UNIT-2-NUTRI.DIET-NOTES:-
🌿 Introduction to Diet Therapy 🌿
Diet therapy is a scientific and therapeutic approach that uses planned and regulated diets to treat or prevent diseases. It involves modifying the normal diet according to the patient’s medical condition and nutritional needs. 🍎
💡 Meaning
Diet therapy means the use of food as a tool of treatment. It’s not just about eating right — it’s about eating specifically for recovery, healing, and maintaining health. It plays a vital role in hospitals, nursing care, and rehabilitation. 🏥
🥗 Definition
➡️ Diet therapy is the adaptation of the normal diet to meet the nutritional needs of individuals suffering from diseases, to correct deficiencies, and to prevent complications.
🎯 Objectives of Diet Therapy
- 🍞 To maintain good nutritional status even during illness.
- 🩺 To correct nutritional deficiencies like anemia, protein deficiency, etc.
- 🧠 To help the body’s metabolism and promote tissue healing.
- 💊 To prevent further complications due to improper diet.
- 🌾 To modify existing diet plans according to the disease condition (e.g., diabetes, hypertension).
- ❤️ To restore health and improve the patient’s quality of life.
🧩 Principles of Diet Therapy
- 🥣 Individualization: Every diet plan is tailored according to the patient’s disease, age, sex, and activity.
- 🍽️ Simplicity: Diet should be simple, easily digestible, and palatable.
- 🧂 Moderation: Avoid over-restriction unless essential.
- 🧃 Nutrient Balance: Include all nutrients—carbohydrates, proteins, fats, vitamins, and minerals.
- 💧 Hydration: Adequate fluid intake is essential unless restricted.
- 🕐 Regularity: Meals should be given at regular intervals.
🩹 Types of Therapeutic Diets
- 🍚 Clear Liquid Diet – For postoperative or acute illness.
- 🥣 Full Liquid Diet – More nourishment than clear liquid, includes milk, soups.
- 🍞 Soft Diet – Easy to chew and digest; used in recovery.
- 🥗 Regular/Normal Diet – Balanced diet for healthy individuals.
- 🚫 Special Diets – Modified for diseases (e.g., low salt for hypertension, low fat for gallbladder disease, diabetic diet, etc.).
🧬 Modifications in Diet Therapy
Diet may be modified in:
- 🔥 Consistency – Liquid, soft, or solid.
- 🧂 Nutrients – High/low protein, carbohydrate, fat, or salt.
- 💦 Calories – High or low caloric value.
- 🌡️ Method of cooking – Boiled, steamed, baked, or fried.
🌻 Role of Nurse in Diet Therapy
❤️ Motivate patients to follow dietary restrictions sincerely.
👩⚕️ Educate patients about their therapeutic diet.
📋 Ensure correct diet is served to the right patient.
🥤 Encourage adequate fluid intake.
🍽️ Observe and record food tolerance and intake.
🏥 Routine Hospital Diet
A routine hospital diet (also called normal or regular diet) is the standard meal plan prescribed for patients who do not require any dietary modification. It is designed to maintain good nutrition, support recovery, and prevent malnutrition during hospitalization. 🌿
🍛 Purpose
✨ To provide adequate energy, protein, vitamins, and minerals for body maintenance and healing.
✨ To help the patient recover strength and immunity.
✨ To maintain normal body weight and metabolic balance.
✨ To serve as the base diet for modification when specific conditions arise (like diabetic, renal, or cardiac diet).
🥗 Main Characteristics
🌾 Balanced Diet: Contains carbohydrates, proteins, fats, vitamins, minerals, and water in proper proportion.
🍞 Calorie Range: Usually provides about 2000–2500 kcal/day, depending on the patient’s age, sex, and activity.
🥦 Easily Digestible: Foods are prepared to be light, clean, and easily digestible.
💧 Adequate Fluids: Around 2–3 liters of fluids per day, unless restricted.
🧂 Normal Salt Intake: About 5–10 grams per day, unless otherwise advised.
🍳 Normal Consistency: Solid, semi-solid, or liquid depending on chewing and swallowing ability.
🕒 Meal Pattern
🍽️ Generally served in three main meals and two snacks —
- 🌅 Breakfast: Milk, tea, bread, porridge, or eggs.
- 🌞 Lunch: Chapati or rice, dal, vegetables, curd, salad, and fruit.
- 🌇 Evening Snack: Tea, milk, biscuits, or light snacks.
- 🌙 Dinner: Similar to lunch but lighter and early.
🧠 Principles of Routine Hospital Diet
💪 Adequacy: Meets the body’s energy and nutrient needs.
🍎 Variety: Includes food from all five groups for taste and nutrition.
🌿 Hygiene: Prepared under strict sanitary conditions to prevent infection.
🥣 Palatability: Should be appetizing to encourage food intake.
🕰️ Regular Timing: Meals are served at fixed intervals to maintain digestion rhythm.
🍎 Nutrient Composition
🌾 Carbohydrates: Major source of energy (rice, roti, cereals).
🍗 Proteins: For tissue repair (milk, eggs, pulses, meat, fish).
🧈 Fats: For energy and fat-soluble vitamins (ghee, oil, butter).
🥬 Vitamins & Minerals: For metabolic functions (fruits, vegetables, milk).
💧 Water: Maintains hydration and helps in excretion.
🚫 Food Restrictions (if Needed)
⚠️ In some patients, routine diet may be modified —
- 🧂 Low Salt: For hypertensive or cardiac patients.
- 🍬 Low Sugar: For diabetic patients.
- 🥛 Low Fat: For obese or liver disorder cases.
- 🧀 High Protein: For burns or post-surgery healing.
❤️ Advantages
🌟 Promotes quick recovery and maintains nutritional balance.
🌟 Prevents hospital malnutrition.
🌟 Easy to prepare, digest, and modify as per need.
🌟 Maintains patient comfort and satisfaction.
🩺 Nurse’s Role in Routine Hospital Diet
👩⚕️ Assess patient’s nutritional needs and appetite.
🍽️ Ensure timely serving and observe tolerance to food.
📝 Record intake and report any loss of appetite or nausea.
🤝 Encourage the patient to take complete meals for better recovery.
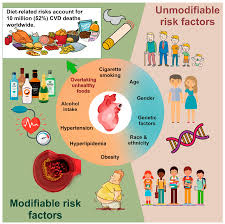
💖 Cardiovascular Diseases (CVDs) Diet
🫀 Cardiovascular diseases are disorders affecting the heart and blood vessels — such as coronary artery disease, hypertension, heart failure, and stroke. Diet plays a crucial role in both prevention and management of these conditions. A heart-healthy diet focuses on reducing fat, salt, and sugar intake, while increasing fiber, antioxidants, and good fats.
🌾 1. Focus on Whole Grains
- Choose whole-grain breads, oats, brown rice, quinoa, and millets.
- They provide dietary fiber, which helps in lowering LDL (bad cholesterol) and maintaining healthy blood pressure.
- Avoid refined products like white rice, maida, or sugary cereals.
🥦 2. Increase Fruits and Vegetables
- Eat at least 5 servings daily 🥗.
- Rich in vitamins, minerals, antioxidants, and fiber — these protect blood vessels and prevent plaque formation.
- Prefer colorful options: spinach, beetroot, carrots, papaya, berries, and citrus fruits 🍊.
🐟 3. Include Healthy Fats
- Prefer omega-3 rich fats such as found in fish (salmon, tuna, sardine), flaxseed, walnuts, chia seeds.
- Use olive oil, mustard oil, sunflower, or rice bran oil instead of butter or ghee.
- Limit saturated and trans fats (avoid deep-fried snacks, bakery items, cream, and processed meat).
🧂 4. Reduce Salt Intake
- Excess sodium increases blood pressure ⚠️.
- Limit added salt, pickles, papad, sauces, and processed foods.
- Use herbs and spices like lemon, garlic, coriander, and pepper for flavor instead of salt.
🍭 5. Limit Sugar and Refined Carbohydrates
- Avoid soft drinks, sweets, pastries, and refined snacks.
- High sugar intake leads to obesity and diabetes, which further increase CVD risk.
- Choose natural sweeteners like jaggery or honey in small amounts if necessary.
🥛 6. Choose Low-Fat Dairy
- Prefer skimmed milk, low-fat yogurt, and paneer made from toned milk.
- Avoid cream, butter, and full-fat cheese.
- Helps maintain calcium without adding excess cholesterol.
🍗 7. Select Lean Protein Sources
- Include legumes, lentils, soybeans, fish, egg whites, and skinless chicken.
- Avoid red meat and organ meats as they are high in saturated fat and cholesterol.
- Plant-based proteins are especially beneficial 💚.
💧 8. Maintain Adequate Hydration
- Drink 8–10 glasses of water daily.
- Avoid excessive tea, coffee, and energy drinks containing caffeine, as they may raise heart rate and blood pressure.
🚭 9. Lifestyle and Meal Pattern Tips
Avoid alcohol and smoking, which directly harm the cardiovascular system.
Eat small frequent meals rather than heavy ones.
Maintain ideal body weight and physical activity (like walking, yoga, or cycling).
🌿 Diet in Gastrointestinal Diseases
🩺 Introduction
The gastrointestinal (GI) tract includes the mouth, esophagus, stomach, intestines, liver, pancreas, and gallbladder.
A proper diet plays a vital role in both prevention and management of GI diseases by reducing irritation, improving digestion, and promoting healing.

🍞 1. General Dietary Principles
✅ Eat small, frequent meals instead of large ones.
✅ Prefer soft, bland, and easily digestible food.
✅ Avoid spicy, oily, fried, or very hot/cold food.
✅ Drink plenty of fluids but avoid carbonated or caffeinated drinks.
✅ Maintain good hydration and fiber balance (as per condition).
✅ Chew food slowly and avoid rushing meals.
✅ Restrict alcohol, tobacco, and high-fat foods.
🧃 2. Diet in Common GI Diseases
🦠 A. Gastritis / Peptic Ulcer
💡 Goal: Reduce gastric irritation and acid secretion.
🍽️ Recommended:
- Milk and milk products (non-fat) 🥛
- Soft cooked rice, porridge, or suji 🍚
- Boiled vegetables, fruits like banana, apple 🍌🍏
- Avoid strong tea/coffee, pickles, and citrus fruits.
🚫 Avoid: - Fried, spicy foods 🌶️
- Alcohol, smoking 🚭
- Carbonated beverages 🥤
💧 B. Diarrhea
💡 Goal: Replace lost fluids and electrolytes.
🍽️ Recommended:
- Oral rehydration solution (ORS) 💧
- Soft, low-fiber diet (banana, apple sauce, rice) 🍌🍎🍚
- Boiled potatoes, curd, toast 🍞
🚫 Avoid: - Milk, fried food, raw vegetables 🧈🥗
- Caffeine, high-fat and spicy food ☕🌶️
🍠 C. Constipation
💡 Goal: Stimulate bowel movement through fiber.
🍽️ Recommended:
- High-fiber foods (whole grains, fruits, vegetables) 🥕🥦
- Adequate water (2–3 L/day) 💧
- Prunes, papaya, figs for natural laxative effect 🍇🍈
🚫 Avoid: - Refined foods (maida, bakery items) 🍰
- Low-fiber diets, fast food 🍟
🤢 D. Nausea and Vomiting
💡 Goal: Maintain hydration and prevent dehydration.
🍽️ Recommended:
- Clear liquids like coconut water, lemon water 🥥🍋
- Bland soft foods: khichdi, toast, soup 🍲
- Eat small frequent meals.
🚫 Avoid: - Strong odor foods, fried items, and caffeine 🧄☕
🔥 E. Gastroesophageal Reflux Disease (GERD)
💡 Goal: Prevent reflux by avoiding trigger foods.
🍽️ Recommended:
- Non-acidic fruits (banana, melon) 🍌🍈
- Lean proteins (chicken, fish, paneer) 🍗🐟
- Avoid lying down after meals 🕒
🚫 Avoid: - Chocolate, coffee, citrus, tomato 🍫☕🍊
- Fatty meals, mint, alcohol 🍔🍷
💨 F. Flatulence / Gas
💡 Goal: Reduce fermentation and bloating.
🍽️ Recommended:
- Small meals, chew food well 🍴
- Ginger, carom seeds (ajwain), warm water 🌿
🚫 Avoid: - Beans, cabbage, carbonated drinks 🥤
- Smoking and chewing gum 🚭
💩 G. Irritable Bowel Syndrome (IBS)
💡 Goal: Normalize bowel habits and relieve discomfort.
🍽️ Recommended:
- Balanced diet with soluble fiber (oats, fruits) 🌾🍎
- Probiotics (curd, buttermilk) 🥛
- Identify and avoid trigger foods (each person differs).
🚫 Avoid: - Caffeine, alcohol, spicy foods ☕🍷🌶️
🥗 3. Foods That Promote Healthy Digestion
🌾 Whole grains – improve bowel movement
🍎 Fruits – fiber & vitamins
🥦 Vegetables – regulate digestion
🥛 Probiotics – restore gut flora
💧 Water – essential for metabolism and excretion
⚕️ 4. Nursing / Health Teaching Points
👩⚕️ Encourage regular eating habits and stress management.
👩⚕️ Teach avoidance of self-medication for GI pain.
👩⚕️ Reinforce hygiene: handwashing before meals 🧼
👩⚕️ Educate about symptom monitoring and diet record keeping
Renal Diseases: Medical Nutrition Therapy (MNT) — What to Eat & Why

🎯 Core goals
- Protect remaining kidney function 🛡️
- Control edema, BP, acidosis & mineral-bone issues 💧📉🦴
- Prevent malnutrition & maintain energy 🍚⚡
- Cut uremic toxin load (urea, K⁺, P) 🧪
🔑 Master levers you’ll always adjust
- Protein 🍗
- CKD (non-dialysis): controlled protein (usually low to moderate) to reduce uremic load.
- Dialysis (HD/PD): higher protein to replace dialytic losses. Prefer HBV sources (egg white, milk in measured portions, lean chicken/fish if non-veg).
- Sodium (Na⁺) 🧂
- Keep low to control BP & edema. Avoid packaged/processed, pickles, papads, namkeen, sauces. “Cook without salt; add a pinch only if allowed.”
- Potassium (K⁺) 🥔🍌
- If serum K⁺ high: use low-K⁺ produce + leaching (double-boil veggies, discard water).
- Prefer: lauki (bottle gourd), tori (ridge gourd), tindora, cucumber, pumpkin, cabbage, apple, papaya, pear, grapes.
- Limit: banana, chikoo, custard apple, jackfruit, coconut water, potato, tomato, spinach, beetroot, dry fruits.
- Phosphorus (P) 🧀🥜
- Keep low to protect bones & vessels. Limit: cola, processed cheese, organ meats, bakery with “phosphate additives,” nuts/seeds, bran.
- If prescribed, use phosphate binders with meals.
- Fluids 🥤
- If oliguric/edematous: intake = yesterday’s urine output + ~500 mL (accounts for insensible losses), unless doctor says otherwise.
- Calories 🍛
- Adequate energy (rice, roti, oils in moderation, poha, upma, sabudana) prevents body from breaking down muscle → less urea.
- Micronutrients 💊
- CKD: often need water-soluble vitamin support; iron/B12/folate if anemic; vit D/calcium per labs & doctor. Avoid OTC supplements with K⁺/P.
- Fiber & gut 🥗
- Helps uremic toxin binding. Choose low-K⁺ veggies in measured portions + isabgol if advised.
🧭 Stage-wise snapshots (what changes)
1) CKD (non-dialysis)
- Protein: controlled; emphasize HBV (egg white best).
- Na⁺: low; avoid processed foods.
- K⁺/P: adjust strictly to labs; use leaching for veggies.
- Fluids: individualize (watch edema/BP).
- Plates look like: rice/roti, 1 dal measured or egg whites, low-K⁺ veggie sabzi (leached), curd only if allowed, fruit like apple/pear/papaya slice.
2) Hemodialysis (HD) / Peritoneal dialysis (PD)
- Protein: higher (HBV focus) to replace losses—egg white, paneer (watch P/Na), lean chicken/fish.
- Na⁺/Fluid: still restricted (thirst control: ice chips, mouth rinse, lemon wedges).
- K⁺: tightly controlled between sessions.
- P: binder + limit high-P foods.
- PD needs more energy (dialysate glucose); watch weight & sugars.
3) Acute Kidney Injury (AKI)
- Dynamic plan: match phase & urine output. Often low Na⁺/K⁺/P, fluids per medical order, protein adjusted to catabolic state ± RRT.
4) Nephrotic Syndrome
- Protein: moderate (not high) + adequate calories; very low Na⁺ to reduce edema; manage dyslipidemia (avoid fried/processed, prefer MUFA/PUFA oils in limits).
🧊 Kidney stones (type-wise quick diet tweaks)
- Calcium oxalate (most common) 🪨
- Normal dietary calcium (don’t cut it; binds oxalate in gut).
- Low oxalate: limit spinach, beet, nuts, tea, chocolate, rhubarb, soy.
- Citrate up: lemon/lime water (if fluids allowed).
- Na⁺ low; animal protein moderate.
- Uric acid stones 🧬
- Limit purines: organ meats, certain fish (anchovy/sardine), meat gravies; keep alkaline fluids (nimbu pani) if permitted; weight & sugar control.
- Cystine/struvite
- High fluids (if not contraindicated), Na⁺ low; medical therapy as directed.
🍽️ Practical Indian plate building (examples)
- Breakfast 🌅
- Poha/upma (low-salt; add lauki/tori), or 2 egg whites + 1–2 phulkas; papaya/apple slice if K⁺ allows.
- Lunch 🍱
- Rice or phulka + leached low-K⁺ sabzi (lauki-chana is classic; keep chana small if K⁺/P high) + curd only if allowed; dal in measured portion or swap with egg white bhurji.
- Snack 🕒
- Murmura chivda (no nuts), khakhra (low-salt), roasted makhana (small; note P), lemon water (no salt) for thirst.
- Dinner 🌙
- Vegetable daliya (with low-K⁺ veggies, leached) or plain rice + ridge-gourd curry; paneer/tofu only if P/potassium plan allows (small cubes).
- Flavor tricks ✨
- Use jeera, hing, ajwain, kasuri methi, lemon, vinegar, pepper, herbs instead of salt & packaged masalas.
🧪 Lab-guided fine-tuning (how to respond to numbers)
- K⁺ high: cut high-K⁺ foods, leach veggies, review salt substitutes (often contain potassium chloride 🚫).
- P high: stop cola/processed cheese/“phos-additive” bakery, take binders with meals.
- Na⁺ high/BP up: re-audit hidden salt, pickles, outside food.
- Urea/creatinine rising + weight loss: increase calories and HBV protein within prescription; check for infection/inflammation.
- Phosphate & PTH high with low Ca: ask about vit D/Ca plan; don’t self-supplement.
🥄 Portion & prep hacks
- Leaching 🫗: peel → small cubes → boil 10–15 min → discard water → cook. Best for potato, brinjal, spinach, cauliflower.
- Soups/curries 🍲: avoid using the first boil water if K⁺ restriction.
- Gravies: tomato & nut pastes raise K⁺/P—use onion-yoghurt-lauki bases instead.
- Thirst control 😮💨: ice chips, cold mouth rinses, lip balm, sour candy/lemon slice (if ulcers absent), limit spicy/salty snacks.
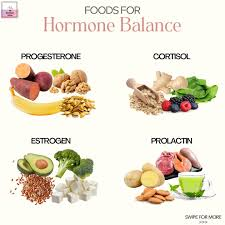
🌿 Endocrine and Metabolic Diet
💡 Introduction
The endocrine system controls hormones that regulate metabolism, growth, and energy balance.
A metabolic diet supports the proper function of these hormones, especially insulin, thyroid hormones, cortisol, and sex hormones.
Such a diet is crucial for people with diabetes, thyroid disorders, obesity, metabolic syndrome, and adrenal imbalance.
🍽️ Main Goals of the Diet
✅ Maintain stable blood sugar levels
✅ Support hormonal balance
✅ Promote healthy metabolism and weight management
✅ Prevent complications of endocrine disorders
✅ Provide adequate nutrients for gland function
🥦 Key Dietary Principles
- 🍞 Balanced Macronutrients – Include carbohydrates, proteins, and fats in proper ratio.
- Focus on complex carbohydrates (whole grains, vegetables).
- Include lean proteins (fish, poultry, legumes).
- Use healthy fats (olive oil, nuts, avocado).
- 🩸 Low Glycemic Index (GI) Foods
- Choose foods that cause slow glucose release to prevent insulin spikes.
- Example: Oats, brown rice, sweet potatoes, lentils.
- 🚫 Reduce Refined Sugar and Processed Food
- Avoid bakery items, soft drinks, candy, and fast food.
- These increase insulin resistance and fat storage.
- 🥛 Adequate Calcium and Vitamin D
- Important for thyroid and parathyroid health.
- Include milk, yogurt, paneer, eggs, and sunlight exposure.
- 🧂 Limit Sodium Intake
- Especially for Cushing’s syndrome or hypertension related to adrenal disorders.
- Prefer natural herbs for seasoning.
🍎 Diet for Common Endocrine Disorders
🩺 1. Diabetes Mellitus
- Eat small frequent meals to maintain glucose levels.
- Include fiber-rich foods like vegetables, fruits (in moderation), and legumes.
- Avoid sugar, jaggery, sweetened drinks.
- Use artificial sweeteners if needed.
- Drink plenty of water 💧.
🦋 2. Hypothyroidism
- Include iodine-rich foods (iodized salt, seaweed in small amounts).
- Eat selenium and zinc sources – nuts, fish, eggs.
- Avoid goitrogenic foods (raw cabbage, cauliflower, soy) in large quantities.
- Prefer high-protein and low-fat diet to maintain metabolism.
🔥 3. Hyperthyroidism
- High-calorie, high-protein diet to compensate for weight loss.
- Include vitamin and mineral-rich foods.
- Avoid caffeine ☕ and spicy food.
🧠 4. Adrenal Disorders
- Include complex carbs and lean proteins.
- Maintain regular meal timings.
- Limit caffeine and alcohol 🍷.
- Ensure adequate vitamin C and B-complex intake.
⚖️ 5. Obesity / Metabolic Syndrome
- Focus on calorie-controlled, high-fiber diet.
- Increase physical activity 🏃♀️.
- Avoid saturated fats and fried foods.
- Prefer steamed, baked, or grilled preparations.
🥗 Important Nutrients in Endocrine & Metabolic Diet
- Iodine 🧂 – for thyroid hormone synthesis.
- Chromium 🧬 – enhances insulin activity.
- Zinc & Selenium 🌰 – for thyroid and immune function.
- Omega-3 fatty acids 🐟 – improve metabolism and reduce inflammation.
- Vitamin D ☀️ & Calcium 🥛 – essential for bone and hormone balance.
- B-complex vitamins 🍞 – regulate energy metabolism.
🌞 Lifestyle Modifications
💧 Drink 8–10 glasses of water daily.
🚶♀️ Engage in regular exercise or yoga.
😴 Maintain proper sleep cycle.
🧘♀️ Manage stress to balance cortisol.
🚭 Avoid smoking and alcohol
🌿 Allergy Diet – Detailed Explanation
An Allergy Diet is a special eating plan designed to identify and avoid foods that trigger allergic reactions in a person. It helps maintain good nutrition while preventing symptoms like rashes, itching, swelling, or breathing difficulties.
🧠 Understanding Food Allergy
A food allergy occurs when the body’s immune system mistakenly identifies a specific food protein as harmful.
➡️ The immune system releases histamine and other chemicals that cause allergic symptoms.
➡️ Even a small amount of the allergen can trigger a reaction.
🍎 Common Food Allergens
Some foods are more likely to cause allergies than others:
🥛 Milk (especially cow’s milk)
🥚 Eggs
🌰 Nuts (like peanuts, almonds, cashews)
🐟 Fish and shellfish
🌾 Wheat and gluten products
🍤 Soy products
🍓 Certain fruits (like strawberries or citrus)
🚫 Elimination Diet (Avoidance Phase)
This is the first step in an allergy diet.
👉 All suspected foods are completely eliminated for 2–4 weeks.
👉 The goal is to see if allergy symptoms improve or disappear.
👉 Always done under medical supervision to avoid nutrient deficiency.
🔄 Reintroduction Phase
After the elimination period, foods are slowly reintroduced one by one.
➡️ Each food is eaten in small amounts while monitoring for symptoms.
➡️ If symptoms appear, that food is confirmed as an allergen.
➡️ A detailed food diary is often maintained for tracking reactions.
🥗 Safe Foods and Substitutes
When allergenic foods are avoided, safe and nutritious alternatives should be used:
🧈 Use plant-based milks (soy, almond, oat) instead of cow’s milk.
🥔 Choose gluten-free grains (rice, millet, quinoa).
🥩 Replace seafood with lean poultry or plant proteins.
🍎 Prefer fresh fruits and vegetables that don’t cause reactions.
🍞 Always check food labels for hidden allergens (like casein, whey, gluten).
💪 Nutritional Considerations
Avoiding major food groups can lead to nutrient deficiencies, so:
🥛 Include calcium and vitamin D if avoiding dairy.
🌾 Add iron and B vitamins if avoiding wheat/gluten.
🥜 Include omega-3 rich seeds (flaxseed, chia) if avoiding fish.
🧩 Tips for Managing Food Allergy
✅ Always read ingredient labels carefully.
✅ Inform restaurants or friends about your food allergies.
✅ Carry emergency medicines like antihistamines or epinephrine if prescribed.
✅ Educate children about safe and unsafe foods.
✅ Keep cross-contamination in mind—avoid sharing utensils or cooking oils.
❤️ Role of Nurse and Dietitian
👩⚕️ Nurses and dietitians help:
Monitor nutritional status and symptoms regularly.
Identify possible allergens.
Design balanced, allergy-free meal plans.
Educate patients on label reading and food safety.
🌿 Diet for Infections and Fever :-
When the body is fighting an infection or fever, the metabolic rate increases, leading to higher energy and nutrient requirements. The right diet supports recovery, immunity, and hydration.
🌞 1. Purpose of the Diet
- To provide adequate calories and nutrients for healing.
- To maintain fluid and electrolyte balance.
- To boost immunity and promote quick recovery.
🥣 2. General Dietary Principles
- 🧊 Light, easily digestible foods — reduce the burden on the digestive system.
- 💧 High fluid intake — to prevent dehydration from sweating and high temperature.
- 🧂 Include electrolytes — sodium and potassium help maintain fluid balance.
- 🕐 Small frequent meals — every 2–3 hours to sustain energy levels.
- 🚫 Avoid spicy, oily, and heavy foods — they can irritate digestion.
🍚 3. Energy Requirements
- Energy needs are increased due to higher metabolism.
- Provide high-calorie foods like rice, porridge, banana, boiled potato, and fruit juice.
- Use easy-to-digest carbohydrates (rice, toast, khichdi, oats, semolina).
🥛 4. Protein Intake
- Essential for tissue repair and immune function.
- Include milk, curd, paneer, eggs, dal water, chicken soup, or lentil soup.
- Avoid heavy meat initially — prefer soft or liquid proteins.
🧈 5. Fat Requirement
- Fats should be moderate — they provide energy but are harder to digest.
- Use light fats like ghee, butter, or vegetable oils in small amounts.
- Avoid fried and greasy foods.
🍎 6. Vitamins and Minerals
- Vitamin C 🍊 – strengthens immunity and tissue repair (found in citrus fruits, amla, lemon water).
- Vitamin A 🥕 – maintains mucous membrane health (carrots, pumpkin).
- Iron and Zinc 🫘 – aid in healing and infection control (green leafy vegetables, pulses).
- B-complex vitamins – improve energy metabolism (whole grains, milk).
💧 7. Fluid and Electrolyte Balance
- Drink plenty of fluids — 2.5–3 liters/day or more if fever is high.
- Include ORS, soups, fruit juices, coconut water, barley water, lemon water.
- Replace salt loss with lightly salted liquids or soups.
🍵 8. Suitable Foods During Fever
✅ Clear soups
✅ Rice gruel or dal water
✅ Vegetable or chicken broth
✅ Fruit juices (orange, apple, pomegranate)
✅ Soft boiled eggs or curd
✅ Steamed vegetables or mashed potato
✅ Toast, khichdi, upma, porridge
🚫 9. Foods to Avoid
❌ Fried, spicy, or oily foods
❌ Caffeine and carbonated drinks
❌ Hard-to-digest meats
❌ Excess sugar and sweets
❌ Alcohol and smoking
🌿 10. Example Daily Routine
- 🌅 Morning: Lemon water or light tea
- 🍚 Breakfast: Oats or porridge with milk
- 🥣 Mid-morning: Fruit juice or coconut water
- 🍲 Lunch: Soft rice with dal or khichdi + boiled vegetables
- ☕ Evening: Clear soup or fruit
- 🍜 Dinner: Light gruel or vegetable broth
- 🌙 Bedtime: Warm milk with turmeric (for immunity)
🏥 Pre-Operative and Post-Operative Diets
🩺 1. Pre-Operative Diet (Before Surgery)
🕒 Purpose:
To prepare the patient’s body for surgery, ensure good nutritional status, and prevent complications during or after the procedure.
🍎 Key Points:
- 🥦 High-Protein Diet:
Proteins help strengthen body tissues and support healing after surgery. Foods like eggs, milk, pulses, chicken, and fish are encouraged. - 🥣 High-Carbohydrate Diet:
Carbs provide energy and maintain glycogen stores. Include rice, chapati, potatoes, fruits, and cereals. - 💧 Adequate Hydration:
Fluids such as water, fruit juices, soups, and coconut water help maintain electrolyte balance and prevent dehydration. - 🍊 Vitamin-Rich Foods:
Vitamin C (from citrus fruits, tomatoes) and Vitamin A (from carrots, spinach) promote wound healing and immunity. - 🧂 Minerals (Iron & Zinc):
Iron supports oxygen transport, and zinc helps tissue repair. Found in meat, leafy greens, nuts, and whole grains. - 🚫 Avoid Certain Foods:
No oily, spicy, or heavy meals before surgery. Alcohol and caffeine are restricted. - ⏳ Fasting (NPO Status):
Usually, patients are kept nil per oral (NPO) for 6–8 hours before anesthesia to prevent aspiration. - 🫖 Light Diet a Day Before:
A soft, easily digestible diet (like khichdi, soup) is preferred on the day before surgery.
💉 2. Post-Operative Diet (After Surgery)
🕒 Purpose:
To restore strength, promote wound healing, and prevent infection or digestive disturbances after surgery.
🍲 Key Points:
- 🍼 Clear Liquid Diet (Initially):
Begins with water, clear soups, tea, and diluted fruit juice once bowel sounds return. - 🧃 Full Liquid Diet:
Includes milk, porridge, custard, fruit juices, and smooth soups once tolerated. - 🍚 Soft Diet (Gradual Progression):
Soft, semi-solid foods such as khichdi, mashed vegetables, boiled rice, dal, and soft fruits are added next. - 🍗 High-Protein Foods:
Continue rich sources of protein to help wound and tissue healing — eggs, milk, pulses, and lean meat. - 🍞 Energy-Rich Foods:
Carbohydrates (rice, roti, cereals) provide energy for recovery. - 🥕 Vitamin & Mineral Support:
- Vitamin C: Aids healing and immunity (citrus fruits, guava).
- Vitamin A: Restores epithelial tissue (carrots, pumpkin).
- Zinc & Iron: Prevent anemia and aid repair.
- 🚫 Avoid Constipating or Gas-Forming Foods:
No spicy food, fried food, cabbage, or carbonated drinks. - 💧 Hydration:
Encourage plenty of fluids unless contraindicated (e.g., cardiac or renal conditions). - 🕊️ Gradual Return to Normal Diet:
Once the patient’s digestion and appetite normalize, the diet is slowly changed back to normal meals
🌾 Diet for Deficiency and Malnutrition
Malnutrition refers to an imbalance between the body’s nutrient requirements and intake. It may be due to under-nutrition (deficiency of calories, proteins, vitamins, or minerals) or over-nutrition (excess intake).
Deficiency diseases develop when the essential nutrients are not supplied adequately for a long time.
🧠 Main Objectives of the Diet
- 🥗 To provide adequate calories and proteins for energy and tissue repair.
- 🧃 To supply vitamins and minerals in required amounts.
- 💪 To restore normal body weight and muscle tone.
- 🫶 To correct anemia, fatigue, and poor immunity caused by nutritional deficiency.
- 🩺 To promote growth and recovery especially in children and undernourished individuals.
🥦 General Dietary Principles
- 🍛 Provide high-calorie, high-protein meals (e.g., milk, eggs, pulses, meat, fish, soybean).
- 🍞 Include easily digestible carbohydrates such as rice, roti, cereals, and fruits.
- 🧈 Add fats and oils (ghee, butter, nuts, coconut, vegetable oils) for extra energy.
- 🥬 Give plenty of green leafy vegetables for vitamins A, C, and folic acid.
- 🍊 Add fresh fruits for natural sugars and vitamin C.
- 🧂 Include iodized salt and fortified foods (iron-fortified flour, vitamin-A-enriched oil).
- 💧 Encourage adequate water intake to maintain hydration and metabolism.
- 🍵 Serve small, frequent meals (5-6 times/day) for better digestion and absorption.
🧫 Protein Deficiency (Kwashiorkor / Marasmus)
- 🍖 Emphasize protein-rich foods – milk, curd, cheese, paneer, pulses, groundnuts, soybeans, fish, and eggs.
- 🥣 Add cereal-pulse combination (e.g., khichdi, dal-roti) for better protein quality.
- 🧈 Include moderate fats and carbohydrates for calorie support.
- 🍌 Give banana, jaggery, honey for energy in children.
- 🩹 Supplement with multivitamin syrup or fortified milk.
🩸 Iron Deficiency (Anemia)
- 🥬 Eat green leafy vegetables (spinach, methi, drumstick leaves).
- 🫘 Include legumes, jaggery, liver, meat, beetroot for iron.
- 🍊 Combine with vitamin-C-rich foods (lemon, amla, orange) to enhance absorption.
- 🧂 Avoid tea and coffee immediately after meals as they reduce iron absorption.
🥕 Vitamin Deficiency
- 🧈 Vitamin A → milk, butter, egg yolk, carrot, papaya, mango.
- 🍋 Vitamin C → citrus fruits, amla, guava, tomatoes.
- 🌾 Vitamin B-complex → whole grains, pulses, green vegetables, milk, liver.
- 🧂 Vitamin D → sunlight exposure, fish liver oil, fortified milk.
- 🧀 Vitamin E & K → vegetable oils, nuts, leafy vegetables.
🧂 Mineral Deficiency
- 🧄 Calcium deficiency → milk, curd, ragi, sesame seeds.
- 🐟 Iodine deficiency → iodized salt, seafood.
- 🫘 Zinc & Selenium deficiency → meat, eggs, nuts, whole grains.
👶 Special Considerations for Children
- 🍼 Start early weaning with energy-dense foods (mashed banana, khichdi, dal, suji kheer).
- 🧃 Ensure supplementary feeding programs (ICDS, Mid-Day Meal).
- 🩺 Provide nutrition education to mothers on balanced diet and hygiene.
🧘♀️ For Adults and the Elderly
- 🍽 Maintain balanced diet with adequate fiber, protein, and fluids.
- 💧 Prevent dehydration and constipation.
- 🚶♀️ Combine diet with moderate physical activity to improve metabolism.
- 🧂 Monitor weight and hemoglobin levels regularly.
💡 Nursing Responsibilities
- 🩺 Assess nutritional status (weight, BMI, dietary intake).
- 📋 Plan and record dietary chart for each patient.
- 👩🍳 Encourage nutritious, locally available, affordable foods.
- 💬 Provide health education on hygiene, food preparation, and feeding habits.
- 🧃 Monitor response to diet therapy and prevent relapse
🌿 Diet for Overweight Individuals (Obesity Management)
💡 Goal:
To achieve gradual weight reduction by decreasing calorie intake and promoting healthy metabolism without nutritional deficiencies.
🥦 Key Principles:
- 🍽️ Calorie Control: Reduce total daily calorie intake according to body needs (around 1200–1500 kcal/day depending on activity).
- 🥗 High-Fiber Foods: Include green leafy vegetables, salads, whole grains, fruits with skin — they give fullness and reduce overeating.
- 🚫 Limit Fats & Oils: Avoid fried, oily, and processed foods. Use minimal healthy oils (olive oil, sunflower oil).
- 🍞 Avoid Refined Carbs: Limit white rice, sweets, bakery items, and sugary beverages.
- 🧂 Reduce Salt Intake: Helps to prevent water retention and hypertension.
- 🥛 Prefer Low-Fat Dairy: Skimmed milk, low-fat curd, and paneer are better options.
- 🥚 Adequate Protein: Include pulses, legumes, egg whites, and fish for muscle preservation.
- 💧 Hydration: Drink plenty of water and herbal teas; avoid soft drinks and alcohol.
- 🕐 Meal Timing: Eat small frequent meals every 3–4 hours to avoid overeating.
- 🚶 Lifestyle Changes: Combine diet with regular physical activity like walking, swimming, yoga, or cycling.
⚠️ Avoid:
- Junk foods 🍟
- Sweets, desserts 🍰
- Sugary drinks 🥤
- Late-night eating 🌙
🥑 Diet for Underweight Individuals (Weight Gain Plan)
💡 Goal:
To promote healthy weight gain through nutrient-dense, balanced food intake and improved appetite.
🧀 Key Principles:
- 🍚 Increase Calorie Intake: Consume more calories than your daily expenditure with nutrient-rich foods (2500–3000 kcal/day).
- 🍗 High-Protein Foods: Eggs, chicken, fish, milk, paneer, pulses, and soy products help in muscle building.
- 🥜 Healthy Fats: Add nuts, seeds, peanut butter, avocado, and olive oil to meals.
- 🍞 Complex Carbohydrates: Prefer brown rice, whole wheat bread, oats, and potatoes for sustained energy.
- 🧃 Energy-Rich Snacks: Include fruit smoothies, milkshakes, cheese sandwiches, and dry fruits between meals.
- 🥛 Full-Fat Dairy: Use full-cream milk, ghee, butter, and cheese to increase calorie intake healthily.
- 🕐 Regular Meal Pattern: Eat 5–6 small meals per day — don’t skip breakfast.
- 🍉 Micronutrients: Eat a variety of fruits and vegetables for vitamins and minerals.
- 💧 Hydration: Drink enough fluids but not just before meals to avoid fullness.
- 🧘 Physical Activity: Light exercise or resistance training helps build muscle mass and stimulates appetite.
⚠️ Avoid:
- Skipping meals ⏳
- Drinking excessive tea/coffee ☕
- Consuming empty-calorie junk foods 🍩