ENGLISH PEDIATRIC NURSING UNIT 4
Describe the management of behavioral disorders and common health problems of children.
Disorder and health problems of a child.
Selected key terms.
1) Explain/Define Failure to thrive
Failure to thrive is a chronic potentially life-threatening disorder in which infants and children do not gain adequate weight for their age and lose weight.
In a child who has the condition of failure to thrive, the child does not grow adequately and the well-being of the child is also impaired.
2) Explain/Define Diarrhea
Diarrhea is a condition in which liquid or watery stool is passed frequently and its frequency is more than three times in a whole day (24 hours).
Due to this condition of diarrhea, excessive amount of water and electrolytes are lost from the body and the condition of dehydration arises in the child.
Under five age morbidity (diseased rate) and mortality (death) rate is high due to diarrhea.
3) Explain/Define Vomiting.
Vomiting is also called emesis.
Vomiting is a condition in which stomach contents are forcefully expelled through the mouth.
4) Explain/ define Communicable disease
Communicable diseases are called infectious diseases and contagious diseases.
A communicable disease is an infection that is transmitted from one person to another. This type of infection is transmitted through different routes such as respiratory, droplet, bodily fluids, contaminated food and water etc.
5) Explain/Define Tonsillitis
Tonsillitis is a condition in which the tonsils become infected and inflamed.
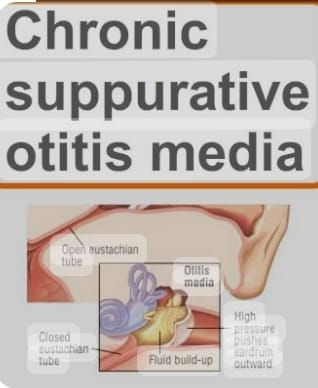
6) Infection and inflammation of the middle ear it’s known as a ….
Ans:= Otitis media.
7) Explain/ define Child Abuse
Child Ambush means that when a child is intentionally harmed physically and emotionally by caregivers, parents and adults who take care of the child, it is called child abuse.
And because of that, the child is physically, emotionally, and developmentally harmed.
8) Explain/ Define Breath holding spell
A breath holding spasm is an involuntary child’s breathing stops and consciousness is briefly lost. A breath holding spell is a reflex response caused by a trigger such as anger, frustration, pain and fear.
A breath holding spell is a common situational disorder. That is called infantile syncope.
In this condition the child holds the bridle for a few moments which is a very anxious moment for the child’s parents.
9) Explain/ define Enuresis
Enuresis is also called bedwetting.
Enuresis is a condition in which any child urinates involuntarily at night time even after the age of five years or when the child has time to achieve adequate bladder control, it is called enuresis.
10) Explain/Define Nail biting
Nail biting is also called onychophagia.
Nail biting is a common habit of childhood life and sometimes thumb sucker is changed into nail biting.
Nail biting involves the involvement of ten fingers in which the child is biting the nail and also involves the skin margin and surrounding tissues around the nails.
11) Inflammation of the Alveoli its known as a….
Ans := Alveolitis,
12) Platelet count decrease from normal level is called what.
Ans:= Thrombocytopenia,
- Define/explain Failure to thrive (FTT).
Failure to thrive is especially prevalent in infants and young children of parents whose socioeconomic conditions are poor.
Failure to thrive was described in 1915. Then in 1969, it was named as “emotional deprivation” and “maternal deprivation syndrome” by Bowlby.
Failure to thrive is a chronic potentially life-threatening disorder of infants and young children.
In which infants and children do not gain weight adequately according to their age and such children lose weight. A child who has the condition of failure to thrive does not grow as expected and the child’s well-being is also impaired. And it indicates psychosomatic growth failure.
Failure to thrive means any infant and young children should have gained as much weight as the child should at that age and if the child has not gained weight, this condition is called failure. called To Thrive.

Explain the etiology/cause of the child with the failure to thrive (FTT). (Give reasons for failure to thrive).
Reasons for failure to thrive are divided into 3 categories.
1) Organic Failure to Thrive (FTT)
Failure to thrive occurs due to pediatric illness in organic causes.
Congenital heart disorder,
malabsorption syndrome,
tuberculosis,
asthma,
Celiac disease.
Cystic fibrosis.
Lactose intolerance.
Intestinal Parasitosis.
Juvenile diabetes mellitus.
Pyloric stenosis.
Liver abscess.
Gastroesophageal reflux.
Galactosemia. (Galactosemia is a metabolic autosomal recessive genetic error in which galactose is not converted to glucose because of a deficiency of the enzyme that converts galactose to glucose, such as galactose-1-phosphate uridyl transferase.)
2) Non Organic Failure to Thrive (FTT)
Inorganic failure to thrive is a psychosocial problem in which the parent-child relationship is disturbed, resulting in emotional deprivation in the child.
like,
poverty,
elitancy,
Faulty Food Habit,
Ignorance.
Due to conflict in the family.
Due to all these reasons nutritional intake is poor and feeding problems are observed due to which the child no growth is a failure.
3) Mixed failure to thrive
In this organic and inorganic causes are seen in a combine.
Other Causes
Due to feeding problem,
Because of poverty.
Due to ignorance and conflict in family.
Due to parasitic infection.
Due to tuberculosis in infants and children.
Due to environmental factors.
Due to psychosocial factors.
Due to genetic factors.
Due to premature and low birth weight.
Explain the clinical manifestation/ sign and symptoms of the child with the failure to thrive.
poor growth,
weight loss,
In Adequate Weight Gain,
Delayed developmental milestones.
wickness,
feel tired,
Behavioral changes occur,
Poor feeding and feeding difficulty,
Like diarrhea vomiting, stomach pain, abdominal bloating,
Look at the nutritional sign of the product.
Decreased immunity,
To see emotional and social issues.

Explain the diagnostic evaluation of the child with the failure to thrive. (Specify diagnostic evaluation for failure to thrive)
history taking and physical examination.
Growth Assessment,
Nutritional Assessment,
Developmental Assessment,
laboratory test,
Imaging studies.
ultrasound,
x ray,
Psychosocial Assessment,
Explain the medical management of the child with the failure to thrive. (Give medical management of failure to thrive child)
For the management of failure to thrive, the child’s physical, social and emotional needs should be fulfilled.
Assessing the child’s proper physical and mental health status.
Proper screening of child.
Proper stool examination of the child.
To properly assess the socioeconomic status of the child’s family.
Proper physical examination and laboratory investigation of the child.
If any intestinal parasites are detected in the child, proper antiparasitic medicine should be provided.
To improve the relationship between child and parent and to try to remove the conflict between them.
To take proper care of the child who has been hospitalized.
If the child has any kind of medical condition, treat it properly.
Regular assessment of child’s growth chart.
Providing proper psychological support to the child.
Explain the nursing management of children with failure to thrive. (Nursing Management of Failure to Thrive Wada Child)
Proper assessment of child’s growth parameters.
To properly assess the nutritional status of the child.
Proper assessment of the child’s developmental milestones.
Provide proper nutritious feeding to the child.
Properly assess the socioeconomic status of the parents.
Maintaining child’s growth chart regularly.
Proper supervision of child’s feeding.
Advising the child’s family members and relatives to provide proper emotional care, love and affection to the child.
Involvement of parents in child’s care and treatment plan.
Provide proper emotional support to the child’s parents and give advice to improve parent child relationship and decrease conflict.
Advising parents of child to take regular follow up.
Advising parents to improve their socioeconomic status.
Giving advice to the parents so that the child gets proper love and affection.
To provide a properly comfortable environment to the child.
Giving advice to the parents of the child to take regular follow-up and regular assessment of the child.
- Define/Explain Diarrhoea. (Define Diarrhea)
Diarrhea is a condition in which liquid, loose and watery stools are passed more than three times in a day (in 24 hours). And the frequency of these loose, watery stools is also high.
Due to diarrhoea, excessive amount of fluids and electrolytes are lost from the body, resulting in the condition of dehydration.
Diarrhea is one of the top three causes of mortality rates in developing countries.
1: = respiratory infection such as pneumonia.
2: = diarrheal diseases and malaria,
3= premature birth complications.
(Diarrhoea is a disease in which passage of loose, liquid or watery stool more than three times per day)
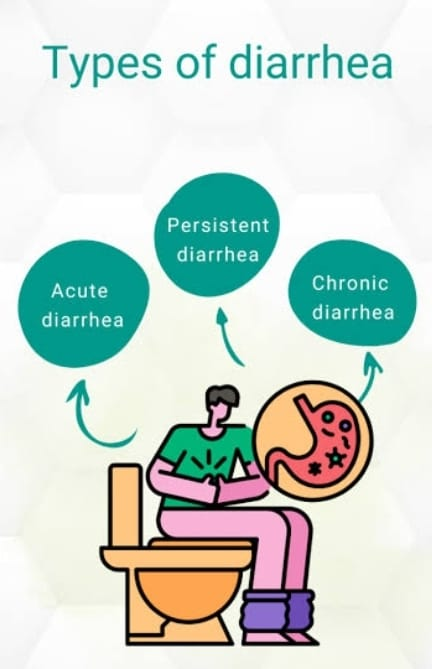
Explain the types of diarrhea. (specify the type of diarrhoea)
There are four main types of diarrhea.
1) Acute Diarrhoea
2) Chronic Diarrhoea
3) Persistent Diarrhoea
4) Dysentery
1) Acute Diarrhoea
Acute diarrhea is a condition in which the onset of diarrhea is sudden and of short duration. And for a period of less than two weeks.
Acute diarrhea is mainly caused by any infection.
2) Chronic Diarrhoea
Chronic diarrhea is a condition in which loose watery stool is present for more than 3 weeks, it is called chronic diarrhea.
Chronic diarrhea is due to any organic disease.
3) Persistent Diarrhoea,
Persistent diarrhea is a condition in which attacks of acute diarrhea persist for more than two weeks and the diarrhea is caused by an infection.
4) Dysentery
Dysentery is a condition in which blood, mucus, and pus are present in the stool, accompanied by abdominal colic, fever, and tenesmus (a condition in which there is a need to pass stool even though the bowel is already emptied.) Get.
Explain the Etiology/cause of the Diarrhoea
Due to unhygienic condition.
Due to infection.
Due to viral infection :=
rota virus,
enterovirus,
Due to AD virus,
Caused by measles virus.
Caused by influenza virus.
Due to bacterial infection.
E coli,
Due to Shigella bacteria,
Caused by salmonella bacteria.
Caused by staphylococcus bacteria.
Caused by Vibrio cholerae.
Due to parasitic infection.
Entamoeba histolytica,
Giardia lamblia,
cryptosporidium,
P falciparum, P vivax, P ovali and P malaria.
Due to fungal infection.
Due to Candida albicans,
Due to infectious conditions.
Due to upper respiratory infection,
Due to otitis media,
Due to tonsillitis,
Due to pneumonia,
Due to urinary tract infection.
Due to dietary and nutritional factors.
overfeeding,
Due to starvation,
Due to food allergy and food poisoning.
Due to other predisposing conditions
like,
age,
season,
artificial feeding,
Explain the Clinical manifestation/ sign and symptoms of the child with the Diarrhoea.
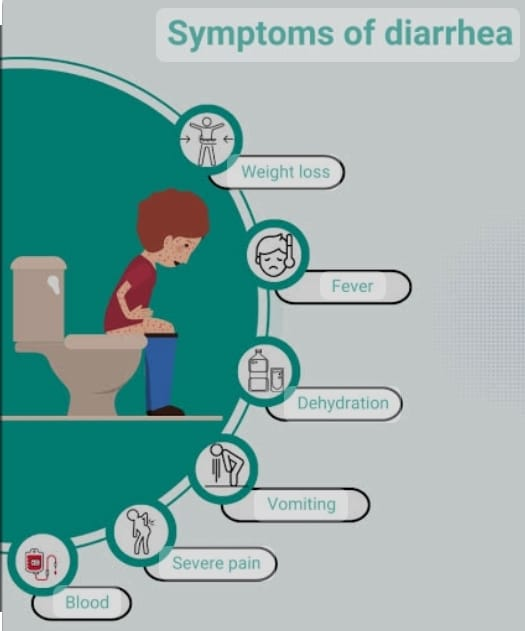
Passing loose watery stools frequently.
Dehydration,
Abdominal pain.
Getting a low grade fever.
Loss of appetite.
Abdominal distension.
Behavioral changes such as
irritability,
restlessness,
coming to wickness,
feeling tired,
Not sleeping properly,
Physical changes can be seen like,
weight loss,
Poor skin turgor,
Dryness of mucus membrane.
Lips become dry,
Paleness,
Eyes become infected,
Fontanelle to be depressed,
Changes in vital signs such as,
low blood pressure,
tachycardia,
Rapid respiration,
limns to be cold,
Decreased urinary output,
loss of consciousness,
Explain the diagnostic evaluation of the patient with the diarrhea. (Give diagnostic evaluation of child with diarrhea)
History taking and physical examination,
stool examination,
blood examination,
Erythrocyte Sedimentation Rate Testing (ESR),
stool culture,
Ova and parasite assessment,
Endoscopic examination.
Explain the medical management of the diarrhea. (State the medical management of a child with diarrhoea)
1) Provide rehydration therapy to the child.
Provide oral rehydration solution (ORS) to maintain child’s hydration status.
Oral rehydration therapy is considered an effective treatment for treating mild to moderate dehydration.
2) Provide intravenous fluid therapy to the child.
If the child has a condition of dehydration and ORS therapy is not properly effective, provide intravenous fluid therapy to the child.
3) Providing proper feeding to the child with intravenous therapy due to which Malnutrition can be prevented.
Providing easily digestible food to the child who can take food by mouth.
Ex:= Toast, rice, blanned food.
4) Maintaining adequate fluid and electrolyte levels of the child.
5) Provide antibiotic medicine to child if diarrheal disease due to any bacterial infection.
6) Provide antidiarrheal medicine to the child
like,
Loperamide,
Bismuth Subsalicylate.
7) Explain the Nursing management of the child with the Diarrhoeal disease.
State the nursing management of a child with diarrheal diseases.
To properly assess the child.
Assessing the Severity of Diarrheal Diseases
Assess the frequency, volume and consistency of diarrhoea.
Assess the child for any symptoms of dehydration.
Maintaining proper fluid and electrolyte levels of the child.
Provide oral rehydration solution to maintain child’s hydration status.
If the child has severe dehydration, provide intravenous fluid therapy.
Provide proper nutritional support to the child.
Providing continuous breast fitting to the child.
If the child is able to intake food through mouth, then providing easily digestible food to that child.
Provide proper medication to the child.
If the child has contracted diarrhea due to any bacterial infection, provide antibiotic medication.
If the child has any parasitic infection then provide antiparasitic medicine.
Advise the child to practice proper hand hygiene techniques to avoid any type of infection.
Monitor the child continuously.
Providing education to the child’s parents or safe water and food handling, due to which the condition of diarrhea can be prevented.
Advise the parents of the child to provide regular medication to the child.
8) Explain the prevention care of the Diarrhoea. (Explain prevention care of diarrhea)
Advising the parents to provide continuous breast feeding to the child.
Advise parents of child to maintain proper hand hygiene.
Giving advice to the child’s parents to properly prepare safe water and hygienic food.
Provide proper hygienic bottle fitting to the child.
Advising the child’s parents not to use any type of specifier.
Advise parents of child to maintain strict personal hygiene.
Giving advice to keep the child’s nails short and giving advice to keep the child’s hands and toys always clean.
Provide adequate fluid to the child.
Providing education to parents to provide easily digestible food like rice, dal, soup, coconut water to children.
Advise parents to provide homemade ORS solution to child if required.
Advise the parents or provide regular medication to the child.
Giving advice to the parents to take proper care of the child.
- Explain / Define Tonsillitis. (Define Tonsillitis)
Tonsils are a part of the lymphatic system
That is present in the neck tonsils is an immune system
Maintains
Tonsillitis is a condition in which the tonsils
Infections that are present in the neck and
If inflammation occurs, it is called tonsillitis.
Tonsillitis is a painful painful disease condition
Due to which infection and inflammation occur
Tonsils are swollen, red and painful and tender
happens

Explain Etiology/cause of the patient with the Tonsillitis. (Give reasons for tonsillitis)
Due to bacterial infection,
Group A Streptococcus,
Streptococcus pneumoniae,
chlamydia,
Bordella
Due to viral infection.
edito virus,
Rehno virus,
coronavirus,
influenza virus,
Ebstein Barr virus, etc.
Explain the types of Tonsillitis. (Specify type of tonsillitis)
There are total two types of tonsillitis.
1) Acute tonsillitis
2) Chronic tonsillitis
1) Acute tonsillitis
The onset of acute tonsillitis is rapid
And it is due to bacterial and viral infections
May be.
2) Chronic tonsillitis
Chronic tonsillitis is of long duration and if acute tonsillitis occurs frequently it is called chronic tonsillitis.

Explain the clinical manifestation / sign and symptoms of the child with the Tonsillitis. (State the signs and symptoms of tonsillitis)
Swallowing and pain in throat.
Swelling in the lymph nodes of the neck.
Getting a fever.
Feeling cold.
Difficulty swallowing.
Pain in the muscles.
Neck stiffening.
Referred pain in the ear.
Swelling in the eyes, face and neck.
Bad bridh come.
Halitosis.
Disturbance of sleep patterns.
Dry mouth.
Difficulty in swallowing and breathing.
The voice thickens.
to become one
feeling tired
Explain the diagnostic evaluation of the child with Tonsillitis. (State diagnostic evaluation of tonsillitis)
History taking and physical examination.
Throat swab.
Blood test.
Imaging studies.
x ray
Ultrasound.
Explain the medical management of the Tonsillitis
Provide proper antibiotic medicine to the child.
Ex :=
Penicillin,
Amoxicillin,
Erythromycin.
Administer analgesic medicine to the child properly.
Ex :=
Ibuprofen,
Acetaminophen.
Provide proper fluid to the child.
Gargling with proper vam water.
Explain the surgical management of the child with Tonsillitis. (Give surgical management of Tonsillitis Wada child)
Tonsillectomy
During tonsillectomy infection in tonsils and
To remove inflamed tonsils
Is performed.
Explain the Nursing management of the child with the Tonsillitis
Proper assessment of the child.
Child’s symptoms viz
Assess for throat pain, difficulty swallowing, fever, and signs and symptoms of dehydration.
Provide analgesic medicine to the child for proper pain management.
Advise the child for proper fluid intake.
To provide properly nutritious feeding to the child.
To provide a properly comfortable environment to the child.
Provide proper respiratory support to the child.
Advise the parent to properly hydrate the child.
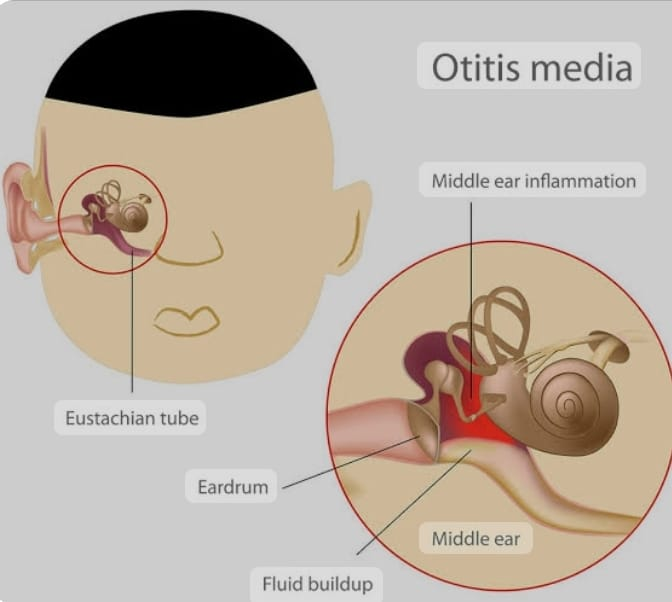
- Explain/Define Otitis media. (Define otitis media)
Otitis means inflammation of the ear, media means relating to the middle ear, otitis media means infection and inflammation of the middle ear is called otitis media.
Otitis media is a common disease of infancy and childhood and is mainly due to upper respiratory tract infection. If there is an infection in the pharyngs (nasopharynges), it is transmitted to the middle ear through the Eustachian tube and the condition of otitis media arises.
Otitis media in children is mainly due to short, wide and horizontal eustachian tubes of children, the infection in the nasopharynges spreads to the middle ear and the condition of otitis media arises. Middle ear infection is seen in children due to upper respiratory tract infection, teeth eruption, gums congestion, etc
Explain the types of Otitis media. (State the type of otitis media).
There are total 3 types of otitis media.
1) Acute Otitis Media (AOM),
2) Otitis media with effusion (OME),
3) Chronic Suppurative Otitis Media (CSOM)
1) Acute Otitis Media (AOM)
Acute otitis media is mainly upper
After a respiratory infection or rubella,
After measles and influenza infection
can be seen.
In acute otitis media, middle ear infection occurs rapidly and for short duration. If acute otitis media is not treated, there is a collection of fluid and pus in the middle ear.
Its most common causative organism is Streptococcus Pneunoniae and
Haemophilus influenzae is.
2) Otitis Media with Effusion (OME)
Otitis media with effusion is called “glue ear” and “serous otitis media”. Otitis media with effusion (OME) is mainly caused by acute otitis media (AOM). In the condition of otitis media with effusion, there is a collection of fluid in the middle ear space which creates a negative pressure in the middle ear. This negative pressure leads to obstruction of the Eustachian tube if not treated properly and the fluid becomes thick such as Otitis media with effusion due to glue is also called “glue ear”.
3) Chronic Suppurative Otitis Media (CSOM)
When repeated episodes of acute otitis media occur in the middle ear, it results in chronic suppurative otitis media.
Chronic otitis media is a persistent infection and inflammation of the middle ear. And it is mainly for more than three months.
Explain the Etiology/cause of the Otitis media
Due to bacterial infection.
Streptococcus pneumoniae,
Haemophilus influenzae,
Due to viral cause,
rheumatic virus,
Respiratory syncytial virus (RSV),
Due to family history,
Due to low birth weight,
Due to altered immunity,
Gastroesophageal Reflux Disease,
prematurity,
Due to low immunity,
Due to external ear infection,
Due to bottle feeding,
diphtheria,
Because of overcrowded.
Explain the clinical manifestation / sign and symptoms of the child with the Otitis media. (State the symptoms and signs of otitis media).
Pain in the ear,
Hearing loss,
hearing tinnitus sound,
Feeling of fullness,
confusion,
Changes in gait,
Sleep pattern disturbance,
vertigo,
Nausea and vomiting
Irritability,
A feeling of fullness in the ear,
Balance problem.
Discharge from the ear.
Pain while chewing.
Explain the Diagnostic evaluation of the Otitis media. (State diagnostic evaluation of otitis media)
History taking and physical examination.
Lab Investigation.
CT scan.
M.R.I.
Lab Studies.
Culture of specimens.
Tympanogram.
Pure tone audiometry,
Tympanosynthesis
Explain the medical management of the child with Otitis media. (State the medical management of a child with otitis media)
If the child has contracted otitis media due to any bacterial infection, then give antibiotic medicine.
If the child is in pain, provide analgesic medicine to relieve it.
If the child has a condition of fever then provide antipyretic medicine to the child.
If the patient has any inflammatory condition, provide anti-inflammatory medicine.
If the child has an otitis media condition due to inflammation, instill antibiotics and corticosteroid ear drops to reduce inflammation and fight infection.
Provide left ear compression to the affected ear to relieve pain and discomfort.
Encouraging the child to have adequate water intake to prevent the condition of dehydration.
Explain the surgical management of the child with Otitis media. (State surgical management of otitis media)
1) Tympanosynthesis
In the tympanosynthesis procedure, fluid and pus are aspirated through a needle. This procedure is mainly done when there is a small amount of fluid and pus collection.
2) Myringotomy/ Tympanotomy
In this procedure, an incision is made in the tympanic membrane, after which debris and pus in the middle ear are removed using forceps and tubing.
Tube Name := Grommet Tube.
3) Mastodectomy
This procedure is mainly performed when the infection in the middle ear has increased a lot.
In mastectomy, an incision is made on the mastoid process and the affected area of the middle ear is removed.
There are two types of mastectomy
A) Simple mastodectomy
In this, the affected area of the middle ear is mainly removed.
B) Radical mastodectomy
Radical mastectomy a
Three bones of the ear are removed to remove the tympanic membrane and close the opening of the Eustachian tube.
4) Otalum
A small hole is made in the tympanic membrane using a laser in the Otalum procedure Otalum is an alternative method of myringotomy. In this procedure, the debris in the middle ear is removed.
Explain the Nursing management of the child with the Otitis media
Properly assess the child’s symptoms such as ear pain, irritability, fever, and general health of the child.
Observe the child’s ear canal for any inflammation or swelling present and assess for any redness of the tympanic membrane.
To properly assess the child’s hearing acuity.
Use simple language, short sentences and slow speaking with the child.
Examining the child’s ear canal for any drainage.
Providing the child with prescribed analgesic medicine if the child is in pain.
Ex := Acetaminophen,
Ibuprofen.
To provide complete information to the child’s parents about the child’s disease condition, its causes, its symptoms and signs and its treatment.
Advise the child’s parents to lie down on the affected side to reduce the pressure in the ear.
If the child is experiencing pain and discomfort, proper comfort measures around the ear such as ear compresses and gentle massage can be used to relieve the child’s discomfort.
To properly assess the child’s vital signs.
Advise the parents to provide proper antipyretic medication to the child if the child has fever condition.
Advise on proper fluid intake to maintain child’s hydration status.
Giving advice to maintain proper hygienic condition while handling the child.
Advising the child’s parents to ensure proper nutritional food intake of the child.
Providing proper antibiotic medication to the child and properly instilling ear drops.
Advise the parents of the child to properly provide medication to the child.
Advising parents of children to provide a properly comfortable environment to the child.
- Explain/Define Child Abuse. (Define child abuse)

Child abuse is also called battered child syndrome.
Child abuse is primarily a non-accidental injury.
On the child, its adults, parents and
Any type of violence and abuse by the caregiver, mainly physical, sexual, emotional, maltreatment and neglect of the child, is called child abuse.
Child Abuse When a child is harmed by parents, caregivers and other adults, it is called child abuse.
A child who has been abused once is repeatedly abused by an adult in his life and experiences many types of difficulties in his life.
Child abuse can happen mainly at home school, residential care, street and public places.

Explain the type of child abuse. (Write type of child abuse)
There are total five types of child abuse.
1) Physical abuse,
2) Emotional aids,
3) Sexual abuse,
4) Neglect
5) Child exploitation
1) Physical abuse,
Physical abuse involves physical abuse of a child by an adult. Physical abuse involves hitting, burning, slapping, punching, kicking or striking children with an object.
In physical abuse, physical force is exerted on the child in an intentional manner, resulting in bodily injury, physical harm and impairment.
2) Emotional abuse,
Non-supportive during child development in emotion abuse
If there is an environment, the child is emotionally abused.
Emotional abuse is called psychological and verbal abuse. in which the child
is emotionally maltreated and the child is psychologically harmed.
Emotional abuse includes belittling, shaming, humiliating, threatening and constantly criticizing the child, which undermines the child’s self-esteem and emotional well-being.
3) Sexual abuse,
In sexual abuse, the child is engaged in any sexual activity. In sexual abuse
Includes sexual assault, molestation, rape etc.
4) Neglect
Neglect is a form of abuse in which the child’s caregiver fails to fulfill a child’s developmental (basic) needs on purpose. In Neglect
Involvement of non protective environment and happy situation.
The child’s parents and caregivers cannot provide adequate care as per the child’s needs.
Like Child Ne Food,
Medicine, shelter, emotional support, clothing, supervision, are not properly provided.
5) Child Exploitation
Child exploitation is the exploitation of a child for economic gain, labor and other purposes including child labour, forcing a child to engage in illegal activities and using a child for prostitution and exploiting children.
Explain the etiology/cause of the child abuse. (Give reasons for child abuse)
Due to emotional stress,
Family factors like parental stress,
domestic violence,
Marital Conflict,
Parenteral Substance Abuse
Financial instability,
social isolation,
social factors,
impaired interpersonal relationships,
Due to domestic violence,
Because parents have high expectations with their child.
Parents have depression and mental handicap.
Parents being mentally ill.
Explain the clinical manifestation/ sign and symptoms of child abuse. (State the symptoms and signs of child abuse)
Poor personal hygiene.
Inability to concentrate.
Poor school attendance.
Having problems in speech.
Unexplained injuries, burns and cuts.
Poor self-esteem.
Being emotionally traumatized.
Suicide attacks occur.
Trust in people is low.
Difficulty in relationship.
Aggression against others.
Physical abuse
fracture,
In the abuse area
Redness.
To see the marks.
Get to see the scars.
Head injury and internal organ injury.
Sexual abuse
infection.
Genital injury.
Abdominal injury and pain.
Constipation.
Chronic and Urinary Urinary Infections.
Behavior problem.
Emotional abuse
Getting depressed.
anxiety,
Neglect
Failure to Thrive,
Even basic health care cannot be obtained.
Failure to fulfill basic nutritional needs.
Poor hygiene.
Inadequate supervision.
Explain the diagnostic evaluation of the child abuse. (Specify diagnostic evaluation of child abuse)
History taking and physical examination.
Ashes should be done whether any scars and burns are present in the body.
Genitalia proper
Inspection.
Assess the child for any injuries on the body such as oral mucosa, breast, and throat.
Laboratory Investigation.
Explain the management of the child abuse
Taking a complete history of the child’s family and its relatives and doing a proper physical examination of the child.
Properly counseling the parents of the child.
To provide a properly safe environment to prevent further harm to the child.
Providing cognitive behavioral therapy to a child who has been physically abused.
Removing the child from the abusive environment and providing adequate medical care if needed.
If there is a suspected case of child abuse, it should be properly reported to the proper authorities such as Child Protective Services and Law Enforcement.
Provide proper medical care to a child who has been physically abused and needs medical treatment and medical evaluation.
If a child is emotionally abused, provide him/her with proper psychological support. Providing psychological support to the child can help cope properly with any betrayal.
To provide a properly safe environment to the child.
To provide proper education to the family members of the child and his parents to avoid child abuse.
- Explain/Define Breath holding spell. (Define breath holding spell)
A breath holding spell is a common situational disorder.
A breath holding spell is also called “infantile syncope”.
Breath holding spells are involuntary reflexive episodes and psychosomatic disorders that are mainly seen in young children i.e. children from six months to six years.
In a breath holding spell, the child involuntarily holds his/her breathing for a while while crying. Breathing is temporarily held and the child loses consciousness due to this. This breath holding spell is seen during anger, festeration.
During a breath holding spell, the child’s consciousness is lost, cyanosis is seen and the child also has twitching and tonic-clonic movements, the child becomes limp, lifeless and very pale. And the heart rate becomes slow and laryngeal spasm is seen and this type of attack is seen for one to two minutes.
.

Explain the etiology of the breath holding spell. (Give reason for bridh holding spell)
Exact cause unknown,
Due to frustration,
Due to disciplinary conflict between parent and child,
Due to genetic predisposition,
Due to dysregulation of autonomic nervous system,
Due to emotional triggers,
Due to iron deficiency anemia,
Due to dysfunction of the brain stem.
Explain the types of the breath holding spell. (Specify type of bridh holding spelling)
There are two types of breath holding spells.
1) Pallid type,
2) Cyanotic type
1) Pallid type,
Paled Type is also called Pale Spell.Paleid Type
Less is a common type of breath holding spell.
This spell is seen in the early years of life i.e. after minor injuries and when the child is upset.
Ama opens her mouth when the child cries but no sound comes out and the child becomes very pale.
The pallid type is thought to occur after cardiac asystole, similar to a vasovagal attack, and is induced by ocular compression.
2) Cyanotic type
The cyanotic type is called “blue spell”.
A cyanotic spell is the most type of breath holding spell in which the child experiences sudden and intentional emotional triggers such as anger and frustration causing cessation of breathing.
In cyanotic spell intra thoracic pressure increases followed by cerebral circulation increases and heart rate also decreases due to which unconsciousness and syncope develop.
In a cyanotic breath holding spell, the child has a bluish discoloration due to the decreased amount of oxygen in the blood. And child’s consciousness is lost.
After loss of consciousness, breathing usually resumes spontaneously, and the child gradually returns to normal color and consciousness.
Explain the clinical manifestation/ sign and symptoms of the breath holding spell. (State the symptoms and signs of bridh holding spell)
Symptoms and signs depend on the type of breath holding spell.
1) Pallid Breath Holding Spell ( PBHS ).
A pallid breath holding spell is mainly caused by any pain or fear.
The child becomes pale,
Child’s consciousness is lost.
Muscles are twisting.
The body becomes stiff.
Caesars come.
2) Cyanotic Bridge Holding Spell.
cyanosis,
Breathing is stopped,
loss of consciousness,
convulsive twitching,
slow heart rate,
spasm in the laryngeal muscles,
One to three attacks are seen throughout the day.
Explain the diagnostic evaluation of the child with the breath holding spell. (Give diagnostic evaluation of bridh holding spell)
History taking and physical examination.
laboratory test,
Complete blood count test,
Serum iron level assessment,
Electrolyte Assessment,
genetic testing,
electrocardiogram,
Holter monitoring,
Neurological evaluation,
imaging studies,
CT scan,
MR. eye.
Explain the management of the child with the breath holding spell. (Describe management of child with breath holding spell)
Providing complete education and explanation to the parents about the child’s disease and reducing the anxiety of the parents.
Advise the parents not to overprotect the child.
Identify trigger factors that increase child’s breath holding spells such as anger, frustration, pain, fear and assess.
To provide education to the parents of the child or to provide adequate nutrition to the child, to provide adequate sleep and stressful situation.
Maintaining child safety properly.
Provide proper medical treatment to the child and carry out proper medical evaluation.
If the main cause of the child’s breath holding spell is iron deficiency anemia, provide the child with proper iron supplementation.
Providing proper cognitive behavioral therapy to the child.
Advise parents not to provide any kind of punishment to the child.
Properly identifying the causes of the child’s condition and taking steps to reduce them.
To provide proper work and comfortable environment to the child.
Giving advice to parents or providing adequate love and affection to the child.
Advise the parents to take the child’s treatment regularly or take proper follow up.
- Explain/Define Enuresis. (Define enuresis)
Enuresis is a common pediatric problem in which a child has frequent involuntary urination while sleeping.
While voluntary urine control should normally be achieved, the condition of frequent involuntary urination while slipping is called enuresis. And this condition is seen in the child even after 5 years.
Enuresis (bedwetting) is also called nocturnal incontinence.
Explain the Etiology/cause of the Enuresis
Since the bladder is small,
Due to hormonal imbalance,
Due to urinary tract infection,
Due to diabetes,
Due to chronic constipation,
Due to structural problems in the urinary tract,
Due to delayed bladder maturation,
Due to genetic predisposition,
Due to impaired secretion of antidiuretic hormone (ADH),
Due to overactive bladder muscles,
Due to psychological factors,
Due to family conflict,
Due to goods adjustment.
Being very strict parents.
Due to neuromuscular bladder function alteration,
Due to neurological deficits,
Due to genitourinary infection,
Due to anatomical defect,
Due to improper toilet training,
Because the parent child relationship is impaired,
As the child is mentally disturbed,
Explain the types of the Enuresis
There are total two types of enuresis.
1) Primary enuresis
2) Secondary enuresis
1) Primary enuresis
When due to any organic cause the child has not achieved normal bladder control even once and the condition of bedwetting occurs, it is called primary enuresis.
In primary and persistent enuresis, when the neurological maturation of the child’s urinary bladder control is delayed, it is called primary enuresis.
2) Secondary enuresis
Secondary enuresis is when the child has achieved bladder control for a few months but when due to any stressful environment such as illness, hospitalization, family conflict, separation of parents, the child’s bladder control is again impaired and night time bed wetting is called secondary enuresis. Called enuresis.
Explain the clinical manifestation/sign and symptoms of the child with enuresis. State the symptoms and signs of a child with enuresis.
Involuntary urination during sleep,
Increased frequency of urination,
nocturnal enuresis,
A psychological impact is seen
Low self-esteem, shame,
Social withdrawal,
get frustrated,
Child’s daily routine activity is impaired,
Passing urine even in daytime,
Explain the Diagnostic evaluation of the child with the Enuresis
History taking and physical examination,
Interviewing the child and parents in detail,
Complete physical examination of the side,
lumbosacral spine x-ray,
Intravenous urogram,
Urine Analysis,
Urine culture.
Bladder function test.
Euroflow Meter Test.
Explain the medical management of the child with Enuresis. (Give medical management of child with enuresis)
Medical management of a child with enuresis depends on various factors such as the child’s age, severity and frequency of bedwetting episodes,
Depending on any medical and psychological factors, etc.
Fluid restriction
Advise the child to have less fluid intake in the evening time and advise the child’s parents to provide less amount of special beverages like cold drinks, cold drinks, tea, coffee etc. in the evening time.
Bladder control
Advise parents to provide regular bladder control training to the child.
Provide proper medication to the child.
1) Desmopressin
Desmopressin is a synthetic form of antidiuretic hormone. This type of medication helps to reduce urine production at nighttime.
2) Anticholinergic medication
Anticholinergic medications help to reduce the contractions of the bladder muscles.
Ex:=
Oxybutynin, Tolterodine.
3) Tricyclic antidepressant
This type of medication helps to achieve bladder control and induce deep sleep.
Ex:=
Amitriptyline, Nitroxazepine, Imipramine.
Explain the Nursing management of the child with the Enuresis
To properly assess the child.
Proper assessment of frequency, pattern, severity of child’s bed wetting.
To provide complete education about enuresis to the child and his family members.
To provide proper education to the parents of the child or to make the child drink any kind of fluid in a limited amount in the evening time.
To provide proper emotional support to the child and his family members.
Advising the child’s parents to take proper medication.
Giving proper advice to the child
Properly empty the bladder completely before bed time.
Advise the child to have a proper enuresis alarm.
Advising parents to provide proper bladder training to the child.
Advising the parents of the child to use an electrical bell (buzzer) for the child.
Providing emotional support and environmental modification to the child and his parents.
Giving advice on positive reinforcement to the child by the parents.
To provide proper work and comfortable environment to the child.