COH-1903-COMMUNITY HEALTH NURSING-SYNOPSIS (FULL)
COH-1903-COMMUNITY HEALTH NURSING–SYNOPSIS
Stages of Disease Cycle
- Incubation Period – Time between exposure and symptom onset (Pathogen multiplies, but no signs).
- Prodromal Stage – Early, mild symptoms (e.g., fever, fatigue); pathogen spreads.
- Acute Stage – Severe symptoms, peak infection, high transmission risk.
- Decline Stage – Symptoms reduce, pathogen count decreases, recovery begins.
- Convalescence Stage – Recovery phase, immune system repairs, may still be contagious.
- Chronic/Latent Stage (Optional) – Dormant infection (e.g., TB, HIV), can reactivate later.
🔹 Key for Exams:
- Incubation Period varies (e.g., COVID-19: 2–14 days).
- Carrier State: Asymptomatic but transmits disease (e.g., Typhoid carrier).
- Quarantine (for exposed) vs. Isolation (for infected).
- Helps in outbreak control, vaccination, public health interventions.
Levels of Prevention
- Primordial Prevention – Prevention of Risk Factors
- Focus: Policy-making, lifestyle changes to prevent disease risk factors.
- Example: Banning tobacco ads, promoting healthy diets.
- Primary Prevention – Preventing Disease Occurrence
- Focus: Health promotion & specific protection.
- Example: Vaccination, sanitation, safe drinking water, health education.
- Secondary Prevention – Early Diagnosis & Treatment
- Focus: Screening, early detection, preventing complications.
- Example: Mammography for breast cancer, BP screening for hypertension.
- Tertiary Prevention – Reducing Disability & Rehabilitation
- Focus: Managing disease to prevent worsening & improving quality of life.
- Example: Physiotherapy for stroke patients, insulin therapy for diabetes.
- Quaternary Prevention – Avoiding Overmedicalization
- Focus: Preventing unnecessary treatments & interventions.
- Example: Avoiding excessive antibiotics, reducing unnecessary surgeries.
🔹 Key for Exams:
- Primary = Prevent, Secondary = Detect, Tertiary = Treat, Quaternary = Avoid harm.
- Screening = Secondary Prevention (e.g., Pap smear for cervical cancer).
- Vaccination = Primary Prevention.
- Rehabilitation = Tertiary Prevention.
Iceberg of Disease
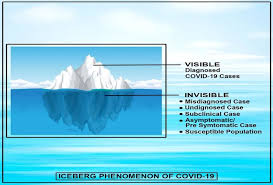
🔹 Concept: Diseases exist in a visible (clinical) and hidden (subclinical) form, like an iceberg where only a small part is seen above water.
- Clinical Cases (Visible Part of Iceberg)
- Diagnosed, symptomatic cases seen in hospitals.
- Example: Diagnosed TB, COVID-19 with symptoms.
- Subclinical Cases (Hidden Part of Iceberg)
- Undiagnosed, asymptomatic, carriers, latent infections.
- Example: Asymptomatic COVID-19 cases, latent TB, Hepatitis B carriers.
🔹 Key for Exams:
- Larger hidden burden = Challenges in disease control.
- Screening helps detect subclinical cases (e.g., HIV, TB, cancer screening).
- More subclinical cases = Higher disease transmission.
Spectrum of Disease
🔹 Concept: Diseases progress through various stages, from exposure to outcome.
- Exposure – Contact with the causative agent.
- Subclinical Stage – No symptoms, but pathogen present (e.g., HIV before AIDS develops).
- Clinical Stage – Signs & symptoms appear, may be mild or severe (e.g., Dengue fever).
- Outcome – Recovery, disability, or death.
🔹 Key for Exams:
- Acute diseases (e.g., flu) → Short duration.
- Chronic diseases (e.g., diabetes, TB) → Long-term effects.
- Spectrum explains disease progression & helps in intervention planning.
Modes of Disease Transmission
🔹 1. Direct Transmission – Person-to-Person Contact
- Droplet infection – Coughing, sneezing (e.g., COVID-19, TB, Influenza)
- Contact transmission – Touching, kissing, sexual contact (e.g., HIV, Herpes, Scabies)
- Transplacental (Vertical) – Mother to child (e.g., HIV, Syphilis, Rubella)
🔹 2. Indirect Transmission – Via Intermediaries
- Fomite transmission – Objects like towels, utensils (e.g., Hepatitis B, MRSA)
- Vector-borne – Through insects/animals
- Mechanical (Passively carried) – Flies spreading cholera
- Biological (Inside vector’s body) – Mosquitoes spreading malaria, dengue
- Airborne (Droplet Nuclei) – Suspended particles (e.g., Measles, TB)
- Waterborne/Foodborne – Contaminated food/water (e.g., Cholera, Hepatitis A)
- Zoonotic – From animals to humans (e.g., Rabies, Plague, Brucellosis)
🔹 Key for Exams:
- HIV, Syphilis = Direct (Sexual, Vertical)
- TB, Measles = Airborne
- Malaria, Dengue = Vector-borne (Biological)
- Cholera, Typhoid = Waterborne/Foodborne
- Rabies = Zoonotic
- Prevention Strategies: Hand hygiene, vaccination, vector control, sanitation
Integrated Management of Neonatal and Childhood Illness (IMNCI) –
🔹 Full Form:
IMNCI = Integrated Management of Neonatal and Childhood Illness
🔹 Purpose:
A strategy to reduce neonatal and childhood mortality & morbidity by improving healthcare services at all levels.
Key Components of IMNCI
IMNCI follows a three-pronged approach:
- Improvement in Case Management Skills of Health Workers
- Training healthcare workers (ANMs, ASHAs, Nurses, Doctors)
- Early identification & treatment of childhood illnesses
- Focus on pneumonia, diarrhea, malaria, measles, and malnutrition
- Strengthening Health System
- Ensuring adequate supplies of drugs & equipment
- Improving referral services
- Strengthening health facilities
- Family & Community-Level Interventions
- Health education to caregivers and mothers
- Promotion of breastfeeding, nutrition, hygiene
- Recognition of danger signs (e.g., fast breathing, fever, convulsions)
IMNCI Case Management Process
🔹 1. Assessment
- Check for danger signs (Convulsions, lethargy, inability to feed, vomiting)
- Measure temperature, respiration, weight
- Assess for specific diseases (Diarrhea, Pneumonia, Malaria, Malnutrition)
🔹 2. Classification (Diagnosis)
- Green (Mild): Home care, counseling, follow-up
- Yellow (Moderate): Treat with medicines, refer if needed
- Red (Severe): Immediate referral to a higher facility
🔹 3. Treatment
- Provide antibiotics, ORS, antimalarials, zinc supplementation
- Nutritional support for malnourished children
- Vitamin A, deworming
🔹 4. Referral & Follow-up
- Severe cases referred to hospitals
- Follow-up visits ensure recovery
IMNCI Vs. IMCI
- IMCI (Integrated Management of Childhood Illness) – WHO strategy for children aged 2 months to 5 years
- IMNCI (Integrated Management of Neonatal and Childhood Illness) – Includes neonates (0–2 months) & children (2 months–5 years)
- IMNCI is adapted for India, with greater focus on newborn care
Key for Exams
✅ IMNCI covers 0–5 years, while IMCI covers 2 months–5 years
✅ 3 components: Health workers training, Health system strengthening, Community interventions
✅ Covers pneumonia, diarrhea, malaria, malnutrition, measles
✅ Danger signs: Convulsions, fast breathing, unable to feed, fever
✅ Treatment: ORS, antibiotics, zinc, Vitamin A, nutrition support
Important Child Health Programs in India
1. Navjaat Shishu Suraksha Karyakram (NSSK)
🔹 Full Form: Navjaat Shishu Suraksha Karyakram
🔹 Launch Year: 2009
🔹 Objective: Reduce neonatal mortality by improving newborn care at delivery points.
🔹 Key Components:
- Training of healthcare workers (Doctors, Nurses, ANMs) in essential newborn care.
- Focus on Resuscitation, Prevention of infection, Thermal protection, Breastfeeding.
- Use of Neonatal Resuscitation Devices for birth asphyxia management.
🔹 Target Group: Newborns (0-28 days)
✅ Key for Exams:
- Focus: Essential newborn care (Golden Hour Concept).
- Trained healthcare workers: Doctors, Nurses, ANMs.
- Main aim: Reduce Neonatal Mortality Rate (NMR).
2. Rashtriya Bal Swasthya Karyakram (RBSK)
🔹 Full Form: Rashtriya Bal Swasthya Karyakram
🔹 Launch Year: 2013
🔹 Objective: Early identification and management of health conditions in children.
🔹 Key Components:
- Screening for 4D’s:
1. Defects at Birth (Congenital anomalies)
2. Diseases in Childhood (Anemia, Malnutrition, Skin conditions)
3. Deficiencies (Iron, Vitamin A, Iodine deficiency)
4. Developmental Delays and Disabilities (Hearing, Vision, Neuromotor issues) - Screening at schools & Anganwadi centers.
- Referral services to District Early Intervention Centers (DEICs).
🔹 Target Group: Children 0-18 years
✅ Key for Exams:
- Focus: 4D’s – Defects, Diseases, Deficiencies, Developmental Delays.
- Screening at: Schools, Anganwadi Centers.
- Referral to: DEIC (District Early Intervention Centers).
3. Bal Sakha Yojana (BSY)
🔹 Full Form: Bal Sakha Yojana
🔹 Launch Year: 2008 (By Gujarat Government)
🔹 Objective: Ensure medical care for neonates born to BPL families.
🔹 Key Components:
- Free neonatal care for BPL families at private hospitals.
- First 30 days of life covered for preterm, low birth weight, birth asphyxia, sepsis, jaundice cases.
- Neonatal Intensive Care Unit (NICU) treatment provided at private hospitals.
🔹 Target Group: Newborns of BPL families
✅ Key for Exams:
- State-Specific Program (Gujarat).
- Focus: Free neonatal care for BPL families.
- Duration: First 30 days of life.
Quick Comparison Table for Exams
| Program | Launch Year | Target Age | Key Focus |
|---|---|---|---|
| NSSK | 2009 | 0-28 days | Essential newborn care (Resuscitation, Infection Prevention) |
| RBSK | 2013 | 0-18 years | Screening for 4Ds (Defects, Diseases, Deficiencies, Disabilities) |
| Bal Sakha Yojana | 2008 (Gujarat) | Newborns (BPL families) | Free neonatal care in private hospitals |
✅ NSSK = Newborn care, Golden Hour, Neonatal resuscitation.
✅ RBSK = 4Ds screening (Defects, Diseases, Deficiencies, Disabilities) + DEIC referrals.
✅ Bal Sakha Yojana = Free neonatal care for BPL newborns in Gujarat.
Occupational Health & Diseases
Occupational diseases are caused due to exposure to physical, chemical, biological, ergonomic, and psychosocial hazards at the workplace.
1. Occupational Diseases Classification & Key Disorders
A. Diseases Due to Physical Hazards
| Disease | Cause | High-Risk Occupations |
|---|---|---|
| Noise-Induced Hearing Loss (NIHL) | Continuous exposure to loud noise (>85 dB) | Factory workers, Aviation staff, Construction workers |
| Radiation Sickness | Ionizing radiation (X-rays, UV, gamma rays) | Radiologists, Nuclear plant workers, Astronauts |
| Vibration White Finger (Hand-Arm Vibration Syndrome – HAVS) | Use of vibrating tools | Jackhammer operators, Miners, Lumberjacks |
| Heat Stroke & Heat Exhaustion | Prolonged heat exposure | Glass factory workers, Foundry workers, Firefighters |
| Cold Stress & Frostbite | Exposure to extremely low temperatures | Ice factory workers, Arctic researchers |
B. Diseases Due to Chemical Hazards
| Disease | Cause | High-Risk Occupations |
|---|---|---|
| Lead Poisoning (Plumbism) | Lead exposure | Battery, Paint, Printing workers |
| Mercury Poisoning | Mercury inhalation | Dentists, Thermometer factory workers |
| Arsenic Poisoning | Exposure to arsenic compounds | Pesticide industry, Glass manufacturing |
| Benzene Poisoning (Aplastic Anemia, Leukemia) | Benzene fumes | Petrochemical workers, Paint industry |
| Carbon Monoxide Poisoning | Inhalation of CO gas | Firefighters, Tunnel workers, Foundry workers |
| Chromium Toxicity (Nasal Septum Perforation, Lung Cancer) | Chromium dust exposure | Leather tanning, Dye industry workers |
C. Pneumoconiosis (Lung Diseases Due to Inhalation of Dust)
| Disease | Cause | High-Risk Occupations |
|---|---|---|
| Silicosis | Inhalation of silica dust | Miners, Stone cutters, Glass industry |
| Asbestosis | Inhalation of asbestos fibers | Shipyard workers, Construction workers |
| Coal Workers’ Pneumoconiosis (Black Lung Disease) | Coal dust | Coal miners |
| Byssinosis (Brown Lung Disease) | Cotton dust | Textile industry, Cotton mill workers |
| Bagassosis | Sugarcane dust inhalation | Sugarcane industry |
| Farmer’s Lung Disease | Mold spores in hay & grain | Farmers, Agricultural workers |
D. Diseases Due to Biological Hazards
| Disease | Cause | High-Risk Occupations |
|---|---|---|
| Anthrax (Wool Sorters’ Disease) | Bacillus anthracis | Farmers, Wool industry workers |
| Brucellosis (Undulant Fever) | Brucella bacteria from livestock | Dairy farm workers, Veterinarians |
| Leptospirosis (Weil’s Disease) | Bacteria from contaminated water | Sewer workers, Flood-affected areas |
| Tuberculosis (TB) | Airborne transmission of Mycobacterium tuberculosis | Healthcare workers, Prison staff |
| Hepatitis B & C | Bloodborne virus | Healthcare workers, Lab technicians |
| COVID-19 & SARS | Respiratory virus | Healthcare workers, Airport staff |
E. Musculoskeletal & Ergonomic Disorders
| Disease | Cause | High-Risk Occupations |
|---|---|---|
| Carpal Tunnel Syndrome (CTS) | Repetitive hand movement | IT professionals, Typists |
| Tennis Elbow (Lateral Epicondylitis) | Repeated wrist & arm motion | Mechanics, Painters |
| Back Pain & Disc Herniation | Heavy lifting, Poor posture | Construction workers, Nurses |
| Cervical Spondylosis | Long sitting hours, Poor posture | IT professionals, Office workers |
| Varicose Veins | Prolonged standing | Nurses, Shopkeepers, Hairdressers |
F. Psychological & Social Hazards
| Disease | Cause | High-Risk Occupations |
|---|---|---|
| Occupational Stress & Depression | Work pressure, Job insecurity | Call centers, IT professionals, Nurses |
| Burnout Syndrome | Chronic workplace stress | Healthcare workers, Social workers |
| Workplace Violence & PTSD | Exposure to trauma & abuse | Police officers, Military personnel |
| Alcoholism & Substance Abuse | Work-related stress | Corporate jobs, Entertainment industry |
2. Prevention & Control of Occupational Diseases
A. Primary Prevention (Eliminate Exposure)
- Engineering Controls: Proper ventilation, noise reduction, machine safety.
- Administrative Controls: Reducing work hours, job rotation.
- Personal Protective Equipment (PPE): Gloves, masks, goggles, earplugs.
- Workplace Hygiene: Safe disposal of chemicals, clean environment.
B. Secondary Prevention (Early Detection & Treatment)
- Regular Health Checkups (X-rays for miners, hearing tests for factory workers).
- Medical Surveillance & Screening Programs.
C. Tertiary Prevention (Rehabilitation & Compensation)
- Medical Treatment & Rehabilitation for affected workers.
- Disability Benefits & Compensation (ESIC, Workmen’s Compensation Act).
The Employees’ State Insurance (ESI) Act, 1948 & The Factories Act, 1948
1. The Employees’ State Insurance (ESI) Act, 1948
🔹 Objective:
- To provide social security & health insurance to employees in case of sickness, maternity, disability, or work-related injuries.
🔹 Applicability:
- Applicable to: Factories, Shops, Establishments with ≥ 10 employees.
- Wage Limit: Employees earning up to ₹21,000/month (₹25,000 for disabled workers) are covered.
🔹 Key Benefits Under ESIC:
- Medical Benefit: Free medical care for insured workers & families.
- Sickness Benefit: 70% of wages paid for 91 days during certified illness.
- Maternity Benefit: 100% wages for 26 weeks for pregnancy.
- Disablement Benefit:
- Temporary: 90% of wages paid for injury-related leave.
- Permanent: Pension based on disability percentage.
- Dependents’ Benefit: Monthly pension for family if worker dies due to occupational injury.
- Unemployment Allowance: 50% of wages paid for 24 months in case of job loss.
🔹 ESI Fund Contributions:
- Employer: 3.25% of wages
- Employee: 0.75% of wages
- Government: Contributes for specific schemes
🔹 Key Features for Exams:
✅ Covers medical, sickness, maternity, disability, and dependents’ benefits.
✅ Covers factories & establishments with 10+ workers (₹21,000 salary limit).
✅ Employer (3.25%) & Employee (0.75%) contribute to ESIC.
✅ Administered by: Employees’ State Insurance Corporation (ESIC).
2. The Factories Act, 1948
🔹 Objective:
- To ensure worker safety, health, and welfare in industrial settings.
🔹 Applicability:
- Factories with 10+ workers (power-operated) & 20+ workers (non-power).
🔹 Key Provisions of the Act:
A. Health Provisions
✅ Cleanliness – Factories must be kept clean & hygienic.
✅ Ventilation & Temperature Control – Proper airflow to avoid suffocation.
✅ Drinking Water – Safe drinking water must be provided.
✅ Toilets & Washing Facilities – Adequate sanitary provisions.
B. Safety Provisions
✅ Fencing of Machinery – Dangerous machines must be covered.
✅ Precautions Against Fire – Fire safety measures are mandatory.
✅ Worker Training & PPE – Workers must be trained in machinery handling.
✅ Prohibition of Child Labor – Employment of children under 14 years is banned.
C. Welfare Provisions
✅ Canteens – Compulsory in factories with 250+ workers.
✅ Restrooms & Crèche – Mandatory for factories with 30+ women workers.
✅ Working Hours:
- Adults: Max 48 hours/week (9 hrs/day), 1 weekly off.
- Overtime: Extra pay for work beyond 9 hours/day.
- Women Workers: Allowed only 6 AM – 7 PM (No night shifts).
🔹 Key Features for Exams:
✅ Factories with 10+ (power) & 20+ (non-power) workers covered.
✅ 48-hour work week, restrooms, safety measures, no child labor.
✅ Canteens (250+ workers), Crèche (30+ women workers) mandatory.
✅ Ensures worker safety, hygiene, and well-being.
Quick Comparison for Exams
| Aspect | ESI Act, 1948 | Factories Act, 1948 |
|---|---|---|
| Objective | Provides social security & medical benefits | Ensures worker health, safety & welfare |
| Applicability | Factories/establishments with 10+ workers | Factories with 10+ (power) & 20+ (non-power) workers |
| Coverage | Workers earning ≤ ₹21,000/month | All factory workers |
| Key Benefits | Medical, Sickness, Maternity, Disability, Pension | Hygiene, Safety, Working hours, Welfare |
| Contributions | Employer (3.25%), Employee (0.75%) | Not contribution-based |
| Administering Body | ESIC (Employees’ State Insurance Corporation) | State Labor Departments |
| Work Hours | 48 hours/week | 48 hours/week, 9 hours/day |
| Special Provisions | Cash benefits for sickness, pregnancy, disability | Canteens, Creches, Safety, Fire Precautions |
Key Takeaways for Exams:
✅ ESI Act = Social Security, Factories Act = Worker Safety.
✅ ESI applies to ₹21,000 salary workers; Factories Act applies to all workers.
✅ ESI = Medical, Sickness, Maternity Benefits; Factories Act = Health, Safety, Working Hours.
✅ ESI contributions are employer (3.25%) & employee (0.75%); Factories Act has no direct financial contribution.
Primary Health Care (PHC)
1. Elements of Primary Health Care (As per Alma-Ata Declaration, 1978)
🔹 Acronym to Remember: “CHEAP SIR”
| Element | Description |
|---|---|
| C – Community Participation | Encouraging community involvement in healthcare programs. |
| H – Health Education | Spreading awareness about disease prevention & healthy living. |
| E – Essential Drug Supply | Availability of basic medicines at PHCs. |
| A – Adequate Food & Nutrition | Addressing malnutrition & food security. |
| P – Promotion of Maternal & Child Health | Immunization, safe childbirth, postnatal care. |
| S – Safe Water & Sanitation | Providing clean drinking water & proper waste disposal. |
| I – Immunization | Protecting against vaccine-preventable diseases. |
| R – Rural Health Services | Extending healthcare to remote & rural areas. |
✅ Key for Exams:
- 8 essential elements ensure preventive, curative, and promotive care.
- First-level healthcare approach as per Alma-Ata Declaration, WHO 1978.
2. Principles of Primary Health Care
🔹 Acronym to Remember: “EQUITY”
| Principle | Description |
|---|---|
| E – Equitable Distribution | Health services accessible to all, especially rural & underserved areas. |
| Q – Quality of Care | Services should be effective, evidence-based, and people-centered. |
| U – Universal Coverage | Ensuring health services for all, irrespective of socio-economic status. |
| I – Inter-sectoral Coordination | Collaboration between health, education, nutrition, water, and sanitation sectors. |
| T – Technology that is Appropriate | Using cost-effective, locally suitable health technologies. |
| Y – Your Community Involvement | Active participation of individuals & communities in their health. |
✅ Key for Exams:
- Focus on equity, accessibility, & community participation.
- Multi-sectoral approach for health improvement.
3. Levels of Health Care
Health services are provided at three levels:
| Level | Key Features | Example Facilities |
|---|---|---|
| Primary Level | First point of contact, Preventive & Basic Curative Care | Sub-Centers, Primary Health Centers (PHCs) |
| Secondary Level | Referral services, Specialized treatment | Community Health Centers (CHCs), District Hospitals |
| Tertiary Level | Advanced care, Super-specialty hospitals | Medical Colleges, AIIMS, Corporate Hospitals |
✅ Key for Exams:
- Primary (First Contact, Basic Care) → Secondary (Specialized Care) → Tertiary (Super-Specialized Care).
- Primary = PHCs & SCs, Secondary = CHCs & District Hospitals, Tertiary = AIIMS & Medical Colleges.
Quick Summary
| Concept | Key Points |
|---|---|
| Primary Health Care Elements | “CHEAP SIR” – Community Participation, Health Education, Essential Drugs, Nutrition, Maternal & Child Health, Safe Water, Immunization, Rural Health Services |
| Principles of PHC | “EQUITY” – Equitable Distribution, Quality, Universal Coverage, Inter-sectoral Coordination, Appropriate Technology, Community Participation |
| Levels of Healthcare | Primary (Basic) → Secondary (Specialist) → Tertiary (Super-Specialty). |
Primary Health Care in India with Population Coverage & Levels of Health Care System
1. Primary Health Care in India
🔹 Definition:
Primary Health Care (PHC) in India focuses on providing essential health services to people at the grassroots level, especially in rural and underserved areas.
🔹 Based on:
- Alma-Ata Declaration, 1978 (WHO’s goal of Health for All by 2000).
- National Health Policy, 1983, 2002, 2017 aimed at strengthening PHC.
🔹 Objectives of PHC in India:
✅ Accessible & affordable healthcare for all.
✅ Reduction in Infant & Maternal Mortality Rates (IMR & MMR).
✅ Prevention & control of communicable & non-communicable diseases.
✅ Providing maternal & child healthcare, immunization, family planning.
✅ Improving sanitation, hygiene, & nutrition.
2. Health Care System in India (Three-Tier System)
A. Primary Level (First Contact & Basic Care)
🔹 Population Coverage & Facilities:
| Facility | Population Coverage | Staffing | Services Provided |
|---|---|---|---|
| Sub-Center (SC) | 5,000 (Plains), 3,000 (Hills/Tribal Areas) | 1 ANM, 1 Male Health Worker | Immunization, Antenatal Care, Family Planning, Minor Ailments |
| Primary Health Center (PHC) | 30,000 (Plains), 20,000 (Hills) | Medical Officer, Nurses, Pharmacist | Outpatient Care, Minor Surgeries, MCH Services, Disease Control |
| Health & Wellness Centers (HWCs) | Same as PHCs/SCs | Community Health Officers (CHOs) | Non-Communicable Disease Care, Telemedicine, Screening |
✅ Key for Exams:
- SC = First Contact, Basic Health Needs.
- PHC = Referral Unit for SCs, Basic OPD & Maternal Services.
- HWCs = Upgraded PHCs with focus on Preventive & Chronic Diseases.
B. Secondary Level (Referral & Specialized Care)
🔹 Population Coverage & Facilities:
| Facility | Population Coverage | Services Provided |
|---|---|---|
| Community Health Center (CHC) | 1,20,000 (Plains), 80,000 (Hills) | 30-bedded Hospital, General Surgery, Emergency Care |
| District Hospital (DH) | One per District | Multi-specialty Care, ICU, Surgical & Trauma Care |
✅ Key for Exams:
- CHC = Serves as a referral center for PHCs, provides surgical care.
- DH = Highest facility at district level, caters to major health issues.
C. Tertiary Level (Super-Specialty Care & Research)
🔹 Facilities:
| Facility | Population Coverage | Services Provided |
|---|---|---|
| Medical Colleges & AIIMS | Regional/National | Super-specialty services, Research, Training |
| Specialty Hospitals | Large Population | Cancer Institutes, Cardiology Centers, Neurology Centers |
✅ Key for Exams:
- Medical Colleges = Provide tertiary care & train doctors.
- AIIMS = Apex institute for research & advanced care.
3. Summary Table of Healthcare Levels in India
| Level | Facilities | Population Coverage | Services Provided |
|---|---|---|---|
| Primary | SC, PHC, HWC | SC: 5,000 (Plains), 3,000 (Hills) PHC: 30,000 (Plains), 20,000 (Hills) | Preventive, OPD, MCH, Family Planning |
| Secondary | CHC, District Hospitals | CHC: 1,20,000 (Plains), 80,000 (Hills) | Surgical, Emergency, Specialist Care |
| Tertiary | Medical Colleges, AIIMS, Specialty Hospitals | Regional/National | Super-specialty care, Research, Teaching |
4. Key
✅ Sub-Center (SC) → PHC → CHC → District Hospital → Medical College (3-Tier System).
✅ SC (5,000) → PHC (30,000) → CHC (1,20,000) → District Hospital (Whole District).
✅ PHCs & CHCs = Backbone of rural healthcare.
✅ Tertiary Care = AIIMS, Medical Colleges, Specialized Hospitals.
✅ Health & Wellness Centers (HWCs) = Strengthened PHCs with NCD focus.
Millennium Development Goals (MDGs) and Sustainable Development Goals (SDGs)
1. Millennium Development Goals (MDGs)
🔹 Introduction:
Adopted in 2000 by the United Nations, the MDGs aimed at addressing global challenges and improving living standards by 2015.
🔹 8 Key MDGs:
| Goal | Objective |
|---|---|
| MDG 1 | Eradicate Extreme Poverty and Hunger |
| MDG 2 | Achieve Universal Primary Education |
| MDG 3 | Promote Gender Equality and Empower Women |
| MDG 4 | Reduce Child Mortality |
| MDG 5 | Improve Maternal Health |
| MDG 6 | Combat HIV/AIDS, Malaria, and Other Diseases |
| MDG 7 | Ensure Environmental Sustainability |
| MDG 8 | Develop a Global Partnership for Development |
🔹 Achievements:
✅ Reduced extreme poverty rates by more than half.
✅ Increased primary school enrollment in developing regions.
✅ Reduced child mortality by nearly 50%.
✅ Improved access to drinking water and sanitation.
🔹 Challenges:
🚫 Persistent inequalities in income, gender, and education.
🚫 Incomplete maternal health and disease combat goals.
✅ Key for Exams:
- 8 Goals set in 2000, aimed for 2015.
- Focus on poverty, education, gender equality, health, environment.
- Successful in reducing poverty & improving education.
2. Sustainable Development Goals (SDGs)
🔹 Introduction:
Adopted in 2015, the SDGs are a universal call to end poverty, protect the planet, and ensure peace and prosperity by 2030.
🔹 17 Key SDGs:
| Goal | Objective |
|---|---|
| SDG 1 | End Poverty in all forms everywhere |
| SDG 2 | Zero Hunger |
| SDG 3 | Good Health and Well-being |
| SDG 4 | Quality Education |
| SDG 5 | Gender Equality |
| SDG 6 | Clean Water and Sanitation |
| SDG 7 | Affordable and Clean Energy |
| SDG 8 | Decent Work and Economic Growth |
| SDG 9 | Industry, Innovation, and Infrastructure |
| SDG 10 | Reduce Inequality within and among countries |
| SDG 11 | Sustainable Cities and Communities |
| SDG 12 | Responsible Consumption and Production |
| SDG 13 | Climate Action |
| SDG 14 | Life Below Water |
| SDG 15 | Life on Land |
| SDG 16 | Peace, Justice, and Strong Institutions |
| SDG 17 | Partnerships for the Goals |
🔹 Targets:
- 169 specific targets across 17 goals.
- Comprehensive focus on economic, social, and environmental sustainability.
🔹 Key Features:
✅ Universal Applicability: Applicable to all countries.
✅ Integrated Approach: Balances economic, social, and environmental dimensions.
✅ Leave No One Behind: Inclusive and equitable growth.
✅ Key for Exams:
- 17 Goals with 169 Targets set in 2015, aimed for 2030.
- Focus on broader issues: Poverty, Health, Education, Environment, Justice, Partnerships.
- SDGs are more comprehensive and interconnected than MDGs.
Comparison: MDGs vs. SDGs
| Aspect | MDGs (2000–2015) | SDGs (2015–2030) |
|---|---|---|
| Number of Goals | 8 | 17 |
| Number of Targets | 21 | 169 |
| Focus | Poverty, Health, Education, Gender | Poverty, Health, Education, Gender, Environment, Justice, Economy |
| Scope | Developing Countries | Universal (All Countries) |
| Approach | Top-Down | Participatory, Inclusive |
| Monitoring | Limited | Robust, Annual Voluntary Reviews |
| Key Achievement | Poverty Reduction | Comprehensive Sustainable Development |
Key Takeaways for Competitive Exams:
✅ MDGs = 8 Goals (2000–2015) → Focused on Basic Human Rights.
✅ SDGs = 17 Goals (2015–2030) → Comprehensive Global Sustainability Agenda.
✅ SDGs Cover New Areas: Climate Action, Sustainable Cities, Responsible Consumption.
✅ SDGs Encourage Partnerships: Global collaboration for development.
✅ “Leave No One Behind” = Core Principle of SDGs.
