BSC SEM 1 UNIT 8 APPLIED NUTRITION AND DIETETICS
UNIT 8 Nutritional deficiency disorders
Nutritional Deficiency Disorders:

1. Introduction to Nutritional Deficiency Disorders
Nutritional deficiency disorders occur due to an inadequate intake, absorption, or utilization of essential nutrients. These deficiencies can lead to a wide range of health problems, affecting growth, immunity, metabolism, and organ function.
2. Types of Nutrients and Their Deficiencies
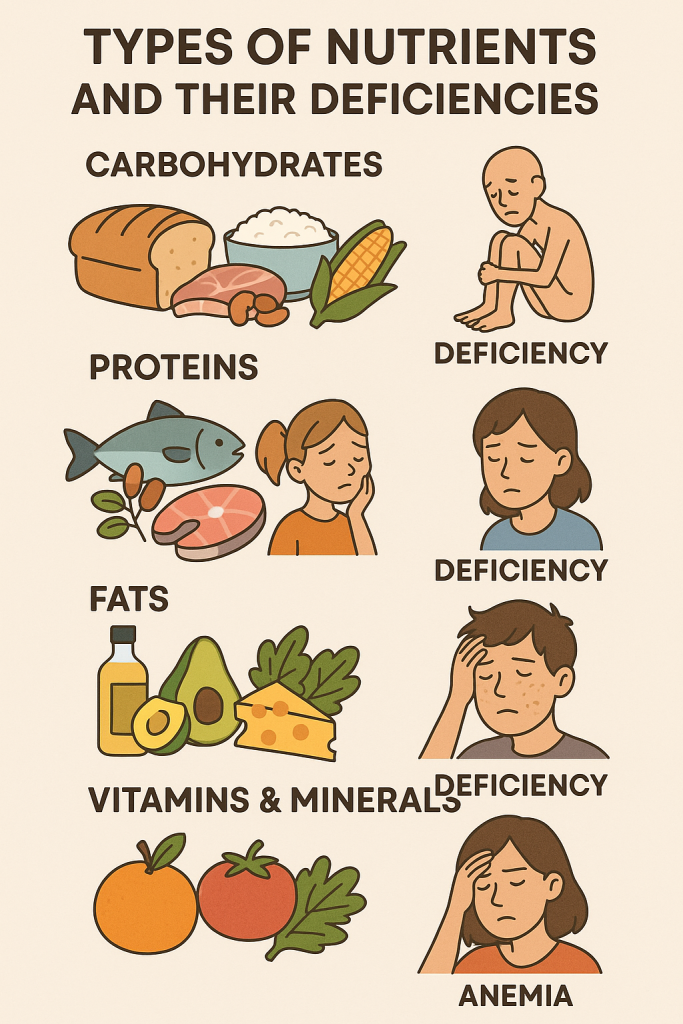
A. Macronutrient Deficiencies
Macronutrients provide energy and include carbohydrates, proteins, and fats.
1. Protein-Energy Malnutrition (PEM)
PEM results from inadequate intake of proteins and calories. It is common in children and affects growth and immunity.
Types:
- Kwashiorkor: Protein deficiency with adequate calorie intake.
- Symptoms: Edema, muscle wasting, hepatomegaly, flaky paint dermatitis, moon face.
- Marasmus: Severe calorie and protein deficiency.
- Symptoms: Extreme weight loss, muscle wasting, wrinkled skin, lethargy.
Prevention & Management:
- Balanced diet with adequate protein (meat, fish, eggs, legumes, dairy).
- Nutritional rehabilitation and supplementation.
B. Micronutrient Deficiencies
Micronutrients include vitamins and minerals essential for body functions.
2. Vitamin Deficiencies
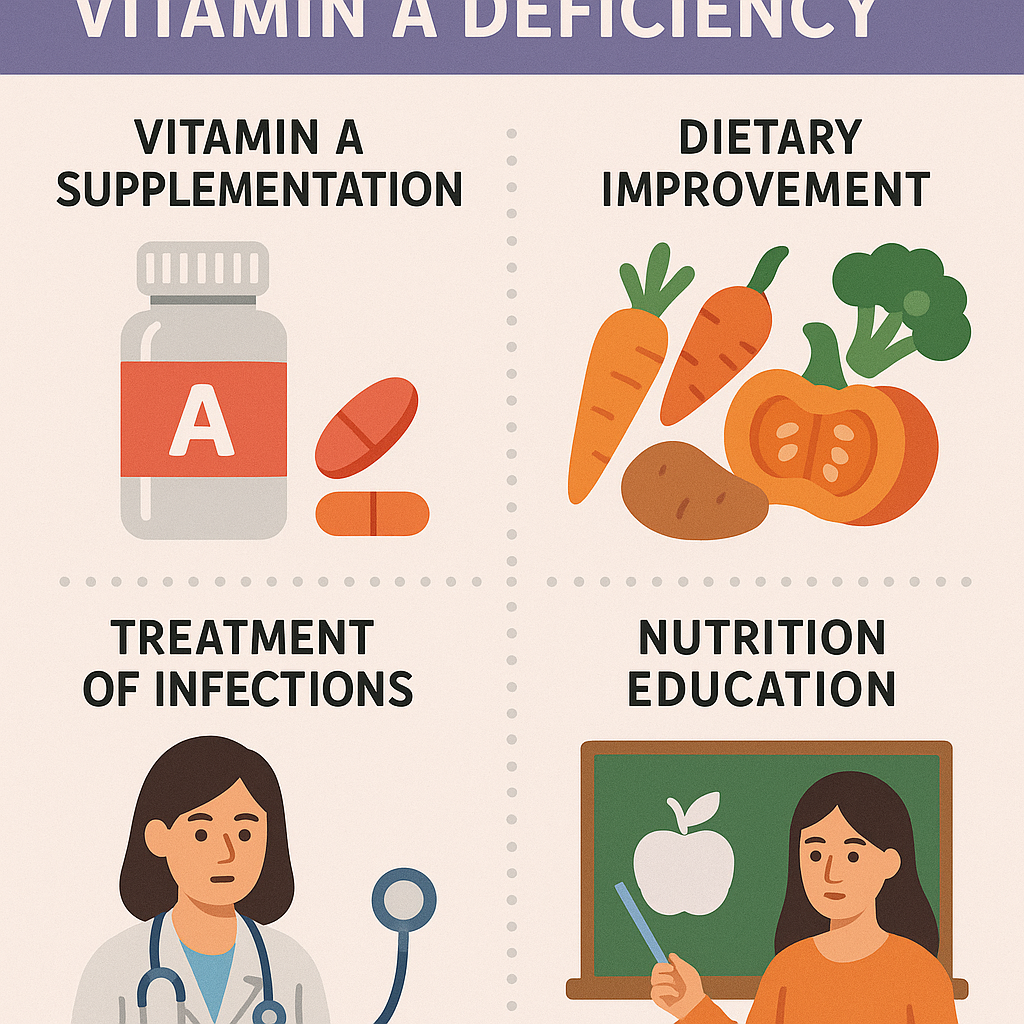
a) Vitamin A Deficiency (VAD)
- Function: Important for vision, immunity, and skin health.
- Deficiency Symptoms:
- Night blindness (Nyctalopia)
- Xerophthalmia (dryness of eyes)
- Bitot’s spots (foamy patches in the eye)
- Keratomalacia (softening of the cornea)
- Sources: Carrots, sweet potatoes, leafy greens, liver, fish oil.
- Prevention: Vitamin A supplementation, fortified foods.
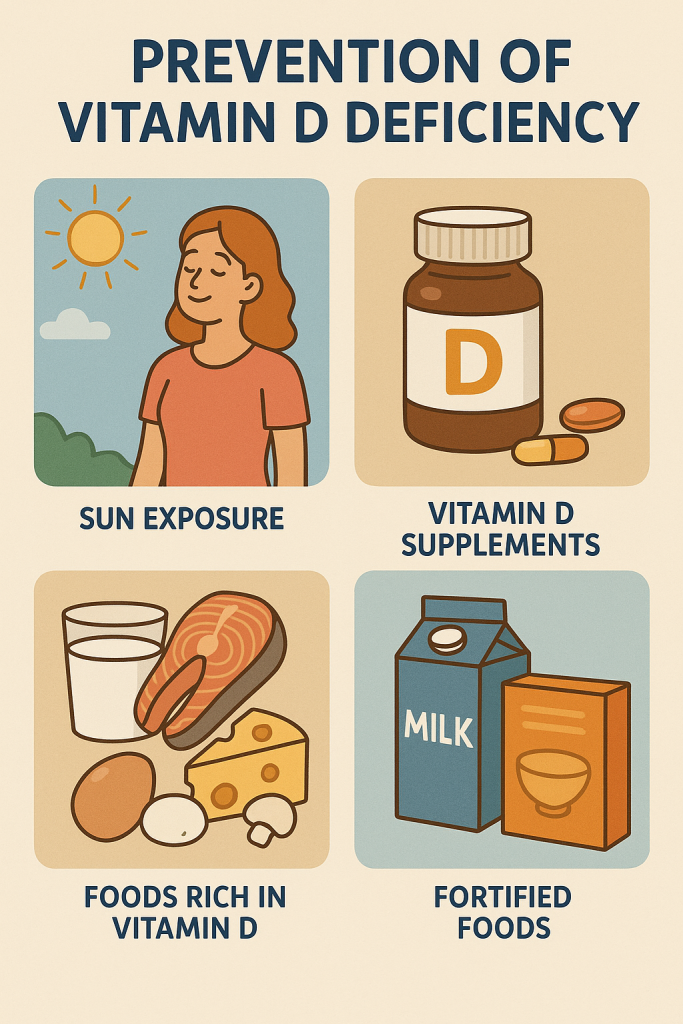
b) Vitamin D Deficiency
- Function: Essential for calcium absorption and bone health.
- Deficiency Symptoms:
- Rickets (children): Bowed legs, bone deformities.
- Osteomalacia (adults): Bone pain, muscle weakness.
- Sources: Sunlight, fortified milk, fish, egg yolk.
- Prevention: Sun exposure, fortified foods, Vitamin D supplements.
c) Vitamin E Deficiency
- Function: Antioxidant, protects cells.
- Deficiency Symptoms:
- Neuromuscular disorders, hemolytic anemia.
- Sources: Nuts, seeds, vegetable oils, green leafy vegetables.
d) Vitamin K Deficiency
- Function: Essential for blood clotting.
- Deficiency Symptoms:
- Excessive bleeding, easy bruising.
- Sources: Leafy greens, broccoli, liver.
- Prevention: Vitamin K-rich diet, supplementation in newborns.
e) Vitamin C Deficiency (Scurvy)
- Function: Collagen synthesis, immune function.
- Deficiency Symptoms:
- Bleeding gums, delayed wound healing, joint pain.
- Sources: Citrus fruits, tomatoes, bell peppers.
- Prevention: Vitamin C-rich diet.
f) Vitamin B-Complex Deficiencies
- Vitamin B1 (Thiamine) Deficiency (Beriberi)
- Symptoms: Muscle weakness, nerve damage, heart failure.
- Sources: Whole grains, nuts, meat.
- Vitamin B2 (Riboflavin) Deficiency
- Symptoms: Cracked lips, sore throat, skin rashes.
- Sources: Dairy, eggs, green vegetables.
- Vitamin B3 (Niacin) Deficiency (Pellagra)
- Symptoms: 3 D’s – Dermatitis, Diarrhea, Dementia.
- Sources: Meat, fish, peanuts.
- Vitamin B6 (Pyridoxine) Deficiency
- Symptoms: Irritability, depression, anemia.
- Sources: Bananas, nuts, whole grains.
- Vitamin B12 Deficiency (Pernicious Anemia)
- Symptoms: Fatigue, weakness, nerve damage.
- Sources: Meat, eggs, dairy.
3. Mineral Deficiencies
a) Iron Deficiency (Anemia)
- Function: Essential for hemoglobin synthesis.
- Deficiency Symptoms:
- Fatigue, pale skin, dizziness, shortness of breath.
- Sources: Meat, spinach, legumes, fortified cereals.
- Prevention: Iron supplements, iron-rich diet.
b) Iodine Deficiency (Goiter)
- Function: Required for thyroid hormone production.
- Deficiency Symptoms:
- Goiter (enlarged thyroid), hypothyroidism, cretinism (in infants).
- Sources: Iodized salt, seafood, dairy.
- Prevention: Use of iodized salt.
c) Calcium Deficiency
- Function: Bone and teeth health.
- Deficiency Symptoms:
- Weak bones, osteoporosis, muscle spasms.
- Sources: Dairy, green leafy vegetables, fortified foods.
d) Zinc Deficiency
- Function: Immune function, wound healing.
- Deficiency Symptoms:
- Growth retardation, hair loss, poor wound healing.
- Sources: Meat, nuts, dairy.
e) Magnesium Deficiency
- Function: Muscle and nerve function.
- Deficiency Symptoms:
- Muscle cramps, irregular heartbeat.
- Sources: Nuts, seeds, whole grains.
3. Causes of Nutritional Deficiencies
- Poor diet: Lack of variety, processed foods.
- Malabsorption disorders: Celiac disease, Crohn’s disease.
- Increased nutrient needs: Pregnancy, lactation, childhood.
- Chronic illnesses: Diabetes, kidney disease.
- Alcoholism: Poor nutrient absorption.
- Poverty and food insecurity: Limited access to nutritious food.
4. Diagnosis and Management
A. Diagnosis
- Clinical examination: Symptoms like pale skin, stunted growth.
- Blood tests: Hemoglobin (for anemia), Vitamin D levels, thyroid function.
- Dietary history: Evaluating food intake.
- Imaging: Bone density scans for osteoporosis.
B. Management & Prevention
- Balanced Diet: Include all food groups.
- Supplementation: Multivitamins, iron, calcium.
- Fortified Foods: Iodized salt, fortified cereals.
- Public Health Programs:
- Midday meal scheme
- Vitamin A supplementation programs
- Iron and folic acid supplementation for pregnant women.
Protein Energy Malnutrition (PEM).
1. Introduction
Protein Energy Malnutrition (PEM) is a condition caused by a deficiency of proteins and calories in the diet. It primarily affects children in developing countries but can also occur in adults with chronic illnesses or severe malnutrition.
2. Magnitude of the Problem
Global Burden
- WHO estimates: Around 45 million children under 5 years suffer from wasting (severe acute malnutrition).
- PEM contributes to ~45% of all child deaths globally.
- Malnourished children have a 9–10 times higher risk of mortality from infections.
- Highest prevalence in: South Asia, Sub-Saharan Africa, and low-income countries.
Indian Scenario
- NFHS-5 (2020-21) Data:
- Stunting (low height for age): 35.5%
- Wasting (low weight for height): 19.3%
- Underweight (low weight for age): 32.1%
- States with High PEM Prevalence: Bihar, Jharkhand, Madhya Pradesh, Uttar Pradesh.
3. Causes of PEM
A. Primary Causes (Inadequate Intake)
- Poverty: Low socioeconomic status limits access to nutritious food.
- Poor maternal nutrition: Leads to low birth weight and stunted growth.
- Improper weaning practices: Early or late introduction of complementary feeding.
- Large family size: Divided food resources lead to malnutrition.
- Food insecurity: Unavailability of sufficient food.
B. Secondary Causes (Diseases and Conditions)
- Gastrointestinal infections: Chronic diarrhea reduces nutrient absorption.
- Parasitic infections: Hookworms, giardiasis cause nutrient loss.
- Chronic illnesses: Tuberculosis, HIV/AIDS increase metabolic demands.
- Malabsorption disorders: Celiac disease, Crohn’s disease.
- Frequent infections: Reduce appetite and nutrient absorption.
4. Classification of PEM
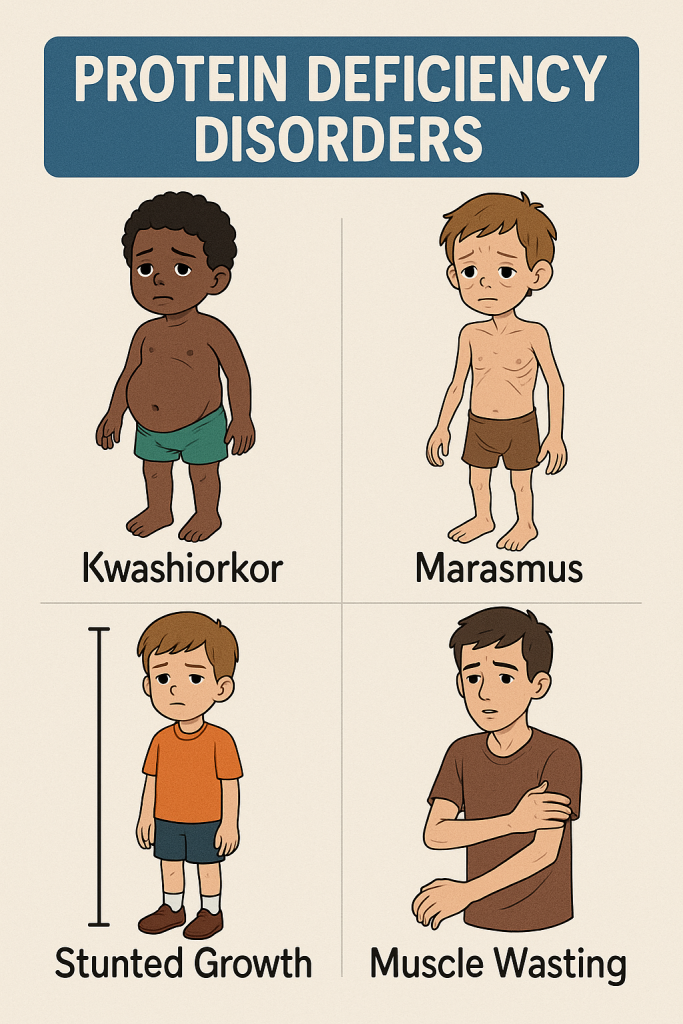
PEM is classified into two major types:
A. Kwashiorkor (“Edematous Malnutrition”)
- Cause: Severe protein deficiency with adequate calorie intake.
- Age Group: 1-3 years (after weaning from breast milk).
- Pathophysiology:
- Low albumin levels → Fluid leakage → Edema
- Fatty liver → Enlarged liver (hepatomegaly)
- Suppressed immune system → Increased infection risk.
Clinical Features of Kwashiorkor
✅ Edema (swollen legs, face, and feet)
✅ Moon face (puffy appearance)
✅ Flaky paint dermatitis (skin peeling)
✅ Hair changes (reddish-brown, brittle)
✅ Hepatomegaly (enlarged liver)
✅ Apathy & irritability
B. Marasmus (“Wasting Syndrome”)
- Cause: Severe deficiency of both calories and protein.
- Age Group: 6 months – 1 year (during breastfeeding or early weaning).
- Pathophysiology:
- Body uses fat & muscle for energy → Extreme weight loss
- Reduced immune function → High infection susceptibility.
Clinical Features of Marasmus
✅ Extreme thinness (“Bag of bones”)
✅ Muscle wasting (loss of fat and muscle)
✅ Wrinkled skin (due to fat loss)
✅ Sunken eyes & hollow cheeks
✅ Growth retardation
✅ Frequent infections (diarrhea, pneumonia)
Comparison: Kwashiorkor vs. Marasmus
| Feature | Kwashiorkor | Marasmus |
|---|---|---|
| Cause | Protein deficiency | Calorie & protein deficiency |
| Edema | Present | Absent |
| Weight loss | Mild to moderate | Severe |
| Appetite | Poor | Good |
| Hair changes | Yes | Yes |
| Fat loss | Minimal | Extreme |
| Muscle wasting | Moderate | Severe |
5. Diagnosis of PEM
Clinical Assessment
- Anthropometry:
- Weight-for-age: Underweight
- Height-for-age: Stunting
- Weight-for-height: Wasting
- Mid-upper arm circumference (MUAC):
- <11.5 cm (Severe malnutrition)
- 11.5 – 12.5 cm (Moderate malnutrition)
Laboratory Investigations
- Serum Albumin: Low in kwashiorkor.
- Complete Blood Count (CBC): Detects anemia.
- Electrolytes: Low potassium and sodium.
- Liver Function Test (LFTs): Fatty liver in kwashiorkor.
- Stool Examination: To rule out parasitic infections.
6. Management of PEM
A. Immediate Care (Treatment of Severe Cases)
- Stabilization Phase (First 7 Days)
- Treat dehydration using Rehydration Solution for Malnutrition (ReSoMal) (Not ORS).
- Correct hypoglycemia, hypothermia, and infections.
- Provide small, frequent feeds.
- Rehabilitation Phase (2-6 Weeks)
- Gradual introduction of calories & proteins (F-75, F-100 formulas).
- Micronutrient supplementation (Iron, Zinc, Vitamin A).
- Therapeutic Feeding using:
- Ready-to-Use Therapeutic Food (RUTF)
- Fortified milk-based diet
B. Long-term Nutritional Rehabilitation
- High-calorie, high-protein diet (eggs, milk, pulses, nuts).
- Deworming & infection control.
- Psychosocial support for mothers (Education on feeding practices).
7. Nurse’s Role in PEM Prevention & Management
✅ Early Identification & Screening
- Regular growth monitoring (weight, height, MUAC).
- Detect early signs of malnutrition.
✅ Nutritional Education
- Teach mothers about breastfeeding, complementary feeding.
- Promote balanced diets (fortified cereals, pulses, vegetables).
✅ Community Awareness Programs
- Conduct camps on maternal nutrition.
- Promote kitchen gardening for better food security.
✅ Hospital-Based Care
- Administer therapeutic feeds (F-75, F-100).
- Monitor hydration & electrolyte balance.
- Educate mothers on nutritious cooking practices.
✅ Public Health Initiatives
- Supplementary Nutrition Programs (Midday meals, ICDS scheme).
- Vitamin A supplementation.
- Food fortification programs (Iron-fortified rice, wheat).
8. Prevention of PEM
✅ Promote Exclusive Breastfeeding (0-6 months)
✅ Timely Introduction of Complementary Feeding (6 months onwards)
✅ Balanced Diet with Proteins & Calories
✅ Nutritional Supplementation for Pregnant & Lactating Mothers
✅ Improve Food Security & Hygiene Practices
Severe Acute Malnutrition (SAM).
1. Introduction
Severe Acute Malnutrition (SAM) is a life-threatening condition caused by extreme deficiency of calories and proteins. It primarily affects children under 5 years of age and is a major contributor to child morbidity and mortality worldwide.
- Global prevalence: ~45 million children suffer from wasting (WHO, 2023).
- High-risk regions: South Asia, Sub-Saharan Africa.
- India’s burden: According to NFHS-5 (2020-21):
- Wasting (low weight for height) – 19.3%
- Severe wasting (SAM) – 7.7%
- Stunting (low height for age) – 35.5%
2. Causes of Severe Acute Malnutrition (SAM)
A. Primary Causes (Dietary Deficiencies)
- Inadequate breastfeeding (early weaning, bottle feeding)
- Lack of nutritious complementary feeding after 6 months
- Food insecurity due to poverty
- Frequent infections reducing food intake
B. Secondary Causes (Disease-Related)
- Diarrhea → Nutrient loss & dehydration
- Parasitic infections (intestinal worms)
- Pneumonia, tuberculosis increasing energy demands
- Congenital conditions (e.g., cleft lip, metabolic disorders)
3. Clinical Features of SAM
A. Two Major Types of SAM
- Marasmus (“Wasting Syndrome”)
- Cause: Deficiency of calories and proteins.
- Symptoms: ✅ Severe weight loss (“Bag of bones”)
✅ Muscle wasting & loss of subcutaneous fat
✅ Sunken eyes, wrinkled skin
✅ Growth retardation
✅ Weak immune system → Frequent infections
- Kwashiorkor (“Edematous Malnutrition”)
- Cause: Severe protein deficiency with normal calorie intake.
- Symptoms: ✅ Bilateral pitting edema (swelling of feet, face, hands)
✅ Flaky paint dermatitis (skin peeling)
✅ Hepatomegaly (fatty liver)
✅ Hair changes (brittle, reddish-brown)
✅ Apathy, irritability
B. Associated Complications
- Hypoglycemia (low blood sugar) → Lethargy, seizures
- Hypothermia (low body temperature) → Cold extremities
- Severe anemia → Pallor, fatigue
- Electrolyte imbalance → Arrhythmias, weakness
- Weakened immunity → Pneumonia, tuberculosis, sepsis
4. Diagnosis of SAM
A. Anthropometric Measurements
✅ Mid-Upper Arm Circumference (MUAC):
- <11.5 cm → Severe malnutrition (SAM)
- 11.5-12.5 cm → Moderate malnutrition
✅ Weight-for-Height (WHO Growth Chart):
- Z-score < -3 SD → SAM
✅ Edema Assessment:
- Bilateral pitting edema → Kwashiorkor
B. Laboratory Tests
- Serum albumin (low in Kwashiorkor)
- Hemoglobin levels (to detect anemia)
- Blood sugar (hypoglycemia common in SAM)
- Electrolyte levels (low potassium & sodium)
- Stool microscopy (parasitic infections)
5. Management of SAM
A. Immediate Management (Critical Phase)
1. Treat Hypoglycemia
- First-line treatment: 50 ml of 10% dextrose orally
- If unconscious: IV 10% dextrose + normal saline
2. Correct Hypothermia
- Skin-to-skin contact (Kangaroo Mother Care)
- Warm room temperature
3. Treat Dehydration
- Use ReSoMal (Rehydration Solution for Malnutrition)
- Avoid ORS (as it has high sodium, worsening edema)
4. Treat Infections
- Empirical antibiotics:
- Amoxicillin or Ceftriaxone for infections
- Antiparasitic treatment if worms present
B. Nutritional Rehabilitation (Stabilization & Catch-up Growth)
✅ Dietary Support Using WHO Protocols
- F-75 Formula (first 7 days) – Low calorie, high electrolytes
- F-100 Formula (rehabilitation phase) – High protein, calorie-dense
- Ready-to-Use Therapeutic Food (RUTF) (Plumpy’Nut, BP-100)
✅ Micronutrient Supplementation
- Vitamin A (prevents blindness & infection)
- Iron & folic acid (given after treating infections)
- Zinc supplementation (for diarrhea)
- Deworming (Albendazole/Mebendazole)
✅ Gradual Introduction of Family Diet
- Mashed lentils, eggs, bananas, dairy-based foods
✅ Psychosocial Care
- Counseling parents about feeding & hygiene
- Encouraging breastfeeding up to 2 years
6. Nurse’s Role in SAM Management
A. Hospital-Based Care
✅ Early Identification
- Screen children using MUAC, growth charts
- Monitor weight gain & nutritional response
✅ Administer Therapeutic Feeds
- Prepare & feed F-75, F-100, RUTF
- Monitor for refeeding syndrome (electrolyte shifts)
✅ Manage Infections & Hydration
- Start antibiotics, ReSoMal for dehydration
- Prevent hypothermia & hypoglycemia
B. Community-Based Care
✅ Home-Based Nutritional Counseling
- Teach mothers proper feeding practices
- Promote exclusive breastfeeding for 6 months
✅ Community Growth Monitoring
- Conduct nutrition screening camps
- Provide micronutrient supplements (Vitamin A, Iron, Zinc)
✅ Public Health Programs
- Integrated Child Development Services (ICDS)
- National Nutrition Mission (Poshan Abhiyan)
- Mid-Day Meal Scheme
- Supplementary Nutrition Programs (Anganwadi centers)
7. Prevention of Severe Acute Malnutrition
✅ Exclusive Breastfeeding (0-6 months)
✅ Timely Complementary Feeding (from 6 months)
✅ Balanced Diet Rich in Proteins & Calories
✅ Food Fortification & Supplementation
✅ Hygiene & Safe Drinking Water (prevents infections)
✅ Growth Monitoring & Regular Health Checkups
Kwashiorkor.
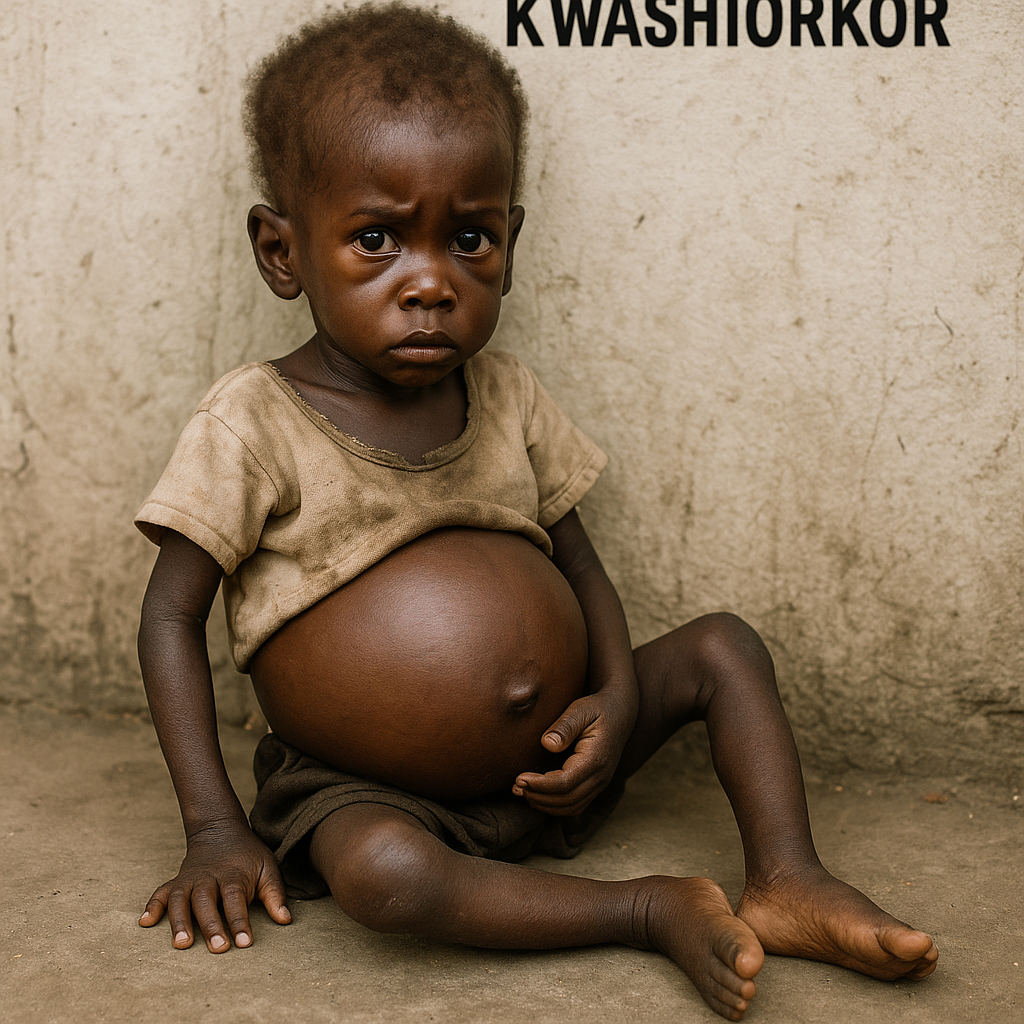
1. Introduction
Kwashiorkor is a form of severe acute malnutrition (SAM) caused by severe protein deficiency despite an adequate calorie intake. It primarily affects children aged 1-3 years in developing countries and is characterized by edema, skin changes, and a swollen belly. The term “Kwashiorkor” originates from Ghana and means “the disease the first child gets when the second child is born,” as it often occurs when a child is weaned off breast milk too early.
2. Magnitude of the Problem
Global Burden
- Approximately 45 million children under 5 years suffer from wasting (acute malnutrition) globally.
- Kwashiorkor prevalence: Most common in Africa, South Asia, and Southeast Asia.
- Contributes to 50% of childhood deaths related to malnutrition.
Indian Scenario (NFHS-5, 2020-21)
- Wasting (low weight for height): 19.3%
- Severe wasting (SAM, including Kwashiorkor): 7.7%
- Stunting (low height for age): 35.5%
- Underweight (low weight for age): 32.1%
- High prevalence in: Bihar, Jharkhand, Madhya Pradesh, Uttar Pradesh.
3. Causes of Kwashiorkor
A. Primary Causes (Nutritional Deficiencies)
- Lack of protein-rich foods (meat, eggs, dairy, legumes).
- Premature weaning (replacing breast milk with starchy foods).
- Food insecurity due to poverty and famine.
- Unbalanced diet (high in carbohydrates, low in proteins).
- Lack of education on proper infant nutrition.
B. Secondary Causes (Underlying Conditions)
- Chronic infections (tuberculosis, HIV/AIDS).
- Parasitic infestations (intestinal worms, giardiasis).
- Frequent diarrhea leading to nutrient loss.
- Liver disease affecting protein metabolism.
4. Pathophysiology of Kwashiorkor
- Severe protein deficiency → Hypoalbuminemia (low blood protein levels).
- Fluid retention (edema) due to low oncotic pressure.
- Fatty liver (hepatomegaly) due to impaired fat metabolism.
- Weakened immune system → High infection risk.
- Reduced melanin production → Skin and hair changes.
5. Clinical Features of Kwashiorkor
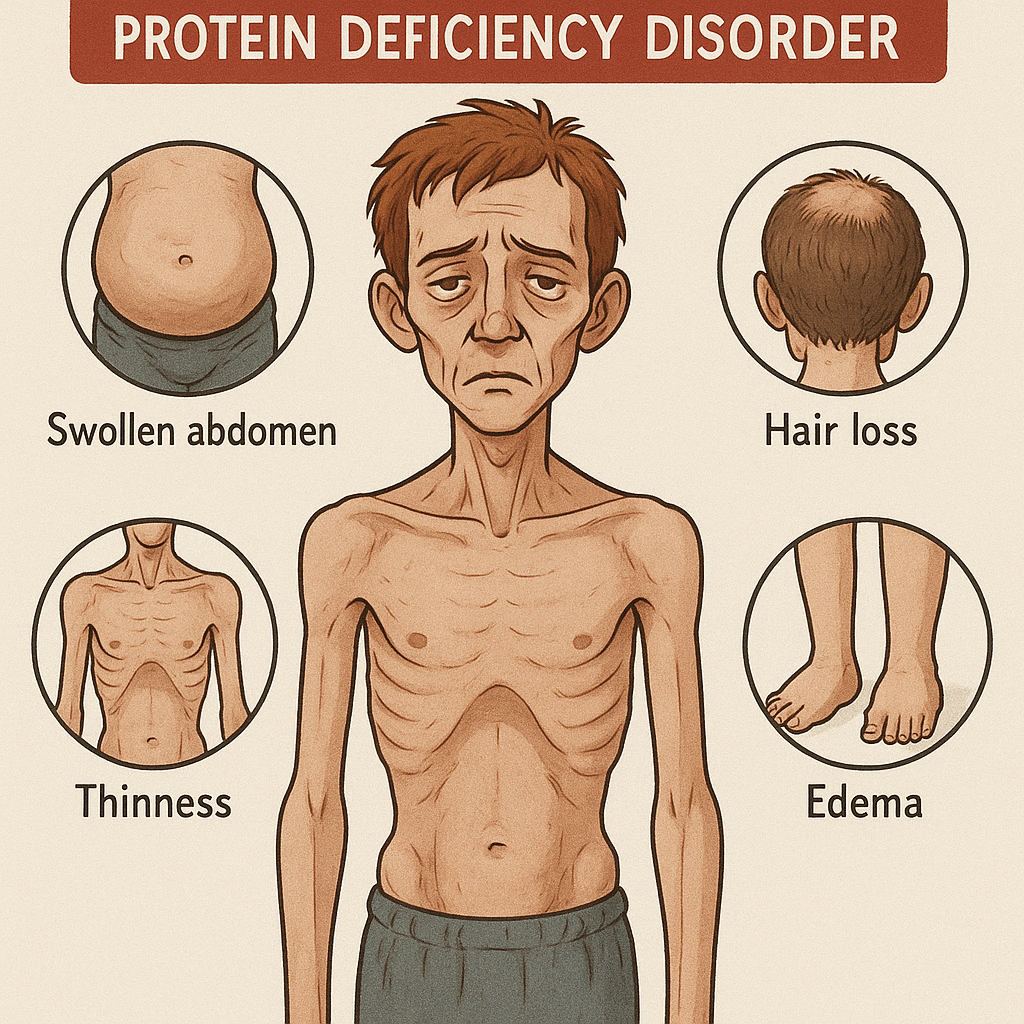
✅ Bilateral pitting edema (swelling of feet, hands, face).
✅ Swollen abdomen (“Pot Belly”) due to hepatomegaly.
✅ Flaky paint dermatitis (skin peeling with dark patches).
✅ Sparse, brittle hair (reddish-brown or gray in color).
✅ Irritability, apathy, lethargy (child is weak and unresponsive).
✅ Poor appetite (often refuses to eat).
✅ Slow wound healing and frequent infections.
6. Diagnosis of Kwashiorkor
A. Anthropometric Measurements
✅ Mid-Upper Arm Circumference (MUAC):
- <11.5 cm → Severe Malnutrition (Kwashiorkor/SAM).
- 11.5-12.5 cm → Moderate Malnutrition.
✅ Weight-for-Height Z-score (< -3 SD) (WHO Growth Chart).
✅ Presence of Bilateral Pitting Edema (Diagnostic sign).
B. Laboratory Investigations
- Serum Albumin: Low (<2.8 g/dL).
- Hemoglobin Levels: Low (anemia is common).
- Liver Function Tests: Elevated liver enzymes (due to fatty liver).
- Blood Glucose: Low (risk of hypoglycemia).
- Electrolytes: Low potassium, sodium imbalance.
- Stool Test: To check for parasitic infections.
7. Management of Kwashiorkor
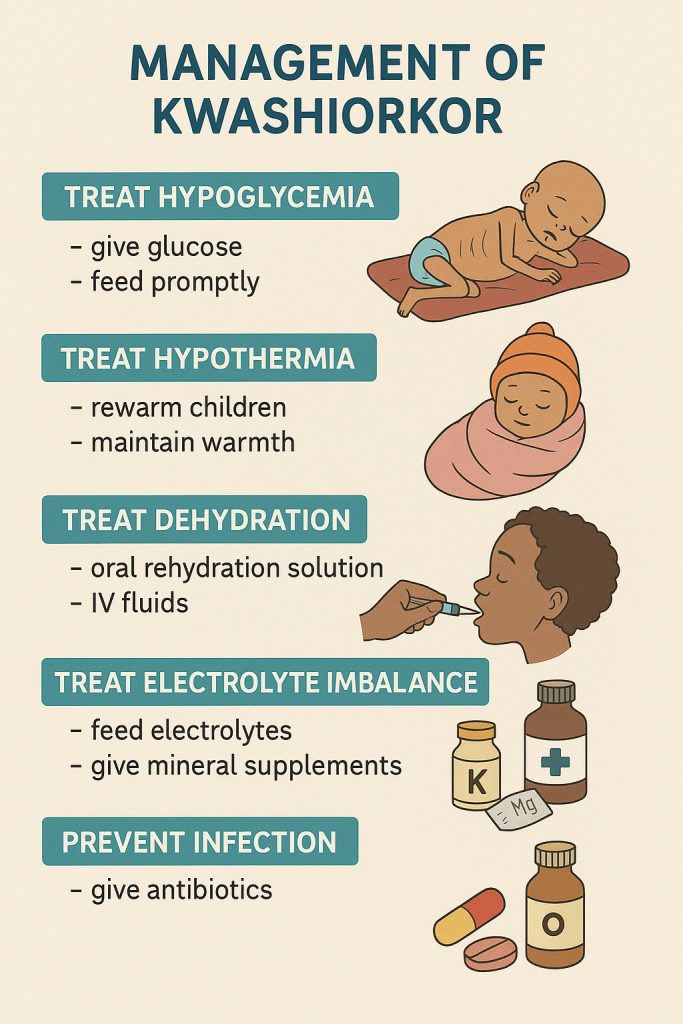
A. Emergency Treatment (Stabilization Phase)
1. Treat Hypoglycemia (Low Blood Sugar)
- Give 50 ml of 10% dextrose orally or IV.
- If unconscious: IV 10% dextrose + normal saline.
2. Correct Hypothermia (Low Body Temperature)
- Wrap child in warm blankets.
- Skin-to-skin contact (Kangaroo Mother Care).
3. Rehydration Therapy (For Dehydration)
- Use ReSoMal (Rehydration Solution for Malnutrition).
- Do NOT use ORS (high sodium worsens edema).
4. Treat Infections (Empirical Antibiotics)
- Amoxicillin or Ceftriaxone (for bacterial infections).
- Antiparasitic treatment (Albendazole for worms).
B. Nutritional Rehabilitation (Catch-Up Growth)
✅ Step 1: Start with WHO Formula Feeds
- F-75 Formula (First 7 Days):
- Low protein, high electrolytes to stabilize the child.
- F-100 Formula (After 7 Days):
- High-protein, high-calorie diet for weight gain.
✅ Step 2: Introduce Ready-to-Use Therapeutic Foods (RUTF)
- Examples: Plumpy’Nut, BP-100 (energy-dense peanut paste).
- Given in small, frequent feeds.
✅ Step 3: Micronutrient Supplementation
- Vitamin A (Prevents blindness, infections).
- Iron & folic acid (After treating infections).
- Zinc (For diarrhea & immunity).
✅ Step 4: Gradual Introduction of Family Diet
- Protein-rich foods: Eggs, fish, meat, pulses, dairy.
- Fruits & vegetables for vitamins and minerals.
✅ Step 5: Psychosocial Support
- Counseling mothers on breastfeeding & complementary feeding.
- Encourage mother-child bonding to stimulate appetite.
8. Nurse’s Role in Kwashiorkor Management
A. Hospital-Based Care
✅ Early Identification & Screening
- Measure MUAC, weight-for-height Z-score.
- Identify bilateral pitting edema (Kwashiorkor indicator).
✅ Administer Therapeutic Feeds
- Prepare & feed F-75, F-100, RUTF.
- Monitor for refeeding syndrome (electrolyte shifts).
✅ Manage Infections & Hydration
- Antibiotics for infections.
- ReSoMal instead of ORS for dehydration.
B. Community-Based Prevention & Education
✅ Nutrition Education for Mothers
- Promote exclusive breastfeeding (0-6 months).
- Teach proper complementary feeding after 6 months.
- Encourage diverse food sources (proteins, vegetables, fortified foods).
✅ Growth Monitoring in Anganwadi Centers
- Conduct monthly MUAC screenings.
- Provide supplementary nutrition for undernourished children.
✅ Public Health Programs
- Integrated Child Development Services (ICDS).
- National Nutrition Mission (Poshan Abhiyan).
- Vitamin A Supplementation Program.
- Mid-Day Meal Scheme (for school children).
9. Prevention of Kwashiorkor
✅ Exclusive Breastfeeding for First 6 Months.
✅ Balanced Weaning Diet with Protein-Rich Foods.
✅ Nutritional Supplementation for Pregnant & Lactating Mothers.
✅ Fortified Foods & Micronutrient Supplementation.
✅ Hygiene & Safe Drinking Water (Prevents infections).
✅ Regular Growth Monitoring & Health Checkups.
Marasmus.
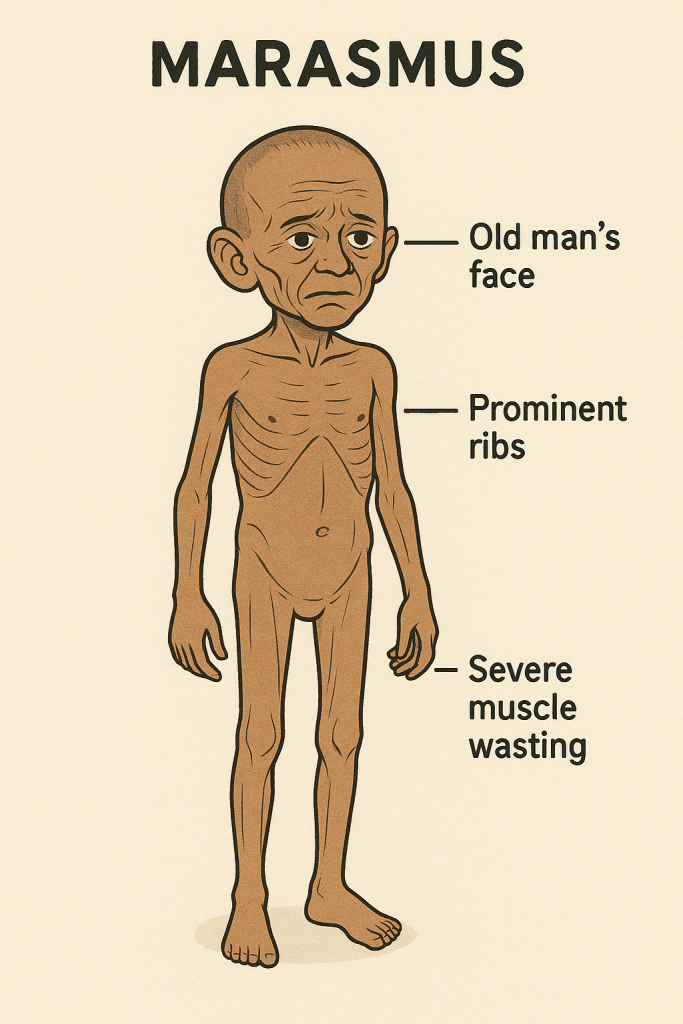
1. Introduction
Marasmus is a severe form of protein-energy malnutrition (PEM) caused by deficiency of both calories and proteins. It primarily affects children under 5 years of age and is characterized by extreme weight loss, muscle wasting, and weakness. Unlike Kwashiorkor, edema is absent in Marasmus.
- High-risk group: Infants (6 months – 2 years)
- Common in: Developing countries with food insecurity
- Mortality risk: Very high if untreated
2. Magnitude of the Problem
Global Prevalence
- 45 million children under 5 suffer from wasting (WHO, 2023).
- Marasmus is more common than Kwashiorkor in famine-affected regions.
- High mortality risk if untreated, mainly due to infections.
Indian Scenario (NFHS-5, 2020-21)
- Wasting (low weight for height): 19.3%
- Severe wasting (Marasmus & SAM): 7.7%
- Underweight (low weight for age): 32.1%
- Stunting (low height for age): 35.5%
- High prevalence in: Bihar, Jharkhand, Madhya Pradesh, Uttar Pradesh
3. Causes of Marasmus
A. Primary Causes (Nutritional Deficiencies)
- Lack of breastfeeding or early weaning.
- Insufficient calorie and protein intake (due to food shortages).
- Inappropriate complementary feeding after 6 months.
- Prolonged starvation or neglect.
B. Secondary Causes (Disease-Related)
- Chronic infections (Tuberculosis, HIV/AIDS).
- Frequent diarrhea → Loss of essential nutrients.
- Parasitic infestations (Worms, Giardiasis).
- Congenital conditions (Cystic fibrosis, metabolic disorders).
4. Pathophysiology of Marasmus
- Severe calorie and protein deficiency → Body breaks down muscle & fat for energy.
- Depletion of fat stores → Severe weight loss & muscle wasting.
- Impaired immunity → High risk of infections.
- Reduced enzyme production → Poor digestion & absorption.
- Delayed brain development in children.
5. Clinical Features of Marasmus
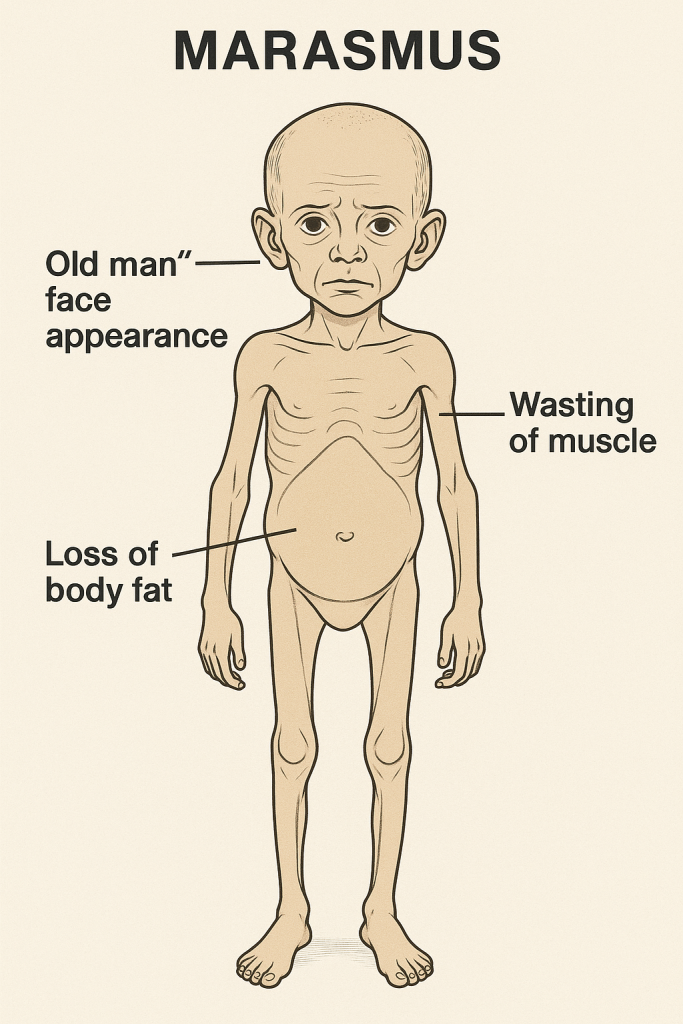
✅ Extreme weight loss (“Bag of bones”)
✅ Muscle wasting & loss of subcutaneous fat
✅ Wrinkled, dry, and loose skin (due to fat loss)
✅ Sunken eyes & hollow cheeks
✅ Severe growth retardation
✅ Weakness, irritability, lethargy
✅ Increased susceptibility to infections (diarrhea, pneumonia)
✅ Delayed wound healing & slow recovery from illness
✅ No edema (unlike Kwashiorkor)
6. Diagnosis of Marasmus
A. Anthropometric Measurements
✅ Mid-Upper Arm Circumference (MUAC):
- <11.5 cm → Severe Malnutrition (Marasmus).
- 11.5-12.5 cm → Moderate Malnutrition.
✅ Weight-for-Height Z-score (< -3 SD) (WHO Growth Chart).
✅ No Bilateral Pitting Edema (Unlike Kwashiorkor).
B. Laboratory Investigations
- Serum Albumin: Normal or slightly low (Unlike Kwashiorkor).
- Hemoglobin Levels: Low (anemia is common).
- Blood Glucose: Low (risk of hypoglycemia).
- Electrolytes: Low potassium, sodium imbalance.
- Stool Test: To check for parasitic infections.
7. Management of Marasmus
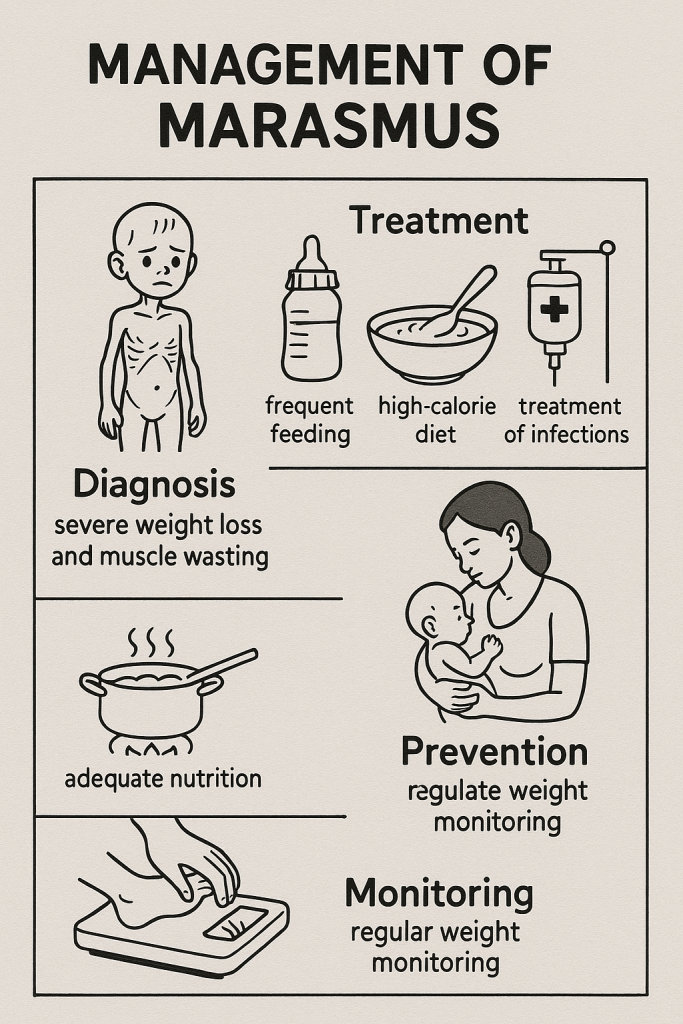
A. Emergency Treatment (Stabilization Phase)
1. Treat Hypoglycemia (Low Blood Sugar)
- Give 50 ml of 10% dextrose orally or IV.
- If unconscious: IV 10% dextrose + normal saline.
2. Correct Hypothermia (Low Body Temperature)
- Wrap child in warm blankets.
- Skin-to-skin contact (Kangaroo Mother Care).
3. Rehydration Therapy (For Dehydration)
- Use ReSoMal (Rehydration Solution for Malnutrition).
- Do NOT use ORS (high sodium can worsen dehydration).
4. Treat Infections (Empirical Antibiotics)
- Amoxicillin or Ceftriaxone (for bacterial infections).
- Antiparasitic treatment (Albendazole for worms).
B. Nutritional Rehabilitation (Catch-Up Growth)
✅ Step 1: Start with WHO Formula Feeds
- F-75 Formula (First 7 Days):
- Low protein, high electrolytes to stabilize the child.
- F-100 Formula (After 7 Days):
- High-protein, high-calorie diet for weight gain.
✅ Step 2: Introduce Ready-to-Use Therapeutic Foods (RUTF)
- Examples: Plumpy’Nut, BP-100 (energy-dense peanut paste).
- Given in small, frequent feeds.
✅ Step 3: Micronutrient Supplementation
- Vitamin A (Prevents blindness, infections).
- Iron & folic acid (After treating infections).
- Zinc (For diarrhea & immunity).
✅ Step 4: Gradual Introduction of Family Diet
- Protein-rich foods: Eggs, fish, meat, pulses, dairy.
- Fruits & vegetables for vitamins and minerals.
✅ Step 5: Psychosocial Support
- Counseling mothers on breastfeeding & complementary feeding.
- Encourage mother-child bonding to stimulate appetite.
8. Nurse’s Role in Marasmus Management
A. Hospital-Based Care
✅ Early Identification & Screening
- Measure MUAC, weight-for-height Z-score.
- Identify severe weight loss & muscle wasting.
✅ Administer Therapeutic Feeds
- Prepare & feed F-75, F-100, RUTF.
- Monitor for refeeding syndrome (electrolyte shifts).
✅ Manage Infections & Hydration
- Antibiotics for infections.
- ReSoMal instead of ORS for dehydration.
B. Community-Based Prevention & Education
✅ Nutrition Education for Mothers
- Promote exclusive breastfeeding (0-6 months).
- Teach proper complementary feeding after 6 months.
- Encourage diverse food sources (proteins, vegetables, fortified foods).
✅ Growth Monitoring in Anganwadi Centers
- Conduct monthly MUAC screenings.
- Provide supplementary nutrition for undernourished children.
✅ Public Health Programs
- Integrated Child Development Services (ICDS).
- National Nutrition Mission (Poshan Abhiyan).
- Vitamin A Supplementation Program.
- Mid-Day Meal Scheme (for school children).
9. Prevention of Marasmus

✅ Exclusive Breastfeeding for First 6 Months.
✅ Balanced Weaning Diet with Protein-Rich Foods.
✅ Nutritional Supplementation for Pregnant & Lactating Mothers.
✅ Fortified Foods & Micronutrient Supplementation.
✅ Hygiene & Safe Drinking Water (Prevents infections).
✅ Regular Growth Monitoring & Health Checkups.
Nurses’ Role in Nutritional Deficiency Disorders.
1. Introduction
Nutritional deficiency disorders occur due to inadequate intake, absorption, or utilization of essential nutrients. These deficiencies lead to various health issues, including growth retardation, weakened immunity, anemia, and metabolic disorders. Nurses play a crucial role in the prevention, diagnosis, management, and rehabilitation of patients suffering from these deficiencies.
2. Nurses’ Role in Nutritional Deficiency Disorders
The role of nurses in nutritional deficiency disorders can be classified into preventive, curative, rehabilitative, and health promotion activities.
3. Preventive Role of Nurses
Nurses play a vital role in preventing nutritional deficiencies through education, screening, and supplementation programs.
A. Nutritional Screening & Growth Monitoring
✅ Anthropometric Assessments:
- Measure weight, height, Mid-Upper Arm Circumference (MUAC) to detect malnutrition.
- Identify stunting (low height-for-age), wasting (low weight-for-height), and underweight conditions.
✅ Biochemical Screening:
- Check hemoglobin levels for anemia.
- Assess serum albumin levels in cases of protein-energy malnutrition (PEM).
- Monitor vitamin and mineral levels (e.g., Vitamin D, Calcium, Iron).
✅ Dietary History Assessment:
- Evaluate patients’ food intake, meal frequency, and dietary diversity.
- Identify deficiencies in essential nutrients.
B. Health Education & Counseling
✅ Breastfeeding Promotion:
- Encourage exclusive breastfeeding for the first 6 months.
- Promote continued breastfeeding up to 2 years with complementary feeding.
✅ Complementary Feeding Education:
- Teach mothers to introduce nutrient-rich foods from 6 months.
- Recommend protein sources like eggs, lentils, and fish.
✅ Micronutrient Education:
- Educate on Iron-rich foods (green leafy vegetables, meat).
- Emphasize Vitamin A sources (carrots, dairy).
- Promote Iodized salt use to prevent goiter.
✅ Food Hygiene & Safe Drinking Water:
- Prevent infections that cause malabsorption of nutrients.
- Teach handwashing techniques before food preparation.
C. Nutritional Supplementation Programs
✅ Administer Iron & Folic Acid (IFA) Supplements:
- Prevent and manage iron-deficiency anemia.
- Educate pregnant women on iron-rich foods.
✅ Vitamin A Supplementation:
- Administer biannual Vitamin A doses to children (6 months-5 years).
✅ Deworming Programs:
- Provide Albendazole/Mebendazole to prevent intestinal parasites.
✅ Promote Fortified Foods:
- Encourage the consumption of fortified cereals, milk, and salt.
4. Nurses’ Role in Clinical Management of Nutritional Deficiencies
Nurses are responsible for early detection, medical care, and dietary rehabilitation of patients suffering from nutritional deficiencies.
A. Management of Protein-Energy Malnutrition (PEM)
✅ Hospital-Based Care:
- Start therapeutic feeds (F-75, F-100) for severe cases.
- Monitor for hypoglycemia, dehydration, and electrolyte imbalances.
✅ Rehydration Therapy:
- Use ReSoMal (Rehydration Solution for Malnutrition) for dehydration.
- Avoid ORS with high sodium in cases of Kwashiorkor.
✅ Gradual Nutritional Rehabilitation:
- Introduce high-protein, high-calorie diets (milk, pulses, nuts).
- Provide Ready-to-Use Therapeutic Foods (RUTFs) (Plumpy’Nut).
✅ Monitor Weight Gain & Recovery:
- Track weight-for-height improvement.
- Ensure nutritional follow-up after discharge.
B. Management of Micronutrient Deficiencies
1. Iron-Deficiency Anemia
✅ Administer Iron Supplements (oral/IV).
✅ Educate on Iron-Rich Foods (spinach, red meat).
✅ Encourage Vitamin C intake (citrus fruits) to enhance iron absorption.
2. Vitamin A Deficiency
✅ Give high-dose Vitamin A supplements (for children).
✅ Treat night blindness and xerophthalmia early.
✅ Encourage intake of yellow/orange vegetables (carrots, pumpkin).
3. Iodine Deficiency (Goiter)
✅ Educate on iodized salt consumption.
✅ Monitor thyroid hormone levels in severe cases.
✅ Refer cases for thyroid hormone therapy if needed.
4. Vitamin D Deficiency (Rickets, Osteomalacia)
✅ Encourage sunlight exposure (20-30 minutes daily).
✅ Administer Vitamin D supplements if required.
✅ Promote dairy products & fortified cereals.
C. Infection Control & Immunization
✅ Administer vaccines (measles, tuberculosis, polio) to prevent infections that worsen malnutrition.
✅ Manage diarrhea promptly (ORS, zinc supplements) to prevent dehydration.
✅ Educate on hygiene practices to reduce foodborne illnesses.
5. Nurses’ Role in Rehabilitative Care
A. Psychosocial Support
✅ Encourage Family Involvement in feeding and care.
✅ Address emotional distress in children with severe malnutrition.
✅ Provide counseling for parents to maintain proper nutrition.
B. Home-Based Nutritional Rehabilitation
✅ Teach meal planning with affordable, local foods.
✅ Promote home gardening for nutrient-rich vegetables.
✅ Follow-up visits to monitor nutritional status.
6. Nurses’ Role in Community Health & Public Health Programs
A. Growth Monitoring & Nutritional Surveillance
✅ Conduct monthly weight and height checks in Anganwadi centers.
✅ Identify high-risk children & refer for nutritional intervention.
✅ Maintain health records for malnourished children.
B. Implement Government Nutrition Programs
✅ Integrated Child Development Services (ICDS)
- Provides supplementary nutrition for undernourished children.
- Includes health check-ups & preschool education.
✅ Mid-Day Meal Scheme (MDMS)
- Ensures nutritious meals for school children.
- Helps in reducing malnutrition & dropout rates.
✅ National Nutrition Mission (Poshan Abhiyan)
- Focuses on reducing stunting, wasting & anemia.
- Uses growth tracking through digital tools.
✅ Supplementary Nutrition Program (SNP)
- Provides fortified foods & take-home rations.
- Targets pregnant/lactating mothers & malnourished children.
Childhood Obesity.
1. Introduction
Childhood obesity is a serious public health issue where excess body fat accumulates in children and adolescents, increasing the risk of chronic diseases such as diabetes, hypertension, and cardiovascular disorders. It is mainly caused by poor diet, lack of physical activity, genetic factors, and environmental influences.
Global and Indian Scenario
- Worldwide Prevalence: Over 39 million children under 5 years are overweight or obese (WHO, 2023).
- India’s Scenario (NFHS-5, 2020-21):
- Prevalence of obesity among children (5-19 years): 8%–10%.
- Rising obesity rates due to urbanization, junk food consumption, and reduced physical activity.
2. Signs & Symptoms of Childhood Obesity

✅ Excessive weight gain (compared to height).
✅ Increased Body Mass Index (BMI) ≥ 95th percentile for age and gender.
✅ Fat accumulation around the abdomen, face, and neck.
✅ Shortness of breath with mild activity.
✅ Frequent fatigue, lethargy, and poor stamina.
✅ Stretch marks (Striae) on skin due to rapid weight gain.
✅ Dark patches of skin (Acanthosis Nigricans) around the neck, armpits (insulin resistance).
✅ Psychological issues – low self-esteem, anxiety, depression.
✅ Sleep apnea (breathing pauses during sleep).
3. Causes of Childhood Obesity
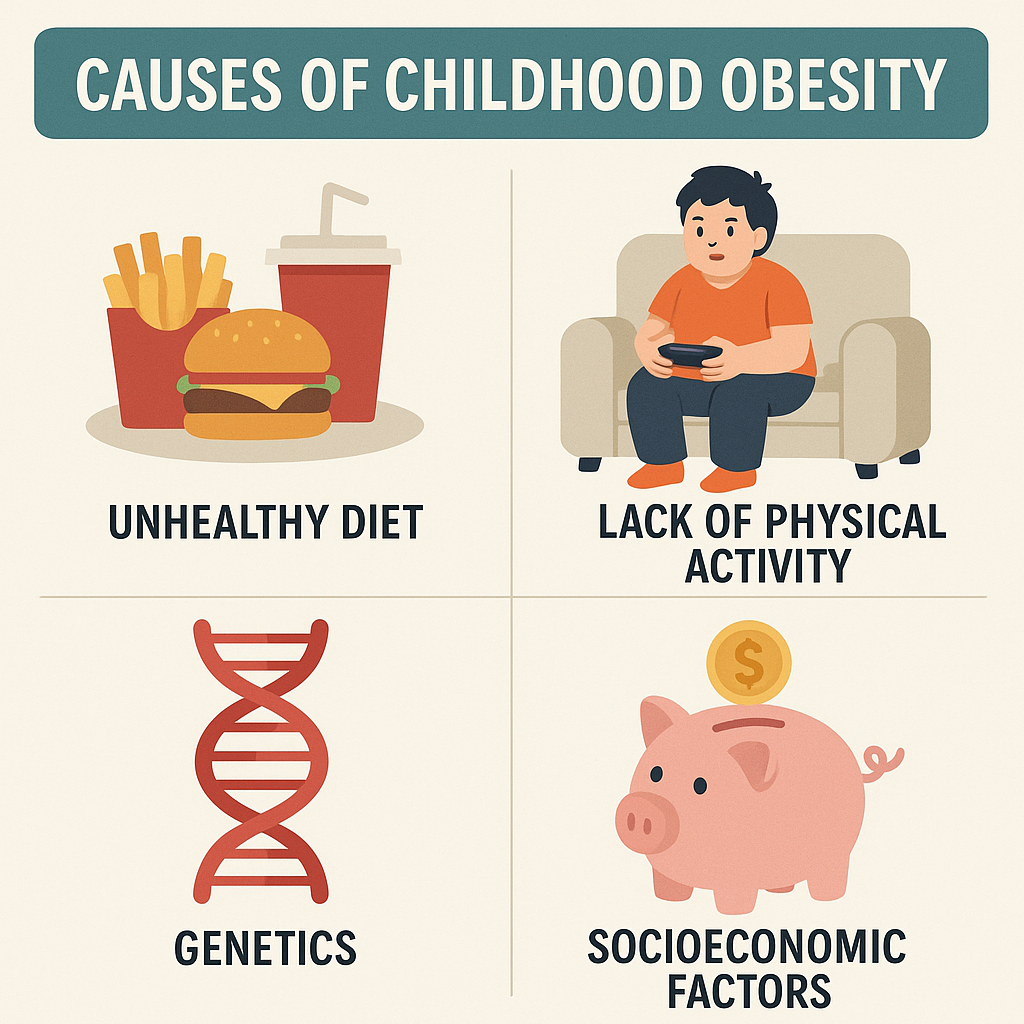
A. Lifestyle & Environmental Factors
✅ Unhealthy Diet:
- High-calorie, low-nutrient foods (fast food, sugary drinks).
- Processed foods rich in trans fats and sugar.
- Skipping breakfast and irregular meals.
✅ Lack of Physical Activity:
- Increased screen time (TV, video games, mobile phones).
- Lack of outdoor play & exercise.
✅ Family and Parental Influence:
- Overfeeding habits in infancy and childhood.
- Sedentary lifestyle among family members.
✅ Sleep Deprivation:
- Less than 7-8 hours of sleep can disrupt metabolism.
B. Genetic & Medical Factors
✅ Family History of Obesity
✅ Hormonal Imbalances:
- Hypothyroidism (underactive thyroid → weight gain).
- Polycystic Ovary Syndrome (PCOS) (in adolescent girls).
✅ Certain Medications:
- Steroids, antidepressants can cause weight gain.
4. Diagnosis of Childhood Obesity
✅ Body Mass Index (BMI) Measurement:
- BMI ≥ 85th percentile – Overweight.
- BMI ≥ 95th percentile – Obese.
- BMI ≥ 99th percentile – Severe Obesity.
✅ Waist-to-Height Ratio (WHtR):
- Ratio > 0.5 indicates central obesity.
✅ Skinfold Thickness Measurement:
- Measures subcutaneous fat using skinfold calipers.
✅ Laboratory Investigations:
- Blood Sugar Test – To check for Type 2 Diabetes.
- Lipid Profile – To assess cholesterol levels.
- Thyroid Function Test (T3, T4, TSH) – To rule out hypothyroidism.
- Liver Function Test (LFT) – To check for fatty liver disease.
- Insulin Resistance Test – If symptoms of prediabetes exist.
5. Assessment of Childhood Obesity
A. Nutritional Assessment
✅ Dietary History:
- Intake of junk food, sugary drinks, and high-fat foods.
- Eating patterns (snacking, portion sizes).
✅ Physical Activity Assessment:
- Hours spent on screen time (TV, mobile, computer).
- Daily exercise routine (if any).
✅ Growth Monitoring:
- Compare child’s weight and height with growth charts.
- Check BMI trends over months/years.
✅ Psychosocial & Behavioral Assessment:
- Screen for emotional eating (stress, boredom).
- Evaluate self-esteem & social issues.
6. Management of Childhood Obesity

Management of obesity requires a multi-disciplinary approach involving lifestyle modifications, behavioral therapy, and medical interventions.
A. Lifestyle Modifications
✅ Healthy Diet Plan:
- Increase fruits, vegetables, whole grains, and lean proteins.
- Reduce processed foods, trans fats, and sugary drinks.
- Portion control – Teach mindful eating.
- Avoid skipping breakfast – Ensures metabolism regulation.
✅ Encouraging Physical Activity:
- At least 60 minutes of moderate-intensity exercise daily.
- Outdoor activities: cycling, skipping, running, swimming.
- Reduce screen time to <2 hours per day.
✅ Improve Sleep Hygiene:
- Ensure 8–10 hours of sleep for metabolism balance.
- Avoid screen exposure before bedtime.
B. Behavioral & Psychological Therapy
✅ Cognitive Behavioral Therapy (CBT):
- Helps identify triggers for emotional eating.
- Encourages self-monitoring of food intake.
✅ Family-Based Therapy:
- Parental involvement in healthy meal planning.
- Encouraging active family outings (hiking, sports).
✅ School-Based Interventions:
- Nutrition education programs for students.
- Banning junk food in school canteens.
C. Medical & Pharmacological Treatment
✅ Medications (in severe cases):
- Metformin – For insulin resistance and diabetes prevention.
- Orlistat – FDA-approved for adolescent obesity (reduces fat absorption).
- Thyroid supplements – If hypothyroidism is diagnosed.
✅ Bariatric Surgery (Extreme Cases Only)
- For adolescents with BMI > 40 or severe obesity-related complications.
- Types: Gastric bypass, sleeve gastrectomy.
7. Prevention of Childhood Obesity
A. Parental Guidance & Healthy Home Environment
✅ Encourage Home-Cooked Meals:
- Reduce fast-food intake.
- Promote balanced meals with fiber & protein.
✅ Portion Control & Mindful Eating:
- Use smaller plates to control portion sizes.
- Avoid using food as a reward or punishment.
✅ Limit Sugary Drinks & Junk Food:
- Encourage water, fresh fruit juices, and homemade snacks.
B. School & Community-Based Prevention
✅ School Nutrition Programs:
- Midday meal schemes with balanced nutrition.
- Ban on sugary drinks & junk food in schools.
✅ Physical Activity Promotion:
- Compulsory sports & outdoor playtime in schools.
- Encourage cycling/walking instead of transport.
✅ Regular Health Check-Ups:
- Annual BMI screening in schools.
- Early identification of at-risk children.
Nurses’ Role in Childhood Obesity.
1. Introduction
Childhood obesity is a major global health concern characterized by excessive body fat accumulation, increasing the risk of diabetes, cardiovascular diseases, and psychological disorders. Nurses play a key role in the prevention, early detection, management, and education of children, parents, and the community regarding obesity.
2. Nurses’ Role in Childhood Obesity
The role of nurses in managing childhood obesity involves prevention, assessment, treatment, rehabilitation, and public health initiatives.
3. Preventive Role of Nurses
A. Health Education and Counseling
✅ Promoting Healthy Eating Habits
- Educate parents and children on balanced diet choices.
- Encourage intake of fruits, vegetables, whole grains, and proteins.
- Reduce processed foods, sugary drinks, and junk food consumption.
✅ Encouraging Physical Activity
- Advise at least 60 minutes of daily physical activity.
- Promote outdoor play, sports, cycling, and swimming.
- Discourage excessive screen time (TV, mobile, video games).
✅ Parental Guidance and Home-Based Prevention
- Educate parents on portion control & mindful eating.
- Encourage family meals and healthy cooking habits.
- Avoid using food as a reward or punishment.
✅ School-Based Prevention
- Support school nutrition programs & health education.
- Encourage ban on junk food in school canteens.
- Advocate for physical education & sports participation.
✅ Promoting Good Sleep Hygiene
- Encourage 8-10 hours of sleep per night.
- Discourage screen exposure before bedtime.
4. Nurses’ Role in Early Detection and Screening
A. Anthropometric Assessment
✅ Measuring BMI (Body Mass Index)
- BMI ≥ 85th percentile – Overweight.
- BMI ≥ 95th percentile – Obese.
- BMI ≥ 99th percentile – Severe Obesity.
✅ Waist-to-Height Ratio (WHtR)
- Ratio > 0.5 indicates central obesity.
✅ Skinfold Thickness Measurement
- Measures subcutaneous fat using skinfold calipers.
B. Clinical and Laboratory Assessments
✅ Blood Tests to check for:
- Blood sugar levels (Type 2 Diabetes risk).
- Lipid profile (cholesterol, triglycerides).
- Thyroid function tests (to rule out hypothyroidism).
- Liver function tests (to assess fatty liver).
- Insulin resistance tests (for prediabetes).
✅ Psychosocial Assessment
- Identify emotional eating patterns.
- Assess for low self-esteem, anxiety, depression.
- Screen for bullying or social isolation.
5. Nurses’ Role in Clinical Management of Childhood Obesity
A. Lifestyle Modifications (Non-Pharmacological Management)
✅ Personalized Dietary Plans
- Work with dietitians to create low-calorie, nutrient-rich diets.
- Encourage frequent small meals instead of binge eating.
- Promote adequate water intake and fiber-rich foods.
✅ Behavioral Therapy for Obese Children
- Cognitive Behavioral Therapy (CBT) for emotional eating.
- Encourage self-monitoring (food diaries, weight tracking).
- Provide group counseling and peer support programs.
✅ Physical Activity Interventions
- Develop customized exercise plans based on age and ability.
- Encourage fun activities like dancing, yoga, swimming.
- Ensure school-based sports programs and active play.
✅ Reducing Sedentary Lifestyle
- Limit screen time to less than 2 hours/day.
- Encourage active play and outdoor activities.
B. Pharmacological and Medical Interventions
✅ Medication for Severe Cases (as per doctor’s advice)
- Metformin (for insulin resistance and prediabetes).
- Orlistat (for reducing fat absorption in adolescents).
- Thyroid supplements (if hypothyroidism is diagnosed).
✅ Bariatric Surgery (For Severe Morbid Obesity)
- Reserved for adolescents with BMI > 40 with life-threatening conditions.
- Types: Gastric bypass, Sleeve gastrectomy.
6. Nurses’ Role in Psychosocial Support and Rehabilitation
A. Emotional and Psychological Support
✅ Addressing Emotional Eating & Stress Management
- Encourage healthy coping mechanisms (exercise, hobbies).
- Provide counseling for depression & anxiety related to obesity.
✅ Building Self-Esteem and Social Skills
- Support children in developing confidence and positive body image.
- Address bullying and stigma in schools.
B. Family Involvement and Support
✅ Encouraging Family Participation
- Involve parents in meal planning and activity schedules.
- Organize family exercise programs and cooking workshops.
✅ Follow-Up Care and Weight Maintenance
- Regular check-ups every 3-6 months to monitor progress.
- Provide long-term counseling to prevent weight regain.
7. Nurses’ Role in Community Health and Public Health Programs
A. Community Awareness and Education
✅ Organizing Health Campaigns
- Workshops on healthy eating habits.
- Nutritional awareness camps in schools and communities.
✅ Growth Monitoring and Early Intervention
- Conduct BMI screenings in schools.
- Identify and refer high-risk children for early intervention.
✅ Policy Advocacy
- Support government policies for healthy school meals.
- Encourage bans on junk food advertisements targeting children.
8. Nurses’ Role in Government and Public Health Programs
A. Implementation of National Health Programs
✅ Poshan Abhiyan (National Nutrition Mission)
- Focuses on reducing childhood malnutrition & obesity.
✅ Integrated Child Development Services (ICDS)
- Provides nutritional supplements & health checkups.
✅ Mid-Day Meal Scheme (MDMS)
- Ensures balanced nutrition for school children.
✅ Fit India Movement
- Promotes physical activity in schools and communities.
✅ Junk Food Restrictions in Schools
- Advocate for ban on unhealthy foods in schools & public places.
9. Prevention Strategies for Childhood Obesity
A. Individual-Level Prevention
✅ Exclusive Breastfeeding for First 6 Months
✅ Introducing Healthy Complementary Feeding from 6 Months
✅ Teaching Children Healthy Eating Habits
✅ Encouraging Regular Physical Activity
B. Community and School-Based Prevention
✅ School Nutrition Education Programs
✅ Physical Education & Active Playtime in Schools
✅ Community-Based Growth Monitoring and Awareness
C. Government Policy and Public Health Initiatives
✅ Regulation of Food Advertisements Targeting Children
✅ Nutritional Labeling on Packaged Foods
✅ Taxation on Sugary Drinks and Junk Food.
Vitamin A Deficiency Disorders.
1. Introduction
Vitamin A is a fat-soluble vitamin essential for vision, immune function, growth, and cellular differentiation. Vitamin A deficiency (VAD) is a major public health problem, especially in developing countries, leading to blindness, impaired immunity, and increased child mortality.
2. Causes of Vitamin A Deficiency

Vitamin A deficiency occurs due to inadequate intake, poor absorption, or increased demand.
A. Primary Causes (Dietary Deficiency)
✅ Inadequate dietary intake:
- Lack of Vitamin A-rich foods (e.g., liver, fish, dairy, green leafy vegetables, orange-colored fruits).
- Common in low-income populations relying on cereal-based diets.
✅ Premature Weaning & Poor Infant Feeding:
- Lack of breast milk, which is a natural source of Vitamin A.
- Early introduction of low-nutrient complementary foods.
B. Secondary Causes (Disease-Related)
✅ Malabsorption Disorders:
- Chronic diarrhea, Crohn’s disease, celiac disease reduce absorption.
- Cystic fibrosis, pancreatic insufficiency affect fat digestion.
✅ Liver Disease:
- Since Vitamin A is stored in the liver, conditions like cirrhosis, hepatitis reduce Vitamin A storage.
✅ Chronic Infections & Increased Demand:
- Measles, tuberculosis, HIV/AIDS increase Vitamin A requirements.
- Pregnancy & lactation demand higher Vitamin A intake.
3. Signs & Symptoms of Vitamin A Deficiency
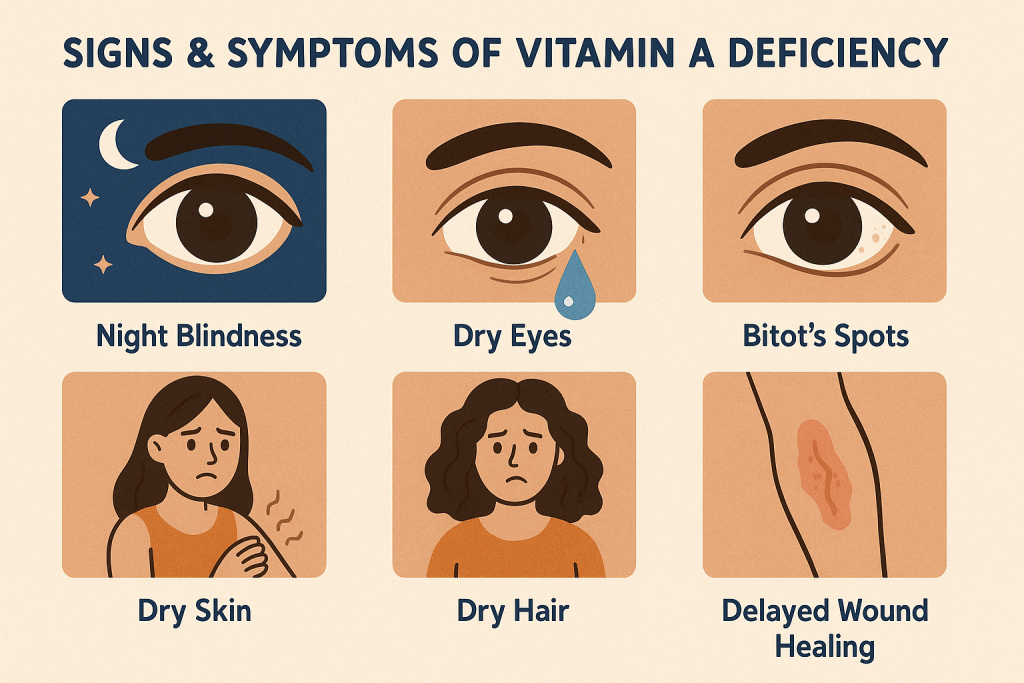
A. Ocular Manifestations (Eye Problems)
✅ Night Blindness (Nyctalopia) – Early symptom; difficulty seeing in dim light.
✅ Xerophthalmia – Dryness of conjunctiva & cornea due to lack of tears.
✅ Bitot’s Spots – White foamy patches on the conjunctiva.
✅ Corneal Ulceration & Keratomalacia – Severe cases leading to blindness.
B. General Systemic Symptoms
✅ Impaired Immunity – Increased risk of respiratory infections, diarrhea, measles.
✅ Skin Problems – Dry, scaly, and rough skin (Follicular hyperkeratosis).
✅ Growth Retardation – Stunted growth in children.
✅ Anemia – Reduced iron metabolism leading to iron-deficiency anemia.
✅ Reproductive Issues – Infertility & pregnancy complications.
4. Diagnosis of Vitamin A Deficiency
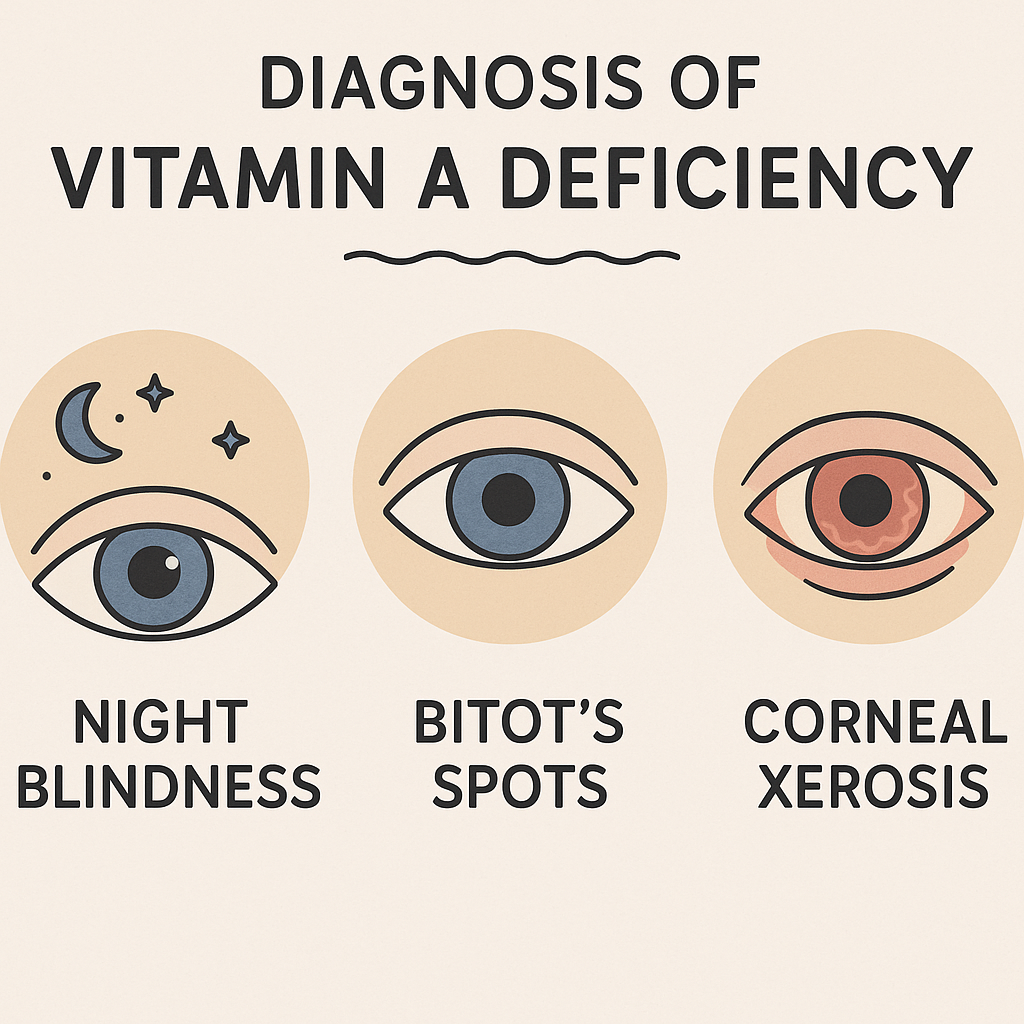
✅ Clinical Examination:
- Assess night blindness & xerophthalmia symptoms.
- Check for Bitot’s spots, dry skin, and frequent infections.
✅ Biochemical Tests:
- Serum Retinol Level:
- < 20 µg/dL – Deficiency.
- 10-19 µg/dL – Mild deficiency.
- <10 µg/dL – Severe deficiency.
- Liver Function Test (LFTs) – Since Vitamin A is stored in the liver.
✅ Dark Adaptation Test:
- Evaluates night vision impairment.
✅ Conjunctival Impression Cytology (CIC):
- Detects abnormal epithelial cells in the eye.
5. Management of Vitamin A Deficiency
A. Mild to Moderate Deficiency
✅ Dietary Modification:
- Increase intake of Vitamin A-rich foods:
- Animal sources: Liver, egg yolk, dairy products, fish oil.
- Plant sources: Carrots, mangoes, papaya, spinach, pumpkin.
- Encourage fortified foods (milk, margarine, cereals).
✅ Oral Vitamin A Supplementation:
- Children 6-11 months: 100,000 IU once.
- Children 12-59 months: 200,000 IU every 4-6 months.
- Pregnant & lactating women: 10,000 IU daily.
B. Severe Vitamin A Deficiency (Xerophthalmia, Keratomalacia)
✅ High-Dose Vitamin A Therapy (WHO Protocol):
- Day 1: 200,000 IU orally (or 100,000 IU for infants <12 months).
- Day 2: 200,000 IU.
- Day 14: 200,000 IU.
- If corneal ulceration: Immediate treatment + hospitalization.
✅ Supportive Treatment:
- Topical antibiotic eye drops for secondary infections.
- Lubricating eye drops to prevent dryness.
- IV fluids & nutrition support if associated with severe malnutrition.
6. Prevention of Vitamin A Deficiency
✅ Exclusive Breastfeeding (First 6 Months) – Provides sufficient Vitamin A to infants.
✅ Balanced Diet with Vitamin A-Rich Foods – Include vegetables, dairy, and liver.
✅ Fortified Foods & Supplements – Use Vitamin A-enriched milk, cereals, and oils.
✅ Vitamin A Supplementation Programs:
- WHO recommends biannual high-dose Vitamin A supplementation for high-risk children.
✅ Measles Vaccination – Prevents severe Vitamin A depletion.
7. Nurses’ Role in Vitamin A Deficiency
Nurses play a crucial role in prevention, early detection, treatment, and education related to Vitamin A deficiency.
A. Preventive Role
✅ Health Education on Vitamin A-Rich Diet:
- Teach parents about nutritious foods (liver, dairy, leafy greens).
- Promote home gardening for fresh vegetables.
✅ Promote Exclusive Breastfeeding:
- Educate mothers about breastfeeding benefits.
- Teach proper complementary feeding after 6 months.
✅ Community-Based Vitamin A Supplementation:
- Assist in Vitamin A distribution programs.
- Ensure compliance with high-dose supplementation.
✅ Measles Prevention & Immunization:
- Administer Vitamin A along with measles vaccines.
- Monitor for Vitamin A deficiency during outbreaks.
B. Nurses’ Role in Screening & Early Diagnosis
✅ Growth Monitoring & Health Checkups:
- Assess weight, height, and eye symptoms in undernourished children.
- Identify high-risk groups (malnourished, premature babies).
✅ Assess Vision Problems:
- Check for night blindness, Bitot’s spots.
- Refer severe cases to ophthalmologists.
✅ Biochemical Screening:
- Assist in serum retinol testing for suspected cases.
C. Nurses’ Role in Treatment & Hospital Care
✅ Administer Vitamin A Therapy (As per WHO Protocol).
✅ Provide Eye Care for Severe Cases:
- Apply lubricating drops for dryness.
- Give antibiotic ointment for corneal ulcers.
✅ Manage Malnutrition & Coexisting Deficiencies:
- Ensure proper nutrition rehabilitation.
- Monitor iron levels (as anemia is common with VAD).
✅ Educate Parents on Treatment Adherence:
- Emphasize the importance of follow-up Vitamin A doses.
- Encourage dietary improvements for long-term health.
8. Nurses’ Role in Public Health & Government Programs
✅ Implement National Nutrition Programs:
- Integrated Child Development Services (ICDS).
- National Vitamin A Supplementation Program.
- Mid-Day Meal Scheme (MDMS) in Schools.
✅ Community Growth Monitoring:
- Conduct health check-up camps for malnourished children.
- Provide Vitamin A supplements in Anganwadi centers.
✅ Policy Advocacy for Food Fortification:
- Promote fortified rice, milk, and cooking oil.
Vitamin B Deficiency Disorders.
1. Introduction
Vitamin B is a group of water-soluble vitamins essential for energy metabolism, nervous system function, red blood cell production, and skin health. Deficiency of any B vitamins leads to neurological, hematological, and metabolic disorders.
There are 8 types of B vitamins, each with specific functions and deficiency disorders:
- Vitamin B1 (Thiamine) – Beriberi, Wernicke’s Encephalopathy
- Vitamin B2 (Riboflavin) – Ariboflavinosis
- Vitamin B3 (Niacin) – Pellagra
- Vitamin B5 (Pantothenic Acid) – Rare deficiency
- Vitamin B6 (Pyridoxine) – Neuropathy, anemia
- Vitamin B7 (Biotin) – Hair loss, skin disorders
- Vitamin B9 (Folate/Folic Acid) – Neural tube defects, megaloblastic anemia
- Vitamin B12 (Cobalamin) – Pernicious anemia, neuropathy
2. Causes of Vitamin B Deficiencies
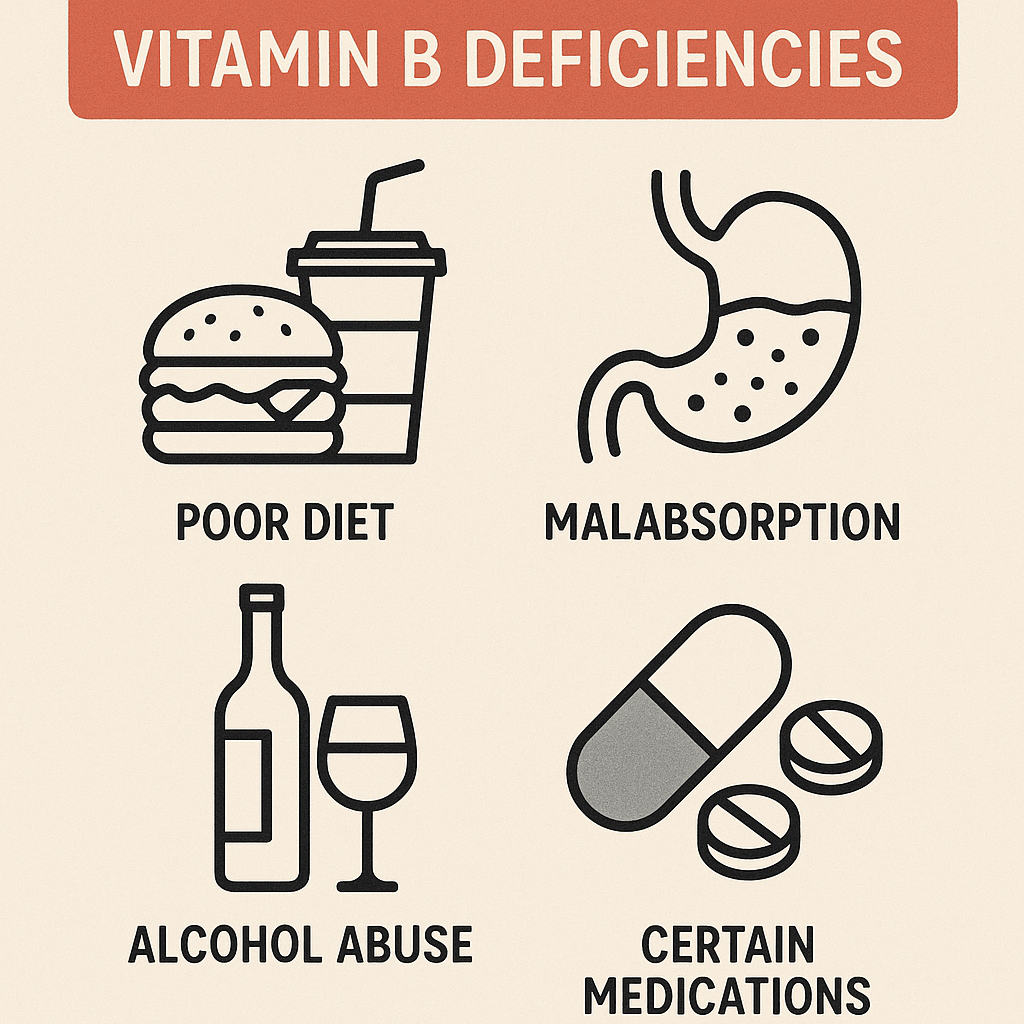
A. Primary Causes (Dietary Deficiency)
✅ Poor diet lacking B-vitamin-rich foods
✅ Alcoholism (reduces absorption and metabolism)
✅ Vegetarian/Vegan diet (Vitamin B12 deficiency)
✅ Malnutrition & food insecurity
B. Secondary Causes (Disease & Medical Conditions)
✅ Gastrointestinal disorders (Crohn’s disease, celiac disease, IBS)
✅ Liver disease (affects B-vitamin storage & metabolism)
✅ Chronic infections (HIV/AIDS, tuberculosis)
✅ Pregnancy & lactation (increased demand)
✅ Long-term use of medications (antacids, metformin, antibiotics)
3. Signs & Symptoms of Vitamin B Deficiency
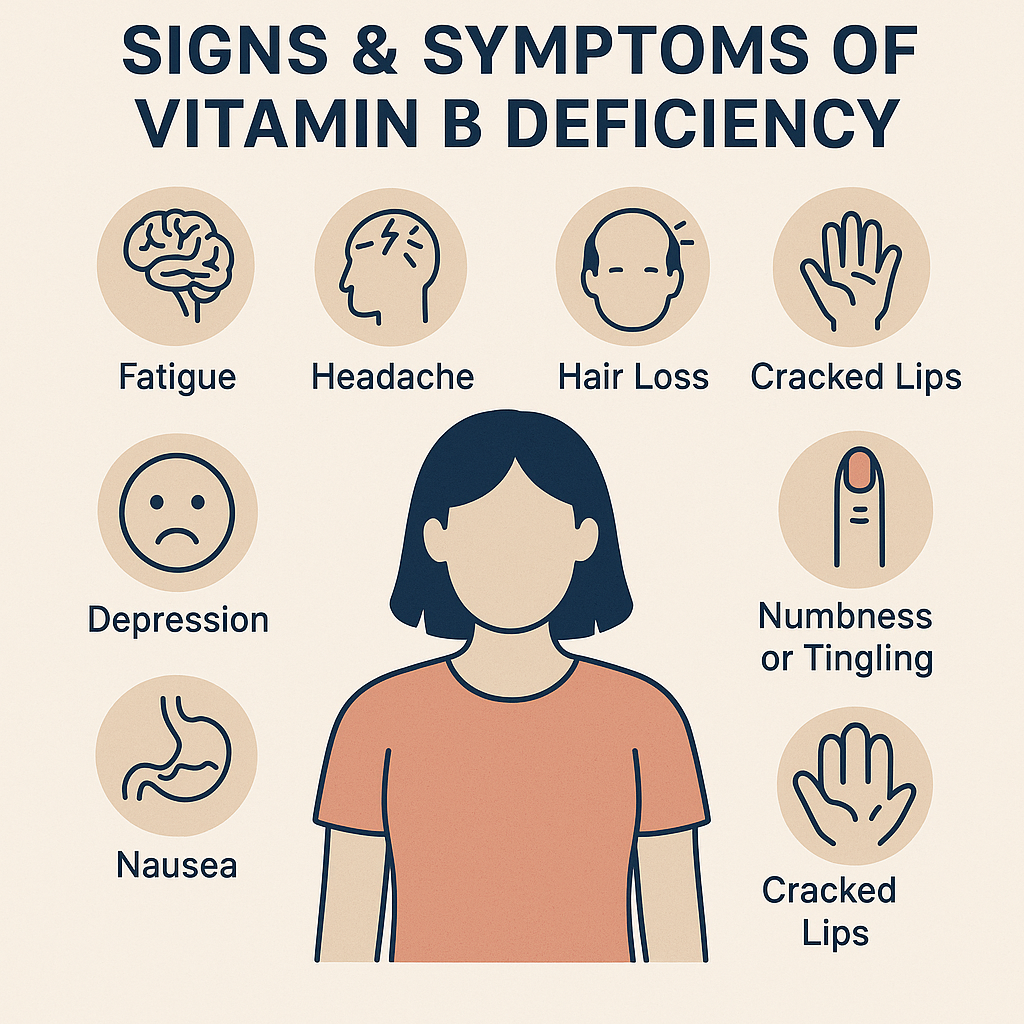
A. Common Symptoms
✅ Fatigue & weakness
✅ Nerve damage (tingling, numbness)
✅ Anemia (pallor, dizziness)
✅ Poor memory & confusion
✅ Skin problems (dermatitis, cracks in lips)
✅ Digestive issues (loss of appetite, weight loss)
B. Specific Vitamin B Deficiencies & Their Symptoms
| Vitamin | Deficiency Disease | Symptoms |
|---|---|---|
| B1 (Thiamine) | Beriberi, Wernicke’s Encephalopathy | Muscle weakness, nerve pain, confusion, heart failure |
| B2 (Riboflavin) | Ariboflavinosis | Cracked lips, sore throat, red tongue, eye irritation |
| B3 (Niacin) | Pellagra | 4 D’s – Dermatitis, Diarrhea, Dementia, Death |
| B5 (Pantothenic Acid) | Rare | Fatigue, depression, irritability |
| B6 (Pyridoxine) | Neuropathy, Anemia | Nerve pain, depression, seizures |
| B7 (Biotin) | Biotin Deficiency | Hair loss, brittle nails, skin rashes |
| B9 (Folate/Folic Acid) | Megaloblastic Anemia, Neural Tube Defects | Fatigue, glossitis, birth defects |
| B12 (Cobalamin) | Pernicious Anemia, Neuropathy | Memory loss, balance issues, numbness |
4. Diagnosis of Vitamin B Deficiency
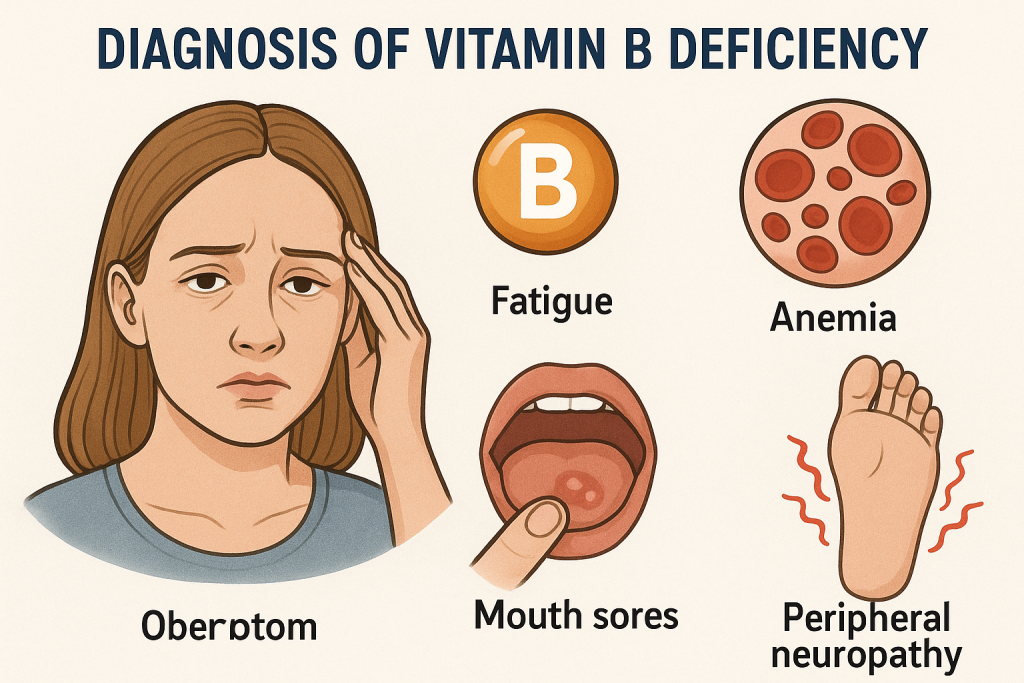
A. Clinical Examination
✅ Assess for fatigue, pallor, neurological symptoms
✅ Check for skin changes, glossitis, mouth sores
✅ Assess diet history & risk factors
B. Laboratory Tests
✅ Complete Blood Count (CBC) – Detects anemia
✅ Serum Vitamin B12 & Folate Levels
✅ Serum Homocysteine & Methylmalonic Acid (MMA) – Elevated in B12 deficiency
✅ Urinary Excretion Test (for B1, B2, B6, B7)
✅ Neurological Tests – Reflexes, coordination, nerve conduction
5. Management of Vitamin B Deficiency
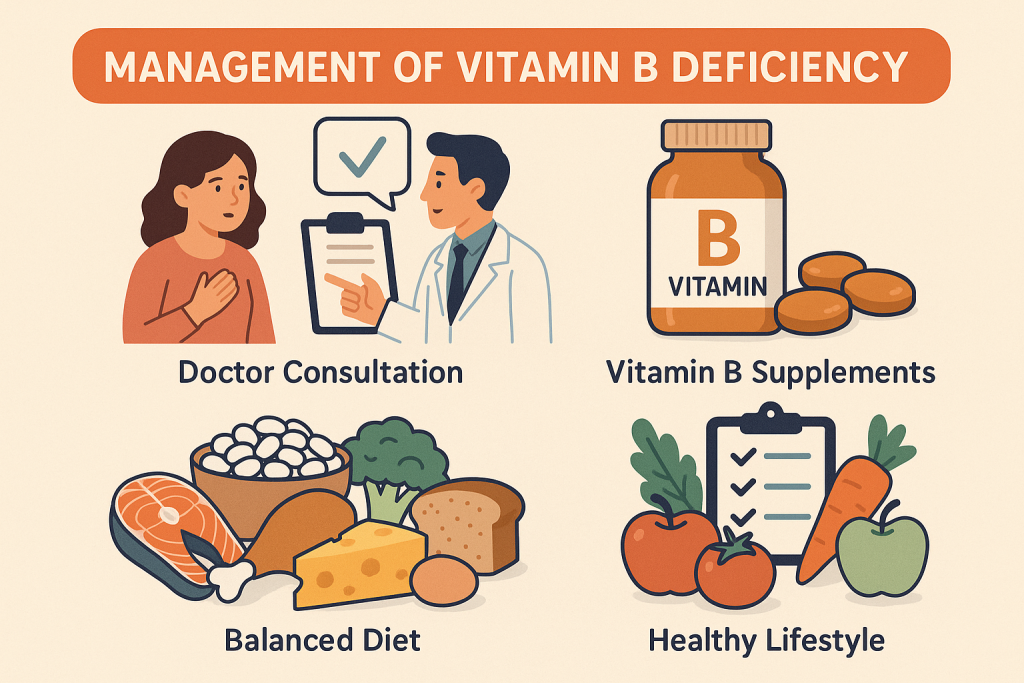
A. Dietary Modification
✅ Increase intake of Vitamin B-rich foods:
- Animal sources: Meat, eggs, fish, dairy (B12, B2, B6)
- Plant sources: Whole grains, nuts, legumes, green vegetables (B1, B3, B9)
- Fortified foods: Cereals, bread, nutritional yeast
B. Vitamin Supplementation
✅ Oral Supplements:
- Mild cases: Multivitamin tablets or single-vitamin therapy
- Pregnancy: 400-600 mcg of folic acid daily
✅ Intramuscular Injections: - B12 injection (1000 mcg IM weekly for 4 weeks, then monthly for life in pernicious anemia)
✅ Therapeutic Protocol for Severe Cases:
- B1 (Thiamine) for Beriberi: 50–100 mg IV/IM daily for severe cases
- B3 (Niacin) for Pellagra: 300 mg/day divided into 3 doses
- B6 (Pyridoxine) for Neuropathy: 50–100 mg/day
6. Prevention of Vitamin B Deficiency
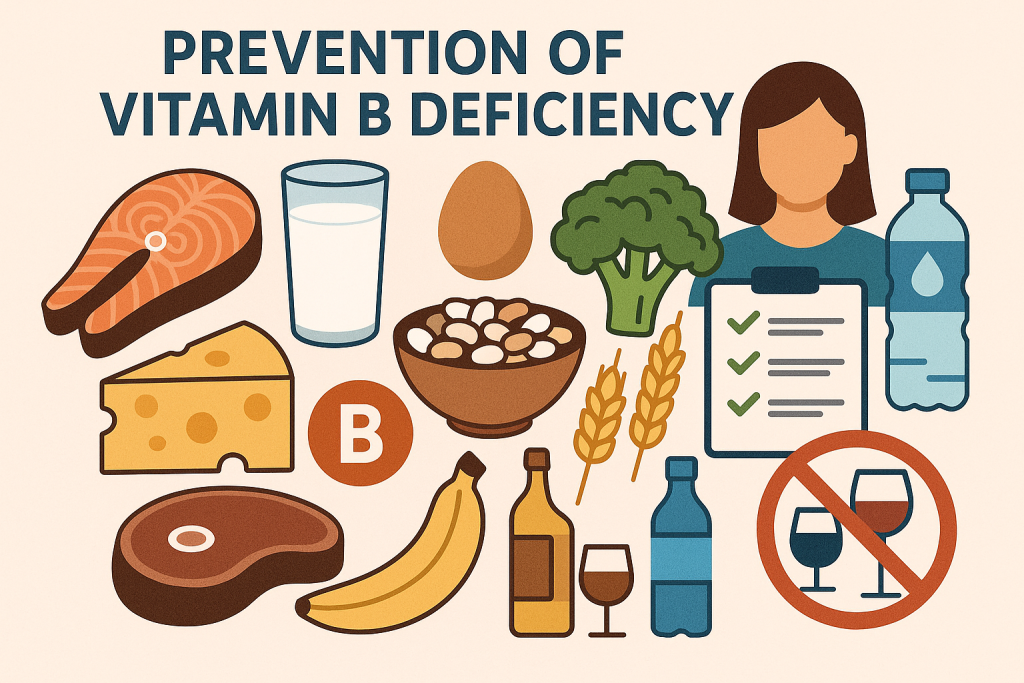
✅ Balanced Diet – Include B-vitamin-rich foods
✅ Food Fortification – B12-fortified cereals for vegetarians
✅ Prenatal Supplements – Folic acid for pregnant women to prevent birth defects
✅ Alcohol Reduction – To improve B-vitamin absorption
✅ Regular Health Check-ups – Especially for high-risk individuals
7. Nurses’ Role in Vitamin B Deficiency
A. Preventive Role
✅ Health Education on Diet & Nutrition
- Teach families about Vitamin B-rich foods
- Encourage home gardening of leafy vegetables
- Promote fortified foods & nutritional supplements
✅ Community Screening & Growth Monitoring
- Conduct nutritional assessment in children & pregnant women
- Identify early signs of anemia, nerve damage, and skin issues
✅ Pregnancy & Maternal Health Education
- Educate mothers on importance of folic acid supplements
- Monitor for neural tube defects & anemia in prenatal check-ups
✅ Alcoholism Awareness Programs
- Educate patients about alcohol-induced B-vitamin deficiencies
B. Nurses’ Role in Diagnosis & Management
✅ Assist in Diagnostic Testing
- Collect blood samples for vitamin level testing
- Monitor neurological signs & anemia symptoms
✅ Administer Vitamin Therapy
- Give B12 injections for pernicious anemia
- Provide oral B-complex supplements for mild deficiencies
✅ Manage Neurological Symptoms
- Encourage physical therapy & nerve stimulation for neuropathy
- Monitor coordination, gait, and mental health in elderly patients
✅ Educate on Medication Interactions
- Inform patients on medications that deplete B vitamins (antacids, metformin)
- Adjust dietary intake for long-term medication users
C. Nurses’ Role in Public Health & Government Programs
✅ Implement National Nutrition Programs
- Poshan Abhiyan – Nutritional support for children & pregnant women
- Mid-Day Meal Scheme – Balanced meals with fortified grains
- National Anemia Control Program – Iron & folic acid supplementation
✅ Community-Based Nutritional Interventions
- Organize nutrition camps & school health check-ups
- Ensure Vitamin B supplementation in high-risk areas.
Vitamin C Deficiency Disorders.
1. Introduction
Vitamin C (Ascorbic Acid) is a water-soluble vitamin essential for collagen synthesis, wound healing, immunity, and iron absorption. Vitamin C deficiency can lead to scurvy, a serious condition affecting the skin, joints, gums, and overall immune function.
2. Causes of Vitamin C Deficiency

Vitamin C deficiency occurs due to inadequate dietary intake, increased requirement, poor absorption, or excessive loss.
A. Primary Causes (Dietary Deficiency)
✅ Inadequate intake of fruits & vegetables
✅ Alcoholism & poor diet choices
✅ Infant formula feeding without supplementation
✅ Food insecurity & malnutrition
B. Secondary Causes (Medical Conditions)
✅ Gastrointestinal disorders (Crohn’s disease, celiac disease, ulcerative colitis)
✅ Chronic infections (tuberculosis, HIV/AIDS)
✅ Diabetes & kidney disease (increased vitamin C loss in urine)
✅ Smoking & drug abuse (reduces vitamin C levels)
✅ Pregnancy & lactation (increased demand)
3. Signs & Symptoms of Vitamin C Deficiency (Scurvy)
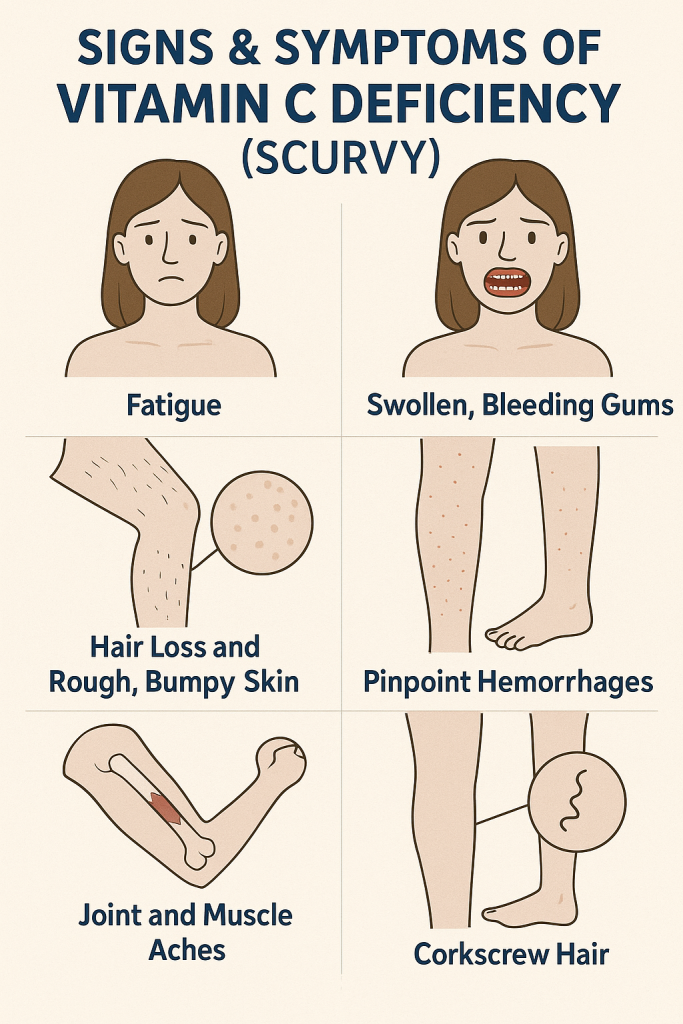
A. Early Symptoms
✅ Fatigue & weakness
✅ Muscle pain & joint stiffness
✅ Irritability & mood changes
✅ Frequent infections due to weakened immunity
B. Severe Symptoms of Scurvy
✅ Bleeding Gums & Loose Teeth
✅ Swollen, painful joints (Hemarthrosis)
✅ Corkscrew Hair (Coiled, brittle hair)
✅ Purpura & Petechiae (Bleeding under the skin)
✅ Slow wound healing & easy bruising
✅ Anemia (due to poor iron absorption)
✅ Scorbutic Rosary (swelling of rib joints in infants)
4. Diagnosis of Vitamin C Deficiency
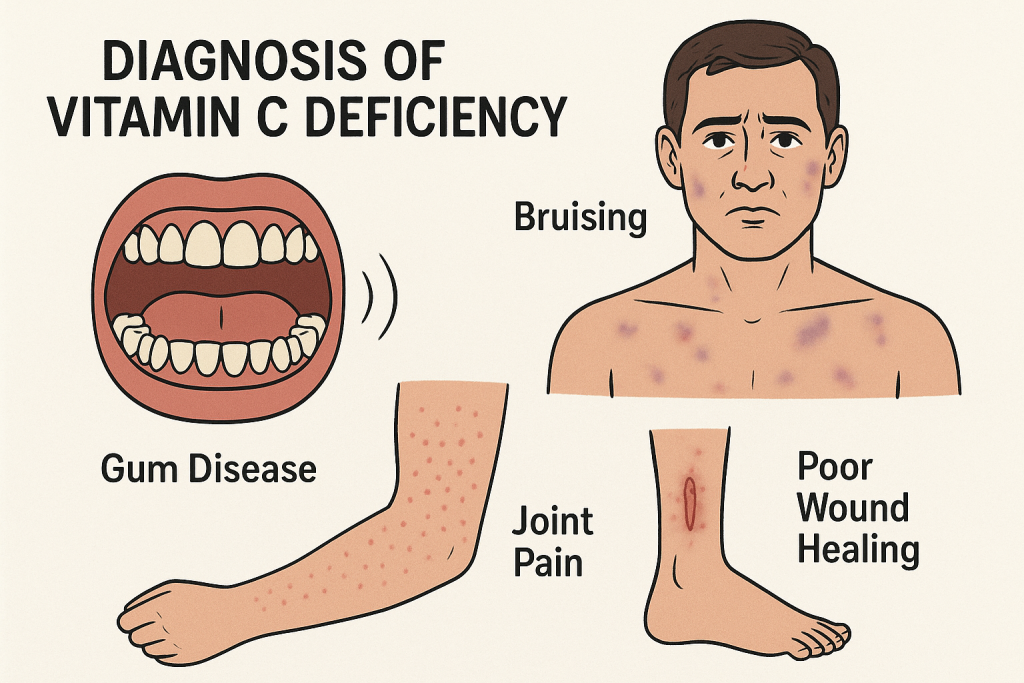
A. Clinical Examination
✅ Assess for bleeding gums, easy bruising, corkscrew hair
✅ Check for joint pain & swollen legs
✅ Evaluate history of poor dietary intake
B. Laboratory Tests
✅ Plasma Vitamin C Level:
- <11 µmol/L – Deficiency
- <6 µmol/L – Severe deficiency (Scurvy)
✅ Complete Blood Count (CBC) – Identifies anemia
✅ Coagulation Profile – Rules out clotting disorders
✅ Bone X-ray (for children) – Detects Scorbutic Rosary, osteoporosis
5. Management of Vitamin C Deficiency
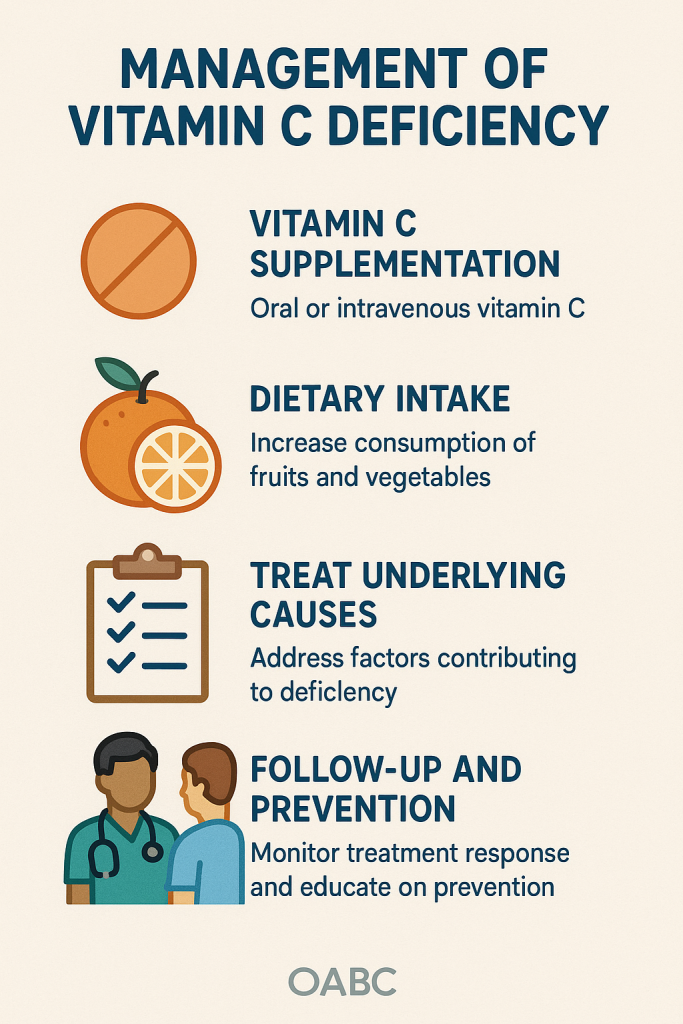
A. Dietary Modification
✅ Increase intake of Vitamin C-rich foods:
- Fruits: Oranges, lemons, strawberries, kiwis, mangoes
- Vegetables: Bell peppers, spinach, tomatoes, broccoli
- Fortified foods: Cereals, juices
B. Vitamin C Supplementation
✅ Mild Deficiency:
- 50-100 mg/day orally for 1 month
✅ Scurvy (Severe Deficiency): - 300-1000 mg/day for 2 weeks
- Symptoms improve within 48 hours, full recovery in 2-4 weeks
✅ Intravenous Vitamin C (Severe Cases):
- IV ascorbic acid 500 mg/day
- Used for malabsorption disorders, post-surgical patients
6. Prevention of Vitamin C Deficiency
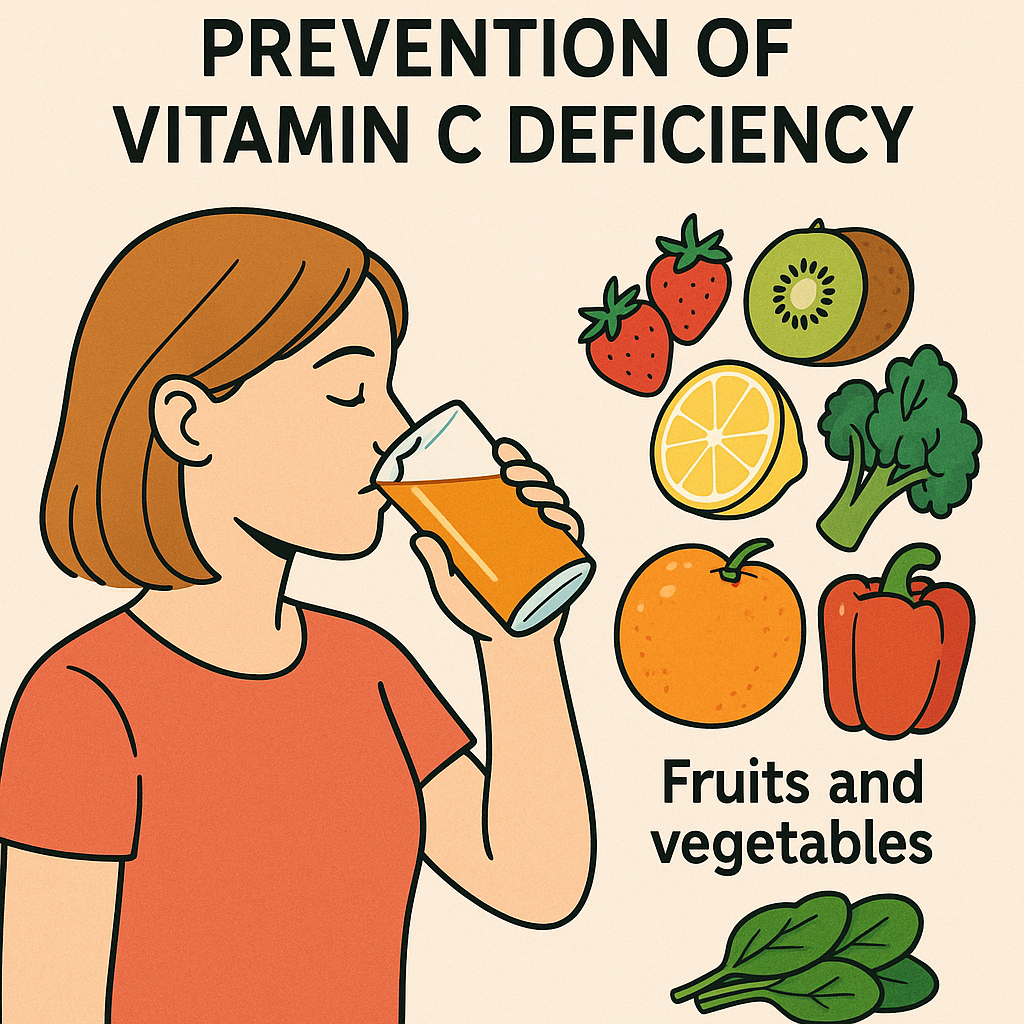
✅ Daily intake of Vitamin C-rich foods
✅ Education on proper infant feeding (avoid formula without supplementation)
✅ Avoiding excessive alcohol & smoking
✅ Regular vitamin C supplementation in at-risk individuals
✅ Fortification of staple foods
7. Nurses’ Role in Vitamin C Deficiency
A. Preventive Role
✅ Health Education on Nutrition:
- Teach importance of Vitamin C-rich diet
- Encourage intake of fresh fruits & vegetables
✅ Growth Monitoring & Early Detection:
- Assess infants & elderly for scurvy symptoms
- Identify high-risk groups (alcoholics, pregnant women, smokers)
✅ Community-Based Vitamin C Supplementation:
- Promote use of fortified foods & dietary supplements
✅ Public Health Programs:
- Implement nutrition awareness campaigns
- Support school meal programs with fresh fruit inclusion
B. Nurses’ Role in Diagnosis & Management
✅ Assess & Monitor Symptoms:
- Bleeding gums, bruising, joint pain, delayed wound healing
✅ Administer Vitamin C Therapy:
- Provide oral or IV vitamin C supplementation
- Monitor for improvement in symptoms
✅ Supportive Care:
- Encourage hydration & balanced diet
- Manage anemia with iron & folic acid supplements
✅ Refer Severe Cases:
- If neurological symptoms, severe anemia, or bleeding persist
C. Nurses’ Role in Public Health & Government Programs
✅ Implement National Nutrition Programs:
- Poshan Abhiyan – Nutritional supplementation for children
- Mid-Day Meal Scheme (MDMS) – Vitamin C-enriched school meals
✅ Community-Based Nutritional Interventions:
- Organize health camps for early detection
- Ensure Vitamin C supplementation in at-risk populations.
Vitamin D Deficiency Disorders.
1. Introduction
Vitamin D is a fat-soluble vitamin essential for calcium absorption, bone health, immune function, and muscle strength. Vitamin D deficiency (VDD) can lead to rickets in children, osteomalacia in adults, and osteoporosis in the elderly.
2. Causes of Vitamin D Deficiency
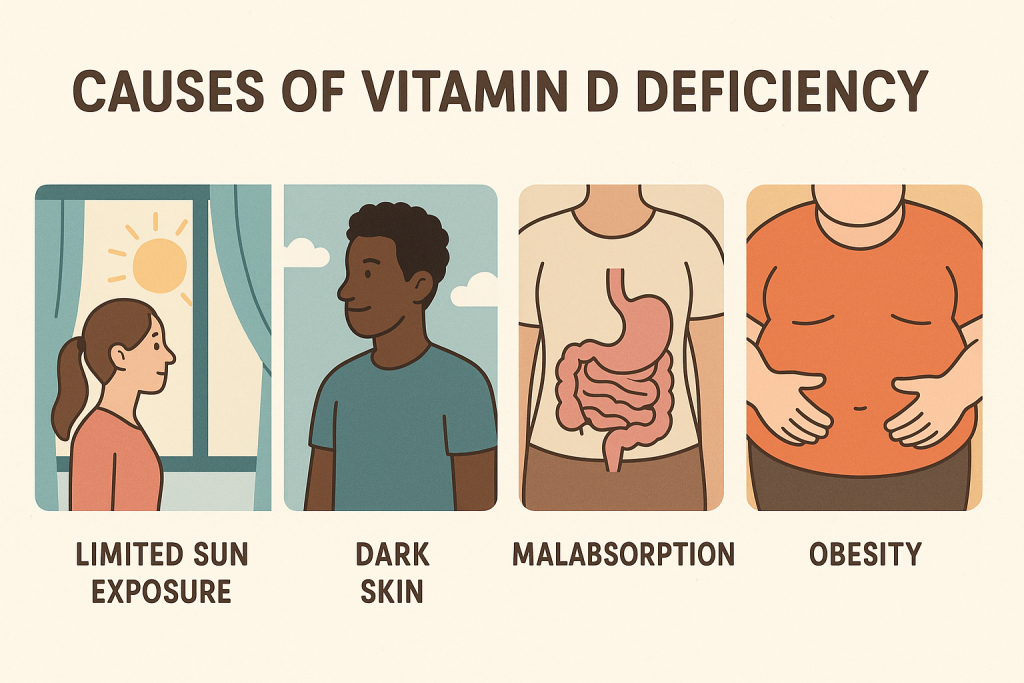
Vitamin D deficiency occurs due to inadequate sunlight exposure, dietary deficiency, malabsorption, or increased demand.
A. Primary Causes (Lifestyle & Dietary Deficiency)
✅ Inadequate Sunlight Exposure:
- Spending most time indoors.
- Use of sunscreen and covering clothing.
- Living in high-latitude areas with low UV exposure.
✅ Poor Dietary Intake:
- Lack of Vitamin D-rich foods (fish, dairy, eggs, fortified foods).
- Vegetarian or vegan diets (low in animal sources of Vitamin D).
B. Secondary Causes (Medical Conditions)
✅ Malabsorption Disorders:
- Celiac disease, Crohn’s disease, cystic fibrosis, liver disease.
- Gastric bypass surgery affecting Vitamin D absorption.
✅ Kidney & Liver Disorders:
- Chronic kidney disease (CKD) → Cannot convert Vitamin D into active form.
- Liver disease → Reduces Vitamin D metabolism.
✅ Increased Vitamin D Demand:
- Pregnancy & lactation.
- Elderly individuals (reduced skin synthesis of Vitamin D).
- Obesity (Vitamin D gets trapped in fat tissue and is unavailable for use).
✅ Long-Term Use of Medications:
- Antiepileptic drugs (Phenytoin, Carbamazepine).
- Steroids (Prednisone).
- Weight-loss drugs (Orlistat).
3. Signs & Symptoms of Vitamin D Deficiency

A. Bone & Muscular Symptoms
✅ Bone pain & tenderness (especially in lower back, pelvis, legs).
✅ Muscle weakness & cramps.
✅ Frequent fractures (due to weak bones).
✅ Osteoporosis (brittle bones in elderly adults).
B. Specific Disorders
✅ Rickets (Children):
- Delayed growth, bowing of legs, soft skull bones.
- Dental problems (delayed tooth eruption, enamel defects).
- Knock-knees & bone deformities.
✅ Osteomalacia (Adults):
- Soft, weak bones leading to fractures.
- Difficulty walking, waddling gait.
✅ Immune System Dysfunction:
- Frequent infections (increased risk of respiratory infections, COVID-19).
✅ Neurological & Psychological Issues:
- Fatigue & depression.
- Memory loss & confusion (in elderly).
✅ Cardiovascular Issues:
- Increased risk of hypertension, heart disease.
4. Diagnosis of Vitamin D Deficiency

A. Clinical Examination
✅ Assess bone pain, muscle weakness, fractures.
✅ Check for rickets (bowed legs, enlarged joints in children).
✅ Evaluate history of limited sun exposure & poor diet.
B. Laboratory Tests
✅ Serum 25-Hydroxyvitamin D (25-OH D) Level:
- >30 ng/mL – Normal
- 20–30 ng/mL – Insufficient
- <20 ng/mL – Deficient
- <10 ng/mL – Severe Deficiency
✅ Serum Calcium, Phosphorus, and Alkaline Phosphatase:
- Low calcium & phosphorus levels.
- High alkaline phosphatase (in bone diseases).
✅ Parathyroid Hormone (PTH) Test:
- Elevated PTH (secondary hyperparathyroidism due to low Vitamin D levels).
✅ X-rays & Bone Densitometry (DEXA Scan):
- Detects bone softening (osteomalacia) or bone density loss (osteoporosis).
5. Management of Vitamin D Deficiency
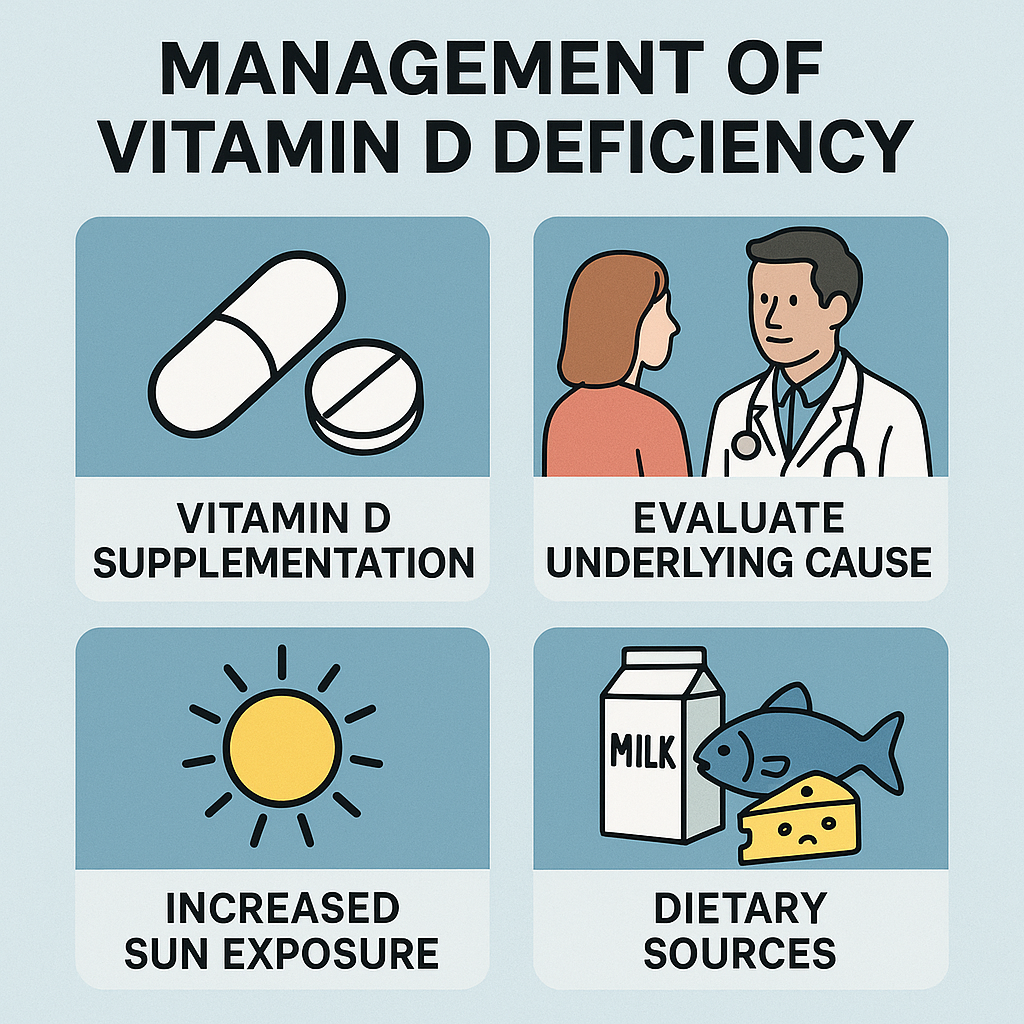
A. Dietary Modification
✅ Increase intake of Vitamin D-rich foods:
- Fatty fish (salmon, mackerel, tuna).
- Egg yolks, dairy products, cheese.
- Fortified foods (milk, cereals, orange juice, soy products).
✅ Encourage cooking with Vitamin D-fortified oils.
B. Sunlight Exposure (Natural Vitamin D Synthesis)
✅ Daily sun exposure (10-30 min on face, arms, hands without sunscreen).
✅ Best time for exposure: 10 AM to 3 PM.
C. Vitamin D Supplementation
✅ For Mild Deficiency (20–30 ng/mL):
- 600–1000 IU/day (adults & children).
- During pregnancy: 1000 IU/day.
✅ For Moderate Deficiency (10–20 ng/mL):
- 50,000 IU weekly for 6-8 weeks, then maintenance dose of 1000–2000 IU/day.
✅ For Severe Deficiency (<10 ng/mL, Rickets, Osteomalacia):
- Intramuscular Vitamin D (Cholecalciferol 300,000 IU once).
- Oral high-dose Vitamin D (50,000 IU weekly for 8 weeks).
✅ For Osteoporosis & Elderly:
- Vitamin D3 (1000–2000 IU daily) + Calcium supplements (1000 mg/day).
6. Prevention of Vitamin D Deficiency
✅ Daily Sunlight Exposure (10–30 minutes per day).
✅ Balanced Diet with Vitamin D-Rich Foods.
✅ Fortified Milk, Cereals, and Orange Juice.
✅ Regular Health Checkups for High-Risk Groups (elderly, pregnant women, people with malabsorption disorders).
✅ Vitamin D Supplements in High-Risk Individuals.
7. Nurses’ Role in Vitamin D Deficiency
A. Preventive Role
✅ Health Education on Sunlight Exposure & Diet:
- Teach importance of sun exposure for Vitamin D synthesis.
- Educate on Vitamin D-rich foods & fortified products.
✅ Screening & Early Detection:
- Conduct growth monitoring & bone health assessments.
- Identify high-risk individuals (elderly, pregnant women, malnourished children).
✅ Community-Based Vitamin D Supplementation:
- Provide prenatal & postnatal supplements to mothers & infants.
- Encourage fortified food consumption.
B. Nurses’ Role in Diagnosis & Management
✅ Assess & Monitor Symptoms:
- Bone pain, muscle weakness, fractures, growth delays.
✅ Administer Vitamin D Therapy:
- Oral & IV Vitamin D supplementation as prescribed.
- Ensure adherence to treatment in high-risk patients.
✅ Supportive Care:
- Encourage regular exercise to strengthen bones.
- Provide calcium supplementation when needed.
✅ Refer Severe Cases:
- Patients with severe osteoporosis, fractures, neurological complications.
C. Nurses’ Role in Public Health & Government Programs
✅ Implement National Health Programs:
- Poshan Abhiyan – Nutrition for pregnant & lactating mothers.
- Mid-Day Meal Scheme (MDMS) – Fortified school meals.
- National Osteoporosis Awareness Program.
✅ Community Awareness Campaigns:
- Organize Vitamin D awareness workshops.
- Promote early detection & nutritional interventions.
Vitamin E Deficiency Disorders.
1. Introduction
Vitamin E is a fat-soluble antioxidant essential for immune function, neurological health, and cell membrane protection. Vitamin E deficiency (VED) is rare but can lead to nerve damage, muscle weakness, vision problems, and immune dysfunction.
2. Causes of Vitamin E Deficiency
Vitamin E deficiency occurs due to poor dietary intake, malabsorption, increased oxidative stress, or genetic disorders.
A. Primary Causes (Dietary Deficiency)
✅ Inadequate intake of Vitamin E-rich foods:
- Nuts, seeds, vegetable oils, leafy greens, whole grains.
✅ Strict low-fat diets: - Reduces absorption of fat-soluble vitamins like Vitamin E.
B. Secondary Causes (Medical Conditions & Increased Demand)
✅ Malabsorption Disorders:
- Celiac disease, Crohn’s disease, cystic fibrosis, chronic pancreatitis.
- Biliary disorders (gallbladder/liver diseases) reduce fat digestion.
✅ Genetic Disorders:
- Ataxia with Vitamin E Deficiency (AVED): A rare genetic disorder.
✅ Premature Birth & Low Birth Weight:
- Neonates born before 32 weeks have low Vitamin E stores.
✅ Increased Oxidative Stress:
- Smokers, alcoholics, and individuals exposed to pollutants.
✅ Long-Term Use of Medications:
- Fat blockers (Orlistat), anticonvulsants (Phenytoin), chemotherapy drugs.
3. Signs & Symptoms of Vitamin E Deficiency
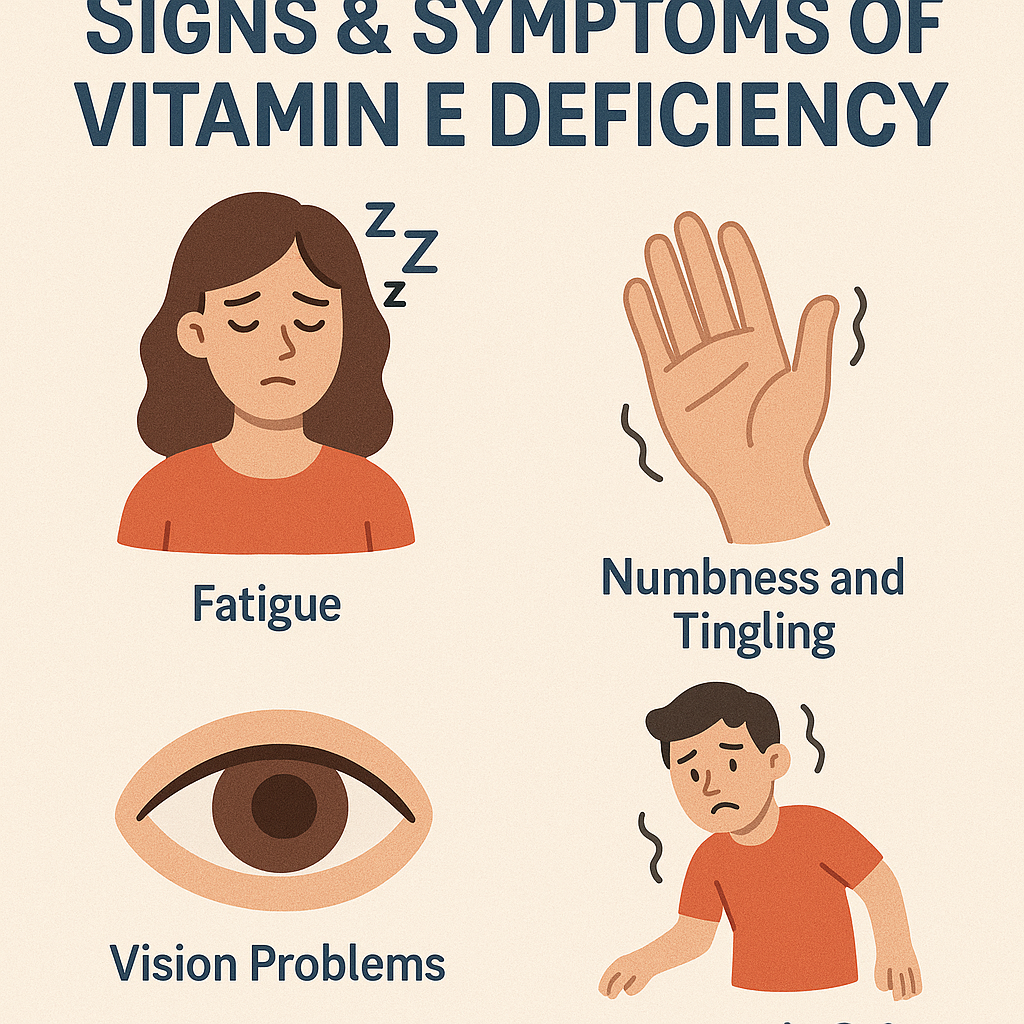
Vitamin E deficiency primarily affects neuromuscular function, vision, and immune system.
A. Neurological Symptoms (Peripheral Neuropathy)
✅ Muscle weakness (due to nerve damage).
✅ Loss of coordination (Ataxia) – Difficulty walking.
✅ Numbness & tingling in extremities (peripheral neuropathy).
✅ Decreased reflexes & balance problems.
B. Vision Problems
✅ Blurry vision (due to retinal degeneration).
✅ Night blindness & eye muscle weakness.
✅ Increased risk of cataracts.
C. Immune Dysfunction
✅ Frequent infections & slow wound healing.
✅ Increased susceptibility to respiratory illnesses.
D. Hematological Symptoms
✅ Hemolytic anemia (Red blood cell breakdown in newborns).
✅ Increased oxidative damage leading to premature aging.
4. Diagnosis of Vitamin E Deficiency

A. Clinical Examination
✅ Assess for muscle weakness, coordination problems, vision issues.
✅ Check history of malabsorption disorders or poor diet.
B. Laboratory Tests
✅ Serum Alpha-Tocopherol Levels:
- >5 mg/L – Normal.
- 2–5 mg/L – Insufficient.
- <2 mg/L – Deficient.
✅ Nerve Conduction Studies – Identifies neuropathy.
✅ Retinal Examination – Detects vision-related complications.
✅ Complete Blood Count (CBC) – To check for hemolytic anemia.
5. Management of Vitamin E Deficiency
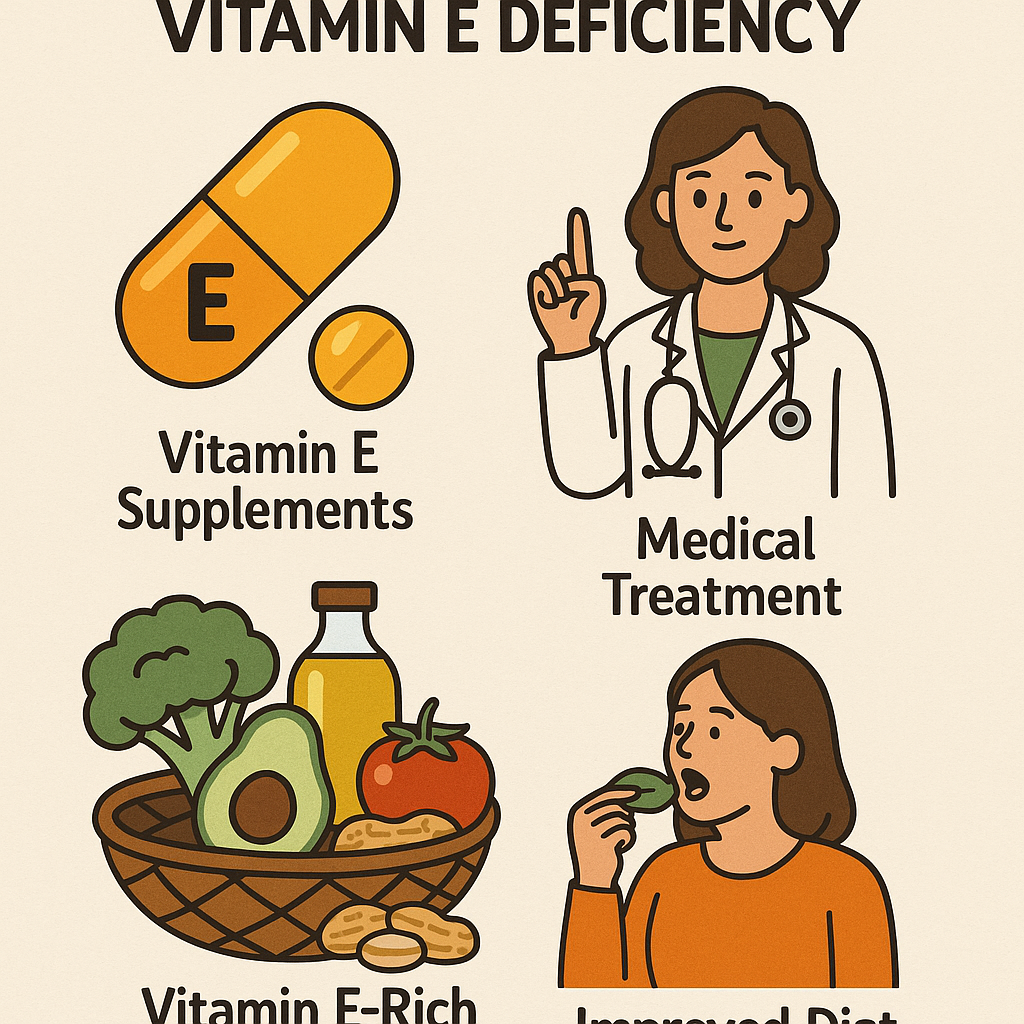
A. Dietary Modification
✅ Increase intake of Vitamin E-rich foods:
- Nuts & seeds: Almonds, sunflower seeds, hazelnuts.
- Vegetable oils: Sunflower, safflower, olive oil.
- Leafy greens: Spinach, kale, broccoli.
- Whole grains, avocados, and fortified cereals.
✅ Cooking with healthy oils to enhance Vitamin E absorption.
B. Vitamin E Supplementation
✅ For Mild Deficiency:
- Oral Vitamin E (100-400 IU/day).
✅ For Moderate Deficiency (Neurological Symptoms):
- 800–1000 IU/day (Alpha-Tocopherol).
✅ For Severe Deficiency (Ataxia, Neuropathy, Vision Loss):
- 1500–2000 IU/day (under medical supervision).
✅ For Premature Infants at Risk of Hemolytic Anemia:
- Vitamin E supplementation via IV or nasogastric feeding.
✅ For Malabsorption Syndromes:
- High-dose Vitamin E (Intramuscular injection if necessary).
6. Prevention of Vitamin E Deficiency
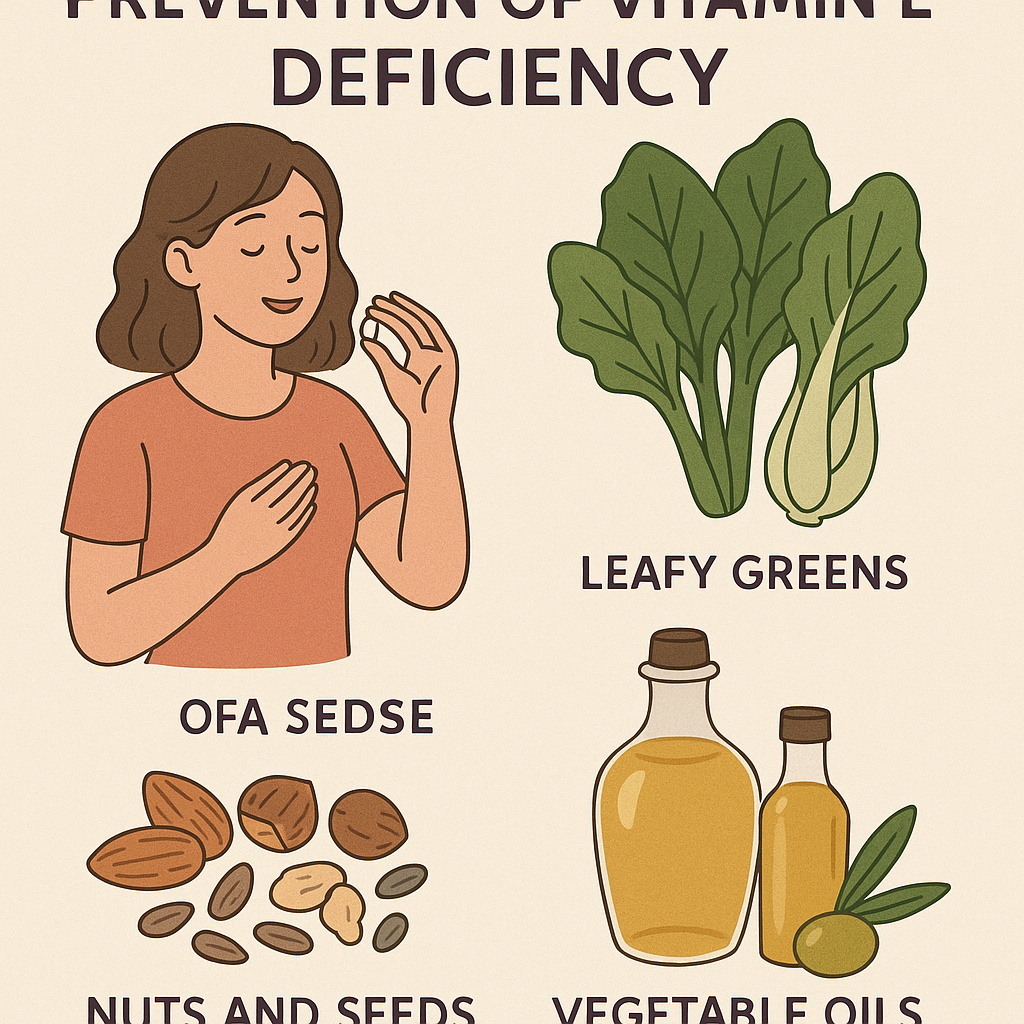
✅ Daily consumption of Vitamin E-rich foods.
✅ Breastfeeding or fortified infant formula for neonates.
✅ Balanced diet with sufficient healthy fats.
✅ Regular health checkups for high-risk individuals (malabsorption conditions, premature infants).
✅ Avoiding excessive alcohol & smoking (reduces oxidative stress).
✅ Food fortification programs (Vitamin E-enriched cereals, dairy).
7. Nurses’ Role in Vitamin E Deficiency
A. Preventive Role
✅ Health Education on Nutrition:
- Promote Vitamin E-rich diets.
- Teach proper cooking methods to preserve Vitamin E.
✅ Screening & Early Detection:
- Assess children, elderly, and malnourished individuals for deficiency symptoms.
- Identify high-risk groups (smokers, alcoholics, chronic illness patients).
✅ Community-Based Nutritional Support:
- Encourage fortified foods for at-risk populations.
- Support prenatal & infant supplementation programs.
✅ Public Health Programs:
- Implement nutrition awareness campaigns.
- Support government food fortification initiatives.
B. Nurses’ Role in Diagnosis & Management
✅ Assess & Monitor Symptoms:
- Muscle weakness, poor reflexes, vision impairment.
✅ Administer Vitamin E Therapy:
- Provide oral or IV Vitamin E supplements as prescribed.
- Ensure adherence to treatment in high-risk patients.
✅ Supportive Care:
- Encourage physical therapy for neuropathy.
- Monitor vision changes & refer to ophthalmology if needed.
✅ Refer Severe Cases:
- Patients with severe neurological impairments or retinal damage.
C. Nurses’ Role in Public Health & Government Programs
✅ Implement National Nutrition Programs:
- Poshan Abhiyan – Nutritional support for pregnant women & children.
- Mid-Day Meal Scheme (MDMS) – Fortified school meals.
- Neonatal Nutrition Programs – Preventing Vitamin E-related anemia in infants.
✅ Community Awareness Campaigns:
- Organize Vitamin E awareness workshops.
- Promote early detection & nutritional interventions.
Vitamin K Deficiency Disorders.
1. Introduction
Vitamin K is a fat-soluble vitamin essential for blood clotting, bone metabolism, and cardiovascular health. Vitamin K deficiency leads to excessive bleeding (hemorrhagic disorders), bone fragility, and vascular calcification.
2. Causes of Vitamin K Deficiency
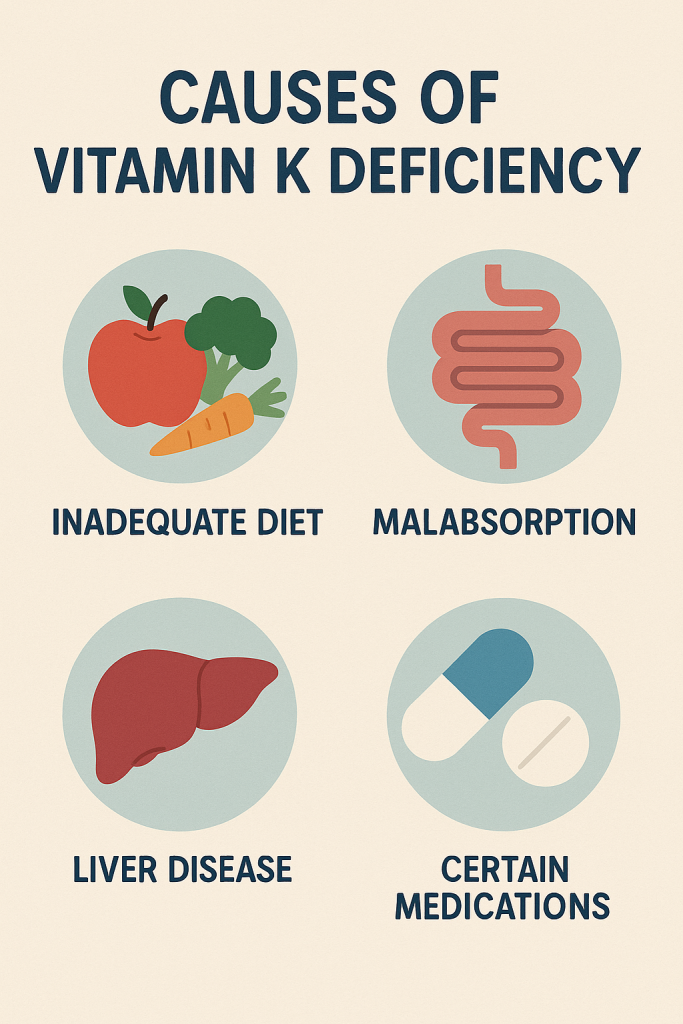
Vitamin K deficiency occurs due to poor dietary intake, impaired absorption, liver disease, or use of certain medications.
A. Primary Causes (Dietary Deficiency)
✅ Inadequate intake of Vitamin K-rich foods:
- Green leafy vegetables, liver, dairy, fermented foods.
✅ Strict low-fat diets: - Reduces absorption of fat-soluble vitamins.
B. Secondary Causes (Medical Conditions & Increased Demand)
✅ Malabsorption Disorders:
- Celiac disease, Crohn’s disease, cystic fibrosis, chronic pancreatitis.
- Biliary disorders (gallbladder/liver diseases) reduce fat digestion.
✅ Liver Disease:
- Liver synthesizes clotting factors that require Vitamin K.
- Cirrhosis, hepatitis, liver failure increase bleeding risk.
✅ Prolonged Antibiotic Use:
- Kills gut bacteria that synthesize Vitamin K (especially in newborns).
✅ Newborn Vitamin K Deficiency (Hemorrhagic Disease of the Newborn):
- Newborns lack gut bacteria to produce Vitamin K.
- Poor placental transfer of Vitamin K.
✅ Long-Term Use of Medications:
- Blood thinners (Warfarin, Heparin) – Inhibits Vitamin K function.
- Antibiotics (Cephalosporins) – Reduce Vitamin K absorption.
- Cholesterol-lowering drugs (Bile acid sequestrants).
3. Signs & Symptoms of Vitamin K Deficiency
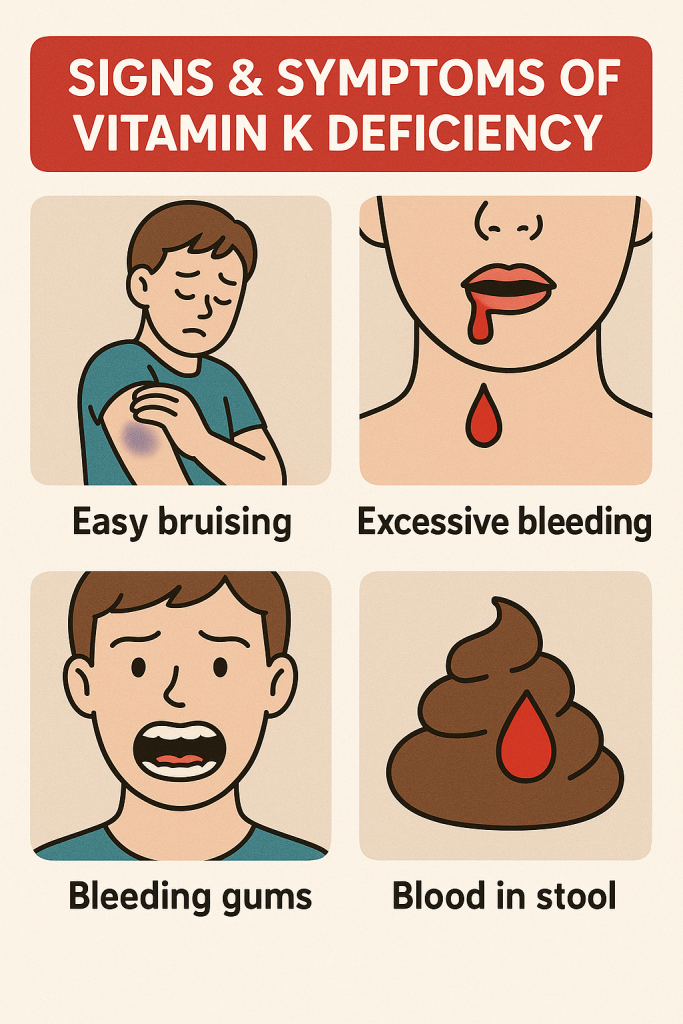
A. Bleeding Disorders (Hemorrhagic Symptoms)
✅ Easy bruising & frequent nosebleeds.
✅ Bleeding gums & prolonged bleeding from minor cuts.
✅ Heavy menstrual bleeding in women.
✅ Gastrointestinal bleeding (bloody stools, black tarry stools).
✅ Intracranial bleeding (severe cases in newborns).
B. Bone & Skeletal Issues
✅ Osteoporosis & weak bones (due to reduced calcium regulation).
✅ Increased risk of fractures.
C. Newborn Hemorrhagic Disease
✅ Bleeding from the umbilical cord stump.
✅ Brain hemorrhages (intracranial bleeding).
✅ Excessive post-circumcision bleeding.
4. Diagnosis of Vitamin K Deficiency
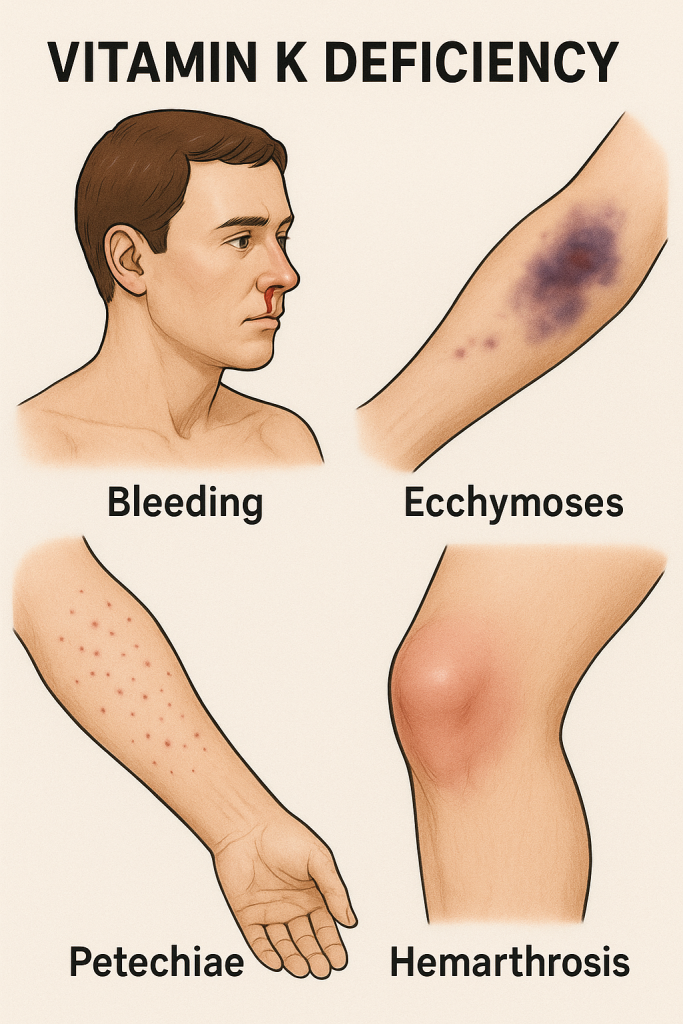
A. Clinical Examination
✅ Assess for unexplained bleeding, bruising, and slow clotting.
✅ Check history of liver disease, malabsorption disorders, and medication use.
B. Laboratory Tests
✅ Prothrombin Time (PT) & International Normalized Ratio (INR):
- PT prolonged (>14 sec) indicates Vitamin K deficiency.
- INR >1.4 suggests impaired clotting.
✅ Activated Partial Thromboplastin Time (aPTT) – May be prolonged.
✅ Plasma Vitamin K Levels – Low in deficiency.
✅ Liver Function Tests – To check for liver disease.
5. Management of Vitamin K Deficiency
A. Dietary Modification
✅ Increase intake of Vitamin K-rich foods:
- Green leafy vegetables: Spinach, kale, broccoli, cabbage.
- Animal sources: Liver, eggs, dairy products.
- Fermented foods: Natto (Japanese fermented soybeans).
✅ Cooking with healthy oils (olive oil, canola oil) to improve absorption.
B. Vitamin K Supplementation
✅ For Mild Deficiency (Bleeding Tendency)
- Oral Vitamin K1 (Phytonadione) 2.5–10 mg/day.
✅ For Severe Bleeding (Excessive Bruising, Hemorrhage)
- Intravenous (IV) Vitamin K1 (Phytonadione 1–10 mg slow IV push).
✅ For Patients on Warfarin with High INR
- Oral Vitamin K1 (2.5–5 mg) for moderate INR elevation.
- IV Vitamin K1 for INR >6 with bleeding symptoms.
✅ For Newborns (Prevention of Hemorrhagic Disease)
- Single intramuscular (IM) injection of Vitamin K1 (1 mg) at birth.
✅ For Malabsorption Syndromes
- High-dose Vitamin K (Oral or IV, 10 mg daily).
6. Prevention of Vitamin K Deficiency
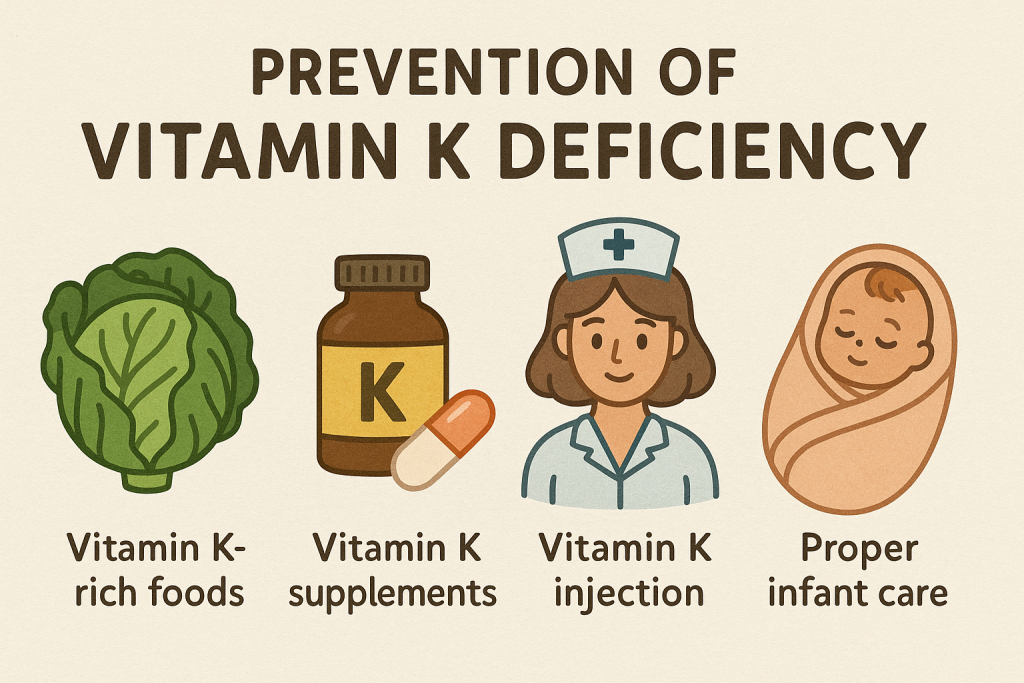
✅ Daily consumption of Vitamin K-rich foods.
✅ Routine Vitamin K injection at birth for newborns.
✅ Balanced diet with sufficient healthy fats to aid Vitamin K absorption.
✅ Regular health checkups for liver and gastrointestinal conditions.
✅ Avoiding long-term use of antibiotics and Warfarin without monitoring.
✅ Food fortification programs (Vitamin K-enriched dairy & cereals).
7. Nurses’ Role in Vitamin K Deficiency
A. Preventive Role
✅ Health Education on Diet & Nutrition:
- Promote Vitamin K-rich diets.
- Teach importance of dietary fat for vitamin absorption.
✅ Screening & Early Detection:
- Assess infants, elderly, and malnourished individuals.
- Identify high-risk individuals (patients on Warfarin, liver disease patients).
✅ Community-Based Nutritional Support:
- Ensure Vitamin K supplementation in high-risk populations.
- Encourage fortified food consumption.
✅ Public Health Programs:
- Implement nutrition awareness campaigns.
- Support government food fortification initiatives.
B. Nurses’ Role in Diagnosis & Management
✅ Assess & Monitor Symptoms:
- Easy bruising, excessive bleeding, prolonged clotting.
✅ Administer Vitamin K Therapy:
- Provide oral, IM, or IV Vitamin K supplements as prescribed.
- Ensure adherence to treatment in high-risk patients.
✅ Supportive Care:
- Monitor for signs of excessive bleeding & clotting abnormalities.
- Assist with wound care & prevention of injury in bleeding patients.
✅ Refer Severe Cases:
- Patients with severe hemorrhage, liver failure, or surgical bleeding risks.
C. Nurses’ Role in Public Health & Government Programs
✅ Implement National Nutrition Programs:
- Poshan Abhiyan – Nutritional support for pregnant women & children.
- Mid-Day Meal Scheme (MDMS) – Fortified school meals.
- Neonatal Nutrition Programs – Preventing Vitamin K deficiency in infants.
✅ Community Awareness Campaigns:
- Organize Vitamin K awareness workshops.
- Promote early detection & nutritional interventions.
Nurses’ Role in Vitamin Deficiency Disorders.
1. Introduction
Vitamin deficiency disorders occur due to inadequate intake, poor absorption, or increased bodily demand for vitamins. These deficiencies affect multiple systems, leading to conditions such as anemia (Vitamin B12, Folate), rickets (Vitamin D), night blindness (Vitamin A), bleeding disorders (Vitamin K), and neurological issues (Vitamin B1, B6, E).
Nurses play a crucial role in the prevention, early detection, management, and rehabilitation of individuals suffering from vitamin deficiencies.
2. Nurses’ Role in the Prevention of Vitamin Deficiency Disorders
A. Health Education & Awareness
✅ Educating Communities on Balanced Diet:
- Promote vitamin-rich foods (fruits, vegetables, dairy, meats, whole grains).
- Encourage consumption of fortified foods (milk, cereals, oils, rice).
- Guide vegetarians and vegans on alternative sources of vitamins (e.g., plant-based Vitamin B12 supplements).
✅ Importance of Breastfeeding & Infant Nutrition:
- Encourage exclusive breastfeeding for the first 6 months (rich in Vitamins A, D, E, K).
- Guide mothers on nutritious complementary feeding from 6 months.
✅ Sunlight Exposure for Vitamin D Synthesis:
- Recommend 10-30 minutes of daily sun exposure for children & adults.
✅ Hygiene & Safe Food Practices:
- Prevent contaminated food intake, which can lead to malabsorption syndromes.
B. Nutritional Screening & Growth Monitoring
✅ Anthropometric Assessments:
- Monitor weight, height, and Mid-Upper Arm Circumference (MUAC) for malnutrition.
- Identify children at risk of stunting (Vitamin A, D deficiency) or wasting (protein-energy malnutrition).
✅ Dietary History & Risk Assessment:
- Assess patients’ daily intake of vitamin-rich foods.
- Identify pregnant/lactating women, elderly, alcoholics, and malabsorption patients at high risk.
✅ Neonatal & Infant Vitamin Deficiency Screening:
- Newborns are screened for Vitamin K deficiency (risk of hemorrhagic disease).
- Monitor for Vitamin D deficiency (rickets prevention in infants).
✅ Immunization & Vitamin Supplementation:
- Ensure administration of Vitamin A mega-doses as per WHO recommendations.
- Provide prenatal vitamin supplements to pregnant women (Folic acid, Iron, Calcium, Vitamin D).
3. Nurses’ Role in Diagnosis & Early Detection
✅ Identify Early Symptoms of Vitamin Deficiencies:
- Vitamin A Deficiency → Night blindness, dry skin.
- Vitamin D Deficiency → Rickets (children), osteomalacia (adults).
- Vitamin E Deficiency → Muscle weakness, vision problems, neuropathy.
- Vitamin K Deficiency → Excessive bleeding, bruising.
- Vitamin B Deficiencies → Fatigue, anemia, neurological issues.
- Vitamin C Deficiency → Scurvy (bleeding gums, poor wound healing).
✅ Laboratory Investigations:
- Assist in blood tests for Vitamin B12, Vitamin D, Folate, and Iron levels.
- Monitor clotting time (INR/PT) in suspected Vitamin K deficiency cases.
- Support X-rays for bone deformities in rickets.
✅ Neurological & Physical Assessments:
- Test reflexes, muscle coordination, balance (Vitamin B12, E deficiency).
- Observe for bone deformities, gait abnormalities (Vitamin D deficiency).
4. Nurses’ Role in the Management of Vitamin Deficiency Disorders
A. Dietary & Lifestyle Interventions
✅ Personalized Nutrition Plans:
- Recommend high-protein diets for Vitamin B12, Iron, and Folate deficiency.
- Advise high-calcium and Vitamin D diets for bone health.
- Encourage Vitamin C-rich foods for immunity and wound healing.
✅ Encouraging Physical Activity & Sunlight Exposure:
- Guide patients on safe sun exposure for Vitamin D synthesis.
- Promote exercise to prevent osteoporosis and muscle weakness.
B. Medical & Supplement Therapy
✅ Administer Vitamin Supplements:
- Vitamin A Deficiency:
- Oral dose: 100,000–200,000 IU every 6 months for children.
- Vitamin D Deficiency:
- 600–1000 IU/day for adults; 400 IU/day for infants.
- Vitamin B12 Deficiency:
- 1000 mcg IM injection for severe cases.
- Vitamin C Deficiency:
- 300–1000 mg/day (oral or IV for severe scurvy).
- Vitamin K Deficiency:
- 1 mg IM injection at birth for newborns to prevent hemorrhagic disease.
✅ Manage Associated Conditions:
- Iron & Folic Acid for anemia (in Vitamin B12/B9 deficiency).
- Calcium & Vitamin D for osteoporosis.
- Vitamin E for nerve protection in neurological disorders.
C. Monitoring & Follow-Up Care
✅ Regular Monitoring of At-Risk Patients:
- Pregnant women (Folate, Iron, Calcium, Vitamin D levels).
- Elderly individuals (Vitamin B12, D, Calcium levels).
- Children with growth failure or developmental delays.
✅ Prevent Relapse:
- Teach proper cooking methods to retain vitamin content in food.
- Educate on long-term dietary changes for sustained improvement.
✅ Emotional & Psychosocial Support:
- Address food insecurity issues by referring families to community nutrition programs.
5. Nurses’ Role in Public Health & Government Nutrition Programs
A. Implementation of National & WHO Nutrition Programs
✅ Integrated Child Development Services (ICDS) – Nutritional support for children & mothers.
✅ Mid-Day Meal Scheme (MDMS) – Fortified school meals to combat malnutrition.
✅ National Nutrition Mission (Poshan Abhiyan) – Awareness campaigns on vitamin deficiencies.
✅ Iron & Folic Acid Supplementation (IFAS) Program – Anemia prevention among women & children.
✅ Neonatal Vitamin K Injection Program – Prevents newborn hemorrhagic disease.
B. Community-Based Interventions
✅ Organizing Health Camps for Nutritional Screening.
✅ Ensuring Supplement Distribution in High-Risk Areas.
✅ Advocating for Fortified Foods in Schools & Public Programs.
✅ Raising Awareness on the Risks of Vitamin Deficiencies.
Iron Deficiency Diseases.
1. Introduction
Iron is an essential mineral required for hemoglobin formation, oxygen transport, enzyme function, and cellular metabolism. Iron deficiency leads to anemia, fatigue, cognitive impairment, and weakened immunity. It is one of the most common nutritional deficiencies worldwide, affecting women, children, and individuals with poor dietary intake.
2. Causes of Iron Deficiency
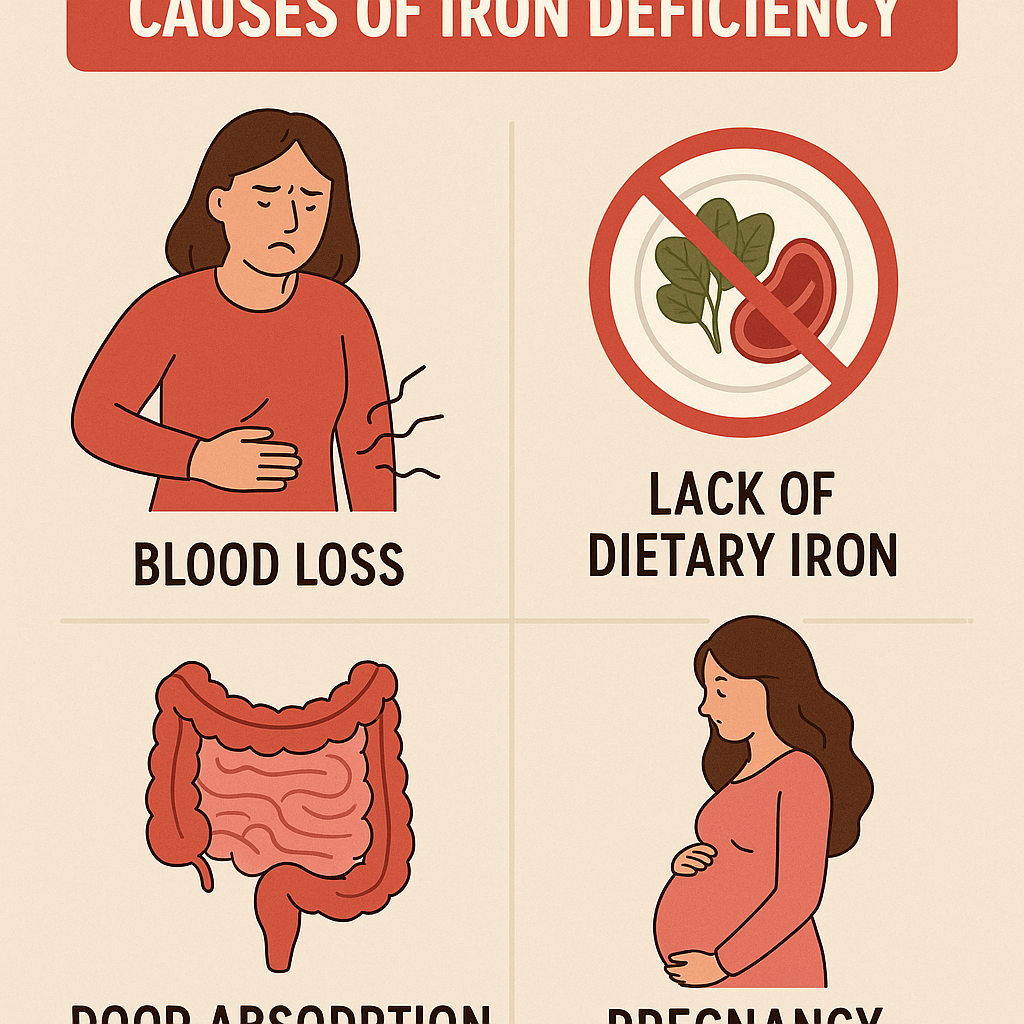
Iron deficiency occurs due to insufficient intake, poor absorption, increased demand, or excessive loss.
A. Primary Causes (Dietary Deficiency)
✅ Inadequate intake of iron-rich foods:
- Lack of red meat, poultry, fish, leafy greens, fortified grains.
✅ Vegetarian/Vegan diets: - Plant-based iron (non-heme iron) has lower absorption than animal-based iron (heme iron).
✅ Frequent consumption of tea/coffee: - Inhibits iron absorption due to tannins and polyphenols.
B. Secondary Causes (Increased Demand & Excessive Losses)
✅ Blood Loss:
- Heavy menstrual bleeding (Menorrhagia).
- Gastrointestinal bleeding (Ulcers, hemorrhoids, colorectal cancer, parasitic infections).
- Frequent blood donation.
✅ Poor Absorption:
- Celiac disease, Crohn’s disease, Helicobacter pylori infection.
- Bariatric surgery or chronic diarrhea reduces iron absorption.
✅ Increased Iron Requirement:
- Pregnancy & lactation (fetal development and maternal blood expansion).
- Rapid growth in infants, children, and adolescents.
3. Signs & Symptoms of Iron Deficiency

Iron deficiency progresses in stages, leading to mild, moderate, or severe anemia.
A. General Symptoms (Mild to Moderate Deficiency)
✅ Fatigue & weakness.
✅ Pale skin (Pallor) – noticeable on face, inside lower eyelids, and nails.
✅ Shortness of breath (Dyspnea), even with mild activity.
✅ Dizziness & headaches.
✅ Cold hands and feet due to poor circulation.
B. Severe Deficiency (Iron Deficiency Anemia – IDA)
✅ Brittle nails (Koilonychia – spoon-shaped nails).
✅ Cracked lips & sore tongue (Glossitis, Angular Cheilitis).
✅ Unusual cravings (Pica – eating non-food items like ice, dirt, chalk).
✅ Frequent infections due to weakened immunity.
✅ Restless legs syndrome (Neurological symptoms in severe cases).
4. Diagnosis of Iron Deficiency
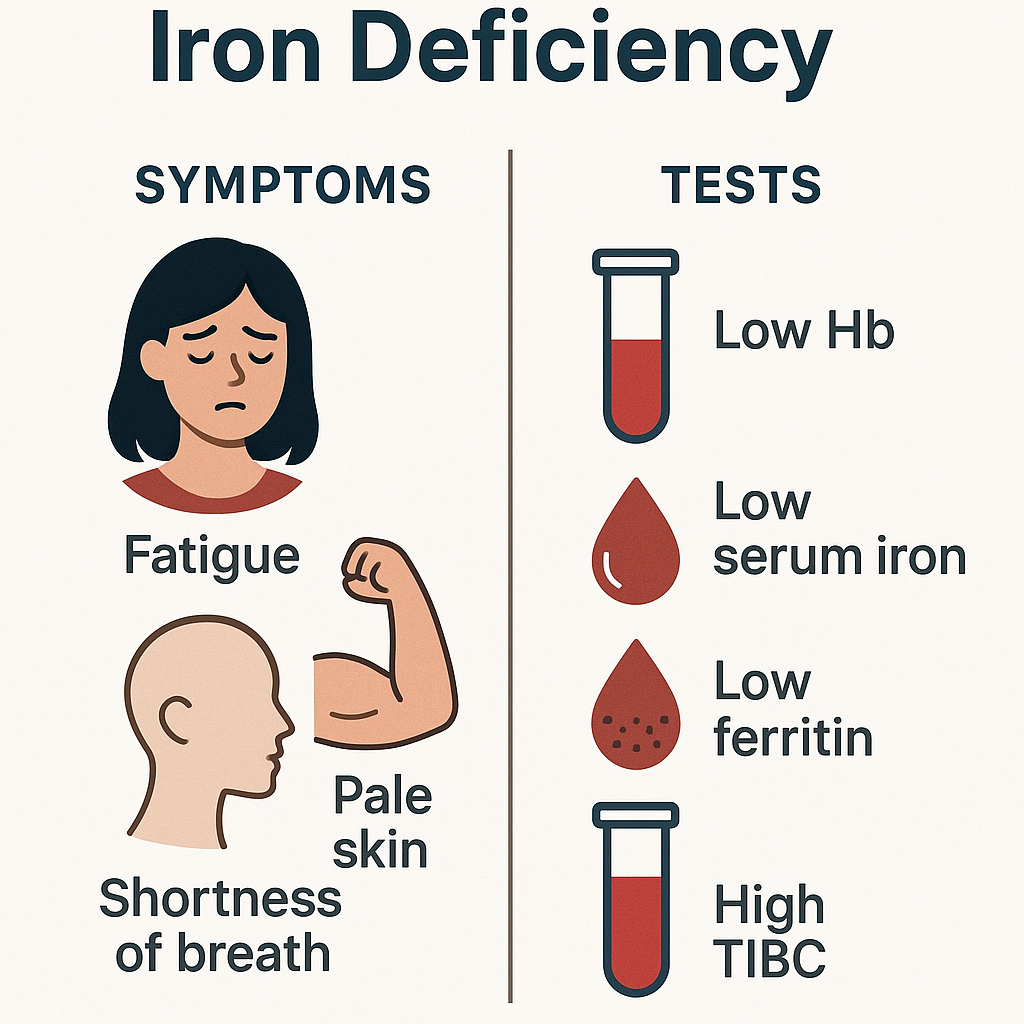
A. Clinical Examination
✅ Assess for symptoms: Fatigue, pallor, dizziness, brittle nails.
✅ Check dietary history & menstrual history for risk factors.
B. Laboratory Tests
✅ Complete Blood Count (CBC):
- Low hemoglobin (Hb): <12 g/dL (women), <13 g/dL (men).
- Low hematocrit (Hct) & Mean Corpuscular Volume (MCV) – Microcytic anemia.
✅ Serum Ferritin (Iron storage levels):
- <15 ng/mL – Iron deficiency.
✅ Serum Iron & Total Iron Binding Capacity (TIBC):
- Low serum iron, high TIBC indicates iron deficiency.
✅ Peripheral Blood Smear:
- Microcytic (small) and hypochromic (pale) red blood cells.
✅ Reticulocyte Count:
- Low in iron deficiency, high in blood loss anemia.
✅ Fecal Occult Blood Test (FOBT):
- Checks for hidden blood loss in stools.
✅ Bone Marrow Biopsy (Severe Cases):
- Confirms absence of iron stores.
5. Management of Iron Deficiency
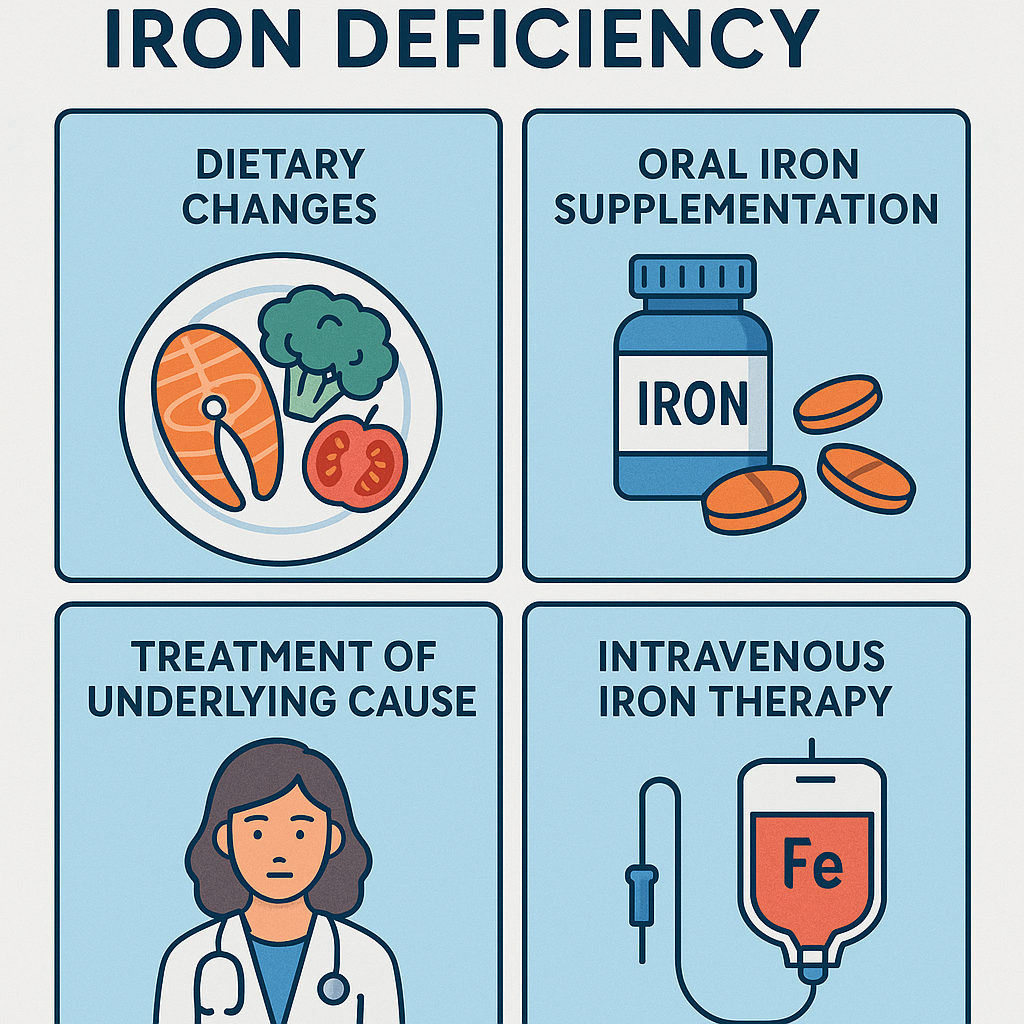
A. Dietary Modification
✅ Increase intake of iron-rich foods:
- Heme iron (better absorption): Red meat, liver, fish, chicken.
- Non-heme iron (plant-based): Spinach, lentils, beans, tofu, nuts.
- Iron-fortified foods: Cereals, bread, milk.
✅ Enhance iron absorption:
- Vitamin C-rich foods (oranges, tomatoes, bell peppers) boost iron uptake.
- Avoid tea/coffee with meals (tannins inhibit iron absorption).
B. Iron Supplementation Therapy
✅ Oral Iron Therapy (Mild to Moderate Cases):
- Ferrous sulfate (325 mg/day) for 3-6 months.
- Side effects: Constipation, black stools, nausea (reduce by taking with meals).
✅ Intravenous (IV) Iron Therapy (Severe Cases or Malabsorption):
- Iron sucrose, iron dextran, or ferric carboxymaltose IV infusions.
- Used in chronic kidney disease (CKD), gastric bypass patients.
✅ Blood Transfusion (Life-Threatening Anemia, Hb <7 g/dL):
- Given when severe symptoms like heart failure or organ dysfunction occur.
6. Prevention of Iron Deficiency
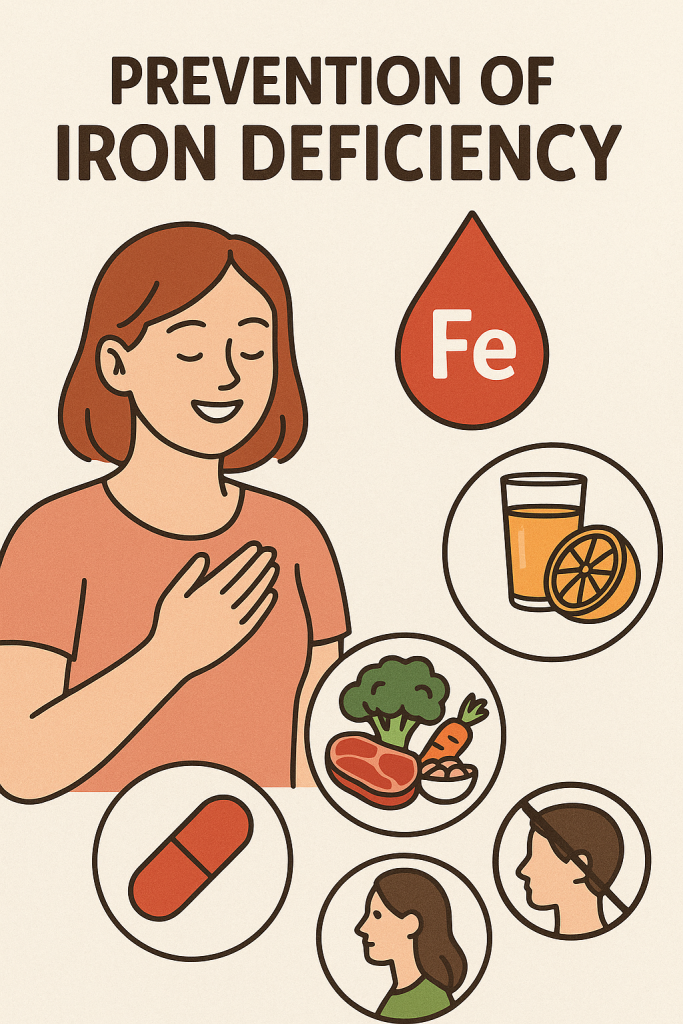
✅ Balanced Diet with Iron-Rich Foods.
✅ Vitamin C Intake for Better Iron Absorption.
✅ Iron-Fortified Foods for At-Risk Populations.
✅ Menstrual Health Awareness for Women (to prevent heavy blood loss).
✅ Deworming Programs (Albendazole/Mebendazole in endemic areas).
✅ Prenatal Iron Supplementation for Pregnant Women.
✅ Regular Health Checkups for High-Risk Groups.
7. Nurses’ Role in Iron Deficiency Anemia
A. Preventive Role
✅ Health Education on Iron-Rich Diets:
- Encourage animal and plant-based iron sources.
- Teach importance of Vitamin C to enhance iron absorption.
- Advise reducing tea/coffee intake around meals.
✅ Growth Monitoring & Early Screening:
- Check weight, height, and hemoglobin levels in infants & children.
- Screen pregnant women for anemia in prenatal clinics.
✅ Public Health Interventions:
- Support iron fortification programs in schools & communities.
- Promote deworming in school-aged children.
- Educate menstruating women on iron loss & supplementation.
B. Nurses’ Role in Diagnosis & Treatment
✅ Assess & Monitor Symptoms:
- Fatigue, pallor, shortness of breath, brittle nails.
✅ Administer Iron Therapy:
- Oral iron supplementation (educate on side effects & adherence).
- Intravenous iron infusions (for severe cases, CKD patients).
- Blood transfusions in critically anemic patients.
✅ Manage Side Effects of Iron Therapy:
- Advise taking iron supplements with meals to reduce nausea.
- Encourage high-fiber foods & fluids to prevent constipation.
✅ Supportive Care:
- Monitor hemoglobin improvement every 4-6 weeks.
- Encourage compliance with long-term iron therapy.
- Provide counseling for women with heavy menstrual bleeding.
✅ Refer Severe Cases:
- Uncontrolled anemia requiring transfusion.
- Suspected gastrointestinal bleeding requiring endoscopy.
C. Nurses’ Role in Public Health & Government Programs
✅ Implement National Anemia Control Programs:
- Iron & Folic Acid Supplementation (IFAS) for adolescent girls & pregnant women.
- Mid-Day Meal Scheme (MDMS) for school nutrition.
- Weekly Iron-Folic Acid Supplementation (WIFS) in schools.
✅ Community-Based Nutritional Interventions:
- Organize health camps for hemoglobin screening.
- Ensure iron-fortified food distribution in rural areas.
Iodine Deficiency Disorders.
1. Introduction
Iodine is an essential trace mineral required for the synthesis of thyroid hormones (T3 & T4), which regulate growth, metabolism, brain development, and energy production. Iodine deficiency leads to goiter, hypothyroidism, mental impairment, and developmental disorders.
Global & Indian Scenario
- Over 2 billion people worldwide are affected by iodine deficiency.
- India: Iodine deficiency remains a public health concern, despite the Universal Salt Iodization Program.
2. Causes of Iodine Deficiency
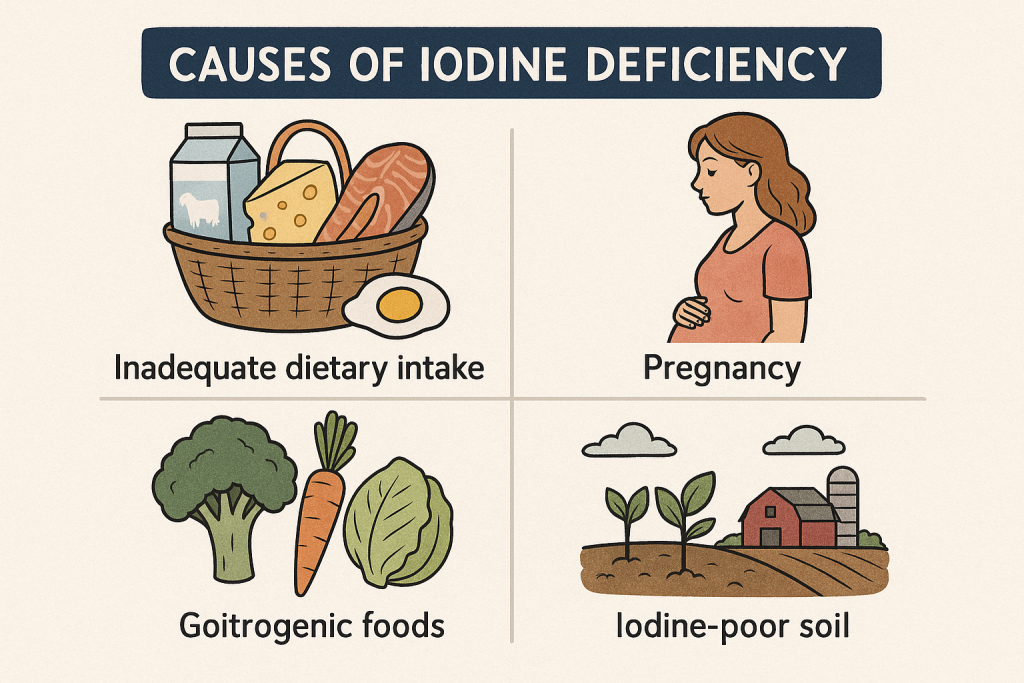
Iodine deficiency occurs due to inadequate intake, poor absorption, increased demand, or goitrogen consumption.
A. Primary Causes (Dietary Deficiency)
✅ Low intake of iodine-rich foods:
- Lack of iodized salt, seafood, dairy products, seaweed, eggs.
✅ Geographical iodine deficiency: - People in hilly regions & flood-prone areas (e.g., the Himalayas) have iodine-poor soil & water.
✅ Strict vegetarian/vegan diets: - Plant-based diets often lack sufficient iodine sources.
B. Secondary Causes (Increased Demand & Interference)
✅ Goitrogens (Substances that Block Iodine Absorption):
- Found in cabbage, cauliflower, broccoli, soybeans, cassava, peanuts.
✅ Pregnancy & Lactation: - Increased iodine requirement for fetal brain development.
✅ Chronic Illness & Malabsorption Disorders: - Celiac disease, Crohn’s disease, gastric bypass surgery.
3. Signs & Symptoms of Iodine Deficiency

Iodine deficiency leads to thyroid dysfunction, developmental delays, and metabolic disorders.
A. Goiter & Thyroid Disorders
✅ Enlarged thyroid gland (Goiter).
✅ Hypothyroidism (Low Thyroid Hormones):
- Fatigue, weight gain, dry skin, cold intolerance.
✅ Cretinism (Severe Iodine Deficiency in Infants): - Stunted growth, intellectual disability, deaf-mutism.
B. Neurological & Cognitive Impairment
✅ Poor memory, difficulty concentrating.
✅ Delayed brain development in children.
✅ Mental retardation (Severe deficiency in pregnancy & infancy).
C. Other Symptoms
✅ Hair thinning, brittle nails.
✅ Slow heart rate (Bradycardia), low energy levels.
✅ Depression, mood swings.
4. Diagnosis of Iodine Deficiency
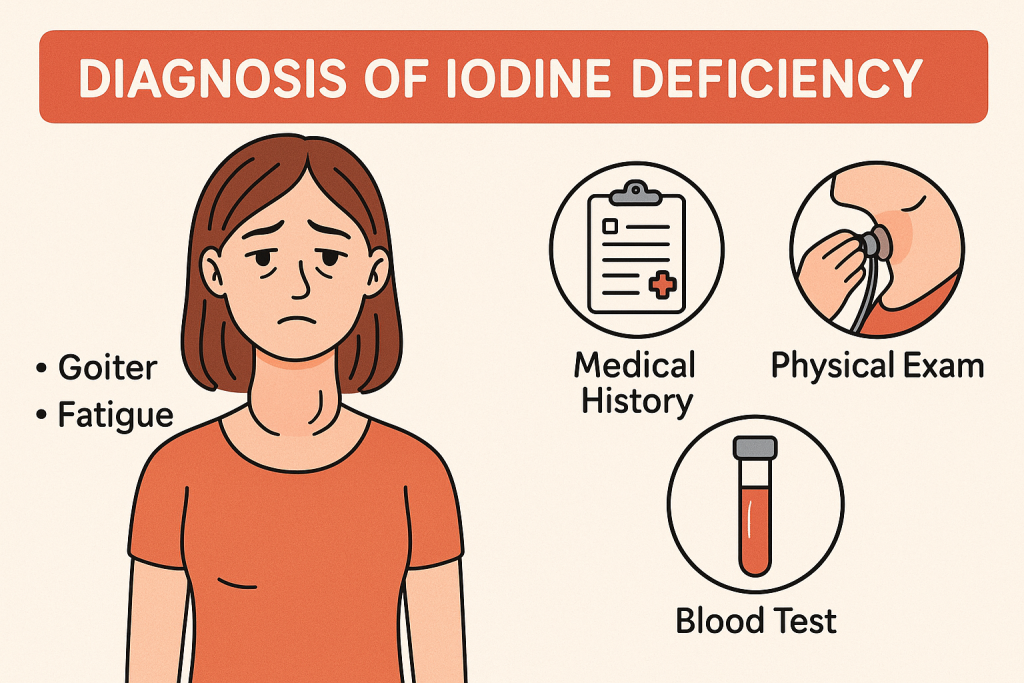
A. Clinical Examination
✅ Assess for goiter, dry skin, weight changes, cold intolerance.
✅ Evaluate dietary history & risk factors.
B. Laboratory Tests
✅ Urinary Iodine Excretion Test:
- <100 µg/L → Iodine deficiency.
- <50 µg/L → Severe deficiency.
✅ Thyroid Function Tests (TFTs):
- Low T3 & T4, high TSH indicates iodine deficiency hypothyroidism.
✅ Thyroid Ultrasound:
- Detects goiter or thyroid nodules.
✅ Blood Thyroglobulin Levels:
- Elevated in iodine-deficient individuals.
5. Management of Iodine Deficiency
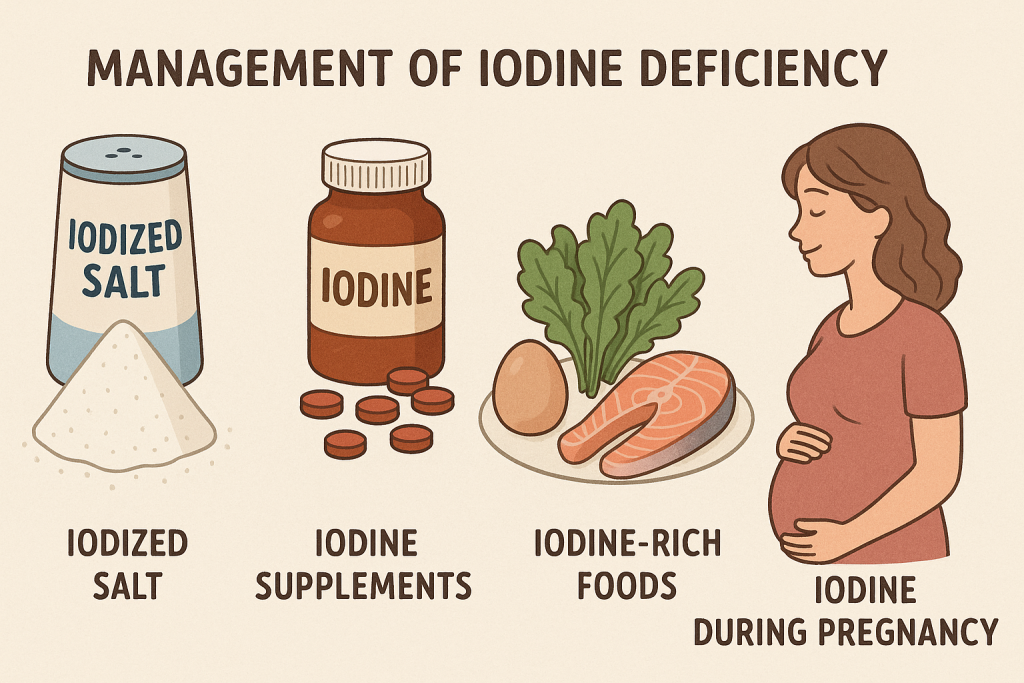
A. Dietary Modification
✅ Increase intake of iodine-rich foods:
- Seafood (fish, shrimp, seaweed, shellfish).
- Dairy products (milk, yogurt, cheese).
- Egg yolks, iodized salt, fortified grains.
✅ Avoid excessive consumption of goitrogens (cabbage, soy, peanuts, cassava).
B. Iodine Supplementation Therapy
✅ For Mild Deficiency:
- Iodized salt (30-50 mg iodine per year).
✅ For Moderate to Severe Deficiency:
- Oral potassium iodide (200-400 µg/day).
- Iodine oil injections in high-risk populations.
✅ For Pregnant & Lactating Women:
- 250 µg/day iodine supplementation.
✅ For Children with Goiter:
- Iodine-fortified food or oral iodine therapy.
C. Thyroid Hormone Therapy (For Severe Cases)
✅ Levothyroxine (T4) therapy for hypothyroidism.
✅ Surgical intervention for large goiters affecting breathing/swallowing.
6. Prevention of Iodine Deficiency

✅ Universal Salt Iodization (USI) – Use iodized salt.
✅ Regular screening in high-risk groups (pregnant women, children).
✅ Fortification of food with iodine (milk, cereals, oil).
✅ Public awareness about iodine-rich diets.
✅ Routine thyroid function tests for early detection.
7. Nurses’ Role in Iodine Deficiency Disorders
A. Preventive Role
✅ Health Education on Iodine-Rich Diets:
- Encourage use of iodized salt in daily cooking.
- Promote seafood, dairy, eggs, and fortified grains.
- Educate on reducing goitrogenic foods in excess.
✅ Prenatal & Infant Nutrition Awareness:
- Ensure pregnant women take iodine supplements to prevent cretinism.
- Promote exclusive breastfeeding for the first 6 months.
✅ Community-Based Screening & Awareness Campaigns:
- Conduct goiter screening in schools & communities.
- Organize iodine education camps in endemic areas.
✅ Universal Salt Iodization Advocacy:
- Support government policies on iodized salt distribution.
- Educate on proper salt storage (iodine evaporates in open containers).
B. Nurses’ Role in Diagnosis & Management
✅ Assess & Monitor Symptoms:
- Goiter, fatigue, weight gain, cognitive decline.
✅ Assist in Thyroid Function Testing:
- Blood sampling for TSH, T3, T4, & urinary iodine tests.
✅ Administer Iodine Supplementation:
- Oral iodine therapy in children & pregnant women.
- Ensure compliance with iodine therapy.
✅ Monitor & Support Thyroid Hormone Therapy:
- Levothyroxine therapy for hypothyroid patients.
- Educate on adherence & regular follow-ups.
✅ Refer Severe Cases:
- Patients with large goiters requiring surgery.
- Infants with congenital iodine deficiency requiring specialist care.
C. Nurses’ Role in Public Health & Government Programs
✅ Implement National Iodine Deficiency Disorders (IDD) Control Programs:
- Promote iodized salt usage in communities.
- Ensure iodine supplementation for pregnant/lactating women.
✅ Community-Based Nutritional Interventions:
- Organize awareness drives in iodine-deficient regions.
- Conduct health camps for thyroid disorder screening.
✅ Advocate for Government Food Fortification Policies:
- Support policies on iodized salt, fortified grains, and dairy.
Calcium Deficiency Disorders.
1. Introduction
Calcium is an essential mineral required for bone health, muscle contraction, nerve function, blood clotting, and enzyme activity. Calcium deficiency (Hypocalcemia) can lead to osteoporosis, rickets, tetany, muscle weakness, and cardiovascular issues.
2. Causes of Calcium Deficiency

Calcium deficiency occurs due to poor dietary intake, impaired absorption, increased demand, or excessive loss.
A. Primary Causes (Dietary Deficiency)
✅ Low intake of calcium-rich foods:
- Lack of milk, cheese, yogurt, leafy greens, fortified cereals.
✅ Lactose intolerance or dairy avoidance: - Leads to calcium deficiency due to limited dairy consumption.
✅ Vegan diets without proper supplementation.
B. Secondary Causes (Increased Demand & Impaired Absorption)
✅ Vitamin D Deficiency:
- Vitamin D is essential for calcium absorption in the intestine.
✅ Hormonal Imbalance: - Low estrogen (postmenopausal women) leads to osteoporosis.
- Low parathyroid hormone (Hypoparathyroidism) reduces calcium regulation.
✅ Pregnancy & Lactation: - Increased calcium requirement for fetal bone growth and milk production.
✅ Gastrointestinal Disorders: - Celiac disease, Crohn’s disease, chronic diarrhea reduce calcium absorption.
✅ Renal Disease: - Chronic Kidney Disease (CKD) causes excessive calcium loss.
✅ Long-Term Medication Use: - Corticosteroids, diuretics, antacids (aluminum-based), anticonvulsants affect calcium balance.
3. Signs & Symptoms of Calcium Deficiency
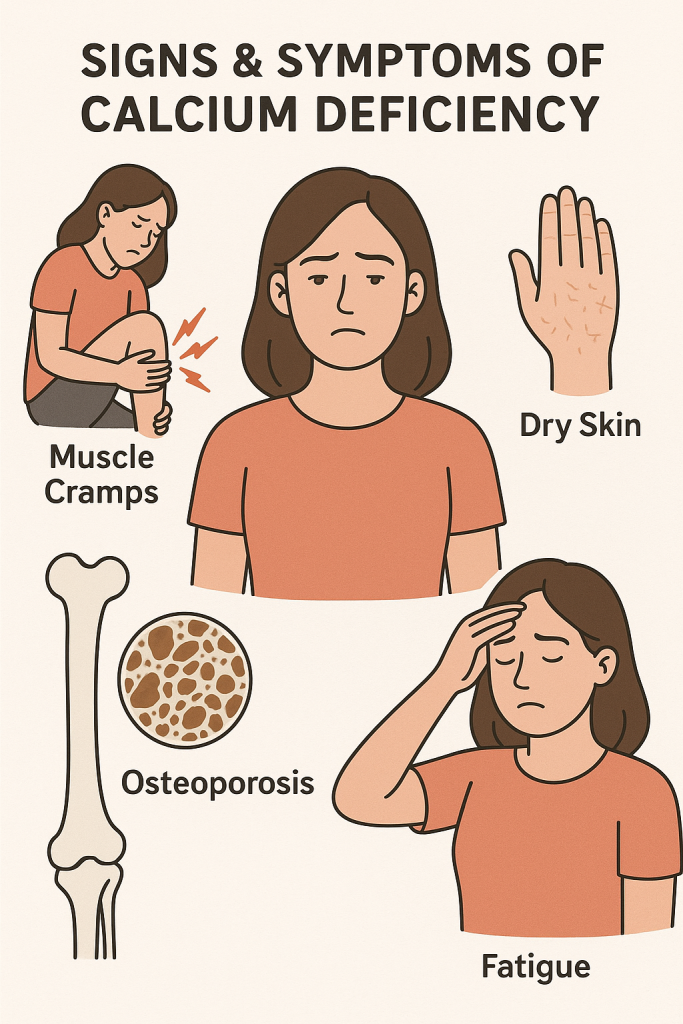
Calcium deficiency affects bones, muscles, nerves, and blood circulation.
A. Neuromuscular Symptoms (Tetany & Muscle Cramps)
✅ Muscle cramps & spasms (Tetany) – involuntary contractions, especially in hands & feet.
✅ Numbness & tingling (Paresthesia) – in fingers, lips, and toes.
✅ Severe cases → Seizures or life-threatening spasms.
B. Bone & Skeletal Issues
✅ Osteoporosis (Brittle Bones in Adults) – increased fracture risk.
✅ Osteopenia (Low Bone Density, Early Stage of Osteoporosis).
✅ Rickets (Children) – soft bones, bowed legs, delayed growth.
✅ Osteomalacia (Adults) – bone pain, weakness, fractures.
C. Cardiovascular & Other Symptoms
✅ Abnormal Heart Rhythms (Arrhythmias) – due to calcium’s role in heart function.
✅ Dry skin, brittle nails, and hair thinning.
✅ Memory problems, confusion, depression (in severe deficiency).
4. Diagnosis of Calcium Deficiency
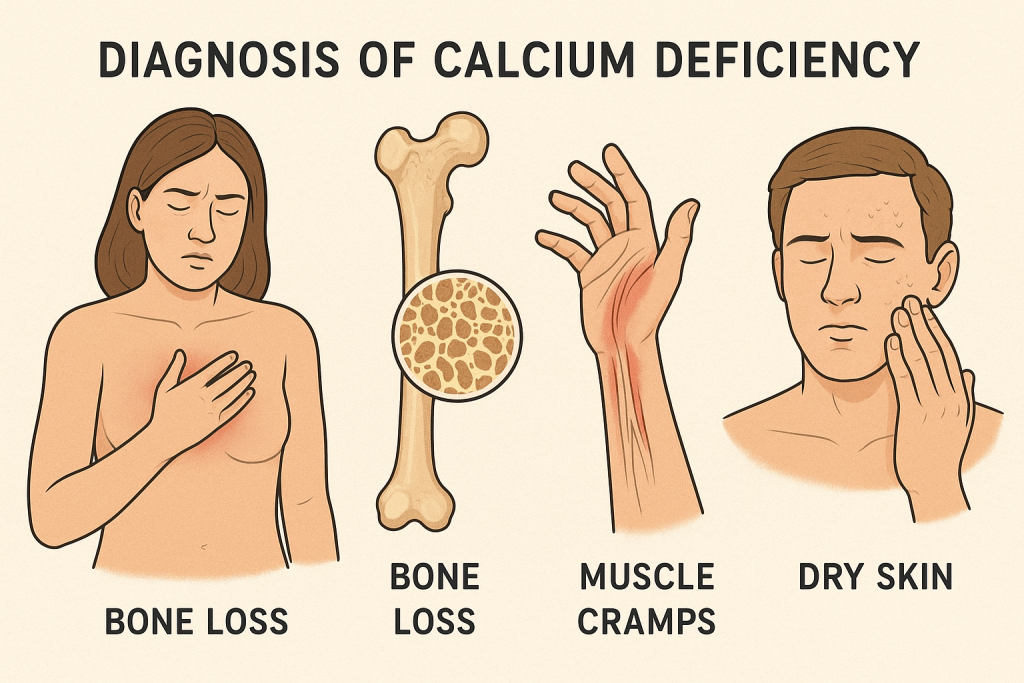
A. Clinical Examination
✅ Assess for muscle cramps, bone pain, numbness, fractures.
✅ Check history of osteoporosis, kidney disease, or malabsorption disorders.
B. Laboratory Tests
✅ Serum Calcium Level:
- Normal: 8.5–10.5 mg/dL.
- Hypocalcemia: <8.5 mg/dL.
- Severe Hypocalcemia: <7 mg/dL (requires urgent treatment).
✅ Serum Ionized Calcium (Biologically Active Calcium):
- More accurate than total calcium measurement.
✅ Parathyroid Hormone (PTH) Test:
- Low PTH → Hypoparathyroidism causing calcium deficiency.
- High PTH → Secondary response to vitamin D deficiency.
✅ Vitamin D Level:
- Deficiency (<20 ng/mL) reduces calcium absorption.
✅ Bone Mineral Density (DEXA Scan):
- Detects osteoporosis or osteopenia in adults.
✅ ECG (Electrocardiogram):
- Prolonged QT interval (seen in severe hypocalcemia).
5. Management of Calcium Deficiency
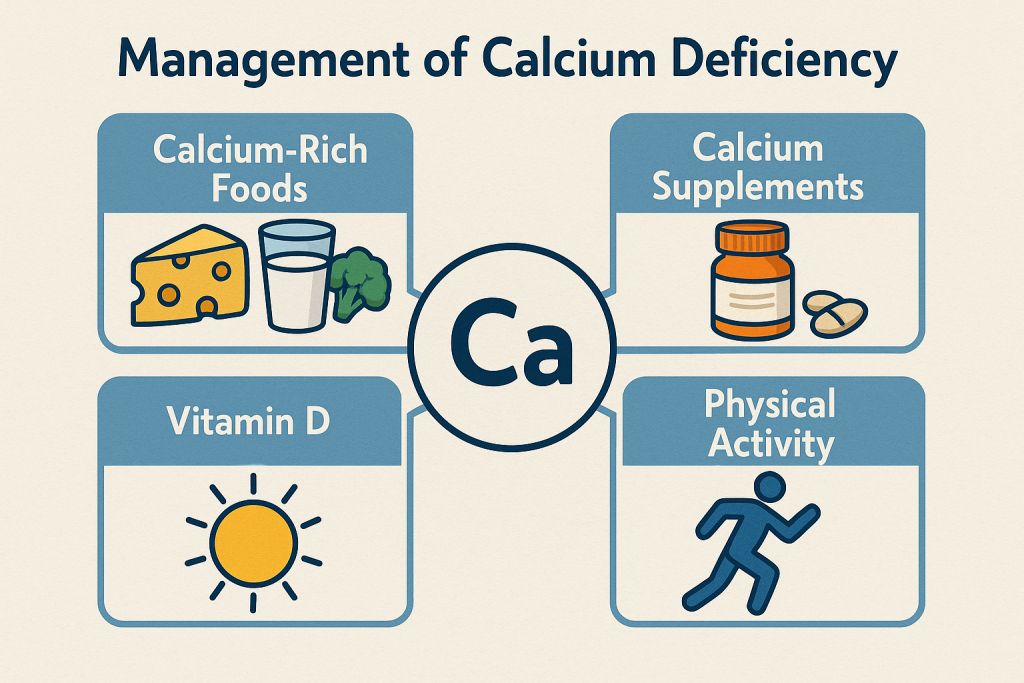
A. Dietary Modification
✅ Increase intake of calcium-rich foods:
- Dairy products: Milk, cheese, yogurt.
- Leafy greens: Kale, broccoli, spinach.
- Nuts & Seeds: Almonds, sesame seeds.
- Fortified foods: Orange juice, cereals, tofu, soy milk.
✅ Reduce factors that inhibit calcium absorption:
- Limit caffeine & alcohol intake (interferes with calcium metabolism).
- Avoid excessive salt (promotes calcium excretion).
B. Calcium Supplementation Therapy
✅ For Mild Deficiency:
- Calcium carbonate or calcium citrate (500–1000 mg/day).
- Best taken with food for better absorption.
✅ For Severe Deficiency (Symptomatic Hypocalcemia):
- IV Calcium Gluconate or Calcium Chloride (1-2 g IV over 10-20 min).
- Continuous calcium infusion if symptoms persist.
✅ For Postmenopausal Osteoporosis:
- 1200 mg/day calcium + 800–1000 IU Vitamin D.
- Bisphosphonates (Alendronate, Risedronate) to prevent fractures.
✅ For Rickets & Osteomalacia:
- High-dose Calcium + Vitamin D therapy.
- Regular weight-bearing exercises for bone strength.
C. Hormone & Other Medical Therapy
✅ Parathyroid Hormone Therapy (If Hypoparathyroidism is Present).
✅ Calcitonin (For Hypercalcemia Prevention in Osteoporosis).
✅ Estrogen Replacement Therapy (For Postmenopausal Women).
6. Prevention of Calcium Deficiency
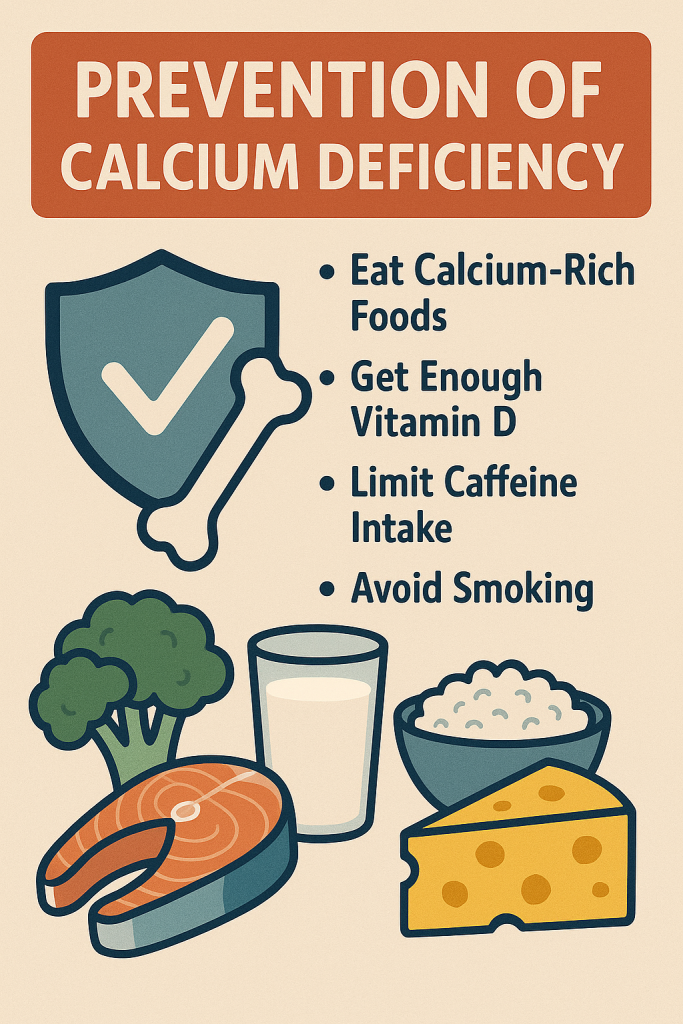
✅ Daily calcium-rich diet & Vitamin D supplementation.
✅ Regular weight-bearing exercise (walking, jogging, resistance training).
✅ Routine screening for osteoporosis in older adults.
✅ Avoid excessive caffeine, alcohol, and smoking.
✅ Ensure proper calcium intake during pregnancy & lactation.
✅ Fortified foods for individuals with dietary restrictions (vegans, lactose intolerant).
7. Nurses’ Role in Calcium Deficiency Disorders
A. Preventive Role
✅ Health Education on Calcium & Bone Health:
- Promote calcium-rich diets & Vitamin D for better absorption.
- Teach importance of sun exposure for natural Vitamin D production.
✅ Prenatal & Postmenopausal Nutritional Awareness:
- Ensure adequate calcium intake during pregnancy & lactation.
- Prevent osteoporosis in postmenopausal women through diet & exercise.
✅ Growth Monitoring & Screening for Osteoporosis:
- Conduct bone density tests for older adults & at-risk individuals.
- Screen children for rickets & provide calcium-rich diet guidance.
✅ Community-Based Nutritional Support:
- Encourage fortified food consumption in vulnerable populations.
- Organize osteoporosis awareness programs for elderly women.
B. Nurses’ Role in Diagnosis & Management
✅ Assess & Monitor Symptoms:
- Muscle cramps, fractures, numbness, bone pain, fatigue.
✅ Administer Calcium Therapy:
- Oral or IV calcium supplements as prescribed.
- Monitor for side effects (hypercalcemia – nausea, kidney stones, constipation).
✅ Supportive Care & Fall Prevention:
- Educate elderly patients on preventing fractures & falls.
- Recommend assistive devices for osteoporosis patients.
✅ Refer Severe Cases:
- Uncontrolled hypocalcemia requiring IV therapy.
- Severe osteoporosis with multiple fractures.
C. Nurses’ Role in Public Health & Government Programs
✅ Implement National Osteoporosis Awareness Programs.
✅ Promote calcium & vitamin D fortification policies.
✅ Organize community exercise & nutrition programs for bone health.
✅ Educate families on calcium intake & fracture prevention.
Nurses’ Role in Mineral Deficiency Diseases.
1. Introduction
Minerals play an essential role in various physiological functions, including bone health, blood formation, muscle function, nerve transmission, and enzyme activity. Deficiencies in minerals such as iron, calcium, iodine, zinc, magnesium, and potassium can lead to severe health issues, including anemia, osteoporosis, thyroid disorders, muscle weakness, and cardiovascular diseases.
Nurses play a crucial role in preventing, diagnosing, managing, and educating individuals about mineral deficiencies to improve public health outcomes.
2. Nurses’ Role in the Prevention of Mineral Deficiency Diseases
A. Health Education & Awareness
✅ Educating Patients on a Balanced Diet:
- Promote mineral-rich foods such as dairy (calcium), seafood (iodine), nuts/seeds (magnesium), leafy greens (iron & zinc), and whole grains (selenium & phosphorus).
- Encourage fortified foods (iron-fortified cereals, iodized salt, calcium-fortified milk).
- Advise on proper cooking techniques to prevent nutrient loss.
✅ Importance of Maternal & Child Nutrition:
- Promote iron & folic acid supplementation during pregnancy to prevent anemia.
- Educate on calcium & Vitamin D intake for fetal bone development.
- Encourage exclusive breastfeeding for 6 months (rich in essential minerals).
✅ Community Education & Public Awareness:
- Conduct workshops in schools, hospitals, and rural areas about mineral-rich diets.
- Distribute nutritional booklets, pamphlets, and posters.
✅ Encouraging Lifestyle Modifications:
- Promote regular physical activity & weight-bearing exercises to strengthen bones and prevent osteoporosis.
- Advise against excessive tea/coffee consumption (reduces iron absorption).
- Encourage reduced salt intake to prevent calcium loss.
B. Nutritional Screening & Growth Monitoring
✅ Growth Monitoring in Children & Adolescents:
- Assess weight, height, and BMI to detect stunted growth due to calcium or zinc deficiency.
- Check for signs of rickets (Vitamin D & calcium deficiency).
✅ Routine Hemoglobin & Iron Screening:
- Screen pregnant women, adolescent girls, and malnourished individuals for anemia.
- Ensure regular deworming to prevent iron loss due to intestinal parasites.
✅ Bone Density Testing & Osteoporosis Screening:
- Conduct DEXA scans in postmenopausal women and elderly at risk for osteoporosis.
- Educate patients on fall prevention and bone-strengthening exercises.
✅ Goiter & Thyroid Function Screening:
- Palpate thyroid gland to detect iodine deficiency-related goiter.
- Conduct TSH, T3, T4 tests in pregnant women and children.
✅ Electrolyte & Blood Tests for Severe Deficiencies:
- Check potassium, magnesium, and sodium levels in patients with muscle weakness, irregular heartbeat, or dehydration.
3. Nurses’ Role in Early Detection & Diagnosis
✅ Identifying Early Signs of Mineral Deficiencies:
- Iron Deficiency Anemia → Fatigue, pale skin, dizziness, shortness of breath.
- Calcium Deficiency → Muscle cramps, brittle bones, osteoporosis.
- Iodine Deficiency → Enlarged thyroid (goiter), slow metabolism, developmental delays.
- Zinc Deficiency → Delayed wound healing, poor immunity, hair loss.
- Magnesium Deficiency → Muscle spasms, irregular heartbeat, irritability.
- Potassium Deficiency → Weakness, irregular heartbeat, fatigue.
✅ Referring for Laboratory Tests:
- CBC test for anemia detection.
- Serum calcium, Vitamin D, and phosphorus levels for bone health assessment.
- Thyroid function tests (TSH, T3, T4) for iodine deficiency disorders.
- Electrolyte panel for potassium, magnesium, and sodium imbalances.
4. Nurses’ Role in the Management of Mineral Deficiency Diseases
A. Dietary & Lifestyle Interventions
✅ Develop Personalized Nutritional Plans:
- Guide patients on iron, calcium, and iodine-rich foods.
- Encourage Vitamin C intake to enhance iron absorption.
- Reduce goitrogenic foods (cabbage, soy, peanuts) in iodine-deficient individuals.
✅ Encouraging Physical Activity & Sunlight Exposure:
- Recommend 30 minutes of daily sunlight for Vitamin D & calcium absorption.
- Promote weight-bearing exercises to strengthen bones.
B. Medical & Supplement Therapy
✅ Administering Mineral Supplements:
- Iron Deficiency → Ferrous sulfate 325 mg/day for 3-6 months.
- Calcium Deficiency → Calcium carbonate or citrate (500–1000 mg/day).
- Iodine Deficiency → Iodized salt, potassium iodide supplements (200-400 µg/day).
- Zinc Deficiency → Zinc sulfate (10-40 mg/day).
- Magnesium Deficiency → Oral magnesium citrate (300-400 mg/day).
- Potassium Deficiency → Oral potassium chloride (20-40 mEq/day).
✅ IV Therapy for Severe Cases:
- IV calcium gluconate for severe hypocalcemia.
- IV iron therapy for chronic anemia or malabsorption.
- Electrolyte correction for severe potassium/magnesium imbalances.
✅ Administering Hormone Therapy (If Needed):
- Thyroid hormone (Levothyroxine) for iodine-related hypothyroidism.
- Estrogen therapy for postmenopausal osteoporosis prevention.
C. Monitoring & Follow-Up Care
✅ Regular Monitoring of At-Risk Patients:
- Pregnant women (Iron, Folic Acid, Calcium, Iodine levels).
- Children at risk for stunting and growth delays.
- Elderly individuals for osteoporosis & electrolyte imbalances.
✅ Prevent Relapse & Ensure Compliance:
- Encourage adherence to mineral supplementation.
- Reinforce dietary modifications & lifestyle changes.
- Educate on potential side effects of supplements (e.g., iron-induced constipation).
✅ Psychosocial & Emotional Support:
- Address food insecurity and socioeconomic barriers to adequate nutrition.
- Provide counseling for patients with chronic deficiencies.
5. Nurses’ Role in Public Health & Government Nutrition Programs
A. Implementation of National Nutrition & Fortification Programs
✅ Integrated Child Development Services (ICDS) – Nutritional support for children & mothers.
✅ Mid-Day Meal Scheme (MDMS) – Fortified meals to prevent malnutrition.
✅ National Nutrition Mission (Poshan Abhiyan) – Awareness campaigns on mineral deficiencies.
✅ Iron & Folic Acid Supplementation (IFAS) Program – Prevention of anemia among adolescents & pregnant women.
✅ Universal Salt Iodization (USI) Program – Ensuring iodine sufficiency in the population.
✅ Calcium & Vitamin D Fortification in Dairy Products – Prevention of osteoporosis.
B. Community-Based Nutritional Interventions
✅ Organizing Growth Monitoring Camps & Health Check-ups.
✅ Ensuring Distribution of Fortified Foods in Rural Areas.
✅ Conducting School & Community-Based Nutritional Education Programs.
✅ Raising Awareness on the Risks & Prevention of Mineral Deficiencies.