ENGLISH Unit-12-neurological Disorder(deepali)(part-3)
- Explain/ Define the Increase intracranial pressure.
Intra cranial pressure is the pressure felt inside the skull, brain tissues and CSF is called intra cranial pressure.
Increased intracranial pressure means when the intracranial pressure is elevated above the normal intracranial pressure in the cranial cvt, it is called increased intracranial pressure.
Normal intracranial pressure is 5 – 15 mmhg.
In increase intracranial pressure pressure in the cranial cavity is > 15 mmhg.
{ if pressure into the cranial cavity is > 15 mmhg its known as an increase intracranial pressure. }
Temporary intracranial pressure increases due to cuffing, sneezing, straining, bending forward, vomiting.
Explain the Etiology/cause of the increase intracranial pressure.
Due to infection,
Due to tumor formation,
Due to stroke,
Due to aneurysm,
Due to epilepsy,
due to seizure,
Due to hydrocephalus,
Due to hypertensive brain injury.
Due to hypoxemia.
Due to meningitis.
Due to head injury.
Due to brain abscess.
Due to encephalitis.
Due to intracranial hemorrhage.
Explain the clinical manifestation/ sign and symptoms of the patient with the increase intracranial pressure.
Changes in the level of consciousness.
Decrease in patient’s consciousness level.
Pupillary reflex absence of the patient.
Patient has loss of bowel and bladder control.
headache.
Nausea.
Vomiting.
Patient’s blood pressure increases.
Alteration of patient’s respiratory pattern.
Elevation of patient’s body temperature.
Decreasing mental ability of the patient.
Confusion.
Double vision.
Caesar is coming.
Loss of consciousness.
Coma.
Abnormal flexion and extension of the patient.
Bluured vision coming.
Diplopia.
Abnormal eye movement.
Explain the Diagnostic evaluation of the increased intracranial pressure.
History taking and physical examination.
Lumbar puncture.
CT-scan.
MRI scan.
PET scan.
Transcranial dropper.
Cerebral angiography.
Neurological assessment.
Vital signs assessment.
Pupillary Changes Assessment.
Explain the medical management of the patient with the increased intracranial pressure.
Assess the patient properly.
To properly assess the patient’s vital signs.
Assess the patient’s neurological status.
The bed of the patient should be elevated at a 30° angle.
Provide oxygen properly if patient has respiratory difficulty.
Provide ventilatory support to the patient by mechanical ventilation.
Provide intravenous fluid by measuring properly so that the condition of fluid overload does not arise in the patient’s body.
Administer loop and osmotic diuretic medicine to the patient.
Ex:=inj. lasix (frusemide), Inj.mannitol.
Provide corticosteroid medicine to the patient.
Ex:= Dexamethasone.
Provide anticonvulsant medicine to the patient.
Ex:= phenytoin.
Provide antacid medicine to the patient.
Ex:= Ranitidine, Pantoprazole.
sedation and paralysis drug to the patient like,
Morphone, Propofol, Vecuronium.
Provide isotopic drug and intravenous fluid to maintain the patient’s blood pressure.
Providing a nasogastric fitting to the patient.
To provide proper total parenteral nutrition to the patient.
If the patient is in pain, provide medication to properly manage the pain.
Proper close monitoring of the patient.
Explain the surgical management of patients with the increased intracranial pressure.
1) Ventriculostomy:=
In ventriculostomy, a special type of catheter is inserted into the lateral ventricles to drain the cerebrospinal fluid.
2) Craniotomy :=
If hematoma and tumor are present, craniotomy is performed.
Explain the Nursing management of patients with the increase intracranial pressure.
Perform a neurological assessment of the patient.
Properly assess the patient by Glass Go Co Scale (GCS).
To continuously monitor patient’s vital signs.
Properly assess patient’s blood pressure, respiratory status, temperature heart rate in vital signs.
Keep the patient’s head elevated at a proper 30° angle.
Advise the patient to avoid activities that increase intracranial pressure.
Provide proper oxygen and ventilation to the patient.
Properly monitor fluid and electrolyte levels of the patient.
If the patient has a condition of seizures, provide proper anti-epileptic medicine.
Provide proper position and comfort measures to the patient.
To maintain normal body temperature of the patient.
Keeping the patient’s neck in a neutral position.
To provide quite environment to the patient.
Do not restrain the patient as it plays an important role in increasing the intra cranial pressure.
Keeping the patient’s airway properly patent.
Provide chest physiotherapy and postural drainage to remove the secretion.
Properly maintain the fluid and electrolyte balance of the patient’s body.
Provide proper antibiotic medication to prevent infection to the patient.
Maintain streak aseptic technique while performing nursing activities to prevent patient infection.
Advising Ticent to follow up properly.
Advising the patient to take medication properly.
- Explain/Define the intracranial surgery. Define intracranial surgery.
Intracranial surgery is a surgical procedure that is performed in the cranial cavity.
In this type of surgery, any type of surgical procedure is performed in the brain.
Intracranial surgery is performed for a variety of purposes.
Intracranial surgery is performed to remove tumors, vascular abnormalities, structural problems, etc.
Burr Hole surgery:=
Burr hole surgery is a type of neurological procedure in which a small hole is performed in the skull, primarily with a specialized drill called a burr.
This surgical procedure is mainly used to access the brain and to treat different types of neurological conditions.
Burr hole surgery is also mainly done to remove blood and fluid in the brain.
Craniotomy:=
A craniotomy is a surgical procedure in which a small section of the bone of the skull is surgically removed, mainly to gain access to the intracranial compartment. But in this procedure the bone flap which is removed is mainly replaced in its position after the operation.
craniectomy:=
In a craniectomy, the bone flap is removed but not replaced.
Explain the indication of the intracranial surgery.
Being a brain tumor.
Due to vascular abnormalities.
Due to cerebral aneurysm.
Due to traumatic brain injury.
Being a condition of epilepsy.
Due to intracranial hemorrhage.
Due to hydrocephalus.
Due to cranial nerve disorders.
Due to meningiomas.
Due to functional neurosurgery.
Due to intracranial infection.
Due to skull fracture.
Due to formation in the hematoma.
Explain the pre operative teaching to the patient and family.
Assess the patient’s blood test properly.
Proper radiological examination of the patient.
Explain the complete procedure to Poosnut including anesthesia and the estimated length of the procedure followed by recovery time.
To provide complete information to the patient about post-operative procedures like dressing, catheter, ET tube, intravenous fluid, and his pain management.
Taking proper consent before performing surgery.
Properly prepare the operative area.
To properly monitor the patient’s vital signs.
Explain the post operative management of the patient with the intracranial surgery.
Assess the patient’s neurological status every 30 minutes for the first 24-48 hours.
Assess patient’s vital signs frequently.
Keep the patient’s bed elevated at an angle of 30 to 45 degrees.
Keeping the patient’s neck in a neutral position.
Advise the patient to prevent head movement.
Keep peanuts away from painful stimuli.
Taking measures to prevent pesnut from constipation.
Do not restrain the patient.
If the patient is in pain, provide analgesic medicine.
Checking patient drainage and following streak sterile technique.
Proper suctioning of the patient.
Monitor patient’s fluid and electrolyte balance.
Monitoring the nutritional status of the patient.
If the patient is conscious, provide oral fluids.
Advise the patient to perform range of motion exercises.
If the patient has a condition of seizures, keep the side rails up.
Advise the patient to maintain proper personal hygiene.
Providing proper rehabilitation therapy to the patient, Like:= Speech therapy, Physical therapy etc.
To provide proper psychological support to the patient and his family members.
3). Explain/Define headache. (Define header.)
A headache is a pain in the head. Which is mainly pain above the eyes and ears, back of the head (occipital), back of the upper neck.
Headache is also called Cephalalgia.
The word Cephalalgia comes from Greek.
“Kephale meaning “HEAD”,
Algos meaning “PAIN”
Cephalalgia means headache.
Headache means discomfort in the head, neck and scalp is called a headache.
Headache is the most common complaint among people and the severity, intensity and duration of headache also differ from person to person.
Explain the etiology/cause of the headache. (State the reason for the headache)
A tension headache
muscle tension,
Due to stress.
Migraine
genetics,
neurological factor,
Due to triggers (changes in food,
Due to lack of sleep, environmental
Cluster headache
Due to hypothalamus activation, vasodilation.
Due to intracranial infection,
Due to head injury,
Due to bacterial and viral meningitis,
Due to acute systemic infection,
Due to severe hypertension,
Due to intracranial tumor,
Due to acute and chronic diseases of eye, ear, nose and fruit.
Headache occurs due to different reasons like fever, anxiety, working for long hours, lack of sleep etc.
- Explain the Classification of the Headache.
The header is mainly divided into three categories.
1) Primary Headache,
2) Secondary Headache,
3) Cranial neuralgia, facial pain and other headaches
1) Primary Headache,
Primary headache involves 1) migraine, 2) tension headache and 3) cluster headache.
2) Secondary Headache,
A secondary headache is mainly caused by any structural problem in the head and neck.
3) Cranial neuralgia, facial pain and other headaches
Cranial neuralgia means if a headache occurs due to inflammation of the nerves in the head and neck or a problem in its structure, it is called cranial neuralgia.
Headache is seen due to different reasons in this type.
Thus, there are mainly three classifications of headache.
Primary Headache
A) Explain/Define Migraine Headache.
20% of all headaches are migraines.
Migraine is mainly due to constriction of the blood vessels in the head and neck, due to which the blood does not flow properly in the head, the condition of migraine is seen.
Migraine headaches occur on one side of the head or on both sides of the head.
Migraine type of headache is more common in females than males.
Migraines are mainly caused by anatomical and nervous system dysfunction.
Explain the Etiology/cause of the migraine headache.
Due to genetic factors,
Due to neurotransmitter imbalance,
Due to vascular changes,
Due to hormonal fluctuation,
Due to environmental stimuli,
Having a family history of migraines.
Prolong due to muscle tension and stress.
Due to the use of alcohol,
Due to smoking,
Due to consumption of tobacco,
Due to lack of sleep,
for women := due to menstrual period and use of oral contraceptives.
Explain the Classification of the migraine.
1) Migraine with the aura (classic migraine)
In this classic migraine, headache and disturbances in visual disturbance, motor function and accessory function are seen. In this, the symptoms are mainly seen for a few minutes and even hours.
2) Migraine without aura (common migraine)
Moderate to severe pulsating headache pain is seen in this type of migraine.
This type of pain is mainly seen on one side of the head.
It has other symptoms like nosia, vomiting, photophobia (Sensitivity to light).
, Phonophonia
(Sensitivity to sound) is seen.
Explain the clinical manifestation/sign and symptoms of the patient with the .Migraine Headache. (State the symptoms and signs of a migraine headache patient.)
Having a headache.
Quality := Thrombing pulsating pain,
Location := Usually on one side of the head
But sometimes pain is seen on both sides.
Intensity:= Moderate to intense.
Along with headache, nausea, vomiting, dizziness and visual disturbances are also seen.
Photophobia (Sensitivity to light),
Phonophobia (Sensitivity to sound),
Osmophobia (smell sensitivity)
Sensitivity to light and noise.
Paraesthesia (abnormal sensation).
Diplopia and blurred vision.
Irritability.
Restlessness.
feeling tired
Changes in mood.
Irritability
Explain the management of the patient with the migraine headache. (State the management of a patient with migraine headache.)
If the patient is in pain, provide Analgesic medicine.
Like:= Acetaminophen,
Ibuprofen,
Aspirin.
2) If the patient has a condition of inflammation, provide medicine of triptans group.
Ex:=
sumatriptan,
Rizatriptan,
If the patient has the condition of vomiting, then provide antiemetic medicine to the patient.
Provide a properly quiet and dark room to the patient.
Advising the patient on proper lifestyle modification such as avoiding caffeine rich food.
Advise the patient to sleep regularly.
Properly maintain the patient’s hydration status.
If the patient has a condition of stress then giving advice to do proper meditation, yoga.
Advise the patient to do regular exercise.
If the patient has severe migraine, the patient should be treated with beta blockers, calcium channel blockers,
Provide anti-depressant medicine, anti-convulsive medicine.
If the patient has a condition of chronic migraine, provide botulinum toxin injection.
Advise the patient to avoid smoking.
Advise the patient to avoid tyramine rich food.
B) Explain / Define tension headache. (Define tension headache.)
A tension headache is the most common type of primary headache.
This type of headache is mainly caused by the contraction of the head and neck muscles.
Tension headache is also seen due to emotional crisis and intense worry.
This type of headache is mainly seen in people who have depression and anxiety.
Explain the etiology/cause of the tension headache. (Give reasons for tension headache.)
Due to contraction of muscles.
Due to stress and anxiety.
Due to environmental factors.
Due to sleep pattern disturbance.
eye strain.
Due to use of tobacco and alcohol.
Due to hormonal changes.
Due to excessive caffeine intake.
Excessive Smoking.
Due to nasal congestion.
Due to sinus infection.
Explain the clinical manifestation / sign and symptoms of the patient with the tension headache. (Mention the symptoms and signs of tension headache.)
Headache.
Muscle tenderness.
Sensitivity to light and sound.
Muscle tightening.
Feeling pain in head and neck.
Explain the diagnostic evaluation of the patient with the tension headache. (State the diagnostic evaluation of a tension headache patient.)
history taking and physical examination.
Neurological examination.
ct scan.
MRI.
Blood test.
Explain the management of the patient with the tension headache. (State the management of a patient with tension headache.)
Advise the patient to get adequate sleep.
Advise the patient to take a balance diet.
Advise the patient to do regular exercise.
Advise the patient to adopt stress relaxation techniques.
Advise the patient for muscle relaxation.
Provide non-steroidal anti-inflammatory drugs to relieve the patient’s pain.
Advise the patient on muscle relaxant techniques.
Provide proper psychological support to the patient.
C). Explain/Define cluster headache. (Define cluster hydc.)
A cluster headache is a one-sided headache that also has eye tearing and stuffiness.
A cluster headache is a chronic and repeated headache.
Cluster headaches last from minutes to hours.
But a cluster headache can last for 45 to 90 minutes.
Cluster headache is the most common type of painful headache.
Explain the etiology/cause of the cluster headache.
Hypothalamus involvement.
Due to vascular changes.
Due to neurotransmitter imbalance.
Due to genetic factor.
Due to taking certain medicines.
Due to interruption in normal sleep pattern.
Due to some hormone imbalance.
Due to alcohol and cigarette smoking.
Due to high altitude.
Due to the consumption of cocaine.
Explain the clinical manifestation / sign and symptoms of the patient with the cluster headache. (State the symptoms and signs of a patient with cluster headache.)
Severe pain.
Tearing, redness and drooping of the eyelids.
Nasal congestion.
Restlessness.
Severe sudden, burning, aching, and steady headaches.
Pain and cluster headaches are short term usually lasting 30 to 90 minutes.
Swelling around the eyes.
Rhinorrhea (runny nose)
Red and flushed face.
Explain the Diagnostic evaluation of the patient with the cluster headache.
history taking and physical examination.
Imaging studies.
CT scan.
like this. RI
Blood test.
Explain the management of the patient with the cluster headache. (Cluster Head State the management of a Wada patient.)
Provide oxygen in adequate amount to the patient.
Provide sumatriptan medication to the patient.
Provide the patient with verapamil, lithium, divalproex sodium, prednisone, and ergotamine tartrate medication to prevent cluster headaches.
To provide proper work and comfortable environment to the patient.
Providing proper psychological support to the patient.
Provide calm and comfortable environment to the patient.
Providing the patient with properly minded diversional therapy.
2). Explain/Define secondary headache. (Define Secondary Heading.)
Secondary headaches are mainly caused by any structural problem of the head and neck.
In general, secondary headache is seen mainly due to sinus infection, head injury, medication side effect, bleeding in the brain, tumor, meningitis and encephalitis.
Explain the etiology/cause of the secondary headache. (State the cause of secondary headache.)
Due to infection,
Due to trauma,
Due to vascular disorders,
Due to medication overuse,
Due to structural issues.
Due to metabolic disorder.
Due to inflammatory conditions.
Due to exposure.
Due to the occurrence of neurological disorders.
Due to endocrine disorder.
Explain the clinical manifestation / sign and symptoms of the patient with the secondary headache. (State the symptoms and signs of a patient with headache.)
Headache has different qualities like seviarity, location, type etc.
The patient presents with various neurological symptoms like dizziness, visual disturbance, weakness.
Frequency and duration of headache are different.
Fever.
Sinus congestion.
Joint pain.
A neurological disorder.
feeling tired
Weight loss.
Changes in appetite.
Nausea and vomiting.
Photophobia.
Stiff neck.
to come up with a fever.
Changes in vision.
to be startled
Altered mental status.
Facial pain.
Slip Disturbance.
Hormonal changes.
Explain the diagnostic evaluation of the patient with the secondary headache. (Secondary head State the diagnostic evaluation of a Wada patient.)
history taking and physical examination.
Blood test.
Imaging studies.
ct scan.
MRI.
Lumbar puncture.
Electroencephalogram.
Hormonal test.
Allergy testing.
Medication history review.
Eye Examination.
Explain the management of the patient with the secondary headache. (Secondary head State the management of a Wada patient.)
If the patient has an infection, provide antibiotic medicine.
Provide analgesic medicine to patient for management of pain.
Provide antiepileptic medication to the patient.
Provide anti-inflammation to reduce the patient’s inflammation.
Provide corticosteroid medication to reduce patient inflammation.
Advising the patient for lifestyle modification.
Provide physical therapy to patients.
Advise the patient to take regular follow up.
Provide proper medication to the patient.
To provide work and comfortable environment to the patient.
4). Explain/Define seizures. (Define Caesars.)
Seizures are a condition in which the electrical activity of the brain becomes uncontrolled.
Seizures are a condition in which uncontrolled electrical discharges occur in the brain and a condition arises in the brain called seizures.
If there is an uncontrolled electrical discharge in the brain, the normal function of the brain is impaired and due to this a particular situation arises, it is called seizures.
Explain/Define the epilepsy
If the patient has repeated episodes of seizures, the condition converts to epilepsy.
Epilepsy is a mental abnormality in which a person’s brain
In the neuron’s electrical impulses are very disturbed
Due to which abnormal electrical activity is seen in the neuron
Gets and causes condition epilepsy due to which
A jerking moment arises in the body.
Explain the etiology/cause of the seizures. (Give reasons for seizures.)
Due to genetic factors.
Due to head trauma.
Due to brain tumor.
stroke.
Due to alcohol withdrawal.
Due to brain infection.ex:= Meningitis.
Due to drug abuse and withdrawal.
due to hypoglycemia.
Due to hypoxia.
Due to dehydration.
Due to fever.
Due to high blood pressure.
Due to septicemia.
Due to diabetes mellitus.
Due to electric shock.
Due to birth injury.
Due to developmental disorder.
Due to traumatic brain injury.
Due to brain tumor.
Due to exposure to any poisonous substance, Ex:= lead, carbon monoxide.
Explain the Classification of the seizures.
Seizures are mainly classified into three types.
A) General seizures
B) Partial or focal onset seizures. (Partial and focal onset seizures.)
C) Psychogenic seizures
A) General seizures
There are six types of General Caesars.
1) Tonic – clonic seizures.
2) Absent Caesar.
3) Myoclonic seizures.
4) Tonic Caesar.
5) Atonic Caesar.
6) Clonic seizures.
B) Partial or focal onset seizures.
There are two types of partial and focal onset seizures.
1) Simple focal seizure.
2) Complex focal seizures.
3) Psychogenic seizures
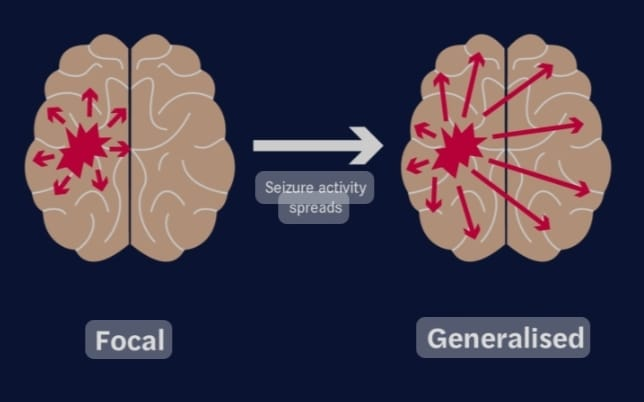
A) General seizures
There are six types of General Caesars.
In generalized seizures, both the right and left hemispheres of the brain are involved.
That is, uncontrolled electrical discharges occur in both hemispheres of the brain.
In this type of seizure, the patient becomes unconscious.
These seizures last from a few seconds to a few minutes.
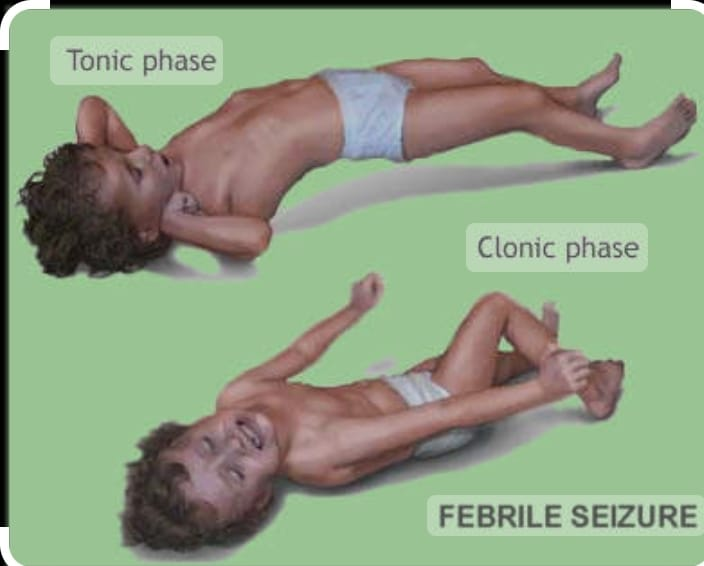
1) Tonic – clonic seizures.
Tonic clonic seizures are also called Grandmal seizures.
In this seizure, the patient’s consciousness is completely lost. And the patient also falls on the ground.
In the tonic stage, the patient’s muscles stiffen and muscle tone increases.
In the clonic phase, the patient’s muscle tone is lost.
2) Absent seizures.
Absence seizures are also called petitmal seizures.
This type of seizure is mainly seen in children.
These seizures are seen only for a few seconds.
In these seizures, the patient has episodes lasting only a few seconds and the patient does not even know that he has any kind of issue.
3) Myoclonic seizures.
Muscles are involved in myoclonic seizures
And an excessively jerking moment of the body occurs.
So in myoclonic seizures, the body jerks excessively.
4) Tonic Caesar.
In this seizure, the muscle tone increases suddenly and the body becomes stiff and the muscle tone increases greatly.
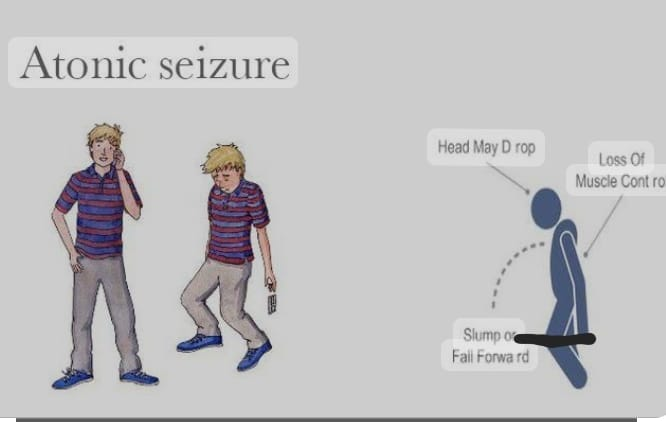
5) Atonic Caesar.
In this seizure, muscle tone is lost, so a drop attack is seen in this, i.e. the patient is
Standing up falls because in this seizure the patient’s muscle tone stops suddenly. In this seizure, the patient suddenly regains consciousness after a drop attack. In this seizure, the patient has a high risk of head injury.
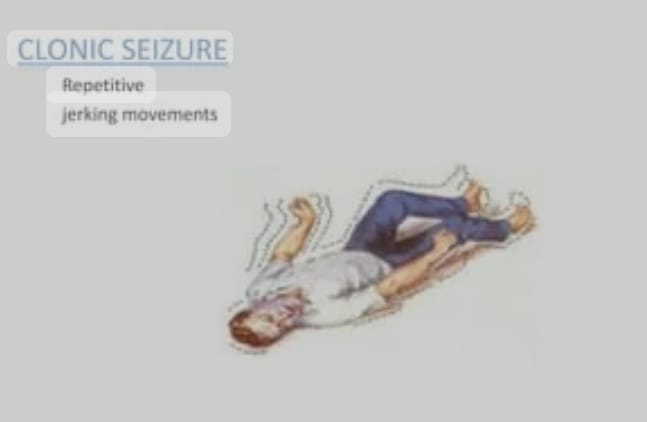
6) Clonic seizures.
In this seizure, the muscle mass of the patient is suddenly lost.
In this the person is seen unconscious and his muscle stone is also lost.
In this seizure, jerking moment of limb and jerking moment of extremities are seen.
B) Partial or focal onset seizures. (Partial and focal onset seizures.)
These seizures are also called partial focal focal seizures and partial seizures.
These seizures have unilateral hemisphere involvement.
Affection is therefore seen in whatever bodily activity is regulated by the hemisphere involved.
There are two types of partial and focal onset seizures.
1) Simple focal seizure.
In this type of seizure, the patient seems to be conscious, but there is an unusual feeling and sensation.
In this, the usual feeling is that the person is very happy, very angry, or the person is suddenly sad or the feelings of nozia are seen suddenly and without any reason.
This seizure involves the involvement of only one hemisphere, so the person experiences feelings of things that do not exist in reality.
2) Complex focal seizures.
In this seizure, the patient’s level of consciousness is altered or lost.
In this seizure, a person has a dream-like experience.
In this type of seizure, the person does not even properly remember what he did.
It is called a complex focal seizure.
C) Psychogenic seizures
These seizures are also called pseudo seizures.
These seizures are mainly seen due to psychiatric conditions.
In this seizure, the person feels like they are having a seizure but they are not actually having one.
Explain the clinical manifestation/ sign and symptoms of seizure.
Temporary confusion.
Uncontrollable jerking moment of arms and legs.
Loss of consciousness.
Loss of awareness.
Temporary confusion may occur.
Numbness in body parts.
Loss of memory.
Visual changes occur.
Dizziness.
Tingling sensation in the chest.
Explain the diagnostic evaluation of the patient with the seizures. (State the diagnostic evaluation of a patient with a seizure.)
History taking and physical examination.
Blood test.
Lumbar puncture.
Electroencephalogram.
Computerized tomography (CT scan).
Magnetic resonance imaging (MRI).
Positron emission tomography (PET test).
Single Photo Emission Computerized Tomography ( SPECT ).
Neuropsychological test.
Brain mapping.
Explain the medical management of the patient with the seizures.
Provide anticonvulsant medication if patient has condition of seizures.
1) Provide Phenytoin sodium medication to the patient.
If the patient has partial and generalized seizures, provide phenytoin medication.
This meditation is mainly used when there is a condition of cardiac dysrhythmia or some kind of nerve pain.
2) Provide carbamazepine meditation to the patient.
Carbamazepine is mainly used for partial and generalized seizures.
Carbamazepine decreases synaptic transmission in the central nervous system.
3) Administer valporic acid medication to the patient.
Valporic acid is used for partial and generalized seizures.
Valporic acid increases GABA.
4) Ethosuxamide :=
This meditation is mainly used for Absense Seizures.
5) Diazepam
Diazepam medication mainly works as a sedative which is mainly used in generalized seizures (Absence, Atonic, Myoclonic).
Explain the surgical management of patients with seizures. (State the surgical management of Caesarean section patient.)
Surgery is mainly done for patients who have any intracranial tumor, cyst, abscess and vascular abnormality.
1) Resective and palliative operations:=
If there is increased electrical activity within the brain and to treat its signs and symptoms, resection of the part of the brain causing increased electrical activity is performed.
2) Temporal Lobectomy:
If the seizure is primarily caused by the temporal lobes, the temporal lobe is removed.
3) Corpus Callosum.
If the seizure is due to coppice collosum, the affected party is removed.
4) Extra temporal resection
In this, if the seizure is mainly caused by the temporal lobe, resection of the temporal lobe is done.
5) Hemispherectomy :=
If the seizure is primarily due to either hemisphere, no part is removed.
Explain the nursing management of patients with seizures. (State nursing management of Caesarean section patient.)
Maintain a properly safe environment to prevent patient injury.
Keep the side rails up to prevent injury to the patient.
Do not put anything in the patient’s mouth.
If the patient is wearing anything around the neck, loosen it.
Failure to provide patient restraints may prevent injury.
Provide a small pillow under the patient’s head.
If the patient is vomiting, take proper care not to aspirate.
Keep suction readily available.
Keeping the patient’s airway patent allowing for proper breathing.
Advise the patient to take proper bed rest.
Advising the patient to take a specially ketogenic diet mainly low in carbohydrates and high in fiber, minerals and protein.
Providing intravenous fluids to the patient.
Provide oxygen therapy to the patient.
To provide proper work and comfortable environment to the patient.
Advising patients to take proper medication.


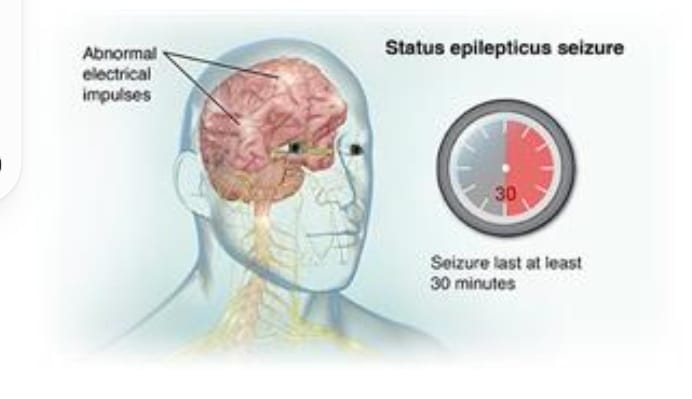
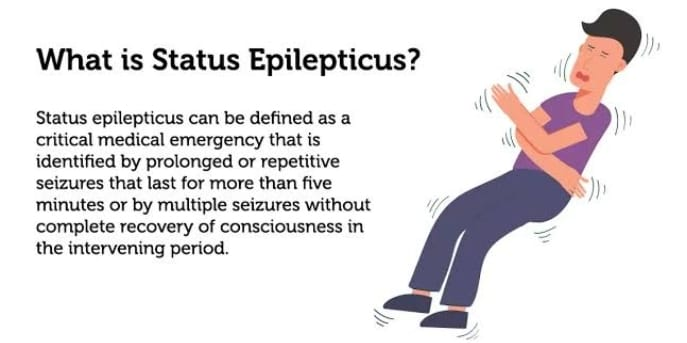
5). Explain/Define status epilepticus. (Define status epilepticus.)
Status epilepticus is a medical emergency. In which continuous, prolonged, recurrent seizures are seen.
If the patient has prolonged, continuous and repetitive seizures i.e. for more than 5 minutes without any gap between them, they are called status epilepticus.
Explain the etiology/cause of the patient with the status epilepticus. (State the cause of status epilepticus in Wada patient.)
Due to brain injury.
Due to infection.
Due to metabolic imbalance.
Due to drug withdrawal.
due to stroke.
Due to certain types of medication.
Due to sudden anticonvulsant drug withdrawal.
Due to any infection in the central nervous system.
encephalitis,
meningitis,
Due to the condition of hypoxia.
Due to any type of psychiatric condition.
Explain the clinical manifestation / sign and symptoms of the patient with the status epilepticus. (State the symptoms and signs of status epilepticus Wada patient.)
Prolonged and repetitive seizures.
Loss of consciousness.
Convulsions.
Muscle stiffness.
Changes in breeding pattern.
Altered mental status.
Confusion.
Behavior changes.
Loss of bowel and bladder control.
Explain the Diagnostic evaluation of the patient with the status epilepticus.
History taking and physical examination.
Electroencephalogram.
Blood test.
Imaging studies.
Computed tomography (CT scan).
Magnetic resonance imaging (MRI).
Lumbar puncture.
Complete Blood Count (CBC Test).
Serum electrolyte test.
Assess calcium level.
Assess the magnesium level.
Assess the creatinine level.
Assess the blood urea nitrogen (BUN) level.
Assess the liver function test (LFT).
Assess the Arterial Blood Gas Analysis (ABG Level).
Urine test.
Explain the medical management of the patient with status epilepticus. (State the medical management of a patient with status epilepticus.)
Provide anti-epileptic drug to the patient.
Ex:=
Phenytoin Sodium,
Provide sedative medication to the patient.
Ex:= Diazepam.
To continuously monitor the patient’s vital signs.
Keep the patient’s airway properly patent.
Monitoring the patient continuously.
Giving advice for modification of patient’s lifestyle.
To provide a properly safe environment to the patient.
Explain the nursing management of patients with status epilepticus. (State the nursing management of a patient with status epilepticus.)
To continuously monitor the patient’s vital signs.
Keep the patient’s airway properly patent.
Provide oxygen to the patient properly.
Properly documenting the type of seizure the patient has and how long it lasts.
Provide proper medication to the patient.
To provide proper safety measures to the patient.
To provide proper information about the patient’s condition to the patient and his family members.
Providing proper emotional support to the patient and his family members.
Collaborating properly with other health care personnel for patient care.
To provide a properly safe environment to the patient.
To provide proper working and comfortable environment to the patient.
Advising the patient to take medication properly.
Advising the patient to follow up regularly.