint
- Movements:
- Flexion / Extension
- Slight medial/lateral rotation when flexed
🔸 6. Ankle and Foot
- Ankle (talocrural joint): Dorsiflexion, plantarflexion
- Subtalar joint: Inversion, eversion
- Toes: Flexion, extension, abduction, adduction
🧬 III. Types of Movements Across Joints
| Movement | Description |
|---|---|
| Flexion | Decreasing the angle between bones (e.g., bending the elbow) |
| Extension | Increasing the angle (e.g., straightening the knee) |
| Abduction | Moving away from midline (e.g., lifting arm sideways) |
| Adduction | Moving toward the midline |
| Rotation | Movement around an axis (e.g., head turning left/right) |
| Circumduction | Circular movement combining flexion, extension, abduction, adduction |
| Supination | Turning palm upward |
| Pronation | Turning palm downward |
| Dorsiflexion | Lifting foot upward at ankle |
| Plantarflexion | Pointing toes downward |
🩺 IV. Clinical and Nursing Relevance
| Condition | Implication |
|---|---|
| Arthritis | Limits joint mobility and causes pain |
| Fractures | Restricts movement; requires immobilization and rehabilitation |
| Stroke/Paralysis | Impairs voluntary movement in appendicular skeleton |
| Post-op orthopedic care | Nurses must assist with mobility, support, and range of motion exercises |
| Musculoskeletal exams | Include assessing symmetry, range of motion, and functional movement |
The physiology of skeletal movement involves a coordinated system of bones, joints, and muscles. The axial skeleton stabilizes and protects vital structures while allowing posture and flexibility. The appendicular skeleton provides a wide range of motion for locomotion and task performance. Understanding these movements aids in assessment, rehabilitation, and patient education in nursing care.
🦴 Bone Healing
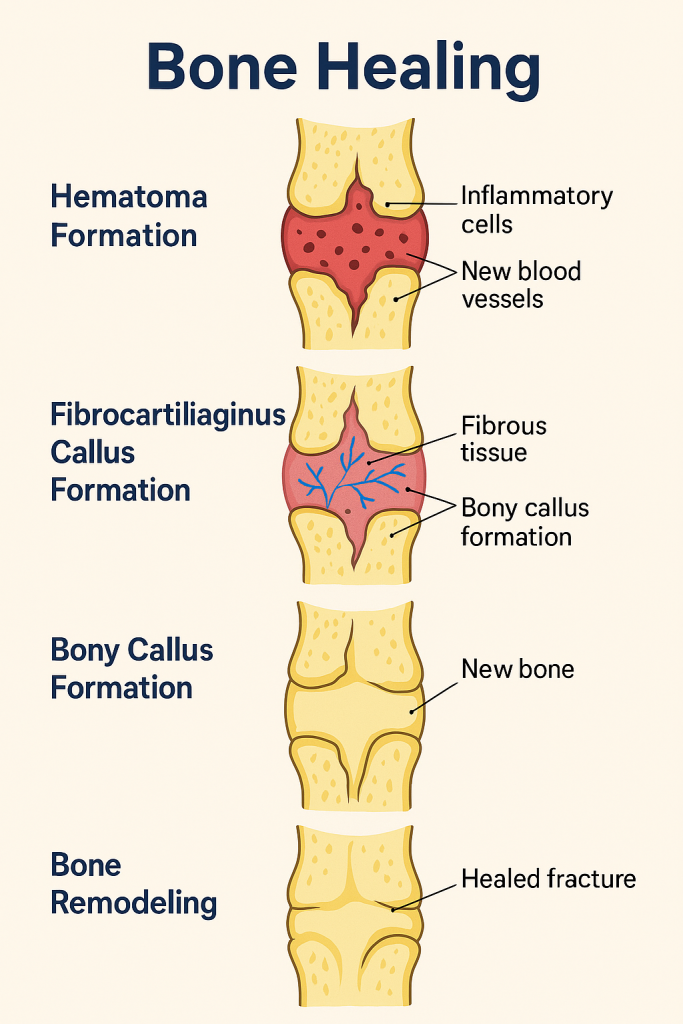
Bone healing is a natural regenerative process that occurs after a fracture or surgical bone injury, involving a complex series of biological events. Unlike most tissues, bone heals by regeneration, not scar formation. This process restores the bone’s original strength and structure through cellular, vascular, and biochemical activities.
🔬 I. Phases of Bone Healing
Bone healing occurs in four overlapping but distinct phases:
🔹 1. Hematoma Formation (Inflammatory Phase)
Timeframe: First 1–5 days after fracture
- Blood vessels rupture → hematoma forms at fracture site
- Platelets release cytokines and growth factors (e.g., PDGF, TGF-β)
- Inflammatory response recruits:
- Neutrophils (early response)
- Macrophages and monocytes (clean up debris)
- Prepares the site for new tissue formation
🔸 Clinical relevance: Swelling, warmth, and pain are prominent.
🔹 2. Soft Callus Formation (Reparative Phase – Fibrocartilaginous Callus)
Timeframe: Days 5–21
- Fibroblasts and chondroblasts migrate to the site
- Formation of granulation tissue followed by:
- Fibrous tissue
- Cartilage matrix (soft callus)
- Angiogenesis restores blood supply
- Endochondral ossification begins
🔸 Clinical relevance: Immobilization is crucial; callus is not yet calcified.
🔹 3. Hard Callus Formation (Bony Callus Formation)
Timeframe: 3–6 weeks
- Osteoblasts replace the cartilage with woven bone
- Cartilage undergoes endochondral ossification
- Soft callus is mineralized → hard (bony) callus
- Early bone is disorganized (woven) and not as strong
🔸 Clinical relevance: Fracture site begins to regain strength but requires continued protection.
🔹 4. Bone Remodeling (Maturation Phase)
Timeframe: Several months (6 weeks to several years)
- Woven bone is replaced by lamellar bone
- Osteoclasts resorb unnecessary bone
- Osteoblasts lay down new bone
- Bone is reshaped to its original structure in response to mechanical stress (Wolff’s law)
🔸 Clinical relevance: Return to full activity is guided by radiographic evidence of healing.
🧬 II. Cellular Players in Bone Healing
| Cell Type | Role |
|---|---|
| Osteoblasts | Bone formation and mineralization |
| Osteoclasts | Bone resorption and remodeling |
| Chondroblasts | Cartilage production during soft callus formation |
| Fibroblasts | Produce collagen and extracellular matrix |
| Endothelial cells | Angiogenesis and blood vessel regeneration |
| Stem cells (MSCs) | Differentiate into chondroblasts and osteoblasts |
🧾 III. Factors Affecting Bone Healing
✅ Positive Influences:
- Good blood supply
- Adequate nutrition (protein, calcium, vitamin D)
- Proper immobilization
- Early but appropriate weight-bearing (stimulates remodeling)
❌ Negative Influences:
- Smoking
- Poor nutrition
- Diabetes mellitus
- Infection
- Use of NSAIDs or corticosteroids (inhibit inflammation and bone repair)
- Inadequate immobilization or excessive motion
🦠 IV. Complications in Bone Healing
| Complication | Explanation |
|---|---|
| Delayed union | Healing takes longer than expected |
| Non-union | Failure of healing; fibrous tissue forms instead |
| Malunion | Bone heals in an abnormal position |
| Infection (osteomyelitis) | Especially in open fractures |
| Pseudoarthrosis | Formation of false joint due to non-union |
📚 V. Bone Healing Phases
| Phase | Key Events |
|---|---|
| Hematoma | Blood clot, inflammation, cytokine release |
| Soft Callus | Granulation tissue, fibrocartilage formation, neovascularization |
| Hard Callus | Osteoblast activity, cartilage replaced by woven bone |
| Remodeling | Woven bone replaced by lamellar bone, restores shape and strength |
🩺 VI. Clinical and Nursing Implications
- Monitor for signs of infection and neurovascular compromise
- Ensure immobilization compliance
- Encourage diet rich in calcium, protein, and vitamin D
- Educate on smoking cessation
- Support rehabilitation and physiotherapy as healing progresses
- Assist with pain management and mobility
The physiology of bone healing is a multistep, highly coordinated process involving cellular activity, angiogenesis, mineralization, and remodeling. A solid understanding of these phases helps healthcare providers optimize care, prevent complications, and support effective recovery in patients with bone injuries.
🦴 Joints: A Detailed Academic Insight into Structure, Classification, and Function
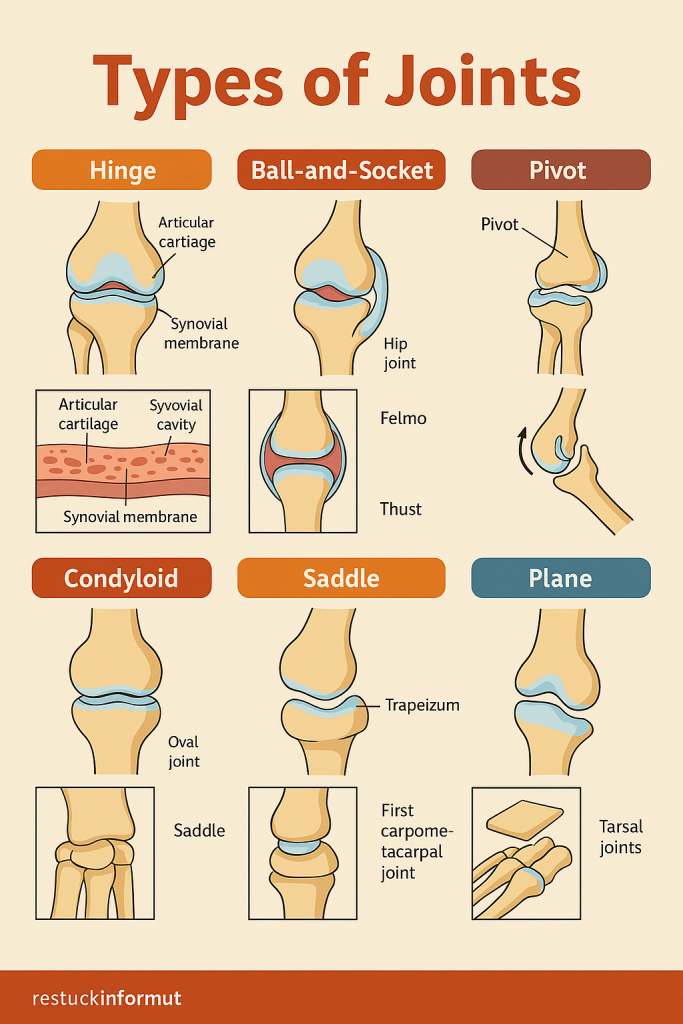
Joints, or articulations, are anatomical structures where two or more bones meet. They are essential for mobility, structural integrity, and force transmission in the human body. The characteristics of a joint—its structure, connective tissues, and surrounding musculature—determine the range and direction of motion it can perform. Understanding joint physiology is critical in healthcare fields for assessing movement disorders, managing injuries, and supporting rehabilitative care.
Structural and Functional Classification of Joints
Joints are commonly classified in two primary ways: structurally, based on the physical nature of the connection between bones, and functionally, based on the degree of movement they permit.
Structurally, joints are categorized as:
- Fibrous joints, which are connected by dense fibrous connective tissue. These joints are typically immobile (synarthroses), such as the sutures in the adult skull.
- Cartilaginous joints, where bones are joined by hyaline cartilage or fibrocartilage. These allow limited movement (amphiarthroses) and are exemplified by intervertebral discs and the pubic symphysis.
- Synovial joints, the most common and freely movable type (diarthroses), consist of a joint cavity filled with synovial fluid. This category includes major joints like the knee, shoulder, hip, and wrist.
Functionally, joints are defined by their movement capabilities:
- Synarthroses are immovable joints providing stability (e.g., cranial sutures).
- Amphiarthroses allow slight movement, useful in shock absorption (e.g., vertebral joints).
- Diarthroses, or synovial joints, allow a wide range of motions and are the basis of limb movement.
Anatomy of a Synovial Joint
Synovial joints are highly specialized to permit smooth and controlled movement. They are characterized by several key features:
- Articular cartilage covers the bone ends, providing a smooth, low-friction surface.
- A joint (synovial) cavity is filled with synovial fluid, which lubricates and nourishes the articular surfaces.
- The synovial membrane, which lines the inner capsule, produces this fluid.
- Fibrous joint capsules enclose the entire joint, maintaining its structural integrity.
- Ligaments reinforce the joint, providing mechanical support and limiting excess movement.
- Bursae and tendon sheaths reduce friction between tendons, ligaments, and bones during dynamic movement.
Types of Synovial Joints and Their Movements
Synovial joints are further subclassified based on the shapes of their articulating surfaces and the types of motion they allow. These include:
- Hinge joints, such as the elbow and knee, which allow flexion and extension in one plane.
- Ball-and-socket joints, like the shoulder and hip, permitting multi-directional movement including rotation.
- Pivot joints, exemplified by the atlantoaxial joint (C1–C2), enabling rotational movement.
- Condyloid (ellipsoid) joints, such as the wrist, allow movement in two planes without rotation.
- Saddle joints, like the thumb’s carpometacarpal joint, allow angular movements with greater freedom than condyloid joints.
- Plane (gliding) joints, found in the intercarpal region, enable sliding movements across flat surfaces.
Movements across these joints include flexion, extension, abduction, adduction, rotation, and circumduction, as well as specialized actions such as supination, pronation, dorsiflexion, and plantarflexion at specific joints.
Physiological Importance of Joint Mobility
Joint mobility enables the body to perform coordinated activities such as walking, grasping, turning, and expressing emotions through facial muscles. This mobility is governed by the congruency of joint surfaces, ligamentous constraints, neuromuscular control, and proprioceptive feedback. Additionally, joints absorb mechanical forces during activities, distributing loads across the musculoskeletal system and protecting bones and soft tissues from damage.
Clinical Relevance and Nursing Considerations
Joints are frequently involved in common clinical conditions such as arthritis (inflammatory and degenerative), bursitis, tendinitis, dislocations, and ligament injuries (sprains). In nursing practice, joint assessment is vital for identifying limitations in movement, monitoring post-operative recovery (e.g., after joint replacement), and promoting early mobilization to prevent complications such as joint stiffness or deep vein thrombosis.
Nurses play a central role in:
- Performing range-of-motion (ROM) assessments
- Supporting rehabilitation and physiotherapy routines
- Assisting with joint protection strategies
- Educating patients about joint health, fall prevention, and assistive device use
Joints are complex anatomical and physiological structures that allow for a wide spectrum of human movement and adaptability. Their design reflects the balance between mobility and stability, and their integrity is essential for functional independence. For healthcare professionals, particularly nurses, an in-depth understanding of joint physiology is crucial for delivering holistic care, optimizing mobility, and promoting long-term musculoskeletal health.
🔁 Joint Movements
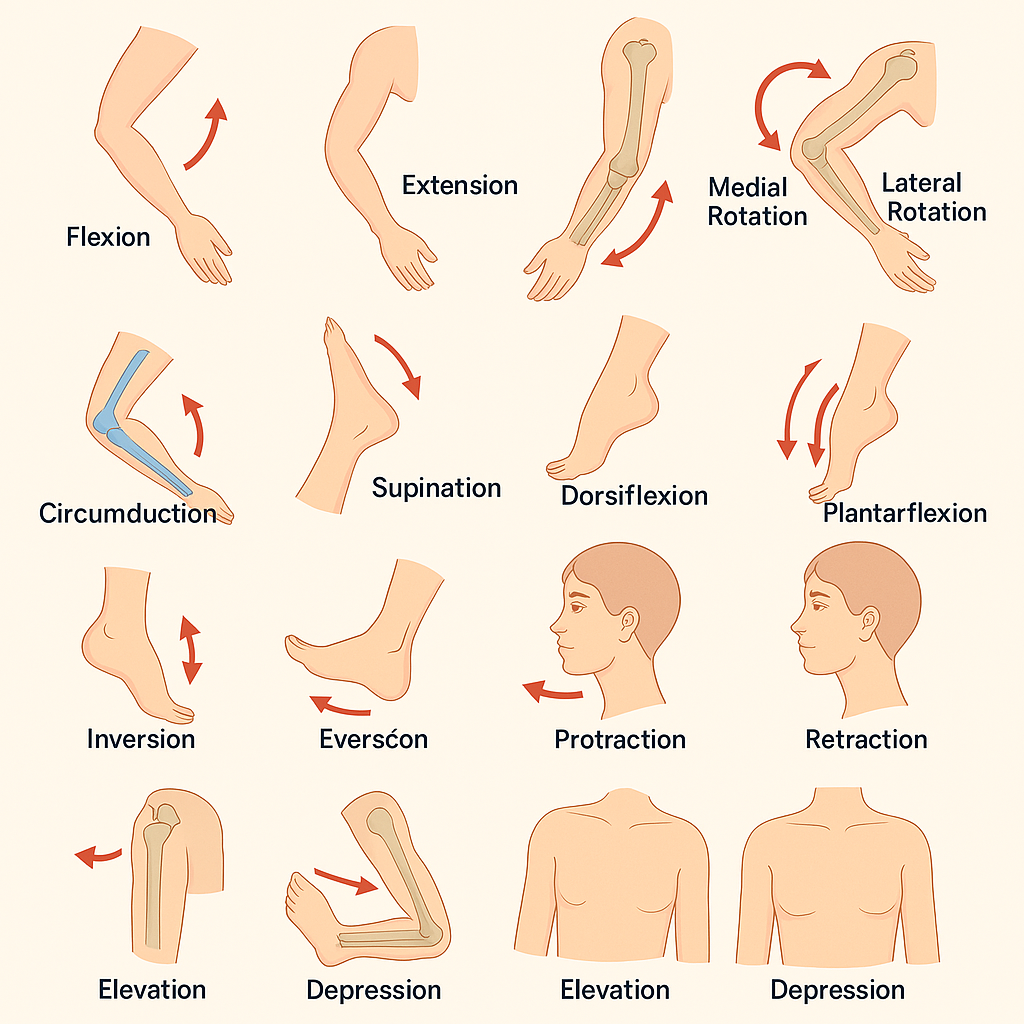
Joint movements refer to the actions performed at the articulations between bones, enabled by muscle contraction, joint structure, and nerve control. The type and range of movement a joint allows is primarily determined by its anatomical classification (e.g., hinge, ball-and-socket, pivot).
🔬 I. Types of Basic Joint Movements
1. Flexion
- Bending movement that decreases the angle between two bones.
- Example: Bending the elbow or knee.
2. Extension
- Movement that increases the angle between two bones.
- Example: Straightening the arm or leg.
3. Hyperextension
- Extension of a joint beyond its normal range.
- Example: Looking up at the ceiling extends the neck past neutral.
4. Abduction
- Movement of a limb away from the midline of the body.
- Example: Raising the arm or leg sideways away from the body.
5. Adduction
- Movement of a limb toward the midline.
- Example: Bringing the arm or leg back to the body.
6. Rotation
- Circular movement around a central axis.
- Can be:
- Medial (internal): Rotation toward the midline
- Lateral (external): Rotation away from the midline
- Example: Turning the head side to side.
7. Circumduction
- A circular movement that combines flexion, extension, abduction, and adduction.
- Example: Moving the arm in a circle at the shoulder.
🔄 II. Special Movements
1. Supination
- Rotation of the forearm so the palm faces upward or forward.
2. Pronation
- Rotation of the forearm so the palm faces downward or backward.
3. Dorsiflexion
- Lifting the foot so the toes point upward (ankle movement).
4. Plantarflexion
- Pointing the toes downward, away from the leg.
5. Inversion
- Turning the sole of the foot inward.
6. Eversion
- Turning the sole of the foot outward.
7. Protraction
- Moving a body part forward in the transverse plane.
- Example: Pushing the jaw outward.
8. Retraction
- Moving a body part backward in the transverse plane.
- Example: Pulling the jaw back.
9. Elevation
- Lifting a body part superiorly.
- Example: Shrugging the shoulders.
10. Depression
- Moving a body part inferiorly.
- Example: Dropping the shoulders after a shrug.
🧠 III. Clinical Importance of Joint Movements
- Assessment of range of motion (ROM) is vital in nursing and physiotherapy.
- Helps in diagnosing musculoskeletal injuries, arthritis, and neurological disorders.
- Used during rehabilitation, exercise programs, and daily care (e.g., passive ROM in bedridden patients).
🦴 Alteration of Joint Diseases
Joint diseases encompass a wide range of pathological conditions that affect the structure and function of joints. These alterations may involve inflammatory, degenerative, autoimmune, infectious, or traumatic processes. The result is often pain, restricted mobility, deformity, and functional limitation, significantly impacting an individual’s quality of life and independence.
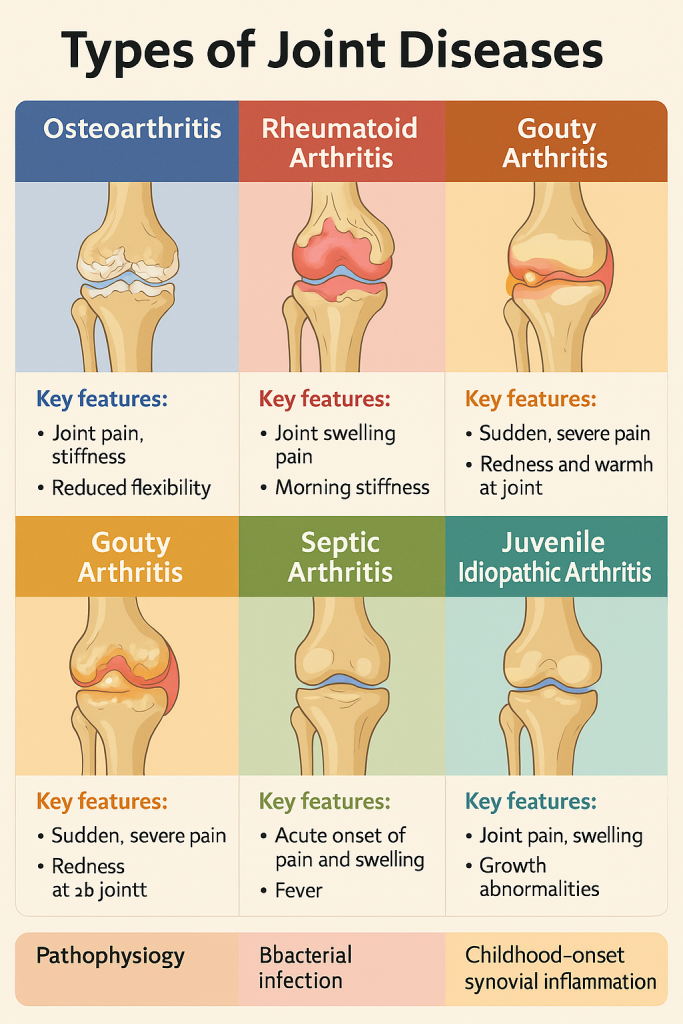
🔬 I. Common Joint Diseases and Pathophysiological Alterations
🔹 1. Osteoarthritis (OA)
Also called: Degenerative Joint Disease
- Pathophysiology:
Progressive wear and tear of articular cartilage → cartilage becomes thin, rough, and eventually erodes. Subchondral bone thickens and forms osteophytes (bone spurs). - Key Alterations:
- Cartilage degeneration
- Joint space narrowing
- Subchondral bone sclerosis
- Synovial inflammation (mild)
- Clinical Features:
- Joint pain (worse with activity)
- Morning stiffness (<30 minutes)
- Crepitus
- Deformities (e.g., Heberden’s and Bouchard’s nodes)
🔹 2. Rheumatoid Arthritis (RA)
Type: Autoimmune, systemic inflammatory disease
- Pathophysiology:
The immune system attacks synovial membrane, leading to chronic synovitis, pannus formation, and erosion of cartilage and bone. - Key Alterations:
- Synovial inflammation and thickening
- Formation of pannus (granulation tissue)
- Cartilage destruction and joint deformity
- Systemic inflammation (fever, fatigue)
- Clinical Features:
- Symmetrical joint involvement (esp. small joints)
- Prolonged morning stiffness (>1 hour)
- Joint swelling, redness, warmth
- Deformities (swan-neck, ulnar deviation)
🔹 3. Gouty Arthritis
- Pathophysiology:
Elevated uric acid levels lead to deposition of monosodium urate crystals in joints, especially in the first metatarsophalangeal (big toe). - Key Alterations:
- Crystal-induced inflammation
- Recurrent attacks of acute joint pain
- Chronic tophaceous deposits in cartilage and soft tissue
- Clinical Features:
- Sudden, severe joint pain
- Redness, swelling, tenderness
- Tophi (chalky urate deposits in chronic cases)
🔹 4. Septic (Infectious) Arthritis
- Pathophysiology:
Bacterial invasion of the joint (usually Staphylococcus aureus) leads to acute purulent synovitis and rapid cartilage destruction. - Key Alterations:
- Synovial membrane infection and inflammation
- Accumulation of purulent exudate
- Joint space destruction if untreated
- Clinical Features:
- Single hot, swollen joint
- Fever and systemic illness
- Emergency: can cause joint destruction in hours to days
🔹 5. Juvenile Idiopathic Arthritis (JIA)
- Pathophysiology:
Autoimmune inflammatory joint disease of unknown cause affecting children under 16. - Alterations:
- Synovial hypertrophy
- Persistent joint inflammation
- Growth disturbances
- Clinical Features:
- Joint stiffness
- Limping
- Eye involvement (uveitis)
🔹 6. Ankylosing Spondylitis
- Pathophysiology:
Chronic inflammation of the axial skeleton, especially the sacroiliac joints and spine. Strongly associated with HLA-B27. - Key Alterations:
- Enthesitis (inflammation at ligament/bone insertion)
- Spinal fusion (“bamboo spine”)
- Loss of spinal flexibility
- Clinical Features:
- Chronic back pain and stiffness (worse in the morning)
- Kyphosis
- Reduced chest expansion
🧠 II. General Pathological Consequences in Joint Diseases
- Synovial inflammation → swelling, increased fluid, pain
- Cartilage erosion → joint space narrowing, friction
- Bone remodeling → sclerosis, osteophytes, deformities
- Ligament and tendon damage → joint instability
- Joint capsule thickening → reduced flexibility
- Ankylosis → abnormal fusion of bones
🧾 III. Summary of Key Alterations in Joint Disease
- Inflammatory conditions (e.g., RA, JIA): Synovitis, immune-mediated destruction
- Degenerative conditions (e.g., OA): Cartilage loss, osteophyte formation
- Crystal deposition disorders (e.g., gout): Crystal-induced synovitis
- Infectious arthritis: Bacterial invasion, pus formation, rapid destruction
- Spondyloarthropathies: Enthesitis, axial involvement, spinal fusion
🩺 IV. Nursing and Clinical Implications
- Assessment of joint pain, swelling, and ROM is crucial for early diagnosis.
- Monitor for systemic symptoms (fever, fatigue) in inflammatory arthritis.
- Support medication compliance (NSAIDs, DMARDs, urate-lowering agents).
- Encourage physiotherapy to maintain mobility and prevent deformity.
- Implement fall prevention and joint protection techniques.
- Educate patients on joint-friendly exercise, weight management, and adaptive devices.
Alterations in joint disease involve complex immune, mechanical, metabolic, or infectious processes that disrupt joint anatomy and function. Prompt recognition, holistic management, and multidisciplinary care are essential to preserve joint mobility, relieve pain, and enhance the patient’s quality of life.
💪 Skeletal Muscles – Properties and Functions
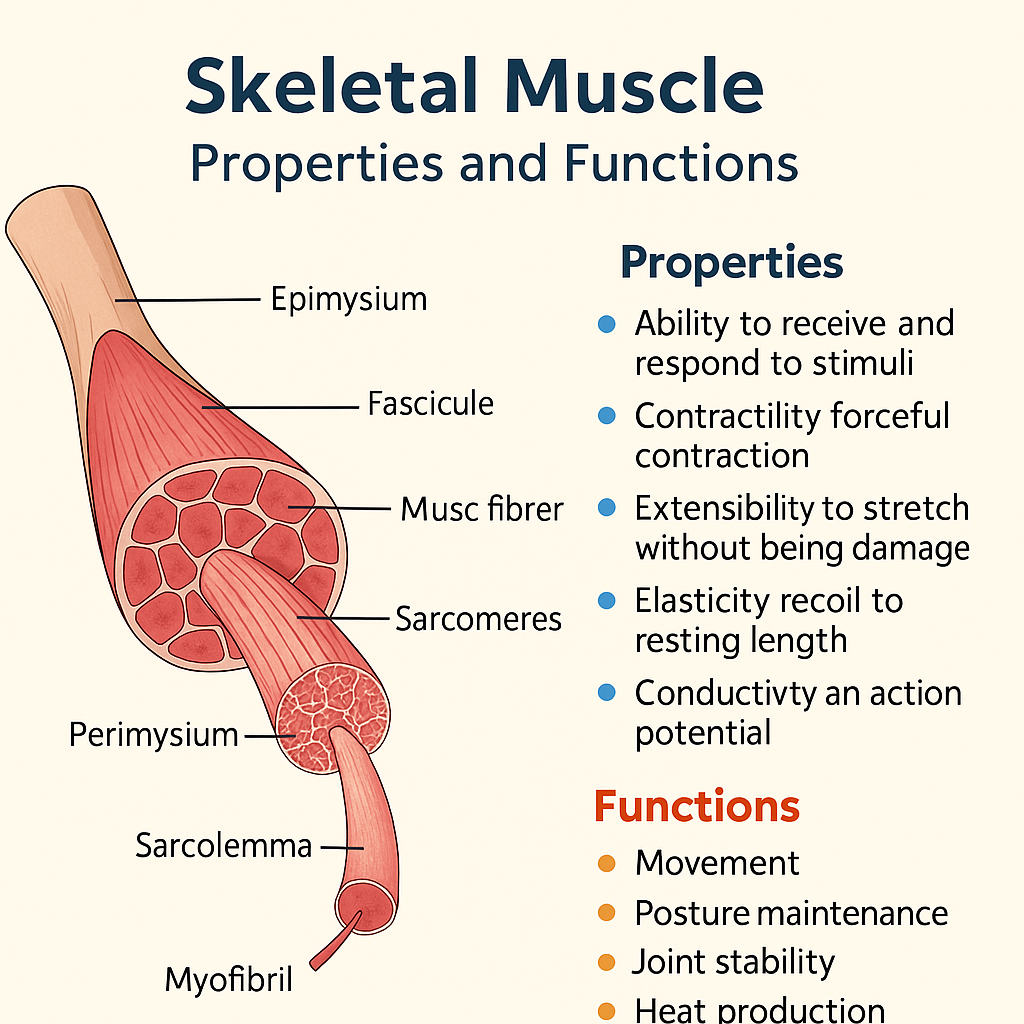
Skeletal muscles are voluntary, striated muscles attached to bones via tendons. They are essential for movement, posture, joint stability, and heat production. These muscles are under somatic nervous system control and exhibit unique physiological properties that enable quick, forceful, and precise contractions.
🔬 I. Properties of Skeletal Muscle (Physiological Characteristics)
Skeletal muscle fibers exhibit the following five fundamental properties:
1. Excitability (Irritability)
- The ability of muscle fibers to respond to stimuli (especially from motor neurons).
- Stimuli generate action potentials through neurotransmitter (acetylcholine) activation at the neuromuscular junction.
- This electrical impulse initiates contraction.
🔍 Clinical relevance: Loss of excitability can lead to paralysis or flaccidity.
2. Contractility
- The muscle’s unique ability to shorten and generate force when stimulated.
- Due to interaction of actin and myosin filaments within sarcomeres (the functional unit of muscle).
- Allows conversion of chemical energy (ATP) into mechanical energy.
🔍 Excessive contractility may cause spasms or cramps.
3. Extensibility
- The ability of a muscle to be stretched or lengthened without damage.
- Muscles can stretch beyond their resting length due to elastic connective tissue and sarcomere arrangement.
🔍 Important for range of motion and flexibility.
4. Elasticity
- The ability of muscle fibers to return to their original shape after contraction or extension.
- Provided by connective tissue elements like titin protein and extracellular matrix.
🔍 Loss of elasticity occurs in fibrosis, aging, or injury.
5. Conductivity
- The capacity to transmit electrical impulses along the sarcolemma and T-tubules.
- Ensures coordinated and synchronized contraction across the entire fiber.
🔍 Disorders of conductivity (e.g., muscular dystrophy) can impair contraction efficiency.
🧬 II. Structural Characteristics of Skeletal Muscle
- Multinucleated and striated appearance
- Comprised of muscle fibers (cells) bundled into fascicles
- Surrounded by:
- Endomysium (around individual fibers)
- Perimysium (around fascicles)
- Epimysium (around entire muscle)
Each muscle fiber contains:
- Myofibrils (with actin and myosin filaments)
- Sarcomeres (contractile units)
- Sarcoplasmic reticulum (stores Ca²⁺)
- T-tubules (transmit action potentials deep into fibers)
🧠 III. Functions of Skeletal Muscle
1. Movement
- Skeletal muscles produce voluntary body movements by pulling on bones.
- Responsible for actions such as walking, writing, speaking, and facial expressions.
2. Posture Maintenance
- Constant low-level contractions (muscle tone) maintain upright posture and stabilize joints.
- Antigravity muscles prevent collapse during standing or sitting.
3. Joint Stability
- Muscles and their tendons reinforce joints, especially those with large ranges of motion (e.g., shoulder).
- Muscle balance is critical for preventing dislocations and injuries.
4. Heat Production (Thermogenesis)
- Muscle contraction generates heat, which is essential for body temperature regulation.
- Up to 85% of body heat can be produced by skeletal muscle activity.
5. Blood and Lymph Circulation Assistance
- Muscle contractions help propel blood and lymph in veins and vessels (muscle pump mechanism), especially in the lower limbs.
6. Respiration
- Diaphragm and intercostal muscles, which are skeletal muscles, facilitate breathing movements.
7. Protection of Internal Organs
- Muscles act as physical shields around vital organs (e.g., abdominal wall protecting intestines).
📚 IV. Summary of Properties and Functions
| Property | Function |
|---|---|
| Excitability | Responds to nervous stimulation |
| Contractility | Generates force for movement |
| Extensibility | Allows muscle to be stretched |
| Elasticity | Returns to resting shape after being stretched or contracted |
| Conductivity | Transmits electrical signals across muscle fibers |
| Function | Role in Physiology |
|---|---|
| Movement | Facilitates locomotion and daily activities |
| Posture maintenance | Maintains body alignment |
| Joint stabilization | Prevents dislocation |
| Heat generation | Maintains body temperature |
| Circulatory support | Aids in venous and lymphatic return |
| Respiratory movement | Enables inhalation and exhalation |
| Organ protection | Shields delicate internal structures |
🩺 Clinical and Nursing Relevance
- Monitoring muscle strength is essential in neurological, orthopedic, and geriatric care.
- Muscle tone and reflexes help detect motor neuron damage or muscular disorders.
- Conditions like myasthenia gravis, muscular dystrophy, spasticity, and atrophy reflect changes in muscle function or properties.
- Rehabilitation nursing emphasizes exercises that improve extensibility, strength, and elasticity.
- Early ambulation and mobility programs post-surgery prevent muscle wasting and circulatory issues.
Skeletal muscles are not just motors of movement; they are complex, responsive tissues with multiple physiological roles crucial for maintaining body mechanics, circulation, posture, and thermal balance. Their unique properties make them capable of dynamic action, endurance, and adaptability, highlighting their central importance in both health and disease.
💪 Mechanism of Skeletal Muscle Contraction
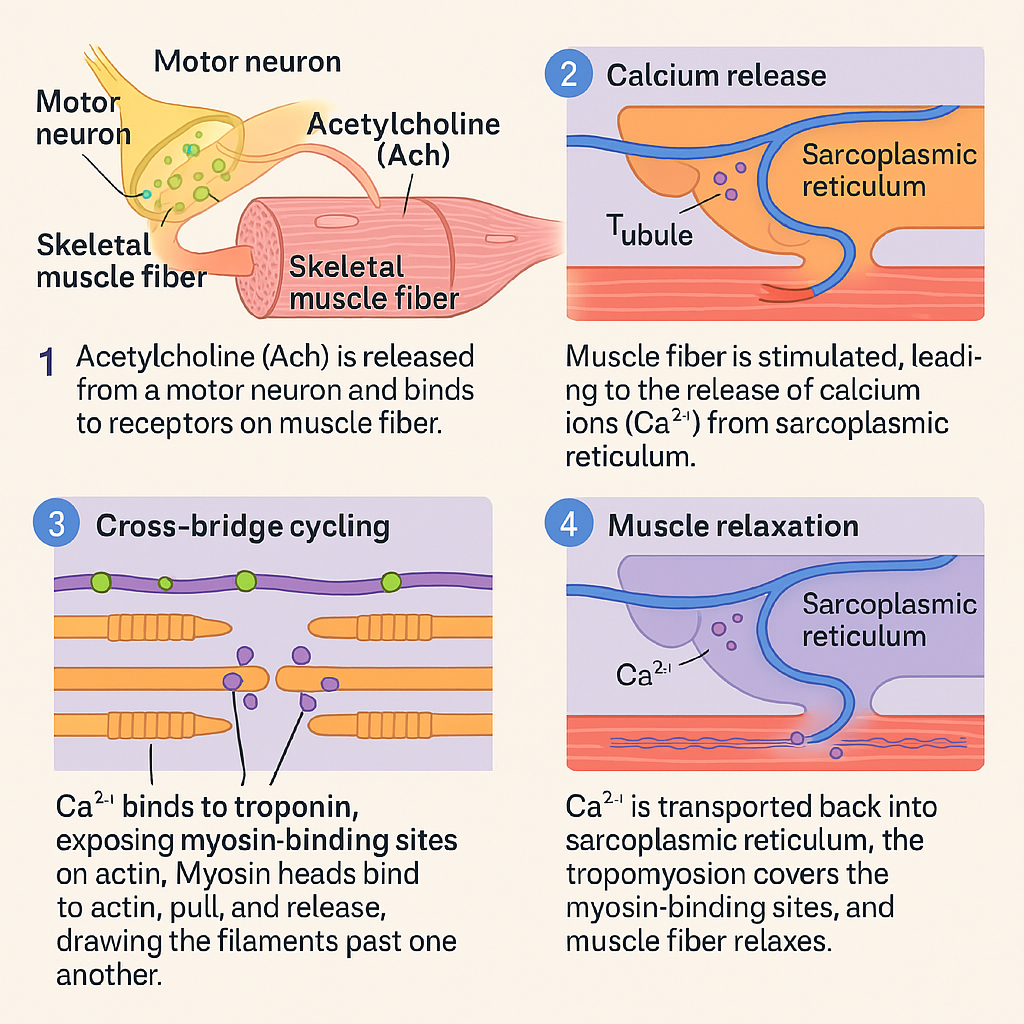
Skeletal muscle contraction is a highly coordinated process that transforms electrical impulses into mechanical force. This process is governed by the sliding filament theory and involves the interaction of actin and myosin filaments within the sarcomere, the functional unit of muscle fibers.
The entire contraction process is regulated by calcium ions, ATP, and neuromuscular signaling. It is classically described in three stages: Excitation, Excitation-Contraction Coupling, and Contraction (Cross-bridge Cycling).
🧠 I. Structural Basis – The Sarcomere
The sarcomere is the repeating unit of myofibrils, bordered by Z lines, and composed of:
- Actin (thin filaments) – contain tropomyosin and troponin
- Myosin (thick filaments) – have heads with ATPase and actin-binding sites
- Z line – anchor point for actin
- A band – dark area (myosin length)
- I band – light area (actin only)
- H zone – myosin only, within the A band
Contraction shortens the sarcomere, but the filaments themselves do not change length.
🔁 II. Steps in Muscle Contraction Mechanism
🔹 1. Excitation – Neuromuscular Transmission
- An action potential reaches the axon terminal of a motor neuron.
- Acetylcholine (ACh) is released into the neuromuscular junction.
- ACh binds to receptors on the sarcolemma (muscle membrane), causing depolarization.
- The action potential spreads across the sarcolemma and into T-tubules.
🔍 Clinical note: Curare, botulinum toxin, and myasthenia gravis affect this stage.
🔹 2. Excitation-Contraction Coupling
- The depolarization of T-tubules triggers the sarcoplasmic reticulum (SR) to release calcium ions (Ca²⁺).
- Ca²⁺ binds to troponin C on the actin filament.
- This causes tropomyosin to shift, exposing binding sites on actin.
🔍 Without calcium, tropomyosin blocks the myosin-binding sites on actin, preventing contraction.
🔹 3. Contraction – Sliding Filament Mechanism (Cross-Bridge Cycling)
This involves four major steps:
A. Cross-Bridge Formation
Myosin head, energized by ATP hydrolysis, binds to actin → forming a cross-bridge.
B. Power Stroke
Myosin head pivots, pulling actin toward the center of the sarcomere → shortening the muscle.
C. Cross-Bridge Detachment
ATP binds to myosin → causing it to detach from actin.
D. Reactivation of Myosin Head
ATP is hydrolyzed → myosin returns to “cocked” position, ready to bind again.
🔁 This cycle continues as long as Ca²⁺ and ATP are available.
🔹 4. Relaxation
- When nerve stimulation stops, ACh is broken down by acetylcholinesterase.
- Ca²⁺ is pumped back into the sarcoplasmic reticulum (via Ca²⁺-ATPase).
- Troponin-tropomyosin complex returns to resting position, blocking actin’s binding sites.
- Muscle fiber returns to resting length.
⚡ III. Energy Requirements
- ATP is essential for:
- Myosin head detachment
- Calcium reuptake into SR
- Energizing the myosin head for the next cycle
Sources of ATP:
- Stored ATP (lasts ~2 seconds)
- Creatine phosphate system (rapid, short-term energy)
- Anaerobic glycolysis (short bursts, produces lactic acid)
- Aerobic respiration (long-term, endurance)
🧾 IV. Key Events in Muscle Contraction
- Nerve signal → Acetylcholine release
- Muscle depolarization → Ca²⁺ release from SR
- Ca²⁺ binds troponin → myosin-binding sites exposed
- Myosin binds actin → power stroke → contraction
- ATP enables detachment → cycle continues
- Ca²⁺ removed → muscle relaxes
🩺 Clinical Correlation
- Rigor mortis: After death, ATP is depleted → myosin cannot detach from actin → muscles stiffen.
- Myasthenia gravis: Autoimmune destruction of ACh receptors → muscle weakness.
- Malignant hyperthermia: Excessive Ca²⁺ release → sustained contraction and heat production.
- Muscle fatigue: Due to ATP depletion, lactic acid buildup, or impaired neural transmission.
Skeletal muscle contraction is a precise and energy-dependent process, regulated by nervous signals, calcium dynamics, and ATP availability. Understanding its mechanisms is fundamental in diagnosing and managing neuromuscular disorders, ensuring safe use of anesthesia, and promoting rehabilitation.
❤️ Cardiac Muscle – Structure and Properties: Academic Overview
Cardiac muscle, found only in the heart, is a specialized form of involuntary, striated muscle tissue. It is responsible for the rhythmic contraction and relaxation that pumps blood throughout the body. Cardiac muscle combines features of both skeletal and smooth muscle but also has unique structural and physiological properties that support its continuous, fatigue-resistant function.
🧬 I. Structure of Cardiac Muscle
🔹 1. Muscle Fibers
- Short, branched, and cylindrical
- Uninucleated or binucleated (1–2 central nuclei per cell)
- Striated like skeletal muscle due to organized sarcomeres
- Surrounded by endomysium (connective tissue layer)
🔹 2. Intercalated Discs
- Specialized junctions that connect cardiac muscle cells end to end
- Contain:
- Desmosomes – provide mechanical strength, prevent separation during contraction
- Gap junctions – allow for rapid electrical conduction between cells
📌 Intercalated discs allow the heart muscle to act as a functional syncytium, contracting in a coordinated and unified manner.
🔹 3. Sarcomeres and Myofibrils
- Like skeletal muscle, cardiac muscle has actin and myosin filaments arranged in sarcomeres
- This accounts for its striated appearance
🔹 4. Sarcoplasmic Reticulum and T-tubules
- Less extensive than in skeletal muscle
- T-tubules are larger and located at the Z lines
- Dependent on both intracellular and extracellular calcium for contraction
⚡ II. Properties of Cardiac Muscle
Cardiac muscle exhibits several unique electrophysiological and mechanical properties:
1. Automaticity (Autorhythmicity)
- Cardiac muscle can initiate its own impulse without external stimulation.
- Due to pacemaker cells in the SA node which spontaneously depolarize.
🔍 Allows for continuous, rhythmic heartbeat.
2. Excitability
- Ability to respond to an electrical or chemical stimulus by generating an action potential.
- The threshold potential must be reached for depolarization to occur.
3. Conductivity
- Gap junctions in intercalated discs transmit impulses quickly from cell to cell.
- Ensures that the atria and ventricles contract as unified chambers.
4. Contractility
- Ability to generate forceful contractions when stimulated.
- Strength of contraction is influenced by calcium availability and autonomic nervous system (especially sympathetic stimulation).
5. Refractoriness
- Cardiac muscle has a long refractory period (~250 ms), during which it cannot be re-excited.
- Prevents tetanic contractions, which are incompatible with heart function.
6. All-or-None Law
- Once the action potential reaches threshold, the entire muscle fiber contracts maximally.
- Unlike skeletal muscle, cardiac muscle contracts as a whole unit, not partially.
🩸 III. Key Differences: Cardiac vs Skeletal Muscle
| Feature | Cardiac Muscle | Skeletal Muscle |
|---|---|---|
| Nucleus per cell | 1–2, central | Multiple, peripheral |
| Striations | Present | Present |
| Voluntary control | No (autonomic) | Yes (somatic nervous system) |
| Intercalated discs | Present | Absent |
| Pacemaker activity | Present (SA node) | Absent |
| Calcium source | Intra- and extracellular | Mostly intracellular (SR) |
| Regeneration ability | Very limited | Moderate with satellite cells |
| Tetanus possible? | No | Yes |
🔬 IV. Clinical Relevance of Cardiac Muscle Properties
- Arrhythmias: Disorders of automaticity or conductivity
- Heart block: Interruption in electrical conduction
- Heart failure: Weakened contractility, reduced cardiac output
- Myocardial infarction: Damage to cardiac muscle → impaired conductivity and contraction
- Calcium channel blockers: Affect contraction strength by modulating Ca²⁺ influx
Cardiac muscle is highly specialized to sustain continuous, rhythmic, and powerful contractions for life. Its structural adaptations, such as intercalated discs and pacemaker cells, allow it to function as an integrated, self-regulating pump. Understanding its unique structure and properties is essential for diagnosing and managing cardiovascular conditions, making it a vital focus in nursing and medical education.
❤️ Structure and Properties of Cardiac Muscle – Academic Explanation
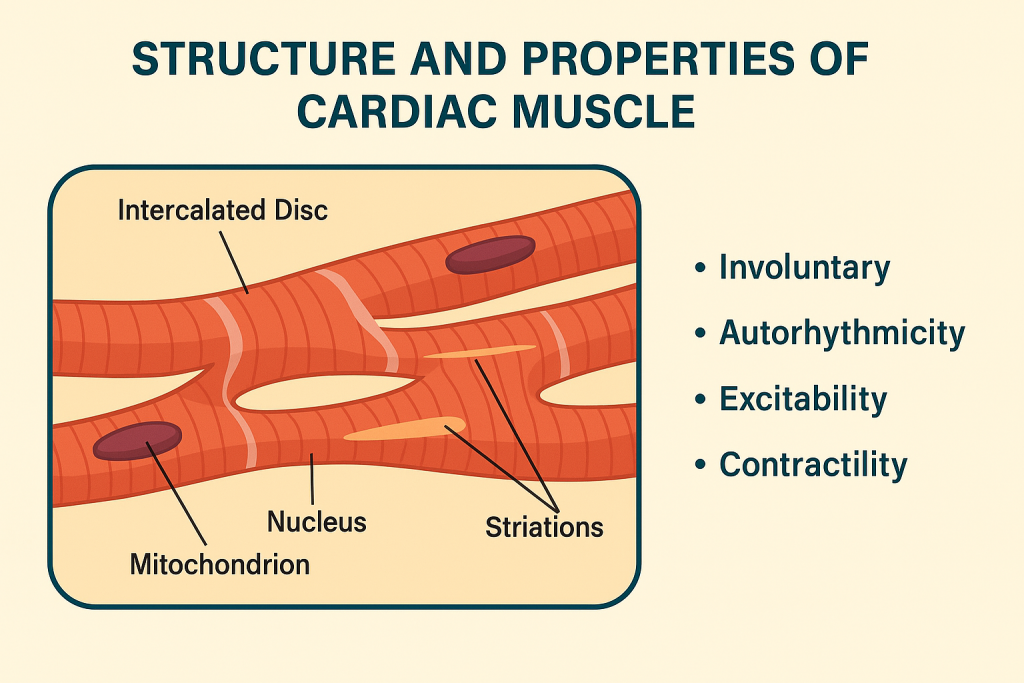
🧠 Introduction
Cardiac muscle is a specialized, involuntary, and striated muscle tissue found only in the walls of the heart (myocardium). It combines features of both skeletal and smooth muscle, with unique adaptations that allow it to contract rhythmically and continuously throughout life without fatigue.
🔬 I. Structural Features of Cardiac Muscle
- Striated Appearance
- Like skeletal muscle, cardiac muscle shows cross striations due to the organized arrangement of actin and myosin in sarcomeres.
- Branched Fibers
- Cardiac myocytes are short, branched, and mononucleated (or binucleated), forming a network that facilitates coordinated contraction.
- Intercalated Discs
- Unique junctions between cardiac muscle cells.
- Contain:
- Desmosomes – maintain mechanical integrity
- Gap junctions – allow electrical impulses to spread rapidly cell-to-cell, enabling synchronous contraction
- Central Nucleus
- Each cardiac myocyte typically has one centrally located nucleus, unlike skeletal muscle fibers, which are multinucleated and peripheral.
- Abundant Mitochondria
- Cardiac cells contain numerous mitochondria (~30% of volume) to support continuous aerobic respiration.
- Involuntary Control
- Regulated by the autonomic nervous system (sympathetic and parasympathetic), not conscious effort.
- Presence of T-tubules and Sarcoplasmic Reticulum
- T-tubules are wider and fewer than in skeletal muscle.
- Calcium-induced calcium release is essential in cardiac excitation-contraction coupling.
🔁 II. Physiological Properties of Cardiac Muscle
- Automaticity (Autorhythmicity)
- Ability to generate its own electrical impulses (action potentials) via pacemaker cells (e.g., SA node).
- No need for external nerve stimulation.
- Rhythmicity
- Cardiac contractions occur in a regular, repeating pattern, which is crucial for coordinated heartbeat.
- Conductivity
- Impulses travel through specialized conduction pathways (e.g., AV node, Bundle of His) and via gap junctions.
- Contractility
- Strong and sustained contraction generated by sliding filament mechanism, regulated by Ca²⁺ and ATP.
- Excitability
- Ability to respond to electrical stimuli and depolarize.
- Influenced by hormones (e.g., epinephrine) and drugs (e.g., beta-blockers).
- Long Refractory Period
- Prevents tetanus or sustained contraction, allowing the heart to relax and refill between beats.
- All-or-None Law
- If one cell in a syncytium is stimulated, the entire group contracts simultaneously, due to gap junctions.
🧾 Structural and Functional Highlights
| Feature | Cardiac Muscle |
|---|---|
| Striation | Present (similar to skeletal muscle) |
| Nucleus | Single, central |
| Cell shape | Branched, interconnected |
| Intercalated discs | Present – allow coordinated contractions |
| Control | Involuntary (autonomic nervous system) |
| Pacemaker potential | Present (SA node, AV node) |
| Refractory period | Long – prevents tetany |
| Mitochondria | Numerous – supports high aerobic activity |
| Regeneration | Very limited regenerative capacity |
🩺 Clinical Relevance
- Myocardial infarction: Death of cardiac muscle due to lack of oxygen.
- Arrhythmias: Abnormal conduction and contractility.
- Heart failure: Impaired contractility or relaxation.
- Cardiomyopathies: Structural or functional abnormalities of cardiac muscle.
- Drugs: Calcium channel blockers, beta-blockers, and digitalis act on cardiac muscle properties.
🧬 Smooth Muscle – Structure and Properties
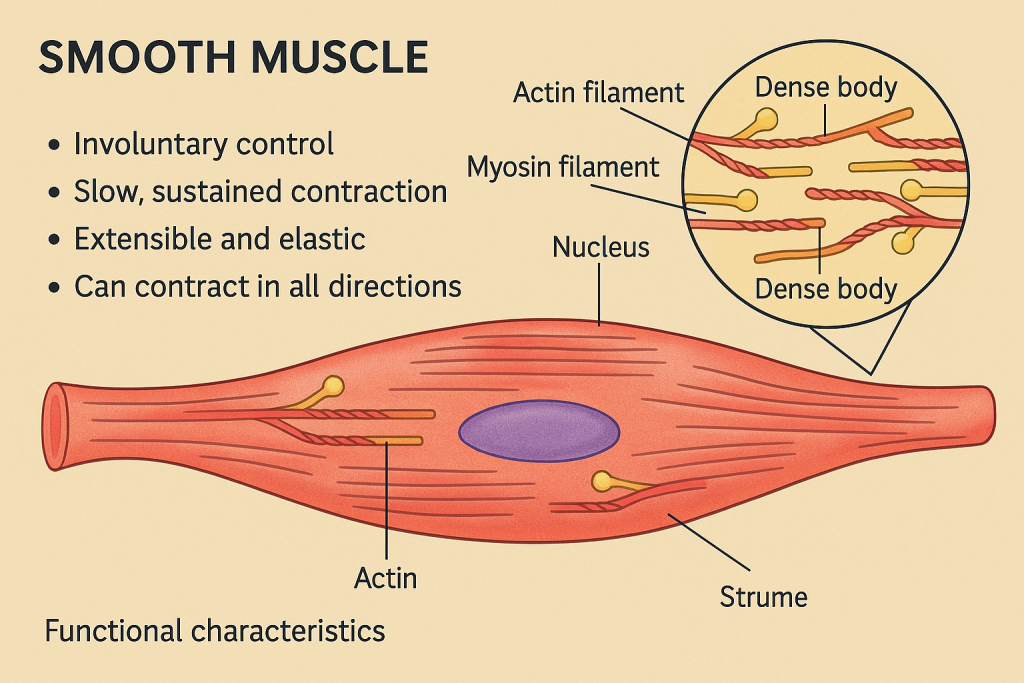
🔍 Introduction
Smooth muscle is a type of involuntary, non-striated muscle found primarily in the walls of hollow organs such as the intestines, blood vessels, bladder, uterus, and respiratory tract. Unlike skeletal and cardiac muscles, smooth muscle fibers do not exhibit striations, and their contractions are slower, sustained, and regulated autonomously by the autonomic nervous system.
🧠 I. Structural Features of Smooth Muscle
🔹 Shape and Size
- Smooth muscle cells are spindle-shaped (fusiform): wide in the center and tapering at both ends.
- Each cell contains a single, centrally located nucleus.
🔹 Cytoskeleton and Contractile Apparatus
- No sarcomeres (unlike striated muscle), hence no striations.
- Actin and myosin filaments are arranged diagonally across the cell, enabling contraction from all directions.
- Dense bodies (analogous to Z-discs) anchor actin filaments and help transmit force throughout the cell.
- Intermediate filaments support the cytoskeleton.
🔹 Sarcoplasmic Reticulum and Caveolae
- Smooth muscle lacks T-tubules but contains caveolae (small plasma membrane invaginations) that help in Ca²⁺ entry.
- The sarcoplasmic reticulum is less developed than in skeletal muscle.
🔹 Innervation
- Innervated by the autonomic nervous system (ANS) — both sympathetic and parasympathetic.
- No motor end plates; neurotransmitters are released into diffuse junctions affecting multiple cells.
🔹 Cell Communication
- Many smooth muscles are interconnected by gap junctions, which allow synchronized contraction (especially in visceral organs).
📌 II. Properties of Smooth Muscle
1. Involuntary Control
- Controlled unconsciously via the autonomic nervous system and hormones (e.g., oxytocin, epinephrine).
- Contraction can also be myogenic (originating from within the muscle itself).
2. Slow and Sustained Contraction
- Contractions are slower in onset but long-lasting.
- Useful for maintaining tone in blood vessels, intestines, and bladder.
3. Plasticity (Stress-Relaxation Response)
- Smooth muscle can stretch and still maintain contractility (important in the bladder, uterus).
- Unlike skeletal muscle, it doesn’t get overstretched easily.
4. Excitability
- Responds to a variety of stimuli: neural, hormonal, chemical, or mechanical.
5. Elasticity
- Can recoil back to its original shape after stretching.
6. Automaticity
- Some smooth muscles (e.g., intestinal) can generate spontaneous depolarizations (pacemaker potentials).
7. Tonic vs. Phasic Contractions
- Tonic smooth muscle maintains constant tone (e.g., sphincters).
- Phasic smooth muscle contracts in bursts (e.g., peristalsis in the gut).
🔬 III. Functional Classification
- Single-Unit (Visceral) Smooth Muscle
- Cells act as a single coordinated unit via gap junctions.
- Found in walls of digestive tract, uterus, and bladder.
- Multi-Unit Smooth Muscle
- Cells function independently, with fine motor control.
- Found in the iris of the eye, arrector pili muscles, and some vascular walls.
🩺 Clinical Relevance
- Asthma: Hyperreactivity of bronchial smooth muscle.
- Hypertension: Overactivity or resistance in vascular smooth muscle.
- Irritable Bowel Syndrome (IBS): Abnormal gut motility.
- Labor induction: Oxytocin stimulates uterine smooth muscle.
Smooth muscle plays a vital role in maintaining homeostasis, regulating the movement of substances through internal organs, and responding to internal stimuli without conscious control. Its structure and function are highly adapted to long-duration, low-energy contractions critical for internal organ function.
🦴🦵 Musculoskeletal System – Application and Implications in Nursing
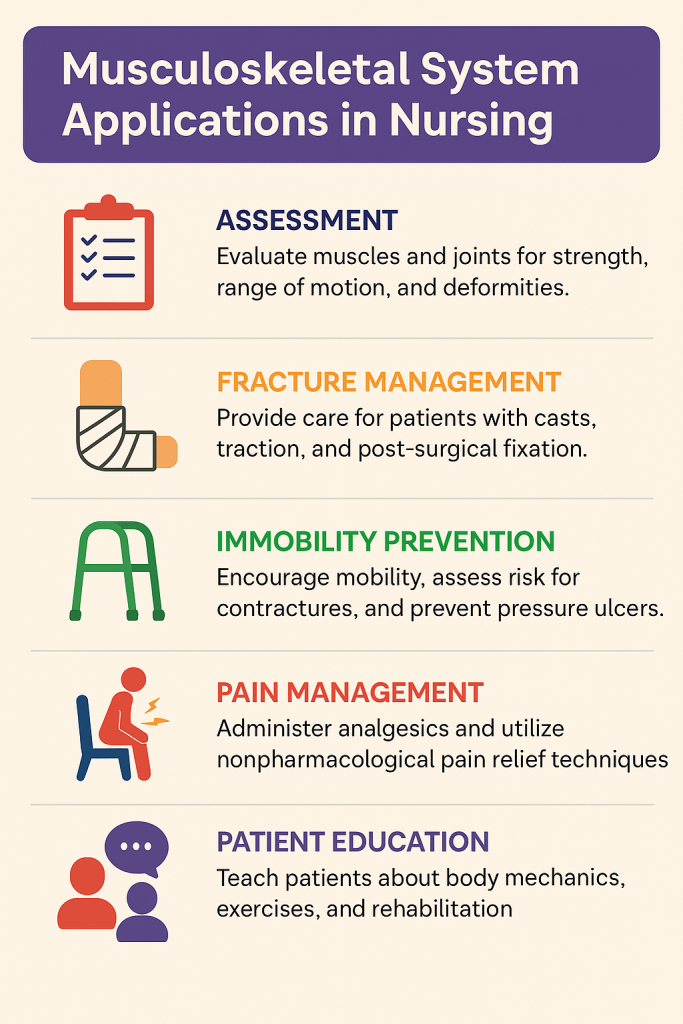
The musculoskeletal system comprises bones, joints, muscles, tendons, ligaments, and connective tissues, working together to support the body, enable movement, and protect vital organs. In nursing practice, a comprehensive understanding of this system is essential for mobility support, injury prevention, rehabilitation, pain management, and holistic care.
🧠 I. Key Applications of the Musculoskeletal System in Nursing Practice
🔹 1. Patient Mobility and Activity Support
- Nurses assess and assist with body mechanics, transfers, and ambulation.
- Promote range of motion (ROM) exercises to maintain or restore joint mobility.
- Use of assistive devices: crutches, walkers, canes, and wheelchairs.
🩺 Implication: Prevents muscle atrophy, contractures, and venous stasis in immobile patients.
🔹 2. Postoperative and Orthopedic Care
- Nurses care for patients recovering from fractures, joint replacements, or spinal surgeries.
- Monitor for complications such as infection, compartment syndrome, deep vein thrombosis (DVT).
- Provide wound care, immobilization (splints, casts), and traction management.
🩺 Implication: Requires knowledge of skeletal anatomy, healing physiology, and mobility protocols.
🔹 3. Pain Assessment and Management
- Musculoskeletal disorders often present with pain, swelling, stiffness, and weakness.
- Nurses use pain scales (e.g., VAS, numeric rating) and administer analgesics, anti-inflammatory drugs, or cold/heat therapy.
🩺 Implication: Enables individualized pain management, enhances comfort and function.
🔹 4. Fall Prevention and Safety Measures
- Elderly and post-op patients are at higher risk due to bone fragility, joint instability, or muscle weakness.
- Nurses implement fall risk assessments, environmental modifications, and patient education.
🩺 Implication: Prevents fractures, disability, and hospital-acquired injuries.
🔹 5. Rehabilitation and Physiotherapy Collaboration
- Nurses work with physiotherapists to support muscle strengthening, gait training, and joint mobilization.
- Encourage ADL (Activities of Daily Living) independence.
🩺 Implication: Promotes functional recovery and psychosocial well-being.
🔹 6. Nutritional and Metabolic Support
- Skeletal and muscular health depends on calcium, vitamin D, protein, and phosphate balance.
- Nurses provide dietary guidance and supplementation support for bone/muscle healing.
🩺 Implication: Crucial in osteoporosis prevention, fracture recovery, and muscle mass maintenance.
🔹 7. Neuromuscular Assessments
- Assess muscle tone, strength, coordination, reflexes, and sensation.
- Important in conditions like stroke, multiple sclerosis, spinal injuries, or neuromuscular disorders.
🩺 Implication: Early detection of deficits, supports neurological care planning.
🔹 8. Pediatric and Geriatric Considerations
- Children may present with growth-related musculoskeletal issues (e.g., scoliosis, clubfoot).
- Older adults often face osteoporosis, sarcopenia, arthritis, and reduced balance.
🩺 Implication: Requires age-specific assessments, interventions, and mobility aids.
📌 II. Summary – Nursing Implications of the Musculoskeletal System
| Nursing Focus | Application |
|---|---|
| Mobility | Assistive devices, safe transfer techniques |
| Pain management | Use of analgesia, heat/cold therapy, inflammation control |
| Rehabilitation | Collaboration with therapists, patient motivation |
| Postoperative orthopedic care | Monitoring, traction, cast care, complication prevention |
| Fall prevention | Risk assessment, environmental safety, education |
| Muscle and bone health | Nutritional advice, supplements, physical activity encouragement |
| Neurological screening | Muscle tone, strength, and reflex evaluation |