ENGLISH 🟢GNM-T.Y-CHN-II-GNC-PAPER SOLUTION-YEAR-23/03/2021(DONE-upload paper no.2)
GNM-T.Y-CHN-II-GNC-PAPER SOLUTION
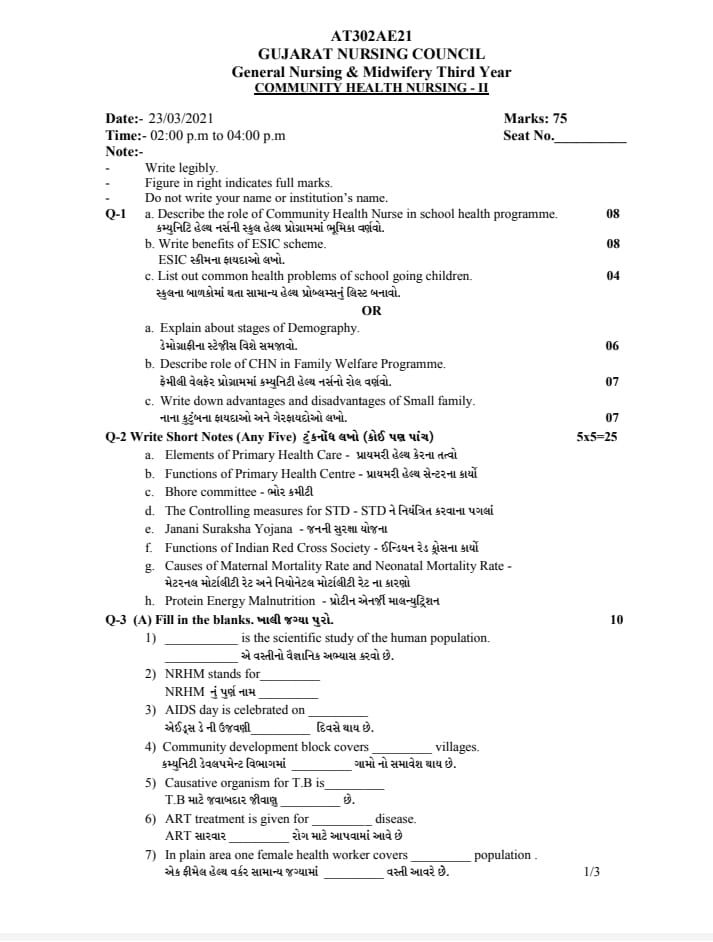
⏩Q-1
🔸 a. Describe the role of Community Health Nurse in school health program. 08 Describe the role of the community health nurse in a school health program.
The role of the community health nurse in the school health program is multiple and vital in promoting student health and well-being.
Here are some key aspects of his role:
1) Health Promotion and Education:
Community health nurses provide education to students, teachers and their parents on health related topics such as hygiene, nutrition, sexual health, and mental health.
Nurses conduct health promotion activities to encourage healthy behavior and prevent diseases.
2) Health Screening:
The nurse performs screening tests such as vision test, hearing test, body mass index (BMI) assessment and dental checkup etc. for early identification of health issues seen in the school going child.
The nurse also monitors immunization records to ensure that the child has received up to date vaccinations.
3) Managing Chronic Conditions:
Nurses provide support to students who have chronic health related conditions such as asthma, diabetes by administering medication, monitoring their symptoms and providing health education for proper self-management.
The nurse also collaborates with the child’s parents and teachers to create the child’s individualized health plan.
4) First Aid and Emergency Care:
A nurse is trained to provide immediate first aid and emergency care in the event of any injury, illness, or accident occurring to the child while the child is in school hours. The nurse assesses the situation and provides the necessary treatment accordingly and also refers the child to the hospital immediately if he needs further medical treatment.
5) Referral and Follow-up: The nurse refers the child to the health care facilities when the need arises or if the child needs any medical treatment or specialty care during an emergency.
They follow up on referrals to ensure students receive appropriate care and support.
6) Health Advocacy:
The nurse advocates for school health policies and practices that promote a safe and healthy environment for students.
The nurse collaborates with school administrators, teachers, and community helpers to implement health promoting initiatives.
7) Counseling and Support:
The nurse provides counseling and emotional support to the child to face the child’s health related challenges and personal issues.
The nurse provides services as a trusting avenue for students to discuss confidentiality concerns.
8) Collaboration and Partnership:
The nurse works collaboratively with teachers, school counselors, social workers, and other health care personnel to fulfill the child’s holistic needs.
The nurse participates with interdisciplinary team members to formulate strategies to improve the child’s health and well-being.
9) Health Record and Management:
The nurse properly records and documents the child’s assessment, screening treatment and intervention.
The nurse maintains the child’s privacy and confidentiality.
10) Health Promotion Campaigning:
The nurse organizes health campaigns and events to raise awareness of specific health issues in school communities, to anchor healthy lifestyles, and to support the school environment.
Overall, nurses play a crucial role in improving the physical, mental, social, and spiritual health of children in school settings.
b. Write benefits of ESIC scheme.
Write the advantages of ESIC scheme. 08
Benefits of ESIC SCRIM:
ESI: Employees State Insurance (ESI) Act
The Employees’ State Insurance (ESI) Act, was passed in 1948.
This act is a comprehensive social security act in the country. This act is an important measure to provide social services and health insurance in the country.
Certain benefits in case of sickness, maternity, disability and death due to employment injury to the employee such as,
Provides case and medical benefits in certain amount.
•>Benefits of ESI Act :
1) Medical benefit,
2) Sickness benefit,
3) Maternity Benefit,
4) Disability Benefit,
5) Dependent Benefit,
6) Funeral Benefit,
7) Rehabilitation benefit.
1) Medical Benefit:
Medical benefit includes full medical care provided during hospitalization.
Comprehensive medical care is provided to the insured person and their dependents through a network of ESI hospitals, dispensaries and tie-up hospitals as follows:
OPD care,
Providing drugs and dressings,
All types of specialties medical services,
free drugs,
Pathological and Radiological Investigation,
Immunization and Family Planning Services,
Domiciliary Services,
Antenatal and Postnatal Services,
Emergency Services,
Ambulance Services,
Health Education in Patient Treatment.
etc. medical services are provided,
And also in complicated cases where specialized treatment is required, the patient is referred for institutional treatment outside the state at the expense of ESI Corporation.
Other Medical Benefits:
- Dentures,
•Artificial limbus, - Spectacles (prostheses),
•Hearing Aid,
•Hernia belt,
•Walking Caliper, - Jackets, etc. are also provided when required.
2) Sickness Benefit:
If the sickness is certified by the Insured Medical Officer or Insurance Medical Practitioner then the assured is entitled to the sickness benefits.
Sickness benefit is payable for a maximum of 91 days in any continuous period of 365 days on a case by case basis. In this case the rate of payment is 50% of the daily wage.
A person receiving sickness benefit has to undergo medical treatment provided under the Act.
Extended Sickness Benefit:
If an insured person suffers from a long term illness, as per the Act, he is entitled to extended sickness benefit for a maximum of two years in addition to 91 days of sickness benefits. There are 34 illnesses for which a person who has been in continuous employment for more than two years Extended benefits may be paid.
Enhance Sickness Benefit:
Enhanced Sickness Benefit is provided for 14 days after Tubectomy to Assured Women and 7 days to Assured Males who have undergone Vasectomy.
3) Maternity Benefit:
An employee woman who is pregnant gets 120 to 180 days leave under maternity benefit.
Such pregnant women are not provided night work from 7.00 pm to 06.00 am.
In case of Medical Termination of Pregnancy (MTP) 15 days leave is given for the same.
In case of abortion, women are given 6 weeks or 45 days leave.
Paternity leave is granted up to 15 days.
Working pregnant women with excessive weight carrying are not covered under this act.
Antenatal, intranatal and post-partum services are also provided free of charge to pregnant women.
4) Disability Benefit:
Case benefit is provided in case of temporary or permanent disability due to employment injury.
The amount of benefit changes depending on the disability.
Temporary Disability Benefit (TDB) is payable from the first day of entry into indemnifiable employment and any contribution is paid in case of employment injury at the rate of 90% of wages for as long as the disability continues.
Permanent Disestablishment Benefit:
Permanently disabled benefits are paid at the rate of 90% of wages in the form of monthly payments based on the extent of loss of earning capacity as certified by the Medical Board.
In case of total disability, they are given life pension.
5) Dependent Benefit:
Dependent benefits are paid at the rate of 90% of wages to the dependents of the deceased or injured person in cases where death or injury occurs due to employment injury or occupational hazards.
6) Funeral Benefit:
Funeral benefits provide a cash payment of ₹10,000/- payable towards the funeral expenses of the insured on his death.
7) Rehabilitation Benefit:
The insured person and his family members can continue to receive medical treatment even after permanent disability or retirement.
An artificial limb is provided to the insured worker as and when required and the case is also provided as artificial and sickness benefits rate until replacement of the artificial limb is done.
Overall, the Employees State Insurance Act, 1948 stands as a crucial pillar of social security in India, improving the welfare of covered employees and their dependents through various benefits aimed at providing financial assistance and medical care in times of need.
c. List out common health problems of school going children. 04 Make a list of common health problems in school children.
List of common health problems in school children:
Different health problems seen in school going children are generally different based on their age, religion and socioeconomic factors.
Here, the list of health problems seen in school going child is as follows:
1) Respiratory Infections: Tema, Common Cold, Flu, Tonsillitis, and Bronchitis.
2) Gastrointestinal system: ie, diarrhea, constipation, and abdominal pain.
3)Dental problems: eg, cavities, tooth decay, and gingivitis.
4) Allergies: Allergic rhinitis (hay fever), food allergies, and skin allergies.
5) Injuries:
Injuries due to falls,
Sports activity or playground accident.
6) Vision problems: Refractive errors like (nearsightedness) or astigmatism.
7) Hearing problem: Hearing loss or ear infection.
8) Mental Health Issues: Anxiety Disorders, Depression, and Behavioral Changes.
9) Obesity and overweight due to excessive intake of fatty and spicy food and lack of physical activity.
10) Skin conditions: Eczema, dermatitis, and fungal infections like ringworm.
11) Nutritional deficiency: iron deficiency anemia, vitamin deficiency.
12) Chronic Conditions: Asthma, Diabetes Epilepsy and Other Long Term Health Conditions.
13) Social and Emotional Issues: Bullying, peer pressure, family and academic related stress.
14) Infectious Diseases: Measles, Chicken Pox, and Other Communicable Diseases.
15) Sleep Disorders: Insomnia, sleep apnea, and inadequate amount of sleep due to various causes.
16) Others: Tiredness, Defective Posture, Headache, Urinary Infection, Congenital Health Problem.
17) Anti Social Problem: Stealing, Lying, Assembling, Cruelty,
18) Habit disorder: thumb sucking, nail biting, bed wetting.
19) Personality Disorders: Jealousy, Irritability, Timidity, Shyness, Daydreaming, Fear and Anxiety.
20) Psychosomatic Complaint: Tremors, Headache, Asthma, Depression, Delusions, Hallucinations.
21) Educational Difficulties:
Being behind in studies, school phobia, school failure.
The collaboration of the child’s teachers, parents and health care personnel is important for timely assessment of this common health problem seen in the child and for its appropriate intervention, so that the child’s condition can be treated timely and it can be prevented from becoming further complicated.
🔸OR🔸
🔸 a. Explain about stages of Demography.
Explain the stages of demography. 06
Demographic Stages:
Demos Means People
Graphene Means the Record.
Demography: The scientific study of human population and its elements ie size, composition and distribution is called demography. Demography means the scientific study of population.
Concept of Demography:
Demography is a branch of science that studies human population with special provision on only three elements.
1) If there is any change in the size of the population i.e. the size increases or decreases.
2) Structure of Population (basic of age and size).
3) Geographical distribution based on state or territory.
There are mainly 5 stages of the demographic cycle.
1) First stage = high stationary stage,
2) Second Stage = Early Expanding,
3)Third Stage = Late Expanding,
4) Fourth Stage = Low Stationery,
5) Fifth Stage = Decline Stage
1) First Stage = High Stationary Stage:
In the high stationary stage there are no changes in the size and composition of the population.
Birth Rate : ↑High
Death Rate : ↑High
Because it has high birth rate and high death rate i.e. both cancel each other and due to this the population remains stationary.
Until the mid-17th century, the world’s population was in this stage, and India was in this stage until the 1920s.
Ex: India in 1920
2) Second Stage = Early Expanding:
In the second stage, early expanding stage, the death rate decreases as the health condition improves and the birth rate remains unchanged.
Birth Rate : ↑Unchanged
Death rate : ↓decline
In the early expanding stage the birth rate does not change but the death rate decreases due to which there is a slight increase in the size of the population.
The world population was in this stage from the middle of the 17th century to the middle of the 19th century. India was in this stage from 1921 to 1950
Ex: South Asia, Africa
3)Third Stage = Late Expanding:
In the third stage, late expanding stage, the death rate declines slightly and the birth rate declines slightly.
Birth rate: ↓slide (slight) decline
Death rate :↓further decline
In the late expanding stage the birth rate declines a little while the death rate declines a little more but because the birth date is a little higher than the death rate, there is population growth.
Ex: China, Singapore and India
4) Fourth Stage = Low Stationery:
In the fourth stage, the low stationary stage, the birth date is low and the birth rate is also low, due to which the population is observed to be stationary (stable).
Birth Rate : ↓low
Death Rate : ↓low
In this stage there is stability in population due to low birth rate and death rate and this is usually seen mainly in developed and industrialized countries.
Australia recorded zero population growth during 1980-1985.
Ex:=Australia in 1980-1985.
5) Fifth Stage = Decline Stage:
In the fifth stage decline stage the birth date is further reduced while the date remains unchanged due to which a decrease in population is seen.
Birth Rate : ↓Further Lo
Death Rate : ↓Unchanged
Thus in this decline stage there is a decrease in population due to the decrease in birth date and death rate which is usually seen in Germany and Hungary.
Ex:= Germany and Hungary.
The demographic cycle helps explain how a population evolves and transitions through different stages of development, affected by socio-economic factors, technological advancement and cultural changes.
b. Describe role of CHN in Family Welfare Programme.
Describe the role of Community Health Nurse in Family Welfare Programme. 07
Role of Community Health Nurse in Family Welfare Programme:
The role of a nurse in a family welfare program is diverse and multifaceted. Nurses play different roles in different settings of family welfare services. It generally depends on their post and their working capacity.
The role of the community health nurse (CHN) in family welfare services is important in promoting reproductive health, family planning and overall well-being in the community.
Here are the key aspects of his role:
1) Survey work:
The nurse collects demographic facts through a survey.
It makes a list of house numbers and their locations in the community.
The nurse collects information from pregnant mothers, ineligible couples, contraceptive users, children and children below school going age through a survey.
Couples are then classified into high, medium and low priority.
To collect reviews about how many couples use contraceptives and how many people do not use them for the formation of further action plans.
2) Health Education:
To provide education about health and family planning to the individual, family, and community.
To make people aware about available family planning services.
Provide education and detailed information about different types of contraceptives to couples so that they can adopt them according to their choice.
Providing education to mothers or athletes to breastfeed their child up to one year because it works as a natural contractile.
To provide education about immunization, nutrition, first aid and personal and environmental hygiene in the community.
3) Coordinator and Provider of Family Welfare Services:
Provision of various types of contraceptives available to ineligible couples.
To arrange family planning clinics and camps to create awareness about people’s needs and available services.
To follow State Government and State Rules and Regulations and to provide direct services within legal and professional limits.
It coordinates the services of Gynecologists and other Family Welfare Services personnel.
4) Magnification function:
Encourages ineligible couples to adopt small family norms by using contraceptives.
Works to explain the need and importance of family planning.
To identify women who need medical termination of pregnancy and refer them to a doctor early.
Establishment of depots for adequate contraceptive supply and distribution in every village due to which adequate supply of contraceptives can be provided.
5) Administrative Role:
Fixing date and location of family planning clinics Arranging equipment, supplies and other resources in clinics.
Supervise and guide multipurpose health workers in clinics and distribute contraceptives and insert and remove IUDs.
To provide assistant to the Medical Officer in conducting the clinic.
Organizing camps for family planning and assisting doctors in male-female and female sterilization operations.
Maintain aseptic technique during operation.
To provide follow up services to couples who have accepted the method of family planning.
Planning and evaluation of education programs.
6) Consultant:
It is important to consult family welfare services as coordinators and direct care providers before starting any type of health care program in the community.
7) Counsellor: The nurse counsels the ineligible couples and the target couple on different contraceptive methods and provides them an opportunity to choose the best suitable method for spacing.
8) Supervisory Role: As a supervisor, the nurse working in the family welfare department encourages her staff to participate actively in the family welfare program.
As a supervisor, the nurse organizes in-service education programs for health workers, professionals, and nursing personnel.
9) Domiciliary Services:
Home visits are an important part of the family program.
These services are provided by multipurpose health workers and health assistants.
In which as services, providing education and upbringing to illegible couples.
If using IUD and pills, provide advice for follow-up and provide education for follow-up in cases of vasectomy, tubectomy, medical termination of pregnancy (MTP).
Providing domiciliary care to antenatal, postnatal, newborn and toddler.
Providing referral services if anyone has post-operative complications.
10) Record Maintenance: The nurse is responsible for maintaining all the records in the family planning program viz.
- Illegible couple records,
•Target couple records, - Intra uterine devices record,
•Sterilization operation record,
Clinic and camp records,
•Health Education Activity Record,
•Training record,
•Medical records etc.
The nurse is responsible for preparing monthly reports and submitting them to the authorities.
11) Role in Research: The Community Health Nurse is a primary member of a multidisciplinary research team. Nurses have to cooperate and participate in research activities of family welfare services.
12) Evaluation Role: The nurse evaluates the work performed in the family welfare program and prepares its reports. On the basis of this evaluation any further changes are made in the implementation of the program and the desirable targets are achieved.
13) Collaborator: A community health nurse works for the improvement of health care services by collaborating with health teachers and non-governmental organizations in the community.
Nurses work collaboratively with doctors, dispensers, vaccinators, train birth attendants, and lady health visitors to provide family welfare services in the community.
Community health nurses play a crucial role in helping individuals and families make informed decisions about their reproductive health, support healthy pregnancy and child birth, and contribute to the overall well-being of the community through effective family welfare programs.
c. Write down advantages and disadvantages of small family.
Write the advantages and disadvantages of small family. 07
Advantages and Disadvantages of Small Family:
Advantages of Small Family
1) Better Financial Stability:
A primary advantage of a small family is that it maintains financial stability. To support fewer children, parents can allocate more financial resources per child. It involves involvement in education, health care services, extracurricular activities, and overall quality of life.
A small family has less expenses compared to a large family due to which more savings, investment, college fund, and better planning for future expenses like retirement can be done.
2) Closer Parent Child Relationship:
In a small family, parents can give each child more individual attention and emotional support. Because of this, a close relationship forms between parents and children and also increases communication between parents and children.
Children from small families may experience less rivalry and competition with siblings for parental attention, thereby developing a strong sense of security and self-esteem in the child.
3) Reduces Environmental Impact:
Small families use less resources and produce less waste than large families.
This makes a positive contribution to environmental sustainability by reducing carbon footprints, energy consumption and overall ecological impact.
4) Imprude Education Opportunity
Parents in small families have more financial resources available to invest in their children’s education. This may include tuition, enrichment programs, tutoring and educational materials for private schools.
Children from small families have better access to educational opportunities and can receive more personalized educational support from parents and teachers.
5) Enhance Career Opportunity and Mobility:
Smaller families have greater flexibility in career choice, job relocation, and professional development opportunities.
Without the constraints of large family responsibilities, parents have more time and energy to focus on advancing their careers.
Due to this flexibility there is also an improvement in job satisfaction and an increase in earning opportunities is also seen due to which a better life is passed out.
6) Healthier Parental Wellbeing:
Parenting fewer children can reduce stress and physical strain on parents, especially mothers. It provides opportunities for good maternal health before, during and after pregnancy.
Multiple pregnancy related challenges are less common in small families. Like risk of maternal complication and child birth.
DISH Advantages of Small Family:
1) Loneliness and Social Isolation:
Children from small families may experience feelings of loneliness or social isolation, especially if there are few playmates or siblings to interact with at home.
Lack of sibling support can affect social skill development and emotional resilience, especially during childhood and adolescence.
2) Limited Family Support System:
Small families have a small network of close relatives and extended family members. This can limit access to family support, options for elder parent care, and emotional connection across multiple generations.
During times of emergency or times of need, small families rely more on external resources and professional services for support.
3) High Expectations and Pressure:
Parents and society have high expectations from children of small families, expecting them to excel academically, socially and professionally. Children may experience additional pressure and stress to meet these expectations.
Children have a tendency to overburden themselves with responsibilities or achievements, potentially affecting their mental health and wellbeing.
4) Economic Burden and Care Giving Responsibility:
In small families parents bear the primary responsibility of care giving, financial support and emotional nurturing without the support of siblings.
This can increase the stress and exhaustion of parents, especially during the challenging phase of raising children.
Financial pressure can increase if unexpected expenses or economic downturns occur, affecting the family’s financial stability and long-term planning.
5) Excessive Physical Features:
If there are fewer children, there is a risk of spoilage of children. Parents compensate for the absence of siblings by giving their children extravagant material goods, special rights or freedoms.
Excessive material wealth can hinder the development of responsibility, self-discipline and resilience in children, affecting their ability to cope with challenges and setbacks later in life.
6) Demographic Imbalance:
At a broader level, the preference for small families can lead to demographic imbalance in society.
Aging populations and declining birth rates in some regions may pose challenges to workforce sustainability, economic growth, and social welfare systems.
Thus, small family has few advantages like,
Financial stability,
Along with these benefits of close parent-child relationships, and low environmental impact, they also present challenges related to social dynamics, parental expectations, and family support systems.
⏩Q-2 Write Short Notes (Any Five) 5×5=25
🔸 a. Elements of Primary Health Care-elements of primary health care
Elements of Primary Health Care:
Primary Health Care
Primary health care is an essential health care that is universally made accessible to everyone and the care should be acceptable through full participation of everyone and primary health care should be affordable to the community and the country. should
The essential 8 elements of primary health care are as follows:
ELEMENTS:
1) E : Ensure safe water supply,
2) L: Control of Locally Endemic Diseases
3) E: Education
4) M: Maternal and Child Health (Immunization Against Infectious Diseases)
5) E: Environmental Sanitation
6) N:Nutrition
7) T : Treatment of minor alignment
8) S: School Health Services.
•>1) E : Ensure safe water supply:
Supply of safe drinking water in adequate amount and sanitation is important for good health and is an important factor of environment.
Access to safe drinking water is important to prevent water borne diseases and promote overall health.
Primary health care includes efforts to ensure that communities have access to clean and safe water sources, which are fundamental to disease prevention and health promotion.
2) L: Control of Locally Endemic Diseases:
The main focus of primary health care is to control any endemic disease in any particular region or community.
It involves surveillance, preventive measures (such as vaccination and vector control) and early detection and treatment of locally prevalent diseases.
Prevention and control of local and endemic diseases to reduce the morbidity rate.
3) E: Education:
Health education is a key component of primary health care.
It aims to empower individuals and communities with the knowledge and skills to make informed decisions about their health.
Education covers a wide range of topics including hygiene practices, nutrition, family planning, sexual health, and prevention of disease.
To provide education to people about health and existing health problems. Some measures are devised to control and prevent these health problems and to make people aware of the health services available to them so that they can be availed when needed.
4) M: Maternal and Child Health (Immunization Against Infectious Diseases):
Mother and child are the most vulnerable group to suffer from health problems and account for a large percentage of the population. Primary health care of mother and child
Places significant emphasis on health services.
This includes prenatal care to ensure healthy development during critical stages of life,
Safe Child Birth,
Properly Post Natal Care,
Newborn Care, Immunization,
Growth monitoring and nutrition are involved.
Protection of mother and child from illness and other risks ensures good health of families and communities.
Immunization Against Infectious Diseases:
Provide proper immunization to the child to protect them from major infectious diseases like,
Poliomyelitis,
diphtheria,
tetanus,
Missals,
tuberculosis,
Hepatitis B.
To provide proper immunization to the child to prevent from infectious conditions like etc.
5) E: Environmental Sanitation:
Environmental sanitation is essential to prevent diseases caused by poor hygiene and environmental conditions.
Improving sanitation in primary health care, properly disposing of waste materials, and providing education for hygienic practices to reduce risks such as communicable diseases in the community.
6) N:Nutrition:
Good nutrition is essential for health and growth and development of the child.
People should be encouraged to focus on a balance diet.
Nutrients are the foundation of primary health care, which addresses both malnutrition and overnutrition as issues.
It involves promotion of balanced diet, micronutrients, supplementation, support breastfeeding, and nutritional counseling to improve health outcomes and prevent nutritional deficiency.
It is necessary to provide knowledge for food preparation and preserving the nutrients present in the diet.
7) T : Treatment of Minor Alignment:
Primary health care provides accessible and timely treatment for common health conditions and minor alignments. Primary health care is provided by trained health care personnel to manage illnesses (such as respiratory infections, diarrhea, skin conditions and minor injuries). And there should be easy availability of drugs.
8) S: School Health Services:
School health services are integrated with primary health care to improve the health and well-being of the school-age child.
These services include screening, immunization, health education sessions, counseling, and referral for further evaluation and treatment when needed.
Thus, total 8 elements are involved in primary health care.
b. Functions of Primary Health Center –
To provide health services in rural areas, the Bhor Committee established a Primary Health Center (PHC) which is a PHC for a population of 30,000 in a plain area while a PHC for a population of 20,000 in a hilly, tribal, and backwater area. Which provides health care services to the people of the community.
The functions of a Primary Health Center (PHC) are as follows:
1) Medical care
2) MCH Services including Family Planning.
3) Safe water supply and basic sanitation.
4) Prevention and Control of Locally Endemic Diseases
5) Collection and Reporting of Vital Statistics.
6) Education about health.
7) National Health Program Establishment and Awareness
8) Referral Services
9) Training of Health Guide, Health Worker, Local Dai and Health Assistant.
10) Basic Laboratory Services.
Description:
1) Medical Care:
Primary health centers provide basic medical care to treat acute and chronic health conditions. It also provides outpatient services through diagnosis, treatment and treatment for minor illnesses and injuries.
PHC medical care is essential to meet the immediate health needs of the community.
In medical care, tablets, injections, dressings, and other treatments are provided to the patients according to their disease, besides preventive, curative, promotional care is provided.
2) MCH (Maternal and Child Health) Services including Family Planning:
Primary health centers provide comprehensive maternal and child health care including prenatal care,
antenatal checkup,
Safe Delivery Services,
Post Natal Care,
And immunization is also provided for the child.
In order to support family planning initiatives,
family planning,
counselling,
contraceptive,
And reproductive health services are provided.
This also includes RCH in Maternal and Child Health which covers maternal reproductive child health to adolescent care.
It explains about mother’s antenatal care, nutrition, hygiene, immunization, and laboratory examination etc.
Regular checkups, observations, and education about family planning are provided in the post-natal period.
3) Safe Water Supply and Basic Sanitation:
A primary health center works to improve public health in the community by providing safe drinking water and sanitation facilities in the community.
Primary Health Centers provide education on sanitation, promoting clean water sources and hygienic practices to prevent water borne diseases and improve the overall health of the community.
Steps are taken to maintain environmental cleanliness by providing education to people about basic sanitation, excreta disposal, and cleanliness of kitchen, garden.
Apart from this, there should be drinking water wells and taps which should be chlorinated for safe water supply.
4) Prevention and Control of Locally Endemic Diseases:
Primary health centers play a crucial role in the prevention, surveillance, and control of locally endemic diseases.
Measures are taken to prevent disease including providing vaccinations, providing treatment for endemic diseases, and monitoring disease trends to prevent outbreaks.
5) Collection and Reporting of Vital Statistics:
Primary Health Centers work to collect and report vital statistics such as birth rate, death rate, and incidence of any disease in a particular community. These collected data are essential for monitoring health trends for health planning, allocation of resources, improvement of health outcomes and prioritization of health interventions.
6) Education About Health:
Primary health centers provide education to individuals and communities about preventive health practices, nutrition, hygiene, sanitation and disease prevention strategies.
The Primary Health Center organizes health education sessions, workshops and seminars to bring about improvement in health conditions.
7) National Health Program Establishment and Awareness:
The Primary Health Center implements the National Health Program and Campaigns whose main aim is,
Targeting specific health issues including, immunization drives,
Campaigns are conducted on disease eradication effects, nutrition supplementation, and health awareness.
They spread awareness about national health priorities and encourage community participation in health initiatives.
Each National Health Program has important functions. The clinic provides services related to the National Health Program such as,
Anemia Control Program,
Malaria, Diarrhea, Leprosy, Immunization, TB Control Program, Supplementary Program Referral of mother in abnormal condition during labor for additional services, refer her to Primary Health Center to Female Health Worker, Auxiliary and Nurse Midwife or Medical Officer.
8) Referral Services:
When a patient requires any specialist medical treatment or requires any specific diagnosis and if its facilities are not available in the primary health center then the primary health center also works to refer the patient.
The primary health center provides immediate referral services as per the patient’s need, due to which the patient’s health condition can be improved and complications can be prevented.
9) Training of Health Guide Health Workers, Local Dais, and Health Assistants.
Primary health centers conduct training programs in which training is provided to community health workers, traditional birth attendants, health assistants, and other health care personnel to improve their skills and knowledge.
The main objective of this training is to promote health, prevention of diseases, maternal and child health, and improving the skills of health care personnel in basic medical care.
10) Basic Laboratory Services:
Primary health centers conduct basic laboratory services in which tests like diagnostic tests, blood tests, microscopic tests, urine tests etc. are performed.
Through all these functions provided by the primary health center, preventive, promotional, curative care is provided to the community due to which the overall health condition of the people of the community can be improved and their well-being can be maintained.
c. Bhore committee –
Introduction:
The Bhor Committee was appointed by the British Government of India in 1943 to survey the present health condition and health organization in India and to make recommendations for its future development and was chaired by Sir Joseph Bhor. He was a pioneer of public health. They met regularly for two years and submitted their report in 1946.
Bhor Committee was established in “1946”. Its founder was “Sir Joseph Bhor”, hence it is called Bhor Committee.
Bhor Committee is known as “Health Survey and Development Committee”.
Recommendation: The committee forwarded a comprehensive proposal for the first time for the development of the National Program of Health Services.
The important recommendations of the Bhor Committee were:
Integration of preventive and curative services at all administrative levels.
Development of Primary Health Center in two stages:
1) Short term measures
2) Long term measures
1) Short Term Measures: To provide a Primary Health Center (PHC) covering a population of 40,000 in each rural area.
In Primary Health Center (PHC),
Doctors : 2,
Public Health Nurse : 4,
Nurse : 1,
Midwife : 4,
Train Dai : 4,
Sanitary Inspector : 2,
Health Assistance : 2,
Pharmacist : 2,
Class IV Employees: 15.
will be administered by
Also Secondary Health Centers are envisaged to provide support to the Primary Health Center (PHC) and to coordinate and supervise its functions.
2) Long Term Measures:
3 million scheme to set up centers (PHCs) with 75 bedded hospitals for every 10,000 and 20,000 population is also called.
Preparation of 650 bed hospital as secondary health unit and 2500 bed hospital at district level.
Major changes to be made in medical education including provision of three months training in preventive and social medicine to prepare social physicians.
Establishment of Village Health Committee for better coordination and support in the development programme.
A District Health Board will be established with representation from the public and District Health Officials.
d. The Controlling measures for STD – STD control measures
Measures to control STD (Sexually Transmitted Diseases): Controlling measures of sexually transmitted diseases involve a combination of strategies aimed at prevention, diagnosis, treatment, and public health interventions.
The following are the controlling measures of Sexually Transmitted Diseases (STD):
1) Preventive Measures: Health Education and Promotion
Awareness:
Sexually Transmitted Diseases (STD) to the public through community outreach, schools, media, and health care facilities.
Providing education on its mode of transmission, and its preventive measures.
Behavioral Intervention: Adopting safer sexual behavior such as using barrier methods of contraceptive methods and reducing the number of sexual partners.
Prevention Program: Comprehensive sexual health education program is implemented in which STD prevention and contraception programs are conducted.
Access to Contraception: Ensuring availability and access to contraceptives can reduce the risk of unintended pregnancy which increases the risk of STD (Sexually Transmitted Disease) transmission.
Vaccination:
HPV (human papillomavirus) vaccine: Promoting and administering the human papillomavirus (HPV) vaccine to prevent HPV infection, which can cause cervical cancer and other genital cancers.
Hepatitis B vaccine: Provide universal vaccination against hepatitis B virus to prevent liver disease and reduce transmission through sexual contact.
2) Screening and Early Detection:
Routine Testing:
Tests for common sexually transmitted diseases including HIV, syphilis, gonorrhea, chlamydia, and human papilloma virus (HPV).
Screening for sexually transmitted diseases regularly as part of comprehensive health visits.
Partner Notification: Encouraging individuals diagnosed with STDs to notify their sexual partners and seek diagnosis and treatment to prevent further transmission.
3) Treatment and Management: Early diagnosis of sexually transmitted disease (STD) and after diagnosis, providing appropriate antibiotic and antiviral medication to cure the infection, relieve symptoms and prevent complications.
Partner Treatment: Proper testing of the sexual partner of a person who has been diagnosed with a sexually transmitted infection (STI) can prevent further infection and transmission and can be used if complications occur.
4) Public Health Interventions:
Surveillance and Monitoring: Monitoring the prevalence and trends of STDs through surveillance systems to inform public health strategies and allocate resources effectively.
Outreach and Testing Program: Implement outreach programs, mobile clinics, and community-based testing initiatives to reach underserved populations and promote testing for STDs.
Contact Tracing: Conduct contact tracing, offer testing and provide counseling and treatment services to identify and notify persons in contact with STDs.
5) Promotion of Vaccine Availability: Promote and implement vaccination programs for preventable STDs like HPV (Human Papillomavirus) and Hepatitis B to reduce the incidence of associated cancer and liver disease.
6) Addressing Social and Behavioral Determinants:
Health Equity: Addressing the social determinants of health such as poverty, stigma, discrimination, and health inequities due to lack of health care facilities that increase the risk of sexually transmitted infections (STIs).
Behavioral Counseling To provide behavioral counseling and support services to empower individuals to adopt safe sexual practices and reduce risk factors.
7) Research and Innovation:
Provide support to research initiatives for the development of new diagnostic tools, treatments, vaccines, and preventive strategies for sexually transmitted diseases.
By implementing these compliant controlling measures, public health authorities, health care providers and communities can effectively reduce the burden of STDs, promote sexual health and improve overall population health outcomes.
🔸 e. Janani Suraksha Yojana –
Public Safety Plan:
Jani Suraksha Yojana (JSY) is a centrally sponsored scheme implemented by the Government of India, its objective is to reduce maternal and neonatal mortality rate by anchoring and promoting institutional deliveries of pregnant women especially women from economically disadvantaged areas.
National Maternal Benefit Scheme which has been modified as a new scheme and made a Jana Sukhara Yojana. It was launched on 12 April 2005.
In which transport facility of 108 ambulances, diet blood transfusion referral transport, and medication are provided with free delivery.
Objective:
The primary aim of JSY (Jan Jani Suraksha Yojana) is to anchor pregnant women for institutional delivery and to ensure that all pregnant women have access to skilled care during child birth.
To reduce the maternal and infant mortality rate by encouraging institutional delivery.
Focusing on institutional care among BPL women.
100% institutional delivery should be done.
Under the National Rural Health Mission (NRHM), case assistants in this program provide free post-partum care during the antenatal period along with delivery.
Reducing Maternal Mortality Rate (MMR) and Infant Mortality Rate (IMR).
Under this scheme, pregnant women deliver in government health services and are provided with cash assistance.
Financial Incentives:
Under the Jani Suraksha Yojana, cash is provided to pregnant women who deliver in health facilities.
The scheme provides financial support to cover costs associated with delivery and encourages women to seek care from trained medical personnel.
In areas where institutional delivery is not possible or accessible, and delivery takes place at home, a cash incentive of Rs. 500.and
For pregnant women delivering at Government Health Services or a recognized provide health facility, cash incentives amounting to Rs. 1,400.
Asha worker is given ₹ 200 under this programme.
Target Beneficiaries: Jani Suraksha Yojana Women from Below the Poverty Line (BPL) and women from Backward Marginalized Areas who do not have access to quality maternal health care services.
4) Components:
Conditional Case Transfer: Women who deliver in a health facility (public or recognized private) are eligible for cash incentives. These incentives help offset costs related to transportation, hospital stay and post-delivery care.
Case Assistant for Delivery: Pregnant women in backward and inaccessible areas where health care facilities are not available are encouraged to seek the presence of skilled attendants during home delivery by providing incentives under the Jan Sankarsha Yojana.
5) Coverage and Implementation: JSY is implemented in all states and Union Territories of India. It is administered by the Ministry of Health and Family Welfare at the national level and by the respective state health department at the state level.
6) Impact: JSY has made a significant contribution to increasing institutional delivery in India, thereby improving access to skilled care during childbirth. This has reduced maternal and newborn mortality by enhancing timely medical intervention and emergency obstetric care.
7) Monitoring and Evaluation:
The plan includes monitoring and evaluation methods to track utilization of services, measure impact indicators such as Maternal Mortality Rate (MMR) and Newborn Mortality Rate (NMR) and assess the effectiveness of cash incentives to promote institutional delivery. happens
Thus, this Jana Suraksha Yojana scheme is formulated to improve institutional delivery and improve maternal and newborn health.
🔸f. Functions of Indian Red Cross Society –
Functions of Indian Red Cross: Indian Red Cross was started in 1920 and has more than 400 branches in India.
Functions of Indian Red Cross:
1) Relief work,
2) Milk and Medical Supplies
3) Care of Sick and Disabled Children
4) Maternal and Child Welfare Services
5) Family Planning,
6) Research,
7) Provide scholarship for nurses to upgrade themselves.
8) Blood bank.
9) Aid to Institutional
10) Junior Red Cross,
11) First Aid and Ambulance Services.
1) Relief work: During natural calamities like flood, drought, earthquake, flood, or war, relief work is done by collecting food and clothes and delivering them to those in need.
It also works during pandemic or epidemic disease.
Arranges workshops for workers during disaster management.
2) Milk and Medical Supply: Provides milk powder and medication to hospitals, maternity homes, children welfare centers, schools and orphanages etc.
3) Care of Sick and Disabled Soldiers: To provide care and first aid to injured, sick and wounded soldiers in battle is the main aim of the Red Cross Society.
4) Maternal and Child Welfare Services: Many centers are available for setting up maternal homes and child centers as well as providing technical advice.
5) Family Planning: Indian Red Cross Society also provides family planning services in which camps are planned and family planning services are provided.
6) Research: Indian Red Cross Society also helps in research activities, it distributes materials for child care and mother care. St.john Ambulance association, it conducts first aid classic training for males and nursing courses for females.
7) Provide Scholarships for Nurses to Upgrade Themselves: It provides scholarships to nurses for further studies. Due to which the nurse can be upgraded.
8)Blood Bank: Indian Red Cross Society runs a first aid service and a blood bank, maintains a list of donors and provides services when required.
9) Aid to Institutional: Provides assistance to Hospital Dispensaries, Maternal Health Care (MCH), Reproductive and Child Health (RCH) Centers, Schools, Orphanages.
10) Junior Red Cross: Junior Red Cross is a children’s branch which gives opportunity to boys and girls to work during epidemics and helps youth to live with a sense of brotherhood and prepare them for first aid service.
11)First Aid and Ambulance Services: It provides first aid services and also provides ambulance services.
12) Health Education:
Health education is provided by Indian Red Cross through posters, pamphlets, slides and films due to which the health related awareness among the people can be improved.
Thus, Indian Red Cross Society plays an important role in providing health services.
🔸g. Causes of Maternal Mortality Rate and Neonatal Mortality Rate –
Causes of Maternal Mortality Rate (MMR) and Neonatal Mortality Rate (NMR):
Maternal Mortality Rate (MMR) and Neonatal Mortality Rate (NMR) are critical indicators of health care system and socio-economic development of a country.
By identifying the causes for the occurrence of these indicators, it is possible to know what effective interventions are needed to improve the condition of maternal and neonatal health.
Causes of Maternal Mortality Rate (MMR)
1) Obstetric Haemorrhage: Antenatal haemorrhage (bleeding before birth) and postpartum haemorrhage (bleeding after child birth) is a major cause of maternal mortality and is usually more prevalent in areas where emergency obstetric care facilities are scarce. Available or unavailable places are more common.
2) Hypertensive disorder: Conditions like preeclampsia and eclampsia during pregnancy in which the blood pressure of the mother increases and seizures are seen in the mother can also increase the maternal mortality rate due to this reason.
3) Infection: Infections like sepsis (infection of blood stream), post partum infection (
4) Obstructed Labour: When there is a condition of prolonged labor i.e. in a condition where the labor process is obstructed, uterine rupture may occur or infection may also occur, then in such a condition, immediate emergency obstetrical care is provided to the mother in an adequate amount of health care facilities in the area. Maternal death may occur due to unavailability.
5) Unsafe Abortion: Maternal death can occur due to complications of unsafe abortion practices in areas where abortion services are unavailable and restricted.
6) Pre-Existing Medical Conditions: Any health-related conditions such as diabetes, heart diseases, and HIV/AIDS can cause complications during pregnancy and child birth and increase the maternal mortality rate. can
7) Lack of Access to Quality Maternal Health Services: Due to limited facilities of skilled birth attendants, emergency obstetrical care, essential medication, and blood transfusion and limited access to the mother, maternal death occurs mainly in rural areas and backward areas due to these causes.
Causes of Neonatal Mortality Rate (NMR):
1) Preterm Birth Complications: A child who is born prematurely (before 37 mix of gestation) may die due to respiratory distress syndrome, infection and other complications.
2) Birth Asphyxia: Oxygen deficiency during birth is called birth asphyxia. Brain death can also occur due to this condition, i.e. if immediate resuscitation and neonatal intensive care is not provided, the child may die.
3) Infection: Due to infection like sepsis, pneumonia, tetanus in neonatal infection, the child gets severe illness due to which the child can die. Particularly when a premature, newborn baby has a compromised immune system.
4) Congenital Anomalies: Any structural and functional abnormality of the child at the time of birth which requires immediate medical intervention can also lead to neonatal death.
5) Neonatal Jaundice:
When a newborn has a severe condition of jaundice, it can lead to complications if not treated immediately.
(Carnicterus: brain damage due to high bilirubin level) can occur which can lead to child death.
6) Nutritional Factors: When the newborn is not provided with the best nutrition in adequate amount and its nutritional requirements are not fully met, the immune system of the child is weakened due to which the child can easily get any infection due to which Newborn may die.
7) Limited Access to Neonatal Health Care Services:
When the Neonatal Intensive Care Unit (NICU), Skilled Neonatal Care Providers, Essential Medication, Essential Medical Equipment, all these services are in inadequate amount, care is not provided to the child immediately and as per his need, neonatal death can also occur.
Thus, conditions like maternal mortality rate and neonatal mortality occur due to all these causes.
🔸 h. Protein Energy Malnutrition –
Definition: Protein Allergy Malnutrition (PEM) is a nutritional problem in a child formerly known as Protein Calorie Malnutrition (PCM) that results from inadequate intake of protein and calories in food, resulting in impaired growth, development and Overall health is impaired
There are two main types of PEM.
1) Marasmus
2) Kwashiorkor
1) Marasmus
Marasmus of PEM is caused by severe calorie deficiency, resulting in weakness, loss of muscle mass, and wasting in body tissues.
Children with marasmus usually appear very thin and have an appearance of a
“Starved”.
2) Kwashiorkor
Kwashiorkor is a form of PEM caused by a deficiency of solid protein, despite adequate caloric intake.
Children who have kwashiorkor have a swollen abdomen (edema), fatty liver, skin lesions, and stunted growth due to water retention. And the child with quasisurecore than marasmus is normal but his body weight is higher.
Classification of protein energy malnutrition.
1) Syndromal classification
There are total five types of syndromal classification.
1) Nutritional Marasmus,
2) Kwashiorkor,
3) Nutritional Dwarfing,
4) Marashmike Kwashiorkor,
5) Pre Kwashiorkor
1) Nutritional Marasmus:
Nutritional marasmus is a severe form of protein energy malnutrition.
In which chronic starvation is seen and the intake of both protein and calories is inadequate.
The condition of nutritional marasmus is mainly when there is extreme poverty, food insecurity, lack of access to nutritious food.
It is seen due to the presence of small amounts in the mother.
2) Kwashiorkor:
Kwashiorkor is a form of PEM caused by a deficiency of solid protein, despite adequate caloric intake.
Children who have kwashiorkor have a swollen abdomen (edema), fatty liver, skin lesions, and stunted growth due to water retention. And the child with quasisurecore than marasmus is normal but his body weight is higher.
3) Nutritional Dwarfing:
Nutritional dwarfing is also called stunted growth and growth retardation.
Nutritional dwarfing is one manifestation of protein allergy malnutrition (PEM) in children. It is a condition where children fail to achieve their expected growth due to inadequate intake of essential nutrients including protein and calories.
Nutritional dwarfing is mainly seen during the period of growth and development of the child such as infancy and early childhood.
In it, the child has skeletal growth delay, short stature,
Delayed puberty, cognitive deficits,
etc. symptoms are seen.
4) Marashmike Kwashiorkor :
Marasmic Kwashiorkor is a protein energy food nutrition in a solid form. It has the combined symptoms of marasmus and quasi-cerebral chorea. This condition of marasmic kwashiorkor is seen mainly when the child has prolonged and severe malnutrition.
And mainly seen due to extreme poverty and food insecurity.
5) Pre Kwashiorkor:
“Pre-kwashiorkor” involves the early stage or warning sign of kwashiorkor, a severe form of protein-energy malnutrition (PEM). It has early symptoms of kwashiorkor.
In prequasiorchor, children may show signs of moderate to severe malnutrition.
1) Marasmus Definition:
Marasmus word comes from the Greek word “marasmos” meaning wasting.
Marasmus in PEM (Protien Energy Malnutrition) is caused by severe calorie deficiency, resulting in weakness, loss of muscle mass and wasting in body tissues and loss of subcutaneous fat.
Children with marasmus usually appear very thin and have a “starved” appearance.
In marasmus, the child loses more than 50% of the expected weight for age.
Etiology:
Due to the innate diet,
Due to inadequate amount of calories in the diet,
Due to poor feeding,
Due to certain medical conditions,
As due to chronic vomiting,
Due to chronic infection,
Ex := Syphilis, Tuberculosis, Upper Respiratory Infection,
Due to certain environmental factors,
Due to poverty,
Marasmus is most commonly seen in infants,
Due to congenital diseases like cleft palate hydrocephalus, Hisprung’s disease etc.
Due to certain metabolic disorders such as galactosemia.
Classification of Marasmus:
There are total 4 classifications according to the grade of marasmus.
1) Grade-1 := In this grade there is loss of fat from axilla and groin area.
2) Grade-2 := In this grade there is loss of fat from axilla and groin area. Also, fat is lost from the abdominal and gluteal regions.
3) Grade-3 := In this grade there is loss of fat from axilla and groin area. Also, fat is lost from the abdominal and gluteal regions. Along with this, the fat of the chest and spine is also involved.
4) Grade-4 := In this grade there is involvement of first three grades along with fat loss of bucklepad.
Symptoms and Signs of Marasmus:
Severe wasting in body tissues,
Subcutaneous fat loss,
Child becomes very thin,
Facial features become suspicious,
Child has growth retardation,
Developmental delay of the child,
Subcutaneous fat loss from a child’s buttock abdomen, Thai.
The face looks like an aged one.
Loss of fat from the child’s cheeks.
Child becomes irritable.
Finding severe malnutrition in the child.
Electrolyte imbalance in the child.
Neurological in Child
Symptoms are observed,
Child becomes less active,
Child’s spleen, gonads,
And reducing the size of the liver,
The child feels weak, tired, and tired.
To observe changes in the child’s behavior,
Decreased physical activity,
Child’s extreme weight loss,
Diagnostic Evaluation:
History taking and physical examination,
x ray,
Taking anthropometric measurements of the child,
Carrying out laboratory investigation of the child,
Complete blood count,
Assay serum electrolyte and serum albumin test,
Performing imaging testing of the child properly,
Management of Child with Marasmus:
Providing adequate nutritional supplements to the child,
Providing adequate high calorie feeding to the child.
Advising the child on nutritious food intake.
Maintaining adequate fluid and electrolyte levels of the child.
Provide adequate ion supplementation to the child.
Giving advice to gradually increase the child’s diet.
If the child has any infection, provide adequate antibiotic medicine.
To provide adequate psychological support to the child.
Daily recording of child no weight.
Advise the child to provide adequate breastfeeding.
Provide nutritious food like green leafy vegetables, soup, banana, pulse, cereals milk etc.
Provide diet to the child in small and quantifiable amounts.
To provide adequate work and comfortable environment to the child.
2) Quasicore Definition:
Quasicore is a form of solid protein energy mal nutrition (PEM). Kwashiorkor is a form of PEM. Which is caused by deficiency of solid protein despite adequate calorie intake.
Children who have kwashiorkor have a swollen abdomen (edema), fatty liver, skin lesions, and stunted growth due to water retention. And the child with quasisurecore than marasmus is normal but his body weight is higher.
Kwashiorkor is also called “Red Hairy Boy”.
Kwashiorkor was first described by British physician Dr. Cicely Williams in 1933. But a particular kwashiorkor tumor was described in 1935.
Quasarcore’s condition is predominantly seen in preschool children.
Symptoms of kwashiorkor include edema of the body due to fluid retention.
Etiology:
Due to poverty,
By providing an inadequate amount of bestfitting to the child,
Due to intake of protein rich food in inadequate amount,
Due to non-availability of protein rich food,
Being of low socio economic status,
Due to faulty feeding habit,
Due to imbalance diet,
Due to not consuming nutritious diet in adequate amount,
Due to certain medical conditions such as chronic infections,
Gastro Intestinal Disorders, etc.
Due to certain metabolic disorders,
Due to environmental factors,
Due to providing adequate weaning diet to the child,
Due to intake of essential vitamins and minerals in inadequate amounts,
Symptoms and signs:
Edema (in pitting ED) is found in the body mainly in lower extremities, upper extremities, abdomen, face etc.
A condition of bloated stomach due to collection of fluid in the abdomen,
Skin becomes dry and scaly,
Muscle wasting and muscle atrophy,
Skin changes such as pigmentation,
Hyperpigmentation, skin roughness, discolouration etc.
Hepatomegaly (liver enlargement) in a child,
Child neapatite decreases,
Observe behavioral changes in the child,
Child’s growth and development deal,
Impaired skeletal growth of the child,
Finding the condition of anemia in the child,
Changes in the child’s hair,
Child should not be interested in any activity,
Muscular wasting is seen in the child,
A child’s face may appear “moon-faced” due to edema.
To observe psychomotor changes in the child,
Finding intellectual impairment in the child,
Diagnostic Evaluation:
History Collection,
Physical Examination,
Anthropometric Measurement,
laboratory test,
Complete blood count test,
Serum albumin test,
Serum Electrolyte Test,
Arterial blood gas analysis,
Medical Management of Kwashiorkor Wada Child:
Providing adequate protein rich diet to the child.
Advise the child for adequate calorie intake.
Advise the child to intake adequate nutritious rich food.
Provide adequate glucose solution if child has hypoglycemic condition.
If the child has anemic condition, treat it properly by blood transfusion.
Giving advice to the child to take proper skin care.
To provide proper play therapy and recreation therapy to the child.
Advise parents of children to provide nutritious rich food to the child.
Provide adequate vitamin A supplements to the child.
If Quasiorcor is in an advanced stage, hospitalize immediately.
Assess the child’s fluid and electrolyte levels properly.
Assessing child’s height, weight, and nutritional status.
Providing proper psychological support to the child.
Nursing Management of Kwashiorkor Wada Child:
To provide properly comprehensive support to the child.
Assessing the child’s proper nutritional status such as breast fitting, weaning, food habit, balance diet, assessing socioeconomic status.
Assess the child’s growth chart properly.
Providing proper nutrition rehabilitation to the child.
Collaborating with other health care personnel for child care.
Advising the parents for adequate nutritious food intake of the child.
Maintain hydration status properly.
Provide properly prescribed medication to the child.
Providing proper psychological support to the child.
To provide complete information to the child’s parents about the causes of the disease, its symptoms and signs, and its treatment.
Providing supplementary feeding to the child.
Antibiotic medicine should be provided if the child has any infection.
Provide adequate vitamins and mineral supplements to the child.
⏩Q-3 (A) Fill in the blanks. 10
1) …….is the scientific study of the human population.
………is to make scientific study of population.
Demography
2) NRHM stands for……
Full Name of NRHM……
NRHM:
National Rural Health Mission (National Rural Health Mission).
3) AIDS day is celebrated on……..
AIDS Day is celebrated on…,….
1st December
4) Community development block covers…….. villages.
The Community Development Department consists of ………villages.
100 villages
5) Causative organism for T.B is…….
The organism responsible for T.B is….
Mycobacterium tuberculosis,
(Mycobacterium tuberculosis).
6) ART treatment is given for …….disease.
ART treatment is given for ……disease
HIV/AIDS (Human Immunodeficiency Virus/Acquired Immunodeficiency Syndrome).
7) In plain area one female health worker covers ……..population.
A female health worker covers ……population in a common area.
1000 populations.
8) BCG vaccine is given by…….. route.
intradermal route
9) One CHC covers about …….population in plain area.
A CHC covers a population of …… in a general area.
120,000 population
10) WHO stands for……
Full Name of WHO….
WHO:=
World Health Organization (World Health Organization).
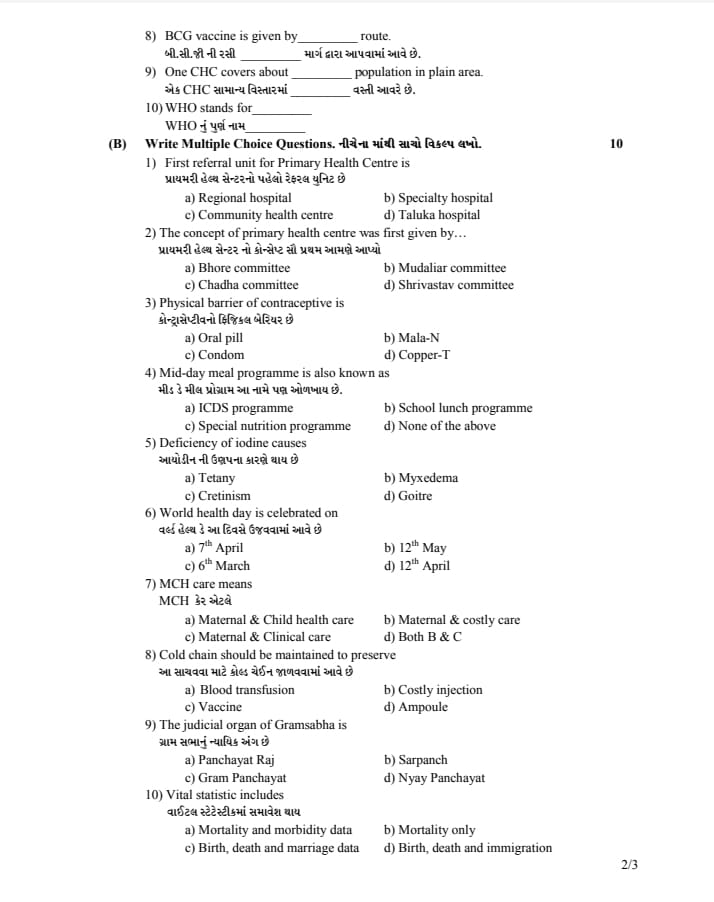
⏩(B) Write Multiple Choice Questions, write the correct option from the following. 10
1) First referral unit for Primary Health Center is – The first referral unit of Primary Health Center is.
a) Regional hospital
b) Specialty hospital
c) Community health center
d) Taluka hospital
2) The concept of primary health center was first given by…
We first gave the concept of Primary Health Center
a) Bhore committee
b) Mudaliar committee
c) Chadha committee
d) Shrivastava committee
3) Physical barrier of contraceptive is – There is a physical barrier of contraceptive
a) Oral pill
b) Mala-N
c) Condom
d) Copper-T
4) Mid-day meal program is also known as-
Mid Day Meal Program is also known by this name.
a) ICDS programme
b) School lunch program
c) Special nutrition program
d) None of the above
5) Deficiency of iodine causes-
Caused by iodine deficiency
a) Tetany
b) Myxedema
c) Cretinism
d) Goitre
6) World health day is celebrated on this day
a) 7th April
b) 12th May
c) 6th March
d) 12th April
7) MCH care means
MCH Care ie
a) Maternal & Child health care
b) Maternal & costly care
c) Maternal & Clinical care
d) Both B & C
8) Cold chain should be maintained to preserve
-A cold chain is maintained to preserve this
a) Blood transfusion
b) Costly injection
c) Vaccine
d) Ampoules
9) The judicial organ of Gramsabha is
a) Panchayat Raj
b) Sarpanch
c) Gram Panchayat
d) Nyay Panchayat
10) Vital statistic includes – Vital statistic includes
a) Mortality and morbidity data
b) Mortality only
c) Birth, death and marriage data
d) Birth, death and immigration
Q:2 (b) Write Multiple Choice Questions:
Q: (1) Ans:
c) Community health center
Q: (2) Ans:
a) Bhore committee
Q: (3) Ans:
c) Condom
Q: (4) Ans:
B) School Lunch Programme.
Q: (5) Ans:
D) Goiter
Q: (6) Ans:
A) 7 th April
Q: (7) Ans:
A) Maternal and Child Health Care
Q: (8) Ans:
c) Vaccine
Q: (9) Ans:
d) Nyay Panchayat
Q: (10) Ans:
c) Birth, death and marriage data.
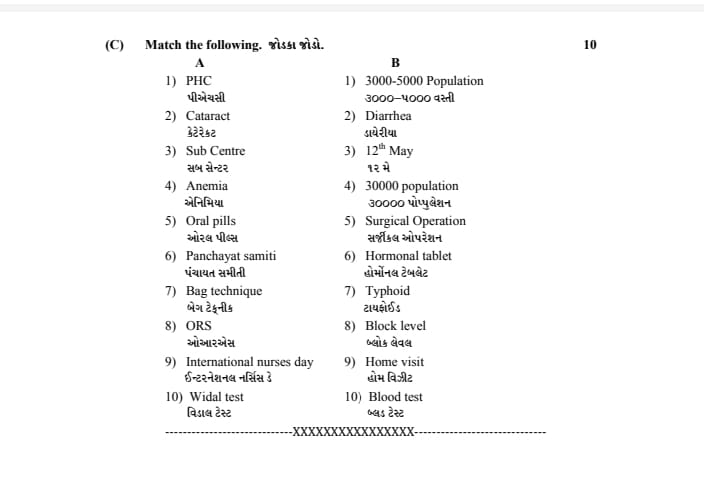
⏩(C) Match the following. Connect the Jodka.10
A B
1) PHC 1) 3000-5000 Population – 3000-5000 Population
2) Cataract- Cataract 2) Diarrhea – Diarrhea
3) Sub Center 3) 12th May
4) Anemia 4) 30000 population
5) Oral pills – Oral pills 5) Surgical Operation- Surgical operation
6) Panchayat samiti 6) Hormonal tablet
7) Bag technique – Bag technique 7) Typhoid – Typhoid
8) ORS- ORS 8) Block level- Block level
9) International nurses day 9) Home visit – Visit International Nurses Day
10) Widal test- Vidal test 10) Blood test – Blood test
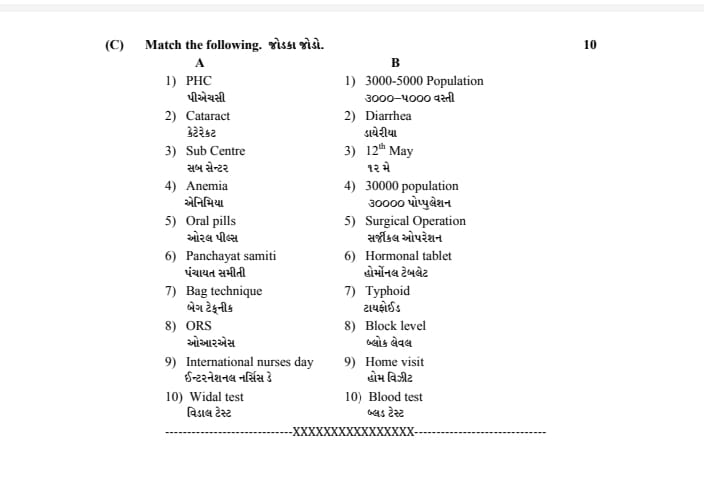
Answer :-
1) 1-4
2) 2-5
3) 3-1
4) 4-10
5) 5-6
6) 6-8
7) 7-9
8) 8-2
9) 9-3
10) 10-7