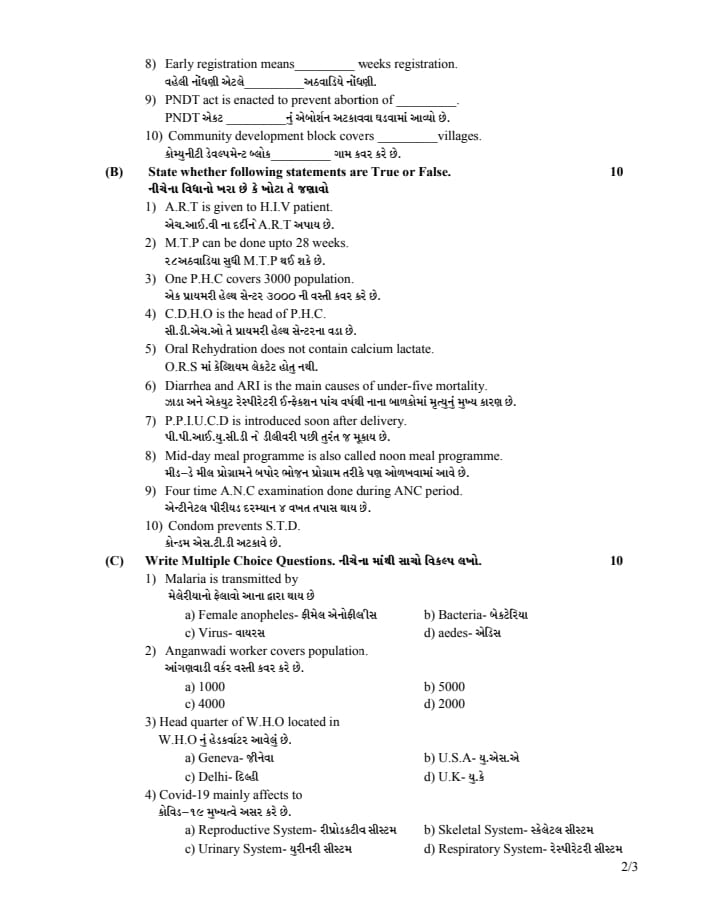
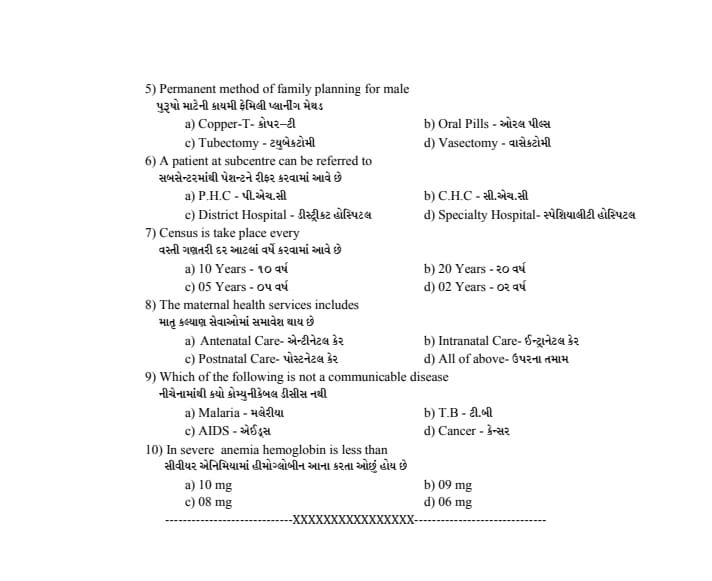
ENGLISH MIDWIFERY(Third Year) COMMUNITY HEALTH 14/09/2021 (paper no.5) (modified pending.mcq upload pending)
MIDWIFERY(Third Year) COMMUNITY HEALTH 14/09/2021
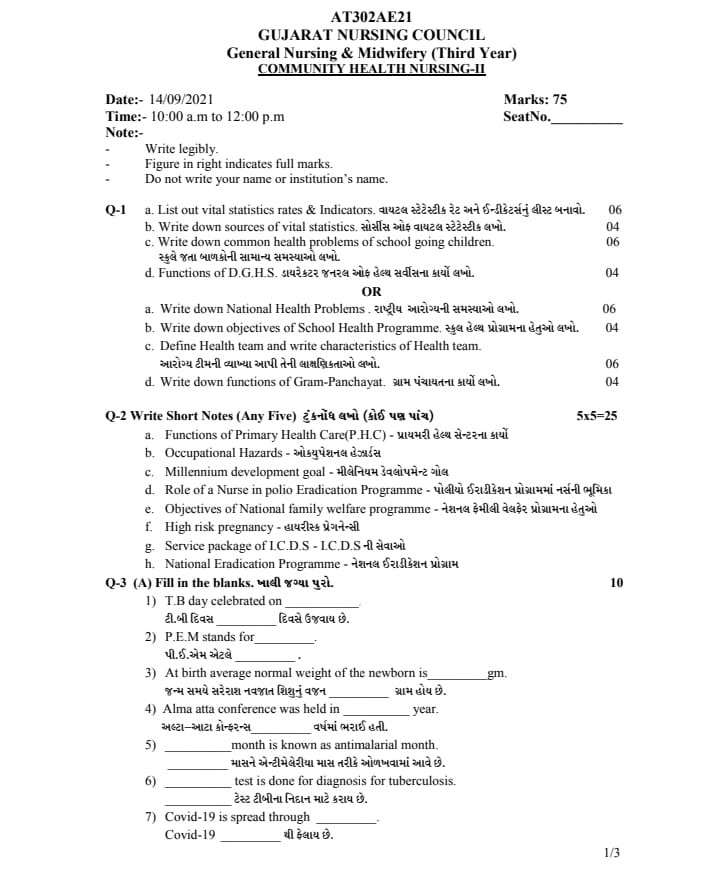
⏩Q-1 🔸a. List out vital statistics rates & indicators. 06 Make a list of vital statistical rates and indicators.
Vital Statistics Rate and Indicators:
Vital statistics rates and indicators serve as essential metrics for assessing the health, population dynamics, and overall well-being of a population.
••>Vital Statistics Rates
1) (CBR) Crude Birth Rate
Definition:
It can be defined as “the estimated mid-year number of live births per 1,000 population in a given year”.
Formula:
(CBR) Crude Birth Rate :=
Number of live births during the year
—————— × 1000
Estimated mid-year population
2) (CDR) Crude Death Rate
Definition:
It can be defined as “the estimated mid-year number of deaths per 1,000 population in a given year”.
Formula:
(CDR) Crude Death Rate :=
Number of Deaths during the year
—————— × 1000
Estimated mid-year population
3)NMR (Neonatal Mortality Rate)
Definition
Neonatal Mortality Rate (NMR) is the number of deaths of neonates occurring at an age of 28 days in a given area, in a given year, per 1000 live births in the population.
formula
NMR (Neonatal Mortality Rate:=
Number of deaths of children under 28 days of age in an area during the year.
—————- × 1000
The number of live births occurring during a leap year in the same area
4) IMR (Infant Mortality Rate)
Definition
The number of children who die under the age of 1 year out of the total number of live births in a population of 1000 in a given leap year is called Infant Mortality Rate (IMR).
formula
IMR(Infant Mortality Rate) =
Number of deaths of children under one year of age
——————- x 1000
Total number of live births in the year
5)(U5MR) Under Five Mortality Rate :
Definition
The number of deaths of children under the age of five per 1,000 live births (U5MR) is called the under-five mortality rate.
(U5MR) Under Five Mortality Rate:=
Number of deaths of children under 5 years
————— × 1000
Number of live births
6) MMR (MMR/Maternal Mortality Rate)
MMR
Definition
Maternal Mortality Rate (MMR) Maternal Mortality Rate (MMR) is the number of maternal deaths per 100,000 live births during a specific period, usually a year.
formula
Maternal mortality rate (M.M.R) =
Total number of maternal deaths due to complications within 42 days of childbirth or delivery during a given year
—————- × 100,000
Total Number of Live Births in Same Year.
7) Life Expectancy at Birth
Definition
The average number of lives of a newborn if the current mortality rate continues.
8) TFR (Total Fertility Rate)
Definition
The average number of children a woman can give birth to in her total reproductive year at the rate at which children are born in each age group is called Total Fertility Rate (TFR).
formula
Total fertility rate (TFR):=
45 – 49
5× Σ (ASFR)
15 – 19
1000
(ASFR = Age Specific Fertility Rate)
9)(GRR) Gross Reproductive Rate:
Definition
If a woman experiences current fertility patterns through her reproductive period (15-44 or 49 years), assuming no mortality, she will give birth to the average number of girls.
formula
(GRR) Gross Reproductive Rate:=
45 – 49
5× Σ (ASFR)
15 – 19
1000
(ASFR = Age specific fertility rate for female live birth)
10)NRR (Net Reproductive Rate)
Definition
How many daughters a newborn girl will give birth to during her life time is called Net Reproductive Rate (NRR).
Net Reproductive Rate (NRR) is a demographic indicator. The target is to bring it to one.
11)( GFR ) General Fertility Rate
Definition
It is the number of live births during a year per 1000 women in the reproductive age group of 15-45 years (GFR) is called General Fertility Rate.
formula
( GFR ) General Fertility Rate:=
Number of live births
——————- × 1000
Total number of females of age group from 15 to 45 years
12) (ASFR) Age Specific Fertility Rate
Definition
The number of live births per 1,000 women in a particular age group (ASFR) is called the Age Specific Fertility Rate.
formula
(ASFR) Age Specific Fertility Rate:=
Number of live births in a particular age group
—————- × 1000
Population of Midyear Female Population of Same Age Group
13) Child Woman Ratio:
Definition
Number of children aged 0-4 years per 1,000 women of childbearing age (15-49 years).
formula
Child Woman Ratio:
Number of children aged 0-4 years
—————- × 1000
Number of women aged {15-49}
14) Sex Ratio at Birth
Definition
Number of male births per 1,000 female births.
formula
Sex ratio at Birth:=
Number of mail births
——————– × 1000
Number of female births
15) Dependency Ratio
Definition
The ratio of combined age group 0-14 years + 65 years and above and age group 15-65 years is known as Total Dependency Ratio.
Total Dependency Ratio:=
Children aged 0-14 years + Population aged above 65 years
—————— × 100
Population 15 – 64 years
16) Aging ratio
Definition
Ratio of elderly (65+) to children (0-14).
formula
Aging ratio:=
Population aged 65+
————— × 100
Population aged 0-14
2) ••> Vital Statistics Indicators
1) Population growth rate
Definition
The rate at which a population increases or decreases over time.
formula
Population Growth Rate:=
Births – Deaths + Net Migration
—————– × 100
Total population
2) Healthy life expectancy
Definition
The average number of years a person can expect to live in good health.
3)( PMR ) Proportional Mortality Ratio
Definition
Ratio of deaths from specific cause to total deaths.
formula
( PMR ) Proportional Mortality Ratio:=
Death from a specific cause
————- × 100
total death
4)( SMR ) Standardized Mortality Ratio
Definition
The ratio of expected deaths to observed deaths in a specific population.
formula
( SMR ) Standardized Mortality Ratio:=
Observed death
————— × 100
Expected Death
5) Age Standardized Mortality Ratio
Definition
Age-adjusted mortality rates for comparison between populations.
formula
Calculations are made using the age specific molality rate and the standard age.
6) Crude Birth Rate (CBR) and Crude Death Rate Ratio (CDR)
Definition
Comparison of crude birth rate with crude death rate.
formula
Crude Birth Rate ( CBR ) and Crude Death Rate Ratio ( CDR ):=
Crude Birth Rate (CBR)
Crude Death Rate Ratio (CDR)
7) Net Reproductive Rate
Definition
Average number of daughters of a woman taking into account the mortality rate.
8) Per Capita Gross Domestic Product (G.D.P.)
Definition
A measure of economic output per person.
formula
Per Capita Gross Domestic Product* (G.D.P):=
Gross Domestic Product
Total population
9) Population density
Definition
Number of people per unit area on
formula
Population Density:=
Total Population
Land Area
10) Proportion of population aged 65 and over
Definition
Percentage of population aged 65 years or older.
formula
Proportion of population aged 65 and over:=
Population aged 65+
—————– × 100
Total population
Thus, the vital statistics and indicators are as follows.
b. Write down sources of vital statistics 04
Sources of Vital Statistics:
Civil Registration System (CRS):
Description: A civil registration system is a continuous, permanent and compulsory recording of the occurrence and characteristics of vital events (births, deaths, marriages etc.).
Authority: Administered by the Registrar General of India under the Minister of Health.
Significance:
Provides primary data on birth and death rates, which are crucial for planning and policy making.
2) Sample Registration System (SRS):
Conduct large-scale demographic surveys for reliable annual estimates of birth rates, death rates and other fertility and mortality indicators.
Authority:
Conducted by the Office of the Registrar General and Census Commissioner of India.
Significance:
CRS (Sample Registration Systems) supplement the data and provide more accurate and timely estimates.
Census: Description:
Conducted every ten years, the Census of India collects comprehensive data on the population. As such, it collects information including age, caste and marital status. Authority:
Conducted by the office of Registrar General of India and Census Commissioner. Significance:
Provides detailed demographic information that supports various statistical analyzes and socio-economic planning.
National Family Health Survey (NFHS): Description:
A large-scale, multi-round survey was conducted in a representative sample of households across India. Authority:
Conducted by Ministry of Health and Family Welfare in coordination with International Institute for Population Sciences (IIPS). Significance:
Provides data on population, health and nutrition, as well as fertility rates, maternal and child health.
Health Management Information System (HMIS): Description:
An online portal that collects data from health facilities across India. Authority:
Managed by the Minister of Health and Family Welfare.
Significance:
Health indicators, services delivery,
and provides data on health program performance.
6) Annual Health Survey (AHS)
Provides district-level estimates on key indicators, such as fertility and mortality rates.
Authority:
Conducted by the Office of the Registrar General and Census Commissioner of India.
Significance:
Helps to evaluate the effects of health programs and policies at a more localized level.
7) Demographic and Health Survey (DHS):
Conducted periodically to collect data on population, health and nutrition.
Authority:
Coordinated by various institutions and often in partnership with international agencies.
Significance:
Provides internationally comparable data for monitoring and evolution.
8) Medical Certification of Cause of Death (MCCD)
A system for recording the cause of death by medical practitioners using a standardized format.
Authority:
India, managed by the Office of the Registrar General.
Significance:
Provides accurate data on mortality patterns and causes of death, which is essential for public health planning.
9) Health Survey and Research
Various surveys and research studies are conducted by government agencies, academic institutions and international organizations.
Examples:
National Sample Survey (NSS), India Human Development Survey etc.
Significance:
The survey provides additional data on various health and demographic parameters, which helps in comprehensive analysis and policy formulation.
Vital statistics in India are derived from multiple sources, playing a crucial role in providing accurate and comprehensive data on health and demographic characteristics of each population.
These statistics are essential for effective planning, implementation and evaluation of health and social programmes.
c. Write down common health problems of school going children. 06
Different health problems seen in school going children are generally different based on their age, religion and socioeconomic factors.
Here, health problems seen in school going child :
1) Respiratory Infection:
Tema, common cold, flu, tonsillitis, and bronchitis.
2) Gastrointestinal System:
Such as, diarrhea, constipation, and abdominal pain.
3)Dental problem:
Such as, cavities, tooth decay, and gingivitis.
4) Allergies:
Allergic rhinitis (hay fever), food allergies, and skin allergies.
5) Injuries:
Injuries due to falls,
Sports activity or playground accident.
6) Vision Problems:
Refractive errors like (nearsightedness) or est…
d. Functions of D.G.H.S. 04 .
Functions of Director General of Health Services (DGHS):
The Directorate General of Health Services (DGHS) acts as the principal advisor to the Central Government on medical and public health matters. The Health Service appoints a Director who is assisted by Additional Directorate General of Health Services, Deputy Officers and other administrative staff.
There are three main units of the Directorate.
1) Medical Care and Hospitals,
2) Public Health,
3) General Administrative.
Functions of Director General Health Services (DGHS)
The Director General of Health Services has two main functions.
1) General Function,
2) Specific function
1) General Function:
1) Survey,
2) Planning,
3) Coordination,
4) Programming,
5) Appraisal of all health matters in the country.
1) Survey:
DGHS conducts surveys and assessments to collect data on public health indicators, disease prevalence, care needs and demographic trends.
These surveys help to understand the health status of the population and inform health and programs.
2) Planning:
After surveying and finding other data, Director General of Health Services (DGHS) plans strategies for health care services.
It involves developing long-term and short-term plans to improve healthcare infrastructure, effectively allocate resources and reduce health issues.
3) Coordination:
Director General Health Services (DGHS) coordinates activities with various health departments, agencies and stakeholders.
Due to this, it can be ensured that health programs are implemented effectively, duplication of efforts can be prevented, and utilization of resources can be optimized.
4) Programming:
Development and implementation of health programs and initiatives is the main function of DGHS.
In which, for prevention of DCs, promotion of health, maternal and child health, vaccination campaigns and other public health interventions.
including the creation of programs for
5) Appraisal of all health matters in the country:
DGHS conducts assessments and evaluations to assess the effectiveness, impact and compliance of health programs and policies.
Regular assessment helps identify strengths, weaknesses and areas for improvement in the health care system.
2) Specific Functions:
1) International Health Relations and Quarantine.
2) Control of Drug Standards
3) Medical store depots
4) Post Graduation Training
5) Medical Education
6) Medical Research
7) Central Government Health Scheme
8) National Health Programme
9) Central Health Education Bureau (C.H.E.B.)
10) Health Intelligence
11) National Medical Library Management
Explanation:
1) International Health Relations and Quarantine
Directly manages the country’s major ports and international airports, maintains health relations with various countries and exchanges information and plays an important role in controlling the spread of diseases.
2) Control of Drug Standard:
Maintains quality and standard of medication under the supervision of Drug Controller. Proper production and distribution of medicines by central and state government officers as per the set standards.
It also checks the quality of drugs as per the Drug Act of 1940.
3) Medical Store Depots:
The central level runs major medical depots such as Mumbai, Chennai, Kolkata, Guwahati, Karnal, Hyderabad which distribute and manage the medical equipment etc. as required by the states in their area. They produce cheap and quality medicine and supply it as needed.
4) Post Graduation Training:
Different National Medical Institutes are responsible for imparting Post Graduation (P.G. Course) training to different health persons in which,
•All India Institute of Medical Sciences at (AIIMS)- New Delhi.
All India Institute of Hygiene and Public Health – Kolkata.
All India Institute of Mental Health and Neuro Sciences- Bangalore.
National Tuberculosis Institute- Bangalore.
Central Research Institute- Kasauli.
National Institute of Communicable Diseases-Delhi.
National Institute of Health and Family Welfare Fair- New Delhi.
Rajkumari Amrit Core (RAK) College of Nursing – New Delhi.
Post Graduation Institute of Medical Education- Chandigarh. 5) Medical Education: Conducts direct management of various medical colleges viz.
•Lady Hardinge Medical College and Associated SSK and KSC,
•Maulana Azad Medical College,
Medical College Puducherry & Goa Apart from these medical colleges, there are many medical colleges in India which are provided guidance and support by the Centre. 6) Medical Research: Medical research in the country is mostly organized by the Indian Council of Medical Research (I.C.M.R = founded in 1911) New Delhi.
Provides economic and other assistance in research into human diseases and their causes, treatment, survey and prevention. All kinds of funds are provided by the Union Ministry of Health.
It operates various research institutes in the medical field such as:
•Cancer Research Centre- Chennai,
Tuberculosis Chemotherapy Centre- Chennai,
Virus Research Centre- Pune,
National Institute of Nutrition at – Hyderabad. 7) Central Government Health Scheme (C.G.H.S):
Which provides insurance cover under which help is available in various accidents, diseases and death etc.
8) National Health Programme:
The National Health Program runs programs that require funds of crores of rupees. Generally these programs cannot succeed without central assistance. A very important function of planning, guidance and coordination is done by this department.
9) Central Health Education Bureau (C.H.E.B):
It does an excellent job of preparing health education to create awareness about health among the people which also plans to provide different types of training to health workers of different levels.
10) Health Intelligence:
Health Intelligence provides information regarding health in all state and international agencies.
11) National Medical Library:
The National Medical Library was declared in 1966 with the main purpose of bringing advancement in medical health and allied sciences and its main objective is to exchange professional books, journals and medical reports etc.
🔸OR🔸
🔸 a. Write down National Health Problems 06 Write down National Health Problems.
National Health Problems
(National Health Issues):
A health problem is a condition in which a person cannot function normally.
Among them, some of the major health problems include:
1) Communicable Disease,
2) Non-communicable diseases,
3) Nutritional problem,
4) Environment problem,
5) Medical care problem,
6) Population problem
•>1) Communicable Diseases:
A communicable disease is an illness that is transmitted from one person to another by infectious agents or their toxic products. This transmission can be mainly directly or indirectly. Its transmission can occur through contact with body fluids, respiratory droplets, and contact with contaminated surfaces.
Communicable diseases are a major health problem in India and account for 54% of deaths in India due to communicable diseases.
communicable diseases such as malaria, tuberculosis, diarrhoea,
Acute respiratory disease,
Filaria,
HIV/AIDS,
Sexually Transmitted Disease (STD) / Sexually Transmitted Infection (STI).
These communicable diseases are considered a major health problem in India.
a) Malaria:
Malaria is a major health problem in India.
Malaria is caused by the Plasmodia parasite which is transmitted by the bite of a mosquito.There are four types of malarial parasites:
1) Plasmodium vivax,
2) Plasmodium ovali,
3) Plasmodium malaria
4) Plasmodium falciparum.
Malaria continues to be a major health problem in India. Although the total number of cases has decreased compared to previous years, the prevalence of Plasmodium falciparum has increased.
According to WHO, malaria affects 36% of the world’s population, with India contributing more than 70% of the 2.5 million cases reported in South East Asia, while two-thirds of the Indian population lives in malaria zones, with the highest number of malaria cases. High Proportion: Found in states of Madhya Pradesh, Chhattisgarh, Jharkhand, Orissa, Andhra Pradesh, Maharashtra, West Bengal and North Eastern states.
During 2015, 1.13 million cases of malaria were detected, of which P. falciparum was detected in 67% of cases, while 287 deaths were reported.
b) Tuberculosis:
Tuberculosis is a bacterial disease caused by Mycobacterium tuberculosis. Tuberculosis bacteria affects the lungs and is spread by sneezing, coughing.
India is the country with the highest TB burden. It remains a major health problem. One-fifth of the world’s incidence of tuberculosis disease is found in India alone.
About 2.2 million people develop tuberculosis disease each year of which 0.62 million are new smear positive highly infectious cases and 0.24 million die from tuberculosis disease each year.
According to WHO 2010, the incidence of tuberculosis in India was estimated to be 249 per 100,000 population and mortality due to tuberculosis disease is 23 per 100,000 population.
( C ) Leprosy:
Leprosy is another major health problem in India.
It is a bacterial disease caused by bacteria called mycobacterium laprae. This disease, which occurs in close contact with an infected person, affects the skin, mucus membrane, nervous system. In which skin discoloration and nerve damage occurs.
Leprosy is a major health problem in India. According to the World Health Organization (WHO), 65% of the new cases of leprosy are found in India. As many as 1.27 lakh cases were detected during 2013-14, of which 9.49% were children under 15 years of age and deformity grade II.
51.48% of these cases were estimated to be multibacillary. All states and union territories report cases of leprosy. However, there is considerable variation not only between one state and another but also between one district and another.
India is home to 54% of leprosy in the world.
(d) Diarrhea:
Diarrhea is caused by bacteria, viruses and other disease conditions.
Diarrheal diseases are considered a major cause of morbidity and mortality in children under five years of age.
There are about 11.67 million cases of diarrheal diseases in India due to poor environmental conditions.
In 2013, more than 100,000 children under 11 months of age died of diarrhea.
After pneumonia, diarrhea is the second leading killer disease of young children worldwide.
India has the highest number of diarrheal diseases. Diarrhea is a preventable and treatable disease. It is also the leading cause of malnutrition in children under the age of five.
More than 2.3 million children die each year, of which 334,000 are due to diarrheal diseases.
(e) Acute respiratory diseases:
Acute respiratory diseases are a major cause of morbidity and mortality in children under five years of age in India.
During 2014, 34.81 million episodes of acute respiratory disease were reported with 2,932 deaths.
(f) Filaria:
Filaria is endemic in about 255 districts of 16 states and five union territories in India. About 630 million people are at risk. To achieve the elimination of LF (lymphatic filariasis), the GOI (Government of India) initiated Nationwide Mass Drug Administration (MDA) with an annual single recommended dose of diethylcarbamazine citrate tablets, in addition to scaling up home-based foot care and hydrocele operations. have done
The National Filarial Control Program was started in 1955.
(G)HIV/AIDS:
HIV (Human Immunodeficiency Virus)/AIDS (Acquired Immunodeficiency Syndrome).
AIDS (acquired immunodeficiency syndrome) is caused by coming into contact with infected blood semen (vaginal fluid).
The Indian Ministry of Health and Family Welfare estimated that HIV prevalence among adults (15–49 years) was 0.27% in 2011, while the number of persons living with HIV was 420,88,642, the number of adults with new HIV infections was 1,16,456 and is the annual number.
(h) STD/ STI:
More than 1 million people contract sexually transmitted infections every day. About 550 million people get sick every year from STIs—chlamydia, gonorrhea, syphilis, and trichomoniasis.
More than 530 million people have genital herpes. More than 290 million women have human papillomavirus infection. Most STI infections present without symptoms. This sexually transmitted infection can be transmitted from the mother to the child through the placenta or at the time of delivery of the baby.
2) Non Communicable Diseases:
Noncommunicable diseases are diseases that are not spread by infection or other people, but are usually caused by unhealthy behavior. They are a leading cause of death worldwide and represent a major threat to health and development, particularly in low- and middle-income countries.
Specially in non-communicable diseases
cardiovascular disease,
hypertension,
cancer,
diabetes mellitus,
mental disorder,
Tobacco Consumption,
alcoholism,
accident,
chronic lung disease,
Catrack, etc
Involvement of diseases like stroke.
(a) Cardio Vascular Disease:
Ischemic heart disease is one of the main causes of death, which is generally increasing rapidly in economically developed countries and developing countries, and is estimated to be the single most important cause of death in India by 2015.
According to the WHO, an estimated 17 million people died from heart-related disease in 2005, accounting for 30% of global deaths. And about 80% of those deaths occurred in low and middle income countries like India. According to the World Health Federation, 35% of cardiovascular diseases in India occur between the ages of 35-64 years.
(b) Cancer:
Cancer has become an important health problem in India.
It is estimated that there are 25 lakh cases of cancer in the country with around 7-9 lakh estimated cases occurring every year. About half of the total cancer cases are tobacco-related cancers in males and 20% of tobacco-related cases are in females.
About 1 million tobacco-related deaths occur each year.
Approximately 50% of deaths in developing countries are caused by cancer. Breast cancer in women-20.01,
Cervical cancer-14.42 and ovarian cancer-5.6 were reported.
Currently India has more cases of oral cancer in the world as a result of tobacco chewing in its rural areas.
(c) Diabetes Mellitus:
India is often referred to as the “diabetes capital of the world” due to the high prevalence of diabetes, especially type 2 diabetes. Rates of diabetes are increasing due to genetic predisposition, urbanization and dietary changes.
In 2011, it was estimated that 62.4 million people were affected by diabetes mellitus and there was an increase of almost 2 million in just 1 year.
In India, 77.2 million people are estimated to be pre-diabetic.
About 4.4 million Indians in their most productive years, between the ages of 20 and 79, do not know they have diabetes. In 2011, diabetes killed nearly one million people in India.
India’s rural population is more affected by diabetes (34 million), while urban population (28 million) is affected by diabetes mellitus. India ranks second after China.
(d) Mental Disorder:
Mental disorders account for 13% of the global burden of disease. According to the National Institute of Mental Health (NIMH) the prevalence rate of schizophrenia is 1.1% of the total population in India while the overall lifetime rate of mental disorder in the total population is 10-12%.
(e) Tobacco consumption:
According to the National Family Health Survey-3, the prevalence of smoking among males and females aged 15-49 years was 32.7% and 1.4% respectively.
Among youth 40% male and 5% female use tobacco.
19% reported smoking cigarettes or bidi and 30% used pan rasala, gutkha or other tobacco.
Tobacco use in any form is a major cause of cancer, especially oral cancer in people who chew tobacco.
(f) Alcoholism:
The pattern of alcohol intake in India varies with geographical area. The highest incidence is in Punjab, Andhra Pradesh, Goa and North-Eastern states where alcohol intake in mail is higher than rest of the country. Arunachal Pradesh, Assam and Sikkim have higher rates of female alcohol intake. In 2005, the estimated number of alcohol consumers was 62.5 million, of which 10.6 million are alcohol addicts in India.
(G) Accident:
According to WHO, road accidents in India have increased from 1.32 lakh (in 2010) to 1.43 lakh (in 2011).
During 1990-2000 the number of deaths due to accidents was 47% of which 93% were due to unnatural causes, 7% due to natural causes.
The death rate due to accidents in the under 14 age group was 8.2%; 15-44 years were 62%, 45-59 years 20% and above 60 years age group was 9.2%.
(h) Chronic Lungs Disease:
Chronic lung diseases include conditions such as chronic obstructive pulmonary disease (COPD) and asthma, which are exacerbated by air pollution and tobacco use.
(I) Catrac:
In India, more than 12 million people are blind. 19.70% cases have refractive error. Cataract surgery with intraocular lens (IOL) implantation has increased significantly from less than 5% in 1994 to 95% in 2011–12.
(j) Strokes:
The increase in coronary heart disease and stroke in India is mainly seen in urban communities than in rural communities. Cardiovascular disease, mainly heart disease and stroke, was the cause of death in 17.5 million individuals.
After heart disease, stroke is the second leading cause of death with 5.8 million fatal cases each year, 40% of which are in people under the age of 70. About 12% of strokes occur in the population under the age of 40. The number of stroke cases in India has increased by 17.5% in the last few decades.
3) Nutritional problem:
Among the major nutritional problems within India,
PEM (Protein Energy Malnutrition),
nutritional anemia,
No Birth Weight Babies,
Xerophthalmia (nutritional blindness),
Iodine Deficiency Disorder,
latherism,
Involvement of fluorosis occurs.
a)PEM (Protein Energy Malnutrition):
Protein energy malnutrition is a problem caused by protein and calorie deficiency and is caused by underconsumption of food.
There are generally two types of protein energy food nutrition.
1) Quasiorkor
Which is seen due to protein deficiency.
2) Marasmus
It is seen due to deficiency of calories.
Thus, due to the deficiency of protein and calories, the child’s weight is less in proportion to his age.
Protein energy mal nutrition occurs from insufficient food or food gap.
This problem is seen in every state of India.
But nutritional marasmus is more common than quasiorchor.
(b) Nutritional anemia:
Nutritional anemia is usually caused by inadequate nutritious diet.
Generally, 60 to 80% of women develop anemic conditions due to vitamin B12 deficiency.
Adult girls are more common.
(c) Low Birth Weight Babies:
Low birth weight babies are more common in developing countries where babies weigh less than 2.5 kg at birth and have maternal malnutrition or anemic conditions as the main cause.
(d) Xerophthalmia:
Xerophthalmia Means Dry Ice This is a medical condition in which tears are not produced in the ice. This condition is usually seen due to deficiency of vitamin A (Av) and mainly this condition is seen in children below 1 to 3 years of age.
(e) Iodine deficiency disorders:
Iodine deficiency causes goiter which is an enlargement of the thyroid gland which is located in the neck. 71 million people in India are affected by goiter.
(f) Latherism:
Latherism is caused by a particular type of mollusk. In which this type of problem is seen especially from fennel saffron dal (Lathyrus sativus). In which weakness, muscular spasm, weakness and paraplegia are seen. In India, this problem is especially seen in states like Madhya Pradesh, Jharkhand and Bihar.
(h) Fluorosis:
Fluorosis is caused by excessive fluoride content in drinking water.Fluorosis is also a major health problem in India.In India, it is found in Tamil Nadu, Andhra Pradesh, Punjab, Bihar, Rajasthan, Kerala, Jharkhand.
4) Environmental Problem:
Environmental problems are mainly seen due to two reasons.
(I) Lake of Safe Drinking Water,
(II) Improper sanitation method for excreta disposal
Mainly soil pollution and water pollution are seen due to these two reasons.
At present, 95% of safe water is found in urban areas and 79% in rural areas.
And the facilities for excreta disposal are found in 61% in urban areas while only 15% in rural areas due to which soil pollution occurs.
Apart from this, environmental pollution is seen in urban areas due to vehicle fumes, improper disposal of waste products from factories, which affects people’s health.
5) Medical Care Problem:
It is seen that medical care is more developed in urban areas than in village areas.
In urban areas, due to overcrowding in hospitals, inadequate staff and lack of adequate amount of drugs and medicine also affect people’s health.
While 80% of the population in rural areas believe on the Indian system of medicine along with inadequate health resources affecting the health of the people.
Lack of proper distribution of health care services in urban and rural areas also affects people’s health.
Due to lack of sufficient manpower, material, money, and inadequate health services in the village, health problems are created due to which morbidity and mortality are seen.
6) Population Problem:
Population problem is one of India’s biggest health problems which affects many aspects of development including, employment, education, housing, health care sanitation and environment.
After China, India comes second in population.
People migrate from rural to urban areas to get more facilities due to which population density increases in urban areas.
Thus, health problems are seen in Nesan like this
b. Write down objectives of School Health Programme. 04 Write the objectives of school health program.
Objectives of the School Health Program
A school health program has multiple objectives, the aim of which is to promote and maintain the health and well-being of students, leading to improvements in their overall educational experience and outcomes.
The objects of the School Health Program are as follows:
1) Promotion of Health Education:
To provide education to students on health related topics such as nutrition, physical activity, hygiene, mental health, substance abuse prevention and sexual health.
Improvement in education and awareness of students.
2) Prevention and Control of Disease:
Measures are taken to prevent and control communicable diseases in children (ex: vaccination, hygiene practices).
Screening of the child for common health issues like vision, hearing etc and early management of any DCs can be done.
3) Promotion of Mental Health:
To create awareness about child mental health and remove social stigma.
If the child has stress anxiety and any other mental problem, provide proper support to the child and take proper measures for its treatment.
4) Promotion of Healthy Behaviour:
Advising the child to do proper physical activity like playing games, exercising, going for outdoor games etc. And educating the child for healthy eating habits like giving advice for adequate nutritive diet intake.
5) Environmental Health and Safety:
To ensure that the school environment is safe and clean in which,
Clean Drinking Water Sanitation Facility,
Safe playground etc. Involvement of students and providing education for accident prevention and safety measures.
6) Counseling and Support Services:
To provide proper counseling to the child who is going through personal and family issues. To provide support to the social and emotional development of the child through peer support groups and counseling sessions.
7) Cooperation and Partnership:
Proper collaboration with families, community organizations, health care providers and government agencies can effectively enhance efforts for health promotion.
8) Other Objectives:
•For positive health promotion of child.
For early detection of any health related problem in the child and to provide immediate referral services to the child.
Apprentice and control the communicable diseases occurring in the child.
To improve health awareness among children.
To provide a healthy environment to the child.
To provide proper hospital services to the children’s class teachers for early detection of any health problems such as eye, skin, ear and dental problems seen in the children.
To reduce morbidity rate in child. Accordingly, the objectives of the school health program have been formulated.
c. Define health team and write characteristics of health team. 06
•>Definition of Health Team,
•> Characteristic of health team
•>Definition of Health Team
A health team is a group of trained medical and non-medical personnel with different levels of knowledge, qualifications, abilities, personality and skills who are complementary to each other and who work together to provide comprehensive health services to individuals, families and communities. Have a goal.
•> Characteristic of Health Team:
1) Interdisciplinary Collaboration:
Definition
Team members come from different professional backgrounds and work together to integrate their expertise.
Example: A team consists of doctors, nurses, social workers and dieticians.
2) Share goal and objective
Definition
All team members work towards achieving common health outcomes and objectives.
Example: improving patient health outcomes, reducing the incidence of disease or managing a chronic condition.
3) Effective Communication
Definition
Open, clear and respectful information exchange among team members.
Example: regular team meetings, sharing of electronic health records and clear documentation.
4) Role Clarity and Respect
Definition
Each member understands their own role and respects the contributions of others.
Example: Knowing who provides patient counseling versus who performs medical diagnosis.
5) Patient Centered Approach
Definition
The team prioritizes the needs and preferences of the patient or community.
Example: Meeting individual patient needs and involving patients in decision making.
6) Mutual support and trust
Definition
Team members support each other and trust each other’s professional judgment.
Example: Team members anchor each other’s input and provide support in challenging situations.
7) Ser decision making
Definition
Decisions are taken collectively, with input from all relevant team members.
Example:
Development of a treatment plan based on the experiences of all team members with contributions.
8) Coordination and Integration of Services
Definition
Team members work together so that service is well organized and care is continuous.
Example: Coordination between specialists and primary care providers for patient care.
9) Adaptability and flexibility
Definition
The team can adjust strategies and roles based on the patient’s changing needs and situation.
Example: Adapting a care plan based on a patient’s progress or new health information.
10) Conflict Resolution Skills
Definition
Team members can resolve and manage conflict constructively.
Example: Addressing differences through discussion and finding mutually agreeable solutions.
11) Commitment to professional development
Definition
Team members are dedicated to continuing education and staying updated on best practices.
Example: Attending workshops, training sessions and professional conferences.
12) Evaluation and Accountability
Definition
Regularly evaluate team performance and hold team members accountable for their responsibilities.
Example: Reviewing outcomes of patient interventions and adjusting strategies as needed.
13) Leadership and Co-ordination
Definition
Effective leadership guides the team and ensures proper functioning.
Example: A team leader or coordinator conducts meetings, delegates tasks, and facilitates collaboration.
14) Evidence Based Practice
Definition
The team uses the best available evidence to make decisions about patient care.
Example: Implementation of treatment guidelines based on the latest research.
15) Cultural Competence
Definition
Understanding different cultural backgrounds and providing respect to them.
Example: Providing care that is sensitive to the patient’s cultural beliefs and practices.
Thus, according to these characteristics of health care team members through which appropriate care can be provided to the patient.
d. Write down functions of Gram-Panchayat. 04 Write the name of Gram Panchayat.
Functions of Gram Panchayat:
Gram Panchayats, which are local self-governing bodies in rural areas of India, have several key functions aimed at grassroots governance and development.
Here are some of the primary functions of Gram Panchayats:
1) Local governance
2) Developmental tasks
3) Social Justice
4) Health and Education
5) Economic Development
6) Environmental protection
7) Welfare Programme
8) Revenue (Mehsul) generation
1) Local Governance:
Gram Panchayats are responsible for local governance and administration within their jurisdiction. They perform various administrative functions such as issuing birth and death certificates, maintaining local records and managing local resources.
2) Developmental Functions:
Gram Panchayats play a crucial role in local development. They are responsible for planning and implementing schemes related to infrastructure development including roads, water supply, sanitation, street lighting and local markets.
3) Social Justice:
Gram Panchayats are tasked with promoting social justice and ensuring equitable distribution of resources and opportunities in the community. They resolve local grievances and settle disputes through (mediation) mediation or arbitration.
4) Health and Education:
Gram Panchayats work to improve healthcare and education facilities in villages. They can establish and maintain primary health centers, schools and other educational institutions to cater to the local population.
5) Economic Development:
Gram Panchayats promote economic activities within the village. They can facilitate agricultural development, promote small-scale industries and support employment generation initiatives to improve the economic well-being of villagers.
6) Environmental Protection:
Gram Panchayats take steps for environmental protection and sustainable development. This includes managing local water bodies, promoting afforestation and implementing waste management practices.
7) Welfare Programme:
Gram Panchayats implement various welfare programs and schemes aimed at the welfare of the weaker sections of the society, including women, children, the elderly and differently-abled persons.
8) Revenue (Mehsul) Generation:
Gram Panchayats are empowered to collect certain local taxes, fees and revenues to fund their activities and developmental projects.
Gram Panchayats serve as important institutions for local governance and development in rural India, ensuring participatory democracy and decentralized decision-making at the grassroots level.
⏩Q-2 Write Short Notes (Any Five) Lakhs (Any Five) 5×5=25
🔸 a. Functions of Primary Health Care (P.H.C) –
To provide health services in rural areas, the Bhor Committee established a Primary Health Center (PHC) which is a PHC for a population of 30,000 in a plain area while a PHC for a population of 20,000 in a hilly, tribal, and backwater area. Which provides health care services to the people of the community.
The functions of a Primary Health Center (PHC) are as follows:
1) Medical care
2) MCH Services
Including family planning.
3) Safe water supply and basic sanitation.
4) Prevention and Control of Locally Endemic Diseases
5) Collection and Reporting of Vital Statistics.
6) Education about health.
7) National Health Program Establishment and Awareness
8) Referral Services
9) Training of Health Guide, Health Worker, Local Dai and Health Assistant.
10) Basic Laboratory Services.
Description:
1) Medical Care:
Primary health centers provide basic medical care to treat acute and chronic health conditions. It also provides outpatient services through diagnosis, treatment and treatment for minor illnesses and injuries.
PHC medical care is essential to meet the immediate health needs of the community.
In medical care, tablets, injections, dressings, and other treatments are provided to the patients according to their disease, besides preventive, curative, promotional care is provided.
2) MCH (Maternal and Child Health) Services including Family Planning:
Primary health centers provide comprehensive maternal and child health care including prenatal care,
antenatal checkup,
Safe Delivery Services,
Post Natal Care,
And immunization is also provided for the child.
In order to support family planning initiatives,
family planning,
counselling,
contraceptive,
And reproductive health services are provided.
This also includes RCH in Maternal and Child Health which covers maternal reproductive child health to adolescent care.
It explains about mother’s antenatal care, nutrition, hygiene, immunization, and laboratory examination etc.
Regular checkups, observations, and education about family planning are provided in the post-natal period.
3) Safe Water Supply and Basic Sanitation:
A primary health center works to improve public health in the community by providing safe drinking water and sanitation facilities in the community.
Primary Health Centers provide education on sanitation, promoting clean water sources and hygienic practices to prevent water borne diseases and improve the overall health of the community.
Steps are taken to maintain environmental cleanliness by providing education to people about basic sanitation, excreta disposal, and cleanliness of kitchen, garden.
Apart from this, there should be drinking water wells and taps which should be chlorinated for safe water supply.
4) Prevention and Control of Locally Endemic Diseases:
Primary health centers play a crucial role in the prevention, surveillance, and control of locally endemic diseases.
Measures are taken to prevent disease including providing vaccinations, providing treatment for endemic diseases, and monitoring disease trends to prevent outbreaks.
5) Collection and Reporting of Vital Statistics:
Primary Health Centers work to collect and report vital statistics such as birth rate, death rate, and incidence of any disease in a particular community. These collected data are essential for monitoring health trends for health planning, allocation of resources, improvement of health outcomes and prioritization of health interventions.
6) Education About Health:
Primary health centers provide education to individuals and communities about preventive health practices, nutrition, hygiene, sanitation and disease prevention strategies.
The Primary Health Center organizes health education sessions, workshops and seminars to bring about improvement in health conditions.
7) National Health Program Establishment and Awareness:
The Primary Health Center implements the National Health Program and Campaigns whose main aim is,
Targeting specific health issues including, immunization drives,
Campaigns are conducted on disease eradication effects, nutrition supplementation, and health awareness.
They spread awareness about national health priorities and encourage community participation in health initiatives.
Each National Health Program has important functions. The clinic provides services related to the National Health Program such as,
Anemia Control Program,
Malaria, Diarrhea, Leprosy, Immunization, TB Control Program, Supplementary Program Referral of mother in abnormal condition during labor for additional services, refer her to Primary Health Center to Female Health Worker, Auxiliary and Nurse Midwife or Medical Officer.
8) Referral Services:
Primary health centers also work to refer patients when the patient requires any specialist medical treatment or any specific diagnosis and if its facilities are not available in the primary health center.
The primary health center provides immediate referral services as per the patient’s need, due to which the patient’s health condition can be improved and complications can be prevented.
9) Training of Health Guide Health Workers, Local Dais, and Health Assistants.
Primary health centers conduct training programs in which training is provided to community health workers, traditional birth attendants, health assistants, and other health care personnel to improve their skills and knowledge.
The main objective of this training is to promote health, prevention of diseases, maternal and child health, and improving the skills of health care personnel in basic medical care.
10) Basic Laboratory Services:
Primary health center conducts basic laboratory services in which tests like diagnostic test, blood test, microscopic test, urine test etc. are done.
Through all these functions provided by the primary health center, preventive, promotional, curative care is provided to the community due to which the overall health condition of the people of the community can be improved and their well-being can be maintained.
b. Occupational Hazards –
Occupation hazards involve a wide range of risks that workers may experience depending on their specific job role and environment.
Occupation hazards are potential risks or hazards that health care workers are exposed to.
Exposure occurs in the workplace environment.
These hazards arise from different aspects of the workplace such as,
physical condition,
Chemical Materials,
Involvement of biological agents, psychological factors, and mechanical hazards etc., these factors pose a threat to the health, safety and well-being of the works and if proper precautions and safety measures are not taken, injuries, illnesses or even loss of life may occur. can
Occupation workers may be exposed to the following hazards:
1) Physical Hazards,
2) Chemical Hazards,
3) Biological Hazards,
4) Mechanical Hazards,
5) Psychological Hazards.
1) Physical Hazards:
Physical hazard is caused by exposure to heat and cold. Workers are those who come in direct exposure to high temperature of sun like farmers, builders, laborers etc.
Even within valleys with high temperatures, such as the Kottar Gold Valley in Mysore, some industries will have local ‘hot spots’ of ovens and furnaces that radiate heat such as bakeries, metal works, asbestos factory engine rooms, etc.
Effects of high temperature include extreme heat, heat allergy, heat exhaustion, muscle cramps.
Many workers are exposed to low temperatures like ice factories, high altitudes, cold storage, cold laboratories etc. This worker may experience chills (when excessive exposure to cold causes pain, itching, and swelling in hands and feet due to poor blood supply), erythrocyanosis and respiratory difficulties.
Hi humidity:
High humidity, along with exposure to extreme temperatures in industries such as textile, paper and ice factories, exacerbates the effects of heat and cold.
Noise:
Loud noise is produced in steel, oil, textile and automobile factories. Loud noise is harmful to health. Its effects depend on the intensity and duration of exposure to loud noise. Loud noise can cause fatigue, nervousness, irritation and partial or complete hearing loss.
Light:
Works may come into contact with poor or glaring and bright light. Poor light causes eye strain and pain, eye strain, headache. Blurring and bright lights cause discomfort, blurring of vision, irritability and visual fatigue.
Vibration:
Vibration occurs while working on machines like grinding, cutting, drilling, boring machines etc. Vibration can cause fatigue, nervousness and local effects such as hand and joint injuries.
Radiations:
Exposure to X-rays and radioactive isotopes can cause skin and blood cancer, genetic changes, malformations, sterility, etc. A person working in radiology department, working in watch factories, ammunition factories come in contact with ionizing radiation. Ultraviolet (UV) radiation such as during welding causes conjunctivitis and keratitis. Ultraviolet radiation can cause sunburn. Road builders, sailors, shepherds and farmers can be affected by ultraviolet radiation.
2) Chemical Hazards:
Factories use some or other chemicals. Chemicals work in 3 ways.
1) Local Action
Some chemicals can cause conditions like dermatitis and eczema.
2) Inhalation
Inhalation of gases and vapors can cause respiratory diseases.
3) Ingestion
Mercury, lead, arsenic, zinc, chromium and cadmium, phosphorus etc. cause various diseases.
Types of Witch are Hazardous
•Gases like carbon monoxide, ozone, carbon dioxide, hydrogen and cyanide etc.
Fumes and vapors from various types of acids, mercury vapour, etc.
Mistus
Mist from the electroplating industry.
•Dust: Small particles broken down by crushing and grinding of rock, ore, metal wood etc.
Chemical agents that are harmful to the skin, respiratory system and gastrointestinal interstitial system.
Skin problems involve dermatitis, eczema, urticaria, ulcers and cancer etc.
•Respiratory problems include various types of pneumoconiosis. Silicosis due to quartz dust,
Anthracosis due to coal dust,
Byssinosis due to cotton dust,
Asbestosis due to asbestos dust,
- Shortness of breath due to carbon monoxide, hydrogen sulphide and hydrogen
- Various pungent gases like cyanide chlorine, ozone, nitrogen oxide, sulfur dioxide can cause throat irritation. Asbestos, beryllium, coal tar, mineral oil can cause lung cancer.
3) Biological Hazards:
Biological hazards are caused by infectious and parasitic agents like viruses, rickettsia, bacteria. Due to this, hookworm infestation can also occur in farmers. Leptospirosis can occur in workers working in valleys.
Various zoonotic diseases like brucellosis, mycotic infections, parasitic infections and anthrax can occur in tanning factories, veterinary hospitals and dispensaries, zoos, circuses, agricultural workers, butcher houses etc.
Health workers working in hospitals/dispensaries may be exposed to patient infections such as tuberculosis, tuberculosis, HIV and serum hepatitis etc.
4) Mechanical Hazards:
Various accidents and injuries can occur due to unprotected machines and their protruding and moving parts and machines with low safety can cause partial and permanent disability.
5) Psychological Hazards:
Different types of maladjustment problems like lack of proper job satisfaction,
A person cannot adjust properly due to insecurity, frustration and environmental tension. Due to this condition, physical health problems such as increased blood pressure, indigestion, insomnia,
Conditions like loss of appetite and hardburn may occur.
Thus, it is important to take measures to prevent these types of hazards in workers by identifying them early and properly.
c. Millennium development goal –
The Millennium Development Goals (MDGs) were eight global objectives established by the United Nations in 2000 to combat extreme poverty and improve global health by 2015.
Each goal had specific targets and indicators to measure progress.
1) Eradicate extreme poverty and hunger.
The goal aims to halve the proportion of people living on less than $1.25 a day and achieve food security for all. It seeks to eradicate extreme poverty and focus on malnutrition through various programs focused on economic development, food security and poverty reduction strategies.
2) Achieve Universal Primary Education
(Achieving Universal Primary Education)
Thus, the target was to ensure that all children, regardless of gender or background, complete the entire primary school curriculum.
This involves not only increasing school enrollment rates but also aims to remove barriers to education such as child labour, inadequate school infrastructure and socio-cultural factors.
3) Promote Gender Equality and Empower Women.
(Promoting Gender Equality and Empowering Women)
These goals seek to eliminate disparities in primary and secondary education and empower women in all aspects of life.
It addresses issues such as educational inequality, employment discrimination and violence against women, with the aim of creating equal opportunities for both sexes.
4) Reduce Child Mortality
Its aim was to reduce the under-five mortality rate by two-thirds (2/3).
Efforts under this objective include improving child health through better nutrition, vaccination programs and access to health care services to combat preventable diseases and reduce infant and child deaths.
5) Improve Maternal Health
The goal aims to reduce the maternal mortality ratio by three-fourths (3/4) and improve reproductive health.
Maternal health care services, to reduce pregnancy and child birth related deaths.
Skill focuses on increasing access to birth attendants and family planning resources.
6) Combat HIV/AIDS, Malaria and Other Diseases
Its goal was to prevent and reverse the transmission of HIV/AIDS, malaria and other major diseases.
These include prevention, treatment and care efforts as well as initiatives to reduce the incidence of these diseases through public health campaigns and increasing access to medical services.
7) Ensure Environmental Sustainability
These goals seek to integrate the principles of sustainable development into national policies and reverse environmental degradation.
It aimed to reduce deforestation, promote clean water and sanitation, and address issues such as climate change and biodiversity loss.
8) Develop a Global Partnership for Development
This final goal focuses on creating a global environment conducive to development by increasing international cooperation.
It includes goals to increase aid to developing countries, improve trade opportunities, address debt relief and promote technology transfer.
Thus, a total of 8 goals are involved in the Millennium Development Goals
d. Role of a Nurse in Polio Eradication Program –
Nurses play a crucial role in the program of polio eradication.
The aim is to prevent and eliminate this disease through different responsibilities and activities. Here, the key roles and responsibilities of nurses in polio eradication efforts are given:
1) Vaccination administration
Provide Oral Polio Vaccine (OPV)
A nurse administers OPV to children, ensuring that every child under the age of five receives the required dose during the vaccination campaign.
Proper handling of vaccines
The nurse is responsible for maintaining the cold chain to ensure that the vaccine remains effective from storage to administration.
2) Community Education and Awareness
Educating Parents and Care Givers
The nurse provides information to the child’s parents and caregivers about the importance of polio vaccination, how the vaccine works, and the risks of polio.
Addressing vaccine hesitancy
They address parents’ concerns and misinformation about vaccination, helping to increase community acceptance and participation in vaccination campaigns.
3) Surveillance and Monitoring
Reporting Cases of the Cute Flaccid Paralysis (AFP)
The nurse is involved in the surveillance of AFP (acute flaccid paralysis) cases, which can be a symptom of polio.
They should be reported immediately for investigation and diagnosis of these cases.
Monitoring vaccination coverage
They track and report vaccination coverage rates, identify areas of low coverage, and coordinate efforts to reach those areas.
4) Health Education and Promotion
Promoting hygiene and sanitation
The nurse educates the community about procedures that help prevent the spread of polio, such as proper hand washing and maintaining hygiene.
Supporting routine immunization
They promote a regular vaccination schedule and help integrate polio vaccination into regular health services.
5) Coordination and Collaboration
Collaborate with other health workers
The nurse works with other health care professionals, community leaders, and organizations to plan and implement health education initiatives for vaccination campaigns.
Participation in vaccination days and campaigns:
They are key participants in National Immunization Days (NID) and Sub-National Immunization Days (SNIDs), which are aphots of mass vaccination.
6) Data Collection and Reporting
Collecting vaccination data
The nurse collects and records data on vaccination coverage, adverse events after vaccination, and outcomes of the vaccination campaign.
Reporting and Documentation
They document the effects of vaccination, report on the results of vaccination campaigns, and help analyze data to inform future strategies.
7) Emergency Response
Responding to Polio Outbreak
Nurses participate in emergency response efforts in case of polio outbreaks,
This includes intensified vaccination campaign and control measures to prevent outbreaks.
Providing clinical care
In rare cases, nurses provide care to polio survivors or individuals with polio-related complications.
8) Advocating for resources and support
The nurse advocates for adequate resources to fund and support polio eradication programs at the community and policy levels.
By fulfilling this role, nurses are essential to the success of polio eradication efforts, helping to achieve high vaccination coverage, maintaining strong surveillance systems, and fostering community support for the program.
🔸 e. Objectives of National Family Welfare Programme-
Enlist the objectives of Family Welfare Programme
The National Family Welfare Program in India is a comprehensive set of initiatives aimed at improving family health and well-being.
Family welfare programs are designed to achieve various objectives to improve family life and societal health.
Here are the objectives of the Family Welfare Programme:
1) Promote maternal and child health and reduce mortality:
Objective:
Improving family health, with particular focus on maternal and child health, reducing infant and maternal mortality rates.
Action
Provide prenatal and positive care to the mother
Implementing child vacation program to prevent child from disease.
Providing nutritional support to children and monitoring their growth.
Improvement in access to health care services for mother and child. 2) Enhance Reproductive Health and Family Planning: Objective
Assisting individuals and couples in managing reproductive health and family size. Action
Contraceptive methods and family planning services are offered.
Education and counseling about reproductive health is provided.
- To promote safe motherhood and prevent unwanted pregnancy. 3) Imprude Education and Awareness: Objectives
Improvement in public knowledge about health, family planning and welfare services. Action - Programs are conducted to create awareness among the public about health and family planning.
Educational workshops are organized for parenting, nutrition and health.
Integrating family welfare topics into the school curriculum. 4) Support Economic Stability: Objectives
Achieving the financial security of the family and improving its quality of life. Action
- Providing financial assistance through subsidy and welfare programs.
- Offer job training programs and support for small businesses.
- Facilitate microfinance opportunities for low income families. 5) Promote Gender Equality: Objective
- Eliminate gender imbalance and empower women and girls. Action
- Provide legal aid and shelter for victims of domestic violence.
Supporting women’s rights and gender equality initiatives.
To provide education and professional opportunities for women and girls. 6) STRANDHEN FAMILY STRUCTURE: OBJECTIVES
Strengthening healthy family relationships and providing support to families in crisis situations. Action:
To provide family counseling services for relationship and family issues.
•Organizing parenting workshops and support groups.
- To provide crisis intervention services for families facing domestic violence. 7) Support Elderly and Disabled Family Members: Objective
To provide support to elderly and disabled persons. Action
To provide pension and financial support for elder person.
To provide home care services and specialized medical care for disabled persons.
To provide accessibility of assistive technology for disabled persons. 8) Promote Child Development and Protection: Objective
Children should be healthy, safe and have opportunities to develop. Action
Implementation of Early Childhood Education Programme.
- Development of child protection services to prevent child abuse and misuse.
Advocating for child’s rights and legal protection. 9) Anchorage Community Involvement: Objectives
To promote community engagement in family welfare affairs. Action
To provide support to community best welfare programs and voluntary opportunities.
Involvement of local organizations to provide family welfare services.
- To promote community awareness about family health and welfare issues. 10) Address Urban and Rural Disparities: Objectives
Family welfare services can be accessed equally in both urban and rural areas. Action
To develop target programs in rural and affected areas.
Allocating resources to bridge the gap between urban and rural services.
Involvement of special initiatives to meet the unique needs of different communities. 11) Facilitate Mental Health Support: Objective
Assessing mental health issues in families and promoting mental wellbeing. Action
Provide mental health counseling and psychological support.
To create awareness among community members about mental health issues in the community and to eliminate mental health related stigma.
Implementation of programs for stress management and emotional support. 12) Promote Safe and Healthy Environment: Objective
Making living conditions safe and promoting environmental health. Action
- Implementation of public health initiatives to ensure clean water, hygiene and safe housing.
•Promoting environmental stability through community programs. Thus, the Family Welfare Program aims to improve the overall well-being of families through various objectives focusing on health, education, economic stability, and social support.
🔸f. High risk pregnancy
A high-risk pregnancy involves a pregnancy in which there is an increased risk of health complications for the mother or the baby. Many factors can make a pregnancy high risk, and the management of such a pregnancy often requires specialized care to ensure the best outcome for both mother and baby.
Categories of High Risk Pregnancy
1) Maternal health condition
Pre-Existing Conditions:
Conditions like diabetes, hypertension, thyroid disorders and heart disease.
Pregnancy Related Conditions
These include conditions like gestational diabetes, preeclampsia,
Conditions such as eclampsia.
2) Age factor
Advance Maternal Age
Women over the age of 35 are considered to be at higher risk for complications.
Teenage pregnancy
A very young mother’s pregnancy is considered high risk because of potential health and developmental issues.
3) Pregnancy complications
Multiple pregnancy
Carrying twins, triplets or multiple fits can increase the risk of preterm labor and other complications.
Common Pregnancy Complications
Due to history of complications like preterm birth, miscarriage etc.
4) Life style factor
Substance Abuse
Use of tobacco, alcohol or illegal drugs.
Poor nutrition
Due to not intake of diet in adequate amount or if there is any eating disorder.
5) Fittal condition
Genetic disorders
In this condition pregnancy can be high risk due to any genetic disorder like Downsyndrome or any other genetic cause.
Growth Issue
Fits is a condition characterized by intrauterine growth retardation.
6) Obstetric history
Previous complications
History of severe complications in previous pregnancy such as,
Having a condition of stillbirth (stillbirth) or severe preeclampsia
••>Management Strategies
1) Regular monitoring
Regular antenatal checkup to assess the condition of maternal and fit health.
Ultrasound and proper diagnostic tests should be done properly during pregnancy so that the growth of the fetus can be assessed and early intervention can be done if there are any complications.
2) Medical intervention
Seek appropriate medical treatment for any pre-existing disease condition or condition arising during pregnancy.
Getting special treatment for conditions like preeclampsia or gestational diabetes.
3) Life style modification
Provide advice on nutritious diet, exercise and avoidance of harmful substances.
Advise on managing stress effectively and improving overall well-being.
4) Planning for Delivery
Detailed birth planning including discussion of delivery method (vaginal or caesarean section) based on risk and condition.
5) Educational support
Educate the mother about high-risk pregnancies and provide education about what to expect during the labor process.
Effective management of high-risk pregnancies requires a collaborative approach by obstetricians, maternal-fetal medicine specialists, and other health care personnel to ensure the best outcome for mother and child.
🔸g. Service package of I.C.D.S-
ICDS (Integrated Child Development Services):
ICDS (Integrated Child Development Services) is one of the most important services for child welfare.
ICDS was launched on 2 October 1975. In which 33 projects were implemented all over the country, including 4 urban areas, 19 rural and 10 tribal areas.
ICDS is a program in which growth and development of 3 to 6 year old children is done by providing a natural joyful and simulating environment through Anganwadi.
ICDS provides basic education to the child.
In this service,
- Supplementary Nutrition,
- Immunization,
•Health checkup,
•Medical Referral Services,
nutrition,
- Health Education for Women,
- Child up to 6 years
Non Formal Education,
And pregnant and nursing mothers of rural, urban, slum and tribal areas are also involved in this scheme.
Preventive and Developmental Aids are taken up in Integrated Child Development Services (ICDS). Objectives:
1) To improve the nutritional status of children aged 0-6 years.
2) Children can have proper psychological, physical and social development.
3) To reduce the mortality rate, morbidity rate, malnutrition and school drop out rate of children.
4) Effective coordination with different departments working for the development of children.
5) To enhance mother’s capability and child’s nutritional needs through proper nutrition and health education.
Service Package:
1) Supplementary Nutrition,
2) Nutritional Health Education,
3) Immunization,
4) Health Checkup,
5) Pre School Non Formal Education,
6) Referral Services,
•>1) Supplementary Nutrition:
Target Group:
Children between 0-6 years,
pregnant women,
lactating woman,
Expectant Mother.
Services Provided by:
Anganwadi Worker (AWW),
Anganwadi Helper.
In this,
Supplementary feeding is provided.
•Growth monitoring is done.
- Worked for prophylaxis of vitamin-A deficiency.
•Also works to control nutritional anemia. A survey is conducted in the community to identify pregnant women and children. Supplementary nutrition is provided 300 days in a year. Growth monitoring and nutritional surveillance are also two activities carried out. For that growth chart is monitored. This growth chart is helpful in detecting the nutritional status. A child below 3 years of age is measured once a month and a child of 3-6 years of age is measured four times during the year. Severely malnourished children are provided with special care and referred for better medical services. 2) Nutritional Health Education ( NHED ): Target Group
Women (15-45) years. Services provided by
Anganwadi Worker (AWW)
Auxiliary Nurse and Midwife (ANM),
Medical Officer (MO). Nutrition and health education is a key element to the work of an anganwadi worker. In Nutrition and Health Education (NHED) to build the capacity of women in the same group between 15 to 45 to provide them with education about their own health development needs and child and family care. Health education on nutrition is provided to every pregnant and lactating mother and nursing and expectant mothers are given the highest priority. 3) Immunization: Target Group
A child below the age of 6 years,
pregnant mother,
Lactating mother. Services provided by
Auxiliary Nurse and Midwife (ANM),
Medical Officer (MO) Immunization is specifically given to pregnant women and children to prevent 6 killer diseases. The six killer diseases like diphtheria,
Pertussis, tetanus, polio, hepatitis B and measles are involved. By providing vaccine, morbidity mortality, disability, and malnutrition seen in children due to these major diseases can be prevented.
Immunization of pregnant women against TT prevents rates of maternal and neonatal tetanus. 4) Health Checkup: Target Group
A child below six years of age,
pregnant women,
Lactating Woman. Services provided by Auxiliary Nurse and Midwife (ANM),
Medical Officer (MO),
Anganwadi Worker (AWW). In it, care is provided to antenatal mother, poster mother for children under six years of age.
Different health services are provided by Anganwadi workers, PHC staff.
In it,
Regular health checkup,
immunization,
Management of Malnutrition,
Treatment of Diarrhea,
deworming,
Medicine Distribution,
Antenatal-Postnatal Checkup,
Iron and folic acid supplementary medication,
Services to treat respiratory tract infections,
This type of service is provided. It also provides services of prophylaxis against deficiency of vitamin A and anemia. 5) Pre School Non Formal Education: Target Group
Children from three to six years. Service provided by
Anganwadi Worker(AWW). Non-formal pre-school education is an important component. Pre-School Education (PSE) is the backbone of Integrated Child Development Services (ICDS).
These services are provided by Anganwadi Centers. 6) Referral Services: Target Group: Children below six years,
pregnant woman,
Lactating Mother Services Provided by Auxiliary Nurse and Midwife (ANM),
Medical Officer (MO),
Anganwadi Worker (AWW). While doing health checkup and growth monitoring of children, sick and malnourished children and children who require immediate medical attention are identified and referred to Primary Health Center (PHC) and sub-centres. The Anganwadi Worker (AWW) prepares a list of children with disabilities detected and creates a special register for the same and refers such children for further treatment. Thus, Integrated Child Development Services (ICDS) play a crucial role in assessing maternal and child health issues, reducing malnutrition and promoting childhood development.
🔸 h. National Eradication Program –
National Eradication Programs are comprehensive public health initiatives aimed at eradicating or preventing particular diseases.
The goals, strategies, and objectives of these programs may vary depending on the disease targeted.
Here are some of the major National Eradication Programs available in India:
1) National Vector Borne Disease Control Program (NVBDCP)
objective
Control or elimination of vector borne diseases like malaria, dengue, chikungunya and filariasis.
Key Strategies
Disease Surveillance
Regular monitoring of incidence of diseases and vector population.
Vector control
Indoor Residual Spraying,
Distribution of bed nets
and taking measures like larvicidal activity.
Public Awareness
To start health education campaign as prevention of vector borne diseases.
Diagnosis and Treatment
Diagnosis and treatment through public health facilities.
2) National Immunization Program (NIP)
objective
Achieving universal immunization coverage to prevent vaccine-preventable diseases.
Key Strategies
Vaccination Services
Provide routine immunization for children and pregnant women.
Vaccination Campaign
Special campaign for high risk area and catch-up immunization.
Cold chain maintenance
Ensuring safe storage and transportation of vaccines.
Monitoring and Evaluation
Tracking of Immunization Coverage and Effectiveness.
3) National Polio Eradication Program (NPEP)
objective
Eradication of polio from India.
Key Strategies
Pulse polio immunization
Nation Vice Vaccination Campaign
Surveillance
Conducting surveillance of acute flaccid paralysis (AFP) and environmental monitoring.
Mass Immunization
Regular National Immunization Day.
4) National Tuberculosis Elimination Program (NTEP)
objective
Elimination of Tuberculosis as a Public Health Problem.
Key Strategies
Direct Observe Treatment Short Course (DOTS)
Ensuring adherence to TB treatment regimens.
Case finding
Detection of active cases through screening programs.
Public Health Education
To conduct awareness campaign for prevention and treatment of TB.
Drug Management
Ensuring availability of antituberculosis drugs.
5) National Leprosy Eradication Program (NLEP)
objective
Eradication of Leprosy as a Public Health Problem.
Key Strategies
Multidrug therapy
Providing free treatment through public health system.
Surveillance
Identifying and treating new cases.
Public Awareness
To provide education about leprosy in the community and reduce sigma about it.
6) National Filaria Control Program ( NFCP ):
objective
Control or elimination of lymphatic filariasis.
Key Strategies
Mass. Drug Administration
Providing anti-fibrial medication in the affected population.
Vector control
Breeding sites of mosquitoes and taking measures to reduce them.
Surveillance and Monitoring
Tracking the incidence of diseases and the effectiveness of the program.
•>General Objectives of National Eradication Programme
1) Disease Elimination
Eradication of targeted diseases from the population.
2) Health promotion
Bringing improvement in public health through disease prevention and health education.
3) Early detection
To prevent the outbreak of any DCs, early identification and treatment should be provided.
4) Access to care
To provide equitable health care services to all population.
This program reflects India’s commitment to improving public health, and controlling diseases that pose a significant threat to health.
Thus, National Eradication Programs are comprehensive public health initiatives aimed at eradicating or preventing particular diseases.
⏩Q-3 (A) Fill in the blanks. Vacancy filled .10
🔸1) T.B day celebrated on——- T.B day——–
24 March
🔸2) P.E.M stands for ————
PEM:
Protein-Energy Malnutrition.
🔸3) At birth average normal weight of the newborn is —–gm. Average newborn weight at birth is———– grams.
2.5 – 3.8 Kg
🔸4) Alma atta conference was held in———-year. The Alta-Ata Conference was held in ——–year.
1978
🔸5)——-month is known as antimalarial month. ——–Mass is known as antimalarial mass.
June
🔸6) ———–test is done for diagnosis for tuberculosis. ———Test is done to diagnose TB.
Tuberculin Skin Test (TST) (Mantoux test)
🔸7) Covid-19 is spread through ———– Covid-19 is spread from —–
respiratory droplets.
🔸8) Early registration means——-weeks registration. Early registration means —— week registration.
12 week registration
🔸9) PNDT act is enacted to prevent abortion of
female foeticide
🔸10) Community development block covers———-villages. Community Development Block covers———Village.
100 villages.
⏩(B) State whether the following statements are True or False. 10 State whether the following statements are true or false
1) A.R.T is given to H.I.V patient. An HIV patient is given A.R.T.
True
2) M.T.P can be done upto 28 weeks. M.T.P can be done up to 28 weeks.
False
(Reason := According to the Medical Termination of Pregnancy (MTP) Act, married women, rape survivors and vulnerable groups like differently-abled and minors are allowed for termination up to 24 weeks.)
3) One P.H.C covers 3000 population. A primary health center covers a population of 3000.
False
(Reason := A Primary Health Center (PHC) covers a population of 30,000 in plain area and 20,000 in hilly, tribal and backward areas. )
4) C.D.H.O is the head of P.H.C. The CDHO is the Head of the Primary Health Centre.
False
(CDHO (Chief District Health Officer):
The Chief District Health Officer oversees public health programs and health administration at the district level.
Whereas, the Head Medical Officer (MO) of a Primary Health Center (PHC).
5) Oral rehydration does not contain calcium lactate. O.R.S does not contain calcium lactate.
True
6) Diarrhea and ARI are the main causes of under-five mortality. Diarrhea and acute respiratory infections are the leading causes of death in children under five.
True
7) P.P.L.U.C.D is introduced soon after delivery. PPIUCD is placed immediately after delivery.
True
8) Mid-day meal program is also called noon meal program. Mid-day meal program is also known as mid-day meal program.
True
9) Four time A.N.C examination done during ANC period. Examination is done 4 times during the antenatal period.
True
10) Condom prevents S.T.D. Condoms prevent STDs.
True.
⏩(C) Write Multiple Choice Questions. Write the correct option from the following. 10
1) Malaria is transmitted by
a) Female anopheles- female anopheles
c) Virus- virus
b) Bacteria- Bacteria
d) aedes- Aedes
2) Anganwadi worker covers population. Anganwadi worker covers the population.
a) 1000
c) 4000
b) 5000
d) 2000
3) Head quarter of W.H.O located in the headquarters of W.H.O.
a) Geneva- Geneva
c) Delhi- Delhi
b) U.S.A.
d) U.K.
4) Covid-19 mainly affects to
a) Reproductive System – Reproductive system
c) Urinary System- Urinary system
b) Skeletal System- Skeletal System
d) Respiratory System- Respiratory system
5) Permanent method of family planning for male Permanent family planning method for men
a) Copper-T- Copper-T
c) Tubectomy – Tubectomy
b) Oral Pills – Oral pills
d) Vasectomy – Vasectomy
6) A patient at subcentre can be referred to
a) P.H.C
c) District Hospital – District Hospital
b) C.H.C – C.S.C.
d) Specialty Hospital – Specialty Hospital
7) Census is take place every year
a) 10 Years – 10 years
с) 05 Years -05 years
b) 20 Years – 20 years
d) 02 Years – 02 years
8) The maternal health services includes
a) Antenatal Care- Antenatal care
c) Postnatal Care- Postnatal care
b) Intranatal Care- Intranatal care
d) All of above
9) Which of the following is not a communicable disease?
a) Malaria – Malaria
c) AIDS – AIDS
b) T.B – T.B
d) Cancer – Cancer
10) In severe anemia hemoglobin is less than
a) 10 mg
c) 08 mg
b) 09 mg
d) 06 mg
Q: (1) Ans
a) Female Anopheles mosquito
Q: (2) Ans
(a)1000
Q: (3) Ans
(a) Geneva
Q: (4) Ans
D) Respiratory System
Q: (5) Ans
(d) Vasectomy
Q: (6) Ans
(a)PHC – P.H.C.
Q: (7) Ans
(a) 10 years
Q: (8) Ans
(d) All of the Above
Q: (9) Ans
(d) Cancer
Q: (10) Ans
(d) 06 mg
💪 💥☺ALL THE BEST ☺💥💪

Note :-MCQ ANSWER in unique pattern of APP in both languages is given below paper solution / click here. Clicking on “A” will change the language.
IF ANY QUERY OR QUESTION, REVIEW-KINDLY WATSAPP US NO. – 84859 76407