Research-unit-1-b.sc-sem-5-Research and research Process
Unit 1 Research and research Process
Definition of Research
& nursing research

What is Research?
Research is a systematic, logical, and scientific investigation undertaken to explore new facts, verify existing knowledge, and solve real-world problems. It plays a central role in advancing knowledge across disciplines like health, science, technology, education, and social sciences.
✍️ “Research is formalized curiosity. It is poking and prying with a purpose.”
— Zora Neale Hurston
Definition of Research
Simple Definition
“Research is a systematic and scientific process of inquiry that aims to discover new knowledge, verify existing facts, and solve practical problems through careful observation, investigation, and analysis.”
Academic Definitions
- Creswell (2014): “Research is a process of steps used to collect and analyze information to increase our understanding of a topic or issue.”
- Polit & Beck (2004) – in Nursing Context: “Research is a systematic inquiry that uses disciplined methods to answer questions and solve problems, with the goal of generating new knowledge that is applicable to nursing practice.”
- Oxford Dictionary: “The systematic investigation into and study of materials and sources in order to establish facts and reach new conclusions.”
Key Elements in the Definition
- Systematic: Follows a structured process or methodology
- Objective: Free from personal bias
- Empirical: Based on observed and measurable evidence
- Analytical: Involves data collection, interpretation, and reasoning
- Purposeful: Aims to discover, verify, or solve
In the Context of Nursing
In nursing, research helps in:
- Improving patient care
- Developing clinical protocols
- Enhancing nursing education
- Supporting evidence-based practice
Summary
Research is the heart of scientific advancement and evidence-based practice. A clear understanding of its definition lays the foundation for meaningful inquiry, especially in healthcare and nursing.
Definition of Nursing Research
Simple Definition
“Nursing research is a systematic, scientific process that helps improve nursing care, develop best practices, and contribute to evidence-based healthcare through inquiry, observation, and analysis.”
Standard Definitions
- Polit & Beck (2004): “Nursing research is a systematic inquiry designed to develop knowledge about issues important to nurses, including nursing practice, education, administration, and informatics.”
- International Council of Nurses (ICN): “Nursing research is designed to develop the knowledge base of nursing, to improve nursing practice and patient outcomes.”
- American Nurses Association (ANA): “Nursing research is the development of knowledge about health and the promotion of health over the full lifespan, care of persons with health problems and disabilities, and nursing actions to enhance the ability of individuals to respond effectively to actual or potential health problems.”
Key Features of Nursing Research
- Systematic and scientific approach
- Evidence-based for clinical decision-making
- Focuses on nursing practice, education, and administration
- Aims to improve patient care and outcomes
- Often includes qualitative, quantitative, or mixed methods
Application Areas
| Area | Examples |
|---|---|
| Clinical Practice | Improving wound care, reducing infections |
| Nursing Education | Evaluating teaching methods or simulation |
| Community Health | Assessing health awareness in rural populations |
| Nursing Administration | Studying nurse-patient ratios and burnout |
Summary
Nursing research is a cornerstone of professional nursing practice. It ensures care is scientifically grounded, continuously improved, and responsive to patient needs. Every nurse is both a consumer and contributor of research.
Concept of Research

What is the Concept of Research?
The concept of research refers to the systematic process of investigating, analyzing, and interpreting information to answer questions or solve problems. It involves curiosity, structured inquiry, and the application of scientific methods to generate new knowledge or validate existing information.
✍️ “Research begins with a question and ends with answers based on evidence.”
Core Components of the Research Concept
| Component | Description |
|---|---|
| Purposeful Inquiry | Research is always goal-oriented, not random |
| Systematic Process | Follows organized steps like planning, data collection, analysis |
| Evidence-Based | Based on observations, experiments, or surveys |
| Scientific Method | Uses logical and objective techniques |
| Knowledge Expansion | Leads to new insights, improvements, and innovations |
Key Objectives of Research
- To explore unknown areas or phenomena
- To describe facts or current situations
- To explain relationships between variables
- To predict future outcomes or behaviors
- To control or influence variables and outcomes
In Nursing Context
In nursing, research helps:
- Improve patient outcomes
- Enhance nursing practice and education
- Guide policy-making and health planning
- Promote professional development and critical thinking
Types of Research Based on Purpose
| Type | Focus |
|---|---|
| Basic Research | Expands general knowledge (theoretical) |
| Applied Research | Solves practical problems in clinical settings |
| Action Research | Immediate improvement in local practice |
| Clinical Research | Involves patient-centered investigations |
Summary
The concept of research forms the foundation of scientific inquiry and innovation. In nursing, understanding this concept empowers professionals to ask questions, find answers, and apply findings to provide safe, evidence-based, and high-quality care.
Commonly Used Terms in Research (With Nursing Examples)
A. General Research Terms
Research
A scientific and systematic inquiry into a problem to generate new knowledge or verify existing facts.
Scientific Method
A step-by-step logical approach to research including observation, hypothesis formulation, testing, and conclusion.
Research Problem
A specific issue or gap that the researcher intends to address.
✅ Example: High incidence of pressure ulcers in ICU patients.
Statement of the Problem
A concise description of the problem to be studied, forming the foundation of the research.
Aim/Purpose
Broad direction or intention of the study.
✅ To improve postnatal care practices among rural mothers.
Objectives
Specific, measurable goals that the study seeks to achieve.
Research Question
A clear, focused, and researchable question that guides the study.
✅ What is the effectiveness of handwashing on infection control?
Hypothesis
A tentative prediction or explanation of the relationship between variables.
✅ There is a significant difference in knowledge before and after health education.
B. Variables and Related Concepts
Variable
Any characteristic that can vary or change during research.
| Type | Meaning | Example |
|---|---|---|
| Independent | Cause or intervention | Health teaching |
| Dependent | Effect or outcome | Knowledge level |
| Controlled | Kept constant to avoid influence | Time, environment |
| Extraneous | External factors that may interfere | Family influence |
Operational Definition
How the researcher defines and measures a concept in the study.
✅ “Knowledge” may be operationalized by a structured questionnaire score.
C. Population and Sampling Terms
Population
The complete group under study.
✅ All antenatal mothers attending a PHC.
Target Population
The entire group to whom the researcher wishes to generalize results.
Accessible Population
The portion of the target population available for data collection.
Sample
A subset of the population selected for study.
✅ 60 adolescent girls from XYZ school.
Sampling
The process of selecting the sample from the population.
Sampling Frame
A list of all individuals in the population eligible for the study.
Sampling Technique
The method used to select the sample.
| Type | Example |
|---|---|
| Random Sampling | Lottery method |
| Stratified Sampling | Dividing population into subgroups |
| Purposive Sampling | Selecting based on purpose |
| Convenience Sampling | Selecting those available easily |
D. Research Design and Methodology
Research Design
The blueprint or overall plan of the research process.
| Type | Examples |
|---|---|
| Descriptive | Surveys, observational studies |
| Experimental | Randomized controlled trials |
| Quasi-Experimental | Pre-test/post-test without randomization |
| Qualitative | Focus group discussion, phenomenology |
Tool/Instrument
The device used to collect data (e.g., questionnaire, checklist, rating scale).
Validity
The extent to which a tool measures what it is intended to measure.
Reliability
The consistency and stability of a measuring tool over time.
Pilot Study
A small-scale preliminary trial to test the feasibility and reliability of tools/methods.
Ethical Considerations
Protecting participants’ rights: consent, confidentiality, autonomy, non-maleficence.
E. Data Collection and Analysis
Data
Facts or information collected for analysis.
| Type | Example |
|---|---|
| Primary Data | Data collected by the researcher (survey, interview) |
| Secondary Data | Already available (records, literature) |
Data Collection Methods
- Observation
- Interview
- Questionnaire
- Document analysis
Data Analysis
Processing and interpreting collected data using statistical or thematic methods.
Descriptive Statistics
Summarizes data: Mean, Median, Mode, SD, Frequency.
Inferential Statistics
Generalizes data and tests hypotheses: t-test, Chi-square, ANOVA.
Statistical Significance
Indicates the probability that results are due to chance (p-value < 0.05 = significant).
F. Reporting and Dissemination
Research Report
A formal document describing the research process and findings.
Abstract
A brief summary of the study, usually 250–300 words.
Discussion
Interpretation and explanation of results in light of objectives and literature.
Conclusion
Final thoughts and implications of the study.
Recommendation
Suggestions for practice, policy, or further research.
Reference
Proper citation of all sources used, commonly in APA format.
Appendix
Supplementary materials like tools, consent forms, ethical approval letters.
Plagiarism
Copying others’ work without proper credit — a serious ethical violation.
Evidence-Based Practice (EBP)
Using current best evidence to guide nursing care and decisions.
Peer Review
Evaluation of a research paper by experts before publication.
Dissemination
Sharing research findings through presentations, journals, or community programs.
Summary
Understanding these research terms is essential for every nurse and student involved in research. It helps in conceptual clarity, quality writing, viva preparation, and ensures scientific integrity throughout the research process.
Need and Areas of Research in Nursing

This content is ideal for academic writing, thesis, presentations, or viva preparation.
Need for Research in Nursing
Nursing is an evolving, evidence-driven profession. With advancing technology, complex patient needs, and increasing focus on quality care, nursing research is essential to:
1. Improve Patient Care
- Research helps identify the most effective nursing interventions.
- It leads to development of new techniques, protocols, and tools for patient safety and comfort.
2. Promote Evidence-Based Practice (EBP)
- Encourages nurses to base their decisions on scientific evidence, not just tradition or intuition.
- Strengthens the credibility and professionalism of nursing care.
3. Develop and Refine Nursing Knowledge
- Contributes to the growth of nursing theories and conceptual frameworks.
- Bridges the gap between theory and clinical practice.
4. Solve Clinical and Community Health Problems
- Provides solutions to real-world issues like infection control, maternal health, chronic disease management, etc.
5. Improve Nursing Education
- Enhances teaching methods, curriculum development, and assessment strategies.
- Research in education ensures that nursing students receive quality training.
6. Guide Health Policy and Administration
- Informs health administrators and policymakers for better staffing models, resource allocation, and protocol development.
7. Promote Professional Development
- Encourages critical thinking, leadership, and continuous learning.
- Prepares nurses for roles such as researcher, educator, consultant, and policymaker.
Areas of Research in Nursing
Nursing research can be conducted in various domains, broadly categorized as follows:
1. Clinical Nursing Practice
Research focused on improving bedside care, procedures, and outcomes.
Examples:
- Pain management in post-operative patients
- Prevention of pressure ulcers
- Infection control in ICUs
2. Nursing Education
Focuses on developing and evaluating teaching strategies, curricula, and student learning.
Examples:
- Effectiveness of simulation-based learning
- Online vs. classroom teaching
- Stress and coping among nursing students
3. Community Health Nursing
Addresses health needs of individuals, families, and communities.
Examples:
- Impact of health education on malaria prevention
- Awareness on reproductive health among adolescents
- Nutritional status of under-five children
4. Mental Health Nursing
Explores care practices and interventions in psychiatric settings.
Examples:
- Coping strategies of caregivers of schizophrenia patients
- Effect of counseling on anxiety among nursing students
5. Nursing Administration and Management
Research related to workload, leadership, staffing, and decision-making in nursing.
Example:
- Job satisfaction of nurses
- Effectiveness of team-based care
- Nurse-patient ratio and quality of care
6. Maternal and Child Health Nursing
Enhancing care during pregnancy, childbirth, and early childhood.
Examples:
- Safe motherhood practices
- Effectiveness of breastfeeding counseling
- Kangaroo mother care in preterm infants
7. Medical-Surgical Nursing
Focused on surgical and medical patient care across systems.
Examples:
- Fluid and electrolyte management
- Pre- and post-operative nursing care effectiveness
8. Evidence-Based Practice & Quality Improvement
Integration of best evidence into routine practice.
Examples:
- Comparing outcomes using standard vs. non-standard protocols
- Auditing clinical practices
9. Nursing Informatics
Application of technology and data management in nursing.
Examples:
- Use of electronic health records
- Impact of mobile apps in patient education
Summary
Nursing research is not optional—it is essential. It empowers nurses to become change-makers by advancing knowledge, solving problems, improving care, and contributing to the overall health system. The scope of research in nursing is broad, covering clinical, educational, community, and administrative domains.
Steps of the Scientific Method in Nursing Research
What is the Scientific Method?
The scientific method is a systematic, objective, and evidence-driven process used by researchers to investigate phenomena, test hypotheses, and arrive at conclusions. In nursing, it provides a foundation for evidence-based practice, clinical decision-making, and improving patient outcomes.
✍️ “The scientific method transforms observation into evidence and evidence into action.”
Key Characteristics of the Scientific Method
- Systematic – Follows an ordered sequence of steps
- Empirical – Based on observed and measurable data
- Logical – Rooted in reasoning and critical thinking
- Replicable – Can be repeated and verified
- Evidence-based – Ensures valid, reliable outcomes
Detailed Steps of the Scientific Method
Observation / Identification of a Problem
- The first step begins with noticing a clinical issue or knowledge gap.
- Based on personal experience, literature, or patient feedback.
✅ Nursing Example: Increased rate of urinary tract infections (UTIs) in catheterized patients.
Formulation of the Research Problem / Question
- Convert the observation into a specific, focused, and researchable question.
- Must include population, intervention, comparison, and outcome (PICO format).
✅ Example:
Does using a closed urinary drainage system reduce the incidence of UTIs compared to an open system in catheterized patients?
Review of Literature
- Conduct a thorough analysis of existing research, theories, and evidence.
- Helps refine the problem, avoid duplication, and identify gaps.
✅ Sources:
PubMed, CINAHL, Scopus, Google Scholar, Nursing Journals.
Developing Hypothesis (if applicable)
- A hypothesis is a tentative, testable prediction that establishes a relationship between variables.
✅ Types of Hypotheses:
- Null Hypothesis (H₀): No relationship exists.
- Alternative Hypothesis (H₁): A relationship or effect exists.
✅ Example:
H₁: Closed drainage system significantly reduces UTI incidence.
H₀: There is no difference between the systems.
Research Design / Planning the Study
- This involves selecting an appropriate research approach (qualitative, quantitative, or mixed method) and design (descriptive, experimental, etc.)
✅ Includes:
- Selection of population and sample
- Sampling technique
- Research setting
- Data collection tools and timeline
- Budget and resources
- Ethical considerations and approvals
✅ Nursing Example:
Using a quasi-experimental design to assess effectiveness of health education on anemia prevention.
Data Collection
- Gathering information using reliable and valid tools like:
- Questionnaires
- Checklists
- Observation schedules
- Interviews
- Lab tests or patient records
✅ Tips:
- Ensure informed consent
- Maintain confidentiality and standardization
- Follow strict ethical protocols
Data Analysis
- Applying statistical or qualitative techniques to analyze collected data.
- Helps in identifying patterns, trends, and relationships.
✅ Quantitative Tools:
- Mean, Median, Standard Deviation
- t-test, Chi-square, ANOVA
✅ Qualitative Tools: - Thematic analysis, coding, content analysis
✅ Software: SPSS, Excel, R, NVivo
Interpretation of Results
- Go beyond numbers — assign meaning to the findings.
- Compare results with objectives, hypotheses, and literature.
✅ Interpretation Includes:
- Significance of findings
- Explanation of trends or patterns
- Addressing limitations
- Discussing implications for nursing practice
Conclusion and Recommendations
- Summarize the major findings in relation to research objectives.
- Provide practical recommendations for nursing education, clinical practice, administration, or further research.
✅ Example:
“The teaching program significantly improved adolescent girls’ knowledge about menstrual hygiene. It is recommended to include such sessions in school health programs.”
Dissemination of Research Findings
- Sharing results with the academic, clinical, and policy-making communities.
✅ Modes of Dissemination:
- Research report
- Journal article
- Conference presentation
- Poster or infographic
- Staff workshops
Scientific Method in Action – A Nursing Example
Scenario:
Nurses observe frequent falls among elderly in a hospital ward.
| Step | Action |
|---|---|
| Observation | Frequent patient falls reported |
| Problem | What are the risk factors contributing to falls? |
| Literature Review | Studies on fall risk, prevention strategies |
| Hypothesis | Increased staffing reduces fall rates |
| Design | Observational study |
| Data Collection | Fall incidents before and after intervention |
| Analysis | Compare rates using t-test |
| Interpretation | Staffing levels impact patient safety |
| Conclusion | Suggest staff-to-patient ratio improvement |
| Dissemination | Submit findings to hospital admin and publish |
Summary
The scientific method provides a rigorous and trustworthy pathway for nurses to explore problems, develop knowledge, and improve care. It ensures that nursing practices are rational, evidence-based, and outcome-oriented.
Steps of the Research Process
The research process is a structured sequence of steps that guide the researcher from identifying a problem to reporting results.
1. Identifying and Defining the Research Problem
This is the foundation of the entire research process.
- Clearly recognize a real-life problem or knowledge gap in the field.
- Frame it as a problem statement.
Example (Nursing):
High rates of medication errors among new staff nurses.
2. Reviewing the Literature
A comprehensive review of existing research, theories, and published data.
- Helps understand what is already known.
- Identifies gaps in knowledge.
- Helps refine research questions and methodology.
Sources: PubMed, CINAHL, textbooks, journals.
3. Formulating the Research Objectives / Hypotheses
Define what the study aims to achieve.
- Objectives: Specific, measurable goals
- Hypothesis: Testable statement predicting the outcome
Example:
To assess the effectiveness of a structured teaching program on breastfeeding techniques among new mothers.
4. Selecting the Research Design and Methodology
Choose how the study will be carried out.
- Research Approach: Quantitative, Qualitative, or Mixed
- Design: Experimental, Descriptive, Exploratory, etc.
- Variables: Independent, Dependent, Control
Example:
Quasi-experimental one-group pre-test post-test design.
5. Defining the Population and Sampling
Identify whom the study will involve.
- Population: All individuals relevant to the study
- Sample: A portion selected from the population
- Sampling Method: Random, Purposive, Convenience, etc.
- Sample Size: Determined statistically or based on feasibility
Example:
60 antenatal mothers selected using purposive sampling.
6. Developing the Research Tools / Instruments
Choose or create the tools to collect data.
- Examples: Questionnaires, checklists, rating scales, interview schedules
- Ensure validity (accuracy) and reliability (consistency)
Example:
Structured knowledge questionnaire on hand hygiene.
7. Pilot Study
A small-scale version of the study to test feasibility.
- Helps detect flaws in tools, methods, and time planning
- Allows revision before actual data collection
8. Collecting Data
The core of research—gathering information from participants.
- Use the chosen tools to collect data ethically and consistently
- Ensure informed consent, privacy, and non-bias
Methods: Observation, interview, self-report, record review
9. Organizing, Analyzing, and Interpreting Data
Convert raw data into meaningful results.
- Organize using charts, tables
- Analyze using statistical software (SPSS, Excel)
- Interpret: What do the numbers mean in relation to the objectives?
Example:
Mean post-test score increased significantly (p < 0.001), indicating effectiveness of the intervention.
10. Drawing Conclusions and Making Recommendations
Summarize findings and relate them to the objectives and hypothesis.
- Highlight major insights
- Provide suggestions for clinical practice, education, or policy
11. Writing the Research Report
A formal written presentation of the research process and findings.
- Follow standard chapters:
Introduction → Review → Methodology → Results → Discussion → Conclusion
12. Dissemination of Findings
Sharing your research with others to create impact.
- Present at seminars, workshops, or conferences
- Publish in journals or bulletins
- Implement findings in clinical practice or nursing education
Summary Table: Research Process Steps
| Step | Description |
|---|---|
| 1 | Identify the problem |
| 2 | Review literature |
| 3 | Set objectives/hypotheses |
| 4 | Choose research design |
| 5 | Select population and sample |
| 6 | Develop tools |
| 7 | Conduct pilot study |
| 8 | Collect data |
| 9 | Analyze and interpret data |
| 10 | Draw conclusions and recommendations |
| 11 | Write report |
| 12 | Disseminate finding |
Summary
The research process is a systematic journey from identifying a problem to implementing evidence-based solutions. For nurses, it empowers them to improve care, innovate, and advocate for best practices through scientific inquiry.
Characteristics of Good Research
Perfect for nursing students, research presentations, assignments, or thesis writing.
Definition of Good Research
Good research is a systematic, objective, ethical, and logical process that leads to reliable, valid, and generalizable results, contributing to knowledge and practical improvements, especially in health and nursing care.
✍️ “Good research doesn’t just answer a question—it ensures the answer is trustworthy and useful.”
Key Characteristics of Good Research
Systematic
- Follows a step-by-step process: problem → objectives → methodology → analysis → conclusions.
- Ensures structure and clarity in the research process.
✅ Example: Clearly defined steps from planning to data interpretation.
Logical
- Based on sound reasoning and scientific logic.
- Conclusions are drawn from the evidence, not assumptions.
✅ Example: Using statistical significance to support findings.
Empirical
- Based on real-world observations or data.
- Not just theoretical—it relies on measurable facts.
✅ Example: Survey results, clinical measurements, or lab data.
Objective and Unbiased
- Free from personal opinions, emotions, or researcher bias.
- Factual, neutral, and evidence-driven.
✅ Example: Using blinded assessments or standardized tools.
Replicable / Verifiable
- The study can be repeated with similar results.
- Others can verify findings by following the same method.
✅ Example: Publishing detailed methodology for reproducibility.
Relevant and Significant
- Addresses current problems or gaps in practice.
- Has practical implications in clinical, educational, or administrative settings.
✅ Example: Studying hand hygiene compliance to reduce infections.
Ethical
- Protects the rights, dignity, and confidentiality of participants.
- Follows ethical guidelines like informed consent, autonomy, beneficence.
✅ Example: Approval from Institutional Ethics Committee.
Evidence-Based
- Builds upon or contributes to existing scientific knowledge.
- Supports evidence-based nursing practice.
✅ Example: Findings help revise clinical care protocols.
Accurate and Precise
- Data collection, analysis, and reporting must be free from errors.
- Measurements are consistent and valid.
✅ Example: Use of calibrated tools and validated questionnaires.
Generalizable
- The findings can be applied to other populations or settings.
- Increases the usefulness and scope of the research.
✅ Example: A study on nursing burnout applicable to multiple hospitals.
Innovative / Creative
- Offers new ideas, approaches, or improvements in care.
- Encourages original thinking and problem-solving.
✅ Example: Using gamification to teach nursing students.
Well-Documented
- Research process and findings are clearly recorded for review and dissemination.
- Includes proper referencing and citation.
✅ Example: APA-style bibliography, detailed appendices.
Summary
Good research is more than data collection — it is methodical, ethical, relevant, and applicable. For nurses, good research forms the backbone of safe, effective, and patient-centered care.
Evidence-Based Practice (EBP)
Definition of Evidence-Based Practice (EBP)
Evidence-Based Practice (EBP) is the conscientious, explicit, and judicious use of the best current evidence, combined with clinical expertise and patient preferences, to guide decision-making in healthcare.
✍️ “EBP integrates the best research with clinical expertise and patient values for optimum care.” — Sackett et al.
Key Elements of EBP
EBP is based on a three-part framework:
| Component | Description |
|---|---|
| Best Research Evidence | From systematic research, RCTs, reviews, clinical studies |
| Clinical Expertise | Skills and experience of the healthcare provider |
| Patient Preferences and Values | Respecting choices, needs, and culture of the individual |
Goal of EBP
- To improve patient outcomes
- To provide high-quality, cost-effective care
- To reduce variation in clinical practice
- To update nursing knowledge and practice
- To ensure safe and ethical healthcare delivery
Characteristics of EBP
- Systematic and scientific
- Patient-centered
- Collaborative (team-based approach)
- Dynamic (evolves with new evidence)
- Ethical and transparent
- Improves care quality, safety, and satisfaction
Relevance of EBP in Nursing
EBP helps nurses:
- Make informed clinical decisions
- Standardize care using clinical guidelines and protocols
- Reduce medical errors and complications
- Educate patients with up-to-date information
- Promote critical thinking and autonomy
- Build professional credibility and accountability
Examples of EBP in Nursing
| Clinical Area | EBP Practice |
|---|---|
| Wound Care | Using hydrocolloid dressings for pressure ulcers |
| Infection Control | Alcohol-based hand rubs to reduce hospital-acquired infections |
| Patient Education | Tailored teaching strategies based on literacy levels |
| Pain Management | Non-pharmacological methods like guided imagery and positioning |
Summary
Evidence-Based Practice is not just a concept — it is a standard of modern nursing care. By blending research, experience, and patient needs, EBP ensures that nursing interventions are safe, effective, and ethical. Every nurse should be an active participant in the EBP process to promote quality care and continuous improvement.
Meaning of Evidence-Based Practice (EBP)
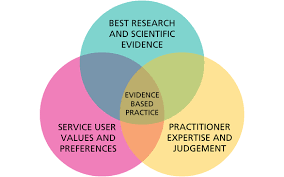
Meaning
Evidence-Based Practice (EBP) refers to the process of making clinical decisions based on a combination of the best available scientific evidence, professional expertise, and patient values.
It ensures that healthcare interventions are:
- Scientifically proven,
- Clinically appropriate, and
- Aligned with individual patient preferences.
In Simple Terms:
EBP = Best Evidence + Clinical Expertise + Patient Values
This means nurses and healthcare professionals do not rely solely on tradition or routine, but use up-to-date research findings and individual judgment, while also respecting patients’ choices and cultural beliefs.
Why It Matters
- Provides safe, effective, and high-quality care
- Promotes critical thinking in clinical practice
- Helps standardize care based on proven outcomes
- Reduces errors and unnecessary interventions
Purposes of Evidence-Based Practice (EBP)
1. To Improve Patient Outcomes
- Ensures that patients receive the most effective, up-to-date, and safe care.
- Reduces complications, errors, and hospital stay duration.
2. To Promote Quality and Safety in Healthcare
- Establishes standardized protocols based on research.
- Minimizes variations in care delivery across settings or practitioners.
3. To Support Clinical Decision-Making
- Helps nurses and healthcare professionals make informed and confident decisions.
- Reduces reliance on outdated practices or personal bias.
4. To Integrate Best Research Evidence into Practice
- Encourages the use of scientific findings rather than tradition or routine.
- Keeps practice aligned with current advancements in nursing and medicine.
5. To Enhance Cost-Effective Care
- Reduces unnecessary tests and treatments.
- Prevents errors, readmissions, and wastage of resources.
6. To Promote Professional Accountability
- Encourages nurses to justify their actions with credible evidence.
- Builds trust and credibility with patients, families, and interdisciplinary teams.
7. To Encourage Lifelong Learning
- Fosters a culture of continuous improvement and critical thinking.
- Motivates nurses to stay updated with the latest research and innovations.
8. To Influence Health Policy and Practice Guidelines
- EBP contributes to the development of evidence-based policies, standards, and procedures at institutional, national, or global levels.
The primary purpose of EBP is to bridge the gap between research and clinical practice, ensuring that every patient receives care that is backed by the best available evidence, is cost-effective, and tailored to their needs.
Steps of the Evidence-Based Practice (EBP) Process
“EBP is not just about reading research—it’s about applying it to care, step by step.”
The EBP process follows a structured approach to integrate best evidence into clinical decision-making.
Ask a Clinical Question (Formulate a Clear Question)
- Identify a problem or area of uncertainty in patient care.
- Use the PICO format to frame the question:
| P | Patient/Problem – Who is the patient population? |
|---|---|
| I | Intervention – What is the proposed intervention? |
| C | Comparison – Is there an alternative to compare? |
| O | Outcome – What result are you looking for? |
✅ Example:
In elderly patients (P), does regular repositioning (I) compared to no schedule (C) reduce pressure ulcers (O)?
Acquire the Best Evidence (Search for Evidence)
- Search for current, credible, and relevant literature.
- Use databases like:
- PubMed
- CINAHL
- Cochrane Library
- Google Scholar
- Scopus
✅ Include: Systematic reviews, meta-analyses, RCTs, clinical practice guidelines.
Appraise the Evidence Critically
- Evaluate the quality, validity, and applicability of the evidence.
- Ask:
- Is the study well-designed?
- Are the results reliable?
- Are they relevant to your clinical setting?
✅ Look for bias, sample size, strength of evidence, and p-values.
Apply the Evidence to Clinical Practice
- Integrate the evidence with:
- Clinical expertise
- Patient preferences
- Resources available in the healthcare setting
✅ Modify care plans or interventions accordingly.
✅ Example: Use evidence-based wound dressing protocol for diabetic foot care.
Evaluate the Outcomes
- Assess whether the application of evidence has led to improvement in patient outcomes.
- Ask:
- Were the goals achieved?
- Is the new practice more effective?
- Were there any side effects or challenges?
✅ Collect data using feedback forms, clinical indicators, or patient satisfaction surveys.
Share the Results (Dissemination)
- Communicate outcomes with peers, team members, and administrators.
- Share via:
- Case presentations
- Journal articles
- Staff workshops
- Posters or conferences
✅ Encourages a culture of learning and continuous improvement.
Summary Table: EBP Process
| Step | Description |
|---|---|
| 1. Ask | Formulate a clinical question (PICO format) |
| 2. Acquire | Search for the best evidence |
| 3. Appraise | Critically evaluate the evidence |
| 4. Apply | Integrate evidence with practice and patient preferences |
| 5. Assess | Evaluate the outcomes and effectiveness |
| 6. Share | Disseminate the results for broader application |
Why Nurses Should Follow the EBP Process
- Improves patient care and safety
- Supports clinical decision-making
- Keeps practice up-to-date and ethical
- Builds professional accountability
Barriers to Evidence-Based Practice (EBP)
“Despite its benefits, EBP is not always easy to implement. Various factors can hinder its application in real-life nursing settings.”
What are Barriers to EBP?
Barriers to EBP are obstacles or challenges that prevent healthcare professionals from searching for, interpreting, or applying research evidence in clinical decision-making.
They can occur at:
- The individual level (nurse or provider)
- The organizational level (institution or system)
- The external level (access to resources or research)
A. Individual-Level Barriers
These are related to knowledge, skills, or attitudes of nurses and health professionals:
| Barrier | Description |
|---|---|
| Lack of EBP Knowledge | Nurses may not be trained in research or critical appraisal. |
| Limited Research Skills | Difficulty in reading, interpreting, or applying findings. |
| Negative Attitudes | Belief that research is not practical or necessary. |
| Time Constraints | Heavy workload leaves no time to read or implement evidence. |
| Fear of Change | Hesitation to move away from traditional practices. |
B. Organizational-Level Barriers
These stem from the work environment, leadership, and resources:
| Barrier | Description |
|---|---|
| Lack of Administrative Support | No encouragement from managers or supervisors to use EBP. |
| Insufficient Staffing | Low nurse-patient ratios make EBP implementation difficult. |
| Limited Access to Resources | No access to journals, databases, or library support. |
| No EBP Culture | The workplace may not value research or continuous learning. |
| Poor Communication | Lack of collaboration or sharing of findings among staff. |
C. External Barriers
These include policy and system-level issues:
| Barrier | Description |
|---|---|
| Paywalls for Journals | Research articles are often not freely available. |
| Language or Technical Barriers | Research papers may be hard to understand. |
| Outdated Guidelines | Practice protocols may not reflect current evidence. |
| Lack of Time to Conduct Research | Especially for nurse educators or clinicians. |
Examples in Nursing Context
- A staff nurse wants to implement a new wound dressing technique, but:
- Her supervisor prefers traditional methods.
- She doesn’t have access to journals.
- The ward is short-staffed.
→ Result: The new practice is not adopted, even though it’s evidence-based.
Why It’s Important to Address These Barriers
- To ensure patient care is safe, effective, and updated
- To encourage a culture of lifelong learning among nurses
- To reduce errors and variations in practice
- To empower nurses as change agents and leaders
Summary
Barriers to EBP are real and common, but they can be overcome with:
- Training & education
- Supportive leadership
- Easy access to resources
- Collaborative teamwork
- Time allocation for research activities
Every nurse plays a vital role in overcoming these barriers and promoting a culture of evidence-based care.