ENGLISH GNM-T.Y–Midwifery& Gynecological-date-03/09/2019 (done-UPLOAD-PAPER NO.1)
GNM-T.Y–Midwifery& Gynecological-date-03/09/2019

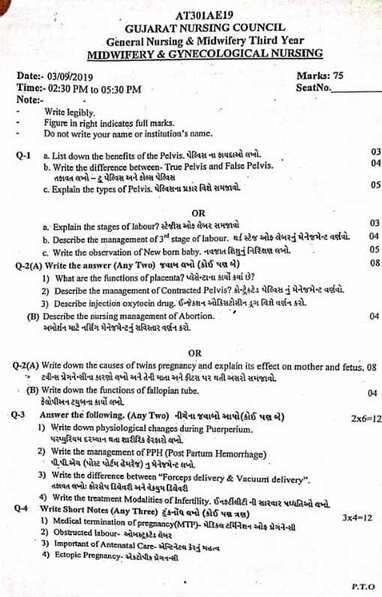
⏩ Q-1 🔸 a. List down the benefits of the Pelvis. 03 benefits of pelvis are millions.
Benefits of Pelvis:
The pelvis is a crucial anatomical structure in the human body, which provides several key benefits:
1) Support and Stability:
The pelvis forms the base of the spine and supports the weight of the upper body when standing and sitting. It also acts as a stable base for movement and locomotion.
2) Protection of Organs:
Pelvis works to enclose and protect vital reproductive organs (such as uterus, ovaries and testes), urinary bladder, and part of the gastrointestinal system.
3) Child Birth:
During child birth, the pelvis plays a critical role by providing a passageway (birth canal) through which the child can be born. Ease or difficulty in delivery depends on the shape and size of the pelvis.
4) Attachment of muscles:
Numerous muscles are attached to the pelvis bone such as the muscles of the lower back, abdomen, buttocks (gluteal muscles) and pelvic floor muscles. These muscles provide a contribution to posture, movement and stability.
5) Weight Distribution:
The pelvis helps distribute the weight of the upper body evenly over the lower limbs when standing and walking, reducing stress on the spine and lower back.
6) Support and Protect Reproductive Organs:
The pelvic floor muscles also play an important role in providing proper support and protection to the reproductive organs.
7)Blood Vessels and Nerve Pathway:
The pelvis contains major blood vessels and nerve pathways that supply the lower limbs and pelvic organs and work to maintain proper circulation and nerve pathways.
Overall, the pelvis is important for maintaining posture, facilitating movement, protecting internal organs, and providing support for reproductive and urinary function.
Its structural integrity is vital to overall health and well-being.
Thus, the pelvis has many important benefits.
🔸 b. Write the difference between- True Pelvis and False Pelvis. 04 Differentiate between-two pelvis and false pelvis
Difference between True Pelvis and False Pelvis:
The human pelvis is divided into two main regions:
True pelvis (lesser pelvis) and false pelvis (greater pelvis).
Here is the difference between true pelvis and false pelvis:
True Pelvis (Laser Pelvis):
1) Location and Size:
Location
The true pelvis is located deep and inferior to the pelvic cavity, located between the pelvic brim (pelvic inlet) and the pelvic floor.
size
The pelvis is relatively small and narrow compared to the pelvis.
2) Content:
Pelvic inlet
The upper boundary of the true pelvis is called the pelvic inlet.
Pelvic outlet
The lower boundary of the true pelvis involving the pelvic floor and structures through which the baby passes during childbirth.
Pelvic cavity
A space of true pelvis that involves the pelvic organs like bladder, rectum and reproductive organs and parts of the gastrointestinal tract.
3) Functions:
Provides support and protection to the pelvic organs.
At the time of child birth, it works as a passageway for the birth canal.
Plays a crucial role in pelvic stability and weight transmission from the spine to the lower limbs.
4) Shape: It is of curved cylindrical shape.
5) Clinical Significance: Assessment of the dimensions and shape of the true pelvis is important in obstetric evaluation as it affects the timing of labor and delivery.
••>False Pelvis (Greater Pelvis):
1) Location and Size:
Location False pelvis refers to the part above the pelvic brim.
Larger and covers more space as compared to size true pelvis.
2) Contents: Abdominal organs and structures are mostly present in place of pelvic organs.
The iliac crest falls as the upper boundary of the pelvis, formed by the iliac bone.
Abdominal Organs
Abdominal organs involve the intestines (small and large intestines), kidneys, and the lower portion of the abdominal cavity.
3) Functions:
Provides support to the weight of the abdominal organs.
The attachment side provides the muscles and ligaments that connect the spine to the pelvis and lower limbs.
Provides facilities for movement and stability during standing and walking.
Provides support to the enlarged uterus during pregnancy.
4) Shape: Flatter and more open compared to true pelvis.
5) CLINICAL SIGNIFICANCE: The false pelvis has less involvement in obstetric evaluation but plays an important role in abdominal cvt and pelvic region surgery, as it provides access and support to the lower abdomen and pelvis during surgical procedures.
••>In short:
True pelvis: lies deep within the pelvic cavity, is small in size, and contains the pelvic organs. The true pelvis plays a direct role during child birth and in pelvic stability.
False pelvis: A false pelvis is located above the pelvic brim, enlarged in size and involves the organs of the abdomen. It provides support to the abdominal cavity and works as a base for the true pelvis.
Thus, the difference between true pelvis and false pelvis is as follows.
c. Explain the types of Pelvis. 05
Types of pelvis:
In anatomy, the pelvis can be categorized into 4 types based on its shape and dimensions.
This classification is important in various medical fields, mainly obstetrics and orthopedics, because it can influence the outcome of child birth and the risk of pelvic fracture.
Here are the main (4) types of pelvis:
1) Gynecoid pelvis,
2) Android Pelvis,
3) Anthropoid pelvis,
4)Platypeloid pelvis.
1) Gynecoid Pelvis: About 50% of the pelvis in the human being is of the gynecoid type. So Gynecoid is the highest type of pelvis than other types of pelvis.
Description: Gynecoid pelvis is commonly called female pelvis, which is round in shape.
The cavity of the gynecoid pelvis is wide and cellular.
Optimal for Childbirth: This shape is ideal for childbirth as it provides an adequate amount of space for the child to pass through the birth canal.
Clinical Significance: Gynecoid pelvis is associated with easy and smooth child birth compared to other pelvis types.
2) Android Pelvis: Android pelvis is found in about 20% of human beings.
Description Android pelvis resembles male pelvis in shape and structure.
And it is heart shaped.
characteristic
Heart Shape Pelvic Inlet In the android pelvis, the pelvic brim is heart-shaped and has a narrow anterior-posterior diameter and a wide transverse diameter.
Prominent sacrum The sacrum protrudes further, causing the pelvic cavity to narrow.
Less favorable for child birth: Android pelvises are less favorable for child birth due to narrow pelvic inlet and reduced ability to pass the child.
CLINICAL SIGNIFICANCE An android pelvis may increase the risk of obstructed labour. Because of this, there is a need for further intervention for child birth.
3) Anthropoid Pelvis: Anthropoid pelvis is found mostly in 25% of human beings.
Description Anthropoid pelvis is an oval shaped pelvis.
features
Oval pelvic inlet In the anthropoid pelvis the anterior-posterior diameter is large while the transverse diameter is narrow.
The long and narrow anthropoid pelvis is long from front to back, providing adequate space for the passage of the fetus.
Favorable for child birth Anthropoid pelvis is generally favorable for child birth as it provides adequate space for the descent of the fetus.
CLINICAL SIGNIFICANCE Women with an anthropoid pelvis usually experience an uncomplicated labor and delivery.
4)Platypeloid Pelvis: Platypelloid pelvis is mostly seen in 5% of human beings.
Description
A platypelloid pelvis is flat and wide.
Since the inlet and outlet of platypelloid pelvis are compressed, this type of pelvis is kidney shaped.
Features:
Flattened Pelvic Inlet An inlet is flat or oval in shape with a transverse diameter significantly wider than the anteroposterior diameter.
Wide pelvic cavity:
The pelvic cavity is wide but shallow.
A less common platypelloid pelvis is less common and can pose challenges during childbirth due to the shape of the pelvic inlet.
Clinical Significance: Women with a platypeloid pelvis may experience prolonged labor or difficulties with descent of the fitus, requiring careful monitoring during child birth.
Thus, there are total four types of pelvis.
🔸 OR🔸
🔸a.Explain the stages of labour? Explain the stages of labor 03
Stages of Labour:
The stages of labor are divided into four stages.
1) First Stage of Labour,
2) Second Stage of Labour,
3) Third Stage of Labour,
4) Fourth stage of labor
••>1) First Stage of Labor (Cervical Stage):
The first stage of labor is the initial phase of childbirth. In which the cervix gradually opens (dilate) and thins (effacement). Due to this, the baby can pass from the uterine cavity into the birth canal (vagina). In which regular and rhythmic uterine contractions are seen and the frequency, intensity and duration of uterine contractions gradually increase.
The first stage of labor starts with true labor pain and lasts until full dilatation of the cervix (10 cm). This stage is also called the “cervical stage”.
The first stage of labor is further divided into 3 stages:
First Stage No Time Period:
Primigravida:=12-16 hours, and
Multigravida:=6-8 hours, no.
The first stage of labor is divided into three phases.
1) Latent Phase,
2) Active phase,
3) Transitional phase
1) Latent Phase,
The latent phase is known as “prodomal labor” or “pre-labor”.
Cervical dilatation of 1-4 cm centimeters occurs in this stage.
Contractions in this phase repeat every 15-30 minutes and last for 15-30 seconds.
In this phase the mother is talkative.
2) Active phase,
Active phase is also known as dilatation phase.
In this second phase, the cervix dilates by 5-7 centimeters. And contractions are repeated every 3-5 minutes and last for 45-60 seconds. In this stage mother feels restlessness.
3) Transitional phase
In the transitional phase, the dilatation of the cervix is 8-10 cm.
Contractions are repeated every 2-3 minutes and last for 60 to 90 seconds.
The first stage of overall labor is the critical period in which, after the cervix opens, the uterus prepares for delivery by providing the proper position of the baby in the uterine cavity. Continuous monitoring by health care providers is important to improve the condition and well-being of the mother and fetus during this stage.
2) Second Stage of Labor (Expulsion of Fits):
The period from full dilatation of the cervix to the birth of the baby through the birth canal is called the second stage of labor.
its duration,
In primi gravida: 1-2 hrs
In multigravida: 20-30 minutes.
The second stage of labor is further divided into two phases:
1) Propulsive phase,
2) Explosive phase.
1) Propulsive Phase:
The propulsive phase starts from full dilatation of the cervix until the presenting part of the fitus descends to the pelvic floor (+4 +5 stations).
2) Explosive Phase: This is the explosive phase until the baby is completely expelled from the uterine cavity along with the mother’s bearing down efforts.
3) Third Stage of Labor (Expulsion of Placenta):
This stage is the period from the expulsion of the baby to the expulsion of the placenta and membranes is called the third stage.
Its time duration is 15 minutes in primi gravida and multigravida
4) Fourth Stage of Labor (Observation Stage):
The observation stage after the birth of the baby is called the 4th stage of labor. During this stage, the general condition of the mother and the condition of the newborn and the behavior of the uterus are carefully monitored.
Its time duration is 1 hour.
Thus, the time duration of all four stages of total labor (1st stage + 2nd stage + 3rd stage + 4th stage) is 13-15 hours in primigravida and 6-8 hours in multigravida.
b. Describe the management of 3rd stage of labor. 04 Describe the management of third stage of labour.
Management of Third Stage of Labour:
Management of the third stage is most crucial because it involves separation and expulsion of the placenta from the uterine cavity, and to prevent complications of postpartum hemorrhage in the third stage.
Management of the third stage requires strict vigilance of the placenta to prevent complications of postpartum hemorrhage.
Stage of Management Two methods are currently used in the management of the third stage.
1) Expectant (watchful) management
2) Active management
1) Expectant (watchful) management
In this management, separation of the placenta and its descent into the vagina is allowed to occur spontaneously.
For this management, placental expulsion is minimally assisted.
In this stage, constant watch is kept on the mother i.e. not leaving the mother alone even for a short period of time.
If the mother is in a lateral position, placing her in a dorsal position will allow a proper understanding of the sign of placental separation and the extent of blood loss.
In this management, only placenta separation, descent and expulsion are properly watched.
One hand is placed on the fundus so that,
a) Separation of placenta can be realized.
b) State of uterine activity i.e. contraction and relaxation can be understood.
Separation of placenta
The placenta begins to separate from the uterine wall within minutes of the baby’s birth, so wait 15 to 20 minutes for the placenta to separate on its own.
No touch technique is used in this.
Ama has a “no touch policy” ie the placenta is expelled by gravity within 15-20 minutes ie no massaging of the fundus.
Do not use any type of uterotonic and do not use any manual method for expulsion of placenta.
Expulsion of placenta
Following points to follow when placenta is expelled:
Advise the patient to apply beer down afters when the uterus becomes hard.
Raised intra-abdominal pressure is important to expel the placenta.
And the placenta may be expelled on its own.
2) Active management
1) Oxytocin is not the drug of choice in the management of the third stage of uterotonic labour.
Provide 10 units of oxytocin IM (intracellular) in management of third stage.
Oxytocin enhances uterine contractions and helps expel the placenta.
2) CCT (Control Cord Traction) Control cold traction uses a manual method in which the umbilical cord is tracked and gently pulled downwards and backwards, allowing the placenta to separate from the uterine wall and then expel it, but the control cord Traxon is performed by placing the hand on the suprapubic area while uterine contractions are present.
3) Delay Coda Cutting Wait for one to three minutes after delivery of fits and then cut the umbilical cord. This technique is more useful in term newborns. Because the newborn can receive an adequate amount of blood from the placenta due to which the condition of anemia can be prevented.
But in pre-term babies, the liver is immature and the red blood cells break down in excess and if delayed coda cutting is done, due to this, the condition of hyperbilirubinemia (jaundice) may arise in the newborn.
4) Post partum vigilance
Proper inspection of placenta after delivery of placenta including proper assessment of cotylodon, lobes and maternal and fetal site followed by fundal massage after delivery of placenta so that uterine contractions can be continued and if retained bits of placenta can be expelled properly. .
c. Write the observation of New born baby.05 Observation of new born baby lakhs.
Observation of Newborn Baby:
Observation of newborns immediately after birth is crucial to assess their overall health, well-being and development.
Here, some aspects for newborn observations are given:
1) General Appearance:
Color: Assess the color of the child’s skin, most children are pink or red in color. If there is cyanosis (bluish discoloration), it indicates breathing difficulties.
Posture: Note the baby’s muscle tone. A healthy newborn baby has their hands slightly flexed and their feet slightly curved along the spine.
Activity: Observation of spontaneous movement involving sucking reflex and grasping reflex.
2) Vital Sign:
Heart rate: Normal range is 120-160/minute.
Respiratory Rate: Normal respiratory rate is 30-60 breaths.
Temperature: Normal temperature is 36.5-37.5°C (97.7-99.5°F).
3) Head and Face:
Fontanels: Palpate the anterior fontanel (soft spot) and posterior fontanel of the newborn. To perform proper closure and tension of the fontanelles.
Ice: Checking ice for its cementery. Assessing red reflex (indicative of normal eye structure) and response to light.
Nose: Assess the patency of the nose so that breathing can be appropriate.
4) Mouth and Neck:
Oral Mucosa: Assess for cleft palate, oral thrush and any lesions in the oral mucosa.
Neck: Assess for any mass like structure or abnormalities in the neck.
5) Chest and Lungs:
Breathing Sound: Properly listening to child’s breathing sound.
Chest Movement: Properly assess whether the child’s chest rises symmetrically and falls down with breathing.
6) Heart and Abdomen:
Heart Sound:
Proper auscultation of heart sound to assess for any murmur type abnormal voice and abnormalities.
Abdomen:
Palpate the abdomen and auscultate bowel sounds to assess whether there is any mass-like structure in the child’s abdomen.
7) Genital Area and Anus:
Genital Area:
To assess whether the anatomical structure of the genital area of the child i.e. male (presence of testes in male child) and female (labial structure in female child) is proper or not.
Anus:
Assess the patency of the anus and assess for any abnormality.
8) Extremities:
Hand and Fits: Counting a child’s fingers and toes. and to assess symmetry or to assess whether there are any abnormalities.
Movement: Assess whether the child has spontaneous movement and the range of motion of the hands and legs.
9) Skin and Umbilicus:
Skin: Assess the child for any birthmarks, lesions and recesses on their skin.
Umbilical cord: Provide proper cord care to the child and assess for any signs and symptoms of infection and bleeding.
10) Behavioral Assessment:
State of Alertness: Properly assess the baby’s level of awareness and the amount of response to stimuli.
Crying: Properly assess whether the child is crying properly or not due to which the respiration status of the child can be properly assessed.
Additional Considerations:
Documentation: To accurately record all findings in the newborn assessment chart.
Parenteral Education:
Parents should be informed about newborn care including proper feeding technique, maintain hygiene, and seek immediate health care if any signs and symptoms of infection are observed in the child.
To provide education to parents for going to the center.
By properly observing the child after birth, if there is any congenital abnormality or potential risk factor of any disease in the child, it can be identified early and adequate measures can be taken and the child’s condition can be prevented from getting complicated.
⏩ Q-2(A) Write the answer (Any Two) 08
🔸1) What are the functions of placenta? Did the placenta?
Functions of Placenta:
Definition:
The placenta has a “discoid shape” due to its septum.
It is “hemochorionic” because its chorion comes into direct contact with maternal blood, and it is “deciduous” because the placenta sheds off after birth.
Placenta is a mass like structure. It usually develops in the anterior or posterior side of the upper uterine segment from two sources namely the fetal component chorion frondozum and the maternal component decidua basalis.
The placenta is connected to the fetus through the umbilical cord and the pregnancy is maintained. The placenta supports the life of the embryo by providing oxygen and food to the embryo and removing toxic materials.
••>Function of placenta
1) Respiratory function The fetus receives oxygen and excretes carbon dioxide through the placenta.
Just as oxygen from the mother’s blood passes into the fetal blood, carbon dioxide in the fetus is transmitted to the maternal blood through the placenta.
2) Nutritive function All types of nutrients like amino acids, glucose, vitamins, minerals, lipids, water and electrolytes are transmitted from the mother to the fitters.
The food taken in the maternal diet reaches the placental side where it is converted into simple form, then the placenta selects the substances required by the fetus and transmits them to the fetus.
3) Storage function Placenta stores glucose, iron and vitamins. And the placenta provides it when the fetus needs it.
4) Excretory function The waste product in the fetus is transmitted to the placenta.
5) Protection Placental membrane has limited barrier function. Some of the antibodies passed from the mother to the fetus provide immunity to the baby for up to three months after birth.
6) Immunological function Antigens of the fetus and placenta act as foreign to the mother. However, graft rejection does not occur because the placenta provides immunological protection against rejection.
7) Hormonal function
steroid hormones
estrogen,
Progesterone.
Protein hormones
HCG (Human Chorionic Gonadotrophin),
HPL (Human Placental Lactogen),
relaxin,
PAPPA (Pregnancy Associated Plasma Protein:= A).
•>HCG (Human Chorionic Gonadotrophin),
HCG (human chorionic gonadotrophin) is produced from the cytotrophoblastic layer of the chorionic villi.
HCG (human chorionic gonadotrophin) is high during 7 to 10 weeks of pregnancy then decreases as the pregnancy progresses it maintains the corpus luteum.
HCG (human chorionic gonadotrophin) is used in pregnancy tests because it is excreted in the mother’s urine.
HCG (human chorionic gonadotrophin) is detected in blood on day 7 and urine on day 9 after fertilization, which indicates a positive pregnancy test.
••> HPL (Human Placental Lactogen)
HPL (Human Placental Lactogen) is produced from the placenta and is involved in lactogenic and metabolic processes of pregnancy. When the level of human chorionic gonadotropin trophin decreases, the level of human placental lactogen (HPL) increases and it continues in throwout pregnancy.
Human placental lactogen (HPL) works as an anti-insulin that increases blood glucose levels and helps supply glucose to the fetus.
••>Relaxin
Relaxin is produced by decidual cells. And it softens the cervix and helps the pelvic ligaments and symphysis pubis to relax the labor process.
••>PAPPA (Pregnancy Associated Plasma Protein:= A)
Pregnancy Associated Plasma Protein:= A works as an immunosuppressant and works to maintain pregnancy.
••> Estrogen
Estrogen is produced by the placenta in a throwout pregnancy. It is essential for welling of the phytoplacenta.
Estrogen increases during labour, which helps in the release of oxytocin, which increases uterine contractions.
••> Progesterone
Progesterone is produced from the synovial layer of the placenta which works as a tocolytic agent and prevents uterine contractions as well as works as an immunosuppressant to help maintain the pregnancy.
🔸2) Describe the management of Contracted Pelvis? Describe the management of contorted pelvis.
Management of Contracted Pelvis:
Management of a contracted pelvis, which refers to a pelvis that is abnormally small and has an abnormal shape that can make the birth of a child difficult, involves careful assessment and intervention to ensure the safety of both mother and child during labor and delivery. need of
Management of Contracted Pelvis:
1) Diagnosis and Assessment:
Pelvimetry
Pelvimetry is a measurement of the pelvis to estimate its dimensions and shape.
This measurement can be done clinically (external measurement) or radiologically (X-ray, MRI).
Take a complete history of the mother Take a complete history of the mother to assess whether any difficulties have arisen in the mother previously at the time of delivery or at the time of cesarean delivery.
Clinical Evaluation A complete physical examination of the mother including mostly pelvic measurements can be done to properly assess the condition of the contracted pelvis.
2) Antenatal care:
EARLY DETECTION Early identification of contracted pelvis through routine antenatal checkup or ultrasound examination during the early period of pregnancy.
CONSULTATION Referring women with high-risk pregnancies to specialist obstetricians and perinatologists for their comprehensive management.
3) Labor Management:
Continuous monitoring Close monitoring of maternal and fetal condition during labor including proper monitoring of fetal heart rate and proper assessment of maternal vital signs.
Labor Progress Continuously Assessing the Labor Process If labor is slow or arrested, it indicates a condition of cephalopelvic disproportion.
Positioning Provide the mother with a proper position that provides optimal pelvic dimensions for labor to progress.
4) Intervention During Labour:
Artificial Rupture of Membrane If the membrane is intake and the progress of labor is slow, then the progress of labor can be improved by artificially rupturing the membrane.
Oxytocin Infusion Provide oxytocin infusion to improve contractions along with continuous monitoring of fetal and uterine contractions.
Instrumental delivery: Vacuum extraction or forceps delivery can be performed if the baby is in distress and vaginal delivery is possible.
5) Cesarean section:
Indications Cesarean section is performed when vaginal delivery is impossible to prevent fits and any maternal complications.
Timing When vaginal delivery is impossible, it is important to take the decision to perform a timely caesarean section to prevent complications for the fetus and the mother.
6) Postpartum Care:
Maternal monitoring Closely monitoring the mother during the postpartum period due to which any complications occurring during the postpartum period such as postpartum hemorrhage can be prevented.
Neonatal Care Providing immediate newborn care after the birth of the newborn especially when any condition of complicated labor arises so as to ensure that the newborn is properly well-being.
7) Counseling and Education:
Education To educate the mother and her family members by providing complete information about the mother’s condition and its causes and interventions.
Future Pregnancy Planning Discuss the effect of a contracted pelvis on future pregnancy and delivery options.
8) Multidisciplinary Approach:
Team collaboration Obstetricians, midwives, anaesthetists, neonatologists should be available as specialists when the condition is too complicated.
9) Psychological Support:
The condition of contracted pelvis is stressful and emotionally challenging for the woman, so proper psychological support should be provided to the mother and family members.
Thus, proper management of contracted pelvis is important to prevent complications to mother and child.
🔸3) Describe injection oxytocin drug Describe about injection oxytocin drug.
Injection Oxytocin:
•>Introduction
Oxytocin is an octopeptide. Oxytocin is naturally produced in the hypothalamus but is stored and released in the posterior pituitary. Oxytocin has a half life of 3-4 minutes and its duration of action is about 20 minutes.
It is rapidly metabolized and degraded by oxytocinase.
•>Mode of Action
Oxytocin helps the uterine muscles contract. Oxytocin’s main mode of action is contraction of the fundal part of the uterus and relaxation of the cervix.
Oxytocin also helps in the release of prostaglandins from the decidua and also helps in stimulating milk ejection from the breast.
•>Preparation used
1) Synthetic Oxytocin (Syntocin or Pitocin)
It has oxytocic effect apart from vasopressor action.
Syntocin is available in ampoules containing 5 IU/Ml.
Pitocin 5 IU/ml.
2) Syntometrine ( Sandoz):
Combination of Syntocin 5 unit and Ergometrine 0.5 mg.
3) Desamino Oxytocin:
Not inactivated by oxytocinase and is 50-100% more effective than oxytocin. It is available in buccal tablets.
Contains 50 IU.
4) Oxytocin Nasal Solution:
Contains 40 units/ml.
Indications:
Oxytocin is used as a therapeutic and diagnostic test during pregnancy, labor and the puerperium period.
1) Pregnancy:
Early pregnancy
Used to accelerate abortion and for induction of abortion with other abortifacient agents.
To stop bleeding after evacuation of uterus.
Late Pregnancy:
For induction of labour.
After expulsion of the placenta.
For cervical ripening.
2) Labor
Augmentation of Labour.
Uterine inertia.
During the active management of the third stage of labor.
Used after expulsion of placenta as an alternative to ergometrine.
To prevent and treat post partum haemorrhage.
3) Purperium or postpartum
To prevent and treat post partum haemorrhage.
To increase milk ejaculation.
•> Contraindication:
Pregnancy
Grand Multipara,
Contracted pelvis,
History of previous caesarean section,
hysterotomy,
Malpresentation.
During labor
All contraindications during pregnancy,
obstructed labour,
Incoordinate uterine contractions,
Fetal distress.
Its time
hypo volemic state,
Cardiac Diseases.
•> Dangers/ Complications of Oxytocin:
Maternal
Uterine hyperstimulation
(over activity),
uterine rupture,
water intoxication,
hypotension,
antidiuresis,
Pituitary Soc.
fits
Fital Distress,
fetal hypoxia,
Increase incidence of neonatal jaundice.
•>Route and Dose of Oxytocin Administration
controlled intravenous infusion,
Bolus IV (intravenously),
IM (Intra Muscular),
Buccal tablets or nasal spray.
Induction or Augmentation of Labour:
IV (intravenously) Initial dose is started at a low rate (1-2 milliunits per minute) then the dose can be gradually increased to increase uterine contractions. A maximum of 20-40 munits/minute can be administered and it Every woman vice is different.
To increase uterine contractions and to prevent and treat post-partum haemorrhage:
IM (Intra Muscular)
If IM (intra muscular) administration is to be done, 10 IU is given immediately after delivery of the baby.
OR
If IV (intravenous) administration is to be done, 20 IU is administered in a pint of 500 ml of normal saline or Ringer’s lactate and then the infusion is provided.
•> Nursing Responsibilities
Administering injection oxytocin is a critical responsibility for the nurse Although oxytocin plays an important role in facilitating labor and managing labor progression, the nursing responsibilities for oxytocin administration are as follows.
1) Assessment and Preparation
assessment
Before administering injection oxytocin, the nurse should properly assess the pregnant woman’s labor progress, fetal heart rate, and uterine contractions and maternal vital signs. Due to which medication can be properly initiated and continued.
Preparation
Properly prepare oxytocin solution as per hospital protocols and as prescribed by health care personnel.
2) Monitoring
Uterine contractions
Continuously monitor uterine contractions by palpation method and assess whether urine contractions are regular and proper or not.
Fetal heart rate
Continuously monitor fetal heart rate and assess for signs and symptoms of fetal distress.
3) Administration
Initiation and Adjustment
Properly administering medication prescribed by a health care provider.
Keep the infusion rate low initially and then increase the infusion based on uterine contractions and labor progression.
4) Patient education
Explanation
Provide explanation to the mother and her support portion about the purpose of oxytocin infusion, its side effects, and continuous monitoring.
Expectations
Provide an explanation to the mother and her spotters about the expected increase in intensity and frequency of uterine contractions after administration of oxytocin.
5) Documentation
charting
Documentation of oxytocin administration, including starting time, infusion rate, maternal vital signs, uterine contraction pattern, and continuous charting of fetal heart rate.
Response to treatment
Properly monitor uterine contractions and assess progress of labor to assess how effective oxytocin is after oxytocin infusion.
And any side of oxytocin
Assess whether there is an effect or not.
6) Communication
Communication with other healthcare personnel for oxytocin administration eg.
obstetrician,
Collaboration with midwife and other nurses.
Patient updates
Provide ongoing patient updates to the mother and her support person including information on labor progress, fetal well-being, and any changes after oxytocin administration.
7) Emergency Response
If any type of side effect is observed during the administration of oxytocin and other symptoms are observed such as uterine hyperstimulation, then oxytocin should be discontinued immediately and supportive care should be provided.
Thus there is a need to perform this type of nursing responsibility while providing injectable oxytocin.
🔸(B) Describe the nursing management of Abortion. 04 Describe nursing management for abortion in detail.
Nursing Management for Abortion:
Nursing management of abortion involves comprehensive care and support for women undergoing termination of pregnancy, whether spontaneous (miscarriage) or induced (therapeutic) abortion.
1) Patient Assessment:
History Collection
Completing a complete history of a woman’s medical, obstetric and gynecological conditions.
Assessing the gestational age of pregnancy.
Identifying Reasons for Abortion
Physical Examination:
Vital sign
Complete vital sign monitoring of the mother including,
blood pressure,
pulse,
Properly and continuously monitoring respiration and temperature etc.
Assess the client for any signs of hemorrhage such as excessive bleeding, pallor, etc.
Perform an abdominal examination to assess the tenderness of the uterine cavity.
Then perform a pelvic examination to assess whether cervical dilatation and products of conception are present in the uterine cavity.
2) Psychological Support:
Providing proper emotional support and counseling to mother and family members.
Advising the patient to explain his feelings.
Providing education about available resources for psychological support such as support groups and counseling services.
3) Pain Management:
Provide prescribed analgesic medication such as NSAID or Acetaminophen to relieve the patient’s pain.
Advise the patient to use non-pharmacological measures such as heating pads and relaxation techniques to relieve the patient’s pain.
4) Management and Monitoring of Complications:
Hemorrhage
Assess the patient for signs of excessive building.
Properly assessing the amount of blood loss to the mother Preparing for blood transfusion if the patient needs it
infection
Assess the patient for signs and symptoms of infection such as,
fever,
foul smelling,
Properly assess for symptoms like discharge and lower abdominal pain.
Provide adequate antibiotic medication to the patient as prescribed.
Retained product of conception
Properly monitor the patient for signs of incomplete abortion such as continuous heavy bleeding and camping pain.
Preparing the patient for possible surgical intervention such as dilatation and curettage (D & C).
5) Patient Education:
Post Abortion Care
Provide patient education about signs and symptoms requiring immediate medical care such as heavy bleeding, pain, and fever.
Provide instruction to maintain perineal hygiene to prevent infection.
Follow up care
Advise the patient to make a follow-up appointment one to two weeks after the abortion so that complete recovery can be properly ascertained.
Provide complete patient education about the importance of follow up visits.
Contraceptive counselling
Provide information to patients about available contraceptive options to prevent unintended pregnancy.
Also provide patient education about the timing of using contraceptives after abortion.
6) Discharge Planning:
Discharge planning involves ensuring that the patient is able to go home and that the patient can receive adequate support and a safe environment at home.
Then provide instructions in a written (written) form that includes information on meditation use, activity restrictions, and signs of complications.
Provide information about support services and resources available in the community.
Documentation:
Properly and accurately document all assessments, interventions, patient responses and education provided.
Recording the emotional states of patients and providing counseling and psychological support to them.
The nurse plays a critical role in the comprehensive management of women who have had an abortion, which involves providing compassionate care, ensuring the patient’s physical and emotional well-being, and providing patient education about post-abortion care and contraceptive options. is
Proper assessment, monitoring and providing proper intervention of the patient can prevent complications and facilitate the recovery process.
Thus, proper management of abortion plays an important role in improving the mother’s well-being.
🔸OR🔸
⏩ Q-2 🔸(A) Write down the causes of twins pregnancy and explain its effect on mother and fetus, 08 Write down the causes of twins pregnancy and explain its effects on mother and fetus.
•> Causes of Twins Pregnancy,
•>Effects of twins pregnancy on mother and fetus
Causes of Twins Pregnancy: When two fetuses develop together in the uterine cavity, they are called twins.
••> Causes: Exit cause is unknown.
1) Due to maternal environmental factors like:
Race: Highest found in Negrons.
Hereditary: This is mainly transmitted from the maternal side more commonly.
Advanced Age of Mother: Due to advanced age of mother like 30-35 years.
Hormonal factor: Due to some type of hormones releasing more than one egg in ovulation at some time.
Due to Influence of Parity: Mainly 5th gravida due to increase parity.
Iatrogenic in this due to drugs used in ovulation.
Due to previous pregnancy: If there are twins in the first pregnancy, there is a slight chance of twins in the next pregnancy.
Hyperovulation: Certain conditions such as polycystic ovary syndrome (PCOS) and other hormonal imbalances increase the chances of multiple ovulation.
2) Superfecundation In which two different ova are released in the same cycle and fertilized in a short period of time by separate acts of coitus is called superfecundation.
3) Superfetation, in which two ova are released through different menstrual cycles and fertilization occurs, this is called superfetation.
4) Fitters papyraces or compresses in which a placenta has died early and dead placentas have a flat end and compressed between the membrane of the living placenta and the uterine wall.
5) Fetal acardiasis occurs in these uniovular twins.
6) Assisted Reproductive Techniques: Fertility treatments such as in vitro fertilization (IVF) can lead to multiple pregnancies by fertilizing multiple eggs.
••>Effects of Twins Pregnancy on Mother and Fetus:
Twins pregnancy means that more than one child is growing in the uterine cavity, due to which the need for the growth and development of the twins is also higher, then due to this reason there is an effect on the health of the mother and the fetus.
Effect on Mother:
1) Physiological Demand:
Increase Risk of Complications:
Gestational diabetes, hypertension,
There is an increased risk of conditions such as pre-eclampsia, anemia and placental abnormalities such as placenta previa and abruptio placenta.
Hyperemesis gravidarum:
Twins pregnancy causes hyperemesis gravidarum i.e. excessive amount of nausea and vomiting which can lead to conditions like dehydration, nutritional deficiency and electrolyte imbalance in the mother.
Increase Weight Gain:
When a woman has a twin pregnancy, the mother’s weight gain is greater in comparison to a singleton pregnancy.
Fatigue and Discomfort:
Compared to a singleton pregnancy, the uterus in twin pregnancy is larger and stretches rapidly, which causes discomfort, back pain and fatigue to the mother.
2) Delivery Complications:
Higher Chances of Cesarean Section:
When there is a condition of twins pregnancy, the chances of delivering by caesarean section are high due to abnormal presentation of the fetus (breech presentation) and any other type of complications.
Increase risk of pre-term birth:
When there is a twin pregnancy, the chances of pre-term birth are high due to which complications can arise in the newborn. Due to which there is a need for specialized care.
3) Emotional and Psychological Impact:
Due to twin pregnancy, the physical demand increases and the risk of potential complications also increases, so coping with this situation can lead to conditions like mother anxiety, fear of stress and emotional strain etc.
••>Effect on Fits:
1) Intra uterine environment:
Intra uterine growth retardation (IUGR):
When twins are pregnant, the nutritional needs of twins are higher than that of singleton fetuses and there is less space for twins to develop in the uterine cavity, due to which the fetus may grow less than its normal gestational age and intrauterine growth. A condition of retardation (IUGR) may arise.
Twin-to-twin transfusion syndrome (TTTS):
Twin-to-twin transfusion syndrome (TTTS) can occur when the placentas in a pregnancy with identical twins share a (monochorionic) placenta, where there is unequal blood flow between the placentas, affecting their growth and development.
2) Developmental Challenges:
Preterm Birth Complications:
Complications due to premature birth can arise in twins child like respiratory distress syndrome, jaundice and infection.
Monitoring and Care:
In the condition of twins pregnancy, regular ultrasound scan and fetal monitoring is necessary due to which if there is any complication of the fitus, it can be identified early with the help of which appropriate measures can be taken.
3) Position and Presentation:
In the condition of twins pregnancy, the condition of malpresentation (ex: breech presentation) in the fetus is more common due to which caesarean section is required.
Thus, twins pregnancy affects the health status of mother and fetus. Due to which complications may arise, it is important to take proper care of the health status of mother and fetus to prevent these complications. Due to which complications arising can be prevented and improvement in the health status of mother and fetus can be brought.
🔸 (B) Write down the functions of fallopian tube. 04 Write the functions of fallopian tubes.
Functions of Fallopian Tube: Fallopian tube is also called uterine tube or ovi duct.
It performs several important functions in the female reproductive system which are as follows:
1)Transportation of Oocytes:
The primary function of the fallopian tube is to transport oocytes (eggs) released from the ovary to the uterus. This transportation is done by cilia and muscular contractions inside the tube.
2) Fertilization:
The fallopian tube is the site where,
Fertilization usually occurs. After ovulation, if sperm is present in the fallopian tube, it can fertilize the egg released in the tube.
3) Nutrient Support:
Secretions by the epithelial cells in the fallopian tubes help provide a suitable environment by transporting essential nutrients to the early embryo.
4) Guidance for Embryo:
Once fertilization occurs, the fallopian tubes provide guidance for the embryos formed by fertilization to implant in the uterus.
5) Secretarial Function:
Epithelial cells lining the fallopian tubes release substances that provide nourishment to the ovum and sperm, causing the embryo to form in the fallopian tube and undergo early development.
6) Defense Mechanism:
When a fertilized embryo is implanted in the uterine cavity through the fallopian tube, the fallopian tube has a mechanism that prevents the embryo from becoming infected, so that the embryo can implant properly in the uterine cavity.
7) Hormonal sense:
Fallopian tubes can sense hormonal changes during the reproductive cycle, which can affect their maturation and secretory function.
Overall fallopian tube is crucial for fertilization as it provides necessary environment for fertilization and early development of embryo formed by fertilization before implantation in uterine cavity for further development.
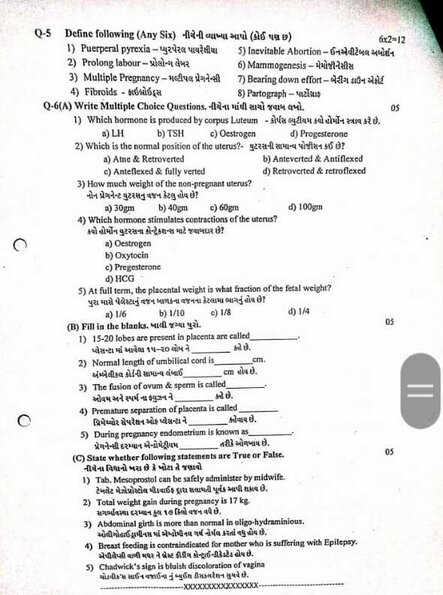
⏩ Q-3 Answer the following. (Any Two) 2×6=12
🔸1) Write down physiological changes during Puerperium. Write the physiological changes that occur during purpureum.
Physiological changes during purpureum period:
Purperium:
Puerperium means the period of 6 weeks (42 days) after child birth in which body tissues specially pelvic organs return to prepregnant stage both anatomically and physiologically is called perperium.
Duration:
The beginning of the puerperium is about 6 weeks after the placenta is expelled, and the uterus is almost nonpregnant in size.
The duration is roughly divided as follows:
- Immediate : Within 24 Hours,
Early: Up to 7 days,
- Remote : Up to 6 Vic
1) Physiological changes in reproductive system in periperium period:
(a) Involution of uterus:
Involution The process in which the bulky uterus progressively returns to its normal pre-pregnant state after delivery is called involution of uterus.
Anatomically Considerations
After the placenta is delivered, it heals into the endometrium of the placental site. After delivery, the uterus becomes firm and constricted with alternate hardening and softening.
The size of the uterus during pregnancy is approx.
Length: 20 cm, Width: 12 cm,
Thickness: About 7.5 cm.
And the weight of the uterus is about 900-1000 gm.
which,
Purperium period i.e. after 6 weeks of child birth the uterus returns to its pre-pregnant state i.e. the size of the uterus during the purperium period
Length: 7.5 cm, Width: 5 cm,
Thickness: About 2.5 cm.
And the weight of the uterus is about 60 gm.
Reduction of the size and position of the uterus:
After labor the fundus is 5 cm below the umbilicus and 12 cm above the symphysis pubis.
After 24 hours it is at the level of the umbilicus. The uterus descends into the pelvic cavity at a rate of 1.25 cm/hr and after 10 days the symphysis is not palpated abdominally above the pubis.
Consistency of the uterus:
Due to repeated strong myometrial contractions blood flow control towards the uterus becomes hard Palpating its consistency should feel firm and round If the fundus is soft it is called a boggy uterus Contractions are inadequate and blood loss is ongoing Suggests.
(b) Involution of cervix:
After delivery, the lower uterine segment and cervix remain loose, thin and stretched.
It may be oedematous, bruised and have small tears and lacerations. It takes a few weeks for the isthmus to return to normal shape and size.
The consistency of the first post partum day service remains normal until two fingers are admitted. Then at the end of the first week, the tip of the fingers remains as much as admitted. The evolution of the cervix is continuous for 3-4 months. But a parous cervix never gets the look of a non-parous cervix, the external os that first looked like a dimple looks like a slit.
C) Vaginal canal:
A distensible vagina takes about 4 to 8 weeks to involute. After delivery, the vaginal canal appears swollen and smooth, gradually becoming small and firm but never of pre-pregnancy size, the introitus remains permanently large, and the hymen is lacerated. Represented in the form of nodular tags.
(d) Perineum:
The muscles of the perineum floor are stretched, swollen and bruised with an episiotomy scar.
(e) Broad ligaments and round ligaments:
Broad ligaments and round ligaments take some time to recover from stretching. Initially the ligaments are stretched but by the end of the periperium period the ligaments are back to their non-pregnant length.
(f) Pelvic floor and pelvic fascia:
The pelvic floor and pelvic fascia take a long time to involute from the stretching effect.
(f) Lokia:
During the first 15 days of the puerperium period, the vaginal discharge called lochia comes from the uterine body, cervix, and vagina.
It contains blood vessels, decidual tissues, epithelial cells of vaginal mucus, bacteria, fragments of membranes and small clots.
Odair of Lokia
Odor (smell) of lokia is fishy.
Type of Lokia:
There are three types of lokia.
1) Lokia rubra,
2) Lokia cirrhosa,
3) Lokia Alba
1) Lochia rubra :
Lokia rubra is the first phase of Lokia. Discharge which is red and bloody lasts for 1 to 4 days after child birth.
In the lokia rubra
blood,
Fital membrane, decidua,
Vernix caseosa and lanugo are present.
2) Lochia cirrhosa:
Lochia cirrhosa is the second phase of lochia.
Which is seen as yellowish pale or pale brownish color.
Lochia cirrhosa lasts for 5 to 9 days.
It has low amount of red blood cells but high amount of leukocytes.
Wound exudate,
survive mucus,
And microorganisms are found in it.
3) Lokia Alba:
Lokia Alba is the third phase of Lokia. It is usually pale white in color.
Lochia alba is observed for 10-14 days.
in it,
Excess decidual cells,
leukocytes,
mucus,
Cholestrin crystals,
Fatty and Glandular Epithelial Cells,
And microorganisms are found in it.
Amount:
The average amount of lochia is around 250 ml during the first 5 to 6 days.
Normal Duration:
The normal duration of lochia is up to three weeks, if it persists after three weeks, local license may be available.
Clinical Importance of Local Discharge:
As the lochia provides information on the mother’s peripheral state, it is important to assess the lochia.
Odor (Smell): May be due to offensive infection.
Odor: Scanty or absent may be due to infection.
Amount:
Scanty or absent may be due to infection.
Color: Continuous red color Nokia may be due to subinvolution.
Duration: A local license may be in place if the lock is up to three weeks or longer.
(2) Breast and Lactose:
breast
Breasts are developed during pregnancy due to hormonal stimulus. Both feeding and non-feeding breasts secrete colostrum for a few days after delivery. Colostrum is the creamy yellow precursor of milk. In which the breast is soft and non-tender.
After three days, prolactin levels increase and breasts become firm and tender. When milk starts to secrete, the breast becomes distended, hard and warm due to increased blood flow, venous and lymphatic congestion, this is called physiological engorgement.
It lasts 24 to 48 hours and then resolves on its own. Milk production is stimulated by baby’s shaking. Breasts feel firm, full and tender until empty.
Lactation:
Lactation is the process of breast feeding which is based on interplay of hormones, instinctive reflexes, learned behavior of mother and newborn.
Latestation is particularly controlled by the hormones prolactin and oxytocin and is maintained by three factors:
1) Anatomical structure of mammary gland, development of alveoli, duct and nipple.
2) Initiation and maintenance of milk secretion.
3) Milk ejection or propulsion of milk from alveoli to nipple.
Milk Production: A healthy mother produces 500 to 800 ml of milk to feed her baby.
(3) Cardiovascular Changes:
Blood volume
The increased blood volume during pregnancy decreases and the circulatory system returns to its prepregnancy state.
cardiac output
Excess water in the body is removed due to diuresis and diaphoresis from the body and the cardiac output comes to its normal range.
Hemoglobin and Hematocrit Level:
Due to blood loss during pregnancy, hemoglobin and hematocrit levels are initially low, but within a few weeks, the blood stabilizes in its normal range.
4) Respiratory function:
After delivery abdominal pressure decreases as the diaphragm descends so lung expansion and ventilation improves but there are no noticeable changes in respiratory rate.
(5) Endocrine Changes:
Hormone Shift:
Pregnancy related hormones are reduced such as estrogen, progesterone and human chorionic gonadotrophin (HCG) hormone.
The level of prolactin hormone is elevated to maintain breast feeding.
(6) Renal changes
Diuresis
Urine output increases due to which fluid accumulated in the body during pregnancy is excreted from the body.
Bladder function
The bladder regains its tone and function, although some temporary issues such as urinary retention or urinary incontinence occur.
(7) Gastrointestinal Changes:
Bowel function
Bowel function takes some time to return to normal but the condition of constipation is seen due to reduction in its size.
Appetite in women becomes normal in some time but in some women bowel changes are seen for some time.
(8) Musculoskeletal Changes:
Abdominal muscles
The tone of the abdominal muscles regains within a short time while the pelvic floor muscles also return to normal within a short time but Kegel exercises are important in strengthening the pelvic floor muscles.
(9) Psychological Changes
Hormonal fluctuations, physical recovery, and the demands of newborn care impact emotional well-being. It also features common experience mood swings such as “baby blue”. And post partum depression is also seen in some women.
Thus, these types of physiological changes are seen in women during the post partum period.
2) Write the management of PPH (Post Partum Hemorrhage) Write the management of PPH (Post Partum Hemorrhage).
Management of Post Partum Hemorrhage (PPH):
Postpartum haemorrhage is a condition that occurs from the birth of the baby to the end of the periperal period (after birth of baby up to 6 weeks period) from the genital tract in excessive amount which adversely affects the general condition of the mother. In which pulse rate increases as evidence and blood pressure falls down. So this condition is called Post Partum Haemorrhage (PPH).
If 500 ml or more after vaginal delivery,
Excessive bleeding of 1000 ml or more after cesarean section is called postpartum hemorrhage.
Management of Postpartum Haemorrhage:
Postpartum hemorrhage is a major cause of maternal morbidity and mortality, so proper and effective management of postpartum hemorrhage remains important to prevent complications.
The management of postpartum hemorrhage involves a systemic approach that involves controlling bleeding, stabilizing the mother, and identifying the cause of postpartum hemorrhage.
1) Immediate Action:
Early recognition
Early identification of signs and symptoms of postpartum haemorrhage such as excessive bleeding (more than 500 ml if vaginal delivery and more than 1000 ml if cesarean section), tachycardia, hypotension, pallor and signs of shock Identify why.
Call for help
Notify senior obstetricians, anesthesiologists and other necessary health care personnel to assist in the management of postpartum hemorrhage.
assessment
Quantity of Blood Loss To properly assess the amount of blood loss.
Clinical assessment
Perform a focused clinical examination to assess for uterine tone, size, and any signs of trauma and whether a retained product is present.
Establish intravenous (IV) access
Large intravenous (IV) access for rapid fluid administration and administration of medications in women with postpartum hemorrhage.
Oxygen administration
Provide supplemental oxygen to maintain tissue oxygenation.
2) Pharmacological management
Uterotonic medication
Administer uterotonic agents to stimulate uterine contractions and control bleeding.
Oxytocin
Oxytocin is a first-line agent with a bolus dose of 10 to 40 units added to 1 liter of crystalloid solution and provided as an infusion over 10 to 30 minutes.
Followed by
Infusion of 40 units in 1 liter of IV fluid over 4-6 hours.
Misoprostol
See If oxytocin is not available, administer 800 mcg rectally and 600 orally.
3) Non pharmacological management:
Uterine massage
Gently massage the uterine fundus to enhance uterine contractions and control bleeding.
Balloon tamponade
In post-partum haemorrhage, if there is continuous bleeding even after giving utratonic drugs and uterine massage, then use balloon tampons (Bakery balloon and Follis catheter) to apply pressure to the uterine wall again, thereby achieving hemostasis and controlling the bleeding. can be done
4) Surgical intervention
Manual removal of placenta
If placental tissue appears to be present in the uterine cavity, provide anesthesia and manually remove the placenta.
Compression sutures
Apply uterine compression sutures to mechanically compress the uterus and control bleeding.
Uterine artery ligation
In some cases, uterine artery ligation is performed as a surgical option to reduce blood flow to the uterus.
Hysterectomy
Hysterectomy is performed as an emergency measure when the bleeding is not controlled by any other measures and the patient’s condition is deteriorating.
5) Supportive care and monitoring:
Fluid administration
Adequate intravenous fluid administration to the patient to improve tissue perfusion such as:
Normal saline
Or Ringer lactate solution.
Blood transfusion
Provide blood transfusion as per patient’s need when excessive amount of bleeding has occurred.
monitoring
Continuously monitor the patient’s vital signs, urine output, and level of consciousness.
Repeat hematological and biochemical tests to assess response to treatment.
Psychological support
Post Partum Haemorrhage (PPH) is a traumatic condition so proper psychological support should be provided to the patient and her family members.
6) Prevention
Antenatal care
Early identification of risk factors for postpartum hemorrhage during antenatal period can lead to early management and prevention of complications.
Active management of third stage of labor
Use of prophylactic uterotonic medication to prevent post-partum haemorrhagic conditions and reduce the risk of uterine atony.
Skill Birth Attendance
Train personnel to be available to recognize and manage obstetrical emergencies immediately.
7) Follow up and Documentation:
Post management care
Advising the patient for proper follow-up so that recovery can be monitored and if the patient has anemic condition, it can also be assessed.
Documentation
Proper documentation of the event occurred, the interventions performed for it, and the patient’s response to treatment etc.
Thus, it is important to properly manage postpartum hemorrhage to prevent complications caused by conditions such as postpartum hemorrhage in women after child birth.
🔸3) Write the difference between “Forceps delivery & Vacuum delivery”. Write the difference: Forceps Delivery and Nacule Delivery
Difference Between Forceps Delivery and Vacuum Delivery:
1) Forceps delivery:
In forceps delivery, the baby is delivered using forceps.
Obstetric forceps are a pair of instruments specially designed to extract the fetal head.
Forceps delivery does not require maternal aftertaste.
Equipment in forceps delivery is less complex.
The incidence of cephalohematoma in forceps delivery remains low.
Forceps delivery is safer for premature babies because the fetal head remains within a protective cage.
Ventos delivery is performed using forceps in contracted cases such as anterior face or breech presentation.
Used in non-sephalic presentation.
Full dilatation of the cervix is necessary to apply the forceps.
For the application of forceps, the athlete’s femoral head should be at +2, +3 station.
Adequate anesthesia remains essential in forceps delivery.
In this the blade of the forceps will be directed upwards on the parietal eminence, the shank in contact with the perineum and the handle on the superior surface.
Forceps delivery is associated with third and fourth degree perineal lacerations.
The blades of the forceps hold the spot.
Maternal tissues are injured.
In case of conditions like fetal distress, it provides a quicker delivery with less time consumption.
2) Vacuum delivery:
In vacuum delivery, the baby is born through a vacuum.
A vacuum is an instrumental device designed to assist delivery by creating a vacuum between the device and the fetal scalp.
A small amount of maternal aftertaste is required in vacuum delivery.
It can be done even if there is little expertise in it.
In it, the incidence of cephalohaematogen may be higher.
Contraindicated for premature babies because the fetal head is soft.
Contraindicated in non-vertex presentation (face, brow, breech).
It is not used in non-selflike presentations.
Vacuum delivery can be used even if the cervix is less dilated than full dilatation. But in modern obstetrics it is applied after full dilatation.
For the application of vacuum, the femoral head should be at the athlete’s zero station.
Vacuum delivery requires less anesthesia.
A vacuum cup is placed in the fetal head near the occiput.
Vacuum delivery is associated with solder dystocia and cephalohematoma.
A vacuum does not occupy space like forceps blades.
If the vacuum is applied correctly, it does not injure the maternal tissues.
The failure rate of vacuum is high
🔸4) Write the treatment Modalities of Infertility. Describe the treatment methods of infertility.
Treatment Modalities of Infertility:
Treatment modalities of infertility are different and generally depend on the cause of infertility.
1) Life Style Modifications:
Weight management
Achieving a healthy Body Mass Index (BMI) through an adequate diet and regular exercise can improve fertility.
Smoking and Alcohol Cessation:
Both smoking and alcohol consumption in excessive amounts have a negative impact on fertility. So it should be avoided.
Stress Reduction:
Yoga, meditation, and counseling techniques help reduce stress and its effects on fertility.
2) Medical Treatment:
Ovulation induction
Women who have an ovulatory disorder (polycystic ovary syndrome) are prescribed medications such as clomiphene citrate, laterozole, or gonadotrophins that stimulate ovulation.
Hormonal therapy
Correcting hormonal imbalances that affect fertility such as thyroid disorders and hyperprolactinemia.
Treatment of infection
If there is an infectious condition like pelvic inflammatory disease (PID) then providing the patient with adequate antibiotic medication to treat the infection that affects fertility.
3) Surgical Intervention:
Laparoscopic surgery
Used to treat conditions that affect fertility, such as endometriosis, pelvic adhesions, and fibroids.
Tubal surgery
Tubal surgery involves repairing a blocked or damaged fallopian tube that prevents sperm from reaching the ovum.
4) Assisted Reproductive Technologies (ART):
Intra Uterine Insemination (IUI):
Intra-uterine insemination is a process to improve fertilization in which sperm are inserted directly into the uterine cavity at the time of ovulation.
In Vitro Fertilization (IVF)
In the in vitro fertilization process, the ovum and sperm are fertilized outside the body i.e. in the laboratory.
In whose step,
Ovarian stimulation
Medications are used that stimulate the ovaries to produce multiple eggs.
Egg retrieval
A surgical procedure for collecting eggs from the ovaries.
Fertilization
Eggs and sperm are mixed in a laboratory dish and then the embryo is cultured.
Embryo transfer
Now more than one embryo is transferred into the uterine CVD.
Intra cytoplasmic injection
In this procedure, sperm are directly injected into the egg to improve fertilization.
5) Donor gametes:
Couples who have serious fertility issues and couples whose infertility is genetic can use donor eggs or donor sperm for fertility.
Donor Egg
A donor egg is fertilized with sperm from a partner or donor through IVF.
Donor sperm
Used when there is severe male infertility. And due to the genetic risk through mail, donor sperm is also not used.
6) Surrogacy:
In surrogacy another female (surrogate) carries and gives birth to a child for individuals or couples who are unable to conceive or carry a pregnancy to term:
Gestational surrogacy
In gestational surrogacy, both the woman’s egg and the male’s sperm (surrogate gametes) are collected and transmitted to the surrogate mother after in vitro fertilization in the laboratory.
7) Psychological support
Infertility is emotionally challenging. In which, counseling, support groups, and therapy are important for individuals and couples to cope with the condition of infertility.
Thus, the treatment for infertility depends on their different causes in each individual. Reproductive endocrinologists, urologists, surgeons and mental health professionals provide each infertility couple with adequate treatment according to their causes and needs.
⏩ Q-4 Write Short Notes (Any Three) 3×4=12
🔸1) Medical termination of pregnancy (MTP)–
Medical Termination of Pregnancy (MTP)
Medical termination of pregnancy is a medical procedure in which a woman can terminate a pregnancy in order to maintain her health or well-being by considering certain criteria.
Termination of pregnancy by medical or surgical method before the stage of viability of the fetus is called induction of abortion, legal or illegal. Abortion was legalized as medical termination of pregnancy in India in August 1971 and came into effect from April 1972 and revised by Happened in 1975.
indication
When a woman’s life is in danger and her physical and mental health is severely damaged.
Child may have physical and mental abnormalities.
In the condition that the child has any congenital anomaly.
Pregnancy due to rape.
Due to social or economic reasons, mother’s health is damaged and contraceptive measures have failed.
According to Indian law, abortion is allowed up to 20 weeks, the opinion of one registered medical practitioner is required for pregnancies up to 12 weeks and two registered medical practitioners for 12 to 20 weeks.
Returned (written) consent of the patient and consent of the guardian is required in cases where the patient is under 18 years or mentally handicapped.
Contraindications
Have uncontrolled blood pressure greater than 160/100,
Having Cardio Vascular Diseases,
Women are above 35 years of age,
Have severe renal failure, liver disease or respiratory disease,
Using systemic corticosteroids,
coagulopathy or women receiving anticoagulant therapy,
Mother is anemic,
Have an uncontrolled seizure disorder.
Who can perform medical termination of pregnancy?:
The Chief Medical Officer or Civil Surgeon authorizes the following doctors for medical termination of pregnancy:
Holder of Post Graduate Degree or Diploma in Obstetrics and Gynaecology.
Six months training as a resident in obstetrics and gynaecology.
One year experience in Obstetrics and Gynecology Department.
Registered Medical Practitioner assisted in 25 cases of Medical Termination of Pregnancy (MTP). Place for MTP (Medical Termination of Pregnancy): A hospital established or maintained by the Government or a place approved by the Chief Medical Officer or Civil Surgeon. Records: To record medical termination of pregnancy in the form. Maintain confidentiality and report to Director of Health Services. Penalty:
A person who does not comply with this act can be punished with imprisonment of 2 to 7 years. Methods of Medical Termination of Pregnancy (MTP): First Trimester (up to 12 weeks): Medical
This involves terminating the pregnancy using medication such as,
Mifepristone,
Mifepristone and Misoprostol,
Mithotrexate and Misoprostol,
Tamoxifen and misoprostol. surgical
In this case, the pregnancy is terminated using a surgical procedure.
like,
Menstrual Regulation, Vacuum Aspiration,
Saxan Evacuation and Curettage,
Dilatation and evacuation. Second Trimester (13-20 wks):
prostaglandins,
Dilation and evacuation,
Intra uterine instillation of hyperosmotic solutions,
oxytocin infusion,
Hysterotomy.
Complications:
Complications usually depend on the method by which Medical Termination of Pregnancy (MTP) is performed.
Immediate complications
Cervical lacerations,
uterine perforation,
hemorrhage,
grief,
thrombosis,
embolism,
The post-abortal triad may include pain, bleeding, and low-grade fever, depending on the method used for medical termination of pregnancy.
remote
Gynecological complications,
Obstetric complications,
Failed Abortion,
Ectopic pregnancy etc.
Nursing Role with the Patient Undergoing MTP:
The nurse should provide comfort and support to the mother and her family members and provide proper reassurance by clearing all their queries.
If the mother decides to have an abortion, her husband and the patient’s own consent should be obtained along with their written permission.
Continuous monitoring and providing support to the patient before medical termination of pregnancy, during the procedure and even after the procedure is completed.
Providing proper education to the mother about the complications that may arise after abortion such as,
Continuous vaginal bleeding with clots up to three weeks after abortion,
Providing education to women about fever, continuous pain, and burning micturition etc.
First menses start 2 to 8 weeks after a woman is advised to have an abortion.
Advise women that if lactase is started, it is in mild amounts and lasts for 48 hours if the breast is not stimulated.
Provide them with education or follow-up visits two to eight weeks after medical termination of pregnancy (MTP) to ensure that the reproductive organs have returned to their prepregnancy state.
Thus, termination of pregnancy is done in medical termination of pregnancy.
🔸2) Obstructed labour-
Obstructed Labour:
Definition
Obstructed labor is a condition in which despite good uterine contractions, the presenting part of the fitus, which is progressively descending, is arrested due to mechanical obstruction is called “obstructed labour”.
Obstructed labor can also lead to fetal death due to not getting adequate amount of oxygen to the fetus.
etiology
1) Fault in passage (birth canal),
2) Fault in passenger (fits)
1) Fault in passage (birth canal):
(a) Bonnie,
(b) Soft tissue obstruction
(a) Bonnie:
contracted pelvis,
Cephalopelvic Disproportion (CPD),
Abnormal Pelvis (Ex : Android, Anthropoid)
(b) Soft tissue obstruction:
Due to cervical dystocia caused by prolapse or prior operative scarring,
Cervical or broad ligament fibroid,
Impacted ovarian tumor,
Due to having tumors in the rectum, bladder and pelvic bone.
Being a bicornuate uterus.
Due to abnormalities in the uterus.
Having vaginal stenolosis.
Due to the vaginal septum.
Having a rigid perineum.
2) Fault in passenger (fits):
transverse lie,
bro presentation,
Due to Congenital Malformation of Fetus (Ex : Hydrocephalus),
Being a Big Baby,
Occipito-posterior position,
Compound Presentation,
Locked Twins.
Clinical Features:
Effect on Mother
Immediate
Immediate Exhaustion,
dehydration,
metabolic acidosis,
genital sepsis,
Injury to genitourinary track,
Post partum haemorrhage,
mourning
remote
Genito Urinary Fistula/ Recto Vaginal Fistula,
vaginal atresia,
Secondary amenorrhea.
Effect on the fitters
asphyxia,
acidosis,
intracranial hemorrhage,
infection.
Nursing Management
Identification of obstructed labor during the antenatal period of the mother itself so that early measures can be taken.
Proper mother monitoring during intranatal period and proper maintenance of partograph for early detection of obstructed labour.
To prevent dehydration, ketoacidosis and sepsis in the mother and to maintain the hydration status of the mother.
Administering intravenous fluids to the mother which mainly
Provide Ringer lactate fluid to correct dehydration and acidosis.
If the mother has a condition of acidosis, correct it with 100 ml of 8.4% sodium bicarbonate.
Carrying out biochemical monitoring such as
Serum bicarbonate level.
Providing proper antibiotic medication to the mother like,
Administer 500 mg ampicillin and then repeat at 6 hour intervals.
Centrifuge the blood sample to the laboratory for blood grouping and cross-matching. And if operative interference is to be performed, keep a blood bottle ready.
Take a vaginal swab and send it to the laboratory for culture and sensitivity tests.
Early relief of obstruction through safe delivery in obstetric management. Do not give oxytocin or trial for safe delivery of the patient.
If the baby’s head is down and the baby is alive, perform a forceps delivery and then check for uterine rupture and tear.
If the baby is dead, deliver by destructive operation.
Not performing internal version in obstructed labor.
If the case is detected early and the condition of the fetus is good, perform a caesarean section.
Symphysiotomy
As an alternative to caesarean section, an opening is made in the symphysis pubis to widen the pelvic cavity during outlet contractions.
3) Importance of Antenatal Care-
The importance of antenatal care is to improve the overall health of the fetus and the mother and to improve the well-being of the mother and the fetus and to prevent complications.
1) Monitoring maternal health
Regular health checkups can monitor the mother’s overall health, such as blood pressure, weight gain, and overall well-being, etc., so that early identification of any complications can be done. And by treating it early, it can be prevented from happening further.
2) Monitoring fetal health
In antenatal care, assessment of the fetus including ultrasound scan, fetal heartbeat monitoring, and other tests can be done properly due to which the growth and development of the fetus can take place properly. If the child has any abnormality, it can be detected early and properly managed.
3) Health Education
Antenatal care provides an opportunity for appropriate education to expectant mothers, including pregnancy, child birth, breastfeeding, nutrition and parenting. This education can be helpful to the antenatal mother in making proper decisions.
4) Early detection of pregnancy related complications for proper management.
By visiting antenatal care, early detection of pregnancy related complications can be done and its timely management can be done. like,
gestational diabetes,
Preeclampsia, infection and other pregnancy related risks that can affect the pregnancy.
5) Preparation for Childbirth
Birth planning, preparation for labor, and delivery options are discussed in antenatal care sessions. By having this discussion, the mother and her family members can mentally and practically prepare for child birth.
6) Psychological support
Emotional and psychological changes are seen due to pregnancy. Antenatal care provides a supportive environment in which the expectant mother can discuss her anxiety, fear and doubts and clear them and reduce her anxiety and fear and feel emotionally well-being.
7) Prevention and Management of Maternal and Infant Complications
Antenatal care interventions include immunization, iron and folic acid supplementation, and preventive treatment to prevent pregnancy and childbirth related risks and complications.
8) Promotion of healthy behavior
Antenatal care provides education to promote behaviors such as smoking cessation, alcohol and drug avoidance, maintaining a balanced diet, and being physically active, which are important for healthy pregnancy outcomes.
9) Postpartum planning
Post-partum care is also discussed in antenatal care in which, post-partum care,
Breast feeding support and family planning options are discussed.
The objectives of overall antenatal care are to have a healthy pregnancy, properly manage any risks and complications, prepare the mother for child birth, and properly maintain the health of the mother and fetus during the throwout pregnancy.
4) Ectopic Pregnancy-
Definition
When a fertilized ovum implants and develops outside the normal endometrial cavity, it is called an ectopic pregnancy.
Anatomical site of implantation of ectopic pregnancy:
Tubal pregnancy is more common, normally occurring in the right fallopian tube more often than in the left fallopian tube.
The ampulla of the fallopian tube is the most common site of implantation of an ectopic pregnancy.
If an ectopic pregnancy occurs at the isthmus of the fallopian tube, it is considered a dangerous site that can also lead to tubal rupture.
etiology
Due to certain factors, the migration of fertilized ovum into the uterine cavity is delayed.
Due to factors that provide a favorable environment for fertilized ovum to implant in the tubal mucosa.
Due to hormonal factors,
Due to birth defect,
Due to a medical condition.
Risk factors
Due to prior ectopic pregnancy,
Due to previous surgery in the uterine tube,
Due to tubal reconstructive surgery,
Intra uterine contraceptive device no use due to failure,
Due to some type of infection like,
Pelvic Inflammatory Diseases,
chlamydia infection,
Gonorrhea etc.
Having a history of infertility,
Due to Assisted Reproductive Techniques (ART),
Due to infertility treatment like,
In Vitro Fertilization (IVF),
As the mother’s age is more than 35 years,
Due to inducing prior abortion,
Having a history of endometriosis.
Signs and Symptoms:
Symptoms and signs of ectopic pregnancy are classified into two types:
1) Acute type
2) Chronic type
1) Acute type
An acute type of ectopic pregnancy presents with a triad of symptoms such as:
amenorrhea,
Sharp colicky abdominal pain,
Vaginal bleeding
Nausea and vomiting,
Palency usually depends on the amount of hemorrhage.
To see signs and symptoms of mourning,
like,
Rapid and Fable Pulse,
Falling blood pressure,
Extremities are cold and clammy.
On abdominal examination, the abdomen feels tense, tense, and tender.
Abdominal tenderness.
Bowel is distended.
Massive intraperitoneal hemorrhage occurs with tubal rupture and tubal abortion.
Cullen sign positivity: dark bluish peri-umbilical ecchymosis due to hemoperitoneum.
Vaginal area pale during pelvic examination.
The uterus appears to float in the water.
2) Chronic type
Tubal mole is common in the chronic type
It is not known at first.
Its signs include anemia, bladder irritability, tachycardia and increased temperature.
amenorrhea,
abdominal pain,
Vaginal bleeding that appears dark in color shortly after abdominal pain.
Bladder irritation such as dysuria, frequency of urination, retention of urination.
Increase in body temperature.
Examination reveals that the patient is ill,
Seeing the pallor,
An increase in pulse rate even when resting.
Abdominal tenderness on the affected side.
Filling of mass like structure on lower abdominal site which is irregular.
Extreme tenderness of the cervix.
Diagnostic Evaluation:
History Collection,
Physical Examination,
blood examination,
Caldosynthesis (Tapping of Pouch of Douglas),
sonography,
Assessment of hcg level,
laparoscopy,
laparotomy,
Dilatation and Curettage,
Trans vaginal ultrasonography (USG)
Management of Ectopic Pregnancy
Management of ectopic pregnancy is divided into two types,
like,
1) Acute ectopic pregnancy management,
2) Management of chronic ectopic pregnancy
Principles of Management
To prevent complications to the mother.
In case of ectopic pregnancy, laparotomy should be performed immediately because the fertilized ovum cannot survive outside the uterine cavity so the tissues are removed to prevent serious complications.
1) Management of acute ectopic pregnancy:
Provide anti-shock treatment to patient and prepare for urgent laparotomy.
Advise the patient to lie down flat on the bed.
Provide patient with inj.morphine 15 mg (IM).
If needed, start a 5% dexrose drip.
Arrangement of blood for blood transfusion.
Even if blood is not available or arranged and the patient is in a state of shock, performing a laparotomy is imperative.
The fallopian tube containing the gestational sac is removed through a laparotomy and a partially surgical procedure.
Performing a salpingectomy. In whose step,
Referring the patient to the hospital,
Advise the patient to lie down on a flat bed.
If the patient is collapsed, raise the bed towards the foot end.
Assessing the patient’s hemoglobin level.
If the patient needs blood transfusion, keep the blood ready.
Administer adequate intravenous fluids to the patient until blood is available.
Ex:=Ringer lactate,
Dexran.
Perform a quick laparotomy under general anesthesia on the patient for salpingectomy.
Then placing the incision on the line of intra umbacus.
After that recognize the uterus and shake out the blood continuously.
Both sites of the uterus should then be assessed to identify gestational shock in the fallopian tubes.
After that the affected tube and ogre are observed.
Clamps are then applied.
Then the gestational sac wadi affected fallopian tubes with and without ovaries are removed.
The clamps are replaced by chromic catgut ligatures which should not be tightened.
Proper hemostasis is then ensured.
A tubectomy or salpingectomy for hydrosalpinal fluid is performed for the other fallopian tube when the patient wants sterilization.
When a blood clot is free present in the peritoneal cavity, it should be aspirated as much as possible.
Then wash the pelvic cavity properly with normal saline and quickly close the abdomen.
In case of interstitial tubal pregnancy, only the gestational scar should be removed but sometimes for the purpose of better hemostasis, quick subtotal hysterectomy is required.
2)Management of chronic ectopic pregnancy:
All cases with chronic ectopic pregnancy should be admitted to emergency.
Keeping the patient properly under observation.
To carry out all investigations of the patient properly.
Control bleeding quickly and effectively.
Keeping blood transfusion available.
Provide intravenous infusion to the patient as prescribed.
Advise the patient to perform laparotomy as early as possible.
Preparing the patient for laparoscopy or laparotomy.
Then advise to perform salpingectomy.
With medical management in ectopic pregnancy, the ectopic pregnancy is removed by making an incision on the fallopian tube or removing a section of the tube.
If the patient has suppurative pelvic hematocele, provide appropriate antibiotics and drain the pus.
Removal of tubal mole by laparotomy and partial incision on the fallopian tube.
To provide proper management to the patient after surgery.
Providing systemic methotrexate 50 mg IM to patients under medical treatment.
Rh antigen is not sensitized in positive Rh women. Anti-D gamma globulin-50 micrograms should be provided to the patient immediately after operation to prevent isoimmunization.
Providing care to resuscitate the patient in acute rupture of the fallopian tube.
Properly maintain vital sign intake output chart of patient.
Providing antibiotic medication to the patient.
Anchoring the patient to early movement.
Advising the patient for proper follow-up.
⏩ Q.5 Define following (Any Six) Give following definition (Any Six) 6×2=12
🔸1) Puerperal pyrexia-
Peripheral pyrexia A condition in which the body temperature increases to more than 100.4°F (38 °C) within 14 days after delivery is called “peripheral pyrexia”.
Or
When oral temperature at two different times in 10 days after first 24 hours of delivery
A temperature of 100.4°F (38°C) or higher is called “purereal pyrexia”.
🔸2) Prolong labour-
When the combined duration of the first and second stages of labor is more than 18 hours, it is called prolonged labor.
Cervical dilatation rate <1 cm/hr and descent of the presenting part <1 cm/hr in at least four hours of observation is called prolonged labour.
🔸3) Multiple Pregnancy
When more than one fetus develops in the uterus simultaneously and at the same time, it is called “multiple pregnancy”.
When two fetuses develop together in the uterus, they are called twins.
When three fetuses develop simultaneously in the uterus, they are called triplets.
When four fits develop simultaneously, they are called quadruplets.
Varieties and types of twin pregnancy
1) Dizygotic twins:
This commonest ie fertilization of two ova is the result of fertilization by two spermatozoa.
Two placentas are seen in this.
In this case, communication vessels are absent.
In this case, there may be two amnion and two chorion membranes.
Genetic features may be different in this.
They do not accept skin grafts.
2) Monozygotic twins
Monozygotic twins develop due to fertilization of this single ovum by a single sperm.
Communication vessels are present in this.
It contains two amnion membranes.
Monozygotic twins usually have the same sex.
Genetic features are also found to be the same.
Physical features like ice, hair color, ear sap, palmar crisis etc are seen in it.
He also accepts skin grafts.
4) Fibroids –
Fibroids are also known as “uterine fibroids” or “leiomyomas”. It is a non-cancerous (benign) growth that develops in the uterine tissues and muscles.
They differ in size, from small nodules to large masses that can distort the shape of the uterus. Fibroids can develop as single growths or multiple growths, and are fairly common, affecting 70-80% of women by age 50.
5) Inevitable Abortion-
Inevitable abortion is a type of abortion in which the expulsion of the conceptus progresses with cervical dilatation. In this abortion, the pregnancy cannot be saved because most of the portion of the placenta is detached (from the uterine wall).
This is a clinical type of abortion in which the changes in the abortion have progressed to the point where continuation of the pregnancy becomes impossible. It is called “inevitable abortion”.
6) Mammogenesis –
Maemogenesis is the first phase of the physiology of lactation. which prepares the breast for lactation. In this stage, the ductal and lobulo-alveolar system of the breast grows, preparing the breast for the secretion of milk.
7) Bearing down effort –
Bearing down efforts are extra voluntary expulsive efforts seen in the second stage of labor in the mother. Stretching of the vagina by the presenting part of the fetus initiates a nerve reflex. Expulsive efforts usually start spontaneously with full dilatation of the cervix. Women are asked to increase downward pressure similar to straining while passing stool with uterine contractions and are discouraged after uterine contractions.
Symptoms seen during bearing down attacks:
Sudden sweating on mother’s upper lip.
vomiting,
And the show is visible.
8) Partograph-
Partograph A Cervical dilatation,
A graphic recording and tool for fetal head descent and labor progress and the condition of the mother and fetus. Partograph provides immediate and relevant information about the condition of the mother and fetus.
It recognizes the need to take action for appropriate time and timely referral. Morbidity and mortality rate of mother and fetus can also be improved through partograph.
Objectives:
1) To record observations during labor properly.
2) To understand the latent and active phase of labour.
3) Interpreting the partograph to identify any deviation from normal and take appropriate action.
4) To know the progress of labor so that action can be taken and referred at the right time.
5) Records can be seen at a glance in a single seat and easily handed over.
6) To avoid having to record the event of labor repeatedly.
7) To prolong labor and reduce the rate of education.
Q-6(A) Write Multiple Choice Questions.
1) Which hormone is produced by corpus luteum?
a) LH
b) TSH
c) Estrogen
d) Progesterone
2) Which is the normal position of the uterus?
a) Atne & Retroverted
b) Anteverted & Antiflexed
c) Anteflexed & fully inverted
d) Retroverted & retroflexed
3) How much weight of the non-pregnant uterus? What is the weight of a non-pregnant uterus?
a) 30gm
b) 40gm
c) 60gm
d) 100gm
4) Which hormone stimulates contractions of the uterus? Which hormone is responsible for uterine contractions?
a) Estrogen
b) Oxytocin
c) Progesterone
d) HCG
5) At full term, the placental weight is what fraction of the fetal weight? What fraction of the child’s weight is the weight of Pura Mase Palesta?
a )1/6
b) 1/10
c) 1/8
(d) 1/4
Q-6(A) Write Multiple Choice Questions.
Q: (1) Ans
(d) Progesterone
Q: (2) Ans
b) Anteverted & Antiflexed.
Q: (3) Ans
c) 60 gm
Q: (4) Ans
b) Oxytocin
Q: (5) Ans
a) 1/6
⏩ (B) Fill in the blanks. 05
1) 15-20 lobes are present in placenta are called
Cotyledons,
2) Normal length of umbilical cord is———-cm. The normal length of the umbilical cord is cm.
50-60 cm
3) The fusion of ovum & sperm is called ——
Fertilization
4) Premature separation of placenta is called ——– Premature separation of placenta is called ————.
Abruption placenta
5) During pregnancy endometrium is known as —-
Decidua
⏩ (C) State whether the following statements are True or False. 05 State whether the following statements are true or false
1) Tab. Mesoprostol can be safely administered by midwife. Tablet mesoprostol can be safely given by a midwife.
True
2) Total weight gain during pregnancy is 17 kg Total weight gain during pregnancy is 17 kg.
False
(Reason := An average pregnant woman usually gains about 11 kg of weight during pregnancy which
During 1st trimester :=1 kg,
During 2nd trimester :=5kg,
During 3rd trimester :=5 kg, thus, a total weight gain of 11 kg. No weight gain of 17 kg).
3) Abdominal girth is more than normal in oligo-hydraminous. Abdominal girth in Oligohydraminus is greater than normal
False
(Reason: Oligohydramnios is a condition in which the amount of amniotic fluid is reduced during pregnancy, due to which the abdominal girth of the pregnant woman is smaller than her gestational age, i.e. the abdominal girth does not enlarge.)
4) Breast feeding is contraindicated for mother who is suffering with Epilepsy. Best Freeding is contraindicated in mothers with epilepsy.
False
(Reason: If the mother uses antiepileptic medication, it will not affect the child, otherwise there is no problem)
5) Chadwick’s sign is bluish discoloration of vagina Chadwick’s sign indicates bluish discoloration of vagina.
True
💪 💥☺ALL THE BEST ☺💥💪
Note :-MCQ ANSWER in unique pattern of APP in both languages is given below paper solution / click here. Clicking on “A” will change the language.
IF ANY QUERY OR QUESTION, REVIEW-KINDLY WATSAPP US NO. – 84859 76407
