😡B.SC. NURSING- September-2021-Management of Nursing Services and Education (UPLOAD PAPER NO.1)
B.SC. NURSING- September-2021-Management of Nursing Services and Education (BKNMU)
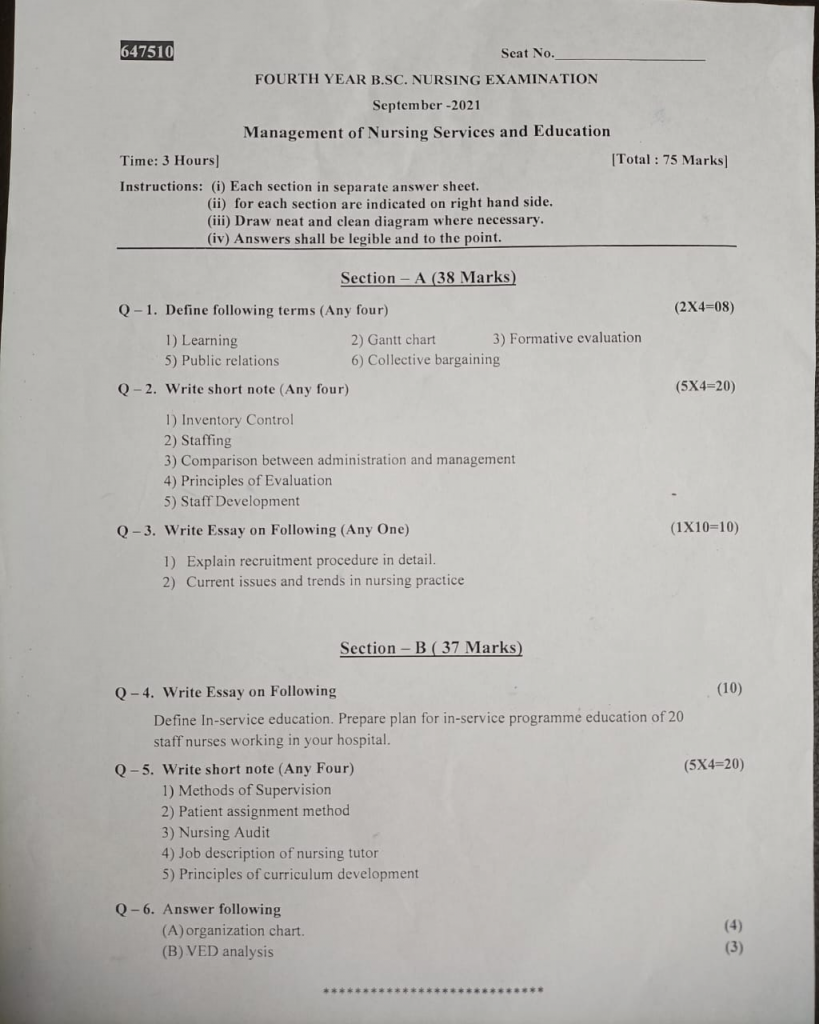
🔸Section A🔸
Q1. Define following terms (Any four)
🔸1) Learning
- “The ongoing process through which nursing professionals and educators acquire, update, and refine their knowledge, skills, and competencies to improve patient care, enhance professional practices, and advance the field of nursing. It encompasses formal education, hands-on training, reflective practice, and continuous professional development aimed at improving individual and organizational effectiveness in healthcare settings.
- This definition highlights that learning in this field is not only about gaining new information but also about applying it to enhance patient outcomes and advance nursing practices.
🔸2) Gantt chart
- A Gantt chart is a type of bar chart that visually represents a project schedule. It displays tasks or activities along the horizontal axis and time intervals along the vertical axis. Each task is represented by a horizontal bar whose length corresponds to the duration of the task. Gantt charts also show the start and end dates of each task, dependencies between tasks, milestones, and the overall project timeline. They are commonly used in project management to plan, schedule, and track progress, providing a clear and organized view of project activities and timelines.
🔸3) Formative evaluation
Formative evaluation
- Formative evaluation refers to a type of assessment conducted during the development or implementation of a program, course, or intervention. Its primary purpose is to provide ongoing feedback to improve and refine the process or content. Unlike summative evaluation, which measures the overall effectiveness at the end, formative evaluation focuses on identifying areas for improvement to enhance outcomes and effectiveness.
- Example:In a nursing education course, formative evaluation might include quizzes, peer reviews, and feedback sessions to help students understand and master the material before the final exam.
🔸4) Public relations
- Public relations
- is the strategic practice of managing and shaping the public image and communications of an organization, individual, or institution. It involves creating and maintaining positive relationships with various stakeholders through media relations, community engagement, and promotional activities to build a favorable reputation and achieve organizational goals.
Example: A hospital might use public relations to communicate new health initiatives, address community concerns, and promote positive stories about patient care.
🔸5) Collective bargaining
- Collective bargaining is a process whereby representatives of employees (often labor unions) negotiate with representatives of employers to establish terms and conditions of employment. This negotiation typically covers wages, working hours, benefits, workplace conditions, and other aspects of the employment relationship. The goal of collective bargaining is to reach a mutually agreed-upon contract or collective agreement that governs the working conditions and rights of employees within the organization or industry.
Q-2. Write short note (Any four)
🔸1) Inventory Control
- Inventory ControlIn the Management of Nursing Services and Education, inventory control is a critical function that ensures the efficient and effective use of resources within healthcare and educational settings. It involves a range of practices designed to manage the supply of medical equipment, medications, and educational materials.
Inventory Control
Definition: Inventory control in the management of nursing services and education is the systematic process of overseeing the acquisition, storage, and utilization of medical supplies, equipment, and educational resources. The objective is to maintain optimal inventory levels, minimize costs, prevent shortages or excesses, and ensure that resources are available to meet patient care and educational needs effectively.
Key Components:
1.Stock Monitoring: Regularly tracking inventory levels of medical supplies, medications, and educational materials to ensure they meet current needs without surplus. This involves using inventory management systems to monitor quantities, expiration dates, and usage rates.
2.Demand Forecasting: Analyzing trends and historical data to predict future needs for supplies and resources. Accurate forecasting helps in ordering the right quantities to avoid shortages or overstocking.
3.Ordering Procedures: Establishing efficient procedures for ordering new supplies, including selecting suppliers, negotiating prices, and placing orders. This involves maintaining good relationships with suppliers and ensuring timely deliveries.
4.Storage Management: Organizing and maintaining inventory storage areas to ensure that items are stored properly to prevent spoilage, contamination, or damage. This includes implementing procedures for safe storage and regular inventory checks.
5.Cost Control: Implementing strategies to manage and reduce inventory costs, including monitoring purchase prices, minimizing waste, and optimizing the use of resources.
Example: In a hospital setting, effective inventory control might involve using a computerized system to track medication levels, scheduling regular audits to ensure that supplies are not expired, forecasting future needs based on patient admission rates, and negotiating bulk purchase agreements to reduce costs.
Benefits:
Improved Patient Care: Ensures that necessary medical supplies and medications are available, which is crucial for providing high-quality patient care.
Cost Efficiency: Reduces excess inventory and lowers costs through better demand forecasting and procurement practices.
Resource Optimization:
Ensures that educational materials and medical resources are used efficiently, supporting both nursing education and patient care.
By effectively managing inventory, nursing service managers and educators can enhance operational efficiency, reduce costs, and ensure the availability of essential resources.
🔸2) Staffing
Definition:
Staffing in the management of nursing services and education refers to the strategic process of recruiting, selecting, training, and scheduling qualified personnel to ensure that healthcare facilities and educational institutions operate effectively. It encompasses the activities necessary to meet staffing needs, optimize team performance, and deliver high-quality patient care and educational outcomes.
Key Components:
1.Recruitment and Selection:
Recruitment: Identifying staffing needs based on patient care requirements or educational goals and attracting qualified candidates through job postings, networking, and outreach.
Selection:Evaluating candidates through interviews, background checks, and assessments to choose individuals who possess the necessary skills, experience, and qualifications.
2 Training and Development:
Orientation: Providing new hires with essential information about organizational policies, procedures, and expectations.
Ongoing Education: Offering continuous professional development opportunities to keep staff updated on best practices, new technologies, and regulatory changes.
3.Scheduling and Staffing Plans:
Scheduling: Creating work schedules that ensure adequate coverage for all shifts while considering staff availability, preferences, and legal requirements.
Workforce Planning: Developing long-term staffing strategies to address future needs, manage turnover, and adapt to changes in healthcare demands or educational programs.
4.Performance Management:
Evaluation: Monitoring and assessing staff performance through regular reviews, feedback, and performance appraisals.
Support: Providing support and resources for staff to address performance issues, improve skills, and achieve career goals.
5.Retention Strategies:
Job Satisfaction: Implementing initiatives to improve job satisfaction and morale, such as competitive compensation, recognition programs, and a supportive work environment.
Career Development: Offering opportunities for career advancement, mentorship, and professional growth to retain talented staff.
Example: In a nursing home, effective staffing involves recruiting registered nurses and nurse aides, providing them with initial training on patient care protocols, creating schedules that ensure 24/7 coverage, conducting regular performance reviews, and offering career development opportunities to prevent staff burnout and ensure high-quality care for residents.
Benefits:
Quality Patient Care: Ensures that there are enough qualified staff members to meet patient care needs, which leads to better health outcomes and patient satisfaction.
Effective Education: Supports the delivery of high-quality nursing education through competent instructors and well-structured training programs.
Operational Efficiency:Optimizes resource allocation, reduces costs associated with staff turnover, and ensures that staff workloads are manageable.
Challenges:
Recruitment Difficulties: Finding and attracting qualified candidates can be challenging due to high demand for healthcare professionals.
Staff Retention: Keeping staff motivated and engaged in a demanding work environment requires ongoing effort and resources.
By addressing these components, managers can ensure that staffing practices contribute to the effective functioning of nursing services and educational programs.
🔸3) Comparison between administration and management
Comparison Between Administration and Management
Administration and management are two distinct but interrelated functions within an organization, each playing a crucial role in its success.
Focus and Scope:
- Administration is primarily concerned with setting the overarching policies and strategic goals for the organization. Administrators focus on the long-term vision and direction, establishing the framework within which the organization operates. For instance, a hospital board might develop a five-year plan to expand services and improve patient care.
- Management, on the other hand, is focused on the implementation of these policies and managing daily operations. Managers handle the practical aspects of running the organization, ensuring that the day-to-day tasks align with the strategic objectives set by the administration. For example, a department manager in the hospital would organize staff schedules and oversee daily patient care to meet the board’s expansion goals.
Responsibilities:
- Administrators are responsible for high-level decision-making, which includes defining the organization’s mission, vision, and long-term strategies. They make decisions that shape the future of the organization and determine the resources needed for achieving strategic goals. For instance, administrators might decide to invest in new medical technologies or expand healthcare services.
- Managers handle the execution of these strategic plans. Their responsibilities include organizing resources, coordinating activities, and overseeing staff to ensure that operational goals are met. Managers address the immediate needs of the organization, such as managing budgets for departments or ensuring that medical supplies are adequately stocked.
Decision Making:
- The decision-making process for administrators involves making strategic, long-term decisions that impact the overall direction of the organization. These decisions are often complex and require a broad perspective on the organization’s future. For example, administrators might decide on entering new markets or forming partnerships with other healthcare providers.
- In contrast, managers make tactical decisions focused on the implementation of administrative policies and the resolution of daily operational issues. Their decisions are more focused on immediate and short-term concerns, such as resolving staff conflicts or improving workflow efficiencies.
Levels of Operation:
- Administration operates at the top level of the organizational hierarchy, often involving executives, board members, or senior leaders. Their role is to oversee the entire organization and ensure that it is on the right path to achieve its long-term objectives.
- Management operates at various levels throughout the organization, including middle management and lower management. Managers are responsible for carrying out the day-to-day operations and ensuring that the strategic goals set by administrators are implemented effectively.
Approach:
- Administrators take a strategic and future-oriented approach, focusing on setting goals and establishing policies that guide the organization’s direction. They work on conceptualizing the future of the organization and setting the vision for its growth.
- Managers take a practical, present-oriented approach. They focus on the implementation of policies and procedures, ensuring that operations run smoothly and efficiently on a daily basis. Their work involves solving current problems and making adjustments to achieve immediate objectives.
Skills and Competencies:
- Administrators require skills in strategic planning, policy development, and high-level decision-making. They must be able to envision the future of the organization and establish the frameworks necessary for its success.
- Managers need skills in operational planning, resource management, and staff supervision. They must effectively translate administrative goals into actionable plans and manage resources and personnel to achieve those plans.
Example in a Healthcare Setting:
- In a hospital, the administration might be responsible for setting strategic goals such as expanding patient services or improving community health outreach. They would focus on the vision and long-term plans for the hospital’s growth. Managers, on the other hand, would be responsible for the day-to-day implementation of these goals, such as organizing staff schedules, managing patient care processes, and handling operational challenges.
🔸4) Principles of Evaluation.
- Evaluation is a systematic process used to assess the effectiveness, efficiency, and impact of programs, projects, or initiatives. Here are key principles of evaluation that guide the process:
- 1.Utility
Definition: The evaluation should be designed to meet the needs of stakeholders and provide relevant information for decision-making.
Explanation: Evaluation must serve the interests of those involved in or affected by the program, such as funders, participants, or policymakers. It should generate findings that are useful for improving the program or informing future decisions.
Example: A health program evaluation might focus on providing data that helps healthcare managers make decisions about resource allocation or program modifications.
- 2.Feasibility
Definition: The evaluation should be practical and achievable within the constraints of time, budget, and resources.
Explanation: Evaluations must be designed to work within the limits of available resources and should be manageable for the evaluators and stakeholders.
Example: If a school wants to evaluate a new teaching method, the evaluation plan should account for the time teachers have available and the budget for collecting and analyzing data.
- 3.Propriety
Definition: The evaluation should be conducted in an ethical manner and respect the rights of participants.
Explanation: Evaluations should uphold ethical standards, including obtaining informed consent, ensuring confidentiality, and conducting the evaluation with integrity and fairness.
Example: In evaluating a nursing training program, evaluators must ensure that participants’ personal data is kept confidential and that they are fully informed about the study’s purpose and procedures.
- 4.Accuracy
Definition: The evaluation should produce reliable and valid findings.
Explanation: Evaluations must employ appropriate methods and techniques to ensure that the data collected is accurate and that conclusions drawn are based on sound evidence.
Example: A health intervention’s effectiveness should be measured using validated tools and methods to ensure that the results accurately reflect the impact of the intervention.
- 5.Systematic Approach
Definition: The evaluation process should be organized and structured.
Explanation: Evaluations should follow a systematic approach, including defining objectives, developing a plan, collecting data, analyzing results, and reporting findings in a structured manner.
Example: An educational program evaluation might follow a structured process including setting clear objectives, designing an evaluation framework, collecting feedback from students and teachers, analyzing the results, and documenting the findings.
- 6.Inclusiveness
Definition: The evaluation should consider the perspectives of all relevant stakeholders.
Explanation: To ensure a comprehensive assessment, the evaluation should incorporate feedback from various stakeholders, including those directly involved in the program and those affected by it.
Example:When evaluating a community health initiative, feedback should be gathered from health workers, patients, community members, and funders to get a full picture of the program’s impact.
- 7.Clarity
Definition: The evaluation goals, methods, and findings should be clearly defined and communicated.
Explanation: All aspects of the evaluation should be clearly articulated so that stakeholders can understand the purpose, process, and outcomes of the evaluation.
Example: The evaluation report of a new public health policy should clearly explain the methods used, the findings, and their implications for future policy decisions.
- 8.Timeliness
Definition: The evaluation should be conducted in a timely manner to ensure that findings are relevant and useful.
Explanation: Evaluations should be completed within a timeframe that ensures the findings are relevant for decision-making and that recommendations can be implemented.
Example: An evaluation of a seasonal health campaign should be completed before the next campaign cycle to allow for improvements based on the findings.
- 9.Ethical Considerations
Definition: Evaluations should adhere to ethical principles, ensuring fairness and respect for all involved.
Explanation: Ethical evaluation practices involve honesty, respect for participants, and avoiding conflicts of interest.
Example: Evaluators should avoid biases in their analysis and reporting and ensure that participants are treated with respect and dignity throughout the evaluation process.
- 10.Sustainability
Definition: The evaluation should consider the long-term impacts and sustainability of the program or initiative.
Explanation: Evaluations should not only assess current effectiveness but also explore whether the program’s benefits can be maintained over time.
Example: Evaluators of a community development project might assess not only the immediate outcomes but also the potential for long-term community benefits and ongoing success.
By adhering to these principles, evaluators can ensure that their assessments are effective, ethical, and useful for all stakeholders involved.
🔸5) Staff Development
Definition: Staff development refers to a comprehensive process designed to enhance the skills, knowledge, and capabilities of employees to improve their performance and support the organization’s goals. It involves planned activities and programs aimed at professional growth, career advancement, and improving job effectiveness.
Key Components of Staff Development:
- 1.Training Programs:
Training programs provide employees with the specific skills and knowledge needed to perform their current job roles effectively. These programs can include workshops, seminars, and online courses focused on both technical skills and soft skills.
Example: A hospital might offer training workshops on the latest medical technologies or patient care techniques to ensure that nurses and doctors stay up-to-date with industry advancements.
- 2.Professional Development:
Professional development includes opportunities for employees to advance their careers through activities like obtaining certifications, attending conferences, or participating in mentorship programs. It helps employees prepare for future roles and responsibilities.
Example: A nursing staff member might be encouraged to pursue advanced certifications or attend professional conferences to enhance their expertise and career prospects.
- 3.Performance Appraisals:
Performance appraisals involve regular evaluations of employees’ job performance to identify strengths, weaknesses, and areas for improvement. These evaluations are used to set development goals and provide feedback.
Example: A manager might conduct annual performance reviews to assess an employee’s progress, discuss development goals, and provide constructive feedback for improvement.
- 4.Mentorship and Coaching:
Mentorship and coaching involve experienced professionals guiding less experienced staff members. Mentors provide advice, support, and feedback, while coaches work on specific skills and performance improvement.
Example: A senior nurse might mentor a new nurse by providing guidance on patient care strategies and offering support during the initial months of their role.
- 5.Educational Opportunities:
Offering access to further education, such as degree programs or specialized courses, supports employees in gaining advanced knowledge and skills related to their profession.
Example: An organization might provide tuition reimbursement for employees pursuing advanced degrees in healthcare management or nursing.
- 6.Career Planning:
Career planning helps employees set long-term career goals and develop a pathway to achieve them. It includes discussions about career aspirations, skill gaps, and potential career advancement opportunities.
Example: A healthcare administrator might work with employees to create individual career development plans, setting goals for promotions or shifts into different specialties.
- 7.Knowledge Sharing:
Knowledge sharing involves creating opportunities for employees to share their expertise and learn from each other through activities like team meetings, internal workshops, and collaborative projects.
Example: In a nursing department, staff might hold regular meetings to discuss best practices, share experiences, and learn from one another’s successes and challenges.
- 8.Leadership Development:
Leadership development focuses on preparing employees for future leadership roles. This can include training on management skills, decision-making, and strategic thinking.
Example: A management program for emerging leaders might cover topics such as conflict resolution, team building, and strategic planning for future leadership roles.
Benefits of Staff Development:
1.Improved Job Performance: Staff development programs enhance employees’ skills and competencies, leading to better job performance and higher quality work.
2.Increased Employee Satisfaction: Providing opportunities for growth and advancement increases job satisfaction, motivation, and morale among employees.
3.Career Advancement: Development programs help employees achieve their career goals, preparing them for promotions and new roles within the organization.
4.Organizational Effectiveness: Well-trained and developed staff contribute to the overall effectiveness and success of the organization by improving productivity and achieving strategic objectives.
5.Retention of Talent: Investing in staff development helps retain talented employees by demonstrating a commitment to their professional growth and career advancement.
Challenges in Staff Development:
- 1.Resource Constraints:
Effective staff development requires time, money, and resources, which can be challenging for organizations with limited budgets.
- 2.Resistance to Change:
Employees may resist development efforts due to fear of change, perceived additional workload, or lack of confidence in their abilities.
- 3.Measuring Effectiveness:
Evaluating the impact of staff development programs can be difficult, as it involves assessing long-term outcomes and changes in performance.
Example in a Healthcare Setting: In a healthcare organization, staff development might involve a variety of initiatives such as offering continuing education for nurses, implementing a mentorship program for new healthcare professionals, and providing leadership training for senior staff to prepare them for future executive roles.
By focusing on these components, organizations can create effective staff development programs that support both individual growth and organizational success.
Q-3. Write Essay on Following (Any One)
🔸1) Explain recruitment procedure in detail.
- The recruitment procedure is a structured process used to identify, attract, and select suitable candidates for job openings within an organization. It involves several stages designed to ensure that the best candidates are chosen for the role. Here is a detailed explanation of each step in the recruitment procedure:
- 1.Identifying Recruitment Needs
Definition: Determining the necessity for a new hire based on current and future staffing requirements.
Steps: Assess Staffing Requirements: Analyze the current workforce and identify gaps or additional needs. This can be due to growth, replacement, or new projects.
Job Analysis: Review job descriptions, responsibilities, and required qualifications to determine the skills and experience needed for the role.
Example: A hospital might identify a need for additional nurses due to increased patient admissions and determine the qualifications required for the role.
- 2.Developing a Job Description and Person Specification
Definition: Creating documents that outline the role’s duties and the qualifications required.
Steps:
Job Description: Write a detailed description of the job’s duties, responsibilities, and reporting relationships. This should include job title, main tasks, and work environment.
Person Specification: Define the qualifications, skills, experience, and personal attributes required for the position. This includes educational requirements, professional experience, and specific competencies.
Example: The job description for a new nurse might include responsibilities like patient care and administering medication, while the person specification might include a nursing degree and relevant clinical experience.
- 3.Advertising the Vacancy
Definition: Communicating the job opening to potential candidates through various channels.
Steps:
Choose Advertising Channels: Select appropriate platforms such as job boards, company website, social media, and professional networks.
Create a Job Ad: Develop an engaging job advertisement that includes the job description, person specification, and application instructions.
Example: A clinic might advertise a new administrative position on a job portal, its website, and LinkedIn to reach a broad audience of potential candidates.
- 4.Receiving and Screening Applications
Definition: Collecting and reviewing applications to shortlist candidates.
Steps:
Collect Applications: Gather applications through the chosen channels.
Screen Applications: Review resumes and cover letters to ensure candidates meet the minimum qualifications and select those who best fit the job requirements.
Example: For a new IT support role, the HR department might screen resumes for relevant technical skills and experience before selecting candidates for interviews.
- 5.Conducting Interviews
Definition: Evaluating candidates through structured conversations to assess their suitability.
Steps: Interview Planning: Schedule interviews, prepare questions, and decide on the interview format (one-on-one, panel, etc.).
Conduct Interviews: Ask questions related to the candidate’s experience, skills, and fit for the role. Use behavioral or situational questions to gauge competencies.
Example: A healthcare administrator might interview candidates for a new administrative role by asking about their experience managing office tasks and handling patient inquiries.
- 6.Administering Selection Tests
Definition: Using tests to assess specific skills or abilities relevant to the job.
Steps:
Design Tests: Create or select tests that measure relevant skills, such as technical abilities, problem-solving, or personality traits.
Administer Tests: Conduct the tests as part of the selection process and evaluate results to inform decision-making.
Example: For a nursing position, candidates might be given a practical skills test to demonstrate their clinical competencies.
- 7.Checking References
Definition: Verifying the candidate’s background and previous work experience through references.
Steps:
Request References: Ask the candidate to provide contact details for previous employers or professional references.
Contact References: Reach out to references to confirm the candidate’s work history, performance, and professional behavior.
Example: An HR manager might contact a candidate’s previous supervisor to discuss their job performance and reliability.
- 8.Making a Job Offer
Definition: Extending an official offer to the selected candidate.
Steps:
Prepare Offer Letter: Draft a formal offer letter that includes details of the job position, salary, benefits, and start date.
Extend the Offer: Contact the selected candidate to offer the position and provide them with the offer letter for their review and acceptance.
Example: After selecting the best candidate for a new teaching position, a school principal might send an offer letter outlining the job details and terms of employment.
- 9.Onboarding and Induction
Definition: Integrating the new employee into the organization.
Steps:
Prepare Onboarding Program: Develop a plan for introducing the new employee to the organization, including orientation sessions, training, and initial tasks.
Conduct Induction: Welcome the new hire, provide necessary training, and introduce them to the team and organizational culture.
Example: A new nurse might go through an orientation program that includes hospital tours, introduction to policies, and initial training on patient care procedures.
- 10.Evaluating the Recruitment Process
Definition: Assessing the effectiveness of the recruitment process for future improvements.
Steps: Gather Feedback: Collect feedback from candidates, interviewers, and other stakeholders.
Analyze Outcomes: Review the recruitment process to identify successes and areas for improvement.
Example: After hiring a new employee, the HR team might survey interviewers and the new hire to assess how well the recruitment process worked and make adjustments for future hires.
- Benefits of a Well-Managed Recruitment Procedure:
Attracts Qualified Candidates: A structured process helps attract candidates who are well-suited for the role.
Ensures Fairness: A clear and consistent process ensures that all candidates are evaluated fairly.
Reduces Turnover: Effective recruitment leads to better hires, which can reduce employee turnover and associated costs.
Improves Organizational Performance: By hiring the right people, the organization can improve its overall performance and achieve its objectives.
- Challenges in the Recruitment Procedure:
Time-Consuming: Recruitment can be a lengthy process, requiring significant time and resources.
Competition for Talent: Attracting qualified candidates in competitive job markets can be challenging.
Ensuring Objectivity: Avoiding biases and ensuring a fair evaluation of all candidates can be difficult.
By following these steps, organizations can develop an effective recruitment procedure that helps in selecting the best candidates and supporting long-term success.
🔸2) Current issues and trends in nursing practice
The field of nursing is continually evolving to address emerging challenges and incorporate advancements in healthcare. Here is a detailed overview of current issues and trends shaping nursing practice today:
- 1.Nursing Shortages
Issue: There is a significant and growing shortage of nurses across the globe, exacerbated by an aging population, high burnout rates, and insufficient numbers of new nurses entering the profession.
Trends: Increased Recruitment Efforts: Healthcare institutions are implementing aggressive recruitment strategies, including offering sign-on bonuses and tuition reimbursement.
Expansion of Nursing Education Programs: Schools are increasing the number of nursing programs and offering accelerated degree options to address the shortage.
International Recruitment: Some countries are looking abroad to fill nursing vacancies, leading to increased international mobility for nurses.
Example: In the U.S., projections indicate that there will be a shortage of up to 1.2 million nurses by 2030, prompting initiatives to expand nursing education and streamline licensing processes.
- 2.Burnout and Mental Health Issues
Issue: High levels of burnout and stress among nurses due to increased workloads, long hours, and high patient-to-nurse ratios are major concerns.
Trends:
Focus on Mental Health Support: Institutions are beginning to offer mental health resources, counseling services, and stress management programs for nurses.
Work-Life Balance Initiatives: There is a growing emphasis on improving work-life balance through flexible scheduling and reduced overtime requirements.
Wellness Programs: Programs aimed at physical and emotional well-being, such as yoga sessions or mindfulness training, are being introduced.
Example: In response to burnout exacerbated by the COVID-19 pandemic, many hospitals have expanded their employee assistance programs and offered mental health support services.
- 3.Advancements in Technology
Issue: The rapid advancement of healthcare technologies and the integration of electronic health records (EHRs) pose both opportunities and challenges for nurses.
Trends:
Telehealth and Remote Monitoring: The use of telehealth platforms and remote patient monitoring systems has become increasingly common.
Electronic Health Records: Continued adoption and optimization of EHR systems for better patient management and data accuracy.
AI and Robotics: Emerging technologies like artificial intelligence for diagnostics and robotic systems for surgery and patient care are being explored.
Example: Telehealth services surged during the COVID-19 pandemic, with many healthcare providers and patients using virtual appointments for consultations and follow-ups.
- 4.Increased Emphasis on Evidence-Based Practice
Issue: There is a growing need for nursing practices to be grounded in the best available evidence to improve patient outcomes.
Trends: Integration of Research into Practice:
Emphasis on incorporating research findings into clinical practice to ensure that care is effective and up-to-date.
Educational Programs Focused on Evidence-Based Practice: Nursing curricula are increasingly focused on teaching evidence-based practice methodologies.
Research and Quality Improvement Initiatives: There is a push for nurses to participate in research and quality improvement projects.
Example: Evidence-based guidelines for managing chronic diseases like diabetes are being actively developed and updated based on the latIssue: There is a strong movement towards providing care that respects and responds to individual patient preferences, needs, and values.
Trends:
Patient Engagement: Initiatives to involve patients in decision-making about their care plans and treatment options.
Holistic Care Models: Adoption of models that consider the physical, emotional, and social aspects of patient care.
Patient Satisfaction Metrics: Increased focus on patient satisfaction as a key performance indicator for healthcare services.
Example: Many hospitals are implementing patient-centered care models that include patient feedback mechanisms and involve patients in the development of their care plans.
- 6.Advanced Practice Roles
Issue: The expanding scope of advanced practice roles is transforming the traditional roles of nurses.
Trends:
Growth of Nurse Practitioners (NPs) and Clinical Nurse Specialists (CNSs):
Expansion of advanced practice roles to address gaps in primary care and specialized services.
Legislative Changes: Increasing efforts to pass legislation that grants NPs full practice authority and supports advanced practice roles.
Expansion of Roles: Advanced practice nurses are taking on roles traditionally reserved for physicians, such as diagnosing conditions and prescribing medications.
Example: Nurse practitioners in many states now have full practice authority, allowing them to operate independently from physicians in providing primary care.
- 7.Interprofessional Collaboration
Issue: Effective teamwork among healthcare professionals is crucial for improving patient care and outcomes.
Trends:
Interprofessional Education: Emphasis on training healthcare professionals to work collaboratively across disciplines.
Collaborative Care Models: Development of care models that promote communication and cooperation among physicians, nurses, and other healthcare providers.
Shared Decision-Making: Encouragement of shared decision-making processes involving multiple healthcare professionals.
Example: Many healthcare facilities are adopting collaborative care teams where nurses, doctors, and other professionals work together to create comprehensive treatment plans.
- 8.Diversity, Equity, and Inclusion
Issue: Addressing issues of diversity, equity, and inclusion in the nursing workforce and patient care.
Trends:
Diversity Initiatives: Efforts to recruit and retain a diverse nursing workforce to better reflect and serve diverse patient populations.
Cultural Competency Training: Programs focused on improving cultural competency and reducing health disparities.
Equitable Access to Care: Strategies aimed at ensuring all patients have equal access to healthcare services.
Example: Hospitals are implementing diversity and inclusion training programs to foster a more inclusive environment for both patients and staff.
- 9.Regulatory and Policy Changes
Issue: The evolving healthcare regulatory environment affects nursing practice.
Trends:
Policy Advocacy: Nurses are becoming more involved in healthcare policy advocacy to influence legislation and regulations affecting the nursing profession.
Regulatory Reforms: Changes in regulations related to nurse staffing ratios, scope of practice, and accreditation standards.
Compliance Requirements: Adherence to updated regulations and standards for quality care and patient safety.
Example: The recent push for legislative changes to improve nurse staffing ratios in hospitals reflects a broader trend towards advocating for better working conditions and patient outcomes.
- 10.Focus on Chronic Disease Management
Issue: The increasing prevalence of chronic diseases requires a shift in care strategies.
Trends:
Chronic Disease Programs: Development of comprehensive management programs for diseases like diabetes, heart disease, and asthma.
Patient Education: Initiatives aimed at educating patients on self-management techniques and preventive care.
Coordination of Care: Enhanced approaches for coordinating care across different healthcare providers and settings.
Example: Chronic disease management programs often include patient education, regular monitoring, and coordinated care plans to help manage conditions like diabetes or hypertension.
🔸Section B🔸
Q-4. Write Essay on Following
🔸Define In-service education. Prepare plan for in-service programme education of 20 staff nurses working in your hospital.
Definition of In-Service Education
- In-Service Education refers to a structured, ongoing educational program designed for employees to enhance their skills, knowledge, and professional development while they are actively engaged in their job roles. This type of education aims to improve job performance, update staff on new practices or technologies, and ensure that employees are up-to-date with the latest standards and protocols in their field.
- Key Objectives of In-Service Education:
1 Skill Enhancement: To improve and update the clinical and non-clinical skills of staff.
2.Knowledge Updates: To provide current information on best practices, new technologies, and evolving standards in healthcare.
3.Professional Development: To support career growth and development opportunities for staff.
4.Quality Improvement: To improve patient care and organizational efficiency.
5.Compliance: To ensure adherence to legal, regulatory, and institutional requirements.
Plan for In-Service Education Program for 20 Staff Nurses
Objective: To enhance the clinical skills, knowledge base, and professional development of 20 staff nurses working in the hospital.
Duration: 6 months
Format: A combination of workshops, seminars, hands-on training, and online modules.
- 1.Needs Assessment
Activities:Conduct a survey to identify specific learning needs and interests of the staff nurses.
Review recent performance evaluations and feedback to identify areas for improvement.
Consult with department heads to determine critical training needs based on patient care and operational goals.
Timeline: Week 1
Responsibilities:
- In-Service Coordinator
- Department Heads
Example Questions for Survey: What are the key areas where you feel additional training would be beneficial?
- Are there any new technologies or procedures you would like more information on?
- What types of training formats do you prefer (workshops, online courses, etc.)?
- 2.Developing the Curriculum
Activities: Based on the needs assessment, design a curriculum that addresses identified training gaps.
Create a schedule for training sessions and select appropriate trainers or facilitators.
Timeline: Week 2
Responsibilities:
- In-Service Coordinator
- Subject Matter Experts (SMEs)
Example Curriculum Topics:
- Advanced Patient Care Techniques
- Updated Infection Control Practices
- Emergency Response and First Aid
- Ethical and Legal Issues in Nursing
- Effective Communication Skills
- Time Management and Stress Reduction
- Implementation of Training Sessions
Activities:
- Conduct workshops, seminars, and hands-on training sessions.
- Deliver online modules for self-paced learning.
- Provide materials and resources for each training session.
Timeline: Weeks 3-20
Responsibilities:
- Trainers/Facilitators
- In-Service Coordinator
Training Methods:
Workshops: Interactive sessions led by experienced nurses or external experts.
Seminars: Presentations and discussions on new topics or updates in nursing practice.
Hands-On Training: Practical sessions in simulation labs or clinical settings.
Online Modules: Self-paced learning with quizzes and assignments.
- Evaluation of the Program
Activities: Collect feedback from participants on the effectiveness of the training.
Assess the impact of the training on job performance and patient care.
Review the achievement of learning objectives and adjust future programs based on feedback.
Timeline: Week 21
Responsibilities:
In-Service Coordinator
Staff Nurses
- Evaluation Methods:
Feedback Surveys:
Collect opinions on the content, delivery, and relevance of the training sessions.
Pre- and Post-Tests: Assess knowledge gained and changes in skills.
Observation: Evaluate improvements in clinical practice and patient care.
Performance Metrics: Review changes in performance evaluations and patient care outcomes.
Sample Feedback Questions:
- How useful was the training in improving your skills?
- Were the training materials and resources adequate?
- Did you feel that the training met your professional development needs?
- Reporting and Continuous Improvement
Activities:
- Prepare a report summarizing the program outcomes and areas for improvement.
- Share findings with staff and management to inform future training initiatives.
- Update the training plan based on feedback and performance metrics.
Timeline: Week 22
Responsibilities:
In-Service Coordinator
Department Heads
Report Content:
Summary of Training Activities: Overview of sessions held and topics covered.
Participant Feedback: Summary of feedback from staff nurses.
Impact Assessment: Analysis of changes in performance and patient care.
Recommendations: Suggestions for future in-service education programs.
Example Report Sections:
- Introduction
- Training Activities and Attendance
- Participant Feedback Summary
- Impact on Performance
- Recommendations for Future Programs
This detailed plan for an in-service education program for 20 staff nurses covers the essential steps from identifying needs to evaluating the program. By following this plan, you can ensure that the in-service education is effective, relevant, and beneficial for both the staff and the patients they care for.
By addressing these aspects, the program can enhance the skills of staff nurses, improve patient care, and contribute to the overall effectiveness of the healthcare organization.
Q-5. Write short note (Any Four)
🔸1) Methods of Supervision
Methods of Supervision in Nursing
Supervision in nursing
is crucial for maintaining high standards of patient care, supporting staff development, and ensuring adherence to protocols. Here are the primary methods of supervision used in nursing, each with a description of its purpose, benefits, and challenges.
- Direct Supervision
Definition: Direct supervision involves the supervisor being physically present to observe, guide, and assess staff performance in real-time.
Methods:
On-the-Job Observation: Supervisors watch staff during patient care activities and provide immediate feedback.
Clinical Rounds: Regular visits to various departments or units to monitor staff performance and patient care quality.
Shadowing: The supervisor works alongside staff to offer real-time guidance and support.
Benefits:
- Immediate correction of errors and real-time feedback.
- Direct assessment of staff performance and patient interactions.
- Challenges:Time-consuming and can be perceived as intrusive.
- Does not account for performance during unsupervised periods.
Example: A nurse manager conducts daily rounds to observe patient care practices and address any issues.
- Indirect Supervision
Definition: Indirect supervision involves oversight through methods that do not require physical presence at the time of care.
Methods:
Reviewing Documentation: Supervisors assess patient records, care plans, and incident reports to evaluate care quality.
Performance Audits: Regular audits of clinical practices, medication administration, and adherence to protocols.
Performance Reviews: Periodic evaluations of staff performance based on documented evidence and feedback.
Benefits:Provides a comprehensive view of staff performance over time.
Less intrusive compared to direct supervision.
Challenges:
- May not capture real-time issues or immediate patient care situations.
- Limited to documented evidence, which might not reflect actual performance.
Example: Reviewing patient charts to ensure accurate documentation and adherence to care protocols.
- Peer Supervision
Definition: Peer supervision involves staff members supporting and reviewing each other’s performance.
Methods:
Peer Review: Staff members review and discuss each other’s performance and patient care strategies.
Mentorship Programs: Experienced staff provide guidance and support to less experienced colleagues.
Benefits:
- Encourages a supportive work environment and collaborative learning.
- Promotes sharing of knowledge and best practices among peers.
Challenges:
- Potential for conflicts of interest and less objective evaluations.
- May not address all performance issues effectively.
Example: A senior nurse mentoring a junior nurse and providing feedback on patient care practices.
- Self-Supervision
Definition: Self-supervision encourages staff to evaluate and improve their own performance.
- Methods:
Self-Assessment Tools: Tools or questionnaires for staff to assess their own skills and identify areas for improvement.
Reflective Practice: Encouraging staff to reflect on their experiences and learning.
Benefits:
- Promotes self-awareness and professional growth.
- Encourages continuous self-improvement.
Challenges:
- Less objective and may overlook personal weaknesses.
- Requires a high level of self-discipline and honesty.
Example: Nurses using self-assessment checklists to evaluate their adherence to care standards and identify improvement areas.
- Group Supervision
Definition: Group supervision involves addressing staff performance and development in a group setting.
Methods:
Team Meetings: Regular meetings to discuss patient care issues, share updates, and address concerns.
Case Conferences: Group discussions on specific patient cases to review care plans and outcomes.
Educational Workshops: Group sessions focused on skill development and knowledge enhancement.
Benefits:
- Facilitates shared learning and problem-solving.
- Provides a platform for open discussion and collective decision-making.
Challenges:
- Individual issues may not be fully addressed.
- Group dynamics can influence the effectiveness of the supervision.
Example: Holding a monthly team meeting to discuss patient care strategies and review clinical practices.
🔸2) Patient assignment method
Patient Assignment Methods in Nursing
- Patient assignment is a crucial component of nursing management that involves allocating patients to nursing staff based on various factors to ensure effective and efficient care. Understanding different patient assignment methods helps in managing nursing resources and improving patient outcomes.
- Functional Nursing Assignment
Definition: Functional nursing involves assigning specific tasks to nursing staff based on their functions rather than assigning entire patients to individual nurses. Each nurse performs a designated role such as administering medications, taking vital signs, or managing wound care.
- Benefits:
Specialization: Allows nurses to focus on specific tasks, improving efficiency.
Coverage: Ensures that all essential nursing functions are performed.
Efficiency: Streamlines care processes through role specialization.
- Challenges:
Fragmentation: May lead to fragmented patient care and lack of continuity.
Nurse Satisfaction: May reduce job satisfaction due to repetitive tasks.
Example: One nurse handles medication administration for all patients, while another manages patient hygiene and another monitors vital signs.
- Primary Nursing Assignment
Definition: In primary nursing, one nurse is responsible for the care of a specific patient throughout their hospital stay, providing continuity of care.
- Benefits:
Continuity of Care: One nurse provides consistent care, fostering a therapeutic nurse-patient relationship.
Accountability: The primary nurse is accountable for all aspects of the patient’s care plan.
- Challenges:
Workload: Can lead to high workloads for the primary nurse, especially in busy units.
Coverage Issues: Requires coverage for the primary nurse during breaks and absences.
Example: A nurse assigned as the primary nurse for a patient manages all aspects of the patient’s care plan, including daily assessments and coordination with other healthcare providers.
- 3.Team Nursing Assignment
Definition: Team nursing involves a team of nurses with different skills working together to care for a group of patients, with one nurse acting as the team leader.
Benefits:
Collaborative Care: Encourages teamwork and allows for the sharing of knowledge and skills.
Flexibility: Allows for the distribution of tasks based on individual team members’ strengths.
- Challenges:
Coordination: Requires effective communication and coordination among team members.
Leadership: Relies on the team leader’s ability to manage and delegate tasks effectively.
Example: A team led by a charge nurse might include RNs, LPNs, and nursing assistants working together to care for all patients on a unit.
- Patient-Care Assignment
Definition: Patient-care assignment refers to the method where nurses are assigned a set number of patients to manage their care on a day-to-day basis.
Benefits:
Structured Care: Provides a clear structure for managing patient care assignments.
Direct Accountability: Nurses are responsible for all aspects of care for their assigned patients.
Challenges:
Balanced Workload: Ensuring that patient assignments are balanced in terms of patient acuity and nurse workload.
Responsibility: Nurses must manage diverse patient needs and coordinate with other healthcare professionals.
Example: A nurse is assigned five patients and is responsible for administering medications, monitoring vital signs, and coordinating with doctors for those five patients.
- Case Management Nursing
Definition: Case management nursing involves assigning a nurse to oversee the entire care process for a specific group of patients, focusing on outcomes and efficient care.
- Benefits:
Coordination:
Ensures comprehensive care by coordinating between patients, families, and healthcare providers.
Outcome Focused: Aims to improve patient outcomes through effective care planning and resource management.
- Challenges:
Complexity: Requires managing complex patient needs and coordinating multiple services.
Resource Intensive: May require additional resources and time for managing cases effectively.
Example: A case manager nurse oversees a patient’s care from admission to discharge, coordinating with specialists, and managing care transitions.
🔸3) Nursing Audit
Definition: A nursing audit is a systematic and formal evaluation of nursing practices and patient care to ensure adherence to established standards and identify areas for improvement. It aims to assess the quality of care provided, ensure compliance with guidelines, and support continuous improvement in nursing services.
- Types of Nursing Audits:
1.Clinical Audits: Clinical audits focus on reviewing patient care against established clinical standards. This type of audit evaluates whether nursing practices meet specific criteria related to patient care and outcomes. For instance, a clinical audit might review how effectively nurses manage wound care according to best practices.
Benefits: Clinical audits help identify gaps in care and ensure that best practices are followed to improve patient outcomes.
Challenges: These audits can be time-consuming and may face resistance from staff who perceive them as a form of criticism.
2.Process Audits: Process audits evaluate the procedures and methods used in patient care. They examine whether nursing tasks and processes are performed correctly according to established protocols. For example, a process audit might assess whether hand hygiene practices are consistently followed.
Benefits: Process audits help ensure that procedures are executed as intended and can reveal inefficiencies or deviations from standards.
Challenges: They require careful observation and documentation, and may be resource-intensive.
3.Outcome Audits: Outcome audits focus on the results of nursing interventions and care. They assess whether the desired patient outcomes, such as recovery rates or reduced infection rates, are achieved. An example would be auditing patient outcomes for those receiving diabetes management care.
Benefits: These audits measure the effectiveness of care interventions and help identify areas for improvement based on patient outcomes.
Challenges: Measuring outcomes can be complex and may involve factors beyond the control of nursing care alone.
4.Compliance Audits:
Compliance audits ensure that nursing practices adhere to legal, ethical, and organizational regulations. These audits review documentation, policies, and procedures to ensure all practices comply with relevant standards. For example, a compliance audit might check if patient confidentiality is maintained according to legal requirements.
Benefits: Compliance audits help ensure that nursing practices meet legal and ethical standards, reducing the risk of violations.
Challenges: Keeping up with changing regulations and maintaining thorough documentation can be demanding.
- Steps in Conducting a Nursing Audit:
The audit process generally involves several key steps:
Planning: Define the objectives of the audit, select the standards for evaluation, and prepare an audit plan.
Collecting Data: Gather information through methods like chart reviews, observations, and staff interviews.
Analyzing Data: Compare the collected data against the established standards to identify discrepancies and areas for improvement.
Reporting Results: Document findings, highlighting strengths and weaknesses, and provide recommendations for improvement.
Implementing Changes: Develop and execute an action plan based on the audit findings to address identified issues.
Reviewing Process: Evaluate the effectiveness of the changes and make necessary adjustments for ongoing improvement.
Benefits of Nursing Audits:Nursing audits improve patient care by identifying and addressing gaps in practices, ensuring compliance with standards, and fostering a culture of continuous improvement. They provide valuable feedback for staff development and support organizational goals.
Challenges of Nursing Audits: Challenges include potential resistance from staff, the need for significant time and resources, and the complexity of maintaining objectivity and thoroughness in the audit process.
Example: An example of a nursing audit might involve reviewing how well nurses follow infection control procedures by observing hand hygiene practices and checking compliance with protocols. The audit might reveal that while most nurses follow hand hygiene protocols, there are areas where adherence is inconsistent, leading to targeted training to address these gaps
🔸4) Job description of nursing tutor
- A nursing tutor plays a vital role in nursing education, focusing on developing the next generation of nurses by teaching theoretical concepts, guiding practical skills, and supporting student learning. Here’s a detailed job description for a nursing tutor, outlining key responsibilities, qualifications, and skills required for the role.
Job Title: Nursing Tutor
Job Summary:
- A Nursing Tutor is responsible for delivering educational content, facilitating clinical practice, and supporting nursing students through their academic and professional development. The role involves creating a conducive learning environment, assessing student performance, and ensuring that educational programs meet established nursing standards.
Key Responsibilities:
1.Teaching and Instruction:
Deliver Lectures: Present theoretical concepts in nursing, including subjects such as medical-surgical nursing, pharmacology, and nursing ethics.
Conduct Practical Sessions: Oversee and guide students during clinical practice, including skills labs, simulation exercises, and patient care scenarios.
Develop Curriculum: Assist in designing and updating course content, learning objectives, and assessment methods in alignment with nursing standards and regulatory requirements.
2.Student Support:
Academic Advising: Provide academic and career advice to students, helping them navigate their educational path and set professional goals.
Mentoring: Offer guidance and support to students to foster their personal and professional growth. Address academic or clinical concerns and provide feedback.
3.Assessment and Evaluation:
Design Assessments: Create and administer exams, quizzes, and practical assessments to evaluate student knowledge and skills.
Evaluate Performance: Assess student performance through grading assignments, providing constructive feedback, and documenting progress.
4.Administrative Duties:
Maintain Records: Keep accurate records of student attendance, grades, and performance evaluations.
Participate in Meetings: Attend faculty meetings, contribute to discussions on program development, and engage in departmental activities.
5.Professional Development:
Stay Updated: Keep abreast of advancements in nursing practice, educational techniques, and healthcare regulations.
Attend Workshops: Participate in professional development opportunities, including workshops, conferences, and training sessions.
6.Collaboration:
Work with Healthcare Facilities: Collaborate with hospitals, clinics, and other healthcare settings to arrange clinical placements and ensure that students receive quality learning experiences.
Engage with Colleagues: Work collaboratively with other educators, staff, and professionals to enhance the educational program and address institutional needs.
- Qualifications:
Educational Requirements:
- A Master’s degree in Nursing (MSN) or a Doctoral degree (DNP, PhD) is preferred.
- A Bachelor’s degree in Nursing (BSN) is required.
- Current and active Registered Nurse (RN) license.
Experience Requirements:
- A minimum of 2-3 years of clinical nursing experience.
- Prior teaching experience or a background in nursing education is preferred.
Skills and Competencies:
Teaching Skills: Ability to effectively convey complex nursing concepts and facilitate engaging learning experiences.
Clinical Expertise: Strong clinical background to guide students in practical settings and provide relevant real-world examples.
Communication Skills: Excellent verbal and written communication skills for interacting with students, colleagues, and healthcare professionals.
Organizational Skills: Ability to manage multiple responsibilities, including teaching, assessment, and administrative tasks.
Mentoring Abilities: Skills in providing guidance, feedback, and support to foster student development.
- Working Conditions:
Environment: Primarily based in educational institutions such as nursing schools or colleges, with occasional clinical site visits.
Hours: Typically involves a combination of classroom hours, clinical practice supervision, and administrative duties. May require flexible hours based on the academic schedule.
Example of Daily Activities:
- Delivering a lecture on advanced nursing techniques.
- Observing and evaluating students during a clinical skills lab.
- Meeting with students for academic advising and career counseling.
- Updating course materials and preparing assessments.
- Attending faculty meetings to discuss curriculum changes and program improvements.
🔸5) Principles of curriculum development
Curriculum development involves designing and planning educational programs to meet specific learning objectives and student needs. Here are key principles that guide the process of curriculum development:
1.Alignment with Educational Goals and Objectives
Curriculum should align with the overarching educational goals and objectives of the institution or educational system. It should reflect desired learning outcomes, competencies, and skills that students are expected to achieve.
2.Relevance and Responsiveness
Curriculum should be relevant to the needs of learners, society, and the workforce. It should address current societal issues, technological advancements, and global trends to prepare students effectively for the future.
3.Flexibility and Adaptability
A flexible curriculum allows for adjustments based on evolving educational research, learner feedback, and changing needs. It should accommodate diverse learning styles, abilities, and cultural backgrounds of students.
4.Progressive Sequencing and Integration
Curriculum should be logically organized with content and activities sequenced in a progressive manner. It should scaffold learning experiences, building upon prior knowledge and skills, and integrating interdisciplinary or cross-curricular connections.
5.Engagement and Active Learning
Curriculum development should promote active learning strategies that engage students in meaningful and interactive experiences. It should incorporate opportunities for inquiry-based learning, problem-solving, collaboration, and critical thinking.
6.Assessment and Evaluation
Effective curriculum includes methods for assessing student learning outcomes aligned with curriculum goals. Assessment strategies should be valid, reliable, and varied to measure both knowledge and skills development.
7.Continuous Improvement and Evaluation
Curriculum development is an iterative process that involves ongoing evaluation, reflection, and improvement based on feedback from stakeholders, including students, educators, and community members. It should respond to emerging educational research and best practices.
8.Ethical Considerations and Equity
Curriculum development should adhere to ethical principles, promoting fairness, inclusivity, and respect for diverse perspectives and backgrounds. It should address equity issues in access to educational opportunities and outcomes.
By adhering to these principles, curriculum developers can create comprehensive, effective, and responsive educational programs that support student learning, growth, and development in diverse educational settings.
Q-6. Answer following
🔸(A)organization chart
An organization chart visually represents the hierarchical structure of an organization, illustrating the relationships between different roles and departments. In the context of nursing services, the chart outlines the structure of nursing leadership, staff roles, and the flow of authority and communication. Below is a detailed explanation of a typical organization chart for a nursing service department in a healthcare setting.
- Chief Nursing Officer (CNO) or Director of Nursing
Role:
The Chief Nursing Officer is at the top of the nursing services hierarchy. The CNO oversees the entire nursing department, setting strategic goals, managing budgets, and ensuring that nursing practices comply with legal and regulatory standards.
Responsibilities:
Develop nursing policies and procedures.Ensure high standards of patient care.
Collaborate with other healthcare executives.
- Nursing Managers or Nurse Administrators
Role:
Reporting directly to the CNO, Nursing Managers oversee specific units or departments within the nursing service, such as the Medical-Surgical Unit, Emergency Department, or Intensive Care Unit.
Responsibilities:
- Manage daily operations of their assigned units.
- Supervise nurse supervisors and staff.
- Implement policies and procedures at the unit level.
- Nurse Supervisors
Role: Nurse Supervisors are responsible for managing the clinical and administrative aspects of the nursing staff on their units. They ensure that patient care is provided effectively and that staff comply with hospital policies.
Responsibilities:
- Supervise and support staff nurses.
- Handle staffing schedules and resolve conflicts.
- Conduct performance evaluations.
- Charge Nurses
Role: Charge Nurses are experienced nurses who lead shifts within specific units. They coordinate patient care, manage staff assignments, and address immediate issues that arise during their shifts.
Responsibilities:
- Lead and coordinate the activities of the nursing team.
- Ensure that patient care is delivered according to protocols.
- Serve as a liaison between staff nurses and supervisors.
- Staff Nurses
Role: Staff Nurses provide direct patient care and are responsible for implementing care plans, administering medications, and monitoring patient progress.
Responsibilities:
- Perform patient assessments and provide care.
- Administer treatments and medications.
- Document patient interactions and progress.
- Nurse Practitioners or Clinical Nurse Specialists
Role: These advanced practice nurses may work within various units and provide specialized care in areas like cardiology or oncology.
Responsibilities:
- Perform advanced assessments and provide specialized treatment.
- Collaborate with physicians and other healthcare providers.
- Educate patients and families on managing health conditions.
- Nursing Educators
Role: Nursing Educators focus on the training and development of nursing staff and may also be involved in developing educational materials and conducting training sessions.
Responsibilities:
- Develop and deliver educational programs for nursing staff.
- Evaluate the effectiveness of training programs.
- Support professional development and continuing education.
- Nurse Assistants or Nursing Aides
Role: Nurse Assistants support nurses by performing basic patient care tasks and assisting with daily living activities.
Responsibilities:
- Provide basic patient care such as bathing, dressing, and feeding.
- Assist with patient mobility and comfort.
- Report patient concerns to registered nurses.
- Sample Organizational Chart
- Key Relationships in the Chart
Chief Nursing Officer (CNO)
oversees the entire nursing department and sets strategic direction.
Nursing Managers
implement policies and manage unit-level operations.
Nurse Supervisors
manage day-to-day operations on their units.
Charge Nurses
lead shifts and ensure smooth operations during their shifts.
Staff Nurses
- provide direct patient care.
- Nurse Practitioners and Clinical Nurse Specialists offer advanced, specialized care.
- Nursing Educators focus on training and development.
Nurse Assistants
support staff nurses with basic care tasks.
🔸(B) VED analysis
Definition: VED Analysis is a management technique used in inventory management to categorize items based on their importance to the organization. VED stands for Vital, Essential, and Desirable, which are the three categories used to classify inventory items. This method helps prioritize inventory management efforts and resources to ensure that critical items are available for effective service delivery.
Categories in VED Analysis:
- Vital:
Definition: Items that are crucial for the operation of a department or organization. Without these items, essential services or operations would be severely disrupted. Examples: Life-saving medications, critical medical equipment (e.g., ventilators, defibrillators). Management Focus: Ensure high availability and prioritize procurement to avoid shortages.
2.Essential:
Definition: Items that are important but not critical for immediate operations. Their absence might cause inconvenience or operational inefficiencies but not a complete breakdown.
Examples: Routine medications, basic medical supplies (e.g., bandages, syringes).
Management Focus: Maintain adequate stock levels and ensure timely replenishment to prevent disruptions.
3.Desirable:
Definition: Items that are useful but not necessary for day-to-day operations. Their absence does not significantly impact the core functions of the organization.
Examples: Non-essential equipment, luxury patient amenities (e.g., decorative items, optional patient comfort items).
Management Focus: Monitor inventory to ensure cost-effectiveness and avoid overstocking.
- Purpose of VED Analysis:
VED Analysis helps organizations:
Prioritize Inventory: Focus resources on maintaining the availability of vital items.
Optimize Resources: Allocate budget and storage space effectively by categorizing inventory needs.
Improve Efficiency: Streamline inventory management processes based on the importance of items.
- Example of VED Analysis:
In a hospital setting:
Vital: Emergency medication, surgical instruments.
Essential: Routine medical supplies, regular medications.
Desirable: Extra comfort items for patients, non-essential accessories.
- Benefits of VED Analysis:
1.Effective Resource Allocation: Ensures that critical items are always in stock and that inventory costs are managed efficiently.
2.Operational Continuity: Helps avoid disruptions in essential services by maintaining adequate levels of vital and essential items.
3.Cost Management: Helps in budgeting and inventory control by differentiating between necessary and non-essential items.