Unit-1-NML-Health care and developmentof nursing services in India
Current Health Care Delivery System in India

India has a vast and complex healthcare delivery system designed to cater to its large and diverse population. The healthcare system is structured into multiple levels, ranging from primary to tertiary care, and is provided by both public and private sectors.
1. Levels of Health Care Delivery System in India
India’s health care delivery system is categorized into three levels:
A. Primary Health Care
Primary health care is the first level of contact between individuals and the healthcare system. It focuses on preventive, promotive, and basic curative services.
Key Components:
- Sub-centres (SCs) – The first point of contact in rural areas. Each SC covers about 5,000 people (3,000 in hilly/tribal areas) and is manned by an Auxiliary Nurse Midwife (ANM) and a Multipurpose Health Worker (MPHW).
- Primary Health Centres (PHCs) – Covers about 30,000 people in plain areas and 20,000 in hilly areas. It serves as a referral unit for sub-centres and has doctors, nurses, and paramedics.
- Community Health Centres (CHCs) – Covers about 1,20,000 people in plain areas and 80,000 in hilly areas. CHCs serve as referral units for PHCs and provide specialized services.
Services Provided at Primary Level:
- Maternal and child health services (antenatal and postnatal care)
- Immunization programs
- Family planning services
- Management of common illnesses (malaria, tuberculosis, diarrhea)
- Basic health education and sanitation programs
B. Secondary Health Care
Secondary health care is provided at the district and sub-district levels, offering more specialized medical services.
Key Components:
- District Hospitals – These are referral hospitals for CHCs, providing specialized services like surgery, gynecology, pediatrics, and orthopedics.
- Sub-District/Taluk Hospitals – Located at the sub-divisional level, catering to the needs of nearby PHCs and CHCs.
Services Provided at Secondary Level:
- Emergency care and minor surgeries
- Management of complicated pregnancies and deliveries
- Specialist consultations
- Basic laboratory and diagnostic services
C. Tertiary Health Care
Tertiary care provides advanced medical services and super-specialty care at regional and national levels.
Key Components:
- Medical Colleges & Teaching Hospitals – These are high-end referral institutions offering specialized medical care and training for medical professionals.
- Super-Specialty Hospitals – These include institutions such as AIIMS, PGIMER, NIMHANS, and private corporate hospitals providing specialized services in cardiology, neurology, oncology, and organ transplants.
Services Provided at Tertiary Level:
- Complex surgical procedures (e.g., heart surgery, organ transplantation)
- Advanced cancer treatment (chemotherapy, radiotherapy)
- Super-specialty care in neurology, nephrology, cardiology, etc.
- High-tech diagnostic facilities (MRI, CT scan, PET scan)
2. Public and Private Health Care System
A. Public Health Care System
The government provides healthcare services through its network of PHCs, CHCs, and district hospitals. Major government initiatives include:
- Ayushman Bharat (PM-JAY) – World’s largest health insurance scheme covering hospitalization costs for economically weaker sections.
- National Health Mission (NHM) – Focuses on maternal and child health, non-communicable diseases, and strengthening health infrastructure.
- Integrated Disease Surveillance Programme (IDSP) – Monitors and controls outbreaks of communicable diseases.
- Universal Immunization Programme (UIP) – Provides free vaccinations to children and pregnant women.
B. Private Health Care System
The private sector plays a significant role in India’s healthcare delivery, providing about 70% of outpatient care and 60% of inpatient care. It includes:
- Corporate hospitals (e.g., Apollo, Fortis, Max Healthcare)
- Private nursing homes and clinics
- Diagnostic centers and laboratories
- Pharmaceutical and biotechnology industries
Challenges with Private Health Care:
- Expensive treatment leading to high out-of-pocket expenditures
- Unequal access in rural and urban areas
- Ethical concerns regarding over-prescription and unnecessary procedures
3. Key Health Programs in India
India has several health programs aimed at improving public health and achieving Universal Health Coverage (UHC):
- Ayushman Bharat – Pradhan Mantri Jan Arogya Yojana (AB-PMJAY) – Provides free hospitalization coverage up to ₹5 lakh per family per year.
- Reproductive, Maternal, Newborn, Child, and Adolescent Health (RMNCH+A) – Focuses on maternal and child healthcare services.
- National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases, and Stroke (NPCDCS) – Addresses the growing burden of non-communicable diseases.
- Rashtriya Bal Swasthya Karyakram (RBSK) – Early detection and intervention for child health issues.
- Janani Suraksha Yojana (JSY) – Encourages institutional deliveries to reduce maternal and infant mortality.
4. Challenges in the Indian Health Care Delivery System
Despite progress, India’s healthcare system faces several challenges:
A. Infrastructure and Manpower Shortages
- Shortage of doctors, nurses, and allied healthcare workers
- Insufficient number of hospitals and diagnostic centers in rural areas
- Poor maintenance and lack of medical equipment in government hospitals
B. High Out-of-Pocket Expenditure
- Nearly 60% of healthcare costs in India are borne by individuals, leading to financial burdens.
C. Rural-Urban Disparity
- Quality healthcare is more accessible in urban areas compared to rural regions.
D. Disease Burden
- Rising burden of non-communicable diseases (NCDs) like diabetes, heart disease, and cancer
- Re-emergence of communicable diseases like tuberculosis and vector-borne diseases (malaria, dengue)
E. Poor Health Insurance Coverage
- Though Ayushman Bharat covers millions, a significant portion of the population remains uninsured.
F. Lack of Preventive Care Focus
- Greater emphasis on curative care than preventive measures like lifestyle modifications and vaccinations.
5. Recent Developments and Future Directions
A. Digital Health Initiatives
- National Digital Health Mission (NDHM) – Creating digital health records for all citizens.
- Telemedicine & e-Sanjeevani – Online consultation services for rural populations.
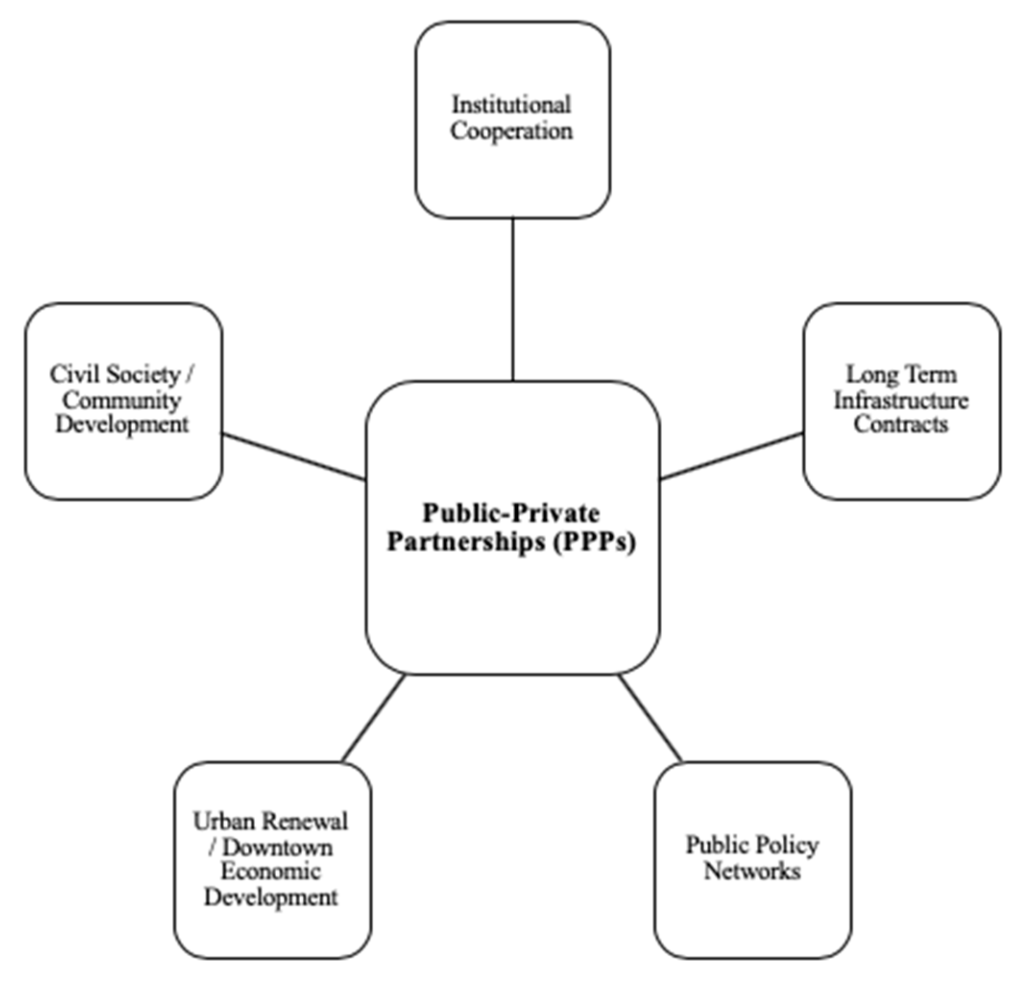
B. Strengthening Public-Private Partnerships (PPP)
- Encouraging collaboration between the government and private sector to improve healthcare services.
C. Expansion of Health Insurance
- Enhancing the reach of PM-JAY and state-specific health insurance schemes.
D. Focus on Strengthening Primary Health Care
- Establishing more Health and Wellness Centres (HWCs) under Ayushman Bharat.
E. Strengthening Medical Education and Workforce
- Opening new AIIMS institutions and increasing medical college seats.
Public-Private Partnership (PPP) in Healthcare in India
1.Public-Private Partnership (PPP) in Healthcare
Public-Private Partnership (PPP) is a collaborative model where the government (public sector) partners with private entities to provide healthcare services efficiently. The aim is to leverage private sector expertise, technology, and investment while ensuring accessibility and affordability through government intervention.
Why PPP in Healthcare?
- To bridge the gap in healthcare infrastructure and service delivery.
- To reduce the financial burden on the government.
- To improve efficiency through private sector expertise.
- To enhance accessibility in rural and underserved areas.
2. Models of Public-Private Partnership in Healthcare
There are various models of PPP in healthcare, depending on the level of government involvement and private sector participation.
A. Build-Operate-Transfer (BOT) Model
- Private companies build healthcare facilities, operate them for a specific period, and then transfer them to the government.
- Example: Establishment of hospitals under Viability Gap Funding (VGF).
B. Management Contract Model
- Private sector manages and operates government-owned hospitals and facilities.
- Example: Private agencies managing district hospitals under National Health Mission (NHM).
C. Joint Venture Model
- Government and private companies jointly invest in infrastructure and operations.
- Example: AIIMS partnering with corporate hospitals for super-specialty services.
D. Service Delivery Model
- Private players provide specific healthcare services while the government funds or regulates them.
- Example: Telemedicine services in rural areas through PPP.
E. Lease Model
- Government leases healthcare facilities to private players for a defined period.
- Example: Leasing diagnostic centers in government hospitals.
F. Voucher Scheme Model
- The government provides health service vouchers to economically weaker sections, redeemable at private hospitals.
- Example: Chiranjeevi Yojana in Gujarat for maternal health services.
3. Key Public-Private Partnership Initiatives in India
Several successful PPP models have been implemented in India to improve healthcare services:
A. National Health Mission (NHM) and PPP
- NHM partners with private players for services like ambulance services (108 Emergency Ambulance) and diagnostic services.
B. Ayushman Bharat (PM-JAY) and Private Sector Collaboration
- Private hospitals provide cashless treatment to insured individuals under PM-JAY (Pradhan Mantri Jan Arogya Yojana).
C. Janani Suraksha Yojana (JSY) and Private Hospitals
- The government reimburses private hospitals for maternal and child healthcare services.
D. Telemedicine Projects
- e-Sanjeevani Telemedicine Service – A government initiative in collaboration with private telemedicine companies to provide remote healthcare.
E. Chiranjeevi Yojana in Gujarat
- The government funds private hospitals for free maternal care to reduce maternal mortality rate (MMR).
F. Free Dialysis under PPP
- Pradhan Mantri National Dialysis Programme (PMNDP) allows free dialysis services at private hospitals under government funding.
4. Benefits of Public-Private Partnership in Healthcare
A. Improved Infrastructure
- Private sector investment leads to better hospitals, clinics, and diagnostic centers.
B. Cost-Effective Services
- PPP ensures that treatment remains affordable while maintaining quality.
C. Accessibility in Rural Areas
- Private hospitals extend healthcare services to remote and rural populations.
D. Technology and Innovation
- Use of advanced medical technology, telemedicine, AI-driven diagnostics, and e-health records.
E. Reduced Burden on Government Hospitals
- Diverts patient load to private hospitals while maintaining affordability.
5. Challenges of PPP in Healthcare
A. Regulatory Issues
- Ensuring quality standards and ethical practices in private healthcare institutions.
B. Financial Sustainability
- Government funding is not always timely, leading to financial risks for private players.
C. Unequal Distribution
- Most private healthcare facilities are in urban areas, leaving rural regions underserved.
D. Risk of Commercialization
- Private hospitals may prioritize profit over patient welfare, leading to unnecessary treatments.
E. Monitoring and Accountability
- Need for strict government regulation to ensure transparency and avoid corruption.
6. Future Scope and Recommendations for PPP in Healthcare
A. Strengthening Regulations
- Better monitoring systems to ensure compliance with healthcare standards.
- Implement strict pricing regulations for PPP healthcare services.
B. Encouraging Rural Healthcare Investment
- Offering tax benefits and incentives for private players to set up hospitals in rural areas.
C. Expanding Digital Health Initiatives
- Enhancing telemedicine partnerships for remote consultations.
- Strengthening National Digital Health Mission (NDHM) for e-health records.
D. Improving Health Insurance Integration
- Expanding PM-JAY coverage to more private hospitals.
- Strengthening state-level health insurance PPP programs.
E. Capacity Building and Training
- PPP should focus on training healthcare workers, nurses, and paramedics to improve healthcare delivery.
Planning and Development of Nursing Services and Education at Global and National Levels
Nursing services and education are fundamental components of the healthcare system, ensuring the availability of skilled professionals to provide quality patient care. Over the years, the planning and development of nursing services and education have evolved globally and nationally to meet the increasing healthcare demands, technological advancements, and workforce shortages. Both international and national organizations, including the World Health Organization (WHO), International Council of Nurses (ICN), and Indian Nursing Council (INC), have been instrumental in shaping nursing education and practice to meet the challenges of modern healthcare.
1. Global Scenario of Nursing Services and Education
Globally, nursing services and education have undergone significant transformations to address healthcare disparities, meet the growing burden of diseases, and ensure quality healthcare delivery.
1.1 Global Planning for Nursing Services
A. WHO Global Strategic Directions for Nursing and Midwifery (2021–2025)
The WHO has formulated strategic directions to enhance nursing and midwifery services worldwide. These include:
- Education – Strengthening nursing curricula and ensuring quality education aligned with global standards.
- Leadership – Promoting nurses in leadership roles for healthcare policymaking.
- Employment – Expanding job opportunities and improving working conditions for nurses.
- Service Delivery – Enhancing nurses’ roles in primary healthcare and community settings.
B. Role of the International Council of Nurses (ICN)
The ICN works towards:
- Strengthening nursing education, workforce policies, and professional practice standards.
- Advocating for nurses’ rights, leadership roles, and fair wages.
- Supporting research and innovation in nursing.
C. Nursing and the Sustainable Development Goals (SDGs)
- SDG 3: Good Health and Well-being – Nursing services are vital for reducing maternal and infant mortality, preventing communicable diseases, and improving healthcare accessibility.
- SDG 5: Gender Equality – Promoting equal opportunities for women in nursing leadership.
- SDG 8: Decent Work and Economic Growth – Ensuring fair pay and safe working conditions for nurses.
D. Global Workforce Challenges
- Shortage of Nurses – The WHO estimates a shortage of 5.9 million nurses globally.
- Workforce Migration – Many nurses from developing countries migrate to developed nations, leading to a crisis in home countries.
- Workplace Burnout – High workload, stress, and inadequate mental health support contribute to burnout.
1.2 Global Planning for Nursing Education
A. Standardization of Nursing Education
- WHO and ICN emphasize competency-based curricula to ensure high standards of nursing education.
- Global recognition of nursing degrees allows nurses to work across different healthcare systems.
B. Technological Advancements in Nursing Education
- Simulation-based training using Virtual Reality (VR) and Artificial Intelligence (AI).
- E-learning platforms such as Coursera, edX, and WHO OpenWHO offer global access to nursing education.
C. Nursing Specializations
- Nurse Practitioners (NPs), Clinical Nurse Specialists (CNS), Nurse Anesthetists, and Nurse Educators are gaining importance globally.
D. Research and Evidence-Based Practice (EBP)
- Emphasis on research-based nursing practices to improve patient care outcomes.
2. National Scenario of Nursing Services and Education in India
India has made significant progress in the planning and development of nursing services and education through government policies, initiatives, and infrastructure development.
2.1 Planning and Development of Nursing Services in India
A. National Health Policies Supporting Nursing Services
- National Health Policy 2017: Focuses on strengthening nursing roles in primary healthcare.
- Ayushman Bharat Program: Nurses are crucial in delivering healthcare services at Health and Wellness Centers (HWCs).
- National Rural Health Mission (NRHM) and National Urban Health Mission (NUHM): Promote nursing services in rural and urban areas.
B. Regulatory Bodies for Nursing in India
- Indian Nursing Council (INC) – Regulates nursing education and practice standards.
- State Nursing Councils – Manage licensure and professional development.
- NITI Aayog and MoHFW – Formulate policies to improve nursing workforce conditions.
C. Expansion of Nursing Workforce
- Increased recruitment under Community Health Officer (CHO) roles in primary healthcare.
- Strengthening Advanced Nurse Practitioners (ANPs) to reduce dependence on doctors.
D. Public-Private Partnerships (PPP) in Nursing Services
- Collaborations with private hospitals, NGOs, and global organizations to enhance healthcare service delivery.
2.2 Planning and Development of Nursing Education in India
A. Growth of Nursing Education Institutions
- Increased nursing colleges under AIIMS, State Government, and Private Institutions.
- Expansion of ANM, GNM, B.Sc. Nursing, M.Sc. Nursing, and Ph.D. programs.
B. Revised Nursing Curriculum (2020)
- Competency-Based Learning: Focus on clinical skills, critical thinking, and ethical practices.
- Integration of Digital Learning: AI-driven education, telemedicine training, and virtual simulations.
C. Research and Innovation in Nursing
- Growth in nursing research institutes for policy development and academic advancements.
D. National Digital Health Mission (NDHM)
- Training nurses in electronic health records (EHRs), telemedicine, and e-health services.
3. Challenges in Nursing Services and Education
3.1 Challenges in Nursing Services
- Shortage of Nurses – India has 1.7 nurses per 1,000 population (WHO recommends 3 per 1,000).
- Rural-Urban Disparity – Healthcare facilities are urban-centric, while rural areas face workforce shortages.
- Burnout and Mental Health Issues – Long working hours, staff shortages, and inadequate wages impact nurses’ well-being.
- Limited Career Growth – Need for more leadership roles and professional recognition.
3.2 Challenges in Nursing Education
- Shortage of Nursing Faculty – Many institutions face a lack of qualified educators.
- Infrastructure Issues – Need for advanced labs, research facilities, and clinical exposure.
- High Cost of Education – Private nursing colleges charge high tuition fees, making it unaffordable for many.
- Lack of Practical Training – Many students lack exposure to real-life clinical scenarios.
4. Future Directions in Nursing Services and Education
A. Strengthening the Nursing Workforce
- Recruitment drives to meet the growing demand.
- Better salary structures and mental health support for nurses.
B. Enhancing Nursing Education
- Expanding scholarships and funding for nursing students.
- More simulation-based learning and competency-based training.
C. Digital Transformation in Nursing
- AI and Virtual Reality (VR) in nursing education.
- Telehealth and mobile health (mHealth) training for nurses.
D. Global Collaboration for Nursing Development
- Exchange programs and mutual recognition of Indian nursing degrees in global institutions.
- Public-Private Partnerships (PPP) to improve research, education, and service delivery.
E. Strengthening Leadership and Research
Expanding Ph.D. programs and nursing research institutions.
Encouraging nurses in policymaking roles.
Recent Trends and Issues in Nursing Service and Management

Nursing services and management are evolving rapidly due to advancements in healthcare, changes in patient demographics, technological innovations, and policy reforms. These trends impact patient care, workforce management, and healthcare delivery. This document explores the recent trends and issues in nursing service and management, covering technological advancements, leadership roles, ethical challenges, and workforce concerns.
1. Recent Trends in Nursing Service and Management
Several emerging trends are transforming the nursing profession and healthcare systems globally and nationally.
A. Technological Advancements in Nursing
- Electronic Health Records (EHRs) and Digital Documentation
- Nurses are now required to use electronic health records (EHRs) to document patient care efficiently.
- Reduces paperwork and improves communication between healthcare providers.
- Telemedicine and Telehealth Services
- Remote healthcare services allow nurses to monitor patients virtually, provide consultations, and offer home-based care.
- Used extensively during the COVID-19 pandemic and continues to be a growing field.
- Artificial Intelligence (AI) in Nursing
- AI-powered systems assist in diagnosis, medication administration, and patient monitoring.
- AI-based chatbots are being used for triage and patient education.
- Wearable Health Technologies
- Devices like smartwatches, biosensors, and fitness trackers help in real-time monitoring of vital signs, glucose levels, and cardiac activity.
- Nurses use these devices for patient data tracking and early warning systems.
- Simulation-Based Learning in Nursing Education
- Virtual Reality (VR) and Augmented Reality (AR) are enhancing nursing education through simulation-based training.
- Helps in practicing complex procedures in a risk-free environment.
B. Evolving Roles and Specializations in Nursing
- Advanced Practice Nursing (APN)
- Increased demand for Nurse Practitioners (NPs), Clinical Nurse Specialists (CNS), Nurse Anesthetists, and Nurse Midwives.
- NPs are taking over some physician roles, particularly in primary care.
- Expansion of Community Health Nursing
- Focus on preventive healthcare, chronic disease management, and home-based care.
- Community Health Officers (CHOs) are being integrated into primary healthcare.
- Geriatric and Palliative Care Nursing
- Due to aging populations, there is a rising demand for geriatric and palliative care nurses.
- End-of-life care and pain management have become critical nursing responsibilities.
- Mental Health Nursing Expansion
- Increased focus on mental health awareness, psychiatric nursing, and psychological support for patients.
- Nurses are being trained in counseling and crisis intervention.
- Globalization and Nursing Migration
- Increased demand for Indian nurses in USA, UK, Canada, Middle East, and Australia.
- Standardization of NCLEX-RN, OET, and IELTS to facilitate international job placements.
C. Leadership and Management Trends in Nursing
- Nursing Informatics and Data-Driven Decision-Making
- Nurses are being trained in informatics to use data for patient care planning, quality improvement, and policy development.
- Evidence-Based Practice (EBP) in Nursing
- Emphasis on scientific research and clinical guidelines to improve patient care outcomes.
- Interdisciplinary Collaboration and Team-Based Care
- Nurses are working alongside doctors, pharmacists, physiotherapists, and social workers for holistic patient care.
- Restructuring Nursing Education and Training
- Adoption of competency-based training models and lifelong learning programs.
- Introduction of blended learning models (online + practical training).
2. Key Issues in Nursing Service and Management
Despite advancements, several challenges persist in nursing services and management.
A. Nursing Workforce Shortages
- Global and National Shortage of Nurses
- WHO reports a shortage of 5.9 million nurses globally.
- In India, there are 1.7 nurses per 1,000 people (WHO recommends 3 per 1,000).
- High Nurse-to-Patient Ratio
- Overburdened nurses face physical and mental exhaustion.
- Leads to burnout, stress, and reduced patient safety.
- Migration of Nurses to Developed Countries
- Many skilled Indian nurses migrate abroad due to better salaries, working conditions, and career opportunities.
- Causes a shortage of experienced nurses in India.
B. Ethical and Legal Challenges
- Ethical Dilemmas in Patient Care
- Nurses often face end-of-life care decisions, organ donation concerns, and patient confidentiality issues.
- Violence and Harassment Against Nurses
- Increased incidents of physical and verbal abuse from patients and their families.
- Workplace safety laws are being implemented, but enforcement remains weak.
- Legal Liabilities and Medical Negligence
- Nurses are held accountable for medication errors, misdiagnoses, and improper documentation.
- Need for legal awareness and training in handling medico-legal cases.
C. Work Environment and Job Dissatisfaction
- Long Working Hours and Poor Working Conditions
- Nurses work 12 to 16-hour shifts due to staffing shortages.
- Leads to stress, fatigue, and reduced efficiency.
- Low Salaries and Limited Career Growth
- In India, government nurses earn ₹40,000 to ₹70,000 per month, while private hospital salaries are lower.
- Lack of promotions and leadership opportunities lead to job dissatisfaction.
- Mental Health and Burnout
- COVID-19 increased psychological stress among nurses.
- Many nurses report depression, anxiety, and PTSD symptoms.
D. Gaps in Nursing Education and Training
- Outdated Nursing Curriculum
- Need for revision to include modern healthcare technologies, AI, and robotic nursing.
- Shortage of Nursing Educators
- Many nursing colleges lack qualified faculty, affecting education quality.
- Lack of Practical Exposure
- Need for simulation labs and clinical training facilities.
3. Future Directions in Nursing Service and Management
A. Strengthening the Nursing Workforce
- Government initiatives to recruit more nurses and improve nurse-to-patient ratios.
- Higher salaries and better working conditions to retain nurses in India.
B. Digitalization of Nursing Services
- EHR training and AI-based clinical decision-making.
- Expansion of telemedicine services for remote healthcare delivery.
C. Promoting Nurse Leadership
- Encouraging nurses in hospital administration and policymaking roles.
- More scholarships and funding for higher education in nursing.
D. Enhancing Research and Evidence-Based Nursing
- Increased focus on nursing research centers and Ph.D. programs.
- Encouraging nurses to participate in clinical trials and public health research.
E. Strengthening Mental Health Support for Nurses
- Providing mental health counseling and stress management programs.
- Ensuring workplace safety and reducing nurse burnout.