BSC SEM 1 UNIT 7 APPLIED NUTRITION AND DIETETICS
UNIT 7 Balanced diet
Balanced Diet

Introduction to a Balanced Diet
A balanced diet is one that provides all the essential nutrients in appropriate amounts to maintain health, growth, and overall well-being. It consists of a combination of macronutrients (carbohydrates, proteins, and fats) and micronutrients (vitamins and minerals) along with adequate water and fiber.
Importance of a Balanced Diet
- Supports Growth & Development – Essential for children, adolescents, and pregnant women.
- Maintains Energy Levels – Provides the required calories for daily activities.
- Boosts Immunity – Helps fight infections and diseases.
- Prevents Malnutrition & Deficiencies – Reduces the risk of anemia, rickets, scurvy, and other conditions.
- Reduces Risk of Chronic Diseases – Lowers the risk of heart disease, diabetes, obesity, and hypertension.
- Enhances Mental Health – Improves cognitive function and reduces stress.
Components of a Balanced Diet
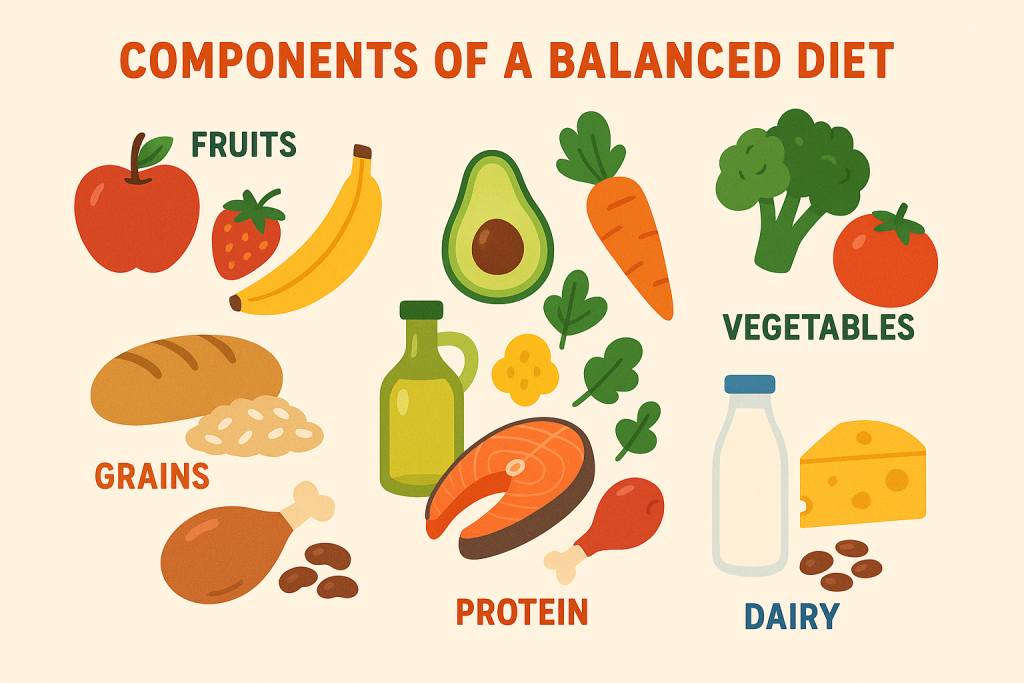
A balanced diet includes different food groups to ensure adequate nutrition.
1. Macronutrients
- Carbohydrates (50-60%): Main source of energy.
- Sources: Rice, wheat, oats, potatoes, fruits.
- Proteins (10-15%): Essential for body repair and growth.
- Sources: Meat, fish, eggs, dairy, legumes, nuts.
- Fats (20-30%): Provides energy and aids in absorption of fat-soluble vitamins.
- Sources: Butter, oils, avocados, nuts, seeds.
2. Micronutrients
- Vitamins:
- Fat-soluble: A, D, E, K (found in dairy, fish, eggs).
- Water-soluble: B-complex, C (found in citrus fruits, vegetables).
- Minerals:
- Calcium (milk, cheese) for bones and teeth.
- Iron (green leafy vegetables, meat) for blood production.
- Zinc, magnesium, potassium for various bodily functions.
3. Water
- Essential for digestion, circulation, and temperature regulation.
- Recommended intake: 2-3 liters/day.
4. Fiber
- Aids digestion and prevents constipation.
- Sources: Whole grains, fruits, vegetables, legumes.
Nutritional Requirements in Nursing
Nurses play a crucial role in ensuring proper nutrition in patients, promoting health, and preventing malnutrition.
1. Nutritional Assessment
- Anthropometric Measurements: Weight, height, BMI, body fat percentage.
- Biochemical Tests: Blood tests for anemia, protein levels.
- Clinical Examination: Skin, hair, nails, tongue (for deficiency signs).
- Dietary History: Food intake analysis.
2. Nutritional Needs in Different Conditions
- Infants & Children: High protein, calcium, iron needs.
- Pregnant & Lactating Women: Increased calories, folic acid, iron, calcium.
- Elderly: Lower calorie needs but high vitamin & mineral intake.
- Patients with Chronic Diseases: Diabetic, renal, cardiac diets as per conditions.
3. Therapeutic Diets in Nursing
- Regular Diet: Well-balanced for general health.
- Soft Diet: For patients with difficulty chewing.
- Liquid Diet: Post-surgical or critically ill patients.
- Diabetic Diet: Low sugar, high fiber.
- Cardiac Diet: Low salt, low cholesterol.
- Renal Diet: Low protein, low potassium.
4. Role of a Nurse in Nutritional Care
- Assessing and identifying nutritional needs.
- Educating patients on healthy eating habits.
- Ensuring compliance with dietary recommendations.
- Administering enteral or parenteral nutrition if required.
- Monitoring weight changes and health improvements.
Principles of a Balanced Diet
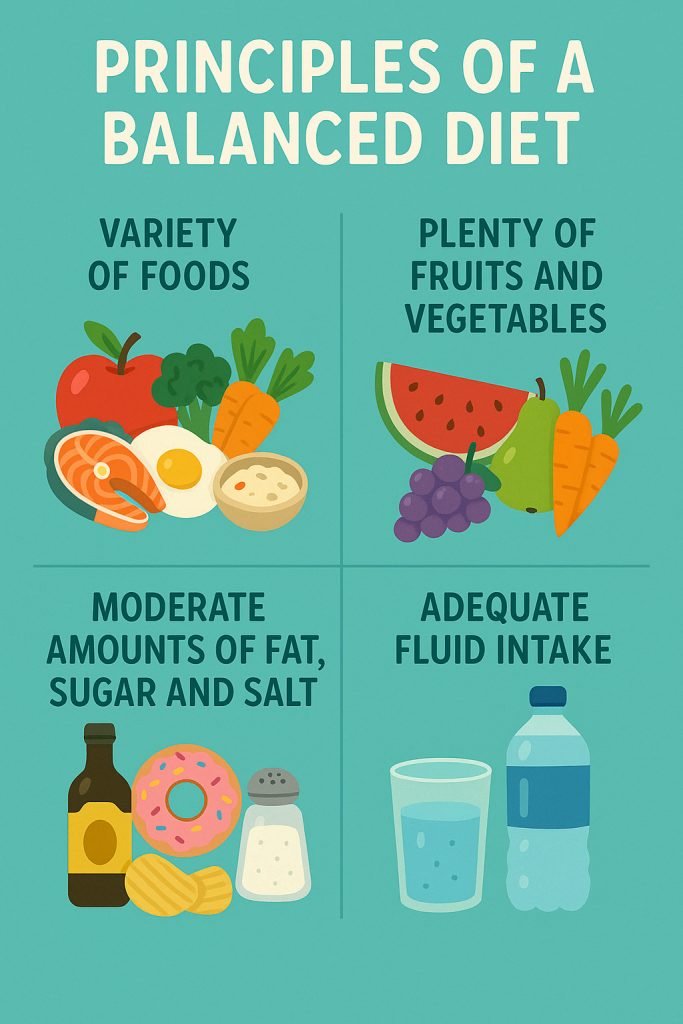
A balanced diet ensures that an individual gets all the essential nutrients in the right proportions to maintain good health, prevent malnutrition, and support overall well-being. The principles of a balanced diet guide the proper selection, proportion, and consumption of food to meet the body’s nutritional requirements.
1. Adequacy
- A diet should provide all essential nutrients such as carbohydrates, proteins, fats, vitamins, minerals, fiber, and water.
- The food intake should meet the body’s daily energy and nutrient requirements.
- Example: A diet rich in protein for growth in children, adequate iron for women to prevent anemia.
2. Proportionality (Balance)
- The intake of macronutrients (carbohydrates, proteins, and fats) and micronutrients (vitamins and minerals) should be in proper proportion.
- No single food contains all essential nutrients, so different food groups should be consumed in balanced quantities.
- Example: Excess carbohydrates may lead to obesity, while insufficient protein may cause muscle loss.
3. Variety
- A balanced diet should include a wide range of foods from different groups to ensure diversity in nutrient intake.
- Eating a variety of foods reduces the risk of nutrient deficiencies and ensures a balanced intake of essential nutrients.
- Example: Including fruits, vegetables, whole grains, dairy, and protein sources in daily meals.
4. Moderation
- Excessive intake of calories, sugar, salt, and fat should be avoided to prevent lifestyle diseases like obesity, diabetes, and hypertension.
- Portion control is essential to prevent overconsumption and maintain a healthy weight.
- Example: Limiting sugary drinks, processed foods, and saturated fats while consuming more natural, whole foods.
5. Nutrient Density
- Foods should be chosen based on their nutrient density, meaning the amount of vitamins and minerals per calorie.
- Nutrient-dense foods provide more health benefits without excessive calories.
- Example: Whole grains, lean meats, dairy, fruits, and vegetables are nutrient-dense compared to processed foods high in empty calories.
6. Energy Balance
- The energy intake (calories consumed) should equal energy expenditure (calories burned) to maintain a healthy weight.
- Overeating leads to weight gain, while undereating results in weight loss and malnutrition.
- Example: Athletes need higher caloric intake, while sedentary individuals should limit calorie intake.
7. Hydration
- Water is a crucial component of a balanced diet as it aids digestion, circulation, temperature regulation, and excretion.
- The recommended intake is 2-3 liters of water per day, but it may vary based on climate, activity level, and health conditions.
- Example: People in hot climates or athletes need more water to stay hydrated.
8. Meal Timing and Distribution
- Eating at regular intervals (breakfast, lunch, dinner, and snacks) maintains metabolism and energy levels.
- Avoid skipping meals, as it leads to overeating in the next meal.
- Example: Having a protein-rich breakfast, a balanced lunch, and a light dinner with healthy snacks in between.
9. Personalization (Age, Gender, and Health Status)
- Dietary requirements vary based on age, gender, health conditions, and activity levels.
- Example:
- Infants & Children: Need more proteins, calcium, and iron for growth.
- Pregnant Women: Require extra calories, folic acid, and iron.
- Elderly: Need more vitamins, minerals, and fiber with reduced calorie intake.
10. Avoiding Processed and Junk Foods
- Processed foods are often high in trans fats, sugar, salt, and artificial additives, leading to health problems.
- Instead, prefer fresh and natural foods for better health benefits.
- Example: Choosing home-cooked meals over fast food to avoid preservatives and unhealthy fats.
Steps to Achieve a Balanced Diet
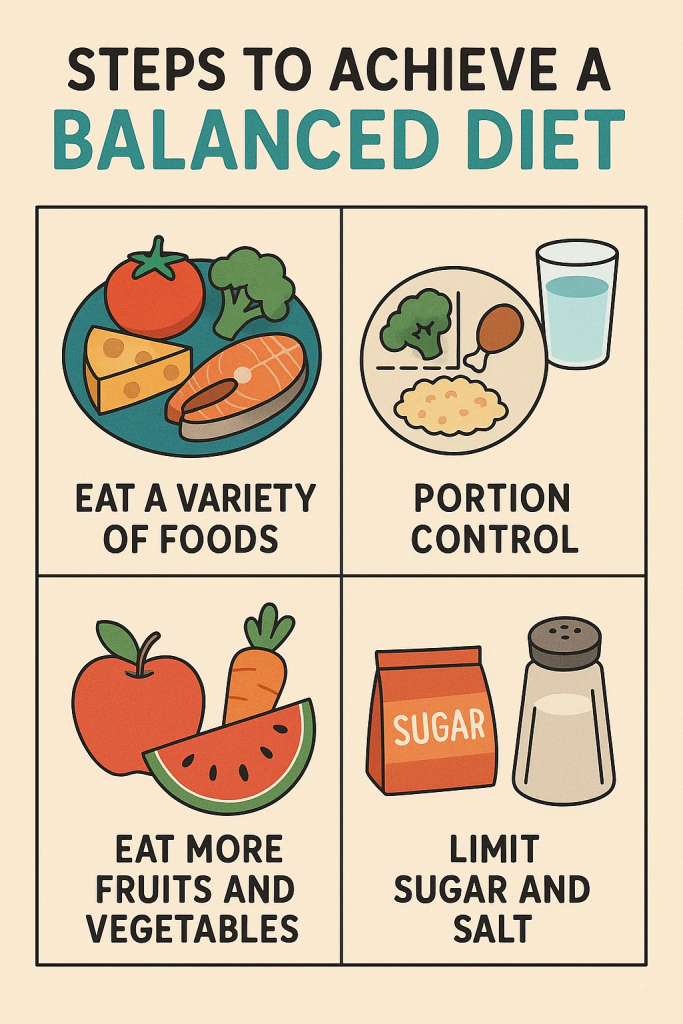
Maintaining a balanced diet requires careful planning, proper food selection, and adherence to nutritional guidelines. The following steps will help individuals achieve and sustain a nutrient-rich, well-balanced diet for optimal health and well-being.
1. Assess Nutritional Needs
- Understand individual caloric and nutrient requirements based on age, gender, activity level, and health conditions.
- Consider dietary needs for growth, pregnancy, lactation, old age, and medical conditions like diabetes or hypertension.
- Example: A pregnant woman needs more iron and folic acid, whereas an athlete requires high-energy foods.
2. Include All Food Groups
- A balanced diet must incorporate macronutrients (carbohydrates, proteins, and fats) and micronutrients (vitamins and minerals) in proper proportions.
- Food groups to include:
- Carbohydrates: Whole grains, rice, oats, potatoes
- Proteins: Lean meats, fish, eggs, legumes, dairy
- Fats: Nuts, seeds, healthy oils, avocado
- Vitamins & Minerals: Fruits, vegetables, dairy
- Fiber & Water: Whole grains, fruits, vegetables, water
- Example: A plate should have a mix of grains, protein, vegetables, and a healthy fat source.
3. Follow Proper Meal Planning
- Plan balanced meals that distribute nutrients evenly throughout the day.
- Meal schedule:
- Breakfast – High protein & fiber-rich foods for sustained energy.
- Lunch – Balanced meal with proteins, carbs, and vitamins.
- Dinner – Light but nutritious, with moderate portions.
- Snacks – Healthy options like nuts, fruits, or yogurt instead of processed snacks.
- Example: A meal plan that includes brown rice, grilled chicken, and steamed vegetables for lunch.
4. Control Portion Sizes
- Eating in moderation prevents excessive calorie intake and weight gain.
- Use small plates and mindful eating techniques to avoid overeating.
- Follow recommended serving sizes for each food group.
- Example: A serving of protein should be the size of a palm, while carbs should fit a fist.
5. Choose Nutrient-Dense Foods Over Empty Calories
- Nutrient-dense foods provide vitamins, minerals, and fiber without excess calories.
- Avoid processed foods, sugary drinks, and deep-fried items that add unhealthy fats and sugars.
- Example: Replace white bread with whole-grain bread and soda with fresh fruit juice.
6. Maintain Proper Hydration
- Water is essential for digestion, circulation, and waste elimination.
- Recommended intake: 2-3 liters per day, or more in hot weather and physical activity.
- Prefer water, coconut water, and herbal teas over sugary drinks.
- Example: Drinking a glass of water before meals aids digestion and prevents overeating.
7. Avoid Excess Salt, Sugar, and Fats
- High salt intake leads to hypertension, while excess sugar contributes to diabetes.
- Prefer natural sweeteners (honey, fruits) over refined sugar.
- Choose healthy fats (olive oil, nuts) instead of trans fats (fried foods, margarine).
- Example: Use herbs and spices for flavor instead of excessive salt.
8. Cook Food Using Healthy Methods
- Cooking methods influence the nutrient content of food.
- Healthiest cooking techniques:
- Steaming, grilling, baking, roasting, boiling
- Avoid deep-frying or overcooking vegetables, which destroys nutrients.
- Example: Grilled fish with steamed vegetables retains more nutrients than deep-fried fish.
9. Balance Energy Intake with Physical Activity
- Calories consumed should match calories burned to prevent obesity or malnutrition.
- Include daily exercise (walking, running, yoga, gym) to maintain a healthy metabolism.
- Example: A sedentary person should reduce calorie intake, while an athlete requires more energy-dense foods.
10. Adapt the Diet to Special Needs
- Consider age, medical conditions, and lifestyle while planning meals.
- Modify the diet for:
- Children – High protein and calcium for growth
- Pregnant women – More folic acid, iron, and fiber
- Elderly – Soft, nutrient-dense, fiber-rich foods
- Chronic illnesses – Low salt for hypertension, low sugar for diabetes
- Example: A diabetic patient should replace white rice with brown rice to control blood sugar levels.
11. Avoid Skipping Meals
- Regular meals regulate metabolism and prevent overeating in the next meal.
- Breakfast is crucial to kick-start metabolism for the day.
- Example: Eating a healthy breakfast with eggs, whole grains, and fruit prevents snacking on unhealthy foods later.
12. Follow a Sustainable & Practical Diet
- A balanced diet should be realistic and adaptable to lifestyle.
- Avoid fad diets that eliminate entire food groups.
- Make small, gradual changes instead of sudden dietary shifts.
- Example: Instead of cutting out all carbs, opt for whole grains over refined ones.
13. Monitor and Adjust the Diet Regularly
- Track weight, energy levels, and overall health to ensure the diet meets nutritional needs.
- Modify food intake based on age, activity, and health conditions.
- Example: A growing child may need increased protein, while an elderly person may need more fiber.
Food Guides – The Basic Four Food Groups
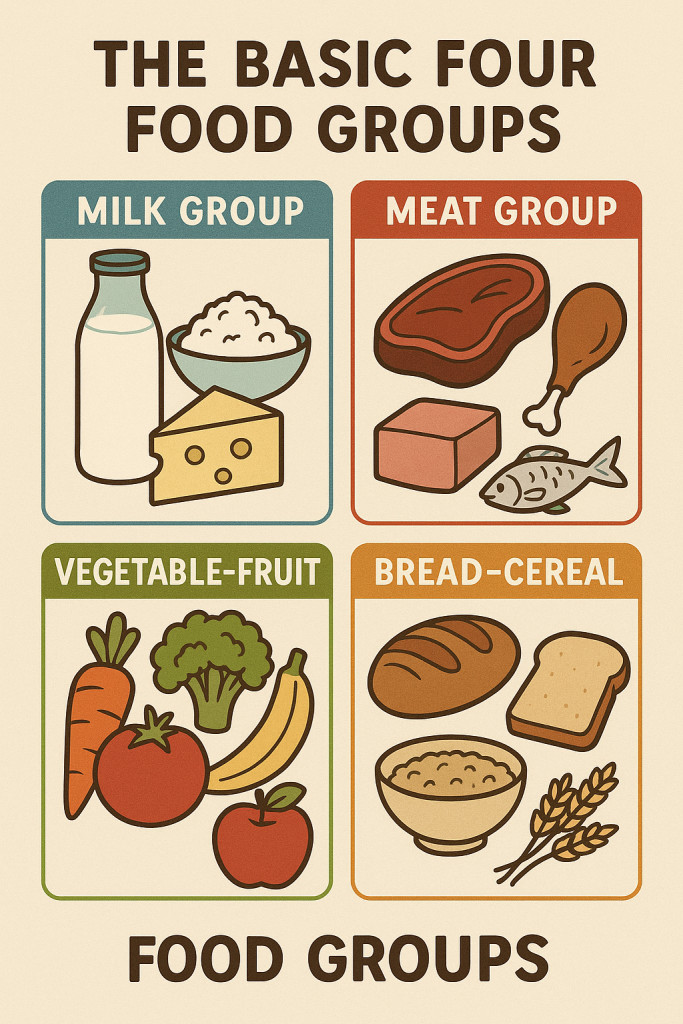
Food guides are used to educate individuals about proper nutrition and ensure they receive a balanced diet by consuming different food groups in appropriate proportions. One of the earliest and most widely recognized food guides is the Basic Four Food Groups, developed by the U.S. Department of Agriculture (USDA) in the 1950s and used until the 1990s.
The Basic Four Food Groups emphasize the consumption of four essential food categories to maintain good health.
1. Milk and Dairy Group (Rich in Calcium & Protein)
- Includes: Milk, cheese, yogurt, buttermilk, paneer.
- Nutrients Provided:
- Calcium (for strong bones and teeth).
- Protein (for growth and tissue repair).
- Vitamin D (for bone health).
- Recommended Servings: 2-3 servings per day.
- Example: A glass of milk in the morning and yogurt with lunch.
2. Meat, Poultry, Fish, Eggs, Nuts, and Legumes Group (Protein-Rich Foods)
- Includes:
- Animal-based proteins: Chicken, fish, eggs, lean beef, pork.
- Plant-based proteins: Lentils, beans, chickpeas, tofu, nuts, and seeds.
- Nutrients Provided:
- Protein (for muscle growth and repair).
- Iron (for red blood cell production).
- Vitamin B12 (for nerve function and DNA production).
- Omega-3 fatty acids (from fish, for brain and heart health).
- Recommended Servings: 2-3 servings per day.
- Example: An egg for breakfast, grilled fish for lunch, and lentils (dal) for dinner.
3. Fruits and Vegetables Group (Vitamins, Minerals & Fiber)
A. Vegetables
- Includes: Leafy greens (spinach, kale), root vegetables (carrots, potatoes), cruciferous vegetables (broccoli, cauliflower), and others.
- Nutrients Provided:
- Vitamins A, C, K (for immunity, skin health, and blood clotting).
- Fiber (for digestion and gut health).
- Antioxidants (for reducing disease risk).
- Recommended Servings: 3-5 servings per day.
- Example: A salad with lunch, cooked greens with dinner.
B. Fruits
- Includes: Apples, bananas, oranges, berries, mangoes, grapes.
- Nutrients Provided:
- Vitamin C (for immune function).
- Potassium (for heart health).
- Natural sugars (for energy).
- Recommended Servings: 2-4 servings per day.
- Example: A banana in the morning and an orange as a snack.
4. Grains and Cereals Group (Energy-Rich Foods)
- Includes: Rice, wheat, oats, barley, corn, bread, pasta.
- Nutrients Provided:
- Carbohydrates (primary energy source).
- Fiber (for digestion and gut health).
- B vitamins (for metabolism and brain function).
- Recommended Servings: 5-8 servings per day.
- Example: Whole wheat toast for breakfast, brown rice for lunch.
Limitations of the Basic Four Food Groups
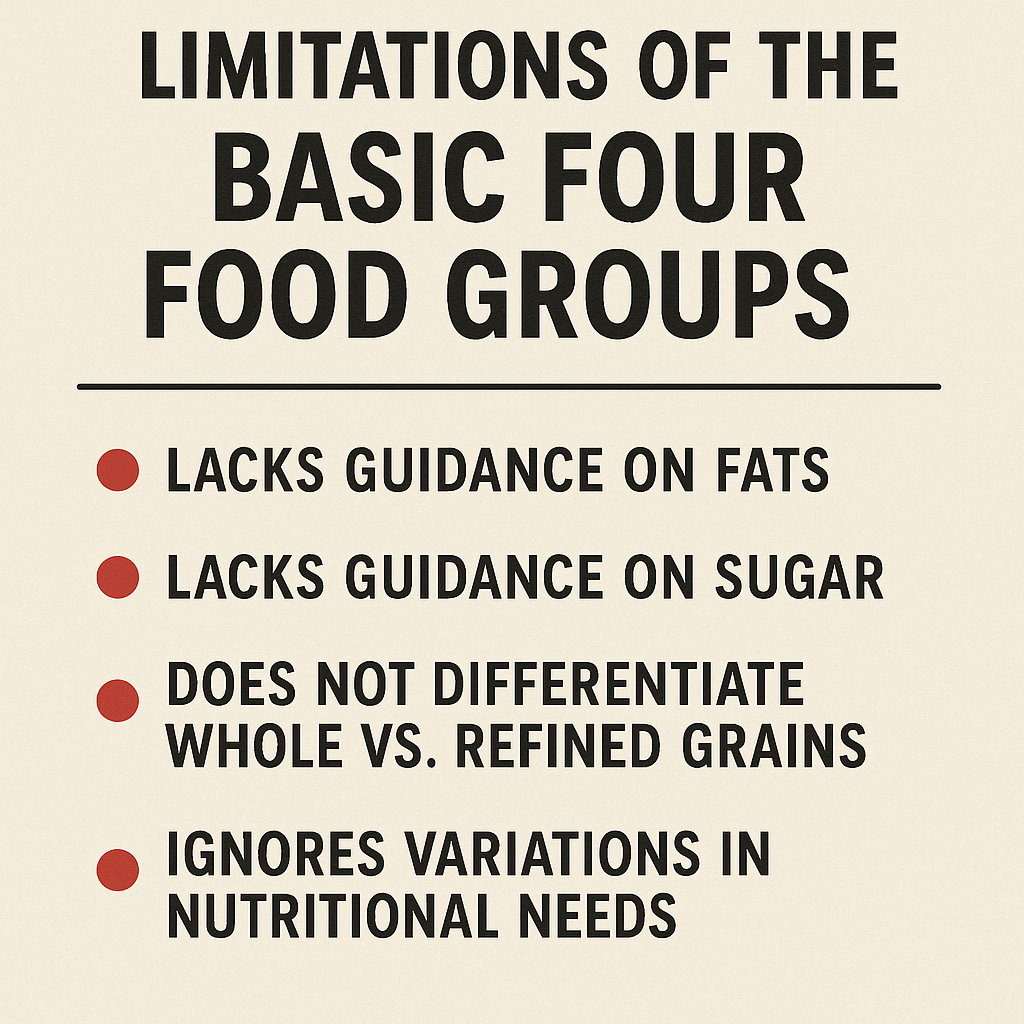
Although this food guide was widely used, it had some limitations, which led to the development of newer models such as the Food Pyramid and MyPlate:
- Did not differentiate between healthy and unhealthy fats.
- Lacked emphasis on fiber-rich foods like whole grains.
- Did not highlight the risks of excessive sugar and processed foods.
- Portion control was not well-defined, leading to overconsumption.
Recommended Dietary Allowance (RDA) – Definition, Limitations, and Uses
Definition of RDA
The Recommended Dietary Allowance (RDA) is the average daily intake level of essential nutrients that is sufficient to meet the dietary needs of nearly 97-98% of healthy individuals in a specific age, gender, and life-stage group. It serves as a guideline for planning and assessing adequate nutrient intake.
- Developed by: The Food and Nutrition Board of the National Academy of Sciences, USA.
- Based on: Scientific research on human nutrition and metabolism.
- Expressed as: Daily recommended intake of macronutrients (carbohydrates, proteins, fats), micronutrients (vitamins, minerals), and water.
Example of RDA Values (for Adults)
| Nutrient | RDA for Men | RDA for Women |
|---|---|---|
| Protein | 56g | 46g |
| Calcium | 1000mg | 1000mg |
| Iron | 8mg | 18mg |
| Vitamin C | 90mg | 75mg |
| Energy (Calories) | 2500 kcal | 2000 kcal |
Limitations of RDA
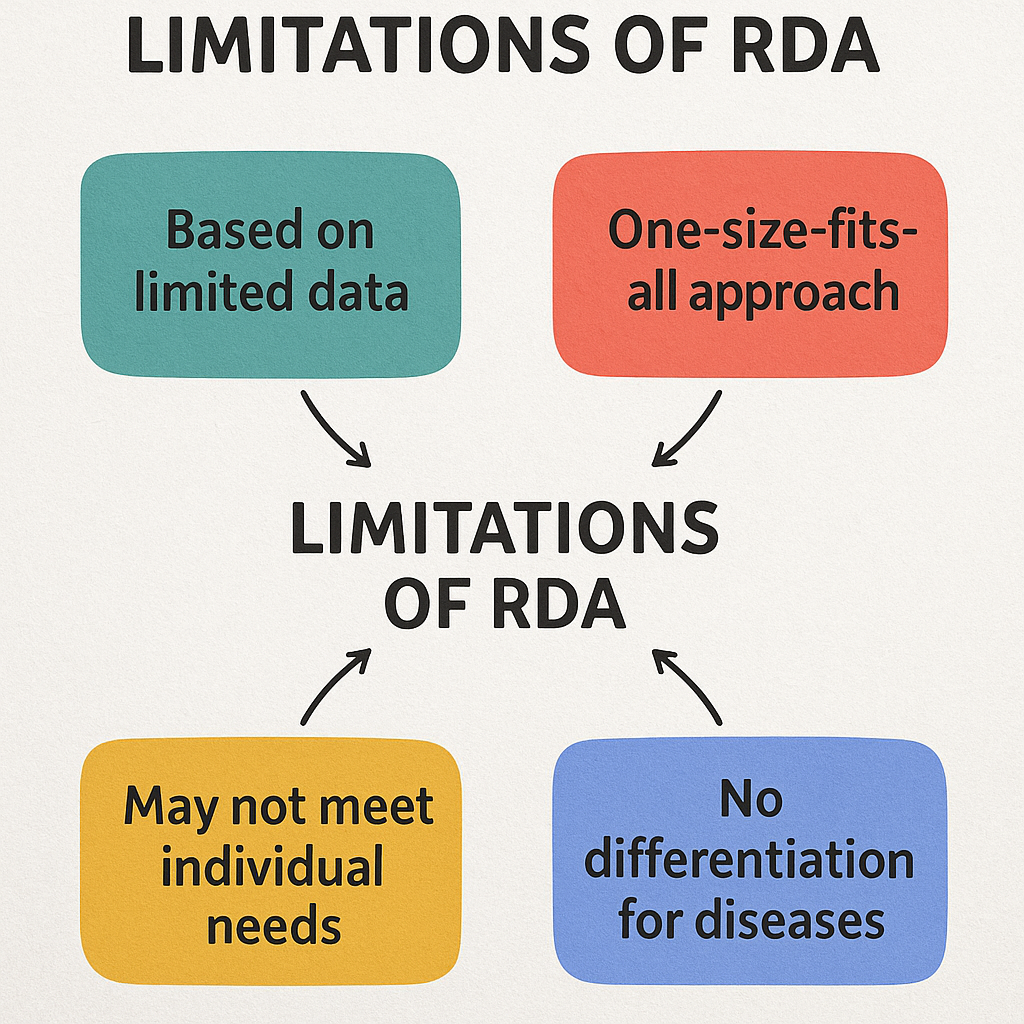
Although RDA is widely used, it has several limitations:
1. Based on Healthy Individuals Only
- RDA is meant for healthy individuals and does not apply to people with chronic diseases, metabolic disorders, or special medical conditions.
- Example: People with diabetes or kidney disease may have different nutritional needs.
2. Does Not Consider Lifestyle Factors
- RDA does not account for individual variations in physical activity levels, stress, environmental factors, and genetic predispositions.
- Example: Athletes require higher protein and energy intake, but RDA does not specify adjustments.
3. Generalized Nutrient Recommendations
- RDA provides a single value for each nutrient, rather than a range that allows flexibility based on individual needs.
- Example: Some people might need more iron or calcium due to physiological conditions like pregnancy or heavy menstrual cycles.
4. Does Not Address Nutrient Interactions
- Nutrients do not function in isolation; they interact with each other in the body.
- Example: Calcium absorption is affected by Vitamin D levels, but RDA does not consider such interactions.
5. Ignores Food Quality and Bioavailability
- RDA lists the amount of nutrients required, but it does not specify the best food sources or bioavailability (how well the body absorbs the nutrient).
- Example: Iron from plant sources (non-heme iron) is less bioavailable than iron from meat (heme iron).
6. Limited Guidance on Micronutrient Toxicity
- While RDA gives minimum required levels, it does not always specify the maximum safe limit (Tolerable Upper Intake Level – UL) for some nutrients.
- Example: Excess Vitamin A can be toxic, but RDA does not provide warnings.
Uses of RDA
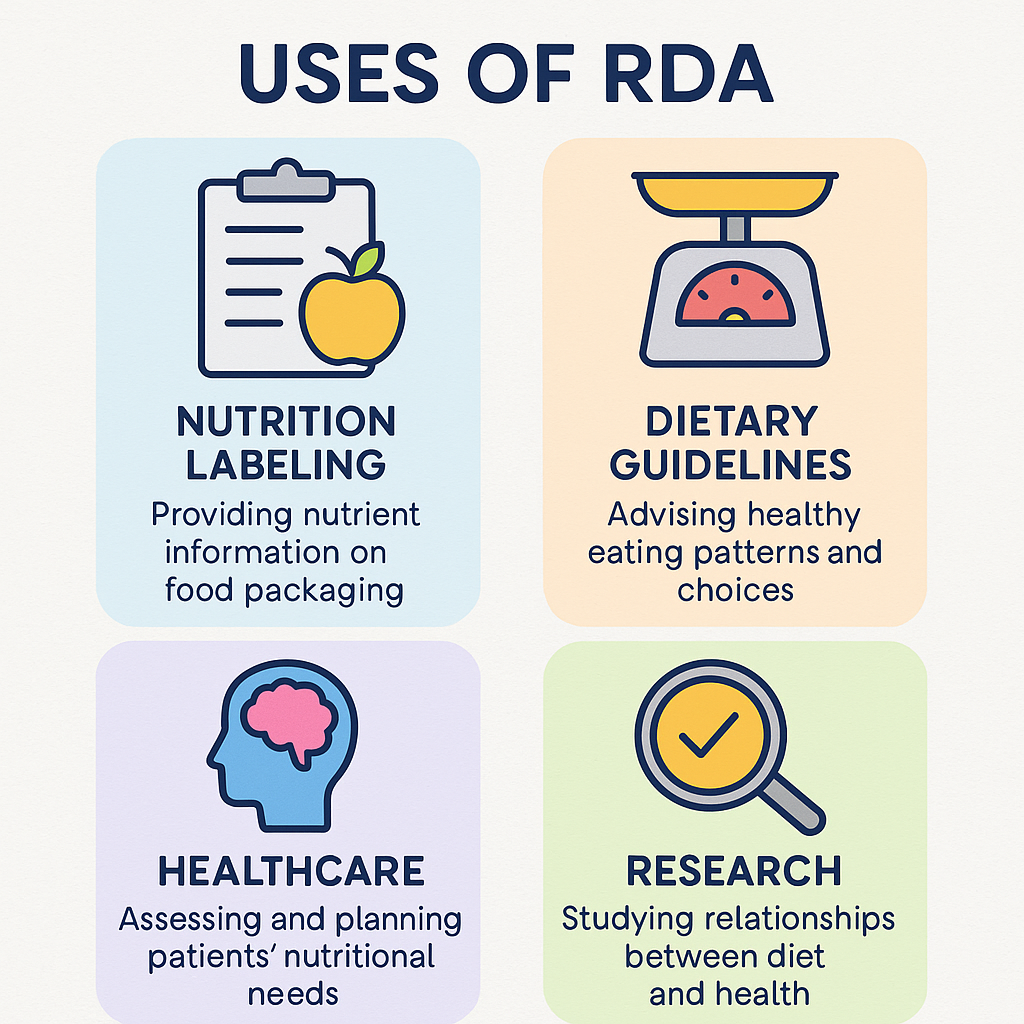
Despite its limitations, RDA is widely used in various health, nutrition, and policy-making applications.
1. Meal Planning and Dietary Guidelines
- Used by dietitians, nutritionists, and healthcare professionals to design balanced diets for individuals and communities.
- Example: Planning school meal programs to ensure children meet their daily nutrient needs.
2. Nutritional Labeling and Food Fortification
- Food manufacturers use RDA values to fortify foods with essential nutrients and display nutritional information on labels.
- Example: Fortified cereals with iron and folic acid to prevent anemia.
3. Public Health and Policy Development
- Governments and health organizations use RDA data to develop national dietary guidelines and nutrition policies.
- Example: The Indian Council of Medical Research (ICMR) sets RDA values for Indians based on their dietary habits.
4. Clinical and Hospital Nutrition Management
- Hospitals use RDA to plan therapeutic diets for patients recovering from illness, surgery, or malnutrition.
- Example: High-protein diets for post-surgical patients to promote healing.
5. Preventing Deficiency Diseases
- Helps identify and prevent nutritional deficiencies such as rickets (Vitamin D deficiency), anemia (Iron deficiency), and scurvy (Vitamin C deficiency).
- Example: Encouraging pregnant women to take iron and folic acid supplements to prevent neural tube defects in babies.
6. Research and Scientific Studies
- Used in nutrition and biomedical research to study diet-disease relationships and recommend dietary interventions.
- Example: Studies on the role of Omega-3 fatty acids in heart health.
Food Exchange System
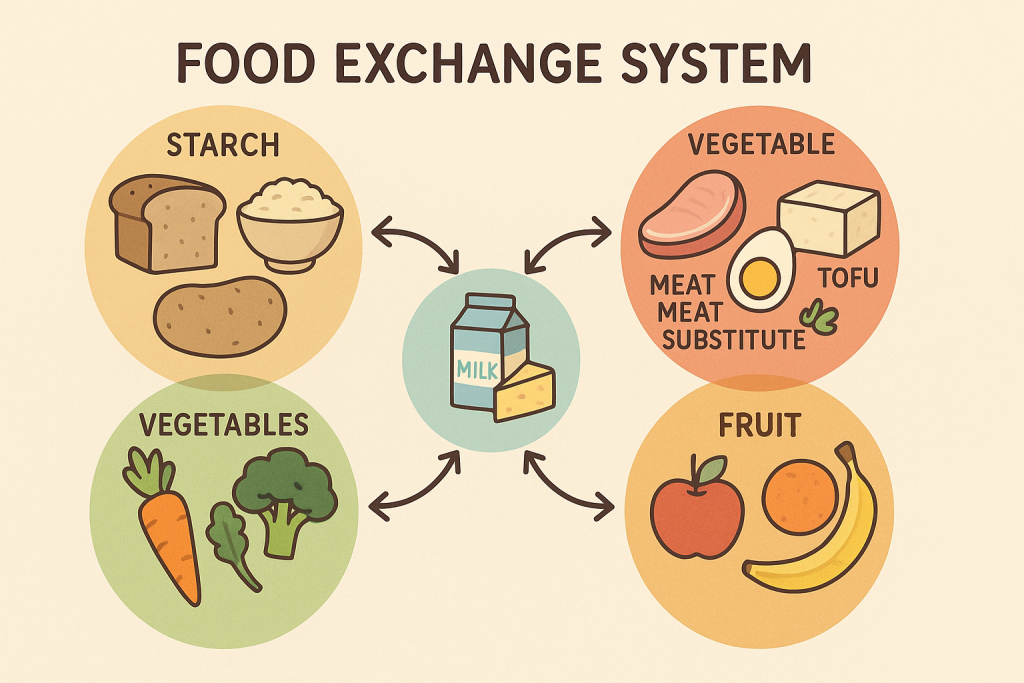
The Food Exchange System is a meal planning method that groups foods with similar nutrient content, calorie values, and portion sizes to help individuals manage their diet, weight, and medical conditions (such as diabetes). This system allows interchangeable food choices within each group while maintaining balanced nutrition.
Definition of Food Exchange System
The Food Exchange System is a method of categorizing foods into different groups based on their carbohydrate, protein, fat, and calorie content. It enables individuals to substitute one food for another of equal nutritional value while maintaining dietary balance.
- Developed by American Dietetic Association (ADA) in collaboration with the American Diabetes Association (ADA).
- Commonly used for diabetes management, weight control, and therapeutic diets.
- Helps in meal planning while ensuring variety and flexibility.
Food Groups in the Exchange System
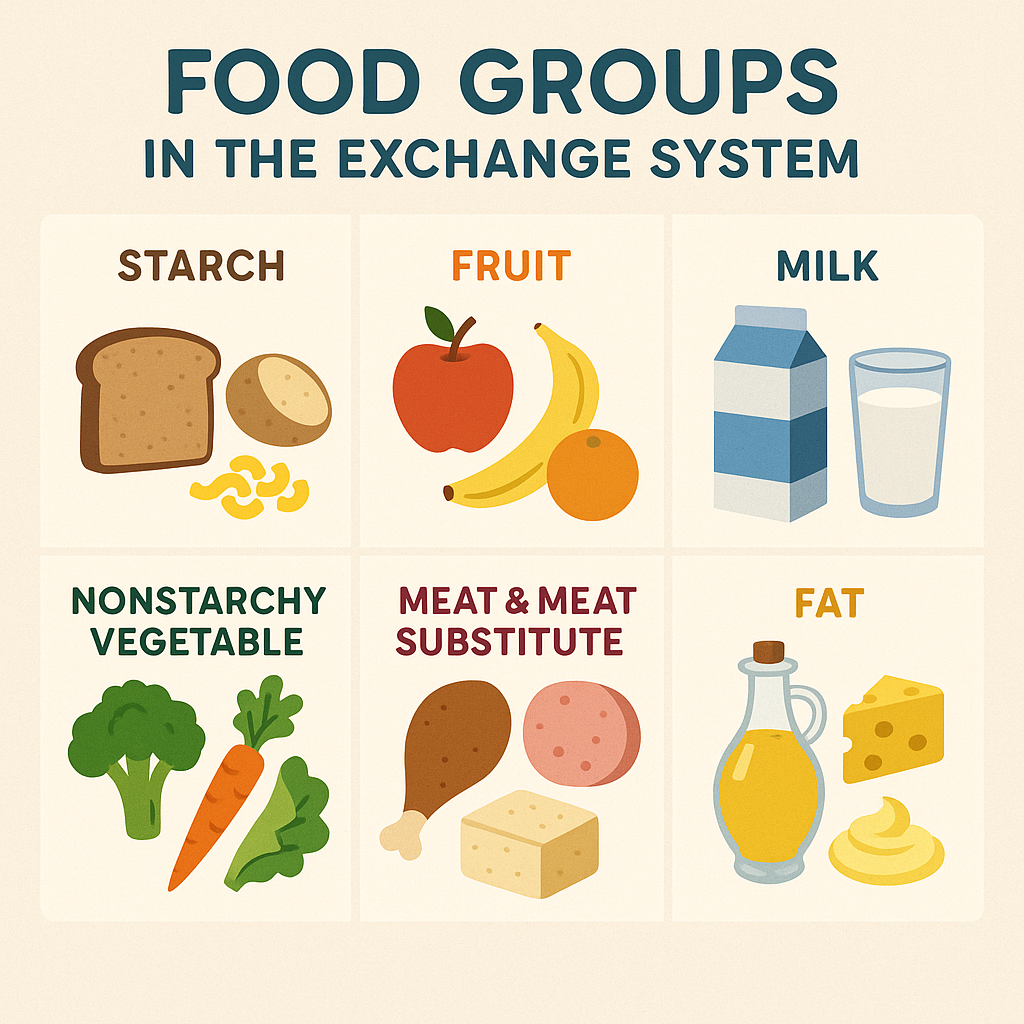
The Food Exchange System categorizes foods into six main groups, with each group having specific portion sizes that provide nearly the same amount of calories, carbohydrates, proteins, and fats.
| Food Group | Carbohydrates (g) | Protein (g) | Fat (g) | Calories |
|---|---|---|---|---|
| 1. Starches (Cereals, Grains, and Breads) | 15 | 3 | 0-1 | 80 kcal |
| 2. Fruits | 15 | 0 | 0 | 60 kcal |
| 3. Vegetables | 5 | 2 | 0 | 25 kcal |
| 4. Milk & Dairy | 12 | 8 | 0-8 | 90-150 kcal |
| 5. Protein (Meat & Meat Substitutes) | 0 | 7 | 2-8 | 45-100 kcal |
| 6. Fats & Oils | 0 | 0 | 5 | 45 kcal |
1. Starch (Carbohydrate) Exchange Group
- Includes: Rice, wheat, bread, pasta, oats, corn, potatoes, chapati.
- Nutritional Value (per exchange):
- Carbohydrates: 15g
- Protein: 3g
- Fat: 0-1g
- Calories: 80 kcal
- Examples:
- 1 slice of bread (30g)
- ½ cup cooked rice or pasta (100g)
- 1 small chapati
2. Fruit Exchange Group
- Includes: Apples, bananas, oranges, mangoes, grapes, pears.
- Nutritional Value (per exchange):
- Carbohydrates: 15g
- Protein: 0g
- Fat: 0g
- Calories: 60 kcal
- Examples:
- 1 small apple (150g)
- ½ medium banana
- ¾ cup orange juice
3. Vegetable Exchange Group
- Includes: Spinach, cabbage, carrots, cucumbers, tomatoes.
- Nutritional Value (per exchange):
- Carbohydrates: 5g
- Protein: 2g
- Fat: 0g
- Calories: 25 kcal
- Examples:
- ½ cup cooked vegetables
- 1 cup raw leafy greens
- ½ cup tomato juice
4. Milk and Dairy Exchange Group
- Includes: Milk, yogurt, cheese, buttermilk.
- Nutritional Value (per exchange):
- Carbohydrates: 12g
- Protein: 8g
- Fat: 0-8g (varies by type)
- Calories: 90-150 kcal
- Examples:
- 1 cup skim milk (90 kcal)
- 1 cup whole milk (150 kcal)
- 1 cup yogurt
5. Protein (Meat & Meat Substitutes) Exchange Group
- Includes: Chicken, fish, eggs, tofu, beans, nuts.
- Nutritional Value (per exchange):
- Carbohydrates: 0g
- Protein: 7g
- Fat: 2-8g (varies by type)
- Calories: 45-100 kcal
- Examples:
- 1 boiled egg (75 kcal)
- 1 oz (30g) chicken or fish
- ½ cup cooked lentils
6. Fats & Oils Exchange Group
- Includes: Butter, oil, nuts, seeds, ghee.
- Nutritional Value (per exchange):
- Carbohydrates: 0g
- Protein: 0g
- Fat: 5g
- Calories: 45 kcal
- Examples:
- 1 tsp butter or oil
- 1 tbsp peanut butter
- 6 almonds
Uses of the Food Exchange System
1. Meal Planning for Diabetics
- Helps individuals with diabetes maintain stable blood sugar levels by ensuring controlled carbohydrate intake.
- Example: A diabetic patient can replace 1 slice of bread with ½ cup rice while keeping the same carbohydrate intake.
2. Weight Management
- Helps in calorie-controlled diets for weight loss or gain.
- Example: A weight-loss diet may limit starch exchanges while increasing protein intake.
3. Therapeutic Diets
- Used in hospitals for diet planning in medical conditions like hypertension, kidney disease, and heart disease.
- Example: A kidney disease patient can exchange high-protein foods (meat) for low-protein alternatives (tofu).
4. Ensures Nutrient Balance
- Prevents nutrient deficiencies by ensuring that meals contain all food groups in the right proportions.
- Example: A vegetarian diet using lentils as a protein exchange ensures adequate protein intake.
5. Flexibility in Diet Choices
- Allows people to swap similar food items without affecting total nutrient intake.
- Example: If someone does not eat fish, they can replace it with chicken or paneer.
Limitations of the Food Exchange System
1. Does Not Address Nutrient Bioavailability
- It does not consider how well the body absorbs nutrients from different foods.
- Example: Iron from meat is absorbed better than from vegetables.
2. Not Personalized
- The system is generalized and may not meet individual metabolic needs.
- Example: A physically active person may need higher protein intake than what is recommended.
3. May Be Complex for Some Individuals
- Requires calculation and portion control, which can be difficult for elderly or uneducated individuals.
- Example: People unfamiliar with food weights may struggle to follow portion sizes.
4. Does Not Address Food Quality
- It groups foods based on macronutrient content, but does not differentiate between healthy and unhealthy sources.
- Example: A person can exchange healthy whole grains for refined white bread, which lacks fiber.
Calculation of Nutritive Value of Foods –
Calculating the nutritive value of foods involves determining the energy (calories), macronutrients (carbohydrates, proteins, and fats), micronutrients (vitamins and minerals), and fiber present in a given quantity of food. This process helps in diet planning, nutrition research, and food labeling.
Steps to Calculate Nutritive Value of Foods
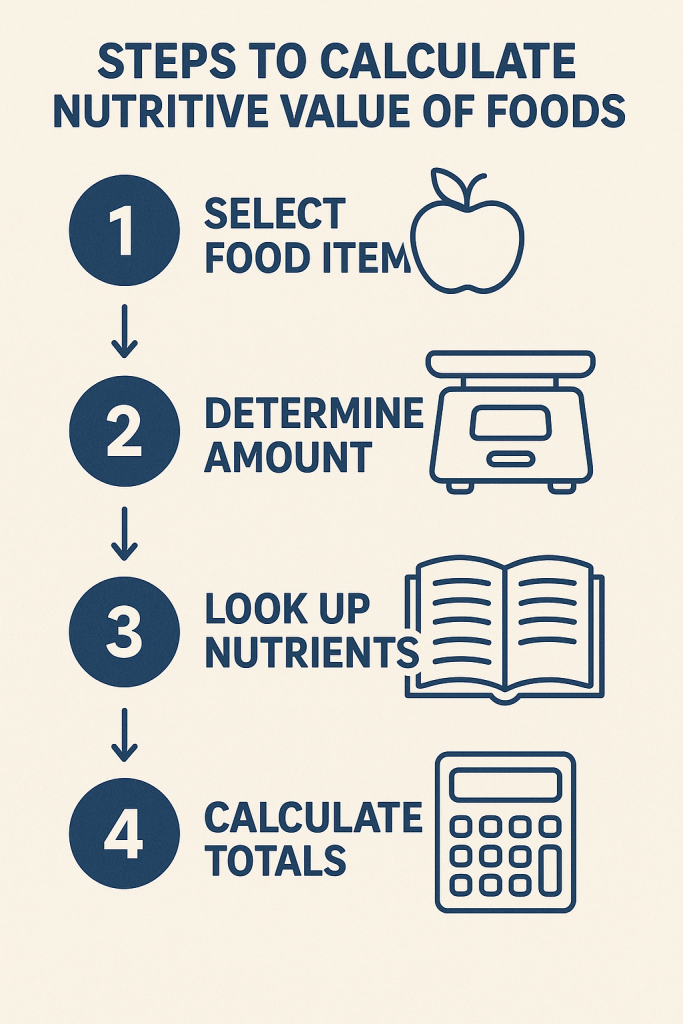
1. Identify the Food Item and Its Quantity
- Select the food item and decide on the quantity to be analyzed.
- Example: 100g of cooked rice or 1 medium-sized apple.
2. Obtain Standard Nutrient Composition Data
- Refer to food composition tables or databases to get the nutrient content per 100g of food.
- Reliable sources include:
- Indian Food Composition Tables (IFCT) by National Institute of Nutrition (NIN), India
- USDA Food Database
- FAO Food Composition Databases
- Nutritive Value of Indian Foods (NIN)
Example: Standard Nutrient Composition of 100g Cooked Rice
| Nutrient | Amount per 100g |
|---|---|
| Energy | 130 kcal |
| Carbohydrates | 28.7g |
| Proteins | 2.4g |
| Fats | 0.3g |
| Fiber | 0.4g |
| Calcium | 10 mg |
| Iron | 0.2 mg |
| Vitamin C | 0 mg |
3. Adjust for Actual Consumption
- If the actual quantity is more or less than 100g, adjust the values accordingly using the ratio method.
Example: If a person consumes 150g of cooked rice
- Energy = (130×150)÷100=195(130 \times 150) \div 100 = 195(130×150)÷100=195 kcal
- Carbohydrates = (28.7×150)÷100=43.05(28.7 \times 150) \div 100 = 43.05(28.7×150)÷100=43.05 g
- Proteins = (2.4×150)÷100=3.6(2.4 \times 150) \div 100 = 3.6(2.4×150)÷100=3.6 g
- Fats = (0.3×150)÷100=0.45(0.3 \times 150) \div 100 = 0.45(0.3×150)÷100=0.45 g
4. Calculate Total Energy Contribution
The total energy of a food is calculated based on the macronutrient composition using Atwater factors:
| Macronutrient | Calories per Gram |
|---|---|
| Carbohydrates | 4 kcal |
| Proteins | 4 kcal |
| Fats | 9 kcal |
Example: Energy Calculation for 150g Cooked Rice
- Carbohydrate energy = 43.05×4=172.243.05 \times 4 = 172.243.05×4=172.2 kcal
- Protein energy = 3.6×4=14.43.6 \times 4 = 14.43.6×4=14.4 kcal
- Fat energy = 0.45×9=4.050.45 \times 9 = 4.050.45×9=4.05 kcal
- Total Energy = 172.2 + 14.4 + 4.05 = 190.65 kcal
5. Consider Cooking Losses and Bioavailability
- Cooking and processing can reduce nutrient content. For example:
- Vitamin C degrades with heat.
- Protein quality may improve with cooking (e.g., dal).
- Water-soluble vitamins may be lost during boiling.
- Some foods have low bioavailability, meaning the body does not absorb all the nutrients.
- Iron from plant sources is absorbed less efficiently than iron from animal sources.
- Calcium absorption is affected by oxalates and phytates.
Adjustments for Cooking Losses
| Nutrient Loss During Cooking | Percentage Loss (%) |
|---|---|
| Vitamin C | 30-50% |
| Folic Acid | 40-70% |
| Iron | 10-15% |
| Protein | 5-10% |
6. Summarize the Nutritive Value Per Meal or Per Day
Once the nutrient values of different foods are calculated, sum them to obtain the total daily intake. This is essential in:
- Dietary planning for different age groups.
- Therapeutic diets for medical conditions (e.g., diabetes, heart disease).
- Food labeling for packaged foods.
Example: Nutritive Value of a Full Meal (Rice, Dal, Vegetables, and Yogurt)
| Food Item (150g each) | Energy (kcal) | Carbs (g) | Protein (g) | Fat (g) |
|---|---|---|---|---|
| Rice | 195 | 43.05 | 3.6 | 0.45 |
| Dal (Lentils) | 200 | 30 | 14 | 2 |
| Cooked Vegetables | 50 | 10 | 2 | 0.5 |
| Yogurt | 100 | 4 | 5 | 3 |
| Total Per Meal | 545 kcal | 87.05 g | 24.6 g | 5.95 g |
7. Compare with RDA (Recommended Dietary Allowance)
The calculated values can be compared with RDA guidelines to determine if the meal meets daily nutritional requirements.
Example: Comparing a Meal’s Nutrient Intake with RDA for an Adult Male
| Nutrient | Meal Value (kcal/g) | RDA for Adult Male | % RDA Met |
|---|---|---|---|
| Energy | 545 kcal | 2500 kcal | 21.8% |
| Carbohydrates | 87.05g | 300g | 29% |
| Protein | 24.6g | 56g | 44% |
| Fat | 5.95g | 70g | 8.5% |
This table shows that this one meal meets 44% of daily protein requirements but only 8.5% of the daily fat intake, suggesting that healthy fats should be included in the next meal.
Uses of Nutritive Value Calculation

1. Meal Planning for Individuals & Communities
- Helps individuals, dietitians, and public health planners design balanced diets.
- Used in hospitals, schools, military food services, and elderly care homes.
2. Food Labeling & Fortification
- Used by food manufacturers to display nutritional information on packaged foods.
- Helps in fortifying foods with essential nutrients to prevent deficiencies (e.g., iodine in salt, Vitamin D in milk).
3. Therapeutic and Clinical Nutrition
- Used in specialized diets (e.g., high-protein diets for malnourished patients, low-sodium diets for hypertensive patients).
- Helps monitor macronutrient intake in chronic diseases.
4. Research and Nutritional Policy Development
- Used by government agencies and research institutions to set dietary guidelines.
- Example: Indian Council of Medical Research (ICMR) uses it to create National Nutrition Policies.
5. Evaluating Food Quality
- Helps in comparing processed vs. natural foods to make healthier choices.
- Example: 100g of whole wheat bread vs. 100g of white bread – whole wheat bread has more fiber and nutrients.
Dietary Fibre
Definition of Dietary Fibre
Dietary fibre refers to the indigestible part of plant-based foods that passes through the digestive system without being broken down or absorbed. It plays a crucial role in maintaining digestive health, regulating blood sugar levels, and preventing chronic diseases.
- Also known as roughage or bulk.
- Found in fruits, vegetables, whole grains, nuts, seeds, and legumes.
- Not digested by human digestive enzymes but fermented by gut bacteria.
Types of Dietary Fibre
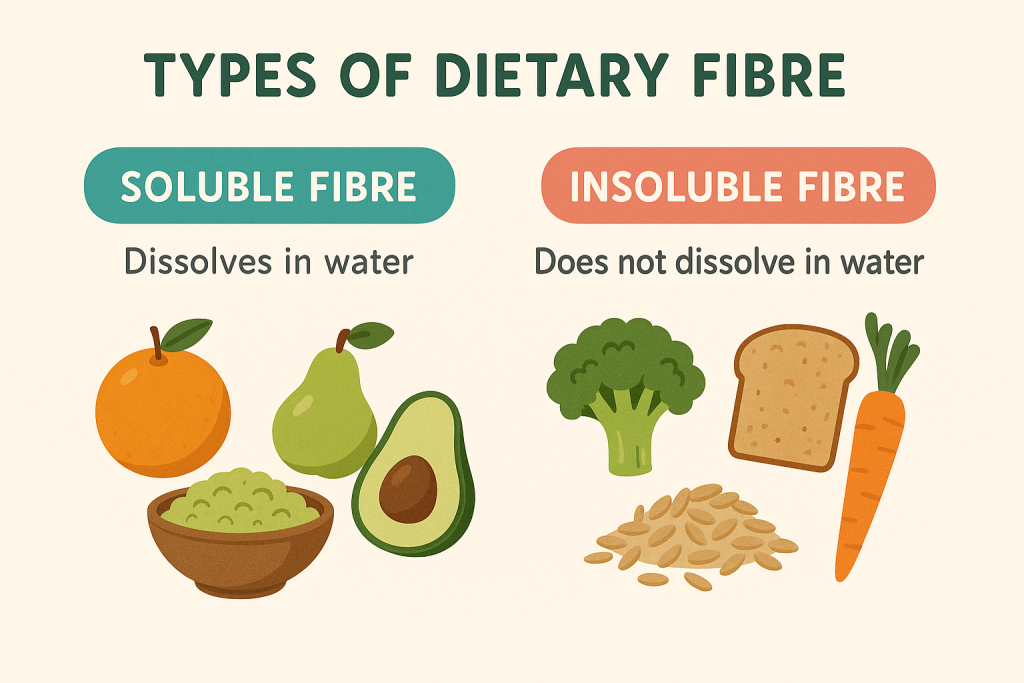
Dietary fibre is classified into two main types, based on its solubility in water.
1. Soluble Fibre
- Dissolves in water to form a gel-like substance.
- Helps in lowering cholesterol, controlling blood sugar, and promoting gut bacteria growth.
- Sources:
- Oats, barley
- Apples, citrus fruits
- Beans, lentils, peas
- Psyllium husk
2. Insoluble Fibre
- Does not dissolve in water and remains intact in the digestive system.
- Helps in increasing stool bulk, preventing constipation, and promoting bowel movements.
- Sources:
- Whole grains (wheat bran, brown rice)
- Nuts and seeds
- Vegetables (carrots, celery, cabbage)
- Skins of fruits (apples, pears)
Functions and Benefits of Dietary Fibre
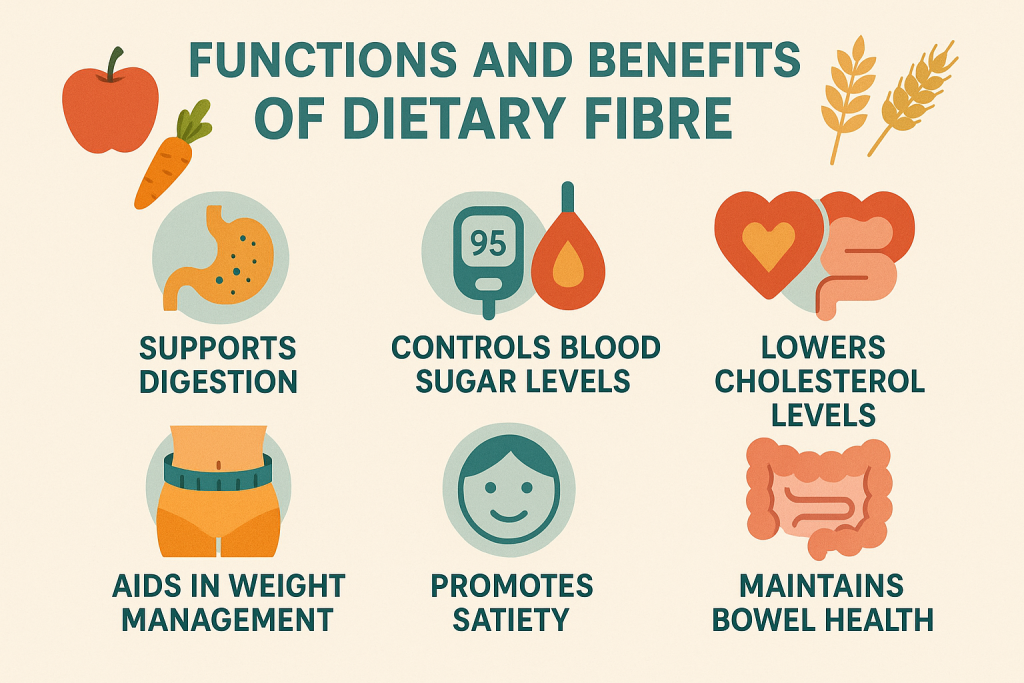
1. Improves Digestive Health
- Prevents constipation by adding bulk to stool.
- Insoluble fibre promotes faster digestion and regular bowel movements.
- Reduces the risk of hemorrhoids and diverticulosis.
2. Controls Blood Sugar Levels
- Soluble fibre slows down the absorption of sugars, preventing spikes in blood glucose.
- Beneficial for diabetic patients to regulate insulin levels.
3. Lowers Cholesterol Levels
- Soluble fibre binds to bad cholesterol (LDL) and helps remove it from the body.
- Reduces the risk of heart diseases and stroke.
4. Aids in Weight Management
- Fibre-rich foods increase satiety (feeling of fullness), reducing calorie intake.
- Helps in preventing overeating and managing obesity.
5. Promotes Healthy Gut Bacteria (Prebiotic Effect)
- Certain fibres act as prebiotics, feeding beneficial gut bacteria.
- Supports gut microbiome health and prevents digestive disorders.
6. Reduces Risk of Certain Cancers
- High fibre intake is linked to a lower risk of colorectal cancer.
- Helps in removing toxins and carcinogens from the gut.
Daily Recommended Intake of Dietary Fibre (RDA)
| Age & Gender | Recommended Fibre Intake |
|---|---|
| Children (1-3 years) | 19g/day |
| Children (4-8 years) | 25g/day |
| Males (9-18 years) | 31-38g/day |
| Females (9-18 years) | 26g/day |
| Adult Males | 30-38g/day |
| Adult Females | 21-25g/day |
| Pregnant Women | 28g/day |
| Lactating Women | 29g/day |
Sources of Dietary Fibre
| Food | Fibre Content (per 100g) |
|---|---|
| Wheat Bran | 42g |
| Oats | 10g |
| Brown Rice | 3.5g |
| Apple (with skin) | 2.4g |
| Banana | 2.6g |
| Carrot | 2.8g |
| Almonds | 12.5g |
| Lentils (Cooked) | 7.9g |
| Chia Seeds | 34g |
| Flaxseeds | 27 |
Effects of Fibre Deficiency
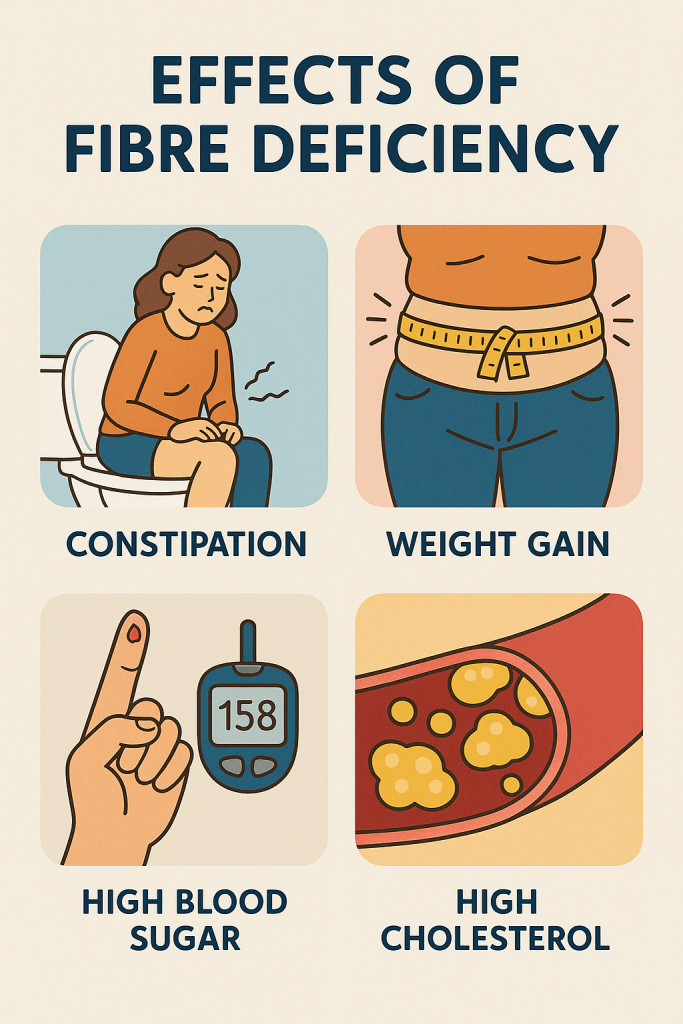
- Constipation and digestive issues
- Increased risk of heart disease (due to high LDL cholesterol)
- Blood sugar fluctuations (higher risk of diabetes)
- Weight gain and obesity (due to overeating)
- Increased risk of colorectal cancer
Excess Fibre Consumption – Side Effects
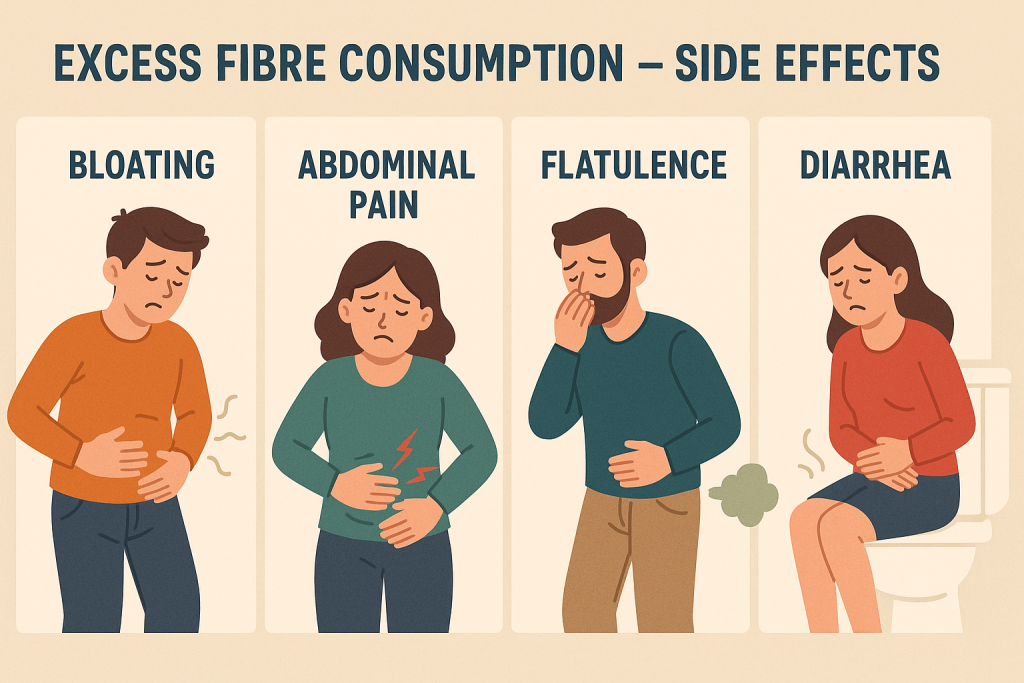
While fibre is beneficial, consuming too much fibre can lead to:
- Bloating and gas
- Abdominal cramps
- Diarrhea or loose stools
- Interference with nutrient absorption (especially iron, calcium, and zinc)
Tip: Always increase fibre intake gradually and drink plenty of water to prevent digestive discomfort.
Tips to Increase Fibre Intake
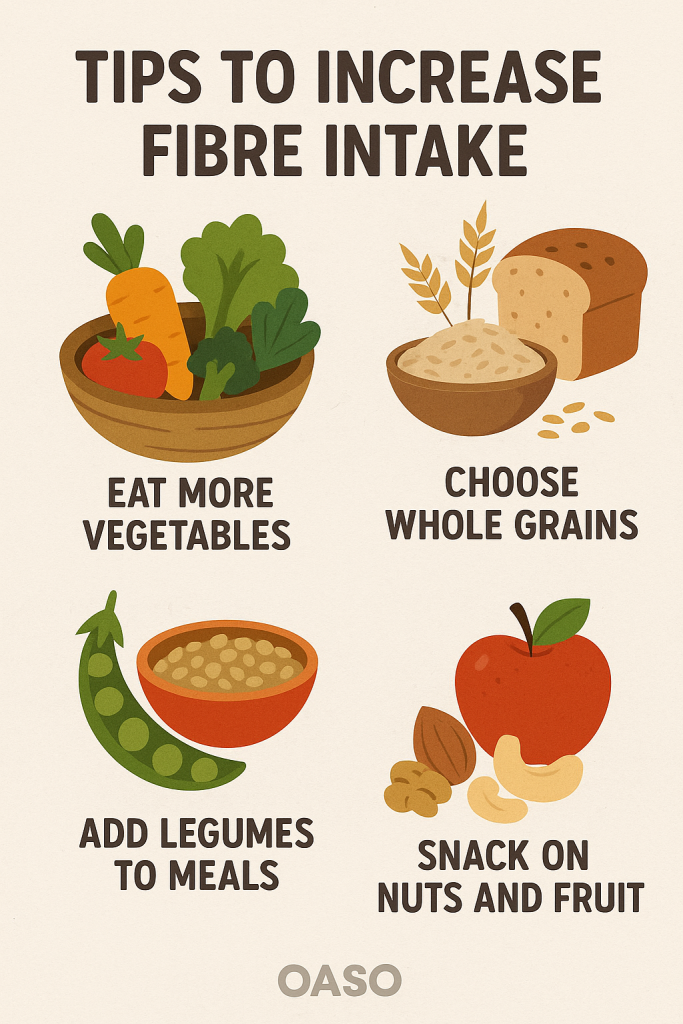
- Choose whole grains over refined grains (e.g., brown rice instead of white rice).
- Eat fruits with their skin instead of peeling them.
- Add legumes and beans to soups, salads, and curries.
- Include nuts and seeds as snacks.
- Use flaxseeds or chia seeds in smoothies or yogurt.
- Drink plenty of water to help fibre move through the digestive tract.
Balanced Diet for Different Age Groups.
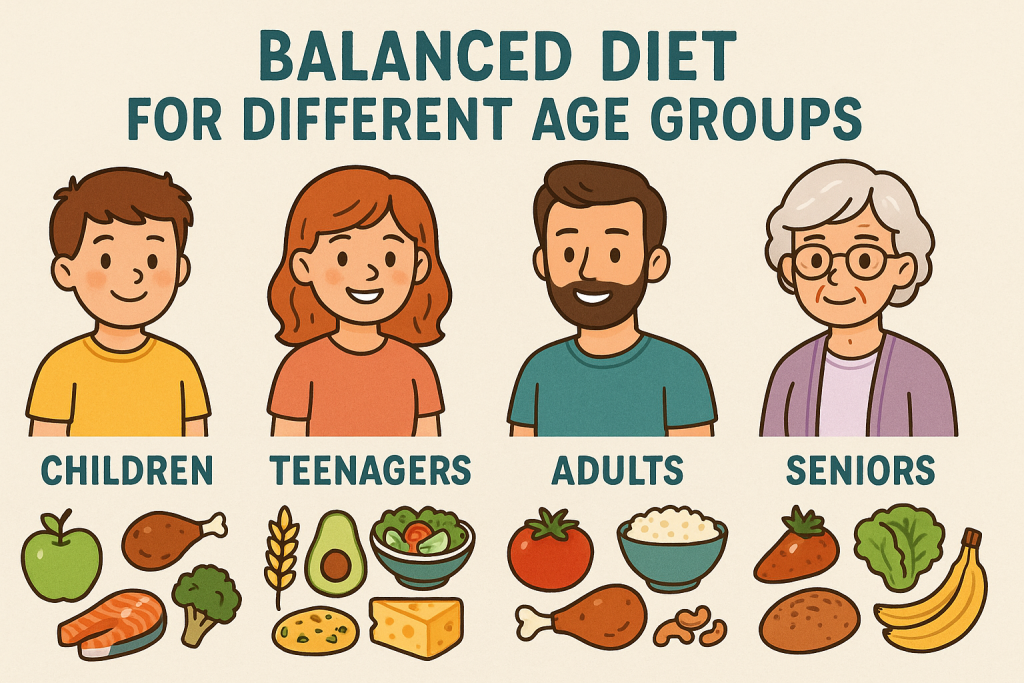
A balanced diet provides all the essential nutrients required for growth, development, and overall health. Nutritional needs vary based on age, gender, physiological conditions (such as pregnancy and lactation), and activity levels.
This guide explains the nutritional requirements for different age groups and provides sample meal plans for each category.
1. Balanced Diet for Infants (0-1 Year)
Nutritional Requirements
- Breast milk (or infant formula) is the primary source of nutrition for the first 6 months.
- Introduce semi-solid foods from 6 months onwards.
- Iron and vitamin D supplements may be needed if breast milk is the only source of nutrition.
Sample Diet Plan for Infants
| Age | Food Recommendations |
|---|---|
| 0-6 Months | Exclusive breastfeeding or infant formula |
| 6-8 Months | Mashed banana, soft rice, lentil soup, vegetable puree |
| 8-12 Months | Soft chapati, boiled egg yolk, mashed potatoes, yogurt |
2. Balanced Diet for Toddlers (1-3 Years)
Nutritional Requirements
- High energy and protein for rapid growth.
- Calcium and vitamin D for bone development.
- Iron-rich foods to prevent anemia.
- Frequent small meals due to small stomach size.
Sample Diet Plan for Toddlers
| Meal | Food Suggestions |
|---|---|
| Breakfast | Milk with whole-grain cereal, banana |
| Mid-Morning Snack | Yogurt, fruit slices |
| Lunch | Rice, dal, vegetables, small portion of fish/chicken |
| Evening Snack | Whole wheat toast with peanut butter |
| Dinner | Soft chapati with mashed lentils, carrot soup |
3. Balanced Diet for Preschoolers (4-6 Years)1
Nutritional Requirements
- High protein for muscle growth.
- Calcium & vitamin D for strong bones.
- Fiber-rich foods to aid digestion.
- Encourage healthy eating habits and variety.
Sample Diet Plan for Preschoolers
| Meal | Food Suggestions |
|---|---|
| Breakfast | Milk with oats, boiled egg, fruit |
| Mid-Morning Snack | Dry fruits and nuts |
| Lunch | Whole wheat roti, dal, sabzi, yogurt |
| Evening Snack | Roasted chana or homemade cookies |
| Dinner | Rice with vegetable curry, paneer |
4. Balanced Diet for School-Age Children (7-12 Years)
Nutritional Requirements
- Balanced intake of all nutrients for growth.
- Protein and iron for muscle and brain development.
- Calcium-rich foods for bone strength.
- Healthy snacks to prevent junk food consumption.
Sample Diet Plan for School-Age Children
| Meal | Food Suggestions |
|---|---|
| Breakfast | Whole wheat bread, peanut butter, milk |
| Mid-Morning Snack | Apple or orange, nuts |
| Lunch | Rice, dal, chicken, green salad |
| Evening Snack | Homemade sandwich, fresh juice |
| Dinner | Chapati, sabzi, yogurt, soup |
5. Balanced Diet for Adolescents (13-18 Years)
Nutritional Requirements
- Higher energy needs due to puberty.
- Protein-rich diet to support muscle growth.
- Iron and folic acid (especially for girls to prevent anemia).
- Calcium and vitamin D for bone health.
Sample Diet Plan for Adolescents
| Meal | Food Suggestions |
|---|---|
| Breakfast | Milk, boiled eggs, whole grain toast |
| Mid-Morning Snack | Yogurt with fruit |
| Lunch | Brown rice, lentils, fish/chicken, salad |
| Evening Snack | Sprouts or dry fruits |
| Dinner | Whole wheat chapati, vegetable curry, yogurt |
6. Balanced Diet for Adults (19-50 Years)
Nutritional Requirements
- Balanced intake of carbohydrates, proteins, and fats.
- Fiber-rich foods to prevent lifestyle diseases.
- Healthy fats (nuts, olive oil) over trans fats.
- Hydration (2-3 liters of water daily).
Sample Diet Plan for Adults
| Meal | Food Suggestions |
|---|---|
| Breakfast | Oats with milk, nuts, and fruit |
| Mid-Morning Snack | Green tea, handful of almonds |
| Lunch | Multigrain roti, dal, mixed vegetables, yogurt |
| Evening Snack | Sprouts or buttermilk |
| Dinner | Brown rice, grilled fish/tofu, sautéed vegetables |
7. Balanced Diet for Pregnant Women
Nutritional Requirements
- Increased calories (+300 kcal/day in the second and third trimesters).
- High protein for fetal growth.
- Iron and folic acid to prevent anemia and birth defects.
- Calcium and vitamin D for fetal bone development.
- Plenty of fluids to prevent dehydration.
Sample Diet Plan for Pregnant Women
| Meal | Food Suggestions |
|---|---|
| Breakfast | Whole wheat toast, boiled eggs, milk |
| Mid-Morning Snack | Fruits, almonds, walnuts |
| Lunch | Brown rice, dal, paneer curry, salad |
| Evening Snack | Yogurt with flaxseeds |
| Dinner | Multigrain roti, grilled chicken/fish, vegetable soup |
8. Balanced Diet for Lactating Mothers
Nutritional Requirements
- Increased energy (+500 kcal/day).
- High protein intake for milk production.
- Iron and calcium-rich foods for mother and baby.
- Plenty of fluids to maintain hydration.
Sample Diet Plan for Lactating Mothers
| Meal | Food Suggestions |
|---|---|
| Breakfast | Oats with milk, nuts, banana |
| Mid-Morning Snack | Buttermilk, dry fruits |
| Lunch | Rice, dal, green leafy vegetables, paneer |
| Evening Snack | Whole wheat biscuits with tea |
| Dinner | Chapati, fish curry, vegetable salad |
9. Balanced Diet for Elderly (Above 50 Years)
Nutritional Requirements
- Low-calorie but nutrient-dense diet to prevent weight gain.
- High fiber intake to prevent constipation.
- Calcium and vitamin D to prevent osteoporosis.
- Low salt and sugar to manage blood pressure and diabetes.
Sample Diet Plan for Elderly
| Meal | Food Suggestions |
|---|---|
| Breakfast | Porridge, milk, banana |
| Mid-Morning Snack | Almonds, herbal tea |
| Lunch | Soft chapati, dal, boiled vegetables |
| Evening Snack | Fruit smoothie |
| Dinner | Khichdi, yogurt, steamed vegetables |
Meal Planning / Menu Planning

Definition of Meal Planning
Meal planning refers to the process of organizing meals in advance to ensure a balanced, nutritious, and cost-effective diet. It involves selecting foods that meet nutritional requirements, cultural preferences, availability, and budget constraints.
Key Elements of Meal Planning:
- Nutritional adequacy – Ensuring all essential nutrients are included.
- Variety – Incorporating different food groups and flavors.
- Portion control – Avoiding overconsumption or deficiencies.
- Economic feasibility – Planning meals within a budget.
- Time efficiency – Reducing preparation time and food waste.
Definition of Menu Planning
Menu planning is the systematic selection of meals for a specific time frame (daily, weekly, or monthly) based on nutritional guidelines, dietary needs, and food preferences.
Types of Menu Planning:
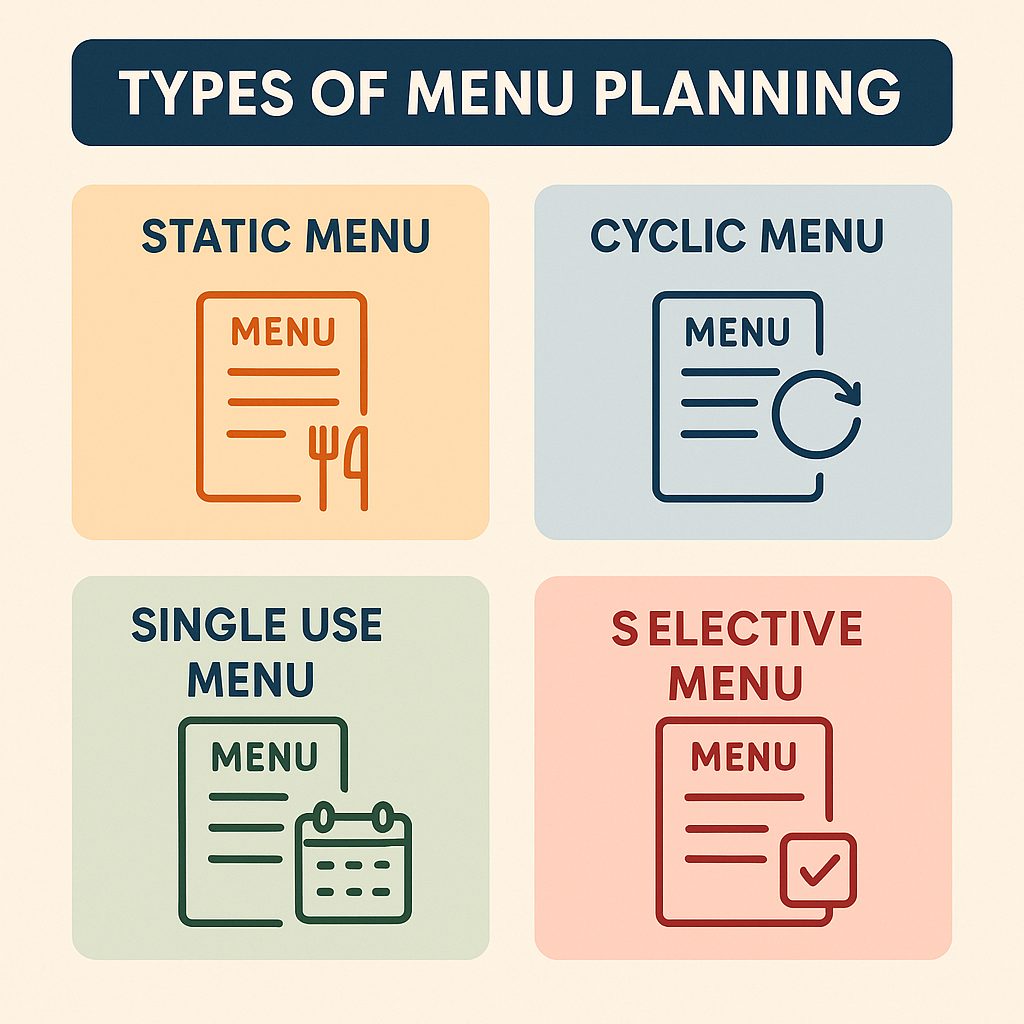
- Cyclic Menu – Repeats every 1-4 weeks (used in hospitals, schools).
- Selective Menu – Offers multiple choices for different meals.
- Non-selective Menu – A fixed meal plan with no choices (used in military, correctional facilities).
- Therapeutic Menu – Designed for medical conditions (e.g., diabetic diet, low-sodium diet).
Introduction to Meal & Menu Planning
A well-planned meal ensures optimal health and well-being by providing balanced nutrition, meal variety, and portion control. Meal planning helps in:
1. Promoting Nutritional Balance
- Includes all food groups (carbohydrates, proteins, fats, vitamins, minerals).
- Prevents nutrient deficiencies and lifestyle diseases.
2. Saving Time & Effort
- Reduces daily decision-making stress.
- Ensures efficient grocery shopping and meal prep.
3. Reducing Food Waste & Budget Management
- Encourages buying only necessary ingredients.
- Minimizes unnecessary expenses on fast food and unhealthy snacks.
4. Customizing Meals for Specific Needs
- Helps cater to different age groups, dietary restrictions, and medical conditions.
- Example: High-protein diet for athletes, diabetic-friendly menu for diabetics.
Principles of Meal Planning / Menu Planning
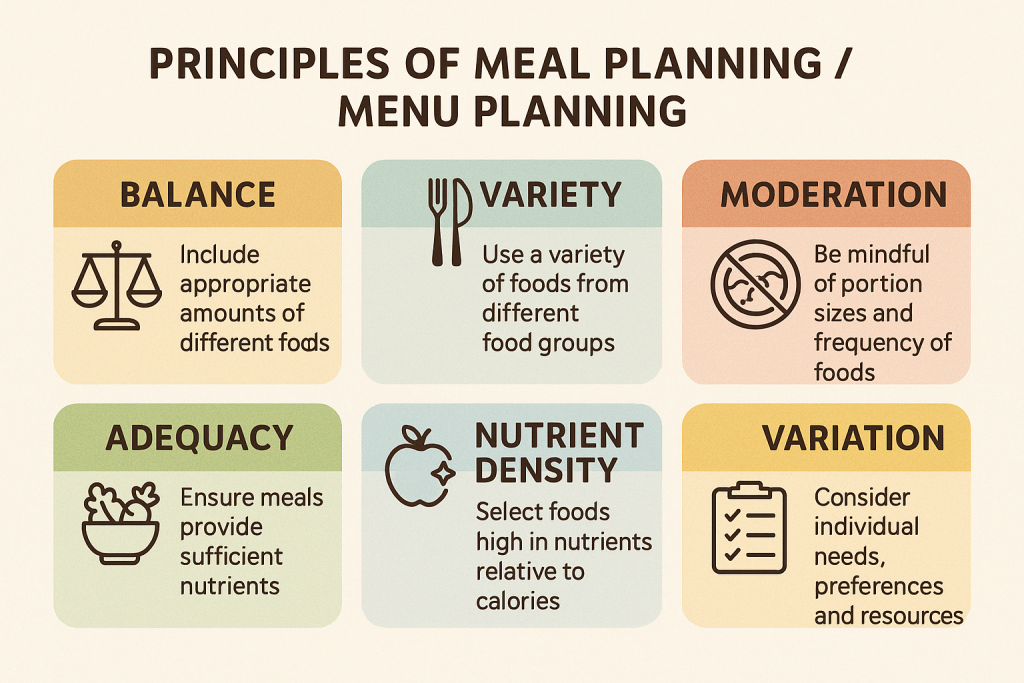
Meal planning and menu planning are systematic approaches to organizing meals that meet nutritional, economic, and practical requirements. Following scientific principles ensures that meals are balanced, cost-effective, and culturally appropriate.
1. Nutritional Adequacy
A meal should provide all essential nutrients (carbohydrates, proteins, fats, vitamins, minerals, fiber, and water) in the right proportions to meet daily dietary needs.
Key Considerations:
- Balanced Diet: Meals should include all food groups (grains, vegetables, fruits, dairy, and protein).
- Age-Specific Needs: Different age groups have unique dietary requirements.
- Medical Considerations: Special diets for conditions like diabetes, hypertension, and kidney disease.
Example:
A meal plan for an adult male should provide 2500 kcal/day, with a balanced proportion of macronutrients:
- Carbohydrates: 50-60%
- Proteins: 10-15%
- Fats: 20-30%
2. Variety in Food Selection
A meal plan should include a wide range of foods to ensure diversity in nutrients, flavors, colors, and textures.
Key Considerations:
- Prevents monotony and food fatigue.
- Ensures a better intake of all essential nutrients.
- Increases appetite and enjoyment of meals.
Example:
A weekly meal plan should include:
- Different protein sources (chicken, fish, tofu, lentils).
- Variety of grains (wheat, rice, oats, quinoa).
- Seasonal fruits and vegetables to ensure maximum nutrient intake.
3. Balance of Food Groups
Meals should contain all major food groups in the correct proportions.
Key Considerations:
- Macronutrient balance: Carbohydrates, proteins, and fats should be distributed correctly.
- Micronutrient balance: Include iron, calcium, vitamins, and minerals to prevent deficiencies.
Example of a Balanced Plate:
- Carbohydrates: Brown rice or whole wheat chapati.
- Protein: Lentils, chicken, or paneer.
- Healthy Fats: Nuts, olive oil, or seeds.
- Vegetables & Fruits: Leafy greens, carrots, apples.
4. Portion Control & Energy Balance
Meals should be proportionate to an individual’s daily calorie and activity level.
Key Considerations:
- Prevent overconsumption to avoid obesity.
- Prevent underconsumption, which can lead to malnutrition.
- Distribute calories evenly throughout the day (breakfast, lunch, dinner, snacks).
Example:
For a sedentary adult, portion control should follow:
- Breakfast: 25% of daily calories (e.g., oats, milk, nuts).
- Lunch: 35% of daily calories (e.g., rice, dal, vegetables).
- Dinner: 30% of daily calories (e.g., chapati, paneer curry, salad).
- Snacks: 10% of daily calories (e.g., fruit, yogurt).
5. Inclusion of Fiber & Hydration
- Dietary fiber is essential for digestion and gut health.
- Adequate water intake prevents dehydration and aids metabolism.
Key Considerations:
- Fiber-rich foods prevent constipation, heart disease, and diabetes.
- Hydration helps detoxify the body and maintain body functions.
Example:
- Fiber Sources: Whole grains, vegetables, fruits, legumes.
- Hydration: At least 8-10 glasses of water per day.
6. Economic Feasibility (Budget-Friendly Planning)
Meals should be affordable and within the family’s financial capacity.
Key Considerations:
- Use seasonal and locally available foods to reduce costs.
- Reduce food wastage by planning portion sizes.
- Substitute expensive ingredients with economical alternatives.
Example:
- Replace expensive protein sources (chicken, fish) with cheaper alternatives (lentils, eggs, soy).
- Buy fresh and seasonal vegetables instead of imported foods.
7. Availability & Accessibility of Ingredients
A meal plan should consider food availability in a given location and season.
Key Considerations:
- Use locally grown produce for freshness and better nutrition.
- Avoid out-of-season foods that are expensive and less nutritious.
- Plan meals around easily available staple foods.
Example:
- Use millets and ragi in regions where wheat or rice is scarce.
- Fresh vegetables and fruits should be prioritized over processed food.
8. Simplicity & Ease of Preparation
Meals should be easy to prepare, cook, and serve, especially in busy households.
Key Considerations:
- Minimize complex recipes that take too long.
- Choose nutritious, quick-cooking options like boiled eggs, salads, or one-pot meals.
- Ensure meals are enjoyable for all age groups.
Example:
- Breakfast: Oats with fruits & nuts (quick and nutritious).
- Lunch: Rice, dal, vegetables (simple yet balanced).
- Dinner: Multigrain chapati, paneer curry, salad (light and healthy).
9. Cultural & Religious Considerations
Meals should align with cultural traditions, religious beliefs, and food habits.
Key Considerations:
- Respect vegetarian or non-vegetarian preferences.
- Consider fasting practices and dietary restrictions.
- Adapt regional flavors and traditional cooking methods.
Example:
- Hindu meals may avoid beef.
- Muslim meals may include halal-certified foods.
- Jain meals exclude onion and garlic.
10. Meal Timing & Frequency
Proper meal timing is crucial for better digestion and metabolism.
Key Considerations:
- Breakfast is the most important meal and should be rich in protein and fiber.
- Lunch should be the largest meal, providing sustained energy.
- Dinner should be light, avoiding heavy foods close to bedtime.
- Healthy snacks prevent overeating at main meals.
Example:
| Time | Meal |
|---|---|
| 7:30 AM | Breakfast (high-protein, fiber-rich) |
| 10:30 AM | Mid-morning snack (fruit, yogurt) |
| 1:30 PM | Lunch (balanced meal with carbs, protein, vegetables) |
| 5:00 PM | Evening snack (nuts, sprouts, buttermilk) |
| 8:00 PM | Dinner (light, easily digestible meal) |
11. Special Dietary Needs (Customization)
Meal plans should be customized for different groups like children, pregnant women, elderly, and people with medical conditions.
Key Considerations:
- Children & Adolescents: High protein, calcium, and vitamins for growth.
- Pregnant & Lactating Women: More iron, folic acid, and calcium.
- Elderly: Soft foods, low salt, high fiber for easy digestion.
- Medical Diets: Special modifications for diabetes, hypertension, and kidney disease.
Example:
- A diabetic menu should include low-glycemic foods like whole grains, lean proteins, and fiber-rich vegetables.
- A meal plan for an elderly person should focus on soft foods, high calcium, and low sodium.
Steps of Meal Planning / Menu Planning

Meal planning is a systematic process that involves selecting, preparing, and organizing meals to ensure nutritional balance, cost-effectiveness, and efficiency. The following steps help in designing a well-structured, healthy, and practical meal plan.
1. Assess Nutritional Requirements
Before planning meals, it is essential to determine the nutritional needs based on:
- Age and gender (children, adults, elderly).
- Activity level (sedentary, moderate, high activity).
- Health status (pregnancy, lactation, medical conditions like diabetes or hypertension).
- Dietary preferences (vegetarian, non-vegetarian, religious restrictions).
Example:
- A pregnant woman requires additional iron, folic acid, and calcium.
- A school-age child needs high protein and energy for growth.
2. Decide on the Number of Meals per Day
Plan the frequency of meals, ensuring adequate energy distribution throughout the day.
| Meal Timing | Purpose |
|---|---|
| Breakfast (7:00–9:00 AM) | Provides energy for the day |
| Mid-Morning Snack (10:00–11:00 AM) | Prevents overeating at lunch |
| Lunch (1:00–2:00 PM) | Largest meal of the day |
| Evening Snack (4:00–5:00 PM) | Boosts metabolism, prevents cravings |
| Dinner (7:00–9:00 PM) | Light meal for easy digestion |
3. Select a Variety of Foods from All Food Groups
To ensure nutritional balance, meals should include:
- Carbohydrates (whole grains, rice, wheat, oats).
- Proteins (lentils, eggs, chicken, fish, tofu).
- Healthy fats (olive oil, nuts, seeds).
- Vitamins & Minerals (fruits, vegetables, dairy).
- Fiber & Hydration (whole grains, fruits, vegetables, 8-10 glasses of water).
Example:
For a balanced lunch:
- Carbohydrates: Brown rice or whole wheat chapati.
- Proteins: Lentils or grilled chicken.
- Healthy fats: Nuts or olive oil dressing.
- Vegetables: Leafy greens, carrots, cucumbers.
4. Consider Dietary Restrictions and Preferences
Meal planning should be adaptable to:
- Cultural and religious restrictions (e.g., vegetarian diets, halal/kosher foods).
- Allergies and intolerances (e.g., lactose intolerance, gluten-free diets).
- Medical conditions (low-sodium diet for hypertension, diabetic-friendly meals).
Example:
- A Jain diet avoids onions and garlic.
- A diabetic meal should have low-glycemic foods like whole grains and vegetables.
5. Plan Meals Based on Seasonality and Availability
- Choose seasonal and locally available foods for freshness and cost-effectiveness.
- Avoid imported or processed foods that are expensive and less nutritious.
Example:
- Use mangoes in summer, and green leafy vegetables in winter.
- In coastal areas, include fresh fish instead of frozen meat.
6. Ensure Economic Feasibility (Budget Planning)
- Plan meals within a budget to avoid overspending.
- Use affordable and nutritious alternatives (e.g., lentils instead of expensive meat).
- Reduce food wastage by purchasing only what is needed.
Example:
- Instead of expensive protein sources like salmon, choose local fish or eggs.
- Buy whole grains in bulk to save costs.
7. Create a Weekly or Monthly Menu Plan
- List all meals and snacks for the week.
- Ensure variety and balance in food choices.
- Adjust portion sizes based on nutritional needs.
Example: Weekly Meal Plan (for an adult)
| Day | Breakfast | Lunch | Dinner |
|---|---|---|---|
| Monday | Oats with milk & nuts | Brown rice, dal, vegetables | Multigrain chapati, paneer curry |
| Tuesday | Boiled eggs, whole wheat toast | Quinoa salad, grilled chicken | Khichdi with yogurt |
| Wednesday | Idli with coconut chutney | Whole wheat chapati, sabzi, curd | Rice with fish curry |
| Thursday | Poha with peanuts | Lentil soup, steamed vegetables | Millet roti, dal |
| Friday | Vegetable upma | Rice, rajma, cucumber salad | Roti, soybean curry |
| Saturday | Paratha with curd | Grilled paneer, spinach soup | Rice with chana masala |
| Sunday | Sprouts with lemon | Chicken curry, brown rice | Vegetable khichdi |
8. Prepare a Grocery List
- List down all ingredients required for weekly meal preparation.
- Buy fresh produce first, followed by grains, dairy, and proteins.
- Check pantry supplies before purchasing new items.
Example:
For a weekly meal plan, a grocery list may include:
- Whole grains: Brown rice, whole wheat flour, oats.
- Protein sources: Lentils, eggs, paneer, chicken.
- Vegetables & fruits: Spinach, carrots, tomatoes, bananas.
- Dairy: Milk, yogurt, cheese.
- Spices & oils: Turmeric, cumin, olive oil.
9. Plan for Meal Preparation & Storage
- Batch cooking to save time (e.g., prepare large portions of dal, soups, curries).
- Use proper food storage techniques to maintain freshness.
- Cook perishable items first, store dry foods for longer use.
Example:
- Prepare chapati dough in advance and refrigerate.
- Soak lentils overnight for quick cooking the next day.
- Cut vegetables and store in airtight containers for convenience.
10. Evaluate and Adjust the Meal Plan
- Review if the meal plan meets nutritional goals.
- Modify based on family feedback, seasonal changes, and health conditions.
- Ensure no food wastage and cost-effectiveness.
Example Adjustments:
- If a child is not eating enough protein, increase egg, paneer, and milk intake.
- If someone has gastric issues, reduce spicy and heavy foods.
Conclusion
Following structured steps in meal planning ensures meals are nutritious, cost-effective, and time-efficient. A well-planned menu helps in:
✅ Maintaining health and wellness.
✅ Reducing food wastage and expenses.
✅ Providing variety and balanced nutrition.
By implementing these steps, individuals and families can enjoy a well-balanced diet, prevent nutritional deficiencies, and improve overall quality of life.
Infant and Young Child Feeding (IYCF) Guidelines
Introduction to IYCF
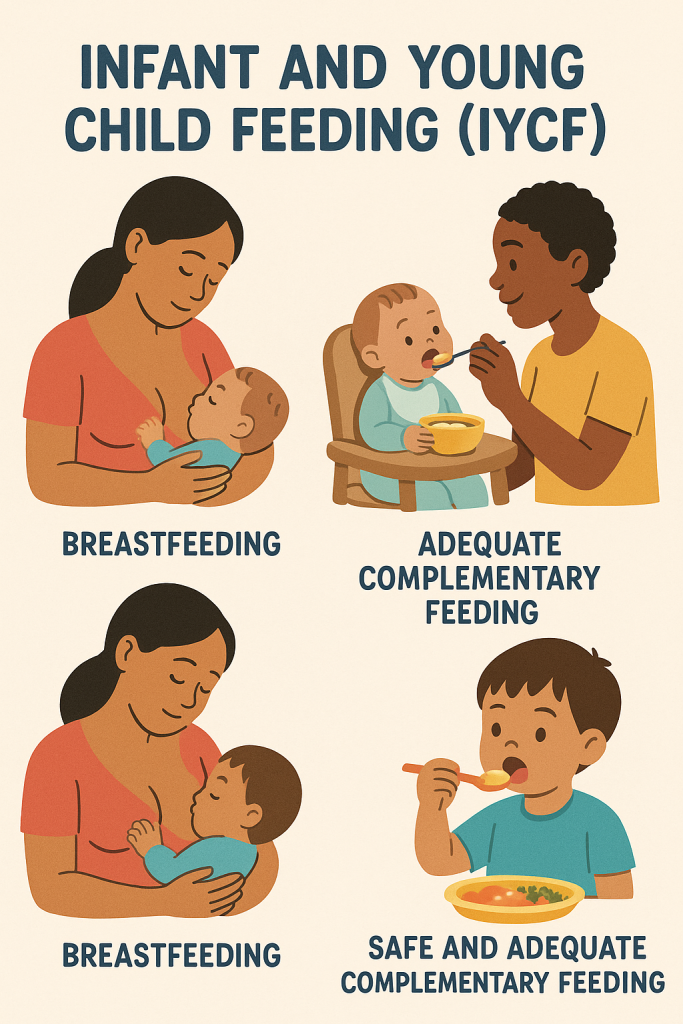
Infant and Young Child Feeding (IYCF) refers to a set of globally recommended feeding practices to ensure optimal nutrition, growth, and development in children from birth to 2 years of age. These guidelines are developed by organizations such as WHO (World Health Organization), UNICEF, and national health authorities to promote child survival and prevent malnutrition, infections, and developmental issues.
Key Components of IYCF Guidelines:
- Exclusive breastfeeding for the first 6 months.
- Timely introduction of complementary foods after 6 months.
- Continued breastfeeding up to 2 years or beyond.
- Safe and appropriate complementary feeding.
- Hygiene and responsive feeding practices.
IYCF Guidelines in Detail
1. Early Initiation of Breastfeeding (Within 1 Hour of Birth)
Why is it Important?
- Provides colostrum (first milk), which is rich in antibodies and nutrients.
- Helps in developing immunity and reducing neonatal mortality.
- Promotes bonding between mother and baby.
Guideline:
- Start breastfeeding immediately after birth, even in C-section deliveries.
- Encourage skin-to-skin contact to stimulate lactation.
- Avoid giving pre-lacteal feeds (honey, sugar water, formula milk).
2. Exclusive Breastfeeding for the First 6 Months
Why is it Important?
- Provides all essential nutrients (carbohydrates, proteins, fats, vitamins, and minerals).
- Enhances brain development and reduces risk of infections (diarrhea, pneumonia).
- Promotes healthy weight gain and digestion.
Guideline:
- Give only breast milk for the first 6 months (no water, formula, or solids).
- Breastfeed on demand (every 2-3 hours, both day and night).
- Ensure correct positioning and latch for effective milk transfer.
- Monitor for adequate weight gain and urine output (at least 6-8 times/day).
3. Introduction of Complementary Feeding at 6 Months
Why is it Important?
- By 6 months, breast milk alone is not enough to meet nutritional needs.
- Complementary foods provide extra energy, protein, iron, and vitamins.
Guideline:
- Start with soft, mashed, or pureed foods (cooked cereals, fruits, and vegetables).
- Continue breastfeeding along with solid foods.
- Introduce one new food at a time (to identify allergies).
- Increase meal frequency and portion sizes gradually.
| Age | Consistency of Food | Meal Frequency |
|---|---|---|
| 6-8 Months | Mashed/pureed food | 2-3 meals/day + breast milk |
| 9-12 Months | Soft, chopped food | 3-4 meals/day + 1-2 snacks |
| 12-24 Months | Family foods (small pieces) | 4 meals/day + 2 snacks |
4. Continued Breastfeeding Up to 2 Years or Beyond
Why is it Important?
- Provides half of a child’s energy needs from 6-12 months and one-third from 12-24 months.
- Boosts immunity and protects against infections.
- Supports brain and emotional development.
Guideline:
- Breastfeed along with complementary feeding until at least 2 years.
- Allow the child to self-wean gradually.
- Breastfeeding can be continued beyond 2 years if desired by the mother and child.
5. Appropriate Complementary Feeding Practices
To ensure nutritional adequacy, complementary feeding should follow WHO’s “FADUA” principle:
| Principle | Description |
|---|---|
| Frequency | Feed age-appropriate number of meals per day. |
| Amount | Increase portion sizes gradually. |
| Density | Provide energy-dense foods (not watery soups). |
| Utilization | Ensure hygienic food preparation and responsive feeding. |
| Active Feeding | Encourage self-feeding and respond to hunger cues. |
Food Groups for Complementary Feeding:
✔ Grains (Rice, wheat, oats) – Energy source
✔ Proteins (Lentils, eggs, fish, meat) – Growth & muscle development
✔ Fruits & Vegetables – Vitamins, minerals, fiber
✔ Dairy (Milk, curd, cheese) – Calcium for bones
✔ Healthy Fats (Nuts, ghee, oil) – Brain development
6. Responsive Feeding Practices
Why is it Important?
- Encourages healthy eating habits.
- Prevents feeding difficulties.
Guideline:
- Feed the child in a calm, distraction-free environment.
- Allow self-feeding when the child is ready.
- Avoid force-feeding.
- Observe the child’s hunger and fullness cues.
7. Food Safety & Hygiene
Why is it Important?
- Prevents diarrhea and infections.
- Ensures safe food preparation for infants.
Guideline:
- Wash hands before preparing or feeding food.
- Use clean utensils and prepare fresh food daily.
- Avoid bottle feeding (risk of contamination) – use a cup and spoon instead.
- Store food properly to prevent spoilage.
8. Feeding During Illness & Recovery
Why is it Important?
- Prevents malnutrition and weight loss.
- Speeds up recovery from infections.
Guideline:
- Increase breastfeeding during illness.
- Give small, frequent meals that are easy to digest.
- Provide ORS (Oral Rehydration Solution) and fluids to prevent dehydration.
- Resume normal diet as soon as the child recovers.
9. Avoiding Junk Food and Sugary Drinks
Why is it Important?
- Prevents obesity and nutrient deficiencies.
- Reduces the risk of tooth decay and diabetes.
Guideline:
- Avoid processed foods, fast food, and sugary drinks.
- Encourage homemade, natural foods.
- Limit salt, sugar, and artificial flavors in baby food.
Special Considerations in IYCF
For Low Birth Weight & Preterm Babies:
- Encourage kangaroo mother care (KMC) for warmth and bonding.
- Provide fortified breast milk or donor milk if needed.
For Working Mothers:
- Encourage expressed breast milk storage for later use.
- Educate about breastfeeding rights at the workplace.
For Infants of HIV-Positive Mothers:
- WHO recommends exclusive breastfeeding with antiretroviral therapy (ART) to prevent transmission.
- If replacement feeding is used, it should be safe, affordable, and sustainable.
Breastfeeding
Introduction
Breastfeeding is the natural process of feeding an infant with human breast milk, either directly from the mother’s breast or through expressed milk. It is the optimal source of nutrition for newborns and infants, providing all the essential nutrients required for growth, immunity, and development.
- WHO & UNICEF Recommendation:
- Early initiation of breastfeeding within one hour of birth.
- Exclusive breastfeeding for the first 6 months (no other food or drink, not even water).
- Continued breastfeeding up to 2 years or beyond, along with complementary foods.
Types of Breastfeeding
1. Exclusive Breastfeeding (0-6 Months)
- The infant receives only breast milk, without any other liquids or solids.
- No water, honey, or formula milk is given.
- Provides complete nutrition and immunity for the baby.
2. Predominant Breastfeeding
- The infant receives breast milk as the main source of nutrition, but small amounts of water, juice, or oral rehydration solution (ORS) may be given.
- Less beneficial than exclusive breastfeeding.
3. Partial Breastfeeding
- The infant receives both breast milk and other food sources (formula milk, solids).
- Common in infants above 6 months.
4. Expressed Breast Milk Feeding
- The mother expresses milk manually or with a breast pump, and it is fed to the baby using a cup, spoon, or bottle.
- Useful for working mothers or sick infants.
Composition of Breast Milk
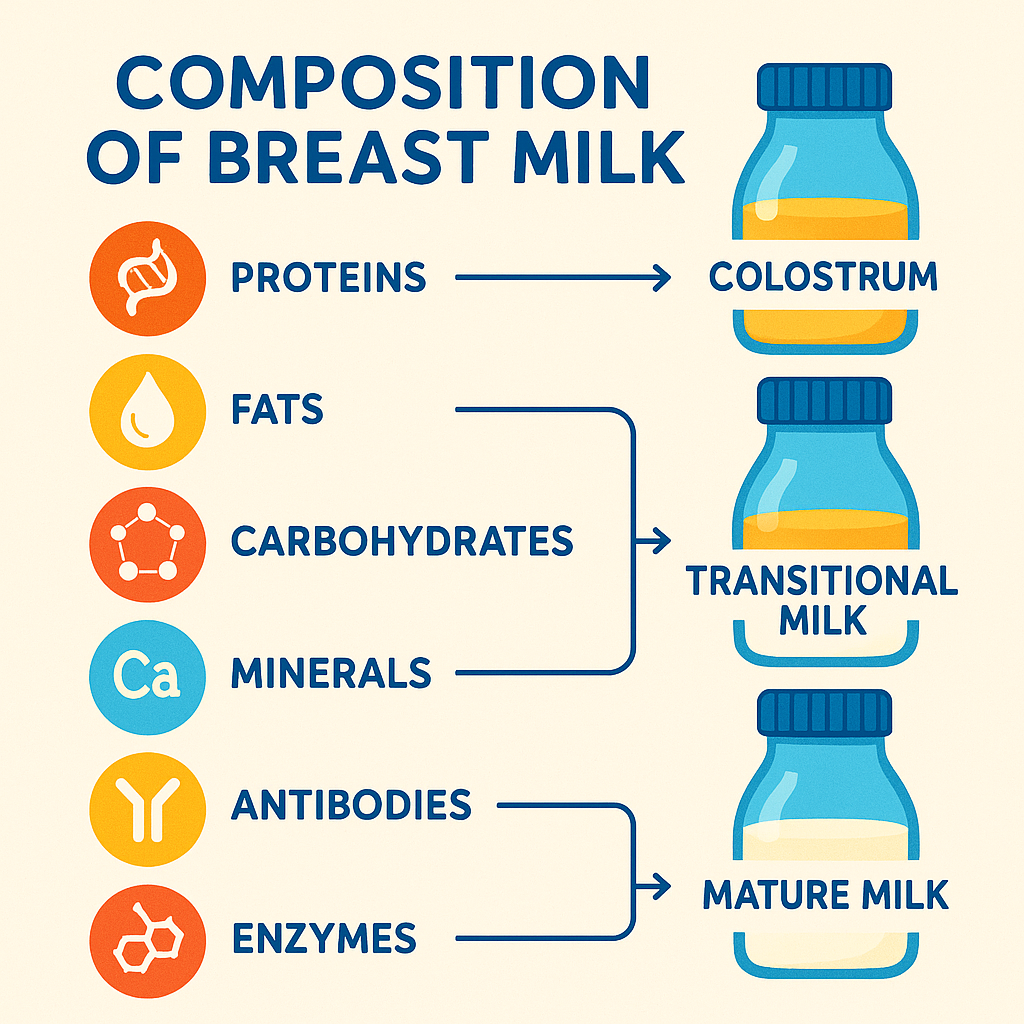
Breast milk is a dynamic and living fluid that changes according to the baby’s needs. It consists of:
| Component | Function |
|---|---|
| Colostrum (First milk) | Thick, yellowish milk produced in the first 2-4 days. Rich in antibodies, white blood cells, and protein for newborn immunity. |
| Transitional Milk | Produced 4-10 days postpartum, has higher fat and lactose content than colostrum. |
| Mature Milk | Appears after 10 days, providing complete nutrition with balanced proteins, fats, carbohydrates, and vitamins. |
Nutritional Content of Breast Milk
| Nutrient | Function |
|---|---|
| Proteins (Whey & Casein) | Easy digestion, brain development, immunity |
| Carbohydrates (Lactose) | Energy, absorption of calcium, gut health |
| Fats (DHA, Omega-3) | Brain and nerve development |
| Vitamins & Minerals | Growth, immunity, bone development |
| Antibodies (IgA, IgG, IgM) | Protection against infections |
| Water (87%) | Hydration, temperature regulation |
Benefits of Breastfeeding

1. Benefits for the Baby
✅ Boosts Immunity – Breast milk contains antibodies that protect against infections.
✅ Supports Brain Development – Rich in DHA (omega-3 fatty acids) for cognitive growth.
✅ Prevents Malnutrition – Ensures adequate nutrition for proper weight gain.
✅ Reduces Disease Risk – Lowers chances of diarrhea, pneumonia, ear infections, and allergies.
✅ Improves Digestion – Easily digestible compared to formula milk.
✅ Reduces SIDS (Sudden Infant Death Syndrome) – Promotes safe sleep patterns.
2. Benefits for the Mother
✅ Promotes Uterine Contraction – Releases oxytocin, helping the uterus shrink faster.
✅ Reduces Risk of Diseases – Lowers the chances of breast and ovarian cancer, osteoporosis, and heart disease.
✅ Helps in Postpartum Weight Loss – Burns 500 extra calories per day.
✅ Delays Menstruation and Natural Birth Spacing – Reduces ovulation (natural contraception).
✅ Strengthens Mother-Infant Bonding – Releases hormones like oxytocin.
Breastfeeding Techniques & Proper Latching
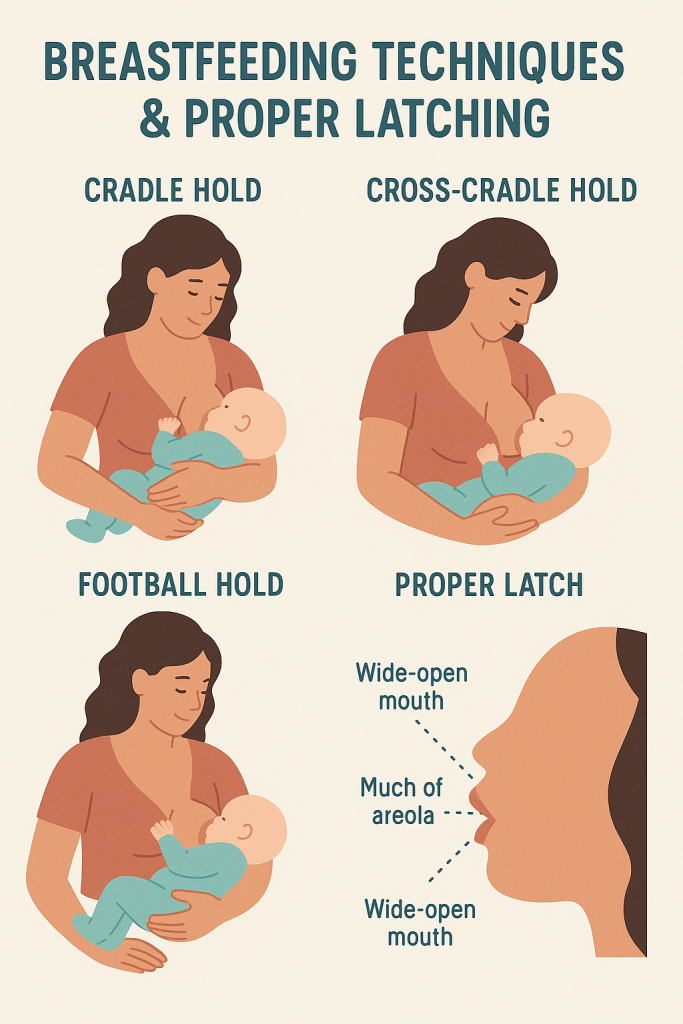
1. Positioning the Baby for Breastfeeding
A comfortable position ensures effective feeding and prevents nipple pain.
✅ Cradle Hold – The baby’s head rests in the mother’s elbow bend.
✅ Cross-Cradle Hold – Baby’s head is supported with the opposite hand.
✅ Football Hold – Baby is tucked under the mother’s arm (useful after a C-section).
✅ Side-Lying Position – Lying down while feeding (useful at night).
2. Signs of a Good Latch
🔹 Baby’s mouth is wide open and covers the areola (not just the nipple).
🔹 Baby’s lips are flanged outward (not tucked in).
🔹 Baby is swallowing milk rhythmically.
🔹 Mother feels a pulling sensation but no pain.
3. Frequency of Breastfeeding
📌 Newborns should be breastfed 8-12 times per day (every 2-3 hours).
📌 As the baby grows, feeding frequency reduces but volume increases.
Common Breastfeeding Problems & Solutions
| Issue | Cause | Solution |
|---|---|---|
| Sore Nipples | Incorrect latching | Adjust position, apply breast milk to nipples |
| Low Milk Supply | Stress, dehydration, infrequent feeding | Increase skin-to-skin contact, feed often, stay hydrated |
| Engorgement (Full, painful breasts) | Baby not feeding properly | Express milk, use cold compress, gentle massage |
| Blocked Milk Ducts | Improper milk drainage | Warm compress, massage, frequent feeding |
| Mastitis (Breast Infection) | Bacterial infection | Continue breastfeeding, take antibiotics if prescribed |
| Flat/Inverted Nipples | Genetic condition | Use nipple shields or express milk |
Breastfeeding in Special Situations
1. Breastfeeding for Preterm or Low Birth Weight Babies
- Encourage Kangaroo Mother Care (KMC) for warmth and bonding.
- Feed through expressed breast milk if direct latching is difficult.
2. Breastfeeding for Working Mothers
- Express milk using a breast pump and store it in the refrigerator.
- Use cup and spoon feeding instead of bottles to avoid nipple confusion.
- Breastfeeding rights at the workplace should be supported.
3. Breastfeeding for HIV-Positive Mothers
- WHO recommends breastfeeding if the mother is on antiretroviral therapy (ART).
- If formula is used, it must be safe, affordable, and sustainable.
Safe Storage of Expressed Breast Milk
| Storage Method | Temperature | Storage Time |
|---|---|---|
| Room Temperature | 25°C | 4-6 hours |
| Refrigerator | 4°C | Up to 4 days |
| Freezer | -18°C | 6 months |
Important:
✅ Store milk in clean, BPA-free containers.
✅ Label with date and time before storage.
✅ Thaw frozen milk in warm water (do not microwave).
Weaning: Transition from Breastfeeding to Solid Foods
- Start complementary feeding at 6 months while continuing breastfeeding.
- Gradually reduce breastfeeding sessions by replacing with family foods.
- Stop breastfeeding when the child is nutritionally ready (usually after 2 years).
Infant Foods

Introduction
Infant foods refer to the various forms of nutrition provided to babies from birth to 12 months of age. The nutritional needs of infants change as they grow, requiring breast milk or formula initially, followed by the gradual introduction of solid foods (complementary feeding) from 6 months onward.
- WHO & UNICEF Recommendations:
- Exclusive breastfeeding for the first 6 months.
- Introduction of safe and nutritious complementary foods at 6 months.
- Continued breastfeeding along with complementary feeding up to 2 years or beyond.
Types of Infant Foods
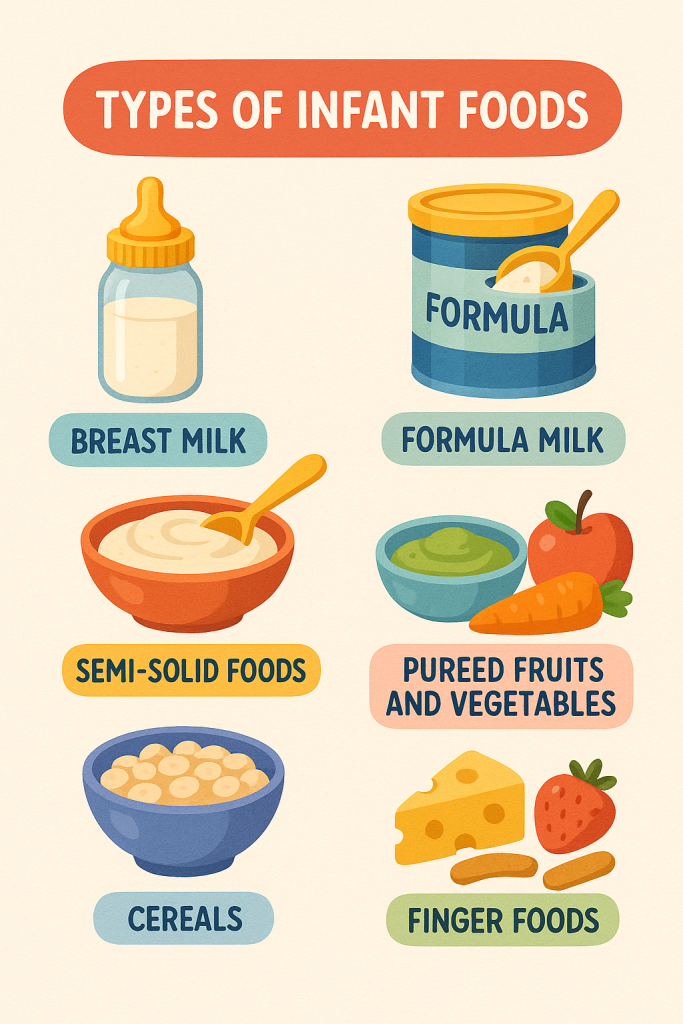
1. Breast Milk (0-6 Months) – The Ideal Infant Food
- Provides complete nutrition, including proteins, fats, carbohydrates, vitamins, and minerals.
- Contains antibodies that protect against infections.
- Supports brain development and digestion.
- Should be given on demand (8-12 times per day).
2. Infant Formula (When Breastfeeding Is Not Possible)
- Used in cases where breastfeeding is not possible or insufficient.
- Commercially prepared with essential nutrients like iron and DHA.
- Requires proper preparation (boiled water, sterilized bottles) to prevent infections.
| Formula Type | Use Case |
|---|---|
| Cow’s Milk-Based Formula | Standard option for most infants |
| Soy-Based Formula | For lactose-intolerant or cow milk-allergic babies |
| Hypoallergenic Formula | For infants with protein allergies |
| Preterm Infant Formula | For low birth weight babies needing extra nutrition |
3. Complementary Foods (6 Months Onward)
- Introduction of soft, mashed, and nutrient-dense foods along with continued breastfeeding.
- Must be iron-rich, easy to digest, and free from added salt/sugar.
- Gradual increase in variety, texture, and quantity over time.
Introduction of Complementary Feeding (Weaning Process)
At 6 months, babies require additional energy, iron, and vitamins, which breast milk alone cannot provide. Complementary feeding ensures healthy growth and development.
| Age Group | Consistency of Food | Meal Frequency |
|---|---|---|
| 6-8 Months | Mashed/pureed | 2-3 meals/day + breast milk |
| 9-12 Months | Soft, finely chopped | 3-4 meals/day + snacks |
| 12-24 Months | Family foods | 4 meals/day + 1-2 snacks |
Best First Foods for Infants (6-8 Months)
🔹 Iron-Rich Foods: Mashed lentils, pureed meat, egg yolk
🔹 Energy Foods: Soft rice, mashed banana, cooked oats
🔹 Vitamin-Rich Foods: Pureed carrots, sweet potatoes, pumpkin
🔹 Calcium-Rich Foods: Mashed paneer, yogurt
🔹 Healthy Fats: Avocado, ghee (small amounts)
Progression of Infant Foods by Age
Stage 1: 6-8 Months (Soft, Mashed Foods)
✅ Vegetable Purees: Carrots, pumpkin, spinach
✅ Fruit Purees: Banana, apple, pear
✅ Grain-Based Foods: Soft-cooked rice, dal, ragi porridge
✅ Protein Sources: Lentils, well-cooked egg yolk
🔸 Avoid: Whole nuts, honey (risk of botulism), cow’s milk as a main drink
Stage 2: 9-12 Months (Soft Finger Foods)
✅ Soft chapati, mashed potatoes, porridge
✅ Small pieces of boiled vegetables
✅ Dairy (cheese, yogurt, paneer)
✅ Well-cooked minced chicken, fish, eggs
🔸 Avoid: Hard foods (choking risk), excessive salt/sugar, processed foods
Stage 3: 12-24 Months (Family Foods)
✅ Well-cooked family meals in small pieces
✅ Whole grain foods (brown rice, wheat)
✅ Fruits and vegetables in natural form
✅ Healthy snacks (boiled eggs, fruit slices, roasted nuts in small amounts)
🔸 Avoid: Junk foods, excess sweets, aerated drinks
Guidelines for Safe Infant Feeding
1️⃣ Wash hands before preparing or feeding food.
2️⃣ Use boiled and cooled water for mixing foods.
3️⃣ Introduce one new food at a time (wait 3-5 days before introducing another).
4️⃣ No salt, sugar, or honey before 1 year.
5️⃣ Feed in a calm environment, encourage self-feeding.
6️⃣ Ensure proper hygiene of utensils (use a spoon/cup, not a bottle).
Homemade Infant Food Recipes
1. Rice & Lentil Porridge (Khichdi)
✅ Ingredients: 2 tbsp rice, 1 tbsp moong dal, ½ tsp ghee
✅ Method:
- Wash and cook rice and dal together with water.
- Mash well and add a drop of ghee before feeding.
2. Ragi Porridge
✅ Ingredients: 2 tbsp ragi flour, 1 cup water, ½ tsp jaggery
✅ Method:
- Cook ragi flour in water, stirring continuously.
- Add jaggery for sweetness (avoid sugar).
3. Mashed Banana with Yogurt
✅ Ingredients: 1 banana, 2 tbsp yogurt
✅ Method:
- Mash banana well and mix with yogurt.
- Serve fresh (do not store).
Foods to Avoid Before 1 Year
🚫 Honey (risk of botulism)
🚫 Salt & Sugar (kidney overload, unhealthy habits)
🚫 Cow’s Milk as a Drink (can cause iron deficiency)
🚫 Nuts & Popcorn (choking hazard)
🚫 Raw Eggs & Undercooked Meat (risk of infection)
Nutritional Benefits of Infant Foods
| Food Type | Key Nutrients | Benefits |
|---|---|---|
| Breast Milk | Proteins, DHA, Antibodies | Immunity, brain development |
| Lentils & Dal | Iron, Protein | Muscle and blood health |
| Vegetable Purees | Vitamins A, C | Vision, immunity |
| Fruit Purees | Fiber, Natural Sugars | Digestion, energy |
| Egg Yolk | Iron, DHA | Brain and nervous system |
| Ragi & Oats | Calcium, Iron | Bone health |
Common Infant Feeding Challenges & Solutions
| Issue | Cause | Solution |
|---|---|---|
| Refusing New Foods | Baby is unfamiliar with taste | Introduce gradually, mix with familiar food |
| Choking Risk | Large food pieces | Give soft, mashed, or small pieces |
| Constipation | Low fiber intake | Increase water, offer fruits like prunes, pears |
| Food Allergies | Sensitivity to dairy, eggs, wheat | Introduce allergenic foods one at a time |
| Underweight Baby | Low-calorie intake | Add ghee, banana, yogurt to meals |
Weaning & Transitioning to Family Foods
📌 Start introducing soft, mashed versions of family meals after 9-12 months.
📌 By 12-24 months, the child should eat the same meals as the family (with minimal modifications).
📌 Ensure adequate protein, iron, and healthy fats to support rapid growth.
📌 Encourage self-feeding with finger foods to develop fine motor skills.
Diet Plan and Nutritional Requirements for Infants (0-12 Months) – Full Details
Introduction
Infants (0-12 months) have unique nutritional needs as they undergo rapid growth and development. Proper nutrition in the first year ensures optimal brain development, immunity, and healthy weight gain. The primary source of nutrition for infants is breast milk or formula, followed by the gradual introduction of complementary foods after 6 months.
WHO & UNICEF Recommendations:
✅ Exclusive breastfeeding for the first 6 months (no water, no other foods).
✅ Introduction of safe, nutritious complementary foods at 6 months.
✅ Continued breastfeeding along with complementary feeding up to 2 years or beyond.
Nutritional Requirements for Infants (0-12 Months)
| Nutrient | 0-6 Months (Exclusive Breastfeeding) | 6-12 Months (Complementary Feeding + Breast Milk) |
|---|---|---|
| Energy | 500-550 kcal/day | 700-900 kcal/day |
| Protein | 9-11g/day | 13-15g/day |
| Fat | 30-35% of total energy | 30-40% of total energy |
| Carbohydrates | Primary source from lactose in breast milk | Introduce soft grains (rice, oats, wheat) |
| Iron | 0.27 mg/day (breast milk is sufficient) | 11 mg/day (iron-rich foods needed) |
| Calcium | 200 mg/day | 270 mg/day |
| Vitamin A | 400 mcg/day | 500 mcg/day |
| Vitamin D | 10 mcg (400 IU) | 10 mcg (400 IU) |
Diet Plan for Infants (0-6 Months) – Exclusive Breastfeeding
🔹 Breast milk is the ONLY recommended food and drink.
🔹 Feed on demand (every 2-3 hours, 8-12 times per day).
🔹 No additional water, sugar, honey, or formula unless prescribed by a doctor.
🔹 Colostrum (first milk) is essential for immunity.
Alternative for Non-Breastfed Babies
- Formula milk should be iron-fortified and prepared hygienically.
- Avoid cow’s milk as a primary drink before 1 year.
📌 Sample Feeding Schedule (0-6 Months)
| Time | Feeding |
|---|---|
| 6:00 AM | Breastfeeding |
| 9:00 AM | Breastfeeding |
| 12:00 PM | Breastfeeding |
| 3:00 PM | Breastfeeding |
| 6:00 PM | Breastfeeding |
| 9:00 PM | Breastfeeding |
| 12:00 AM | Night feeding |
| 3:00 AM | Night feeding |
Diet Plan for Infants (6-12 Months) – Introduction of Complementary Foods
🔹 Continue breastfeeding (at least 5-6 times per day).
🔹 Start with soft, mashed foods, then gradually introduce textures and finger foods.
🔹 Introduce iron-rich foods first (fortified cereals, lentils, mashed eggs).
🔹 Avoid salt, sugar, honey, and processed foods.
6-8 Months: First Foods (Mashed/Pureed)
📌 Meal Frequency: 2-3 times/day + 1 small snack
✅ Grain-Based Foods: Rice porridge, wheat porridge, ragi porridge
✅ Vegetable Purees: Carrots, pumpkin, potatoes
✅ Fruit Purees: Banana, apple, pear
✅ Protein Sources: Mashed dal, egg yolk, fish puree
✅ Dairy: Unsweetened yogurt, paneer
📌 Sample Feeding Schedule (6-8 Months)
| Time | Feeding |
|---|---|
| 6:00 AM | Breastfeeding |
| 9:00 AM | Mashed banana with yogurt |
| 12:00 PM | Rice & dal porridge + Breastfeeding |
| 3:00 PM | Steamed carrot puree |
| 6:00 PM | Oats porridge |
| 9:00 PM | Breastfeeding |
9-12 Months: Soft Finger Foods & Family Foods
📌 Meal Frequency: 3-4 meals/day + 1-2 snacks
✅ Protein-Rich Foods: Well-cooked eggs, minced chicken, soft fish
✅ Fruits & Vegetables: Sliced bananas, cooked peas, steamed broccoli
✅ Whole Grains: Soft chapati pieces, multigrain porridge
✅ Healthy Fats: Ghee in khichdi, nut powder in porridge
📌 Sample Feeding Schedule (9-12 Months)
| Time | Feeding |
|---|---|
| 6:00 AM | Breastfeeding |
| 9:00 AM | Scrambled egg + fruit |
| 12:00 PM | Soft chapati + dal + vegetable |
| 3:00 PM | Yogurt with mashed mango |
| 6:00 PM | Rice with chicken curry (soft) |
| 9:00 PM | Breastfeeding |
Best Foods for Infants (6-12 Months)
| Food Type | Examples | Nutrients Provided |
|---|---|---|
| Grains | Rice, oats, ragi, wheat | Carbohydrates, Fiber |
| Vegetables | Carrots, spinach, pumpkin | Vitamins A, C, Iron |
| Fruits | Banana, apple, pear | Natural Sugars, Fiber |
| Protein | Lentils, egg yolk, fish | Iron, Omega-3, Protein |
| Dairy | Yogurt, paneer, cheese | Calcium, Probiotics |
| Healthy Fats | Ghee, nuts (powdered), avocado | Brain Development |
Foods to Avoid Before 1 Year
🚫 Honey (Risk of botulism)
🚫 Salt & Sugar (Overloads immature kidneys)
🚫 Whole Nuts & Popcorn (Choking hazard)
🚫 Raw Eggs & Undercooked Meat (Bacterial infections)
🚫 Cow’s Milk as a Primary Drink (Iron-deficiency risk)
Common Infant Feeding Challenges & Solutions
| Challenge | Cause | Solution |
|---|---|---|
| Refusing New Foods | Baby is unfamiliar with the taste | Introduce gradually, mix with breast milk |
| Choking Risk | Large food pieces | Offer soft, mashed foods |
| Constipation | Low fiber, inadequate fluids | Increase fruits (prunes, pears), water intake |
| Allergic Reactions | Sensitivity to eggs, dairy, nuts | Introduce allergenic foods one at a time |
| Underweight Baby | Insufficient calorie intake | Add ghee, banana, yogurt to meals |
Transition to Family Foods (After 12 Months)
📌 By 12 months, the child should be eating nutrient-rich, home-cooked meals.
📌 Ensure sufficient protein, iron, and healthy fats for continued growth.
📌 Encourage self-feeding with soft, chopped family foods.
📌 Avoid spicy, highly processed, or junk foods.
Diet Plan and Nutritional Requirements for Toddlers (1-3 Years).
Introduction
The toddler stage (1-3 years) is a period of rapid physical and cognitive growth, requiring proper nutrition to support development, immunity, and activity levels. This is also the stage where children develop eating habits, making it crucial to introduce a balanced diet rich in essential nutrients.
✅ Energy-dense foods for growth and play.
✅ Balanced meals with proteins, carbohydrates, fats, vitamins, and minerals.
✅ Encouraging self-feeding and healthy eating habits.
✅ Avoiding processed and sugary foods to prevent obesity and nutrient deficiencies.
Nutritional Requirements for Toddlers (1-3 Years)
| Nutrient | Recommended Daily Intake | Sources |
|---|---|---|
| Energy | 1000-1400 kcal/day | Whole grains, fruits, dairy |
| Protein | 13-15g/day | Eggs, lentils, milk, fish |
| Carbohydrates | 130g/day | Rice, wheat, oats, potatoes |
| Fats | 30-40% of total energy | Ghee, nuts, avocado |
| Calcium | 700 mg/day | Milk, cheese, yogurt |
| Iron | 7 mg/day | Leafy greens, eggs, chicken |
| Vitamin A | 400 mcg/day | Carrots, mangoes, spinach |
| Vitamin C | 15 mg/day | Citrus fruits, tomatoes |
| Fiber | 19g/day | Whole grains, vegetables, fruits |
| Water | 1-1.5 liters/day | Plain water, fresh juices |
Balanced Diet Plan for Toddlers (1-3 Years)
A toddler’s diet should be nutrient-dense, balanced, and diverse, including grains, proteins, dairy, fruits, vegetables, and healthy fats.
1. Ideal Meal Frequency for Toddlers
📌 Three main meals + 2-3 snacks per day.
📌 Portion size should be small but frequent to match a toddler’s small stomach.
| Meal | Time | Purpose |
|---|---|---|
| Breakfast | 7:30 – 8:30 AM | Provides energy for the day |
| Mid-Morning Snack | 10:00 – 11:00 AM | Prevents hunger, improves digestion |
| Lunch | 12:30 – 1:30 PM | Main balanced meal |
| Evening Snack | 4:00 – 5:00 PM | Provides sustained energy |
| Dinner | 7:00 – 8:00 PM | Light and nutritious meal |
2. Sample Diet Plan for Toddlers
📌 Day 1
| Meal | Food Suggestions |
|---|---|
| Breakfast | Whole wheat toast + scrambled eggs + milk |
| Mid-Morning Snack | Banana slices + yogurt |
| Lunch | Soft chapati + dal + mashed vegetables |
| Evening Snack | Homemade fruit smoothie |
| Dinner | Rice + soft-cooked fish + steamed carrots |
📌 Day 2
| Meal | Food Suggestions |
|---|---|
| Breakfast | Ragi porridge + almonds |
| Mid-Morning Snack | Cottage cheese cubes + orange juice |
| Lunch | Multigrain roti + paneer curry + cucumber |
| Evening Snack | Mashed sweet potato with butter |
| Dinner | Brown rice + curd + mashed peas |
📌 Day 3
| Meal | Food Suggestions |
|---|---|
| Breakfast | Oats porridge + chopped apple |
| Mid-Morning Snack | Whole wheat crackers + peanut butter |
| Lunch | Soft khichdi + carrot sticks |
| Evening Snack | Roasted makhana (fox nuts) |
| Dinner | Chapati + dal + spinach |
3. Key Food Groups for Toddlers
A toddler’s diet should include variety and balanced portions from all food groups.
| Food Group | Examples | Function |
|---|---|---|
| Grains & Cereals | Rice, wheat, oats, ragi, quinoa | Energy & fiber |
| Proteins | Eggs, lentils, fish, chicken, nuts | Growth & muscle development |
| Dairy | Milk, yogurt, cheese | Bone development |
| Vegetables | Carrots, spinach, pumpkin | Vitamins & fiber |
| Fruits | Banana, apple, mango | Natural sugars & minerals |
| Healthy Fats | Ghee, nuts, avocado, olive oil | Brain development |
4. Important Feeding Tips for Toddlers
🔹 Encourage self-feeding – Helps with motor skills and independence.
🔹 Introduce one new food at a time – To identify allergies.
🔹 Avoid distractions during meals – No TV or mobile while eating.
🔹 Be patient with fussy eaters – Offer variety, do not force-feed.
🔹 Ensure proper hydration – Give plain water instead of sugary drinks.
5. Foods to Avoid for Toddlers
🚫 High-Sugar Foods – Candies, sodas, chocolates (risk of obesity, diabetes).
🚫 Excess Salt – Chips, packaged snacks (harms kidney health).
🚫 Processed & Junk Foods – Burgers, fries (low in nutrients, high in unhealthy fats).
🚫 Nuts & Popcorn (Whole) – Choking hazard, serve in crushed form.
🚫 Raw Honey – Risk of botulism infection.
🚫 Caffeinated Drinks – No tea, coffee, or soft drinks.
6. Common Nutritional Deficiencies in Toddlers & Prevention
| Deficiency | Symptoms | Food Sources |
|---|---|---|
| Iron Deficiency (Anemia) | Weakness, pale skin | Eggs, spinach, lentils, chicken |
| Calcium Deficiency | Weak bones, slow growth | Dairy, sesame seeds, tofu |
| Vitamin D Deficiency | Rickets, weak muscles | Sunlight, fish, fortified milk |
| Protein Deficiency | Poor weight gain, delayed growth | Paneer, yogurt, eggs, nuts |
7. Common Toddler Eating Problems & Solutions
| Problem | Cause | Solution |
|---|---|---|
| Fussy Eating | Preference for specific foods | Offer variety, make food fun (shapes, colors) |
| Not Eating Enough | Small appetite | Small, frequent meals, avoid force-feeding |
| Choking Risk | Large food pieces | Cut food into small pieces, supervise eating |
| Refusing Vegetables | Strong taste | Mix in soups, parathas, or smoothies |
| Food Allergies | Reaction to dairy, nuts, eggs | Introduce allergens one at a time, consult a doctor |
8. Transition to Family Foods (After 2 Years)
📌 By age 2, toddlers should be eating similar foods as the family.
📌 Ensure meals are soft-textured, nutrient-dense, and portion-controlled.
📌 Encourage self-feeding with child-friendly utensils.
📌 Avoid spicy, deep-fried, and overly processed foods.
Diet Plan and Nutritional Requirements for School-Going Children (4-12 Years).
Introduction
The school-age period (4-12 years) is a crucial stage for physical growth, brain development, and immune strengthening. Proper nutrition supports learning, concentration, physical activity, and overall well-being. During this stage, children develop food habits, making it essential to introduce healthy eating practices that prevent malnutrition, obesity, and lifestyle diseases.
✅ Balanced diet with essential nutrients for growth and learning.
✅ Healthy eating habits to prevent junk food addiction.
✅ Adequate hydration and portion-controlled meals.
✅ Nutrient-dense meals for strong immunity and brain function.
Nutritional Requirements for School-Going Children (4-12 Years)
| Nutrient | 4-6 Years | 7-9 Years | 10-12 Years | Sources |
|---|---|---|---|---|
| Energy | 1300-1600 kcal/day | 1600-1900 kcal/day | 1800-2200 kcal/day | Whole grains, fruits, dairy |
| Protein | 16-20g/day | 20-30g/day | 30-40g/day | Eggs, lentils, fish, paneer |
| Carbohydrates | 150-200g/day | 200-250g/day | 250-300g/day | Rice, wheat, oats, potatoes |
| Fats | 25-30% of total energy | 25-30% of total energy | 25-30% of total energy | Ghee, nuts, avocado, olive oil |
| Calcium | 600 mg/day | 700 mg/day | 1000 mg/day | Milk, cheese, yogurt, ragi |
| Iron | 10 mg/day | 12 mg/day | 15 mg/day | Leafy greens, eggs, chicken |
| Vitamin A | 500 mcg/day | 600 mcg/day | 700 mcg/day | Carrots, mangoes, spinach |
| Vitamin C | 25 mg/day | 30 mg/day | 40 mg/day | Citrus fruits, tomatoes |
| Fiber | 19g/day | 20g/day | 25g/day | Whole grains, vegetables, fruits |
| Water | 1.5 liters/day | 1.8 liters/day | 2 liters/day | Plain water, fresh juices |
Balanced Diet Plan for School-Going Children
A school-going child’s diet should include all essential food groups in appropriate portions.
1. Ideal Meal Frequency for School-Going Children
📌 Three main meals + 2 healthy snacks per day
📌 Portion sizes should be adjusted as per activity levels
| Meal | Time | Purpose |
|---|---|---|
| Breakfast | 7:00 – 8:00 AM | Provides energy for school |
| Mid-Morning Snack | 10:00 – 11:00 AM | Boosts metabolism & prevents hunger |
| Lunch | 12:30 – 1:30 PM | Main balanced meal for growth |
| Evening Snack | 4:00 – 5:00 PM | Provides energy for activities/homework |
| Dinner | 7:30 – 8:30 PM | Light, nutritious meal for recovery |
2. Sample Diet Plan for School-Going Children
📌 Day 1
| Meal | Food Suggestions |
|---|---|
| Breakfast | Whole wheat bread + peanut butter + milk |
| Mid-Morning Snack | Banana slices + yogurt |
| Lunch | Rice + dal + vegetable curry + paneer |
| Evening Snack | Roasted makhana + fresh juice |
| Dinner | Soft chapati + chicken curry + cucumber salad |
📌 Day 2
| Meal | Food Suggestions |
|---|---|
| Breakfast | Vegetable upma + almonds + milk |
| Mid-Morning Snack | Cheese cubes + orange juice |
| Lunch | Brown rice + rajma + mixed vegetables |
| Evening Snack | Mashed sweet potato with butter |
| Dinner | Roti + fish curry + boiled spinach |
📌 Day 3
| Meal | Food Suggestions |
|---|---|
| Breakfast | Oats porridge + chopped apple |
| Mid-Morning Snack | Whole wheat crackers + homemade hummus |
| Lunch | Khichdi + curd + carrot sticks |
| Evening Snack | Nuts + buttermilk |
| Dinner | Chapati + dal + sautéed vegetables |
3. Key Food Groups for School-Going Children
A child’s diet should be nutrient-dense, balanced, and diverse.
| Food Group | Examples | Function |
|---|---|---|
| Grains & Cereals | Brown rice, wheat, oats, ragi, quinoa | Energy & fiber |
| Proteins | Eggs, lentils, fish, chicken, paneer | Growth & muscle development |
| Dairy | Milk, yogurt, cheese | Bone development |
| Vegetables | Carrots, spinach, pumpkin | Vitamins & fiber |
| Fruits | Banana, apple, mango | Natural sugars & minerals |
| Healthy Fats | Ghee, nuts, avocado, olive oil | Brain development |
4. Important Feeding Tips for School-Going Children
🔹 Encourage balanced meals – Teach portion control and food variety.
🔹 Limit processed foods and sugary snacks – Prevents obesity and diabetes.
🔹 Ensure proper hydration – Provide enough water, avoid aerated drinks.
🔹 Make meals enjoyable – Present food in colorful and appealing ways.
🔹 Encourage physical activity – Diet should be paired with exercise.
5. Foods to Avoid for School-Going Children
🚫 Sugary Snacks – Candies, cakes, chocolates (risk of obesity, diabetes).
🚫 Excess Salt – Packaged chips, instant noodles (risk of high BP).
🚫 Fried & Junk Foods – Burgers, fries, pizza (low in nutrients, high in fats).
🚫 Soft Drinks & Artificial Juices – High in sugar, causes dental issues.
6. Common Nutritional Deficiencies in School-Going Children & Prevention
| Deficiency | Symptoms | Food Sources |
|---|---|---|
| Iron Deficiency (Anemia) | Fatigue, poor concentration | Spinach, eggs, nuts, meat |
| Calcium Deficiency | Weak bones, slow growth | Milk, cheese, sesame seeds |
| Vitamin D Deficiency | Weak immunity, rickets | Sunlight, fish, fortified milk |
| Protein Deficiency | Weak muscles, slow growth | Paneer, yogurt, lentils, eggs |
7. Common Eating Problems in School-Going Children & Solutions
| Problem | Cause | Solution |
|---|---|---|
| Skipping Breakfast | Lack of time, poor appetite | Give easy-to-eat foods (fruits, milk, smoothies) |
| Picky Eating | Preference for junk food | Introduce foods creatively (shapes, colors) |
| Low Water Intake | Preference for sugary drinks | Offer flavored water, fruit-infused water |
| Overeating Junk Food | Easy availability | Replace with healthy snacks (nuts, fruits, yogurt) |
8. Transition to Healthy Eating Habits
📌 Encourage home-cooked meals instead of processed foods.
📌 Teach children about balanced nutrition through storytelling or activities.
📌 Make healthy food exciting (e.g., fun lunchbox ideas, colorful plates).
📌 Monitor portion sizes to prevent overeating.
Diet Plan and Nutritional Requirements for Adolescents (13-18 Years)
Introduction
Adolescence (13-18 years) is a critical period of growth and development where the body undergoes rapid physical, hormonal, and cognitive changes. Proper nutrition is essential to:
✅ Support rapid growth and puberty-related changes.
✅ Enhance cognitive function and academic performance.
✅ Prevent nutritional deficiencies and eating disorders.
✅ Reduce the risk of obesity and lifestyle diseases.
Nutritional Requirements for Adolescents (13-18 Years)
| Nutrient | Boys (13-18 Years) | Girls (13-18 Years) | Sources |
|---|---|---|---|
| Energy | 2500-2800 kcal/day | 2000-2200 kcal/day | Whole grains, fruits, dairy |
| Protein | 45-55g/day | 40-50g/day | Eggs, lentils, fish, paneer |
| Carbohydrates | 300-400g/day | 250-350g/day | Rice, wheat, oats, potatoes |
| Fats | 25-30% of total energy | 25-30% of total energy | Ghee, nuts, avocado, olive oil |
| Calcium | 1300 mg/day | 1300 mg/day | Milk, cheese, yogurt, ragi |
| Iron | 11 mg/day | 15 mg/day | Leafy greens, eggs, chicken |
| Vitamin A | 900 mcg/day | 700 mcg/day | Carrots, mangoes, spinach |
| Vitamin C | 75 mg/day | 65 mg/day | Citrus fruits, tomatoes |
| Fiber | 25-30g/day | 25-30g/day | Whole grains, vegetables, fruits |
| Water | 2.5-3 liters/day | 2-2.5 liters/day | Plain water, fresh juices |
Key Nutritional Concerns in Adolescence
📌 Increased need for calcium and vitamin D for bone development.
📌 Higher protein intake for muscle growth, especially for active teens.
📌 Iron-rich diet for girls to prevent anemia due to menstruation.
📌 Balancing energy intake to prevent obesity or malnutrition.
Balanced Diet Plan for Adolescents
1. Ideal Meal Frequency for Adolescents
📌 Three main meals + 2 healthy snacks per day.
📌 Ensure proper balance of macronutrients (carbs, proteins, fats).
| Meal | Time | Purpose |
|---|---|---|
| Breakfast | 7:00 – 8:00 AM | Provides energy for the day |
| Mid-Morning Snack | 10:00 – 11:00 AM | Prevents hunger, boosts metabolism |
| Lunch | 12:30 – 1:30 PM | Main balanced meal |
| Evening Snack | 4:00 – 5:00 PM | Provides energy for studies/sports |
| Dinner | 7:30 – 8:30 PM | Light and nutritious meal for recovery |
2. Sample Diet Plan for Adolescents (13-18 Years)
📌 Day 1
| Meal | Food Suggestions |
|---|---|
| Breakfast | Scrambled eggs + whole wheat toast + milk |
| Mid-Morning Snack | Apple + almonds |
| Lunch | Brown rice + dal + vegetable curry + chicken |
| Evening Snack | Greek yogurt + berries |
| Dinner | Roti + paneer bhurji + cucumber salad |
📌 Day 2
| Meal | Food Suggestions |
|---|---|
| Breakfast | Oats porridge + banana + walnuts |
| Mid-Morning Snack | Whole wheat crackers + peanut butter |
| Lunch | Quinoa salad + grilled fish + steamed broccoli |
| Evening Snack | Sprouts chaat + buttermilk |
| Dinner | Chapati + moong dal + sautéed spinach |
📌 Day 3
| Meal | Food Suggestions |
|---|---|
| Breakfast | Ragi dosa + coconut chutney |
| Mid-Morning Snack | Cottage cheese cubes + orange juice |
| Lunch | Whole wheat roti + rajma + mixed vegetables |
| Evening Snack | Mashed sweet potato with butter |
| Dinner | Rice + lentil soup + curd |
3. Key Food Groups for Adolescents
| Food Group | Examples | Function |
|---|---|---|
| Grains & Cereals | Brown rice, wheat, oats, quinoa | Energy & fiber |
| Proteins | Eggs, lentils, fish, chicken, paneer | Growth & muscle development |
| Dairy | Milk, yogurt, cheese | Bone development |
| Vegetables | Carrots, spinach, broccoli | Vitamins & fiber |
| Fruits | Banana, apple, mango | Natural sugars & minerals |
| Healthy Fats | Ghee, nuts, avocado, olive oil | Brain development |
4. Important Feeding Tips for Adolescents
🔹 Encourage balanced meals – Teach portion control and food variety.
🔹 Avoid excessive junk food and sugary drinks – Prevents obesity, diabetes.
🔹 Ensure proper hydration – 2.5-3 liters of water daily.
🔹 Promote home-cooked meals – Reduces unhealthy eating habits.
🔹 Include protein-rich foods – Supports muscle growth and fitness.
5. Foods to Avoid for Adolescents
🚫 High-Sugar Snacks – Candies, sodas, chocolates (risk of obesity, diabetes).
🚫 Fast Foods – Pizza, burgers, fries (low in nutrients, high in fats).
🚫 Soft Drinks & Energy Drinks – High sugar content, harmful for health.
🚫 Packaged Chips & Instant Noodles – Loaded with sodium and preservatives.
🚫 Processed Meats – Sausages, salami, hot dogs (high in unhealthy fats).
6. Common Nutritional Deficiencies in Adolescents & Prevention
| Deficiency | Symptoms | Food Sources |
|---|---|---|
| Iron Deficiency (Anemia) | Fatigue, weakness, pale skin | Spinach, eggs, nuts, meat |
| Calcium Deficiency | Weak bones, slow growth | Milk, cheese, sesame seeds |
| Vitamin D Deficiency | Weak immunity, joint pain | Sunlight, fish, fortified milk |
| Protein Deficiency | Poor muscle development, hair loss | Paneer, yogurt, lentils, eggs |
7. Common Eating Problems in Adolescents & Solutions
| Problem | Cause | Solution |
|---|---|---|
| Skipping Breakfast | Lack of time, poor appetite | Quick meals (fruit, milk, smoothie) |
| Unhealthy Snacking | Easy availability of junk food | Stock healthy snacks (nuts, yogurt) |
| Excessive Dieting | Peer pressure, body image issues | Educate about balanced nutrition |
| Emotional Eating | Stress, anxiety | Encourage physical activity, hobbies |
8. Transition to Healthy Eating Habits
📌 Encourage home-cooked meals instead of fast food.
📌 Teach adolescents about portion control and nutrient balance.
📌 Make healthy food exciting (e.g., colorful plates, smoothie bowls).
📌 Monitor eating patterns and educate about long-term health.
Diet Plan and Nutritional Requirements for the Elderly (60+ Years)
Introduction
Aging brings physiological, metabolic, and functional changes that affect nutritional needs, digestion, and metabolism. A well-balanced diet is essential to:
✅ Maintain muscle mass and prevent weakness.
✅ Boost immunity and prevent infections.
✅ Support digestion and prevent constipation.
✅ Manage chronic diseases (diabetes, hypertension, osteoporosis).
✅ Maintain cognitive health and mental well-being.
Nutritional Requirements for the Elderly (60+ Years)
| Nutrient | Daily Requirement | Sources |
|---|---|---|
| Energy | 1600-2000 kcal/day | Whole grains, fruits, dairy |
| Protein | 50-60g/day | Eggs, lentils, fish, paneer |
| Carbohydrates | 150-200g/day | Rice, wheat, oats, potatoes |
| Fats | 20-25% of total energy | Ghee, nuts, avocado, olive oil |
| Calcium | 1200 mg/day | Milk, cheese, yogurt, ragi |
| Iron | 8-10 mg/day | Leafy greens, eggs, chicken |
| Vitamin A | 600-700 mcg/day | Carrots, mangoes, spinach |
| Vitamin C | 75-90 mg/day | Citrus fruits, tomatoes |
| Vitamin D | 15-20 mcg (600-800 IU) | Sunlight, dairy, fish oil |
| Fiber | 25-30g/day | Whole grains, vegetables, fruits |
| Water | 2-2.5 liters/day | Plain water, fresh juices |
Key Nutritional Concerns in Elderly
📌 Increased need for calcium and vitamin D to prevent osteoporosis.
📌 Higher protein intake to maintain muscle strength and prevent sarcopenia.
📌 High-fiber diet to prevent constipation and improve digestion.
📌 Lower calorie intake due to decreased metabolism and activity levels.
Balanced Diet Plan for the Elderly
1. Ideal Meal Frequency for the Elderly
📌 Three main meals + 2 healthy snacks per day.
📌 Easy-to-digest foods with soft texture and high fiber content.
| Meal | Time | Purpose |
|---|---|---|
| Breakfast | 7:00 – 8:00 AM | Provides energy for the day |
| Mid-Morning Snack | 10:00 – 11:00 AM | Prevents hunger, boosts metabolism |
| Lunch | 12:30 – 1:30 PM | Main balanced meal |
| Evening Snack | 4:00 – 5:00 PM | Provides energy for evening activities |
| Dinner | 7:30 – 8:30 PM | Light and nutritious meal for easy digestion |
2. Sample Diet Plan for the Elderly (60+ Years)
📌 Day 1
| Meal | Food Suggestions |
|---|---|
| Breakfast | Oats porridge + almonds + milk |
| Mid-Morning Snack | Banana + walnuts |
| Lunch | Soft chapati + dal + spinach curry |
| Evening Snack | Roasted makhana + buttermilk |
| Dinner | Brown rice + curd + steamed vegetables |
📌 Day 2
| Meal | Food Suggestions |
|---|---|
| Breakfast | Ragi porridge + boiled egg |
| Mid-Morning Snack | Cottage cheese cubes + fresh orange juice |
| Lunch | Whole wheat roti + moong dal + carrot-beetroot salad |
| Evening Snack | Mashed sweet potato with butter |
| Dinner | Khichdi + curd + sautéed broccoli |
📌 Day 3
| Meal | Food Suggestions |
|---|---|
| Breakfast | Scrambled eggs + multigrain toast + green tea |
| Mid-Morning Snack | Fruit smoothie with yogurt |
| Lunch | Soft millet roti + lentil soup + sautéed vegetables |
| Evening Snack | Nuts + herbal tea |
| Dinner | Rice + paneer curry + cucumber salad |
3. Key Food Groups for the Elderly
| Food Group | Examples | Function |
|---|---|---|
| Grains & Cereals | Brown rice, wheat, oats, ragi, quinoa | Energy & fiber |
| Proteins | Eggs, lentils, fish, chicken, paneer | Muscle maintenance |
| Dairy | Milk, yogurt, cheese | Bone health |
| Vegetables | Carrots, spinach, broccoli | Vitamins & fiber |
| Fruits | Banana, apple, mango | Natural sugars & minerals |
| Healthy Fats | Ghee, nuts, avocado, olive oil | Brain function & joint health |
4. Important Feeding Tips for the Elderly
🔹 Encourage smaller, frequent meals – Prevents bloating and indigestion.
🔹 Ensure proper hydration – 2-2.5 liters of water daily.
🔹 Include high-fiber foods – Prevents constipation.
🔹 Limit processed foods and excess salt – Reduces hypertension risk.
🔹 Soft-textured foods for easy chewing and digestion.
5. Foods to Avoid for the Elderly
🚫 High-Sodium Foods – Processed snacks, pickles, instant noodles (risk of high BP).
🚫 Sugary Foods & Refined Carbs – Sweets, pastries, white bread (risk of diabetes).
🚫 Fried & Junk Foods – Burgers, fries, deep-fried snacks (high in trans fats).
🚫 Caffeinated Beverages – Excess tea, coffee (causes dehydration, acidity).
🚫 Red Meat & Processed Meats – Sausages, hot dogs (high in saturated fat).
6. Common Nutritional Deficiencies in the Elderly & Prevention
| Deficiency | Symptoms | Food Sources |
|---|---|---|
| Iron Deficiency (Anemia) | Fatigue, pale skin, dizziness | Spinach, eggs, nuts, meat |
| Calcium Deficiency | Weak bones, osteoporosis | Milk, cheese, sesame seeds |
| Vitamin D Deficiency | Joint pain, weak immunity | Sunlight, fish, fortified milk |
| Protein Deficiency | Muscle loss, fatigue | Paneer, yogurt, lentils, eggs |
7. Common Eating Problems in the Elderly & Solutions
| Problem | Cause | Solution |
|---|---|---|
| Loss of Appetite | Reduced taste sensitivity | Add herbs/spices for flavor, smaller meals |
| Chewing Difficulty | Tooth problems | Use soft, mashed foods |
| Constipation | Low fiber intake | Increase fruits, vegetables, and water |
| Weak Digestion | Reduced enzyme production | Eat light, avoid spicy/oily food |
| Dehydration | Low water intake | Encourage sipping fluids throughout the day |
8. Transition to Healthy Eating Habits
📌 Encourage home-cooked meals instead of processed foods.
📌 Teach portion control to avoid overeating.
📌 Make healthy food choices a habit by including variety.
📌 Ensure social interaction during meals for mental well-being.
Diet in Pregnancy: Nutritional Requirements and Balanced Diet Plan
Introduction
Pregnancy is a crucial period that requires optimal nutrition to support the health of the mother and developing baby. A balanced diet ensures:
✅ Healthy fetal growth and development
✅ Reduced risk of birth defects and complications
✅ Strong maternal immunity and energy levels
✅ Proper weight gain and postpartum recovery
Nutritional Requirements During Pregnancy
| Nutrient | Daily Requirement | Function | Food Sources |
|---|---|---|---|
| Energy | 2200-2500 kcal/day | Supports fetal growth & maternal health | Whole grains, dairy, nuts |
| Protein | 60-80g/day | Builds fetal tissues & placenta | Eggs, lentils, fish, dairy |
| Carbohydrates | 175-200g/day | Provides energy for mother & baby | Rice, wheat, oats, potatoes |
| Fats | 25-30% of total energy | Supports brain & nervous system | Avocado, nuts, olive oil |
| Calcium | 1000-1200 mg/day | Bone & teeth formation | Milk, cheese, yogurt, ragi |
| Iron | 27 mg/day | Prevents anemia & ensures oxygen supply | Spinach, eggs, chicken |
| Folic Acid | 600 mcg/day | Prevents neural tube defects | Green leafy vegetables, citrus fruits |
| Vitamin A | 770 mcg/day | Eye & immune development | Carrots, mangoes, pumpkin |
| Vitamin C | 85 mg/day | Boosts immunity & iron absorption | Citrus fruits, tomatoes |
| Vitamin D | 15 mcg (600 IU) | Calcium absorption & bone health | Sunlight, dairy, fish oil |
| Fiber | 28-30g/day | Prevents constipation & supports digestion | Whole grains, vegetables, fruits |
| Water | 2.5-3 liters/day | Hydration, amniotic fluid maintenance | Plain water, fresh juices |
Key Nutritional Concerns in Pregnancy
📌 Increased need for iron and folic acid to prevent anemia and birth defects.
📌 Higher calcium and vitamin D intake for fetal bone development.
📌 Balanced protein intake to support fetal growth and maternal tissue repair.
📌 Adequate fiber intake to prevent constipation.
Balanced Diet Plan for Pregnancy
1. Ideal Meal Frequency During Pregnancy
📌 Three main meals + 2-3 healthy snacks per day.
📌 Frequent, small meals to prevent nausea, heartburn, and indigestion.
| Meal | Time | Purpose |
|---|---|---|
| Breakfast | 7:30 – 8:30 AM | Provides energy for the day |
| Mid-Morning Snack | 10:00 – 11:00 AM | Boosts metabolism & prevents nausea |
| Lunch | 12:30 – 1:30 PM | Main balanced meal |
| Evening Snack | 4:00 – 5:00 PM | Provides energy for physical activity |
| Dinner | 7:30 – 8:30 PM | Light and nutritious meal for digestion |
2. Sample Diet Plan for Pregnancy (Balanced Meal Plan)
📌 Day 1
| Meal | Food Suggestions |
|---|---|
| Breakfast | Oats porridge + almonds + milk |
| Mid-Morning Snack | Banana + yogurt |
| Lunch | Soft chapati + dal + spinach curry |
| Evening Snack | Roasted makhana + buttermilk |
| Dinner | Brown rice + curd + steamed vegetables |
📌 Day 2
| Meal | Food Suggestions |
|---|---|
| Breakfast | Ragi porridge + boiled egg |
| Mid-Morning Snack | Cottage cheese cubes + fresh orange juice |
| Lunch | Whole wheat roti + moong dal + carrot-beetroot salad |
| Evening Snack | Mashed sweet potato with butter |
| Dinner | Khichdi + curd + sautéed broccoli |
📌 Day 3
| Meal | Food Suggestions |
|---|---|
| Breakfast | Scrambled eggs + multigrain toast + green tea |
| Mid-Morning Snack | Fruit smoothie with yogurt |
| Lunch | Soft millet roti + lentil soup + sautéed vegetables |
| Evening Snack | Nuts + herbal tea |
| Dinner | Rice + paneer curry + cucumber salad |
3. Key Food Groups for Pregnancy
| Food Group | Examples | Function |
|---|---|---|
| Grains & Cereals | Brown rice, wheat, oats, ragi, quinoa | Energy & fiber |
| Proteins | Eggs, lentils, fish, chicken, paneer | Muscle & fetal development |
| Dairy | Milk, yogurt, cheese | Bone & teeth formation |
| Vegetables | Carrots, spinach, broccoli | Vitamins & fiber |
| Fruits | Banana, apple, mango | Natural sugars & minerals |
| Healthy Fats | Ghee, nuts, avocado, olive oil | Brain & nervous system development |
4. Important Feeding Tips for Pregnancy
🔹 Eat small, frequent meals – Prevents nausea and heartburn.
🔹 Ensure proper hydration – 2.5-3 liters of water daily.
🔹 Include high-fiber foods – Prevents constipation.
🔹 Limit processed foods and excess salt – Reduces swelling and hypertension risk.
🔹 Consume foods rich in iron and folic acid to prevent anemia.
5. Foods to Avoid During Pregnancy
🚫 Raw & Undercooked Meats – Risk of infections like toxoplasmosis.
🚫 Unpasteurized Dairy & Soft Cheeses – Risk of listeria infection.
🚫 Excess Caffeine – Can affect fetal growth, limit to 200mg/day.
🚫 Alcohol & Smoking – Causes fetal growth retardation and birth defects.
🚫 Excess Salt & Processed Foods – Risk of high blood pressure and swelling.
🚫 Raw Eggs & Sushi – Risk of bacterial infections.
6. Common Nutritional Deficiencies in Pregnancy & Prevention
| Deficiency | Symptoms | Food Sources |
|---|---|---|
| Iron Deficiency (Anemia) | Fatigue, dizziness, pale skin | Spinach, eggs, nuts, meat |
| Calcium Deficiency | Weak bones, muscle cramps | Milk, cheese, sesame seeds |
| Vitamin D Deficiency | Weak immunity, joint pain | Sunlight, fish, fortified milk |
| Folic Acid Deficiency | Neural tube defects in baby | Green leafy vegetables, lentils |
7. Common Eating Problems in Pregnancy & Solutions
| Problem | Cause | Solution |
|---|---|---|
| Morning Sickness | Hormonal changes | Eat small, dry snacks (crackers) |
| Heartburn | Acid reflux due to pregnancy hormones | Avoid spicy, fried foods; eat small meals |
| Constipation | Slow digestion | Increase fiber & water intake |
| Gestational Diabetes | High sugar levels | Avoid refined carbs, choose whole grains |
8. Transition to Postpartum Nutrition
📌 Continue a high-protein, calcium-rich diet to support breastfeeding.
📌 Increase hydration and fiber intake to aid postpartum recovery.
📌 Consume iron-rich foods to replenish blood loss after delivery.
📌 Include healthy fats to support brain development of the newborn.
Conclusion
A well-balanced diet during pregnancy ensures healthy fetal development, proper weight gain, and reduced pregnancy complications. By focusing on proteins, calcium, iron, vitamins, and fiber, expectant mothers can ensure optimal health for themselves and their baby.
Key Takeaways:
✅ Three main meals + 2-3 healthy snacks daily with variety.
✅ Consume nutrient-rich foods, limit junk food intake.
✅ Ensure adequate protein, calcium, iron, and folic acid.
✅ Promote hydration, digestion, and an active lifestyle.
By following these nutritional guidelines and meal plans, pregnant women can ensure a safe and healthy pregnancy! 🤰🥗💪
Anemia in Pregnancy
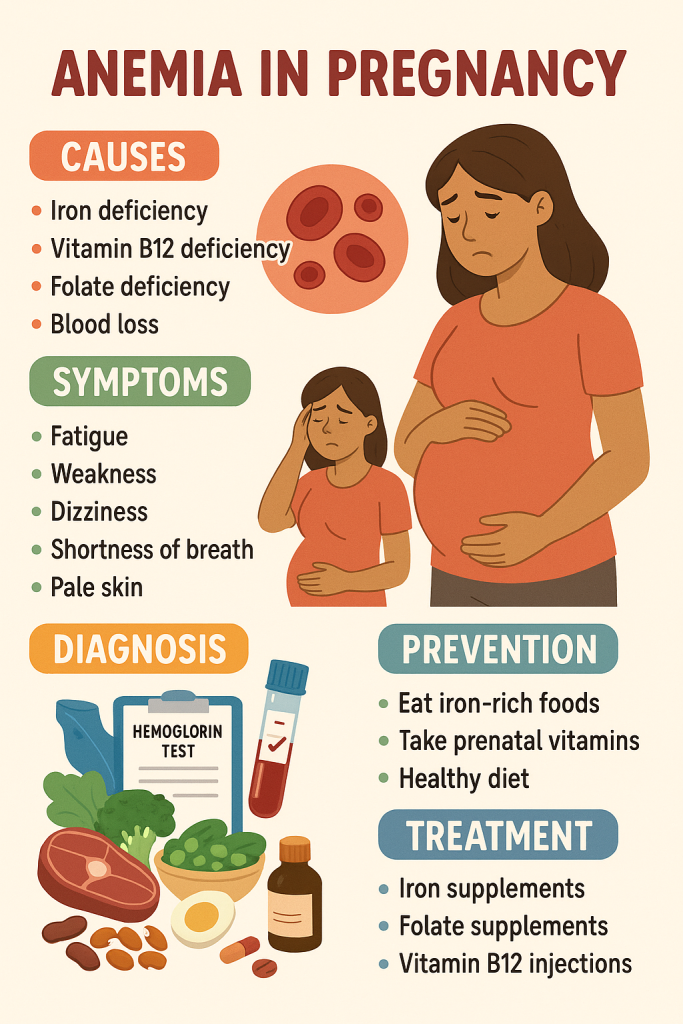
Introduction
Anemia during pregnancy is a condition where the hemoglobin (Hb) level drops below 11 g/dL, leading to fatigue, weakness, and complications for both the mother and the baby. Iron-deficiency anemia is the most common type, but folic acid and vitamin B12 deficiencies can also cause anemia.
Types of Anemia in Pregnancy
- Iron-Deficiency Anemia – Low iron levels lead to reduced hemoglobin production.
- Folate-Deficiency Anemia – Low folic acid affects red blood cell formation.
- Vitamin B12-Deficiency Anemia – Poor absorption of vitamin B12 affects red blood cell formation.
- Hemolytic Anemia – Premature destruction of red blood cells.
Normal Hemoglobin Levels in Pregnancy:
- 1st Trimester: ≥11 g/dL
- 2nd Trimester: ≥10.5 g/dL
- 3rd Trimester: ≥11 g/dL
Diagnosis of Anemia in Pregnancy
1. Symptoms of Anemia in Pregnancy
✅ Fatigue, weakness, dizziness
✅ Pale skin, lips, and nails
✅ Shortness of breath, rapid heartbeat
✅ Cold hands and feet
✅ Headaches, difficulty concentrating
✅ Cravings for non-food items (pica – craving for ice, clay, chalk)
2. Diagnostic Tests for Anemia
| Test Name | Purpose |
|---|---|
| Complete Blood Count (CBC) | Measures hemoglobin, hematocrit, and RBC levels |
| Serum Ferritin Test | Checks stored iron levels |
| Peripheral Blood Smear | Examines RBC shape and size |
| Serum Iron & TIBC (Total Iron Binding Capacity) | Evaluates iron absorption |
| Folate & Vitamin B12 Levels | Detects folic acid or B12 deficiency |
✅ Hemoglobin Levels for Diagnosis
| Severity | Hemoglobin (Hb) Level |
|---|---|
| Mild Anemia | 10-10.9 g/dL |
| Moderate Anemia | 7-9.9 g/dL |
| Severe Anemia | <7 g/dL |
Diet for Anemic Pregnant Women
A well-planned diet rich in iron, folic acid, vitamin B12, and vitamin C helps prevent and treat anemia.
1. Iron-Rich Foods (Heme & Non-Heme Sources)
| Food Category | Examples |
|---|---|
| Heme Iron (Animal Sources, better absorbed) | Chicken liver, beef, fish, eggs |
| Non-Heme Iron (Plant Sources, requires Vitamin C for absorption) | Spinach, lentils, beans, tofu, nuts, fortified cereals |
| Iron-Absorption Boosters | Citrus fruits, tomatoes, bell peppers (rich in Vitamin C) |
2. Folic Acid-Rich Foods
| Food Category | Examples |
|---|---|
| Leafy Greens | Spinach, kale, broccoli |
| Legumes | Lentils, chickpeas, beans |
| Citrus Fruits | Oranges, lemons |
| Fortified Cereals | Whole grain cereals, bread |
3. Vitamin B12-Rich Foods
| Food Category | Examples |
|---|---|
| Animal Products | Milk, eggs, meat, fish |
| Fortified Foods | B12-fortified cereals, plant-based milk |
4. Foods to Avoid
🚫 Tea & Coffee (Inhibits iron absorption)
🚫 High-Calcium Foods with Iron (Calcium competes with iron absorption)
🚫 Processed & Junk Foods (Low in nutrients, high in sugar & unhealthy fats)
Balanced Diet Plan for Anemic Pregnant Women
📌 Sample Meal Plan for Iron & Folic Acid Deficiency
| Meal | Food Suggestions |
|---|---|
| Breakfast | Ragi porridge + boiled egg + orange juice |
| Mid-Morning Snack | Sprouts chaat + lemon water |
| Lunch | Multigrain roti + dal + spinach curry + curd |
| Evening Snack | Roasted makhana + buttermilk |
| Dinner | Brown rice + fish curry + beetroot salad |
✅ Tip: Include Vitamin C-rich foods (lemon, oranges, bell peppers) to enhance iron absorption.
Iron & Folic Acid Supplementation During Pregnancy
1. Recommended Daily Supplements
| Nutrient | Daily Requirement During Pregnancy | Supplement Dosage |
|---|---|---|
| Iron | 27 mg/day | 60 mg elemental iron (as per WHO) |
| Folic Acid | 600 mcg/day | 400-600 mcg folic acid |
| Vitamin B12 | 2.6 mcg/day | If deficient, 1000 mcg/day |
2. Iron Supplementation Guidelines
✅ Start iron supplements after 12 weeks of pregnancy (to avoid nausea).
✅ Take iron on an empty stomach or with Vitamin C (avoid calcium at the same time).
✅ For severe anemia, IV iron therapy may be required.
✅ Continue iron supplementation for 3 months postpartum to replenish iron stores.
3. Folic Acid Supplementation Guidelines
✅ Start folic acid at least 1 month before conception and continue through the first trimester to prevent birth defects.
✅ If anemia is severe, additional folic acid supplementation may be needed.
Counseling for Anemia in Pregnancy
1. Importance of Nutrition Counseling
🔹 Explain the role of iron and folic acid in pregnancy.
🔹 Encourage a balanced diet with iron, folic acid, and vitamin C.
🔹 Educate about food choices that enhance or inhibit iron absorption.
🔹 Advise meal planning to include iron-rich foods in daily diet.
2. Lifestyle Modifications
✅ Encourage regular light exercise to improve blood circulation.
✅ Avoid excessive tea and coffee to improve iron absorption.
✅ Ensure proper hydration to prevent constipation from iron supplements.
3. Managing Side Effects of Iron Supplements
| Side Effect | Management Strategy |
|---|---|
| Constipation | Increase fiber & water intake |
| Nausea | Take iron after meals |
| Black Stools | Normal side effect, no need to worry |
4. High-Risk Groups for Anemia
✅ Teenage Pregnant Women – Higher risk due to increased nutrient demand.
✅ Women with Multiple Pregnancies – Increased iron & folic acid requirement.
✅ Women with Low Iron Stores Pre-Pregnancy – Need early intervention.
Conclusion
Anemia in pregnancy is preventable and treatable with proper diet, supplements, and lifestyle changes. Ensuring adequate iron, folic acid, and vitamin B12 intake helps maintain maternal health and fetal development.
Key Takeaways:
✅ Diagnose anemia early through blood tests (CBC, iron levels).
✅ Include iron, folic acid, and vitamin C-rich foods in the diet.
✅ Start iron & folic acid supplementation as per WHO guidelines.
✅ Counsel pregnant women on nutrition, supplements, and anemia prevention.
✅ Monitor hemoglobin levels regularly to track improvement.
By following these dietary and medical recommendations, anemia in pregnancy can be effectively managed, ensuring a healthy mother and baby.
Nutrition in Lactation – Nutritional Requirements & Diet for Lactating Mothers
Introduction
Lactation is a nutritionally demanding phase where a mother’s body produces breast milk to nourish the baby. Proper nutrition during lactation ensures:
✅ Adequate milk production for infant growth
✅ Maternal health recovery post-pregnancy
✅ Optimal immunity and energy levels
✅ Prevention of postpartum deficiencies
Breastfeeding mothers require higher energy, protein, vitamins, and minerals than during pregnancy.
Nutritional Requirements for Lactating Mothers
| Nutrient | Daily Requirement | Function | Food Sources |
|---|---|---|---|
| Energy | 2500-2700 kcal/day | Supports milk production | Whole grains, dairy, nuts |
| Protein | 70-80g/day | Builds milk protein, supports tissue repair | Eggs, lentils, fish, dairy |
| Carbohydrates | 210-250g/day | Provides energy for breastfeeding | Rice, wheat, oats, potatoes |
| Fats | 30-35% of total energy | DHA for brain & nervous system | Avocado, nuts, olive oil, ghee |
| Calcium | 1000-1200 mg/day | Maintains maternal & infant bone health | Milk, cheese, yogurt, ragi |
| Iron | 9-10 mg/day | Prevents postpartum anemia | Spinach, eggs, chicken |
| Folic Acid | 500 mcg/day | Supports milk production | Leafy vegetables, citrus fruits |
| Vitamin A | 1300 mcg/day | Infant eye & immune development | Carrots, mangoes, pumpkin |
| Vitamin C | 120 mg/day | Enhances immunity & iron absorption | Citrus fruits, tomatoes |
| Vitamin D | 15 mcg (600 IU) | Calcium absorption & bone health | Sunlight, dairy, fish oil |
| Fiber | 30-35g/day | Prevents constipation & supports digestion | Whole grains, vegetables, fruits |
| Water | 3-3.5 liters/day | Hydration & milk production | Plain water, fresh juices |
Key Nutritional Concerns in Lactation
📌 Increased calorie requirement due to milk production (extra 500 kcal/day).
📌 Higher protein, calcium, and iron intake for maternal recovery and milk composition.
📌 Sufficient hydration to maintain milk supply.
📌 Balanced omega-3 intake (DHA) for the baby’s brain development.
Balanced Diet Plan for Lactating Mothers
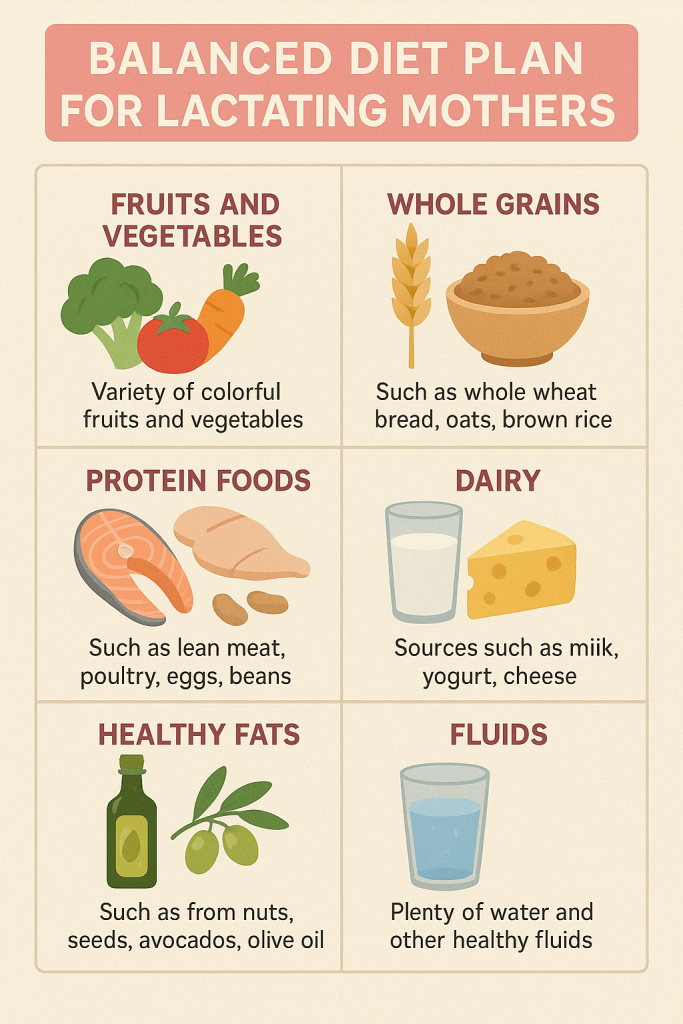
1. Ideal Meal Frequency for Lactating Mothers
📌 Three main meals + 2-3 healthy snacks per day.
📌 Frequent, nutrient-dense meals to maintain milk supply and energy.
| Meal | Time | Purpose |
|---|---|---|
| Breakfast | 7:30 – 8:30 AM | Provides energy for the day |
| Mid-Morning Snack | 10:00 – 11:00 AM | Boosts metabolism & milk supply |
| Lunch | 12:30 – 1:30 PM | Main balanced meal |
| Evening Snack | 4:00 – 5:00 PM | Provides energy for breastfeeding |
| Dinner | 7:30 – 8:30 PM | Light and nutritious meal for digestion |
2. Sample Diet Plan for Lactating Mothers (Balanced Meal Plan)
📌 Day 1
| Meal | Food Suggestions |
|---|---|
| Breakfast | Oats porridge + almonds + milk |
| Mid-Morning Snack | Banana + yogurt |
| Lunch | Soft chapati + dal + spinach curry |
| Evening Snack | Roasted makhana + buttermilk |
| Dinner | Brown rice + curd + steamed vegetables |
📌 Day 2
| Meal | Food Suggestions |
|---|---|
| Breakfast | Ragi porridge + boiled egg |
| Mid-Morning Snack | Cottage cheese cubes + fresh orange juice |
| Lunch | Whole wheat roti + moong dal + carrot-beetroot salad |
| Evening Snack | Mashed sweet potato with butter |
| Dinner | Khichdi + curd + sautéed broccoli |
📌 Day 3
| Meal | Food Suggestions |
|---|---|
| Breakfast | Scrambled eggs + multigrain toast + green tea |
| Mid-Morning Snack | Fruit smoothie with yogurt |
| Lunch | Soft millet roti + lentil soup + sautéed vegetables |
| Evening Snack | Nuts + herbal tea |
| Dinner | Rice + paneer curry + cucumber salad |
3. Key Food Groups for Lactating Mothers
| Food Group | Examples | Function |
|---|---|---|
| Grains & Cereals | Brown rice, wheat, oats, ragi, quinoa | Energy & fiber |
| Proteins | Eggs, lentils, fish, chicken, paneer | Muscle & milk production |
| Dairy | Milk, yogurt, cheese | Bone & teeth formation |
| Vegetables | Carrots, spinach, broccoli | Vitamins & fiber |
| Fruits | Banana, apple, mango | Natural sugars & minerals |
| Healthy Fats | Ghee, nuts, avocado, olive oil | Brain & nervous system development |
4. Important Feeding Tips for Lactating Mothers
🔹 Eat small, frequent meals – Prevents fatigue and maintains milk supply.
🔹 Ensure proper hydration – 3-3.5 liters of water daily.
🔹 Include high-protein & calcium-rich foods for postpartum recovery.
🔹 Consume omega-3 rich foods (flaxseeds, walnuts, fatty fish) for infant brain development.
🔹 Avoid excess sugar and processed foods to prevent postpartum weight gain.
5. Foods to Avoid During Lactation
🚫 Excess Caffeine – Can cause irritability in the baby (limit to 200mg/day).
🚫 Spicy & Gas-Producing Foods – May cause colic in the baby.
🚫 Alcohol & Smoking – Can pass through breast milk, affecting the baby’s development.
🚫 Excess Tea & Coffee – Reduces iron absorption.
🚫 Highly Processed & Junk Foods – Low in essential nutrients.
6. Common Nutritional Deficiencies in Lactating Mothers & Prevention
| Deficiency | Symptoms | Food Sources |
|---|---|---|
| Iron Deficiency (Anemia) | Fatigue, dizziness, pale skin | Spinach, eggs, nuts, meat |
| Calcium Deficiency | Weak bones, muscle cramps | Milk, cheese, sesame seeds |
| Vitamin D Deficiency | Weak immunity, joint pain | Sunlight, fish, fortified milk |
| Protein Deficiency | Poor muscle recovery | Paneer, yogurt, lentils, eggs |
7. Common Eating Problems in Lactating Mothers & Solutions
| Problem | Cause | Solution |
|---|---|---|
| Low Energy Levels | High energy demand for breastfeeding | Eat small, frequent, nutrient-rich meals |
| Weight Gain | High-calorie diet, low activity | Focus on healthy fats, include light exercise |
| Low Milk Supply | Dehydration, low calorie/protein intake | Increase water intake, eat lactogenic foods |
| Constipation | Low fiber & water intake | Increase fiber, drink plenty of fluids |
8. Transition to Post-Lactation Nutrition
📌 Gradually reduce calorie intake as milk production decreases.
📌 Continue calcium & vitamin D intake for bone health.
📌 Ensure a high-protein diet to support body recovery.
📌 Maintain hydration and a balanced diet to prevent postpartum fatigue.
Conclusion
Proper nutrition during lactation ensures healthy milk production, maternal recovery, and infant growth. By following a nutrient-dense diet rich in protein, calcium, iron, vitamins, and healthy fats, lactating mothers can stay healthy and provide the best nourishment for their baby.
Key Takeaways:
✅ Three main meals + 2-3 healthy snacks daily with variety.
✅ Consume nutrient-rich foods, limit junk food intake.
✅ Ensure adequate protein, calcium, iron, and folic acid.
✅ Promote hydration, digestion, and an active lifestyle.
By following these nutritional guidelines and meal plans, lactating mothers can ensure optimal health for themselves and their babies!
Complementary Feeding (Weaning).
Introduction
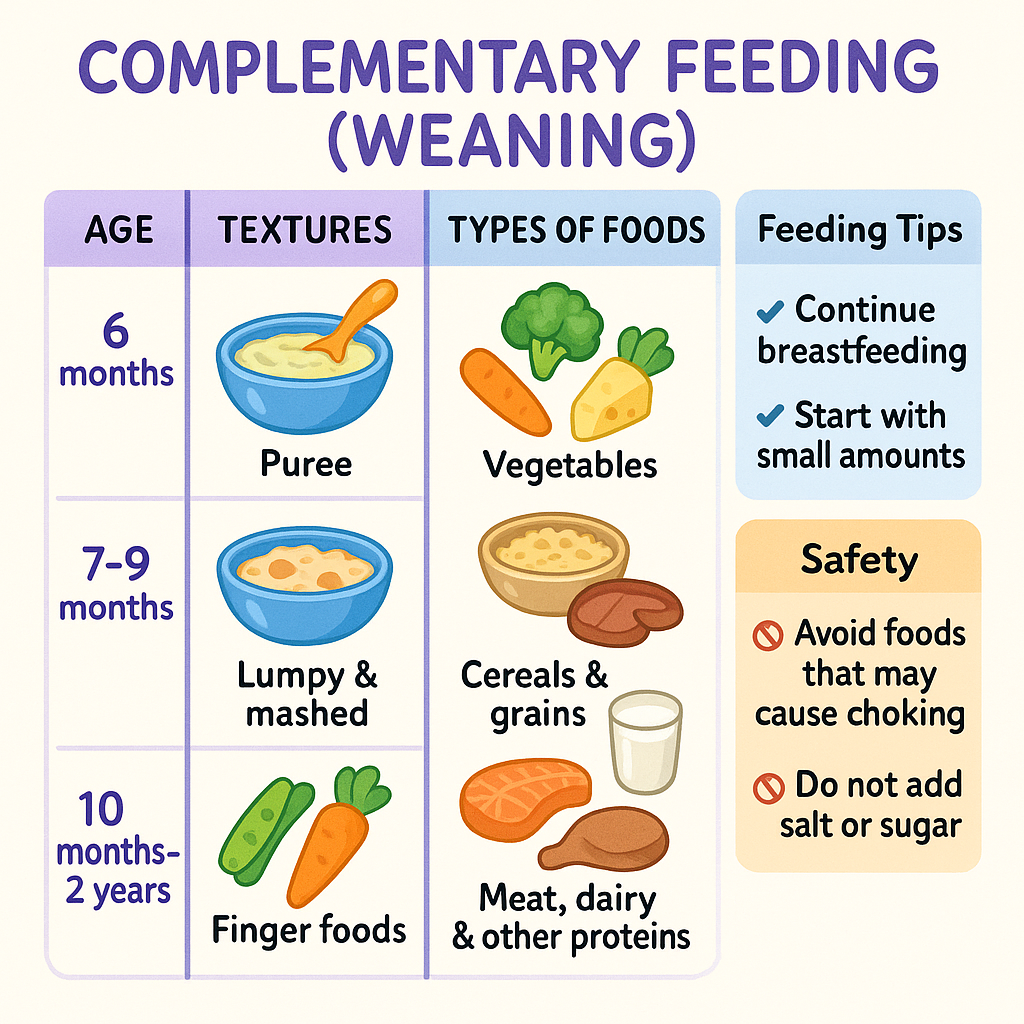
Complementary feeding (weaning) is the gradual transition from exclusive breastfeeding to solid and semi-solid foods while continuing breastfeeding. It begins at 6 months of age and provides additional energy, protein, vitamins, and minerals needed for growth and development.
✅ WHO & UNICEF Recommendations:
- Exclusive breastfeeding for the first 6 months.
- Introduce complementary foods at 6 months while continuing breastfeeding up to 2 years or beyond.
- Age-appropriate, nutritious, and safe foods should be introduced gradually.
Nutritional Requirements for Complementary Feeding
| Nutrient | Daily Requirement (6-12 Months) | Function | Food Sources |
|---|---|---|---|
| Energy | 700-900 kcal/day | Supports growth & activity | Whole grains, dairy, nuts |
| Protein | 13-15g/day | Builds muscles & tissues | Eggs, lentils, fish, dairy |
| Carbohydrates | 100-150g/day | Provides energy for brain & body | Rice, wheat, oats, potatoes |
| Fats | 30-40% of total energy | Brain & nervous system development | Avocado, nuts, olive oil, ghee |
| Calcium | 270 mg/day | Bone & teeth formation | Milk, cheese, yogurt, ragi |
| Iron | 11 mg/day | Prevents anemia, supports brain development | Spinach, eggs, chicken |
| Folic Acid | 80 mcg/day | Supports cell growth | Green leafy vegetables, citrus fruits |
| Vitamin A | 500 mcg/day | Eye & immune development | Carrots, mangoes, pumpkin |
| Vitamin C | 35 mg/day | Enhances immunity & iron absorption | Citrus fruits, tomatoes |
| Vitamin D | 10 mcg (400 IU) | Calcium absorption & bone health | Sunlight, dairy, fish oil |
| Fiber | 10-15g/day | Prevents constipation & supports digestion | Whole grains, vegetables, fruits |
| Water | 800-1000 ml/day | Hydration & digestion | Plain water, fresh juices |
Key Nutritional Concerns in Weaning
📌 Introduce iron-rich foods to prevent anemia.
📌 Provide energy-dense foods to meet growing needs.
📌 Ensure vitamin C intake to enhance iron absorption.
📌 Maintain hygiene to prevent infections.
Phases of Complementary Feeding
| Age | Food Consistency | Meal Frequency |
|---|---|---|
| 6-8 Months | Mashed/pureed foods | 2-3 meals/day + breast milk |
| 9-12 Months | Soft, finely chopped foods | 3-4 meals/day + 1-2 snacks |
| 12-24 Months | Family foods (small portions) | 4 meals/day + 1-2 snacks |
Balanced Diet Plan for Complementary Feeding
1. Ideal Meal Frequency for Complementary Feeding
📌 2-3 meals/day at 6-8 months, increasing to 3-4 meals/day by 9-12 months.
📌 Small portions that gradually increase as the child grows.
| Meal | Time | Purpose |
|---|---|---|
| Breakfast | 7:30 – 8:30 AM | Provides energy for the day |
| Mid-Morning Snack | 10:00 – 11:00 AM | Boosts metabolism & prevents hunger |
| Lunch | 12:30 – 1:30 PM | Main balanced meal |
| Evening Snack | 4:00 – 5:00 PM | Provides energy for play |
| Dinner | 7:30 – 8:30 PM | Light and nutritious meal for digestion |
2. Sample Diet Plan for Complementary Feeding (6-12 Months)
📌 Day 1
| Meal | Food Suggestions |
|---|---|
| Breakfast | Mashed banana + yogurt |
| Mid-Morning Snack | Soft-boiled egg yolk |
| Lunch | Mashed rice + dal + ghee |
| Evening Snack | Steamed carrot puree |
| Dinner | Soft oats porridge |
📌 Day 2
| Meal | Food Suggestions |
|---|---|
| Breakfast | Ragi porridge + mashed apple |
| Mid-Morning Snack | Cottage cheese cubes |
| Lunch | Multigrain khichdi + soft-cooked vegetables |
| Evening Snack | Soft mashed potato |
| Dinner | Rice + moong dal + mashed spinach |
📌 Day 3
| Meal | Food Suggestions |
|---|---|
| Breakfast | Oats porridge + mashed dates |
| Mid-Morning Snack | Whole wheat crackers + peanut butter |
| Lunch | Dal + soft chapati + boiled carrot |
| Evening Snack | Roasted makhana |
| Dinner | Rice + soft-cooked fish + beetroot puree |
3. Key Food Groups for Complementary Feeding
| Food Group | Examples | Function |
|---|---|---|
| Grains & Cereals | Rice, wheat, oats, ragi, quinoa | Energy & fiber |
| Proteins | Eggs, lentils, fish, chicken, paneer | Muscle & brain development |
| Dairy | Milk, yogurt, cheese | Bone & teeth formation |
| Vegetables | Carrots, spinach, pumpkin | Vitamins & fiber |
| Fruits | Banana, apple, mango | Natural sugars & minerals |
| Healthy Fats | Ghee, nuts, avocado, olive oil | Brain & nervous system development |
4. Important Feeding Tips for Complementary Feeding
🔹 Introduce one new food at a time (observe for allergies).
🔹 Encourage self-feeding with soft finger foods.
🔹 Ensure proper hydration with small sips of water.
🔹 Do not add salt, sugar, or honey before 1 year.
🔹 Maintain food hygiene to prevent infections.
5. Foods to Avoid Before 1 Year
🚫 Honey – Risk of botulism.
🚫 Salt & Sugar – Burden on immature kidneys.
🚫 Cow’s Milk as a Primary Drink – Risk of iron deficiency.
🚫 Whole Nuts & Popcorn – Choking hazard.
🚫 Raw Eggs & Undercooked Meat – Risk of bacterial infections.
6. Common Nutritional Deficiencies in Weaning & Prevention
| Deficiency | Symptoms | Food Sources |
|---|---|---|
| Iron Deficiency (Anemia) | Fatigue, poor growth | Spinach, eggs, nuts, meat |
| Calcium Deficiency | Weak bones, slow growth | Milk, cheese, sesame seeds |
| Vitamin D Deficiency | Weak immunity, rickets | Sunlight, fish, fortified milk |
| Protein Deficiency | Poor weight gain | Paneer, yogurt, lentils, eggs |
7. Common Weaning Problems & Solutions
| Problem | Cause | Solution |
|---|---|---|
| Refusing New Foods | Unfamiliar taste | Introduce gradually, mix with favorite food |
| Choking Risk | Large food pieces | Offer soft, mashed, or small pieces |
| Constipation | Low fiber, inadequate fluids | Increase water, offer fruits like prunes, pears |
| Food Allergies | Sensitivity to eggs, dairy, nuts | Introduce allergens one at a time |
| Underweight Baby | Insufficient calorie intake | Add ghee, banana, yogurt to meals |
Conclusion
Complementary feeding ensures a smooth transition from breast milk to family foods, promoting growth, brain development, and immunity. A balanced diet with iron-rich, energy-dense, and vitamin-packed foods ensures optimal health and development for the infant.
Key Takeaways:
✅ Start complementary foods at 6 months, with soft, mashed foods.
✅ Gradually introduce new textures and flavors as the baby grows.
✅ Include iron-rich, vitamin-rich, and protein-packed foods.
✅ Avoid salt, sugar, honey, and processed foods before 1 year.
✅ Ensure safe, hygienic food preparation and proper hydration.
By following these nutritional guidelines and meal plans, parents can ensure healthy growth and development for their baby! 🥣👶💪