ENGLISH UNIT-4-MSN-II-OPTHALMOLOGY AND OPTHALMIC NURSING-DIAGNOSIS (PART-2)
Assessment of function of eyes
Health history (subjective data)
Health history includes present health history, past health history, past surgical history, personal history, family history and occupational history.
Present health history / chief complaint
Asking the patient about their current complaints.
Asking the patient about eye and vision related problems.
Asking the patient if there is pain, redness, inflammation in the eye.
Asking about its duration, intensity and severity if present.
To know if the patient has any kind of vision problem or not.
If there is a vision problem, getting information about it in detail.
Asking when the vision is impaired. Night blindness may occur if the problem occurs at night.
Asking whether the patient has trouble seeing near or far.
Knowing whether black spots are seen during vision or not.
Asking whether the patient has difficulty identifying colors.
Asking if the patient has sensitivity to light.
Past health history
Obtain information about whether the patient has had any type of eye disease in previous years.
To know whether the patient has systemic conditions like diabetes, hypertension or not.
Collecting information about whether the patient was previously admitted to the hospital or not.
Collecting information about childhood diseases and immunization.
Past surgical history
To know whether the patient has undergone any eye surgery in previous years or not.
Also to know whether the patient has undergone any other surgery or not.
Personal history
Collecting the patient’s personal history.
Knowing whether the patient is a smoker or not.
Knowing whether the patient consumes alcohol or not.
Asking whether the patient is allergic to any substance or medication.
To know about the patient’s visual habit.
Knowing the frequency and duration of the patient’s screen time. That is to know how long the patient uses laptop, computer, smart phone.
Also know about the patient’s dietary pattern.
Family history
Collecting the patient’s family history.
Asking if any of the patient’s family members have eye disease.
Collect information about whether or not there is a hereditary condition in the family. (such as retinitis pigmentosa)
Occupational history
Obtaining occupation related information of the patient.
Like knowing whether the patient does computer related work or not.
Knowing whether the patient is exposed to radiation or chemicals during his work.
Physical examination / objective data
The inspection method is used in the physical examination of the eye.
Inspect the external eye area first, then inspect the internal eye area.
Examining the eyebrows for their symmetry and inspecting them for hair distribution.
Then check the eye position and alignment.
Inspect the eyelids for redness, swelling discharge, ptosis.
Inspecting the eyelid for entropion, ectropion.
Inspect conjunctiva and sclera for color, texture, redness, lesions, secretions.
Inspect the cornea for opacity and dullness.
Then check the corneal reflex.
Checking the iris for obesity, claudiness and redness.
Inspecting the pupil for size, shape and location.
Checking the pupillary reflex.
Checking the lens for opacity.
Diagnostic test for eye disorder
Opthalmoscopy
Ophthalmoscopy is a diagnostic procedure in which the back part of the eye is examined with the help of an ophthalmoscope. Such as retina, choroid, optic disc and blood vessels are examined. There are two types of ophthalmoscopy:
1) Direct Ophthalmoscopy
2) Indirect Ophthalmoscopy
1) Direct Ophthalmoscopy :
Direct ophthalmoscopy is used to examine the anterior structures of the eye. Direct ophthalmoscopy uses a handheld (torch-like) instrument (ophthalmoscope). In which light source and lens are installed. The ophthalmoscope is held close to the eye and the anterior structure of the eye is examined.
2) Indirect Ophthalmoscopy :
Indirect ophthalmoscopy provides a wider view than direct ophthalmoscopy, i.e. provides a complete view of the retina. In indirect ophthalmoscopy, the examiner wears a headband to which the lens is attached, and the lens is held close to the patient’s eye and examined. A bright light source (such as a slit lamp) is used for this purpose.



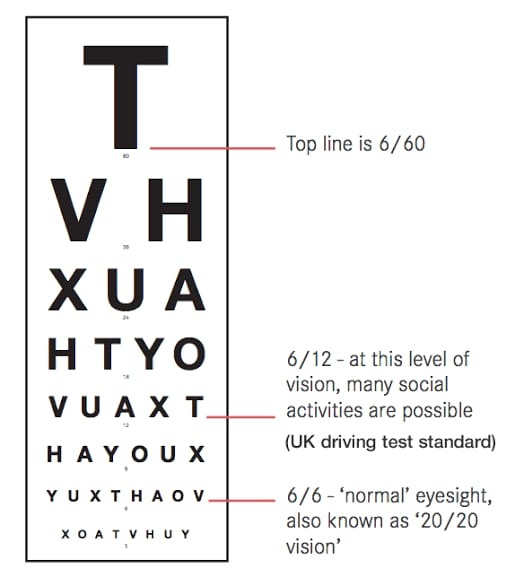
Visual acuity test
A visual acuity test is a diagnostic method used to check the sharpness of vision. For which mainly Snellen chart method is used. In this method, a person is exposed to rows of different sizes of words and symbols in the Snellen chart as shown below from a distance of 20 feet (6 meters) and the visual acuity of the person is checked. During this test one eye of the person is covered. During which a person stops reading, the number written in that row and which eye is noted. Then this procedure is done in the other eye and its visual acuity is checked. 20/20 or 6/6 is considered normal vision.
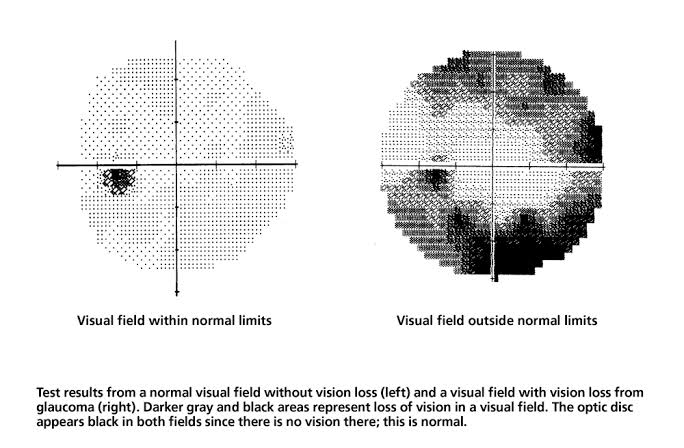
Visual field test
A visual field test, also known as perimetry, is a diagnostic test used to check peripheral vision. During this test, the patient is seated in front of the machine and asked to focus on a target light, in addition, a light or other stimulus is placed in a different area of his visual field and the patient’s response to this stimulus is checked and the boundaries of the visual field are drawn. And the area of visual loss is detected. A visual field test is used to detect blind spots and to evaluate glaucoma, optic nerve damage, and neurological conditions that affect vision.
Refraction test
A refraction test is a standard procedure used to determine a person’s eyeglass prescription, i.e. helps determine the number of lenses needed in people with vision problems. In this test, the doctor asks to read from a chart using different lenses and identify the lens for accurate vision. Refractive errors like myopia, hypermetropia, presbyopia and astigmatism can be detected with the help of a refraction test.

Gonioscopy

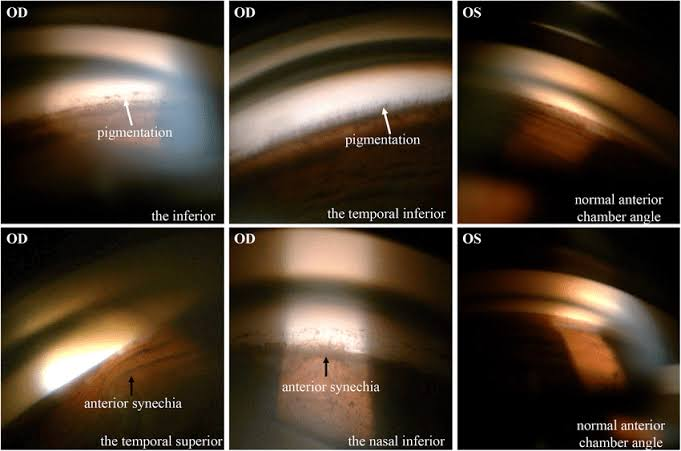
Gonioscopy is a diagnostic method used to examine the angle formed between the iris and the cornea. This angle is located where the aqueous humor drains from the eye. In a gonioscopy test, a numbing drop is instilled into the eye and then a special lens called a gonioscope is placed in the eye. With the help of which the internal structure of the eye is examined, especially the angle between the iris and the cornea. With the help of which one can know whether the angle is open, close or narrow. Gonioscopy is used to examine eye angles in conditions such as glaucoma.
Ultrasound biomicroscopy



Ultrasound biomicroscopy is a non-invasive imaging technique. In which high frequency ultrasound waves are used to examine the eye structure, providing a detailed image of the anterior part of the eye. Ultrasound biomicroscopy is used to detect glaucoma, cataracts, tumors and anterior segment abnormalities.
Slit lamp examination


Slit lamp examination is a common procedure used by eye care professionals to visualize eye structure. Slit lamp examination involves examining the eye structure in detail with the help of a specialized microscope called a slit lamp. A thin focus light beam is produced by this slit lamp and is used to examine the iris, cornea, retina and lens. Slit lamp examination provides 10-25 times magnification.
Tonometry
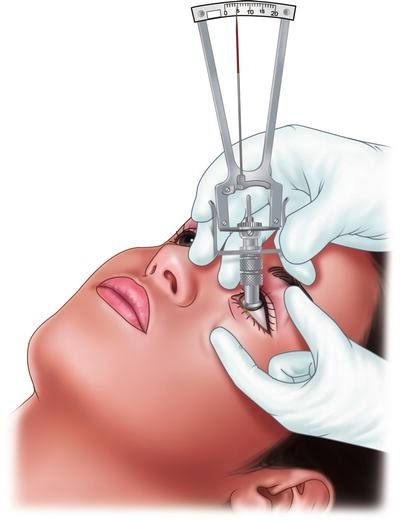

Tonometry is a diagnostic test. It is used to measure the pressure inside the eye, called intraocular pressure. Tonometry involves measuring intraocular pressure using a tonometer instrument. Tonometry involves instillation of a topical anesthetic eye drop into the lower conjunctival sac. Then with the help of a tonometer instrument, pressure is gently applied to the eye and a puff or air sand is applied to its surface and the intraocular pressure is measured. This pressure is measured in millimeters of mercury (mmHg) units. Tonometry is used to measure intraocular pressure in glaucoma as well as other eye conditions.
Pupillary dilation test


This is a simple test in which a special drop is instilled in the eye that dilates the pupil. With the pupil dilated, the retina can be systematically examined.
Electroretinography
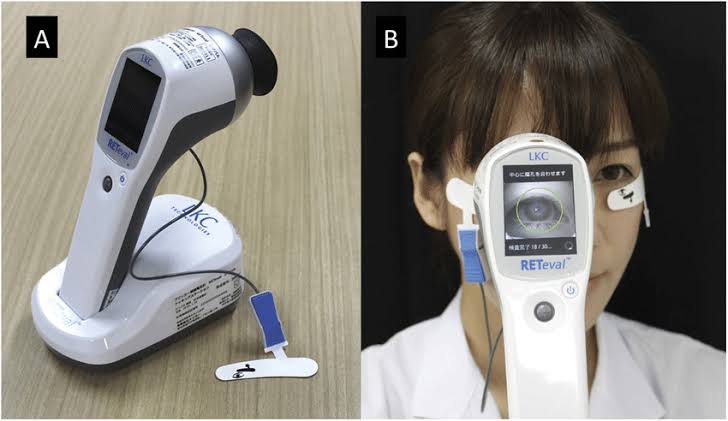
Electroretinography is a type of diagnostic test that measures the retina’s response to light. Electroretinography measures the electrical response of different cell types in the retina such as photoreceptor cells, inner retinal cells, and ganglion cells. In electroretinography, electrodes are placed in the skin surrounding the cornea or eye and the electrical response generated by retinal cells is checked when stimulated by light. The patient’s eye is then dilated and asked to focus on light sources and the electrical signal is recorded and analyzed. Electroretinography is used to evaluate retinal function and diagnose various retinal disorders such as retinitis pigmentosa, macular degeneration, diabetic retinopathy.
Color fundus photography

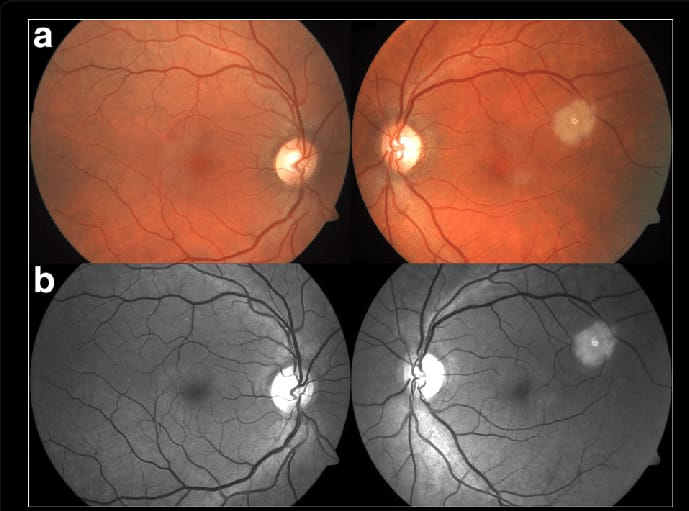
Color fundus photography is a non-invasive diagnostic method that provides a detailed image of the back part of the eye. Specifically retina, optic disc, macula, blood vessels. In color fundus photography, the eye of the patient is dilated, then a specialized camera with a front side lens and filter is placed on the patient and the camera is focused on the back part of the eye and a photo is clicked from different angles and that photo is analyzed. Color fundus photography is used to detect retinal diseases early. Like diabetic retinopathy, retinal detachment, age related macular degeneration
Fluorescein angiography
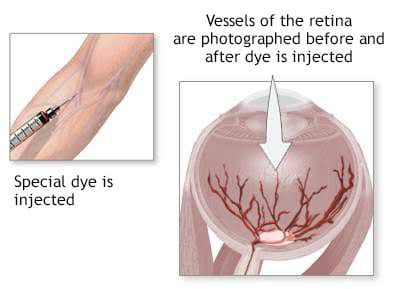
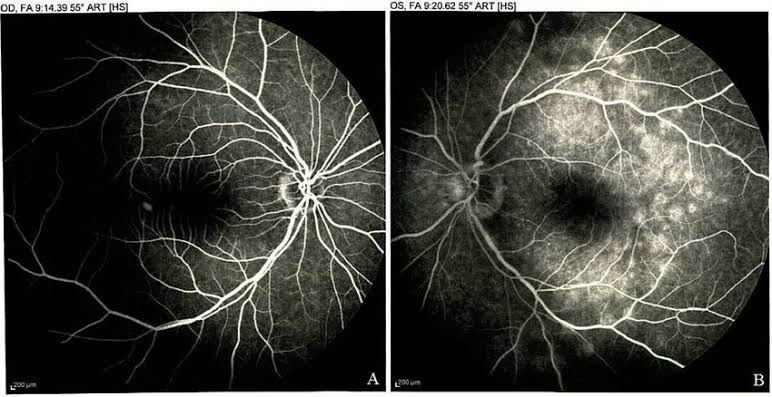
Fluorescein angiography is an invasive imaging study. It is used to check the status of blood vessels in retina and choroid. In fluorescein angiography, a small amount of fluorescein dye is injected into a vein, mainly in the arm, which reaches the blood circulation through the eye. Then, with the help of a specialized camera, the photo of that area is taken and observed. Conditions like retinal vascular disease, macular degeneration, diabetic retinopathy can be detected with the help of fluorescein angiography.
Corneal topography
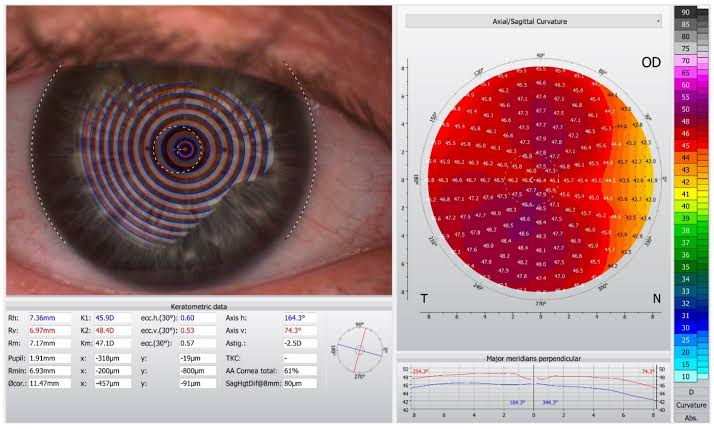
Corneal topography is a non-invasive diagnostic method in which a map of the cornea is prepared to obtain information about the shape, curvature and elevation of the cornea.
Corneal topography is used to identify astigmatism, keratoconus, and irregular corneal shape. In addition, this method is used before refractive surgery, fitting contact lenses, and corneal transplants.