ENGLISH General Nursing & Midwifery (Second Year) CHILD HELATH NURSING 04/07/2023 (PAPER 6)
GNC CHILD HEALTH NURSUNG DATE: 04/07/2023
⏩Q-1 🔸a) Define Hydrocephalus. Define hydrocephalus. (03)
- Hydrocephalus is a Greek word with hydro meaning “water” and cephalus meaning “head”. Hydrocephalus is an abnormal condition in which there is an abnormal accumulation of cerebrospinal fluid in the ventricular system and subarachnoid space. The pressure increases.
- This condition of hydrocephalus usually results from an imbalance in the production and absorption of cerebrospinal fluid due to obstruction in the CSF pathway. Due to this, dilatation of the cerebral ventricles, enlargement of the head, cognitive impairment, seizures and other neurological problems are seen.
🔸b) Write the clinical manifestations of Hydrocephalus. (04)
- Accumulation of cerebrospinal fluid in the ventricles of the brain.
- Excessive enlargement of the head.
- To become a sine skull.
- Separation of cranial sutures due to head enlargement.
- Fontanels are bulging, scalp is singed and veins are dilated.
- Percussion of the skull produces a “cracked pot” resonance (Macewen’s sign).
- See the sunset sign (sclera visible above the iris).
- His face looks small compared to his head.
- Increased intracranial pressure.
- Having hemiplegia.
- Cry is hoarseness.
- Often occurring in papilloae.
- Spasticity occurs.
- Ataxia.
- Urinary incontinence.
- Progressive deterioration of mental function.
- Nozia.
- Vomiting.
- Restlessness.
- Irritability.
- Irregular and decreased respiration.
- The pulse will decrease.
- Having a convulsion.
- feeling tired
- Stupor and coma.
- Head one.
- Lethargy.
- from the app.
- Changes in personality.
- Irritability.
- Confusion.
- Visual problem.
🔸c) Describe the nursing management of client with Hydrocephalus. (05)
- Preoperative nursing management
- Properly and continuously assess the child including baseline health status, vital signs, neurological status and hydration status of the child.
- Continuously monitor the child’s intracranial pressure.
- Continuously measure the child’s head circumference.
- Palpate the child’s fontanelles to assess for any increased intracranial pressure.
- Assess the child’s pupillary response and level of consciousness.
- To continuously monitor the child’s vital signs.
- To provide proper work and quiet environment to the child.
- Maintain aseptic technique while handling the child to prevent nosocomial infection.
- Changing the child’s position continuously.
- To properly maintain the child’s nutritional status.
- Provide intravenous fluid to the child properly.
- Keeping the child Nil Per Oral (Nil Per Oral).
- Continuously monitor child’s intake output chart.
- To properly collaborate with other health care personnel for proper care of the child.
- Surgery is a stressful condition for the child and its family members, so proper education and psychological support should be provided to the child’s parents.
- To provide proper assurance and emotional support to the parents of the child.
Post operative management
- Monitoring the child continuously and closely after the surgery.
- To monitor the child’s vital signs frequently every fifteen to twenty minutes.
- Properly monitoring the neurological status of the child.
- Monitoring the child frequently if there is an alteration in body temperature.
- Position the child at the non-operative site to prevent pressure on the shunt.
- After surgery, the child is usually provided with a flat position on the bed for 24 hours.
- Assess the child’s photoreceptors to immediately notice if depressed.
- If the child is in pain, provide analgesic medication to relieve it.
- Do this if the child has any complications after the surgery or not.
Provide proper fluid to the child and maintain his hydration status. To continuously monitor the intake output chart of the child. And continuously maintain the child’s electrolyte level.
Provide dressing to the child by maintaining proper aseptic technique on the surgical side.
To provide proper support and education to the child and his family members.
🔸 OR🔸
🔸a) Define Nephrotic Syndrome (03)
- Nephrotic syndrome is a combination of two words.
- Nephron Meaning Basic Structure of Kidney.
A syndrome meaning a group of symptoms.
Nephrotic syndrome in children is a kidney disorder in which protein is excreted from the body through urine, mainly albumin, due to damage to the glomeruli, which are the filtering units of the kidney, or due to increased permeability of the glomeruli.
Due to the excretion of protein from the body through this urine, the amount of protein in the blood decreases, due to which the condition of edema occurs in the heel (swelling) particularly around the ice, ankle and abdomen. Because of this, the lipid and cholesterol levels in the blood also increase.
Nephrotic symptoms are a collection of symptoms that occur primarily due to damage to the glomeruli in the kidney.
Four symptoms are mainly seen in nephrotic syndrome.
- 1) Body excretion of high levels of protein in urine (proteinuria).
- 2) Decreasing amount of protein in blood. (Hypoalbuminemia).
- 3) Increased amount of lipids in the blood (hyperlipidemia).
- 4) Swelling in body part (in heels).
These four main symptoms are seen in nephrotic syndrome.
Nephrotic syndrome affects people of all ages.
In children, it is mainly seen in children of 1 to 7 years.
🔸b) Write the clinical manifestations of Nephrotic Syndrome. (04)
- Swelling.
- Weight gain in the child.
- Swelling is mainly seen on the lining of the eye socket and around the eye (in the periorbital AD).
- Swelling is mainly seen in feet and ankles due to prolonged sitting or standing.
- The face is puffy.
- Proteinuria.
- Hypoalbuminemia.
- Hypercholesterolemia.
- Diarrhea.
- Vomiting.
- Anorexia.
- Liver enlargement.
- Blood pressure increases.
- Anemia.
- Infection of respiratory tract, peritoneum and skin.
- Skin is pale.
- Skeletal muscle wasting.
- Sometimes swelling is also seen in the wall body which is called Anasarka.
- ascites,
- pitting edema,
- Oliguria (decrease in urine output).
- Weight gain.
- Hematuria (blood in urine)
- Respiratory distress.
- Blood pressure increases.
- Kidney failure.
- Cholesterol level increases in the body.
- feeling tired
- Accumulation in the body
- Getting infected immediately.
- Loss of appetite.
- feeling tired
🔸c) Describe the nursing management of client with Nephrotic (05)
- Proper assessment of the child.
- To monitor the child’s vital signs.
- Monitoring the child’s fluid balance.
- Monitor the child’s weight regularly.
- Monitoring child’s intake output chart.
- Elevate the extremities if the child has a condition of edema.
- If the child has a condition of edema, then diuretic medicine and fluid level monitoring.
- Continuous maintenance of nutritional status of child.
- Advise the child to avoid protein, salt.
- Provide proper medication to the child.
- To provide complete information to the child’s parents about the disease condition, its causes, symptoms and signs and diagnostic evaluation.
- Advise the child’s parents to maintain personal hygiene to prevent infection.
- Providing emotional support to the child’s parents.
- To maintain a proper interpersonal relationship (IPR) with the child’s parents.
- To provide complete education to the child’s family members.
- To clear all the doubts of the child and his family members.
- Encouraging the child to participate in different play activities.
- To monitor the child’s vital signs frequently.
- Providing properly prescribed medication to the child.
- Continuous monitoring of the amount of fluid intake by the child or the amount of intravenous fluid provided to the child.
- Providing a nutritious diet to the child.
- Advise the child to take small frequent feedings.
- Provide education to parents to provide sodium restricted diet to child.
- Provide supplementary vitamins and iron to the child properly.
- Giving advice to the parents of the child or taking regular follow up.
⏩ Q-2 🔸a) Define growth and development. Write down the factors influencing on growth and development. (08 )
- Growth and development depends on many factors. All these factors play an important role in promoting or inhibiting growth directly or indirectly. If all these factors are positively affecting then the growth and development is good and normal. If there are any kind of problems related to these factors then problems are seen in growth and development.
Types of growth and development are as follows.
Biological growth.
It includes height, weight, head circumference, chest circumference etc.
Motor development.
Which includes gross motor and fine motor development.
Sensory Development.
This development is seen due to the sensory stimulation coming from the sensory organs like skin, eye, ear etc.
Factors affecting growth and development mainly include hereditary factors and environmental factors which are described in detail below.
Hereditary factors.
It is also called genetic factor. Which is the main factor affecting growth and development. Different types of characteristics seen in a child like height, body structure, hair and eye color, skin color, all these factors are seen according to the genetic inheritance received from the parents, that is why the children of tall mothers and fathers are usually tall enough. .
Similarly, hereditary or genetic factor, if there is any defective genetic structure in the mother father, it can also produce any type of defect or disease in the children. Genetic diseases like thalassemia, down syndrome, hemophilia etc. are also seen in children from mother father.
Thus, if a normal genetic structure is transmitted from mother to father, the growth and development remains normal, if a defective genetic structure is transmitted, then there is an interruption in its growth and development due to a disease or illness.
A male child or a female child is born due to the sex of the child i.e. caste at the time of conception in the hereditary or genetic structure. Because of this, the characteristics of growth and development are different in both. As a boy child will have more weight at birth and further his body structure growth is more than that of a female child. Similarly, a female child has lesser growth characteristics than a male child but a female child attains maturity and development earlier than a boy child. This difference is also seen due to hereditary factor.
Due to heredity, different patterns of growth and development are seen in different children according to their nation and race. Like the people of one country are different from the people of another country in terms of height, body structure, skin color, intelligence etc.
Thus, many changes are seen in growth and development due to hereditary factors.
Environmental factors.
These are important factors affecting growth and development. Which includes the following factors.
- Antenatal Environmental Factors.
- Postnatal Environmental Factors.
Antenatal Environmental Factors.
The period from conception to the birth of the baby, when the fetus is in the mother’s uterus, is called the antenatal period. During this period, many factors related to the mother are responsible for positively and negatively affecting the growth and development of the child in the uterus. If these factors positively affect the mother, then the growth and development of the child in the womb is better. Similarly, due to the negative effect of this factor, the growth and development of the mother’s child is seen to be defective. These factors are as follows.
A. Infectious Conditions and Illnesses of Mother.
Any type of infection or communicable disease or illness of the mother during the antenatal period can adversely affect the growth and development of her micro-organism fetus through the placenta. Due to this infection the baby may be born with congenital anomaly or infection. Which hinders its further growth and development.
B. Maternal mal nutrition.
During the antenatal period, the growth of the child in the uterus is hindered due to the mother not getting enough nutritious diet and due to anemia and nutritional deficiency in the mother. Due to which many problems related to preterm delivery, low birth weight and growth and development are seen in the child.
C. Maternal substance abuse.
During the antenatal period, the mother consumes any type of harmful substance such as tobacco, alcohol, drugs etc. due to its direct side effects on the fetus in the uterus, and its growth and development is disturbed.
Apart from this, the use of any type of medicine without prescription by the mother during this period may also cause congenital problems in the child due to the harmful effects of that medicine, and its growth and development is altered.
D. Hormonal imbalance of mother.
Due to hypo or hyper secretion of any hormone in the mother during the antenatal period, congenital problems can occur in the child. Due to hormonal disturbances in the mother, its side effects are also seen on the intra-uterine growth and development of the children. For example, if a mother has hypothyroidism, her child may have congenital hypothyroidism or growth retardation.
E. Other Maternal Factors.
Other important causes such as reproductive tracks or abnormality such as uterus deformity, placenta’s emotional disturbances, and inadequate. Development found on
All the above factors affect the growth and development of the child during the antenatal period.
Postnatal Environmental Factors.
After the delivery of the mother, the baby arrives in the extra-uterine environment. During this period the following factors affecting the growth and development of the child are seen.
A. Birth condition.
- If the weight of the child is normal at the time of birth, the chances of its growth and development being normal later on increases. Apart from this, if the weight of the child is less than normal at the time of birth, then due to many problems related to infection and adjustment, this low weight child is likely to have defective growth and development going forward. So the birth condition in which the child has any congenital anomaly at the time of birth or whether the child has any congenital infection is very important.
B. Nutrition.
- After the birth of the child, if the nutritional requirement of the child is fulfilled, the growth and development of the child is seen to be normal. For this the baby should get exclusive breast feeding for six months after birth. Then a weaning diet should be started and should include adequate amounts of protein, carbohydrates, vitamins and minerals. If a child does not get the nutritional supplements mentioned above, its growth and development is found to be defective. Along with this, many nutritional deficiency disorders can also be seen.
C. Childhood Illness.
- If the child has been hospitalized due to any kind of illness or disease during the childhood period, it also affects the growth and development parameters of the child. Apart from this, if there is an acute illness, it does not affect the child much, but if the child has chronic inflammation and frequent hospitalization, then problems in growth and development can be seen.
D. Physical Environment.
- The growth and development of the child is affected due to factors such as the condition of the child’s house, the condition around the house, cleanliness, pure water supply, ventilation, safety around the house etc.
E. Psycho – Social and Cultural Factors.
- Psychological factors include child’s mother-father relationship, love and affection of every member of the household, healthy and happy family environment etc. affect the positive growth and development of the child. Broken family, unhealthy family member relationship, lack of love, affection and security, stress and inappropriate environment among family members all these factors have a bad effect on the growth and development of the child.
- A child’s siblings, society’s neighbors and the surrounding environment and school environment can also have both positive and negative effects on a child’s growth and development.
- The growth and development of the child is also affected due to the culture, habits, traditional belief and education, job and economic condition of the family members of the child’s mother and father.
- Apart from this, the birth order of the child is also a very important factor. In which the first child gets love and affection very well in the beginning and is given more importance. Then he gets attention for the new child in the family and the first child is neglected. So the birth order of the child is also an important factor for growth and development.
F. Seasonal Change.
- In some seasons the growth of the child is seen well and in some seasons the increase in height or length of the child is seen well. The season affects the growth and development of the child.
G. Recreation and Exercise.
- Physical activity and exercise in children promotes their growth and development and is very important for healthy growth and development of children.
H. Other Factors.
- The intelligence of the child, the balance of the hormones in his body, the child’s behavior and his adjustment capacity etc. are also important factors affecting the growth and development.
- Due to the positive influence of all the above factors, the growth and development of the child is promoted and due to its negative influence, the growth and development of the child is stopped or there is an alteration in it.
🔸b) Write down about baby friendly hospital initiative. (04)
BFHI is promoted by WHO and UNICEF for the promotion, protection and support of breastfeeding.
The main aim for this is to provide exclusive breast feeding to the child till six months and continuous breast feeding as complementary feeding till the child turns two years old.
A baby friendly hospital should formulate a policy for successful breastfeeding promotion of breastfeeding. The policy should work for the promotion of exclusive breast feeding of the child by the hospital staff and the mother. whose steps should be in return. These steps are as follows.
The hospital should have a return (written) for B F HIV and every staff should be aware of it.
All staff working in the hospital should be aware of this policy and should be trained to implement this policy.
According to this policy every expectant mother should be given full information about the advantages of breast feeding and breast feeding.
Mother should be assisted to breast feed the baby within half an hour after birth.
All aspects of best fitting should be explained to the mother and education should be given to the mother to maintain lactation.
The mother should be explained that her child should not be given any food or water except the best milk for a period of six months.
According to this policy, the practice of mother staying with the child continuously i.e. complete mother and child stay together is called rooming in. This practice should be promoted.
The mother should be persuaded to give breast feeding only when the child is in demand.
The baby should not be given any artificial pacifiers for breast feeding.
The mother should be matched with a breastfeeding support group and arrangements should be made for such members to meet the mother during discharge.
🔸 OR🔸
🔸a) List down common behavioral problems in children and write down the nursing responsibilities in behavioral disorder of children. (08)
Behavioral problems are defined as patterns of disruptive behavior in children that are unusual for the child’s age and developmental stage and that are continuous over time.
This type of behavior interferes with the child’s ability to function effectively in social, academic, and family settings. Behavioral problems cause difficulties in managing emotions, following rules, communicating properly with other people, and controlling impulses.
This issue can arise due to biological, psychological, social and environmental factors.
Following are the common behavioral problems seen in children.
- Enuresis
- Breath holding spell
- Child abuse
- Failure to Thrive
- Nail biting
- Thumb shucking
- Somnabulism
- Ticks
- Pica
- Anorexia Nervosa and Bulimia Nervosa
- Juvenile delinquency
- Childhood obesity etc.
Role of Pediatric Nurse in Addressing Behavioral Problems:
- The pediatric nurse plays an important role in managing behavioral problems seen in children such as:
Assessment:
- Identifying the main causes of behavioral problems in the child through observation and collaboration with the child’s parents and other health care professionals.
Education:
- Providing proper guidance to parents and caregivers on effective behavior management techniques and strategies.
Interview:
- Implementing behavioral interventions and therapeutic approaches such as,
- Positive reinforcement, time out strategies, and behavioral modification plans etc.
Support:
- Providing emotional support to both the child and his family members to help them cope with the challenges of managing behavioral problems.
Referral:
- Provide referrals of the child to specialists such as child psychologists, psychiatrists, or counselors for further evaluation and treatment when necessary.
- Advocate for the child’s needs in a variety of settings, including school and community programs, to ensure the child receives appropriate supports and accommodations.
- Effective management of behavioral problems in pediatric nursing requires a comprehensive and multidisciplinary approach that fulfills the unique needs of each child and their family.
🔸b) Write the advantages of breast feeding. (04)
- Breastfeeding develops a psychological bond between mother and baby.
- Human milk is available for the baby only as per the body temperature requirement.
- Milk is fresh and sterile and free from contamination directly into the baby’s mouth.
- Human milk is ideal if it is readily available.
- Breast milk is a safe and protective food.
There is perfect food for infants. - Meets the total nutrient requirement of the baby for the first six months.
- It is very important for the baby’s brain growth because breast milk contains high amounts of lactose and galactose.
- Breast milk contains vitamins, minerals, electrolytes and water which are essential for the maturation of the infant’s intestinal system.
- Breast milk provides a facility that increases the absorption of calcium so that the baby’s bone growth is good.
- Breast milk is easily digested.
- Breast milk contains all the essential nutrients that a baby needs.
- Breast milk protects the baby from infection and deficiency.
Breast milk is already prepared.
Breast feeding is a method of family planning, breast feeding is a natural contraception that has a major effect on population for developing countries. - It prevents children from diarrhea and also has laxative action.
- Breast feeding has no dangerous allergic effects.
- Breast feeding can save time and money and energy.
- Breast feeding helps in building a healthy relationship between mother and child.
- Chances of conception decrease during lactation.
- Best feeding helps in involution of uterus (i.e. bringing uterus to pre-pregnant state).
- Breast feeding reduces the chances of sunstroke, gastrointestinal infections and ectopic eczema.
And the chances of scurvy and rickets are also reduced. - Breast feeding reduces the chances of breast cancer.
- Breast milk contains IgA and IgM macrophages, lymphocytes, lysosomes, etc. due to which diarrhea and acute respiratory infections can be prevented in babies.
And prevents against malaria and viral and bacterial infections.
- Breast milk protects against conversion, hypocalcemia, tetanus, deficiency of vitamin E and zinc.
- Exclusive breast feeding can prevent malnutrition in children.
- Breast feeding increases the intelligence of the baby, and gives the baby a sense of security (due to the infant-mother bond).
- The chances of illness in the child are reduced.
- Breast feeding reduces the chances of postpartum hemorrhage (excessive bleeding from the genital tract after delivery).
- Chances of ovarian cancer are also reduced.
- Helps in reducing the excess fat that is stored in the mother during pregnancy.
⏩ Q-3 Write short answer (any two) (6+6=12)
🔸a) Write down fundamental rights of children –
The rights of children were declared by the United Nations on 20 November 1959. The purpose of which was to meet the special needs of the children.
In India too, these rights have been implemented for the all-over development of the child. These rights of children are as follows.
Right to Name and Nationality
Right to free education
A right to grow in an atmosphere of love and affection
Right to be protected against any form of neglect, exploitation, trafficking, etc
Right to get basic benefits like nutrition, housing, medical care etc
Right to opportunities for play and recreation
Right to Special Treatment, Special Education and Appropriate Care for Handicapped Children
Right to first protection and relief during times of disaster
The right to be brought up in an environment of freedom and dignity and the right to live as a useful member of society
Right to be brought up in a society with a sense of mutual brotherhood and peace
Every child has the right to enjoy all the above rights without any discrimination of color, sex, religion or caste.
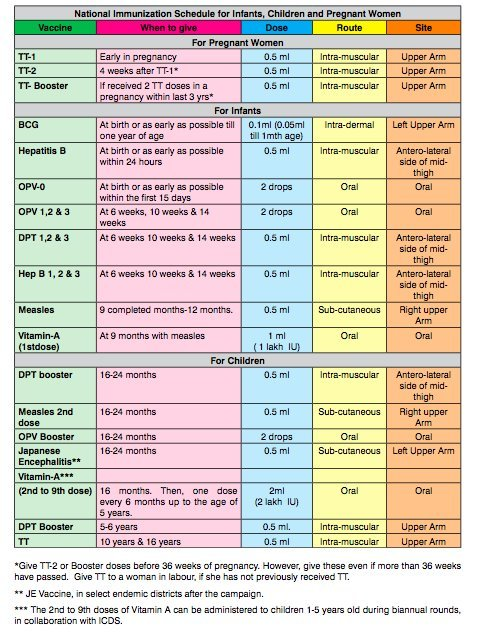
🔸b) Recent national immunization schedule –
🔸c) Tetrology of fallots –
Tetralogy of Fallot is a congenital heart defect. In which four heart defects are seen simultaneously in the child.
1) Ventricular septal defect,
2) pulmonary stenosis,
3)overriding aorta,
4) Right ventricular hypertrophy.
••>
1) Ventricular septal defect,
In a ventricular septal defect, an abnormal opening is present in the septum separating the right and left ventricles.
2) pulmonary stenosis,
In pulmonary stenosis, there is a narrowing of the pulmonary artery (the blood vessel that carries deoxygenated blood from the right ventricle to the lungs) that obstructs blood flow from the right ventricle.
3) Overriding of aorta,
Overriding of aorta is a condition in which normally the aorta (the main blood vessel that carries and transports oxygenated blood from the heart to the wall body) originates from the left ventricle of the heart but overriding of the aorta in the aorta over the left ventricles. On the side, the origin is directly above the ventricular septal defect
4) Right ventricular hypertrophy.
When the pulmonary artery (the blood vessel that carries deoxygenated blood from the right ventricle and delivers blood to the lungs for oxygenation in the lungs) narrows and stenoses, the heart’s right ventricle contracts to deliver blood from the right ventricle to the lungs. There is a need to do extra work (pumping) because of this extra pumping, the muscles of the right ventricle of the heart become thickened which is called hypertrophy.
Explain the Etiology/cause of the Tetralogy of Fallot
- Due to genetic factors,
- Due to environmental factors during pregnancy like,
- maternal age,
- Maternal health conditions such as diabetes.
- Due to the mother coming in contact with certain types of toxic substances during pregnancy.
- Due to certain medications taken by the mother during pregnancy.
- Due to improper nutrition intake by the mother during pregnancy.
- Due to chromosomal abnormalities.
- Due to failure of proper heart development during intrauterine life of fetus.
Explain the Clinical manifestation/ Sign and symptoms of the Tetralogy of Fallot.
- Cyanosis is seen,
- Bluish discoloration of lips, skin and nails,
- Shortness of breath,
- go clubbing,
- feel tired,
- Growth is poor,
- Breathing difficulty,
- Abnormal murmur sounds,
- Irritability,
- dyspnea,
- Episodes of cyanotic spell (tet spell) in which the child has cyanosis, hypoxia and breathing difficulties after feeding and after any painful procedure.
- polycythemia,
- The child’s skin is rough and clammy,
Explain the Diagnostic evaluation of the Tetralogy of Fallot.
- History taking and physical examination,
- Heart sound auscultation,
- Electrocardiogram (ECG),
- echocardiography,
- chest x-ray,
- Cardiac Magnetic Resonance Imaging (MRI),
- cardiac catheterization,
Explain the medical management of the Tetralogy of Fallot.
- Provide oxygen properly to treat the child’s hypoxic condition and cyanosis condition.
- Provide proper sedative medicine to the child.
- Provide proper intra venous fluid to the child.
- Treating Child Dehydration Properly
- If the child has the condition of anemia, it should be treated properly.
- Provide proper chest position to treat child’s hypoxic spell.
- Administer an intravenous vasopressor such as methoxamine to the child.
- If the child has a severe technology of Fallot condition, provide the child with prostaglandin E1 intravenously. Due to this, dilatation of ducts occurs and pulmonary blood flow increases.
- If the child has a condition of acidosis, treat it properly.
Explain the Surgical management of the Tetralogy of Fallot.
- Surgical management of Technology of Fallot usually consists of correcting the defect and providing palliative procedures. Performing this procedure increases the blood flow in the lungs and treats the cyanosis condition.
- Most common surgeries involve intracardiac repair and complete repair.
- Complete intracardiac repair
Complete intracardiac repair is the preferred surgical procedure to treat most tetralogy of Fallot conditions. In this procedure, the ventricular septal defect is treated with a patch. Then the obstruction of the pulmonary artery which is stenosis is relieved so that the blood can be transported from the right ventricle to the lungs properly after which repositioning of the overriding aorta is provided. The aim of this procedure is to improve the blood flow in the lungs and treat the child’s condition properly.
- Blalock Tossing or Modified Blalock Tossing Sunt.
When it is impossible to completely repair the condition of tetralogy of fallot, blactosing sunt is not used. In this procedure, a connection is made between the subclavian artery, innominate artery and pulmonary artery, due to which the blood flow in the lungs can be improved.
- Pulmonary valve stenosis
- In pulmonary valve stenosis, the stenotic valve is properly repaired.
- Explain the Nursing management of the Tetralogy of Fallot.
- Monitoring the child properly.
- To properly assess the child’s vital signs.
- Assess the child’s cardiac function properly.
- Properly assess the child’s symptoms like breathing difficulty, sweating, tiredness.
- To provide complete education to the child’s parents about the child’s condition, its causes, its symptoms and signs, its treatment and lifestyle modification.
- Preoperative nursing management
- To provide proper position to the child.
- Provide oxygen to the child.
- To provide proper psychological support to the child.
- Monitoring the child’s blood oxygen level regularly.
- Provide proper protection to prevent infection and trauma to the child.
- To provide complete education to the child’s parents and caregivers about the child’s condition, its causes, symptoms and signs.
- Provide care by maintaining proper aseptic technique of the child.
- Provide intravenous fluids to maintain the nutritional status of the child.
- Keep the child properly clothed to prevent hypothermia.
- Provide proper antibiotic medicine to prevent the child from infection.
- Postoperative nursing management
- Proper close monitoring of the child.
- Continuously monitoring the child’s vital signs.
- To continuously monitor the intake output chart of the child.
- Provide adequate intravenous fluids to maintain the nutritional status of the child.
- Provide adequate respiratory support to the child.
- Administer oxygen properly to the child.
- Proper ventilation to keep the child’s air passage clear.
- Maintaining body temperature of child continuously Avoiding exposure of child to external environment.
- Providing a nutritious diet to the child.
- Maintain proper hygienic condition to prevent child from infection.
- Provide dressings maintaining proper aseptic technique on the operative side.
- Daily weight monitoring of child.
- Continuously monitoring the child for any complications.
- To provide education to the parents to provide adequate care to the child.
- Providing complete education to the parents about the child’s condition.
- Provide proper psychological support to reduce the anxiety of the child and his family members.
- Advising the parents of the child to provide the prescribed medication to the child.
- To provide proper psychological support to the parents of the child.
- Advising the child’s parents to follow up regularly.
🔸d) Diarrhea–
- Diarrhea is a condition in which liquid, loose and watery stools are passed more than three times in a day (in 24 hours). And the frequency of these loose, watery stools is also high.
- Due to diarrhoea, excessive amount of fluids and electrolytes are lost from the body, resulting in a condition of dehydration.
- Diarrhea is one of the top three causes of mortality rates in developing countries.
- (Diarrhoea is a disease in which passage of loose, liquid or watery stool more than three times per day)
Explain the types of diarrhea. (specify the type of diarrhoea)
There are four main types of diarrhea.
- 1) Acute Diarrhoea
- 2) Chronic Diarrhoea
- 3) Persistent Diarrhoea
- 4) Dysentery
1) Acute Diarrhoea
- Acute diarrhea is a condition in which the onset of diarrhea is sudden and of short duration. And for a period of less than two weeks.
- Acute diarrhea is mainly caused by any infection.
2) Chronic Diarrhoea
- Chronic diarrhea is a condition in which loose watery stool is present for more than 3 weeks, it is called chronic diarrhea.
- Chronic diarrhea is due to any organic disease.
3) Persistent Diarrhoea,
- Persistent diarrhea is a condition in which attacks of acute diarrhea persist for more than two weeks and the diarrhea is caused by an infection.
4) Dysentery
- Dysentery is a condition in which blood, mucus, and pus are present in the stool, accompanied by abdominal colic, fever, and tenesmus (a condition in which there is a need to pass stool even though the bowel is already emptied.) Get.
Explain the Etiology/cause of the Diarrhoea
- Due to unhygienic condition.
- Due to infection.
Due to viral infection :=
- rota virus,
- enterovirus,
- Due to AD virus,
- Caused by measles virus.
- Caused by influenza virus.
- Due to bacterial infection.
- E coli,
- Due to Shigella bacteria,
- Caused by salmonella bacteria.
- Caused by staphylococcus bacteria.
- Caused by Vibrio cholerae.
- Due to parasitic infection.
- Entamoeba histolytica,
- Giardia lamblia,
- cryptosporidium,
- P falciparum, P vivax, P ovali and P malaria.
- Due to fungal infection.
- Due to Candida albicans,
- Due to infectious conditions.
- Due to upper respiratory infection,
- Due to otitis media,
- Due to tonsillitis,
- Due to pneumonia,
- Due to urinary tract infection.
- Due to dietary and nutritional factors.
- overfeeding,
- Due to starvation,
- Due to food allergy and food poisoning.
- Due to other predisposing conditions
- like,
- age,
- season,
- artificial feeding,
- Explain the clinical manifestation/ sign and symptoms of the child with the Diarrhoea.
- Passing loose watery stools frequently.
- Dehydration,
- Abdominal pain.
- Getting a low grade fever.
- Loss of appetite.
- Abdominal distension.
- Behavioral changes such as
- irritability,
- restlessness,
- coming to wickness,
- feeling tired,
- Not sleeping properly,
- Physical changes can be seen like,
- weight loss,
- Poor skin turgor,
- Dryness of mucus membrane.
- Lips become dry,
- Paleness,
- Eyes become infected,
- Fontanelle to be depressed,
- Changes in vital signs such as,
- low blood pressure,
- tachycardia,
- Rapid respiration,
- limns to be cold,
- Decreased urinary output,
- loss of consciousness,
Explain the diagnostic evaluation of the patient with the diarrhea.
- History taking and physical examination,
- stool examination,
- blood examination,
- Erythrocyte Sedimentation Rate Testing (ESR),
- stool culture,
- Ova and parasite assessment,
- Endoscopic examination.
Explain the medical management of the diarrhea.
- 1) Provide rehydration therapy to the child.
- Provide oral rehydration solution (ORS) to maintain child’s hydration status.
- Oral rehydration therapy is considered an effective treatment for treating mild to moderate dehydration.
- 2) Provide intravenous fluid therapy to the child.
- If the child has a condition of dehydration and ORS therapy is not properly effective, provide intravenous fluid therapy to the child.
- 3) Providing proper feeding to the child with intravenous therapy due to which Malnutrition can be prevented.
- Providing easily digestible food to the child who can take food by mouth.
- Ex:= Toast, rice, blanned food.
- 4) Maintaining adequate fluid and electrolyte levels of the child.
- 5) Provide antibiotic medicine to child if diarrheal disease due to any bacterial infection.
6) Provide antidiarrheal medicine to the child
- like,
- Loperamide,
- Bismuth Subsalicylate.
- 7) Explain the Nursing management of the child with the Diarrhoeal disease.
- State the nursing management of a child with diarrheal diseases.
- To properly assess the child.
- Assessing the Severity of Diarrheal Diseases
- Assess the frequency, volume and consistency of diarrhoea.
- Assess the child for any symptoms of dehydration.
- Maintaining proper fluid and electrolyte levels of the child.
- Provide oral rehydration solution to maintain child’s hydration status.
- If the child has severe dehydration, provide intravenous fluid therapy.
- Providing proper nutritional support to the child.
- Providing continuous breast fitting to the child.
- If the child is able to intake food through mouth, then providing easily digestible food to that child.
- Provide proper medication to the child.
- If the child has contracted diarrhea due to any bacterial infection, provide antibiotic medication.
- If the child has any parasitic infection then provide antiparasitic medicine.
- Advise the child to practice proper hand hygiene techniques to avoid any type of infection.
- Monitor the child continuously.
- Providing education to the child’s parents or safe water and food handling, due to which the condition of diarrhea can be prevented.
- Advise the parents of the child to provide regular medication to the child.
- 8) Explain the prevention care of the Diarrhoea. (Explain prevention care of diarrhea)
- Advising the parents to provide continuous breast feeding to the child.
- Advise parents of child to maintain proper hand hygiene.
- Giving advice to the child’s parents to properly prepare safe water and hygienic food.
- Provide proper hygienic bottle fitting to the child.
- Advising the child’s parents not to use any type of specifier.
- Advise the child’s parents to maintain strict personal hygiene.
- Giving advice to keep the child’s nails short and giving advice to keep the child’s hands and toys always clean.
- Provide adequate fluid to the child.
- Providing education to parents to provide easily digestible food like rice, dal, soup, coconut water to children.
- Advise parents to provide homemade ORS solution to child if required.
- Advise the parents or provide regular medication to the child.
- Giving advice to parents to take proper care of child
⏩ Q-4 Write short notes. (any three) (12)
🔸a) Under five clinic-
- Children are a high risk group for developing any disease. Especially children below five years of age are vulnerable and special risk group for getting any diseases or infections.
- In developing countries, the death rate is high among children under the age of five.
- Among the causes of mortality and morbidity in children, prematurity, low birth weight (LBW), acute respiratory infection (ARI), diarrhoea, infectious diseases and accidents are the major causes.
- The Under Five Clinic focuses on all types of preventive services as well as nutritional surveillance, health education and treatment for children under the age of five.
- The concept of Under Five Clinic is derived from Well Baby Clinic. It provides all types of comprehensive health care services for children under five years of age.
- The majority of causes of mortality and morbidity in children under five are preventable. So all these types of services are provided by Under Five Clinic in the form of a triangle symbol as follows.

- Care in Illness.
Under 5 Clinic services provide immediate care and treatment to any child under five years of age during any type of illness or illness.
In which any disease or illness is diagnosed early and proper care is given.
All care related to children is provided on an institutional basis and when required, the child is also referred for further treatment using referral services.
- Adequate Nutrition.
During the developing period of the child, it is very essential for him to get a proper nutritious diet for his normal growth and development.
A baby should be exclusively breastfed from birth to six months. A suitable weaning diet should then be provided.
In order to prevent Protein Energy Malnutrition (PEM) and anemia, rickets and different types of nutritional deficiency disorders in children, they should receive a proper nutritional balance diet.
- Immunization…
Immunization is a very important service in preventive pediatric services. By giving vaccine, specific protection is developed against specific diseases.
Immunization provides specific protection against diseases seen as dangerous infections in children such as poliomyelitis, diphtheria, pertussis, measles, rubella, hepatitis B, pneumonia, viral diarrhea etc., which are particularly responsible for mortality and morbidity in children.
Immunization in children produces immunity to specific diseases, and protects children from specific diseases or infections.
- Family Planning
During the Under Five Clinic programme, mothers should be counseled and guided about family planning and its methods and services so that they can better focus on their children’s health and well-being.
- Health Education
These are very essential and highly needed services of Under Five Clinic. In which mothers and fathers are given health education on every aspect of their children’s care.
It provides health education on every aspect of disease prevention, health promotion, normal growth and development, best feeding, nutritional balance diet, periodic assessment, immunization, hygiene and cleanliness.
All the above services are provided under Under Five Clinic.
These clinics are usually run in villages, backward areas and remote areas.
The clinic is managed by a trained health worker and also conducts home visits and provides comprehensive home care to children under 5 years of age and mothers during home visits.
🔸b) UNICEF.
UNICEF (United Nations International Children’s Emergency Fund) is a global organization dedicated to advocating and protecting the rights of the child.
Founded in 1946, UNICEF works to improve the lives of children and their families in more than 190 countries and territories. The focus is on the most vulnerable and marginalized populations.
Its interests span across various sectors including health, education, nutrition, child protection and emergency relief.
•> Key Area of UNICEF
Health and Nutrition:
- Ensuring access to essential health care services and nutrition, including immunization, maternal and newborn care and treatment of malnutrition.
- Emphasis on issues like HIV/AIDS, water sanitation and hygiene.
Education:
- To take measures to ensure that all children, especially girls and in crisis-affected areas, have access to quality education.
- Supporting early childhood development and bringing about improvement in educational infrastructure and resources.
Child Protection:
- To provide protection to children from violence, exploitation and abuse.
- Addressing issues like child labour, trafficking and child marriage.
- Providing support to legal and social systems to protect the rights of children.
Emergency Response:
- To provide life saving assistance during emergencies including natural disasters, conflicts and epidemics.
- Ensuring proper access to shelter, food, clean water, medical care and psychological support to children and families during emergencies.
Advocacy and Policy:
- Advocating for policies and practices that promote child rights and well-being at local, national and international levels.
- Partnering with government, NGOs and other stakeholders to influence policy changes and secure funding for child fixed programmes.
Guiding Principles of UNICEF:
- UNICEF’s work is guided by the principles of the Convention on the Right of the Child (CRC). It outlines the fundamental rights of all children including the rights of survival, development, protection and participation.
- The organization works on the belief that every child should get a fair chance in life irrespective of their background and circumstances.
••>How UNICEF Operates Fundraising and Donations:
- UNICEF is funded entirely through voluntary contributions from governments, private donors and fundraising initiatives.
Partnership:
- Government, Non-Governmental Organizations (NGOs) collaborate with civil society, private sector and community to implement the program and reach the needy child.
Field Office:
- Resources operates field offices around the world to directly implement and monitor projects, ensuring they reach the child and their families.
Key Programs and Initiatives:
Gavi, Vaccine Alliance:
Works with partners to increase access to immunization in low-income countries.
UNICEF-School in a Box:
- Provides portable learning supplies to children in emergency and conflict situations.
Impact:
- UNICEF has made significant strides to improve the lives of children globally.
- They have contributed to reduced child mortality rates, increased school attendance, better nutrition and stronger child protection.
- UNICEF creates a vital force through global efforts to shape a world where every child is healthy, educated, protected and respected.
🔸c) Role of pediatric nurse in child care –
- Due to changes in the field of medicine and technical advancements, the role of the pediatric nurse has also seen many changes to meet the new demands in child health care.
- The role of the pediatric nurse has become specialized in every aspect of care. All care is provided through a comprehensive approach by nurses at every stage of the child whether healthy or sick.
- The role of a nurse changes in different institutes, but its basic responsibilities and roles are the same everywhere.
- A pediatric nurse has specialized training in pediatrics. Its detailed roles are classified as follows.
CARE GIVER.
Preventive, promotive, curative and rehabilitative care is given to the child in every set up by the pediatric nurse. This care is planned based on the needs of the child. It includes all needs related to therapeutic needs, comfort, safety and personal hygiene.
HEALTH EDUCATOR.
Pediatric nurses provide incidental and planned health teaching to the child’s parents and family members on all matters related to child care. So that the child can be given proper care.
ADVOCATIVE ROLE.
Pediatric nurses use scientific principles of child health care to ensure that children receive quality care. Works to give the child maximum benefit of its karma.
MANAGER.
A nurse acts as a manager of pediatric care unit to fill every care of the child and helps to organize his every care properly.
TEAM LEADER.
A pediatric nurse acts as a team leader in her unit and leads to provide better care by maintaining proper communication between all staff and subordinates. Distributes responsibility among everyone.
NURSE AS A RECREATIONIST.
Plan different types of recreational activities to modify the child’s stress during hospital adjustment procedures and hospitalization and help modify the child’s behavior.
NURSE AS A COUNSELOR.
Counsels and provides guidance to the child during critical care decisions and any problem solving approach to the parents.
SOCIAL WORKER.
It works to provide special welfare agencies and necessary social support for social problems and adjustment related to the child and his family members.
NURSE AS A RESEARCHER.
The nurse conducts different types of research during her clinical practice in the pediatric unit and tries to come up with new concepts. Finds new ways to deal with health problems. Nursing plays a role as continuous research to provide better health care facilities.
🔸d) Difference between kwashiorkor and marasmus –
- (Note that this question is written on both sides as the difference is given here in both lines for the sake of fluency. And in each line information is given first about Kwashiorkor and then about Marasmus.)
- Kavasiorkor is mainly due to protein deficiency whereas marasmus is due to deficiency of both protein and calories.
- It is usually seen in a child of six months to three years….It is usually seen in a child under one year..
- No loss of subcutaneous fat is seen in this.. Loss of subcutaneous fat is seen in this..
- Swelling is seen in this body..
- The part of the ribs of this child is not very prominent.. The part of the ribs is seen prominently..
- The child appears lethargic… The child appears alert and irritable..
- This child has no or normal muscle wasting… this child has severe muscle wasting.
- It is observed that the child has less appetite… This child has a high appetite and the child takes good food as soon as it is fed.
- This baby’s face is seen as a moon shape… This baby’s face is seen as a monkey shape..
- Hair changes in this child are seen in gray or red color… Hair changes in this child are not seen much..
In this condition, when the child is given adequate amount of protein, the condition of the child often improves… If the child is given adequate amount of protein along with carbohydrates and fat, the condition of the child improves soon.
🔸e) Thalassemia –
- Thalassemia is a type of hereditary disease. It is also known as hereditary hemolytic anemia.
- There is a decrease in the synthesis of hemoglobin.
- Defects and abnormalities are mainly found in the messenger RNA (mRNA) that synthesizes the polypeptide chain of hemoglobin.
- Different types of thalassemia have defects in different chains of this polypeptide. Which includes alpha, beta and gamma chain.
- Due to defects in this polypeptide chain, proper hemoglobin synthesis does not take place. It is called thalassemia.
- Hypochromic microcytic anemia is seen in this condition due to defective hemoglobin fixation in RBCs.
- Thalassemia is derived from the Greek word thalassa meaning great sea.
- This disease was first identified in 1925 by a scientist named Cooley. Hence thalassemia major is also known as Coolis anemia.
Types of Thalassemia.
- Thalassemia is divided into following types based on its condition.
Thalassemia Major..
- It is also known as Cullis anemia or Mediterranean anemia. Because it was first seen mainly on the Greek and Italian side.
- Thalassemia major is the most serious condition of all its types. The gene responsible for thalassemia i.e. beta chain is defective from both mother and father. Due to which this hereditary problem is transferred to the child.
- In this erythropoiesis i.e. the process of making mature RBC is not proper, hemolysis occurs and due to this anemia is observed.
- Due to anemia, more erythropoietin is stimulated by the kidneys for RBC production and again the action of defective erythropoiesis occurs due to which defects are also seen in the medullary canal of bone.
- Hepatosplenomegaly is seen over time in this condition due to the accumulation of RBCs in the liver and spleen through the action of repeated hemolysis.
- In this condition, RBC breaks down and is released into the blood, and due to this, hemosiderosis develops, i.e. excess iron is deposited in every organ of the body and eventually disturbs the function of the organ.
- Thalassemia major is a condition of hypoproliferative anemia caused by defective hemoglobin.
- Thalassemia intermedia.. This type of thalassemia is caused by defective synthesis of alpha and beta chains. This condition is also somewhat related to thalassemia major.
Thalassemia minor.. This is a common illness among the types of thalassemia. In which alpha or beta defective gene is inherited from mother or father to the child. This is characterized by heterozygosity, i.e. the copies of the defective gene from the mother and father do not match, either alpha and beta copies of different genes are transferred from both sides.
Hence this is a mild condition in the child. In this condition the child is completely asymptomatic or mild anemia is seen in the child. Children with this condition have a very good prognosis. Along with mild anemia, mild jaundice or mild abdominal pain can also be seen in the child. A child with thalassemia minor can lead a normal life and usually does not require any type of management.
Management of patients with thalassemia.
- It is necessary to diagnose the condition of a child with thalassemia and give proper treatment to prevent complications.
- A child with thalassemia major requires frequent hospitalization, it is especially important to psychologically prepare the child for hospitalization.
- Blood transfusion and iron chelating agents as needed are the mainstays of treatment for a child with thalassemia major as medical management.
- This baby has a special need for rest and comfort so provide it.
- Give the child a proper balance diet, give a diet with vitamins and supplements specially available and stop iron in the child’s diet.
- Working with the child during hospital stay with complete aseptic technique to prevent infection.
- Informing the child’s parents about the disease’s prognosis and treatment.
- Providing special psychological and emotional support to the child’s parents.
- The need for surgical intervention may also arise when the child and his parents are in need of diathesis. Provide perioperative nursing care related to this.
- Providing health education regarding follow up care and teaching the parents to take care of the child at home.
⏩ Q-5 Define following (any six) (12)
🔸a) Pediatric-
- Pediatric nursing is a branch of nursing. Which provides holistic nursing care to children from CONCEPTION to Adolescence age. The main goal of which is for proper growth and development of children and physical, mental and social well-being development of the child. In pediatric nursing, preventive, promotive, curative and rehabilitative nursing care is given to every child in this group.
🔸b) Infant Mortality –
- Infant Mortality Rate (IMR) is the rate of death of children under one year of age compared to 1000 live births in a year.
🔸c) Weaning
- A baby is given exclusive breast feeding for six months after birth. But then taking into account its growth and development, only breast milk cannot meet its needs, so after six months the need for additional supplement feeding arises which is called supplementary feeding or weaning.
- Weaning is an important process to gradually shift the baby from breast feeding to normal foods prepared at home.
- During this time, breast feeding is not stopped, but along with breast feeding, additional foods are introduced to the baby including clear liquids, semisolids and gradually the baby is shifted to solid diet. All these processes are called weaning.
🔸d) Failure to thrive –
- FTT is especially common in infants and young children. In which the expected growth of the child is not seen.
- FTT is a problem especially seen in children of poor socio-economic groups. After this terminology was mentioned in 1915, it was also known as emotional deprivation.
- FTT is a chronic and progressive disorder of infants and children. In which the child does not have the expected weight for his age and loses weight. His weight is less than normal for his age.
- In Failure to Thrive, there is not much problem in the length or height of the child or in all aspects of its development. Especially his weight is not seen normal according to his age are the main characteristics.
- FTT has many psychological and physiological causes and some external and internal factors are also responsible.
🔸e) Otitis Media –
- Otitis media is an infection of the middle ear. In which inflammation is seen in the middle ear.
- This is a common problem in children. Which is especially seen in the infant and early childhood period.
- It is usually associated with infection of the upper restorative track, as the pharyngs become infected, which can easily reach the middle ear through the Eustachian tube.
- A short eustachian tube of the child is also a reason that the infection can easily get into the middle ear. Apart from this, due to the fact that the child is breastfeeding while sleeping, there are also chances of infection in the middle ear.
🔸f) Spina bifida-
- This is a type of neural tube defect. During the developmental age during pregnancy, due to the failure to join the posterior part of the vertebral column of the child, the protrusion of the spinal cord structure and the meninges layer is seen on the outside or this defect is also seen without protrusion.
- It is a congenital defect. In which the connecting structure of the lamina of the spinal cord and the vertebrae is not complete. From this gap the inner structure protrudes outward.
- Here there is a slight gap in the structure of the lamina on the poster part of the vertebral column or it is also seen that there are options of complete lamina.
- Based on the structural defect it is divided into several types such as spina bifida occulta and spina bifida cystica.
🔸g) Rheumatic fever –
- This group is an infection caused by a beta hemolytic streptococcal pathogen.
- Which usually causes inflammation of connective tissue and endothelial tissue of the body and inflammatory lesions are seen there.
- Usually this is an autoimmune collagen. Due to these diseases, serious damage and inflammation is seen in the structures of the body like heart, joint, blood vessels etc.
- Genetic structure, environmental change, unhygienic living conditions, overcrowded population, unhealthy diet and body’s immunological response are also responsible for rheumatic fever.
🔸h) Epispadias –
- In this condition the urethral opening is found in the upper surface of the penis. This urethral opening can be anywhere on the upper side of the penis. This leads to abnormal urine passing in the child which also creates a psychological discomfort.
This condition is surgically corrected.
⏩ Q-6(A) Fill in the blanks. (05)
1.Toilet training needs to be initiated at——— age. 18 months to 3 years
2.Universal children’s day celebrated on——-20 November
3.ICDS stand for——– Integrated Child Development Services
4.The causative organism of diphtheria is——— Corynebacterium diphtheriae.
5.ORS solution should be used within———– hours. .24 hours
⏩ (B) True or False – (05)
- Poliomyelitis is diagnosed by stool examination. . True.
- The green stick fracture are commonly occur in children. True
- Rickets disease occurs in the children due to deficiency of vitamin-A. False
- Uncontrolled proliferation of immature WBC known as Leukemia. True
- Marasmus is also known as edematous malnutrition False