ENLGISH msn-2-oncology-Part-02
Oncology:-
♦ What is Oncology?? (What is oncology??
Oncology is the branch of medicine that deals with the diagnosis and treatment of cancer. A person who is associated with the practice of Oncology is called an oncologist.
Oncology is
ONKOS MEANING= BULK, MASS, TUMOR.
LOGY MEANING: = STUDY OF
Words have come together Oncology.
There are three main branches of Oncology.
1) Medical oncology: In this treatment starts with drugs and chemotherapy.
2) Surgical oncology:- In this cancer is treated by biopsy, any surgery, and surgical resection of any tumor etc.
3) Radiation oncology: In this any type of cancer is treated by therapeutic radiation.
♦ DEFINE CANCER OR WHAT IS CANCER:=
Cancer is a group of diseases in which there is uncontrolled growth of cells and there is invasion in the nearby tissue and it can also spread in the whole body system. Cancer is a disease in which there is uncontrollable growth and multiplication of cells that can go nearby and spread throughout the body. Cancer cells spread through the blood and lymphatic system in the body. Cancer is not a disease but a group of about 100 cancers. Cancer is anywhere in the body or not. Cancer is named after the part it is on.
♦ EXPLAIN STRUCTURE OR CHARACTERISTICS OF NORMAL CELLS.
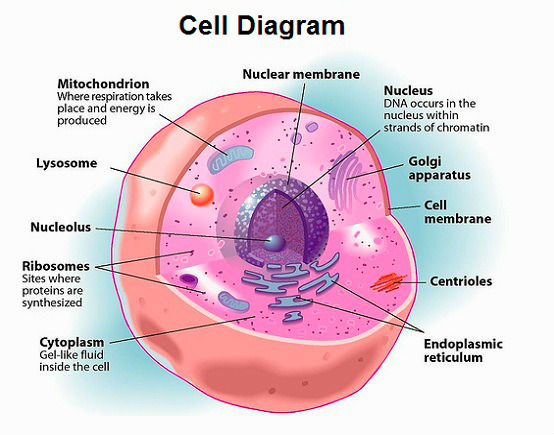
1) Mitotic division leads to the formation of two daughter cells.
2) In this, the shape, size, and arrangement of the daughter cell are the same as the original cell.
3) In this cell is built for any specific function.
4) It does not invade blood circulation and lymphatic circulation.
5) In this the division of the cell is stopped. When it comes in contact with any other cell i.e. it has properties for contact inhibition.
6) These cells cannot spread to other places in the body.
♦ EXPLAIN STRUCTURE OR CHARACTERISTICS OF ABNORMAL CELLS.
1) Cell division in this produces many daughter cells that do not even look like the parent cell.
2) It causes rapid growth of cells.
3) In this the daughter cell is different from the normal cell in shape, size and appearance.
4) These cells are not produced for a specific purpose but grow abnormally.
5) This CELL travels in the blood to the lymphatic circulation and to other systems of the body.
6) It does not have contact inhibition characteristics so the CELL continues to grow abnormally and forms a tumor like structure.
7) It spreads to other organs in the body and causes growth.
♦ What are the differences between Benign tumor or Malignant tumor? What is the difference between a benign tumor and a malignant tumor (cancerous tumor)?
Benign tumor:-
1) CELL feature:= In this CELL growth takes place and forms a tumor like structure but this tumor is not cancerous.
2) CELL growth rate:= In this the growth of CELL is done slowly.
3)Tissue damage:= In this the tissue is slightly damaged.
4)Metastasis:= Tumor of CELL stays in the same place where it formed and does not go to another place.
5) General effect := This benign tumor is less harmful as it does not exert any pressure on the circulation.
6) Treatment and follow up: After this tumor is surgically removed, no follow up is required.
7)
Malignant tumor (malignant tumor) 1)CELL features:= Thus. The tissue is undifferentiated and often bears little resemblance to the normal cells of the tissue and the growth of the malignant cells.
2) GROWTH RATE:= This CELL grows very fast.
3)Tissue damage:= This damages the tissue to a very high extent and causes necrosis of the tissue.
4) Metastasis:= This tumor can spread to nearby organs and distant organs.
5)General effect:= This is extremely damaging as it damages normal shell as well.
6)Treatment and follow up:= Chemo therapy and radiation therapy are required after surgical removal of this tumor.
7)Severity:= This tumor is not controlled and this tumor leads to death.
Cancer: Cancer is a very large disease in which cells grow abnormally and form a tumor-like structure and this tumor spreads to other parts of the body It alters the function of cancer so it is very dangerous There is a disease.
Etiology and risk factors:= Etiology:=
1) Age: The chances of getting cancer increases with age because as age increases, the immune system of the body decreases and due to this, diseases like cancer occur.
2) Gender:= In male:= Prostate, lung, gastrointestinal tract, bladder etc.
In females:= Breast cancer, colon, lung, uterus are the most common cancerous site in females.
3)Race:= Black community has more chances of getting cancer than white community.
4) Genetic / Hereditary: = The chances of cancer to their sons or daughters are higher than that of normal people who are inherited.
5)Immunological Factor:= When the immune system of the body is reduced, there are chances of getting cancer because the immune system is not a fighting force against the cancerous cell and due to this condition like cancer occurs.
6) Psychological factors:= In the psychological sector, people who take too much stress cause the hormone level to increase and the immune system of the body gets altered. And it causes conditions like cancer.
7) Hormonal Factor: = Endogenous: = This has a body’s hormone changing and causing cancer of organ, uterus and prostate gland.
Exogenous: = In this, due to taking any kind of oral contraceptives, hormone imbalance occurs and due to this, cancer occurs in the body.
External risk factor:= External factors include any type of chemical, radiation, virus, tobacco and alcohol, obesity, and excessive exposure to sunlight. Cancer is caused due to coming.
1) Chemical carcinogens:= Cancer condition can arise in the body due to coming into contact with certain types of chemicals.
Example:=asbestos, arsenic, chemical therapy.
2) Radiation therapy:= In this there are more chances of skin cancer due to thinning of ozone layer due to ultraviolet rays of sunlight.
3)viruses: = Some types of viruses lead to cancer in humans.
Example:= Epstein barr virus is linked with ->Lymphoma,
herpes simplex,
Cytomegalovirus,
human papillomavirus type 16-18,
HIV virus.
4)Diet:= Certain types of food and food additives cause cancer of the gastrointestinal tract. Low fiber diet causes colon cancer Smoked and processed meat causes liver cancer. Excessive fat, alcohol, food containing nitrate, high calories in diet also cause cancer.
5)Tobacco:= Due to tobacco and smoking, cancers like mouth cancer, esophageal cancer, esophageal cancer and lung cancer, oral cancer etc. are caused.
6) Alcohol use := Cancer of oral cavity, larynx, esophagus etc. is caused due to consumption of alcohol.
7) Recreational drug use := Due to this, the immunity of the body decreases. Marijuana smoke is more dangerous because it causes lung cancer.
8)Obesity:= Excess body fat causes hormone related cancer.
9) Sun exposure:= Excessive exposure to sunlight causes skin cancer.
Chemical agent := Aromatic amyl, Different type of dyes, arsenic, benzene, zinc, wood dust, polyvinyl chloride. Cancer is also caused by chemical substances like etc
Classification of cancer cells:=
1) GRADDING,
2) STAGGING,
3) T.N.M.
(T=TUMOR, N=NODE, M=METASTASIS.)
GRADDING:= A = Anaplasia
(This shell is not identical to its parent cell but looks different.)
GRADE 1:=
This grade is called low grade malignancy. Cells are similar to normal parent cells. It has <25% Anaplasia cells.
Grade2:=
These are low to moderate degree malignant cells. Some cells are normal and some cells are cancerous.It contains 25 to 50 % Anaplasia cells.
Grade 3:=
It has moderate to high grade cell malignancy. It has 50 to 75% Anaplasia cells.
Grade 4 :=
thus. There is high grade malignancy.And all shells are malignant. It has >75% Anaplasia cells.
Staging:=
Stage (0): = No of any type of ab normal cell is found because it is in the first layer of the Abnormal Cell A cell.
Stage 1:= In this the cancer is in the cell primary site only.
Stage 1 (a): = The canceric cell has a small amount and visible in the microscope.
Stage: = 1 (b): = It has a high amount of cancer.
★ Stage 2:= In this, the cancer spreads to the nearby area.
stage2(a):= In this cancer is the primary area. only spreads.
stage 2 (b):= In this the cancer has spread to other tissues and organs.
stage 3:= In this the cancer spreads in the area near the throw out.
Stage 4: In this, the cancer spreads to other parts of the body.
Stage 4(a) := In this the cancer has spread to nearby body parts.
Stage 4(b):= In this the cancer has spread to other organs and tissues of the body.
Classification on the basis of TNM (TUMOR, NODE AND METASTASIS)
1) TUMOR:= This depends on the size of the tumor and its extension. Tx:= Tumor cannot be evaluated in this. To := In this some cells are abnormal but no sign like tumor is seen.
T1234:= Tumor size and extension similar to primary tumor.
N =NODE := Thus. Depends on the extent of lymph node involvement.
Nx:= It cannot be evaluated that there is a cancerous cell in the lymph node.
N1:= meta stasis of cancer cells in this no lymph node. Found in nearby area and region.
N2:= In this case, the cancer cells are between N1 and N3, meaning they have not spread to all tissues.
N3:= In this the sarcoid cells are spread in many areas of the lymph node.
METASTASIS: In this the cancer cell spreads to another part of the body. M1:= It does not show umeta stasis of the cell. M2:= In this, the cancerous cell is in another part of the body (organ). But spreads
Detection of cancer:= >History taking, >Physical examination, >Laboratory investigation.
History taking:= In this a complete assessment of the patient is done in which the patient is asked whether the patient has any type of surgical history in the past or any signs and symptoms of cancer in the past or not.
Physical examination:= Looking at the patient when we are doing physical examination
Anorexia:= ( Anorexia := Loss of appetite). weight loss:= (weight loss = weight loss).
Anemia
weakness
Fatigue
To see if the patient has signs and symptoms like pain etc.
1) lymphadenopathy, 2) suspicious mole, 3) Breast mass, 4) Thyroid mass, 5) Prostate enlargement, 6) oral leukoplakia = white sores in the mouth) so see if the patient has any such sign or not.
Laboratory test:=
1) Phosphate specific antigen:= This is a laboratory test for detection of prostate gland cancer.
2)Complete blood count (cbc):= This test is done to see if there is a condition like anemia or not and if there is anemia then almost colon cancer can be detected.
3) Stool test (blood*in stool):= If blood is found in the stool, it can be the cause of colon rectal cancer.
4)Biopsy:= Thus. If there is any abnormal cell growth, a small piece of that cell is taken and it is subjected to microscopic examination in the laboratory and detection of cancer is done.
This biopsy can be taken from organs like liver, kidney, spleen, lungs, breast etc. and detection of cancer can be done.
5) Cytological study (Psychological study):= In this diagnostic test, samples like papsmear are taken and it can be taken mainly from cervix and oral cavity.
6)Ultrasound test:= High frequency sound wave is used in this test and ultrasound is mostly done for detection of abdominal, pelvic and breast cancer.
7) MRI (magnetic resonance imaging):= This test is done to see if there is any cancer of central nervous system spine, head and musculoskeletal system etc.
8) Radiological study:= X-ray is done to check for bone cancer and cancer of any hollow organ. Chest x-ray is done for detection of lung cancer. Mammography is done for detection of breast cancer.Contrast media is used for detection of cancer of bone, gastrointestinal system, urinary system etc.
9) CT SCAN (COMPUTED TOMOGRAPHY):= CT scan gives a 3-dimensional, cross sectional, computerized body nu picture CT scan shows the size of any tumor and its location accurately. Ct scan shows differentiation between malignant and non malignant.
10) Nuclear imaging procedure:= This test is done to detect cancer of organs like brain, kidney, liver, lungs, pericardium (outer layer of heart) and bone etc.
11) pet test (positron emission tomography):= This test is done to detect cancer of organs like lungs, colon breast, bone, brain etc.
Other test:= Blood test, urine test, pap smear test, Afp (alpha photo protein for liver cancer) etc test used for detection of cancer.
Prevention of cancer :=
Primary prevention
It is done to reduce the risk factors.
OBJECTIVE:= 1) To strengthen healthy lifestyle. 2) To minimize Weakness. 3) To reduce the risk factors of cancer.
Influencing factor of carcinogenesis:=
Diet:= Fatty, alpha toxin, non antioxidant, smoky, uncooked raw food.
smoking and drinking,
★viral infection,
★parasite,
★ chemical agents,
★ultraviolet rays, x-ray,
★Obesity,
★polluted environment,
lack of exercise,
★Limited to health care services.
prevention of cancer:=
1) Eat green leafy vegetables.
2) Consuming fiber rich food.
3) Do not take Vitamin A and Vitamin C.
4) To improve the quality of life style.
5) Exercise daily.
6) Eating less fatty matter in food.
7) Less intake of sweet substance in food.
8) To use medical facilities properly.
9) Avoiding the things that are responsible for causing cancer like tobacco, cigarette smoking, sedentary life, stress, fatty and spicy food and many other things that are responsible for cancer.
10) Do not use alcohol.
11) Avoid excessive sun exposure.
12) Avoid excessive exposure to X-rays and ultraviolet rays.
13) To provide health education to the people about the causes of cancer and also to provide health education to prevent it.
14) Telling people to work little by little Telling them not to lead a sedentary life.
15) Asking people to keep doing regular health checkups.
2) secondary prevention:=
This secondary prevention includes early diagnosis and prompt treatment which requires early screening of cancer.
objective:= 1) Early diagnosis and investigation of Abnormality. 2) Assessment of the risk group. 3) Cancer screening and early detection.
THE WARNING SIGN OF CANCER:=
CAUTION:= C:=CHANGE IN BOWEL AND BLADDER HABIT, in this there is a change in the color of the stool, its size and its shape.ex:=Diarrhea, constipation.thus. Blood is present in urine and stool.
A:=A SORE WHICH DOES NOT HEAL, as in any kind of sore. healing does not come.
★more bigger, ★more pain full, ★start bleeding from the sore.
U :=UNUSUAL DISCHARGE AND BLEEDING, Blood comes in urine and stool.
Discharge from any part of the body like nipple, penis.
T: = THICKENING OF LUMP IN BREAST AND OTHER BODY PARTS, When breast self examination is done, lump, mass is seen in breast. Lump can be found on any part of the body.
I := INDIGESTION AND DIFFICULTY IN SWALLOWING, in this there is pressure in the throat and chest and due to this difficulty in swallowing (SWALLOWING). Even if a little is eaten, the stomach feels very full.
O :=OBVIOUS CHANGE IN MOLE, USE THE ABCD RULE,
A:= ASYMMETRY See if the mole looks the same or different from all the parts.
B:=Border See whether the border is sharp or rough.
C:= color To see what kind of color is found in the mall.
D:=Diameter To see if the diameter of this mole is bigger than the eraser ie bigger or smaller than 6 mm.
N:=NAGGING, COUGH SORENESS.
To see if there is a change in the voice or not, to see how long the phlegm comes, to see whether blood is seen in the phlegm or not. Ask the patient about all these cancer warnings.
To do health assessment of the patient.:=
tacking history (asking patient history),
family and personal history of cancer, (asking any people if they have a history of a disease like cancer or not).
tobacco use and alcohol consumption,
occupation (asking about his occupation),
Medication (asking about medicine).
Encourage the client for early detection of cancer:=
MAMMOGRAPHY (Mammography) := Examination of breast is done in mammography.
Age 20-30 should have mammography done once in 3 years. All women >40 years of age should have a mammogram every year. > Every woman should do breast self examination after the age of 20.
★ If there is any abnormality in the breast, immediately report it to the health care worker and if any perpendicular mass or size symmetrical abnormality is observed in the breast, immediately inform the health care professional or the health care personnel.
★ Daughters should seek advice from a health care member if anyone in the family has a history of breast cancer.
Colon and rectal cancer: After the age of 50, every man and woman is at risk of developing colorectal cancer. So after the age of 50 the following tests should be done.
1) FECAL OCCULT BLOOD TEST (FOBT) should be done every year.
2) ( FIT ) FECAL* IMMUNOLOGICAL TEST should be done every year.
3) FLEXIBLE SIGMOIDOSCOPY should be done every five years.
4) Colonoscopy should be done every 10 years.
5) DOUBLE CONTRAST BARIUM ENEMA TEST should be done every 5 years.
6) CT COLONOGRAPHY should be done every five years.
7) stool DNA test.
CERVICAL CANCER :=
1) After vaginal intercourse every woman should be screened for cervical cancer every 3 years.
2) After the age of 30 years women, if 3 pap smear tests are normal, then they should continue to undergo pap smear test every two to three (2-3) years.
3) If a woman has a risk factor such as Diethylstilbestrol exposure, HIV infection, or a weakened immune system due to organ transplantation, chronic steroid use, such women should undergo a pap smear test every year.
4) If a woman is above 70 years and her 3 pap smears are negative, she should be examined every 10 years.
Endometrial cancer (uterine) If a woman has had a total hysterectomy, she does not need to undergo a pap smear test.
If a woman has a history of colon or rectal cancer, she should undergo a pap smear test
TERTIARY PREVENTION:=
Tertiary prevention is done to prevent metastasis of normal cells, to provide cancer treatment, to cure it, to do rehabilitation and to provide palliative care.
The following treatment is useful for cancerous patients
RADIATION THERAPY
CHEMOTHERAPY, (Chemotherapy)
GENE THERAPY
BIOTHERAPY (Biotherapy)
BONE MARROW TRANSPLANTATION
1) Radiation therapy: Ionizing radiation is used in radiation therapy. >Abnormal cellular growth is prevented using radiation. >This radiation therapy damages and causes necrosis of the cancer cells.
purpose:= 1) primary:= primary purpose is only for the treatment of cancer and its cure.
Example := Hodgkin’s disease, skin cancer, Prostate Cancer, cancer of cervix.
2) Adjuvant:= This is used only in pre-operative and post-operative conditions. And it is used with chemotherapy.
3) Palliative: This is used in any emergency condition. > Like, superior vena cava compression and spinal cord compression etc.
4) Prophylactic purpose: This radiation therapy is given only in the suspected area.
Action of radiation therapy:= 1)Normal cell:= Radiation therapy affects the normal cell but the normal cell has the capacity to grow back. So radiation therapy does not cause problems in normal cells.
2) Abnormal cell: X-ray and gamma rays destroy the genes of cancerous cells and allow them to grow.
type of radiation therapy: = 1) External = telly therapy, 2) Internal
1) External therapy:= In this therapy, x-rays and gamma rays are applied directly over the cancerous cell. And its most common advantage is that this therapy affects the maximum depth area of the cell. It not only affects the upper surface area but also goes deep inside and destroys the cancer.
2) Internal therapy: = (brachytherapy) In this, radiation therapy is directly implanted inside the cell.
It has Two Types: = 1) Sealed (Shield): = Ama radiation therapy is used by needle, tube and applications and providers Abonermalsel.
2)unsealed:= In this radiation is provided in the form of tablets and injections.
safety standards of radiation therapy:=
Distance: Health care personnel should stay away from the patient’s bed while providing radiation therapy.
It is not necessary to stand near the continuous patient’s bed while providing radiation therapy.
Time:= While giving radiation therapy to the patient, work can be done by the side of the patient for a maximum of 30 minutes.
Shield: Health care personnel should use a protective shield while providing radiation therapy and cover all parts of the body.
When providing radiation therapy, health care personnel should use a dosimeter to determine the radiation dose.
A separate private room should be kept for health care personnel. In which they can wear personal protective equipment.
Children and pregnant women are the same place when providing radiation therapy. should be kept away from
side effect:= (dish phagia), (difficult Nausea, (Nozia)
vomiting
Diarrhea
Dysphagia
y in swallowing := difficulty in swallowing)
fatigue
weakness,
stomatitis (inflammation of the mucous membrane of mouth),
loss of appetite,
leukoplakia (decrease in WBC), Increase the risk of infection,
Body ache
Alopecia (Alopecia :=hair loss)
Nursing management of radiation therapy:=
-Explaining radiation therapy to the patient.
-Explain to the patient the equipment required and the time of the procedure.
-Telling the patient to visit his relatives less frequently while receiving radiation therapy.
-Insertion of catheter to mt the bladder.
-Giving the patient a low salt diet.
-Give antidiarrheal agent to the patient.
-Assess the patient’s skin integrity.
-Seeing whether the patient has hair loss or shedding of skin.
-Assess the patient’s oral mucosa.
- To see if the patient has conditions like nausea, vomiting, diarrhea or not.
-To check whether the patient has anemia or any blood abnormality.
- To see if the patient has fatigue, malaise and body ache or not.
-Instruct the patient not to use any ointments and lotions or powders.
-Tell the patient to maintain oral or VT hygiene and do not do it in an irritation manner by saying that it is a brush.
-Tell the patient not to come in contact with sunlight.
-Tell the patient and his family members to stay away from the patient and keep contact by telephone while JAY is providing radiation therapy.
2) Chemotherapy: Cancer is treated using chemicals in chemotherapy.
chemo := chemical. ,
Therapy:= treatment.
It uses tablets and injections to treat cancer.
purpose of chemotherapy := curative: to cure cancer in this.
control := This has no purpose to control cancer. Palliative := It has the purpose of reducing the symptoms. Drugs which are used in chemotherapy:=
GROUP:= ALKYLATING AGENT.
Example: = cisplatin,
1) Action:= This drug disturbs the DNA of the cancerous cell.
Responsibilities: Corticosteroids should not be used while administering this medication. It i contraindication.
2) Group:= Antimetabolites agent Example:= fluorouracil.
Action:= This medicine prevents the DNA of cancerous cells from forming.
Nursing responsibilities:= While giving this medicine, also give folic acid pill to the patient.
3) Group:= Mitosis inhibitor agents.
example:=vincristine,
Vinblastine,
Action:= It inhibits mitosis of malignant cell mass.
Nursing responsibilities:=provide palliative care.
4) Group:= Hormonal agents (Antiestrogen):=
Example:= tamoxifen (tamoxifen).
Action: In this, the hormone level of the malignant cell is altered.
Nursing responsibilities:= Provide palliative care to the patient.
5) Radiation therapy (radiological sodium and iodine):=
Action := inhibited the Malignant cell growth. Nursing responsibilities:= To ensure that the patient gets less side effects from coming in contact with radiation.
6) Group:= Antibiotic,
Example:= Bleomycin
Action:= Anti micro bl agent.
Nursing responsibilities:= Do not give live vaccine to the patient.
Route of drug administration:= Oral, Intramuscular, Intravenous, Interactive, Intrathecal, Intraarterial, Subconscious, Applied topically.
common side effect of chemotherapy:=
1) Skin := Anemia, hyperpigmentation, photosensitivity,
2) Blood:= Bone Marrow suppression, Anemia, Leukopenia, Thrombocytopenia,
3) GI tract := nausea, vomiting, constipation, diarrhea, ulcer
4) Genitourinary system:= Nephrotoxicity, Cystitis, Weight loss, Fluid loss, Weakness.
Nursing management:=
To check patient’s vital signs.
Keep the patient in isolation.
Tell the patient to maintain his personal hygiene.
Giving the patient a well balanced diet.
Checking the culture and sensitivity of the patient.
Do a head to toe physical examination of the patient.
View the patient’s bleeding time, clotting time and platelet count.
Prevent the patient from bleeding.
Take care to keep the patient at least erect.
When injecting and
While doing catheterization.
Tell the patient to avoid sweet alcohol and smoking
Give the patient food as he likes.
Give food that is calorie rich, high protein, high fiber, vitamin C and all vitamins are available.
Tell the patient to maintain his oral hygiene.
Give antiemetic to prevent patient from vomiting.
To see if the patient has hair loss.
To cut the patient’s hair before treatment.
Lubricate the patient’s scalp with vitamin A and D.
Tell the patient to keep doing some activity.
Asking the patient to keep his will power strong.
Ask the patient to express his feelings properly.
Giving psychological support to the patient.
Checking the patient’s fluid and electrolyte levels.
Provide chemo therapy to the patient.
To clear all doubts of the patient and his relatives.
BIOTHERAPY := Biological response modifier (BRM) calmette guerin is used in biotherapy and stimulates the body’s natural immune system that fights against cancerous cells and destroys them.
There are three categories of biotherapy :=
1) Non specific, 2) monoclonal antibody, 3) cytokines.
1)Non specific:= In non specific we use non specific agents like bacillus calmette guerin and corynebacterium parvum which stimulate the body’s immune system when any antigen enters the body. produces antibodies to fight against it.
2)Monoclonal antibody := In this method, the same antibody made to fight against any cancerous cell in the body is introduced inside the body and it is done to fight against the cancerous cell.
3) Cytokines: In Cytokines, antibodies are produced from the body’s healthy immune system and are introduced into the patient’s body to fight and destroy the cancerous tumor.
It has four types:= interferon,
interleukin, (intervukin)
colony stimulating factor (colony simulating factor),
tumor necrosis factor
Gene therapy Gene is a functional unit.
In genetics, a normal gene is inserted into the organism to correct the genetic defect.
AIM: = Gene therapy is a permanent therapy. Because it has a permanent gene it is changed and the genetic material of the cancerous cell is changed.
Indication:=
1) cancer,
2) Infectious diseases,
3) Inherited disorder, genetic disorder.
ex: thalassemia, Hemophilia
Process of gene therapy: In gene therapy, abnormal cells are copied. Then the abnormal cell rhythm is removed from the patient’s body and a normal one is inserted into the patient’s body.
Method of gene therapy :=
Ex vivo,
★In vivo.
Ex vivo:= The target gene is taken outside the patient’s body.And that gene is inactivated and abnormal cells are inactivated and introduced back into the patient’s body.
Only some of the cells are developed in to Ex vivo like := Lymphocytes, Hepatocytes, In vivo = In this method the healthy gene is directly inserted into the body of the patient. Through vector (virus), through non vector
By vector:= In this method, the virus is used to take out its gene, after introducing a healthy gene into it, it is administered to the patient through intravenous administration.
In which:= Edino virus, Retrovirus, Herpes virus etc.
Non vector := In this directly organ or artificial chromosomes are entered.
Advantage:= This gene therapy is a permanent therapy because normal gene is inserted with abnormal gene. And if gene therapy is used, then no other therapy is needed, or any other treatment at all. And if ovum and sperm are used in this gene therapy, the genetic disorder can be reduced.
Disadvantages:= If any infectious virus is used in this gene therapy, the chances of infection in the body increases.
It is not useful for all diseases. This process is very expensive.
Immune response: The body of the mother shows an immune response when any foreign body enters.
Bone Marrow Transplantation: In bone marrow transplantation, cells from the marrow are collected from the patient or from a donor and the healthy cells are administered back into the patient’s body for therapeutic purposes.
Indication: Oncology disorder like leukemia, Lymphoma.
Haematological disorder: Anemia, Aplastic Anemia, Sickle cell Anemia.
Type of bone marrow transplant:
1) Autologous,( autologous) 2) Allogeneic, ( allogenic) 3) syngenic. (Cinegenic).
1) Autologous: This is a procedure in which stem cells are collected from the patient’s healthy bone marrow.
Chemo therapy and radiation therapy are then provided to the patient.
And then it is confirmed that almost all the cancerous cells have been destroyed.
Healthy stem cells are then inserted into the patient’s body.
2) Allogeneic:= In this, stem cells are taken from the healthy bone marrow of the patient’s parents (parents) or his siblings.
And it is transplanted into the patient’s body.
3) syngenic: =
In this the stem cells are taken from the twins.
And this bone marrow has a higher chance of matching.
It is then inserted into the patient’s body.
PROCEDURE:= Bone Marrow transplant is done through a central line in the operation theatre.
-> The timing of this depends on the patient’s cancer condition and CVRT.
-> It takes a minimum of 30 minutes and a maximum of 4 (four) hours.
-> When bone marrow is transplanted it gives burning sensation.
->complete bone marrow transplantation is completed only when the patient’s body starts making healthy cells.
Nursing management := –>To prepare the patient physically and psychologically.
Explaining the procedure to the patient and his family members.
The patient and his family members should be informed about the risks, benefits and consent to return.
Keep the patient in isolation.
Restrict entry to visitors.
Monitor the patient for any side effects of chemo therapy and radio therapy during this time.
View patient’s intec output.
To check patient’s vital sign.
Administering i.v. fluid to the patient.
Maintain strict aseptic technique.
To administer the prescribed medicine blood component.
Providing psychological support to the patient.
Communicate coping skills to the patient and his family members.
Dressing properly over the central line after bone marrow transplantation.
To see if there is any type of infection after bone marrow transplantation.
Tell the patient and his family members about regular follow up.
complications :=
-> Hematopoietic := Infection, nosocomial infection, Anemia.
->Gastrointestinal Tract:= Nausea, Vomiting, Diarrhea.
-> Renal and Genitourinary:= Renal failure, Hemorrhagic Cystitis,
-> Hepatic:= Hepatomegaly, Bilirubinemia, Coagulopathy disorder.
-> Pulmonary := Bacterial Pneumonia, Fungal infection, TB toxoplasmosis, Pulmonary, fibrosis.
Nursing management of patients with cancer :=
1)Nursing Assessment:=
-> Assessing patient’s pen level.
-> To check patient’s vital sign.
-> Checking the patient’s urine output.
-> Check the patient for any kind of scratches or sunburn on the body.
-> Assess skin integrity of passion.
-> Being aware of whether the patient has hair loss.
-> Observe patient for bleeding from oral cavity and observe oral hygiene.
-> Asking about Passion’s bowel and bladder habits ie whether he has conditions like diarrhea or vomiting.
Nursing diagnosis:=
1) Chronic pain related to cancerous conditions as evidenced by verbalisation with the client.
Relieving pain:=
1) Assess the patient’s pen level.
2) Giving the patient a comfortable position.
3) Involving the family in the patient’s care.
4) Giving the patient mind diversional therapy.
5) Providing work and kind environment to the patient.
6) Provide analgesic to the patient.
2) Self care deficit related to disease condition As evidenced by observation of the client condition.
Nursing intervention:=
1) Providing work and clean environment to the patient.
2) Provide a clean and wrinkle free bed to the patient.
3) Changing the patient’s bed sheet and clothes daily.
4) Maintaining personal hygiene of the patient.
5) To involve Prashant during his care.
6) Wash hands thoroughly before serving food.
3) Impaired tissue percussion related to disease condition as evidenced by pinching the skin of the patient.
Nursing interventions:
1) Checking the patient’s tissue integrity and skin turgor.
2) Observe the patient’s skin side for bleeding.
3) Tell the patient to maintain his oral hygiene.
4) Don’t brush up on fashion in such a tatty manner.
5) Instruct the patient not to scratch the area of skin exposed to radiation.
6) Tell the patient to wear loose clothing.
4) Disturbed body image related to chemotherapy as evidenced by observing the hair loss of the client. Nursing interventions:= Manage hair fall :=
1) How to maintain rapport with patients and describe their feelings with them.
2) Talking to the patient very politely.
3) Ask the patient for coapency because of hair loss.
4) Tell the patient that hair loss while undergoing therapy is common so there is no need to panic.
5) Tell the patient that the hair will grow back normally after the treatment.
5) Impaired nutritional status pattern less than body requirement related to nausea and vomiting.
Nursing interventions:= Managing diet :=
1) To provide work and comfortable environment to the patient.
2) Do not maintain an environment where the patient has a bad smell while eating.
3) Giving the patient a high calorie and high protein rich diet.
4) Ask the patient to increase fluid intake.
5) Tell the patient to take small and frequent amounts of meals.
6) Feeding the patient as he likes.
6) Activity intolerance is related to weakness as evidenced by observing the activity level of the client.
Nursing interventions:=Promoting activity level
1) Assess the patient’s activity level.
2) Involving the patient in daily routine activities.
3) Ask the patient to take some rest between activities.
4) Tell the patient to do some exercise and yoga.
5) Saying or meditating to the patient.
7) High risk of infection related to bone marrow depression secondary to chemotherapy.
Nursing interventions:= Prevention from infection:=
1) Providing a clean environment to the patient.
2) Minimize visits to the patient’s side.
3) Dress the patient in rice cloth.
4) To check patient’s vital sign.
5) Asking the patient to wear a mask when going out.
6) Giving high protein diet to the patient.
7) Administering the prescribed medicine to the patient.
surgery of cancer
Following types of surgery are used to remove cancer tumor:=
1) Electrosurgery: In this, electric current is used to dissolve the tumor.
2) Cryosurgery:= In this, cancer cells and tumors are destroyed by using liquid nitrogen.
3)Laser surgery:= In this the tumor is destroyed using laser beam.
4) Ectomy: In this an incision is placed on the side of the tumor and the entire tumor is removed.
Surgery has three main aims:=
1) Curative, 2) Palliative, 3) Reconstruction.
1) Curative:= In this aim the entire tumor is removed.
2) Palliative:= In this only the cancerous cells are removed.
3) Reconstructive: In our constructive type, any therapeutic modalities like chemotherapy and radiation therapy are done at the same time as any reconstructive or cosmetic surgery.
Example: plastic surgery.
preoperative and postoperative nursing management:=
preoperative:=
Providing psychological support to the patient.
To try to remove the fear of operation from the patient’s mind.
To prepare the patient physically and psychologically for surgery.
Explain all the information about the surgery to the patient and his relatives.
Tell the patient about reconstructive surgery.
Give the patient high protein high vitamin E, D, and iron containing food.
Administering intravenous (i.v.route) fluid to the patient before surgery.
Provide blood transfusion if the patient needs it.
Preparing the patient’s operation area.
The body area of the patient should be shaved properly.
After shaving, clean the area with spirit and savlon.
Keeping the necessary medicines and blood ready for the patient.
Carry out all laboratory investigations of Eshant.
To check patient’s vital sign.
post operative:=
To check patient’s vital sign after operation.
To properly monitor the patient’s blood pressure.
Keep the patient under close observation.
Observe the patient for conditions such as shock, collapse, and hemorrhage.
Ask the patient to do deep breathing exercises after surgery.
Inspect the area to be grafted for pain, redness, swelling, or infection.
Providing proper patient position after surgery.
Proper dressing on the operation side.
If the patient is suffering from severe pain, provide Analgesic.
Checking the drainage tube and dressing it properly.
Giving antibiotics to prevent infection.
Look at the skin side for any rash, redness and inflammation.
Provide anti inflammatory drug to the patient.
Ask the patient and his family members to take proper follow up.
PALLIATIVE CARE:=
INTRODUCTION:= Palliative care is provided to reduce the patient’s symptoms.
It is provided not for the cure of the patient but for the patient who is dying or terminally ill.
Palliative care improves the patient’s quality of life during the time of death.
Palliative care is provided by trained nurse doctors as well as family members.
Palliative care m. Family members and friends are also involved.
Psychiatric, Councillor, Social worker, Spiritual worker, And Doctor are also involved.
Palliative care involves the involvement of health care personnel as well as family members and friends in the patient’s care.
Goal of palliative care:=
To relieve pain and other symptoms of the patient.
To improve the patient’s emotional status, mental status, and spiritual status.
To support both the patient and his family members.
To provide psychological support to the patient.
Services provided:=
To improve the psychological, spiritual and coping ability of patients when they are in their last stage of life.
To relive the patient’s pain and symptoms.
To teach the patient and his family members how to treat the patient.
Care pro care is provided to provide the drugs and equipment required by the patient.
Thus palliative care is provided to a patient who is in the last stage of his life to relieve the symptoms of his disease.
Hospice care
home and hospital care of patients:=
INTRODUCTION := This care is for a patient who is ill for a long time and is undergoing treatment in a hospital for a long time, so that he can be comfortable at home with his family members and friends etc. Environment (Environment) and the patient is treated.In hospice care, a home-like environment is created around the patient.
service setting:=
home,
Hospice, hospital’s,
Hospice home,
Hospital
In all these areas family members and friends are involved and care is provided to the patient.
This involves the involvement of the hospital health care personnel along with the family members in the patient’s care.
BENEFITS :=
In this, patients receive treatment in a family oriented environment.
In such an environment, the patient gets work and a comfortable environment.
The patient gets the support of his family and friends during his illness.
In such an environment, the patient’s mental health remains good.
Instead of living in an uncomfortable environment like a hospital, the patient stays at home and receives treatment.
care provider:=
All hospitals are staffed with trained professionals.
->physicians,
->Specially trained nurses,
->Social worker,
->Family members,
->friends
So hospice care is not a patient. Treatment is given to patients in a home or hospital environment is called hospice care.
WRITE IN DETAIL ABOUT VARIOUS CANCER AND ITS MANAGEMENT.
1) Lung cancer:= Definition:=
Lung cancer can arise from any part of the body.
About 90 to 95 percent of cancers arise from epithelial cells.
And mostly it originates from the bronchi and bronchioles part of the lungs.
For this reason lung cancer is bronchogenic.
Cancer or bronchogenic (in bronchogenic cancer) is called carcinoma.
Cancer mainly originates from the pleura itself (it’s called mesotheliomas) but occasionally it originates from the tissues of the lungs.
If cancer occurs at any place in the body or if a tumor of cancer occurs, the main part of metastasis from one place to another is the lungs.
Etiological Factor:=
cigarette smoking 🚬, passive smoking Tobacco use,
HEREDITARY AND ENVIRONMENTAL FACTORS.
history of lungs 🫁 cancer, Air pollution, occupational carcinogens, Asbestos fiber,
Radon ⛽ gas, occupational carcinogens, Nutrition deficiency,
clinical manifestation (signs and symptoms):=
->cough,
->Dyspnea (difficulty in breathing),
-> wheezing,
->chest pain,
->Excessive sputum production,
-> Hemoptysis (Hemoptysis := blood in the cough),
->Dysphagia (difficulty in swallowing),
-> nausea,
->vomiting,
->Headache,
-> weight loss,
->Fatigue,
->Anorexia (anorexia := lack of appetite),
->weakness,
->Blurred vision,
-> seizure.
Diagnosis evaluation:=
History taking and physical examination, X Ray, Computed tomorrow (ct scan), MRI (magnetic resonance imaging),
PET (positron emissions tomography), Biopsy, Cytological examination, Pulmonary function test (PFT), Bronchoscopy
(Bronchoscopy.:= means visualizing the bronchi through a bronchoscope.).
Management:=
1) Radiation therapy,
2) Chemotherapy,
3) Bronchoscopy,
4) Phototherapy,
5) Airway stunting (airway stunting),
complication :=
- Superior vena cava syndrome,
2) Hypocalcemia
3) Brain Metastasis
4) Spinal cord compression,
5) Pulmonary 🫁 scarring (pulmonary scarring).
Nursing management:=
Nursing assessment:=
1) To check patient’s vital sign.
2) Checking the patient’s intake output.
3) To check the patient’s pain level.
4) Checking the eating pattern of the patient.
5) To check whether the patient has any kind of complication or not.
6) To check patient anxiety level and coping ability.
7) To check the blood investigation of the patient.
8) Conduct physical examination of the patient.
Nursing Diagnosis :=
1) Impaired breathing pattern related to compromised respiration.
Nursing interventions:=
Improving breathing patterns:=
-> Raise the patient’s head.
-> Teaching breathing exercise to the patient.
-> Patient and giving nebulization.
-> Ask the patient to expectorate by himself.
-> Giving oxygen to the patient.
-> Ask the patient to get enough sleep and how to keep his head slightly lower while sleeping.
-> Put patient in fowler position.
2) Impaired nutritional pattern less than body requirement related to nausea and vomiting.
Nursing interventions:=
Improving nutritional status:=
-> How to get the patient to take small amounts of food.
-> Ask the patient to take high calorie and high protein rich food.
-> Giving prescribed vitamin supplementation.
-> Tell to take little by little soft and liquid diet.
-> Administration of fluids through intravenous route to people who cannot feed on their own.
3) Pain related to abnormal cell growth.
Nursing interventions:=
controlling pain:=
-> To assess the patient’s pain level.
-> Administer prescribed Analgesic drugs to fashion.
-> Asking about the patient’s anxiety, depression level, level and whether he is getting enough 😴 sleep or not.
-> Telling the patient’s family member to take care of his family member in a proper manner.
4) Anxiety, fear, related to therapeutic regimen and prognosis.
Nursing interventions :=
Minimise anxiety:=
-> Checking the patient’s anxiety level.
-> Ask the patient to describe his feelings.
-> Telling the patient that his body pain is due to cancer so asking him for cpe up mechanism.
-> The patient is prescribed NSAIDs. (N.S.A.I.D.) S group or any other type of Analgesic to provide.
-> Ask the patient for proper cope up mechanism.
BRAIN TUMOR
INTRODUCTION / DEFINITION:=
In Brain 🧠 tumor, abnormal growth of cells takes place in the brain and forms a tumor.
This tumor can be malignant or benign.
In brain tumors, abnormal and uncontrolled cell division in the brain leads to cell growth and tumor formation.
This tumor is in the brain, in the lymphatic tissue (lymphatic tissue), in the blood, in the intracranial nerve, in the pituitary gland, in the pineal gland and it is in any other organ of the body and is transferred to the brain and affects the brain.
This tumor can be in the junction of gray matter and white matter of the brain.
classification / type:=
1) Primary brain tumor,
2) secondary brain tumor,
1) Primary Brain tumor:= Primary brain tumor is made from the cells and structures of the brain itself.
A) Intracerebral tumor: The most common primary brain tumor is gliomas which arise from glial cells. There are tumors in many types of cells like :=
Astrocytoma (in astrocytes), Brain stem glioma (Brain stem glioma),
Ependymoma (in ependymoma),
oligodendroglioma
Medulloblastoma (in Medulloblasto).
B) tumor arising from supporting structures:=
Meningioma
schwannoma,
germ cell tumor of the brain,
pineal region tumor, Angioma.
2) Secondary Brain 🧠 tumor:= This secondary brain tumor develops from a structure outside the brain and it is transferred to the brain.
The most common organ like 🧠 brain, lung, Brest, Kidney.
Tumors from all these parts of the body metastasize and transfer to the brain. And there the excessive growth of tumor takes place which results in cancer.
Etiology:=
being male,
Race,
age,
Family history,
Inherited,
occupational,
nutritional factors,
radiation,
HIV infection,
Cigarette smoking,
use of hair dyes,
Head trauma,
Dietary exposure to such factors as nitrates.
clinical manifestation:=
Headache,
Gait disturbance
memory loss
visual disturbance
personality disturbance,
confusion
seizure,
weakness,
paralysis.
Diagnostic evaluation :=
-> history taking and physical examination -> ct scan -> MRI Angiogram -> X Ray ->PET(Positron Emosin Tomography), ->SPECT(Single Photo Emission Computed Tomography),
Management:=
1) Corticosteroids treatment, 2) Palliative treatment, 3) Radiation therapy.
4) Surgery:= (Craniotomy:= Craniotomy)
5) Chemotherapy (Chemotherapy),
Antineoplastic agent:=
A) alkylating agent,
B) Nitrosoureas,
C) Antimetabolites,
D) Antitumor antibiotics,
E) Hormonal agents.
COMPLICATION := Learning difficulty (learning difficulty:= memory difficulty), walking and talking difficulty, Visual difficulty Difficulty in seeing), Hydrocephalus (Hydrocephalus := Collection of cerebrospinal fluid in the brain), Bleeding in Brain (Bleeding in Brain := Bleeding from the head) etc.
Nursing management := Nursing assessment :=
1) Checking the consciousness level of the patient.
2) Perform a neurological examination of the patient.
3) Checking the patient’s pain level.
4) Checking the nutritional status of the patient.
5) Checking the skin integrity of the patient.
6) To observe whether the patient has a condition such as fatigue or weakness or seizures.
7) Checking the patient’s activity level.
8) To take patient’s vital signs.
Nursing diagnosis:=
1) pain related to mass in Brain, nerve compression.
Nursing interventions:= Relieving pain.
Administering the prescribed Analgesic medicine to the patient.
Providing Mind Diversional Therapy to the patient.
If the patient has photophobia, keep him in a completely dark room and wear dark glasses.
Ask the patient to rest.
Provide the patient with prescribed Analgesic.
2) Risk of injury related to gait disturbance.
Nursing interventions: Prevention of injury:
If the patient’s intracranial pressure has increased, then report to the physician.
Maintaining the patient’s position properly.
Maintaining the patient’s intake output.
To see whether the patient responds to pharmacological treatment or not.
Ambulation means making the patient move.
Providing side rails to the patient in the bed.
3) Anxiety related to disease conditions.
Nursing interventions:= Relieving Anxiety:=
Reassurance to the patient.
Ask Shunt to describe his feelings.
Tell the patient to clear all his doubts.
Ask the patient to do a little exercise.
Spend some time with the patient.
Tell the patient to improve his coping abilities.
Tell the patient to be involved in mind diversional therapy.
4) Activity intolerance related* to weakness or fatigue.
Nursing interventions := Promoting activity level:=
Maintain patient’s personal hygiene.
Ask the patient to perform daily routine activities.
Keep the necessary things near him.
Ask the patient to do a little exercise.
5) Uttered nutrition status less than body requirement related to nausea and vomiting.
Nursing interventions:=
improve nutrition status of client:=
Maintain patient’s oral hygiene.
Do not keep any bad smelling things near the patient while he is eating.
Giving the patient what he wants to eat.
Keeping in mind what the patient feels like eating and what he doesn’t feel like eating.
Positioning the patient properly.
Give the patient proper fluids to drink.
Checking the patient’s weight daily.
6) Ineffective family coping related to clients disease and prognosis.
Nursing interventions:=
Reassure the family coping.
Giving reinsurance to a family member.
Involving family members in coping mechanisms.
Provide psychological support to family and patient.
Communicating with the patient and his family members.
To clear all the doubts of the patient and his family members.
If the patient is unconscious, provide care to him.
- ORAL CANCER
INTRODUCTION
Oral cancer is a cancer of the mouth and throat.
In this cancer, the cells of the mouth grow in an uncontrolled and abnormal manner and form a tumor.
Oral cancer can develop from any part of the mouth.
Like:= Oropharynx,
Lips,
Tongue,
Hard and soft palates,
Salivary gland
lining of cheeks (lining of cheeks),
floor of mouth (floor of mouth),
gums(games:= gums),
teeth (teeth:= teeth).
Cancer can develop in any of these parts of the oral or oral cavity.
Etiology
Tobacco,
alcohol,
Exposure to ultraviolet rays,
chronic irritation at the lining of mouth,
Sun Exposure,
A personal history of head and neck cancer.
Diet low in fruits and vegetables.
mouthwash with high alcohol 🍸 content.
Human papilloma virus.
Immune system suppression.
Age above 35 years.
Gender/Sex:=both men and women equally occur.
clinical manifestation:=
A sore in the mouth which does not heal.
pain
A lump on the mouth, lip or in the throat. (A lump develops in the lips, throat and cheeks.).
A persistence white and red patch on the gums, tongue,
tonsil, or lining of the mouth. (White and red crusts occur in the mouth, tongue, gums, tonsils, and lining of the mouth.)
Bleeding from the mouth
Bad breath (Halitosis := bad breath coming from the mouth),
Hoarseness or other change in the voice.
Difficulty chewing and moving the jaw or tongue.
Painful swallowing Difficulty in swallowing or pain while swallowing.
weight loss,
Swelling of jaw
Pain in one ear without hearing loss
A lump or mass in the neck.
voice change
Diagnostic evaluation
History tacking and physical examination,
biopsy,
Cytological test,
x Ray,
ct scan,
MRI Scan,
toludine blue test (toludine blue test),
oral exfoliative cytology (oral exfoliative cytology).
Management
radiation therapy,
chemotherapy,
Surgery
a) primary tumor*resection (primary tumor resection),
B) Mandibulectomy (mandibulectomy),
C)Maxillectomy (Maxillectomy),
D) Moh’s micrograph surgery.(Mohs Micrography Surgery),
E) laryngectomy (laryngectomy),
F) Radical neck dissection (radical neck dissection),
G) plastic surgery (plastic surgery).
Nursing management:=
Assessing the patient’s pain level.
Provide patient with favular and semifavular position.
Oral suctioning of the patient.
Checking the patient’s body temperature.
To check patient’s vital signs.
Check the patient’s weight.
To prepare the patient for chemotherapy and radiation therapy.
Ask the patient to maintain oral.
Provide high calorie diet to the patient.
Tell the patient to avoid tobacco, smoking and alcohol.
Tell the patient to take a healthy diet every day.
Explaining the side effects of chemotherapy and radiation therapy to the patient.
Explain to the patient the side effects of using tobacco or cigarettes.
Provide emotional support to the patient.
To provide psychological support to the patient and his family members.
Providing patient and work and comfortable environment.
Esophagus cancer:=
This causes cancer of the esophagus. >And it involves the lining of the esophagus and its muscles and its lymph nodes, and cancer develops.
Etiology:=
1) Gender more in men 👨🦼
2)Race Esophageal cancer is more common in African and American races.
3)Age:= Occurs more in persons above 50 years of age.
4) use of alcohol and tobacco,
5) GERD ( Gastero esophageal reflux disease := Gastero esophageal reflux disease),
6)hot,spicy dietary intake (due to excessive spicy fried food),
7) Exposure to nitrosomine in food/Environments.
clinical manifestation
Dysphagia (difficulty in swallowing),
feeling of lump in throat.
painfully and difficulty in swallowing
Regurgitation of undigested food
loss of appetite,
loss of weight
Diagnostic evaluation:=
History tacking and physical examination,
X Ray,
Ct scan,
MRI,
PET (Positron Emosin Tomography),
Management:=
Radiation therapy,
chemotherapy,
De bulking surgery,
chemotherapy and radiation therapy combination
Nursing management:=
To check patient’s vital sign.
Providing emotional support to the patient.
Maintain hygienic condition.
Giving the patient balanced calorie and high protein rich food.
To meet all the needs of the patient.
While giving chemo therapy and radiation therapy to the patient, to see if there is any kind of side effect.
If the patient gets any kind of adverse effect, see about it.
To maintain the nutritional status of the patient.
Maintaining the patient’s fluid level.
To clear all the doubts of the patient and his family members.
Providing psychological support to the patient and his family members.
- Cancer of stomach Introduction:=
Stomach cancer is also called gastric cancer.
It develops in any part of the stomach and results in abnormal and uncontrollable growth of the shell and formation of tumor and mass-like structures. This tumor is a
Can be both benign (non cancerous) and malignant (cancerous).
About 85% of gastric cancers are adenocarcinomas.
And it occurs mainly on the lining of the stomach (mucosa).
40% of stomach cancers occur in the lower part of the stomach (pylorus).
40%: = as many cases as in the middle part of the stomach (body). happens
15%:= As many cases occur in the upper part of the stomach (cardia).
And this stomach cancer is a metastasis that means it has transferred and spread to liver, lungs, bone, and in the body.
Spreads in the brain, etc.
And mainly it spreads in the periosteum i.e. abdominal cavity.
Etiology
Age:= seen after 40 years of age.
Gender:= Males are more affected than females.
Region:= More common in Japanese people.
Diet := It can also be caused due to less intake of fruits and vegetables.
Smocking,
alcohol,
Hereditary factors,
cronic infection in the stomach (due to chronic infection in the stomach),
Stomach surgery,
H.pylorus infection (Helico bacterium pylori),
High consumption of red meat 🍖, (due to eating too much meat),
pernicious anemia (due to vitamin B 12 deficiency),
Gastric ulcer,
Hereditary,
Obesity,
Hormonal factors,
Etc.
clinical manifestation :=
There is pain in the part of the stomach.
Difficulty in swallowing.
Nausea and vomiting occur.
Weight is reduced.
Even after eating a little, the stomach feels very bloated.
There is blood in vomiting (hemetemesis).
There is blood in the stool. (hematochezia),
Gastrointestinal bleeding,
Conditions like indigestion and gas (heart burn) occur.
Anorexia (loss of appetite)
Diarrhea (loss of watery stool),
Constipation (difficulty in passing stool),
fatigue (feels tired)😩.
Iron deficiency anemia.
Diagnosis evaluation =
History tacking and physical examination,
biopsy,
Endoscopy,
USG,
X Ray,
ct scan,
MRI,
Management:=
chemotherapy,
radiation therapy,
gastrectomy,
Total gastrectomy,
sub total gastrectomy
esophageal gastrectomy
Billiroth :- I (gasteroduodenostomy),
Billroth:=II (gasterojejunostomy),
Nursing management Emergency management:=
To check the patient’s vital sign every 15 minutes.
Checking patient’s blood pressure every 15 minutes.
Set up two intra venous lines to the patient and prepare blood transfusion.
Giving oxygen to the patient.
To check patient’s bowel sound.
To see if the patient has vomiting and diarrhea.
Catheterization of patient to check urine intake output.
Checking the skin color of the patient.
Maintain intake output chart of patient.
Giving the patient fowler position to avoid aspirating mucus.
Insertion of Nasogastric tube (N.g tube) in the patient.
Start feeding the patient with a clear liquid diet.
-Preoperative and Postoperative nursing management :=
Preoperative nursing management:=
Providing psychological support to the patient.
Explaining the procedure to the patient and his family members.
Setting up an intravenous line to the patient.
Catheterizing the patient.
Maintain intake output chart of patient.
Setting up blood transfusion to the patient.
To carry out all laboratory investigations of the patient.
Administering oxygen to the patient.
To do proper shaving on the part which is the operation part of the patient.
Cleaning or painting the patient with savlon and spirit on the operation side.
Prepare the patient mentally and physically for surgery.
To check patient’s vital signs.
Providing psychological support to the patient and his family members.
Post operative nursing management:=
Close observation of the patient after the operation.
Patient Nadar to check vital sign at 15 minutes.
Provide intravenous fluid to the patient by parenteral route.
To check the patient’s bowel sound.
Giving proper antibiotics to the patient.
Providing psychological support to patients.
Advising the patient’s family member to ensure that the patient does not do very hard work.
Ask the patient to rest.
Providing work and comfortable environment to patients.
Keeping the patient’s nutritional and food status balanced.
Ask the patient to do small amounts of activity.
liver cancer Introduction:=
- Liver cancer originates in the liver. -And it is called hepatocellular carcinoma. – This cancer is produced in the cells of the liver. – It causes abnormal and uncontrollable growth of cells and formation of tumors. – And this tumor can be malignant (cancer yes) or benign (non-cancerous). – This cancer is also called hepatoma.
Etiology
certain type of liver disease:=cirrhosis,
hepatitis B virus,
hepatitis c virus,
diabetes,
obesity,
Aflatoxin:=
-Birth control pills,
-Tobacco use,
-vinyl chloride,
-Anabolic steroids,
-Arsenic,
-Cytological drugs,
- use of steroids.
=clinical manifestation:=
- Abdomen is distended on the right side.
-And this pen is transferred to the back side (back side) and shoulder (shoulder).
- Abdomen right side becomes swollen.
- Lumps in abdomen.
- The liver is enlarged.
- Weight is reduced.
- Malaise occurs.
- Do not feel hungry and the abdomen feels very full as soon as you eat a little.
- Feels very tired.
- Eyes, skin and whole body become yellowish.
-nausea,
-vomiting,
-fever,
-fluid retention (acities),
-liver damage,
-Metabolic disturbance,
-splenomegaly,
-Hepatic encephalopathies,
-Jaundice,
-esophageal varies (the esophagus is enlarged).
- Abdominal distension.
Diagnostic evaluation
-History taking and physical examination,
-Hepatological investigation (hepatological investigation),
->( AFT := Alpha feto protein),
->blood test,
-> liver function test,
->Albumin Alkaline Phosphate,
->Prothrombin time,
-X Ray,
-ultrasonography,
-ct scanning,
-MRI,
-Laparoscopy,
- Biopsy,
-hepatitis b test,
-hepatitis c test
medical management
chemotherapy,
radiation therapy,
Ablation therapy,
Immunotherapy,
Biotherapy,
surgery management
Surgical resection,
liver transplantation (liver transplantation).
complication:=
Malnutrition,
Biliary obstruction,
sepsis,
liver abscess,
Metastasis.
Nursing management: = >Nursing assessment:=
Assessing the patient’s pen level.
Assessing the patient’s coping ability.
To check patient’s vital signs.
Checking the patient’s skin turgor and looking for heel-like conditions.
Dietary conditioning of the patient.
Assess the patient’s activity level and sleep pattern.
Monitor the patient for any side effects of chemotherapy, radiotherapy, and immunotherapy.
Nursing diagnosis
1) Pain related to liver enlargement. >Nursing interventions:= >Controlling pain:=
Providing analgesic drugs to the patient.
Providing Mind Divergent Therapy to the patient* .
Observe the patient for any signs of drug toxicity.
Provide guided imagery to the patient.
Ask the patient to exercise moderately.
Providing comfort measures to the patient.
2) Altered nutrition less than body requirement related to disease and side effects of chemotherapy. >Using interventions:= >Improving nutritional status:=
Tell the patient to take small amounts of food.
Tell the patient to take supplementary drugs.
Give food that the patient likes to eat.
Know the patient’s likes and dislikes.
Giving the patient a high calorie meal.
Do not keep bad smelling things near the patient while he is eating.
3) Fluid level excess related to oedema. >Nursing interventions:= >Relieving excess*fluid volume:=
To check patient’s vital sign.
Checking the patient’s intake output.
Do not give sodium rich food to the patient.
Administer fluids to the patient as prescribed.
Administer diuretic medicine to the patient.
Maintain the patient’s potassium level.
Providing patients with albumin and protein supplementation.
Checking the patient’s abdominal girth daily.
Check the patient’s weight. If there is weight gain, it indicates fluid retention.
Conduct laboratory tests of the patient.
Preparing the patient and his family members for surgery.
To clear all doubts of patient and family members.
Providing psychological support to the patient and his family members.
4) Discomfort related to disease condition.
5) Altered sleeping* pattern related to pain.
6) Activity intolerance related to weakness.
7) Risk for infection* related to* bone marrow depression secondary to chemotherapy
LEUKEMIA CANCER
The word Leukemia is derived from the Greek word leukos.
Leukemia means
” leukos := white
“Aimia :=blood”
Leukemia is a cancerous disorder of the bone marrow and blood system.
Abnormal and uncontrolled growth of white blood cells of Leukemia.
Due to the abnormal and uncontrolled growth of white blood cells, there is not enough space in the bone marrow for the formation of red blood cells.
lack of normal blood cell in bone marrow results in:= lack of normal white blood cell:= = (Increase the risk of infection:= Chances of infection in the body increase.) = lack of red blood cell (result in fatigue, weakness, and Anemia := Fatigue, weakness and lack of blood element in the body due to lack of blood). =lack of normal platelet count production =(Increase the risk of bleeding:= blood continues to flow, blood does not clot due to the decrease of platelets).
classification
A) Acute leukemia,
B) Chronic leukemia.
A)Acute Leukemia:= – In this the formation of blood cells takes place very quickly and the immediate treatment of this acute leukemia is very necessary because in this the blood cells grow rapidly.Its formation takes place and it results in cancer.
B)Chronic Leukemia:- In this Leukemia there is excessive formation of abnormal white blood cells. -And this takes months and years to happen. – But this cell grows faster than normal cells and due to this many white blood cells are formed.
Other classification:=
1) ALL (Acute lymphocytic leukemia),
2) CLL (Chronic lymphocytic leukemia),
3) AML (Acutemyelogenous leukemia),
4) CML (Chronic myelogenous leukemia),
5) HCL (hairy cell leukemia).
) Acute lymphocytic leukemia:= It is very common in young children and it is more common in adults especially people after 65 years.
2)Chronic lymphocytic leukemia:= This is more common in people after 55 years and sometimes in children.
3)Acute myelogenous leukemia:= This leukemia is more common in adults than in children. And mainly it is more common in men than women.
4) Chronic Myelogenous Leukemia := It is mainly seen in adults.
5) Hairy cell leukemia: This leukemia is curative and can be easily treated.
Etiology
Due to excessive exposure to radiation.
Due to working with certain types of chemicals.
atomic 💣bomb explosions.
X Ray,
smocking,
chemotherapy,
inherited disorder,
Human t cell leukemia viral type,
family history.
clinical manifestation
Difficulty breathing,
weight loss,
Fever,
Frequent infections,
Pain in bones and joints,
Aching pain in bones and joints,
feel tired,
weakness,
loss of appetite,
Swollen lymph nodes,
swelling of the spleen,
night sweats,
excessive bleeding,
Patches of purple color in the skin,
headache,
confusion,
pale,
nausea,
seizure,
vomiting,
Diagnostic evaluation
history taking and physical examination,
blood test,
biopsy,
other findings,
->lumbar puncture,
-> Radiography,
->ct scan,
->MRI.
Management
chemotherapy,
radiation therapy,
Stem cell therapy,
biotherapy,
bone marrow transplantation.
Nursing management
Nursing diagnosis
1) High risk of infection related to Neutropenia. Nursing interventions
Wash hands properly before meeting the patient.
Refusing visitors who have communicable diseases to visit the patient.
Keep the patient in isolation.
Bathe the patient properly.
Tell the patient to maintain his oral hygiene.
Do not take any type of suppository, enema, or rectal temperature.
Providing prescribed analgesic and antibiotic drugs to the patient.
Check for any type of infection where the Indra Venus line is inserted.
Observe the patient for any type of fungal infection or viral infection
2) High risk of bleeding related to bone marrow suppression. Nursing interventions Prevent bleeding
Do not administer aspirin or any products containing aspirin to the patient.
Do not give intramuscular injection to the patient.
Give the patient a small toothbrush to brush.
Do not insert the patient rectal suppository.
Not inserting a urinary catheter.
Do not traumatize the oral mucosa while doing suction.
Changing the patient’s position frequently to prevent bed sores.
Do not overinflate the BP cuff.
3) Fluid volume definitely related to less intake. Nursing interventions maintain electrolyte and fluid balance:=
Maintaining intake output chart of patient daily.
Check weight daily.
Observe the patient for any signs of dehydration or fluid overload.
Conduct lab investigation.
Provide intravenous fluid to the patient.
4) Discomfort related to pain. Relief from pain:=
Give a cold sponge to the patient.
Changing patient’s bed linen and daily.
Provide a gentle massage to the patient.
Acetaminophen is used to reduce fever.
Provide anal sex to the patient.
Make proper environment for tack proper sleep.
5) Activity intolerance related to weakness. Nursing interventions:=
improve efficiency level of client.
Tell the patient to maintain a balance between work and rest.
Tell the patient to do proper exercise.
Ask the patient to sit on a comfortable chair or bed.
Tell the patient to keep doing some activity.
6) Altered nutrition less than body requirement related to Anorexia, vomiting secondary to side effect of chemotherapy. = Maintain adequate nutrition.
Providing analgesic and anti-anesthetic medicine to the patient.
Maintaining the patient’s oral care.
Feed the patient in small and frequent amounts.
Check the patient’s weight daily.
Providing fluid to the patient through an intravenous line.
Lymphoma (Hodking’s disease)
introduction:=
This leads to abnormal and uncontrollable growth of cells and formation of tumors. These tumors are cancerous and cause cancer-like disease in the lymphatic system.
It is mainly in the lymphatic system.
Also, spleen and lymph nodes are also involved.
Etiology
Age := peak at 20 years above or 50 years above.
Gender := This is mainly more common in males.
carcinogenesis,
cytotoxic drugs,
other body parts cancer,
other disease conditions.
clinical manifestation
Enlargement of lymph node,
Nodes are firm and painless,
pruritus,
severe pain
fever without chills,
Weight loss,
night sweats,
mild anemia,
Dysapnia (shortness of breath),
expectoration,
Jaundice,
Abdominal pain,
Bone pain
Diagnostic evaluation:=
lymph node biopsy,
presents of” B”symptoms:=like
Fever without chills,
Excessive weight loss,
Night sweat
X Ray,
ct scan,
PET test (prositron emission tomography),
laboratory test,
Bone Marrow Biopsy,
Bone scane.
Management:=
Combination ABVD:=
A:=achiamycin,
B:=Bliomycine,
v:=Vinblastine, D:=Dacrabazine.
Combination of abvd is standard treatment.
General nursing management:=
Explaining disease conditions.
Looking at its advantages and limitations.
To check patient’s vital signs.
To provide the prescribed treatment to the patient.
Provide an environment where the patient can perform small amounts of activity on his own.
To maintain the hyginic condition of the patient.
Care should be taken not to infect the patient.
Providing a well balanced diet to the patient.
Report to physician if there is any type of oncological emergency.
Providing psychological support to the patient and his family members.
To clear all doubts of the patent and its family members.