ENGLISH – Pediatric 06/09/2019-paper no.1
06/09/2019 GNC PAPER
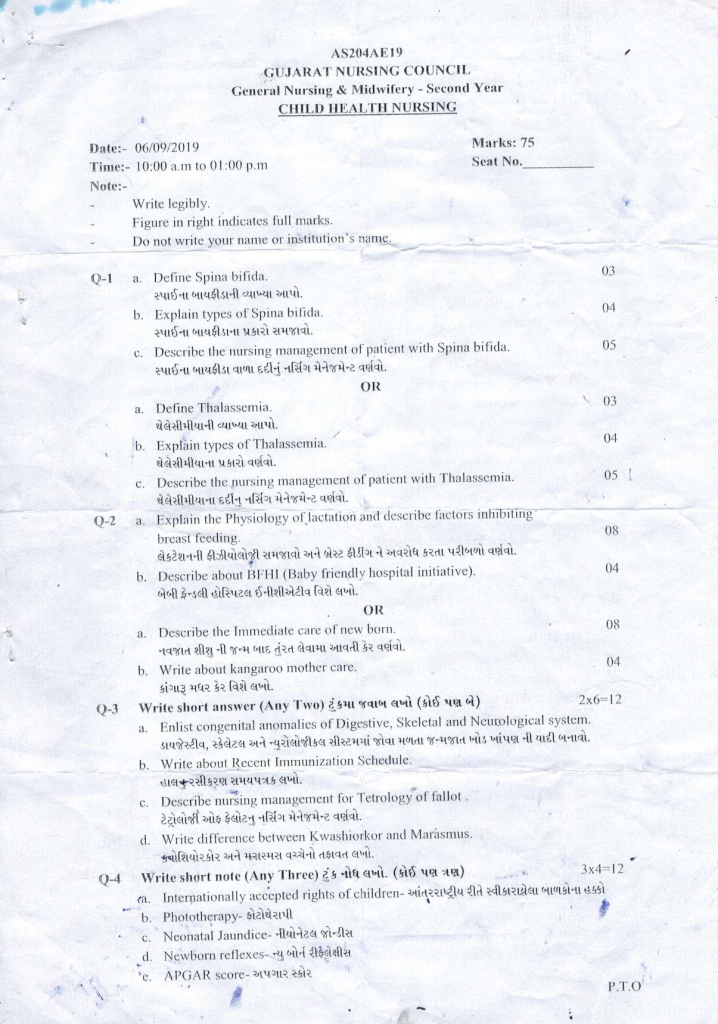
Q-1 🔸a. Define Spina bifida. 03
- This is a type of neural tube defect. During the developmental age during pregnancy, due to the failure to join the posterior part of the vertebral column of the child, the protrusion of the spinal cord structure and the meninges layer is seen on the outside or this defect is also seen without protrusion.
- It is a congenital defect. In which the connecting structure of the lamina of the spinal cord and the vertebrae is not complete. From this gap the inner structure protrudes outward.
- Here there is a slight gap in the structure of the lamina on the poster part of the vertebral column or it is also seen that there are options of complete lamina.
- Based on the structural defect it is divided into several types such as spina bifida occulta and spina bifida cystica.
🔸b. Explain types of Spina bifida. 04
- There are mainly two types of spina bifida. including spina bifida occulta and spina bifida cystica..
- Spina bifida cystica is mainly seen in two forms, minigocele and meningomyelocele. These types can be seen in detail below.
- Spina bi fida occulta..
- This defect is most common in neural tube defects. In which complete closure is not done on the posterior side of the vertebra. Mainly this type of problem is seen in the fifth lumbar vertebra and the first sacrum vertebra.
- No structure is ported to the outside from this defective part. But displacement of the spinal cord is seen.
- Some children have small follicles or hair-like structures growing out near the lumbar and sacrum regions.
Sign and Symbols
- Mainly symptoms are not seen in this case.
Some children may also have the following signs and symptoms including: - Gradually, it is seen that there is difficulty in movement or sensation in the leg.
- There is some change in the normal pattern of passing urine.
- It is seen that the walking pattern of the child changes gradually.
Any type of ulcer or incision can also be seen on the leg. - This problem is mainly diagnosed through physical examination which can be diagnosed through examinations like radiograph, myelogram etc.
Management
In this condition, if there are no neurological signs and symptoms, then no surgical correction is required, but if symptoms are present, then surgical correction is done. In which laminectomy is done, i.e. the part of the lamina of the vertebra is opened and the part inside the spinal cord and the defect are surgically repaired.
Meningocele..
This is a type of defect of spina bifida cystica. A meningocele shake (cell) emerges from the unfused part of the lamina posterior to the vertebral column. In which the meninges and CSF are protruded (extruded). This shaken portion does not contain the spinal cord or its contents.
Mainly this type of meningocele is found in the lumbar and sacral region. Sometimes it is also seen in the thoracic region.
Since there is no spinal cord damage, neurological problems are not seen in this. But if there is any kind of injury in the part of this transparent shake and CSF leaks, then infection is easily seen in this part and in the central nervous system.
A child with this type of problem should be periodically measured for head circumference and bulging of the frontals. So if hydrocephalus develops, it can be known immediately.
Diagnosis of this type of disorder is done through history collection, physical examination, myelography and radiography and CT scan.
management..
Immediately after birth, the baby should be placed on the abdomen to avoid pressure on the sac.
If part of shake is intake then cover it with dressing, if part of shake is damaged and CSF is leaking then moist dressing should be applied on affected part for prevention of infection.
The child should undergo operative measurements for surgical closure of the defect as soon as possible. The prognosis is good but if hydrocephalus or any neurological problems are present then the prognosis depends on the abnormality.
After the surgical operation, the child is kept in a prone position to prevent pressure on the incision site.
Meningomyelocele…
Due to non-closure of the lamina of this vertebral column, the spinal tissue meninges and CSF all these things are portuced to the outside.
This is the most common problem in all types of spina bifida.
Although this problem is mainly seen in the lumbar and sacrum, it can be seen in any part of the whole back.
Displacement of the spinal cord is seen in this protrusion. So mainly this type of problem is seen with neurological problem.
In this type of problem, flaccid paralysis is seen in the child. Sensations are not seen. Reflexes are also absent. Abnormal posture is found in the lower extremity.
Hydrocephalus is also seen with this condition.
Infections are also seen in the central nervous system due to shock and ruptured meninges.
Bowel and bladder function is seen to be altered.
Mainly diagnosis of this type of problem can be done through physical examination, neurological examination, radiographic study, CSF examination and CT scan.
management..
This type of problem is very serious and this child is managed by a multi-sided surgical approach and a team of super specialists.
In which Pediatrician, Neurosurgeon, Orthopaedic, Urologist, Physiotherapist and Dietitian all these team members are doing surgical correction and surgical management of this child.
🔸c. Describe the nursing management of patients with Spina bifida. 05
- After the birth of the baby, if the sac has ruptured, then it is the primary responsibility of the nurse to prevent infection by putting a sterile moist dressing on the sac.
- A spina bifida child should be placed on the abdominal side to prevent pressure on the sac or affected part.
- This child should be kept in an incubator or warmer room so that his body heat can be maintained and the chances of infection can be minimized.
- Close monitoring of the child should be done. Close monitoring and record keeping of the child’s physical condition, neurological condition, sac membrane integrity or rupture, chances of CSF leakage, signs of developing meningitis or hydrocephalus is very important. It is necessary.
- The baby’s position should be changed from time to time so as to prevent break down in the skin, this time it is necessary to pay special attention to the baby’s back.
- It is necessary to take proper care so that the child does not get urinary tract infection. It is equally important to watch the child for urinary retention. Catheterization is also done as needed and as per doctor order. If a catheter is placed, it also needs to be taken care of.
- After surgery the child should be handled very carefully for nutrition. So that the surgical healing can be good and the weight gain of the child can also happen.
- After the surgery, it is necessary to take care of the incision side and dressing part of the child with very sterile technique. So that the spread of infection can be prevented.
- It is very important to promote the growth and development of the child and give him emotional and psychological support.
- It is also necessary to give health education to the parents of this child about child care and various necessary issues. Also explain that it is necessary to follow up the child from time to time.
🔸OR🔸
🔸a. Define Thalassemia. 03 Define thalassemia.
- Thalassemia is a type of hereditary disease. It is also known as hereditary hemolytic anemia.
- There is a decrease in the synthesis of hemoglobin.
- Defects and abnormalities are mainly found in the messenger RNA (mRNA) that synthesizes the polypeptide chain of hemoglobin.
- Different types of thalassemia have defects in different chains of this polypeptide. Which includes alpha, beta and gamma chain.
- Due to defects in this polypeptide chain, proper hemoglobin synthesis does not take place. It is called thalassemia.
- Hypochromic microcytic anemia is seen in this condition due to defective hemoglobin fixation in RBCs.
- Thalassemia is derived from the Greek word thalassa meaning great sea.
- This disease was first identified in 1925 by a scientist named Cooley. Hence thalassemia major is also known as Coolis anemia.
🔸b. Explain types of Thalassemia. 04 Describe the types of thalassemia.
Thalassemia is divided into following types based on its condition.
- Thalassemia Major..
- It is also known as Cullis anemia or Mediterranean anemia. Because it was first seen mainly on the Greek and Italian side.
- Thalassemia major is the most serious condition of all its types. The gene responsible for thalassemia i.e. beta chain is defective from both mother and father. Due to which this hereditary problem is transferred to the child.
- In this erythropoiesis i.e. the process of making mature RBC is not proper, hemolysis occurs and due to this anemia is observed.
- Due to anemia, more erythropoietin is stimulated by the kidneys for RBC production and again the action of defective erythropoiesis occurs due to which defects are also seen in the medullary canal of bone.
- Hepatosplenomegaly is seen over time in this condition due to the accumulation of RBCs in the liver and spleen through the action of repeated hemolysis.
- In this condition, RBC breaks down and is released into the blood, and due to this, hemosiderosis develops, i.e. excess iron is deposited in every organ of the body and eventually disturbs the function of the organ.
- Thalassemia major is a condition of hypoproliferative anemia caused by defective hemoglobin.
- Thalassemia intermedia.. This type of thalassemia is caused by defective synthesis of alpha and beta chains. This condition is also somewhat related to thalassemia major.
- Thalassemia minor.. This is a common illness among the types of thalassemia. In which alpha or beta defective gene is inherited from mother or father to the child. This is characterized by heterozygosity, i.e. the copies of the defective gene from the mother and father do not match, either alpha and beta copies of different genes are transferred from both sides. Hence this is a mild condition in the child. In this condition the child is completely asymptomatic or mild anemia is seen in the child. Children with this condition have a very good prognosis. Along with mild anemia, mild jaundice or mild abdominal pain can also be seen in the child. A child with thalassemia minor can lead a normal life and usually does not require any type of management.
🔸c. Describe the nursing management of patients with Thalassemia. 05 Describe the nursing management of a patient with thalassemia.
- It is necessary to diagnose the condition of a child with thalassemia and provide appropriate treatment to prevent complications.
- A child with thalassemia major requires frequent hospitalization, it is especially important to psychologically prepare the child for hospitalization.
- Blood transfusion and iron chelating agents as needed are the mainstays of treatment for a child with thalassemia major as medical management.
This baby has a special need for rest and comfort so provide it. - Give the child a proper balance diet, give a diet with vitamins and supplements specially available and stop iron in the child’s diet.
Working with the child during hospital stay with complete aseptic technique to prevent infection.
- Informing the child’s parents about the disease’s prognosis and treatment.
Providing special psychological and emotional support to the child’s parents. - The need for surgical intervention may also arise when the child and his parents are in need of diathesis. Provide perioperative nursing care related to this.
Providing health education regarding follow up care and teaching parents to take good care of the child at home.
👉Q-2. 🔸a. Explain the physiology of lactation and describe factors inhibiting breast feeding. 08 Outline the physiology of lactation and describe the factors inhibiting breast feeding.
- Lactation means the act of milk production. After the birth of the child, the mother gives the child complete nutrition through breast feeding. The physiology of this action of lactation can be described as follows.
- Breast tissue of the mother consists of lobes and lobules. Small alveoli and ducts are located in the lobules. These tiny alveoli are connected to the lactiferous duct and the lactiferous duct opens into the areola.
- Each nipple has approximately 20 lactiferous duct openings.
These alveoli secrete the secretion of milk colostrum during the second and third trimesters of the mother’s pregnancy.
- After the delivery of the baby, the placenta is removed and the levels of estrogen and progesterone decrease. Along with this, the level of prolactin hormone increases. These changes initiate the act of lactation. Which is responsible for secretion of milk from breast tissue.
- Apart from this, the secretion of milk from the breast is mainly based on the mechanical stimulation caused by the baby shaking the mother’s breast.
- Two reflexes are mainly important in the process of milk secretion which are as follows.
- Milk producing reflex..
- When the baby is feeding on the mother’s breast, it shakes and due to its shaking action, the nerve endings on the areola of the mother’s breast are stimulated and it gives impulses to the hypothalamus. These impulses from the hypothalamus reach the anterior pituitary gland and the anterior pituitary gland increases the secretion of prolactin hormone into the blood. Thus, the increase in the secretion of prolactin hormone leads to the production of more milk by the breast tissue. As more shaking is done by the baby, more prolactin hormone is produced and more milk is secreted.
- Milk ejection reflex..
This is also called let down reflex.
When this is done by the baby shaking, the nerve endings of the breast stimulate the posterior pituitary gland through the hypothalamus to secrete more oxytocin hormone. This oxytocin hormone contracts the myoepithelium cells surrounding the alveoli within the breast and compresses the alveoli. Due to which the milk comes to the areola of the nipple through the lactiferous duct. In this way the milk is ejected from the duct.
Both the above refluxes are stimulated by the baby sucking the mother’s breast and the process of lactation is maintained… - Factors hindering best feeding are as follows.
- During best feeding there are various other problems including mother or baby which causes breast feeding to be obstructed which are as follows.
- Inverted nipple.
- The nipple portion of the mother’s breast is either flat or inverted. It is called inverted nipple or flat nipple. Due to this type of nipple, normal breast feeding cannot be given to the baby.
- Whenever a mother is diagnosed with an inverted or flat nipple, it should be treated immediately.
- Ask the mother to pull and roll the nipple outward.
- Ask to pull the nipple outward with pressure, taking a series of ten mL. This series is also called Nirmala series. With the help of this, the nipple can be corrected in a short time and breast feeding can be started well.
- Shore nipple..
- That is, getting silver (ulcer) on the nipple or cracked nipple is a painful condition. In which the child cannot be breastfed normally by the mother.
- In the management of this condition, explaining proper breast feeding technique to the mother and telling the mother to maintain proper hygiene of breast and nipple. Applying hind milk at the end of breast feeding on the part with sore nipple or cracked nipple so that the part can heal quickly. Keep this part of the nipple open so that it gets enough air.
- Breast engorgement…
- When the mother does not breastfeed the child soon or the child does not breastfeed, then breast engorgement is seen due to the overflow of breast milk. Baby cannot be properly breast fed.
- Explain proper breast feeding technique to the mother.
- Give warm compress on breast to mother.
- Analgesics medicine to relieve pain if required by the mother.
- Explain the method of expressing and expressing breast milk by milk pump or manually and feeding the baby with the help of a bowl spoon.
- Breast Abscess..
- When pus formation occurs due to infection or inflammation of breast tissue, it is called breast abscess.
- This is a painful condition. In this condition the baby should not be breast fed.
- Analgesics and antibiotic medicine should be given to the mother for treatment of this condition.
- If necessary, an incision should be made on the side of the breast and drainage should be done outside.
- Breast milk should be started on the breast of the other side.
- Also, some babies are not breast feeding so give proper positioning to the mother and explain the technique of attaching the baby well.
Making the child feel a comfortable environment.
Give breast feeding when the baby is hungry.
Give breast feeding only when the baby is awake and not asleep. - It is important to take care of all the above things while giving breast feeding, if there is any problem then breast feeding cannot be done effectively.
🔸b. Describe about BFHI (Baby friendly hospital initiative). 04 Write about Baby Candle Hospital Initiative.
- BFHI is promoted by WHO and UNICEF for the promotion, protection and support of breastfeeding.
- The main aim for this is to provide exclusive breast feeding to the child till six months and continuous breast feeding as complementary feeding till the child turns two years old.
- A baby friendly hospital should formulate a policy for successful breastfeeding promotion of breastfeeding. The policy should work for the promotion of exclusive breast feeding of the child by the hospital staff and the mother. whose steps should be in return. These steps are as follows.
- The hospital should have a return (written) for B F HIV and every staff should be aware of it.
- All staff working in the hospital should be aware of this policy and should be trained to implement this policy.
- According to this policy every expectant mother should be given complete information about the advantages of breast feeding and breast feeding.
- Mother should be assisted to breast feed the baby within half an hour after birth.
- All aspects of best fitting should be explained to the mother and education should be given to the mother to maintain lactation.
- The mother should be explained that her child should not be given any food or water except the best milk for a period of six months.
- According to this policy, the practice of mother staying with the child continuously i.e. complete mother and child stay together is called rooming in. This practice should be promoted.
- The mother should be persuaded to give breast feeding only when the child is in demand.
- The baby should not be given any artificial pacifiers for breast feeding.
- The mother should be matched with a breastfeeding support group and arrangements should be made for such members to meet the mother during discharge.
🔸OR🔸
🔸a. Describe the immediate care of new born. 08 Describe the care taken immediately after birth of a newborn baby.
- The care taken immediately after the birth of the newborn is known as immediate care. In this care, keeping the airway open of the child, proper breathing and circulation of the child and maintaining the temperature of the child are included in this priority care.
- Respiration starts spontaneously after birth in about 90% of total baby births. No extra effort is required, but some children do not start normally, requiring measures of resuscitation.
- Basic care for a healthy neonate includes maintaining body temperature and warmth, providing breast feeding, close monitoring and assessment for any injuries or infections, and not separating the mother from her baby.
- In newborn immediate care, the baby is dried immediately after birth. By drying it quickly, its body heat is maintained and the child can be prevented from going to hypothermia.
- After birth, it is imperative to delay the cord clamping of the baby as long as possible if the baby is healthy and respirations have started properly. So that the child gets enough blood circulation. This cord is cut two to three centimeters from the umbilicus and dried. No substance of any kind is applied to this part of the cord, it is kept open and dry.
- The baby is kept in skin-to-skin contact with the mother immediately after delivery and breast feeding is started as early as possible.
- After birth, the birth weight of the child is assessed and the child is also given vitamins or injectable form. So that the child’s clotting factors develop and the child sees a reduction in the building tendency.
- The child is then quickly given an initial assessment. In this assessment, the child is checked for any birth defects and the normal and healthy characteristics of the child are identified. Any abnormality is identified early.
- After the assessment, the child is covered in a complete dry cloth. The baby is given an identification tag and the sex of the baby is told to the mother.
If no abnormalities are found, the mother is transferred to her bed for observation along with the baby. The mother is persuaded to continue breastfeeding and care for the child.
🔸b. Write about kangaroo mother care. 04
- Kangaroo mother care is a technique that is very useful for low birth weight babies.
- In this technique, the baby is kept in skin-to-skin contact and breastfeeding is promoted by providing emotional support to the baby.
- KMC can be given to mother-child in both hospital and home settings. In which the child is placed between the mother’s two breasts on the chest side in such a way that skin to skin contact is achieved after removing the child’s clothes. In which the child gets enough emotional support and nutrition.
- Important aspects of kangaroo mother care are skin-to-skin contact between mother and baby and exclusive breast feeding.
- Also, by using this technique, the child gains weight quickly. So that a quick discharge can be obtained from the hospital and the mother can give this kind of care to the child at home as well.
Advantages of KMC…
- By maintaining skin-to-skin contact between mother and child through KMC, the body heat and temperature of the child is maintained. Also, its metabolism is also proper.
- During the KMC procedure, the mother can give immediate demand feeding to the baby if needed. The bond between mother and child is strengthened so that breastfeeding can be promoted to the child.
- The constant close contact of the mother with the child during KMC proves to be very important in developing the child’s sense of propriety and psychological satisfaction.
- Due to the baby being in constant skin-to-skin contact with the mother, the baby gets constant stimulation and conditions like apnea can be prevented.
- Since the baby is constantly handled by the mother itself, the chances of the baby getting any kind of infection are greatly reduced.
- Due to the fulfillment of the feeding needs of the child, the child’s weight also increases continuously. Hence, this is an excellent treatment for low birth weight babies.
- As the mother carries the baby through the MC bag, it is also a very important method for easy and safe transportation of the baby.
- As the mother takes constant care of the child, the mother’s psychological anxiety of the child is reduced. Also, due to the improvement in the condition of the child, the mother also feels happy.
Points to keep in mind while providing Kangaroo Mother care…
- The person giving KMC needs to be trained by a trained person. He needs to explain the complete procedure.
- Anyone can take care of a child, but it is more appropriate for the mother to take care of the child. General condition of the child should be stable while doing this procedure.
- A low birth weight baby can be given this therapy if it is stable.
- KMC should be given by the mother as far as possible, for this it is necessary to prepare the mother psychologically. The procedure can be explained to her and mother’s participation can be obtained. If the mother is not available then the father or any member of the family can give this procedure.
- During the KMC procedure, the clothes of the mother’s chest have to be removed and the baby also has to be kept in skin-to-skin contact with the mother’s chest without any clothes. This time mother is advised to wear loose clothes.
- While giving this procedure, the baby is kept in an upright position between the two breasts of the mother with its head turned to one side. During this position, his airway should be open and his eye-to-eye contact with the mother should be maintained. The child should cling to the mother’s chest like a frog.
- While doing this procedure, giving privacy to the mother and explaining to the mother that the child should be observed from time to time.
- A child should be kept in this position for at least 1 to 2 hours in one session. As per the condition and convenience of the mother and the child, this procedure can be continued at the maximum level until done.
- Based on the hours of administration of the KMC procedure it can be described in the following classifications. In which short term MC is given up to 4 hours a day. Extended KMC is given for duration of 5 to 8 hours and Long KMC for 9 to 12 hours and Continuous KMC for more than 12 hours a day.
- KMC can be discontinued after the child gains weight and generally reaches 2,500 grams. But if the mother or family member wishes, this procedure can be carried out for a long time.
👉Q – 3 Write short answer (Any Two) 2×6 =12
🔸a. Enlist congenital anomalies of Digestive, Skeletal and Neurological system. List the congenital malformations found in the digestive, skeletal and neurological systems.
- List the digestive, skeletal and neurological congenital abnormalities…
- Congenital Anomaly means a birth defect in which a child is born with some problem as soon as it is born.
Congenital malformations of the digestive system are as follows.
- Cleft lip and cleft palate
- Esophageal atresia
- Tracheoesophageal fistula
- Congenital hypertrophic pyloric stenosis
- Omphalocele
- Diaphragmatic hernia
- Imperforated anus…
Congenital malformations of the skeletal system are as follows…
- club foot
- Hip displacement
- Bow Leg
- Knock Knee
- Polydactyly
- Syndactyly
Following is a list of neurological birth defects.
- Hydrocephalus
- Cerebral palsy
- Spina bifida
- Meningocele
- Meningo mylosil.
🔸b. Write about Recent Immunization Schedule. Write the current+vaccination schedule.

🔸c. Describe nursing management for Tetralogy of Fallot. Describe the nursing management of tetralogy of Fallot.
Nursing management of tetralogy of Fallot is as follows.
- A child with this cyanotic heart disease condition needs special care when cyanosis is seen in the child.
- Hypoxic spell i.e. the episode that occurs due to the child developing cyanosis due to not getting enough oxygenated blood is called hypoxic spell. During this time giving the baby oxygen therapy, chest position is very important to overcome the special oxygen supplement spell. Give IV fluid to the child.
- Complete history collection from child’s mother and father and decide care plan accordingly.
- Periodically take anthropometric measurements of the child so that growth failure in the child can be identified.
- Keep checking the child’s vital signs from time to time so that the child’s condition and oxygen level can be maintained.
- Feeding behavior of the child, its nutritional need, its intake and output chart, all these things need to be specially monitored and recorded.
- Investigate the child’s lab reports from time to time to get information about the child’s clinical condition.
- Assessment of the child’s respiratory system and heart sound should be done. So that the problem can be identified early.
- It is necessary to explain the condition of the child and its prognosis to the parents.
- The child should be prohibited from playing outdoor games and excessive activities and his attention should be diverted to indoor games and games that reduce physical stress.
- Fear and anxiety will develop in the child and his parents so psychological counseling of each is necessary.
- Being a chronic problem, it is very important to take preventive care of the child as there are chances that the child may get frequent infections.
🔸d. Write difference between Kwashiorkor and Marasmus. Write the difference between kwashiorkor and marasmus.
- (Note that this question is written on both sides as the difference is given here in both lines for the sake of fluency. And in each line information is given first about Kwashiorkor and then about Marasmus.)
- Kavasiorkor is mainly due to protein deficiency whereas marasmus is due to deficiency of both protein and calories.
- It is usually seen in a child of six months to three years….It is usually seen in a child under one year..
- No loss of subcutaneous fat is seen in this.. Loss of subcutaneous fat is seen in this..
- Swelling is seen in this body.. Swelling is not seen in this body..
- The part of the ribs of this child is not very prominent.. The part of the ribs is seen prominently..
- The child appears lethargic… The child appears alert and irritable..
- This child has no or normal muscle wasting… This child has severe muscle wasting.
- It is observed that the child has less appetite… This child has a high appetite and the child takes good food as soon as it is fed.
- This baby’s face is seen as a moon shape… This baby’s face is seen as a monkey shape..
- Hair changes in this child are seen in gray or red color… Hair changes in this child are not seen much..
- In this condition, when the child is given adequate amount of protein, the condition of the child often improves… If the child is given adequate amount of protein along with carbohydrates and fat, the condition of the child improves soon.
👉Q-4 Write short note (Any Three) Write a short note. (Any three). 3×4 = 2
🔸a. Internationally accepted rights of children- Internationally accepted rights of children
The Rights of the Child were declared by the United Nations on 20 November 1959. They were made with the purpose of fulfilling the special needs of the child.
These rights are as follows.
- right to free education.
- right for name and nationality.
- Right to receive special care if the child is handicapped.
- Rite to get affection, love and better understanding.
- The Right to Adequate Quality Nutrition.
- Right to get first treatment or relief in time of any calamity or distress.
- right to get good medical care.
- Right to play well and get re-creational facility.
- The right to develop one’s own abilities and become a good and useful member of society.
Right to be brought up in a calm and brotherly environment.
All the above rights are also given to the children so that every child can use all the rights equally without discrimination of religion, race, caste, sex, color etc.
🔸b. Phototherapy-Phototherapy
- When any child gets jaundice, the liver is not able to metabolize bilirubin in his body. During this condition, photo therapy is used for treatment.
- Phototherapy is a non-invasive, low-cost treatment that uses equipment to convert unconjugated bilirubin into a form that can be excreted from the body by shining rays on the child’s body.
- Conjugated toxic bilirubin is converted to water soluble nontoxic bilirubin with the help of light rays. Which is easily excreted from the body through urine and stool.
- In a child with hyperbilirubinemia, this therapy should be started when the serum bilirubin level is 15 mg/dl. This therapy can be started even before that.
- If the condition is severe, exchange blood transfusion is also done along with this therapy.
- A very good effect is seen if phototherapy is started in the early stage when the serum bilirubin level is increasing in the child.
- Phototherapy can be given to a child continuously or intermittently. It depends on the condition of the child. Fluorescence or halogen light is used in this therapy.
- Compact fluorescent lamps or light emitting diodes are also currently used for effective phototherapy.
- Blue light is used more in phototherapy. Which has a wavelength of 420 to 600 nanometers. Which helps in better absorption of bilirubin.
- The baby is placed in a warmer in the newborn care unit for phototherapy. 6 to 8 such light sources are fitted above it. During this time, the baby’s clothes are removed and only the eyes and private parts are covered to prevent damage to the retina and genitals.
- Phototherapy can be either single surface or double surface i.e. from both sides. The distance between the child and the light source is kept at 45 cm. This distance may be less depending on the different types of light and the severity of the child’s condition.
- It is necessary to change the position of the child every few hours during photo therapy. And feeding the baby is also necessary. During this time the child’s vital signs should be continuously monitored.
- Continuous breast feeding or intravenous or nasogastric feeding is continued to prevent dehydration of the baby during phototherapy.
- Monitoring of the child’s weight and continuous monitoring of input and output is necessary during phototherapy.
- The child’s serum bilirubin level should also be monitored periodically.
- Phototherapy can be discontinued after the child’s serum bilirubin level has decreased and returned to the normal range.
Complications of photo therapy..
Generally photo therapy is a safe treatment but some side effects can be seen which are as follows.
- Dehydration
- Hypothermia or hyperthermia
- Change in stool frequency
- Bronze Baby Syndrome
- Skin Recess
- Electric shock
- Disturbance in Electrolyte
Although the above side effects and complications are rare, it is necessary to take preventive precautions.
🔸C. Neonatal Jaundice- Neonatal Jaundice
- When the serum bilirubin level is more than 5 mg/dl in a neonate for any reason, it is known as hyperbilirubinemia i.e. jaundice.
- In which yellow color skin changes are seen on the face of the child due to increase in serum bilirubin level in the body blood.
- This condition is known as icterus neonatorum or neonatal hyperbilirubinemia or neonatal jaundice.
- At birth, most term babies and preterm babies have serum bilirubin levels above 5 mg/dl, and very few babies have levels above 15 mg/dl.
Types of Neo Natal Pairs..
Physiological Jaundice..
This is a common condition seen in many term babies and preterm babies after birth. In which the unconjugated concentration of serum bilirubin increases in the blood during the first week after birth. There are many reasons for this increase.
Characteristic of Physiological Jaundice..
- It occurs between 30 and 72 hours after birth in term babies and earlier in preterm babies. But no symptoms are seen 24 hours before birth.
- The severity of this condition is highest on the fourth to fifth day.
- In this condition, serum bilirubin never rises above 15 mg/dl.
- Generally after 6th to 7th day the serum level decreases and it becomes completely normal in 10 to 15 days.
- Usually this condition does not require any treatment.
- In this condition, giving the mother continuous breast feeding and maintaining the child’s hydration and observing the child are the main aspects of care.
- Pathological Jaundice..
- Pathological jaundice occurs in five percent of neonates after birth. This also increases the amount of serum unconjugated bilirubin in the blood.
- Pathological jaundice is when any symptoms of jaundice occur within 24 hours of birth.
Characteristics of Pathological Jaundice.
- Its symptoms are seen within 24 hours and in term babies its symptoms are continuously seen for one week and in preterm babies its symptoms are seen for two weeks.
- In this condition, the serum bilirubin level rises rapidly and the total bilirubin level is more than 15 mg/dl.
- This condition is more severe than physiological jaundice. It requires medical or other management to treat and is not automatically subsidized.
Cozies for Neonatal Jaundice..
- Viral Infection, Excessive Destruction of RBC, Defective Conjugation of Bilirubin, Hepatitis, Intra Uterine Infection, Defective Bilirubin Excretion, Maternal Diabetes, Hemolytic Diseases, Rh Incompatibilities
Management of Neonatal Jaundice…
- The main goal of management of neonatal jaundice is to reduce serum bilirubin levels and protect the baby from damage to the nervous system.
- If the mother’s blood group is negative and the child’s blood group is positive at the time of delivery, NTD gamma globulin should be given to the child.
- Treatment of jaundice includes the following treatments.
Photo therapy..
Exchange Blood Transfusion..
- When phototherapy does not work effectively to treat jaundice in a child, an exchange blood transfusion is done to quickly reduce the bilirubin level.
- This treatment can prevent babies from developing kernicterus jaundice, a brain-damaging condition caused by severe hyperbilirubinemia.
- Exchange blood transfusion is a process performed with highly aseptic technique. In which, after inserting a cannula in the umbilical vessels or peripheral vessels of the child, the donor’s blood, which is at normal body temperature, is exchanged with the child’s blood.
- With the help of this series, 10 to 20 ml of blood is withdrawn from the cannula and the same amount of blood from the donor is slowly pumped. This cycle is often repeated. The cycle is repeated as needed according to the condition of the severity of the child.
- This procedure is done under expert guidance and all records of total exchange blood transfusion are maintained.
- Along with this, emergency medicines like heparin, calcium gluconate etc. are also used in treatment.
- Continuous monitoring of the baby’s condition and vital signs is essential throughout the process.
- After the exchange is completed, it is necessary to give the necessary medicine and get the lab investigation done.
- Medical Management of Jaundice..
The role of medical management in jaundice is not much, mainly phototherapy and exchange blood transfusion are given as treatment.
However, some supportive medicines that bind unconjugated bilirubin are given.
🔸d. Newborn reflexes– Newborn reflexes
- Neubon’s reflexes can be determined based on his neurological examination. The neurological status of the child is very important. At birth, a child’s nervous system is anatomically and physiologically immature. Due to which temperature regulation is not seen in the child. Children lack coordination and control of some types of muscles. Hence examination of the newborn’s muscle tone and reflexes is essential.
Two types of reflexes are seen in the newborn.
- Protective reflexes that are necessary for the protection of the baby are fully developed. Which includes blinking, cuffing, sneezing etc.
- Primitive Reflex This reflex is elicited by specific stimulation. Also it has specific maturity and function.
Neurological reflexes are seen as follows.
🔸A. rooting reflex.
Which is stimulated by touching the child’s cheek or the lower part of the mouth or the corner. In which touching the baby turns that side, and also searches for food.
This reflex totally disappears by 7 to 8 months of age.
🔸B. Shaking reflex..
When the nipple part of the breast is touched by the mother with the baby’s lips, this reflex is stimulated and the baby starts the shaking movement for best feeding. This reflex diminishes after the child is six months old.
🔸Ç. gagging reflex..
When the baby is overfed or forcefully fed, this reflex is stimulated and as a result, the baby expels the extra food with nosia or nausea.
This reflex remains life long and never disappears.
🔸D. Solo wing reflex..
The shaking reflex is followed by the loosening reflex automatically. As a result, the food in the posterior part of the mouth is swallowed by the act of swallowing. This reflex never disappears.
🔸E. Sneezing and Coughing Reflex..
When any foreign body or substance enters or irritates the child’s airway, this reflex is stimulated and results in sneezing and coughing activity. So that the respiratory track or air passage is cleared. This reflex never disappears.
🔸F. Blinking reflex..
When there is too much light in the eye, this reflex is stimulated and results in the eyes closing.
This reflex never disappears.
🔸G. Doll’s eye reflex..
This reflex is stimulated or observed when the neonate’s head is turned from side to side. As a result, the eyes do not turn with the head and move in the opposite direction.
This reflex disappears after focusing and fixation of the eye develops.
🔸H. Palmar grasp reflex..
When any object is touched in the child’s hand, this reflex is stimulated and as a result the child grasps the object with his fingers.
This reflex disappears in the child after the age of three months.
🔸I. Stepping or dancing reflex.
This reflex is stimulated when the baby is held upright in an upright position with its feet slightly touching a flat surface. As a result, the child alternates flexion and extension of the leg. So it looks like it is climbing a step or dancing.
This reflex disappears in the baby after two months.
🔸J. Morrow Reflex..
This reflex is stimulated when loud noises are made around the child or when the child is held in a supine position with both hands and brought down quickly from its normal position i.e. when its equilibrium is changed. It results in generalized muscular activity. In which the arms and legs on both sides move away from the body and the fingers are straightened and extension of the extremity is seen after which the baby cries.
This reflex disappears after three to four months of age.
🔸E. APGAR score- – Apgar score
- An important immediate assessment after the birth of a newborn baby is the Apgar score assessment. This scoring system is given by Dr. Virginia Apgar. In which the following parameters of the child are measured immediately after birth viz
- Respiration, heart rate, muscle tone, reflex response and skin color are the five parameters that the neonate is monitored for one to five minutes.
- Each parameter is given a score of 2, 1, and 0 for its normal, subnormal, and absent function.
- After 5 minutes of assessment, the score of each parameter is totaled. The total score is given out of 10.
- If the newborn’s Apgar score is between 7 and 10 after the five-minute assessment, the child is found to have no adjustment or physical problem.
- If a child’s Apkar score is between 4 and 6, it indicates that the child has some difficulty. This score indicates mild to moderate depression.
- If the child’s score is found to be 3 or below 3, this condition indicates severe depression in the child and indicates that the child needs immediate emergency management.
- As this Apgar score is monitored immediately after birth, every parameter in the first minute is associated with extra-uterine life adjustment, so the parameter that occurs at five minutes is known as the true parameter. Because within five minutes the child has adjusted enough with the external environment. So that the normal function of each parameter can be well assessed.
- A room with a comfortable environment should be present while assessing the above Apgar score. There should be enough light. Infection prevention measures should be taken and every information should be recorded. The mother should accompany the child if possible during Apgar assessment.
- It is necessary to rule out the obstetrical history of the mother, her physical condition, the presence of any disease condition, the presence of any risk factor before the birth of the child.
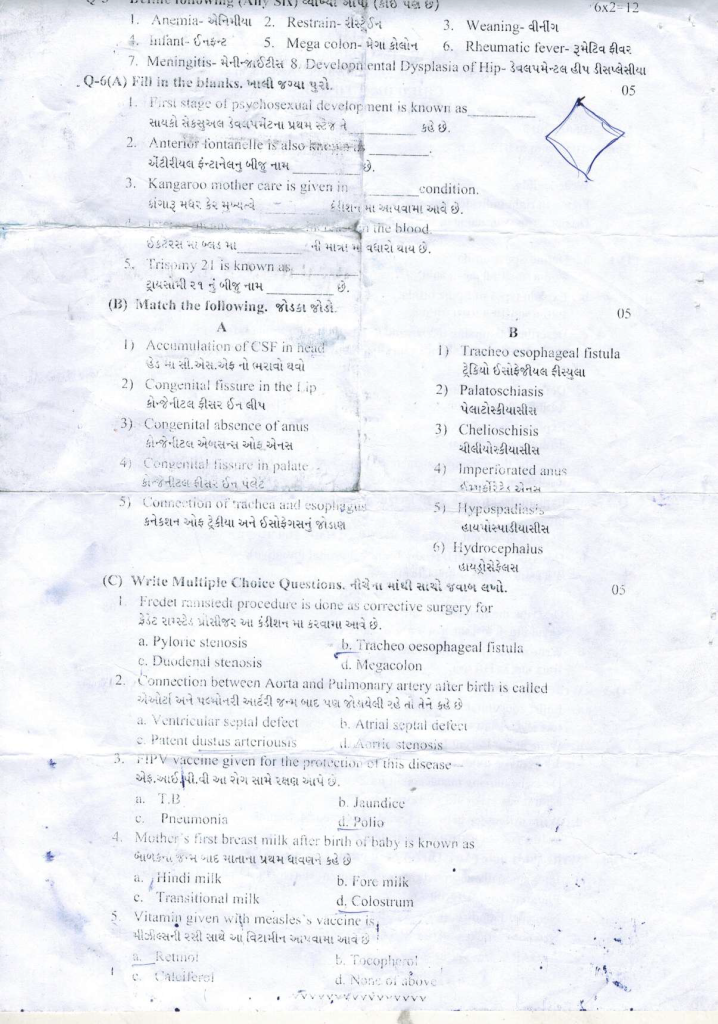
👉Q.5 Define Following. (Any six) Define. 6×2=12
🔸1.Anemia-
- Anemia is the most common blood disorder in children.
- This defect is more common in children of poor socio-economic and backward groups due to lack of adequate nutritious food.
- Anemia i.e. the condition in which there is a decrease in the amount of red blood cells in the circulation and the level of hemoglobin is less than normal is called anemia.
- According to WHO, if hemoglobin is less than 11 gr/dl in children, you are usually called anemic. There are many types of anemia like vitamin B12 deficiency anemia, iron deficiency anemia etc.
🔸2.Restrain-
- Restrain is a procedure to reduce the movement of the child. In which it is also used for the protective function of the child.
- Different types of restraints are used to prevent the movement of the child while performing any physical examination, conducting a test or collecting a specimen. This type of restraint is called short term restraint.
- Long term restraint is done for the safety of the child and also to protect the child from any kind of injury.
- For example Mom Restrain, Elbow Restrain, Jacket Restrain etc..
🔸3.Weaning
- A baby is given exclusive breast feeding for six months after birth. But then considering its growth and development, only breast milk cannot meet its needs, so after six months the need for additional supplement feeding arises which is called supplementary feeding or weaning.
- Weaning is an important process to gradually shift the baby from breast feeding to normal foods prepared at home.
- During this time, breast feeding is not stopped, but along with breast feeding, additional foods are introduced to the baby including clear liquids, semisolids and gradually the baby is shifted to solid diet. All these processes are called weaning.
🔸4.Infant
- A child from birth to 1 year of age is called an infant.
At the time of birth, this child is called a newborn. A baby up to one month after birth is called a neonate. - Hence infant means a child from one month to one year, this period is also known as infancy period.
🔸5.Mega colon- mega colon
- This is a type of congenital anomaly of the gastrointestinal system.
- It is also known as Herschprung’s disease.
- When there are no ganglionic nerve cells in the wall of the intestine, due to its defect, the part becomes swollen and wide, this problem is known as mega colon.
- These nerve cells are absent in the muscular layer and submucosal layer of the intestine.
- The disorder may be limited to a portion of the interstitium or may extend to the entire intestine. Mainly this problem is seen near the part of rectum and sigmoid colon.
🔸6.Rheumatic fever-
- This group is an infection caused by a beta hemolytic streptococcal pathogen.
- Which usually causes inflammation of connective tissue and endothelial tissue of the body and inflammatory lesions are seen there.
- Usually this is an autoimmune collagen. Due to these diseases, serious damage and inflammation is seen in the structures of the body like heart, joint, blood vessels etc.
- Genetic structure, environmental changes, unhygienic living conditions, overcrowded population, unhealthy diet and body’s immunological response are also responsible for rheumatic fever.
🔸7.Meningitis–
- The tissue layer surrounding the brain and spinal cord is called the meninges. Inflammation of this tissue layer due to any reason is known as meningitis.
- A high mortality and morbidity rate is seen due to this problem in children.
- Bacteria, viruses and many pathogens are responsible for causing meningitis.
🔸8.Developmental Dysplasia of Hip – Developmental hip dysplasia
- It is a congenital anomaly of the musculoskeletal system.
- This problem is seen due to the non-normal development of the upper part of the femur bone and the acetabulum cavity during the development of the musculoskeletal system of this child.
- This problem can be seen in both sides of the leg, but it is more common in the left leg. Due to this, the posture of the lower extremity is not fixed properly.
🔸Q-(6) Fill in the blanks. Fill in the blank. 05
First stage of psychosexual development is known as_______. (oral stage)
Anterior fontanelle is also known Another name of anterior fontanelle is_______. (bregma)
Kangaroo mother care is given in _ condition. Kangaroo mother care is mainly provided in __ conditions. (Low Birth Weight)
- The amount of _ in the blood of icterus is increased. (Serum Bilirubin)
5 Trisony 21 is known as_______ The seed name of Trisony 21 is_______. (down syndrome)
🔸(B) Match the following. Connect the Jodka. 05
A B
1) Accumulation of SF in head 1) Tracheo esophageal fistula
2.) Congenital fissure in the fly 2) Palatosc!hiasis
3) Corgenital absence of anus 3) Chelioschisis Congenital absence of anus Chelioschisis
4) Congenital fissure in palate 4) Imperiorated aus
5) Connection of trachea and esopliggas 5) Hypispalins’s connection of trachea and esophagus Hypospadias
5) Hydrocephalus Hydrocephalus
ANSWER
1-5
2-3
3-4
4-2
5-1