ENGLISH GYNECOLOGY GNM UNIT 2
UNIT 2 PHYSIOLOGY PSYCHOLOGY AND PUBERTY
Puberty:
Definition: Puberty is the period that generally connects childhood with adulthood and the gradual development of secondary sexual characteristics in the body of the human being.
Age of Puberty:
Age of puberty is different in boys and girls.
Puberty in gals usually ranges from 10 years to 14 years. While in boys the age of puberty ranges from 12 years to 16 years.
Changes in girls during puberty like,
1) Thelarchy: Best no growth occurs in girls.
2) Adrenarchy: There is no growth of axillary hair.
3) Puberty: There is no growth of pubic hair.
4) Menarchy: It starts the first menstrual cycle in girls.
5)Growth spurt: Height increases rapidly.
Changes in the body during puberty such as,
1) Broadening of Chest and Shoulders: Part of the chest and shoulders become broad in males due to muscle development due to puberty.
2) Voice Changes: The onset of puberty is marked by changes in the voice in boys, the voice becomes deeper and darker.
3)Appearance of facial hair: Growth of facial hair is seen which gradually changes to mustache and beard with age.
4)Appearance of hair on body and pubic area: Hair growth is seen on chest, axilla, legs, arms and groin region.
5) Enlargement of Genital Area: During puberty genital organs like penis and testicles grow in size.
6) Increase in Height: Growth spurt is observed during puberty for a period of 2-3 years. The height of boys increases rapidly and the appearance of the child changes. In general, height can increase about 4.1 inches a year.
6) Ability to Ejaculate: Another important change in the boy at or during puberty is the ability to ejaculate semen through the penis which conforms to the ability of the boy’s life sexual maturity.
7) Breast development: In some boys, the breast grows slightly. It is usually temporary which disappears after some time.
8) Development of acne:
Sweat and oil-producing glands that become clogged and produce acne (acne).
- Menstrual Cycle:

Definition:
Menstruation is derived from Mun. Menstrual cycle is a visible cyclical process of physiological changes in a fertile female that occurs in the endometrium of the uterus and through the interconnection of its hormones leading to vaginal bleeding. The HPO process
(H : hypothalamus,
P: Pituitary Gland,
O: Ovaris ) is caused by
H : Hypothalamus:
The hypothalamus secretes gonadotrophin releasing hormone (GnRH) which stimulates the anterior pituitary gland to release FSH (follicle stimulating hormone).
Stimulates to secrete LH(Luteinizing Hormone).
P : Pituitary Gland :
FSH (follicle stimulating hormone) from pituitary gland
LH (luteinizing hormone) is secreted. He works on Overies.
O: Overies:
Pituitary gland secretes FSH (Follicle Stimulating Hormone) which causes maturation of ovarian follicle, secretion of estrogen and ovulation.
While LH (Luteinizing hormone) promotes development of corpus luteum and secretion of progesterone.
Hormone secretion during the menstrual cycle is regulated by a negative feedback mechanism.
The hypothalamus responds to changes in blood levels of estrogen and progesterone. As hypothalamus is depressed by high blood levels of estrogen and progesterone while hypothalamus is stimulated by low levels of estrogen and progesterone.
The average length of menstruation cycle is 28 days.
Menstruation Cycle:
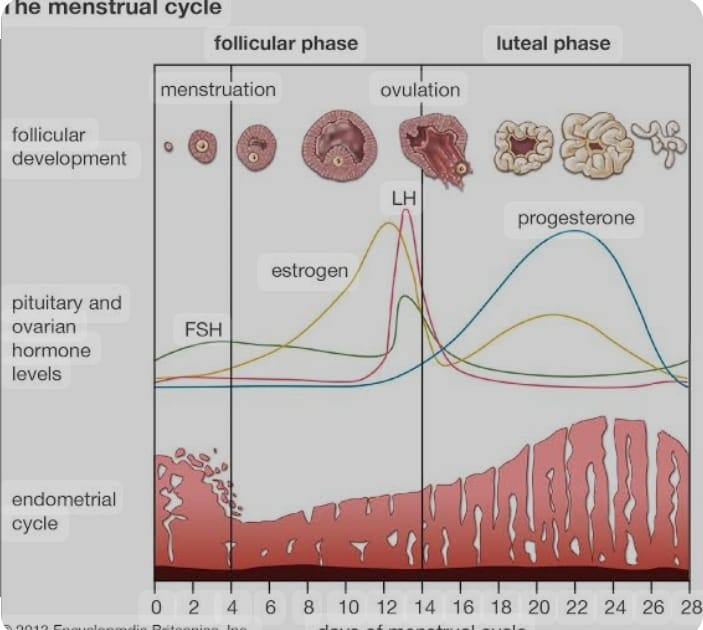
Menstruation cycle has two phases.
1) Ovarian phase
2) Uterine phase
1) Ovarian Phase:
Further two phases are involved in ovarian phase.
a) Follicular phase,
b) Luteal phase
a) Follicular phase:
The follicular phase starts from the first day of menstruation and ends with ovulation. This phase is usually up to 14 days.
In this phase follicles grow due to follicle simulating hormone (FSH).
One of these follicles (dominant follicle) becomes mature.
This mature follicle becomes a Graafian follicle. It releases estrogen.
Estrogen then acts on both follicle stimulating hormone (FSH) and luteinizing hormone (LH).
Estrogen suppresses follicle stimulating hormone (FSH) and stimulates luteinizing hormone (LH).
Then the luteinizing hormone (LH) ruptures the Graafian follicle which is formed from the dominant follicle, releasing the ovum and then the work of the corpus luteum increases.
b) Luteal Phase:
The luteal phase is the cycle from ovulation to the start of the next menstrual cycle, usually lasting 14 days.
During this phase the corpus luteum develops which forms from the remaining ovarian follicle after ovulation.
The corpus luteum produces progesterone that prepares the lining of the uterine cavity for implantation of a fertilized egg.
The luteal phase can have two possibilities:
I : Fertilization absent
II : Fertilization present
I : Fertilization absent
If fertilization is absent, the corpus luteum converts to the corpus menstrualis.
Corpus menstrualis converts to corpus albicans and then disappears on day 28.
II : Fertilization present
If fertilization is present, the corpus luteum converts to the corpus luteum verum, which also contains the hormone progesterone and lasts for three months.
Progesterone hormone suppresses the mother’s immunity, so growth of the fetus in the uterine cavity can occur and the condition of abortion is prevented.
2) Uterine Phase:
The uterine phase is further divided into three phases:
1) Bleeding phase (4 days)
2) Proliferative phase (10 days)
3) Secretarial phase (14 days)
1) Bleeding phase (4 days):
When the ovum is not fertilized, the increased level of progesterone hormone in the blood causes vasoconstriction of the blood vessels of the endometrium (innermost layer of the uterus).
Due to this, the blood supply to the endometrium layer of the uterine cavity decreases.
And the condition of hypoxia arises.
This causes necrosis and death of endometrium layer cells and tissues.
Now, due to necrosis and death of these cells and tissues, the condition of hematometra (collection of blood in the uterine cavity) arises.
Due to this condition, the nerve supply goes to the hypothalamus where it stimulates the pituitary gland. The pituitary gland releases oxytocin which is responsible for causing uterine contractions.
Due to this uterine contraction, blood flow to the vaginal site becomes visible. And menstruation starts. It contains endometrial gland, endometrial cells, capillary blood and unfertilized ovum.
When the level of reduced progesterone reaches a critical level, the second ovarian follicle is stimulated by follicle-stimulating hormone (FSH) and the proliferative phase begins.
2) Proliferative phase (10 days):
The proliferative phase is also called the follicular phase.
In this stage, follicle simulating hormone (FSH) causes ovarian follicles to grow and mature to produce estrogen.
Estrogen stimulates the proliferation of the endometrium and prepares it to receive a fertilized ovum.
Thus the endometrium becomes thick (2 to 3 mm) due to rapid cell multiplication.
And due to the increase of mucus secreting gland and blood capillaries, at the end of this phase, due to the effect of Lutenizing hormone (LH), ovulation occurs and the production of estrogen decreases.
3) Secretarial Phase (14 days):
This phase is also called the luteal phase.
Immediately after ovulation, the lining cells of the ovarian follicle are stimulated by luteinizing hormone (LH) and form the corpus luteum.
Now this corpus luteum produces progesterone.
Due to the effect of this progesterone hormone, the endometrium of the uterine cavity secretes more mucus from the secretory gland and becomes edematous i.e. thick (5 to 6 mm) and the endometrium provides a favorable environment for implantation of the fertilized ovum.
Thus, the menstrual cycle is explained in two phases namely ovarian phase and uterine phase.
- Pre Menstrual Syndrome (PMS):
Pre-menstrual syndrome (PMS) is a psychoneuro-endocrine disorder of unknown cause, which may occur before the menstrual cycle. It is a cluster of mood, cognitive and physical disturbances with hallmark symptoms of irritability. It differs from anxiety disorders and depression.
Etiology/ Causes:
Having a family history of pre-menstrual syndrome (PMS),
Having a family history of depression,
domestic violence,
physical trauma,
emotion trauma,
substance abuse,
Associated conditions such as:
Major Depressive Disorder,
Seasonal Affective Disorder,
Generalized Anxiety Disorder,
schizophrenia,
migraine,
asthma,
Epilepsy.
Symptoms and signs:
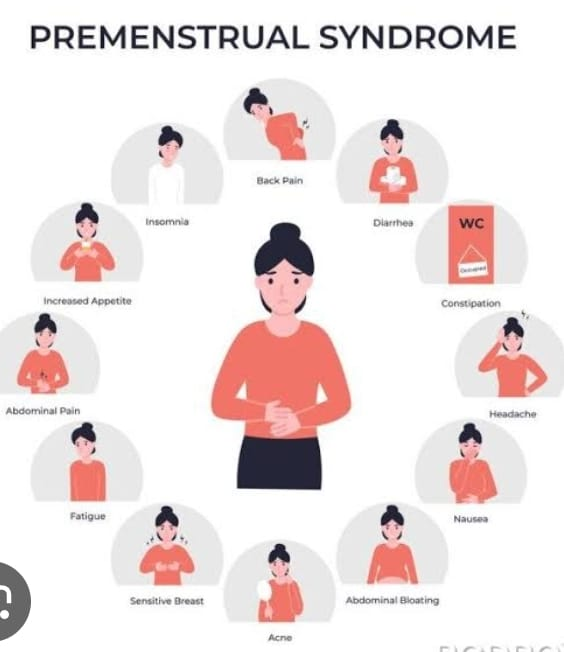
Symptoms of pre-menstrual syndrome (PMS) include physical, emotional and behavioral symptoms.
1) Physical symptoms like,
abdominal bloating,
breast tenderness,
one head,
fatigue,
Muscle and joint pain,
Digestive problems like,
diarrhea,
constipation,
weight gain,
to one
Emotional Symptoms:
1) Mood swings:
irritability,
Sadness.
2) Anxiety:
Tension and pain.
3) Depression:
Feeling of sadness and hopelessness.
Increases sensitivity
Behavioral symptoms:
1) Changes in appetite:
Cravings for eating specific foods (especially sweets).
2) Slip Disturbance:
Changes in slip pattern.
Insomnia.
3)Difficulties in concentration:
Trouble focusing,
Memory issue.
4) Social withdrawal:
Reduced interest in social activities and interactions.
Diagnostic Evaluation:
historytaking,
Physical Examination,
SYMPTOMS ASSESSMENT,
Thyroid test: Weight gain is one of the most common symptoms of premenstrual syndrome. Premenstrual syndrome is conformed by thyroid function. If a thyroid test is done and the thyroid level is normal, it indicates premenstrual syndrome.
Management:
There is no specific treatment for premenstrual syndrome (PMS). Certain treatments can help relieve symptoms such as,
1) Antidepressant and Tranquilizer:
This medicine is generally helpful in relieving anxiety, irritability, restlessness and stress.
Ex: E.g. Alprazolam-0.25 mg taken during the luteal phase reduces anxiety and depression.
2) Diuretic: This diuretic medicine helps to relieve symptoms usually caused by water retention such as abdominal bloating, breast tenderness, swelling of extremities, and weight gain.
3)Pyridoxine 100 mg BD (twice daily) improves tryptophan metabolism especially in case of pills related depression.
4) Selective Serotonin Reuptake Inhibitory (SSRI)
Hormonal treatment:
A) Oral Contraceptive Pills: OCPs aim to suppress ovulation and maintain normal cyclic periods. This is given for 3-6 cycles.
B) Bromocriptine: This is given in cases with certain breast symptoms at a dose of 2.5 mg twice a day daily or as per prescription.
C) Danazol 200-400 mg daily helps produce amenorrhea.
D)GnRH analog/ luteinizing hormone releasing hormone agonist (LHRH agonist) or (LHRH analog).
This is a medication that helps suppress gonadal steroids. They are provided for periods of 6 months also called medical oophorectomy. (To check if bilateral oophorectomy will be of any use) Medicines used are:
A) Goserelin Zoledex: This is a manmade form of the hormone. Dosage – 3.6 mg is provided subcutaneously every 4 weeks.
B) Luprorelin: Brand name LUPRON (works as an agonist at pituitary GnRH receptors).Dose – 3.75 mg subcutaneously or I/M every 4 wk.
C) Triptorelin (Decapeptyl).
Dose – 3mg given I/M every 4 wk.
Nursing Care:
Advise the patient to intake adequate amount of fluid to reduce the condition of abdominal bloating.
Advising the patient to have a well-balanced diet intake.
Advise the client to get at least 8 hours of good sleep. This will help in reducing the level of anxiety and increase the power of judgment and decision making.
Advising the client to engage in regular aerobic exercise and recreational activities will reduce stress levels and keep the client happy.
Provide proper reassurance and psychological support to the client due to which the tension matters and the morale of the client is built up.
Advising the client to join in yoga and meditation properly so that the patient can function properly in a crisis situation.
Salt, coffee, caffeine and alcohol should be avoided especially in the second part of the cycle.
Provide mineral supplements. Because it can reduce both emotional and luteal phase symptoms.
Disorders of Menstruation:
- Dysmenorrhea:
Dysmenorrhea, also known as painful periods or menstrual cramps, is a condition of pain during menstruation. Dysmenorrhea is a term used to describe painful menstruation that usually includes cramps caused by uterine contractions.
Types of Dysmenorrhea:
There are generally two types of dysmenorrhea, namely:
1) Primary or spasmodic,
2) Secondary or congestive
1) Primary or spasmodic:
A condition of painful menstruation with no identifiable pelvic pathology.
The highest level is in the first 2 days of mensis.
2) Secondary or Congestive:
Pathology of the pelvis or uterus causes painful menstruation.
Etiology/ Causes:
1) Primary or spasmodic:
In the ovulatory cycle there is an increase in the production of prostaglandins by the endometrium which causes the contraction of the uterus.
2) Secondary or Congestive:
endometriosis,
adenomyosis,
pelvic infection,
Uterine Fibroids,
intrauterine device,
Congenital uterine and vaginal anomalies.
Symptoms and signs:

Pain (pain starts a few hours before menstruation starts),
The pain lasts for a few hours, usually up to 24 hours, but occasionally up to 48 hours.
The pain is usually spasmodic in the lower area of the abdomen and may radiate to the back and thigh.
Systemic discomfort like,
one head,
Nausea/vomiting,
diarrhea,
fatigue,
Restlessness.
Primary dysmenorrhea may also be accompanied by vasomotor changes such as:
palness,
cold sweat,
Occasional fainting,
sometimes syncope,
Rarely collapse (shock).
Diagnostic Evaluation:
historytaking,
Abdominal Examination,
vaginal examination,
laparoscopy,
Diagnostic laparotomy,
Pelvic ultrasound to detect tumors, endometritis and cysts.
Medical Management of Primary Dysmenorrhea:
Applying local heat such as heating pads increases blood flow and reduces spasm conditions.
- Non-steroidal anti-inflammatory agents such as ibuprofen (Motrin), naproxen (Naprosyn) or valdecoxib (Bextra) for their antiprostaglandin action.
- Exercise increases the level of endorphins. which generally decreases the perception of pain and suppresses the release of prostaglandins.
Medical Management of Secondary Dysmenorrhea:
Treatment of secondary dysmenorrhoea usually involves treating its symptoms and its treatment usually depends on the age of the patient and the severity of the disease.
Treatment:
Medical Management:
A) Prostaglandin synthesis inhibitor:
These medications generally reduce the synthesis of prostaglandins and have a direct analgesic effect.
There are two categories of drugs used
Among them:
FANAMET GROUP:
i Tab. Mefenamic acid (250-500 mg) every 8 hours.
ii. tab. Flufenamic acid (100-200 mg) 8 hourly is recommended.
Propionic acid derivatives:
i Tab. Brufen (400 mg 8 hourly.).
ii. tab. Naproxen (250 mg 6 hourly.)
iii tab. Indomethacin (25 mg 8 hourly.)
B) Oral Contraceptive:
This medication is generally suitable for candidates who,
1) For candidates who are unresponsive to prostaglandin synthesis inhibitor medication
2) Those who have candida condition of heavy periods.
3) Prostaglandin drugs are contraindicated. Oral contraceptives are used in such patients.
Drug Used:
Dydrogesterone: It interferes with ovarian steroidogenesis and helps control pain.
How to take medication?
i It is taken for 3 days to 20 days x 3-6 cycles of cycle.
ii. If the above treatment fails, laparoscopy is indicated to find the cause.
Surgical Management:
Dilatation of cervical canal,
Bilateral block of pelvic plexuses.
Pre-sacral neurectomy.
Nursing Management:
Providing proper psychological support to the patient.
Providing proper explanation to the patient.
Providing education to patients to maintain proper personal hygiene.
Providing instructions to the patient to perform daily routine activities.
Advise the patient for hot drinks and hot compression.
Advise the patient to avoid cold drinks.
Advising the patient for proper daily change of clothes and daily bathing.
Provide proper analgesic medicine to the patient.
Provide anti-spasmodic medication to the patient.
Advise the patient to reduce stress.
Like giving advice for adequate sleep, good nutrition, exercise.
Provide education to patients about adverse effects of medication.
- Amenorrhea:
Definition:
Amenorrhea is a menstrual problem seen in females. In the condition of amenorrhea, there is absence of monthly menstrual periods in females. This condition is called amenorrhea.
Type of Amenorrhea:
Two types of amenorrhea are commonly seen:
1) Physiological amenorrhea,
2) Pathological amenorrhea.
1) Physiological Amenorrhea:
Physiological amenorrhea is a condition in which there is no disease present in the reproductive system of the female during which there is absence of menstrual cycles (periods) in the female, this condition is called physiological amenorrhea.
Physiological amenorrhea is divided into two types viz.
1) Primary amenorrhea,
2) Secondary amenorrhea
1) Primary amenorrhea: When the female does not attain puberty age i.e. when the female does not attain puberty at 13 years and periods are absent during the period before that then this condition is called primary amenorrhea.
2) Secondary Amenorrhea: Secondary amenorrhea is a condition in which a female who is 1) pregnant 2) lactating mother and 3) menopausal female has absence of periods in these three conditions then this condition is called secondary amenorrhea. .
2) Pathological amenorrhoea: i.e. a disease is present in the reproductive system of the female or a pelvic pathology is present in the female due to which the menstrual cycle is absent then this condition is called pathological amenorrhoea pelvic pathology such as infection including, bacterial infection viral infection or female Absence of periods due to trauma or inflammation and adhesions in the reproductive organs is called pathological amenorrhea.
Etiology:
Chromosomal or genetic problem, hormonal imbalance,
Absence of reproductive organs, pregnancy,
Latestation (breastfeeding), menopause,
radiation or chemotherapy,
Polycystic Ovarian Disease (PCOD),
Uterine Surgery,
poor nutrition,
Excessive stress or anxiety,
infection.
Symptoms and signs:
Absence of menstrual cycle,
one head,
to one,
Excessive hair growth,
vaginal dryness,
Abnormal BP,
weight gain,
breast swelling,
Excessive anxiety.
Diagnostic Tests:
History Collection,
Physical Examination,
blood test,
Ultrasonography (USG),
MRI & Ct scan,
thyroid function test,
Hysteroscopy.
Management:
1) Dopamine Agonist: This medication maintains ovulation.
Bromocriptine.
2) Hormonal Replacement Therapy (HRT): That is, in women whose progesterone or estrogen levels decrease, in this condition, progesterone and estrogen levels are replaced.
3) Oral contraceptives are also prescribed to restore the menstrual cycle.
4)Surgery: When there is any anatomical abnormality in the female reproductive system, surgery is also performed to correct the abnormality in any organ.
5) Nutritional supplements are provided to treat the patient’s amenorrhoea condition.
Cryptomenorrhea:
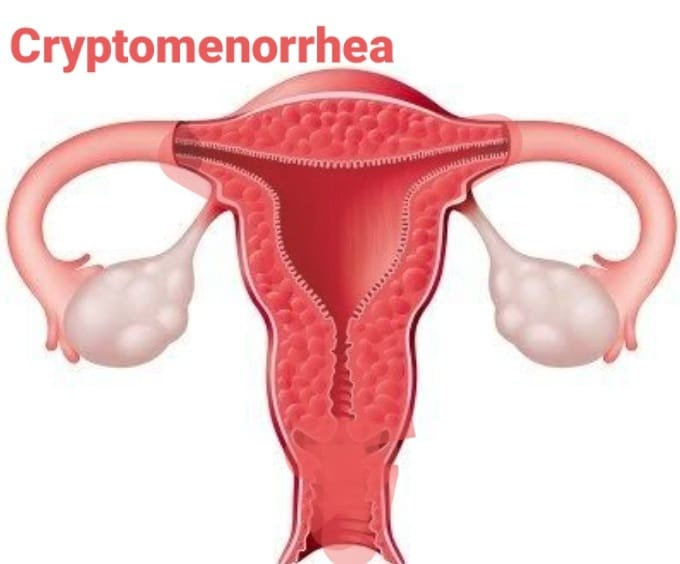
Definition:
Cryptomenorrhea is a condition in which there is periodic shedding of the endometrium, the innermost layer of the uterine cavity, as in the normal menstrual cycle, but this menstrual blood cannot be expelled due to an obstruction in the genital track or passage, i.e. the uterus. If there is accumulation of blood in the KVT itself, then this condition is called cryptomenorrhea.
Types of Cryptomenorrhea:
1) Congenital Cryptomenorrhea This condition is usually present at birth.
2) Acquired cryptomenorrhea: This type of condition arises after birth.
Etiology:
1) Congenital cryptomenorrhea:
imperforate hymen,
Atresia in upper 3rd part of vagina and cervix.
Transverse vaginal septum.
2) Acquired cryptomenorrhea:
Stenosis of cervix
It is usually due to amputation, deep cauterization.
3) Secondary vaginal atresia can usually occur after neglected and difficult vaginal delivery.
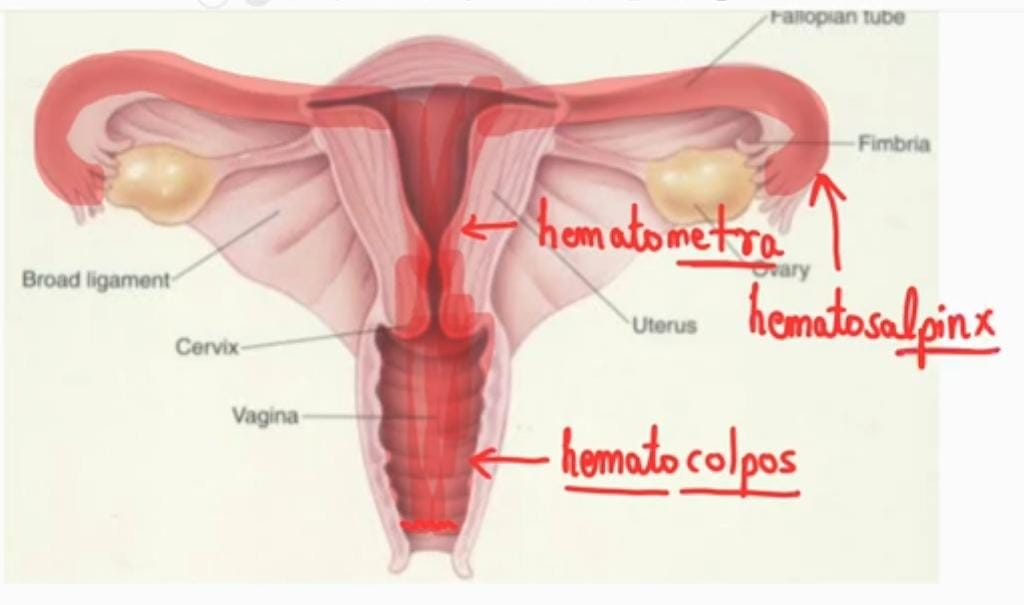
Pathophysiology:
Due to obstruction in the vaginal passage.
↓
Accumulation of blood occurs.
↓
Hematocolpus (retention of menstrual blood in vagina due to imperforate hymen).
↓
Hematometra (accumulation of menstrual blood in the uterine cavity).
↓
Hematosalpinx (accumulation of blood in the fallopian tubes).
Symptoms and signs:
Periodic lower abdominal pain (13-15 years in congenital case),
amenorrhea,
Hematocolpus (retention of menstrual blood in vagina due to imperforate hymen).
Urinary complications such as increased urinary frequency,
dysuria,
or urinary retention.
Complications:
Hematocolpus (retention of menstrual blood in vagina due to imperforate hymen),
Hematometra (accumulation of menstrual blood in the uterine cavity),
Hematosalpinx (accumulation of blood in the fallopian tubes).
Diagnostic Evaluation:
History Collection,
Physical Examination,
A bulging hymen is seen during vulval examination,
Globular mass like structure filling over hypogastium region during abdominal examination.
Vaginal area fullness feeling and uterine mass like structure feeling during rectal examination.
Management:
A simple dilatation of the cervix is done to drain the blood.
In the condition of imperforated hymen, a cruciate incision (X shape) is performed due to which the blood can drain properly.
Reconstructive surgery is performed to maintain patency.
- Menopause:

Introduction: Menopause is the permanent cessation of the menstrual cycle. The word menopause is derived from the Greek word ‘mens’ meaning ‘menstrual’ and possis meaning ‘cessation’ (permanent stop). Menopause is part of a woman’s natural aging process when a woman’s ovaries produce low amounts of estrogen and progesterone and when a woman is no longer able to become pregnant. This condition is called menopause.
Menopause is the permanent cessation (stop) of menstruation at the end of reproductive life in a female due to the loss of ovarian follicular activity. This condition is called menopause. It is also known as climacteric. The average age of menopause is 51 years with a range of (43-57) years.
Etiology:
Age (female whose age is after 45 years),
Loss of ovarian sensitivity to gonadotrophin stimulation leads to follicular decline of function follicles and thus conditions anovulation.
Ovaries are not able to release eggs (ovum) into the fallopian tubes as estrogen levels and progesterone hormone levels decrease.
Symptoms and signs:
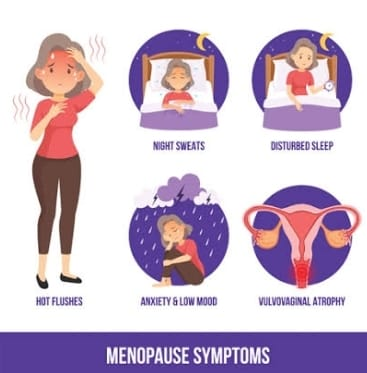
Irregular periods,
Dryness of vaginal area,
Recurrent urinary tract infection,
hot flush,
night sweats,
Slip disturbance and irritability,
Sudden reddening of the skin over the neck and chest with intense heat fillings of the body.
Profuse perspiration.
Breast discomfort.
Filling of cold.
Osteoporosis.
Dryness of skin.
Weight changes.
Head one.
Mood swings.
Slowed metabolism.
Vaginal itching and discomfort.
Urinary problem.
Joint pain.
Dyspareunia.
Buildup of fat in the abdominal area.
Hair thin to be.
Loss of breast size.
Concentration difficulty.
Irregular heart beat.
Health Education and Counselling:
To provide proper reassurance to the client.
Explaining Hormonal Replacement Therapy (HRT) to the client.
If the client has a condition of hot flushes, advise to avoid alcohol, smoking, spicy food, hot coffee and cold liquids.
Advise the client to take the slip in a properly well-ventilated area.
If the client has the condition of insomnia then giving advice to do yoga, exercise and meditation.
Advise the patient to use a proper vaginal moisturizer and lubricant if there is a condition of vaginal dryness.
Provide calcium and vitamin D supplements if the client has the condition of osteoporosis.
Regular checkup of client’s blood pressure, sugar level, cholesterol, weight. And giving advice for female mammogram.
Advise the client for aerobic exercise.
Advising the client to intake frequent and light meals.
Antidepressant medication should be provided if the child is in a depressed mood.
Hormonal Replacement Therapy (HRT):
Hormonal replacement therapy is commonly used to decrease menopausal symptoms such as mood swings, vaginal dryness, night sweats, bone weakness, and more.
HRT (hormonal replacement therapy):
It is generally available in the form of tablets, gels, vaginal creams, skin patches and estrogen-releasing vaginal rings.
1) Oral Estrogen: This is a drug/medicine that usually involves a combination of estrogen hormones used to prevent hot flushes, vaginal problems, hypoestrogenism (low estrogen levels), osteoporosis and some other symptoms of menopause. Hormonal replacements used in oral estrogen include:
premarin,
Micronidase estradiol.
2) Oral progestin: It is commonly used in menopausal women to prevent hot flushes, sleep disturbances, and osteoporosis.
a) Micronized Progesterone (Prometrium)
b) Medroxyprogesterone Acetate.
3) Combination of oral estrogen and progesterone:
It usually helps in relieving menopausal symptoms like hot flushes, chills, sweating. such as,
Activella (estradiol/norethisterone acetate)
Other hormonal replacement methods such as:
Cyclic Oral,
transdermal estrogen preparation,
Vaginal Estrogen Preparation,
Transdermal estrogen and progesterone preparations,
Oral estrogen and androgen combination
And
Involvement of Astratest etc.