ENGLISH GYNECOLOGY GNM UNIT 5
Unit : 5 GYNECOLOGICAL DISORDERS.
Retroversion of Uterus:
Retroversion:
Retro Mins Behind
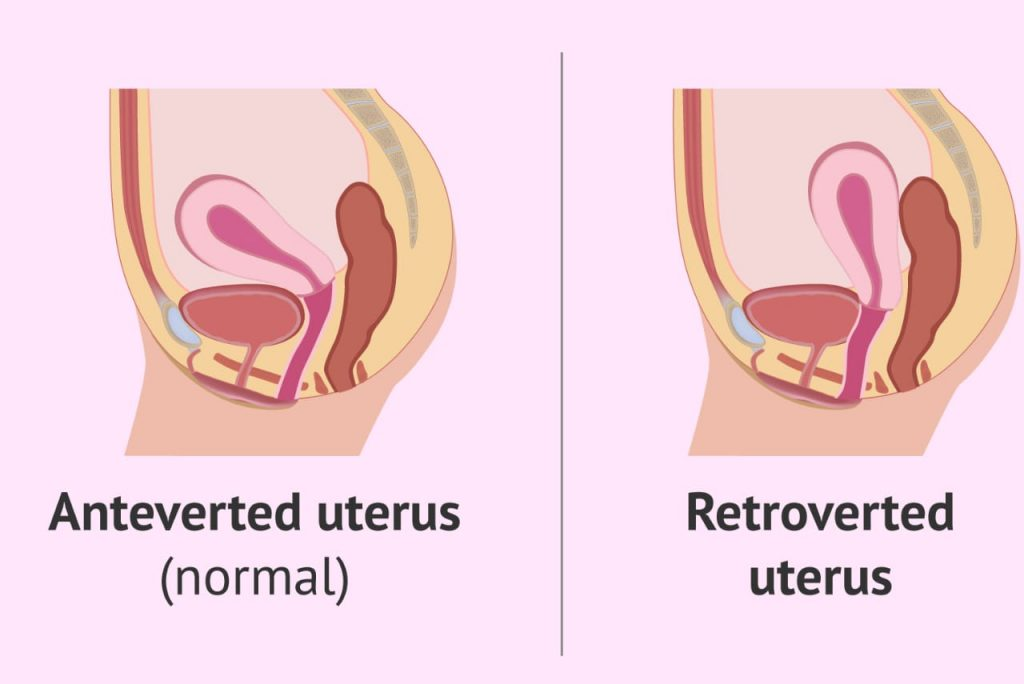
When the long axis of the corpus (body of the uterus) and the cervix are in line and the entire uterus turns backward in relation to the birth canal (vagina), the condition is called retroversion of the uterus, i.e., the position of the uterus is normally anteverted and anti There is flexion but in the condition of retroversion the uterus is displaced towards backward.
Retroflexion:
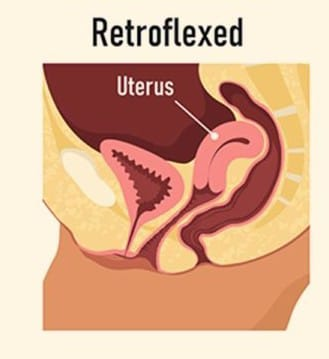
In the condition of retroversion the uterus is usually slightly straight but in the condition of retroflexion the body of the uterus is bent backwards i.e. the body of the uterus is retroflex i.e. bending at the level of the internal os of the cervix. is called retroflexion.
Degree of retroversion:
In retroversion the uterus is displaced i.e. the uterus does not stay in place and bends backwards.
1st degree: In this degree uterus no fundus no part is vertical i.e. slightly straight and its face is pointing to sacralpomentary.
2nd Degree: In this degree the fundus of the uterus is present up to the sacral hollow but not below the internal os of the cervix.
3rd Degree: In this degree the fundus of the uterus lies below the level of the internal os.
Etiology:
Developmental causes
Retrodisplacement is quite common in fit and young children.
Tone in the muscles of the uterus is less amount due to developmental defect. And the infantile position is maintained.
This is often associated with short playing and cello anterior vaginal phonics.
The
Acquired:
Puerperal:
Stretch ligaments caused by child birth are puerperal but fail to keep the uterus in its normal condition. A subinvoluted bulky uterus is common with this condition.
Prolapse:
Retroversion is commonly implicated in the pathophysiology of prolapse caused mechanically by post-cystocele traction.
Tumor:
Due to the presence of tumor in the anterior or posterior wall of the uterus, the fibroid raises the heaviness in the uterus and hence moves posteriorly.
Pelvic Adhesions
: Pelvic adhesions pull the uterus backwards due to operative or pelvic endometriosis.
Other Causes:
Pelvic Inflammatory Diseases,
endometritis,
Uterine Fibroids,
salpingitis,
Vic Muscles,
Surgery such as caesarean section,
multiparity,
Symptoms and signs:
pelvic pain,
back pain,
dyspareunia,
Recurrent Urine Infection,
Retention of urine,
chronic constipation,
Increased chances of miscarriage,
Problems in placement of intrauterine device,
infertility,
Sciatica due to compression of the sacral plexus.
Diagnostic evaluation:
History Collection,
Physical Examination,
imaging studies,
ultrasound,
x ray,
MRI,
Specialize Study:
Hysterosalpingography (HSG)
Sonohysterography,
Laparoscopy.
Treatment:
Causes of retroflexion are treated like fibroid endometriosis etc. Even after this, if the uterus remains in the same position, symptoms will not occur.
Emphasis on knee-chest position for 10 minutes.
Three times a day lie on the back and alternately pull each leg towards the chest and hold for 10 seconds.
Kegel exercises help strengthen the pelvic floor muscles.
Manual manipulation can be done by experts.
A pessary can be provided to aid and anchor forward movement of the interior wall of the uterus.
Conditions of anteversion and antiflexion uterus are also surgically corrected.
- Fistula:
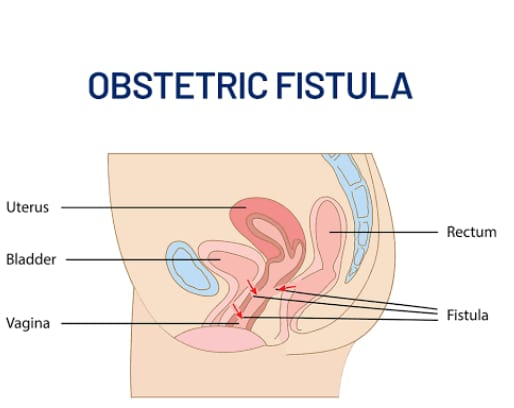
Fistula means abnormal communication or formation of hole between two tubular or hollow structures, then this condition is called fistula.
Obstructive Fistula: Obstructive fistula is the formation of an abnormal hole or opening between the vagina and the rectum or bladder, usually due to prolonged obstructed labour, which can lead to conditions of urinary incontinence and fecal incontinence.
Etiology:
Prolonged Labour,
Due to injury due to neglected child birth,
Due to obstructed labour,
Young age at birth of first child and early child bearing,
malpresentation,
malposition,
CPD (Cephelo Pelvic Disproportion),
Due to injury during gynecological or obstetric surgery,
sexual violence,
In the condition that the episiotomy is not properly repaired after a complicated delivery,
Due to injuries sustained during caesarean section,
Infections such as (lymphogranuloma venereum),
Due to lack of literacy and education related to reproductive health including family planning, nutrition, safe maternal care.
Type of Fistula:

- Recto Vaginal Fistula: A condition in which there is formation of abnormal communication ie hole and opening between the rectum and vagina is called recto vaginal fistula.
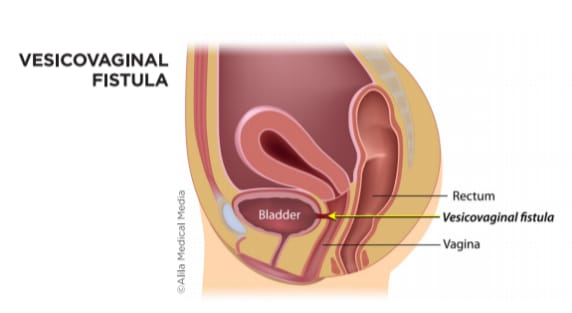
2.Vesicovaginal Fistula: It is a condition in which there is formation of abnormal communication ie hole or opening between the bladder and vagina, this condition is called vesicovaginal fistula.
Symptoms and signs:
Foul smelling vaginal discharge,
Urinary or fecal incontinence,
flatulence,
Ulceration in the vaginal track,
dyspareunia,
Nerve damage can also occur which can lead to foot drop.
Pain in the vagina and its near area,
Irritation in the vagina and its near area,
Repeated infection of the vagina and urinary tract.
Steel birth due to prolonged labour.
Diagnostic Evaluation:
History Collection,
Physical Examination,
speculum examination,
Imaging study
ultra sound,
Cytoscopy,
hysteroscopy,
CT scan,
voiding cystourethrogram (VCUG),
Dye test (to assess vesicovaginal fistula),
Barium swallow or enema (rectovaginal fistula).
Management:
Fistulas usually require surgical repair.
Fistula before surgical repair
Follis is located with the help of a catheter.
The procedure is explained to the patient before the operation.
A complete physical examination should be done.
Taking proper consent of the patient and his family members.
Conduct a complete investigation.
Monitor the patient’s vital signs every 15 minutes during the first hour after the operation, then every half hourly thereafter.
Provide a properly comfortable position to the patient.
Properly maintain the patient’s hydration status as per the patient’s condition.
A ureteral catheter should be removed after a period of one week, while a urinary catheter should be removed after two weeks. During this period, care of the catheter should be provided daily and any sign of bladder distention should be properly checked. If present, report it to the gynecologist immediately, as it may indicate a blockage in the catheter that may allow urine to leak out of the fistula and complicate repair.
The catheter should be irrigated daily with normal saline to prevent blockage.
To check the patient’s bowel sound properly. If bowel sound is present then providing the patient with a proper diet which includes,
Liquid diet, followed by soft diet and then semi-solid diet are provided to the patient.
Removal of vaginal packing on 3rd postoperative day.
Before removing the catheter, it should be clamped briefly (not removed directly), so that the sphincter can regain control.
Advise the patient to avoid sexual intercourse for at least 3 months.
Advising the patient for regular follow-up.
- Uterine prolapse:
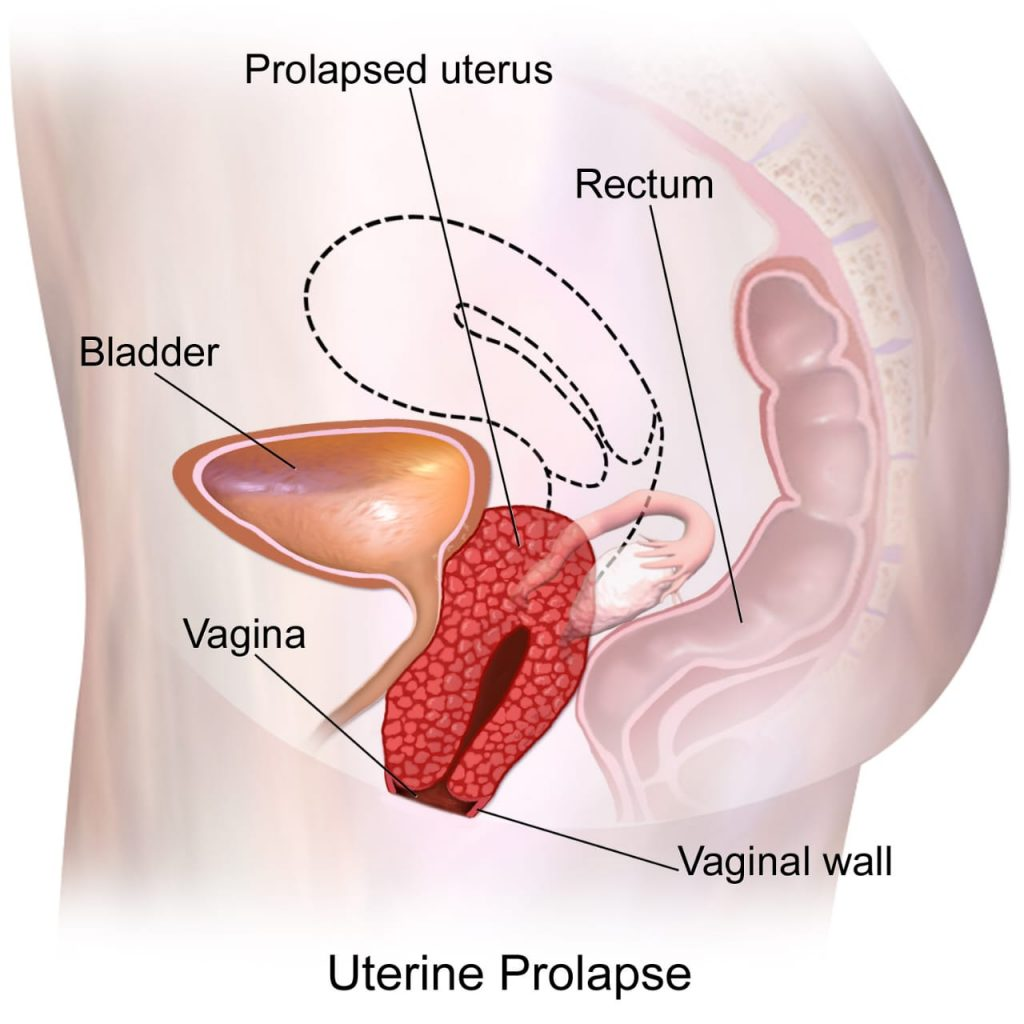
Uterine: Uterus,
Prolapse: Downward displacement of an organ from its normal place.
Uterine prolapse is also known as procidentia.
Uterine prolapse is a condition in which the uterus, uterine tissues or uterine segment protrudes (prolapses) downwards into the vaginal canal. If the uterus protrudes up to the vaginal canal, this condition is called uterine prolapse, and if the uterus slips from its normal position and the mother is displaced to some extent, then this condition is called uterine prolapse.
When the muscles and ligaments of the pelvic floor are stretched and weakened due to which the muscles of the pelvic floor cannot properly support the uterus in its normal place, due to this condition the uterus slips downwards from its normal place i.e. protrudes. and prolapses downward through the vaginal canal.
Etiology:
The uterus may prolapse downwards due to stretch and weakness of the pelvic floor muscles and not being able to provide proper support to the uterine cavity.
Due to multiple pregnancy,
Any injury to vaginal delivery and any injury to its supporting structures.
Hormonal factors (such as the condition of menopause due to the reduced amount of estrogen).
Due to vaginal wall overstretching.
Due to heavy weight lifting.
Due to premature bearing down afters during delivery time.
Due to chronic constipation,
Due to application of forceps during delivery,
Due to genetic factors,
Due to any obstetric trauma,
Due to applying downward pressure on the fundus of the uterus to deliver the placenta,
Because of the
Classification of Uterine Prolapse:
Uterine prolapse is generally given two classifications namely,
- Incomplete uterine prolapse,
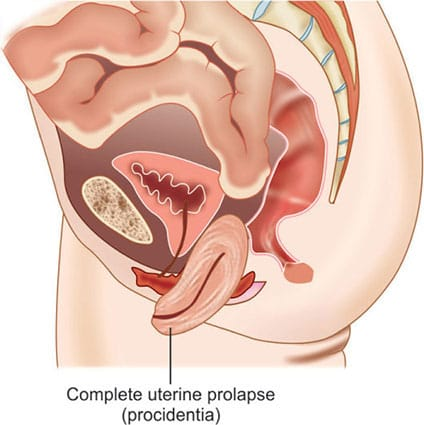
2.Complete uterine prolapse - Incomplete uterine prolapse: In this incomplete uterine prolapse, the uterus usually protrudes partially downwards from its normal place, i.e. the uterus does not protrude completely through the external side of the vaginal opening.
2.Complete uterine prolapse: In this condition of complete uterine prolapse, the uterus protrudes completely outside the vagina.
Degree of Uterine Prolapse:
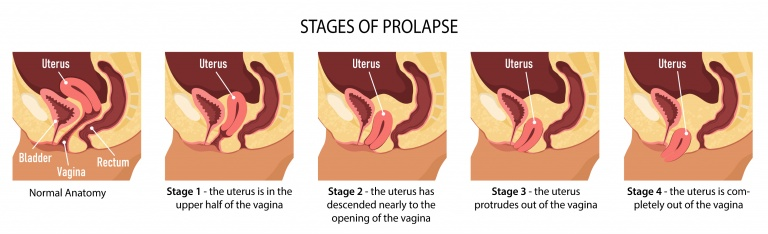
Uterine prolapse is generally divided into four degrees viz.,
1) 1st degree,
2) 2nd Degree,
3) 3rd Degree,
4) 4th Degree,
1) 1st degree: In this first degree, the uterus protrudes (prolapses) up to the upper half of the vagina.
2) 2nd Degree: In this second degree, the uterus prolapses i.e. protrudes up to the vaginal opening.
3) 3rd Degree: In this third degree, the uterus protrudes through the vaginal opening.
4) 4th Degree: In the fourth degree, the uterus prolapses completely through the external side of the uterus.
Symptoms and signs:
Tissues protrude downward from the vaginal canal and fill.
Back pain.
Dragging pain in pelvis.
Difficulty in passing urine.
Vaginal bleeding, discharge and infection present.
Dyspareunia.
Incomplete evacuation of urine.
Difficulty in passing stool.
These symptoms are obesity, due to prolonged standing, due to straining, due to cuffing and due to lifting of any heavy object, abdominal pressure increases and the symptoms are aggravated.
Diagnostic Evaluation:
History Collection,
Physical Examination,
Pelvic examination to identify the condition,
Vaginal examination.
Management:
Management of uterine prolapse is generally done on the basis of 5 points viz.
1) Treatment is provided based on the severity of the patient’s symptoms such as mild, moderate and severe symptoms.
2) Treatment is provided based on the severity of the uterine prolapse i.e. the stage at which the uterine prolapse has occurred.
3) Depending on the age of the patient.
4) Treatment depends on the health status of the female.
5) Treatment depends on future family planning.
Whenever uterine prolapse is treated, it is managed keeping these five points in mind.
Management of uterine prolapse is divided into three phases viz.
1) Preventive Management,
2) Conservative Management,
3) Surgical management.
1) Preventive Management:
Providing effective antenatal care to the patient such as,
1) Provide nutritional supplement in adequate amount to the patient.
2) Advise the patient to maintain proper antenatal hygiene.
3) Advise the patient to perform proper relaxation exercises.
4) Advise the female to have a high fiber diet and a very high water intake to reduce constipation.
5) Advise the patient to avoid heavy lifting.
To provide proper intranatal care of the patient due to which,
1) To prevent the patient from the condition of prolonged labour,
2) To prevent premature bearing down effects.
Providing adequate amount of post natal care to the patient viz.
1) Advise the patient to avoid fundal pushing.
2) Advising the patient for early ambulation.
3) Advising women to do pelvic floor exercises and kegel exercises as these exercises increase the strength of the muscles and also strengthen the pelvic and uterine muscles which are loose and prevent uterine prolapse.
2) Conservative Management:
Provide proper reassurance to the patient.
Advise the patient to improve his nutritional status.
Advise the patient to perform pelvic floor exercises to strengthen the pelvic muscles.
Providing Pessary Treatment to the Patient A pessary is a ring made of rubber or plastic i.e. latex or silicone that is used to hold the uterus in its normal place. Available in different sizes and shapes, this pessary is used to place a prolapsed uterus in its normal place.
3) Surgical Management:
The following surgeries are performed to repair the weakened pelvic floor muscles in the condition of uterine prolapse such as,
Anterior Calporrhaphy,
Colpoperineorrhaphy,
Pelvic floor repair (PFR),
Fothergills Operation
Which happens in case of cystocele, enterocele, rectocele.
Vaginal hysterectomy with PFR (pelvic floor repair) This procedure is performed if there is utero vaginal prolapse.
Cervicopexy
Le Fort Operation. (Colpoclesis)
This procedure is done in vault prolapse.
- Uterine Malformations:
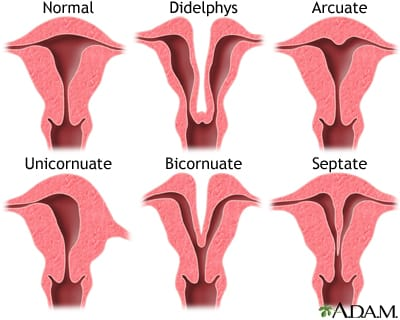
Introduction: The outer shape of normal uterus is pear shape and the inner shape of uterus is triangular shape. Embryogenesis means development of uterus after three months of pregnancy. And it is usually formation of uterus by fusion of two Müllerian ducts with the help of which formation of vagina, cervix, uterus, fallopian tubes takes place. Proper fusion of these Müllerian ducts does not happen and due to this condition of uterine malformation arises.
Definition:
Uterine abnormality occurs due to abnormal fusion and abnormal development of two Müllerian ducts during embryogenesis. The most common types of uterine malformations are due to improper fusion of the Müllerian duct.
Etiology:
Genetic factors: Genetic mutations can cause difficulty in the development and fusion of the Müllerian duct.
Embryonic Developmental Issues: Failure of proper fusion of Müllerian ducts during the embryonic period may lead to uterine malformations such as septate uterus, bicornuate uterus, unicornuate uterus, etc.
Hormonal Influences: Due to abnormal hormonal levels during the critical period of uterine development
Environmental Factors: Abnormalities in uterine development may be seen due to exposure of the mother to certain drugs, infections and toxins.
Maternal conditions: Maternal conditions such as diabetes can cause abnormalities in uterine development during intrauterine life due to autoimmune disorders.
Classification of Uterine Malformation:
There are generally seven classifications of uterine malformation viz.,
1) Müllerian agenesis or hypoplasia (absent uterus)
2) Unicornated uterus (onesided uterus).
3) Uterine didelphis (double uterus).
4) Bicornuate uterus (it has two horns of uterus).
5) Septated uterus (uterine septum or partition).
6)DES (Diethylstilbestrol) Uterus.
7) Arcuate uterus
1) Müllerian agenesis or hypoplasia (absent uterus): If the formation of Müllerian duct is not done during embryogenesis, the condition of Müllerian agenesis occurs due to which the condition of absent uterus can occur.
2) Unicornated Uterus (One Sided Uterus): In this condition the uterus is developed on a single side due to defective Müllerian duct and fallopian tube is also unavailable on one side so this condition is called unilateral uterus.
3) Uterine Didelphys (Double Uterus): During embryogenesis the two Müllerian ducts do not fuse properly and due to this the formation of separate uteri occurs by both the Müllerian ducts i.e. this condition is called double uterus in which both the Müllerian ducts Different uteri are formed but the cavity of these different uteri is small so it is called double uterus (didelphys).
4) Bicornuate Uterus (It has two horns of Uterus): In this condition the Uterus is heart shaped from inside. In this condition there is no fusion of Müllerian duct at fundus site of uterine cavity i.e. During embryogenesis the Müllerian duct is fused downwards but fails to fuse towards the fundus side of the uterus and due to this two horns are formed at the fundus site in the uterus and in this condition single cervix and single vagina are seen. But due to the presence of two horn-like structures at the fundus site of the uterus, this condition is called bicornuate uterus.
5) Septated Uterus (Uterine Septum or Partition): In this condition the Müllerian duct does not fuse properly leading to the formation of a septum between the uterine cavity which is called septated uterus.
6)DES (Diethylstilbestrol) Uterus:
Exposure to diethylstilbestrol (DES) in the uterus may cause uterine malformation in women. such as
T-shaped uterus: One of the most common malformations is a T-shaped uterine cavity. The condition involves a contracted, irregularly shaped uterine cavity that can lead to irregular menstruation and increased risk during pregnancy.
7) Arcuate uterus: This uterus looks like a normal uterus but a dimple like structure is seen in the fundus part of the uterus which is called arcuate uterus.