ENGLISH – PRACTICAL MIDWIFERY GNM MODELS
IMPORTANT MODELS.
- Placenta:
Definition:
The human placenta is ‘discoid’, ‘hemochorial’ and ‘deciduate’. The placenta is attached to the wall of the uterus and provides a connection between mother and fetus via the umbilical cord.
Placenta is a circular disc, spongy, flaky structure, thicker at the center and thin at the corners.
Placenta origin:
Placenta originates from the trophoblastic layer of the fertilized ovum.
It is closely linked with the mother’s circulation and helps the function of the fetus during intrauterine life.
Attachment of placenta:
The placenta is attached to the wall of the uterus and provides a connection between the mother and the fetus through the umbilical cord. It performs many functions and maintains pregnancy.
Development of placenta:
1.fetal component: The fetal side develops from the chorion frondosum.
2.maternal component: It is formed by decidua basalis.
Diameter and thickness of placenta:
1.Diameter : 15-20 cm
2.Thickness: 3 cm
- Weight : 500 g
4.Surface area: 243 sq.cm - Volume : 500 ml
Surface:
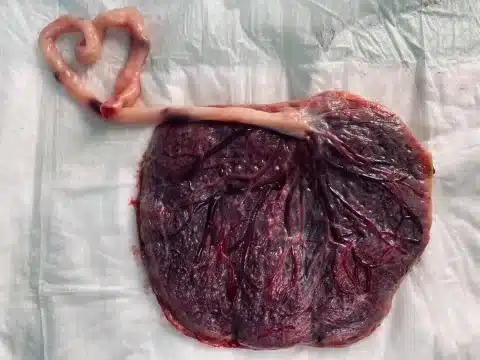
Fetal surface:
Maternal surface
Peripheral margin
1. fetal surface

The fetal surface is smooth and covered with glistening amnion. In its center is the umbilical cord
Umbilical vessels are visible below the amnion.
Amniotic membrane to chorionic
Can be separated from the plate but not from the umbilical cord.
4/5th placenta is of fetal origin.
2.maternal surface
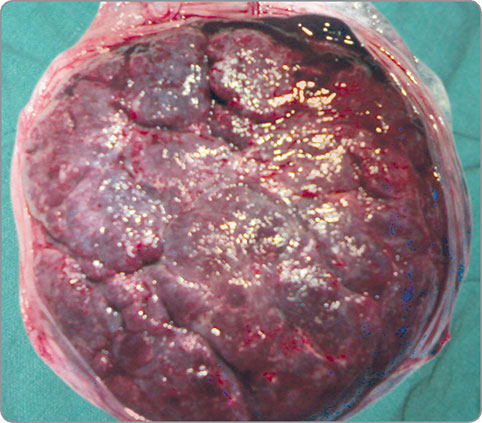
Maternal surface is rough and spongy.
Maternal blood causes its dull red appearance.
It consists of 15 to 20 maternal cotyledons which are separated by sulci.
Many small gray colored sports are visible due to calcium deposition.
Its share is 1/5.
3.peripheral margin
It is formed by the fusion of the basal and chorionic plates
It is continuous with chorion leave and amnion
Attachments
Placenta is attached anteriorly or posteriorly to the upper part of the uterus.
Circulation
1.maternal circulation
2. fetoplacental circulation
1.maternal circulation
Maternal circulation is not fully established until the end of the first trimester.
First theory:
During that trimester, endovascular trophoblasts migrate up the decidual spiral arteries so that maternal blood perfuses into the placental intervelar space.
The second theory:
The tophoblast invades the decidual spiral arteries and forms the trophoblastic plug.
The trophoblastic plug prevents maternal blood flow into the intervillous space until the first trimester.
The plug then loosens and permits maternal blood flow into the continuous intervillous space.
The volume of mature placenta is 500 ml.
Of which 350 ml is in the villi system and 150 ml in the intervillous space.
The blood in the intervillous space is completely replaced three to four times a minute.
The intervalsal space has a pressure of 10 to 15 mmHg during uterine relaxation and 30 to 50 mmHg during uterine contraction.
Blood in maternal sinus remains unclotted by fibrinolytic enzyme.
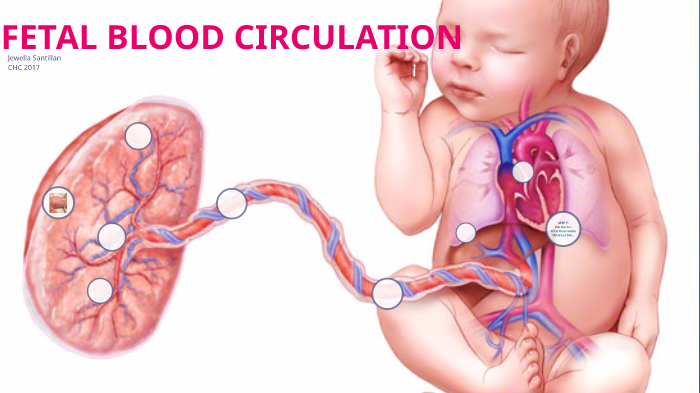
2. fetoplacental circulation
Umbilical arteries carry impure blood from the fetus and supply the placenta.
Arteries divide into small branches and form primary secondary and tertiary vessels.
Blood passes through the terminal capillaries into the venous system.
Due to this, gas exchange takes place between the blood of the mother and the fetus.
Fetal blood moves to the placenta at a minute flow of 400 ml.
Function of placenta
Fetal respiratory function
Fetal alimentary function
Fetal endocrine function
Fetal barrier function
Enzymatic function
Immunological function
Respiratory function
Pulmonary exchange of gas does not occur during intrauterine life. Fetal respiratory function is by simple diffusion.
Oxygen travels from the placenta through the umbilical cord to the fetus by diffusion.
Fetal alimentary function
All nutrients such as glucose, amino acids, lipids, vitamins, water and electrolytes pass through the maternal sinus into the fetal circulation.
Glucose is transferred by facilitated diffusion.
Fatty acids and triglycerides are freely transported.
Cholesterol is made by the fetus.
Water soluble vitamins are actively transported.
Fat soluble vitamins are slowly transported.
Water and electrolytes cross by simple diffusion.
Minerals such as ions calcium and phosphorus are actively transported.
fetal endocrine function
The main job of the placenta is to produce hormones that maintain the pregnancy.
Placenta acts as an additional endocrine gland.
It produces protein hormone and steroidal hormone.
A. protein hormone
1.human chorionic gonadotrophin
It is produced from the cytotrophoblastic layer.
2. human placental lectogen
It is also produced by the placental.
Through it, the metabolic process takes place during pregnancy.
B. steroidal hormones
1. Progesterone
It is produced by the placenta.
It maintains the pregnancy.
Progesterone levels drop during labor.
2. Estrogen
It is produced in large amounts during pregnancy.
Estrogen also maintains pregnancy.
fetal barrier function
Fital membrane performs a protective function.
It protects the body from many harmful agents.
It does not allow substances of large molecular size to reach the fetus.
At the end of pregnancy, small antibodies can reach the fetus.
Protects the fetus from some harmful substances like tubercle bacilli, poliomyelitis virus etc.
enzymatic function
Many placental enzymes are involved in hormone synthesis and metabolism.
such as oxytocin.
immunological function
Placenta is an allograft for the uterus.
However, no graft rejection is observed in pregnancy.
Umbilical cord and its abnormality :-
➡️ Definition :
Umbilical cord which is also called fenus is the structure between the placenta and the fetus. Through the umbilical cord blood and nutrition from the placenta gets to the fetus. And West exits. It extends from the fetal surface of the placenta to the umbilicus of the fetus.
➡️ Characteristics
- Its length is 30 to 90 cm. Its average length is 55 cm. It is found in blues white color.
Its diameter is found to be 1-2.5 cm. It is seen bending from left to right.
It varies in thickness. Swelling and nodules are present. This swelling is due to dilatation of umbilical vein and collection of Wharton’s jelly.
Due to this swelling there are false knots.
Initially, the umbilical cord has two atria and two veins. A vein disappears during 10 weeks of fetal growth.
At birth, one vein and two atria are found inside the umbilical cord.
➡️ development of umbilical cord (development of umbilical cord):
Umbilical cord develops from the body stock of mesodermal tissue. which lies between the embryonic disc and the chorion.
Umbilical cord develops from vitelline duct, allantois and body stock.
Following are the important structures seen in the development of Umbilical Code.
Yolk and its yolk sac:
Yokeshake is a small yellow body. It is an extra-embryonic membrane. It provides nutrition to the developing embryo.
It disappears in later stages.
Allantois
It is an extra-embryonic membrane that originates from the hindgut. It is a blind tubular structure that excretes the nitrogenous waste of the embryo.
The allantois acts as the urinary bladder.
➡️ Structural of umbilical cord
Surrounding Epithelium:
umbilical cord from a single layer of amniotic epithelium
➡️ Structural of umbilical cord
Surrounding Epithelium:
The umbilical cord is covered by a single layer of amniotic epithelium.
Wharton’s Jelly:
It is a gelatinous substance. Its function is to protect the umbilical cord.
It is made of connective tissue and covered by amnion
It contains cells that contain genes for stem cells.
- Blood vessels :
Initially there are two arteries and two veins. But one of them vanishes. Two Atari and one Ven are seen at birth.
These arteries and veins supply oxygen and nutrition and remove waste products.
➡️ Function of umbilical cord:
It acts as a life line between the placenta and the fetus, supplying oxygen and nutrients and removing waste products.
It circulates electrolytes between the amniotic fluid and the umbilical vessels
There are no pain receptors inside Umbilical cord so no pain is felt when cutting it 4.Umbilical cord creates emotional and physical connection between mother and fetus.
Abnormalities of umbilical cord:
short code
long cord
true knot
false knot
Loop of cord
Single umbilical artery
A small amount of Wharton’s Jelly
✅ 1. Short cord
Generally the length of the cod is found between 30 to 90 cm but in this the length falls below 30 cm.
Absence of umbilical cord is called acodia.
A short coda predisposes to placental abruption and uterine inversion.
✅ 2. Long cord
It has a length of more than 100 cm.
Its length is more than 300 cm
A long code can cause knots to develop and code prolapse.
This long code covers the fetus and fetal distress is observed.
✅ 3. true knot
It is seen in 1% cases.
Usually seen in mono amniotic twins.
✅ 4. false knot
It is seen due to tumor in the vessels and problems in development. Also seen due to collection of Vartonus jelly.
✅ 5. Loop of umbilical cord
In it the cod is seen coiled around the fetus.
A loop around the neck (21%)
Two loops around the neck (3.5%)
Three loops around the neck (0.2%)
✅ 6. Single umbilical artery
It occurs in 1% of cases. It is more common in twins and in diabetic mothers.
It occurs due to congenital malformations of the fetus.
It causes obesity and prematurity as well as perinatal mortality.
UTERUS
Uterus is a muscular organ that receives the fertilized oocyte and provides a suitable environment for the development of the fetus
Uterus is a hollow pyriform, guava (guava) shape muscular organ.
The main function of the uterus is to accept the fertilized ovum that implants in the endometrium and receive nourishment from it.
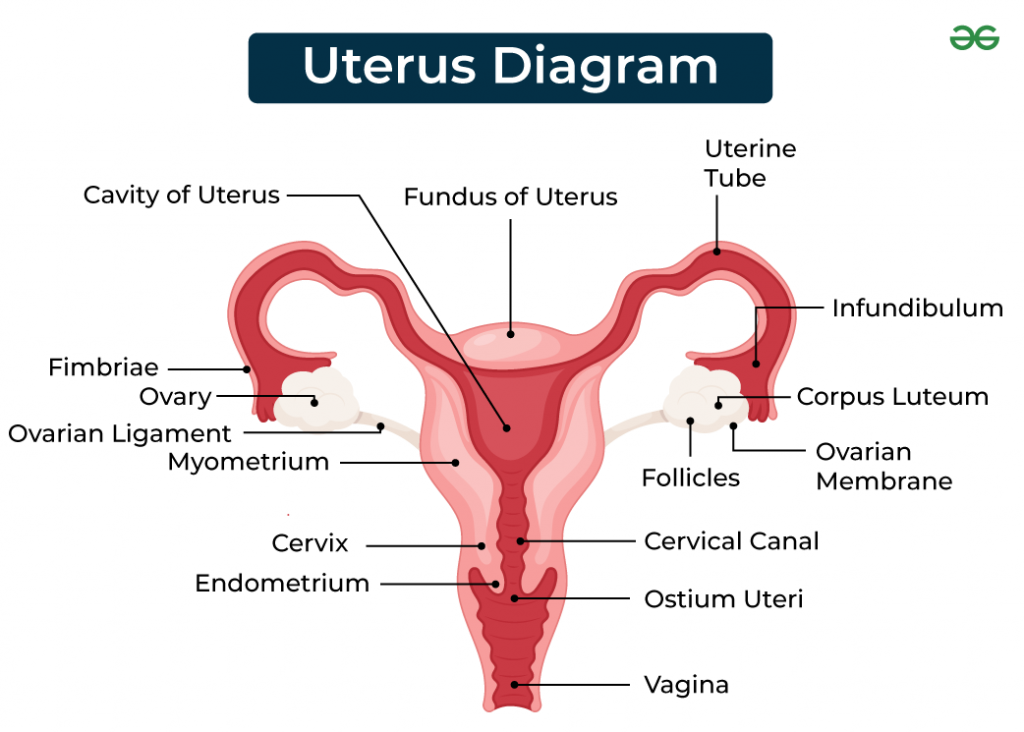
POSITION
The two positions of Uterus are as follows:
(1) anteverted
(2) anteflexed
(1) Anteverted : It is bent forward over the bladder at about right angles to the vagina
(2) anteflexed: slightly bent forward at the internal os between the corpus and the cervix
Uterus lies in front of the urinary bladder and behind the rectum
STRUCTURE:
length of uterus: 7.5-8cm
width of uterus: 5 cm
thickness of uterine wall: 2.5cm
Weight of uterus: 50-80gm
PARTS OF UTERUS:
- body or corpus
2.cervix - body or corpus
- It is the upper five centimeters of the uterus
-The dome-shaped part of the uterus that lies above the attachment of the fallopian tubes is called the fundus.
-The part of the body of the uterus from which fallopian tube or uterus
The tube enters is called cornue
The isthmus is the lower 0.5 cm portion above the internal os that forms the lower uterine segment after the first trimester.
- Cervix:
Cervix is a 2.5cm. It protrudes into the vaja yana
The part of the cervix which is above the vagina is called the supra vaginal portion and the part below the vagina is called the infra vaginal portion.
-Internal os is a narrow opening between the isthmus and cervix and external os is a small round opening at the lower end of the cervix.
LAYERS OF UTERUS:
There are 3 layers in the wall of uterus from outside to inside ward
Perimetrium
Myometrium
Endometrium
- Perimetrium: It is the outermost layer
It is made up of connective tissue and serous membrane and covers the uterus - Myometrium: It is the middle layer, it contains smooth muscle tissue, it contracts during labor and helps to expel the fetus.
- Endometrium: It is the innermost layer, it contains granular tissue and blood vessels, it is thick during menstrual cycle and prepares for embryo implantation.
RELATIONS:
-Anterior: utero vesicle pouch and urinary bladder
-posterior: recto uterine pouch and rectum
-Lateral: broad ligament, uterine tube and ovaries
-superior: intestine
-inferior: vagina
function of uterus and cervix:
The uterus is responsible for periodic menstrual bleeding until menopause
Provides canal for sperm transmission to fallopian tube
Bearing of pregnancy
Nutrients and oxygen are supplied to the fetus through the placenta
At the time of birth, it expels the fetus from the uterine cavity into the external environment
During pregnancy Cervical mucus prevents ascending infection
Cervical mucus helps in sperm transplantation
During labor cervical canaI dilates to fit us to deliver
helps
➡️ Blood supply:
-uterine artery
-ovarian artery
➡️ blood drain: corresponding vein
➡️ lymphatic drainage:
Internal iliac gland and other pelvic lymph gland
➡️ position deviation of uterus:
Anteversion: A condition in which the entire uterus is far forward
Retroversion: A condition in which the entire uterus is tipped backwards
Ante flexion: It is a condition in which the body of the uterus bends sharply near the junction of the cervix
Retroflexion: It is a condition in which the body of the uterus bends just above the cervix.
➡️ Disorders and conditions
-Various disorders and conditions are affected to the uterus.
-1 uterine fibroids: tumor of uterine muscles
-2 endometriosis: growth of endometrial tissue outside the uterus
-3 adenomyosis: thickening of the uterine wall
-4 uterine prolapse: descent of uterus into vagina
-4 uterine cancer: including endometrial cancer and cervical cancer.
Overall, the uterus is the vital organ of the female reproductive system, which plays an essential role in menstruation, pregnancy and childbirth.
FETAL SKULL
INTRODUCTION
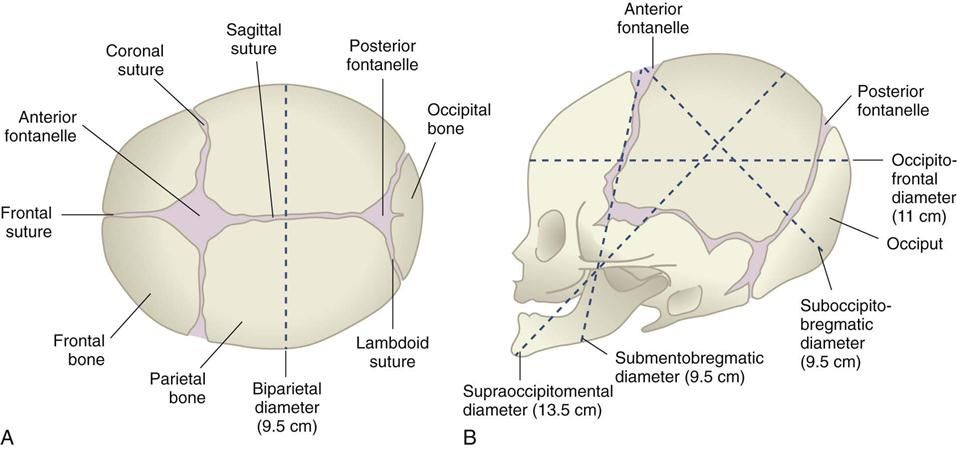
-Fetal skull is the skeletal structure of an unborn baby.
- Some types of changes are seen during delivery.
-It gradually gives shaping to brain and facial features to grow inside.
-Made up of many bones including the frontal, parietal, temporal, and occipital bones as well as smaller bones such as the sphenoid and ethmoid.
-These bones are connected to each other by flexible joints called sutures.
-And which helps the Head in compression and some moments during child birth. Within the femoral skull are two soft frontanelles.
-After birth it gets fused.
AREAS OF THE SKULL
The fetal skull is divided into several zones of obstetrical importance.
Vertex
Bro face
“Vertex” – It is a quadrangular area bounded anteriorly by a coronal suture in Bragg. Posterior lambda n lambdoid suture .Laterally by two parietal eminences.
“Brow”—one side bounded by the coronal suture and anterior frontanal and the other side by the root of the nose and supraorbital.
“Facial”- area is the side bounded by the root of the nose and the supraorbital ridge. While on the other side it is bounded by the junction of mouth and neck.
REGION OF SKULL
- The fetal skull is divided into six regions.
-Volt
- Base
-Face
-Vertex - the occiput
-sensiput
-Or Bro
Vault “-Vault is made up of two parietal bones the upper part of the occiput and the frontal bone and this is the upper most compressible part of a large dome shape.
“Base”-This is the lowest part providing protection of vital center like medulla.And it is made up of united bone.
The “face” is the area formed by the root of the nose and the junction of the chin with the neck.
“Vertex” – anterior fontanelle It is bounded anteriorly by the anterior, laterally by the two parietal eminences and posteriorly by the posterior fontanelle.
The “occiput”_area is the posterior side formed by the posterior fontanelle and the foramen magnum.
“Cinci put and brow”- This area is bounded anteriorly by the orbital, posteriorly by the coronal suture and manly within this is the phonetal bone.
SUTURES AND FONTANELLE
👉SUTURES
Sagittal or longitudinal suture: It lies between two parietal bones.
Coronal suture: It lies between two parietal and frontal bones.
Frontal suture: Located between two frontal bones.
Squamous suture: It is located between two parietal and two temporal bones.
Significance.
Helps the bones overlap and mold during labor and helps the head to engage and internal rotate and mold.
FONTANELLS
There is a wide gap between two sutures called fontanelles. Fontanelles are spaces made up of non ossified membrane. They form when two or more sutures come together.
There are many types of suture main six types.
Two of them are used in obstetrical meanings.
- Anterior fontanelle
2.Posterior fontanelle - Sphenoid fontanelle
- Ethmoid fontanelle
5.Two- Mastoid fontanelle.
ANTERIOR FONTANELLE (bregma)
1.The fontanelle is connected and formed on four sides
(A) Anteriorly: frontal suture
(B) Posteriorly: sagittal suture
(C) Laterally or either side: coronal suture.
2.Shape of anterior fontanelle :Diamond (♦) shape
3.Measurement of anterior fontanelle:
A. Anteroposterior diameter: 4cm
B. Transverse diameter: 2.5cm
- When does the interior fontanelle close: 18-month.
Significance
Anterior fontanelle is important for reasons such as:
1.To perform a rough internal examination and check the degree of flexion of the head.
- Second for molding of the head.
- How much is the intracranial pressure. If the fontanel is depressed then dehydration and if elevated then the intracranial pressure is high.
In rare cases, withdraw cerebrospinal fluid from there and check it up
Sometimes blood collection is also done from there for blood transfusion.
Examination of anterior fontanelle
Fontanel feels soft.
Fantanel should not be congested and should not be bulging.
A crack or crack sound when auscultating the photo indicates a malformation.
If there is a crack pot sound, it indicates increased intracranial pressure, which means there are chances of hydrocephalus.
Causes of abnormal anterior fontanelle
Some of the causes of abnormal fontanel are given below.
causes of bulging fontanelle.
crying, coughing or vomiting.
Increased icp
hydrocephalus
Meningitis, encephalitis
trauma
intracranial hemorrhage
dermoid tumors of the scalp.
causes of sunken fontanel :
Decreased icp, diarrhoea
causes of large fontanelle:
Congenital hypothyroidism
Trisomy 21 (down syndrome)
Rickets
Achondroplasia
Increase icp.
POSTERIOR FONTANELLE (Lambda)
This fontanelle is formed by the junction of three canals.
Lambdoid suture is wide laterally and laterally.
The shape is a triangle shape.
Its measurement is 1.2 x 1.2 centimeters
Confirmation time is 6 to 8 weeks.
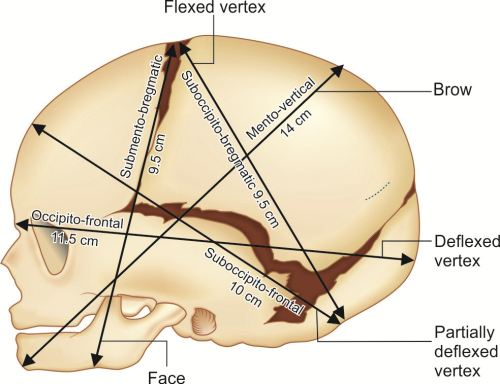
DIAMETER OF SKULL
Sub occipito bregmatic (9.5cm): From the nape of the neck of the occiput to the center of the bag.
suboccipito frontal(10cm): From the nape of the neck to the occiput and the center of the sinus.
Occipito frontal (11.5cm): From the occipital eminence and to the root of the nose.
mento vertical (14cm) to mid point of chin and highest point of sagittal.
Submento vertical (11.5cm): It is the junction of the floor mouth and neck and the highest point of the sagittal suture.
Submento bregmatic (9.5cm) : It extends from the junction of the mouth and neck to the center of the bregma.
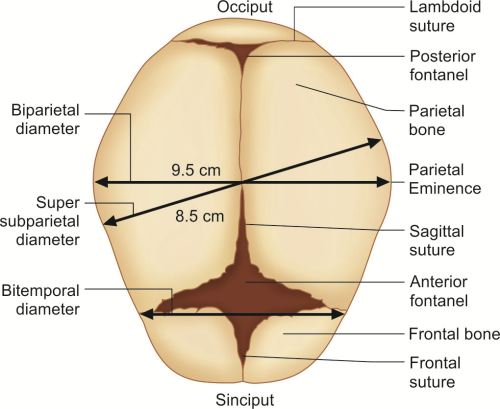
TRANSVERSE DIAMETER
Biparietal diameter (9.5cm)
This diameter lies between the two parietal bones. Engagement is considered to have occurred when the head position is within this diameter.
Super subparietal (8.5cm)
The highest point of the parietal bone of one side and the lowest point of the parietal bone of one side lie between them.
Bitemporal diameter (8.2cm)
This diameter extends to the anterior inferior end of the coronal suture.
Bi_ Mastoid diameter (7.5cm)
This diameter is the distance between the two mastoid processes.
Copper-t:-
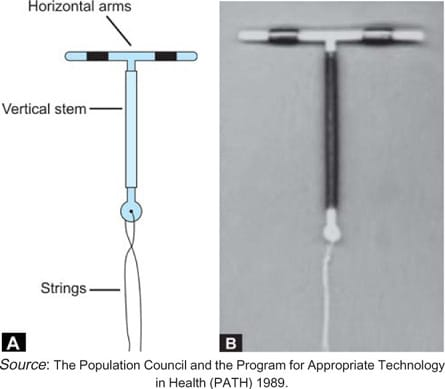
Definition:-
➡️Copper-t is a 2nd generation intrauterine device and it is a small t-shaped device which is inserted in the uterus.
Copper reduces fertility.
➡️It is used for contraception & family planning.
Parts:-
1) T-shaped plastic frame
2) horizontal stem
3) vertical stem
4) copper wires
5) thread
Types:-
1) CuT 200B
2)Multiload 250
3) Multiload 375
4) CuT 380A
1)CuT 200B:-
➡️The vertical stem of this device has copper wire in 215 sq mm surface area and contains 120mg copper.
➡️Lifespan: 4 years.
2)Multiload 250:-
➡️It has copper wire in 250 sq mm surface area.
➡️It releases 60-100 micro gram copper per day.
➡️Lifespan:- 3 years
3)CuT 380A:-
➡️It covers 380 sq mm surface area.
➡️ vertical stem contains 176mg & horizontal stem contains 66.5mg copper.
➡️Lifespan:- 10 years
➡️It is mostly used.
4)Multiload 375:-
➡️It covers 375 sq mm surface area.
➡️Lifespan:-5 years.
Mode of Action:-
1) Biochemical & Histological changes in Endometrium.
2) Increases tubal motility.
3) Impairs sperm descent.
4) Prevent implantation of blastocyst.
Indication:-
1) Normal menstrual cycle.
2) No history of pelvic inflammatory diseases.
3) Contraceptive misuse.
4) Failed coitus interrupts.
Contraindication:-
1) Prolapse uterus
2) severe dysmenorrhea
3) Presence of pelvic inflammatory diseases
4) Dysfunctional uterine bleeding
5) Ectopic pregnancy
6) Nullipara
7) HIV & AIDS
Time of Insertion:-
➡️Interval
➡️Post abortion
➡️Post partum
➡️Post placenta delivery
Methods of Insertion:-
1) Preliminaries:-
➡️History taking.
➡️examination.
➡️consent.
➡️Remove the device from the sealed packet.
➡️Fold the thread, vertical stem & horizontal stem with the vertical stem.
➡️Now the device is ready to introduce.
2)Actual Steps:-
➡️Ask the patient to empty the bladder & then give lithotomy position.
➡️Uterine size & position to be checked.
➡️Introduce posterior vaginal speculum & clean vagina and cervix with antiseptic solution.
Grasp the anterior lip of cervix with Allis forceps.
➡️Uterine sound should be passed through cervical canal and the length of uterine cavity & position of uterus should be noted.
➡️ Then introduce the device of the size of the uterine cavity length.
Indication for Removal:-
1) Persistent excessive uterine bleeding
2) Perforation of uterus
3) flaring up of salpingitis
4) Pregnancy
5) missing thread
Complication:-
- Cramp like pain
-Partial or complete perforation
-abnormal menstrual bleeding
-pelvic infection
-spontaneous expulsion - Perforation of uterus
Advantage:-
➡️Effective Contraceptive.
Fertility can be restored.
➡️inexpensive & easy to use.
➡️No need for constant supervision.
➡️Free from harmful effects.
Disadvantage:-
➡️pain
➡️bleeding
Ectopic pregnancy
➡️spontaneous expulsion
➡️pelvic infection
➡️perforation of uterus
Condom
Male condom:

-It is made of thin latex or plastic.
- It covers the penis before the sexual act.
- Before the contact of vajaina, male has to wear kare.
-Withdraw semen after ejaculation without spilling it - It works as a barrier, it does not allow contact of semen in the female so that sexually transmitted diseases can be prevented.
-Use of condom with spermicidal jelly before intercourse increases its effectiveness.
Advantages:
be easily found,
Inexpensive & safe,
Easy to use,
No side effects,
Sexually transmitted diseases can be prevented,
Light, compact and disposable,
Disadvantages
Breaks or slips during intercourse.
Female condom:
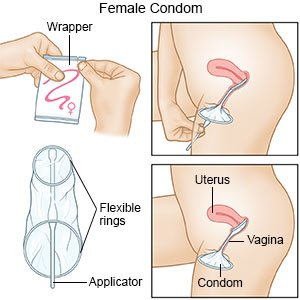
-It is a pouch made of polyurethane with an internal ring that covers the cervix and an external ring that covers the vagina.
It is an effective barrier to prevent sexually transmitted diseases.
Failure rate: 13%
Mechanism of labor
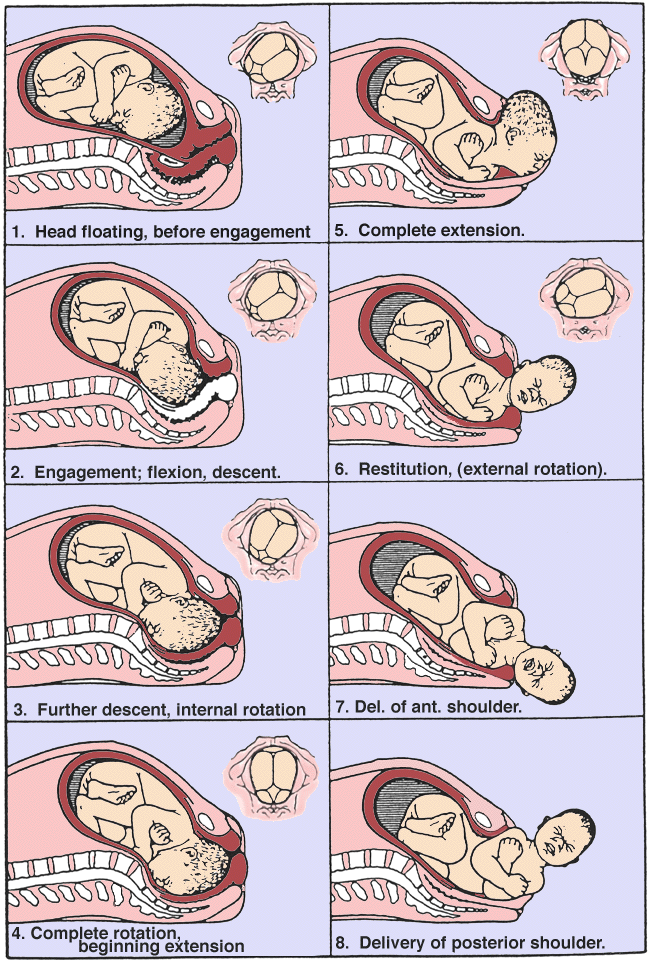
This is a type of process in which the adopted fetus exits through the birth canal through a series of movements called mechanism of labor or normal labor.
The most common RoA ane LOA position of the head in normal labor is the most common transverse diameter and to a lesser extent the oblique diameter.
Lie. -longitudinal
Presentation vertex Denominator occiput
Attitude flexion
Position RoA, LoA
1) engagement
2) decent and flexion
3) internal rotation of head
4) crowning
5) extension of head
6) Restitution
7) external rotation of head
8) Lateral flexion of body (delivery of shoulder and trunk
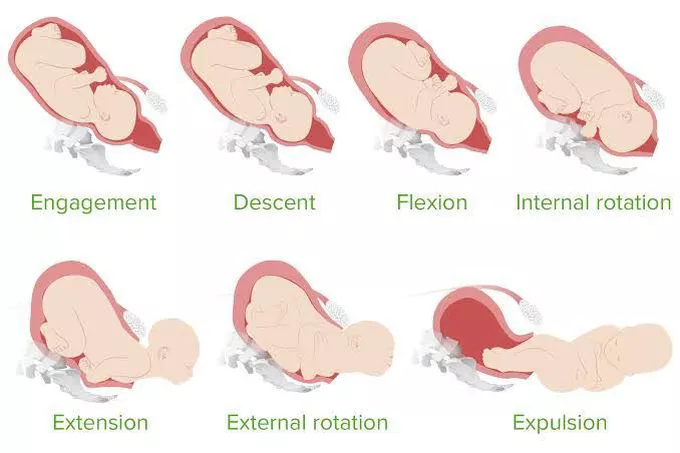
(1) Engagement
In primary gravida, engagement occurs before the onset of labor; in multipara, engagement occurs in early labor or after the onset of labor.
In case of LOA position, the occiput is found near a left iliopectineal eminence and the sinciput is found near the right sacroiliac joint.
The sagittal suture in the maternal pelvis corresponds to the right oblique diameter
Transverse diameter which by parietal 9.5 cm and suboccipito bagmatic both are equal and engagement is seen.
2). Decent and flexion
This is a continuous process in which the head of the fetus is continuously decent.
The process of descent keeps the fetal head continuously descending through contraction and retraction.
Continue the process of descent until the fetul emerges
_factor affecting descent
1) Uterine contraction and retraction
2) bearing down effort
(3) internal rotation
In the pelvic floor, the occiput rotates about 1/8 of a circle and forms an angle of 45 degrees and lies anterior to the pelvic arch.
In LOA the occiput rotates 1/8 circle to the left side from the midline and in RoA the occiput rotates 1/8 circle to the right side from the midline.
(4) crowning
After internal rotation the sub occiput descends below the pubic arch and by parital diameter the vulval outlet is stretched and the head exits by contraction which is called crowning.
(5) extension of head
Delivery of head is followed by extension of head
(6) Restitution
Restitution is the visible passive moment in which the moment of the head is observed and the untwisting neck is observed.
Restitution rotates 1/8 circle in opposition to inter internal rotation
(7) External rotation of head or internal rotation of shoulder
In external rotation the moment of the head is visible in the external location and internal shoulder rotation is seen.
In external rotation, the head performs a movement in the direction of 1/8 circle restitution.
LOA rotates into the left side maternal thigh and RoA rotates into the right side maternal thigh.
(8) Lateral flexion of the body
In lateral flexion the shoulder is positioned on the interior shoulder below the symphysis pubis and exits through anterior shoulder flexion then exits the posterior shoulder.
The body protrudes through lateral flexion.
FEMALE PELVIS
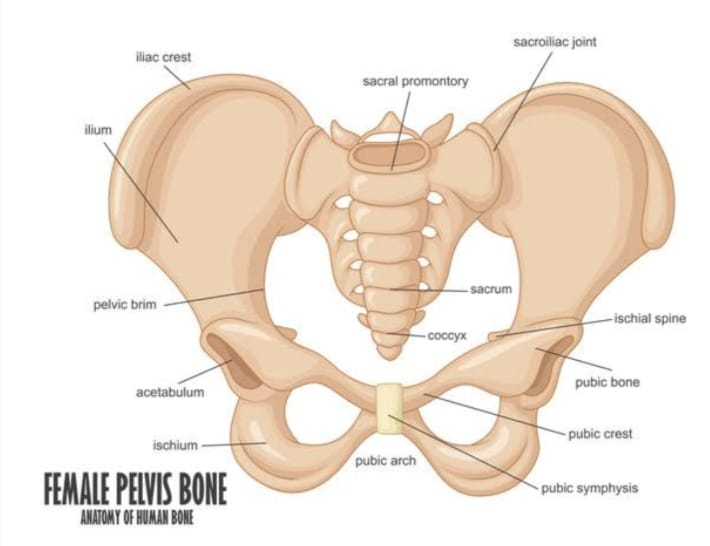
➡️ introduction
▪️Pelvis is a structure of basin sep. It supports the spinal column and protects the abdominal organs.
➡️ Function of pelvis
1) Pelvis helps in body movement.
2) Pelvis helps woman in walking, running and sitting.
3) Woman pelvis has a rounder brim as compared to male pelvis so it helps in child bearing.
4) The pelvis protects the reproductive organs like the rectum and bladder.
➡️ Bones of the pelvis :-
▪️Pelvis is made up of four bones. In which there are two innominate bones. They are made up of three bones each.
1) ilium
2) ischium
3) pubis
➡️ The bones of pelvis are :-
1) Two innominate bones
2) One sacrum (5 fused vertebrae)
3) One coccyx ( 4 fissed vertebrae )
➡️ A) Innominate bones :-
▪️ Ilium is the large outside part. The internal surface inside the ilium is called iliac fossa.
▪️Curved upper border is called iliac crest.
▪️There is a bony prominence in front of the iliac crest which is called the anterior superior iliac spine and below it is called the anterior inferior iliac spine.
▪️Two similar points at the end of iliac crest are called posterior superior and posterior inferior iliac spines.
▪️The ischium forms part of the acetabulum and the thick lower part is called the ischial tuberosity.
▪️The projection behind and above the tuberosity is called ischial spine.
▪️pubis is a small bone which has a body and two projections called superior ramus and inferior ramus.
▪️Two pubic bones meet at symphysis pubis.
▪️Two inferior rami form the apex of the pubic arch. Obturator foramen and form the anterior boundary of the subpubic arch.
➡️ B) Sacrum:
▪️sacrum is a wedge shaped bone which is made up of five fused vertebrae, the first prominent upper border is called sacral promontory. It is an important pelvic landmark.
▪️smooth concave anterior surface is called hollow of sacrum and its side area is called alae or wings of sacrum.
▪️The posterior surface of the sacrum is roughened so that it gives attachment to the muscle.
There are four foramina in the sacrum through which the sacral nerve passes.
➡️ C) Coccyx :
▪️Coccyx is the lower part of the spine. The coccyx is a small triangular shape bone which is formed by fusion of four vertebrae.
▪️Coccyx ligament, deep muscle of pelvic floor and provides attachment to muscle fibers of anal sphincter.
⬛ The pelvis is divided into two parts.
1)True pelvis
2) False pelvis
➡️ False pelvis:
False pelvis is called greater or pelvis major. False pelvis is seen above the pelvic brim. The false pelvis is formed by the upper flat out portion of the iliac bone and protects the abdominal organs. The false pelvis has no obstetrical significance.
➡️ True pelvis :
▪️True pelvis is called lesser or pelvis minor. This bony canal passes through fetus. True pelvis is seen below and behind the pelvis brim.
▪️Sacrum behind it, ischium bone on the side and pubic bone on the front makes a solid ring of bone. It makes brim, cavity and outlet.
➡️ Joints and ligament of pelvis & perineum
Pelvis makes four joints.
1) Two sacroiliac joint :
▪️This is the strongest joint that joins sacrum to ilium.
2) One sacrococcygeal joint :
▪️This joint is formed between the sacrum and the coccyx, in which the base of the coccyx joins with the tip of the sacrum.
3) One symphysis pubis :
▪️Cartilage pad is located between the junction of two pubic bones.
➡️ Ligaments:
Ligaments that hold the joint of the pelvis together. Important ligaments are given below.
1) Sacroiliac ligament
2) sacrospinous ligament
3) sacrotuberous ligament
4) symphysis pubis ligament
5) sacrococcygeal ligament
➡️ Diameter of the pelvic cavity:
▪️Cavity is of circular shape. Cavity is above the brim and below the outlet.
▪️Anterior wall of pelvic bone is made of pubic bone and symphysis pubis whose depth is 4 cm.
▪️Posterior wall is formed by the curve of sacrum whose length is 12 cm.
▪️The diameter of the pelvic cavity is similar in the direction of the brim which is 12 cm.
Diameter of pelvic outlet:
➡️ Anterior posterior diameter
▪️Anterior posterior diameter from sacrococcygeal joint to lower border of symphysis pubis is 13 cm.
➡️ Oblique diameter
▪️Oblique diameter is from sacrospinous ligament to obturator foramen, which is 12 cm.
➡️ Transverse diameter
▪️The diameter between two ischial spine is called transverse diameter which is 11 cm.
➡️ False pelvis
▪️The part above the pelvic brim is called false pelvis. It has no obstetrics significance.
➡️ Important landmarks of pelvis:
▪️Certain points in the pelvic brim are called landmarks. The landmark is as follows.
1) sacral promontory
2) ala or wing of the sacrum
3) Sacroiliac joint
4) Iliopectineal line
5) Iliopectineal eminence
6) symphysis pubis
7) pubic crest
8) Pubic tubercle
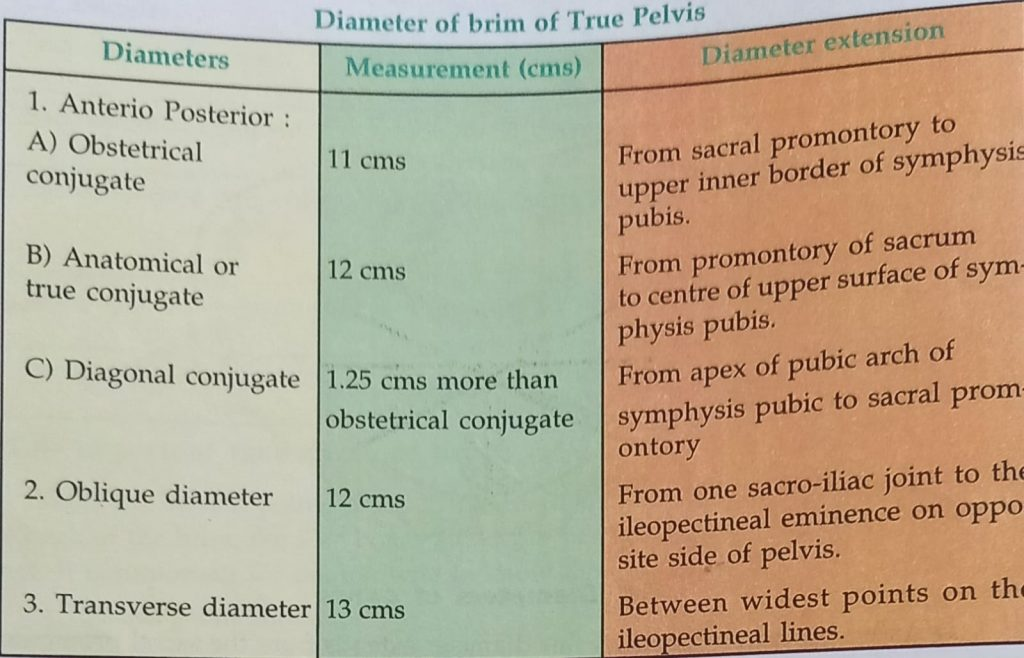
➡️ Diameters of the pelvis:
1)True pelvis
2) False pelvis
Diameters of brim :
1) true pelvis
Diameters are expressed as
▪️Anterior posterior
▪️Oblique diameter
▪️Transverse diameter