BSC SEM 2 UNIT 2 NURSING FOUNDATION 2
UNIT 2 The Nursing Process
The Nursing Process
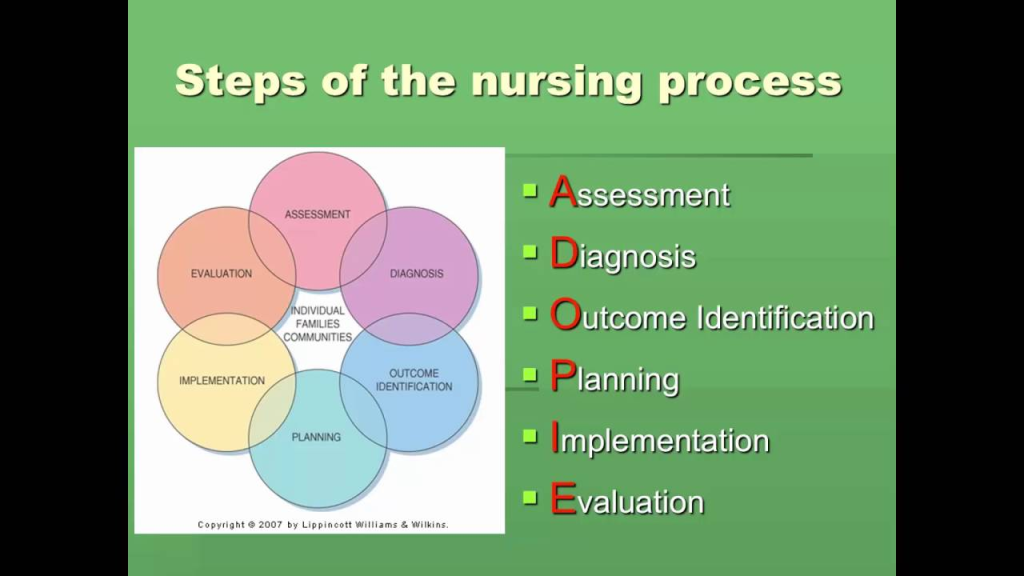
The Nursing Process is a systematic, evidence-based method used by nurses to provide individualized, patient-centered care. It serves as a framework for delivering safe, efficient, and high-quality nursing care. This process is dynamic and cyclical, consisting of five interrelated steps: Assessment, Diagnosis, Planning, Implementation, and Evaluation (ADPIE).
1. Definition of Nursing Process
The American Nurses Association (ANA) defines the nursing process as: “A critical thinking model that integrates the best evidence, clinical expertise, and patient preferences to provide individualized nursing care.”
It is a problem-solving approach that ensures continuity of care, accountability, and scientific reasoning in nursing practice.
2. Characteristics of the Nursing Process
- Systematic: Follows a structured, logical sequence.
- Dynamic: Steps are interconnected and continuous.
- Goal-Oriented: Focused on patient-centered outcomes.
- Client-Centered: Respects patients’ values, preferences, and needs.
- Collaborative: Involves interdisciplinary teamwork.
- Universally Applicable: Can be applied across all healthcare settings.
3. Steps of the Nursing Process (ADPIE)
Step 1: Assessment (Data Collection)
- Definition: The process of gathering, verifying, and documenting patient data to establish a database for nursing care.
- Types of Assessment:
- Initial assessment: Done upon admission.
- Ongoing assessment: Continuous throughout care.
- Focused assessment: Targeted at a specific issue.
- Emergency assessment: Immediate response to life-threatening conditions.
- Methods of Data Collection:
- Subjective data: Symptoms reported by the patient (e.g., pain, nausea).
- Objective data: Measurable, observable signs (e.g., BP, temperature, wound drainage).
- Sources of Data:
- Primary source: The patient.
- Secondary source: Family, healthcare providers, medical records.
- Techniques:
- Inspection
- Palpation
- Percussion
- Auscultation
- Interviewing
Step 2: Nursing Diagnosis
- Definition: A clinical judgment about a patient’s response to actual or potential health problems.
- Components of Nursing Diagnosis (PES format):
- Problem (P): The patient’s issue (e.g., “Impaired mobility”).
- Etiology (E): The cause or contributing factor (e.g., “related to stroke”).
- Signs/Symptoms (S): Supporting evidence (e.g., “as evidenced by weakness in the right arm”).
- Types of Nursing Diagnoses:
- Actual diagnosis: Current health problem (e.g., acute pain).
- Risk diagnosis: Potential health issue (e.g., risk of infection).
- Health promotion diagnosis: Readiness to improve health (e.g., readiness for enhanced nutrition).
Example: “Impaired skin integrity related to prolonged immobility as evidenced by pressure ulcers on the sacral region.”
Step 3: Planning (Goal Setting and Intervention)
- Definition: Developing a structured plan of care based on identified nursing diagnoses.
- Goals and Outcomes (SMART Criteria):
- Specific
- Measurable
- Achievable
- Realistic
- Time-bound
- Types of Interventions:
- Independent nursing interventions: Actions performed without a doctor’s order (e.g., repositioning a bedridden patient).
- Dependent interventions: Requires a physician’s order (e.g., administering medications).
- Interdependent interventions: Collaborative efforts with other healthcare professionals (e.g., working with a dietitian for a diabetic patient).
- Care Plans: Individualized written guidelines outlining nursing care.
Example: “By the end of three days, the patient will demonstrate improved pain control with a pain score of less than 3 on a scale of 10.”
Step 4: Implementation (Executing the Plan)
- Definition: Carrying out the planned interventions to achieve the desired patient outcomes.
- Types of Nursing Actions:
- Direct care interventions: Direct interactions with the patient (e.g., wound dressing, catheter care).
- Indirect care interventions: Actions performed away from the patient but on their behalf (e.g., infection control, documentation).
- Steps in Implementation:
- Reassess the patient.
- Determine the need for assistance.
- Carry out the intervention.
- Document nursing actions and patient response.
Example: Administering analgesics to reduce pain, repositioning the patient to prevent bedsores, and educating the patient on deep breathing exercises.
Step 5: Evaluation (Assessing Effectiveness)
- Definition: Determines whether nursing interventions were successful in achieving goals.
- Components of Evaluation:
- Compare patient response to expected outcomes.
- Determine if interventions need modification.
- Revise care plan if necessary.
- Types of Evaluation:
- Ongoing evaluation: Continuous monitoring (e.g., checking vitals after medication).
- Outcome evaluation: Final assessment (e.g., wound healed after dressing changes).
Example: “After three days of repositioning and skincare interventions, the patient’s sacral ulcer has decreased in size by 20%.”
4. Benefits of the Nursing Process
- Ensures systematic, evidence-based care.
- Promotes individualized, patient-centered care.
- Enhances critical thinking and problem-solving.
- Facilitates documentation and legal protection.
- Encourages interdisciplinary collaboration.
5. Application of Nursing Process in Different Settings
- Medical-Surgical Nursing: Assessing post-operative patients for complications, pain management, wound care.
- Maternal-Child Health Nursing: Monitoring labor progression, postpartum care, neonatal assessments.
- Community Health Nursing: Health education, immunization programs, home care visits.
- Mental Health Nursing: Counseling, behavior modification, medication compliance.
- Critical Care Nursing: Emergency interventions, ventilator management, monitoring life-threatening conditions.
6. Challenges in Implementing the Nursing Process
- Time constraints and heavy workload.
- Lack of nursing knowledge and critical thinking skills.
- Inadequate documentation and assessment tools.
- Resistance from patients and families.
- Shortage of resources and staff in healthcare settings.
Critical Thinking Competencies
1. Introduction to Critical Thinking in Nursing
Critical thinking is an essential skill for nurses, allowing them to make sound clinical decisions, provide quality patient care, and respond effectively to complex healthcare situations. It involves analyzing, reasoning, problem-solving, evaluating evidence, and making informed decisions based on clinical experience and scientific knowledge.
Definition of Critical Thinking in Nursing
According to the American Nurses Association (ANA): “Critical thinking in nursing is a purposeful, self-regulatory process that ensures clinical reasoning, judgment, and problem-solving for quality patient outcomes.”
Importance of Critical Thinking in Nursing
- Enhances clinical decision-making.
- Improves patient safety and quality of care.
- Helps in prioritizing nursing interventions.
- Supports evidence-based practice.
- Strengthens problem-solving in complex situations.
- Encourages ethical decision-making.
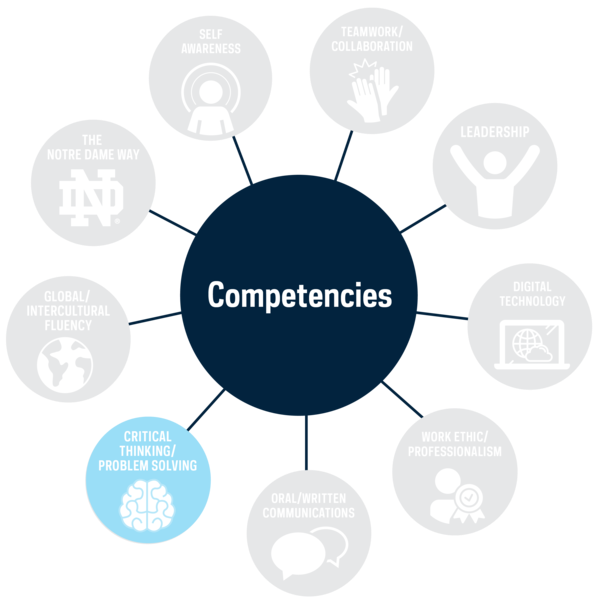
2. Critical Thinking Competencies in Nursing
Critical thinking competencies are intellectual skills that enable nurses to think analytically and solve problems effectively in clinical practice. These competencies can be categorized into three broad types:
- General Critical Thinking Competencies
- Specific Critical Thinking in Clinical Situations
- Specific Critical Thinking in Nursing Process
1. General Critical Thinking Competencies
These are the fundamental reasoning abilities applicable in all disciplines, including nursing.
a) Scientific Method
The scientific method is a structured, logical approach used in research and nursing problem-solving. It includes:
- Identifying the problem – Understanding the issue in patient care.
- Forming a hypothesis – Creating a possible explanation.
- Testing the hypothesis – Conducting assessments and interventions.
- Evaluating results – Analyzing the effectiveness of interventions.
- Drawing conclusions – Modifying the care plan based on findings.
Example: A nurse notices a patient experiencing shortness of breath and uses the scientific method to investigate the cause, test interventions (oxygen therapy), and evaluate patient improvement.
b) Problem-Solving
Problem-solving involves identifying a patient issue, evaluating possible solutions, and selecting the most effective action.
- Trial-and-error problem-solving: Testing different interventions until the best one is found.
- Intuitive problem-solving: Using experience and gut feeling to make decisions.
- Logical reasoning problem-solving: Using evidence-based strategies to address patient needs.
Example: A nurse observes a post-surgical patient with increasing pain despite medication and explores possible reasons (infection, medication effectiveness, positioning).
c) Decision-Making
Decision-making is a deliberate process of choosing the best action from available options based on patient needs.
Steps in Decision-Making:
- Identify the problem.
- Gather relevant data.
- Identify alternatives.
- Weigh the pros and cons of each alternative.
- Select the best course of action.
- Implement the decision.
- Evaluate the effectiveness.
Example: A nurse must decide whether to administer pain medication or use non-pharmacological pain relief measures (heat therapy, repositioning) based on the patient’s condition.
2. Specific Critical Thinking in Clinical Situations
These competencies apply directly to nursing practice and patient care.
a) Diagnostic Reasoning and Inference
- Diagnostic reasoning involves analyzing patient data to determine a health problem.
- Inference means drawing logical conclusions based on available evidence.
Example: A nurse notices wheezing and labored breathing in a patient and infers that the patient may have an asthma attack, leading to appropriate interventions.
b) Clinical Decision-Making
- Clinical decision-making involves assessing patient conditions and selecting appropriate nursing actions.
- It requires prioritization skills to address life-threatening situations first.
Example: A nurse in an emergency room prioritizes a patient with chest pain over a patient with a minor wound.
c) Inductive and Deductive Reasoning
- Inductive reasoning: Starts with specific observations and leads to general conclusions.
- Example: A nurse notices multiple patients with high fever, cough, and difficulty breathing and suspects an outbreak of pneumonia.
- Deductive reasoning: Starts with a general theory or rule and applies it to specific cases.
- Example: A nurse knows that diabetics are at risk of poor wound healing and checks a diabetic patient’s surgical incision site regularly.
3. Specific Critical Thinking in Nursing Process
The Nursing Process (ADPIE) requires critical thinking competencies at each step.
| Step | Critical Thinking Competency Required |
|---|---|
| Assessment | Data collection, observation, interviewing, interpretation. |
| Diagnosis | Analyzing patterns, making clinical inferences. |
| Planning | Setting priorities, goal formulation, predicting outcomes. |
| Implementation | Selecting evidence-based interventions, problem-solving. |
| Evaluation | Measuring patient response, modifying care plans. |
Example: A nurse assesses a post-operative patient and, noticing low urine output, applies critical thinking to determine whether it is due to dehydration or kidney dysfunction.
3. Strategies to Improve Critical Thinking in Nursing
- Ask Reflective Questions: “Why did I choose this intervention?”
- Use Case Studies & Simulations: Practice real-world clinical scenarios.
- Engage in Evidence-Based Practice: Read research articles and apply findings.
- Collaborate with Colleagues: Seek second opinions and discuss cases.
- Practice Clinical Reasoning Daily: Assess patient problems and make logical decisions.
- Keep Learning: Attend workshops, nursing conferences, and continuing education programs.
4. Barriers to Critical Thinking in Nursing
- Lack of knowledge or experience.
- Time constraints and workload pressure.
- Fear of making mistakes.
- Resistance to new ideas or feedback.
- Over-reliance on routines rather than analytical thinking.
5. Role of Critical Thinking in Different Nursing Specialties
| Nursing Specialty | Application of Critical Thinking |
|---|---|
| Medical-Surgical Nursing | Analyzing post-op complications, infection control. |
| Critical Care Nursing | Quick decision-making in emergencies. |
| Mental Health Nursing | Assessing patient behavior, therapeutic communication. |
| Community Health Nursing | Evaluating health promotion programs. |
| Pediatric Nursing | Recognizing developmental delays. |
Attitudes for Critical Thinking in Nursing

1. Introduction
Critical thinking in nursing is not just about having cognitive skills; it also involves adopting certain attitudes that support logical reasoning, sound clinical judgment, and effective decision-making. These attitudes guide how nurses approach problems, evaluate evidence, and interact with patients and colleagues.
Definition of Attitudes in Critical Thinking
Attitudes for critical thinking refer to dispositions or mindsets that enhance a nurse’s ability to analyze situations objectively, question assumptions, and remain open-minded while making clinical decisions.
2. Key Attitudes Essential for Critical Thinking in Nursing
The following attitudes are crucial in fostering critical thinking and improving nursing practice:
1. Independence of Thought (Intellectual Autonomy)
- Nurses must think for themselves rather than relying solely on external authority.
- They should evaluate data and make informed decisions rather than blindly following procedures.
- Example: A nurse questions a routine medication order when it seems inappropriate for the patient’s current condition.
2. Intellectual Humility
- Recognizing that one does not know everything.
- Being open to learning from others, research, and experience.
- Example: A nurse admits to not knowing the latest pain management guidelines and seeks updated information.
3. Intellectual Courage
- Willingness to challenge traditional practices, policies, and authority when necessary.
- Accepting and addressing controversial or new ideas despite opposition.
- Example: A nurse advocates for a change in a hospital’s infection control policy after reviewing recent research.
4. Intellectual Empathy
- Understanding and respecting different perspectives, beliefs, and emotions.
- Seeing situations from the patient’s viewpoint.
- Example: A nurse acknowledges a patient’s cultural concerns about certain medical treatments and seeks alternatives.
5. Intellectual Integrity
- Holding oneself accountable for consistent application of critical thinking.
- Being honest about mistakes and biases.
- Example: A nurse admits an error in documentation and takes immediate steps to correct it.
6. Intellectual Perseverance
- Commitment to exploring all possible solutions rather than settling for the easiest answer.
- Example: A nurse investigates multiple interventions for pressure ulcer prevention rather than relying on standard repositioning.
7. Fair-Mindedness
- Being objective and avoiding personal bias.
- Considering all perspectives before making a decision.
- Example: A nurse treats all patients with equal care, regardless of socioeconomic background.
8. Curiosity (Inquisitiveness)
- A desire to ask questions and seek knowledge.
- Constantly looking for new and better ways to provide patient care.
- Example: A nurse reads recent studies on wound healing to improve patient outcomes.
9. Confidence in Reasoning
- Trusting logical thinking and evidence-based decision-making over emotional responses.
- Example: A nurse uses data from patient monitoring systems rather than subjective observations to assess patient improvement.
10. Open-Mindedness
- Being receptive to different ideas and approaches.
- Avoiding rigid thinking in nursing practice.
- Example: A nurse listens to a junior nurse’s suggestion for a new way to manage pain and considers its validity.
11. Responsibility and Accountability
- Taking ownership of one’s decisions and actions.
- Ensuring patient safety and ethical practice.
- Example: A nurse ensures correct medication administration by double-checking patient records.
12. Creativity
- Thinking outside the box to solve problems.
- Example: A nurse develops an innovative way to educate patients about diabetes management using interactive tools.
3. How to Develop These Attitudes in Nursing Practice
- Self-Reflection: Regularly evaluate personal thinking and decision-making.
- Continuous Learning: Attend workshops, read journals, and stay updated with new research.
- Active Listening: Engage with colleagues, mentors, and patients with an open mind.
- Practice Patience: Develop perseverance by analyzing complex cases before jumping to conclusions.
- Seek Feedback: Encourage constructive criticism to refine critical thinking skills.
Levels of Critical Thinking

1. Introduction
Critical thinking in nursing is a hierarchical process that develops over time with experience, education, and exposure to clinical scenarios. Patricia Benner’s “Novice to Expert” theory and Kataoka-Yahiro and Saylor’s Model describe how nurses progress in their critical thinking abilities.
Understanding these levels helps nurses evaluate their thinking skills and improve their clinical decision-making to provide safe and effective patient care.
2. Three Levels of Critical Thinking in Nursing
According to Kataoka-Yahiro and Saylor’s Model (1994), there are three levels of critical thinking in nursing:
1. Basic Critical Thinking (Novice Level)
- At this level, nurses follow rules and procedures without questioning them.
- Thinking is concrete and task-oriented rather than analytical.
- They rely on experts, senior nurses, or protocols to make decisions.
- Limited ability to analyze alternative solutions or adapt to changing situations.
✅ Example:
A new graduate nurse follows the step-by-step procedure for inserting a Foley catheter but doesn’t adjust for patient discomfort or other clinical signs.
2. Complex Critical Thinking (Intermediate Level)
- Nurses begin to question authority and traditional practices.
- They consider alternative solutions rather than following rigid guidelines.
- Decision-making becomes more independent, and experience helps in clinical reasoning.
- They understand that one rule does not apply to every patient and use multiple sources of information for decision-making.
✅ Example:
A nurse is caring for a post-operative patient experiencing pain despite receiving prescribed pain medication. Instead of blindly administering another dose, the nurse assesses the patient further and considers repositioning, heat therapy, or distraction techniques before escalating medication.
3. Commitment Level of Critical Thinking (Expert Level)
- The nurse makes independent decisions based on evidence, experience, and best practices.
- Uses intuition and deep clinical knowledge to anticipate problems before they occur.
- Takes responsibility for decision-making and evaluates patient outcomes continuously.
- Engages in self-reflection and lifelong learning to improve practice.
✅ Example:
An ICU nurse notices subtle changes in a patient’s vital signs that indicate early signs of sepsis before lab results confirm infection. The nurse advocates for early intervention, preventing complications.
3. Factors Influencing Levels of Critical Thinking in Nursing
- Clinical Experience: More patient encounters help nurses improve reasoning.
- Education and Training: Higher-level degrees and certifications enhance critical thinking.
- Mentorship: Guidance from experienced nurses accelerates skill development.
- Practice Environment: Supportive work environments encourage questioning and problem-solving.
- Reflection and Self-Evaluation: Nurses who analyze their past decisions improve their thinking skills.
Nursing Process Overview
1. Introduction
The Nursing Process is a systematic, patient-centered, and goal-oriented method used by nurses to provide high-quality, individualized care. It serves as the foundation of nursing practice, ensuring that patient needs are identified, interventions are planned and implemented, and outcomes are evaluated.
This process follows a structured five-step model known as ADPIE:
- Assessment
- Diagnosis
- Planning
- Implementation
- Evaluation
2. Characteristics of the Nursing Process
- Systematic: Follows a logical and structured sequence.
- Dynamic: Continuous and flexible based on patient needs.
- Goal-Oriented: Aims to achieve specific patient outcomes.
- Client-Centered: Tailored to meet each patient’s unique needs.
- Collaborative: Involves teamwork with patients, families, and healthcare professionals.
- Universal: Can be applied across different healthcare settings.
3. Five Steps of the Nursing Process (ADPIE)
1. Assessment (Data Collection)
- Definition: Gathering and analyzing patient data to establish a baseline for care.
- Types of Data:
- Subjective data: Patient-reported symptoms (e.g., pain, nausea).
- Objective data: Measurable, observable signs (e.g., vital signs, lab results).
- Data Collection Methods:
- Interviewing the patient and family.
- Conducting physical examinations.
- Reviewing medical history and records.
- Example: A nurse assesses a diabetic patient’s blood glucose levels, dietary habits, and signs of neuropathy to determine care needs.
2. Nursing Diagnosis
- Definition: Identifying the patient’s actual or potential health problems based on assessment data.
- Types of Nursing Diagnoses:
- Actual Diagnosis: Current health issue (e.g., impaired skin integrity).
- Risk Diagnosis: Potential problem (e.g., risk for infection).
- Health Promotion Diagnosis: Readiness to improve health (e.g., readiness for enhanced nutrition).
- Format (PES Model):
- Problem (P): What is the patient’s issue?
- Etiology (E): What is causing it?
- Signs/Symptoms (S): What are the indicators?
- Example: “Impaired mobility related to stroke as evidenced by muscle weakness and difficulty walking.”
3. Planning (Setting Goals and Interventions)
- Definition: Developing measurable goals and interventions to improve the patient’s condition.
- Goal-Setting (SMART Criteria):
- Specific
- Measurable
- Achievable
- Realistic
- Time-bound
- Types of Nursing Interventions:
- Independent: Actions nurses perform without a doctor’s order (e.g., turning a bedridden patient).
- Dependent: Actions requiring a physician’s order (e.g., medication administration).
- Interdependent: Collaborative interventions (e.g., working with a dietitian for meal planning).
- Example: A goal for a patient with pneumonia may be: “The patient’s oxygen saturation will remain above 95% within 24 hours with oxygen therapy.”
4. Implementation (Carrying Out the Plan)
- Definition: Executing the planned nursing interventions.
- Types of Nursing Actions:
- Direct care: Hands-on patient care (e.g., wound dressing, administering IV fluids).
- Indirect care: Supporting patient care (e.g., infection control, documentation).
- Example: A nurse administers prescribed antibiotics and performs respiratory therapy to help a patient recover from pneumonia.
5. Evaluation (Assessing Effectiveness)
- Definition: Determining whether the interventions achieved the desired outcomes.
- Key Actions in Evaluation:
- Comparing patient response to expected outcomes.
- Adjusting the care plan if goals are unmet.
- Continuing or modifying nursing interventions.
- Example: If a patient’s pain level remains high despite medication, the nurse may consult the physician to adjust the pain management plan.
4. Importance of the Nursing Process
- Ensures structured and effective patient care.
- Enhances clinical decision-making and critical thinking.
- Improves communication between healthcare professionals.
- Supports evidence-based practice and patient safety.
- Helps in accurate documentation and legal protection.
5. Challenges in Implementing the Nursing Process
- Time constraints in busy healthcare settings.
- Incomplete or inaccurate patient data collection.
- Resistance from patients and families in accepting care plans.
- Lack of nursing knowledge or critical thinking skills.
Assessment in Nursing

1. Introduction to Assessment in Nursing
Assessment is the first and most critical step in the nursing process (ADPIE). It involves systematic data collection to understand the patient’s health status, identify actual or potential health problems, and establish a baseline for care planning.
Definition of Nursing Assessment:
“Assessment is the collection, validation, and interpretation of patient data to identify health problems and plan effective nursing care.”
2. Purpose of Nursing Assessment
- Establishes baseline data about the patient.
- Identifies actual and potential health problems.
- Determines risk factors affecting health.
- Forms the basis for nursing diagnosis, planning, and interventions.
- Helps monitor patient progress over time.
- Ensures patient-centered care by considering the patient’s needs, values, and preferences.
3. Types of Nursing Assessments
Nursing assessments are categorized into different types based on the timing and purpose of data collection.
1. Initial Assessment (Comprehensive Assessment)
- Conducted at the time of admission or first contact with the patient.
- Provides a holistic view of the patient’s physical, psychological, social, and spiritual health.
- Used to create an individualized care plan.
- Includes detailed medical history, physical examination, and psychosocial assessment.
✅ Example:
A nurse conducts a comprehensive assessment of a newly admitted diabetic patient, including blood sugar levels, dietary habits, physical activity, and medication compliance.
2. Focused Assessment
- Performed when a patient has a specific complaint or condition.
- Targets one body system or a particular health problem.
- Can be done at any time during care.
✅ Example:
A patient reports shortness of breath. The nurse performs a focused respiratory assessment, including lung auscultation, oxygen saturation measurement, and checking for signs of cyanosis
3. Ongoing Assessment
- Conducted throughout patient care to track progress.
- Helps evaluate the effectiveness of interventions.
- Identifies new problems or complications.
✅ Example:
A nurse monitors a postoperative patient’s pain levels, wound healing, and vital signs at regular intervals.
4. Emergency Assessment
- Done immediately in life-threatening situations.
- Focuses on airway, breathing, circulation (ABCs).
- Rapid assessment helps make quick clinical decisions.
✅ Example:
A patient in the ER with a suspected heart attack undergoes an emergency assessment, including ECG, vital signs, oxygen levels, and pain evaluation.
4. Methods of Data Collection
Data is collected from various sources using different techniques.
A. Sources of Data
- Primary Source:
- The patient (best source for subjective data).
- Example: A patient reports nausea, headache, and chest pain.
- Secondary Source:
- Family members, caregivers, medical records, other healthcare professionals.
- Example: A family member states, “My father has been feeling weak and hasn’t eaten for two days.”
- Tertiary Source:
- Research articles, textbooks, healthcare databases (used for evidence-based practice).
B. Types of Data
- Subjective Data (Symptoms):
- Information verbalized by the patient.
- Cannot be measured directly.
- Example: “I feel dizzy and have a sharp pain in my stomach.”
- Objective Data (Signs):
- Observable, measurable, and verifiable findings.
- Collected using inspection, palpation, percussion, and auscultation.
- Example: BP: 150/90 mmHg, HR: 110 bpm, pale skin.
5. Techniques of Physical Assessment
Nurses use four fundamental techniques for a systematic physical examination.
1. Inspection
- Visual examination of the body for abnormalities.
- Observes skin color, posture, facial expressions, and wounds.
- Example: A nurse notices jaundice in a hepatitis patient.
2. Palpation
- Using hands to feel for abnormalities in organs, tissues, or body temperature.
- Assesses swelling, tenderness, masses, and pulse strength.
- Example: A nurse palpates the abdomen for tenderness in appendicitis.
3. Percussion
- Tapping body surfaces to assess underlying structures.
- Determines organ size, fluid accumulation, or air pockets.
- Example: Dullness in lung percussion suggests pneumonia.
4. Auscultation
- Listening to body sounds using a stethoscope.
- Assesses heart sounds, lung sounds, bowel sounds.
- Example: Crackles in lung auscultation may indicate pulmonary edema.
6. Components of a Nursing Health History
A comprehensive health history includes the following:
- Biographical Data: Name, age, gender, marital status, occupation.
- Chief Complaint (CC): The main reason the patient is seeking care.
- History of Present Illness (HPI):
- Onset, duration, intensity, location of symptoms.
- Example: “My headache started two days ago, it’s constant, and feels like a sharp pain on the left side of my head.”
- Past Medical History (PMH): Previous illnesses, surgeries, allergies, medications.
- Family History: Genetic conditions, diabetes, hypertension, cancers.
- Lifestyle and Habits: Diet, smoking, alcohol, exercise.
- Psychosocial History: Stress, anxiety, coping mechanisms, social support.
- Review of Systems (ROS): Assessment of all body systems to identify hidden issues.
7. Documentation of Nursing Assessment
- Accurate, complete, and timely documentation is essential.
- Use standardized formats, such as:
- SOAP Notes:
- Subjective (patient’s statement).
- Objective (measurable data).
- Assessment (nursing diagnosis).
- Plan (interventions).
- DAR Notes (Data-Action-Response).
- Electronic Health Records (EHRs) for systematic data entry.
- SOAP Notes:
✅ Example of Documentation (SOAP Format):
S: “I have been feeling extremely weak and dizzy for the past three days.”
O: BP: 90/60 mmHg, HR: 105 bpm, pale skin.
A: Risk for dehydration related to decreased fluid intake.
P: Encourage oral fluids, monitor electrolytes, administer IV fluids if needed.
8. Common Challenges in Nursing Assessment
- Language barriers affecting patient communication.
- Unreliable patient information due to confusion or memory issues.
- Time constraints in busy clinical settings.
- Lack of patient cooperation in answering health-related questions.
Solution:
- Use interpreters for language barriers.
- Verify information with family or medical records.
- Build trust and establish rapport with the patient.
Collection of Data in Nursing: Types, Sources, and Methods

1. Introduction
Data collection is the first and most crucial step in the assessment phase of the nursing process (ADPIE). It involves gathering, verifying, and documenting information to establish a comprehensive understanding of the patient’s health status.
Proper data collection enables nurses to:
- Identify actual and potential health problems.
- Develop an individualized care plan.
- Monitor patient progress over time.
2. Types of Data in Nursing
Nursing data is classified into two main types based on how the information is obtained.
1. Subjective Data (Symptoms)
- Definition: Information reported by the patient that cannot be directly measured or observed.
- Also known as: Symptoms or patient statements.
- Collected through: Interviews, health history, questionnaires.
- Examples:
- “I feel dizzy and nauseous.”
- “I have a sharp pain in my lower back.”
- “I feel anxious and can’t sleep at night.”
✅ Importance: Helps understand the patient’s perceptions, beliefs, and emotions about their health.
2. Objective Data (Signs)
- Definition: Information that is measurable, observable, and verifiable through physical examination, laboratory tests, or medical equipment.
- Also known as: Signs or clinical findings.
- Collected through: Inspection, palpation, percussion, auscultation, diagnostic tests.
- Examples:
- Blood pressure: 140/90 mmHg.
- Temperature: 102°F (fever).
- Wound: Red, swollen, with pus drainage.
- Heart rate: 120 bpm (tachycardia).
✅ Importance: Provides factual evidence that supports subjective data and aids in accurate diagnosis.
3. Sources of Data in Nursing
Data can come from different primary and secondary sources, depending on the availability and reliability of the information.
1. Primary Source
- Definition: The patient is the main source of information, providing first-hand details about symptoms, feelings, and concerns.
- Examples:
- “I have a headache that started this morning.”
- “I feel anxious when I take this medication.”
- Advantages:
- Most accurate and reliable if the patient is conscious and able to communicate.
- Limitations:
- Unreliable if the patient is unconscious, confused, or non-verbal.
✅ Best for: Health history, pain assessment, emotional status.
2. Secondary Source
- Definition: Information gathered from other people or documents when the patient cannot provide reliable data.
- Examples of Secondary Sources:
- Family Members/Caregivers: Provide details when the patient is too ill, unconscious, or mentally impaired.
- Example: “My father has been vomiting for the past two days and hasn’t eaten.”
- Medical Records: Includes previous diagnoses, lab results, treatment history.
- Example: A nurse reviews past CT scan reports for a stroke patient.
- Healthcare Team (Doctors, Physiotherapists, Dietitians): Provides interdisciplinary insights into the patient’s condition.
- Example: A physiotherapist reports that a stroke patient has limited mobility in the right leg.
- Family Members/Caregivers: Provide details when the patient is too ill, unconscious, or mentally impaired.
✅ Best for: Chronic illness history, previous treatments, medication history.
3. Tertiary Source
- Definition: Information obtained from textbooks, research articles, online databases, or healthcare protocols.
- Examples:
- Medical journals on new treatment guidelines for diabetes.
- Research papers on wound healing techniques.
- Online databases like PubMed, CINHAL, Cochrane Library.
- Used for: Evidence-based practice (EBP), research, updating nursing knowledge.
✅ Best for: Planning interventions, clinical guidelines, and research.
4. Methods of Data Collection in Nursing
There are various ways to collect patient data, categorized into interviewing, observation, physical examination, and diagnostic tests.
1. Interview (Health History Collection)
- Definition: A structured conversation between the nurse and the patient to obtain health-related information.
- Types of Interviews:
- Formal (Structured): Pre-determined set of questions.
- Informal (Unstructured): Open-ended, patient-led discussion.
- Phases of a Nursing Interview:
- Introduction: Establish rapport, explain purpose.
- Working Phase: Ask open-ended and focused questions.
- Termination: Summarize findings, clarify doubts.
✅ Best for: Subjective data collection (patient history, lifestyle, concerns).
2. Observation
- Definition: The process of noticing and interpreting patient behavior, appearance, and symptoms.
- Types of Observations:
- General observation: Body posture, facial expressions, skin color.
- Behavioral observation: Anxiety, confusion, aggression.
- Clinical observation: Sweating, labored breathing, signs of pain.
- Example: A nurse notices that a patient is clutching their chest, pale, and breathing heavily, which may indicate a heart attack.
✅ Best for: Detecting non-verbal symptoms, mental status, and emergency conditions.
3. Physical Examination
- Definition: A hands-on assessment using inspection, palpation, percussion, and auscultation to detect abnormalities.
- Techniques Used in Physical Examination:
- Inspection: Looking at skin, wounds, posture.
- Palpation: Feeling for swelling, lumps, temperature changes.
- Percussion: Tapping to assess fluid/air in organs (e.g., lung sounds).
- Auscultation: Listening to heart, lung, and bowel sounds using a stethoscope.
✅ Best for: Diagnosing respiratory, cardiac, and abdominal issues.
4. Diagnostic and Laboratory Tests
- Definition: Tests that provide objective, measurable data to confirm diagnoses.
- Examples of Diagnostic Tests:
- Blood tests (CBC, glucose, electrolytes).
- Imaging (X-ray, MRI, CT scan, ECG).
- Urine/stool analysis.
- Example: A nurse reviews ECG results to confirm if a patient has arrhythmia.
✅ Best for: Confirming infections, organ dysfunction, metabolic disorders.
5. Challenges in Data Collection
- Communication barriers (language, unconscious patient).
- Inconsistent or incomplete patient history.
- Time constraints in emergency settings.
- Patient’s unwillingness to share information.
✅ Solutions:
- Use interpreters for language barriers.
- Cross-check medical records for accuracy.
- Build trust and rapport with the patient.
Organizing Data in Nursing Assessment
1. Introduction to Data Organization in Nursing
Organizing data is a crucial step in the nursing assessment process. It involves systematically arranging collected patient information to ensure accurate analysis, proper diagnosis, and effective care planning. Proper organization helps in identifying patterns, prioritizing issues, and documenting findings clearly and efficiently.
2. Importance of Organizing Data in Nursing
- Ensures logical and structured care planning.
- Prevents misinterpretation and errors in diagnosis.
- Helps in prioritizing patient needs efficiently.
- Facilitates easy retrieval of information for future reference.
- Improves communication among healthcare professionals.
- Ensures compliance with documentation standards and legal requirements.
3. Methods of Organizing Data in Nursing
Data can be organized using different frameworks and models to provide clarity and efficiency in patient assessment.
1. Gordon’s Functional Health Patterns (FHP)
Developed by Marjory Gordon, this model categorizes patient data into 11 functional health patterns to ensure a comprehensive assessment.
| Functional Health Pattern | Example Data |
|---|---|
| Health Perception–Health Management | Patient’s beliefs about health, past illnesses, adherence to medication. |
| Nutritional-Metabolic | Dietary habits, fluid intake, BMI, lab values (glucose, electrolytes). |
| Elimination | Bowel and bladder function, urinary incontinence, constipation. |
| Activity-Exercise | Mobility, exercise habits, fatigue, ADLs (Activities of Daily Living). |
| Sleep-Rest | Sleep quality, insomnia, use of sleep aids. |
| Cognitive-Perceptual | Memory, problem-solving ability, sensory deficits (vision, hearing). |
| Self-Perception–Self-Concept | Body image, self-esteem, emotional status. |
| Role-Relationship | Family roles, social support, occupational history. |
| Sexuality-Reproductive | Menstrual history, sexual activity, reproductive health. |
| Coping-Stress Tolerance | Stress management, coping strategies, anxiety levels. |
| Value-Belief | Cultural, spiritual, and religious beliefs influencing health decisions. |
✅ Best for: Comprehensive and holistic patient assessments.
2. Body Systems Model (Medical Model)
This model organizes data based on body systems, similar to a head-to-toe assessment.
| Body System | Example Data |
|---|---|
| Neurological | Consciousness level, reflexes, motor function, sensory function. |
| Cardiovascular | Blood pressure, pulse, heart sounds, peripheral circulation. |
| Respiratory | Breath sounds, oxygen saturation, coughing, shortness of breath. |
| Gastrointestinal | Bowel sounds, appetite, nausea, vomiting, stool patterns. |
| Genitourinary | Urinary frequency, incontinence, pain during urination. |
| Musculoskeletal | Muscle strength, joint mobility, posture, gait. |
| Integumentary (Skin) | Skin color, temperature, lesions, wounds, pressure ulcers. |
| Endocrine | Blood glucose levels, thyroid function, diabetes management. |
✅ Best for: Organizing physical examination findings and diagnostic test results.
3. Maslow’s Hierarchy of Needs Model
Maslow’s model prioritizes data based on the urgency of human needs, from basic survival to psychological and self-fulfillment needs.
| Maslow’s Level | Example Data |
|---|---|
| Physiological Needs | Airway, breathing, circulation (ABC), food, hydration, sleep, pain. |
| Safety Needs | Fall risk, infection control, medication safety. |
| Love/Belonging Needs | Social relationships, emotional support, mental health concerns. |
| Esteem Needs | Confidence, self-worth, independence in ADLs. |
| Self-Actualization Needs | Personal growth, goal-setting in recovery. |
✅ Best for: Prioritizing nursing diagnoses and interventions.
4. SOAP Format (Problem-Oriented Documentation)
The SOAP method structures nursing documentation for clarity and efficiency.
| Component | Example Documentation |
|---|---|
| S (Subjective Data) | “Patient reports severe headache and nausea since this morning.” |
| O (Objective Data) | BP: 150/90 mmHg, HR: 100 bpm, Temp: 101°F. |
| A (Assessment) | Risk for dehydration due to persistent nausea and vomiting. |
| P (Plan) | Administer IV fluids, monitor hydration status, educate patient on fluid intake. |
✅ Best for: Structuring progress notes and medical records.
5. PIE Format (Problem-Intervention-Evaluation)
This method focuses on nursing interventions and their effectiveness.
| Component | Example Documentation |
|---|---|
| P (Problem) | “Patient has an elevated temperature of 102°F due to infection.” |
| I (Intervention) | “Administered prescribed antibiotics and encouraged fluid intake.” |
| E (Evaluation) | “Temperature reduced to 99°F, patient reports feeling better.” |
✅ Best for: Tracking nursing care effectiveness.
6. DAR Format (Data-Action-Response)
The DAR format is used for focused charting on specific patient issues.
| Component | Example Documentation |
|---|---|
| D (Data) | “Patient reports pain level of 8/10 in the lower back.” |
| A (Action) | “Administered analgesics as per prescription and repositioned patient.” |
| R (Response) | “Pain reduced to 4/10 within 30 minutes, patient comfortable.” |
✅ Best for: Documenting problem-focused nursing actions.
4. Best Practices for Organizing Data in Nursing
- Ensure systematic data entry: Use structured forms and templates.
- Prioritize urgent patient needs: Follow Maslow’s model in emergencies.
- Maintain consistency: Use SOAP, PIE, or DAR formats for documentation.
- Keep information up to date: Regularly update and validate patient records.
- Ensure confidentiality: Follow HIPAA and hospital policies for secure documentation.
5. Challenges in Data Organization
| Challenge | Solution |
|---|---|
| Large volumes of data | Use electronic health records (EHRs) for efficient storage and retrieval. |
| Inconsistent documentation | Train staff to use standardized formats (SOAP, PIE, DAR). |
| Difficulty in prioritization | Apply Maslow’s Hierarchy or Gordon’s Functional Patterns. |
| Communication barriers | Use structured handoff reports (e.g., SBAR – Situation, Background, Assessment, Recommendation). |
Validating Data in Nursing Assessment
1. Introduction to Data Validation
Data validation in nursing assessment ensures that the information collected is accurate, complete, and reliable before making clinical decisions. It involves double-checking, cross-referencing, and confirming data to prevent errors in diagnosis and treatment.
🔹 Why is Data Validation Important?
- Prevents misdiagnosis and medical errors.
- Ensures accurate nursing diagnoses and care plans.
- Helps avoid false assumptions about patient conditions.
- Improves patient safety and quality of care.
2. Definition of Data Validation
Data validation is the process of verifying that collected patient data is complete, accurate, and consistent before using it for diagnosis and treatment. It involves:
- Checking inconsistencies or discrepancies.
- Comparing subjective and objective data.
- Consulting other sources (medical records, family, lab reports).
✅ Example:
A patient says they are not in pain (subjective data), but their facial expressions and BP of 160/100 mmHg suggest otherwise (objective data). The nurse must validate this discrepancy before concluding.
3. Steps of Validating Data in Nursing
1. Identify Data That Needs Validation
Not all data needs validation, but certain types require further confirmation, including:
- Conflicting data (e.g., patient denies pain, but their vital signs show distress).
- Unusual findings (e.g., extremely high blood sugar in a non-diabetic patient).
- Missing or incomplete data (e.g., patient history lacks medication details).
- Inconsistencies between sources (e.g., patient states they have never had surgery, but their records show an appendectomy).
✅ Example:
A nurse notices a pulse rate of 40 bpm in a healthy athlete. Since this is lower than normal, it should be validated by checking past medical history to confirm if the patient has bradycardia due to fitness.
2. Compare Subjective and Objective Data
- Subjective Data: What the patient says.
- Objective Data: What the nurse observes or measures.
- If there is a mismatch, validation is required.
✅ Example:
A patient reports no fever, but the nurse measures a temperature of 101°F. Further validation is needed to determine if the patient is aware of symptoms or if the reading is incorrect.
3. Check Data with Additional Observations
- Observe non-verbal cues (e.g., grimacing, fidgeting, sweating).
- Reassess using different methods (e.g., measure BP in both arms if one reading is abnormal).
✅ Example:
A patient claims to have no difficulty breathing, but the nurse observes nasal flaring, labored breathing, and wheezing. This requires further validation.
4. Consult Secondary Sources
If data is unclear, cross-check with:
- Family members or caregivers (for confused/unconscious patients).
- Medical records and previous assessments.
- Lab tests and diagnostic reports.
✅ Example:
A patient with memory loss states they are not on any medications, but their medical records show they are on hypertension treatment. The nurse validates the information by confirming with family members.
5. Use Clinical Judgement and Critical Thinking
- Apply nursing knowledge to assess whether data is logical or unusual.
- Consider patient history, cultural beliefs, and environmental factors.
- If in doubt, seek clarification from senior nurses or physicians.
✅ Example:
A patient with diabetes reports no symptoms of hypoglycemia, but their blood sugar is dangerously low (40 mg/dL). The nurse reassesses symptoms and prepares for intervention.
4. Methods of Data Validation in Nursing
1. Reassessing the Patient
- Rechecking vital signs, lab values, and physical assessments.
- Example: If BP seems too high, recheck it after 5 minutes of rest.
2. Comparing Data with Norms and Standards
- Cross-referencing findings with clinical guidelines.
- Example: A pulse of 50 bpm in an elderly patient may indicate bradycardia, while the same in an athlete may be normal.
3. Seeking a Second Opinion
- Consulting another nurse or physician for verification.
- Example: If a lung sound is unclear, ask another nurse to auscultate and confirm.
4. Using Additional Diagnostic Tests
- Confirming with lab tests, X-rays, CT scans, ECG, etc..
- Example: A patient complains of chest pain; an ECG is done to validate the possibility of a heart attack.
5. Reviewing Medical Records
- Checking past medical history, medications, and previous assessments.
- Example: If a patient denies having asthma, but past records show multiple hospitalizations for asthma attacks, validation is needed.
5. Common Errors in Data Collection That Require Validation
| Error Type | Example | Solution |
|---|---|---|
| Incorrect Recording | BP recorded as 180/60 mmHg instead of 120/80 mmHg. | Recheck BP and document accurately. |
| Conflicting Data | Patient reports no pain, but grimaces and holds their abdomen. | Use pain assessment scales for validation. |
| Incomplete Information | Patient doesn’t recall medications they take. | Check medical records and family reports. |
| Unrealistic Findings | Oxygen saturation at 50%, but the patient is talking normally. | Reassess with a different pulse oximeter. |
6. Consequences of Not Validating Data
❌ Inaccurate Nursing Diagnosis – Misinterpretation can lead to incorrect care plans.
❌ Delayed or Wrong Treatment – Can cause serious complications.
❌ Patient Safety Risks – Medication errors, misdiagnosed conditions.
❌ Legal and Ethical Issues – Poor documentation can result in malpractice claims.
✅ Example of Consequence:
A nurse documents a blood glucose level of 30 mg/dL but does not validate it. The patient later becomes unconscious due to undetected hypoglycemia. This could have been prevented with proper validation.
7. Best Practices for Data Validation in Nursing
✔ Always double-check abnormal findings.
✔ Use multiple assessment tools for accuracy.
✔ Compare subjective and objective data.
✔ Consult colleagues or senior healthcare professionals when in doubt.
✔ Ensure clear, accurate documentation.
Documenting Data in Nursing Assessment
1. Introduction to Nursing Documentation
Documentation is a vital part of the nursing process, ensuring that patient data is accurately recorded, communicated, and stored for future reference. Proper documentation improves patient safety, legal protection, continuity of care, and quality improvement.
Definition of Nursing Documentation
“Nursing documentation is the process of systematically recording patient health information, nursing assessments, interventions, and outcomes in a clear, accurate, and timely manner.”
2. Importance of Documenting Data in Nursing
🔹 Ensures continuity of care: Helps in tracking patient progress across shifts and handovers.
🔹 Improves communication: Facilitates coordination among healthcare professionals.
🔹 Provides legal evidence: Serves as proof of care in case of legal disputes.
🔹 Supports clinical decision-making: Aids in diagnosis, treatment, and nursing interventions.
🔹 Enhances research and quality improvement: Helps in audits and policy formulation.
✅ Example: A nurse records a patient’s blood pressure trend, helping the physician adjust hypertension treatment.
3. Principles of Effective Nursing Documentation
✔ Accurate: Use correct details, avoid errors.
✔ Complete: Include all relevant information.
✔ Timely: Document immediately after care.
✔ Legible: Ensure readability (if handwritten).
✔ Objective: Focus on facts, not opinions.
✔ Standardized: Follow hospital protocols (e.g., SOAP, PIE).
✔ Confidential: Protect patient privacy (HIPAA compliance).
✅ Example:
Instead of: “Patient seems anxious.”
Use: “Patient stated, ‘I feel very nervous,’ HR: 110 bpm, pacing in the room.”
4. Types of Documentation in Nursing
1. Narrative Charting
- Description: A detailed, story-like account of patient care.
- Pros: Allows for comprehensive documentation.
- Cons: Time-consuming, lacks structure.
- Example:
“Patient reports severe chest pain at 2:00 AM. Administered nitroglycerin as per physician’s order. Pain reduced to 3/10 after 10 minutes. Vital signs stable.”
2. SOAP Note Format (Problem-Oriented Documentation)
- Definition: Structured documentation using SOAP format.
- Components:
- S (Subjective): Patient’s statements.
- O (Objective): Measurable data (vital signs, lab results).
- A (Assessment): Nursing diagnosis.
- P (Plan): Interventions and next steps.
- Example:
- S: “I have a sharp pain in my chest.”
- O: BP: 140/90 mmHg, ECG shows ST elevation.
- A: Possible myocardial infarction.
- P: Administer oxygen, prepare for ECG and blood tests.
✅ Best for: Standardized and problem-oriented documentation.
3. PIE Note Format (Problem-Intervention-Evaluation)
- Definition: Focuses on nursing interventions and outcomes.
- Components:
- P (Problem): Identified health issue.
- I (Intervention): Actions taken.
- E (Evaluation): Patient response.
- Example:
- P: Acute pain due to surgical incision.
- I: Administered analgesic and repositioned patient.
- E: Pain score reduced from 8/10 to 3/10 after 30 minutes.
✅ Best for: Tracking patient responses to nursing care.
4. DAR Note Format (Focus Charting)
- Definition: Documents patient care in a problem-focused manner.
- Components:
- D (Data): Patient’s symptoms or condition.
- A (Action): Nursing interventions.
- R (Response): Patient outcomes.
- Example:
- D: Patient experiencing shortness of breath (RR: 28/min, SpO₂: 88%).
- A: Provided oxygen therapy, encouraged deep breathing.
- R: SpO₂ improved to 95%, patient reported relief.
✅ Best for: Problem-based charting with quick reference.
5. Charting by Exception (CBE)
- Definition: Only abnormal findings are documented, assuming all other findings are normal.
- Pros: Saves time, reduces redundancy.
- Cons: Can lead to missing important details.
- Example:
- “No changes in neurovascular assessment except for decreased sensation in the left foot.”
✅ Best for: Routine documentation in stable patients.
6. Electronic Health Records (EHRs)
- Definition: Digital storage of patient records.
- Advantages:
- Faster documentation and retrieval.
- Reduces errors from handwriting.
- Allows real-time collaboration.
- Example: A nurse enters vital signs, lab results, and medication history into the hospital’s electronic system.
✅ Best for: Modern hospitals with integrated healthcare systems.
5. Key Components of Nursing Documentation
| Category | What to Include |
|---|---|
| Patient Information | Name, age, gender, medical record number. |
| Vital Signs | Temperature, pulse, respiration, BP, SpO₂. |
| Assessment Findings | Physical, emotional, cognitive status. |
| Nursing Diagnosis | Identified health problems. |
| Interventions | Medications, wound care, therapies provided. |
| Patient Response | Pain reduction, wound healing, symptom relief. |
| Education Provided | Health teaching, discharge instructions. |
| Communication with Team | Physician updates, handovers. |
✅ Example:
“BP 150/90 mmHg, HR 110 bpm. Patient reports headache and dizziness. Administered antihypertensive medication as per order. BP reduced to 130/80 mmHg after 30 minutes.”
6. Legal and Ethical Aspects of Documentation
🔹 Confidentiality (HIPAA Compliance):
- Protect patient privacy, use secure systems.
- Avoid discussing patient information in public areas.
🔹 Accuracy and Truthfulness:
- Never falsify records (e.g., recording vital signs you didn’t measure).
- Use approved abbreviations to prevent misinterpretation.
🔹 Timeliness:
- Document immediately after providing care.
- Late entries must be marked with date and time.
✅ Example:
Instead of: “Patient was given medication at some point in the morning.”
Use: “09:30 AM – Administered 500 mg acetaminophen PO as per order.”
7. Common Documentation Errors and How to Avoid Them
| Error Type | Example | Solution |
|---|---|---|
| Omissions | Forgetting to document medication administration. | Chart immediately after action. |
| Inaccurate Data | Recording “normal heart sounds” without auscultating. | Verify all data before recording. |
| Vague Language | Writing “patient is better” instead of “pain reduced from 7/10 to 3/10.” | Use precise, measurable terms. |
| Illegible Writing | Poor handwriting leads to misinterpretation. | Use electronic documentation or clear handwriting. |
Nursing Diagnosis
1. Introduction to Nursing Diagnosis
Nursing diagnosis is a critical step in the nursing process (ADPIE) that helps identify patient problems and guide nursing interventions. It involves analyzing assessment data to determine the patient’s actual or potential health issues.
Definition of Nursing Diagnosis (NANDA-I, 2021):
“A nursing diagnosis is a clinical judgment about the patient’s response to actual or potential health problems or life processes, providing the basis for selecting nursing interventions to achieve desired outcomes.”
🔹 Why is Nursing Diagnosis Important?
- Guides nursing interventions and care plans.
- Prioritizes patient needs (e.g., life-threatening conditions first).
- Promotes individualized, patient-centered care.
- Enhances communication among healthcare professionals.
- Ensures accurate documentation and legal protection.
✅ Example: Instead of just noting “high blood sugar”, a nurse identifies “Risk for unstable blood glucose levels related to poor dietary habits and medication non-compliance.”
2. Types of Nursing Diagnoses (NANDA-I Classification)
According to the North American Nursing Diagnosis Association-International (NANDA-I), nursing diagnoses are classified into four major types:
1. Actual Nursing Diagnosis
- Definition: Describes current health problems that require immediate intervention.
- Components:
- Problem (P): Patient’s condition.
- Etiology (E): Cause or contributing factor.
- Signs/Symptoms (S): Evidence supporting the diagnosis.
- Example: “Impaired skin integrity related to prolonged immobility as evidenced by pressure ulcers on the sacral region.”
✅ Best for: Immediate nursing interventions (e.g., wound care, pain management).
2. Risk Nursing Diagnosis
- Definition: Identifies conditions that may develop if nursing interventions are not implemented.
- Components:
- Problem: Potential issue.
- Risk Factors: Conditions increasing vulnerability.
- Example: “Risk for infection related to surgical incision and indwelling urinary catheter.”
✅ Best for: Preventive nursing care (e.g., hygiene, wound monitoring)
3. Health Promotion Nursing Diagnosis
- Definition: Focuses on a patient’s readiness to improve health behaviors.
- Components:
- Problem: Positive health condition.
- Supporting Evidence: Statements by the patient or observations by the nurse.
- Example: “Readiness for enhanced nutrition as evidenced by interest in learning about balanced diet options.”
✅ Best for: Health education and lifestyle modifications.
4. Syndrome Nursing Diagnosis
- Definition: A cluster of related nursing diagnoses that occur together due to a common cause.
- Examples:
- Post-trauma syndrome: Anxiety, sleep disturbances, social isolation after a traumatic event.
- Disuse syndrome: Impaired mobility, risk of skin breakdown, muscle weakness in a bedridden patient.
✅ Best for: Complex health conditions requiring multidisciplinary care.
3. Components of a Nursing Diagnosis (PES Format)
A complete nursing diagnosis statement follows the PES format:
| Component | Description | Example |
|---|---|---|
| P (Problem) | The patient’s health issue. | “Impaired mobility” |
| E (Etiology) | The cause of the problem. | “Related to stroke” |
| S (Signs/Symptoms) | Evidence supporting the diagnosis. | “As evidenced by muscle weakness in the right leg and inability to walk independently.” |
✅ Final Diagnosis: “Impaired mobility related to stroke as evidenced by muscle weakness in the right leg and inability to walk independently.”
4. Steps in Formulating a Nursing Diagnosis
Step 1: Collect and Analyze Assessment Data
- Gather subjective data (e.g., “I feel weak and tired”).
- Gather objective data (e.g., BP: 90/60 mmHg, pale skin).
- Identify abnormal findings and patterns.
✅ Example: A nurse observes that a postoperative patient has fever, redness, and swelling around a surgical wound → This suggests a potential infection.
Step 2: Identify the Problem and Classify the Diagnosis
- Is the problem actual, risk, health promotion, or syndrome?
- Use NANDA-I-approved terms to state the diagnosis.
✅ Example: The postoperative patient is at high risk for infection → The nurse writes “Risk for infection related to surgical incision.”
Step 3: Write the Diagnosis in PES Format
- Problem: Risk for infection.
- Etiology: Related to surgical incision and compromised immunity.
- Symptoms (if applicable): Fever, redness, swelling.
✅ Final Diagnosis: “Risk for infection related to surgical incision and compromised immunity.”
Step 4: Validate and Prioritize Nursing Diagnoses
- Confirm accuracy by reviewing patient history and lab results.
- Prioritize diagnoses based on urgency:
- High priority: Life-threatening (e.g., impaired airway).
- Medium priority: Needs prompt intervention (e.g., risk for falls).
- Low priority: Long-term health goals (e.g., knowledge deficit).
✅ Example: “Ineffective airway clearance due to excessive mucus production” takes priority over “Disturbed sleep pattern.”
5. Examples of Common Nursing Diagnoses
| Category | Example Diagnosis (PES Format) |
|---|---|
| Respiratory | “Ineffective airway clearance related to excessive mucus as evidenced by wheezing and productive cough.” |
| Cardiac | “Decreased cardiac output related to myocardial infarction as evidenced by weak pulse and low BP.” |
| Neurological | “Risk for falls related to dizziness and impaired balance.” |
| Pain Management | “Acute pain related to surgical incision as evidenced by facial grimacing and patient’s pain rating of 8/10.” |
| Nutrition | “Imbalanced nutrition: less than body requirements related to decreased appetite as evidenced by weight loss and low serum albumin levels.” |
| Mental Health | “Disturbed sleep pattern related to anxiety as evidenced by difficulty falling asleep and reports of restlessness.” |
6. Difference Between Nursing Diagnosis and Medical Diagnosis
| Feature | Nursing Diagnosis | Medical Diagnosis |
|---|---|---|
| Focus | Patient’s response to illness | Disease condition |
| Who Makes It? | Nurse | Doctor |
| Example | “Impaired gas exchange related to pneumonia” | “Pneumonia” |
| Scope of Treatment | Nursing interventions (oxygen therapy, positioning) | Medical interventions (antibiotics, bronchodilators) |
✅ Key Point: Nurses do not diagnose diseases; they diagnose how a disease affects the patient and how to care for them.
7. Common Mistakes in Nursing Diagnosis
🚫 Using a medical diagnosis instead of a nursing diagnosis.
❌ Wrong: “Diabetes Mellitus”
✅ Right: “Risk for unstable blood glucose levels related to insulin resistance.”
🚫 Writing vague or general statements.
❌ Wrong: “Patient is in pain.”
✅ Right: “Acute pain related to surgical incision as evidenced by patient’s grimacing and pain score of 7/10.”
🚫 Failing to individualize the diagnosis.
❌ Wrong: “Risk for infection.”
✅ Right: “Risk for infection related to presence of indwelling catheter and poor hygiene.”
Identification of Client Problems

1. Introduction
The identification of client problems is a critical step in the nursing process (ADPIE). It involves analyzing assessment data to determine actual and potential health issues that require nursing intervention. This step is essential for formulating accurate nursing diagnoses and creating effective care plans.
Definition of Client Problem Identification
“Client problem identification is the process of recognizing physical, psychological, social, and environmental factors affecting a patient’s health and well-being, leading to the development of a nursing diagnosis.”
2. Importance of Identifying Client Problems
🔹 Ensures early detection of health risks and complications.
🔹 Helps prioritize patient needs for immediate and long-term care.
🔹 Guides the selection of appropriate nursing interventions.
🔹 Enhances patient safety, comfort, and quality of life.
🔹 Supports effective communication between nurses, doctors, and healthcare teams.
✅ Example: A patient reports severe pain after surgery. The nurse identifies acute pain as a client problem, leading to interventions like pain medication, repositioning, and relaxation techniques.
3. Steps in Identifying Client Problems
The identification of client problems follows a systematic approach, starting from data collection to problem validation.
Step 1: Collect and Analyze Assessment Data
- Gather subjective data (e.g., “I feel very weak and dizzy”).
- Gather objective data (e.g., BP: 90/60 mmHg, pale skin).
- Identify abnormal findings, inconsistencies, and patterns.
✅ Example: If a patient reports frequent urination and lab results show elevated blood glucose levels, the nurse identifies a problem related to diabetes.
Step 2: Compare Data with Normal Standards
- Check vital signs, lab results, and physical examination findings.
- Identify deviations from normal ranges.
✅ Example: If a patient’s oxygen saturation is 85% (normal is 95%-100%), the nurse identifies a problem with respiratory function.
Step 3: Identify Actual and Potential Problems
| Type of Problem | Description | Example |
|---|---|---|
| Actual Problem | A present health issue requiring immediate attention. | “Impaired skin integrity due to pressure ulcers.” |
| Potential Problem (Risk) | A condition that may develop if no intervention is taken. | “Risk for infection due to surgical wound.” |
| Health Promotion Need | A need related to improving the patient’s health status. | “Readiness for enhanced nutrition to improve dietary habits.” |
Step 4: Validate Problems with Additional Data
- Compare subjective and objective data to confirm findings.
- Consult secondary sources (medical records, family, doctors) if necessary.
- Use diagnostic tests (lab results, imaging, vital signs) for further verification.
✅ Example: A patient denies feeling anxious, but heart rate is 110 bpm, and they are restless. The nurse validates anxiety as a client problem.
Step 5: Prioritize Identified Problems
- Use Maslow’s Hierarchy of Needs to prioritize problems.
- Address life-threatening issues first, followed by less urgent concerns.
| Priority Level | Example |
|---|---|
| High Priority (Life-threatening) | “Ineffective airway clearance due to respiratory distress.” |
| Medium Priority (Urgent but not life-threatening) | “Acute pain after surgery.” |
| Low Priority (Long-term health goals) | “Knowledge deficit about diabetes management.” |
✅ Example: A patient with difficulty breathing takes priority over a patient with mild discomfort.
4. Common Client Problems in Nursing
Client problems can be classified into physical, psychological, social, and environmental categories.
A. Physical Health Problems
| Category | Example |
|---|---|
| Respiratory | “Ineffective breathing pattern due to pneumonia.” |
| Cardiovascular | “Decreased cardiac output related to heart failure.” |
| Neurological | “Risk for falls due to dizziness and impaired balance.” |
| Musculoskeletal | “Impaired mobility due to arthritis.” |
| Pain Management | “Acute pain related to post-surgical incision.” |
| Integumentary (Skin) | “Risk for infection due to open wound.” |
B. Psychological and Emotional Problems
| Category | Example |
|---|---|
| Anxiety and Stress | “Anxiety related to upcoming surgery.” |
| Depression | “Hopelessness related to chronic illness.” |
| Cognitive Impairment | “Confusion related to Alzheimer’s disease.” |
| Sleep Disturbances | “Disturbed sleep pattern due to hospital environment.” |
C. Social and Environmental Problems
| Category | Example |
|---|---|
| Family and Relationship Issues | “Ineffective family coping related to patient’s chronic illness.” |
| Economic Barriers | “Ineffective health maintenance due to financial constraints.” |
| Cultural or Religious Factors | “Noncompliance with medication due to cultural beliefs.” |
| Environmental Risks | “Risk for falls due to cluttered home environment.” |
✅ Example: A homeless patient with poor hygiene and malnutrition has social and environmental problems that affect their overall health.
5. Tools for Identifying Client Problems
To systematically identify client problems, nurses use various tools and assessment methods:
| Tool | Purpose |
|---|---|
| NANDA-I Nursing Diagnosis | Provides standardized nursing diagnoses for common client problems. |
| Gordon’s Functional Health Patterns | Identifies issues in nutrition, sleep, mobility, and self-care. |
| Maslow’s Hierarchy of Needs | Helps prioritize basic physiological needs before psychosocial issues. |
| Braden Scale | Assesses risk for pressure ulcers. |
| Glasgow Coma Scale (GCS) | Evaluates level of consciousness. |
| Pain Scale (0-10) | Measures pain intensity to determine pain management needs. |
✅ Example: A patient with a Braden Scale score of 10 is at high risk for pressure ulcers, requiring urgent intervention.
6. Common Mistakes in Identifying Client Problems
🚫 Relying only on subjective data without validation.
❌ “Patient says they have no pain,” but their BP and facial expressions suggest otherwise.
✅ Validate with objective findings.
🚫 Using medical diagnoses instead of nursing problems.
❌ “Diabetes mellitus” is a medical diagnosis, not a nursing problem.
✅ Use: “Risk for unstable blood glucose levels related to poor dietary adherence.”
🚫 Failing to prioritize urgent problems.
❌ Focusing on sleep disturbances while ignoring a patient’s respiratory distress.
✅ Address life-threatening issues first.
Identification of Client Risks

1. Introduction
Risk identification in nursing involves recognizing potential health problems that may develop if no preventive measures are taken. By identifying risks early, nurses can implement interventions to minimize complications and enhance patient safety.
Definition of Client Risk Identification
“Client risk identification is the process of assessing a patient’s physical, psychological, social, and environmental factors to determine potential health hazards and prevent complications.”
2. Importance of Identifying Client Risks
🔹 Prevents adverse health outcomes before they occur.
🔹 Improves patient safety and reduces hospital complications.
🔹 Helps in prioritizing nursing interventions.
🔹 Enhances early detection and prevention strategies.
🔹 Supports evidence-based nursing practice.
✅ Example: A patient with immobility is at risk for pressure ulcers. Early identification leads to preventive repositioning and skin care interventions.
3. Steps in Identifying Client Risks
The identification of client risks follows a systematic approach similar to the assessment phase of the nursing process.
Step 1: Collect and Analyze Patient Data
- Gather subjective data (e.g., “I feel weak and tired often”).
- Gather objective data (e.g., BP: 90/60 mmHg, low hemoglobin).
- Identify risk factors in patient history, lifestyle, or environment.
✅ Example: A patient with a history of smoking and high cholesterol is at risk for cardiovascular disease.
Step 2: Identify Specific Risk Factors
Risk factors can be classified into modifiable (can be changed) and non-modifiable (cannot be changed) categories.
| Category | Examples |
|---|---|
| Modifiable Risk Factors | Smoking, poor diet, lack of exercise, high stress levels, medication non-adherence. |
| Non-Modifiable Risk Factors | Age, genetics, family history, gender, pre-existing conditions (e.g., diabetes, hypertension). |
✅ Example: A 65-year-old diabetic is at high risk for foot ulcers, requiring early foot care education and monitoring.
Step 3: Compare Data with Standard Risk Assessment Tools
Nurses use standardized scales and risk assessment tools to determine the level of risk for different health problems.
| Risk Factor | Assessment Tool | Purpose |
|---|---|---|
| Pressure Ulcers | Braden Scale | Assesses skin integrity risks. |
| Falls | Morse Fall Scale | Determines fall risk. |
| Deep Vein Thrombosis (DVT) | Wells Score | Evaluates risk for blood clots. |
| Malnutrition | Mini Nutritional Assessment | Detects risk for undernutrition. |
| Mental Health Risks | Geriatric Depression Scale | Screens for depression in elderly patients. |
✅ Example: A Braden Scale score of 12 indicates high risk for pressure ulcers, leading to early repositioning and skin monitoring interventions.
Step 4: Validate Risks with Clinical Findings
- Compare subjective complaints with objective assessments.
- Seek secondary sources (family reports, medical records) if needed.
- Use diagnostic tests (lab results, imaging, vital signs) to confirm.
✅ Example: A pregnant woman with high BP needs further evaluation for preeclampsia risk.
Step 5: Prioritize Identified Risks
Not all risks require immediate intervention. Use Maslow’s Hierarchy of Needs and nursing judgment to prioritize.
| Priority Level | Example Risk |
|---|---|
| High Priority (Life-threatening risks) | “Risk for ineffective airway clearance due to severe asthma attack.” |
| Medium Priority (Potential complications requiring close monitoring) | “Risk for infection due to post-surgical wound.” |
| Low Priority (Long-term risks, lifestyle factors) | “Risk for social isolation related to hearing impairment.” |
✅ Example: A patient at risk for aspiration due to swallowing difficulties needs immediate intervention (positioning, dietary changes).
4. Common Client Risks in Nursing
Client risks can be categorized based on physical, psychological, social, and environmental factors.
A. Physical Health Risks
| Category | Example Risk |
|---|---|
| Respiratory Risks | “Risk for aspiration due to difficulty swallowing.” |
| Cardiovascular Risks | “Risk for decreased cardiac output related to heart failure history.” |
| Neurological Risks | “Risk for falls related to post-stroke weakness.” |
| Musculoskeletal Risks | “Risk for impaired mobility due to arthritis.” |
| Integumentary Risks (Skin) | “Risk for pressure ulcer development in bedridden patients.” |
✅ Example: A bedridden patient with diabetes is at high risk for bedsores and infection, requiring preventive wound care.
B. Psychological and Mental Health Risks
| Category | Example Risk |
|---|---|
| Anxiety and Depression Risks | “Risk for hopelessness related to chronic illness.” |
| Cognitive Impairment Risks | “Risk for injury related to confusion and disorientation.” |
| Suicide Risks | “Risk for self-harm due to major depressive disorder.” |
✅ Example: A patient with severe depression and social withdrawal is at high risk for suicide, requiring mental health intervention.
C. Social and Environmental Risks
| Category | Example Risk |
|---|---|
| Family and Relationship Risks | “Risk for caregiver role strain related to elderly patient care.” |
| Economic Risks | “Risk for non-compliance with treatment due to financial constraints.” |
| Cultural or Religious Risks | “Risk for health-seeking delay due to cultural beliefs about illness.” |
| Environmental Hazards | “Risk for injury due to cluttered home and poor lighting.” |
✅ Example: An elderly patient living alone has a high risk for falls, requiring home safety modifications.
5. Tools for Identifying Client Risks
Nurses use evidence-based tools to systematically assess risks.
| Assessment Tool | Purpose |
|---|---|
| Braden Scale | Assesses risk for pressure ulcers. |
| Morse Fall Scale | Identifies risk of falls. |
| Glasgow Coma Scale (GCS) | Evaluates consciousness level. |
| Mini Mental Status Exam (MMSE) | Assesses cognitive impairment. |
| Apgar Score (Neonates) | Determines newborn health risks. |
✅ Example: A Morse Fall Scale score of 55 indicates high risk for falls, requiring fall prevention measures.
6. Common Mistakes in Identifying Client Risks
🚫 Ignoring risk factors because no symptoms are present.
❌ A patient with diabetes may have normal skin now, but they are still at risk for foot ulcers.
✅ Provide preventive foot care education.
🚫 Failing to prioritize life-threatening risks first.
❌ Addressing a mild rash before recognizing a patient’s oxygen saturation dropping to 85%.
✅ Airway, breathing, and circulation (ABCs) come first.
🚫 Not validating risks with objective data.
❌ “Risk for infection” written without checking white blood cell count or wound status.
✅ Confirm risk factors through assessment.
Identification of Client Strengths

1. Introduction
Identifying client strengths is an essential aspect of holistic nursing care. While nurses focus on problems and risks, recognizing a patient’s strengths enhances recovery, promotes self-care, and boosts confidence. Strengths help support positive health behaviors and serve as resources for coping with illness or health challenges.
Definition of Client Strength Identification
“Client strength identification is the process of recognizing an individual’s physical, emotional, psychological, social, and environmental abilities that contribute to health maintenance, recovery, and overall well-being.”
2. Importance of Identifying Client Strengths
🔹 Encourages active patient participation in their care.
🔹 Promotes independence and self-efficacy.
🔹 Supports faster recovery and rehabilitation.
🔹 Enhances mental resilience and coping strategies.
🔹 Builds positive relationships between patients and healthcare providers.
🔹 Helps in developing personalized care plans that leverage client abilities.
✅ Example: A post-surgical patient who is motivated to walk has a strength that can be encouraged through early ambulation and physiotherapy.
3. Steps in Identifying Client Strengths
Identifying strengths follows a structured approach, similar to identifying client problems and risks.
Step 1: Collect and Analyze Client Data
- Gather subjective data (e.g., “I am determined to manage my diabetes without complications”).
- Gather objective data (e.g., observing active participation in physical therapy).
- Identify past experiences, coping mechanisms, and resilience factors.
✅ Example: A stroke patient with strong family support and previous experience in managing health conditions may recover faster with home-based rehabilitation.
Step 2: Categorize Strengths Based on Different Domains
Client strengths can be physical, psychological, social, or spiritual.
| Category | Examples of Client Strengths |
|---|---|
| Physical Strengths | Strong immune system, ability to perform self-care, good mobility, adherence to prescribed exercises. |
| Psychological Strengths | Positive mindset, strong coping skills, ability to manage stress effectively. |
| Social Strengths | Supportive family, active participation in community, good communication skills. |
| Spiritual Strengths | Strong religious or spiritual beliefs, sense of purpose, use of meditation or prayer for healing. |
✅ Example: A patient with a history of regular exercise and good nutrition may have better wound healing and faster post-operative recovery.
Step 3: Use Standardized Tools to Identify Strengths
Several assessment tools and models can help identify client strengths:
| Tool/Model | Purpose |
|---|---|
| Gordon’s Functional Health Patterns | Identifies strengths in self-care, nutrition, coping, and health perception. |
| Resilience Scale | Measures ability to cope with stress and challenges. |
| Patient Health Questionnaire (PHQ-9) | Identifies psychological well-being and strengths in emotional regulation. |
| Mini-Mental State Examination (MMSE) | Assesses cognitive strengths in elderly patients. |
| Spiritual Well-Being Scale | Evaluates faith-based coping mechanisms. |
✅ Example: A high score on the Resilience Scale indicates that the patient has strong coping mechanisms to handle chronic illness.
Step 4: Validate Strengths Through Observations
- Compare subjective and objective data to confirm strengths.
- Observe behavioral patterns (e.g., adherence to therapy, motivation to improve health).
- Consult family or caregivers to assess personal and social strengths.
✅ Example: A patient managing their diabetes well without frequent hospital visits has strengths in self-care and medication adherence.
Step 5: Incorporate Strengths into the Care Plan
- Use strengths to enhance patient participation.
- Develop goals that leverage strengths (e.g., setting rehabilitation goals for a motivated stroke survivor).
- Encourage patients to use their strengths to overcome weaknesses.
✅ Example: A patient with a supportive family recovering from surgery can be trained in home-based wound care to reduce hospital visits.
4. Examples of Common Client Strengths in Nursing
A. Physical Strengths
| Category | Example Strength |
|---|---|
| Good Physical Health | “Strong immune response, fast wound healing.” |
| Active Lifestyle | “Engages in regular physical exercise.” |
| Self-Care Ability | “Can perform ADLs (Activities of Daily Living) independently.” |
| Adherence to Treatment | “Takes medications as prescribed without reminders.” |
✅ Example: A patient who maintains a healthy diet and regular exercise has strength in preventing chronic diseases.
B. Psychological Strengths
| Category | Example Strength |
|---|---|
| Resilience and Adaptability | “Patient remains optimistic despite chronic illness.” |
| Effective Stress Management | “Uses relaxation techniques like deep breathing and meditation.” |
| Motivation for Recovery | “Actively participates in physical therapy sessions.” |
| Self-Efficacy | “Patient confidently manages blood sugar levels and makes lifestyle adjustments.” |
✅ Example: A patient who views illness as a challenge rather than a burden has strong resilience, which aids in faster recovery.
C. Social Strengths
| Category | Example Strength |
|---|---|
| Supportive Family and Friends | “Family members provide emotional and physical support.” |
| Active Social Engagement | “Involved in community health programs.” |
| Strong Communication Skills | “Expresses health concerns clearly and effectively.” |
| Financial Stability | “Can afford proper healthcare and medications.” |
✅ Example: A patient with strong family support is less likely to experience depression after a major surgery.
D. Spiritual Strengths
| Category | Example Strength |
|---|---|
| Religious or Spiritual Beliefs | “Patient finds comfort in prayer and meditation.” |
| Positive Life Perspective | “Believes in finding meaning through adversity.” |
| Sense of Purpose | “Engages in volunteer work and community service.” |
| Faith-Based Coping Strategies | “Uses spiritual guidance to deal with chronic pain.” |
✅ Example: A patient using meditation to manage pain demonstrates strong spiritual coping skills.
5. Using Client Strengths in Nursing Interventions
By leveraging client strengths, nurses can create more effective, personalized care plans.
| Client Strength | Nursing Intervention |
|---|---|
| Active participation in therapy | Encourage independence in rehabilitation activities. |
| Supportive family environment | Involve family in patient education and discharge planning. |
| Good stress management skills | Introduce additional relaxation techniques (e.g., guided imagery). |
| High motivation for learning | Provide health education on disease prevention. |
| Ability to perform self-care | Teach advanced self-care techniques for better independence. |
✅ Example: A patient willing to learn about diabetes management should be encouraged to attend education sessions on diet and exercise.
6. Common Mistakes in Identifying Client Strengths
🚫 Focusing only on weaknesses and problems.
❌ Overemphasizing illness without recognizing the patient’s ability to recover.
✅ Balance problem-solving with strength-based care.
🚫 Ignoring self-reported strengths.
❌ Dismissing a patient’s confidence in managing their condition.
✅ Validate strengths through observation and history.
🚫 Underestimating social and emotional strengths.
❌ Neglecting family support in care planning.
✅ Encourage family involvement in patient recovery.
Nursing Diagnosis Statement: Parts
1. Introduction to Nursing Diagnosis Statement
A nursing diagnosis statement is a structured way to define a patient’s health problem based on nursing assessment and clinical judgment. It provides a foundation for selecting appropriate nursing interventions and achieving patient-centered outcomes.
Definition of Nursing Diagnosis Statement (NANDA-I, 2021)
“A nursing diagnosis is a clinical judgment concerning a human response to health conditions/life processes or a vulnerability for that response by an individual, family, or community.”
2. Importance of Nursing Diagnosis Statements
🔹 Helps identify health issues that can be managed by nurses.
🔹 Guides nursing interventions and care planning.
🔹 Enhances communication among healthcare professionals.
🔹 Supports evidence-based nursing practice.
🔹 Promotes patient-centered care by addressing physical, emotional, and social needs.
✅ Example:
Instead of stating “Patient has pneumonia” (which is a medical diagnosis), a nursing diagnosis would be:
“Ineffective airway clearance related to excessive mucus production as evidenced by wheezing, shortness of breath, and weak cough.”
3. Parts of a Nursing Diagnosis Statement
A nursing diagnosis statement typically follows the PES format, which consists of:
| Part | Description | Example |
|---|---|---|
| P (Problem) | The actual or potential health issue that requires nursing care. | “Impaired skin integrity” |
| E (Etiology or Cause) | The underlying cause or contributing factor for the problem. | “Related to prolonged immobility” |
| S (Signs and Symptoms) | The observable evidence that supports the diagnosis. | “As evidenced by pressure ulcers on the sacral area, redness, and broken skin.” |
✅ Final Nursing Diagnosis Statement:
“Impaired skin integrity related to prolonged immobility as evidenced by pressure ulcers on the sacral area.”
4. Types of Nursing Diagnosis Statements (NANDA-I Classification)
According to NANDA International (NANDA-I), nursing diagnosis statements are classified into four types:
1. Actual Nursing Diagnosis
- Definition: Identifies a current health problem that requires immediate intervention.
- Structure: Problem + Related to (cause) + As evidenced by (symptoms).
- Example:
- “Acute pain related to surgical incision as evidenced by patient’s verbal reports of pain (8/10) and grimacing.”
✅ Best for: Immediate nursing care needs like pain management, wound care, and infection control.
2. Risk Nursing Diagnosis
- Definition: Identifies a potential problem that may develop if preventive nursing actions are not taken.
- Structure: Risk for + Problem + Related to (risk factor).
- Example:
- “Risk for falls related to impaired balance and weakness.”
✅ Best for: Preventing pressure ulcers, falls, infections, and complications.
3. Health Promotion Nursing Diagnosis
- Definition: Identifies positive behaviors or readiness for improvement in health.
- Structure: Readiness for enhanced + Health behavior + As evidenced by (patient statement or actions).
- Example:
- “Readiness for enhanced nutrition as evidenced by the patient expressing interest in dietary changes.”
✅ Best for: Encouraging patient education, lifestyle changes, and wellness programs.
4. Syndrome Nursing Diagnosis
- Definition: A cluster of related diagnoses that occur together due to a common cause.
- Example:
- “Post-trauma syndrome related to physical assault, as evidenced by nightmares, hypervigilance, and social withdrawal.”
- “Disuse syndrome related to prolonged bed rest, as evidenced by muscle weakness, joint stiffness, and pressure ulcers.”
✅ Best for: Complex patient conditions requiring multidisciplinary care.
5. Common Nursing Diagnoses with PES Format
| Category | Example Nursing Diagnosis Statement |
|---|---|
| Respiratory | “Ineffective airway clearance related to excessive mucus production as evidenced by wheezing and weak cough.” |
| Cardiovascular | “Decreased cardiac output related to myocardial infarction as evidenced by weak pulse and low BP.” |
| Pain Management | “Acute pain related to surgical incision as evidenced by pain score of 8/10 and guarding behavior.” |
| Integumentary (Skin) | “Risk for impaired skin integrity related to immobility and moisture exposure.” |
| Mental Health | “Disturbed sleep pattern related to stress as evidenced by patient reports of difficulty falling asleep.” |
✅ Tip: Use NANDA-approved terminology for consistency in documentation.
6. How to Write a Nursing Diagnosis Statement Correctly
✅ Dos:
✔ Use clear and specific language (avoid vague statements).
✔ Ensure data supports the diagnosis (signs and symptoms must align).
✔ Use standardized NANDA terminology for accuracy.
✔ Make the problem patient-centered (focus on how the condition affects the patient).
✅ Correct Example:
“Imbalanced nutrition: less than body requirements related to inadequate dietary intake as evidenced by weight loss and low serum albumin levels.”
🚫 Don’ts:
❌ Do not include medical diagnoses (e.g., “Diabetes mellitus”).
❌ Avoid judgmental language (e.g., “Patient is careless about their health”).
❌ Do not write interventions as part of the diagnosis (e.g., “Patient needs insulin injections”).
🚫 Incorrect Example:
“Diabetes-related poor diet management causing high blood sugar.”
✅ Revised Example:
“Risk for unstable blood glucose levels related to inconsistent dietary intake.”
7. Difference Between Nursing Diagnosis and Medical Diagnosis
| Aspect | Nursing Diagnosis | Medical Diagnosis |
|---|---|---|
| Focus | Patient’s response to illness | Disease condition |
| Who Makes It? | Nurse | Doctor |
| Example | “Risk for aspiration related to difficulty swallowing” | “Stroke” |
| Scope of Treatment | Nursing interventions (positioning, feeding modifications) | Medical interventions (medications, surgery) |
✅ Key Point: Nurses do not diagnose diseases but focus on how diseases affect the patient’s functioning and response to treatment.
8. Common Mistakes in Writing Nursing Diagnosis Statements
🚫 Using a medical diagnosis instead of a nursing diagnosis.
❌ “Diabetes mellitus”
✅ “Risk for unstable blood glucose levels related to impaired insulin regulation.”
🚫 Writing vague or general statements.
❌ “Patient is in pain.”
✅ “Acute pain related to surgical incision as evidenced by facial grimacing and a pain score of 8/10.”
🚫 Failing to individualize the diagnosis.
❌ “Risk for infection.”
✅ “Risk for infection related to the presence of an indwelling catheter and poor hygiene.”
Types of Nursing Diagnoses
1. Introduction
A nursing diagnosis is a clinical judgment about a patient’s response to actual or potential health problems. It helps guide nursing interventions and patient care. Nursing diagnoses are different from medical diagnoses, as they focus on how the disease affects the patient’s functioning rather than the disease itself.
Definition of Nursing Diagnosis (NANDA-I, 2021)
“A nursing diagnosis is a clinical judgment concerning a human response to health conditions/life processes or a vulnerability for that response by an individual, family, or community.”
2. Importance of Nursing Diagnoses
🔹 Helps in developing individualized care plans.
🔹 Promotes evidence-based nursing interventions.
🔹 Enhances communication among healthcare professionals.
🔹 Supports continuity of care across healthcare settings.
🔹 Aids in preventing complications and improving patient outcomes.
✅ Example:
Instead of writing “Pneumonia” (a medical diagnosis), a nurse writes:
“Ineffective airway clearance related to excessive mucus production as evidenced by wheezing and weak cough.”
3. Types of Nursing Diagnoses (NANDA-I Classification)
NANDA-I (North American Nursing Diagnosis Association-International) has classified nursing diagnoses into four major types:
1. Actual Nursing Diagnosis
- Definition:
- Describes a current health problem that requires immediate nursing intervention.
- Structure (PES Format):
- Problem (P): What is the patient’s issue?
- Etiology (E): What is causing it?
- Signs/Symptoms (S): What are the indicators?
✅ Example:
“Impaired skin integrity related to prolonged immobility as evidenced by pressure ulcers on the sacral area, redness, and broken skin.”
✔ Best for: Addressing current patient problems like pain management, wound care, and infection control.
2. Risk Nursing Diagnosis
- Definition:
- Identifies a potential health problem that may occur if preventive measures are not taken.
- Structure:
- Risk for + Problem + Related to (Risk factor)
✅ Example:
“Risk for infection related to surgical incision and compromised immunity.”
✔ Best for: Preventing falls, pressure ulcers, infections, and complications.
3. Health Promotion Nursing Diagnosis
- Definition:
- Identifies a patient’s motivation and readiness to improve health and well-being.
- Structure:
- Readiness for enhanced + Health behavior + As evidenced by (Patient statement or actions)
✅ Example:
“Readiness for enhanced nutrition as evidenced by patient expressing interest in balanced diet options.”
✔ Best for: Encouraging self-care, health education, and wellness programs.
4. Syndrome Nursing Diagnosis
- Definition:
- A group of related nursing diagnoses that occur together due to a common cause.
✅ Example:
- “Post-trauma syndrome related to physical assault, as evidenced by nightmares, hypervigilance, and social withdrawal.”
- “Disuse syndrome related to prolonged bed rest, as evidenced by muscle weakness, joint stiffness, and pressure ulcers.”
✔ Best for: Complex conditions requiring multidisciplinary care.
4. Common Nursing Diagnoses with PES Format
| Category | Example Nursing Diagnosis Statement |
|---|---|
| Respiratory | “Ineffective airway clearance related to excessive mucus production as evidenced by wheezing and weak cough.” |
| Cardiovascular | “Decreased cardiac output related to myocardial infarction as evidenced by weak pulse and low BP.” |
| Pain Management | “Acute pain related to surgical incision as evidenced by pain score of 8/10 and guarding behavior.” |
| Integumentary (Skin) | “Risk for impaired skin integrity related to immobility and moisture exposure.” |
| Mental Health | “Disturbed sleep pattern related to stress as evidenced by patient reports of difficulty falling asleep.” |
✔ Tip: Use NANDA-approved terminology for consistency in documentation.
5. How to Write a Nursing Diagnosis Correctly
✅ Dos:
✔ Use clear and specific language (avoid vague statements).
✔ Ensure data supports the diagnosis (signs and symptoms must align).
✔ Use standardized NANDA terminology for accuracy.
✔ Make the problem patient-centered (focus on how the condition affects the patient).
✅ Correct Example:
“Imbalanced nutrition: less than body requirements related to inadequate dietary intake as evidenced by weight loss and low serum albumin levels.”
🚫 Don’ts:
❌ Do not include medical diagnoses (e.g., “Diabetes mellitus”).
❌ Avoid judgmental language (e.g., “Patient is careless about their health”).
❌ Do not write interventions as part of the diagnosis (e.g., “Patient needs insulin injections”).
🚫 Incorrect Example:
“Diabetes-related poor diet management causing high blood sugar.”
✅ Revised Example:
“Risk for unstable blood glucose levels related to inconsistent dietary intake.”
6. Difference Between Nursing Diagnosis and Medical Diagnosis
| Aspect | Nursing Diagnosis | Medical Diagnosis |
|---|---|---|
| Focus | Patient’s response to illness | Disease condition |
| Who Makes It? | Nurse | Doctor |
| Example | “Risk for aspiration related to difficulty swallowing” | “Stroke” |
| Scope of Treatment | Nursing interventions (positioning, feeding modifications) | Medical interventions (medications, surgery) |
✅ Key Point: Nurses do not diagnose diseases but focus on how diseases affect the patient’s functioning and response to treatment.
7. Common Mistakes in Writing Nursing Diagnoses
🚫 Using a medical diagnosis instead of a nursing diagnosis.
❌ “Diabetes mellitus”
✅ “Risk for unstable blood glucose levels related to impaired insulin regulation.”
🚫 Writing vague or general statements.
❌ “Patient is in pain.”
✅ “Acute pain related to surgical incision as evidenced by facial grimacing and a pain score of 8/10.”
🚫 Failing to individualize the diagnosis.
❌ “Risk for infection.”
✅ “Risk for infection related to the presence of an indwelling catheter and poor hygiene.”
Formulating a Nursing Diagnosis:
1. Introduction
Formulating a nursing diagnosis is a crucial step in the nursing process (ADPIE). It involves analyzing patient data, identifying health issues, and writing a structured nursing diagnosis statement that guides patient care.
Definition of Nursing Diagnosis Formulation
“Nursing diagnosis formulation is the process of interpreting patient data, identifying health conditions, and structuring a clear and precise statement that directs nursing interventions.”
2. Importance of Formulating a Nursing Diagnosis
🔹 Helps in developing individualized nursing care plans.
🔹 Guides effective and evidence-based nursing interventions.
🔹 Promotes patient safety and optimal health outcomes.
🔹 Improves communication among healthcare professionals.
🔹 Ensures legal and ethical documentation of patient care.
✅ Example:
Instead of saying “Patient has pneumonia”, a well-formulated nursing diagnosis would be:
“Ineffective airway clearance related to excessive mucus production as evidenced by wheezing and shortness of breath.”
3. Steps in Formulating a Nursing Diagnosis
The process of formulating a nursing diagnosis follows five systematic steps:
Step 1: Data Collection (Assessment Phase)
- Gather subjective data (patient statements, symptoms).
- Gather objective data (vital signs, lab results, physical exam findings).
- Identify abnormal patterns or risk factors.
✅ Example:
- Subjective Data: “I feel very weak and tired all the time.”
- Objective Data: BP 90/60 mmHg, pale skin, low hemoglobin.
- Identified Problem: Possible risk for anemia-related fatigue.
Step 2: Identify the Patient’s Problem
- Analyze collected data to identify actual or potential health issues.
- Compare findings with normal health standards.
- Use clinical judgment to select the most appropriate nursing diagnosis.
✅ Example:
A postoperative patient with a high fever and purulent wound drainage may have the problem of infection risk.
Step 3: Choose the Correct Type of Nursing Diagnosis
According to NANDA-I (North American Nursing Diagnosis Association-International), nursing diagnoses are classified into four types:
| Type of Nursing Diagnosis | Description | Example |
|---|---|---|
| Actual Diagnosis | A current health problem that requires immediate care. | “Impaired skin integrity related to immobility as evidenced by pressure ulcers.” |
| Risk Diagnosis | A potential health problem that may develop. | “Risk for falls related to muscle weakness.” |
| Health Promotion Diagnosis | The patient shows readiness to improve health. | “Readiness for enhanced self-care as evidenced by the patient expressing willingness to learn.” |
| Syndrome Diagnosis | A cluster of related problems occurring together. | “Post-trauma syndrome related to abuse as evidenced by nightmares and anxiety.” |
✅ Key Tip: Use NANDA-I-approved terms for consistency and accuracy.
Step 4: Write the Nursing Diagnosis Statement (PES Format)
The PES format is the standard way of writing a nursing diagnosis:
| Component | Description | Example |
|---|---|---|
| P (Problem) | The patient’s health issue using NANDA terminology. | “Ineffective breathing pattern” |
| E (Etiology/Cause) | The contributing factors causing the problem. | “Related to bronchial constriction” |
| S (Signs/Symptoms) | The evidence supporting the diagnosis. | “As evidenced by wheezing and use of accessory muscles for breathing.” |
✅ Final Nursing Diagnosis Statement:
“Ineffective breathing pattern related to bronchial constriction as evidenced by wheezing and use of accessory muscles for breathing.”
Step 5: Validate and Prioritize the Nursing Diagnosis
- Confirm accuracy of the diagnosis using clinical reasoning.
- Prioritize diagnoses based on urgency and Maslow’s Hierarchy of Needs.
| Priority Level | Example Nursing Diagnosis |
|---|---|
| High Priority (Life-threatening) | “Ineffective airway clearance related to excess mucus as evidenced by low oxygen saturation (85%).” |
| Medium Priority (Acute health issues) | “Acute pain related to post-surgical incision as evidenced by pain rating of 8/10.” |
| Low Priority (Long-term health goals) | “Knowledge deficit related to diabetes management as evidenced by patient asking about insulin use.” |
✅ Example:
A patient with severe respiratory distress needs immediate intervention, so “Ineffective breathing pattern” is prioritized over “Disturbed sleep pattern.”
4. Examples of Well-Formulated Nursing Diagnoses
| Category | Example Nursing Diagnosis Statement |
|---|---|
| Respiratory | “Ineffective airway clearance related to excessive mucus production as evidenced by wheezing and weak cough.” |
| Cardiovascular | “Decreased cardiac output related to myocardial infarction as evidenced by weak pulse and low BP.” |
| Pain Management | “Acute pain related to surgical incision as evidenced by patient grimacing and pain score of 8/10.” |
| Integumentary (Skin) | “Risk for impaired skin integrity related to prolonged immobility and moisture exposure.” |
| Mental Health | “Disturbed sleep pattern related to stress as evidenced by difficulty falling asleep.” |
✅ Tip: Always write clear, concise, and patient-centered diagnoses.
5. Common Mistakes in Formulating Nursing Diagnoses
🚫 Using a medical diagnosis instead of a nursing diagnosis.
❌ “Pneumonia”
✅ “Ineffective airway clearance related to excessive secretions as evidenced by coughing and difficulty breathing.”
🚫 Writing vague or general statements.
❌ “Patient is in pain.”
✅ “Acute pain related to surgical incision as evidenced by a pain score of 8/10.”
🚫 Including interventions in the diagnosis statement.
❌ “Patient needs oxygen therapy to treat breathing problems.”
✅ “Impaired gas exchange related to alveolar damage as evidenced by low oxygen saturation and shortness of breath.”
🚫 Failing to individualize the diagnosis.
❌ “Risk for infection.”
✅ “Risk for infection related to surgical wound and compromised immune response.”
6. Difference Between Nursing Diagnosis and Medical Diagnosis
| Aspect | Nursing Diagnosis | Medical Diagnosis |
|---|---|---|
| Focus | Patient’s response to illness | Disease condition |
| Who Makes It? | Nurse | Doctor |
| Example | “Risk for aspiration related to difficulty swallowing” | “Stroke” |
| Scope of Treatment | Nursing interventions (positioning, feeding modifications) | Medical interventions (medications, surgery) |
✅ Key Point: Nurses do not diagnose diseases but focus on how diseases affect the patient’s functioning and response to treatment.
Guidelines for Formulating a Nursing Diagnosis:
1. Introduction
Formulating a nursing diagnosis is an essential step in the nursing process (ADPIE: Assessment, Diagnosis, Planning, Implementation, and Evaluation). It helps identify actual or potential health issues based on patient data, guiding the selection of appropriate nursing interventions.
Definition of Nursing Diagnosis (NANDA-I, 2021)
“A nursing diagnosis is a clinical judgment concerning a human response to health conditions/life processes or a vulnerability for that response by an individual, family, or community.”
🔹 Why is Proper Formulation Important?
- Ensures clarity and precision in patient care.
- Helps nurses develop individualized and effective care plans.
- Enhances communication among healthcare professionals.
- Promotes evidence-based nursing interventions.
2. Guidelines for Formulating a Nursing Diagnosis
To formulate a nursing diagnosis correctly, nurses should follow specific guidelines to ensure clarity, accuracy, and effectiveness.
1. Base the Diagnosis on Nursing Assessment Data
- Collect subjective data (what the patient reports) and objective data (measurable signs).
- Use patient history, physical examination, lab tests, and observations.
- Look for patterns and trends in patient symptoms.
✅ Example:
- Subjective Data: “I feel short of breath when I walk.”
- Objective Data: SpO₂ 88%, rapid breathing, use of accessory muscles.
- Nursing Diagnosis: “Ineffective breathing pattern related to bronchial constriction as evidenced by dyspnea and SpO₂ 88%.”
2. Use NANDA-I Approved Nursing Diagnoses
- Follow NANDA International (NANDA-I) terminology to ensure standardization and accuracy.
- Use clear, precise language and avoid medical diagnoses.
- Refer to the latest NANDA-I list for standardized nursing terms.
✅ Correct Example: “Impaired physical mobility related to joint stiffness as evidenced by difficulty walking and slow gait.”
🚫 Incorrect Example: “Arthritis” (This is a medical diagnosis, not a nursing diagnosis).
3. Follow the PES Format (Problem, Etiology, Symptoms)
A nursing diagnosis statement should be structured as follows:
| Component | Description | Example |
|---|---|---|
| P (Problem) | The actual or potential health issue. | “Impaired skin integrity” |
| E (Etiology/Cause) | The reason or contributing factor. | “Related to prolonged immobility” |
| S (Signs/Symptoms) | Observable evidence supporting the diagnosis. | “As evidenced by pressure ulcers on the sacral area.” |
✅ Final Nursing Diagnosis:
“Impaired skin integrity related to prolonged immobility as evidenced by pressure ulcers on the sacral area.”
4. Identify the Correct Type of Nursing Diagnosis
A nursing diagnosis can be classified into four categories according to NANDA-I:
| Type | Description | Example |
|---|---|---|
| Actual Diagnosis | A current health problem requiring intervention. | “Acute pain related to surgical incision as evidenced by patient’s pain score of 8/10.” |
| Risk Diagnosis | A potential problem that may develop. | “Risk for infection related to surgical wound.” |
| Health Promotion Diagnosis | The patient’s motivation to improve health. | “Readiness for enhanced nutrition as evidenced by patient requesting diet counseling.” |
| Syndrome Diagnosis | A cluster of related diagnoses occurring together. | “Post-trauma syndrome related to past abuse as evidenced by nightmares and social withdrawal.” |
✅ Example of a Risk Nursing Diagnosis:
“Risk for aspiration related to difficulty swallowing.” (No signs/symptoms because the problem has not yet occurred).
5. Use Clear, Specific, and Measurable Language
- Avoid vague or general terms.
- Use descriptive and measurable words.
- Focus on how the problem affects the patient, not just the condition itself.
✅ Correct Example: “Ineffective airway clearance related to excessive mucus production as evidenced by wheezing and weak cough.”
🚫 Incorrect Example: “Patient has breathing problems.” (Too vague).
6. Avoid Including Medical Diagnoses in Nursing Diagnoses
- A nursing diagnosis focuses on the patient’s response to a disease, not the disease itself.
- Medical diagnoses should be left for doctors to determine.
✅ Correct Example: “Risk for unstable blood glucose levels related to inconsistent dietary intake.”
🚫 Incorrect Example: “Diabetes mellitus.” (Medical diagnosis).
7. Ensure the Diagnosis is Patient-Centered
- The problem statement should focus on the patient, not the nurse.
- Do not blame the patient or include interventions in the diagnosis.
✅ Correct Example: “Impaired physical mobility related to muscle weakness as evidenced by difficulty walking.”
🚫 Incorrect Example: “Patient refuses to walk because they are lazy.” (Judgmental and not patient-centered).
8. Validate the Diagnosis with Additional Data
- Compare subjective and objective findings for consistency.
- Confirm data using medical records, lab results, or family reports.
- If unsure, ask the patient or reassess symptoms.
✅ Example:
- A patient denies having pain, but their facial expression and BP of 160/100 mmHg suggest otherwise. The nurse validates pain presence before formulating a diagnosis.
9. Prioritize Nursing Diagnoses Based on Urgency
Use Maslow’s Hierarchy of Needs to determine which nursing diagnosis to address first:
| Priority Level | Example Nursing Diagnosis |
|---|---|
| High Priority (Life-threatening) | “Ineffective airway clearance related to excessive secretions as evidenced by low oxygen saturation.” |
| Medium Priority (Needs prompt intervention but not life-threatening) | “Acute pain related to post-surgical incision as evidenced by a pain score of 8/10.” |
| Low Priority (Long-term health goals) | “Readiness for enhanced knowledge related to diabetes self-management.” |
✅ Key Tip: Always address breathing, circulation, and safety issues first.
10. Ensure the Diagnosis Leads to Nursing Interventions
- A well-formulated nursing diagnosis should guide appropriate nursing interventions.
- If no nursing actions can be planned, reassess the diagnosis.
✅ Example:
- Nursing Diagnosis: “Impaired skin integrity related to prolonged immobility as evidenced by pressure ulcers.”
- Nursing Interventions: Frequent repositioning, skin barrier creams, and pressure-relieving devices.
3. Common Mistakes in Formulating a Nursing Diagnosis
| Mistake | Example | Corrected Version |
|---|---|---|
| Using a medical diagnosis | “Heart failure.” | “Decreased cardiac output related to heart muscle weakness.” |
| Writing vague statements | “Patient has pain.” | “Acute pain related to surgical incision as evidenced by pain score of 7/10.” |
| Blaming the patient | “Patient does not want to cooperate.” | “Ineffective coping related to anxiety about hospitalization.” |
| Using an intervention instead of a diagnosis | “Patient needs oxygen therapy.” | “Impaired gas exchange related to alveolar damage.” |
NANDA-Approved Nursing Diagnoses:
1. Introduction to NANDA International
NANDA International (NANDA-I) is a professional organization dedicated to standardizing the terminology used in nursing diagnoses. Established in 1982, NANDA-I aims to develop, refine, and promote a standardized language for nursing diagnoses, enhancing the quality of nursing care and facilitating clear communication among healthcare professionals. nanda.org
2. Purpose and Importance of Standardized Nursing Diagnoses
Standardized nursing diagnoses serve several critical functions:
- Enhance Communication: Provide a common language among nurses and other healthcare professionals, ensuring clarity in patient care discussions.
- Guide Care Planning: Assist in the development of individualized care plans by identifying specific patient needs.ar.israa.edu.ps+6ncbi.nlm.nih.gov+6ncbi.nlm.nih.gov+6
- Promote Research and Education: Offer a framework for nursing research, education, and the development of best practices.
- Improve Patient Outcomes: Facilitate targeted interventions, leading to better health outcomes and patient satisfaction.
3. Structure of NANDA-I Taxonomy II
NANDA-I’s Taxonomy II organizes nursing diagnoses into a hierarchical structure comprising 13 domains, 47 classes, and numerous specific diagnoses. This structure ensures a comprehensive approach to various aspects of patient health.en.wikipedia.org+1de.wikipedia.org+1
Domains and Classes
Here is an overview of the 13 domains and their respective classes:
- Health Promotion
- Health Awareness
- Health Management
- Nutrition
- Ingestion
- Digestion
- Absorption
- Metabolism
- Hydration
- Elimination and Exchange
- Urinary Function
- Gastrointestinal Function
- Integumentary Function
- Respiratory Function
- Activity/Rest
- Sleep/Rest
- Activity/Exercise
- Energy Balance
- Cardiovascular/Pulmonary Responses
- Self-Care
- Perception/Cognition
- Attention
- Orientation
- Sensation/Perception
- Cognition
- Communication
- Self-Perception
- Self-Concept
- Self-Esteem
- Body Image
- Role Relationships
- Caregiving Roles
- Family Relationships
- Role Performance
- Sexuality
- Sexual Identity
- Sexual Function
- Reproduction
- Coping/Stress Tolerance
- Post-Trauma Responses
- Coping Responses
- Neuro-Behavioral Stress
- Life Principles
- Values
- Beliefs
- Value/Belief/Action Congruence
- Safety/Protection
- Infection
- Physical Injury
- Violence
- Environmental Hazards
- Defensive Processes
- Thermoregulation
- Comfort
- Physical Comfort
- Environmental Comfort
- Social Comfort
- Growth/Development
- Growth
- Development
Each class within these domains encompasses specific nursing diagnoses that address particular patient issues.
4. Examples of NANDA-I Approved Nursing Diagnoses
Below are examples of nursing diagnoses from selected domains:
- Health Promotion
- Readiness for Enhanced Health Literacy: Indicates a patient’s willingness to improve understanding and management of health information.en.wikipedia.org
- Nutrition
- Imbalanced Nutrition: Less Than Body Requirements: Occurs when nutrient intake is insufficient to meet metabolic needs.
- Elimination and Exchange
- Impaired Urinary Elimination: Dysfunction in urine elimination patterns.ncbi.nlm.nih.gov+1ncbi.nlm.nih.gov+1
- Activity/Rest
- Activity Intolerance: Insufficient physiological or psychological energy to endure or complete required or desired daily activities.
- Perception/Cognition
- Acute Confusion: Abrupt onset of reversible disturbances of consciousness, attention, cognition, and perception.
- Safety/Protection
- Risk for Infection: Increased susceptibility to invasion by pathogenic organisms.
For a comprehensive list of all approved nursing diagnoses, refer to the latest NANDA-I publication. nanda.org
5. Recent Updates and Revisions
NANDA-I periodically updates its list of nursing diagnoses to reflect advancements in nursing knowledge and practice. In the 2018–2020 edition, several new diagnoses were introduced, including:ar.israa.edu.ps
- Risk for Unstable Blood Pressurear.israa.edu.ps
- Risk for Complicated Immigration Transitionar.israa.edu.ps
- Neonatal Abstinence Syndromear.israa.edu.ps
- Risk for Venous Thromboembolism
Additionally, some diagnoses were retired to maintain clinical relevance and accuracy.
6. Application in Clinical Practice
Utilizing NANDA-I approved nursing diagnoses in clinical practice involves:
- Assessment: Collecting comprehensive patient data.
- Diagnosis: Identifying appropriate nursing diagnoses based on assessment data.
- Planning: Developing individualized care plans with specific goals and interventions.
- Implementation: Executing the care plan.
- Evaluation: Assessing patient outcomes and adjusting the care plan as necessary.
This structured approach ensures that nursing care is systematic, evidence-based, and tailored to each patient’s unique needs.
EXAMPLES LIST OF NANDA DIAGNOSIS ACCORDING TO PATIENTS MEDICAL DISEASE CONDITION,
NANDA International (NANDA-I) provides standardized nursing diagnoses that address patients’ responses to medical conditions. Below is a list of common medical conditions paired with corresponding NANDA-I approved nursing diagnoses:
- Diabetes Mellitus
- Risk for Unstable Blood Glucose Level: Susceptible to variations in blood glucose/sugar levels from the normal range, which may compromise health.
- Deficient Knowledge: Absence or deficiency of cognitive information related to diabetes management.
- Hypertension
- Risk for Ineffective Cerebral Tissue Perfusion: Susceptible to a decrease in cerebral tissue circulation, which may compromise health.ncbi.nlm.nih.gov
- Ineffective Health Maintenance: Inability to identify, manage, and seek out help to maintain health.nanda.org+3ncbi.nlm.nih.gov+3ncbi.nlm.nih.gov+3
- Chronic Obstructive Pulmonary Disease (COPD)
- Ineffective Airway Clearance: Inability to clear secretions or obstructions from the respiratory tract to maintain a clear airway.
- Activity Intolerance: Insufficient physiological or psychological energy to endure or complete required or desired daily activities.
- Congestive Heart Failure (CHF)
- Decreased Cardiac Output: Inadequate blood pumped by the heart to meet the metabolic demands of the body.
- Excess Fluid Volume: Surplus retention of fluid in the body.en.wikipedia.org+4nurse.org+4ar.israa.edu.ps+4
- Myocardial Infarction (Heart Attack)
- Acute Pain: Unpleasant sensory and emotional experience arising from actual or potential tissue damage.
- Anxiety: Vague uneasy feeling of discomfort or dread accompanied by an autonomic response.
- Stroke (Cerebrovascular Accident)
- Impaired Physical Mobility: Limitation in independent, purposeful physical movement of the body or of one or more extremities.
- Impaired Verbal Communication: Decreased, delayed, or absent ability to receive, process, transmit, and use a system of symbols.
- Pneumonia
- Impaired Gas Exchange: Excess or deficit in oxygenation and/or carbon dioxide elimination at the alveolar-capillary membrane.
- Ineffective Breathing Pattern: Inspiration and/or expiration that does not provide adequate ventilation.
- Renal Failure
- Risk for Electrolyte Imbalance: Susceptible to changes in serum electrolyte levels, which may compromise health.ncbi.nlm.nih.gov
- Risk for Imbalanced Fluid Volume: Susceptible to a decrease, increase, or rapid shift from one to the other of intravascular, interstitial, and/or intracellular fluid, which may compromise health.ncbi.nlm.nih.gov
- Parkinson’s Disease
- Impaired Physical Mobility: Limitation in independent, purposeful physical movement of the body or of one or more extremities.
- Risk for Falls: Increased susceptibility to falling, which may cause physical harm.intelycare.com
- Alzheimer’s Disease
- Chronic Confusion: Irreversible, long-standing, and/or progressive deterioration of intellect and personality characterized by decreased ability to interpret environmental stimuli.
- Impaired Memory: Inability to remember or recall bits of information or behavioral skills.
These nursing diagnoses enable nurses to develop individualized care plans that address the specific needs and responses of patients to their medical conditions. For a comprehensive and updated list of NANDA-I approved nursing diagnoses, refer to the latest edition of “NANDA International Nursing Diagnoses: Definitions and Classification.”
Difference Between Medical Diagnosis and Nursing Diagnosis
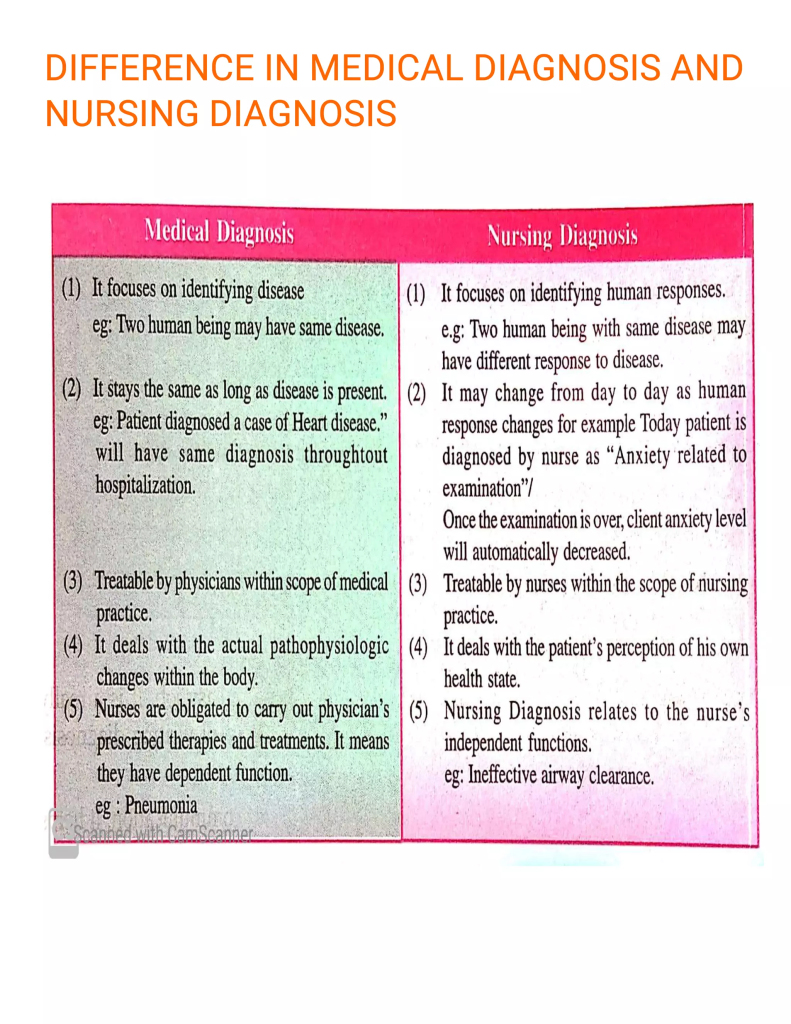
1. Introduction
In healthcare, medical diagnoses and nursing diagnoses are essential for patient care, but they serve different purposes. Medical diagnoses focus on identifying diseases, while nursing diagnoses focus on how the patient responds to health conditions and what care is needed.
Definition of Medical Diagnosis
“A medical diagnosis is the identification of a disease or condition made by a physician or other licensed healthcare provider, based on clinical signs, symptoms, history, laboratory findings, and diagnostic tests.”
Definition of Nursing Diagnosis (NANDA-I, 2021)
“A nursing diagnosis is a clinical judgment concerning a human response to health conditions/life processes or a vulnerability for that response by an individual, family, or community.”
✅ Example:
- Medical Diagnosis: Pneumonia (disease caused by infection in the lungs).
- Nursing Diagnosis: Ineffective airway clearance related to excessive mucus production as evidenced by wheezing and weak cough.
2. Key Differences Between Medical and Nursing Diagnoses
| Aspect | Medical Diagnosis | Nursing Diagnosis |
|---|---|---|
| Focus | Identifies a specific disease or medical condition. | Identifies the patient’s response to a health condition. |
| Who Makes It? | Physicians, Nurse Practitioners, or Specialists. | Registered Nurses (RNs) using the nursing process. |
| Scope of Treatment | Managed with medical interventions (e.g., medications, surgery). | Managed with nursing interventions (e.g., positioning, patient education, wound care). |
| Example | Diabetes mellitus | Risk for unstable blood glucose levels related to inconsistent dietary intake. |
| Standardization | Based on the ICD (International Classification of Diseases). | Based on NANDA-I (North American Nursing Diagnosis Association-International). |
| Duration | Usually remains the same throughout the patient’s condition. | Can change as the patient’s condition improves or worsens. |
✅ Example:
A patient with heart failure:
- Medical Diagnosis: Heart failure (confirmed by echocardiogram and lab tests).
- Nursing Diagnosis: Decreased cardiac output related to weakened heart function as evidenced by shortness of breath and low blood pressure.
3. Examples of Medical vs. Nursing Diagnoses
| Medical Diagnosis | Nursing Diagnosis |
|---|---|
| Stroke | Impaired physical mobility related to muscle weakness as evidenced by inability to walk independently. |
| Pneumonia | Ineffective airway clearance related to thick mucus as evidenced by persistent cough and abnormal lung sounds. |
| Hypertension | Risk for ineffective cerebral tissue perfusion related to high blood pressure. |
| Diabetes Mellitus | Risk for unstable blood glucose levels related to inconsistent dietary intake. |
| Myocardial Infarction (Heart Attack) | Decreased cardiac output related to myocardial damage as evidenced by weak pulse and fatigue. |
| Kidney Failure | Fluid volume excess related to impaired kidney function as evidenced by edema and weight gain. |
| Depression | Risk for self-harm related to feelings of hopelessness and isolation. |
✅ Key Difference:
- Medical diagnoses focus on the disease itself.
- Nursing diagnoses focus on the patient’s experience and response to the disease.
4. How Nursing and Medical Diagnoses Work Together
Both medical and nursing diagnoses are essential for comprehensive patient care.
Example: A Patient with a Stroke
- Medical Diagnosis: Stroke (Cerebrovascular Accident – CVA)
- Nursing Diagnoses:
- Impaired verbal communication related to brain injury as evidenced by difficulty speaking.
- Risk for aspiration related to difficulty swallowing.
- Impaired physical mobility related to weakness on the right side.
- Self-care deficit related to loss of muscle control as evidenced by inability to dress or feed self.
✅ How They Work Together:
- The doctor prescribes medications and therapies for stroke.
- The nurse provides supportive care, helps with mobility exercises, assists in feeding, and educates the patient on recovery.
5. Why Nursing Diagnosis is Important
🔹 Helps create individualized care plans based on the patient’s needs.
🔹 Identifies risks early to prevent complications (e.g., preventing falls in stroke patients).
🔹 Supports evidence-based nursing interventions for better patient outcomes.
🔹 Improves communication among healthcare teams for coordinated care.
🔹 Promotes holistic care by addressing physical, emotional, and psychosocial aspects.
Planning.

1. Introduction to Planning in Nursing
The nursing process is a systematic approach that guides nurses in providing quality patient care. The planning phase follows the assessment and nursing diagnosis stages and focuses on setting goals, priorities, and interventions to address the patient’s health concerns.
Definition of Planning in the Nursing Process
“Planning is the process of establishing patient-centered goals, determining priorities, and selecting appropriate nursing interventions to achieve the desired health outcomes.”
2. Importance of the Planning Phase in Nursing
🔹 Ensures individualized, patient-centered care.
🔹 Helps prioritize interventions based on urgency.
🔹 Promotes collaborative care among healthcare professionals.
🔹 Facilitates effective documentation for continuity of care.
🔹 Improves patient safety and health outcomes.
✅ Example:
A nurse develops a care plan for a post-surgical patient to prevent complications such as infection and pain.
3. Components of Planning in Nursing
The planning phase consists of three essential components:
1. Setting Priorities
- Uses Maslow’s Hierarchy of Needs to prioritize nursing diagnoses.
- Categorizes high, medium, and low-priority issues.
| Priority Level | Example Nursing Diagnosis |
|---|---|
| High Priority (Life-threatening) | “Ineffective airway clearance related to excessive mucus production.” |
| Medium Priority (Potential complications) | “Risk for infection related to surgical wound.” |
| Low Priority (Long-term health goals) | “Readiness for enhanced knowledge about diabetes management.” |
✅ Example: If a patient is having difficulty breathing, that issue takes priority over lack of knowledge about diet.
2. Establishing SMART Goals (Patient Outcomes)
Goals should be SMART (Specific, Measurable, Achievable, Relevant, Time-bound).
| Component | Description | Example |
|---|---|---|
| S (Specific) | Clearly defines what is to be achieved. | “The patient will maintain oxygen saturation above 95%.” |
| M (Measurable) | Can be observed and quantified. | “The patient will report pain at a level of 3/10 or lower.” |
| A (Achievable) | Realistic given the patient’s condition. | “The patient will walk 20 meters without assistance.” |
| R (Relevant) | Addresses the patient’s needs. | “The patient will practice deep breathing exercises.” |
| T (Time-bound) | Specifies a time frame. | “By the end of the shift, the patient will use an incentive spirometer every hour.” |
✅ Example:
“The patient will perform incentive spirometry exercises every hour to prevent pneumonia within 24 hours.”
3. Selecting Nursing Interventions
Nursing interventions are actions nurses take to achieve patient goals. These interventions can be classified into three categories:
| Type of Intervention | Description | Example |
|---|---|---|
| Independent | Actions that nurses perform without a doctor’s order. | “Repositioning a bedridden patient every 2 hours to prevent pressure ulcers.” |
| Dependent | Actions that require a doctor’s order. | “Administering prescribed antibiotics for infection.” |
| Collaborative | Actions performed with other healthcare professionals. | “Working with a physiotherapist to help the patient regain mobility.” |
✅ Example:
A nurse caring for a post-surgical patient selects interventions such as pain management, wound care, and patient education on mobility.
4. Types of Nursing Care Plans
The planning phase results in a nursing care plan, which can be:
| Type | Description | Example |
|---|---|---|
| Formal Care Plan | A structured, written document outlining patient care. | Hospital electronic medical records. |
| Informal Care Plan | A nurse’s mental plan based on patient needs. | Deciding to check a patient’s pain levels frequently. |
| Individualized Care Plan | Tailored to the unique needs of a patient. | A care plan for a stroke patient focusing on speech therapy. |
| Standardized Care Plan | Uses pre-written care plans for common conditions. | A care plan for post-operative recovery. |
✅ Example: A stroke patient’s care plan may include speech therapy, physical therapy, and nutrition interventions.
5. Example of a Nursing Care Plan
| Nursing Diagnosis | Planning (Goal & Interventions) |
|---|---|
| Impaired Skin Integrity related to prolonged immobility as evidenced by stage 2 pressure ulcer on the sacral area. | Goal: “The patient’s sacral wound will show signs of healing within one week.” Interventions: 1) Reposition the patient every 2 hours. 2) Apply prescribed wound care dressings. 3) Encourage a high-protein diet to promote healing. |
✅ Key Tip: The care plan should be continuously updated based on patient progress.
6. Common Mistakes in Nursing Planning
🚫 Setting vague or unrealistic goals
❌ “The patient will feel better soon.”
✅ Corrected Goal: “The patient will verbalize pain relief below a score of 3/10 within 24 hours.”
🚫 Failing to individualize the plan
❌ Using the same interventions for all patients.
✅ Correct Approach: Adjust interventions to match the patient’s specific condition and preferences.
🚫 Not involving the patient in goal setting
❌ Ignoring the patient’s input in their care plan.
✅ Correct Approach: Ask patients about their preferences, abilities, and goals.
Types of Planning.
1. Introduction
Planning is a critical phase in the nursing process, guiding nurses in setting goals, priorities, and interventions to provide effective patient care. There are different types of planning, each serving a specific purpose in nursing practice.
Definition of Planning in Nursing
“Planning is the process of establishing priorities, setting patient-centered goals, and selecting nursing interventions to promote health and improve patient outcomes.”
✅ Example:
A post-surgical patient requires planning for pain management, wound care, and mobility improvement.
2. Types of Planning in Nursing
Planning in nursing can be categorized into four main types:
| Type of Planning | Definition | Example |
|---|---|---|
| Initial Planning | Performed at the beginning of patient care to set the foundation for treatment. | Creating a care plan for a newly admitted patient with pneumonia. |
| Ongoing Planning | Continuous modifications to the care plan based on patient progress. | Adjusting wound care interventions based on healing progress. |
| Discharge Planning | Preparing the patient for safe transition from hospital to home or another facility. | Educating a diabetic patient about insulin self-administration before discharge. |
| Strategic Planning | Long-term planning for hospital-wide nursing policies and improvements. | Developing infection control policies in a hospital setting. |
3. Detailed Explanation of Each Type of Planning
1. Initial Planning
- Occurs upon patient admission to a healthcare facility.
- Focuses on immediate needs and priorities.
- Forms the foundation for future care plans.
- Often based on standardized protocols for common conditions.
✅ Example:
A stroke patient admitted to the hospital will have an initial plan addressing:
- Airway protection (risk for aspiration).
- Mobility assessment (risk for falls).
- Nutrition and hydration monitoring.
2. Ongoing Planning
- Continuous reassessment and updates to the care plan.
- Ensures adaptation to the patient’s changing condition.
- Helps prioritize new problems that arise.
✅ Example:
A post-operative patient initially planned for pain management may later require wound infection prevention if signs of infection appear.
🔹 Key Aspects of Ongoing Planning:
✔ Monitor patient progress and response to interventions.
✔ Modify goals and interventions as needed.
✔ Update care plans to reflect patient condition changes.
3. Discharge Planning
- Begins as soon as the patient is admitted.
- Focuses on helping patients transition safely from hospital to home or another facility.
- Involves patient education, medication management, and follow-up care.
✅ Example:
A patient recovering from heart surgery will require:
- Education on medication adherence.
- Lifestyle modifications (low-sodium diet, exercise).
- Follow-up appointments with a cardiologist.
🔹 Key Components of Discharge Planning:
✔ Teaching self-care techniques (wound care, insulin injection).
✔ Coordinating with family members or caregivers.
✔ Arranging follow-up visits or referrals.
4. Strategic Planning
- Long-term planning at the organizational level.
- Involves developing nursing policies, protocols, and quality improvements.
- Ensures continuous development and efficiency in healthcare services.
✅ Example:
A hospital implements a new policy to reduce medication errors by introducing barcode scanning for drug administration.
🔹 Key Features of Strategic Planning:
✔ Focuses on future healthcare goals and improvements.
✔ Involves leadership, management, and policy-making.
✔ Ensures evidence-based nursing practices are followed.
4. Key Differences Between Types of Planning
| Aspect | Initial Planning | Ongoing Planning | Discharge Planning | Strategic Planning |
|---|---|---|---|---|
| Timing | At patient admission | Throughout hospital stay | Before patient discharge | Long-term hospital goals |
| Focus | Immediate patient needs | Changes in patient condition | Safe transition and self-care | Nursing policies and improvement |
| Example | Planning care for a newly admitted stroke patient | Adjusting care plan based on wound healing progress | Teaching insulin self-injection before discharge | Implementing an electronic medical record system |
5. Importance of Planning in Nursing
🔹 Ensures continuity of care from admission to discharge.
🔹 Improves patient safety by anticipating risks and preventing complications.
🔹 Enhances teamwork and collaboration among healthcare professionals.
🔹 Facilitates effective documentation of patient progress.
🔹 Supports patient education and empowerment for self-care.
✅ Example:
A diabetic patient’s planning includes:
✔ Initial Planning: Assessing blood sugar levels and dietary intake.
✔ Ongoing Planning: Adjusting insulin doses based on blood glucose trends.
✔ Discharge Planning: Teaching self-monitoring techniques and diet management.
6. Common Mistakes in Nursing Planning
🚫 Not individualizing the care plan.
❌ Using the same interventions for all patients.
✅ Correct Approach: Adjust interventions based on patient-specific conditions.
🚫 Failing to update care plans.
❌ Continuing the same interventions despite patient improvement or decline.
✅ Correct Approach: Modify the plan based on ongoing assessments.
🚫 Ignoring patient input.
❌ Setting goals without considering the patient’s preferences and abilities.
✅ Correct Approach: Involve the patient and family in goal-setting.
Establishing Priorities.
1. Introduction
Establishing priorities is a crucial step in the planning phase of the nursing process. It helps nurses decide which patient problems require immediate attention and which can be addressed later. Prioritization ensures efficient use of resources, enhances patient safety, and improves health outcomes.
Definition of Priority Setting in Nursing
“Establishing priorities in nursing involves ranking patient needs in order of urgency to determine the most critical interventions required for optimal patient outcomes.”
✅ Example:
A patient experiencing severe respiratory distress must be treated before a patient with mild anxiety.
2. Importance of Establishing Priorities in Nursing
🔹 Ensures urgent and life-threatening conditions are managed first.
🔹 Helps in allocating resources effectively.
🔹 Reduces complications and enhances patient safety.
🔹 Improves efficiency in nursing care delivery.
🔹 Guides nurses in decision-making during emergencies.
✅ Example:
A post-surgical patient with active bleeding requires immediate intervention before a patient with moderate pain.
3. Principles for Establishing Priorities
To prioritize patient needs, nurses must consider various principles, including Maslow’s Hierarchy of Needs, the ABCDE approach, and urgency levels.
1. Maslow’s Hierarchy of Needs
Maslow’s theory helps prioritize patient problems based on basic human needs.
| Level of Need | Priority | Example Nursing Diagnosis |
|---|---|---|
| Physiological Needs (Basic Needs) | 🔴 Highest Priority | “Ineffective breathing pattern related to airway obstruction.” |
| Safety and Security | 🟠 Moderate Priority | “Risk for falls related to unsteady gait.” |
| Love and Belonging | 🟡 Lower Priority | “Social isolation related to hospitalization.” |
| Self-Esteem | 🟡 Lower Priority | “Chronic low self-esteem related to body image changes.” |
| Self-Actualization | 🟢 Lowest Priority | “Readiness for enhanced coping as evidenced by patient’s interest in mental health counseling.” |
✅ Example:
A patient struggling to breathe (airway obstruction) must be treated before addressing a patient’s low self-esteem due to hair loss from chemotherapy.
2. The ABCDE Approach (Airway, Breathing, Circulation, Disability, Exposure)
The ABCDE method helps prioritize critical conditions that threaten life.
| Category | Priority Level | Example |
|---|---|---|
| A – Airway | 🔴 Highest Priority | “Obstructed airway due to anaphylaxis.” |
| B – Breathing | 🔴 High Priority | “Respiratory distress due to asthma.” |
| C – Circulation | 🟠 Moderate Priority | “Shock due to blood loss from surgery.” |
| D – Disability (Neurological) | 🟡 Lower Priority | “Confusion due to dehydration.” |
| E – Exposure (Temperature, Skin Integrity, etc.) | 🟢 Lowest Priority | “Mild fever due to viral infection.” |
✅ Example:
A patient with severe wheezing (Breathing issue) must be treated before a patient with a mild skin rash (Exposure issue).
3. Urgency-Based Prioritization
This system categorizes nursing priorities into three levels.
| Priority Level | Definition | Example |
|---|---|---|
| High Priority | Life-threatening situations | “Ineffective airway clearance due to choking.” |
| Medium Priority | Problems that could become serious if left untreated | “Risk for infection in a diabetic foot ulcer.” |
| Low Priority | Minor health concerns or long-term goals | “Readiness for enhanced nutrition for weight management.” |
✅ Example:
A patient with chest pain (High priority) requires immediate attention compared to a patient requesting diet counseling (Low priority).
4. Steps in Establishing Priorities in Nursing
The nursing process helps establish priorities systematically.
Step 1: Assess the Patient’s Condition
- Gather subjective data (patient’s complaints).
- Gather objective data (vital signs, lab results, physical findings).
- Identify life-threatening conditions.
✅ Example:
A patient reporting difficulty breathing with SpO₂ of 85% must be assessed immediately.
Step 2: Identify the Nursing Diagnosis
- Use NANDA-approved nursing diagnoses.
- Categorize the diagnosis into high, medium, or low priority.
✅ Example:
- High Priority: Ineffective breathing pattern related to asthma attack.
- Medium Priority: Impaired skin integrity related to pressure ulcer.
- Low Priority: Knowledge deficit related to diabetes self-management.
Step 3: Set Goals Using SMART Criteria
- Goals should be Specific, Measurable, Achievable, Relevant, and Time-bound (SMART).
✅ Example:
“The patient will maintain an oxygen saturation level of 95% or above within 30 minutes after receiving nebulization.”
Step 4: Select Nursing Interventions
- Choose independent, dependent, or collaborative interventions to address priority problems.
✅ Example:
For impaired gas exchange, the nurse will:
✔ Administer oxygen (dependent intervention).
✔ Monitor SpO₂ levels every 30 minutes (independent intervention).
✔ Collaborate with the respiratory therapist for nebulization therapy.
Step 5: Reassess and Adjust Priorities
- Patient conditions change over time, requiring ongoing assessment and prioritization.
✅ Example:
A stable post-operative patient may suddenly develop difficulty breathing, shifting priorities from pain management to airway management.
5. Examples of Prioritization in Different Nursing Scenarios
| Scenario | High Priority | Medium Priority | Low Priority |
|---|---|---|---|
| Post-Surgical Care | Uncontrolled bleeding | Post-op nausea | Dressing change |
| Cardiac Care | Chest pain (possible MI) | Elevated blood pressure | Dietary counseling |
| Respiratory Care | Respiratory distress | Mild cough | Patient education on smoking cessation |
✅ Example:
In a cardiac unit, a patient with chest pain (High priority) must be treated before a patient with mildly elevated blood pressure (Medium priority).
6. Common Mistakes in Establishing Priorities
🚫 Focusing on low-priority issues first
❌ Addressing patient education before stabilizing vital signs.
✅ Correct Approach: Treat critical conditions first.
🚫 Not reassessing priorities
❌ Using the same plan even when the patient’s condition changes.
✅ Correct Approach: Reassess frequently and adjust interventions accordingly.
🚫 Ignoring patient preferences
❌ Setting goals without involving the patient in decision-making.
✅ Correct Approach: Include the patient’s preferences and lifestyle in the plan.
Establishing Goals and Expected Outcomes in the Nursing Process
1. Introduction
In the planning phase of the nursing process, goals and expected outcomes are established based on the patient’s nursing diagnosis. These guide nursing interventions and provide a benchmark to measure patient progress.
Definition of Goals and Expected Outcomes
- Goals: Broad statements that describe what the patient is expected to achieve as a result of nursing interventions.
- Expected Outcomes: Specific, measurable changes that indicate goal achievement.
✅ Example:
Goal: Improve patient’s respiratory function.
Expected Outcome: The patient’s oxygen saturation will remain above 95% within 2 hours of oxygen therapy.
2. Purposes of Establishing Goals and Expected Outcomes
🔹 Provides direction for nursing care.
🔹 Helps in evaluating the effectiveness of interventions.
🔹 Ensures continuity of care among healthcare providers.
🔹 Improves patient engagement and motivation.
🔹 Serves as a basis for documentation and legal records.
✅ Example:
A diabetic patient must learn self-care techniques to manage blood sugar levels. Goals and outcomes ensure measurable improvements in self-management.
3. Types of Goals in Nursing
Goals in nursing are classified into short-term and long-term goals.
| Type | Definition | Example |
|---|---|---|
| Short-Term Goals | Achieved in a few hours or days | “The patient will report a pain level of 3/10 within 4 hours after medication.” |
| Long-Term Goals | Achieved over weeks, months, or beyond discharge | “The patient will maintain an independent walking ability within 6 weeks post-surgery.” |
✅ Example:
For a stroke patient:
✔ Short-Term Goal: The patient will complete swallowing exercises safely within 48 hours.
✔ Long-Term Goal: The patient will regain independent feeding ability within 4 weeks.
4. Guidelines for Establishing Goals and Expected Outcomes
To ensure goals are effective and meaningful, nurses should follow these guidelines:
✅ 1. Goals Should Be Patient-Centered
- Goals must focus on what the patient will achieve, not what the nurse will do.
- Incorrect: “The nurse will monitor blood sugar levels.”
- Correct: “The patient will maintain blood glucose levels between 80-130 mg/dL within one week.”
✅ 2. Goals Must Be Realistic and Achievable
- Goals should match the patient’s physical, emotional, and mental condition.
- Incorrect: “The patient will run a marathon in 2 weeks after hip surgery.”
- Correct: “The patient will walk 10 steps with assistance by the third postoperative day.”
✅ 3. Goals Should Be Measurable and Specific
- Goals should contain clear, observable criteria.
- Incorrect: “The patient will feel better soon.”
- Correct: “The patient will verbalize a pain level of 3/10 or lower within 24 hours.”
✅ 4. Goals Must Be Time-Bound
- Each goal should specify a time frame for expected achievement.
- Incorrect: “The patient will improve lung function.”
- Correct: “The patient’s respiratory rate will be within normal limits (12-20 breaths per minute) within 24 hours.”
5. Components of Goals and Outcome Statements
A well-formulated goal or expected outcome should have the following components:
| Component | Description | Example |
|---|---|---|
| Subject (Who?) | The patient or a specific group | “The patient…” |
| Behavior (What?) | The expected action or response | “…will maintain a blood pressure of less than 140/90 mmHg…” |
| Criteria (How Well?) | The standard of performance or success measure | “…as evidenced by BP readings measured twice daily…” |
| Time Frame (When?) | The deadline for achieving the goal | “…within 1 week of initiating antihypertensive therapy.” |
✅ Final Example of a Complete Goal Statement:
“The patient will maintain a blood pressure of less than 140/90 mmHg as evidenced by BP readings measured twice daily within one week of initiating antihypertensive therapy.”
6. The SMART Criteria for Goal-Setting
Nursing goals should follow the SMART format:
| SMART Component | Definition | Example |
|---|---|---|
| S – Specific | Clearly defines what is to be achieved | “The patient will drink 2000 mL of water per day…” |
| M – Measurable | Can be quantified or observed | “…as evidenced by a urine output of at least 30 mL/hr.” |
| A – Achievable | Within the patient’s ability | “…given the patient’s stable kidney function.” |
| R – Relevant | Addresses the patient’s health needs | “…to prevent dehydration and electrolyte imbalance.” |
| T – Time-bound | Specifies a deadline | “…within 24 hours of hospital admission.” |
✅ Example of a SMART Goal Statement:
“The patient will drink 2000 mL of water per day as evidenced by a urine output of at least 30 mL/hr within 24 hours of hospital admission.”
7. Example Nursing Diagnoses with Goals and Expected Outcomes
| Nursing Diagnosis | Goal | Expected Outcome |
|---|---|---|
| Ineffective Airway Clearance related to mucus obstruction | “The patient will maintain clear airways.” | “The patient will have a respiratory rate of 12-20 breaths per minute within 8 hours.” |
| Risk for Falls related to muscle weakness | “The patient will prevent falls during hospitalization.” | “The patient will ambulate with assistance and report no falls within 24 hours.” |
| Acute Pain related to surgical incision | “The patient will experience pain relief.” | “The patient will report a pain score of 3/10 or lower within 6 hours after pain medication.” |
✅ Key Tip: The goal is broad, while the expected outcome is specific and measurable.
8. Common Mistakes in Establishing Goals and Expected Outcomes
🚫 Setting unrealistic goals
❌ “The patient will regain full mobility within 24 hours after a stroke.”
✅ Correct Approach: “The patient will move from bed to chair with assistance within 48 hours.”
🚫 Failing to make goals measurable
❌ “The patient will feel less anxious.”
✅ Correct Approach: “The patient will verbalize a reduction in anxiety symptoms (heart rate below 90 bpm) within 2 hours of relaxation therapy.”
🚫 Ignoring the patient’s involvement
❌ Setting goals without consulting the patient.
✅ Correct Approach: Discuss goals with the patient and ensure they align with their expectations and willingness to participate.
Types of Nursing Interventions:
1. Introduction
Nursing interventions are the actions taken by nurses to help patients achieve their health goals. These interventions are based on nursing diagnoses, patient needs, and clinical judgment.
Definition of Nursing Interventions
“Nursing interventions are actions taken by a nurse to improve, maintain, or restore a patient’s health status and to prevent complications.”
✅ Example:
A nurse administers oxygen to a patient with impaired gas exchange to maintain adequate oxygen levels.
2. Importance of Nursing Interventions
🔹 Helps in achieving patient goals and expected outcomes.
🔹 Promotes patient safety and comfort.
🔹 Prevents complications and disease progression.
🔹 Supports evidence-based practice in nursing care.
🔹 Enhances patient recovery and quality of life.
✅ Example:
A bedridden patient is turned every 2 hours to prevent pressure ulcers.
3. Types of Nursing Interventions
Nursing interventions are classified into three main categories:
| Type of Intervention | Definition | Example |
|---|---|---|
| Independent Nursing Interventions | Actions that nurses can perform without a physician’s order. | Repositioning a patient to prevent pressure ulcers. |
| Dependent Nursing Interventions | Actions that require a doctor’s prescription or order. | Administering prescribed medications. |
| Collaborative Nursing Interventions | Actions performed in collaboration with other healthcare professionals. | Working with a physiotherapist for rehabilitation exercises. |
✅ Example:
A nurse educating a diabetic patient on insulin administration is an independent intervention, while administering insulin as prescribed is a dependent intervention.
4. Detailed Explanation of Nursing Interventions
1. Independent Nursing Interventions
- Performed without a physician’s order.
- Based on nurse’s professional knowledge and skills.
- Aimed at preventing complications, promoting health, and managing patient needs.
✅ Examples:
✔ Repositioning a patient every 2 hours to prevent bedsores.
✔ Teaching deep breathing exercises to prevent pneumonia.
✔ Providing emotional support to a patient with anxiety.
2. Dependent Nursing Interventions
- Requires a physician’s order or medical prescription.
- Nurses perform these actions as part of the prescribed treatment plan.
✅ Examples:
✔ Administering IV fluids or medications as prescribed.
✔ Inserting a Foley catheter under physician’s instructions.
✔ Performing a dressing change for a wound based on a doctor’s order.
3. Collaborative Nursing Interventions
- Requires teamwork with other healthcare professionals.
- Nurses work with doctors, physiotherapists, dietitians, respiratory therapists, social workers, and pharmacists.
✅ Examples:
✔ Working with a physical therapist to develop a mobility plan for a stroke patient.
✔ Consulting a dietitian for a patient’s diabetic meal plan.
✔ Assisting a respiratory therapist in oxygen therapy management.
5. Categories of Nursing Interventions Based on Function
Apart from the three main types, nursing interventions can also be categorized based on their function or purpose:
| Category | Definition | Example |
|---|---|---|
| Direct Care Interventions | Performed directly with the patient. | Turning a patient to prevent bedsores. |
| Indirect Care Interventions | Actions performed away from the patient to support care. | Consulting with a dietitian about the patient’s nutrition plan. |
| Preventive Interventions | Aimed at preventing illness or complications. | Administering vaccines to prevent infections. |
| Supportive Interventions | Helps patients cope with stress and mental health issues. | Providing emotional support for a grieving patient. |
| Technical Interventions | Involves technical skills and procedures. | Inserting a nasogastric (NG) tube. |
✅ Example:
A nurse providing emotional support to a cancer patient is a supportive intervention, while administering chemotherapy medication is a technical intervention.
6. Examples of Nursing Interventions for Different Conditions
| Condition | Independent Interventions | Dependent Interventions | Collaborative Interventions |
|---|---|---|---|
| Hypertension | Teaching relaxation techniques | Administering antihypertensive drugs | Consulting a dietitian for a low-sodium diet |
| Diabetes Mellitus | Educating on insulin self-administration | Administering insulin as prescribed | Working with a nutritionist for meal planning |
| Respiratory Distress | Teaching deep breathing exercises | Administering oxygen therapy | Collaborating with a respiratory therapist |
| Pain Management | Repositioning the patient for comfort | Giving prescribed pain medication | Consulting a physiotherapist for rehabilitation |
✅ Example:
For a patient with hypertension, the nurse can:
✔ Educate on stress management (Independent).
✔ Give prescribed antihypertensive drugs (Dependent).
✔ Work with a dietitian for diet modifications (Collaborative).
7. Guidelines for Selecting Nursing Interventions
To ensure effective patient care, nurses should follow these guidelines when choosing interventions:
✅ 1. Align with Nursing Diagnoses and Goals
- Each intervention should directly address the patient’s nursing diagnosis and support expected outcomes.
- Example: For a nursing diagnosis of “Impaired Gas Exchange”, an appropriate intervention is positioning the patient in a high Fowler’s position.
✅ 2. Be Evidence-Based
- Use clinical guidelines and best practices when selecting interventions.
- Example: Using incentive spirometry to prevent post-operative pneumonia.
✅ 3. Ensure Safety and Feasibility
- Consider the patient’s physical condition, resources, and safety.
- Example: Avoiding ambulation in a patient with unstable fractures.
✅ 4. Involve the Patient and Family
- Encourage active participation in care to promote adherence.
- Example: Teaching family members how to assist with wound dressing.
✅ 5. Be Specific and Measurable
- Clearly define what, how, when, and why the intervention is performed.
- Example: “Reposition the patient every 2 hours to prevent pressure ulcers.”
8. Common Mistakes in Implementing Nursing Interventions
🚫 Failing to Individualize Care
❌ Using the same interventions for all patients without assessing individual needs.
✅ Correct Approach: Tailor interventions to each patient’s condition.
🚫 Ignoring Patient Preferences
❌ Forcing interventions without considering patient beliefs and choices.
✅ Correct Approach: Involve the patient in decision-making.
🚫 Not Documenting Interventions Properly
❌ Failing to record nursing actions and patient responses.
✅ Correct Approach: Always document interventions accurately for legal and professional accountability.
Selecting Nursing Interventions: Protocols and Standing Orders
1. Introduction
Selecting appropriate nursing interventions is a crucial part of the nursing process, ensuring effective and individualized patient care. Protocols and standing orders provide structured guidelines to help nurses implement evidence-based interventions safely and efficiently.
Definition of Nursing Interventions
“Nursing interventions are specific actions taken by a nurse to promote patient health, prevent complications, and achieve patient-centered goals.”
✅ Example:
A nurse follows a standing order to administer oxygen to a patient with low oxygen saturation without waiting for a physician’s order.
2. Importance of Protocols and Standing Orders in Nursing
- Ensures safe and standardized care.
- Helps nurses act quickly in emergencies.
- Supports evidence-based practice.
- Reduces treatment delays and improves patient outcomes.
- Allows nurses to work independently within their scope of practice.
✅ Example:
In a hospital, a nurse uses a protocol for fall prevention, ensuring all at-risk patients have side rails up and a fall alert bracelet.
3. Definition and Differences Between Protocols and Standing Orders
| Term | Definition | Example |
|---|---|---|
| Protocols | Step-by-step clinical guidelines developed for managing specific conditions, ensuring consistency in care. | A hospital sepsis protocol guides nurses in early recognition, fluid resuscitation, and monitoring. |
| Standing Orders | Pre-approved medical instructions that allow nurses to perform specific interventions without obtaining a new physician order each time. | A standing order for chest pain may instruct nurses to administer aspirin and start an ECG before contacting a doctor. |
✅ Key Difference:
- Protocols provide general guidelines for patient care.
- Standing orders allow nurses to take immediate action without waiting for a doctor’s order.
4. Nursing Protocols: Guidelines for Standardized Care
A nursing protocol is a structured plan that outlines the step-by-step management of specific health conditions. It ensures consistency and adherence to best practices.
Characteristics of Nursing Protocols
✔ Developed based on evidence-based guidelines.
✔ Ensures uniformity in patient care.
✔ Used for common conditions or procedures.
✔ May vary between hospitals, clinics, and long-term care facilities.
Examples of Common Nursing Protocols
| Protocol Type | Example |
|---|---|
| Fall Prevention Protocol | Ensures bed alarms, non-slip socks, and fall risk assessments for high-risk patients. |
| Pain Management Protocol | Guides assessment and administration of pain medications based on pain scores. |
| Sepsis Management Protocol | Directs early recognition, lab tests, and fluid resuscitation for sepsis. |
| Post-Operative Care Protocol | Outlines pain control, mobility exercises, and infection prevention. |
✅ Example:
A hypoglycemia protocol in a hospital instructs nurses to:
✔ Check blood glucose levels immediately.
✔ Administer oral glucose or IV dextrose based on severity.
✔ Monitor the patient’s vital signs and response.
5. Standing Orders: Empowering Nurses for Immediate Care
Standing orders are pre-approved medical instructions that allow nurses to initiate specific treatments without a direct physician’s order.
Characteristics of Standing Orders
✔ Developed by physicians and approved by hospital administration.
✔ Provides quick decision-making power for nurses.
✔ Common in emergency departments, ICUs, and outpatient clinics.
✔ Helps in early intervention and improved patient safety.
Examples of Common Standing Orders
| Standing Order Type | Example |
|---|---|
| Emergency Chest Pain | Administer aspirin, nitroglycerin, and oxygen before physician arrival. |
| Hypoglycemia Management | If blood glucose <70 mg/dL, administer 15g glucose orally or IV dextrose. |
| Hypertension Management | If BP >180/110 mmHg, give PRN antihypertensive medication. |
| Anaphylaxis Treatment | Give epinephrine IM, antihistamines, and corticosteroids immediately. |
✅ Example:
A standing order in a dialysis unit may allow nurses to administer heparin to prevent clotting without contacting a doctor each time.
6. How Nurses Implement Protocols and Standing Orders
1. Assess the Patient
- Check vital signs, symptoms, and lab reports.
- Identify if the patient meets protocol criteria.
✅ Example:
A nurse assessing a patient with fever, low BP, and rapid breathing initiates a sepsis protocol for early treatment.
2. Follow Protocols and Standing Orders
- Identify the correct protocol for the condition.
- Implement interventions step-by-step as outlined.
- Document actions taken and patient response.
✅ Example:
A nurse follows the fall prevention protocol by:
✔ Placing bed rails up.
✔ Giving non-slip socks.
✔ Using a bed alarm for a confused patient.
3. Monitor and Evaluate
- Observe patient response to interventions.
- Reassess symptoms and adjust care if needed.
- Notify the physician if the patient does not improve.
✅ Example:
If a patient with chest pain still has pain after aspirin and nitroglycerin, the nurse calls the physician for further instructions.
7. Benefits of Using Protocols and Standing Orders
| Benefit | Protocols | Standing Orders |
|---|---|---|
| Enhances Patient Safety | Ensures evidence-based practices. | Allows rapid intervention in emergencies. |
| Reduces Delays in Treatment | Standardized guidelines prevent confusion. | Nurses can act immediately without waiting for a doctor. |
| Promotes Consistency | All nurses follow the same procedures. | Ensures uniformity in emergency responses. |
| Improves Healthcare Efficiency | Reduces treatment variability. | Helps manage high-risk conditions efficiently. |
✅ Example:
A hospital stroke protocol ensures rapid CT scans and clot-dissolving medications are given immediately to reduce brain damage.
8. Common Mistakes in Using Protocols and Standing Orders
🚫 Not verifying patient eligibility
❌ Using a diabetes management protocol for a non-diabetic patient.
✅ Correct Approach: Always confirm patient conditions before implementing protocols.
🚫 Failure to document interventions
❌ Administering medications without recording the action.
✅ Correct Approach: Always document the intervention, time, and patient response.
🚫 Overlooking contraindications
❌ Giving antihypertensive medication when the patient’s BP is already low.
✅ Correct Approach: Assess contraindications before following standing orders.
Introduction to Nursing Intervention Classification (NIC)
1. Introduction to Nursing Intervention Classification (NIC)
The Nursing Intervention Classification (NIC) is a standardized system used to classify nursing interventions. It helps organize and describe nursing care in a clear, measurable way. NIC was developed by the University of Iowa’s College of Nursing to support evidence-based practice, nursing education, and research.
Definition of Nursing Intervention Classification (NIC)
“The Nursing Intervention Classification (NIC) is a comprehensive, research-based, standardized classification of interventions that nurses perform to enhance patient outcomes.”
✅ Example:
If a patient has a nursing diagnosis of “Impaired Gas Exchange”, the nurse can select the NIC intervention “Oxygen Therapy (3320)” to improve oxygen levels.
2. Purpose and Importance of NIC
NIC provides a universal language for nurses to document and communicate patient care effectively.
Why is NIC Important?
✔ Standardizes nursing interventions across healthcare settings.
✔ Enhances communication among nurses and healthcare teams.
✔ Facilitates research and evidence-based practice.
✔ Supports electronic health records (EHRs) for accurate documentation.
✔ Improves patient outcomes by guiding appropriate interventions.
✅ Example:
A nurse caring for a diabetic patient can use the NIC “Blood Glucose Monitoring (2300)” intervention to ensure proper blood sugar control.
3. Structure of NIC: How It Works
NIC is structured into seven domains and 30 classes, which group related interventions based on patient needs.
NIC Domains and Classes
| Domain | Classes (Categories of Interventions) | Example Interventions |
|---|---|---|
| 1. Physiological: Basic | Activity and Exercise Management, Elimination Management, Immobility Management, Nutrition Support, Physical Comfort Promotion | Positioning (0840), Pain Management (1400), Nutrition Monitoring (1020) |
| 2. Physiological: Complex | Electrolyte and Acid-Base Management, Drug Management, Neurologic and Cardiovascular Management | Oxygen Therapy (3320), IV Therapy (4200) |
| 3. Behavioral | Behavior Therapy, Cognitive Therapy, Communication Enhancement, Coping Assistance | Anxiety Reduction (5820), Emotional Support (5270) |
| 4. Safety | Risk Management, Infection Control, Tissue Perfusion Management | Fall Prevention (6490), Pressure Ulcer Prevention (3540) |
| 5. Family | Caregiving Facilitation, Family Support, Childbearing Care | Family Integrity Promotion (7160) |
| 6. Health System | Information Management, Health Policy, Health System Mediation | Shift Report (7920), Infection Surveillance (6650) |
| 7. Community | Community Health Promotion, Disaster Preparedness | Disaster Preparedness (7970), Smoking Cessation Assistance (4490) |
✅ Example:
A nurse working in an ICU may use the NIC “Mechanical Ventilation Management (3300)” intervention to optimize patient breathing support.
4. Types of Nursing Interventions in NIC
NIC interventions are categorized based on how nurses deliver care.
| Type of Intervention | Definition | Example |
|---|---|---|
| Independent Nursing Interventions | Actions nurses perform without a doctor’s order. | Repositioning a patient to prevent bedsores (NIC: “Positioning (0840)”). |
| Dependent Nursing Interventions | Actions that require a physician’s order. | Administering IV medications (NIC: “IV Therapy (4200)”). |
| Collaborative Nursing Interventions | Actions performed in coordination with other healthcare professionals. | Working with a dietitian to develop a diabetic meal plan (NIC: “Nutrition Counseling (5240)”). |
✅ Example:
A nurse helping a patient with mobility issues may select the NIC “Ambulation Therapy (0200)” to improve walking ability.
5. Examples of NIC Interventions Based on Patient Conditions
| Condition | Nursing Diagnosis | NIC Intervention |
|---|---|---|
| Hypertension | Risk for ineffective cerebral tissue perfusion | Blood Pressure Monitoring (4315) |
| Diabetes Mellitus | Risk for unstable blood glucose levels | Blood Glucose Monitoring (2300) |
| Post-Surgical Care | Acute pain related to surgical incision | Pain Management (1400) |
| Pneumonia | Ineffective airway clearance | Airway Suctioning (3160) |
| Stroke Recovery | Impaired physical mobility | Range of Motion Exercises (0205) |
✅ Example:
For a patient with pressure ulcers, the nurse may select “Wound Care (3660)” from NIC to promote healing.
6. How to Select the Right NIC Intervention
1. Identify the Nursing Diagnosis
- Use NANDA-I approved nursing diagnoses.
- Example: “Impaired Gas Exchange related to lung disease.”
2. Match with Appropriate NIC Intervention
- Choose an intervention that addresses the nursing diagnosis.
- Example: “Oxygen Therapy (3320)” for impaired gas exchange.
3. Consider Patient Needs and Preferences
- Ensure cultural and personal preferences are respected.
- Example: Dietary Modifications (5246) for a vegetarian diabetic patient.
4. Follow Evidence-Based Guidelines
- Use current best practices and hospital protocols.
- Example: Fall Prevention (6490) for elderly patients at risk.
5. Evaluate the Effectiveness of the Intervention
- Monitor patient response and adjust interventions if needed.
- Example: If “Pain Management (1400)” is ineffective, the nurse may modify the medication plan.
✅ Example:
A nurse caring for a patient with anxiety may select the NIC “Anxiety Reduction (5820)”, which includes relaxation techniques, breathing exercises, and emotional support.
7. Documenting NIC Interventions in Patient Care
Proper documentation ensures effective communication and continuity of care.
| Documentation Requirement | Example |
|---|---|
| Intervention Name | “Oxygen Therapy (3320)” |
| Date & Time | “March 10, 2025, 10:00 AM” |
| Action Taken | “Administered 2L oxygen via nasal cannula.” |
| Patient Response | “Oxygen saturation improved to 96% after 30 minutes.” |
✅ Example:
A nurse documents: “Repositioned patient every 2 hours as per NIC ‘Positioning (0840)’. No new pressure ulcers observed.”
8. Challenges in Implementing NIC
🚫 Lack of Awareness
❌ Some nurses are unfamiliar with NIC interventions.
✅ Solution: Provide training and education on NIC.
🚫 Inconsistent Documentation
❌ Failure to record nursing interventions in medical records.
✅ Solution: Use electronic health records (EHRs) for accurate documentation.
🚫 Limited Resources
❌ Some interventions require specialized equipment or staff.
✅ Solution: Prioritize essential interventions based on available resources.
Nursing Outcome Classification (NOC).

1. Introduction to Nursing Outcome Classification (NOC)
The Nursing Outcome Classification (NOC) is a standardized system that defines measurable patient outcomes in response to nursing interventions. Developed by the University of Iowa’s College of Nursing, NOC helps nurses evaluate the effectiveness of their interventions and improves patient care documentation.
Definition of NOC
“The Nursing Outcome Classification (NOC) is a standardized set of patient outcomes that reflect the impact of nursing interventions on patient health.”
✅ Example:
A nurse implementing the “Pain Management (NIC: 1400)” intervention can measure its success using the NOC “Pain Level (NOC: 2102)”, which evaluates the patient’s pain intensity on a scale.
2. Purpose and Importance of NOC
- Provides a measurable way to assess patient progress.
- Enhances nursing documentation and communication.
- Supports evidence-based practice.
- Helps in quality improvement and research.
- Facilitates continuity of care across healthcare settings.
✅ Example:
If a nurse implements a NIC intervention for respiratory distress, they can use the NOC “Respiratory Status (0415)” to evaluate improvements in oxygen levels and breathing patterns.
3. Structure of NOC: Domains and Classes
The NOC system organizes outcomes into seven domains and 32 classes, grouping similar outcomes together.
NOC Domains and Classes
| Domain | Classes (Categories of Outcomes) | Example Outcomes (NOC Codes) |
|---|---|---|
| 1. Functional Health | Mobility, Activity Tolerance, Self-Care | Walking (0211), Self-Care Status (0300) |
| 2. Physiologic Health | Cardiac, Respiratory, Neurologic, Endocrine | Respiratory Status (0415), Pain Level (2102) |
| 3. Psychosocial Health | Coping, Communication, Mental Well-being | Anxiety Reduction (1211), Social Interaction Skills (1502) |
| 4. Health Knowledge & Behavior | Health Promotion, Medication Adherence | Medication Management (1823), Health Literacy (1802) |
| 5. Perceived Health | Satisfaction, Quality of Life | Quality of Life (2008), Satisfaction with Care (2501) |
| 6. Family Health | Caregiver Well-being, Family Coping | Caregiver Stress (2203), Family Coping (2205) |
| 7. Community Health | Public Health, Access to Care | Community Health Status (2702), Health Promotion (2708) |
✅ Example:
A patient recovering from a heart attack may have the outcome “Cardiac Pump Effectiveness (NOC: 0403)”, which assesses heart function and blood circulation.
4. Types of Nursing Outcomes in NOC
Outcomes in NOC are classified based on how they reflect patient progress.
| Type of Outcome | Definition | Example |
|---|---|---|
| Short-Term Outcomes | Changes within hours or days. | “Pain Level (2102)” improves within 4 hours after pain medication. |
| Intermediate Outcomes | Achieved within a few weeks. | “Mobility Level (0212)” increases after 2 weeks of physiotherapy. |
| Long-Term Outcomes | Achieved after months or more. | “Quality of Life (2008)” improves 3 months after surgery. |
✅ Example:
For a patient with diabetes, the NOC outcome “Blood Glucose Level (0410)” can be measured short-term after insulin administration and long-term with lifestyle changes.
5. Examples of NOC Outcomes Based on Patient Conditions
| Condition | Nursing Diagnosis | NIC Intervention | NOC Outcome |
|---|---|---|---|
| Hypertension | Risk for ineffective cerebral tissue perfusion | Blood Pressure Monitoring (4315) | Blood Pressure Control (0405) |
| Diabetes Mellitus | Risk for unstable blood glucose levels | Blood Glucose Monitoring (2300) | Blood Glucose Level (0410) |
| Post-Surgical Care | Acute pain related to surgical incision | Pain Management (1400) | Pain Level (2102) |
| Pneumonia | Ineffective airway clearance | Airway Suctioning (3160) | Respiratory Status (0415) |
| Stroke Recovery | Impaired physical mobility | Range of Motion Exercises (0205) | Mobility Level (0212) |
✅ Example:
A nurse caring for a patient with pneumonia may use the NIC intervention “Oxygen Therapy (3320)” and assess its success using the NOC “Oxygenation Status (0402)”.
6. How to Select the Right NOC Outcome
1. Identify the Nursing Diagnosis
- Use NANDA-I nursing diagnoses.
- Example: “Impaired Gas Exchange related to COPD.”
2. Match the Diagnosis with a NIC Intervention
- Example: “Oxygen Therapy (3320)” is a suitable intervention.
3. Select a Relevant NOC Outcome
- Example: “Respiratory Status (0415)” measures improvements in breathing.
4. Set a Measurement Scale for Evaluation
- NOC uses 5-point Likert scales (1 = worst, 5 = best).
- Example: A patient’s “Pain Level (2102)” improves from 2 (severe pain) to 4 (mild pain) after treatment.
5. Evaluate and Adjust the Care Plan
- If the expected outcome is not met, adjust the nursing interventions.
- Example: If a patient’s oxygen levels do not improve, the nurse may adjust positioning or increase oxygen flow.
✅ Example:
A nurse treating a post-surgical patient’s pain may document that the NOC outcome “Pain Level (2102)” improved from 3 (moderate pain) to 5 (no pain) after medication.
7. Documenting NOC Outcomes in Patient Care
Proper documentation ensures continuity of care and accurate evaluation of nursing interventions.
| Documentation Requirement | Example |
|---|---|
| Outcome Name & Code | “Pain Level (2102)” |
| Baseline Score | “Initial pain level: 2 (Severe pain)” |
| Intervention Applied | “Administered oral analgesic and repositioned patient.” |
| Final Score | “Pain level improved to 4 (Mild pain) after 30 minutes.” |
✅ Example:
A nurse records:
“Pain Level (NOC: 2102) improved from 2 to 4 after pain medication and ice pack application.”
8. Challenges in Implementing NOC
🚫 Lack of Awareness
❌ Some nurses do not use standardized outcomes.
✅ Solution: Provide training on NOC documentation.
🚫 Inconsistent Outcome Measurement
❌ Nurses may not use measurement scales correctly.
✅ Solution: Ensure proper training on using NOC scales.
🚫 Limited Integration with Electronic Records
❌ Some hospitals lack electronic health records (EHR) compatibility.
✅ Solution: Implement standardized documentation in EHR systems.
Guidelines for Writing a Nursing Care Plan (NCP)
1. Introduction
A nursing care plan (NCP) is a structured document that outlines a patient’s nursing diagnoses, goals, interventions, and expected outcomes. It serves as a roadmap for patient care, ensuring that nursing actions are evidence-based, individualized, and goal-directed.
Definition of a Nursing Care Plan
“A nursing care plan is a written outline of the nursing process that includes assessment, diagnosis, planning, implementation, and evaluation to provide individualized patient care.”
✅ Example:
For a patient with pneumonia, a care plan includes:
✔ Nursing Diagnosis: Ineffective airway clearance
✔ Goal: Patient will maintain clear airways within 48 hours.
✔ Interventions: Positioning, oxygen therapy, deep breathing exercises.
✔ Expected Outcome: Patient’s oxygen saturation will be ≥95%.
2. Importance of a Nursing Care Plan
🔹 Ensures continuity of care across different nurses and shifts.
🔹 Provides a structured, organized approach to patient care.
🔹 Enhances communication between healthcare professionals.
🔹 Supports evidence-based practice and improves patient outcomes.
🔹 Serves as a legal document in case of disputes or audits.
✅ Example:
A post-surgical nursing care plan ensures effective pain management, wound care, and mobility support.
3. Components of a Nursing Care Plan
A well-written nursing care plan consists of five essential components, following the ADPIE (Assessment, Diagnosis, Planning, Implementation, and Evaluation) framework.
| Component | Description | Example |
|---|---|---|
| 1. Assessment | Collect subjective and objective data to identify patient problems. | “Patient reports shortness of breath; SpO₂ = 89%.” |
| 2. Nursing Diagnosis | Identify the problem based on assessment data using NANDA-I approved diagnoses. | “Ineffective airway clearance related to mucus production as evidenced by dyspnea and wheezing.” |
| 3. Goals/Outcomes | Define SMART goals that describe expected patient improvements. | “Patient’s SpO₂ will improve to ≥95% within 24 hours.” |
| 4. Nursing Interventions | List specific nursing actions to achieve goals. | “Administer oxygen therapy, encourage deep breathing exercises.” |
| 5. Evaluation | Assess patient response to interventions and adjust care as needed. | “After 24 hours, SpO₂ improved to 96%; goal met.” |
✅ Example:
For a postoperative patient, the care plan might include:
✔ Assessment: Pain score of 8/10
✔ Diagnosis: Acute pain related to surgical incision
✔ Goal: Pain score will be ≤3/10 within 6 hours
✔ Intervention: Administer prescribed analgesic, apply ice pack, encourage relaxation techniques
✔ Evaluation: Pain score reduced to 3/10 after interventions.
4. Guidelines for Writing a Nursing Care Plan
To ensure clarity and effectiveness, follow these guidelines when writing a nursing care plan.
✅ 1. Use NANDA-I Approved Nursing Diagnoses
- Choose a valid and evidence-based nursing diagnosis from the NANDA International (NANDA-I) list.
- Avoid using medical diagnoses in the nursing care plan.
🚫 Incorrect: “Pneumonia” (Medical diagnosis).
✅ Correct: “Ineffective airway clearance related to mucus production as evidenced by dyspnea and wheezing.”
✅ 2. Follow the PES Format for Writing Nursing Diagnoses
Each nursing diagnosis statement should include three components:
| Component | Definition | Example |
|---|---|---|
| P – Problem | The nursing diagnosis (NANDA-I). | Impaired skin integrity |
| E – Etiology (Cause) | The related factors or causes. | Related to prolonged immobility |
| S – Signs/Symptoms | The evidence supporting the diagnosis. | As evidenced by a stage 2 pressure ulcer on the sacrum. |
✅ Example of a Nursing Diagnosis Statement:
“Impaired skin integrity related to prolonged immobility as evidenced by a stage 2 pressure ulcer on the sacrum.”
✅ 3. Set SMART Goals (Specific, Measurable, Achievable, Relevant, Time-bound)
Each goal or expected outcome should follow the SMART format:
| SMART Component | Definition | Example |
|---|---|---|
| S – Specific | Clearly define the desired change. | “The patient will maintain oxygen saturation ≥95%.” |
| M – Measurable | Include quantifiable criteria. | “Pain score will be ≤3/10 within 6 hours.” |
| A – Achievable | Ensure realistic expectations. | “Patient will ambulate with assistance within 48 hours.” |
| R – Relevant | Address the patient’s actual needs. | “Patient will verbalize effective pain relief techniques.” |
| T – Time-bound | Specify a timeframe for achievement. | “Within 24 hours of intervention.” |
✅ Example of a Goal Statement:
“The patient will report a pain level of ≤3/10 within 6 hours after receiving prescribed analgesics.”
✅ 4. Select Evidence-Based Nursing Interventions
Each intervention should be:
✔ Based on evidence-based guidelines.
✔ Specific and actionable.
✔ Documented properly in the care plan.
| Type of Intervention | Example |
|---|---|
| Independent (Nurse-initiated) | Repositioning a bedridden patient every 2 hours. |
| Dependent (Physician-ordered) | Administering IV antibiotics as prescribed. |
| Collaborative (Multidisciplinary) | Working with a physiotherapist for stroke rehabilitation. |
✅ Example of Nursing Interventions for a Stroke Patient:
✔ Encourage range-of-motion exercises to prevent contractures.
✔ Assist with feeding using adaptive utensils for independent eating.
✔ Provide speech therapy consultation for swallowing difficulties.
✅ 5. Document the Patient’s Response in the Evaluation Phase
- Compare actual outcomes with the expected outcomes.
- Document whether the goal was met, partially met, or not met.
- If goals are not met, revise the care plan accordingly.
✅ Example:
✔ Goal: “Patient will report pain ≤3/10 within 6 hours.”
✔ Evaluation: “After intervention, pain score was 4/10. Adjusted analgesic dosage per protocol.”
5. Example of a Complete Nursing Care Plan
| Component | Details |
|---|---|
| Assessment | “Patient reports difficulty breathing, wheezing, and SpO₂ = 89%.” |
| Nursing Diagnosis | “Ineffective airway clearance related to mucus production as evidenced by dyspnea and wheezing.” |
| Goal/Outcome | “Patient’s oxygen saturation will improve to ≥95% within 24 hours of oxygen therapy.” |
| Nursing Interventions | 1) Administer oxygen therapy as prescribed. 2) Encourage deep breathing exercises every 2 hours. 3) Monitor lung sounds and oxygen saturation every 4 hours. |
| Evaluation | “After 24 hours, SpO₂ improved to 96%. Goal met.” |
✅ Key Takeaway:
The care plan must be specific, measurable, and adaptable based on the patient’s response.
Implementation in the Nursing Process.

1. Introduction to Implementation in Nursing
The implementation phase is the fourth step in the nursing process (after Assessment, Diagnosis, and Planning). This stage involves carrying out the planned nursing interventions to achieve the desired patient outcomes. It is a dynamic, action-oriented phase where nurses apply clinical judgment and skills to improve patient health.
Definition of Implementation in the Nursing Process
“Implementation is the process of executing the planned nursing interventions to achieve patient-centered goals and expected outcomes.”
✅ Example:
For a patient with pneumonia, implementation includes:
✔ Administering oxygen therapy as prescribed.
✔ Encouraging deep breathing exercises.
✔ Monitoring respiratory status and oxygen levels.
2. Purpose of Implementation in Nursing
🔹 Ensures nursing interventions are carried out effectively.
🔹 Helps in achieving patient goals and expected outcomes.
🔹 Provides individualized patient care.
🔹 Facilitates collaboration between nurses, physicians, and other healthcare professionals.
🔹 Promotes evidence-based practice and improves patient safety.
✅ Example:
A post-operative patient requires interventions such as pain management, wound care, and early ambulation to prevent complications.
3. Key Elements of Implementation
The implementation phase includes the following key elements:
| Element | Description |
|---|---|
| 1. Reassessing the Patient | Before carrying out interventions, the nurse must reassess the patient’s condition. |
| 2. Determining the Need for Assistance | If a task requires help, the nurse seeks assistance from other healthcare professionals. |
| 3. Implementing Nursing Interventions | The nurse executes the planned interventions based on the care plan. |
| 4. Supervising Delegated Care | If care tasks are delegated to nursing assistants, the nurse ensures proper execution. |
| 5. Documenting Nursing Interventions | The nurse records actions taken and patient responses in the medical record. |
✅ Example:
A nurse reassesses a patient with high fever and finds the temperature has increased. The nurse adjusts the intervention by administering prescribed antipyretics and increasing fluid intake.
4. Types of Nursing Interventions During Implementation
The nursing interventions implemented during this phase fall into three categories:
1. Independent Nursing Interventions
- Actions nurses can perform without a doctor’s order.
- Based on nursing knowledge, judgment, and experience.
✅ Examples:
✔ Repositioning a patient every 2 hours to prevent pressure ulcers.
✔ Providing emotional support to a patient experiencing anxiety.
✔ Teaching a diabetic patient how to check blood glucose levels.
2. Dependent Nursing Interventions
- Actions that require a physician’s order.
- Nurses execute medical treatments prescribed by doctors.
✅ Examples:
✔ Administering IV medications as prescribed.
✔ Starting oxygen therapy for a patient with low oxygen levels.
✔ Applying a wound dressing as per the physician’s orders.
3. Collaborative Nursing Interventions
- Performed in collaboration with other healthcare professionals.
- Requires coordination with doctors, physical therapists, dietitians, and respiratory therapists.
✅ Examples:
✔ Working with a physical therapist to develop a mobility plan for a stroke patient.
✔ Consulting a dietitian to create a nutritional plan for a malnourished patient.
✔ Collaborating with a pharmacist to monitor medication side effects.
5. Steps in the Implementation Phase
The nursing implementation process follows a systematic approach to ensure effective care.
| Step | Description |
|---|---|
| Step 1: Reassess the Patient | Before performing any intervention, reassess the patient’s condition. |
| Step 2: Validate the Care Plan | Ensure that interventions are still appropriate based on current patient needs. |
| Step 3: Organize Resources and Equipment | Gather all necessary supplies and arrange the environment. |
| Step 4: Implement the Interventions | Carry out nursing actions according to the care plan. |
| Step 5: Monitor the Patient’s Response | Evaluate how the patient reacts to the intervention. |
| Step 6: Document the Care Provided | Record the intervention, patient response, and any modifications. |
✅ Example:
For a patient receiving oxygen therapy, the nurse:
✔ Step 1: Reassesses oxygen levels (SpO₂).
✔ Step 2: Confirms the oxygen order is correct.
✔ Step 3: Ensures oxygen mask and tubing are ready.
✔ Step 4: Administers the oxygen therapy.
✔ Step 5: Monitors respiratory rate and improvement.
✔ Step 6: Documents SpO₂ changes and patient response.
6. Common Nursing Interventions in Different Clinical Scenarios
| Condition | Independent Interventions | Dependent Interventions | Collaborative Interventions |
|---|---|---|---|
| Hypertension | Teach relaxation techniques | Administer prescribed antihypertensives | Work with a dietitian for a low-sodium diet |
| Diabetes Mellitus | Educate on insulin self-administration | Administer prescribed insulin | Collaborate with a nutritionist for meal planning |
| Pneumonia | Encourage deep breathing exercises | Start IV antibiotics as prescribed | Work with a respiratory therapist for chest physiotherapy |
| Pain Management | Apply cold compress, reposition for comfort | Administer prescribed pain medications | Work with a physiotherapist for pain-relief exercises |
✅ Example:
For a patient with post-operative pain, interventions include:
✔ Repositioning for comfort (Independent).
✔ Administering IV analgesics (Dependent).
✔ Coordinating with a physiotherapist for mobilization (Collaborative).
7. Documenting Implementation in Nursing
Proper documentation ensures legal, ethical, and professional accountability.
Key Elements of Documentation in Implementation
✔ Time and date of intervention.
✔ Specific nursing actions taken.
✔ Patient response to interventions.
✔ Any modifications to the care plan.
✅ Example:
“March 10, 2025, 10:00 AM: Administered oxygen therapy at 2L/min via nasal cannula. Patient’s SpO₂ improved from 89% to 96% after 30 minutes. No signs of respiratory distress observed.”
8. Challenges in the Implementation Phase
🚫 Not reassessing the patient before intervention
❌ Incorrect Approach: Performing interventions without checking if they are still needed.
✅ Correct Approach: Always reassess the patient’s condition before proceeding.
🚫 Lack of patient involvement
❌ Incorrect Approach: Providing care without explaining procedures to the patient.
✅ Correct Approach: Educate and involve the patient in decision-making.
🚫 Incomplete documentation
❌ Incorrect Approach: Failing to record patient response to interventions.
✅ Correct Approach: Document all nursing actions and patient outcomes.
Process of Implementing the Plan of Care in Nursing
1. Introduction to Implementation in Nursing
The implementation phase is the fourth step of the nursing process (after Assessment, Diagnosis, and Planning). During this stage, nurses carry out the planned interventions to help the patient achieve the desired health outcomes.
Definition of Implementation
“Implementation is the execution of planned nursing interventions to achieve patient-centered goals and expected outcomes.”
✅ Example:
For a patient with pneumonia, implementation includes:
✔ Administering oxygen therapy.
✔ Encouraging deep breathing exercises.
✔ Monitoring respiratory status and oxygen saturation levels.
2. Steps in the Implementation Process
The implementation process consists of five essential steps to ensure safe and effective nursing care.
| Step | Description | Example |
|---|---|---|
| 1. Reassessing the Patient | Evaluate the patient’s current condition to ensure the selected interventions are still appropriate. | Before administering insulin, check the patient’s blood glucose level. |
| 2. Reviewing and Modifying the Care Plan | Adjust interventions if the patient’s condition has changed or if outcomes are not being met. | If pain persists despite medication, adjust the intervention by changing the dosage or adding non-pharmacological pain relief. |
| 3. Organizing Resources and Delegating Tasks | Gather necessary equipment, supplies, and staff support before implementation. | Before inserting an IV line, ensure sterile gloves, IV fluids, and catheter are available. |
| 4. Implementing the Nursing Interventions | Perform planned independent, dependent, and collaborative interventions. | Repositioning a bedridden patient every 2 hours to prevent pressure ulcers. |
| 5. Documenting the Care Provided | Record interventions performed and the patient’s response in medical records. | “Administered 500mL IV fluids; BP improved from 88/60 to 110/75 mmHg after 30 minutes.” |
✅ Example:
For a post-operative patient, the implementation steps include:
✔ Reassessing pain levels before giving medication.
✔ Modifying the care plan if pain persists despite intervention.
✔ Ensuring the patient has ice packs and analgesics available.
✔ Administering prescribed analgesics and repositioning the patient.
✔ Documenting pain reduction from 8/10 to 3/10 after intervention.
3. Types of Nursing Interventions in Implementation
During implementation, nurses perform three types of interventions:
| Type | Definition | Example |
|---|---|---|
| Independent Nursing Interventions | Actions nurses perform without a doctor’s order based on clinical judgment. | Repositioning a patient to prevent bedsores. |
| Dependent Nursing Interventions | Actions that require a physician’s order. | Administering IV medications as prescribed. |
| Collaborative Nursing Interventions | Actions performed in collaboration with other healthcare professionals. | Working with a dietitian to create a diabetic meal plan. |
✅ Example:
For a patient with hypertension, the nurse will:
✔ Educate on lifestyle modifications (Independent).
✔ Administer prescribed antihypertensive drugs (Dependent).
✔ Collaborate with a nutritionist for dietary planning (Collaborative).
4. Essential Guidelines for Implementing the Plan of Care
To ensure safe and effective patient care, follow these guidelines during the implementation phase.
✅ 1. Base Interventions on Evidence-Based Practice
- Use clinical guidelines, research, and hospital protocols to select interventions.
- Example: Following the WHO pain management ladder for patients with chronic pain.
✅ 2. Reassess the Patient Before Each Intervention
- Never assume that an intervention is still appropriate without reassessing the patient.
- Example: Checking a patient’s temperature before administering antipyretics.
✅ 3. Prioritize Patient Safety
- Follow infection control measures, proper patient positioning, and safe medication administration.
- Example: Using sterile technique for catheter insertion to prevent infections.
✅ 4. Encourage Patient Participation in Care
- Educate patients about their treatment plan and encourage self-care.
- Example: Teaching a diabetic patient how to inject insulin properly.
✅ 5. Maintain Effective Communication with the Healthcare Team
- Collaborate with doctors, physiotherapists, dietitians, and social workers to provide holistic care.
- Example: Updating the physician about a patient’s unresponsiveness to treatment.
✅ 6. Adapt to the Patient’s Cultural and Psychological Needs
- Modify interventions based on the patient’s cultural beliefs and emotional state.
- Example: Using spiritual support or relaxation techniques for a patient experiencing anxiety.
✅ Example:
For a patient recovering from a stroke, interventions include:
✔ Encouraging the patient to perform self-care tasks (to regain independence).
✔ Collaborating with a physiotherapist for mobility training.
✔ Using assistive devices like a walker or handrails.
5. Documentation in the Implementation Phase
Proper documentation is essential for legal, ethical, and professional reasons.
Key Elements of Documentation in Implementation
✔ Date and time of intervention.
✔ Specific nursing actions performed.
✔ Patient response to intervention.
✔ Any modifications made to the care plan.
✅ Example of Documentation:
“March 15, 2025, 10:00 AM: Administered 2L oxygen via nasal cannula. Patient’s SpO₂ improved from 89% to 96% after 20 minutes. No signs of respiratory distress observed.”
6. Common Mistakes in Implementing a Care Plan
🚫 Skipping Patient Reassessment
❌ Performing interventions without checking if the patient’s condition has changed.
✅ Correct Approach: Always reassess before intervention.
🚫 Lack of Patient Involvement
❌ Not explaining procedures to the patient before implementation.
✅ Correct Approach: Educate and gain patient consent whenever possible.
🚫 Poor Documentation
❌ Failing to record nursing actions and patient response.
✅ Correct Approach: Document all interventions immediately.
🚫 Not Prioritizing Urgent Needs
❌ Addressing minor issues before life-threatening conditions.
✅ Correct Approach: Use Maslow’s Hierarchy of Needs and the ABCDE approach to set priorities.
7. Example of a Complete Nursing Care Implementation
| Component | Details |
|---|---|
| Assessment | “Patient complains of difficulty breathing and wheezing; SpO₂ = 89%.” |
| Nursing Diagnosis | “Ineffective airway clearance related to mucus production as evidenced by dyspnea and abnormal lung sounds.” |
| Goal/Outcome | “Patient’s oxygen saturation will improve to ≥95% within 24 hours of oxygen therapy.” |
| Nursing Interventions | 1) Administer oxygen therapy at 2L/min via nasal cannula. 2) Encourage deep breathing exercises every 2 hours. 3) Monitor lung sounds and oxygen saturation every 4 hours. |
| Implementation Actions | – Administered oxygen therapy at 2L/min. – Encouraged incentive spirometry exercises. – Reassessed respiratory rate and lung sounds every 4 hours. |
| Evaluation | “After 24 hours, SpO₂ improved to 96%. Goal met.” |
✅ Key Takeaway:
The care plan should be adaptable based on the patient’s response and changing condition.
Types of Care: Direct and Indirect Nursing Care.

1. Introduction to Nursing Care
Nursing care is provided in two main forms: Direct care and Indirect care. These two types ensure comprehensive and holistic patient care, addressing both immediate patient needs and supportive functions that facilitate high-quality healthcare.
Definition of Nursing Care
“Nursing care involves the application of clinical knowledge, skills, and judgment to improve patient health, prevent illness, and promote well-being.”
✅ Example:
✔ Direct Care: Administering medications to a patient with fever.
✔ Indirect Care: Sterilizing medical instruments to prevent infection.
2. Importance of Understanding Direct and Indirect Care
✔ Helps nurses prioritize tasks effectively.
✔ Ensures holistic, patient-centered care.
✔ Improves time management and delegation of nursing duties.
✔ Enhances patient safety and healthcare efficiency.
✔ Facilitates teamwork among healthcare professionals.
✅ Example:
A nurse assisting a patient with mobility exercises provides direct care, while a nurse coordinating a discharge plan is engaged in indirect care.
3. Types of Nursing Care
Nursing care is broadly divided into two categories:
| Type of Care | Definition | Example |
|---|---|---|
| 1. Direct Nursing Care | Care provided face-to-face with the patient to improve their health condition. | Administering IV medications, performing wound dressing, assisting with feeding. |
| 2. Indirect Nursing Care | Activities performed away from the patient, but essential for their care. | Documenting patient progress, coordinating with the healthcare team, maintaining infection control procedures. |
4. Direct Nursing Care
Definition of Direct Nursing Care
“Direct care refers to hands-on, face-to-face interactions where the nurse performs procedures, treatments, and assessments directly on the patient.”
Characteristics of Direct Care
✔ Requires physical presence and direct interaction.
✔ Involves therapeutic communication and patient education.
✔ Can be preventive, curative, or rehabilitative.
✔ Provides immediate feedback on the patient’s response.
Examples of Direct Nursing Care
| Category | Examples |
|---|---|
| Physical Care | Taking vital signs, assisting with personal hygiene, inserting a catheter. |
| Procedural Care | Administering injections, starting IV therapy, dressing wounds. |
| Emotional Support | Providing reassurance, counseling, and crisis intervention. |
| Patient Education | Teaching about disease management, medication use, and self-care practices. |
✅ Example:
A nurse changing a post-operative wound dressing is performing direct care.
5. Indirect Nursing Care
Definition of Indirect Nursing Care
“Indirect care includes activities performed away from the patient that contribute to patient care, support healthcare delivery, and improve outcomes.”
Characteristics of Indirect Care
✔ Involves behind-the-scenes activities.
✔ Supports continuity of care and healthcare safety.
✔ Improves healthcare efficiency and teamwork.
✔ Includes administrative and coordination tasks.
Examples of Indirect Nursing Care
| Category | Examples |
|---|---|
| Documentation & Reporting | Updating medical records, writing care plans, recording interventions. |
| Coordination & Communication | Collaborating with doctors, dietitians, physiotherapists, and social workers. |
| Equipment & Environment Maintenance | Ensuring medical equipment is functional, maintaining aseptic conditions. |
| Policy & Safety Management | Following infection control protocols, ensuring patient safety guidelines. |
✅ Example:
A nurse preparing a discharge summary for a patient going home is performing indirect care.
6. Comparison of Direct and Indirect Nursing Care
| Aspect | Direct Nursing Care | Indirect Nursing Care |
|---|---|---|
| Interaction with Patient | Face-to-face, hands-on | Not in direct contact with the patient |
| Purpose | Immediate patient care and treatment | Supporting and coordinating healthcare services |
| Examples | Administering medications, wound care, assisting in mobility | Charting, ordering supplies, discussing patient care in team meetings |
| Impact on Patient | Directly influences health improvement | Supports safe, efficient, and continuous care |
✅ Example:
A nurse assisting a patient with a nebulizer is direct care, while a nurse updating patient care notes in a medical record is indirect care.
7. Importance of Balancing Direct and Indirect Care
✔ Ensures comprehensive, high-quality care.
✔ Prevents burnout by delegating indirect tasks effectively.
✔ Improves patient safety and healthcare system efficiency.
✔ Enhances interdisciplinary collaboration.
✅ Example:
A nurse balancing direct care (administering IV fluids) with indirect care (coordinating patient discharge) ensures effective care delivery.
8. Documentation and Legal Considerations
Proper documentation is essential for both direct and indirect care.
Documentation Guidelines
✔ Record all direct patient interactions, including assessments and interventions.
✔ Log indirect care activities, such as communication with healthcare providers.
✔ Use standardized formats and hospital protocols.
✅ Example:
“March 10, 2025, 10:00 AM: Administered 500mL IV fluids as per physician’s order. BP improved from 88/60 to 110/75 mmHg. Patient tolerated the procedure well.”
9. Common Mistakes in Direct and Indirect Care
🚫 Focusing only on Direct Care
❌ Providing treatments but not documenting them properly.
✅ Correct Approach: Always record interventions and patient response.
🚫 Overlooking Indirect Care Activities
❌ Ignoring infection control protocols or failing to restock essential supplies.
✅ Correct Approach: Prioritize both hands-on care and supportive activities.
🚫 Poor Time Management Between Direct and Indirect Care
❌ Spending too much time on documentation while delaying urgent patient care.
✅ Correct Approach: Balance patient interaction with essential paperwork.
10. Example of a Complete Nursing Care Plan Involving Direct and Indirect Care
| Component | Details |
|---|---|
| Patient Condition | 65-year-old female with pneumonia and difficulty breathing. |
| Direct Nursing Care | ✔ Administer oxygen therapy ✔ Perform chest physiotherapy ✔ Encourage deep breathing exercises |
| Indirect Nursing Care | ✔ Document patient’s progress ✔ Coordinate with a respiratory therapist ✔ Ensure availability of oxygen supplies |
| Outcome | Patient’s SpO₂ improved from 89% to 96% after interventions. |
✅ Key Takeaway:
A combination of direct and indirect care ensures effective treatment and healthcare coordination.
Evaluation in the Nursing Process.

1. Introduction to Evaluation in Nursing
Evaluation is the final step in the nursing process (following Assessment, Diagnosis, Planning, and Implementation). This phase helps nurses determine whether the patient goals and expected outcomes have been achieved and whether the nursing interventions were effective.
Definition of Evaluation in Nursing
“Evaluation is the process of assessing the effectiveness of nursing interventions by comparing actual patient outcomes with expected goals.”
✅ Example:
For a patient with hypertension, if the goal was to maintain a blood pressure below 140/90 mmHg, the nurse evaluates if the BP readings have improved after interventions.
2. Purpose of Evaluation in the Nursing Process
✔ Ensures that nursing care is effective and patient-centered.
✔ Helps in decision-making regarding continuing, modifying, or terminating interventions.
✔ Supports evidence-based practice by measuring patient progress.
✔ Improves patient safety and quality of care.
✔ Facilitates clear documentation and communication within the healthcare team.
✅ Example:
If a patient was receiving pain management interventions, evaluation will determine if the pain score decreased from 8/10 to the goal of ≤3/10.
3. Steps in the Evaluation Process
The evaluation phase follows a structured process to ensure systematic assessment of patient progress.
| Step | Description | Example |
|---|---|---|
| 1. Reassess the Patient | Compare the patient’s current condition with baseline data. | Rechecking blood glucose levels after insulin administration. |
| 2. Compare Actual Outcomes with Expected Goals | Determine if the SMART goals set during planning were achieved. | If the goal was SpO₂ ≥95%, check if oxygen therapy was effective. |
| 3. Identify Factors Affecting Outcomes | Analyze whether internal (patient-related) or external (treatment-related) factors influenced progress. | If pain persists despite analgesics, consider tolerance or ineffective dose. |
| 4. Modify the Care Plan if Needed | Adjust interventions or set new goals if initial plans were ineffective. | If BP remains high, adjust medications and add lifestyle modifications. |
| 5. Document Findings and Communicate with the Healthcare Team | Record evaluation results and share with the healthcare team for coordinated care. | “Patient’s temperature reduced from 102°F to 98.6°F after antipyretic therapy.” |
✅ Example:
A nurse assessing a post-surgical patient’s mobility progress evaluates whether the goal “Patient will walk 10 steps independently within 2 days” was achieved.
4. Types of Evaluation in Nursing
Evaluation can be classified into different types based on timing, focus, and method of assessment.
1. Based on Timing
| Type | Definition | Example |
|---|---|---|
| Ongoing Evaluation | Continuous assessment of the patient’s response during care. | Monitoring pain levels every 2 hours after administering analgesics. |
| Intermittent Evaluation | Performed at specific time intervals during care. | Checking BP readings every morning in hypertensive patients. |
| Terminal Evaluation | Conducted at the time of discharge or after treatment completion. | Assessing functional mobility in a stroke patient before discharge. |
✅ Example:
A nurse monitoring oxygen saturation every 4 hours during pneumonia treatment is performing ongoing evaluation.
2. Based on Focus
| Type | Definition | Example |
|---|---|---|
| Formative Evaluation | Evaluates nursing care in real-time to improve interventions. | Checking pain relief after giving morphine. |
| Summative Evaluation | Conducted after interventions to assess overall effectiveness. | Evaluating weight loss in a patient following a 6-week diet plan. |
✅ Example:
After implementing a low-sodium diet for 1 month, a nurse evaluates blood pressure changes (summative evaluation).
3. Based on Method of Assessment
| Type | Definition | Example |
|---|---|---|
| Objective Evaluation | Uses measurable data (vital signs, lab values) to assess outcomes. | Checking blood glucose levels before and after insulin therapy. |
| Subjective Evaluation | Based on patient-reported symptoms and feelings. | Asking a patient, “On a scale of 0-10, how is your pain now?” |
✅ Example:
A nurse measuring SpO₂ levels after oxygen therapy is conducting objective evaluation, while asking the patient if breathing feels easier is subjective evaluation.
5. Comparison of Expected vs. Actual Outcomes
Once interventions are carried out, the nurse compares expected and actual patient outcomes.
| Expected Outcome | Actual Outcome | Result |
|---|---|---|
| BP will be ≤140/90 mmHg | BP is 136/85 mmHg | Goal met ✅ |
| Patient will rate pain ≤3/10 | Patient reports 5/10 pain | Goal partially met 🔄 |
| Patient will ambulate 50 meters | Patient walked only 20 meters | Goal not met ❌ |
✅ Example:
If a goal was “Patient will have a respiratory rate of 12-20 breaths per minute”, and the actual outcome was 22 breaths per minute, the goal was not fully met, and adjustments are needed.
6. Modifying the Care Plan Based on Evaluation
If a goal is unmet or partially met, the care plan must be adjusted.
✅ Reasons for Modifying the Care Plan
✔ Patient condition changed unexpectedly.
✔ Interventions were ineffective or needed reinforcement.
✔ New complications developed requiring a different approach.
✅ Steps for Revising the Care Plan
- Reassess the patient’s condition and new needs.
- Identify new nursing diagnoses if required.
- Set revised SMART goals based on updated findings.
- Modify interventions for better effectiveness.
- Continue evaluation to track progress.
✅ Example:
If a diabetic patient’s blood sugar remains high despite medication, the nurse may:
✔ Reassess dietary intake and insulin effectiveness.
✔ Modify the care plan to include increased physical activity.
✔ Educate the patient on insulin timing adjustments.
7. Documentation in the Evaluation Phase
Proper documentation is critical for tracking patient progress and ensuring continuity of care.
Key Elements of Evaluation Documentation
✔ Date and time of evaluation.
✔ Patient condition before and after interventions.
✔ Comparison of expected and actual outcomes.
✔ Modifications made to the care plan.
✔ Next steps or follow-up actions.
✅ Example of Documentation:
“March 15, 2025, 10:00 AM: Goal was for the patient’s pain level to reduce to ≤3/10. After administering ibuprofen 400mg, the patient reports a pain score of 2/10. Goal met. No further pain medication required.”
8. Common Mistakes in the Evaluation Process
🚫 Failing to Compare Actual vs. Expected Outcomes
❌ Not assessing whether interventions had the desired effect.
✅ Correct Approach: Always compare results with planned goals.
🚫 Incomplete Documentation
❌ Not recording whether a goal was met or not.
✅ Correct Approach: Clearly document patient response to interventions.
🚫 Not Revising Care Plan When Needed
❌ Continuing ineffective interventions without making adjustments.
✅ Correct Approach: Modify the care plan if outcomes are not achieved.
9. Example of a Complete Nursing Care Plan with Evaluation
| Component | Details |
|---|---|
| Assessment | “Patient reports severe pain (8/10) after surgery.” |
| Nursing Diagnosis | “Acute pain related to surgical incision as evidenced by facial grimacing and verbal reports.” |
| Goal/Expected Outcome | “Patient will report a pain level ≤3/10 within 6 hours of intervention.” |
| Interventions | ✔ Administer prescribed pain medications. ✔ Use cold compress therapy. ✔ Encourage relaxation techniques. |
| Evaluation | “Pain level reduced from 8/10 to 2/10 after 4 hours. Goal met.” |
✅ Key Takeaway:
If a goal is not met, interventions must be adjusted and reassessed.
Evaluation Process in Nursing.
1. Introduction to Evaluation in the Nursing Process
The evaluation phase is the final step in the nursing process, following Assessment, Diagnosis, Planning, and Implementation. It determines whether the nursing interventions were successful in achieving the expected patient outcomes and guides future care decisions.
Definition of Evaluation in Nursing
“Evaluation is the systematic process of assessing the effectiveness of nursing interventions by comparing actual patient outcomes with the expected goals.”
✅ Example:
For a patient with pneumonia, evaluation assesses whether oxygen therapy improved oxygen saturation from 88% to the target of ≥95%.
2. Purpose of Evaluation in Nursing
✔ Ensures patient-centered care by assessing progress.
✔ Determines effectiveness of interventions and identifies needed changes.
✔ Prevents complications by addressing unmet goals.
✔ Improves nursing decision-making through evidence-based practice.
✔ Provides legal and professional documentation of patient care.
✅ Example:
If a hypertension patient’s BP remains high despite medication, evaluation helps in modifying the care plan (e.g., adjusting dosage or adding lifestyle modifications).
3. Steps in the Evaluation Process
The evaluation process consists of a structured approach to assess nursing interventions and patient progress.
| Step | Description | Example |
|---|---|---|
| 1. Reassess the Patient | Compare the patient’s current status with baseline assessment. | Checking blood glucose levels after insulin administration. |
| 2. Compare Actual Outcomes with Expected Goals | Determine if the SMART goals set during planning were met. | If the goal was pain reduction to ≤3/10, check the current pain score. |
| 3. Identify Factors Affecting Outcomes | Analyze whether internal (patient-related) or external (treatment-related) factors influenced results. | If a wound is not healing, consider infection or poor nutrition. |
| 4. Modify the Care Plan if Needed | Adjust interventions if the expected outcome is not achieved or partially met. | If BP remains high, adjust medications or add a low-sodium diet. |
| 5. Document Findings and Communicate with the Healthcare Team | Record evaluation results and share with nurses, doctors, and therapists. | “Patient’s SpO₂ improved from 88% to 96% after oxygen therapy.” |
✅ Example:
A nurse monitoring a post-operative patient’s pain evaluates whether the goal “Pain score ≤3/10 within 6 hours” was achieved.
4. Types of Evaluation in Nursing
Evaluation can be classified into different types based on timing, focus, and method of assessment.
1. Based on Timing
| Type | Definition | Example |
|---|---|---|
| Ongoing Evaluation | Continuous assessment of the patient’s response during care. | Monitoring pain levels every 2 hours after giving analgesics. |
| Intermittent Evaluation | Conducted at specific intervals during care. | Checking BP readings daily in hypertensive patients. |
| Terminal Evaluation | Performed at discharge or after treatment completion. | Assessing functional mobility in a stroke patient before discharge. |
✅ Example:
A nurse monitoring oxygen levels every 4 hours during pneumonia treatment is performing ongoing evaluation.
2. Based on Focus
| Type | Definition | Example |
|---|---|---|
| Formative Evaluation | Real-time assessment to improve interventions. | Checking pain relief after giving morphine. |
| Summative Evaluation | Conducted after interventions to assess overall effectiveness. | Evaluating weight loss in a patient following a 6-week diet plan. |
✅ Example:
After implementing a low-sodium diet for 1 month, a nurse evaluates BP changes (summative evaluation).
3. Based on Method of Assessment
| Type | Definition | Example |
|---|---|---|
| Objective Evaluation | Uses measurable data (vital signs, lab values). | Checking blood glucose before and after insulin. |
| Subjective Evaluation | Based on patient-reported symptoms. | Asking “On a scale of 0-10, how is your pain now?” |
✅ Example:
A nurse measuring SpO₂ levels after oxygen therapy is conducting objective evaluation, while asking the patient if breathing feels easier is subjective evaluation.
5. Comparison of Expected vs. Actual Outcomes
Once interventions are carried out, the nurse compares expected and actual patient outcomes.
| Expected Outcome | Actual Outcome | Result |
|---|---|---|
| BP will be ≤140/90 mmHg | BP is 136/85 mmHg | Goal met ✅ |
| Patient will rate pain ≤3/10 | Patient reports 5/10 pain | Goal partially met 🔄 |
| Patient will ambulate 50 meters | Patient walked only 20 meters | Goal not met ❌ |
✅ Example:
If a goal was “Patient will have a respiratory rate of 12-20 breaths per minute”, and the actual outcome was 22 breaths per minute, the goal was not fully met, and adjustments are needed.
6. Modifying the Care Plan Based on Evaluation
If a goal is unmet or partially met, the care plan must be adjusted.
✅ Reasons for Modifying the Care Plan
✔ Patient condition changed unexpectedly.
✔ Interventions were ineffective or needed reinforcement.
✔ New complications developed requiring a different approach.
✅ Steps for Revising the Care Plan
- Reassess the patient’s condition and new needs.
- Identify new nursing diagnoses if required.
- Set revised SMART goals based on updated findings.
- Modify interventions for better effectiveness.
- Continue evaluation to track progress.
✅ Example:
If a diabetic patient’s blood sugar remains high despite medication, the nurse may:
✔ Reassess dietary intake and insulin effectiveness.
✔ Modify the care plan to include increased physical activity.
✔ Educate the patient on insulin timing adjustments.
7. Documentation in the Evaluation Process
Proper documentation is critical for tracking patient progress and ensuring continuity of care.
Key Elements of Evaluation Documentation
✔ Date and time of evaluation.
✔ Patient condition before and after interventions.
✔ Comparison of expected and actual outcomes.
✔ Modifications made to the care plan.
✔ Next steps or follow-up actions.
✅ Example of Documentation:
“March 15, 2025, 10:00 AM: Goal was for the patient’s pain level to reduce to ≤3/10. After administering ibuprofen 400mg, the patient reports a pain score of 2/10. Goal met. No further pain medication required.”
8. Common Mistakes in the Evaluation Process
🚫 Failing to Compare Actual vs. Expected Outcomes
❌ Not assessing whether interventions had the desired effect.
✅ Correct Approach: Always compare results with planned goals.
🚫 Incomplete Documentation
❌ Not recording whether a goal was met or not.
✅ Correct Approach: Clearly document patient response to interventions.
🚫 Not Revising Care Plan When Needed
❌ Continuing ineffective interventions without making adjustments.
✅ Correct Approach: Modify the care plan if outcomes are not achieved.
Documentation and Reporting in Nursing.
1. Introduction to Documentation and Reporting in Nursing
Documentation and reporting are critical components of the nursing process that ensure accurate communication, legal protection, and continuity of care. Proper documentation helps track patient progress, support clinical decisions, and provide evidence for legal and research purposes.
Definition of Documentation in Nursing
“Documentation is the process of recording all nursing actions, observations, and patient responses in a legal, structured, and standardized manner.”
✅ Example:
A nurse documents that a patient’s temperature reduced from 102°F to 98.6°F after administering an antipyretic.
Definition of Reporting in Nursing
“Reporting is the process of verbally or electronically sharing patient-related information with other healthcare professionals for continuity of care.”
✅ Example:
A nurse in the ICU reports a change in a patient’s vital signs to the incoming shift nurse.
2. Importance of Documentation and Reporting in Nursing
✔ Ensures continuity of care by providing a clear record of treatment.
✔ Promotes patient safety by tracking medical history and interventions.
✔ Supports legal protection by serving as evidence in medical lawsuits.
✔ Improves communication among nurses, doctors, and healthcare teams.
✔ Facilitates research and quality improvement in healthcare.
✔ Enhances accountability by tracking actions performed by healthcare professionals.
✅ Example:
If a patient develops an allergic reaction after receiving a medication, documentation ensures the allergy is flagged for future care.
3. Principles of Effective Nursing Documentation
To maintain high-quality records, documentation should follow the FACTUAL format:
| Principle | Description |
|---|---|
| F – Factual | Use objective data (e.g., “BP 140/90 mmHg,” NOT “Patient looks unwell”). |
| A – Accurate | Avoid errors and record precise times, medications, and interventions. |
| C – Complete | Include all essential details, such as patient response and follow-up actions. |
| T – Timely | Document immediately after an intervention to avoid forgetting details. |
| U – Unbiased | Avoid personal opinions (e.g., “Patient was rude,” instead document “Patient expressed frustration”). |
| A – Avoid assumptions | Do not assume symptoms, document only what you observe. |
| L – Legible & Legal | Ensure readable handwriting or use electronic records correctly. |
✅ Example of Proper Documentation:
“March 10, 2025, 10:00 AM: Administered 500mg acetaminophen orally for fever of 101°F. After 30 minutes, patient’s temperature reduced to 98.6°F. No signs of distress observed.”
4. Types of Nursing Documentation
1. Source-Oriented Records (SOR)
- Records kept separately by each healthcare provider (nurse, doctor, therapist).
- Organized by discipline (e.g., nursing notes, physician notes, lab reports).
✅ Example:
A nurse documents wound care in a nursing progress note, while a physician records medication orders in a physician’s chart
2. Problem-Oriented Medical Records (POMR)
- Organized around a patient’s specific problems rather than disciplines.
- Uses SOAP notes (Subjective, Objective, Assessment, Plan).
✅ Example of SOAP Note:
✔ Subjective: “Patient reports severe headache for 2 days.”
✔ Objective: BP: 150/95 mmHg, HR: 90 bpm.
✔ Assessment: Hypertension with possible migraine.
✔ Plan: Administer antihypertensive and pain reliever, monitor BP.
3. Charting by Exception (CBE)
- Only significant changes in patient condition are documented.
- Assumes normal findings unless stated otherwise.
✅ Example:
✔ Normal: “Lung sounds clear bilaterally.” (Not documented)
✔ Abnormal: “Lung sounds diminished in right lower lobe.” (Documented)
4. Narrative Charting
- Detailed, chronological account of patient care.
- Most traditional and flexible format.
✅ Example:
“Patient admitted with complaints of chest pain. Administered nitroglycerin 0.4mg SL at 9:30 AM. Patient reports pain reduction from 8/10 to 2/10 after 10 minutes. No further complaints noted.”
5. Electronic Health Records (EHR)
- Digital version of a patient’s medical history, accessible to multiple healthcare providers.
- Improves legibility, data accuracy, and security.
✅ Example:
✔ A nurse updates an EHR with vital signs, medication administration, and nursing interventions.
5. Types of Nursing Reports
1. Change-of-Shift Report (Handoff Report)
- Given when a nurse transfers care to another nurse at shift change.
- Includes patient status, recent changes, and upcoming tasks.
✅ Example:
“Patient admitted with pneumonia. Received IV antibiotics at 6 PM. Oxygen saturation stable at 96%. Monitor for fever overnight.”
2. Incident Report
- Documents unexpected events or errors in patient care.
- Used for quality improvement and legal protection.
✅ Example:
“Patient fell while attempting to walk to the bathroom unassisted. No visible injuries. Physician notified, and fall risk measures reinforced.”
3. Telephone Report
- Used to update physicians about urgent patient changes.
- Follow SBAR format (Situation, Background, Assessment, Recommendation).
✅ Example of SBAR Report:
✔ Situation: “Patient’s BP dropped to 80/50 mmHg after medication.”
✔ Background: “Patient has a history of hypotension and received antihypertensives.”
✔ Assessment: “Patient is dizzy and confused.”
✔ Recommendation: “Should we stop the medication and give IV fluids?”
4. Transfer Report
- Used when a patient is transferred to another unit or facility.
- Includes diagnosis, treatments, medications, and pending procedures.
✅ Example:
“Patient transferred to ICU due to worsening respiratory distress. On oxygen therapy 4L/min. BP 110/70, HR 88 bpm, SpO₂ 92%.”
5. Discharge Summary Report
- Documents a patient’s final condition and discharge instructions.
- Includes medications, follow-up appointments, and lifestyle recommendations.
✅ Example:
“Patient discharged in stable condition. Prescribed amoxicillin 500mg BID for 7 days. Advised to follow up in 2 weeks.”
6. Common Mistakes in Documentation and Reporting
🚫 Using Subjective or Judgmental Language
❌ “Patient is non-compliant and lazy.”
✅ Correct Approach: “Patient refused medication and verbalized concerns about side effects.”
🚫 Failure to Document in Real-Time
❌ Documenting interventions hours later, leading to missing details.
✅ Correct Approach: Record all actions immediately after performing them.
🚫 Illegible or Incomplete Entries
❌ “Pt. had meds. Feeling better.”
✅ Correct Approach: “Patient received acetaminophen 500mg PO at 9 AM for headache. Reports pain decreased from 6/10 to 2/10.”
🚫 Failing to Correct Errors Properly
❌ Erasing or using correction fluid.
✅ Correct Approach: Draw a single line through the error, write “error,” and sign your initials.
ADDITIONAL DETAILS.
Pain Scale and Assessment of Pain.
1. Introduction to Pain Assessment
Pain assessment is a critical component of nursing care that helps determine the severity, location, and impact of pain on a patient’s well-being. Proper assessment ensures that appropriate interventions are provided to relieve pain and improve quality of life.
Definition of Pain Assessment
“Pain assessment is the systematic process of evaluating a patient’s pain level, type, and response to treatment using subjective and objective measures.”
✅ Example:
A nurse asks a post-surgical patient to rate their pain on a scale of 0-10 to guide pain management.
2. Importance of Pain Assessment in Nursing
✔ Ensures effective pain management and improves patient comfort.
✔ Prevents complications like chronic pain or anxiety.
✔ Guides treatment decisions (medications, physical therapy, alternative therapies).
✔ Supports legal documentation and ethical care.
✔ Enhances communication between patients, nurses, and healthcare teams.
✅ Example:
A patient with arthritis reports severe pain (9/10), prompting the nurse to administer pain medication and reassess later.
3. Types of Pain
Pain is classified into different types based on origin, duration, and mechanism.
1. Based on Duration
| Type | Definition | Example |
|---|---|---|
| Acute Pain | Sudden onset, short duration, usually due to injury or surgery. | Post-surgical pain, fractures, burns. |
| Chronic Pain | Lasts for more than 3-6 months, often due to a long-term condition. | Arthritis, cancer pain, back pain. |
2. Based on Mechanism
| Type | Definition | Example |
|---|---|---|
| Nociceptive Pain | Pain due to tissue damage or inflammation. | Sprains, burns, surgery. |
| Neuropathic Pain | Pain due to nerve damage or dysfunction. | Diabetic neuropathy, sciatica. |
| Psychogenic Pain | Pain influenced by psychological factors without physical injury. | Depression-related pain, phantom limb pain. |
✅ Example:
A patient with nerve injury experiences burning and tingling sensations (neuropathic pain), requiring different treatment than nociceptive pain from a cut.
4. Pain Scales for Pain Assessment
Pain scales are tools used to quantify pain intensity and help nurses tailor pain management strategies.
1. Numerical Rating Scale (NRS)
- Patients rate pain from 0 to 10.
- 0 = No pain, 10 = Worst possible pain.
- Used for adults and verbal patients.
✅ Example:
A patient reports pain as 7/10, indicating severe pain requiring immediate intervention.
2. Wong-Baker Faces Pain Scale
- Uses six facial expressions to represent pain intensity.
- Best for children (3+ years) or non-verbal patients.
- 0 = No hurt, 10 = Hurts worst.
✅ Example:
A child points to the “crying face” (8/10), prompting the nurse to administer pain relief.
3. Visual Analog Scale (VAS)
- A 10 cm horizontal line where one end represents “No pain” and the other “Worst pain possible.”
- The patient marks a point on the line that corresponds to their pain intensity.
- Used for adults who have difficulty with numbers.
✅ Example:
A post-operative patient marks pain at 6/10, guiding pain management decisions.
4. FLACC Scale (Face, Legs, Activity, Cry, Consolability)
- Used for infants, young children (under 3 years), and non-verbal patients.
- Observes five behaviors (face, legs, activity, crying, consolability).
| Category | 0 Points | 1 Point | 2 Points |
|---|---|---|---|
| Face | No expression | Occasional grimace | Constant frown, clenched jaw |
| Legs | Normal | Uneasy, restless | Kicking, rigid |
| Activity | Normal movement | Squirming, tense | Arched back, jerking |
| Cry | No cry | Whimpers | Loud crying, screaming |
| Consolability | Content, relaxed | Comforted by touch | Difficult to console |
✅ Example:
A crying infant with clenched fists scores 8/10, indicating severe pain needing immediate relief.
5. PAINAD Scale (Pain Assessment in Advanced Dementia)
- Used for patients with dementia who cannot verbally communicate pain.
- Observes breathing, vocalization, facial expression, body language, and consolability.
- Score: 0 (no pain) to 10 (severe pain).
✅ Example:
A dementia patient grimacing, moaning, and restless scores 6/10, requiring pain management.
5. Comprehensive Pain Assessment (PQRST Method)
A detailed pain assessment helps identify characteristics of pain.
| Assessment Factor | Questions to Ask | Example Response |
|---|---|---|
| P – Provocation/Palliation | “What makes the pain better or worse?” | “Pain worsens with movement, but improves with rest.” |
| Q – Quality | “Describe the pain (sharp, dull, burning)?” | “It feels like a stabbing pain.” |
| R – Region/Radiation | “Where is the pain? Does it spread?” | “Pain is in my lower back and shoots down my legs.” |
| S – Severity | “How bad is the pain on a scale of 0-10?” | “It is 7/10 right now.” |
| T – Timing | “When did the pain start? Is it constant?” | “It started after my surgery and is constant.” |
✅ Example:
A post-operative patient reports sharp pain (7/10) that worsens with movement, guiding pain relief measures.
6. Documentation of Pain Assessment
Proper documentation ensures effective pain management and continuity of care.
✔ Time of assessment (Before and after interventions).
✔ Pain score using appropriate scale.
✔ Location and characteristics of pain.
✔ Pain-relief measures taken.
✔ Patient’s response to interventions.
✅ Example of Documentation:
“March 15, 2025, 10:00 AM: Patient reports sharp pain in the right knee, rated 8/10 on NRS. Administered acetaminophen 500mg PO. Pain reassessed after 30 minutes, now 3/10. Patient comfortable.”
7. Pain Management Based on Assessment
Based on the pain assessment, nurses select appropriate interventions.
| Pain Level | Intervention |
|---|---|
| Mild (1-3/10) | Repositioning, relaxation, cold compress. |
| Moderate (4-6/10) | Oral pain medications (acetaminophen, ibuprofen). |
| Severe (7-10/10) | IV pain medications (morphine, opioids), urgent medical intervention. |
✅ Example:
A patient with severe cancer pain (9/10) requires opioid analgesics and palliative care measures.
8. Common Mistakes in Pain Assessment
🚫 Not using the right pain scale
❌ Using a numerical scale for infants or dementia patients.
✅ Correct Approach: Use FLACC for infants, PAINAD for dementia.
🚫 Not reassessing after pain relief measures
❌ Failing to check if pain improved after medication.
✅ Correct Approach: Reassess pain after 30-60 minutes.
🚫 Ignoring non-verbal signs of pain
❌ Assuming a silent patient is pain-free.
✅ Correct Approach: Observe grimacing, restlessness, and guarding behavior.