ENGLISH MSN-2-OPTHALMIC DISORDER PART-4.
- Define keratitis
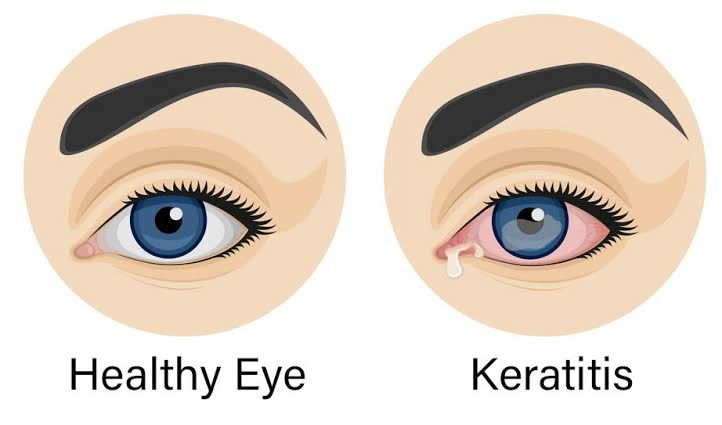
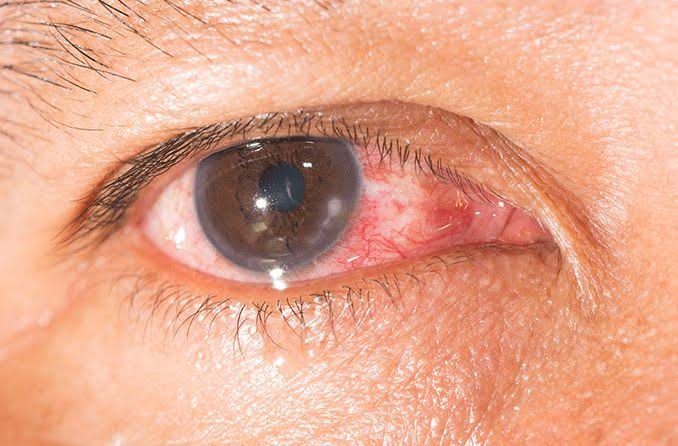
Infection and inflammation of the cornea is known as keratitis.
Write causes of keratitis
Bacterial, viral and fungal infections
trauma
Eye injury
Dry eye
Allergic reaction
Exposure to UV rays
Exposure to Chemicals
Pur contact lens hygiene
Immune system dysfunction
Explain clinical manifestations of keratitis
Eye pain
Redness in eyes
Eye irritation
Blurred vision
Photophobia
Excessive tearing
Discharge from the eye
Feeling Like Something in I
Difficulty opening eye
Write diagnostic evaluation of keratitis
History Collection
Physical Examination (Especially Eye Examination)
Visual acuity test
Slit lamp examination
Corneal staining
Confocal microscopy
Microbial culture
Write management of keratitis
Topical medicine: Use topical antibiotic eye drops and corticosteroids.
Systemic drug: If the keratitis is caused by a bacterial infection, give antibiotics to treat it. If the keratitis is caused by a viral or fungal infection, giving antiviral or antifungal medicine to treat it.
Pain Management: Provide over the counter pain reliever drugs to relieve pain.
Cycloplegic agents: Cycloplegic agents reduce pain and inflammation and temporarily relax the eye muscles.
Warm compresses: Providing warm compresses on the affected eye relieves discomfort and promotes healing.
Avoidance of contact lenses: Tell the patient to avoid wearing contact lenses until the infection resolves.
Protection from the light: Use sun glasses or protective eyewear to get protection from the light. Which gives protection from light sensitivity.
Surgical intervention: Keratoplasty is performed in cases with corneal scarring.
- Define corneal ulcer


Corneal ulcers are also known as ‘ulcerative keratitis’ and ‘isore’.
A corneal ulcer is a painful open sore found on the cornea. (Cornea is the transparent outer layer of the eye)
Write causes of corneal ulcer
Bacterial Infections: Corneal ulcers are caused by bacterial infections with common bacteria like Staphylococcus aureus, Streptococcus viridans, Pseudomonas aeruginosa.
Viral infection: Corneal ulcers are seen due to herpes simplex virus, herpes zoster virus, varicella zoster virus.
Fungal infection: Corneal ulcers are seen due to fungi like Fusarium, Aspergillus, Candida.
Parasitic Infections: Parasitic infections like Acanthamoeba keratitis can cause corneal ulcer-like conditions.
Trauma: Corneal ulcer is seen due to eye injury like scratch, cut etc.
Contact lens wear: Conditions like corneal ulcers are also seen due to improper use of contact lenses and not maintaining proper hygiene while wearing contact lenses.
Dry Eye Syndrome: Corneal dryness and ulcers are seen due to insufficient tear production and poor tear quality.
Immunodeficiency: People with immunodeficiency have an increased chance of developing corneal ulcers.
Underlying Ocular Conditions: Ocular conditions like blepharitis, keratitis, keratoconjunctivitis can cause corneal ulcers.
Chemical Burns: Exposure to chemical substances damages the cornea and causes conditions like corneal ulcers.
Write clinical manifestations of corneal ulcer
Sharp eye pain
Redness
Blurred vision
Sensitivity to light (photophobia)
Excessive tearing
Watery and purulent discharge from the eye
Foreign body sensation
Loss of visual acuity Write diagnostic evaluation of corneal ulcer
History Collection
Physical Examination
Visual acuity test
Slit lamp examination
Culture and sensitivity test
Corneal scraping and biopsy
Management of corneal ulcer
Antibiotic therapy: If the corneal ulcer is caused by a bacterial infection, use antibiotic eye drops to treat it.
Antiviral therapy: If the corneal ulcer is caused by a viral infection, use an antiviral ointment to treat it.
Antifungal Medicine: If the corneal ulcer is caused by a fungal infection, use a topical antifungal agent to treat it.
Corticosteroid eye drops: Corticosteroid eye drops are used to reduce inflammation in selected cases.
Pain Management: Using oral or topical analgesic drugs to relieve pain.
Surgical intervention: Deep corneal ulcers and severe cases require surgical intervention. Surgical intervention involves conjunctival graft or flap and corneal transplantation.
Define cataract
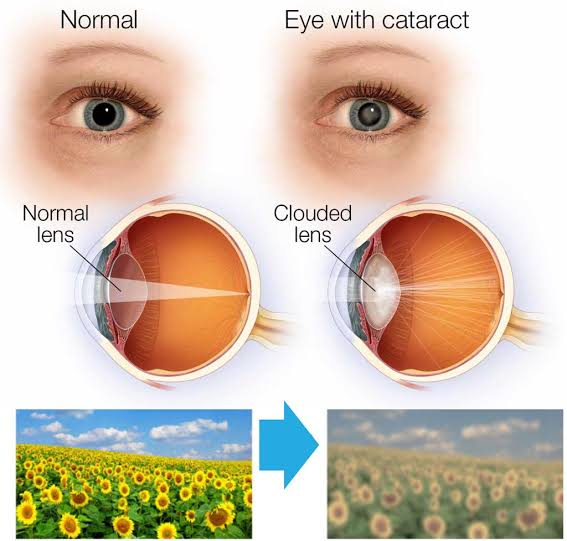
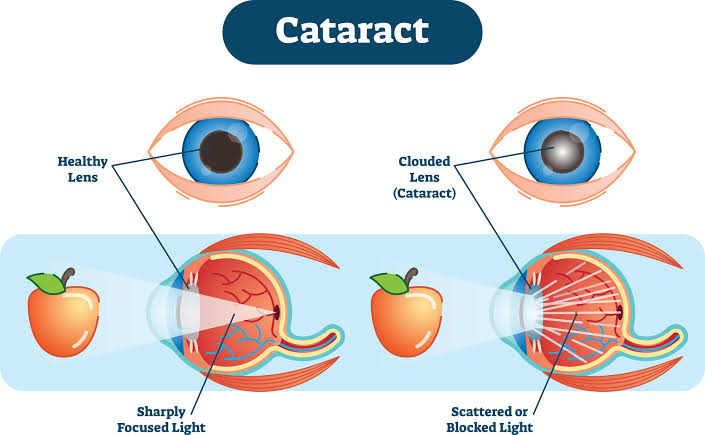
Cataract is an ocular condition characterized by clouding and opacity of the clear crystalline lens. Due to which blurred vision is seen.
Write causes of cataract
Cataracts are caused by many factors. Which are as follows :
Edge:
Hereditary (genetic factor)
Exposure to UV light
Exposure to heat
smoking
Obesity
Diabetes
Eye injury
Previous eye surgery
Intraocular disorders
Use of medication (corticosteroid, oral contraceptive) Write classification of cataract
Classification According to Cos
Age Related (Senile) Cataract: This is the most common type that occurs due to age related changes in the lens.
Congenital Cataract: Congenital cataract is present at birth. Which is seen due to genetic factor.
Secondary Cataract: A secondary cataract develops due to an eye condition or a systemic condition. Like diabetes, trauma, inflammation
Traumatic Cataract: Traumatic cataract occurs due to penetrating or blunt trauma to the eye.
Radiation Cataract: Radiation cataract occurs due to exposure to ionizing radiation.
Electrical Cataract: Electrical cataract is caused by electrical injury or contact with high voltage electrical current.
Toxic Cataract: Toxic cataract occurs due to exposure to toxic chemicals or medicines.
Metabolic Cataract: Metabolic cataract is caused by a metabolic disorder. Like galactosemia, Wilson’s disease
Classification according to location within lens
Nuclear Cataract: In nuclear cataract, the nuclear part of the lens is clouded.
Supra nuclear cataract: In supra nuclear cataract, the upper part of the nucleus ie the deeper part of the cortex is affected.
Cortical Cataract: In cortical cataract, the cortex is affected i.e. the outer layer of the lens is affected.
Capsular Cataract: In capsular cataract, the capsule surrounding the lens is affected.
Posterior subcapsular cataract: In posterior subcapsular cataract, the back part of the lens capsule is affected. Classification According to Degree of Opacity
Incipient Cataract: This is the early stage of cataract. There are minimal visual symptoms and slight opacity in the lens.
Immature Cataract: In this stage, there is moderate opacity in the lens and noticeable visual impairment.
Mature Cataract: In this stage, complete opacity of the lens is seen, leading to significant visual impairment and blindness.
Hypermature Cataract: In this stage, liquefaction of the lens material is seen and shrinkage of the lens capsule is seen. Write clinical manifestations of cataract
Clouded, blurred and dim vision
Trouble seeing at night
Pur vision at night
Double vision in one eye
Halos around lights (discs or circles seen around lights)
Leukocoria or white pupil
Photophobia
Reduce light transmission
Decreases visual acuity
Decreases color perception
Write diagnostic evaluation of cataract
History Collection
Physical Examination
Visual acuity test
Slit lamp examination
Tonometry
Ultrasound Write management of cataract
Phacoemulsification: Phacoemulsification is a modern method used for cataract surgery. In which the cloudy lens is broken up and removed using ultrasound energy.
Intraocular Lens Implantation: After removing the cataract, an intraocular lens is implanted in the eye i.e. the natural lens of the eye is replaced with an artificial lens.
Extracapsular Cataract Extraction: In ECCE, the anterior portion of the lens and capsule is removed while the posterior capsule is left intact.
Intra capsular cataract extraction: In ICCE the lens as well as the capsule is removed. Preoperative care:
First is to identify the patient and check the doctor’s order for cataract surgery on file.
Then collect appropriate history from the patient.
Do his physical examination.
To monitor patient’s vital signs.
Necessary blood tests for surgery. (Like Complete Blood Count, HIV, Hbsag, X Ray, ECG)
Explaining the procedure to the patient, its indications and contraindications. So that his fear and anxiety can be removed.
Consultation of the patient and his family members for surgery.
Ask the patient to wash the face and cut the eyelashes.
Ask the patient to remain oral on Nil for six to eight hours before the operation.
Administer mydriatic and cycloplegic eyedrops shortly before the operation. which dilates and paralyzes the pupil.
Administer antibiotic and antiemetic drug to the patient. Post operative care:
After completion of cataract surgery, the patient is discharged within a few hours.
To monitor patient’s vital signs after completion of surgery.
Checking whether the patient has any operating symptoms or not.
Ask the patient to avoid applying pressure on the operating eye.
Ask the patient to avoid frequent touching and rubbing of the operating eye.
Ask the patient to lie on the side opposite to the operating eye.
Demonstrate the technique for patient eye drop instillation.
Ask the patient to wear an eyelid. So that eye injury can be prevented.
Ask the patient to avoid sneezing, coughing and straining as this may increase intraocular pressure.
Tell the patient to avoid doing close work.
Define Retinopathy
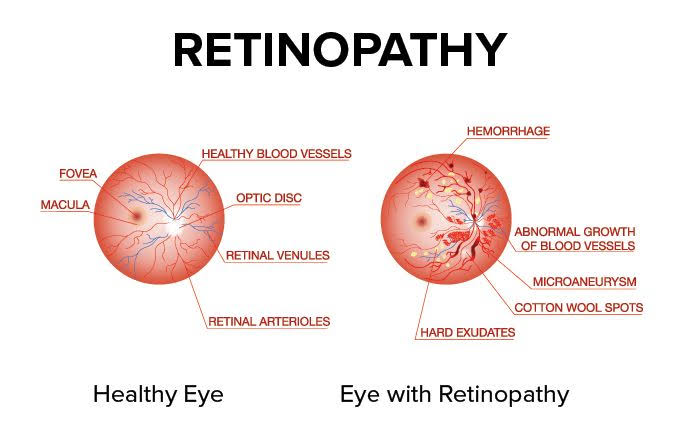

Retinopathy means disease of retina
Retinopathy means any kind of damage to the retina. This damage is seen due to conditions like diabetes, high blood pressure. Due to which vision problem is seen.
Diabetic retinopathy is seen as a complication of diabetes
- Write stages of retinopathy
Mild Nonploriferative :
Small blood vessels in this stage swell and fluid leakage occurs from the blood vessels. Many people have no symptoms at all.
Moderate Nonploriferative :
In this stage, the condition progresses and the blood vessels in the retina become blocked. Due to which the blood supply to that area is cut off and a condition like ischemia is seen.
Severe Nonploriferative:
In this stage, many blood vessels get blocked. Due to which a large part of the brain remains without blood supply and oxygen. which stimulates the growth of new blood vessels.
Proliferative Retinopathy:
In this advanced stage, new blood vessels grow on the retinal surface and vitreous gel (neovascularization). These new blood vessels are fragile, causing leaking blood vessels known as vitreous hemorrhage and severe vision problems.
Write causes of retinopathy
Diabetes
High blood pressure
Medical condition
Eye Condition (Retinal Vein Occlusion)
Genetics
smoking
High cholesterol
radiation
Write clinical manifestations of retinopathy
Blurred vision
Floaters
Decreases visual acuity
Visual field loss
Difficulty at seeing at night.
Eye pain and pressure
Sudden vision loss Write diagnostic evaluation of retinopathy
History Collection
Physical Examination
Ophthalmoscopy
Visual acuity testing
Fluorescein angiography
Optical Coherence Tomography
Fundus photography
Tonometry
Write management of retinopathy
Laser Therapy: Laser therapy is the most common method used to treat retinopathy. In which the leaking blood vessels are sealed using a laser and further damage to the retina can be prevented.
Treat Underline Cause: Control blood sugar levels if retinopathy is due to diabetes. Control blood pressure if retinopathy is caused by high blood pressure. Also, if retinopathy of prematurity is caused by any medical condition, treat that medical condition.
Vitrectomy: In vitrectomy, an opening is made on the eyeball and the fluid collected there is removed.
Define Retinal Detachment
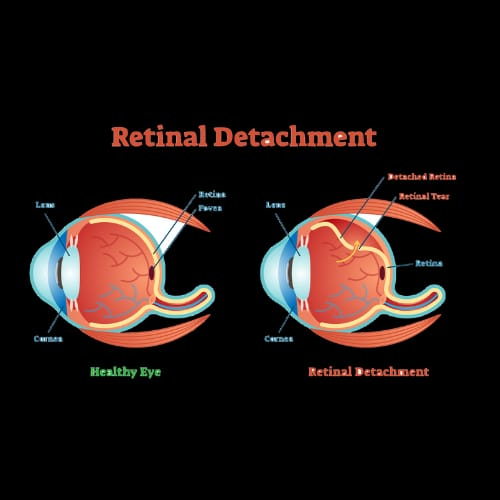
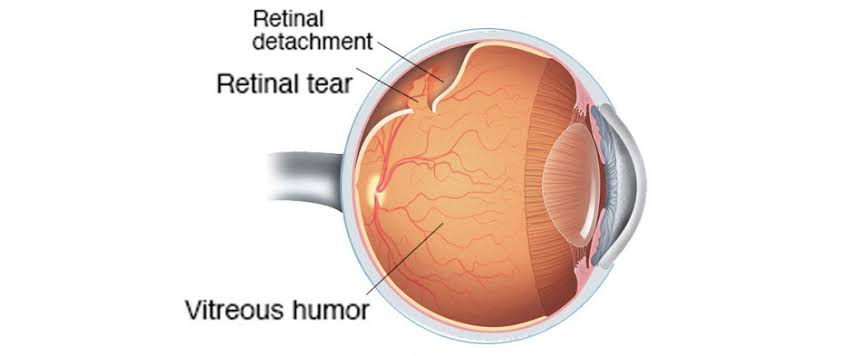
Retinal detachment is a serious eye condition in which the retina, a thin layer of tissue at the back of the eye, moves away from its normal position.
Write causes & risk factor of retinal detachment
Trauma or injury to the eye
Age Related Changes in Retina & Vitreous
Previous Eye Surgery (Cataract Surgery)
Severe near sightedness (myopia)
Inflammatory disorder (uveitis)
Diabetic retinopathy
Hole or tear in the ratina
Macular degeneration
Family history
Tumor in front or behind the retina Write types of retinal detachment (Write types of retinal detachment)
Rhegmatogenous Retinal Detachment:
This is the most common type found mainly in the Old Age. In which holes or small tears are seen in the mat. This causes the vitreous humor to travel through the hole and collect behind the retina so that the retina appears detached.
Tractional Retinal Detachment:
In this type of retinal detachment, the retina moves out of its original position due to the development of scar tissue. This scar tissue mainly develops due to injury, inflammation and conditions like diabetes.
Exudative retinal detachment:
In this type of retinal detachment, fluid collects behind the retina. (Fluid accumulates even though there is no hole or tear) leading to retinal detachment. This fluid is seen due to leaking blood vessels or due to eye swelling.
Write clinical manifestations of retinal detachment
Sudden appearance of floaters (small dark spots and squiggly lines during vision.
Flashes of light in one or both eyes (photopsia)
Blurred vision
Peripheral vision loss
Reduce vision
Distorted vision Write diagnostic evaluation of retinal detachment
History Collection
Physical Examination
Visual acuity test
Visual field testing
Ophthalmoscopy
Ultra sound
Optical Coherence Tomography
Fluorescein angiography
Tonometry Write surgical management of retinal detachment
Vitrectomy: In vitrectomy an opening is made in the eyeball and the vitreous humor is removed and the retinal tear or hole is sealed or scar tissue is removed. The rod is then brought back to its original position with the help of air bubbles, gas or silicone oil.
Laser therapy (photocoagulation): In laser therapy, an argon laser is used to develop scar tissue in the hole or tear so that the hole or tear is sealed.
Cryotherapy: Cryotherapy uses extreme freezing to cause minimal damage and develop scar tissue that seals the hole or tear.
Pneumatic Retinopexy: In pneumatic retinopexy, eye small bubble gas is injected. With the help of this gas or air, the rod returns to its original position. Also the fluid there is absorbed by the body.
Scleral Buckling: In scleral buckling, a flexible band (silicone band, scleral buckle) is placed around the sclera and held there and permanently fixed there. So the ratina comes to its original position. The hole or tear is then sealed.
Define strabismus (Define strabismus
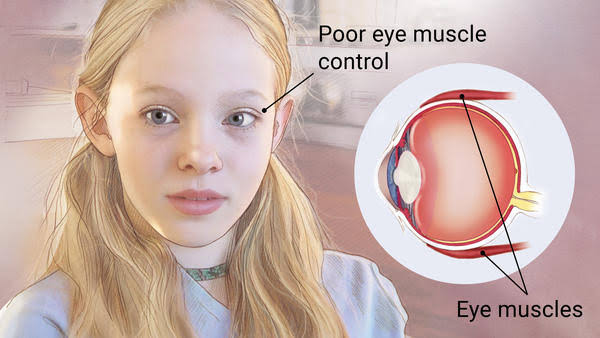
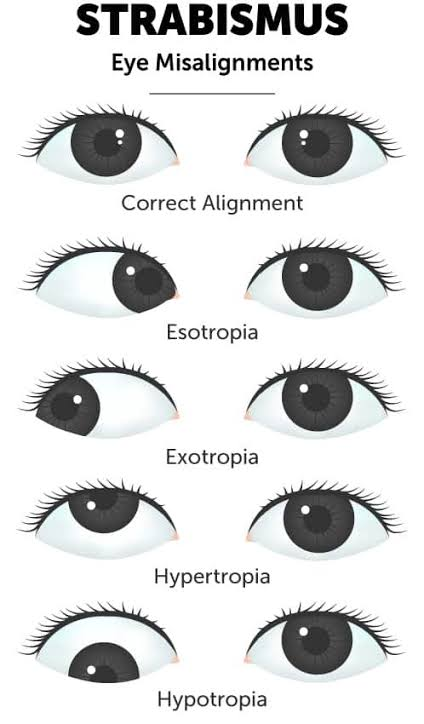
Strabismus is also known as ‘crossed eye’ and ‘squint’.
Strabismus is a vision condition in which the eyes are misaligned, causing one or both eyes to turn inward, outward, upward, or downward. which affects depth perception and binocular vision.
Strabismus is a type of vision condition in which both eyes do not look in the same direction when looking in the same direction at the same time.
Write causes of strabismus
Family History (Genetic Factors)
Dysfunction of muscles controlling eye movement
Nerve injury that controls eye movement
Eye Injury and Trauma
Eye tumor
Refractive error
Congenital abnormality Write clinical manifestations of strabismus (Write clinical manifestation of strabismus)
Misalignment of the eye
Double vision (diplopia)
Amblyopia (lazy eye)
Pure depth perception
Eye fatigue or strain
Abnormal head posture
Reduce visual acuity
Write diagnostic evaluation of strabismus
History Collection
Physical Examination
Ocular Alignment Assessment
Visual acuity testing
Cover test
Ocular Magnitude Testing
Stereopsis test
Write management of strabismus
Corrective Lenses: Use prescription lenses or glasses to correct refractive errors due to strabismus.
Vision Therapy: Vision therapy involves exercises and activities to improve eye coordination, ability to focus, and depth perception. Vision therapy is primarily used in children to help retrain the eye and maintain proper alignment.
Patching: If strabismus is due to amblyopia (lazy eye), then eye patching is done to stabilize the weak eye. which encourages the brain to use the weak eye to improve vision and alignment.
Botulinum toxin injection: Botulinum toxin injection is given in some cases. Which temporarily weakens specific eye muscles and improves alignment.
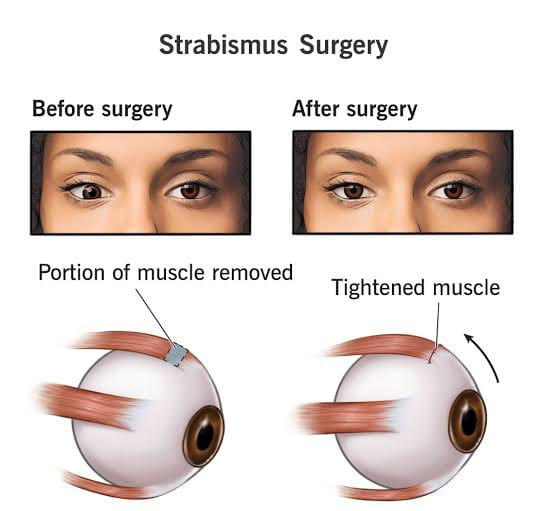
Surgery: Surgery involves adjusting the length and position of the eye muscles and improving alignment.
Refractive error
Refractive error means abnormality refraction
Refractive error is a common eye condition in which the eye fails to focus the image on the retina, resulting in blurred vision. This refractive error is caused by the shape of the eyeball.
Refractive errors are mainly of four types:
1) Myopia
2) Hypermetropia
3) Astigmatism
4) Presbyopia
Define myopia
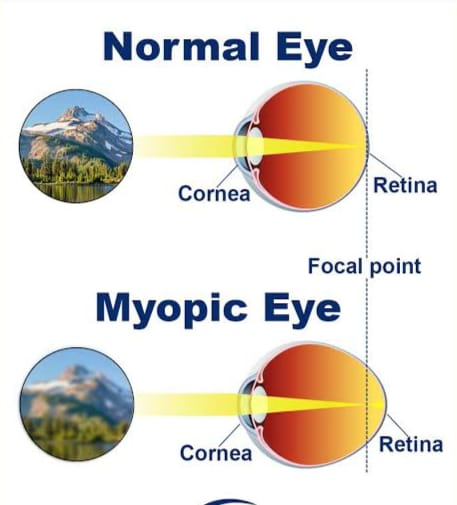
Myopia is also known as ‘shortsightedness’ and ‘nearsightedness’.
Myopia is a type of refractive error in which near objects appear clear while distant objects appear blurry.
In myopia, the size of the eyeball is long and the cornea is seen as steep. Due to which the light rays are concentrated in the front part of the screen. Write causes of myopia
Genetic factor
Environmental Factors (Reading, Writing)
Visual stress
Structural abnormality of eye Write clinical manifestations of myopia (Write clinical manifestation of myopia)
Blur vision for distance objects
I strain
Skiving
Black support floating in front of the eye Write diagnostic evaluation of myopia (Write diagnostic evaluation of myopia)
History Collection
Physical Examination
Visual acuity testing
Refraction test
Auto refractor
Keratometry
Write management of myopia
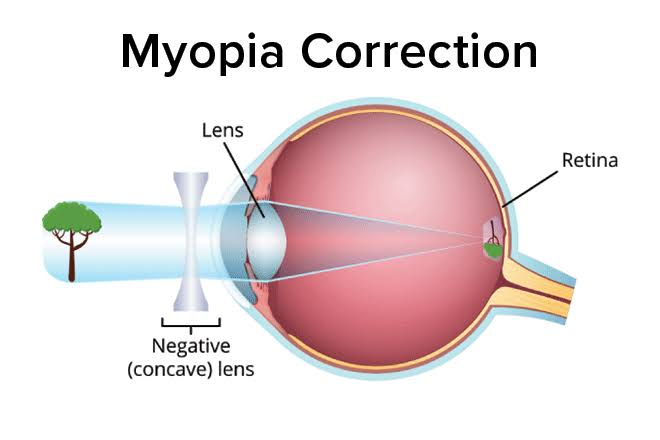
Prescription Glasses or Contact Lenses: Concave spedical glasses are used to correct myopia. which helps to focus the light on the retina.
Orthokeratology: Orthokeratology involves wearing specifically designed gas permeable contact lenses at night. Which reshapes the cornea and provides clearer vision during the day. Hence there is no need to wear contact lenses or glasses.
Environmental and Life Style Modification: Encouraging the patient for outdoor activities and not asking the patient to do prolonged close-up work like reading, screen time. Educate the patient about the 20-20-20 rule. According to this rule, take a break for 20 seconds every 20 minutes to look at an object 20 feet away to reduce eye strain.
Refractive surgery: Surgery such as LASIK (Laser Assisted In Situ Keratomileusis) or PRK (Photo Refractive Keratectomy) is performed to correct myopia.
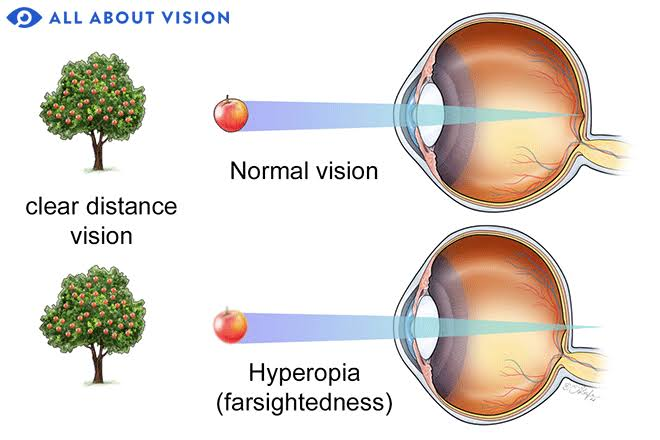
Define hypermetropia
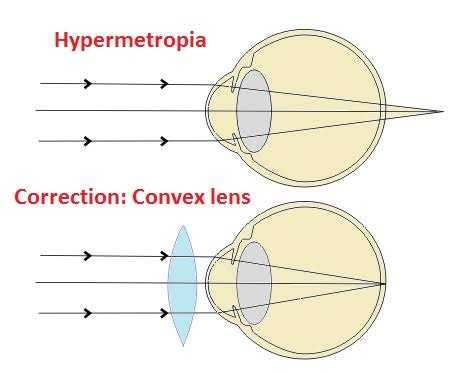
Hypermetropia is also known as ‘farsightedness’ and ‘longsightedness’.
Hypermetropia is a type of refractive error in which distant objects appear clear while near objects appear blurry.
In hypermetropia, the size of the eyeball is short and the cornea appears flat. Due to which the light rays are concentrated at the back of the screen. Write causes of hyper metropia
Shape of eyeball
Genetic factor
Edge
Medical condition
Environmental Factors
Write clinical manifestations of hypermetropia
Blurred near vision
Clear distance vision
Eye strain
Difficulty in close up tasks
Head one
Fatigue and tightness of the eye
Write diagnostic evaluation of hypermetropia
History Collection
Physical Examination
Visual acuity testing
Refraction test
Retinoscopy
Slit lamp examination
Corneal topography
Write management of hyper metropia
Eye Glasses: Convex glasses are used to correct hypermetropia. Convex glasses focus the light on the retina so that the image is clearly visible.
Contact Lenses: Soft or rigid gas permeable contact lenses are used to correct hypermetropia.
Refractive surgery: LASIK (laser assisted in situ keratomileusis) or PRK (photorefractive keratectomy) surgery is performed to correct hypermetropia.
Orthokeratology: In orthokeratology, specifically designed rigid contact lenses are worn at night to temporarily reshape the cornea. Which provides clear vision during the day so there is no need to wear lenses or glasses during the day.
Define presbyopia
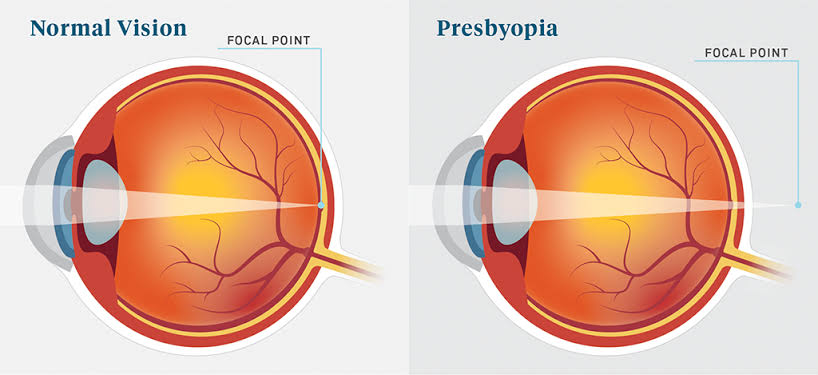
Presbyopia is a type of natural age related refractive error condition. In which the natural lens in the eye loses its flexibility and also loses in accommodation. Due to which close objects cannot be focused. This makes it difficult to see near objects.
This condition is seen after the age of 40 years. Write clinical manifestations of presbyopia
Difficulty in reading small print (news paper, book)
Eye strain and fatigue
Blurred vision
Head one
Write diagnostic evaluation of presbyopia
History Collection
Physical examination
Visual acuity test
Refraction test
Near Vision Test
Slit lamp examination
Write management of presbyopia
Eye Glasses (Contact Lenses): Correct presbyopia with convex spherical lenses.
Is performed.
Refractive surgery: Refractive surgery such as LASIK or PRK is performed to correct presbyopia by reshaping the cornea. Apart from this, surgeries like RLE (refractive lens exchange) and IOL (intra ocular lens) implantation can also be done.
Eye Exercises: Eye exercises and vision training improve focusing ability. So daily eye exercise should be done.
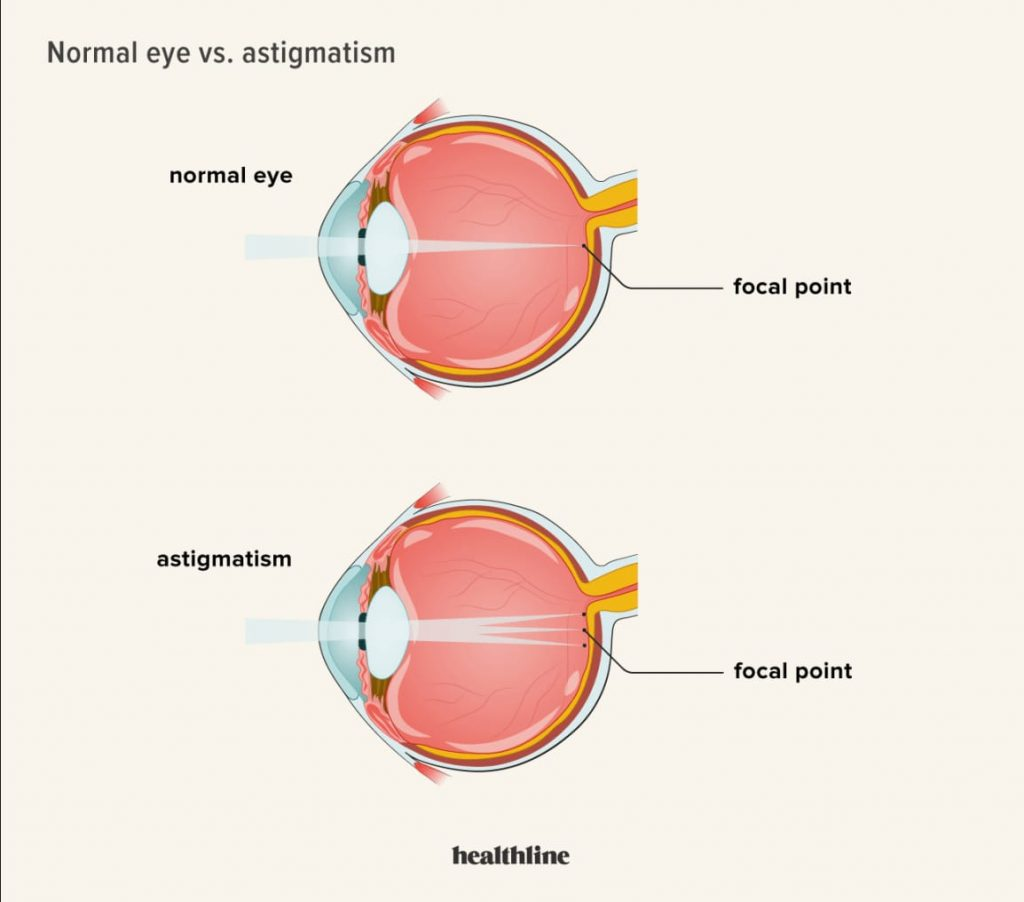
Define astigmatism
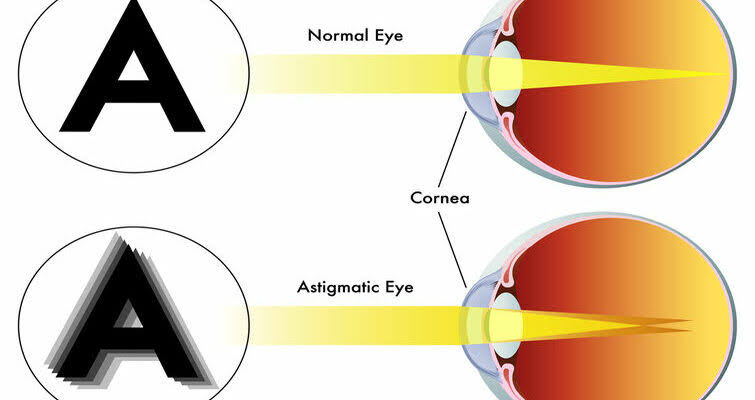
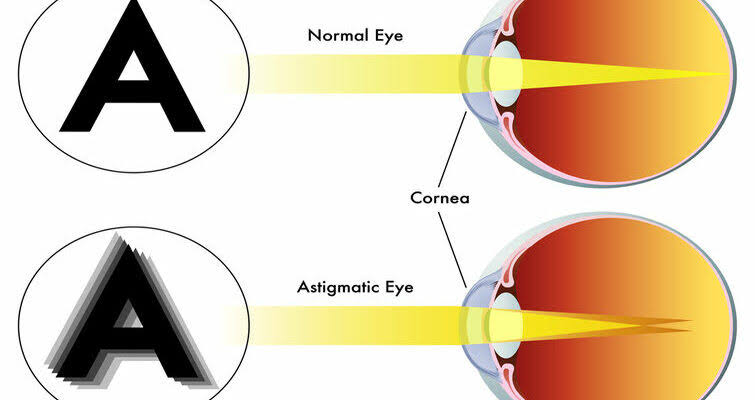
Astigmatism is a common imperfection in eye curvature.
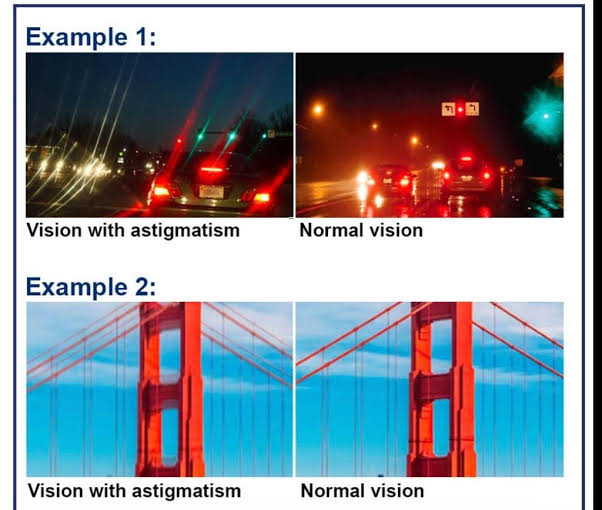
Astigmatism is a type of refractive error in which the cornea or lens has an irregular shape that causes light rays to not focus properly on the retina. Because of which, even if viewed from any distance, the object appears blurry.
Write clinical manifestations of astigmatism
Blurred or distorted vision
I strain
Head one
Skiving
Write management of astigmatism
Eye Glasses (Contact Lenses): Contact lenses are used to correct astigmatism.
Refractive surgery: Refractive surgery such as LASIK or PRK is performed to correct astigmatism to reshape the cornea. Apart from this, surgeries like RLE (refractive lens exchange) and IOL (intra ocular lens) implantation can also be done.
Define color blindness
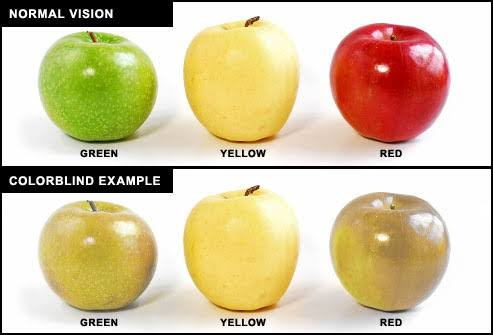
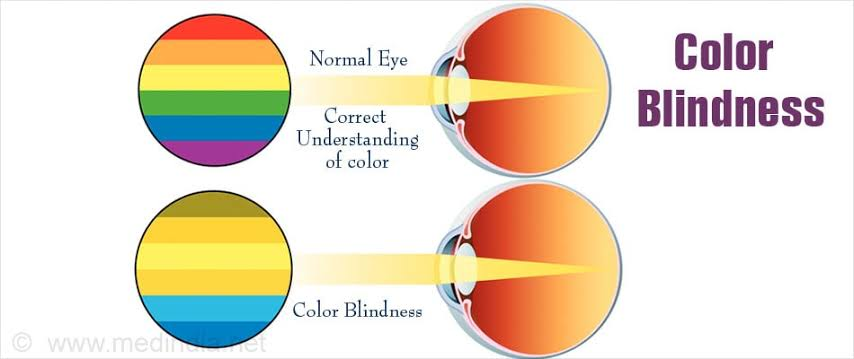
Color blindness is also known as ‘colour vision deficiency’.
Color blindness involves difficulty in distinguishing certain colors.
People with color blindness have difficulty distinguishing between certain colors, especially red and green or blue and yellow. Like reading traffic lights, identifying ripe fruits Write causes of color blindness
Color blindness is mainly found to be inherited.
Color blindness is also acquired in some cases.
Edge
Eye Disorders (Glaucoma, Macular Degeneration)
Eye injury
Certain medications
Write clinical manifestations of color blindness
Difficulty in differentiating color
Reduce color perception
Confusion with color code information
Difficulty in color dependent tasks
Write diagnostic evaluation of color blindness (Write diagnostic evaluation of color blindness)
History Collection
Physical Examination
Ishihar Color Test
Farnsworth Munsell 100 Hue test
Anomaloscope
Color Arrangement Test
Computerized color vision test
Color blindness cannot be treated if it is inherited.
But if it is observed due to an underline cause then that underline cause is treated.
Color blindness cannot be corrected so we use adaptive technology and lifestyle modifications.
Adaptive Technology: Adaptive technology uses specialized software or apps that adjust the colors on the screen and enhance readability.
Define night blindness

- Night blindness is also known as ‘nyctalopia’.
Night blindness is difficulty seeing in dark, dim, or low light. Write causes of night blindness
Vitamin A Deficiency
Genetic disorder (retinitis pigmentosa)
Cataract
Glaucoma
Diabetes
Age related macular degeneration
Birth defect
Disorders Associated with Vitamin A Absorption
Write clinical manifestations of night blindness
Difficulty seeing in low light or dim light
Difficulty seeing at night
Straining to see in low light
Impaired peripheral vision Write diagnostic evaluation of night blindness
History Collection
Physical Examination
Visual acuity test
Visual field test
Refraction test
Measurement of Vitamin A Levels
Electroretinography
Write management of night blindness
Treat Underlying Causes: Treating causes responsible for night blindness.
Vitamin A Supplementation : Provide vitamin A supplement to correct vitamin A deficiency.
Protective measures: Use of sun glasses and protective wear during the day and in bright light at night.
Vision Aid : Use of low vision aids like magnifying glass, night vision goggles in some cases. Which improves vision in low light.
Total blindness
Total blindness means complete loss of vision in both eyes.
Blindness means visual acuity less than 3/60 (20/400).
Blindness means complete lack of light perception
Causes of total blindness
Eye disease
Retinal disease (diabetic retinopathy, retinitis pigmentosa)
Glaucoma
Cataract
Corneal disease
Optic neuritis
Neurological disorders (that affect the visual pathway)
Infection of the eye
Congenital disease (congenital glaucoma, cataract)
Exposure to certain toxins that affect the retina Write clinical manifestations of total blindness (Write clinical manifestation of total blindness)
Lake of response to the light
Inability to see
Complete darkness and absence of visual stimuli
Lake of visual response to Steamyulay
Write diagnostic evaluation of total blindness
History Collection
Physical Examination
Ophthalmologic Examination
Visual acuity test
Visual field testing
Electroretinography Write management of total blindness
Management of total blindness includes practical adaptations, support systems and technology aids.
Orientation and Mobility Training: Provide training for safe and independent tool use such as white cane, guide dog, mobility aids.
Daily Living Skills Training: Providing training for daily living activities like cooking, cleaning, personal grooming
Emotional support and counselling: Vision loss is a challenge so counseling the patient and providing them with emotional support, guidance.
Braille Literacy: Braille enables individuals to read and write tactilely. So readable by touchtile.
Adaptive Technology: Utilizing assistive technology. Like Screen Reader, Magnifiers, Braille Display
National program for control of blindness –NPCB Introduction (Introduction)

India is the first country in the world to launch a national level blindness control programme.
The National Program for Control of Blindness was launched in the year 1976. Which is 100% centrally sponsored program.
The Trachoma Control Program was started in the year 1963 and was merged with the NPCB program in the year 1976.
Causes of blindness are as follows : Cataract (62%), Refractive error (20%), Glaucoma (6%), Posterior segment disorder (5%), Posterior capsular opacification (1%), Corneal blindness (1%), Surgical Complications (1%) and Other Causes (4%) Goal
To reduce the prevalence of blindness from 1.4% to 0.3% by the year 2020.
Objective
Reducing the prevalence of blindness and vision impairment
- Reducing the backlog for blind identification and treatment through blindness.
To develop comprehensive eye care facilities in all districts.
To develop human resources for providing eye care services.
To increase awareness in the community for Eyecare.
Improving the quality of delivery services.
To secure participation of voluntary organizations and private practitioners for eye care.
Expanding research into the prevention of blindness and visual impairment.
Activities under NPCB program
Cataract operation
Involvement of NGOs
IEC Activity
Management Information System
School Eye Screening Program
Collection and Utilization of Donated Ice
Control of Vitamin A Deficiency
Monitoring and Evaluation by Survey
Strategies of NPCB program
Promotion of free cataract surgery through NGOs and private sector
Make the program comprehensive by including eye diseases other than cataract. Like glaucoma, retinopathy
Screening people over the age of 50 for cataracts.
Screening children for refractive error and providing them with free eye glasses.
Covering underserved areas.
Capacity building in eye care providers.
Conducting activities through IEC to create awareness about eye care in the community.
Strengthening the hospital by upgrading the infrastructure, contractual staff and funds of the district hospital.
To establish vision centers in all phc centers.
To create multipurpose district mobile ophthalmic units to improve coverage.
Components of NPCB program
Eye care service
Preventive measure
Infrastructure Development
Human Resources Development
Supply of Essential Drug and Equipment
Data Collection and Monitoring
Partnership and Collaboration
Current trends in management of ophthalmic condition
Advancement in Surgical Techniques: Bringing improvements in techniques like Laser Assisted Cataract Surgery, Minimal Invasive Glaucoma Surgery and Corneal Cross Linking.
Innovations in Pharmacotherapy: Development of Novel Medications. Including biologic and gene therapy. So that options for treatment of conditions like age related macular degeneration, diabetic retinopathy, retinal vein occlusion can be expanded.
Telemedicine and Remote Monitoring: Teleophthalmology allows for remote diagnosis, monitoring and consultation, particularly useful in rural or underserved areas. Remote monitoring devices are useful for timely intervention and better management of diseases for conditions like glaucoma and diabetic retinopathy.
Artificial Intelligence and Machine Learning: AI algorithms are increasingly being used in screening programs for image analysis and diagnosis of ophthalmic diseases, helping in early detection and treatment planning.
Gene Therapy for Inherited Retinal Diseases: Bringing Advances in Gene Therapy to Potential Treatments for Inherited Retinal Diseases.
Regenerative Medicine: Using stem cell therapy and tissue engineering techniques hold promise to repair damaged ocular tissue and restore vision in conditions such as corneal damage and retinal degeneration.
: Hospital corneal retrieval program (HCRP)
The Hospital Corneal Retrieval Program was launched by the Eye Bank Association of India to obtain more corneas.
The main objective of the Hospital Corneal Retrieval Program is to retrieve corneal tissue from willing donors and eligible after death in the hospital.
In addition to establishing a team which includes ICU staff, grief counselors and eye bank staff. which can further enhance this retrieval program.
Under this program trained counselors (Grief Counsellor, Eye Donation Counsellor) are appointed who maintain rapport with the hospital staff.
After a death occurs in any ward, concerned staff of that ward informs the counsellor. This counselor counsels the family members of the deceased person and motivates and requests them for eye donation.
Hospital personnel carry out this activity when the grief counselor is absent. In which Doctor, Nurse, Hospital Social Worker and also specifically ICCU, Surgery, Trauma and Medicine department staff are given chance.
Advantages of HCRP Program
The number of hospital deaths is higher than home deaths so the number of corneas can be increased by increasing the family size.
A lot of young people die in hospital which can lead to many young people’s corneas being collected.
The time interval between death and enucleation or corneal excision can be shortened.
Medical history and investigation report can be easily obtained in the details of the donor.
If the relative wishes, he can donate multiple organs other than eye donation.
Counseling
Following steps are followed for eye donation counselling:
Introduction and rapport building: First, give an introduction to the individual or family member and maintain rapport with them and provide a supportive environment.
Education: To provide knowledge about the impotence of eye donation, its benefits and its misconceptions.
Exploration of Concern: Ask the individual or his family member to express concern and fear for eye donation and empathize with them.
Decision Making: Helping family member in decision making for eye donation.
Consent: If the family member has decided to do eye donation, take their consent on written paper. While taking consent ensure that they are aware of the process and implications of eye donation.
Follow up and support: To support and assist them during the through out process of eye donation. Grief counseling should also be done if needed.
Gratitude: To appreciate them for the decision of eye donation.
Eye banking in eye (Eye banking in India)
An eye bank is a place where corneas are removed from a person’s eyes immediately after death and stored, then transplanted into people with corneal defects.
Eye Banking India collects, processes and distributes donated eyes for corneal transplant and research purposes.
The main objective of Eye Banking India is to explain about corneal blindness and spread awareness for eye donation.
There is i Bank Association of India (EBAI) organization in India. which coordinates the activities of i-banking across the country.
Apart from this, various hospitals, NGOs and government agencies are located in India.
Activities under eye bank association of India
The iBank Association of India coordinates the activities of iBanking in India. The following activities are carried out by iBank Association of India:
Awareness Campaign : EBAI conducts campaigns for public awareness. In which he explains the importance of eye donation and removes the misconceptions about eye donation.
Eye Donation Drives: Organize eye donation drives in collaboration with hospitals, schools, community centers and increase the number of eye donations.
Training Programme: iBank provides training and education to staff, technicians and health care professionals performing eye retrieval on preservation techniques, tissue processing and transplantation procedures.
Quality Assurance: Enhances protocols and quality standards for collection, processing, storage and distribution of corneal tissue as well as corneal transplants.
Networking and Collaboration: iBank provides networking and collaboration facility with hospitals, NGOs and other stakeholders to strengthen iBanking infrastructure, share best practices and optimize resource utilization.
Research and Development: To support research activities to enhance the field of corneal transplants, improve techniques for tissue preservation, enhance surgical outcomes and solve the challenges of corneal blindness.
Advocacy and Policy Development: Developing advocacy and policy promoting eye donation
Define Glaucoma
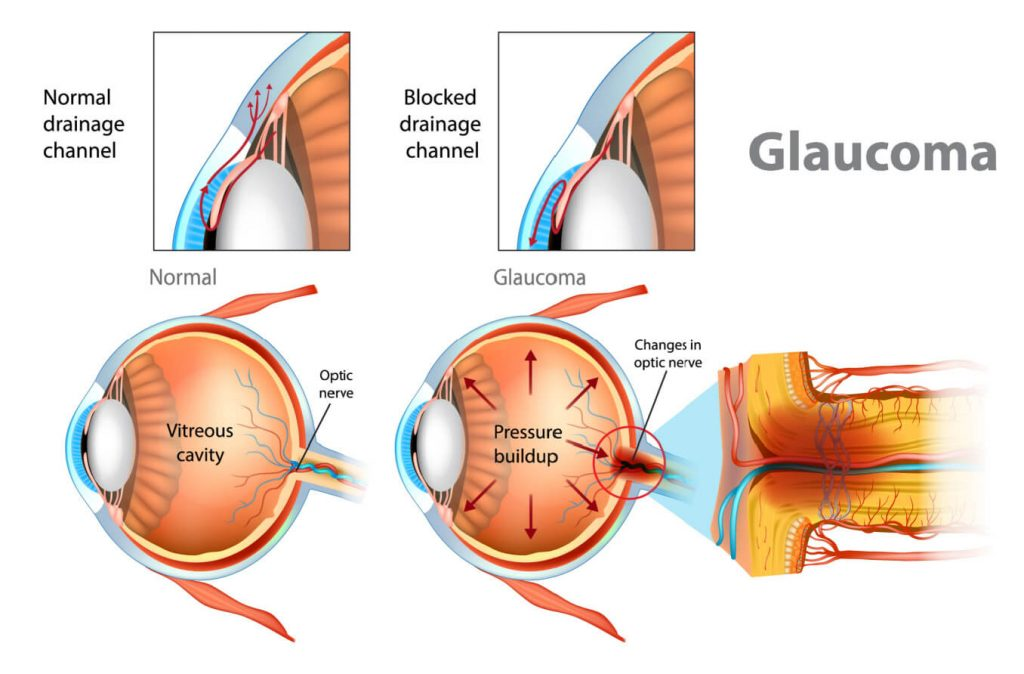
Glaucoma is a group of eye conditions. In which the optic nerve is damaged due to high intraocular pressure, which leads to irreversible blindness.
Glaucoma is a group disorder. Abnormalities in the drainage system of the eye lead to fluid build-up in the eye, which leads to increased intraocular pressure, resulting in optic nerve damage and total vision loss. Write types of glaucoma
Glaucoma is mainly classified into two types:
1) Congenital glaucoma
2) Acquired glaucoma
1) Congenital Glaucoma :
Congenital glaucoma is a rare type of glaucoma in which there is a congenital defect in the drainage system that causes accumulation of aqueous humor and increased intraocular pressure and optic nerve damage.
2) Acquired Glaucoma :
Acquired glaucoma is mainly seen after the age of 40 years. Acquired glaucoma is classified into two types.
A) Primary glaucoma
B) Secondary glaucoma
A) Primary Glaucoma :
Primary glaucoma is caused by abnormalities in the aqueous humor pathway. Primary glaucoma is divided into two types as follows:
i) Primary Open Angle Glaucoma (POAG) :
Primary open angle glaucoma is the most common type of glaucoma. Also known as second chronic open angle glaucoma and chronic simple glaucoma. In which there is an underproduction of aqueous humor or there is an obstruction in the pathway of the aqueous humor due to which the aqueous humor is overfilled, causing increased intraocular pressure and damage to the optic nerve.
ii) Primary Angle Closure Glaucoma :
Primary angle closure glaucoma is also known as secondary narrow angle glaucoma and acute congestive glaucoma. It is an ocular emergency because of the rapid onset and can lead to blindness if not treated within 4-5 days. Primary closure angle glaucoma is caused by abnormalities in the front structure of the eye. In which the angle between the posterior corneal surface and the anterior iris is narrow, due to which there is obstruction in the pathway of the aqueous humor and the outflow of the aqueous humor is blocked, due to which the intraocular pressure increases.
B) Secondary Glaucoma :
Secondary glaucoma is mainly caused by an eye condition or disease. Like uveitis, trauma, tumor, intraocular hemorrhage, previous surgery. In this type of glaucoma, glaucoma is treated as well as the underlying cause.
Write diagnostic evaluation of glaucoma
History Collection
Physical Examination
Tonometry
Visual acuity test
Visual field testing
Gonioscopy
Pachymetry
Optic nerve imaging
Evaluation of drainage angle
Write medical management of glaucoma
Prostaglandin analogs: Prostaglandin analogs increase the outflow of aqueous humor and decrease intraocular pressure. Using latanoprost, bimatoprost eyedrops as prostaglandin analogues.
Beta blockers: Use of beta blocker eye drops to reduce production of aqueous humor and reduce intraocular pressure. For example Timolol, Betazolol
Alpha agonists: Alpha agonists decrease the production of aqueous humor and increase its outflow and decrease intraocular pressure. For example brimonidine eye drop
Carbonic Anhydrase Inhibitors: Carbonic anhydrase inhibitors decrease the production of aqueous humor, which results in a decrease in intraocular pressure. For example brinzolamide eye drop
Write surgical management of glaucoma
Trabeculectomy: In trabeculectomy, a new drainage system is created to allow aqueous humor to exit the eye and reduce intraocular pressure.
Glaucoma drainage implant: In this procedure, a small device is implanted in the eye to help drain the aqueous humor.
Minimally Invasive Glaucoma Surgery: This procedure is less invasive than traditional surgery in which outflow of aqueous humor is increased through trabecular meshwork bypass or suprachoroidal drainage.
Laser trabeculoplasty: In laser trabeculoplasty, drainage is enhanced with the help of a laser to reduce intraocular pressure.
Cyclophotocoagulation: Cyclophotocoagulation uses a laser to reduce the production of aqueous humor and reduce intraocular pressure.
Foreign body in eye
Foreign body in eye is any kind of object or particle from outside getting stuck inside the eye.
Something that entered the eye from outside the body.
Depending on the part of the eye where the foreign body is located, it is divided into two parts:
i) Extraocular foreign body
ii) Intraocular foreign body
i) Extraocular foreign body: In this type, the foreign body is found in the conjunctiva or cornea. Conjunctival foreign bodies are mainly dust, sand, contact lenses, cosmetics etc. Also, metal pieces and rusty objects are seen as corneal foreign bodies.
ii) Intraocular foreign body : In intraocular foreign body, the foreign body is found to have penetrated into the inner part of the eye. In which particles of iron, copper, lead, stone, glass are seen as foreign bodies.
Write sign and symptoms of foreign body in eye
Feeling of pressure or discomfort
Sensation that something in i
Sharp eye pain
Extreme tearing
Excessive blinking
Redness or bloodshot eyes
Difficulty in opening eyes
Congestion in Kanjaktaiva
Sensitivity to Brightlight
Blurred vision Complication of foreign body in eye
Infection and Scarring
Corneal scratches and or abrasions
Ulcer
Penetrating of i
Management
First ask to avoid rubbing the eyes. Because it can scratch the cornea and the foreign body can reach deep.
Then hand wash and flush the eye with clean water or saline solution so that the foreign body can be flushed out.
Then use a clean cloth to clean the area around the eye and remove any debris if present.
Do not manually remove the foreign body if it is deeply penetrated.
Go to the nearest health care center and have it removed by health care personnel.
Acid / alkali burns
Acid/alkali burns or chemical burns are ocular emergencies in which the cornea or conjunctiva is injured due to chemical contact and requires immediate intervention.
Chemical burns are mainly caused by coming into contact with strong acid or strong alkali. Acid Burns:
Acid burns are less serious than alkali burns because they do not penetrate the eye. That is, acid burns damage the front part of the eye.
But in some cases, blindness can also occur due to serious damage to the cornea, such as hydrofluoric burns.
Acid burns have the following symptoms:
Immediate pain
Redness and inflammation
Tissue destruction
Corneal damage
Blurred vision (vision loss may also occur in some cases)
Excessive tearing
Eyelid swelling • Alkali burns:
Alkali burns are the most common and most dangerous eye injury.
Alkali burns can cause severe injury to the external structure of the cornea and the international structure of the lens, including scarring perforation and blindness.
Alkali burns do not show significant symptoms but cause severe eye damage.
Alkali burns have the following symptoms:
Severe pain
Rapid tissue damage
Corneal opacity and cloudiness
Redness and inflammation
Eyelid swelling
Vision Changes and Loss
First aid for chemical burn
First wash the face with running water for 15 to 20 minutes.
So that the chemical in the eye is washed away. In the meantime, take care that the chemical does not touch any other area.
If contact lenses are worn, remove them as early as possible.
Then contact the medical service and transfer the patient to the nearest health care center and tell the staff there about the chemical.
So it can be treated well as Alkali Buns do not show significant symptoms but cause severe eye damage.
Eye drop instillation
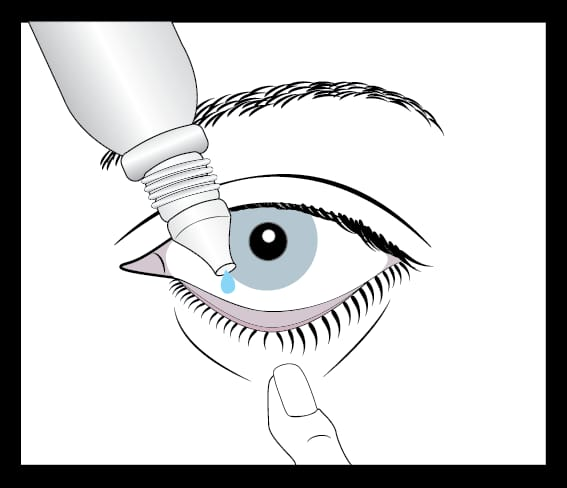
The process of administering drops into the eye is called eye drop instillation. The steps for eye drop instillation are as follows:
The first step is to identify the patient and check the patient’s order for hydro instillation with the patient’s order for eyedrop instillation.
Then explain the entire procedure to the patient.
Wash hands thoroughly with soap and water.
Then provide a comfortable position of the patient like sitting or lying down and tilt the head towards the back.
Then pull down the lower eyelid with one hand and create a small pocket.
Then hold the eyedrop bottle with the other hand. Be careful not to touch the tip part of the eyedrop bottle while holding and prevent contamination.
Administer the prescribed number of eyedrops into the small pocket created by the eyelid.
While administering the eyedrop, be careful that the tip part of the bottle does not touch the eye.
Take the hand holding the eyelid and ask it to close the eye.
Lastly, apply pressure to the eye corner with a clean tissue or finger. So that the medication can be prevented from draining into the tear duct.
Clean excess solution around the eye with a clean tissue.
To maintain record report.
Cold and hot compress
Cold compress


Cold compresses are used to reduce puffiness, swelling and redness. It also relieves symptoms of tired or strained eyes.
Following steps are followed for cold compress:
First wash hands with soap and water.
Then soak a clean cloth or eye mask in cold water or chilled artificial tears.
Wringing out means removing excess water from a cloth or mask.
Provide a comfortable position to the patient and ask him to close the eye followed by applying a cold compress to the eye.
Continue this procedure for 10 to 15 minutes.
While doing the procedure keep the cloth wet with cold water. Hot compress
Hot compresses are useful for soothing dry eyes, relieving eye strain, promoting circulation. Hot compresses are used to loosen oil and debris in conditions such as blepharitis, Meibomian gland dysfunction.
Following steps are followed for warm compress:
First wash hands with soap and water.
Then wet a clean, soft cloth with warm water. The water should be comfortably warm, if too hot it may burn the skin.
Wringing out the excess water in the cloth.
Then fold this cloth according to the size of the eye so that it can cover the eye properly.
Ask to close the eyes and gently apply this warm cloth without putting pressure on the eyes.
Process this way for 10 to 15 minutes.
If the cloth becomes dirty, dip it again in warm water.
After applying the warm compress, dry the eye with a clean towel.
Eye dressing and bandage

Eye dressings and bandages are used to protect and facilitate the eye healing process during eye injury or post surgery. Additionally, they are used to prevent infection, reduce swelling, and protect the eye area. Following steps are followed for eye dressing and bandage:
Prepare the supplies : Preparing the items used for eye dressing. Like sterile gauze pad, sterile saline solution, adhesive tape
Wash your hands: Wash hands properly with soap and water.
Clean the eye area: If discharge or debris is present around the eye, clean it with a sterile saline solution. Use a sterile cotton ball or gauze piece to remove debris.
Position the patient: Provide the patient in a lying down or sitting position and tilt the head slightly backwards.
Place the dressing: Carefully apply a sterile gauze pad to the affected eye. Check whether the affected area is properly covered or not.
Secure the dressing: Use adhesive tape to secure the dressing in place. Apply gentle pressure while applying the tape and avoid excess pressure on the eye.
Check for comfort and vision: To check whether the patient is comfortable with the dressing or not. Also checking for obstruction of vision due to dressing.
Provide Instruction: Provide instructions to the patient on how to care for the eye dressing at home.
Follow up: Instruct the patient for regular follow up.
Assisting for sac syringing
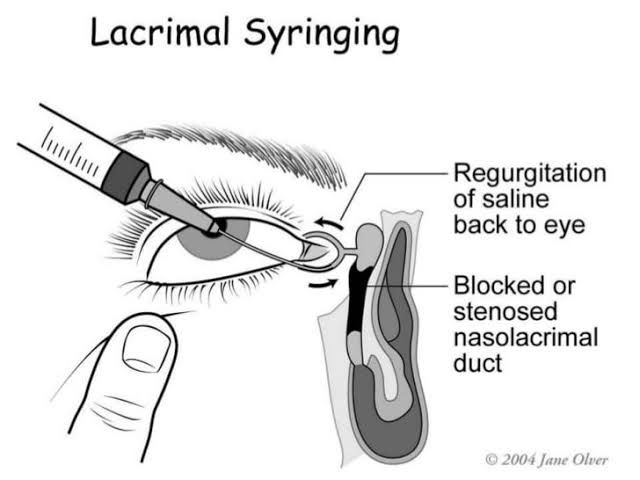
Assisting for sac drainage, also known as second lacrimal sac irrigation, is a procedure used to remove a blockage or obstruction in the teat drainage system. Following are the steps for Sec Siring Assisting:
Prepare Equipment : To prepare the necessary equipment used for sack siring. Like torch, saline solution, cup, basin, syringe, anesthetic eyedrop, cotton swab, gloves
Position the patient: If the patient is comfortable in a sitting position, tilt the head slightly back. If the patient is comfortable in a lying down position, turn the head to the opposite side of the affected eye.
Explain the procedure: Explaining the entire procedure to the patient before the procedure so as to remove the patient’s fear and support the patient during the procedure.
Prepare the eye: Clean the area around the eye with an aseptic solution. So that the chances of infection can be reduced.
Check the Eye: To check whether any kind of foreign body is present in the eye or not. Also to check if any other type of abnormality is present or not.
Apply Anesthetic Drop: Instill a topical anesthetic drop into the eye to relieve discomfort and pain during the procedure.
Assist the Health Care Provider: Assist the health care provider in stabilizing the patient’s head and holding the eyelid open.
Perform the irrigation: Inserting a syringe into the puncta (small opening in the cornea) and flushing the tear duct with saline solution.
Observe for Drainage: Observe whether the drainage is clear and whether debris or blockages are present.
Repeat S Necessary : Repeat this procedure if persistent blockage is found and drainage is not clear properly.
Post Procedure Care: To provide post care instructions to the patient after the procedure is completed. Ask the patient to avoid eye rubbing and touching.
: Assisting in removal of foreign body from the eye
Assess the Situation: First assess the situation. Assessing whether the foreign body is superficial or deeply penetrated.
Prepare the Tray: Prepare the tray of instruments and equipment used to remove the foreign body from the eye. Including clean water, styrene solution, styrene gauze pad or eye ball, tweezers or cotton swab.
Wash the hand: Wash hands properly with soap and water to prevent contamination of eyes.
Position the patient: Provide the patient in a sit or lie down position and tilt his head back slightly.
Examine the eye: Carefully examine the affected eye with a flashlight or pen light. Avoid extra pressure on the eye.
Flush the eye: If the foreign body is small and located on the eye surface, gently flush the eye with a sterile solution or clean water to remove the foreign body. Using a cup or syringe to withdraw the phallus.
Remove the foreign body: If the foreign body is visible and can be easily removed, gently pull it out of the eye with tweezers or a cotton swab and remove it. Care should be taken while removing the foreign body to prevent the foreign body from penetrating the eye and prevent eye injury.
Rinse and Check: After removing the foreign body, rinse the eye with a sterile solution or clean water. Then check if there is any foreign particle present in the eye or not.
Provide Comfort: Providing a comfortable position to the patient. Reassurance to the patient. Ask the patient not to touch and rub the eye frequently