ENGLISH CHN-2-UNIT NO.2-HEALTH CARE DELEIVERY SYSTEM
CHN-2-UNIT NO.2 Health care delivery system
Health care delivery system
a) Heath care concept and trends
b) Health care services – Public sector, Rural,
Urban
c) Private sector
d) Public Private Partnership (PPP)
e) Other agencies
f) Indigenous systems of medicine Ayurvedha,
yoga, unani, siddha and homeopathy
(AYUSH)
g) Voluntary health services
h) National Health Programmes
i) Nurse role in health care services
HEALTH CARE DELIVERY SYSTEM
💜 Health for all by 2000 AD
In 1978, the Indian government prepared a national health policy for the recommendations made at the international level conference held in Alma Ata to ensure that every citizen of its country lives a healthy life, is free from diseases and is healthy by the year 2000. In which it was decided that work would be done for the achievement of health for all by 2000 A.D. The Indian government decided to achieve certain goals in the national policy, which were decided to achieve each goal by 1985-95 and 2000.
Community health care is a holistic approach to health care delivery that focuses on improving the health and well-being of the individual and the community.
Here are some key points related to community health care,
1.Preventive care
Community health care emphasizes preventive measures, such as health education, screenings, vaccinations and lifestyle interventions that promote wellness and prevent disease before it occurs.
2.Population health
It identifies the health needs of entire populations or communities, considering factors such as demographics, socioeconomic status, environmental conditions, and access to health care services.
3.Health promotion and education
Health care promotes health literacy.
It enables individuals and communities to be informed about their health.
Involves health education campaigns, community outreach programs, and partnerships with local organizations to promote healthy behavior.
- Interdisciplinary collaboration
Involves collaboration among health care providers.
In order to meet the health needs of the community, collaboration between health care providers, public health agencies, community organizations, and other stakeholders is involved.
5.Health equity and social justice
The aim of community health care is to improve the health status of the people of the community by providing proper health care services, which includes providing health care services to all individuals without considering their economic status, caste, sex or other factors, thus providing health equity.
Factors such as poverty, education, employment etc. affect the status of health.
Community engagement and empowerment
Community health care engages members of the community as active participants in their own health and the health of their community, including building trust, encouraging participation and making individuals and communities aware of their health needs and priorities,
7.Health systems strengthening
Community health care contributes to the overall strengthening of the health care system by promoting integration, co-ordination and continuity of care at various levels of health delivery, from primary care to specialty services.
Adopting these concepts, community health care strives to create healthy communities, improve the quality of life, and reduce the burden of disease through a collaborative, patient-centered, and culturally sensitive approach to health care delivery and promotion.
Community engagement and empowerment
→ How will we achieve these goals??
ANC care – Care of the mother at risk
Obstetric assistance
Postpartum care
Clean five
Trained staff
Newborn care including,
cry the baby
dry the baby
feeding
protection
immunization- according to the national immunization schedule
Nutrition- regularly weaning diet
Immediate treatment at risk – APH
PPH
6. Adolescent care including, intellectual solution of mental confusion
Family planning services (family planning)
oral pills
Coper-T
Condom
Temporary and permanent method of female and male
MTP
Life-threatening disease
Timely treatment and prevention of HIV
Action to provide financial assistance and cheap fast transport to the poor during illness
Geriatric care
Social pollution
Daughter’s Neglect
Hatred of women
Dowry
Some internal grudges
🧡Health care concept and trends change
Comprehensive care
The issues of the report of the first Bhore Committee in 1946 which have been included in the five year plan are as follows.
- It was decided to provide adequate preventive, curative and promotive health care.
It was decided to provide maximum health benefiting services.
A plan was made to work in such a way that there is coordination between the services provided to the people and the profession.
Pay attention to the capacity of the professional worker and make the worker capable of providing services to the people. 5. Plan the service keeping in mind the vulnerable and weak groups.
- Provide a health full environment at home and workplace. B. Basic health services
There should be a co-ordination unit between the peripheral area and the intermediate health unit so that effective care can be provided to the clients in their area.
This term was used by UNICEF/WHO in their joint health policy in 1965.
They have defined basic health services as follows.
✨️Definition
Basic health services is understood to be a network of a co-ordinate, peripheral and intermediate health units capable of effectively performing over a selected group of functions essential to the health of an area and assuring availability of competent professional and auxiliary personnel to perform these functions.
Basic health services are understood to be a network of co-ordinated, peripheral and intermediate health units capable of effectively performing over a selected group of functions essential to the health of an area and assuring availability of competent professional and auxiliary personnel to perform these functions.
Drawbacks of basic health services
Lack of community participation
Lack of intersectoral coordination
Dissociation from socioeconomic aspects of health
Primary health care
Primary health care is essential health care, which is universally accessible to individuals and acceptable through their full participation and at a cost that the community and the country can afford.
Concepts
Affordable to the country and Community
Universally accessible to all citizens of the country
It should be available irrespective of whether it is a rural or urban area, rich or poor community.
It should be socially acceptable on the basis of practical and scientifically sound technology.
Responsible to the health care agencies of the country Goals
The main goal of primary health care is to fulfill the global commitment of HFA (health for all) by the year 2000 AD. To achieve improved health and quality of life for all people through self-reliance.
Thus putting people’s health in the hands of the people.
Strategies
To strengthen the existing infrastructure of the health care system by providing training to the people and to increase the strength of health care workers, so that health services can reach rural areas and at the basic level.
Objectives
To reduce the incidents of communicable and non-communicable diseases.
To sustain population growth through available resources.
To reduce morbidity and mortality rates in infant and preschool children.
To improve the health care level of the community.
To expand essential health care services in rural areas and underserved areas.
Improvement of basic sanitation
Components of primary health care
There are eight essential components of primary health care.
Education, concerning, Prevailing health problem.
To educate the people and health workers and to inform them about health problems and to make them aware of problem solving measures for their prevention and control.
Promotion of food supply and proper nutrition.
Providing information about food, including the importance of food components in the body and what is proper nutrition? What is a well-balanced diet? And its importance, body structure and the importance of food in the growth and development of the body, as well as providing an understanding of what a healthy diet should be.
Adequate supply of state water and basic sanitation
Including explaining how to purify drinking water, household methods of water purification and ideal wells and wells. In basic sanitation, providing advice on proper use and disposal of sewage water in sewage disposal, waste burning methods and kitchen gardens.
Maternal and child health including family planning
Antenatal care – prevention of anemia
Intra natal care – high risk mother’s care, mother’s weight record
premature labour
new born care including breast feeding
immunization, weaning, supplimentry food and family planning
5.Immunization Against Major Infectious Disease
To provide protection from six killer diseases, including…
Diphtheria
Tetanus
Purtusis
T.B
Polio
Measles
Prevention and control of disease
Diseases such as cholera, chikungunya and dengue fever, which should be prevented and controlled.
7.Treatment of communicable disease
Treatment of communicable disease, including minor treatment of various injuries. In addition, treatment of respiratory disease, common cold etc., and provision of essential drugs.
Control of common diseases and basic prevention.
8.Provision of essential drugs:
– Make all necessary medicines available.
Principles
There are five principles of primary health care which were given by WHO.
Which are as follows-
equitable distribution
community participation
appropriate technology
focus on prevention
intersectoral coordination
👉Equitable distribution
Health care services should be distributed equally on all sides.
In which health care services should be provided without considering any caste, creed, gender, religion, rich, poor, urban or rural creed.
Primary health care should be available to individuals, families and communities, which should be based on social justice.
People who live in rural areas should have a target to get primary health care.
👉 Community Participation
It is difficult to achieve the goal of primary health care without community involvement, so efforts should be made to achieve community involvement, planning and implementation as well as maintenance of health services. Efforts should be made in this so that community involvement can happen. Health care workers who belong to the village should be involved such as village health guides, angadwadi workers, ASHA and trained dai who can provide health care services so that there is no cultural or language barrier.
👉Appropriate technology
To provide primary health care, appropriate technology should be used which is socially acceptable, safe and can be used as required within financial limits.
Such as ORS which is an example for the treatment of Diarrhea.
👉Intersectoral coordination
For the implementation of successful primary care, coordination of other sectors is necessary such as, agriculture, sanitation, housing, nutrition, public works, communication and education.
Working groups were formed in 1996 to address the needs and challenges so that a total comprehensive review of the current health situation could be taken.
The areas included are…
Communicable diseases
Health system and biomedical research development
Indigenous system of medicine
Environmental health
Health education and information education and communication (IEC)
Women’s empowerment
Requirement of supportive and diagnostic services in primary, secondary and tertiary care
💛 Level of Health Care (Level of Care)
Health services are generally organized at three levels. Each is supported by a higher level to which the patient can be referred. The levels are as follows.
(1) Primary health care.
(2) Secondary health care.
(3) Tertiary health care.
(1) Primary health care ():
This is the first level between the patient & the health care system where essential health care is provided. Most health problems are solved at this level. This level is closest to the people. This level is provided by PHC and its sub-centers. Treatment of common diseases like fever, cold, minor ailments etc. is done here.
(2) Secondary health care:
At this level, care is provided to patients with more problems. At this level, essential curative care is provided, and is provided by Community Health Centers. This level works for the first referral unit in the health system. Which provides Intermediate Health care. Which includes Community Health Center (CHC), Sub-District Hospital, and District Hospital. Some more complex problems are solved here.
(3) Tertiary health care:
Super specialist care is provided at this level. This care is provided by regional or central level institutions. These institutions not only provide highly specialist care, but also provide care and teaching by trained and specialized staff and research is done. At this level, if there are any questions from the primary level, they are solved. AIIMS, regional hospitals etc. provide tertiary health care.
HEALTH CARE MODEL IN INDIA
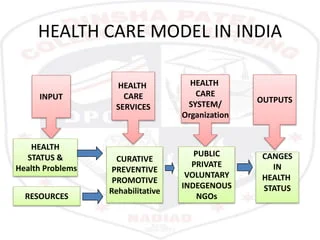
Inputs
Inputs include considering the health status and health problems of the community. Which represents the health needs and health demands of the community. To maintain good health, manpower required resources such as finance equipment and supplies which are limited, hence the health needs of the population increase which cannot be fulfilled, hence careful planning, good managerial skills are essential to fulfill the health needs of the community.
➡️Health status and health problems
The data that judge health status and health problems are as follows,
morbidity and mortality statistics
Demographic condition of the population
environmental condition which influences health status.
Socioeconomic factors which directly affect health.
cultural background, attitudes, beliefs and practices which affect health.
Availability of medical and health services
other services available
Health status and health problems can be analyzed through data. After that, the problem is given priority according to rank.
Resources are allocated on the basis of priority.
The current demographic and mortality profile and health problems in India are discussed below.
Demographic profile
Population explosion is one of the biggest problems of the country.
Demographic profile is characterized as follows,
large population based
High Fertility, both in terms of birth rate and family size
Low or declining mortality
Young age below 15 years, which is approximately 27.6% of the total population.
The illiterate population is close to 34.62%, explain the decline in birth rate, which has been so slow
dependency ratio 54.14 per 100 as per the census 2011, that is every economically productive member has to support almost one dependent. Mortality profile
Death rate has declined from 21 to 7.
Life expectancy has increased since 1951.
There has been a decrease in the cases of malaria, cholera and tuberculosis.
🤒Health problems
The major health problems seen in India are as follows:
Communicable disease problems
non communicable disease problems
nutritional problems
environmental sanitation problems
medical care problems
population problems 😷Communicable disease problems
The diseases that are of great importance are as follows,
👉Malaria-
Malaria is a major health problem seen in India but in recent times there has been a decrease in the cases of malaria compared to the past, but in states like Madhya Pradesh, Chhattisgarh, Jharkhand, Orissa, Andhra Pradesh and Maharashtra there has been an increase in the cases of malaria.
👉Tuberculosis
India accounts for one-fifth of the incidence of tuberculosis in the world.
T.B. It increases the severity of other diseases such as HIV and multi drug resistance.
In March 2006, RNTCP achieved nation wide coverage.
👉Diarrheal disease
Diarrheal disease is especially seen in children under five years of age, which is one of the major causes of their morbidity and mortality.
👉Acute respiratory infection
Acute respiratory infection is also seen in children under five years of age, which is one of the major causes of their morbidity and mortality.
👉Leprosy
Leprosy is another health problem seen in India.
👉Filaria
Filaria is endemic in about 255 districts of 16 states and 5 union territories.
Of which more than 633 million population is at risk.
👉AIDS
AIDS is relatively stable in India.
👉Others
Other important communicable diseases found in India such as Kala Azar, meningitis, viral hepatitis, Japanese encephalitis and enteric fever and helminthic infections are easily treated and prevented with minimum use of resources.
➡️Non communicable disease problems
In 2012, it was estimated that 60% of all deaths were due to non communicable diseases.
Due to the increase in population and changes in the environment, major health problems such as diabetes mellitus, cardiovascular diseases, cancer, strokes, lung disease and cataract are produced.
✅️Nutritional problems
Specific Nutritional problems are,
protein energy malnutrition (PEM)
Nutritional anemia
low birth weight
xeropthalmia due to vitamin A deficiency
Iodine deficiency disorders
Nutritional problems such as lathyrism and endemic goiter are seen in certain parts of the country.
Environmental sanitation problems
Lack of safe water
Excreta disposal
Population explosion, urbanization and industrialization which cause pollution in air, water and food.
As per 2015, 97% of urban areas and 93% of rural population have access to safe water.
After that, 63% of urban and 28% of rural population have access to adequate waste disposal facilities.
🦷Medical care problems
One of the major health problems in India is the inequitable distribution of health care facilities in rural and urban areas.
Also, health problems are seen due to the lack of availability of health resources.
80% of health facilities are concentrated in urban areas but they are not equally distributed everywhere, and 72% of health facilities are unevenly distributed in rural population of India.
Hence the health for all 2000 AD movement and primary health care approach emphasized on equity, intersectoral coordination and community participation for all which is necessary to remove this imbalance.
😓 Population problems
Currently India is facing population explosion which is a major problem.
Due to population explosion it especially affects employment, education, housing, health care, sanitation and environment.
During 2000 AD the government had set a target of 1% population growth in the whole year which was not achieved.
The size and structure of population are important factors affecting manpower planning as well as health.
🏞Resources
To meet the health needs of vast community, resources are required.
Basic Resources for providing health care
health manpower
money and material
time
💚 Health care services
💖 Primary Health Centre (PHC)

PHC was established by the Bhore Committee to provide health services in rural areas.
In plain areas, there is one PHC for every 30,000 population.
In hilly and tribal areas, as well as in backward areas, there is one PHC for every 20,000 population.
On 30 June 1999, 22087 PHCs were opened in All India.
Set up of PHC
There is one PHC for every 20 to 30 thousand population.
First of all, this area should be divided into four sub-units.
The village should be located in the middle and the surrounding people can easily reach it.
In this village too, according to the geographical conditions, it is not too far from the population and there is no dense population such as a market shopping center, which is not a hindrance, and also a place where basic needs can be easily found at this place and vehicles can be moved for referral services.
In addition, the PHC facility should have facilities such as waiting room, office room, OPD room, examination and consulting room, dispensary and laboratory room, dressing room, minor O.T. In addition to indoor room with 4 beds, labor room, recovery room, water room etc.
Plant flowers or trees in the PHC ground to purify the air and make arrangements to provide shade in summer. In short, the PHC should be set up in such a way that the beneficiary who comes is comfortable in every way.
Staffing pattern of PHC
M.O. – 1
Pharmacist- 1
Nurse midwife- 1
Female health worker- 1
Male worker-1
Block extension educator (BEE) – 1
Health assistant – 1
Female health supervisor or H.V – 1
Clark (senior) – 1
Lab technician – 1
Driver – 1
Class 4 – 4
💛 Functions of PHC (Functions of Primary Health Center)
Medical care
MCH and Family planning
Improvement of environmental sanitation
Control and surveillance of communicable disease
Collection and reporting of vital statistics
National health programme
Health education
Training of health personnel
School health services
Referral services
👉1. Medical care
Medical care involves providing care to the patient such as tablets, injections, dressings etc. according to his disease.
Apart from this, preventive, promotive care and treatment of minor diseases are also included in MCH.
👉2. MCH and Family planning
MCH also includes RCHH, in which treatment is provided from mother’s reproductive child health to adolescence care.
In this, care is taken regarding mother’s ANC care, nutritional care, hygiene, immunization, lab examination etc.
In the post natal period, regular checkup, observation, health talk, diet menu as well as surveillance health talk diet menu as well as FP in which temporary method is explained in case of primy para and permanent method is explained in case of multi para.
👉3. Improvement of environmental sanitation
In this, steps are taken to maintain environmental cleanliness.
Also, people are made aware of basic sanitation, including excreta disposal, use of laterine, storage of water, cleanliness and kitchen garden.
In addition, there should be drinking water wells and taps for safe water supply, in which household methods such as boiling, bleaching powder and chlorine tablets should be used.
👉4. Control of surveillance of communicable disease
Survey of communicable disease and take steps to control it.
👉5. Collection and reporting of vital statistics
This includes birth rate, death rate and knowing the cause of death if any, as well as marriage report, epidemic, notification of communicable disease.
👉6. National health programme
The National Health Programme has important functions.
All health-related services are provided in the clinic, in which PHC has intensive operations.
👉7. Health education
People are given health education, health education is provided as per the requirement to remove some of their misconceptions… For example, bananas, papaya or brinjal should not be eaten during pregnancy.
👉8. Training of health personnel
Trained birth attendant, ASHA (Acridited Social Health Activist) etc. to be trained.
Training of all health personnel, refresher training in all health programs.
👉9. School health programme
School health programme is organized every year for health check-up of children of primary school.
Minor or major problems are detected and treated through health check-up in children of 5 to 14 years.
All staff besides the M.O. of PHC are involved in the school health programme.
The main objective of the school health programme is to improve the health status of children of 5 to 14 years through health services.
👉10. Referral services
Referral services are important in the functioning of PHC.
If necessary, referral is made to another unit for primary care.
If a specialist is needed, the patient is sent directly to the specialist from the PHC.
Only if referral is made in time can the patient’s life be saved.
💖 Subcenter
Subcenter is also a unit under PAC. Subcenter is a Peripheral unit in health care. In its general population, for every five thousand population and in tribal and backward areas, there is one subcenter for every 3,000 population. Each subcenter has one male and one female MPW.
Functions of Subcenter
MCH and RCH services
Family planning
Immunization
Treatment of minor illness
Prevention and control of communicable disease
Dai training
Nutritional services (distribution of IFA, calcium, vit-A solution).
Water sanitation
Simple lab investigation
Referral services
Record and reports Setting pattern of Subcenter
MPW – 1 (male)
MPW – 1(female)
Village health guide – 1(VHG)
Trained dai – 1
💖 Village level
Different categories of persons provide health services at the village level.
Village health guide (VHG).
Trained birth attendant (TBA)
Aangad vadi worker (AWW)
ASHA
Village health guide
The VHG team was established on 2 October 1977. For this, initially only females were selected but from 1986 the government of India decided that males can also be placed as VHGs. The selection of VHGs is done from the local area. There is one VHG for every 1000 population. This VHH acts as a link between the community and the government infrastructure.
✅️Training for VHG
A total of 200 hours of training is given at Subcenter and PHC, that is, there is an approximate three-month training. A stipend of Rs. 200 is given during the training. After completing the training, a medicine kit is given, along with a manual book, which can be used to provide health services. He has to work for two to three hours a day. He solves small health problems in his area. In the Ninth Five Year Plan, emphasis was laid on preparing VHG and a goal was set that there should be one VHG for every 1000 in each area.
✨️Medicine kit for VHG
Medicines :-
Tab CHQ (chloroquine)
Tab PCM and cough syrup
ORS packets
➡️External use
Antiseptic lotion
Ointment
Mercurochrome
P.P. lotion
Sulphacetamide
Eye and ear drops
Bliching powder
➡️Equipment
-Pencil
-Clinical thermometer
-Cotton gauge
-Roller bandage
-Triangular bandage
-Adhesive tap
-Soap and soap dish
-Towel and napkin
-Condom and pills 💊
-Notebook and dairy
-Health education material
➡️2.TBA (Trained Birth Attendant)
This TBA is a trained dai. Through this dai, the concept of MCH can be conveyed to the people more strongly. This TBA performs the important work of registration, observation, bed side care and child care of the Antenatal mother in his area.
✅️Training
👉1. There is a 30-day training.
👉2. During the training, he is provided with knowledge about delivery, immunization, Antenatal care etc. at PHC and Subcenter. In which he has to work in the field area with FHW for two days in a week and four days.
👉3. During the training, he has to attend at least two deliveries under supervision and during the training, emphasis is also laid on safe hygienic conditions. So that MMR can be reduced.
👉4. After successful completion of the training, a certificate and delivery kit are given.
👉5. This trained dai works to create awareness for small family norms in his area.
Accredited Social Health Activist (ASHA)
The post of ASHA was created under the National Rural Health Services also known as NRHM.
1000 population is one ASHA.
👉Selection of ASHA
She is selected from the same community.
She should be married/divorcee/widow.
Her age should be between 25 to 45 years.
She should have at least 8th standard education.
She should be known for her communication and leadership skills.
ASHA is a volunteer worker, who is not paid any salary.
She is provided with traveling allowance (TA), dearness allowance, awards and non monetary incentives.
➡️Role and responsibilities of ASHA Asha will be a health activist who will spread awareness about health issues in the community. His responsibilities are as follows:
He will spread awareness and give instructions to the community about health, nutrition, personal hygiene and sanitation.
He will provide counseling to women on safe pregnancy, delivery, breastfeeding and complementary feeding and immunization contraception and prevention of common infections such as Reproductive tract infections and care of young child.
He will advise women to adopt small family norms.
He will keep essential medicine like ORS, iron and folic acid tables, chloroquine tablets, oral pills, condom and disposable delivery kit in his depot holder.
He will mobilize the community to provide health services at sub center and primary health care center.
He will provide necessary treatment to pregnant women.
He will provide primary medical care for fever, diarrhea and first aid for minor injuries.
He will be a provider of directly observed treatment short course (DOTS) under the national tuberculosis control program.
It will provide information about death, birth and health related problems to the sub center and primary health center.
Under the sanitation campaign, it will promote the construction of house hold toilets.
It will work with the village health and sanitation committee of the Gram Panchayat to develop a comprehensive village health plan.
ICDS(Integrated child development services)/ Anganwadi worker
ICDS was established on 2 October 1910 in Chhota Udepur taluka in Baroda district of Gujarat. Initially, only children were beneficiaries of ICDS. But later, the committee that was formed included Antenatal mother, postnatal mother and adolescent girls along with children.
Objective
To improve the health of children between the ages of one and six.
To reduce the rate of morbidity and mortality in children.
To coordinate with the organization working for the development of children.
To provide health education to maintain the nutritional status of mothers and every woman between the ages of 15 and 45.
To decrease school dropout rate. Selection
A person from the same village is selected. (Especially women)
Training covers health, nutrition and child development and non-formal education is taught.
It is a part-time worker and his qualification is 10th standard pass, his helper is 7th standard pass.
There is one Anganwadi for every 1000 population. And in one Anganwadi there is one AWW and helper.
What services are provided in Anganwadi…?
Health check-up
Immunization
Supplementary nutrition
Health education
Referral services and other services
Urban
CHC
Hospital
Special Hospital
💖 CHC
By 31 March 2003, another 3076 PHCs were upgraded.
One CHC is for a population of 80,000 to 12,000 thousand.
There are 30 beds in CHC.
In which, X-Ray, laboratory, gynec and pediatrician facilities should be available.
In addition, X-Ray, laboratory services are available and for promotive aspect as well as for totally health care, a new non-medical post is created, which is known as community health officer. Who is selected from the category of PHC staff who should have at least 7 years of experience in rural health.
From CHC, patients can also be referred directly to state level hospitals, which is based on the need of the patient.
👉Staffing pattern of CHC
medical officer- 4
Nurse midwife- 7
Pharmacist- 1
Laboratory technician-1
X- ray technician-1
Ward boy-2
Dhobi-1
Swiper- 3
Mali- 1
Watchmen-1
Aaya ben- 1
Driver- 1 Peon- 1
👉Function of CHC
Emergency and medical care MCH and family planning services School health program improvement of environmental sanitation control of communicable disease vital statistics (collection of vital statistic) National health program training of health person administrative work organization of various Diagnostic camp
✅️Objective of CHC
To provide total family care in its area.
To provide primary health services.
To provide minor surgery and special services such as facility for minor operation, treatment of children by gynecologist facility.
Provides preventive and promotive care with the help of medical personnel and other staff. Provides refresher services.
💖 District hospital or Hospital
It works differently from a health hospital such as,
Curative services,
Preventive and curative services, all these services are integrated.
2.It does not have a specific area.
3.The hospital is responsible for any area of the community, which is responsible for every population.
4.The hospital staff consists of a team of curative staff, such as doctor, staff nurse, pharmacist, laboratory technician and other specialist. Teaching hospital✨️ which has branches of specialty as well as all therapies, research department as well as various teaching colleges such as dental, aayurvedic, homeopathic, physiotherapy, pharmacy, medical etc…
Health insurance scheme
There is no universal health insurance scheme. Currently, there is a limited scheme for industrial workers and their family members. In addition, the Central government has also covered it under the banner of the scheme for central government employees.
💖 ESIS(employee state insurance scheme)
💖 Central government health insurance scheme-
Central government employees are covered under this scheme. This scheme was first started in Delhi in 1954, in which employees are provided comprehensive care, medical care etc. Both employee and employer are covered in this scheme.
✅️Benefit
A network of mobile dispensaries has been set up for out patient care.
Supply of necessary drugs
Domiciliary visit
Hospitalization facility
Specialized consultant
MCH services
- Investigation facility…(laboratory and X-Ray)
Emergency treatment
Family Welfare services
In this scheme, employees as well as autonomous organizations as well as retired persons and employees’ spouses are eligible to get this benefit. Under this Central government health insurance scheme, besides Delhi, cities like Allahabad, Kanpur, Patna, Meerut, Kolkata, Bhubaneswar, Nagpur, Hyderabad, Bangalore, Jaipur, Pune, Lucknow and Jabalpur have been covered.
💖 Public Private Partnership
Public-private partnerships (PPPs) in health involve collaboration between government agencies and private sector entities to improve healthcare delivery, infrastructure, financing, and innovation. Here is how PPPs are applied in the healthcare sector:
Health infrastructure development:
PPPs are used to develop, upgrade, and operate healthcare infrastructure such as hospitals, clinics, diagnostic centers, and medical colleges.
Private sector partners often invest in the construction, maintenance, and operation of healthcare facilities, while the government provides land, regulatory support, and oversight.
Service delivery:
PPPs involve the delivery of healthcare services through joint ventures between public and private entities.
Private healthcare providers may provide services in public hospitals or primary health centers through contracts or agreements with the government, supplementing existing public healthcare services.
Health Financing:
The objective of PPPs in health financing is to mobilize private sector resources to supplement public funds and expand access to healthcare services.
Public-private health insurance schemes, subsidized health insurance schemes, and community-based health financing initiatives are examples of PPPs that aim to reduce out-of-pocket costs and provide financial security for healthcare costs.
Technology and Innovation:
PPPs promote collaboration between government agencies, private companies, research institutions, and non-profit organizations to develop and deploy innovative healthcare technologies, products, and services.
Joint research and development projects, technology transfer agreements, and public-private partnerships for vaccine development and disease control are examples of PPPs in healthcare innovation.
Capacity Building and Training:
PPPs support capacity building and training programs for healthcare professionals, administrators, and support staff to enhance skills, knowledge, and competencies.
Private sector partners can contribute expertise, resources, and training facilities to support workforce development initiatives in collaboration with government agencies and educational institutions.
Health Promotion and Education:
PPPs promote health education, awareness campaigns, and community outreach programs to improve health literacy and promote healthy behaviors.
Private sector organizations, non-governmental organizations (NGOs), and community-based organizations collaborate with government agencies to design and implement public health initiatives targeting specific health problems or population groups.
Regulatory Framework and Governance:
Effective governance structures, regulatory frameworks and monitoring mechanisms are essential for the successful implementation of PPPs in health.
Governments establish policies, guidelines and legal frameworks to govern PPPs, ensure transparency, accountability and adherence to quality standards, and mitigate potential risks and conflicts of interest.
PPPs in health offer opportunities to leverage the strengths and resources of both the public and private sectors to improve access, quality and efficiency of healthcare, ultimately contributing to better health outcomes for the population. However, careful planning, stakeholder engagement and monitoring are required to ensure that PPPs are aligned with public health goals, prioritize equity and deliver sustainable benefits to communities.
➡️Other agencies
👉A. Health care for railway employee
Railway hospital provides comprehensive care, and railway health unit is set up and service is provided. At places like big railway stations, sanitary inspector and environmental sanitation are maintained. Also, the work of the division is supervised by the chief health inspector. In the work of health, periodic check-up of the employee is done and records are kept. Apart from that, if a new worker comes, his physical fitness is also done and check-up is done and records are kept. There is an indoor hospital for the facility of revisional office health, every facility is available in it.
👉B. Private sector
In which allopathic, homeopathic, Ayurvedic, all practitioners provide health services. All these have private services which are constituted by the medical council of India and practice subject to this constitution.
👉C. Defense medical services
Which runs its own organization in the name of arms force medical services which is an organization constituted by the defense services. Provides services to persons associated with defense. Which also includes preventive and curative services along with integrated and comprehensive care. It provides services to the person connected with the Arm force and provides all kinds of services to his entire family.
👉D. Indigenous system of medicine
This includes different branches of medicine such as allopathic, homeopathic, Ayurvedic and unani system of medicine etc. Practitioners of the above different branches of medicine provide services to the people of rural areas. Based on the study, it has been concluded that 90 percent of Ayurvedic doctors provide services in rural areas only, who live there and are in close contact with the public. Due to this, many state dispensaries were started by the state government and the National Institute of Ayurveda was established in Jaipur by the government of India. In addition, the National Institute of Homeopathy was started in 1972. The best health care can be provided through this indigenous system of medicine.
Voluntary health agencies or organization
Indian red cross society
Bharat Sevak Samaj
Kasturba Memorial Fund
The hindu kasht nivaran sangh
Tuberculosis association of India
Indian council for child welfare
Family planning association
All india women’s conference
All india blind relieve society
The central social welfare board
Professional bodies 1. Indian red cross society
Started in 1920, it has more than 400 branches in India. Its activities are as follows.
Activities
Relief work provides relief work during floods, droughts or earthquakes. At such times, food, clothes and all necessary things are delivered to the needy. In addition, it works during epidemics or epidemics.
Milk and medical supplies Hospital maternity home, children welfare center, school, orphanage etc. It supplies milk powder and vitamins.
Care of the sick and disabled soldiers is closely associated with the soldiers injured in the war.
Provides services to the soldiers and for those who are permanently disabled, there is a red cross home in Bangalore. Which works to protect such soldiers throughout their lives.
Maternal and child welfare services
Providing technical advice to such centers to set up maternity homes and child centers.
All India runs many such centers.
Family planning
Provides family planning services at its center, as well as organizes camps.
Research
Helps in research activities. Distributes materials for child care and mother graft, besides, chent Jones ambulance association which runs first aid classes for men. Also runs nursing courses for women.
Provided scholarship for nurses to study further.
Junior red cross is a branch for children which gives boys and girls the opportunity to work during epidemics.
Also gives the youth an opportunity to live with brotherly feelings and provides first aid treatment.
Blood bank
Runs first aid and blood bank.
Maintains a list of donors.
Provides all services when needed.
Government of India gives grants to red cross society for help.
Sent Jone association which is a part of red cross.
Bharat Sevak Samaj
This organization was started in 1952, it is a none political and non official organizer, its main objectives are as follows.
People should work for their own health.
Does voluntary work for environmental sanitation in villages.
Plans camps for teachers, young and collegiate students. In this way, it does various activities. 3. Kasturba Memorial Fund
Started in 1944 in praise of Kasturba Gandhi.
It was established to do social welfare work for women.
It provides necessary tools for the purpose of empowering village women and for industries.
Apart from this, other agencies also provide funds for the advancement of women.
The Hindu Kasht Nivaran Sangh
It was established in 1950 but originally it was started and inaugurated in 1925 under the name of Indian Council of the British Empiyer Leprosy Relieve Association.
It was established in 1950 under a new name, in which government and voluntary agencies work together.
Activities
To work for Leprosy.
To prepare material for health education for Leprosy.
To provide financial assistance for Leprosy programs.
To publish a magazine.
To open rehabilitation centers in hospitals and clinics for Leprosy.
To carry out research and investigation work for workers.
Tuberculosis Association of India
Established in 1939.
It has an organization in each state, which does different work and collects funds.
Objective
To conduct antituberculosis training
To conduct health education
To conduct clinics and conferences
To publish publications related to TB
To find out TB cases and provide treatment.
Indian Council for Child Welfare
Established in 1952
It is affiliated with the International Union for Child Welfare which works with about 70 national voluntary agencies,
The main objective of which is to provide a normal and healthy environment for the physical, mental, and social health of thousands of children in India.
This organization works to help them, in addition to organizing conferences, annual meetings and other programs to create awareness among the people and the government for the integrated child welfare program.
Family Planning Association
The organization was established in 1949.
It works as a founder in family planning services.
It also helps in providing training for family planning.
For which it has trained many doctors, health visitors and social workers.
All India Women’s Conference
This organization was established in 1926.
It is a voluntary organization only for women.
It has branches in every state.
It runs an MCH clinic and a women’s group.
It runs Mother Craft.
It organizes kindergartens and carries out activities such as adult education and distribution of milk, besides providing family planning services.
All India Blind Relief
This organization was established in 1946 with the aim of improving the condition of blind people.
This organization runs blind relief camps and also does welfare work to provide facilities to help blind people.
The central social welfare board
The Central Social Welfare Board was formed in 1953 and social voluntary agencies like Mahila Mandal, Jaycees Club etc. were formed by this board.
75% grant is given for it, through which different programs are organized like,
Nutrition program, ICDS and many other activities like working women’s hostel, physically handicapped, old age home and services for the welfare of socially backward people are planned.
It came into existence as an independent body in 1968, which is managed by the Ministry of Education, which was started for MCH in rural areas, by doing activities like home industry, sewing, handicrafts, match making etc. and earning income for their families.
Professional bodies
Which publish magazines related to their profession.
General publications.
Organize scientific sessions and maintain the standards of professional organizations.
👉Functions of voluntary health agencies
To provide personal assistance to official agencies and help by providing funds for special equipment.
To help in research.
To provide material for health education and work for mass health education.
To prepare experimental projects and demonstrate them.
To praise the workers of official agencies by giving good examples.
To encourage them to bring forward health legislation.
Nurse’s role in health care services
A nurse plays a key role in the activity of health care services.
She has a specific role in the health care setting and health care services.
Her main tasks and abilities are as follows.
Knowledge
She should have knowledge of the health services she is providing, and she should be familiar with the target of health care services.
Participation
She has participation in the planning, implementation and evaluation of health care services.
Policy
She should be aware of the policy of the work she is doing.
And should have knowledge about the tasks.
Referral system
She should create a link for referral services.
Advance technology
She should be familiar with advanced technology and knowledge.
The patient should be treated according to new techniques.
Resources The resources for health care services should be used as much as possible.
Demonstration
To provide better service, demonstrate the care of sick people at home and at the clinic.
Health team
She is an important person in the health team.
Therefore, she should work responsibly and help in a way that unity is maintained in the team.
Health education
Wherever she works, she should provide health education to the individual, family, society or co-workers.
She should make a new plan and implement it.
Training of co-worker
Give training to the workers working with her and take responsibility for supervision.
Record and report
She should maintain a record and report of her proper performance.
Which is useful for evaluation and future planning.
Skill develop
Develop different skills in herself and use health care services.
Direct care provider
She is a direct care provider in her area, so she should provide all health services. For example, MCH
Educator
should provide health services as a teacher and educator in the community of his/her area.