BSC SEM 2 UNIT 2 COMMUNITY HEALTH NURSING
UNIT 2 Health Care Planning and Organization of Health Care at various levels
Health Care Planning

1. Introduction to Health Care Planning
Health Care Planning is a systematic process of identifying health problems, setting priorities, and formulating strategies and policies to improve health status.
Importance in Community Health Nursing:
- Helps in achieving equitable, accessible, and affordable healthcare.
- Ensures effective utilization of available resources.
- Enables planning preventive, promotive, curative, and rehabilitative services.
2. Objectives of Health Care Planning in Community Setting
- To reduce morbidity and mortality.
- To provide preventive, promotive, curative, and rehabilitative services.
- To improve quality of life.
- To achieve universal health coverage.
- To involve the community in planning and implementation.
3. Levels of Health Care System in India (Based on Three-Tier System)
A. Primary Level (First Contact Care)
- Focuses on preventive, promotive, and basic curative care.
- Delivered through:
- Sub-Centres (SCs)
- Staff: ANM, Male Health Worker
- Population coverage: 5,000 in plain areas, 3,000 in hilly/tribal
- Services: MCH, immunization, family planning, health education
- Primary Health Centres (PHCs)
- Staff: Medical Officer, Staff Nurses, Pharmacist, Lab Tech
- Population coverage: 30,000 in plain, 20,000 in hilly
- Services: OPD, basic lab tests, ANC/PNC, delivery care, national health programs
- Sub-Centres (SCs)
B. Secondary Level (First Referral Care)
- Provides specialist care, referral support.
- Delivered through:
- Community Health Centres (CHCs)
- Staff: 4 Specialists (Surgeon, Physician, Gynaecologist, Paediatrician), nurses, lab techs, etc.
- Population coverage: 1,20,000 in plain, 80,000 in hilly
- Services: 30-bed facility, OPD/IPD care, emergency, surgical services
- Sub-District Hospitals or Taluka Hospitals
- Community Health Centres (CHCs)
C. Tertiary Level (Advanced Care)
- Offers super-specialty services.
- Institutions:
- District Hospitals
- Medical Colleges
- AIIMS, PGI, Regional Institutes
- Private Super-specialty Hospitals
- Services: ICU, surgeries, diagnostics, training, and research.
4. Types of Health Care Services Provided at Each Level
| Level | Type of Services |
|---|---|
| Primary | Immunization, Antenatal care, Health Education, Basic treatment, Nutrition programs, School health |
| Secondary | Specialist consultations, Inpatient care, Emergency services, Lab investigations |
| Tertiary | Intensive care, Organ transplant, Cardiac surgery, Oncology, Neuro-care, etc. |
5. Health Care Planning Bodies and Schemes
| Planning Body/Scheme | Role |
|---|---|
| Ministry of Health & Family Welfare (MoHFW) | Policy formulation, national health programs |
| National Health Mission (NHM) | Strengthening public health at all levels |
| State Health Societies | Implementation of programs at state level |
| Village Health Sanitation and Nutrition Committees (VHSNC) | Local-level community health planning |
6. Role of Community Health Nurse in Health Planning and Organization
| Role | Details |
|---|---|
| Planner | Identifies community health needs, plans interventions. |
| Care Provider | Offers preventive and basic curative services at SCs/PHCs. |
| Educator | Conducts health awareness and behavior change communication. |
| Coordinator | Coordinates with ASHA, Anganwadi, and other health workers. |
| Evaluator | Assesses effectiveness of health programs, collects data. |
| Advocate | Mobilizes community participation and empowers local decision-making. |
7. Health Programs Supporting Health Care Planning
- Reproductive and Child Health (RCH)
- National Tuberculosis Elimination Program (NTEP)
- National AIDS Control Program (NACP)
- National Vector Borne Disease Control Program (NVBDCP)
- Ayushman Bharat (PM-JAY, HWCs)
- Janani Suraksha Yojana (JSY)
- Rashtriya Bal Swasthya Karyakram (RBSK)
8. Challenges in Health Care Planning at Community Level
- Inadequate infrastructure in remote areas.
- Shortage of trained manpower.
- Poor intersectoral coordination.
- Low community participation.
- Social and cultural barriers.
9. Recommendations
- Strengthen sub-centres with equipment and trained staff.
- Integrate digital health records and telemedicine.
- Promote family and community participation.
- Regular training of community health nurses.
- Strengthen monitoring and evaluation mechanisms.
Summary
- Health care planning ensures rational use of resources and equitable service delivery.
- Organization of health care follows a 3-tier system: Primary, Secondary, Tertiary.
- Community health nurses play a central role in delivery and planning at grassroots level.
- Effective planning, implementation, and evaluation is crucial for achieving Universal Health Coverage.
Steps of Health Planning
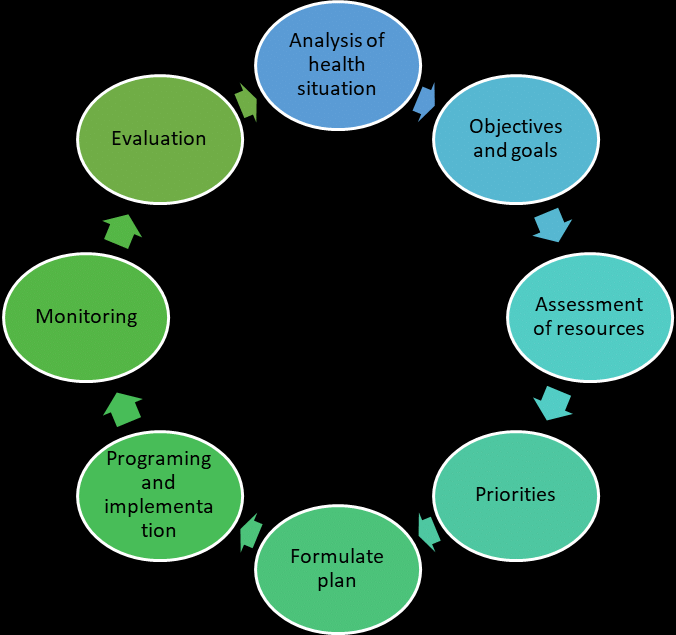
Health planning is a logical and systematic process that helps to identify health needs, set goals, and design interventions to improve community health. It is essential for resource allocation, policy development, and program implementation.
Main Steps of Health Planning
- Analysis of Health Situation
- Setting Objectives and Goals
- Assessing Resources
- Fixing Priorities
- Formulating the Plan
- Programming and Implementation
- Monitoring
- Evaluation
1. Analysis of Health Situation
Also called: Situational Analysis / Situational Assessment
This step involves collecting and analyzing data on the health status of the population.
Data includes:
- Demographics (age, sex, literacy)
- Morbidity and mortality rates
- Disease patterns (communicable/non-communicable)
- Nutritional status
- Availability and accessibility of health services
- Socio-economic and environmental factors
Purpose: To understand the baseline health needs and problems of the community.
2. Setting Objectives and Goals
After identifying problems, goals and objectives are defined.
Objectives should be:
- SMART (Specific, Measurable, Achievable, Realistic, Time-bound)
- Based on priority health issues
Example:
- Reduce IMR from 30/1000 to 20/1000 within 3 years.
- Increase institutional deliveries by 40% in rural areas.
3. Assessing Resources
This step identifies available resources to achieve objectives:
Resources include:
- Manpower: Doctors, nurses, ANMs, ASHAs
- Financial: Government grants, NHM funds
- Infrastructure: Buildings, equipment, transport
- Material: Medicines, vaccines, consumables
- Time: Timeline for implementation
Purpose: To match needs with resources or plan for additional requirements.
4. Fixing Priorities
When resources are limited, priorities must be fixed.
Criteria for prioritization:
- Magnitude of the problem
- Severity and impact on life
- Availability of cost-effective solutions
- Community concern
- Political will
Example:
- Prioritizing immunization over cosmetic surgery in rural health planning.
5. Formulating the Plan
A detailed plan is developed including:
- Activities to be done
- Personnel involved
- Target population
- Time frame
- Budget estimates
- Evaluation indicators
Plan should be: Feasible, Practical, and Inclusive
Example: PHC planning for TB control with X-ray, sputum testing, DOTS services.
6. Programming and Implementation
Plan is converted into operational programs with:
- Work plans
- Task assignments
- Training and orientation
- Resource mobilization
- Supervision guidelines
Implementation starts through existing health systems — Sub-Centres, PHCs, CHCs, and outreach programs.
7. Monitoring
Ongoing supervision and checking of the program to ensure it is:
- On track
- Achieving set objectives
- Efficiently using resources
Tools used:
- Monthly reports
- Field visits
- Performance indicators (e.g., % immunization coverage)
Community Health Nurse plays a major role in real-time monitoring.
8. Evaluation
Evaluation is the final step to measure:
- Effectiveness (Have the objectives been achieved?)
- Efficiency (Were resources used wisely?)
- Impact (Has the health status improved?)
- Sustainability (Can the benefits be maintained long-term?)
Types of Evaluation:
- Formative (during the program)
- Summative (at the end of the program)
- Impact evaluation
Summary Table
| Step | Description |
|---|---|
| 1. Situation Analysis | Identify health problems using data |
| 2. Set Objectives | Define SMART goals |
| 3. Resource Assessment | Identify manpower, funds, materials |
| 4. Priority Fixation | Choose most urgent problems |
| 5. Plan Formulation | Design a detailed action plan |
| 6. Implementation | Execute the plan on ground |
| 7. Monitoring | Track the program continuously |
| 8. Evaluation | Assess the success and areas to improve |
Role of Community Health Nurse in Health Planning
- Participates in community surveys and data collection
- Identifies local health needs
- Assists in setting realistic objectives
- Involves in mobilizing community and resources
- Implements and monitors activities
- Maintains records and submits reports
- Participates in evaluation and feedback
Health Planning in India – Various Committees on Health and Family Welfare
Introduction to Health Planning in India
- Health planning in India started after Independence (1947) to develop an organized, equitable, and efficient health care delivery system.
- The government appointed several expert committees to evaluate existing services and suggest improvements.
- These committees provided the foundation for the structure and functions of the health system in India today.
Major Health Committees in India

1. Bhore Committee (1946)
➡ Official Name: Health Survey and Development Committee
| Feature | Description |
|---|---|
| Chairperson | Sir Joseph Bhore |
| Year | 1946 (pre-independence) |
| Purpose | To survey the health conditions and recommend future planning |
Key Recommendations:
- Integration of preventive and curative services at all levels
- Primary Health Centres (PHC) to be established for 40,000 population
- Long-term goal: Health services for all without financial hardship
- Three-tier system: Primary, Secondary, Tertiary care
- Emphasis on medical education reform
🎯 Significance: Laid the foundation for modern public health system in India
2. Mudaliar Committee (1962)
➡ Official Name: Health Survey and Planning Committee
| Feature | Description |
|---|---|
| Chairperson | Dr. A. Lakshmanaswamy Mudaliar |
| Year | 1962 |
Key Recommendations:
- Strengthen existing PHCs before opening new ones
- One PHC for every 40,000 population
- Create district hospitals as referral centers
- Improve quality of medical education
- Focus on training health workers
🎯 Significance: Emphasis on quality over quantity in health services
3. Chadah Committee (1963)
➡ Related to Family Planning
| Feature | Description |
|---|---|
| Chairperson | Dr. M.S. Chadah |
| Year | 1963 |
Key Recommendations:
- Combine family planning with general health services
- Use Basic Health Workers (BHW) to deliver services
- Emphasized follow-up services and maintaining family planning records
🎯 Significance: Integration of Family Planning with existing health structure
4. Mukherjee Committee (1965 & 1966)
| Year | Purpose |
|---|---|
| 1965 | Review family planning implementation |
| 1966 | Re-evaluation of urban family planning strategies |
Key Recommendations:
- Separate staff for Family Planning Services
- Establish Family Planning Stores
- Appoint a District Family Planning Officer
🎯 Significance: Laid groundwork for independent Family Welfare Programs
5. Jungalwalla Committee (1967)
➡ Focus on Integration of Health Services
| Chairperson | Dr. Jungalwalla |
Key Recommendations:
- Unified cadre of health services (no separate cadres)
- Common seniority, equal pay for equal work
- Eliminate private practice by government doctors
- Better service conditions for health workers
🎯 Significance: Proposed integration of preventive, promotive, and curative services
6. Kartar Singh Committee (1973)
| Chairperson | Kartar Singh | | Year | 1973 |
Key Recommendations:
- Multipurpose workers scheme
- Suggested replacing multiple field workers with one Multipurpose Health Worker (MPHW)
- Sub-centre for 3,000-5,000 population
- Supervisory staff structure with Health Supervisor (Male & Female)
🎯 Significance: Rationalized and simplified field-level staffing in rural health services
7. Srivastava Committee (1975)
➡ Also known as: Group on Medical Education and Support Manpower
| Chairperson | Dr. J.S. Srivastava | | Year | 1975 |
Key Recommendations:
- Develop Community Health Worker (CHW) at village level
- Launch a new cadre of Health Assistants
- Medical and nursing education to be restructured towards rural needs
- Introduction of Village Health Guides (VHG)
🎯 Significance: Led to concept of community participation in health care delivery
8. Bajaj Committee (1986)
➡ Focus: Health manpower planning and development
| Chairperson | Prof. J.S. Bajaj |
Key Recommendations:
- Create national health manpower planning body
- Reform medical, nursing, and paramedical education
- Strengthen health education and research
- Improve career structure of health workers
🎯 Significance: Provided strategies for HR development in health sector
9. Krishnan Committee (1992)
➡ Focus: Voluntary sector participation in health
🔹 Key Recommendations:
- Encourage NGOs and private sector to participate in health care
- Promote public-private partnerships (PPP)
10. National Health Policy Committees (1983, 2002, 2017)
| Year | Focus |
|---|---|
| 1983 | Access to primary care and health for all by 2000 |
| 2002 | Health equity, public-private partnerships |
| 2017 | Universal Health Coverage (UHC), wellness centres, digital health |
🎯 Significance: Guide long-term national planning and priorities
Summary Table – Health Committees in India
| Committee | Year | Focus / Contribution |
|---|---|---|
| Bhore | 1946 | Foundation of Indian health system |
| Mudaliar | 1962 | Improve quality of PHCs and education |
| Chadah | 1963 | Family planning integration |
| Mukherjee | 1965–66 | Dedicated family planning structure |
| Jungalwalla | 1967 | Unified health services |
| Kartar Singh | 1973 | Multipurpose worker scheme |
| Srivastava | 1975 | Community-based workers |
| Bajaj | 1986 | Health manpower development |
| Krishnan | 1992 | Voluntary sector involvement |
| NHP Committees | 1983–2017 | National health policy planning |
Role of Community Health Nurse Based on Recommendations
- Acts as Multipurpose Worker (MPHW) at sub-centres
- Provides maternal, child health, and family welfare services
- Works in coordinated team at PHCs/CHCs
- Acts as community mobilizer and educator
- Maintains health records, immunization registers, and family planning data
- Participates in program implementation and evaluation
Health Planning in India – Various Commissions on Health and Family Welfare
While Committees are temporary expert groups formed for specific health planning issues, Commissions are usually more broad-based and permanent or long-term advisory bodies. Several important Health Commissions have influenced India’s health and family welfare planning over time.
1. Bhore Commission (1943–1946)
➡ Official Name: Health Survey and Development Committee
➡ Commissioned by: British Government of India
| Details | Description |
|---|---|
| Chairperson | Sir Joseph Bhore |
| Year of Report | 1946 |
| Purpose | Comprehensive health system development before Indian independence |
Major Recommendations:
- Integration of preventive and curative services.
- Establish Primary Health Centres (PHCs) for 40,000 people.
- Emphasized free health services for all.
- Development of district hospitals as referral units.
- Reforms in medical education, including community-oriented training.
🎯 Impact: Foundation of modern Indian health system and inspiration for post-independence health planning.
2. National Commission on Macroeconomics and Health (NCMH) – 2005
| Details | Description |
|---|---|
| Established by | Ministry of Health and Family Welfare (MoHFW) |
| Year | 2005 |
| Chairperson | Dr. S. Narayan (former Finance Secretary) |
Key Focus Areas:
- Linking economic growth with health investment.
- Evaluate economic impact of diseases like TB, HIV, NCDs.
- Recommended increased public health spending up to 2–3% of GDP.
- Promote universal access to essential health services.
🎯 Impact: Influenced the framing of National Health Policy 2017 and government health financing strategy.
3. National Commission on Population (NCP)
| Details | Description |
|---|---|
| First Established | 2000 |
| Reconstituted | 2020 |
| Chairperson | Prime Minister of India |
| Vice Chair | Union Minister of Health & Family Welfare |
Objectives:
- Monitor and implement National Population Policy (2000).
- Guide population stabilization efforts.
- Coordinate family planning programs with state governments.
- Support maternal and child health improvements.
🎯 Impact: Ensures long-term planning for population control and demographic management.
4. Law Commission of India (Relevant for Health Law)
Though not a health-specific commission, the Law Commission has periodically submitted reports affecting health and family welfare, such as:
- Surrogacy laws
- Abortion and reproductive rights
- Organ transplantation
- Medical negligence laws
🎯 Impact: Influences the legal framework of healthcare in India.
5. Finance Commission of India (Health Grants)
| Details | Description |
|---|---|
| Recent Commission | 15th Finance Commission |
| Chairperson | N. K. Singh |
Health-Related Recommendations:
- Tied grants for primary health care to urban and rural local bodies.
- Emphasis on strengthening infrastructure at the grassroots.
- Focus on water, sanitation, nutrition, and immunization.
🎯 Impact: Ensures fiscal support for health sector from the central government to states.
6. NITI Aayog (Previously Planning Commission)
| Old Name | Planning Commission (till 2014) | | New Name | NITI Aayog (2015 onward) | | Role | National strategic planning body |
Health Focus:
- Published Health Index Reports (state-wise performance).
- Promotes public-private partnerships (PPP) in health.
- Suggests reforms for Ayushman Bharat, digital health, telemedicine.
- Encourages State-level health innovation.
🎯 Impact: Key driver of modern policy-level planning and innovation in health care.
Summary Table – Important Health Commissions in India
| Commission | Year | Chairperson | Key Contributions |
|---|---|---|---|
| Bhore Commission | 1946 | Sir Joseph Bhore | Foundation of Indian health system, PHCs |
| NCMH | 2005 | Dr. S. Narayan | Health investment, economic impact of disease |
| Population Commission | 2000 / 2020 | PM of India | Population stabilization, family welfare |
| Law Commission | Ongoing | Varies | Legal framework for health and family welfare |
| Finance Commission | 2021 (15th) | N.K. Singh | Tied grants for health infrastructure |
| NITI Aayog | 2015 onward | PM-led | Health reforms, policy innovation, health index |
Role of Community Health Nurse in Implementation of Commission Recommendations
- Helps in population stabilization by educating on family planning.
- Implements maternal and child health programs.
- Coordinates with ASHA, Anganwadi workers for outreach services.
- Participates in health surveys, immunization, and nutrition programs.
- Assists in collecting data used for health planning and policy evaluation.
Five-Year Plans in India
Introduction
- The Five-Year Plans (FYPs) were national level strategies for economic development in India.
- Launched in 1951 under the Planning Commission.
- Aimed to improve agriculture, industry, education, health, and infrastructure.
- Health and Family Welfare was a key component in each plan.
- Discontinued in 2017, replaced by NITI Aayog’s strategic planning.
Detailed Overview of Each Five-Year Plan (with Health Focus)
1st Five-Year Plan (1951–1956)
➡ Focus: Agriculture, Community Development
| Health Achievements |
|---|
- Strengthening Primary Health Centres (PHCs).
- National Malaria Control Programme (1953).
- Bhopal Memorial Hospital initiated.
- Focus on rural health and nutrition.
2nd Five-Year Plan (1956–1961)
➡ Focus: Industrialization and Health Expansion
| Health Achievements |
|---|
- Health Survey & Planning Committee (Mudaliar Committee) formed.
- Strengthening District Hospitals and referral services.
- Emphasis on medical and nursing education.
- Expanded Family Planning Programmes.
3rd Five-Year Plan (1961–1966)
➡ Focus: Self-reliance in economy and health manpower
| Health Achievements |
|---|
- Launched National Smallpox Eradication Programme.
- Introduction of School Health Services.
- Expanded Family Planning and Nutrition Programs.
Plan Holiday (1966–1969)
Due to wars and droughts. Annual Plans instead.
4th Five-Year Plan (1969–1974)
➡ Focus: Growth with Stability
| Health Achievements |
|---|
- Expansion of rural health infrastructure.
- Launch of Minimum Needs Programme (MNP) – Health, water, housing.
- Integrated Maternal & Child Health (MCH) services.
5th Five-Year Plan (1974–1979)
➡ Focus: Poverty Eradication and Self-reliance
| Health Achievements |
|---|
- Integrated Child Development Services (ICDS) launched (1975).
- Introduction of Multipurpose Health Worker Scheme (Kartar Singh Committee).
- Srivastava Committee proposed Village Health Guides (VHGs).
6th Five-Year Plan (1980–1985)
➡ Focus: Health for All by 2000
| Health Achievements |
|---|
- Launch of National Health Policy (1983).
- Strengthening PHCs and CHCs.
- Emphasis on RCH, immunization, sanitation.
7th Five-Year Plan (1985–1990)
➡ Focus: Social Justice and Technology
| Health Achievements |
|---|
- Expanded Universal Immunization Programme (UIP).
- Focus on AIDS Control, TB, Leprosy.
- Strengthened rural health manpower.
Annual Plans (1990–1992)
Transition phase due to political instability.
8th Five-Year Plan (1992–1997)
➡ Focus: Human Development, Health for All
| Health Achievements |
|---|
- Launch of Child Survival and Safe Motherhood Programme (CSSM).
- Emphasis on women and child health.
- Expanded education and training of nurses.
9th Five-Year Plan (1997–2002)
➡ Focus: Quality of Life and Population Control
| Health Achievements |
|---|
- Launch of Reproductive and Child Health (RCH).
- Emphasis on population stabilization.
- Focus on tribal and backward areas.
10th Five-Year Plan (2002–2007)
➡ Focus: Health Indicators – IMR, MMR, TFR
| Health Goals |
|---|
- IMR < 45/1000 live births
- MMR < 2/1000 live births
- TFR = 2.1
- Focus on gender equality, access to basic services.
11th Five-Year Plan (2007–2012)
➡ Focus: Inclusive Growth
| Health Achievements |
|---|
- Launch of National Rural Health Mission (NRHM).
- Focus on maternal and newborn care.
- Janani Suraksha Yojana (JSY) for institutional delivery.
- Infrastructure strengthening of PHCs, SCs, CHCs.
12th Five-Year Plan (2012–2017)
➡ Focus: Faster, Sustainable, and Inclusive Growth
| Health Achievements |
|---|
- NRHM expanded to National Health Mission (NHM).
- Emphasis on universal health coverage.
- Focus on non-communicable diseases (NCDs).
- Launch of Rashtriya Bal Swasthya Karyakram (RBSK).
Discontinuation of Five-Year Plans (2017)
- Planning Commission replaced by NITI Aayog (2015).
- Five-Year Plans discontinued after 12th Plan.
- Now replaced by 3-Year Action Plans, 7-Year Strategy Papers, and 15-Year Vision Documents by NITI Aayog.
Summary Chart – Health Achievements across Five-Year Plans
| Plan | Key Health Initiatives |
|---|---|
| 1st | PHCs, Malaria control |
| 2nd | Mudaliar Committee, FP expansion |
| 3rd | Smallpox, School Health |
| 4th | Minimum Needs Programme |
| 5th | ICDS, Multipurpose workers |
| 6th | NHP 1983, HFA by 2000 |
| 7th | AIDS control, UIP |
| 8th | CSSM, nursing education |
| 9th | RCH program |
| 10th | IMR/MMR/TFR targets |
| 11th | NRHM, JSY |
| 12th | NHM, RBSK, UHC |
Role of Community Health Nurse in Five-Year Plan Implementation
- Works in PHCs and SCs under NRHM/NHM.
- Implements MCH, immunization, family planning programs.
- Participates in health surveys and data collection.
- Delivers health education and counseling.
- Acts as link between community and health system.
Participation of Community and Stakeholders in Health Planning
What is Participation in Health Planning?
Participation means actively involving the community and other stakeholders in the decision-making, planning, implementation, and evaluation of health services and programs.
This ensures that health plans reflect the real needs of the population and encourages ownership, accountability, and sustainability of health programs.
Importance of Participation
| Why It’s Important | Explanation |
|---|---|
| Need-based planning | Community knows its own problems best |
| Better acceptance | People support what they help to build |
| Efficient resource use | Helps mobilize local resources |
| Transparency and accountability | Builds trust in the health system |
| Sustainability | People continue the activities even after programs end |
Who Are the Stakeholders?
Stakeholders are individuals or groups who have an interest or role in health services.
Types of Stakeholders in Health Planning
- Community Members
- Village leaders, women’s groups, adolescents, elderly, etc.
- Local Health Workers
- ANM, ASHA, MPHW, Staff Nurses
- Government Departments
- Panchayati Raj, Health & Family Welfare, Education, Women & Child Development
- Non-Governmental Organizations (NGOs)
- e.g., CARE, UNICEF, CRY
- Private Sector Partners
- Local hospitals, doctors, pharmacies
- Community-Based Organizations (CBOs)
- Self-help groups (SHGs), youth clubs
- Donor Agencies
- WHO, UNDP, World Bank, USAID
Levels of Community Participation (As per WHO)
| Level | Description |
|---|---|
| Information | People are informed of the plan |
| Consultation | People give suggestions |
| Involvement | People take part in activities |
| Collaboration | Shared decision-making |
| Empowerment | Community has full control |
Ways of Community and Stakeholder Participation
| Method | Description |
|---|---|
| Village Health Sanitation and Nutrition Committee (VHSNC) | Local body to plan and monitor health services |
| Rogi Kalyan Samiti (RKS) | Patient welfare committee at PHC/CHC level |
| Gram Sabhas | Community meetings for planning and feedback |
| Participatory Rural Appraisal (PRA) | Mapping and analyzing village health issues with community |
| Public Hearings (Jan Sunwai) | People give opinions and complaints about health services |
| Self-Help Groups (SHGs) | Women-led microfinance groups involved in health awareness |
| ASHA Meetings | Platform to collect feedback and plan health outreach |
Examples of Community Participation in India
- ASHA workers: Chosen by the community, deliver care at home.
- JSY Scheme: Promotes institutional delivery through community mobilization.
- RBSK: School-based health check-up program involving teachers and parents.
- Swachh Bharat Mission: Community-led total sanitation campaign.
Role of Community Health Nurse in Promoting Participation
| Role | Details |
|---|---|
| Facilitator | Organizes meetings with community and stakeholders |
| Educator | Raises awareness about health issues and services |
| Mobilizer | Encourages community involvement in health campaigns |
| Coordinator | Links health department and local people |
| Advocate | Voices community needs to higher authorities |
| Trainer | Trains ASHAs, SHG leaders, youth volunteers |
Barriers to Participation
- Low literacy or awareness
- Cultural or gender bias
- Lack of trust in authorities
- Dominance of powerful groups
- Inadequate incentives or follow-up
Ways to Improve Participation
- Conduct health education programs
- Encourage inclusive leadership (women, youth, marginalized)
- Strengthen local health committees
- Provide training and incentives to volunteers
- Promote transparency and feedback mechanisms
Conclusion
Community and stakeholder participation in health planning:
- Promotes people-centered health services
- Improves quality, equity, and accountability
- Leads to sustainable health outcomes
It is not just a strategy, but a right and responsibility of every citizen and health worker.
Health Care Delivery System in India
1. Introduction
The health care delivery system in India refers to the organization of people, institutions, and resources to deliver health services to meet the health needs of the population.
It includes public and private sectors, and it operates at primary, secondary, and tertiary levels, supported by health programs, health workers, and community involvement.
2. Objectives of Health Care Delivery System
- To provide equitable and accessible health care to all.
- To deliver preventive, promotive, curative, and rehabilitative services.
- To reduce morbidity and mortality.
- To promote community participation and health awareness.
- To ensure universal health coverage (UHC).
3. Structure of Health Care System in India
India follows a three-tier health system, particularly in the public sector:
A. Primary Level (First Contact Point)
➡ Delivers basic health services at the grassroots level.
a) Sub-Centre (SC)
- Coverage: 5,000 population (3,000 in hilly/tribal)
- Staff: 1 ANM (female), 1 MPHW (male), ASHAs
- Services:
- Maternal and child health (MCH)
- Immunization
- Family planning
- Home visits and outreach
- Health education
b) Primary Health Centre (PHC)
- Coverage: 30,000 population (20,000 in hilly)
- Staff: Medical Officer, Nurse, Pharmacist, Lab Tech
- Services:
- Outpatient care
- Minor treatments
- Antenatal/Postnatal care
- Disease control programs
- Referral services
B. Secondary Level (Referral Care)
➡ Provides specialist services and handles referrals from PHCs.
a) Community Health Centre (CHC)
- Coverage: 1.2 lakh population (80,000 in hilly)
- 30-bed hospital
- Staff: 4 specialists – Surgeon, Physician, Gynecologist, Pediatrician + support staff
- Services:
- Emergency care
- Basic surgeries
- Institutional deliveries
- Referral care
b) Sub-District Hospitals / Taluka Hospitals
- Act as first-level referral hospitals
- Offer specialist and inpatient care
C. Tertiary Level (Advanced/Super-Specialty Care)
➡ Provides advanced diagnostic, therapeutic, and surgical care.
Institutions:
- District Hospitals
- Medical Colleges
- AIIMS, PGIs, Specialty Institutes
- Services:
- ICU, NICU, CCU
- Multi-specialty surgeries
- Advanced diagnostics
- Research and training
4. Types of Health Care Providers in India
| Sector | Examples |
|---|---|
| Public Sector | Sub-Centres, PHCs, CHCs, District Hospitals, AIIMS |
| Private Sector | Private clinics, hospitals, nursing homes |
| Voluntary Sector | NGOs (e.g., CRY, SEWA), Mission hospitals |
| Indigenous Systems | AYUSH – Ayurveda, Yoga, Unani, Siddha, Homeopathy |
| Corporate Sector | Apollo, Fortis, Max Hospitals |
5. National Health Programs Supporting the Delivery System
- National Health Mission (NHM)
- Reproductive, Maternal, Newborn, Child and Adolescent Health (RMNCH+A)
- Janani Suraksha Yojana (JSY)
- Ayushman Bharat – PMJAY
- National TB Elimination Program
- Universal Immunization Program (UIP)
6. Human Resources in the Health System
| Cadre | Role |
|---|---|
| ASHA | Bridge between community & health facility |
| ANM / MPHW | Frontline workers at sub-centre |
| Staff Nurse | Provides nursing care at PHC, CHC, hospital |
| Medical Officer | Diagnoses and treats at PHC/CHC level |
| Specialists | Secondary & tertiary care providers |
| District Health Officers | Supervise district-level health services |
7. Role of Central and State Governments
| Authority | Responsibility |
|---|---|
| Central Government | National health policies, major programs, funding |
| State Government | Implementation of health programs, infrastructure, HR |
| Panchayati Raj Institutions (PRIs) | Local-level health planning and monitoring (VHSNC, RKS) |
8. Recent Innovations in Health Delivery
| Innovation | Description |
|---|---|
| Health & Wellness Centres (HWCs) | Strengthened SCs/PHCs offering expanded primary care |
| Telemedicine | Remote consultations and e-health |
| Digital Health Mission | Health ID, electronic health records |
| Mobile Medical Units | Reach remote and underserved areas |
| eSanjeevani | Government’s free teleconsultation platform |
9. Role of Community Health Nurse in Health Care Delivery
- Provides home-based care and health education
- Supports immunization, ANC/PNC, family planning
- Maintains records and reports
- Acts as link between people and system
- Conducts screening and referrals
- Promotes community participation and awareness
10. Challenges in Indian Health System
- Inadequate infrastructure in rural areas
- Shortage of trained health workforce
- Unequal access across urban-rural areas
- High out-of-pocket expenditure
- Poor coordination between sectors
Suggestions for Improvement
- Strengthening primary health care
- Promoting public-private partnerships
- Regular training of health workers
- Encouraging community ownership
- Ensuring equity and quality in care
Infrastructure and Health Sectors, Delivery of Health Services at Sub-Centre (SC)
1. What is Health Infrastructure?
Health infrastructure refers to the physical and organizational structures, human resources, equipment, and services required to deliver health care effectively.
Components of Health Infrastructure
| Component | Includes |
|---|---|
| Buildings | Sub-centres, PHCs, CHCs, Hospitals |
| Manpower | ANM, MPHW, Doctors, Specialists |
| Equipment | BP machine, delivery table, lab kits |
| Transport | Ambulance, mobile medical units |
| Drugs and Supplies | Vaccines, contraceptives, essential medicines |
| ICT | Health Management Information System (HMIS), Telemedicine, eHealth |
2. Health Sectors in India
Health services in India are delivered through different sectors:
A. Public Sector
- Government Sub-centres, PHCs, CHCs, District hospitals
- Funded by: Central and State Governments
- Mission: Provide free/affordable services to all
B. Private Sector
- Clinics, Nursing homes, Hospitals
- Profit-oriented, but important contributor to health services
C. Voluntary Sector
- NGOs, Charitable hospitals
- Often work in rural, tribal, and underserved areas
D. Indigenous Systems (AYUSH)
- Ayurveda, Yoga, Unani, Siddha, Homeopathy
- Promoted by Ministry of AYUSH
3. Sub-Centre (SC): The First Contact Point
Definition:
A Sub-Centre is the most peripheral and first contact point between the community and the health system.
Population Coverage
- 5,000 in plain areas
- 3,000 in hilly, tribal, or difficult areas
Staffing at Sub-Centre
| Staff | Role |
|---|---|
| ANM (Auxiliary Nurse Midwife) – Female | Provides maternal & child health, immunization, FP services |
| MPHW (Male) | Disease control, sanitation, health education |
| ASHA (Accredited Social Health Activist) | Community link, mobilization, home visits |
| Optional: Second ANM or Health Assistant (under NHM) |
4. Delivery of Health Services at Sub-Centre
Sub-Centre provides preventive, promotive, and limited curative services:
A. Maternal Health Services
- Antenatal check-ups (ANC)
- Iron and folic acid (IFA) tablet distribution
- Tetanus toxoid immunization
- Identification of high-risk pregnancies
- Referral to PHC/CHC
- Health education on pregnancy care
B. Child Health Services
- Newborn care and home visits
- Immunization (as per UIP schedule)
- Vitamin A supplementation
- Growth monitoring
- Management of childhood illnesses (e.g., diarrhea, ARI)
C. Family Planning Services
- Counselling for spacing and permanent methods
- Distribution of oral pills and condoms
- Follow-up of IUCD users
- Community-based depot holder (CBD) services
D. Adolescent Health Services
- Menstrual hygiene education
- Counseling for nutrition, anemia, substance abuse
E. Disease Control Activities
- Malaria, TB, Leprosy detection
- Distribution of medicines and follow-up
- Fever surveillance and sample collection
- Vector control activities
F. National Health Programs
- Universal Immunization Program (UIP)
- Janani Suraksha Yojana (JSY)
- Ayushman Bharat (HWC Model)
- National Nutrition Mission
- COVID-19 vaccination and awareness
G. Environmental Sanitation
- Safe water supply
- Construction and use of toilets
- Promotion of hygiene and cleanliness
- School health and sanitation awareness
H. Health Education and Counseling
- On nutrition, hygiene, breastfeeding, immunization
- Use of IEC (Information, Education, Communication) materials
I. Record Maintenance and Reporting
- Eligible couple register
- Antenatal/postnatal register
- Immunization records
- Births and deaths data
- Monthly reporting to PHC/Block
Sub-Centre Upgradation – Health & Wellness Centres (HWCs)
Under Ayushman Bharat Mission, SCs are being upgraded into HWCs to provide:
- Expanded range of primary care services
- Management of non-communicable diseases (NCDs)
- Mental health services
- Telemedicine and digital health records
Role of Community Health Nurse (ANM) at Sub-Centre
| Role | Responsibilities |
|---|---|
| Service provider | MCH, FP, immunization, first aid |
| Educator | Health talks, counseling, school health |
| Coordinator | Coordinates with ASHA, Anganwadi |
| Recorder | Maintains all SC registers and reports |
| Referral agent | Identifies danger signs and refers cases |
| Community mobilizer | Promotes participation in health programs |
Challenges at Sub-Centre Level
- Inadequate infrastructure or space
- Shortage of trained manpower
- Irregular supply of medicines and vaccines
- Difficult terrain or remote locations
- Overburdened ANMs
Suggestions for Improvement
- Regular supply of essential drugs and logistics
- Training and capacity building for ANMs
- Timely salary and incentive for ASHAs
- Strengthening HWC model
- Community participation through VHSNCs
Primary Health Centre (PHC)
1. What is a Primary Health Centre (PHC)?
A Primary Health Centre (PHC) is the first contact point between a village community and a Medical Officer. It acts as a referral unit for Sub-Centres (SCs) and provides integrated curative and preventive health care to the rural population.
Coverage & Staffing
| Criteria | Details |
|---|---|
| Population Coverage | 30,000 in plain areas, 20,000 in hilly/tribal areas |
| Supervises | 5–6 Sub-Centres |
| Staff (as per IPHS) | 1 Medical Officer (MBBS), 1 AYUSH doctor, 3 Staff Nurses, 1 Pharmacist, 1 Lab Technician, 1 Health Educator, 1 Health Assistant (Male & Female), Clerical staff, Class IV |
2. Infrastructure of a PHC
- 6 to 10 bedded facility (for in-patient care)
- Outpatient consultation room
- Labour room
- Minor Operation Theatre (OT)
- Laboratory, Pharmacy
- Staff quarters
- Drinking water and electricity
- Waste management system
3. Services Delivered at PHC Level
PHC provides preventive, promotive, curative, and family welfare services.
A. Outpatient Care (OPD Services)
- Diagnosis and treatment of common illnesses
- Management of minor injuries
- Screening for NCDs (diabetes, hypertension)
B. Maternal and Child Health Services
- Antenatal and postnatal care (ANC/PNC)
- Safe and clean deliveries
- Referral of high-risk pregnancies
- Immunization of infants and pregnant women
C. Family Planning Services
- Counseling on family planning methods
- Distribution of condoms, OCPs
- IUCD insertion
- Referrals for sterilization (tubectomy/vasectomy)
D. National Health Programs Implementation
- Tuberculosis (NTEP)
- Leprosy (NLEP)
- Malaria (NVBDCP)
- AIDS (NACP)
- Immunization (UIP)
- NCDs, Mental health, School health programs
E. Laboratory Services
- Blood tests, urine tests, malaria smears
- Pregnancy test, hemoglobin estimation
F. Basic In-patient Services
- Observation beds for minor ailments
- Post-delivery stay and monitoring
- Minor surgical procedures
G. Emergency and First Aid
- Snake bite, dog bite, poisoning
- First aid for injuries, burns, accidents
H. Health Education and Counseling
- Nutrition, hygiene, breastfeeding
- Substance abuse prevention
- Adolescent reproductive health
I. Referral Services
- To CHC/District hospital for specialized care
- Transport via ambulance (Janani Express, 108)
J. Administrative and Supervisory Role
- Supervises Sub-Centres and ASHAs
- Reviews performance of ANMs, MPHWs
- Monthly meetings and data reporting
PHC as Health & Wellness Centre (HWC-PHC)
Under Ayushman Bharat, PHCs are being upgraded to Health & Wellness Centres offering:
- Expanded services (mental health, NCDs, elderly care)
- Free essential drugs and diagnostics
- Telemedicine facilities
- Community outreach via ASHAs and CHOs
Role of Community Health Nurse / Staff Nurse at PHC
| Role | Responsibilities |
|---|---|
| Care Provider | Administers injections, dressings, IV fluids |
| MCH Services | Assists in deliveries, ANC/PNC care |
| Immunization | Conducts RI sessions, cold chain maintenance |
| Health Educator | Conducts group talks, IEC activities |
| Team Leader | Supervises MPHWs, ANMs, ASHAs |
| Record Keeper | Maintains registers, reporting formats |
| Referral Agent | Identifies complications and arranges transport |
Challenges at PHC Level
- Staff shortages (especially doctors and nurses)
- Inadequate infrastructure
- Irregular supply of drugs and consumables
- Poor transport/referral systems
- Low community participation
Suggestions for Improvement
- Fill all sanctioned posts
- Upgrade PHCs to HWCs with better equipment
- Ensure drug supply and lab services
- Strengthen referral linkage and transport
- Promote use of digital tools (eSanjeevani, HMIS)
Community Health Centre (CHC)
1. What is a CHC (Community Health Centre)?
A Community Health Centre (CHC) is a secondary-level referral health facility. It provides specialist care to patients referred from Primary Health Centres (PHCs) and serves a larger population in rural and semi-urban areas.
Coverage & Role
| Criteria | Description |
|---|---|
| Population Coverage | 1,20,000 in plain areas; 80,000 in hilly/tribal areas |
| Supervises | 4 PHCs and their Sub-Centres |
| Type of Facility | 30-bed hospital with specialist services |
| Role | First referral unit (FRU) for complicated cases from PHCs |
2. Infrastructure as per IPHS (Indian Public Health Standards)
- 30 beds for inpatient care
- Separate OPD and IPD wards
- Operation Theatre (OT)
- Labour Room
- Laboratory, X-ray, Ultrasound
- Blood Storage Unit
- Ambulance Services (108 or Janani Express)
- Staff Quarters for Doctors and Nurses
- Power backup and sanitation facilities
3. Staffing Pattern of a CHC
| Cadre | Numbers (as per IPHS) |
|---|---|
| Specialists | 4 – Surgeon, Physician, Obstetrician/Gynaecologist, Pediatrician |
| Medical Officers | 3–5 (including AYUSH) |
| Staff Nurses | 7–10 |
| Pharmacist, Lab Tech, Radiographer | 1 each |
| ANMs, MPWs, Health Assistants | As per catchment |
| Support Staff (Ward boys, cleaners, driver) | As needed |
4. Services Delivered at CHC Level
CHCs provide both outpatient and inpatient services, with an emphasis on emergency, specialist, and surgical care.
A. Outpatient (OPD) Services
- Daily consultation by medical officers and specialists
- Management of non-communicable and communicable diseases
- Minor ailments and routine follow-up
B. Inpatient (IPD) Services
- Admission for illnesses, injuries, and surgical recovery
- Bed occupancy for deliveries and postnatal care
- Observation of emergency cases
C. Emergency Services
- 24×7 emergency care for trauma, delivery, poisoning, accidents
- First aid for animal bites, burns, and shock
- Management of obstetric emergencies (e.g., eclampsia, PPH)
D. Maternal and Child Health Services
- Institutional deliveries
- Emergency Obstetric Care (EmOC)
- Antenatal/Postnatal care
- Caesarean sections (if FRU designated)
- Newborn care (NBCC, SNCU in some CHCs)
E. Surgical Services
- Appendectomy, hernia repair, abscess drainage
- Minor and emergency surgeries under general/local anesthesia
F. Family Planning Services
- Sterilization procedures (Tubectomy/Vasectomy)
- IUCD insertion and contraceptive counseling
- Follow-up services
G. National Health Programs
- Tuberculosis (DOTS)
- Leprosy, HIV/AIDS, Malaria
- RCH, NCDs, School Health Program
- Immunization, JSY, JSSK implementation
H. Laboratory and Diagnostic Services
- Blood tests, urine tests, X-ray
- ECG and ultrasonography (if available)
- Blood grouping and cross-matching
I. Referral Services
- Acts as referral for PHCs
- Refers further complicated cases to District Hospital or Medical College
5. CHC as First Referral Unit (FRU)
Many CHCs are upgraded as FRUs (First Referral Units) if they fulfill:
- 24×7 delivery and caesarean services
- Newborn care
- Blood storage unit
- Emergency care (esp. obstetrics)
6. Role of Community Health Nurse / Staff Nurse at CHC
| Role | Responsibilities |
|---|---|
| Nursing Care | IPD and emergency care |
| Labour Room Duty | Assisting normal and caesarean deliveries |
| OT Nurse | Assisting surgeries |
| Immunization | Coordination with ANMs and ASHAs |
| Health Education | Conducting sessions for OPD and inpatients |
| Records & Reports | Documentation of services provided |
| Supervision | Guides ANMs and field staff during referrals |
7. Challenges at CHC Level
- Shortage of specialists in rural areas
- Inadequate equipment or power backup
- Irregular drug and supply chain
- Infrastructural limitations (e.g., lack of blood storage or OT)
- Poor referral transportation
8. Suggestions for Improvement
- Fill specialist posts through incentives and telemedicine
- Upgrade all CHCs to fully functional FRUs
- Strengthen referral linkages with PHCs and District Hospitals
- Provide continuous training and skill upgradation for staff
- Community involvement via Rogi Kalyan Samitis (RKS)
District-Level Health Care Delivery System in India

1. Introduction
At the district level, health services form the link between state-level and block-level health care. It is responsible for planning, implementation, monitoring, and supervision of all health programs and services within a district.
Each district has a District Health Society (DHS) under the National Health Mission (NHM) that ensures coordinated functioning of all health institutions.
2. Key Components at the District Level
A. District Hospital (DH)
| Criteria | Details |
|---|---|
| Population Coverage | ~10–20 lakh |
| Bed Strength | 100–500 beds |
| Services Provided | Inpatient & outpatient care, emergency, surgeries, specialist services |
| Staff | Specialists (Medicine, Surgery, Ob-Gyn, Pediatrics, etc.), Nurses, Lab technicians, Pharmacists |
Functions:
- Serves as referral center for CHCs and PHCs.
- Provides secondary-level health care.
- Acts as training center for health personnel.
- Handles disaster and emergency preparedness.
- Implements national health programs.
B. District Health Office (DHO)
| Post | Role |
|---|---|
| Chief Medical Officer (CMO) / Civil Surgeon | Head of all health services in the district |
| District Health Officer (DHO) | Supervises rural health services |
| District Program Officers | Handle specific health programs (e.g., TB, NCD, Immunization) |
| District RCH Officer | Monitors maternal and child health services |
C. District Health Society (DHS)
Under National Health Mission (NHM)
Functions:
- Coordinates all public health programs.
- Ensures proper fund utilization.
- Involves community and PRIs in planning.
- Prepares District Health Action Plan (DHAP).
3. Health Facilities at District Level
| Facility | Role |
|---|---|
| District Hospital (DH) | Secondary/tertiary care |
| Sub-District Hospitals / Civil Hospitals | Intermediate referral |
| CHCs | First referral unit |
| PHCs & Sub-Centres | Primary care |
| Urban Primary Health Centres (UPHCs) | Urban health delivery |
| Mobile Medical Units (MMUs) | Outreach to remote areas |
4. Services Delivered at District Level
| Area | Services |
|---|---|
| Curative | Inpatient care, surgeries, specialist OPDs |
| Preventive | Immunization, health awareness, disease prevention |
| Promotive | Nutrition, lifestyle modification programs |
| Rehabilitative | Disability rehabilitation, physiotherapy |
| Support Services | Blood banks, diagnostic labs, ambulance |
5. National Health Programs Implemented at District Level
- National Tuberculosis Elimination Program (NTEP)
- Reproductive and Child Health (RCH)
- National Vector Borne Disease Control Program (NVBDCP)
- National Leprosy Eradication Program (NLEP)
- Rashtriya Bal Swasthya Karyakram (RBSK)
- National Program for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases and Stroke (NPCDCS)
- Janani Suraksha Yojana (JSY) and Janani Shishu Suraksha Karyakram (JSSK)
6. Role of District-Level Nurses / CHNs / Public Health Nurses
| Role | Responsibility |
|---|---|
| Service provider | Hospital and community-based nursing |
| Trainer | Helps train ANMs, ASHAs, and staff nurses |
| Supervisory role | Monitors PHC and CHC functioning |
| Data Management | Health records, reporting to state HQ |
| Community Engagement | Mobilizing participation through VHNSC, SHGs |
| Emergency Response | Participates in district disaster management and outbreak control |
7. Monitoring and Evaluation
- Health Management Information System (HMIS) reporting
- District Health Surveys
- Review Meetings with PHC/CHC in-charges
- Annual District Health Action Plan (DHAP) preparation and review
8. Challenges at District Level
- Staff vacancies in specialist and nursing positions
- Inadequate infrastructure in sub-district hospitals
- Delays in fund release and utilization
- Data gaps and poor reporting
- Overcrowding in district hospitals
9. Suggestions for Improvement
- Strengthen referral linkages and transport
- Timely recruitment of specialists and nurses
- Upgrade district hospitals as teaching and training centers
- Improve data quality and digital systems
- Enhance public-private partnerships
State-Level Health Care Delivery System in India
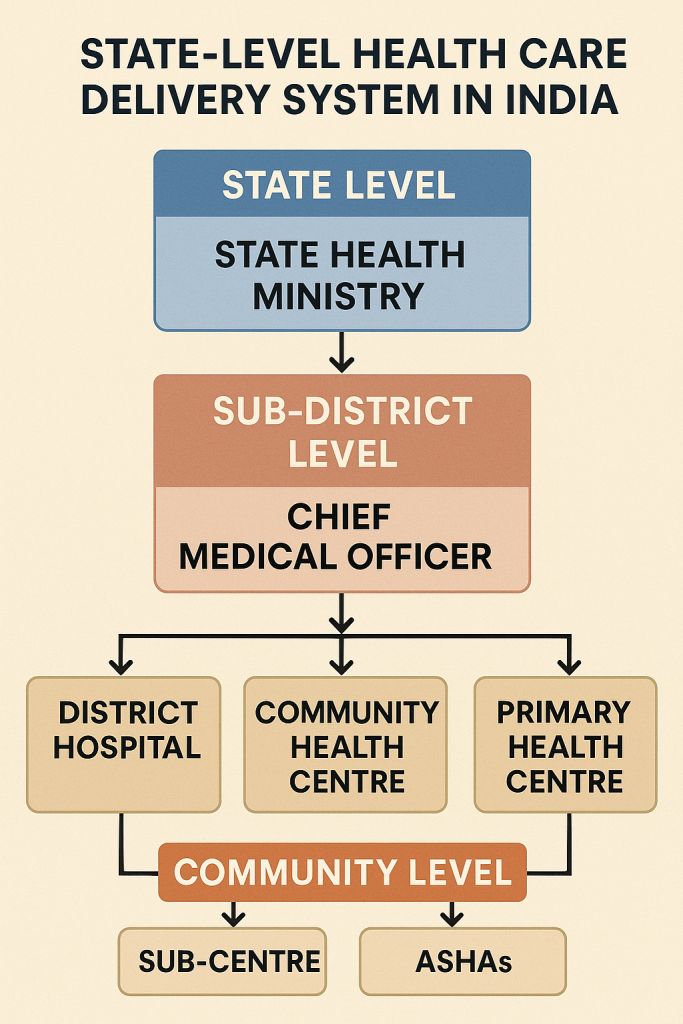
1. Introduction
The State-level health care system plays a critical role in planning, coordinating, financing, and supervising all health activities within the state. It acts as a link between the central government and district/block-level systems.
Every Indian state has its own Department of Health and Family Welfare and associated directorates to ensure implementation of national health programs and state-specific health services.
2. Structure of Health Administration at the State Level
A. State Ministry of Health and Family Welfare
- Headed by the State Health Minister
- Responsible for policy-making, legislation, budgeting, and coordination with the central ministry.
B. State Health Department (Executive Wing)
| Officer | Role |
|---|---|
| Principal Secretary (Health) | Senior IAS officer overseeing overall administration |
| Mission Director (NHM) | Supervises implementation of National Health Mission |
| Director of Health Services (DHS) | Supervises medical and public health services |
| Director of Medical Education and Research (DMER) | Manages medical, nursing, and paramedical education |
| Additional / Joint / Deputy Directors | Supervise specific programs like RCH, NCDs, TB, Leprosy etc. |
3. Key Responsibilities of State-Level Health System
| Function | Description |
|---|---|
| Planning | Develops State Health Action Plan (SHAP) |
| Budgeting | Allocates funds to districts and programs |
| Implementation | Executes national and state-level programs |
| Supervision | Monitors district performance and quality of services |
| Training | Organizes pre-service and in-service training |
| Recruitment | Appoints doctors, nurses, and health workers |
| Monitoring & Evaluation | Tracks health indicators through HMIS |
4. Health Institutions at State Level
| Institution | Role |
|---|---|
| State Hospitals (General Hospitals, Civil Hospitals) | Tertiary care facilities |
| Medical Colleges | Advanced treatment, education, research |
| State Health Training Institutes | Training for ANMs, GNMs, LHVs, MPWs |
| Regional Disease Control Units | Epidemic surveillance and outbreak response |
| State Drug Warehouses | Procurement and distribution of medicines |
5. Key Health Schemes Managed at State Level
- Ayushman Bharat – PMJAY
- National Health Mission (NHM)
- Reproductive, Maternal, Newborn, Child & Adolescent Health (RMNCH+A)
- National Tuberculosis Elimination Program (NTEP)
- Universal Immunization Programme (UIP)
- National Leprosy Eradication Programme (NLEP)
- National Mental Health Programme (NMHP)
- School Health Programme
6. Role of State in Human Resource Development
| Area | Responsibility |
|---|---|
| Recruitment | Appoints staff nurses, ANMs, doctors, lab techs |
| Training | Conducts skill upgradation and orientation |
| Curriculum Approval | For nursing and paramedical education |
| Monitoring | Evaluates performance of healthcare staff |
7. Role of State-Level Nurses / Public Health Nurse / Education Officers
| Role | Responsibility |
|---|---|
| Trainer | Teaches in health training schools or nursing colleges |
| Supervisor | Monitors district-level nurses and CHNs |
| Planner | Contributes to state health action plans |
| Policy Advisor | Assists in nursing policy, HR planning |
| Program Manager | Supervises maternal-child health, family planning, immunization |
| Inspector | Ensures quality control in nursing institutions (for INC/State Nursing Council) |
8. Monitoring and Evaluation Tools Used at State Level
- HMIS (Health Management Information System)
- Facility-based Monthly Reports
- State Health Dashboards
- Supportive Supervision Visits
- Annual Review Workshops
9. Challenges at the State Level
| Challenge | Description |
|---|---|
| Manpower shortages | Especially in rural/tribal areas |
| Uneven fund utilization | Due to delays in planning or implementation |
| Infrastructure gaps | Need for upgradation of state hospitals |
| Urban–rural disparity | In service delivery and access |
| Disease outbreaks | Require timely surveillance and response |
10. Suggestions for Strengthening State-Level Health System
- Digitalization of health records and program data
- Strengthen public-private partnerships (PPP)
- Fill staff vacancies quickly
- Regular training and capacity building
- Improve coordination between medical, nursing, and public health wings
- Ensure timely release of funds to districts
National-Level Health Care Delivery System in India
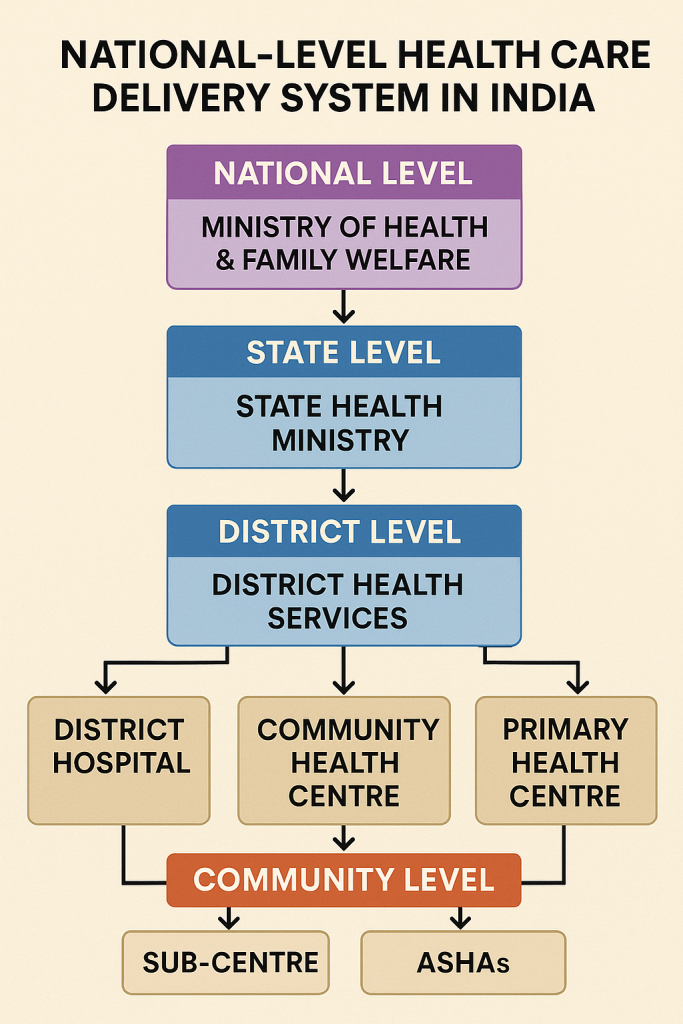
1. Introduction
The National Health Care Delivery System in India is responsible for:
- Formulating health policies,
- Designing national health programs,
- Funding and guiding state and district-level health systems,
- Monitoring and evaluating health outcomes across the country.
It is managed mainly by the Central Government, especially the Ministry of Health and Family Welfare (MoHFW).
2. Ministry of Health and Family Welfare (MoHFW)
The MoHFW is the apex body for health-related matters in India. It consists of two major departments:
A. Department of Health and Family Welfare
- Handles public health, medical education, and national programs.
- Supervises the functioning of:
- Central Government Health Scheme (CGHS)
- National Health Mission (NHM)
- Immunization programs
- Communicable and non-communicable disease programs
B. Department of Health Research
- Oversees medical research and policy development.
- Coordinates with Indian Council of Medical Research (ICMR).
3. National-Level Health Institutions
| Institution | Role |
|---|---|
| AIIMS (All India Institutes of Medical Sciences) | Tertiary care, education, research |
| ICMR (Indian Council of Medical Research) | Health research and disease surveillance |
| NIPCCD, NIHFW | Public health training and research |
| DGHS (Directorate General of Health Services) | Advises the Ministry, supports implementation |
| NCDC (National Centre for Disease Control) | Epidemic surveillance and control |
| NHSRC (National Health Systems Resource Centre) | Technical support for NHM |
| CBHI (Central Bureau of Health Intelligence) | Health statistics and information |
| National Health Authority (NHA) | Implements Ayushman Bharat – PMJAY |
4. Major National Health Missions and Programs
The central government runs flagship programs that are implemented at state and district levels:
| Program | Focus |
|---|---|
| National Health Mission (NHM) | Rural and urban health strengthening |
| Ayushman Bharat – PMJAY | Health insurance for the poor |
| Universal Immunization Program (UIP) | Free vaccination for children and mothers |
| Reproductive, Maternal, Newborn, Child, and Adolescent Health (RMNCH+A) | Comprehensive maternal-child care |
| National Tuberculosis Elimination Program (NTEP) | TB control |
| National Leprosy Eradication Program (NLEP) | Leprosy elimination |
| National Vector Borne Disease Control Program (NVBDCP) | Malaria, Dengue, Kala-azar control |
| National Mental Health Program (NMHP) | Mental health care at all levels |
| National Programme for NCDs (NPCDCS) | Diabetes, hypertension, cancer care |
5. Planning and Policy Making at National Level
| Institution | Function |
|---|---|
| NITI Aayog | Replaced Planning Commission; prepares vision and strategy for health |
| National Population Commission | Population policy and planning |
| National Health Policy (1983, 2002, 2017) | Guides health sector goals and reforms |
| 15th Finance Commission | Recommends grants for health infrastructure |
6. Role of Central Government in Funding
- Provides financial assistance to states via Centrally Sponsored Schemes (CSS).
- Allocates budget for national programs (like NHM, PMJAY).
- Fund disbursal through:
- State Health Societies
- District Health Societies
7. Role of National-Level Nurses & Nursing Bodies
| Role | Institutions |
|---|---|
| Regulatory | Indian Nursing Council (INC) – Approves nursing curriculum, inspects institutions |
| Training | NIHFW, RAK College of Nursing, AIIMS – Provide in-service education |
| Policy | Nurses contribute to policy advisory groups at MoHFW |
| Representation | Represent India in WHO and global health forums |
8. Monitoring and Evaluation at National Level
- Health Management Information System (HMIS)
- Annual Health Survey (AHS)
- National Family Health Survey (NFHS)
- Sample Registration System (SRS)
- District Health Information Software (DHIS2)
9. Challenges at National Level
| Challenge | Description |
|---|---|
| Inequity | Gaps between urban and rural health care |
| Underfunding | Health budget below WHO recommendations |
| HR Shortage | Especially specialists and trained nurses |
| Disease burden | Rising NCDs along with existing communicable diseases |
| Coordination issues | Between center and states in implementation |
10. Suggestions for Improvement
- Increase health budget to 2.5% of GDP
- Strengthen public health education and nursing institutions
- Foster digital health innovations (eHealth, Telemedicine)
- Empower National Health Authority for smooth implementation of PM-JAY
- Enhance multi-sectoral coordination (sanitation, nutrition, environment)
Sustainable Development Goals (SDGs)
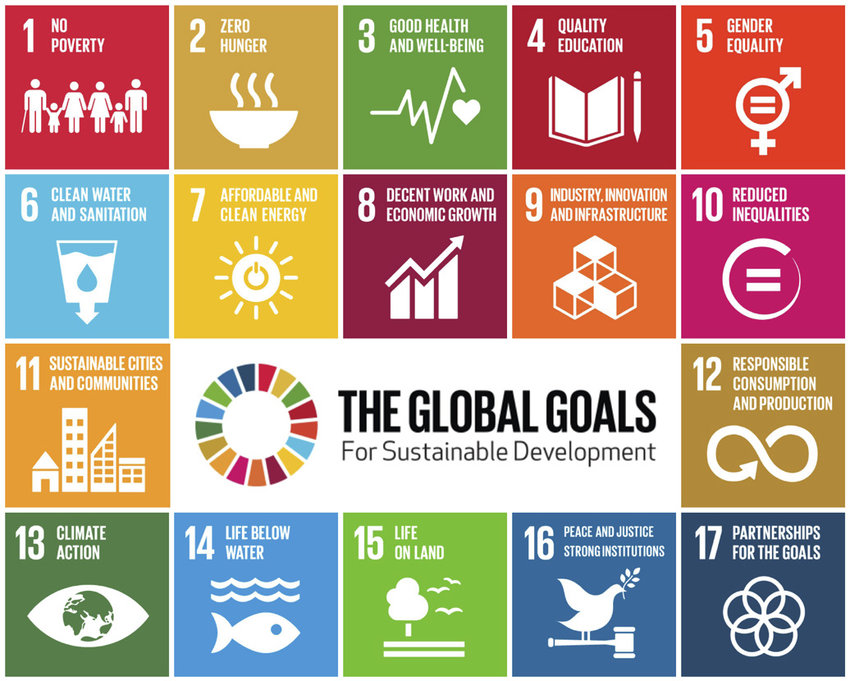
1. Introduction to SDGs
The Sustainable Development Goals (SDGs) are a global blueprint adopted by all United Nations (UN) member states, including India, in 2015.
- Part of the 2030 Agenda for Sustainable Development
- Total of 17 Goals and 169 targets
- Aim to end poverty, protect the planet, and ensure prosperity and peace
- Succeed the Millennium Development Goals (MDGs) – 2000–2015
Timeline
- Launched: September 25, 2015
- Target Year: December 31, 2030
- Duration: 15 years
2. List of 17 Sustainable Development Goals (SDGs)
| Goal No. | SDG Title |
|---|---|
| 1 | No Poverty |
| 2 | Zero Hunger |
| 3 | Good Health and Well-being |
| 4 | Quality Education |
| 5 | Gender Equality |
| 6 | Clean Water and Sanitation |
| 7 | Affordable and Clean Energy |
| 8 | Decent Work and Economic Growth |
| 9 | Industry, Innovation, and Infrastructure |
| 10 | Reduced Inequality |
| 11 | Sustainable Cities and Communities |
| 12 | Responsible Consumption and Production |
| 13 | Climate Action |
| 14 | Life Below Water |
| 15 | Life on Land |
| 16 | Peace, Justice, and Strong Institutions |
| 17 | Partnerships for the Goals |
3. Goal 3: Good Health and Well-being (Focus for Health Sector)
🎯 Goal 3: Ensure healthy lives and promote well-being for all at all ages
Key Targets under Goal 3:
- Reduce maternal mortality ratio to less than 70 per 100,000 live births
- End epidemics of AIDS, TB, Malaria, and neglected tropical diseases
- Reduce under-five mortality to 25/1,000 and neonatal mortality to 12/1,000
- Ensure universal access to sexual and reproductive health care
- Achieve universal health coverage (UHC) including financial risk protection
- Reduce deaths from NCDs (like diabetes, cancer, heart disease) by 1/3
- Strengthen capacity for emergency preparedness and disease surveillance
4. SDGs Related to Health & Community Health Nursing
| Goal | Relevance to Nursing |
|---|---|
| Goal 1 (No Poverty) | Poor people are vulnerable to illness and poor access to care |
| Goal 2 (Zero Hunger) | Nurses address malnutrition, anemia, and infant feeding |
| Goal 3 (Good Health) | Nurses deliver MCH, immunization, NCD care, etc. |
| Goal 4 (Education) | Nurse educators train future workforce |
| Goal 5 (Gender Equality) | Nurses support women’s rights, reproductive health |
| Goal 6 (Clean Water and Sanitation) | Community nurses promote hygiene and sanitation |
| Goal 13 (Climate Action) | Nurses respond to health effects of disasters |
5. India’s Commitment to SDGs
India has:
- Integrated SDGs into national and state health policies
- Established NITI Aayog as the nodal agency for monitoring SDGs
- Published the SDG India Index to measure state-wise progress
- Introduced health missions like:
- Ayushman Bharat
- POSHAN Abhiyaan
- National Health Mission (NHM)
- Swachh Bharat Abhiyan
- Beti Bachao Beti Padhao
6. Monitoring & Evaluation of SDGs in India
| Tool | Description |
|---|---|
| SDG India Index | Developed by NITI Aayog; scores states/UTs |
| NFHS (National Family Health Survey) | Tracks health indicators |
| HMIS (Health Management Information System) | Used for program monitoring |
| Sample Registration System (SRS) | Monitors birth, death, IMR, MMR |
7. Role of Community Health Nurse in Achieving SDGs
| Area | Contribution |
|---|---|
| Health Promotion | Educates community on nutrition, hygiene, family planning |
| Service Provider | Provides MCH, immunization, home-based newborn care |
| Disease Control | Identifies, refers, and follows up on TB, malaria, HIV |
| Advocate | Promotes gender equality and rights-based health care |
| Trainer | Trains ASHAs, health workers in community settings |
| Emergency Response | Participates in disaster relief and outbreak control |
8. Challenges in Achieving SDGs in India
- High maternal and infant mortality in some regions
- Malnutrition and anemia among children and women
- Rising burden of non-communicable diseases (NCDs)
- Urban-rural and gender disparities in healthcare
- Inadequate health infrastructure and workforce
9. Suggestions to Strengthen SDG Achievement
- Strengthen primary health care system
- Recruit and retain more trained nurses and health workers
- Invest in women’s education and empowerment
- Integrate SDG targets into district-level planning
- Strengthen digital health records and data collection
Primary Health Care (PHC) and Comprehensive Primary Health Care (CPHC)
1. What is Primary Health Care (PHC)?
Definition (Alma-Ata Declaration, 1978):
“Primary Health Care is essential health care made universally accessible to individuals and acceptable to them through full participation and at a cost the community and country can afford.”
It is the first level of contact between the individual and the health system.
2. Objectives of Primary Health Care
- Provide equitable access to essential health services
- Promote community participation
- Integrate preventive, promotive, curative, and rehabilitative services
- Focus on health promotion rather than only treatment
- Support intersectoral coordination (e.g., health, water, sanitation)
3. Principles of Primary Health Care
| Principle | Description |
|---|---|
| 1. Equitable Distribution | Health services should reach everyone, especially vulnerable and rural populations |
| 2. Community Participation | Involving people in planning and implementation |
| 3. Intersectoral Coordination | Involving sectors like education, agriculture, water, sanitation |
| 4. Appropriate Technology | Simple, cost-effective, and culturally acceptable methods |
| 5. Health Promotion and Disease Prevention | Emphasis on education, immunization, sanitation, and nutrition |
4. Elements of Primary Health Care (8 Elements – Alma Ata Declaration)
| No. | Element |
|---|---|
| 1️⃣ | Health Education – regarding prevailing health problems and methods of prevention/control |
| 2️⃣ | Promotion of Food Supply and Proper Nutrition |
| 3️⃣ | Adequate Supply of Safe Water and Basic Sanitation |
| 4️⃣ | Maternal and Child Health (MCH) care, including family planning |
| 5️⃣ | Immunization against major infectious diseases |
| 6️⃣ | Prevention and Control of Endemic Diseases |
| 7️⃣ | Appropriate Treatment of Common Diseases and Injuries |
| 8️⃣ | Provision of Essential Drugs |
5. Comprehensive Primary Health Care (CPHC)

Definition:
Comprehensive Primary Health Care (CPHC) is an expanded approach to primary care that ensures universal access to free, equitable, and quality services covering preventive, promotive, curative, rehabilitative, and palliative health care.
Introduced under: Ayushman Bharat – Health & Wellness Centres (HWCs), 2018
Key Features of CPHC:
| Feature | Description |
|---|---|
| Expanded Range of Services | Includes NCDs, mental health, elderly care, oral, eye care |
| Team-Based Care | CHO, ANM, ASHA working in collaboration |
| Continuum of Care | From home to facility (Sub-centre to District Hospital) |
| Use of Technology | Telemedicine, digital health records |
| Community Empowerment | Health promotion and behavior change |
6. Services Delivered Under CPHC (12 Service Packages)
| No. | Service Area |
|---|---|
| 1️⃣ | Maternal and Child Health |
| 2️⃣ | Family Planning and Reproductive Health |
| 3️⃣ | Adolescent Health |
| 4️⃣ | Neonatal and Infant Health |
| 5️⃣ | Communicable Disease Control |
| 6️⃣ | Non-Communicable Diseases (NCDs) |
| 7️⃣ | Mental Health |
| 8️⃣ | Oral Health |
| 9️⃣ | ENT and Eye Care |
| 🔟 | Elderly Care and Palliative Services |
| 1️⃣1️⃣ | Emergency and First Aid |
| 1️⃣2️⃣ | Health Promotion and Prevention |
7. Health & Wellness Centres (HWCs) – Platform for CPHC
| Type | Coverage |
|---|---|
| SC-HWC | Sub-centre converted to HWC for population ~3,000–5,000 |
| PHC-HWC | PHC upgraded to HWC for population ~30,000 |
Staffing at HWC:
- Community Health Officer (CHO)
- ANMs
- ASHA workers
- MPHW (Male)
8. Role of Community Health Nurse in PHC and CPHC
| Role | Responsibilities |
|---|---|
| Service Provider | Immunization, antenatal/postnatal care, chronic disease care |
| Educator | Health education on nutrition, hygiene, family planning |
| Coordinator | Works with ASHA, CHO, and MPHWs |
| Referral Link | Refers cases to PHC/CHC/District Hospital |
| Record Keeper | Maintains family records, immunization cards, health registers |
| Advocate | Promotes health rights and services awareness |
| Technology User | Uses mobile apps, teleconsultation, HMIS data entry |
9. Challenges in Implementation of PHC/CPHC
- Shortage of trained staff (especially CHOs)
- Inadequate infrastructure and supplies
- Difficult terrain and access issues in tribal/rural areas
- Lack of community awareness
- Digital illiteracy and data management issues
10. Suggestions for Improvement
- Ensure regular supply of essential drugs and diagnostics
- Recruit and train adequate CHOs and nurses
- Strengthen digital infrastructure and telemedicine
- Promote community awareness and participation
- Provide performance-based incentives to frontline workers
Summary Chart: PHC vs. CPHC
| Feature | PHC (Basic) | CPHC (Comprehensive) |
|---|---|---|
| Based on | Alma-Ata Declaration (1978) | Ayushman Bharat (2018) |
| Services | Basic preventive and curative | Expanded services incl. NCDs, elderly care |
| Focus | Access and essential care | Universal coverage and quality care |
| Facility | PHC/Sub-centre | Health & Wellness Centres |
| Staff | MO, Nurse, ANM | CHO, ANM, MPHW, ASHA |
Comprehensive Primary Health Care (CPHC) through Sub-Centre / Health & Wellness Centre (HWC)
(As part of Ayushman Bharat – 2018 Initiative)
1. Introduction to CPHC and HWCs
- Ayushman Bharat Programme launched in 2018 aims to achieve Universal Health Coverage (UHC) through:
- Health & Wellness Centres (HWCs) – for Comprehensive Primary Health Care
- PM-JAY (Pradhan Mantri Jan Arogya Yojana) – for secondary and tertiary hospitalization
- Under this, Sub-Centres and PHCs are being transformed into HWCs to deliver expanded primary care services.
2. What is a Health & Wellness Centre (HWC)?

An HWC is a revamped Sub-Centre or PHC that delivers comprehensive primary health care, with free essential medicines, diagnostics, and team-based care.
Types of HWCs:
- SC-HWC (converted from Sub-Centre) – for population 3,000–5,000
- PHC-HWC (converted from PHC) – for population 30,000
3. Goals of CPHC through HWCs
- Provide holistic, preventive, promotive, curative, rehabilitative, and palliative care
- Ensure community-based, people-centered care
- Strengthen continuum of care and reduce burden on higher facilities
- Offer free drugs, diagnostics, and referral linkages
4. Service Packages Delivered at SC-HWC (12 Packages)
| No. | Service Package |
|---|---|
| 1️⃣ | Maternal and Child Health (ANC, PNC, deliveries, growth monitoring) |
| 2️⃣ | Family Planning and Contraceptive Services |
| 3️⃣ | Adolescent Health (counseling, menstrual hygiene) |
| 4️⃣ | Neonatal and Infant Health (HBNC, immunization) |
| 5️⃣ | Communicable Diseases (Malaria, TB, HIV) |
| 6️⃣ | Non-Communicable Diseases (diabetes, BP, cancer screening) |
| 7️⃣ | Mental Health (stress, depression, counseling) |
| 8️⃣ | Oral Health (screening and referral) |
| 9️⃣ | ENT and Eye Care |
| 🔟 | Elderly Care and Palliative Services |
| 1️⃣1️⃣ | Emergency First Aid (minor injuries, burns, snake bite) |
| 1️⃣2️⃣ | Health Promotion, Wellness Activities (Yoga, lifestyle education) |
5. Human Resources at SC-HWC
| Staff | Role |
|---|---|
| Community Health Officer (CHO) | Team leader, provides clinical care, maintains records |
| Auxiliary Nurse Midwife (ANM) | MCH services, immunization, family planning |
| Multipurpose Health Worker (MPHW Male) | Disease control, sanitation, male sterilization counseling |
| ASHA workers | Community mobilization, follow-up care, home visits |
6. Services Available at SC-HWC
| Category | Examples |
|---|---|
| Clinical Services | BP, diabetes, skin problems, infections |
| Diagnostics | BP monitoring, glucometer, pregnancy test, hemoglobin, malaria |
| Medicines | IFA tablets, ORS, paracetamol, antibiotics, contraceptives |
| Referral Services | To PHC/CHC/District Hospital for complications |
| Telemedicine | For consultation with doctors using eSanjeevani |
| Wellness Activities | Yoga, health camps, Swasthya Panchayats |
7. Digital Tools at SC-HWC
- ABHA ID (Ayushman Bharat Health Account)
- Teleconsultation App (eSanjeevani)
- CPHC IT Platform for service delivery, data entry, drug inventory
- HMIS/ANMOL – used by ANMs for real-time reporting
8. Role of CHO, ANM, MPHW, and ASHA in SC-HWC
| Cadre | Responsibilities |
|---|---|
| CHO (BSc Nursing/Post-BSc/CPCH trained) | Clinical care, screening, referrals, data entry |
| ANM | MCH services, FP counseling, immunization, home visits |
| MPHW (Male) | Disease surveillance, sanitation, outbreak response |
| ASHA | Community link, follow-up, birth/death reporting, drug depot holder |
9. Health Promotion & Wellness Activities at SC-HWC
- Yoga sessions (weekly/monthly)
- School health screening
- NCD camps and screening days
- IEC activities (posters, flipcharts, talks)
- Village Health & Nutrition Days (VHNDs)
10. Challenges in Implementing CPHC through SC-HWCs
- Shortage of trained CHOs
- Infrastructure gaps in Sub-Centres
- Inconsistent supply of medicines and diagnostics
- Limited awareness among community members
- Connectivity issues in remote areas (for teleconsultation)
11. Suggestions for Strengthening SC-HWCs
- Fill vacant CHO and ANM posts
- Ensure regular supply of essential medicines and test kits
- Upgrade buildings and equipment at Sub-Centre level
- Conduct community awareness campaigns
- Strengthen digital health tools and mobile health platforms
National Health Care Policies and Regulations

1. Introduction
Health policies are strategic documents or plans made by the government to guide health care services, programs, funding, laws, and standards.
Health regulations are the rules and legal frameworks that ensure quality, safety, equity, and accountability in health care delivery.
2. Major National Health Policies in India
A. National Health Policy (NHP)
India has had three official National Health Policies:
1. National Health Policy – 1983
➡ Focused on: “Health for All by 2000”
Key Features:
- Emphasized primary health care
- Expansion of rural health infrastructure
- Community participation
- Training of multipurpose health workers
- Integration of health services
2. National Health Policy – 2002
➡ Focused on: Improving access and equity
Key Features:
- Emphasized decentralization of health services
- Encouraged public-private partnerships (PPP)
- Increased role of AYUSH systems
- Focus on disease surveillance and emergency response
3. National health policy-2017
➡ Focused on: “Universal Health Coverage (UHC)”
Goals:
- Reduce out-of-pocket expenditure
- Strengthen primary health care
- Free drugs, diagnostics, and emergency care
- Health and Wellness Centres (HWCs) for Comprehensive Primary Health Care
- Digital health records and telemedicine
- Address non-communicable diseases (NCDs) and mental health
Targets by 2025:
- Reduce IMR to 28/1000
- Reduce MMR to 100/100,000
- Increase life expectancy to 70 years
- Reduce fertility rate to 2.1
3. Other Important National Policies Related to Health
| Policy | Year | Purpose |
|---|---|---|
| National Population Policy | 2000 | Population stabilization, FP services |
| National Nutrition Policy | 1993 | Address malnutrition in children and women |
| National Policy on Senior Citizens | 2011 | Welfare, healthcare, and security of the elderly |
| National Mental Health Policy | 2014 | Promote mental health services at all levels |
| National Education Policy | 2020 | Includes reforms in nursing and medical education |
| National Policy for Women Empowerment | 2001 | Addresses women’s health, rights, and safety |
4. Important Health Regulations and Acts in India
Health regulations are legally enforceable rules aimed at ensuring safe, ethical, and standardized healthcare.
A. Constitutional Provisions
| Article | Provision |
|---|---|
| Article 21 | Right to Life includes Right to Health |
| Article 47 | Duty of the state to raise nutrition and standard of living |
| Article 42 | Maternity relief and humane working conditions |
| Concurrent List (List III) | Health is a shared responsibility of Centre and States |
B. Key Health Acts in India
| Act | Year | Purpose |
|---|---|---|
| Drugs and Cosmetics Act | 1940 | Regulates manufacture and sale of drugs and cosmetics |
| Indian Nursing Council Act | 1947 | Governs nursing education and registration |
| Medical Termination of Pregnancy (MTP) Act | 1971 (amended 2021) | Legalizes abortion under conditions |
| The Epidemic Diseases Act | 1897 (used during COVID-19) | Powers to control outbreaks |
| Transplantation of Human Organs Act | 1994 | Regulation of organ donation and transplantation |
| PNDT Act | 1994 | Prevents female feticide (bans sex determination) |
| Clinical Establishments Act | 2010 | Standardizes private health facilities |
| Mental Healthcare Act | 2017 | Rights-based mental health care |
| National Food Security Act | 2013 | Food and nutrition security to all |
| Right to Information Act (RTI) | 2005 | Ensures transparency in health system |
5. Role of National Health Agencies in Policy Implementation
| Agency | Role |
|---|---|
| MoHFW | Main health policy-making body |
| NITI Aayog | Vision documents and SDG monitoring |
| ICMR | Research to inform policy |
| NHM | Implements maternal-child health programs |
| National Health Authority (NHA) | Executes PM-JAY (insurance scheme) |
| National Medical Commission / INC | Sets standards in medical and nursing education |
6. Role of Community Health Nurse in Policy and Regulation Implementation
| Area | Role |
|---|---|
| Health Promotion | Educates community about policies (MTP, vaccination, nutrition) |
| Service Provider | Implements programs at grassroots (NHM, JSY, immunization) |
| Record Keeper | Maintains legal and health registers |
| Law Enforcer | Reports violations (child marriage, PNDT, domestic violence) |
| Advocate | Promotes rights of women, children, disabled, and elderly |
| Trainer | Educates ASHAs and health workers about policy updates |
7. Challenges in Policy Implementation
- Limited awareness among population and health workers
- Poor intersectoral coordination
- Inadequate infrastructure and HR
- Corruption and delays
- Gaps in data collection and monitoring
8. Suggestions for Strengthening Policies and Regulations
- Increase community participation and awareness
- Conduct regular training of nurses and health workers
- Strengthen digital health platforms for transparency
- Promote collaboration between sectors (education, women development)
- Encourage evidence-based policy making using research data
National Health Policy – 1983, 2002, and 2017
What is a National Health Policy?
A National Health Policy (NHP) is a strategic document that provides a vision, priorities, and framework for a country’s health care development. In India, it is issued by the Ministry of Health and Family Welfare to guide health services planning and delivery.
India has had three major health policies:
- NHP 1983
- NHP 2002
- NHP 2017
1. National Health Policy – 1983
📅 Year: 1983
🎯 Goal: “Health for All by 2000” (as per WHO-Alma Ata Declaration)
Key Objectives:
- Provide universal, comprehensive, primary health care to all
- Reduce IMR, MMR, and control communicable diseases
- Increase people’s participation and use of appropriate technology
- Train multipurpose health workers
- Establish district-level health planning
Focus Areas:
- Expand primary health infrastructure in rural areas
- Promote indigenous systems of medicine (AYUSH)
- Ensure minimum health services for all, especially underprivileged groups
Achievements:
- Set the foundation for primary health care (PHC) structure
- Led to programs like:
- Universal Immunization Programme (UIP) – 1985
- National Leprosy Elimination Program
- Expansion of Sub-Centres and PHCs
2. National Health Policy – 2002
📅 Year: 2002
🎯 Goal: Improve access, affordability, accountability, and equity in health care.
Key Objectives:
- Increase government health spending to 2% of GDP
- Reduce IMR to 30/1,000, MMR to 100/100,000, TFR to 2.1
- Promote public-private partnerships (PPP)
- Expand AYUSH integration
- Improve urban health care delivery
- Decentralize services through Panchayati Raj Institutions
Focus Areas:
- Reproductive and Child Health (RCH)
- Disease surveillance and response
- Strengthen tertiary care and referral system
- Encourage health insurance for the poor
Achievements:
- Laid foundation for:
- National Rural Health Mission (NRHM) – 2005
- Disease-specific programs (TB, HIV, Malaria)
- Use of information technology in health care
3. National Health Policy – 2017
📅 Year: 2017
🎯 Goal: “Attainment of the highest possible level of health and well-being for all at all ages” through a preventive and promotive health care orientation.
Vision:
- Universal Health Coverage (UHC)
- Free, equitable, and quality health care
- Financial risk protection
- Focus on wellness and prevention
Key Objectives:
- Strengthen primary health care through Health & Wellness Centres (HWCs)
- Increase government health expenditure to 2.5% of GDP by 2025
- Promote digital health and electronic health records (EHR)
- Provide free essential drugs, diagnostics, and emergency care
- Integrate mental health, palliative care, and NCDs in primary care
Targets by 2025:
| Indicator | Target |
|---|---|
| IMR | ≤ 28 per 1,000 live births |
| MMR | ≤ 100 per 100,000 live births |
| TFR | ≤ 2.1 |
| Life Expectancy | ≥ 70 years |
| Reduction in NCDs | 25% reduction in premature deaths |
| Health Expenditure | 2.5% of GDP (from ~1.1%) |
Comparison Table: NHP 1983 vs. 2002 vs. 2017
| Feature | NHP 1983 | NHP 2002 | NHP 2017 |
|---|---|---|---|
| Launch Year | 1983 | 2002 | 2017 |
| Main Goal | Health for All by 2000 | Access & Equity | Universal Health Coverage |
| Focus | PHC, rural health infra | PPP, decentralization | Wellness, digital health, HWCs |
| Health Spending Target | Not defined | 2% of GDP | 2.5% of GDP |
| TFR Target | – | 2.1 | 2.1 |
| Integration of AYUSH | Promoted | Promoted | Strongly integrated |
| Programs Initiated | UIP, PHC expansion | NRHM | Ayushman Bharat, HWCs |
| Emphasis on NCDs | Low | Moderate | High |
| Digital Health | Not present | Limited | EHR, Telemedicine emphasized |
Role of Community Health Nurse in Policy Implementation
| Role | Contribution |
|---|---|
| Service Provider | Implements immunization, ANC/PNC, family planning |
| Health Educator | Promotes nutrition, hygiene, disease prevention |
| Referral Agent | Identifies and refers high-risk cases |
| Record Keeper | Maintains family registers, HMIS |
| Digital Support | Assists in e-health and teleconsultation (under 2017 policy) |
| Advocate | Promotes health rights and equity |
Conclusion
The evolution of India’s National Health Policies shows a clear shift:
- From infrastructure building (1983) →
- To system reforms and partnerships (2002) →
- To holistic, equitable, digital, and preventive care (2017).
The 2017 policy aligns with Sustainable Development Goals (SDGs) and emphasizes Comprehensive Primary Health Care through HWCs, making community health nurses central players in its implementation.
National Health Mission (NHM)

1. Introduction
The National Health Mission (NHM) is a flagship program of the Government of India, launched to provide accessible, affordable, accountable, and quality health care to all, especially to the vulnerable and poor.
It strengthens the public health system at all levels — from village to district.
📅 Launched On: 12th April 2005
📍 Ministry: Ministry of Health and Family Welfare (MoHFW)
🌐 Website: https://nhm.gov.in
2. Components of NHM
| Component | Launched | Focus |
|---|---|---|
| A. National Rural Health Mission (NRHM) | 2005 | Rural health infrastructure |
| B. National Urban Health Mission (NUHM) | 2013 | Urban poor and slum population |
| NRHM + NUHM = NHM | Unified in 2013 | Single umbrella mission |
3. Vision of NHM
“Attainment of Universal Access to equitable, affordable & quality health care services that are accountable and responsive to people’s needs.”
4. Objectives of NHM
- Strengthen health systems in rural and urban areas
- Reduce maternal and infant mortality
- Control and eliminate communicable and non-communicable diseases
- Promote universal access to reproductive, maternal, child and adolescent health (RMNCH+A)
- Revitalize local health traditions and mainstream AYUSH
- Promote community participation and decentralization
5. Key Strategies under NHM
- Strengthening Sub-Centres, PHCs, CHCs & District Hospitals
- Establishment of Health & Wellness Centres (HWCs)
- Recruitment of ASHA workers
- Free essential drugs and diagnostics
- Capacity building of healthcare providers
- Community-based programs through VHSNCs and Rogi Kalyan Samitis
- Performance-based incentives to frontline workers
- Telemedicine and digital health platforms
6. Key Programs and Services under NHM
| Program Area | Services Provided |
|---|---|
| RMNCH+A | Reproductive, maternal, newborn, child & adolescent health |
| JSY | Janani Suraksha Yojana – cash incentive for institutional deliveries |
| JSSK | Janani Shishu Suraksha Karyakram – free transport, drugs, diagnostics |
| RBSK | Rashtriya Bal Swasthya Karyakram – child screening and early intervention |
| RKSK | Rashtriya Kishor Swasthya Karyakram – adolescent health |
| NCD Control | Screening & treatment for BP, diabetes, cancer |
| NUHM | Health services for the urban poor |
| Disease Programs | TB, leprosy, malaria, HIV, vector-borne disease control |
7. Service Delivery Innovations under NHM
| Initiative | Description |
|---|---|
| ASHA (Accredited Social Health Activist) | Community link worker |
| Health & Wellness Centres (HWCs) | Deliver comprehensive primary health care |
| Mobile Medical Units (MMUs) | Reach underserved and remote areas |
| eSanjeevani | Free teleconsultation services |
| Home-Based Newborn and Young Child Care | By ASHA and ANMs |
| MCTS / RCH Portal | Mother and child tracking system |
8. Monitoring & Evaluation under NHM
- Health Management Information System (HMIS)
- District Level Household Surveys (DLHS)
- Annual Common Review Missions (CRM)
- Facility-Based Data Collection
9. Role of Community Health Nurse under NHM
| Role | Function |
|---|---|
| Service Provider | ANC, immunization, family planning, newborn care |
| Trainer | Training ASHAs, ANMs, MPHWs |
| Health Educator | IEC on nutrition, hygiene, MCH |
| Program Implementer | Executes JSY, JSSK, RBSK, etc. at grassroots |
| Data Reporter | Maintains registers and reports to PHC/Block |
| Team Leader | Leads VHSNCs and coordinates with other health workers |
| Health Promoter | Encourages institutional deliveries, healthy behaviors |
10. Achievements of NHM (as per recent data)
- Significant reduction in IMR, MMR, and TFR
- Institutional deliveries increased to over 80%
- Increased availability of free drugs and diagnostics
- 85,000+ HWCs operational across India
- ASHA workers recognized as Global Health Leaders (by WHO)
11. Challenges in NHM Implementation
- Shortage of specialists in CHCs and PHCs
- Inadequate infrastructure and drug supply in remote areas
- High attrition rate of trained personnel
- Monitoring and data reporting issues
- Urban health systems still underdeveloped
12. Suggestions for Improvement
- Fill staff vacancies, especially doctors and CHOs
- Expand digital health records and telemedicine
- Strengthen referral transport and emergency services
- Increase community participation
- Conduct regular training and supervision of frontline workers
Here’s a complete and detailed explanation of the National Rural Health Mission (NRHM) — ideal for Community Health Nursing, nursing students, and competitive exams:
National Rural Health Mission (NRHM)

1. Introduction
The National Rural Health Mission (NRHM) was launched by the Government of India to provide accessible, affordable, and quality health care to the rural population, especially vulnerable groups like women, children, and the poor.
📅 Launched On: 12th April 2005
👩⚕️ Target Group: Rural population, especially mothers, infants, children, and adolescents
📍 Ministry: Ministry of Health and Family Welfare (MoHFW)
2. Goals and Objectives
Vision:
“Provide effective health care to the rural population throughout the country with a special focus on 18 high-focus states.”
Main Objectives:
- Reduce IMR, MMR, and TFR
- Strengthen rural health infrastructure
- Promote institutional deliveries
- Improve access to maternal and child health services
- Integrate AYUSH into the public health system
- Enhance community participation and decentralized planning
3. Key Strategies under NRHM
| Strategy | Description |
|---|---|
| Strengthening Health Infrastructure | Upgrade SCs, PHCs, CHCs as per IPHS |
| Training Human Resources | Recruitment of ANMs, MPHWs, Doctors, ASHAs |
| ASHA Scheme | Accredited Social Health Activists as community link workers |
| Untied Funds | Rs. 10,000 at SC level for local health needs |
| Village Health and Nutrition Days (VHNDs) | Monthly outreach with immunization, ANC/PNC |
| Janani Suraksha Yojana (JSY) | Cash incentives for institutional deliveries |
| Janani Shishu Suraksha Karyakram (JSSK) | Free drugs, diagnostics, transport for pregnant women & newborns |
| Rogi Kalyan Samiti (RKS) | Local hospital management committee |
| Decentralized Planning | Village, Block, and District Health Plans |
| Health Management Information System (HMIS) | Improved reporting and monitoring |
4. Institutional Strengthening under NRHM
| Level | Facility Strengthened |
|---|---|
| Village | ASHA, Anganwadi, VHSNC |
| Sub-Centre (SC) | 1 per 5,000 people (3,000 in tribal/hilly) |
| Primary Health Centre (PHC) | 1 per 30,000 people (20,000 in hilly areas) |
| Community Health Centre (CHC) | 1 per 1.2 lakh people |
| District Hospital | First referral unit (FRU) |
5. ASHA – Accredited Social Health Activist
- 1 ASHA per 1,000 population (or per village)
- Female health activist from the community
- Roles:
- Promotes institutional deliveries
- Accompanies women to health facilities
- Ensures immunization, newborn care, FP
- Community mobilization and awareness
6. Key Indicators Monitored under NRHM
| Indicator | Target |
|---|---|
| IMR (Infant Mortality Rate) | <30 per 1,000 |
| MMR (Maternal Mortality Ratio) | <100 per 1 lakh live births |
| TFR (Total Fertility Rate) | 2.1 |
| Institutional Deliveries | >80% |
| Child Immunization Coverage | >90% |
7. Major Programs Integrated Under NRHM
| Program | Focus |
|---|---|
| Reproductive and Child Health (RCH) | ANC, PNC, deliveries, immunization |
| National Immunization Program (UIP) | Routine immunization for children & mothers |
| Disease Control Programs | Malaria, TB, Leprosy, HIV/AIDS |
| School Health Program | Screening and health education |
| Adolescent Health Program (RKSK) | Menstrual hygiene, counseling |
8. Role of Community Health Nurse under NRHM
| Role | Responsibility |
|---|---|
| Service Delivery | Provides ANC, PNC, immunization, FP |
| Health Education | IEC on nutrition, hygiene, breastfeeding |
| Training & Supervision | Trains ASHAs, monitors their work |
| Referral & Follow-up | Identifies and refers high-risk cases |
| Data Management | Maintains SC registers and reports |
| Community Mobilizer | Promotes participation in VHNDs and JSY |
9. Monitoring Tools under NRHM
- HMIS (Health Management Information System)
- Mother and Child Tracking System (MCTS)
- Facility and Community Surveys
- Annual Common Review Missions (CRM)
10. Achievements of NRHM (2005–2013)
- Rise in institutional deliveries
- Increase in child immunization coverage
- Deployment of 10 lakh+ ASHA workers
- Upgradation of rural health facilities
- Reduction in IMR and MMR
- Introduction of JSSK, RBSK, RKSK
11. Transition from NRHM to NHM
In 2013, NRHM was subsumed under the National Health Mission (NHM) along with the National Urban Health Mission (NUHM) to form a comprehensive mission covering both rural and urban areas.
12. Conclusion
The National Rural Health Mission (NRHM) played a transformative role in strengthening rural health care infrastructure, empowering community health workers (ASHAs), and improving maternal and child health outcomes. It laid the foundation for NHM, moving India toward Universal Health Coverage (UHC) and Sustainable Development Goals (SDGs).
National Urban Health Mission (NUHM)

1. Introduction
The National Urban Health Mission (NUHM) is a sub-mission under the National Health Mission (NHM) that aims to provide quality and equitable health care services to the urban poor and vulnerable populations in towns and cities.
📅 Launched: 20th May 2013
🏛️ By: Ministry of Health and Family Welfare (MoHFW), Government of India
👥 Target Population: Urban poor, slum dwellers, street vendors, homeless, migrants, construction workers
2. Objectives of NUHM
- Improve the health status of urban populations, especially urban poor
- Provide equitable access to quality health services
- Establish a people-centric health care system
- Integrate public and private sectors for better urban health delivery
3. Key Features of NUHM
| Feature | Description |
|---|---|
| Focus on Slum Population | Special attention to slum dwellers and vulnerable groups |
| Urban Primary Health Centres (UPHCs) | One UPHC per 50,000 population |
| Outreach Services | Mobile Medical Units, Urban Health & Nutrition Days (UHNDs) |
| Public-Private Partnership (PPP) | Collaborate with NGOs, private providers |
| City Health Planning | Participatory health plans developed for each city |
| Community Participation | Mahila Arogya Samitis (MAS), Urban ASHAs, Rogi Kalyan Samitis |
4. Urban Health Infrastructure under NUHM
| Facility | Coverage | Role |
|---|---|---|
| Urban Primary Health Centre (UPHC) | 1 per 50,000 population | Provides OPD, basic lab tests, FP, MCH services |
| Urban Community Health Centre (UCHC) | 1 per 2.5–5 lakh population | Secondary care, referrals |
| Urban Health & Nutrition Day (UHND) | Monthly outreach camp in slums | ANC/PNC, immunization, health education |
| Mahila Arogya Samiti (MAS) | Women-led community groups | Health promotion, sanitation, behavior change |
5. Human Resources under NUHM
| Cadre | Role |
|---|---|
| Urban ASHA | Community mobilization, home visits, follow-up |
| Medical Officer | Diagnosis and treatment at UPHC |
| Staff Nurse | OPD care, immunization, wound dressing |
| ANM/MPHW | MCH, FP, health promotion |
| Pharmacist, Lab Tech | Dispensing medicines, basic investigations |
| Community Organizer | Promotes community participation and supports MAS |
6. Services Provided under NUHM
| Area | Services |
|---|---|
| Maternal Health | ANC, PNC, institutional delivery support |
| Child Health | Immunization, newborn care |
| Family Planning | Counseling, distribution of contraceptives |
| Communicable Diseases | Screening, treatment, referral |
| Non-Communicable Diseases | Screening for BP, diabetes, cancer |
| Adolescent & Geriatric Health | Iron supplementation, counseling, elderly care |
| Referral Services | To UCHCs, District Hospitals |
7. Diagnostics and Free Medicines
- Basic lab services at UPHCs (Hb, Blood Sugar, Malaria, Urine test, Pregnancy test)
- Free essential drugs for common illnesses
- Linkages to diagnostic centers and free drug schemes
8. Community Participation – MAS & ASHA
Mahila Arogya Samiti (MAS):
- A group of 10–12 local women from slum areas
- Facilitates:
- Health education
- Hygiene and sanitation awareness
- Monitoring of health services
- Participation in UHNDs
Urban ASHA:
- One per 2,000 urban population
- Promotes institutional delivery, immunization, FP
- Conducts home visits and community surveys
9. Monitoring Tools under NUHM
| Tool | Use |
|---|---|
| Health Management Information System (HMIS) | Monthly reporting |
| Urban Health Card | For families in urban slums |
| RCH Portal | Tracking mother and child health |
| Periodic Surveys | NFHS, Urban Health Survey, etc. |
10. Role of Community Health Nurse in NUHM
| Role | Functions |
|---|---|
| Service Provider | Provides OPD care, ANC/PNC, immunization |
| Trainer | Trains ASHAs, MAS members |
| Health Educator | IEC on nutrition, sanitation, hygiene |
| Data Manager | Maintains records, reports |
| Community Mobilizer | Encourages participation in health programs |
| Referral Coordinator | Connects with UCHCs and higher centers |
11. Achievements of NUHM (2013–Present)
- More than 5,000 UPHCs established
- Over 75 lakh people reached annually in urban areas
- Introduction of urban ASHA workforce
- Improvement in urban maternal and child health indicators
- Integration with Ayushman Bharat – HWCs in Urban Areas
12. Challenges in NUHM Implementation
- Slums are often unmapped and scattered
- Shortage of staff in UPHCs
- Poor sanitation and water in urban slums
- Migrant population is mobile and hard to track
- Low awareness and utilization of public health facilities
13. Suggestions for Strengthening NUHM
- Conduct slum mapping and population enumeration
- Recruit and train adequate ASHAs, nurses, and MO
- Strengthen referral linkages and transport
- Integrate NUHM with urban development departments
- Promote urban health literacy campaigns
National Health Protection Mission (NHPM)
Also known as: Ayushman Bharat – Pradhan Mantri Jan Arogya Yojana (PM-JAY)

1. Introduction
The National Health Protection Mission (NHPM) was launched as part of Ayushman Bharat, a flagship initiative to achieve Universal Health Coverage (UHC).
It was rebranded as PM-JAY in September 2018 and is now one of the world’s largest government-funded health insurance programs.
📅 Launched On: 23rd September 2018
🏛️ By: Ministry of Health and Family Welfare (MoHFW), Government of India
🌐 Implementing Agency: National Health Authority (NHA)
2. Objectives of NHPM / PM-JAY
- Provide financial protection to poor and vulnerable families from catastrophic health expenditure
- Ensure access to quality secondary and tertiary hospitalization
- Empower beneficiaries with cashless, paperless treatment
- Reduce out-of-pocket (OOP) expenses for the poor
3. Target Beneficiaries
- Covers over 10.74 crore poor and vulnerable families (~50 crore individuals)
- Beneficiaries identified based on Socio-Economic Caste Census (SECC) 2011
- No cap on family size, age, or gender
- Applicable to rural and urban poor
4. Coverage under NHPM / PM-JAY
| Category | Details |
|---|---|
| Coverage amount | Up to ₹5 lakh per family per year |
| Type of care | Secondary and tertiary hospitalization (not OPD) |
| Cashless facility | Yes, at empanelled hospitals |
| Portability | Yes, usable across India in any empanelled hospital |
| Pre-existing conditions | Covered from day one |
5. Types of Services Covered
- Medical and surgical procedures
- Day-care procedures
- Cost of medicines, diagnostics, room charges, OT charges
- 3 days pre-hospitalization and 15 days post-hospitalization
- Cancer care, heart surgeries, orthopedic surgeries, kidney and liver treatment, neonatal care, etc.
6. How It Works
| Step | Process |
|---|---|
| 1️⃣ | Beneficiary identified through SECC database or PM-JAY portal |
| 2️⃣ | Gets Ayushman Card or ABHA ID |
| 3️⃣ | Visits empanelled public or private hospital |
| 4️⃣ | Treatment is cashless and paperless |
| 5️⃣ | Hospital claims expenses from NHA/State Health Agency |
7. Institutional Mechanism
| Level | Institution |
|---|---|
| National Level | National Health Authority (NHA) |
| State Level | State Health Agency (SHA) |
| District Level | District Implementation Unit (DIU) |
8. Implementation Models
States can choose any of these:
- Insurance Model (through insurance companies)
- Trust Model (state pays directly to hospitals)
- Mixed Model
9. Achievements of NHPM / PM-JAY
- Over 6 crore hospital admissions availed by beneficiaries (as of 2024)
- More than 26,000 hospitals empanelled (public + private)
- Significant reduction in out-of-pocket expenditure
- Increased access to specialty care in poor households
- Enabled portability of care for migrant workers
10. Role of Community Health Nurse in NHPM
| Role | Function |
|---|---|
| Health Educator | Informs families about PM-JAY eligibility |
| Facilitator | Helps in registration and Ayushman card generation |
| Referral Coordinator | Refers patients to empanelled hospitals |
| Support Staff | Ensures post-hospitalization follow-up |
| Record Keeping | Maintains household health records and updates ABHA ID |
| Awareness Creation | Conducts IEC campaigns in villages and slums |
11. Challenges in Implementation
- Limited awareness among rural and poor populations
- Infrastructure gaps in some empanelled hospitals
- Claim processing delays in some states
- Fraudulent claims by some private hospitals
- Lack of specialists in government hospitals
12. Suggestions for Improvement
- Strengthen health infrastructure in rural areas
- Increase beneficiary awareness through ASHAs and ANMs
- Use digital tools (ABHA ID, e-RUPI) for faster service
- Ensure timely payment to hospitals
- Capacity building of health professionals and program managers
Ayushman Bharat

1. Introduction
Ayushman Bharat is a flagship health initiative launched by the Government of India in 2018 to achieve Universal Health Coverage (UHC) and fulfill the vision of “Healthy India.”
It aims to transform India’s health system through preventive, promotive, curative, and financial protection-based approaches.
📅 Launched On: 14th April 2018 (Ambedkar Jayanti)
🏛️ By: Ministry of Health and Family Welfare (MoHFW), Government of India
🌐 Based On: Recommendations of the National Health Policy 2017
2. Objectives of Ayushman Bharat
- Provide comprehensive primary health care at the grassroots
- Ensure financial protection through cashless secondary and tertiary care
- Improve access to free health care services
- Promote wellness and disease prevention
- Reduce out-of-pocket expenditure
3. Two Major Components of Ayushman Bharat
| Component | Description |
|---|---|
| 1. Health & Wellness Centres (HWCs) | Strengthen primary health care system |
| 2. Pradhan Mantri Jan Arogya Yojana (PM-JAY) | Provide free health insurance of ₹5 lakh per family per year |
4. Component 1: Health & Wellness Centres (HWCs)
✅ Aim: Deliver Comprehensive Primary Health Care (CPHC)
Key Features:
- Transform existing Sub-Centres and PHCs into HWCs
- Provide preventive, promotive, curative, rehabilitative, and palliative care
- Deliver 12 health service packages
- Run by Community Health Officers (CHOs), ANMs, MPHWs, and ASHAs
Services Provided at HWCs
- Maternal and child health
- Family planning
- Adolescent health
- Non-communicable diseases (BP, diabetes, cancer)
- Mental health
- Oral, eye, and ENT care
- Elderly and palliative care
- Emergency first aid
- Health promotion (yoga, diet, lifestyle)
- Teleconsultation via e-Sanjeevani
5. Component 2: PM-JAY (Pradhan Mantri Jan Arogya Yojana)
✅ Aim: Provide financial protection for secondary and tertiary hospitalization
| Feature | Details |
|---|---|
| Coverage | ₹5 lakh per family per year |
| Beneficiaries | ~10.74 crore poor and vulnerable families |
| Mode | Cashless and paperless treatment at empanelled hospitals |
| Portability | Beneficiaries can access services across India |
| No restriction | On family size, age, gender |
| Pre-existing conditions | Covered from day one |
Identification of Beneficiaries:
- Based on Socio-Economic Caste Census (SECC) 2011
- Verified through Ayushman Card / ABHA ID
6. Health Services Covered Under PM-JAY
- Cardiac surgeries
- Cancer treatment
- Dialysis
- Orthopedic surgeries
- Maternity and neonatal care
- ENT, ophthalmology
- ICU services, diagnostics, and post-hospitalization follow-up
7. Implementation Mechanism
| Level | Agency |
|---|---|
| National | National Health Authority (NHA) |
| State | State Health Agencies (SHA) |
| District | District Implementation Units (DIU) |
8. Role of Community Health Nurse in Ayushman Bharat
| Role | Functions |
|---|---|
| At HWCs | Delivers CPHC services, health education, NCD screening |
| Health Promoter | Educates community on Ayushman card benefits |
| Facilitator | Helps register families for PM-JAY |
| Teleconsultation | Coordinates remote consultations via eSanjeevani |
| Record Keeping | Maintains electronic health records |
| Trainer | Trains ASHAs and field workers |
| Referral Agent | Refers complex cases to PM-JAY empanelled hospitals |
9. Key Achievements of Ayushman Bharat (till 2024)
- 1.5+ lakh HWCs operational across India
- Over 6 crore hospitalizations under PM-JAY
- More than 26,000 empanelled hospitals (public + private)
- Enhanced focus on NCDs and mental health screening
- Strong digital health ecosystem with ABHA ID and e-Sanjeevani
10. Challenges in Implementation
- Low awareness among rural and tribal populations
- Limited specialist services in government hospitals
- Connectivity issues for telemedicine in remote areas
- Fraudulent claims in some private hospitals
- Delays in claim reimbursements
11. Suggestions for Improvement
- Strengthen infrastructure and staffing at HWCs
- Conduct regular IEC/BCC campaigns to increase awareness
- Expand empanelment of hospitals in underserved regions
- Improve monitoring, audit, and grievance redressal mechanisms
- Increase training and capacity building of field-level staff
Universal Health Coverage (UHC)

1. Introduction
Universal Health Coverage (UHC) means that all individuals and communities receive the health services they need — when and where they need them, without financial hardship.
Global Goal:
Declared by World Health Organization (WHO) as part of the Sustainable Development Goals (SDGs) — specifically SDG Goal 3.8.
Goal 3.8: Achieve UHC including financial risk protection, access to quality essential health care services, and access to safe, effective, affordable, and quality medicines and vaccines for all.
2. Objectives of UHC
- Access for all to promotive, preventive, curative, rehabilitative, and palliative care
- Quality services irrespective of socio-economic background
- Financial protection from catastrophic health expenditure
- Improve health equity and outcomes
3. Key Components of UHC (The UHC Cube – WHO)
The UHC Cube has 3 dimensions:
| Dimension | Meaning |
|---|---|
| 1. Population Coverage | Who is covered? (Aim: Everyone) |
| 2. Services Coverage | What services are covered? (Aim: All essential health services) |
| 3. Financial Coverage | What proportion of costs is covered? (Aim: Full financial protection) |
4. Services Covered under UHC
- Health promotion (e.g., sanitation, lifestyle education)
- Preventive care (e.g., immunization, screening)
- Curative care (e.g., treatment of illness and injury)
- Rehabilitative care (e.g., physiotherapy, chronic illness care)
- Palliative care (e.g., end-of-life care, pain management)
5. UHC in the Indian Context
India is committed to achieving UHC by 2030 through the following key initiatives:
| Program | Contribution to UHC |
|---|---|
| Ayushman Bharat | Combines CPHC through HWCs and financial protection through PM-JAY |
| National Health Mission (NHM) | Strengthens rural and urban health systems |
| Janani Suraksha Yojana (JSY) | Promotes institutional deliveries |
| Janani Shishu Suraksha Karyakram (JSSK) | Free delivery, newborn and maternal care |
| Free Drugs and Diagnostics Scheme | Reduces out-of-pocket expenses |
| Digital Health Mission | Enables electronic health records, telemedicine |
6. UHC Indicators – WHO & India
| Indicator | Target |
|---|---|
| Service Coverage Index | Aim: 80+% by 2030 |
| Out-of-Pocket Expenditure | Reduce to <20% of total health expenditure |
| Skilled Birth Attendance | >90% |
| Immunization Coverage | >90% full immunization |
| Essential Services | Available in all PHCs and HWCs |
7. Role of Nurses and Community Health Workers in UHC
| Role | Description |
|---|---|
| Service Provider | Delivers promotive, preventive, and curative care |
| Health Educator | Promotes awareness on hygiene, nutrition, NCDs |
| Screening Agent | Conducts BP, diabetes, cancer, and anemia screening |
| Referral Connector | Links patients from SC/HWC to higher-level facilities |
| Data Manager | Updates electronic records, maintains HMIS |
| Telemedicine Facilitator | Supports remote consultation using e-Sanjeevani |
8. Benefits of Achieving UHC
- Reduces poverty caused by health expenses
- Improves population health outcomes
- Builds resilient health systems
- Ensures equity and social justice
- Empowers communities through health literacy
9. Challenges in Achieving UHC (India)
- Inadequate public health funding (only ~1.5% of GDP)
- Shortage of health workforce, especially in rural areas
- Urban-rural disparity in health infrastructure
- High out-of-pocket expenses for diagnostics and medicines
- Weak referral systems and low health insurance awareness
10. Suggestions to Strengthen UHC in India
- Increase public health investment to at least 2.5% of GDP
- Train and deploy more Community Health Officers, Nurses, ASHAs
- Expand Health & Wellness Centres (HWCs) for better outreach
- Provide free essential medicines and diagnostics
- Strengthen digital health systems and teleconsultation platforms
- Foster intersectoral collaboration (nutrition, sanitation, education)
FOR UNLOCK 🔓 FULL COURSE NOW. MORE DETAILS CALL US OR WATSAPP ON- 8485976407
