Physio-unit-7-The Sensory Organs
🧠 Skin – Functions and Academic Overview
🧬 Physiology of the Skin – Academic Overview
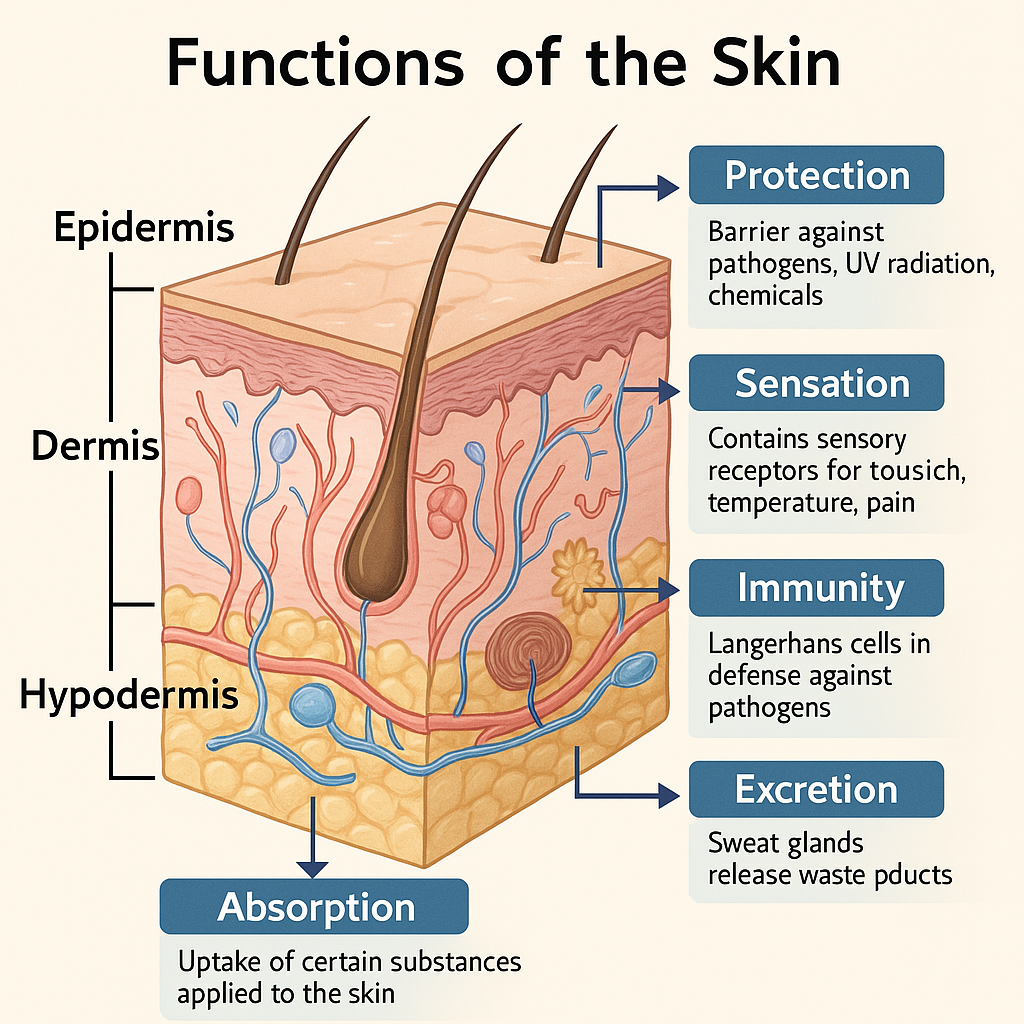
The skin is the largest and most accessible organ of the body, forming a protective and interactive interface with the external environment. It performs vital physiological functions including barrier protection, sensory reception, thermoregulation, immunity, excretion, absorption, metabolic processes, and wound healing.
🧠 I. Structure Overview – Foundation of Physiology
The physiological roles of the skin are based on its three major layers:
- Epidermis (outermost, avascular, stratified squamous epithelium)
- Dermis (vascularized connective tissue layer with nerve endings and appendages)
- Hypodermis or Subcutaneous tissue (fat and connective tissue that insulates and cushions)
🔬 II. Detailed Physiological Functions of Skin
🔹 1. Barrier Function
- Epidermal keratinocytes form a strong, waterproof barrier.
- Stratum corneum: composed of dead keratinized cells embedded in lipids → prevents entry of pathogens and minimizes water loss.
- Tight junctions between keratinocytes enhance selective permeability.
- Melanocytes in basal layer produce melanin → protect from UV radiation.
- Langerhans cells contribute to immune surveillance.
🔹 2. Thermoregulation
- Controlled by the hypothalamus and skin’s blood vessels and sweat glands.
- Sweat glands (eccrine) respond to heat by secreting sweat → evaporative cooling.
- Arteriovenous anastomoses regulate blood flow to the dermis:
- Vasodilation → heat dissipation
- Vasoconstriction → heat conservation
🔹 3. Sensation
- Mechanoreceptors (e.g., Meissner’s, Pacinian corpuscles) detect touch, pressure, vibration.
- Free nerve endings detect pain, itch, and temperature.
- Distributed throughout dermis and epidermis in varying density:
- High density: lips, fingertips
- Low density: back, thighs
🔹 4. Immune Function
- Skin is part of the innate immune system.
- Langerhans cells in the epidermis capture and present antigens.
- Dermal dendritic cells and mast cells trigger inflammatory responses.
- Antimicrobial peptides (e.g., defensins) secreted by keratinocytes.
- Interacts with adaptive immunity via lymphocyte migration.
🔹 5. Excretion and Absorption
- Excretion via sweat glands:
- Removes water, sodium, chloride, potassium, urea, and lactic acid.
- Absorption:
- Lipid-soluble substances (e.g., transdermal drugs: nicotine, fentanyl, estrogen) can penetrate through the stratum corneum.
- Limited compared to GI absorption but useful therapeutically.
🔹 6. Vitamin D Synthesis
- UVB radiation converts 7-dehydrocholesterol → cholecalciferol (Vitamin D₃) in the epidermis.
- Vitamin D is essential for:
- Calcium and phosphate metabolism
- Bone health and immune modulation
🔹 7. Wound Healing and Regeneration
- A highly coordinated process involving:
- Hemostasis – platelet aggregation and clotting
- Inflammation – immune cell infiltration
- Proliferation – keratinocyte migration, fibroblast activation
- Remodeling – collagen realignment, angiogenesis
- Keratinocytes and dermal fibroblasts play central roles.
🔹 8. Pigmentation
- Melanocytes in the basal epidermis produce melanin, transferred to keratinocytes.
- Melanin protects against ultraviolet (UV) radiation and contributes to skin color.
- Regulated by melanocyte-stimulating hormone (MSH).
🔹 9. Communication and Social Function
- Blushing, sweating, and goosebumps are physiological responses to emotion.
- Skin reflects internal health → jaundice, cyanosis, pallor.
🧾 III. Summary Table: Physiological Roles of Skin
| Function | Involved Structures/Processes |
|---|---|
| Protection | Keratinocytes, melanin, lipid barrier, immune cells |
| Thermoregulation | Sweat glands, dermal vasculature |
| Sensation | Receptors (touch, temperature, pain) |
| Immunity | Langerhans cells, antimicrobial peptides |
| Excretion | Sweat glands |
| Absorption | Stratum corneum (for lipid-soluble substances) |
| Vitamin D Synthesis | Epidermis + UV light |
| Wound Healing | Hemostasis → Inflammation → Proliferation → Remodeling |
| Pigmentation | Melanocytes + MSH |
🩺 IV. Nursing and Clinical Relevance
- Skin assessment gives clues to:
- Dehydration, infection, allergic reactions
- Endocrine/metabolic disorders (e.g., hyperpigmentation, jaundice)
- Important in pressure ulcer prevention, wound care, hydration status monitoring
- Vital in burn management, temperature regulation in infants/elderly
- Transdermal drug applications require knowledge of skin absorption properties
The physiology of the skin reflects its role as a multifunctional organ, vital in protection, homeostasis, immunity, metabolism, and communication. A clear understanding is essential for clinical assessment, nursing interventions, and therapeutic skin care.
👁️ Physiology of Vision – Academic Overview
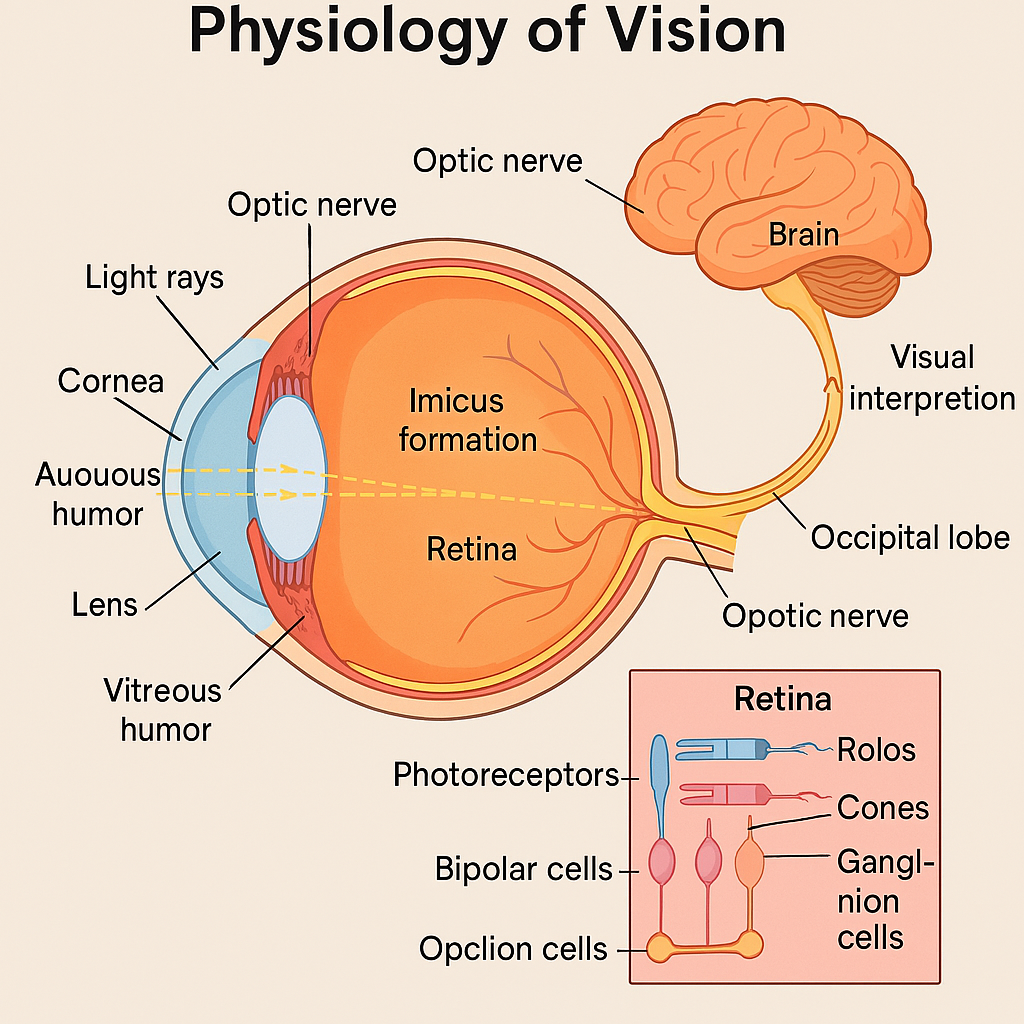
Vision is the complex physiological process by which the eyes receive light, convert it into electrical impulses, and send these signals to the brain for interpretation as images. This process involves coordinated activity of the eye’s anatomical structures, photoreceptor cells, and neural pathways.
🧠 I. Basic Pathway of Vision
Light → Eye → Retina → Optic Nerve → Brain (Occipital Lobe)
🔬 II. Anatomy Involved in Vision
1. Accessory Structures
- Eyelids, conjunctiva, lacrimal apparatus, eyelashes
- Protect the eye and keep the surface moist and clean
2. Refractive Media (Light Bending Structures)
- Cornea – Primary refractive surface
- Aqueous humor – Maintains intraocular pressure and nourishes lens/cornea
- Lens – Changes shape for accommodation (focus)
- Vitreous humor – Gel that maintains shape of the eyeball
👁️ III. Steps in Visual Processing
🔹 1. Light Entry and Refraction
- Light enters through cornea, passes through aqueous humor, pupil, lens, and vitreous humor
- These transparent structures refract (bend) the light rays to focus on the retina
- Cornea provides most of the refraction
- Lens adjusts its curvature for near/far objects (accommodation)
🔹 2. Pupil Regulation
- Controlled by iris muscles (sphincter & dilator pupillae)
- Regulates the amount of light entering the eye
- Controlled via autonomic nervous system:
- Parasympathetic → Constriction (miosis)
- Sympathetic → Dilation (mydriasis)
🔹 3. Image Formation on Retina
- A real, inverted, and reversed image is formed on the retina
- Retina contains photoreceptors:
- Rods: Night (scotopic) vision, black-and-white, peripheral vision
- Cones: Day (photopic) vision, color detection, central vision
🔹 4. Phototransduction (Conversion of Light to Electrical Signal)
- Light strikes photopigments (e.g., rhodopsin in rods, photopsins in cones)
- Initiates a photochemical reaction
- Leads to a change in membrane potential and neurotransmitter release
- Signal passes to:
- Bipolar cells
- Then to ganglion cells
- Axons of ganglion cells form the optic nerve
🔹 5. Neural Pathway to the Brain
- Optic nerve (CN II) from each eye carries visual signals
- Optic chiasm: Partial crossing of fibers
- Nasal retinal fibers cross; temporal fibers do not
- Optic tracts carry the signal to:
- Lateral geniculate nucleus (LGN) of thalamus
- From LGN → optic radiations → primary visual cortex (area 17) in the occipital lobe
🔹 6. Visual Interpretation
- Primary visual cortex decodes basic visual information (e.g., shape, contrast)
- Association visual areas interpret:
- Color
- Motion
- Object recognition
- Depth perception
🌈 IV. Role of Cones in Color Vision
- 3 types of cones (red, green, blue) respond to different wavelengths
- Color blindness: Genetic absence of one or more cone types (commonly red-green)
🔁 V. Accommodation Reflex (Near Vision Adjustment)
Involves:
- Ciliary muscle contraction → lens becomes more convex
- Pupil constriction to improve focus
- Convergence of eyeballs via medial rectus muscles
Controlled by the oculomotor nerve (CN III)
🧾 VI. Summary Table – Key Components in Vision Physiology
| Component | Function |
|---|---|
| Cornea & Lens | Refraction and focusing of light |
| Iris & Pupil | Control light entry |
| Retina (rods & cones) | Light detection and phototransduction |
| Optic nerve/chiasm/tract | Transmission of signals to the brain |
| Visual cortex (Occipital lobe) | Interpretation of visual stimuli |
| Ciliary muscles & lens | Accommodation (focus adjustment) |
🩺 VII. Clinical Significance
| Disorder | Physiological Basis |
|---|---|
| Myopia (nearsightedness) | Long eyeball → image forms before retina |
| Hyperopia (farsightedness) | Short eyeball → image forms behind retina |
| Glaucoma | ↑ Intraocular pressure → optic nerve damage |
| Cataract | Lens opacity → impaired refraction |
| Macular degeneration | Cone degeneration in central retina |
| Retinitis pigmentosa | Progressive rod degeneration → night blindness |
| Optic neuritis | Inflammation of optic nerve (e.g., in MS) |
Vision is a highly integrated sensory function involving precise optics, neuronal signaling, and brain interpretation. Understanding its physiology enables healthcare professionals to assess visual dysfunctions, support patient education, and detect neurological and ocular conditions early.
👂 Physiology of Hearing – Academic Overview
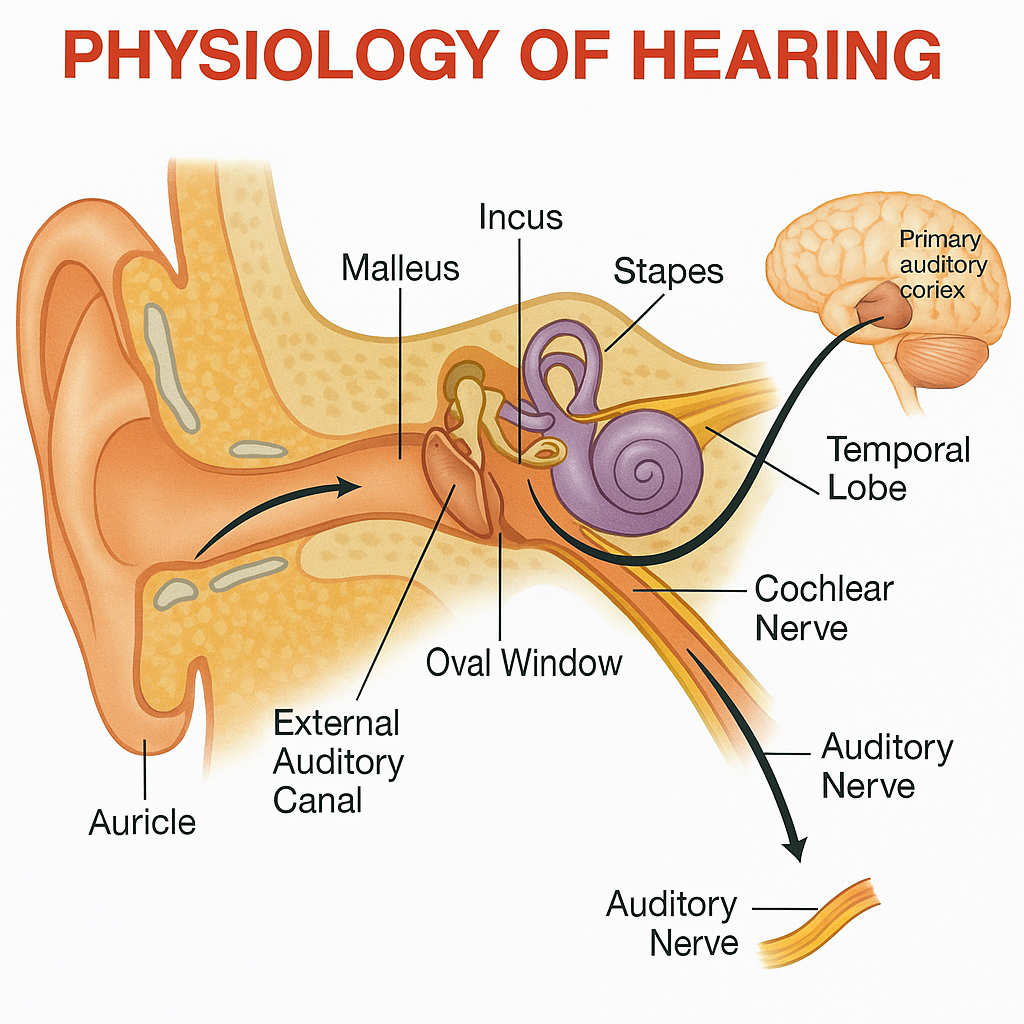
Hearing is the sensory process by which sound waves from the environment are converted into mechanical vibrations, then into electrical signals, and finally interpreted by the auditory cortex in the brain. This process involves the external, middle, and inner ear, as well as complex neural pathways.
🧠 I. Anatomy Involved in Hearing
1. External Ear
- Auricle (Pinna): Collects sound waves.
- External auditory canal: Directs sound waves to the tympanic membrane.
2. Middle Ear
- Tympanic membrane (eardrum): Vibrates in response to sound.
- Auditory ossicles (malleus, incus, stapes): Transmit and amplify vibrations to the inner ear.
- Eustachian tube: Equalizes pressure with the atmosphere.
3. Inner Ear (Cochlea)
- A fluid-filled spiral organ responsible for converting mechanical energy into neural signals.
- Contains:
- Scala vestibuli and scala tympani (contain perilymph)
- Scala media (contains endolymph and organ of Corti)
🔬 II. Step-by-Step Physiology of Hearing
🔹 1. Sound Wave Collection
- Sound waves are collected by the auricle and funneled through the external auditory canal.
🔹 2. Tympanic Membrane Vibration
- Sound waves hit the tympanic membrane, causing it to vibrate.
- Vibrations correspond to the frequency and amplitude of the sound.
🔹 3. Transmission by Ossicles
- Vibrations pass to the malleus, then the incus, and finally the stapes.
- The stapes footplate fits into the oval window of the cochlea.
- The ossicles amplify sound waves (~20-fold).
🔹 4. Fluid Movement in Cochlea
- Stapes movement at the oval window creates waves in perilymph (scala vestibuli).
- These waves travel through the cochlear duct (scala media) and move the basilar membrane.
🔹 5. Stimulation of the Organ of Corti
- The basilar membrane movement displaces the organ of Corti.
- Hair cells in the organ of Corti are topped with stereocilia.
- As they bend against the tectorial membrane, mechanically-gated ion channels open.
🔹 6. Transduction into Electrical Signal
- Ion influx (mainly K⁺ from endolymph) depolarizes the hair cells.
- Depolarization leads to release of neurotransmitters (mainly glutamate).
- This stimulates the afferent fibers of the cochlear nerve.
🔹 7. Auditory Pathway
- Cochlear nerve (part of CN VIII) carries impulses.
- Synapses in the cochlear nuclei (medulla).
- Signal travels bilaterally to:
- Superior olivary complex (pons)
- Inferior colliculus (midbrain)
- Medial geniculate body (thalamus)
- Reaches primary auditory cortex (temporal lobe, area 41 & 42)
🎵 III. Tonotopic Organization
- Basilar membrane is arranged to detect different frequencies:
- Base: Narrow and stiff → detects high-frequency sounds
- Apex: Wide and flexible → detects low-frequency sounds
🧾 IV. Summary Table – Physiology of Hearing
| Step | Event |
|---|---|
| Sound wave entry | Via external auditory canal |
| Tympanic membrane vibration | Converts sound to mechanical energy |
| Ossicle movement | Amplifies vibrations to inner ear |
| Stapes at oval window | Transmits energy into cochlear fluid |
| Basilar membrane & hair cells | Detect specific frequencies, initiate neural signals |
| Auditory nerve transmission | Impulses to auditory cortex for interpretation |
🩺 V. Clinical Relevance
| Disorder | Affected Area | Effect on Hearing |
|---|---|---|
| Conductive hearing loss | External or middle ear | Sound conduction blocked |
| Sensorineural hearing loss | Inner ear or auditory nerve | Hair cell/neural damage |
| Presbycusis | Aging-related cochlear degeneration | High-frequency hearing loss |
| Otosclerosis | Abnormal ossicle fixation | Conductive hearing loss |
| Meniere’s disease | Inner ear fluid imbalance | Vertigo, tinnitus, fluctuating hearing |
| Acoustic neuroma | Tumor on CN VIII | Unilateral sensorineural hearing loss |
The physiology of hearing integrates mechanical, hydraulic, and neural mechanisms to enable accurate sound detection and interpretation. Understanding this process helps healthcare providers diagnose and manage auditory disorders effectively.
👅 Physiology of Taste – Academic Overview
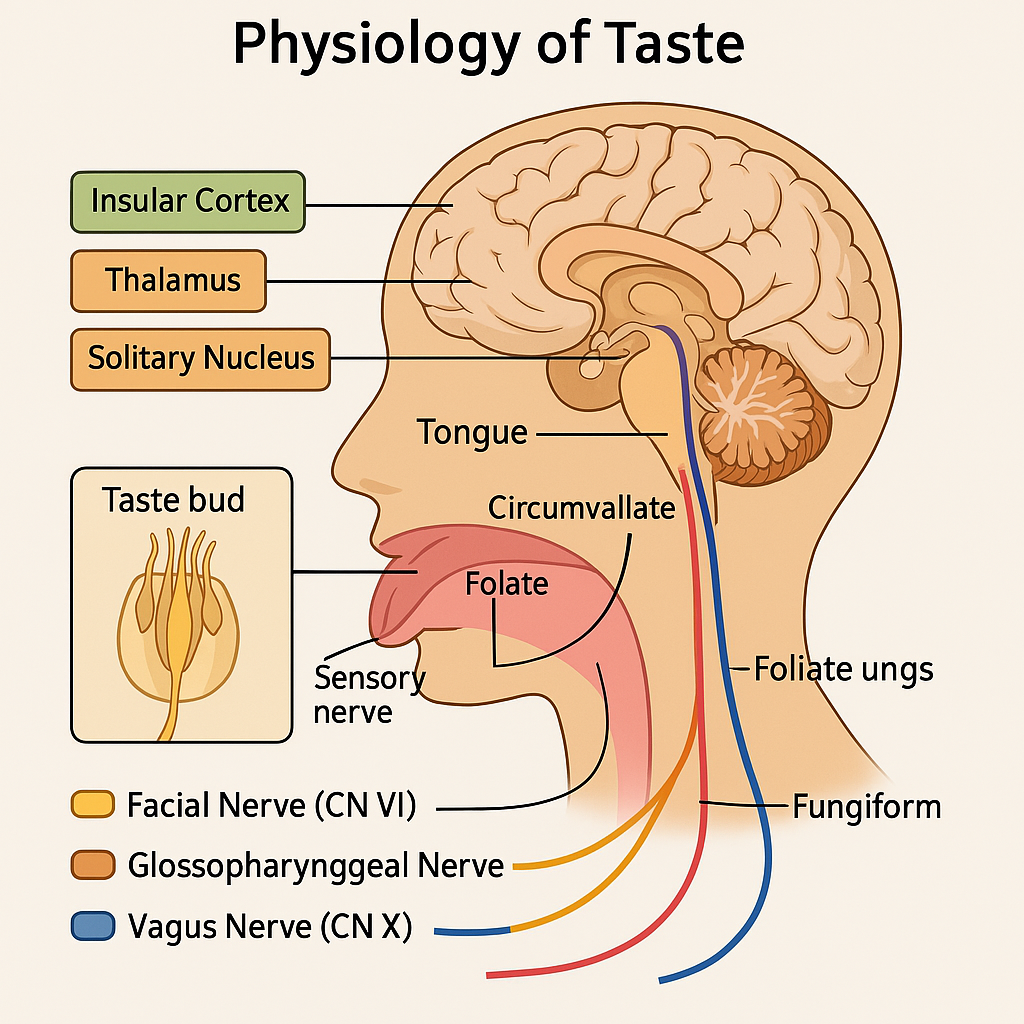
Taste, or gustation, is the chemical sense by which organisms perceive the flavor of soluble substances. The taste system detects chemical stimuli in the mouth and transduces them into neural signals, which are then interpreted by the brain. Taste is closely linked with smell, texture, and temperature for the full flavor experience.
🧠 I. Basic Taste Pathway
Taste molecule (chemical) → Taste receptor (on tongue) → Cranial nerves → Brainstem → Thalamus → Gustatory cortex
🔬 II. Anatomy Involved in Taste
1. Taste Buds
- Located in the epithelium of the tongue, soft palate, pharynx, and epiglottis.
- Contain 50–100 receptor cells.
- Found within papillae:
- Fungiform (anterior tongue)
- Foliate (posterolateral tongue)
- Circumvallate (back of tongue)
- (Filiform papillae do not contain taste buds; they aid in mechanical function)
2. Taste Receptor Cells
- Modified epithelial cells that depolarize when stimulated by tastants.
- Have microvilli (taste hairs) that project through taste pores.
🧪 III. Five Primary Tastes and Their Receptors
| Taste | Stimulus | Mechanism |
|---|---|---|
| Sweet | Sugars (glucose, sucrose) | G-protein coupled receptor (GPCR – T1R2/T1R3) |
| Salty | Sodium ions (Na⁺) | Direct ion channel (ENaC) |
| Sour | Hydrogen ions (H⁺ – acids) | Proton channels or K⁺ channel inhibition |
| Bitter | Alkaloids (e.g., caffeine, quinine) | GPCR (T2R family) |
| Umami | L-glutamate, MSG | GPCR (T1R1/T1R3) |
Each taste modality activates distinct intracellular signaling pathways, ultimately causing neurotransmitter release (e.g., ATP, serotonin) that stimulates adjacent afferent nerve fibers.
🔁 IV. Signal Transduction and Neural Pathways
Step-by-step process:
- Taste molecule binds to receptor on taste cell membrane.
- Depolarization of the taste cell occurs.
- Neurotransmitter release activates sensory neurons.
- Impulse is carried by cranial nerves:
- CN VII (Facial nerve) – anterior 2/3 of tongue
- CN IX (Glossopharyngeal) – posterior 1/3 of tongue
- CN X (Vagus) – epiglottis, pharynx
- Impulses travel to the:
- Solitary nucleus (in medulla oblongata)
- Then to the thalamus
- Finally to the gustatory cortex in the insula and frontal operculum
🧬 V. Integration with Other Sensory Modalities
- Olfaction (smell) contributes significantly to flavor perception.
- Temperature, texture, and pain (e.g., spicy foods) are sensed by:
- Trigeminal nerve (CN V)
🧾 VI.Taste Physiology
| Structure | Function |
|---|---|
| Taste bud | Houses taste receptor cells |
| Receptor cells | Detect and respond to tastants |
| CN VII, IX, X | Transmit taste signals to brainstem |
| Solitary nucleus | First central processing site in brainstem |
| Thalamus | Relay center to cortex |
| Gustatory cortex | Conscious perception of taste |
🩺 VII. Clinical Relevance
| Condition | Description |
|---|---|
| Ageusia | Complete loss of taste |
| Hypogeusia | Reduced taste sensitivity |
| Dysgeusia | Distorted taste perception |
| Loss of taste in COVID-19 | Inflammation or damage to taste receptor cells |
| Neurological damage | CN VII, IX, or X lesions → loss of regional taste |
The physiology of taste involves complex interactions between chemical receptors, neural pathways, and brain regions that collectively allow us to perceive flavors. Nurses and healthcare providers must understand this system for nutritional assessment, neurological evaluations, and patient quality of life considerations.
👃 Physiology of Smell (Olfaction) – Academic Overview
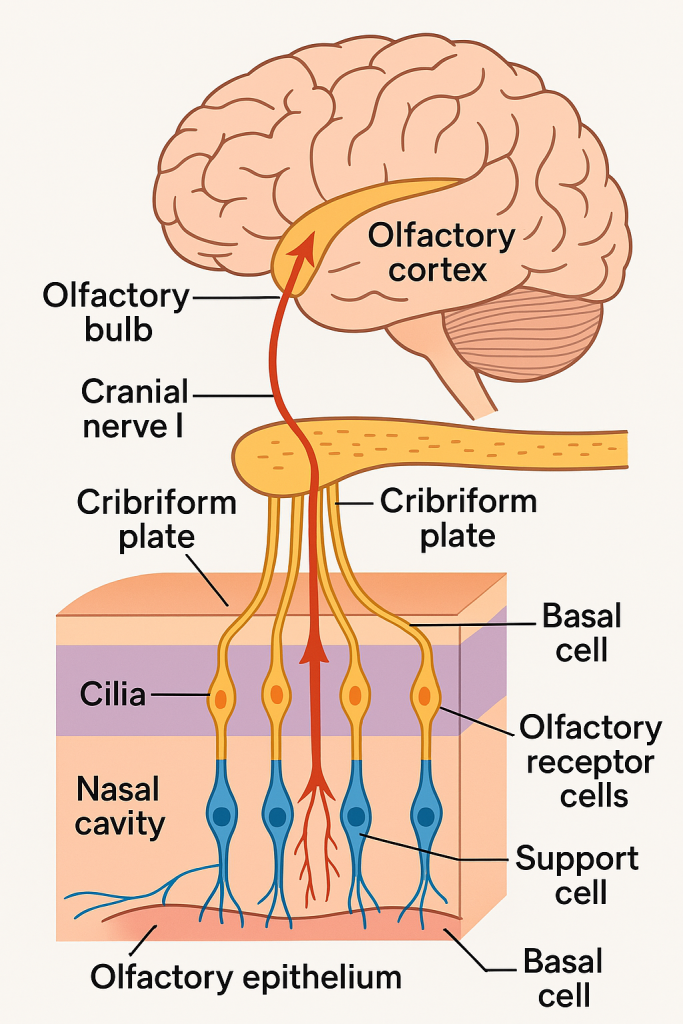
Olfaction is the chemical sense responsible for detecting airborne odorants and converting them into neural signals, which the brain processes as smells. It is closely related to taste, influencing the perception of flavor, and plays roles in memory, emotion, and environmental awareness.
🧠 I. Anatomy of the Olfactory System
🔹 1. Olfactory Epithelium
Located in the superior part of the nasal cavity, it contains:
- Olfactory receptor neurons (ORNs) – bipolar neurons with cilia containing odorant receptors.
- Supporting (sustentacular) cells – provide metabolic support.
- Basal cells – stem cells that regenerate olfactory neurons (unique in CNS).
🔹 2. Olfactory Bulb
- Located above the cribriform plate of the ethmoid bone.
- Receives input from ORNs and contains mitral and tufted cells that relay information deeper into the brain.
🔹 3. Olfactory Nerve (CN I)
- Formed by axons of olfactory receptor neurons.
- Passes through the cribriform plate to synapse in the olfactory bulb.
🔬 II. Steps in the Physiology of Smell
🔹 1. Odorant Detection
- Odor molecules dissolve in the mucus covering the olfactory epithelium.
- They bind to G-protein coupled receptors (GPCRs) on cilia of ORNs.
- Each receptor responds to specific molecular features of odorants.
🔹 2. Signal Transduction
- Binding of odorant activates a G-protein (Golf) → stimulates adenylate cyclase.
- ↑ cAMP opens cyclic nucleotide-gated ion channels → Na⁺ and Ca²⁺ influx.
- This depolarizes the neuron, creating a receptor potential.
🔹 3. Generation of Action Potentials
- If the receptor potential reaches threshold → action potential is generated.
- Travels along the olfactory nerve fibers to the olfactory bulb.
🔹 4. Synaptic Transmission in Olfactory Bulb
- ORN axons synapse on glomeruli in the olfactory bulb.
- Each glomerulus receives input from ORNs expressing the same receptor.
- Synapses occur with:
- Mitral cells
- Tufted cells
- These second-order neurons form the olfactory tract.
🔹 5. Projection to the Brain
Signals from the olfactory bulb are transmitted to:
- Primary olfactory cortex (piriform cortex in the temporal lobe)
- Amygdala (emotion)
- Entorhinal cortex (memory – connection with hippocampus)
- Orbitofrontal cortex (conscious perception of smell)
- Hypothalamus (autonomic and endocrine responses)
🔹 Unique feature: olfactory signals bypass the thalamus before reaching cortex (unlike other senses)
🧾 III. Physiology of Smell
| Step | Description |
|---|---|
| Odorant binding | Odor molecules bind to receptors on olfactory neurons |
| Signal transduction | cAMP-mediated opening of ion channels |
| Neural impulse generation | Depolarization → action potential |
| Olfactory bulb processing | Synapses in glomeruli → relay by mitral/tufted cells |
| CNS processing | Interpretation in olfactory and limbic brain areas |
🧪 IV. Olfactory Receptors and Discrimination
- Humans have ~400 different functional odorant receptors.
- Each receptor can detect multiple odorants, and each odorant can bind to multiple receptors.
- The brain decodes complex combinations to perceive specific smells (combinatorial code).
🧠 V. Clinical Relevance
| Condition | Description |
|---|---|
| Anosmia | Complete loss of smell (e.g., head injury, COVID-19) |
| Hyposmia | Decreased sense of smell |
| Parosmia | Distorted smell perception |
| Phantosmia | Perception of smells without external stimuli |
| Neurodegenerative link | Olfactory dysfunction is early in Parkinson’s, Alzheimer’s |
| COVID-19 | Viral entry affects sustentacular cells → transient anosmia |
The physiology of smell is a finely tuned system involving chemoreception, neural transmission, and limbic integration. It plays vital roles in survival (e.g., detecting smoke, gas), food enjoyment, memory, and emotional responses. An understanding of olfaction is essential in clinical assessments, neurology, and ENT care.
👁️ Errors of Refraction – Academic Overview
Errors of refraction refer to conditions where the eye fails to focus light rays correctly onto the retina, resulting in blurred or distorted vision. These errors arise due to abnormalities in the shape or length of the eye, or irregularities in the refractive surfaces (cornea and lens).
🔬 I. Normal Refraction (Emmetropia)
- In a normal eye (emmetropic eye), parallel light rays entering the eye are focused precisely on the retina.
- The image formed is clear and sharp, without requiring accommodation at rest.
⚠️ II. Common Types of Refractive Errors
🔹 1. Myopia (Nearsightedness)
| Definition | A refractive error where light rays focus in front of the retina. |
|---|---|
| Cause | Eyeball is too long, or cornea is too curved |
| Vision effect | Near objects appear clear, distant objects are blurred |
| Correction | Concave (minus-powered) lenses to diverge light rays |
🔹 2. Hyperopia (Farsightedness)
| Definition | A refractive error where light rays focus behind the retina. |
|---|---|
| Cause | Eyeball is too short, or cornea is too flat |
| Vision effect | Distant vision is clearer than near vision; can blur both with age |
| Correction | Convex (plus-powered) lenses to converge light rays |
🔹 3. Astigmatism
| Definition | A condition where light rays do not focus evenly on the retina due to an irregularly shaped cornea or lens |
|---|---|
| Cause | Cornea or lens is shaped more like a football than a sphere |
| Vision effect | Blurred or distorted vision at all distances |
| Types | – Regular (uniform curvature) |
| Correction | Cylindrical lenses, toric contact lenses, or LASIK surgery |
🔹 4. Presbyopia
| Definition | An age-related refractive error due to loss of elasticity of the lens, impairing near vision. |
|---|---|
| Cause | Stiffening of the crystalline lens after age 40–45 |
| Vision effect | Difficulty reading or focusing on near objects |
| Correction | Reading glasses, bifocals, progressive lenses, or multifocal contact lenses |
🧠 III. Causes of Refractive Errors
| Cause | Mechanism |
|---|---|
| Axial length abnormalities | Too long (myopia), too short (hyperopia) |
| Corneal curvature issues | Too steep or flat; irregular curvature in astigmatism |
| Lens abnormalities | Aging-related stiffness in presbyopia |
| Genetic predisposition | Family history, especially for myopia |
| Environmental factors | Prolonged near work (screen time), poor lighting, eye strain |
🧾 IV. Refractive Errors
| Condition | Light Focuses | Eye Shape | Vision Problem | Correction |
|---|---|---|---|---|
| Myopia | In front of retina | Long axial length | Blurred distance vision | Concave lens (-) |
| Hyperopia | Behind the retina | Short axial length | Blurred near vision | Convex lens (+) |
| Astigmatism | Multiple focal points | Irregular cornea | Distorted vision | Cylindrical lens |
| Presbyopia | Cannot focus near objects | Lens rigidity (age) | Difficulty reading | Reading/bifocal/progressive lens |
🩺 V. Clinical Assessment & Management
👀 Tests Used:
- Visual acuity (Snellen chart)
- Retinoscopy
- Autorefractometry
- Slit-lamp exam
- Keratometry (for corneal curvature)
- Ophthalmoscopy
👓 Treatment Options:
- Eyeglasses
- Contact lenses
- Refractive surgery (LASIK, PRK)
- Orthokeratology (overnight corrective lenses)
🧬 VI. Complications if Left Uncorrected
- Eye strain, headaches, fatigue
- Difficulty in academic performance or driving
- Amblyopia in children (lazy eye)
- Psychological impact due to visual impairment
Refractive errors are the most common cause of visual impairment worldwide. They are easily detectable and treatable with optical aids or surgery. Nurses and healthcare professionals play a key role in early screening, referral, and education on corrective options to prevent vision-related disability.
🧓 Aging Changes in Sensory Organs
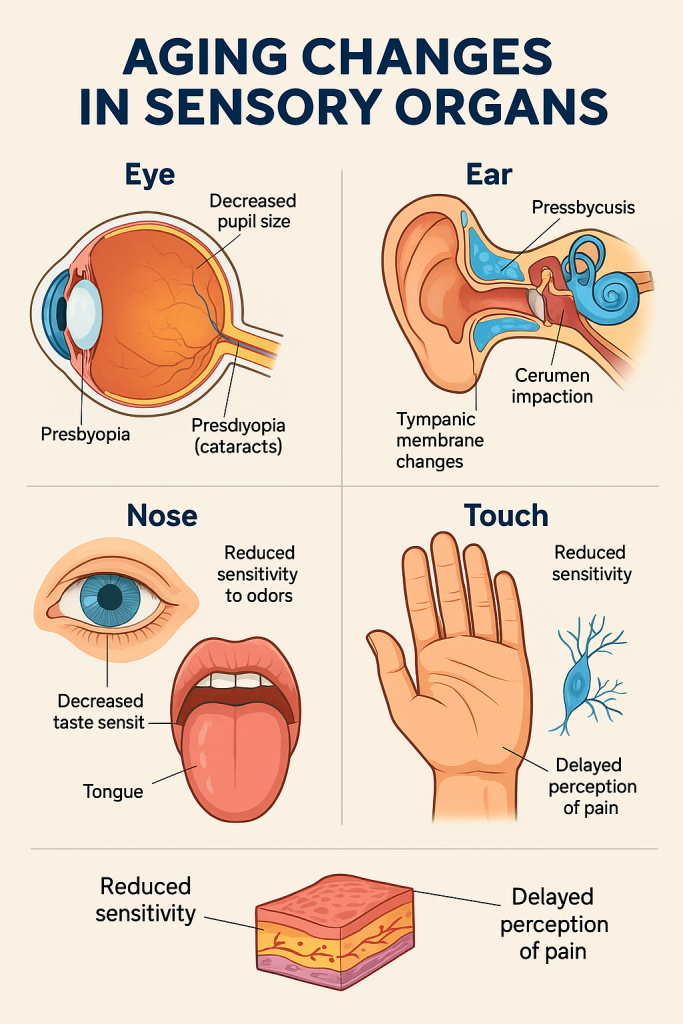
As individuals age, the sensory organs undergo progressive physiological and structural changes that can lead to decreased function and affect quality of life, independence, and safety. These changes are considered part of normal aging, though they may be worsened by disease or environmental factors.
🔬 I. Age-related Changes in the Eye (Vision)
🔹 1. Presbyopia
- Age-related loss of lens elasticity.
- ↓ Ability to focus on near objects (usually begins around 40–45 years).
- Requires reading glasses or bifocals.
🔹 2. Decreased Pupil Size
- ↓ Pupillary reflex and dilation.
- Affects adaptation to changes in light (e.g., bright to dim environments).
🔹 3. Lens Opacification
- Development of cataracts.
- Causes cloudy vision, glare, and difficulty with contrast.
🔹 4. Vitreous Degeneration
- Floaters and flashes due to liquefaction and shrinkage of the vitreous humor.
🔹 5. Decreased Tear Production
- Leads to dry eyes, irritation, and discomfort.
🔹 6. Risk of Age-related Diseases
- Glaucoma – ↑ intraocular pressure damaging optic nerve.
- Age-related macular degeneration (ARMD) – loss of central vision.
- Diabetic or hypertensive retinopathy – retinal blood vessel damage.
👂 II. Age-related Changes in the Ear (Hearing)
🔹 1. Presbycusis
- Age-related sensorineural hearing loss.
- Loss of high-frequency sounds.
- Difficulty hearing in noisy environments.
- Due to degeneration of hair cells in the cochlea and auditory nerve fibers.
🔹 2. Cerumen (Earwax) Impaction
- Cerumen becomes drier and harder.
- Increased risk of conductive hearing loss.
🔹 3. Tympanic Membrane Changes
- Becomes thinner and less flexible, reducing sound conduction.
🔹 4. Ossicle Stiffening
- Middle ear bones become less mobile, further affecting sound transmission.
👃 III. Age-related Changes in Smell (Olfaction)
🔹 1. Hyposmia or Anosmia
- ↓ Number and function of olfactory receptor cells.
- ↓ Sensitivity to odors and impaired detection of danger (e.g., smoke, gas).
- May be early sign of neurodegenerative disease (e.g., Parkinson’s, Alzheimer’s).
👅 IV. Age-related Changes in Taste (Gustation)
🔹 1. Decreased Taste Sensitivity
- ↓ Number of taste buds (especially for sweet and salty).
- ↓ Saliva production → affects solubilization of tastants.
🔹 2. Reduced Appetite
- Often due to combined smell and taste reduction, poor dentition, or medications.
🖐️ V. Age-related Changes in Touch (Tactile Sensation)
🔹 1. Reduced Skin Sensitivity
- ↓ Meissner’s corpuscles and Pacinian corpuscles.
- ↓ Sensitivity to light touch, pressure, and vibration.
🔹 2. Delayed Pain and Temperature Perception
- ↑ Risk of injuries, burns, or pressure ulcers due to reduced awareness.
🧾 VI. Aging Changes in Sensory Organs
| Sensory Organ | Common Age-related Changes |
|---|---|
| Eye | Presbyopia, cataracts, ARMD, dry eyes, decreased light adaptation |
| Ear | Presbycusis, wax buildup, tympanic degeneration |
| Nose | Reduced smell, impaired odor discrimination |
| Tongue | Fewer taste buds, reduced taste sensitivity, dry mouth |
| Skin (Touch) | Reduced tactile sensitivity, delayed pain and temperature response |
🩺 VII. Clinical and Nursing Implications
- Regular screening for vision and hearing problems.
- Encourage use of corrective devices (glasses, hearing aids).
- Modify environment (lighting, minimize background noise).
- Ensure safety: handrails, labeling, food temperature monitoring.
- Educate caregivers on compensating for sensory loss.
- Assess for malnutrition due to loss of taste/smell.
- Be alert to sensory-related confusion or withdrawal, which may mimic dementia.
Sensory organ aging is a natural process that can impact communication, nutrition, safety, and emotional well-being. Early recognition and support can significantly improve the quality of life and independence of older adults.
🧠 The Sensory Organs – Application and Implications in Nursing
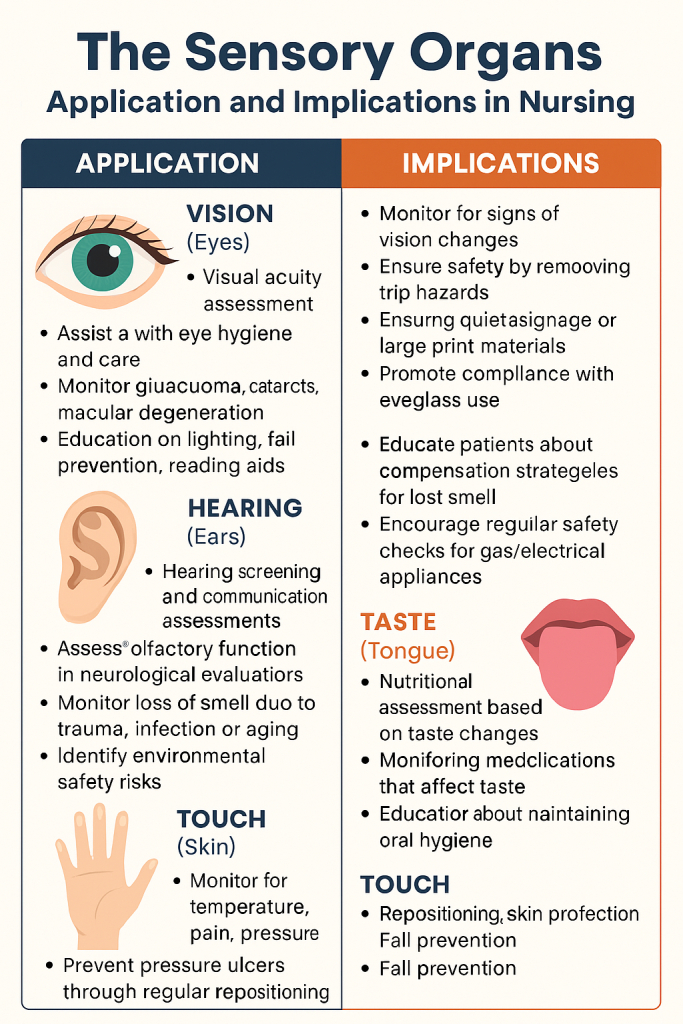
The sensory organs (eyes, ears, nose, tongue, and skin) allow humans to interact with their environment through vision, hearing, smell, taste, and touch. In clinical nursing, understanding their structure and function helps in early detection of dysfunction, ensuring safety, comfort, communication, and quality of life for patients.
👁️ 1. Application of Vision (Eyes) in Nursing
✅ Nursing Applications
- Visual acuity assessment using Snellen chart
- Assisting with eye hygiene and care (cleaning, eye drops)
- Medication administration (e.g., eye ointments or drops)
- Monitoring patients with glaucoma, cataracts, macular degeneration
- Educating on lighting, fall prevention, and reading aids
❗ Nursing Implications
- Monitor for signs of vision changes (squinting, bumping into objects)
- Ensure safety by removing trip hazards
- Provide braille signage or large print materials
- Promote compliance with eyeglass use or eye medication
👂 2. Application of Hearing (Ears) in Nursing
✅ Nursing Applications
- Hearing screening and communication assessments
- Teaching patients how to use and maintain hearing aids
- Recognizing early signs of hearing loss (asking for repetition, isolation)
- Ensuring quiet environments for patients with hearing aids
❗ Nursing Implications
- Speak clearly and face the patient
- Use written instructions when needed
- Encourage regular ear hygiene and cerumen management
- Consider referral to audiologists
👃 3. Application of Smell (Nose) in Nursing
✅ Nursing Applications
- Assessing olfactory function in neurological evaluations
- Identifying loss of smell due to trauma, infection (e.g., COVID-19), or aging
- Monitoring for environmental safety risks (e.g., inability to smell gas or smoke)
❗ Nursing Implications
- Educate patients about compensation strategies for lost smell (e.g., using visual cues while cooking)
- Encourage regular safety checks for gas/electrical appliances
- Support nutritional assessments if smell loss affects appetite
👅 4. Application of Taste (Tongue) in Nursing
✅ Nursing Applications
- Nutritional assessment based on taste changes
- Monitoring patients on medications that affect taste (e.g., chemotherapy, antibiotics)
- Educating patients about maintaining oral hygiene
❗ Nursing Implications
- Offer flavor-enhanced meals for patients with taste loss
- Monitor for weight loss or decreased food intake
- Collaborate with dietitians for alternative nutritional strategies
🖐️ 5. Application of Touch (Skin and Tactile Sensation)
✅ Nursing Applications
- Monitoring for temperature, pain, pressure, or touch loss
- Preventing pressure ulcers through regular repositioning
- Educating patients with diabetic neuropathy about foot care
❗ Nursing Implications
- Use visual and verbal cues for patients with poor tactile feedback
- Assess skin for injuries, burns, or pressure sores
- Provide supportive surfaces and protective devices
🧾 Nursing Applications and Implications
| Sensory Organ | Nursing Applications | Nursing Implications |
|---|---|---|
| Eyes | Visual screening, eye care, glaucoma monitoring | Safety measures, low-vision adaptations |
| Ears | Hearing aid support, communication assistance | Clear speech, minimize background noise |
| Nose | Smell testing, infection screening | Environmental safety education |
| Tongue | Nutrition, taste assessments | Enhance flavor, monitor intake |
| Skin | Tactile testing, pressure sore prevention | Repositioning, skin protection, fall prevention |