NML-UNIT-3-SEM-5-B.SC-Planning nursing services
Planning nursing services
Planning Nursing Services: Vision and Mission
Effective planning in nursing services ensures the delivery of high-quality, patient-centered care that aligns with healthcare goals, organizational values, and evidence-based practices. A well-defined vision and mission serve as the foundation for nursing service planning, guiding professional nursing practice, resource allocation, and decision-making.
1. Vision Statement in Nursing Services
A vision statement describes the aspirational future of nursing services, providing a clear direction for long-term growth and excellence. It reflects what the nursing organization or department strives to achieve in terms of quality care, professional development, and patient satisfaction.
Characteristics of a Strong Vision Statement
- Future-Oriented: Defines long-term goals and objectives for nursing services.
- Inspiring and Motivational: Encourages nursing staff to strive for excellence in patient care.
- Patient-Centered: Focuses on ensuring compassionate, safe, and high-quality care.
- Broad Yet Specific: Provides a clear roadmap without being overly detailed.
- Reflects Professional Values: Includes aspects like ethics, evidence-based practice, teamwork, and leadership.
Examples of Nursing Vision Statements
- “To be a globally recognized leader in compassionate, innovative, and evidence-based nursing care that enhances the well-being of individuals and communities.”
- “To create an inclusive, patient-centered healthcare system where nurses provide exceptional, culturally competent care, ensuring positive health outcomes for all.“
- “To foster a professional nursing environment that prioritizes continuous learning, clinical excellence, and holistic patient care.“
Significance of a Vision Statement in Nursing Services
- Provides a clear long-term direction for nursing professionals.
- Enhances motivation by setting high standards for patient care.
- Influences policy and strategic decisions in healthcare settings.
- Helps in aligning nursing objectives with national and global healthcare trends.
- Attracts and retains skilled nursing professionals by defining a strong organizational identity.
2. Mission Statement in Nursing Services
A mission statement defines the core purpose and responsibilities of nursing services. It highlights what the nursing unit does, who it serves, and how it delivers care while reflecting professional values and ethical principles.
Characteristics of a Strong Mission Statement
- Clearly Defines the Purpose: Explains the role of nursing services in the healthcare system.
- Action-Oriented: Describes how nurses will achieve their goals through professional practice.
- Short and Concise: Easily understood by healthcare providers and the community.
- Emphasizes Core Values: Includes principles such as ethics, patient safety, and evidence-based care.
- Inclusive and Holistic: Reflects care for diverse populations and settings.
Examples of Nursing Mission Statements
- “To provide high-quality, patient-centered, and evidence-based nursing care that enhances health outcomes and promotes patient safety.”
- “To foster an environment of continuous learning, research, and professional growth to empower nurses in delivering compassionate and holistic healthcare.”
- “To ensure equitable and culturally competent nursing care, improving the health and well-being of individuals, families, and communities.”
Significance of a Mission Statement in Nursing Services
- Guides daily operations and patient care strategies.
- Ensures consistency in nursing practices across different healthcare settings.
- Helps in setting priorities for resource allocation and professional development.
- Aligns nursing services with healthcare policies and accreditation standards.
- Encourages accountability among nursing professionals.
3. Difference Between Vision and Mission Statements
| Aspect | Vision Statement | Mission Statement |
|---|---|---|
| Definition | Defines the long-term aspirations of nursing services. | Describes the present purpose and core functions of nursing services. |
| Timeframe | Future-oriented (5–10 years or more). | Short-term to medium-term (daily to annual goals). |
| Focus | Defines what the nursing organization aspires to become. | Specifies how the organization provides services and care. |
| Scope | Broad and overarching. | Specific and action-driven. |
| Purpose | Motivates and inspires nursing professionals. | Provides a concrete action plan for achieving goals. |
| Example | “To be a global leader in nursing excellence and innovation.” | “To provide compassionate, evidence-based care that improves patient outcomes.” |
4. Importance of Vision and Mission in Nursing Service Planning
A well-defined vision and mission ensure that nursing services operate efficiently, ethically, and in alignment with healthcare goals and patient needs. They provide a structured framework for decision-making, staff engagement, and service delivery.
How Vision and Mission Impact Nursing Service Planning
1. Provides Strategic Direction
- Helps healthcare administrators and nursing leaders establish long-term goals for patient care.
- Guides decision-making regarding staffing, training, resource allocation, and quality improvement initiatives.
2. Ensures Consistency in Nursing Practice
- Establishes clear standards for patient care across different departments and settings.
- Helps in creating standard operating procedures (SOPs) for clinical and administrative tasks.
3. Supports Evidence-Based Practice (EBP)
- Encourages nurses to follow scientifically proven methods for diagnosis, treatment, and patient education.
- Ensures that care is delivered according to the latest medical advancements and nursing research.
4. Enhances Patient Safety and Quality of Care
- Promotes a patient-centered approach, ensuring safety, dignity, and high-quality care.
- Encourages continuous professional development for nursing staff to improve competency.
5. Improves Resource Management
- Helps in planning budget allocation, procurement of medical equipment, and workforce planning.
- Ensures optimal staffing levels to meet patient care needs efficiently.
6. Encourages Accountability and Ethical Practice
- Defines the moral and ethical responsibilities of nurses in various settings.
- Encourages compliance with legal, regulatory, and accreditation requirements.
7. Enhances Staff Engagement and Satisfaction
- Provides a shared purpose that motivates nurses to perform effectively.
- Fosters a positive workplace culture, improving retention and reducing burnout.
5. Steps to Develop an Effective Vision and Mission for Nursing Services
Step 1: Assess Healthcare Needs and Trends
- Conduct surveys and research to identify current and future healthcare challenges.
- Analyze patient demographics, disease patterns, and nursing workforce trends.
Step 2: Engage Key Stakeholders
- Involve nurses, patients, healthcare administrators, and policymakers in developing the vision and mission.
- Conduct focus groups and brainstorming sessions for collective input.
Step 3: Define Core Values and Goals
- Identify fundamental principles such as patient safety, ethical care, diversity, and innovation.
- Ensure alignment with international nursing standards (e.g., ICN, WHO).
Step 4: Draft and Review the Vision and Mission Statements
- Develop concise, clear, and impactful statements.
- Ensure statements are easily understood and resonate with nurses at all levels.
Step 5: Implement and Communicate the Vision and Mission
- Integrate them into policies, procedures, staff training, and performance evaluations.
- Display the statements in workplaces, websites, and official documents.
Step 6: Periodic Review and Revision
- Evaluate effectiveness through staff feedback, patient satisfaction surveys, and performance metrics.
- Revise the statements as healthcare policies, technology, and patient needs evolve.
A strong vision and mission are essential for planning and managing nursing services effectively. They ensure that nursing care remains high-quality, patient-centered, and aligned with evolving healthcare needs. By integrating these elements into strategic planning, nursing services can enhance staff engagement, resource efficiency, and patient satisfaction, ultimately leading to improved health outcomes.
Planning Nursing Services: Philosophy
Philosophy in nursing service planning refers to the core beliefs, values, and principles that guide nursing practice and decision-making. It serves as the foundation for nursing care delivery, influencing policies, procedures, and the overall approach to patient care. A well-defined nursing philosophy ensures that healthcare services remain ethical, patient-centered, and evidence-based.
Definition of Nursing Philosophy
A nursing philosophy is a statement that outlines the beliefs, values, and ethical principles that guide nursing practice. It serves as a framework for delivering high-quality, compassionate, and holistic care to patients.
Key Aspects of Nursing Philosophy
- Commitment to Patient Care – Providing safe, effective, and compassionate care to individuals, families, and communities.
- Ethical Nursing Practice – Adhering to professional ethics, confidentiality, and respect for human dignity.
- Evidence-Based Practice (EBP) – Implementing scientific knowledge and research to improve patient outcomes.
- Holistic Care Approach – Addressing the physical, emotional, social, and spiritual needs of patients.
- Commitment to Professionalism – Maintaining competence, integrity, and lifelong learning in nursing.
- Collaboration and Teamwork – Working with healthcare professionals, patients, and families to provide the best care.
- Equity and Inclusivity – Ensuring equal access to healthcare services for all individuals, regardless of background.
Components of Nursing Philosophy in Service Planning
1. Beliefs and Values in Nursing Practice
- Patient-Centered Care: The patient is the primary focus of nursing services.
- Dignity and Respect: Every individual deserves respect, dignity, and compassionate care.
- Ethical Decision-Making: Nurses should always follow ethical principles such as autonomy, beneficence, non-maleficence, and justice.
- Professional Integrity: Nursing services should be transparent, honest, and accountable.
- Cultural Competence: Nursing care should be inclusive and culturally sensitive.
2. Ethical Foundations of Nursing Philosophy
A strong nursing philosophy is rooted in ethical principles that ensure fairness and safety in healthcare.
- Autonomy – Respecting patients’ right to make decisions about their own care.
- Beneficence – Ensuring that nursing actions benefit the patient.
- Non-maleficence – Preventing harm and ensuring patient safety.
- Justice – Providing equal access to healthcare services.
- Confidentiality – Maintaining privacy and trust in nurse-patient relationships.
3. Evidence-Based and Holistic Care
- Scientific Knowledge – Nursing services must be based on research and best practices.
- Holistic Approach – Nursing care should address physical, mental, emotional, and social well-being.
- Patient Education – Nurses should empower patients through health education and self-care guidance.
4. Nursing Leadership and Professional Growth
- Continuous Learning – Nurses should pursue professional development and lifelong learning.
- Leadership in Nursing – Encouraging nurse leadership in healthcare decision-making.
- Advocacy – Nurses should advocate for patient rights, safety, and quality care.
5. Collaboration and Interdisciplinary Approach
- Teamwork – Nursing services should promote collaboration among healthcare professionals.
- Effective Communication – Ensuring clear and respectful communication in patient care.
- Family-Centered Care – Involving families and caregivers in decision-making.
Importance of Nursing Philosophy in Service Planning
| Aspect | Role of Philosophy in Nursing Services |
|---|---|
| Guides Nursing Practice | Ensures that all nursing actions are consistent with core values and beliefs. |
| Enhances Patient Care | Leads to better patient outcomes, satisfaction, and holistic healing. |
| Ensures Ethical and Legal Compliance | Encourages ethical decision-making and adherence to legal standards. |
| Strengthens Professionalism | Promotes accountability, competence, and excellence in nursing practice. |
| Facilitates Policy Development | Helps in creating nursing protocols, policies, and service frameworks. |
| Encourages Research and Innovation | Supports evidence-based improvements in healthcare services. |
| Improves Healthcare Collaboration | Promotes teamwork and communication in the healthcare system. |
Developing a Nursing Philosophy for Service Planning
Step 1: Identify Core Nursing Values
- Define what matters most in nursing care (e.g., compassion, respect, ethics).
- Gather input from nurses, healthcare leaders, and patients.
Step 2: Align with Healthcare Standards and Policies
- Ensure the philosophy aligns with nursing codes of ethics, accreditation standards, and institutional policies.
Step 3: Develop a Nursing Philosophy Statement
- Create a clear and concise statement of beliefs and values that guide nursing services.
Example of a Nursing Philosophy Statement:
“We believe in delivering holistic, compassionate, and evidence-based nursing care that respects the dignity, autonomy, and individual needs of each patient. Our commitment is to promote health, prevent illness, and provide ethical, high-quality care through collaboration, continuous learning, and innovation.”
Step 4: Implement and Integrate into Nursing Services
- Train nurses and staff on the philosophy’s principles.
- Include the philosophy in nursing guidelines, policies, and patient care protocols.
Step 5: Review and Update Regularly
- Reassess and revise the philosophy to adapt to new healthcare challenges and advancements.
A strong nursing philosophy forms the foundation for effective nursing service planning. It ensures that nurses deliver ethical, evidence-based, and patient-centered care, while fostering professional integrity, teamwork, and continuous improvement. By integrating philosophy into nursing services, healthcare organizations can enhance patient care quality, improve staff engagement, and ensure sustainable healthcare practices.
Planning Nursing Services: Objectives
The objectives of planning nursing services serve as specific goals and measurable outcomes that guide nursing care delivery, ensuring efficiency, quality, and patient-centered care. These objectives help in structuring nursing services, optimizing resource allocation, and maintaining high standards of nursing practice.
Objectives of Planning Nursing Services
The objectives of planning nursing services can be categorized into various domains: patient care, professional development, healthcare system improvement, ethical practice, and research and innovation.
1. Objectives Related to Patient Care
- Ensure High-Quality Care – Provide safe, effective, and evidence-based nursing care to all patients.
- Promote Patient Safety – Reduce errors, prevent hospital-acquired infections, and maintain a culture of safety in nursing services.
- Enhance Patient Satisfaction – Improve communication, empathy, and responsiveness in nursing care.
- Provide Holistic Care – Address the physical, emotional, psychological, and social needs of patients.
- Encourage Patient and Family Involvement – Involve patients and families in decision-making and care planning.
- Improve Nursing Response Time – Ensure timely interventions in emergency and routine care settings.
2. Objectives Related to Nursing Staff and Professional Development
- Ensure Competency-Based Training – Implement continuous education, training, and skill enhancement for nursing staff.
- Encourage Leadership and Teamwork – Promote collaborative practice, leadership skills, and effective teamwork.
- Standardize Nursing Procedures – Develop standard operating protocols (SOPs) to maintain uniform nursing care.
- Foster Lifelong Learning – Support continuous professional development (CPD) and encourage nurses to update their knowledge.
- Ensure a Healthy Work Environment – Maintain adequate staffing, stress management programs, and supportive supervision.
- Increase Staff Retention and Satisfaction – Develop incentive programs, career growth opportunities, and recognition initiatives for nurses.
3. Objectives Related to Healthcare System Improvement
- Optimize Resource Utilization – Ensure effective use of medical supplies, hospital beds, and staff allocation.
- Improve Nursing Documentation and Record-Keeping – Implement efficient and accurate patient record systems.
- Enhance Efficiency in Nursing Workflows – Reduce workload imbalance, promote task delegation, and use time management strategies.
- Develop Emergency and Disaster Management Plans – Ensure preparedness and quick response in case of disasters or emergencies.
- Promote Technology Integration – Utilize healthcare technologies like electronic health records (EHRs), telemedicine, and smart monitoring devices.
- Strengthen Primary and Community Nursing Services – Extend nursing care to rural and underserved populations.
4. Objectives Related to Ethical and Legal Aspects
- Uphold Ethical Nursing Practice – Ensure adherence to nursing ethics, patient rights, and confidentiality policies.
- Maintain Compliance with Healthcare Regulations – Align nursing services with national and international healthcare guidelines.
- Implement Patient Advocacy Programs – Empower nurses to advocate for patient rights and access to quality care.
- Ensure Culturally Competent Nursing Care – Provide care that is inclusive and respects diverse patient backgrounds.
5. Objectives Related to Research and Evidence-Based Practice (EBP)
- Promote Evidence-Based Nursing – Encourage nurses to apply research findings and best practices in patient care.
- Facilitate Nursing Research – Support nurses in conducting clinical research and quality improvement projects.
- Implement Quality Assurance Programs – Regularly assess nursing performance and patient outcomes to enhance quality care.
- Support Innovation in Nursing – Encourage the adoption of new care models, technology, and advanced nursing interventions.
SMART Objectives for Planning Nursing Services
A well-defined nursing service objective should follow the SMART criteria:
| SMART Criteria | Application in Nursing Services |
|---|---|
| Specific | Define clear, focused objectives (e.g., reduce patient falls in ICU by 20%). |
| Measurable | Set quantifiable indicators (e.g., improve hand hygiene compliance to 95%). |
| Achievable | Ensure objectives are realistic given available resources. |
| Relevant | Align with healthcare policies and nursing goals. |
| Time-Bound | Set a specific timeframe for achieving goals (e.g., within 6 months). |
Examples of SMART Objectives in Nursing Services
- “Reduce hospital-acquired infections (HAIs) by 30% within the next 12 months through improved hand hygiene and infection control training.”
- “Achieve a 90% patient satisfaction rate in nursing care within the next year by implementing structured feedback mechanisms and patient-centered communication training.”
- “Increase the number of nurses trained in advanced cardiac life support (ACLS) from 50% to 80% within 6 months.”
Importance of Objectives in Nursing Service Planning
| Aspect | Importance of Objectives |
|---|---|
| Guides Nursing Practice | Provides a clear direction for nurses to follow. |
| Enhances Patient Outcomes | Leads to better health outcomes, reduced errors, and improved safety. |
| Improves Efficiency | Ensures optimal use of time, resources, and staff. |
| Supports Quality Assurance | Helps in monitoring, evaluating, and improving nursing services. |
| Facilitates Staff Development | Encourages continuous learning and professional growth. |
| Ensures Compliance with Standards | Aligns nursing services with legal, ethical, and accreditation requirements. |
| Encourages Innovation | Promotes the use of new research, technologies, and care models. |
Steps to Develop and Implement Nursing Service Objectives
Step 1: Assess the Current Nursing Service Needs
- Conduct nursing audits, patient feedback analysis, and workforce assessments.
- Identify areas requiring improvement (e.g., infection control, nurse-patient ratio).
Step 2: Define Clear and Measurable Objectives
- Develop short-term and long-term goals for nursing services.
- Ensure alignment with organizational and national healthcare priorities.
Step 3: Allocate Resources and Responsibilities
- Assign specific roles to nursing staff and leaders.
- Ensure access to training, technology, and medical supplies.
Step 4: Implement Strategies to Achieve Objectives
- Use clinical guidelines, evidence-based protocols, and nursing education programs.
- Encourage interdisciplinary teamwork in patient care.
Step 5: Monitor Progress and Make Adjustments
- Conduct regular evaluations, quality audits, and feedback sessions.
- Revise objectives based on performance data and healthcare trends.
Step 6: Document and Report Outcomes
- Maintain detailed nursing records and performance reports.
- Share best practices with healthcare teams and policymakers.
Establishing clear, strategic, and well-defined objectives is essential for planning efficient, high-quality nursing services. These objectives enhance patient care, optimize nursing workflows, promote professional development, and improve healthcare system outcomes. By following the SMART approach, nursing leaders can ensure that services remain effective, adaptable, and aligned with evolving healthcare needs.
Nursing Service Policies:
Nursing service policies are formal guidelines and procedures that regulate nursing practice, ensuring high-quality, safe, ethical, and efficient patient care. These policies provide a structured framework for decision-making, nursing interventions, professional conduct, and healthcare compliance. They help in standardizing nursing care, improving patient safety, and aligning nursing services with legal and professional regulations.
Objectives of Nursing Service Policies
- Ensure Consistency in Nursing Care – Standardize procedures to maintain uniform patient care across departments.
- Enhance Patient Safety – Reduce medical errors and hospital-acquired infections through clear policies.
- Support Legal and Ethical Compliance – Ensure adherence to national and international nursing regulations.
- Improve Nurse Accountability and Responsibility – Define roles, duties, and professional boundaries for nurses.
- Optimize Resource Utilization – Ensure proper use of equipment, medications, and nursing staff.
- Promote Evidence-Based Practice (EBP) – Implement best practices to improve healthcare outcomes.
Key Components of Nursing Service Policies
1. Patient Care and Safety Policies
These policies define nursing responsibilities in direct patient care, including safety protocols, infection control, and emergency procedures.
Examples:
- Hand Hygiene Policy – Ensures nurses follow strict infection control measures (e.g., WHO’s 5 Moments for Hand Hygiene).
- Patient Identification Policy – Requires double-checking patient identity before administering medications or procedures.
- Medication Administration Policy – Regulates safe drug administration, dosage calculation, and adverse reaction reporting.
- Fall Prevention Policy – Implements fall risk assessment, bed rail use, and safe patient transfer techniques.
- Pain Management Policy – Establishes guidelines for pain assessment, pharmacological and non-pharmacological interventions.
2. Nursing Staffing and Workload Policies
Policies governing staffing ratios, duty hours, and nurse-patient assignments ensure balanced workloads and prevent nurse burnout.
Examples:
- Nurse-Patient Ratio Policy – Specifies optimal staffing levels (e.g., ICU: 1:1 ratio, General Ward: 1:5 ratio).
- Shift Rotation Policy – Regulates fair distribution of shifts (morning, evening, night) to prevent fatigue.
- Overtime and Break Policy – Defines maximum working hours, overtime compensation, and mandated breaks.
3. Professional Conduct and Ethical Nursing Policies
These policies ensure ethical behavior, professionalism, and compliance with nursing codes of conduct.
Examples:
- Code of Ethics Policy – Follows ANA, ICN, and local nursing regulatory guidelines.
- Patient Confidentiality Policy (HIPAA Compliance) – Prevents unauthorized access to patient health records.
- Workplace Harassment Policy – Establishes a zero-tolerance policy for harassment and discrimination.
- Informed Consent Policy – Requires nurses to educate patients about procedures before obtaining consent.
4. Emergency and Disaster Management Policies
Defines nursing roles and responsibilities during medical emergencies and public health disasters.
Examples:
- Cardiopulmonary Resuscitation (CPR) Policy – Ensures all nurses are trained in BLS and ACLS.
- Disaster Preparedness Policy – Guides nurses on mass casualty management, triage, and disaster response coordination.
- Fire Safety and Evacuation Policy – Outlines steps for emergency evacuation, fire drills, and extinguisher use.
5. Infection Control and Prevention Policies
Regulate infection control measures to reduce hospital-acquired infections (HAIs) and ensure a safe hospital environment.
Examples:
- Standard Precaution Policy – Requires the use of PPE, hand hygiene, and disinfection protocols.
- Isolation and Quarantine Policy – Defines procedures for airborne, droplet, and contact isolation precautions.
- Biomedical Waste Management Policy – Ensures proper segregation, handling, and disposal of medical waste.
6. Nursing Documentation and Record-Keeping Policies
Ensures that nurses maintain accurate, legal, and confidential patient records.
Examples:
- Electronic Health Record (EHR) Policy – Defines guidelines for secure digital documentation of patient data.
- Incident Reporting Policy – Mandates reporting of adverse events, medication errors, and patient safety issues.
- Nursing Care Plan Documentation Policy – Requires nurses to update patient progress notes regularly.
7. Nursing Education and Professional Development Policies
Policies supporting nurse training, continuing education, and certification requirements.
Examples:
- Mandatory Continuing Nursing Education (CNE) Policy – Requires nurses to complete certain hours of training annually.
- Competency-Based Training Policy – Ensures nurses undergo regular skill assessments and refresher courses.
- Preceptor and Mentorship Policy – Encourages experienced nurses to mentor junior staff.
8. Legal and Regulatory Compliance Policies
Ensure adherence to government and hospital regulations to maintain nursing licensure and accreditation.
Examples:
- License Renewal and Credentialing Policy – Requires nurses to renew their professional license periodically.
- Patient Rights and Advocacy Policy – Ensures informed decision-making, privacy, and dignity.
- Workplace Safety and OSHA Compliance Policy – Ensures compliance with occupational safety laws.
Implementation of Nursing Service Policies
Step 1: Policy Development
- Identify critical areas needing policies (e.g., infection control, staffing, medication administration).
- Involve nurse managers, hospital administrators, and legal advisors.
Step 2: Policy Approval and Standardization
- Review policies with hospital committees, nursing councils, and regulatory bodies.
- Align policies with national and international nursing standards.
Step 3: Staff Training and Awareness
- Conduct workshops, simulations, and competency tests.
- Ensure easy access to policy manuals and digital platforms.
Step 4: Policy Implementation and Compliance Monitoring
- Assign supervisors to oversee compliance.
- Use quality audits and feedback to improve policies.
Step 5: Periodic Review and Updates
- Review policies annually based on new healthcare trends, research, and regulatory changes.
Importance of Nursing Service Policies
| Aspect | Benefits of Nursing Policies |
|---|---|
| Patient Safety | Reduces medical errors and ensures evidence-based care. |
| Standardized Care | Ensures uniform nursing practices across departments. |
| Legal Protection | Reduces risks of malpractice lawsuits and legal issues. |
| Professional Accountability | Clearly defines nursing responsibilities and expectations. |
| Workplace Efficiency | Improves staff coordination and workflow. |
| Regulatory Compliance | Aligns with national and international nursing standards. |
Challenges in Implementing Nursing Service Policies
- Lack of Awareness – Nurses may be unaware of policy updates.
- Resistance to Change – Some staff may be hesitant to adopt new procedures.
- Inadequate Resources – Insufficient PPE, staff, or technology can hinder policy execution.
- Poor Monitoring – Lack of regular audits leads to policy violations.
- Time Constraints – Busy schedules prevent nurses from participating in training sessions.
Nursing service policies are essential for maintaining high standards of patient care, professionalism, and regulatory compliance. They ensure nurses work efficiently, ethically, and safely, contributing to better health outcomes and an improved healthcare system. Regular training, monitoring, and updates of these policies help in enhancing the effectiveness of nursing services in hospitals and healthcare facilities.
Nursing Service: Procedures and Manuals
Nursing procedures and manuals serve as structured guidelines that standardize clinical nursing practice, ensuring patient safety, efficiency, and quality care. These documents provide step-by-step protocols for performing nursing tasks, handling emergencies, and maintaining compliance with healthcare standards and regulations.
1. Nursing Procedures
Definition:
Nursing procedures are systematic and evidence-based methods used to provide safe, effective, and high-quality nursing care. These procedures ensure standardized practice across healthcare settings and help in maintaining legal and professional accountability.
Objectives of Nursing Procedures:
- Ensure patient safety by following a stepwise approach to nursing interventions.
- Improve efficiency in delivering care by reducing errors and inconsistencies.
- Enhance nurse competency through clear, evidence-based guidelines.
- Facilitate legal and ethical compliance by aligning with hospital policies and healthcare regulations.
- Improve patient outcomes by using best-practice approaches in clinical care.
Categories of Nursing Procedures:
1. Basic Nursing Procedures
These involve fundamental nursing tasks required in daily patient care.
✔ Hand Hygiene and Aseptic Techniques – Proper handwashing, sterilization, and infection control.
✔ Vital Signs Monitoring – Measuring temperature, pulse, respiration, and blood pressure.
✔ Bed-Making and Patient Positioning – Maintaining patient comfort and preventing bedsores.
✔ Administering Medications – Following the rights of medication administration (Right Patient, Drug, Dose, Route, Time, Documentation).
✔ Feeding Techniques – Assisting patients with oral, enteral, or parenteral feeding.
✔ Skin Care and Wound Dressing – Managing pressure ulcers, surgical wounds, and burns.
2. Clinical and Specialized Nursing Procedures
These procedures are performed in critical care units, operation theaters, and specialized nursing areas.
✔ Intravenous (IV) Cannulation and Fluid Therapy – Inserting IV lines and managing fluid administration.
✔ Oxygen Therapy and Suctioning – Delivering oxygen and clearing airway secretions.
✔ Catheterization – Inserting and managing urinary catheters.
✔ Blood Transfusion – Safe administration and monitoring of blood and blood products.
✔ Pre- and Post-Operative Nursing Care – Preparing patients for surgery and post-surgical recovery care.
✔ Pain Management – Administering analgesics and using non-pharmacological interventions.
3. Emergency Nursing Procedures
These procedures are required for life-threatening situations.
✔ Cardiopulmonary Resuscitation (CPR) – Performing BLS (Basic Life Support) and ACLS (Advanced Cardiac Life Support).
✔ Triage and Emergency Assessment – Classifying patients based on the severity of their condition.
✔ Shock and Trauma Management – Handling burns, fractures, and hemorrhage control.
✔ Seizure Management – Protecting the patient and administering emergency anticonvulsants.
✔ Poisoning and Overdose Treatment – Administering antidotes and gastric lavage.
4. Infection Control Procedures
These ensure hospital hygiene and prevent cross-infection.
✔ Standard Precautions – Proper use of PPE (gloves, masks, gowns, eye protection).
✔ Isolation Techniques – Managing infectious diseases like TB, COVID-19, and MRSA.
✔ Sterilization and Disinfection – Decontaminating medical equipment and surfaces.
✔ Needlestick Injury Management – Handling sharps safely and reporting exposures.
2. Nursing Manuals
Definition:
Nursing manuals are comprehensive documents that provide detailed instructions, policies, and guidelines for various nursing functions. They ensure that all nursing procedures are performed according to best practices, legal requirements, and hospital standards.
Types of Nursing Manuals
1. Nursing Policy and Procedure Manual
This manual provides guidelines on nursing duties, legal responsibilities, and hospital policies.
✔ Scope of Nursing Practice – Defines the roles and responsibilities of nurses.
✔ Patient Rights and Ethics – Guidelines for respecting confidentiality, dignity, and autonomy.
✔ Incident Reporting – Steps for documenting adverse events, medication errors, and injuries.
✔ Standard Operating Procedures (SOPs) – Outlines clinical and non-clinical nursing protocols.
2. Infection Control Manual
This manual ensures hospital infection prevention and control.
✔ Hand Hygiene and PPE Guidelines – Stepwise infection prevention measures.
✔ Isolation and Quarantine Policies – Managing communicable diseases.
✔ Biomedical Waste Disposal Guidelines – Safe segregation of hazardous and non-hazardous waste.
3. Nursing Documentation Manual
This manual ensures accurate and legal record-keeping in patient care.
✔ Electronic Health Records (EHRs) Guidelines – Digital patient documentation standards.
✔ Medication Administration Record (MAR) – Recording drug administration details.
✔ Nursing Notes and Care Plans – Maintaining daily nursing progress reports.
4. Emergency Response Manual
This manual provides step-by-step guidelines for handling medical emergencies.
✔ Code Blue (Cardiac Arrest) Protocol – Immediate CPR and defibrillation guidelines.
✔ Disaster Management Plan – Preparedness for earthquakes, floods, and mass casualties.
✔ Fire Safety and Evacuation Protocols – Fire drill procedures and safety exit planning.
5. Nursing Training and Competency Manual
This manual provides training programs and skill assessments for nurses.
✔ Continuing Nursing Education (CNE) – Courses for upgrading nursing knowledge.
✔ Preceptor and Mentorship Programs – Assigning experienced nurses as mentors.
✔ Competency Evaluation Guidelines – Methods to assess nursing skills and knowledge.
Importance of Nursing Procedures and Manuals
| Aspect | Significance |
|---|---|
| Ensures Standardized Nursing Care | Provides a uniform approach to patient care across all nurses. |
| Improves Patient Safety | Reduces errors, infections, and procedural complications. |
| Enhances Nurse Competency | Guides new nurses and supports professional development. |
| Supports Legal and Ethical Compliance | Prevents malpractice and ensures hospital accreditation. |
| Facilitates Training and Education | Helps in nursing education, orientation, and skill evaluation. |
Implementation and Maintenance of Nursing Manuals
Step 1: Development and Approval
- Involve nurse leaders, medical staff, and hospital administrators.
- Ensure manuals align with international nursing standards (ANA, ICN, WHO).
Step 2: Training and Dissemination
- Conduct workshops and online training sessions for nurses.
- Make manuals accessible digitally and in printed format.
Step 3: Compliance Monitoring
- Conduct regular audits and quality checks to ensure policy adherence.
- Use performance indicators to measure compliance.
Step 4: Review and Updates
- Update manuals annually based on new research, technology, and policy changes.
- Gather nurse feedback to refine procedures.
Nursing procedures and manuals are essential for maintaining high-quality, standardized, and evidence-based nursing care. They ensure that nurses follow best practices, comply with regulations, and provide safe, efficient, and ethical patient care. Continuous training, monitoring, and updating of nursing manuals help healthcare institutions maintain excellence in nursing services.
Functional and Operational Planning in Nursing Services
Functional and operational planning in nursing services involves designing and implementing efficient workflows, staffing models, and resource management strategies to ensure high-quality patient care. While functional planning focuses on structuring nursing services based on healthcare goals and objectives, operational planning translates those plans into daily nursing activities and procedures.
1. Functional Planning in Nursing Services
Definition:
Functional planning in nursing refers to the broad and strategic framework that organizes nursing services according to hospital goals, patient needs, and healthcare policies. It sets the foundation for nursing department structures, staffing, and resource allocation.
Objectives of Functional Planning:
- Ensure the availability of well-organized nursing services.
- Establish nursing roles, responsibilities, and departmental hierarchies.
- Optimize staff distribution based on patient needs and acuity levels.
- Align nursing functions with hospital policies and national healthcare standards.
- Improve the efficiency of patient care delivery through systematic organization.
Key Elements of Functional Planning:
1. Organizational Structure and Hierarchy
Functional planning defines the structure of nursing services in hospitals and healthcare institutions.
- Chief Nursing Officer (CNO) → Nursing Supervisors → Ward In-charge Nurses → Staff Nurses → Nursing Assistants.
- Establishes reporting relationships and chain of command for decision-making.
- Differentiates clinical, administrative, and educational roles in nursing.
2. Staffing and Human Resource Planning
- Determines the nurse-patient ratio for different units (e.g., ICU: 1:1, General Ward: 1:5).
- Defines job descriptions, competencies, and responsibilities of nursing staff.
- Plans recruitment, training, promotions, and succession planning for nurses.
3. Infrastructure and Facility Planning
- Allocates wards, nursing stations, emergency units, and specialty areas efficiently.
- Ensures availability of medical equipment, technology, and patient monitoring systems.
- Plans for infection control facilities, isolation rooms, and emergency care areas.
4. Policy and Protocol Development
- Establishes nursing service policies for medication administration, patient safety, and quality improvement.
- Defines standard operating procedures (SOPs) for clinical tasks and emergency response.
- Ensures compliance with regulatory standards and accreditation requirements.
2. Operational Planning in Nursing Services
Definition:
Operational planning in nursing involves day-to-day implementation of functional plans, ensuring that all nursing activities run smoothly within the hospital or healthcare facility. It translates strategic nursing objectives into actionable steps.
Objectives of Operational Planning:
- Improve efficiency in daily nursing workflows and patient care processes.
- Ensure proper allocation of nursing staff based on patient needs.
- Optimize the use of hospital resources such as beds, medical equipment, and medications.
- Enhance coordination between different healthcare departments.
- Monitor and evaluate nursing service performance to maintain quality standards.
Key Elements of Operational Planning:
1. Nurse Scheduling and Shift Management
- Plans daily work schedules to maintain adequate nurse staffing.
- Ensures fair shift rotations to prevent fatigue and burnout.
- Allocates nurses based on patient acuity levels and special care requirements.
2. Patient Admission, Discharge, and Transfer Management
- Ensures seamless admission procedures, including initial assessment and documentation.
- Plans for efficient discharge protocols to reduce patient length of stay.
- Coordinates patient transfers between departments (e.g., ICU to General Ward).
3. Medication and Supply Chain Management
- Ensures timely ordering, storage, and distribution of medications and medical supplies.
- Implements inventory control measures to avoid shortages or overstocking.
- Establishes protocols for emergency drug availability in critical care units.
4. Quality Control and Performance Monitoring
- Conducts regular audits and evaluations of nursing care quality.
- Implements patient satisfaction surveys to gather feedback.
- Uses clinical outcome indicators (e.g., infection rates, patient recovery times) to assess nursing performance.
5. Emergency and Contingency Planning
- Prepares for emergency staffing needs during peak hours, disease outbreaks, or disasters.
- Implements crisis management protocols (e.g., Code Blue for cardiac arrest).
- Ensures availability of backup resources such as additional beds, ventilators, and PPE.
Comparison of Functional vs. Operational Planning
| Aspect | Functional Planning | Operational Planning |
|---|---|---|
| Definition | Long-term planning that organizes nursing services | Short-term planning for daily nursing activities |
| Focus | Strategic goals, policies, and structural organization | Implementation of nursing workflows and procedures |
| Time Frame | Long-term (Annual or Multi-Year Plan) | Short-term (Daily, Weekly, or Monthly Plan) |
| Scope | Staffing models, organizational structure, policy development | Nurse scheduling, patient care management, resource allocation |
| Outcome | Efficient nursing department organization and improved healthcare delivery | Smooth day-to-day operations and optimized nursing performance |
| Example | Developing a nurse staffing model for different departments | Assigning nurses to specific shifts and patient care duties |
Steps in Functional and Operational Planning
Step 1: Assess Healthcare Needs
- Identify patient demographics, disease patterns, and staffing requirements.
- Conduct workload analysis to determine nurse-patient ratios.
Step 2: Develop Functional Plans
- Define nursing department structures and staff roles.
- Establish hospital-wide nursing policies and standards.
- Allocate budgets for nursing resources and equipment.
Step 3: Implement Operational Plans
- Schedule daily nursing shifts and assign patient care duties.
- Ensure medication and supply management in all units.
- Monitor quality assurance measures and performance indicators.
Step 4: Evaluate and Improve Nursing Services
- Conduct regular audits and performance reviews.
- Collect patient and staff feedback for continuous improvement.
- Modify functional and operational plans as per emerging healthcare needs.
Challenges in Functional and Operational Planning
| Challenges | Possible Solutions |
|---|---|
| Staffing Shortages | Implement effective recruitment and retention strategies. |
| Resource Constraints | Optimize resource allocation and use technology for efficiency. |
| Coordination Issues | Strengthen interdepartmental communication and teamwork. |
| Resistance to Change | Provide training programs and encourage staff participation in planning. |
| Emergency Preparedness Gaps | Develop clear disaster management protocols and regular emergency drills. |
Functional and operational planning in nursing services ensures that healthcare facilities operate efficiently, deliver quality patient care, and maintain compliance with professional standards. Functional planning focuses on the structural organization of nursing services, while operational planning ensures that these structures are implemented effectively in daily nursing workflows. A well-planned nursing service improves patient outcomes, enhances nurse satisfaction, and strengthens healthcare delivery systems.
Strategic Planning in Nursing Services
Strategic planning in nursing services is a long-term, goal-oriented process that ensures nursing care is effective, efficient, and aligned with healthcare advancements. It involves analyzing healthcare trends, setting objectives, optimizing resources, and implementing policies to improve patient outcomes and nursing performance.
Strategic planning helps nursing leaders, administrators, and policymakers to anticipate challenges, allocate resources wisely, and develop a roadmap for achieving high-quality nursing services in hospitals, clinics, and community health settings.
Definition of Strategic Planning
Strategic planning in nursing is a systematic approach to defining the direction, priorities, and long-term goals of nursing services while ensuring alignment with institutional, national, and global healthcare objectives.
Key Features of Strategic Planning in Nursing:
✔ Long-term focus (3 to 10 years).
✔ Aligns with organizational vision, mission, and goals.
✔ Data-driven and evidence-based decision-making.
✔ Considers healthcare trends, technology, and policy changes.
✔ Involves collaboration among nurses, administrators, and stakeholders.
✔ Ensures adaptability to changing healthcare environments.
Objectives of Strategic Planning in Nursing Services
- Enhance Quality and Safety in Patient Care
- Implement evidence-based practices to reduce errors and improve outcomes.
- Develop patient safety protocols and quality improvement initiatives.
- Optimize Human Resource Management in Nursing
- Address nurse staffing shortages by planning recruitment and retention strategies.
- Enhance nurse training, leadership development, and continuing education programs.
- Improve Efficiency in Nursing Workflows
- Implement nursing informatics and electronic health records (EHRs) for better documentation.
- Develop strategies for reducing patient wait times and optimizing nursing workload.
- Strengthen Financial and Resource Management
- Plan cost-effective budgeting for nursing equipment, technology, and training programs.
- Identify funding opportunities for nursing research and development projects.
- Ensure Compliance with Legal and Ethical Standards
- Align nursing practices with national and international healthcare regulations.
- Implement policies on patient rights, confidentiality (HIPAA), and ethical nursing practice.
- Adopt Technological Advancements in Nursing
- Integrate telehealth and AI-driven nursing interventions.
- Utilize robotic-assisted nursing care and digital monitoring systems.
- Expand Community-Based and Preventive Healthcare Services
- Develop nursing outreach programs for maternal and child health, elderly care, and chronic disease management.
- Strengthen school health programs and community nursing initiatives.
- Promote Research and Innovation in Nursing
- Encourage evidence-based nursing practices and clinical trials.
- Foster collaborations with universities, research institutions, and global health organizations.
Key Components of Strategic Planning in Nursing
1. Environmental and Situational Analysis (SWOT Analysis)
Before planning, nursing leaders must analyze internal and external factors that influence nursing services.
| SWOT Analysis in Nursing Services | Examples |
|---|---|
| S – Strengths | Well-trained nursing staff, advanced medical technology, effective leadership |
| W – Weaknesses | Shortage of nurses, outdated policies, lack of resources |
| O – Opportunities | New healthcare reforms, funding for research, use of AI and telemedicine |
| T – Threats | Rising patient demand, pandemics, changing government regulations |
2. Goal Setting and Prioritization
- Define clear and measurable strategic goals based on the hospital’s vision and mission.
- Prioritize goals based on urgency, impact, and feasibility.
- Use the SMART (Specific, Measurable, Achievable, Relevant, Time-bound) criteria for setting goals.
Example of a SMART Goal:
✅ “Increase nurse-patient ratio in ICU from 1:2 to 1:1 within the next 5 years by hiring 100 additional trained critical care nurses.”
3. Resource Allocation and Financial Planning
- Plan budget distribution for nursing salaries, training programs, infrastructure, and technology.
- Allocate resources for nursing research, equipment, and patient care innovations.
- Explore grants, government funds, and partnerships with private organizations.
4. Implementation Strategies
To achieve strategic goals, nursing services must implement structured action plans.
A. Workforce Development Strategy
✔ Recruit and train specialized nurses (e.g., ICU, oncology, pediatric nurses).
✔ Develop mentorship and leadership training programs.
✔ Improve nurse retention through incentives and better working conditions.
B. Patient Care Improvement Strategy
✔ Implement standardized nursing protocols for infection control and medication safety.
✔ Increase nursing rounds and bedside patient monitoring.
✔ Improve patient education programs for self-care and disease prevention.
C. Digital Health and Technology Integration
✔ Implement electronic health records (EHRs) and AI-based clinical decision tools.
✔ Expand telehealth services for remote consultations and follow-ups.
✔ Adopt smart hospital technology (e.g., automated medication dispensing).
D. Community and Preventive Care Strategy
✔ Strengthen home healthcare services and chronic disease management programs.
✔ Expand vaccination drives, maternal health programs, and school health initiatives.
✔ Improve public health awareness campaigns on hygiene, nutrition, and mental health.
5. Monitoring, Evaluation, and Continuous Improvement
Key Performance Indicators (KPIs) for Strategic Planning Evaluation:
| KPI Category | Examples of Indicators |
|---|---|
| Quality of Care | Reduction in patient mortality and infection rates |
| Nurse Workforce Management | Increase in nurse retention and recruitment |
| Patient Satisfaction | Improvement in patient feedback and experience |
| Operational Efficiency | Reduced patient wait times and improved documentation |
| Financial Performance | Cost savings through better resource allocation |
Methods for Evaluation:
- Conduct monthly and annual performance reviews.
- Use patient satisfaction surveys and nurse feedback mechanisms.
- Implement data-driven reports and audits to track progress.
Challenges in Strategic Planning for Nursing Services
| Challenges | Solutions |
|---|---|
| Nursing staff shortages | Develop incentive-based recruitment programs and improve retention strategies. |
| Limited budget and resources | Seek government funding, grants, and hospital partnerships. |
| Resistance to change | Conduct training programs, workshops, and leadership engagement. |
| Evolving healthcare policies | Stay updated with regulatory changes and integrate new policies timely. |
| Technology adaptation issues | Provide digital training and technical support to nurses. |
Strategic planning in nursing services ensures long-term success, sustainability, and continuous improvement in patient care. It helps optimize nursing workflows, integrate healthcare technologies, and develop a skilled nursing workforce. By setting clear goals, allocating resources wisely, and monitoring progress, healthcare institutions can achieve higher efficiency, better patient outcomes, and improved nursing satisfaction.
A well-executed strategic plan positions nursing services to adapt to emerging healthcare challenges while maintaining quality, safety, and innovation in patient care.
Program Planning in Nursing Services: Gantt Chart Approach
Introduction
Program planning in nursing services involves designing, organizing, and implementing healthcare programs to improve patient outcomes and optimize nursing workflows. One of the most effective tools for scheduling, tracking progress, and managing resources in program planning is the Gantt Chart.
A Gantt Chart provides a visual timeline of tasks, activities, and milestones, helping nursing administrators and healthcare teams coordinate efforts efficiently.
Definition of a Gantt Chart
A Gantt Chart is a bar chart that represents a project schedule, showing tasks, durations, dependencies, and deadlines in a graphical format. It helps in planning, monitoring, and evaluating nursing programs.
Key Features of a Gantt Chart:
✔ Task Breakdown – Lists all activities needed for program completion.
✔ Timeline View – Displays start and end dates of each task.
✔ Task Dependencies – Shows relationships between activities.
✔ Milestones – Marks critical deadlines or achievements.
✔ Progress Tracking – Helps monitor task completion over time.
Importance of Using a Gantt Chart in Nursing Program Planning
| Aspect | Benefits of Gantt Chart |
|---|---|
| Improves Organization | Clearly defines tasks, deadlines, and responsibilities. |
| Enhances Team Coordination | Ensures efficient resource allocation and task delegation. |
| Prevents Delays | Helps identify bottlenecks and adjust schedules proactively. |
| Improves Time Management | Provides a visual representation of the program timeline. |
| Enhances Communication | Helps nurses, administrators, and stakeholders stay updated. |
| Facilitates Evaluation | Assists in tracking progress and making necessary adjustments. |
Steps for Program Planning Using a Gantt Chart
Step 1: Define the Nursing Program Objectives
- Clearly outline the purpose, goals, and expected outcomes.
- Example: “Reduce hospital-acquired infections (HAIs) by 30% in 6 months.”
Step 2: Identify Key Activities and Tasks
- Break down the program into smaller, manageable tasks.
- Example:
- Develop infection control guidelines.
- Conduct staff training on hand hygiene.
- Monitor compliance and audit results.
Step 3: Assign Responsibilities
- Allocate specific roles and tasks to nursing staff, supervisors, and administrators.
Step 4: Establish a Timeline
- Set realistic start and end dates for each activity.
- Example: Hand hygiene training → Start: March 1, End: March 15.
Step 5: Identify Task Dependencies
- Determine which tasks depend on others before they can begin.
- Example: Develop infection control guidelines → Conduct training.
Step 6: Create the Gantt Chart
- Use software like Microsoft Excel, Google Sheets, Trello, or project management tools (MS Project, Asana, Monday.com).
- Enter tasks, assign dates, and format the timeline view.
Step 7: Monitor and Update Progress
- Regularly track task completion and adjust schedules as needed.
- Identify delays, obstacles, or necessary revisions in real-time.
Example: Gantt Chart for a Nursing Program (Reducing Hospital-Acquired Infections)
| Task | Start Date | End Date | Duration | Responsible Team |
|---|---|---|---|---|
| Develop Infection Control Guidelines | March 1 | March 10 | 10 days | Infection Control Committee |
| Conduct Staff Training on Hand Hygiene | March 11 | March 20 | 10 days | Nurse Educators |
| Implement Hygiene Compliance Monitoring | March 21 | April 30 | 40 days | Nursing Supervisors |
| Audit Hand Hygiene Practices | May 1 | May 10 | 10 days | Quality Assurance Team |
| Analyze and Report Findings | May 11 | May 20 | 10 days | Nursing Administration |
| Implement Corrective Actions | May 21 | June 10 | 20 days | Infection Control Team |
This data is now visually represented using a Gantt Chart.
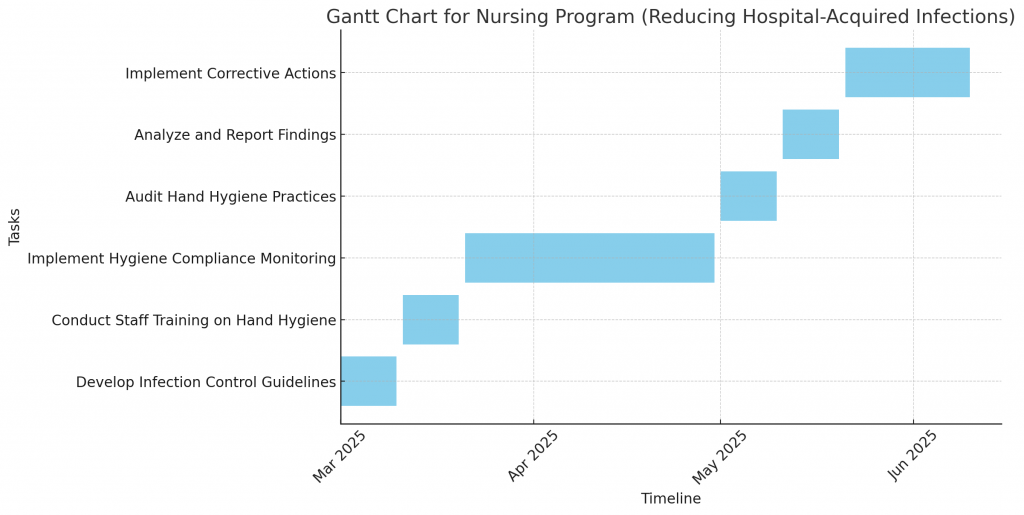
Here is a Gantt Chart for the nursing program on reducing hospital-acquired infections. This chart visually represents the timeline, duration, and sequencing of tasks, allowing for effective monitoring and management of the program.
How to Use the Gantt Chart in Nursing Program Planning:
✔ Identify potential delays and adjust schedules as needed.
✔ Ensure task dependencies are followed to avoid bottlenecks.
✔ Track progress visually to maintain accountability.
✔ Communicate effectively with nursing staff and stakeholders.
Milestone Chart for Nursing Program Planning
Introduction
A Milestone Chart is a project management tool used to track key events, deadlines, and critical achievements in a nursing program. Unlike a Gantt Chart, which focuses on detailed timelines for all tasks, a Milestone Chart highlights major phases or significant achievements in a project.
It is particularly useful in monitoring progress, ensuring accountability, and keeping stakeholders informed about the critical points in a nursing program.
Difference Between Gantt Chart and Milestone Chart
| Feature | Gantt Chart | Milestone Chart |
|---|---|---|
| Purpose | Tracks all tasks, timelines, and dependencies | Focuses on key milestones and achievements |
| Level of Detail | Detailed step-by-step breakdown of tasks | High-level project overview |
| Visualization | Bars representing task durations | Markers showing key events |
| Tracking | Tracks daily/weekly activities | Tracks major phases or deadlines |
| Best Used For | Detailed scheduling and time management | Monitoring progress and goal completion |
Steps to Create a Milestone Chart for a Nursing Program
Step 1: Define Key Milestones
Milestones are significant events or achievements within a nursing program. Example milestones for a Hospital-Acquired Infection Reduction Program:
- Develop Infection Control Guidelines – March 10, 2025
- Complete Staff Training on Hand Hygiene – March 20, 2025
- Launch Compliance Monitoring System – April 1, 2025
- First Infection Control Audit Completed – May 10, 2025
- Submit Progress Report to Administration – May 20, 2025
- Implement Corrective Measures Based on Audit – June 10, 2025
- Final Review and Program Evaluation – June 30, 2025
Step 2: Assign Responsibilities
Each milestone should be assigned to a responsible team.
| Milestone | Deadline | Responsible Team |
|---|---|---|
| Develop Infection Control Guidelines | March 10 | Infection Control Team |
| Complete Staff Training on Hand Hygiene | March 20 | Nurse Educators |
| Launch Compliance Monitoring System | April 1 | Nursing Administration |
| First Infection Control Audit Completed | May 10 | Quality Assurance Team |
| Submit Progress Report to Administration | May 20 | Nursing Administration |
| Implement Corrective Measures Based on Audit | June 10 | Infection Control Team |
| Final Review and Program Evaluation | June 30 | Hospital Management |
Step 3: Visualize in a Milestone Chart
A Milestone Chart provides a timeline view of these key achievements. I will now generate a Milestone Chart for this program.
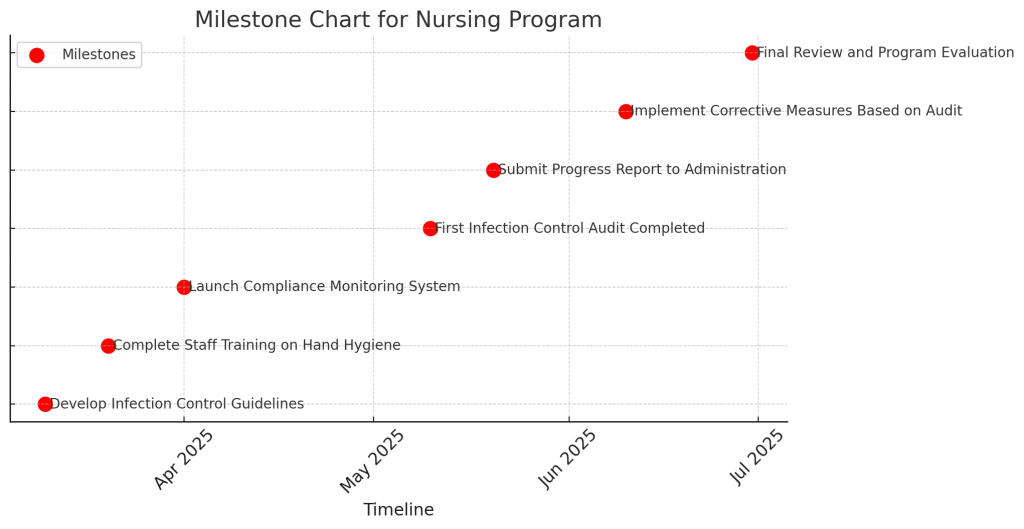
Here is the Milestone Chart for the Hospital-Acquired Infection Reduction Program in nursing. This chart visually represents key achievements and deadlines, ensuring the program stays on track.
How to Use the Milestone Chart in Nursing Program Planning:
✔ Quickly identify critical project phases and deadlines.
✔ Ensure accountability by assigning responsible teams to each milestone.
✔ Monitor progress and address any delays before reaching major deadlines.
✔ Facilitate effective communication among nursing staff and hospital management.
Planning Nursing Services: Budgeting Concepts
Budgeting in nursing service planning is a financial planning process that ensures the optimal allocation of resources to provide high-quality patient care while maintaining cost-effectiveness and efficiency. It helps nursing administrators plan for staffing, medical supplies, equipment, training, and operational expenses to ensure smooth healthcare delivery.
Budgeting in nursing services is critical for financial sustainability, resource allocation, and quality improvement in hospitals, community health centers, and other healthcare institutions.
Definition of Budgeting in Nursing Services
Budgeting is the process of planning, allocating, and controlling financial resources in nursing services to ensure that healthcare operations are sustainable, efficient, and cost-effective.
Key Features of Budgeting in Nursing Services:
✔ Estimates future costs and revenues to ensure financial stability.
✔ Allocates resources efficiently to maintain patient care quality.
✔ Controls expenses and minimizes financial waste.
✔ Aligns nursing objectives with hospital financial policies.
✔ Ensures compliance with regulatory and accreditation standards.
Objectives of Budgeting in Nursing Services
- Ensure Adequate Funding for Nursing Operations – Allocate financial resources for staffing, training, and patient care.
- Enhance Cost-Effectiveness – Optimize expenditures while maintaining quality care.
- Support Workforce Planning – Allocate funds for nurse salaries, overtime, and recruitment.
- Improve Resource Utilization – Ensure efficient use of equipment, medical supplies, and technology.
- Enhance Healthcare Infrastructure – Budget for hospital expansion, renovations, and new facilities.
- Support Continuous Professional Development – Provide funding for nurse education, training, and certifications.
- Plan for Emergencies – Maintain contingency funds for pandemics, natural disasters, and other crises.
Types of Budgets in Nursing Services
| Type of Budget | Definition | Example in Nursing Services |
|---|---|---|
| Operating Budget | Covers day-to-day expenses such as salaries, medical supplies, and utilities. | Nurse salaries, medications, IV fluids, gloves, PPE. |
| Capital Budget | Allocates funds for long-term investments such as equipment and infrastructure. | Purchase of ventilators, hospital beds, electronic health records (EHR) system. |
| Personnel Budget | Covers expenses related to staffing and payroll. | Salaries, overtime pay, recruitment, nurse incentives. |
| Supply and Equipment Budget | Allocates funds for medical and non-medical supplies. | Disposable syringes, wound care kits, sterilization equipment. |
| Training and Education Budget | Covers nurse education, workshops, and professional development. | Continuing Nursing Education (CNE), ACLS/BLS training, leadership workshops. |
| Contingency Budget | Emergency funds for unexpected events and crises. | Disaster preparedness funds for pandemics, outbreaks, or accidents. |
Key Concepts of Budgeting in Nursing Services
1. Revenue and Expense Forecasting
- Estimating expected revenue from healthcare services, insurance, and government funding.
- Forecasting expenses, including salaries, equipment, and administrative costs.
2. Fixed vs. Variable Costs
| Cost Type | Definition | Examples in Nursing Services |
|---|---|---|
| Fixed Costs | Costs that remain constant, regardless of patient volume. | Nurse salaries, rent, utility bills. |
| Variable Costs | Costs that fluctuate based on patient numbers. | Medication usage, lab tests, IV fluids. |
3. Direct vs. Indirect Costs
| Cost Type | Definition | Examples in Nursing Services |
|---|---|---|
| Direct Costs | Expenses directly related to patient care. | Medications, surgical equipment, nursing care. |
| Indirect Costs | Overhead costs that support nursing services. | Administrative salaries, hospital maintenance. |
4. Zero-Based Budgeting (ZBB)
- Each nursing department starts from zero and justifies all expenses before receiving funding.
- Helps eliminate unnecessary costs and optimize financial efficiency.
5. Incremental Budgeting
- Adjusts the previous year’s budget by a fixed percentage based on inflation, demand, or hospital growth.
- Simple but may not consider inefficiencies in previous budgets.
6. Performance-Based Budgeting
- Funds are allocated based on nursing service performance and patient outcomes.
- Example: If infection rates decrease, more funds are allocated to infection control programs.
7. Flexible Budgeting
- Adjusts nursing budgets based on fluctuating patient needs and healthcare trends.
- Useful for hospitals experiencing seasonal patient variations.
Steps in Budgeting for Nursing Services
Step 1: Assess Financial Needs
- Identify nursing staff requirements, medical supply costs, and training needs.
- Evaluate historical budget trends and patient care expenses.
Step 2: Define Budget Priorities
- Allocate funds based on urgent and high-impact areas (e.g., patient safety, staffing).
- Ensure compliance with hospital policies and national healthcare guidelines.
Step 3: Estimate Revenue Sources
- Identify funding from government grants, insurance payments, and private funding.
- Forecast expected reimbursements for nursing services.
Step 4: Allocate Funds and Develop Budget Plans
- Distribute funds across different nursing service departments (ICU, emergency, maternity, etc.).
- Prioritize capital investments in essential equipment and facilities.
Step 5: Implement Budget and Monitor Spending
- Track nursing expenses monthly or quarterly to ensure compliance.
- Adjust spending as per emerging healthcare needs.
Step 6: Evaluate and Revise Budget Annually
- Conduct budget performance reviews to identify gaps or overspending.
- Make necessary adjustments based on new policies, inflation, and patient demand.
Challenges in Nursing Budgeting and Solutions
| Challenges | Solutions |
|---|---|
| Budget constraints and limited funding | Seek grants, public-private partnerships, and cost-cutting measures. |
| Inaccurate forecasting of expenses | Use historical data and trend analysis for better predictions. |
| Rising healthcare costs and inflation | Implement cost-control strategies and negotiate supplier contracts. |
| Shortage of trained nursing staff | Allocate funds for recruitment, training, and retention programs. |
| Unexpected emergency expenses | Maintain contingency funds for unforeseen events. |
Example: Nursing Service Budget Allocation (Estimated Annual Budget)
| Category | Estimated Budget (%) | Example Expenses |
|---|---|---|
| Salaries and Wages | 50% | Nurse salaries, overtime pay, recruitment |
| Medical Supplies and Equipment | 20% | Medications, PPE, IV fluids |
| Training and Education | 10% | Continuing education, workshops, certifications |
| Facility Maintenance and Utilities | 10% | Hospital infrastructure, electricity, water |
| Contingency and Emergency Fund | 10% | Pandemic response, disaster preparedness |
Budgeting in Nursing Services: Principles and Types
Budgeting in nursing services is a financial planning process that ensures the effective allocation of resources to provide high-quality patient care while maintaining cost-efficiency. It helps in planning for staffing, medical supplies, training, equipment, and operational expenses in hospitals, community health settings, and nursing education institutions.
A well-structured budget helps optimize financial resources, improve decision-making, and enhance the sustainability of nursing services.
Principles of Budgeting in Nursing Services
A well-planned nursing budget should follow key financial and operational principles to ensure effective resource utilization and financial sustainability.
| Principle | Description |
|---|---|
| 1. Flexibility | The budget should be adjustable to accommodate unforeseen changes, such as healthcare emergencies or staffing shortages. |
| 2. Accountability | Nursing administrators must ensure responsible spending and maintain transparent financial records. |
| 3. Cost-Effectiveness | Budgeting decisions should focus on maximizing patient care quality while minimizing waste. |
| 4. Efficiency | Resources should be optimally allocated to avoid overstaffing or shortages of essential supplies. |
| 5. Forecasting and Planning | Budgeting should be based on historical data, current trends, and future healthcare needs. |
| 6. Prioritization | Critical areas such as staffing, infection control, and patient safety should receive top priority in budget allocation. |
| 7. Equity | Financial resources should be distributed fairly across various nursing units and departments. |
| 8. Realism | Budget estimates should be practical and based on actual needs, avoiding overestimation or underestimation. |
| 9. Sustainability | The budget should ensure long-term financial stability while meeting short-term healthcare needs. |
| 10. Compliance | Budgeting should align with hospital financial policies, government regulations, and accreditation requirements. |
Types of Budgets in Nursing Services
There are several types of budgets used in nursing and healthcare settings to ensure efficient management of staffing, medical supplies, and operational expenses.
1. Operating Budget
- Covers day-to-day expenses required for nursing operations.
- Includes salaries, patient care supplies, utilities, and administrative costs.
- Example: Annual budget for nursing salaries, gloves, IV fluids, and electricity bills.
✔ Key Components:
- Nursing staff salaries
- Medical and surgical supplies
- Maintenance costs (laundry, electricity, water)
- Medication costs
2. Capital Budget
- Allocates funds for long-term investments such as new equipment, facility upgrades, and technology.
- Focuses on purchasing or upgrading assets that last several years.
- Example: Buying ventilators, installing an electronic health record (EHR) system, or constructing a new ICU unit.
✔ Key Components:
- New hospital infrastructure (ward expansion, new nursing stations)
- Equipment purchases (MRI machines, dialysis units)
- Information technology (EHR, telemedicine systems)
3. Personnel Budget
- Covers nursing workforce expenses, including salaries, benefits, overtime pay, and recruitment.
- Ensures adequate staffing levels to meet patient care demands.
- Example: Hiring 50 new registered nurses (RNs) and providing performance bonuses.
✔ Key Components:
- Staff salaries and benefits
- Nurse recruitment and retention programs
- Overtime pay
4. Supply and Equipment Budget
- Allocates funds for medical and non-medical supplies needed in nursing care.
- Example: Budget for syringes, wound dressings, PPE kits, and sterilization equipment.
✔ Key Components:
- Disposable medical supplies (gloves, masks, syringes)
- Non-medical supplies (cleaning agents, office supplies)
- Sterilization and waste management equipment
5. Training and Education Budget
- Covers continuing education, training workshops, and certifications for nurses.
- Example: Allocating funds for nurses to attend ACLS/BLS certification courses.
✔ Key Components:
- Continuing nursing education (CNE) programs
- Specialty training (ICU, oncology, pediatric nursing)
- Leadership and professional development workshops
6. Contingency Budget (Emergency Budget)
- Maintains reserve funds for unexpected events such as pandemics, natural disasters, or economic downturns.
- Ensures that nursing services can continue without financial disruption during emergencies.
- Example: Emergency funding for additional PPE and ventilators during COVID-19.
✔ Key Components:
- Disaster preparedness funds
- Emergency stock of medical supplies
- Additional staffing resources for crisis situations
7. Zero-Based Budget (ZBB)
- Requires every nursing department to justify all expenses before approval.
- Helps eliminate unnecessary costs and improve financial efficiency.
- Example: Reviewing every expense in a nursing unit and cutting non-essential costs.
✔ Key Components:
- Justifying the necessity of all nursing expenses
- Eliminating outdated or unnecessary programs
- Reallocating funds to critical nursing services
8. Performance-Based Budget
- Funds are allocated based on nursing service performance and patient outcomes.
- Hospitals measure success using KPIs (Key Performance Indicators), such as reduced infection rates or improved patient satisfaction scores.
- Example: Increasing budget for nursing quality improvement programs after achieving a 20% reduction in hospital-acquired infections.
✔ Key Components:
- Incentives for achieving nursing performance goals
- Funding for quality improvement projects
- Reward-based budgeting for well-performing nursing departments
9. Flexible Budget
- Adjusts financial planning based on patient volumes and healthcare demands.
- Example: Increasing nursing staff budget during flu season due to higher patient admissions.
✔ Key Components:
- Adjustable funding for staffing and medical supplies
- Emergency funds for seasonal outbreaks
- Resources for fluctuating healthcare demands
Steps for Budget Preparation in Nursing Services
Step 1: Assess Financial Needs
- Identify staffing, equipment, and supply requirements.
- Analyze past financial reports and trends.
Step 2: Define Budget Priorities
- Allocate funds to critical areas (e.g., infection control, training).
- Prioritize patient safety and high-quality care.
Step 3: Estimate Revenues and Expenses
- Consider expected revenues from insurance payments, government funding, or private contributions.
- Forecast fixed and variable costs.
Step 4: Allocate Funds and Develop Budget Plans
- Divide funds across nursing departments, training programs, and operational expenses.
- Ensure budget aligns with hospital policies and regulations.
Step 5: Implement and Monitor the Budget
- Track monthly and quarterly expenses to ensure compliance.
- Make adjustments based on emerging healthcare needs.
Step 6: Evaluate and Revise the Budget Annually
- Conduct financial performance reviews and adjust the budget for the next year.
- Incorporate feedback from nursing staff and financial audits.
Budgeting in nursing services ensures financial stability, efficient resource utilization, and high-quality patient care. By implementing principles of accountability, cost-effectiveness, and strategic planning, healthcare institutions can optimize nursing services while managing expenses effectively.
Different types of budgets serve various functions, from daily operational expenses to long-term capital investments. A well-structured budget, combined with continuous monitoring and evaluation, ensures sustainable nursing service delivery.
Budget Proposal for Nursing Services
A budget proposal for nursing services is a structured financial plan that outlines estimated income, expenses, and resource allocation required to ensure efficient, high-quality nursing care. It serves as a blueprint for funding requests and justifies why specific budget allocations are necessary for staffing, equipment, supplies, training, and operational improvements.
This document is typically prepared by nursing administrators, finance teams, and hospital management to secure funding from hospital boards, government agencies, or private organizations.
Key Components of a Nursing Service Budget Proposal
| Section | Description |
|---|---|
| 1. Executive Summary | Overview of the proposal, including key objectives and financial requirements. |
| 2. Budget Justification | Explanation of why the requested budget is necessary for improving patient care. |
| 3. Cost Estimates | Detailed breakdown of projected expenses (salaries, supplies, equipment, training, etc.). |
| 4. Revenue Sources | Identifies potential funding sources (hospital funding, government grants, insurance reimbursements). |
| 5. Budget Allocation | Specifies how funds will be distributed among different nursing services. |
| 6. Expected Outcomes | Describes how the proposed budget will improve healthcare quality, patient safety, and staff efficiency. |
| 7. Monitoring and Evaluation Plan | Outlines how expenses will be tracked and measured for efficiency. |
1. Executive Summary
Proposal Title: Nursing Service Budget Proposal for FY 2025
Prepared By: [Your Name / Nursing Administration Team]
Date: [Submission Date]
Objective: To secure funding for nursing operations, improve patient care quality, and enhance nursing workforce efficiency.
Key Budget Highlights:
- Total Requested Budget: $5,000,000
- Key Areas of Investment:
- Nursing staff salaries and recruitment: $2,500,000
- Medical supplies and equipment: $1,200,000
- Training and professional development: $500,000
- Facility maintenance and utilities: $500,000
- Emergency/contingency funds: $300,000
2. Budget Justification
The nursing department requires additional funding to:
- Address nurse shortages by hiring and retaining skilled professionals.
- Upgrade medical equipment and supplies to improve patient care quality.
- Enhance continuing education and training programs to meet healthcare standards.
- Maintain infection control measures to reduce hospital-acquired infections.
- Ensure compliance with healthcare regulations and accreditation standards.
3. Cost Estimates (Projected Expenses)
| Category | Estimated Budget ($) | Justification |
|---|---|---|
| Nursing Staff Salaries & Benefits | $2,500,000 | To cover salaries, overtime, and new hiring for critical care areas. |
| Medical Supplies & Equipment | $1,200,000 | For purchasing PPE, wound care kits, IV fluids, syringes, and monitoring devices. |
| Training & Education | $500,000 | To fund workshops, certifications (ACLS, BLS), and continuing education programs. |
| Facility Maintenance & Utilities | $500,000 | For hospital infrastructure, cleaning services, water, and electricity. |
| Emergency & Contingency Fund | $300,000 | To prepare for pandemics, disasters, or unexpected emergencies. |
| Total Budget Request | $5,000,000 | Comprehensive funding for nursing services and improvements. |
4. Revenue Sources
Funding will be obtained through:
- Hospital operating funds: $3,000,000
- Government healthcare grants: $1,200,000
- Insurance reimbursements: $500,000
- Private donations and partnerships: $300,000
5. Budget Allocation by Department
| Department | Budget Allocation ($) | Purpose |
|---|---|---|
| Intensive Care Unit (ICU) | $1,200,000 | Nurse salaries, ventilators, critical care supplies. |
| Emergency Department (ED) | $1,000,000 | Trauma care resources, emergency medications. |
| Maternity & Neonatal Care | $800,000 | Infant incubators, delivery kits, maternity ward expansion. |
| General Medical-Surgical Units | $1,500,000 | Staffing, infection control, and patient monitoring equipment. |
| Community Nursing & Home Care | $500,000 | Public health programs, vaccination drives, and home care nursing. |
6. Expected Outcomes
With the proposed budget, we anticipate:
✅ 15% increase in nurse staffing levels, reducing patient-nurse ratio.
✅ 20% reduction in hospital-acquired infections through better equipment and training.
✅ Higher patient satisfaction scores due to improved nurse response time.
✅ More skilled nursing workforce through advanced training programs.
✅ Improved healthcare infrastructure ensuring better working conditions for nurses.
7. Monitoring and Evaluation Plan
To ensure efficient budget utilization:
✔ Quarterly financial audits will be conducted to track spending.
✔ Nursing performance indicators (e.g., patient recovery rates, infection control) will be monitored.
✔ Nurse feedback surveys will be collected to assess improvements in working conditions.
✔ Mid-year budget reviews will help adjust funding allocations based on actual needs.
This Nursing Service Budget Proposal outlines the necessary funding and strategic financial allocation required to enhance patient care, nurse workforce, and hospital efficiency. Approval of this proposal will ensure sustainable and high-quality nursing services, benefiting both patients and healthcare professionals.
🔹 Next Steps: We seek budget approval and are open to discussions for modifications or additional funding sources.
Prepared by:
[Your Name]
[Designation]
[Hospital Name]
[Date]
Benefits of a Budget Proposal in Nursing Services
✔ Ensures financial accountability and proper resource allocation.
✔ Improves nurse staffing and retention, leading to better patient care.
✔ Supports training and development, enhancing professional skills.
✔ Justifies financial requests with data-driven planning.
✔ Strengthens emergency preparedness through contingency funds.
Cost-Benefit Analysis (CBA) in Nursing Service Planning
Cost-Benefit Analysis (CBA) is a financial evaluation technique used in nursing service planning to compare the costs of implementing a program or intervention with its expected benefits. It helps healthcare administrators and nursing managers determine whether a particular nursing initiative is financially justifiable and beneficial in improving patient care and operational efficiency.
CBA ensures that resources are allocated efficiently while maximizing quality patient care and cost savings.
Definition of Cost-Benefit Analysis (CBA) in Nursing
Cost-Benefit Analysis (CBA) is a decision-making tool that compares the total costs of a nursing service or intervention with its expected financial and qualitative benefits.
✔ If benefits outweigh the costs, the project is financially viable.
✔ If costs exceed benefits, adjustments or alternative strategies may be needed.
Objectives of Cost-Benefit Analysis in Nursing
- Optimize financial resource allocation for nursing programs.
- Justify budget requests by demonstrating return on investment (ROI).
- Ensure cost-effective healthcare delivery while maintaining quality standards.
- Support evidence-based decision-making in nursing services.
- Reduce unnecessary expenses while improving patient safety and efficiency.
Key Steps in Conducting Cost-Benefit Analysis for Nursing Services
Step 1: Identify the Nursing Initiative or Program
Determine the nursing service, intervention, or project to be evaluated.
📌 Example: Implementing a hospital-acquired infection (HAI) prevention program.
Step 2: Estimate the Total Costs
Calculate all direct and indirect costs associated with the program.
📌 Example Costs for an HAI Prevention Program:
| Cost Category | Estimated Cost ($) |
|---|---|
| Staff training on hand hygiene | $100,000 |
| Purchase of hand sanitizers and PPE | $80,000 |
| Infection surveillance system | $50,000 |
| Nurse workload adjustments | $40,000 |
| Total Cost | $270,000 |
Step 3: Estimate the Expected Benefits
Calculate financial and qualitative benefits such as:
✔ Reduction in hospital readmissions
✔ Savings from reduced patient complications
✔ Increased nurse productivity
📌 Example Benefits for HAI Prevention Program:
| Benefit Category | Estimated Savings ($) |
|---|---|
| Reduction in hospital-acquired infections (saves treatment costs) | $500,000 |
| Decreased patient length of stay | $150,000 |
| Reduced medication costs for infection management | $100,000 |
| Increased patient satisfaction and hospital reputation | Qualitative Benefit |
| Total Benefits | $750,000 |
Step 4: Calculate the Cost-Benefit Ratio
Formula:
Cost-Benefit Ratio=Total BenefitsTotal Costs\text{Cost-Benefit Ratio} = \frac{\text{Total Benefits}}{\text{Total Costs}}
📌 Example Calculation: 750,000270,000=2.78\frac{750,000}{270,000} = 2.78
✔ Since the cost-benefit ratio is greater than 1, the project is financially viable and cost-effective.
Interpreting Cost-Benefit Analysis Results
| Cost-Benefit Ratio | Decision |
|---|---|
| > 1.0 | Benefits outweigh costs → Project is cost-effective ✅ |
| = 1.0 | Costs and benefits are equal → Project is neutral 🔄 |
| < 1.0 | Costs exceed benefits → Project may not be justified ❌ |
Types of Costs and Benefits in Nursing Services
1. Types of Costs in Nursing Services
✔ Direct Costs – Expenses directly related to patient care.
✔ Indirect Costs – Overhead expenses supporting nursing services.
✔ Fixed Costs – Costs that do not change with patient volume.
✔ Variable Costs – Costs that fluctuate with patient demand.
📌 Examples of Costs in Nursing Services:
- Salaries and wages (nurses, support staff).
- Medical supplies (IV fluids, wound dressings, PPE).
- Training and education (CNE programs, workshops).
- Facility maintenance (hospital infrastructure, electricity).
- Technology investments (EHR systems, telemedicine).
2. Types of Benefits in Nursing Services
✔ Financial Benefits – Direct savings and revenue increases.
✔ Quality Benefits – Improvements in patient safety and care.
✔ Operational Benefits – Enhanced efficiency and workflow.
✔ Social Benefits – Positive impact on the community.
📌 Examples of Benefits in Nursing Services:
- Reduction in hospital-acquired infections → Cost savings on treatments.
- Faster patient recovery → Increased bed availability for new patients.
- Higher nurse retention → Lower recruitment costs.
- Improved patient safety → Fewer malpractice claims.
- Better community health → Decreased burden on hospitals.
Cost-Benefit Analysis Example in Nursing
Case Study: Telehealth Implementation in Nursing
A hospital considers investing $500,000 in a telehealth system to reduce unnecessary hospital visits and improve remote patient care.
📌 Projected Costs:
| Expense Category | Estimated Cost ($) |
|---|---|
| Telehealth software & hardware | $300,000 |
| Staff training | $100,000 |
| IT support & maintenance | $100,000 |
| Total Cost | $500,000 |
📌 Projected Benefits:
| Benefit Category | Estimated Savings ($) |
|---|---|
| Reduction in unnecessary hospital visits | $400,000 |
| Lower readmission rates | $250,000 |
| Increased nurse efficiency | $150,000 |
| Improved patient access to care | Qualitative Benefit |
| Total Benefits | $800,000 |
📌 Cost-Benefit Ratio Calculation: 800,000500,000=1.6\frac{800,000}{500,000} = 1.6
✔ Since the ratio is greater than 1, the telehealth system is a financially sound investment.
Challenges in Conducting Cost-Benefit Analysis in Nursing
| Challenges | Solutions |
|---|---|
| Difficulty in quantifying qualitative benefits | Use patient satisfaction surveys and outcome measures. |
| Uncertainty in healthcare cost trends | Conduct risk assessments and sensitivity analysis. |
| Resistance to change in nursing workflow and technology | Implement staff training and gradual adaptation strategies. |
| High initial investment costs | Secure grants, public-private funding, or phased budget allocations. |
Cost-Benefit Analysis (CBA) is an essential tool in nursing service planning to ensure financially responsible decision-making while maintaining quality patient care. By comparing costs with projected benefits, nursing administrators can justify budget requests, optimize resource allocation, and improve healthcare efficiency.
A well-executed CBA helps in strategic planning, enhances patient outcomes, and ensures financial sustainability in nursing services.
Planning Hospital and Patient Care Unit (Ward) in Nursing Services
Planning a hospital and patient care unit (ward) is a critical process in nursing services to ensure efficient patient care, proper resource utilization, and staff management. A well-designed hospital layout and ward organization enhance patient safety, workflow efficiency, infection control, and comfort for both patients and healthcare professionals.
Proper planning includes infrastructure design, staffing requirements, equipment allocation, and workflow optimization, making healthcare delivery seamless and effective.
Objectives of Hospital and Ward Planning
- Ensure Efficient Patient Care Delivery – Proper layout and organization reduce delays and improve accessibility.
- Enhance Infection Control and Safety – Design considerations prevent cross-contamination and improve hygiene.
- Optimize Staff Workflow – Nurses can efficiently monitor and care for patients.
- Improve Patient Comfort and Experience – Ensuring adequate ventilation, lighting, privacy, and safety.
- Ensure Adequate Resource Allocation – Plan for necessary medical equipment, beds, and emergency provisions.
- Enhance Emergency Preparedness – Enable quick response to critical situations and disasters.
- Comply with Healthcare Regulations and Standards – Meet national and international hospital accreditation criteria.
Key Considerations for Hospital Planning
1. Hospital Location and Infrastructure
✔ Accessibility – Proximity to transportation, ambulance services, and emergency response units.
✔ Space and Expansion Possibilities – Future-proof design for expansion and upgradation.
✔ Structural Safety – Earthquake-resistant buildings, fire safety measures, and disaster preparedness.
✔ Environmental Considerations – Adequate ventilation, natural lighting, and noise control.
2. Hospital Layout and Departmental Distribution
| Department | Purpose | Key Considerations |
|---|---|---|
| Emergency Department (ER) | Immediate care for critically ill or injured patients. | Rapid access, triage areas, resuscitation bays. |
| Intensive Care Unit (ICU) | Continuous monitoring of critically ill patients. | Advanced equipment, 1:1 nurse-patient ratio. |
| General Wards | Hospitalization for stable patients. | Segregation by gender, diagnosis, and care needs. |
| Maternity Ward | Care for pregnant women, labor, and postnatal care. | Neonatal care unit, labor rooms, emergency C-section area. |
| Operation Theaters (OTs) | Surgical procedures. | Sterile environment, recovery rooms, anesthesia setup. |
| Outpatient Department (OPD) | Diagnosis and treatment for non-admitted patients. | Consultation rooms, diagnostic labs, pharmacy. |
| Pharmacy & Laboratory | Medicine and diagnostic support. | Adequate storage for essential drugs and equipment. |
Planning a Patient Care Unit (Ward)
A patient care unit (ward) is a dedicated hospital section for admitted patients requiring medical care. Proper ward planning ensures efficient patient management, infection control, and optimal nursing care.
1. Types of Wards in a Hospital
| Ward Type | Purpose |
|---|---|
| General Ward | Shared patient beds, cost-effective healthcare. |
| Private Ward | Individual rooms for patients who need privacy. |
| Semi-Private Ward | Two or more patients in a room. |
| Isolation Ward | For infectious diseases such as TB, COVID-19. |
| ICU (Intensive Care Unit) | For critically ill patients needing 24/7 monitoring. |
| Pediatric Ward | Specialized care for infants and children. |
| Geriatric Ward | Care for elderly patients with chronic illnesses. |
| Maternity Ward | For pregnant women, labor, and postnatal care. |
2. Layout and Design of a Patient Care Unit (Ward)
A well-planned ward layout enhances patient care, infection control, and workflow efficiency.
✔ Key Areas in a Ward:
- Nurses’ Station – Centralized location for nurse monitoring.
- Patient Beds – Arranged in an optimal layout (parallel, circular, single-row, or cubicles).
- Handwashing Stations – For infection prevention.
- Medication Storage Area – For safe drug administration.
- Emergency Equipment Space – Defibrillators, oxygen cylinders, crash carts.
📌 Example: Ideal Ward Layout Plan
✔ Nurses’ station at the center for easy patient monitoring.
✔ 20-30 beds per ward, arranged for easy accessibility.
✔ Proper lighting, ventilation, and noise control to enhance comfort.
✔ Separate entry/exit for infection control and emergency access.
3. Staffing Requirements for a Patient Care Unit
Proper nurse staffing ensures safe, effective, and efficient patient care.
| Ward Type | Recommended Nurse-Patient Ratio |
|---|---|
| General Ward | 1:6 – 1:8 |
| ICU | 1:1 – 1:2 |
| Maternity Ward | 1:3 – 1:4 |
| Pediatric Ward | 1:3 |
| Emergency Room | 1:2 – 1:4 |
✔ Staffing Plan:
- Head Nurse – Oversees ward operations.
- Registered Nurses (RNs) – Direct patient care, medication administration.
- Nurse Assistants – Support tasks like hygiene, mobility, and feeding.
- Ward Clerks – Manage patient records and documentation.
- Housekeeping Staff – Maintain hygiene and cleanliness.
Infection Control Measures in Ward Planning
✔ Hand Hygiene Stations – Every ward should have handwashing sinks and sanitizers.
✔ Isolation Rooms – Designated areas for contagious patients.
✔ Proper Ventilation – Reduces airborne infections.
✔ Medical Waste Disposal – Follow biomedical waste management protocols.
✔ Disinfection Protocols – Regular cleaning of patient areas, beds, and equipment.
Technology Integration in Hospital and Ward Planning
- Electronic Health Records (EHRs) – Digital patient record management.
- Automated Bed Management Systems – Optimize patient flow and reduce waiting times.
- Telemedicine Services – Remote patient monitoring and consultation.
- Smart Nurse Call Systems – Patients can alert nurses when needed.
- IoT-Based Monitoring Systems – Track vital signs and alert for emergencies.
Budgeting for Hospital and Patient Care Unit Planning
📌 Estimated Budget Breakdown:
| Category | Estimated Budget ($) |
|---|---|
| Hospital Construction & Renovation | $50,000,000 |
| Medical Equipment & Beds | $15,000,000 |
| Staffing & Salaries | $30,000,000 |
| Nursing Training & Education | $5,000,000 |
| Technology & IT Systems | $10,000,000 |
| Infection Control & Waste Management | $3,000,000 |
| Total Estimated Budget | $113,000,000 |
✔ Funding Sources:
- Government Health Programs
- Private Investments & Hospital Revenues
- Healthcare Grants & Charitable Donations
Challenges in Hospital and Ward Planning & Solutions
| Challenges | Solutions |
|---|---|
| Limited Budget and Resources | Seek government grants, private funding, and cost-cutting measures. |
| Nurse Shortages | Implement nurse recruitment and retention programs. |
| Overcrowding in Wards | Improve bed management and patient flow systems. |
| Infection Control Issues | Strict hand hygiene and isolation protocols. |
| Technological Adaptation Barriers | Provide training and support for nurses on digital systems. |
A well-planned hospital and patient care unit ensures efficient nursing workflows, better patient outcomes, and improved hospital functionality. By focusing on optimal space utilization, infection control, technology integration, and staffing needs, hospitals can enhance patient safety, nurse productivity, and healthcare service quality.
Planning for Emergency and Disaster in Nursing Services
Emergency and disaster planning in nursing services is essential to ensure preparedness, response, recovery, and mitigation of health crises. A well-structured emergency plan ensures that nurses and healthcare workers can respond effectively to disasters such as pandemics, natural disasters, mass casualties, bioterrorism, and hospital emergencies.
Disaster preparedness involves risk assessment, resource allocation, staff training, emergency protocols, and recovery strategies to minimize loss of life and ensure continuity of healthcare services.
Objectives of Emergency and Disaster Planning in Nursing Services
- Ensure Rapid and Effective Response – Establish protocols for immediate action during emergencies.
- Minimize Casualties and Mortality Rates – Provide life-saving interventions and triage.
- Optimize Resource Utilization – Ensure sufficient medical supplies, equipment, and personnel.
- Enhance Coordination – Strengthen communication and collaboration among healthcare teams, government agencies, and emergency responders.
- Improve Staff Readiness – Conduct regular training, drills, and simulations for emergency response.
- Maintain Hospital Operations – Ensure continuity of care and infrastructure resilience during disasters.
- Comply with National and International Disaster Guidelines – Align with WHO, CDC, FEMA, and national disaster management protocols.
Types of Emergencies and Disasters in Healthcare
1. Natural Disasters
✔ Earthquakes, Floods, Hurricanes, Tsunamis – Cause infrastructure damage, injuries, and mass casualties.
✔ Extreme Heat and Cold Waves – Lead to heatstroke, hypothermia, and dehydration.
2. Man-Made Disasters
✔ Terrorist Attacks and Explosions – Result in mass casualties and trauma cases.
✔ Fires and Industrial Accidents – Cause burn injuries and toxic exposure.
✔ Biological and Chemical Attacks – Require decontamination and mass treatment.
3. Health-Related Disasters
✔ Pandemics (COVID-19, H1N1, Ebola) – Cause overwhelming patient influx, PPE shortages.
✔ Hospital Acquired Infections (HAIs) – Require strict infection control protocols.
✔ Mass Casualty Incidents (MCIs) – Need rapid triage and critical care services.
Key Components of Emergency and Disaster Planning in Nursing Services
| Component | Description |
|---|---|
| 1. Risk Assessment & Hazard Identification | Identifies potential threats and their impact on hospital services. |
| 2. Emergency Response Plan | Establishes protocols for handling various types of disasters. |
| 3. Triage and Patient Management | Implements mass casualty triage (START method, color coding). |
| 4. Resource Allocation & Stockpile Management | Ensures adequate supply of medical resources, PPE, ventilators, medications. |
| 5. Training and Simulation Drills | Conducts regular disaster response training and hospital-wide drills. |
| 6. Communication and Coordination Plan | Strengthens internal and external communication networks (radio, telemedicine, emergency lines). |
| 7. Evacuation and Shelter Planning | Establishes patient evacuation routes, designated safe zones, and emergency shelters. |
| 8. Recovery and Post-Disaster Evaluation | Implements post-crisis mental health support and system evaluation. |
1. Risk Assessment & Hazard Identification
Before planning, hospitals must conduct hazard assessments to identify potential emergencies and their impact.
✔ Hazard Vulnerability Assessment (HVA) – Identifies hospital weaknesses and preparedness levels.
✔ Risk Categorization:
- High-Risk – Earthquakes, Terrorist Attacks, Pandemics.
- Moderate-Risk – Seasonal Flooding, Heatwaves.
- Low-Risk – Power Outages, IT System Failures.
2. Emergency Response Plan (ERP) for Nursing Services
✔ Emergency Activation Procedures
- Who declares an emergency? (Hospital Disaster Committee)
- Who is in charge? (Emergency Nurse Coordinator, Medical Officer)
- What immediate actions are taken? (Triage, Resource Mobilization)
✔ Code-Based Response System (Hospital Emergency Codes)
| Code Name | Emergency Type | Nursing Actions |
|---|---|---|
| Code Blue | Cardiac Arrest | Perform CPR, defibrillation, advanced life support. |
| Code Red | Fire | Evacuate patients, call fire response team. |
| Code Yellow | Mass Casualty | Activate triage, allocate staff to critical areas. |
| Code Black | Bomb Threat | Secure hospital perimeters, initiate evacuation. |
| Code White | Violence in Hospital | De-escalate situation, involve security. |
| Code Orange | Hazardous Material Spill | Wear PPE, contain spill, prevent exposure. |
✔ Incident Command System (ICS) – Defines roles and responsibilities for disaster response:
- Hospital Disaster Coordinator – Oversees hospital-wide emergency response.
- Nursing Team Leader – Coordinates nurse deployment in critical areas.
- Logistics Team – Manages medical supply inventory and transport.
3. Triage and Patient Management During Disasters
✔ START Triage (Simple Triage and Rapid Treatment)
- Red (Immediate) – Life-threatening but treatable (severe bleeding, shock).
- Yellow (Delayed) – Serious but stable injuries (fractures, burns).
- Green (Minor) – Walking wounded (minor cuts, sprains).
- Black (Expectant/Deceased) – No chance of survival.
📌 Example Triage in a Mass Casualty Incident:
| Patient Condition | Triage Color Code | Nursing Action |
|---|---|---|
| Unconscious, No Pulse | Black | Provide comfort, document case. |
| Severe Burns, Responsive | Red | Immediate treatment, transfer to ICU. |
| Fractured Leg, Stable Vitals | Yellow | Stabilize, monitor, delayed surgery. |
| Small Laceration, No Bleeding | Green | First aid, discharge after observation. |
4. Resource Allocation & Stockpile Management
Hospitals must maintain emergency stockpiles of:
✔ Medications – Painkillers, antibiotics, antivirals.
✔ PPE – Masks, gloves, gowns, face shields.
✔ Ventilators and Oxygen Supply – For respiratory crises.
✔ Emergency Beds and Tents – In case of overflow patients.
✔ Disaster Response Kits – Trauma kits, burn dressings, IV fluids.
5. Training and Simulation Drills for Nurses
✔ Annual disaster drills to test hospital response.
✔ CPR, trauma management, and triage training for nurses.
✔ Fire safety and evacuation drills.
✔ Collaboration with paramedics and first responders.
6. Communication and Coordination Plan
✔ Internal Hospital Communication:
- Dedicated Emergency Command Center (ECC) for crisis management.
- Walkie-talkies, satellite phones, mobile apps for coordination.
✔ External Coordination: - Ambulance services, Red Cross, police, fire department.
- Government disaster response teams and NGOs.
7. Evacuation and Shelter Planning
✔ Hospital Evacuation Plans – Clearly marked exit routes, staircases, and assembly points.
✔ Alternative Care Sites – Tents, mobile clinics, and field hospitals.
8. Recovery and Post-Disaster Evaluation
✔ Debriefing sessions – Identify strengths and weaknesses in disaster response.
✔ Mental health support – For patients, families, and frontline workers.
✔ Policy updates – Revise disaster plans based on evaluation findings.
Emergency and disaster planning in nursing services ensures rapid response, minimizes loss of life, and enhances hospital preparedness. By implementing triage systems, training programs, and efficient resource management, hospitals can effectively handle disasters and continue providing critical care.