ENGLISH unit-8- MSN 1-respiratory disorder(juhi-part-3)
Define obstruction of upper airway
This is a life threatening emergency. In which the respiratory passage gets blocked due to upper airway obstruction which obstructs the free flow of the airway.
Write causes of upper airway obstruction
Foreign Object: Inhaling or ingesting a foreign object. that block the airway such as food pieces, toys or small items
Infection: Epiglottitis and infection in the larynx and pharynges can cause edema and spasm. This causes airway blockage.
Trauma: Obstruction in the upper airway is seen due to injuries to the face and neck. such as fracture and dislocation
Allergic Reaction: Severe allergic reactions cause swelling of the airways leading to obstruction.
Tumors: Abnormal growths and tumors in the upper airways cause blockage of the air passages.
Write clinical manifestations of upper airway obstruction
Choking is the main sign due to upper airway obstruction.
Choking: The universal sign for choking is ‘hand clutches to the throat’ i.e. a person clutches his throat during choking.
Difficulty in breathing
Cuffing or gagging
Cyanosis
Distress
Restlessness
Difficulty in speaking
Aphonia
Respiratory distress and death Write management of upper airway obstruction
Assessment: Assess the severity of the obstruction. Checking for signs of respiratory distress are present.
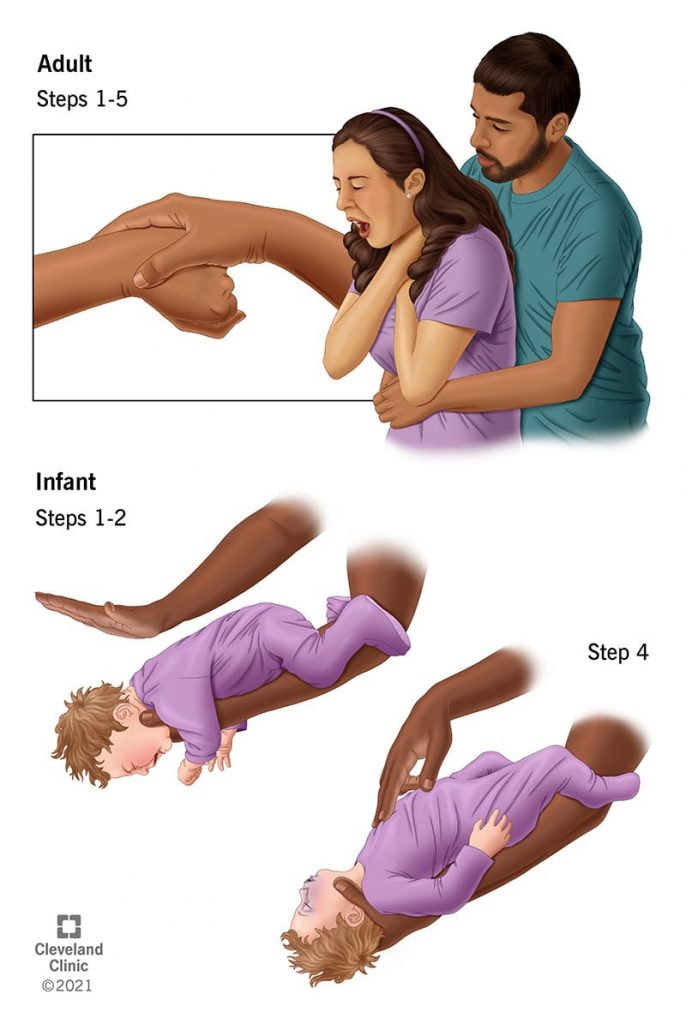
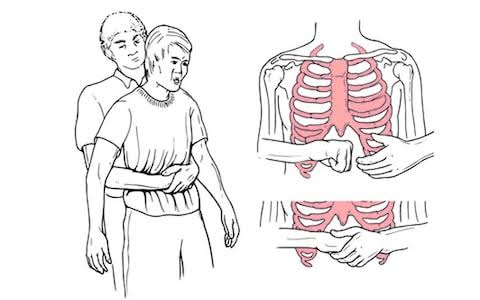
Clear the Airway: Give the Heilmeich maneuver to clear the airway.
Standing on the back of the adult patient. Place one foot slightly in front of the other to create balance. If there is a child, sit behind him with legs folded.
Hold the arm next to the patient’s waist.
•Then make a fist with one hand and place the thumb side of that fist against the person’s stomach, above the navel and below the ribs.
Grasp the fist with the help of the other hand and provide rapid upward thrusts in the abdomen.
To provide repeated thrusts if the object is not yet ejected.
Applying less pressure to the child.
Provide chest thrusts to the patient if the patient is pregnant and the arm is not around the stomach. Chest thrusts involve placing the hand on the breast bone and providing thrusts.
To provide back blow to newborn and infant.
In which placing the baby in the forearm and giving five black blows with Joe’s gripped hand.
Open the airway: If the patient is conscious and has difficulty in breathing, ask the patient to forcefully exhale the cough to clear the obstruction.
Call for help: If the obstruction does not clear and the patient’s condition worsens, call for emergency services.
Oxygen Therapy: Provide supplemental oxygen to improve oxygen levels if oxygen is available.
Define epistaxis
Epistaxis means nose bleed or nasal hemorrhage
Bleeding from the nostril or nasal cavity due to rupture of vessels in any area of the mucus membrane in the nose is known as epistaxis. Type of epistaxis
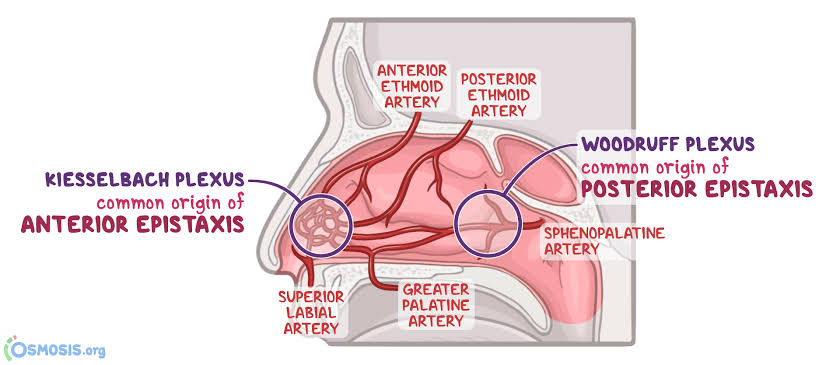
Epistaxis or nose bleed is divided into two types based on its location.
Anterior Epistaxis:
Anterior epistaxis involves bleeding from blood vessels in the front part of the nose. That area is known as the Kisselbach plexus or Little’s area. Anterior epistaxis is the most commonly seen type in which building occurs from the nostril. It can be managed by gently applying pressure or nasal packing.
Posterior Epistaxis:
Posterior epistaxis involves bleeding from the back part of the nose or the deeper nasal cavity. That is, bleeding is seen from the area with the sphenopalatine artery. That area is known as the Woodruff plexus. Posterior epistaxis is less common but is a challenge to control. In which bleeding is seen from the nostrils and blood drains into the throat, hence blood is seen in the sputum. Management of posterior epistaxis requires surgical procedures.
Write causes of epistaxis
Nasal Trauma (Most Common Cause)
Nasal infection
Nasal irritant
dry air
Allergies
Underlying Medication (Heparin, Warfarin) Explain pathophysiology of epistaxis
Due to etiological factors
|
Inflammation is seen in the vessels of the mucus membrane in the nose.
|
This causes vessels to rupture.
|
So nose bleed is seen.
Explain sign & symptoms of epistaxis
Bleeding from the nose (nose bleed)
Blood draping from the nostrils
Presence of blood clot
Mouth bleed
Tachycardia
Head one
Dizziness
Fanting How to diagnose epistaxis (How to diagnose epistaxis)
History Collection
Physical Examination
Nasal endoscopy
x ray
CT scan
Angiography
Biopsy Write medical management of epistaxis
Pressure:
Pressure is applied on the soft part of the nose i.e. the nose is pinched with thumb and index finger for 10 to 15 minutes and mouth breathing is asked. This method is called Trotter method. During this method the patient is given a sitting or semi-fowler position.
Ice Pack:
Apply ice packs or cold compresses to the bridge of the nose to constrict blood vessels and reduce bleeding.
Nasal spray:
Using an over-the-counter saline nasal spray or decongestant. Which helps the blood vessels to shrink.
Topical medicine:
Using petroleum jelly as a topical agent. Which moisturizes the nasal mucosa and protects the nasal mucosa.
Write surgical management of epistaxis
Surgical management is performed to control the bleeding when medical management fails to control the nosebleed. It uses the following surgical methods.
Cauterization:
In cauterization, bleeding blood vessels are sealed using heat, electricity, or chemicals. In which silver nitrate is mostly used as a chemical.
Nasal packing:
In nasal packing, gauze or a special balloon is inserted into the nasal cavity and pressure is applied to the building point to stop the building. Nasal packing includes anterior and posterior nasal packing.
Ligation:
to blood vessels to stop bleeding in ligation
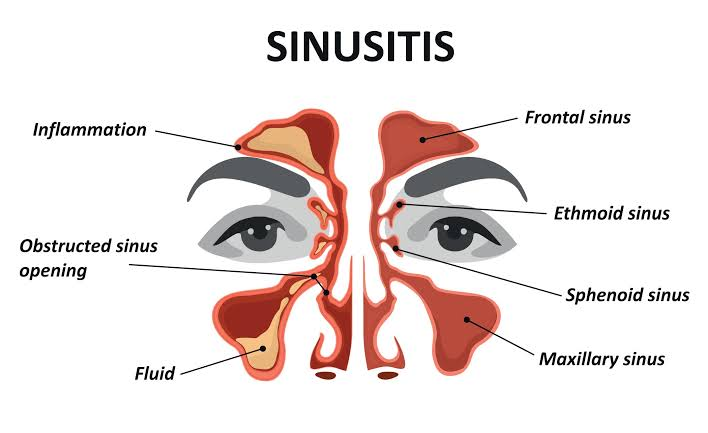
Define sinusitis
Infection and inflammation of the sinuses is known as sinusitis. Sinuses are air field cavities located in the face and skull.
Write causes of sinusitis
Viral infection
Bacterial infection
Allergies
Nasal polyps
Structural problem (deviated nasal septum)
Immune system disorder Risk factor
Changes in the Temperature and Air
swimming
smoking
Driving Classification of sinusitis
Sinusitis is classified as follows based on its duration and severity.
On the basis of duration:
1) Acute sinusitis : In acute sinusitis symptoms of sinusitis are present for less than four weeks. Which is mainly seen due to bacterial or viral infection. In which facial pain, nasal congestion, nasal discharge and fatigue are seen.
2) Subacute Sinusitis : In subacute sinusitis, symptoms of sinusitis occur for 4 to 12 weeks. It has symptoms similar to acute sinusitis but is less severe.
3) Chronic Sinusitis : In chronic sinusitis symptoms of sinusitis persist for 12 weeks or more. Chronic sinusitis is caused by persistent inflammation, recurrent infections, allergies, or structural issues.
4) Recurrent sinusitis : Multiple episodes of acute sinusitis within a year is known as recurrent sinusitis.
On the basis of location:
1) Maxillary sinusitis: Maxillary sinusitis is an inflammation of the maxillary sinus which is located in the cheekbone. Maxillary sinusitis is the most common type of sinusitis.
2) Frontal Sinusitis: Frontal sinusitis involves inflammation of the frontal sinuses. Which is located behind the forehead and does a frontal headache.
3) Ethmoid Sinusitis : Ethmoid sinusitis involves inflammation of the ethmoid sinus. Which is located between the ice. And it causes pain and pressure around the eye.
4) Sphenoid Sinusitis : Sphenoid sinusitis involves inflammation of the sphenoid sinus. It is located behind the ethmoid sinus and deep in the skull. Which causes earache, headache and neck pain.
Write clinical manifestations of sinusitis
Clinical signs depend on the type and severity of sinusitis.
Facial pain and pressure: Pain is seen in the eye, forehead, nose and cheek area.
Nasal Congestion: Blockage and stuffiness in the nasal passages.
Nasal discharge: Thick discolored mucus discharge is seen.
Reduces sense of smell and taste
Cough
Sore throat
Fatigue
Fever
Head one
Toothache
Ear pressure or fullness
Halitosis
Vertigo
Blurred vision Write diagnostic evaluation of sinusitis
History Collection
Physical Examination
x ray
CT scan
Endoscopy Rhinoscopy Write medical management of sinusitis
Nasal decongestants: Administer nasal sprays or oral decongestants to reduce nasal congestion. So that drainage can be promoted. Do not use nasal decongestant sprays for long periods of time. Because it does rebound congestion.
Saline Nasal Irrigation: Using a saline solution to flush out the nasal passages helps clear mucus and reduces inflammation and promotes drainage.
Nasal corticosteroids: Use nasal corticosteroids to reduce inflammation of the nasal passages and sinuses, as well as to relieve symptoms of congestion.
Antibiotic: Provide antibiotic drugs to treat sinusitis if it is caused by bacterial infection.
Pain relievers: Provide over the counter medicines acetaminophen and ibuprofen to relieve facial pain, headache, earache.
Mucolytics: Provide mucolytic drugs to thin and loosen mucus so sinus drainage can be improved. Write surgical management of sinusitis
Surgical management is performed when medical management fails. The following are common surgical procedures performed for the management of sinusitis.
Functional Endoscopy Sinus Surgery (FESS): FESS is the most common surgical procedure used for the treatment of chronic sinusitis. In which a thin flexible tube is attached to the endoscope and a camera is attached to it. With the help of which the sinuses are visualized. The endoscope is introduced into the nostril through the nasal cavity and obstructions such as nasal polyps, scar tissue and bony growth are removed and the sinus opening is widened.
Image Guided Surgery: Image guided surgery is performed when the anatomy is distorted due to previous surgery or other diseases. In which location is decided with the help of CT scan or other image guided method and surgery is done.
Balloon Sinuplasty: This is a minimally invasive procedure in which a small flexible balloon catheter is inserted into the inflamed sinus and the balloon is inflated to dilate and expand the opening of the sinus.
Cardwell Luck Operation : Cardwell Luck operation is mainly performed for the treatment of chronic maxillary sinusitis. In which a large window is created in the maxillary sinus to improve drainage.
Sinus Irrigation: Surgical management in some cases involves placement of a sinus irrigation device such as a sinus stent or irrigation tube to promote drainage and reduce the risk of inflammation and infection.
Ethmoidectomy, maxillary antrostomy, sphenoidotomy: These are specific procedures that target the ethmoid, maxillary, and sphenoid sinuses by opening them and removing abnormal tissue and improving drainage.
Define Pharyngitis
Infection and inflammation of the pharynx is known as pharyngitis.
Also known as ‘sore throat’.
Write causes of pharyngitis
Bacterial infection: Pharyngitis is caused by group A streptococcus bacteria.
Viral infections: Viruses like common cold virus, influenza virus, Epstein Barr virus are responsible for causing pharyngitis.
Allergies: Irritation and inflammation of the throat is seen due to contact with allergens.
Environmental factors: Exposure to smoke, dry air and pollutants can cause pharyngitis.
Irritant: Exposure to strong chemicals and fumes can cause pharyngitis.
Gastroesophageal reflex disease: Backflow of stomach acid into the throat can cause irritation and pharyngitis. Explain sign & symptoms seen in pharyngitis
Sore throat
Throat pain
Redness and swelling
Dysphagia
Hacking Cough
Fever
Head one
Discomfort
Malays Write diagnostic evaluation of pharyngitis (Write diagnostic evaluation of pharyngitis)
History Collection
Physical Examination
Complete blood count
Throat culture Write management of pharyngitis
Antibiotic: Using antibiotic medicine to treat bacterial infections. Like Penicillin, Azithromycin
Antiviral: Using antiviral medicine to treat viral infections. such as acyclovir
Corticosteroids: Using corticosteroid drugs to control inflammation.
Pain relievers: Use over-the-counter drugs such as acetaminophen and ibuprofen to relieve pain. Which relieves pain and reduces body temperature.
Throat Lozenges : Throat lozenges relieve throat irritation.
Hydration: Intake plenty of fluids to maintain hydration.
Warm Salt Water Gargle: Gargle with warm salt water. So throat discomfort is removed.
Avoid Irritants: Avoid irritants like smoking, pollutants etc.
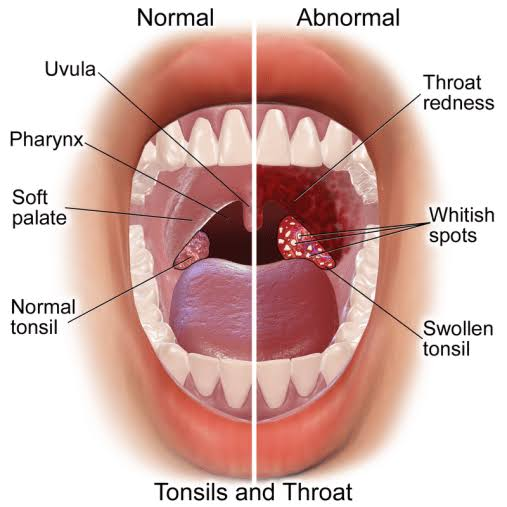
Define Tonsillitis
Infection and inflammation of the tonsils is known as tonsillitis, which is mainly caused by bacterial and viral infections.
(Tonsils are small masses of tissue located at the side of the throat that filter and kill foreign bodies entering through the nose and mouth)
Write causes of tonsillitis
Tonsillitis is mainly caused by bacterial and viral infections. Tonsillitis is mainly caused by Group A Streptococcus bacteria. Common viruses include influenza virus, herpes simplex virus, cytomegalovirus, adenovirus, and Epstein-Barr virus.
Explain pathophysiology of tonsillitis
Due to etiological factors
|
Bacteria and viruses enter the body through the nose and mouth.
|
It is filtered by the tonsils there.
|
White blood cells surround and fight bacteria and viruses.
|
This increases the body temperature. Due to which fever is seen.
|
Tonsils become inflamed and painful.
|
A condition of tonsillitis is seen.
Explain sign & symptoms seen in tonsillitis
Swelling is seen in the throat
Sore throat and throat pain
White and yellow patches are seen on the tonsils
Dysphagia (difficulty in swallowing)
Swelling is seen in the lymph nodes in the neck
Referred pain occurs in the ear (epilateral earache).
Bad breath and foul smelling (halitosis)
Fever
Head one
Chiles
Malays
Discomfort
Fatig
How to diagnose tonsillitis
History Collection
Physical Examination
Complete blood count
Throat Culture (Rapid Strip Test)
Write medical management of tonsillitis
Antibiotics: If tonsillitis is caused by a bacterial infection, antibiotic drugs are given to treat it.
Pain relievers: Provide analgesic medicine to relieve pain.
Corticosteroids: Administration of corticosteroid drugs to reduce inflammation in selected cases.
Antipyretic: Use of antipyretic drug to reduce fever.
Fluid: Provide plenty of fluid to the patient. So that dehydration can be prevented.
Rest: Provide adequate rest to the patient.
Write surgical management of tonsillitis
Tonsillectomy: Tonsillectomy is performed in patients with recurrent or chronic tonsillitis i.e. the tonsils.
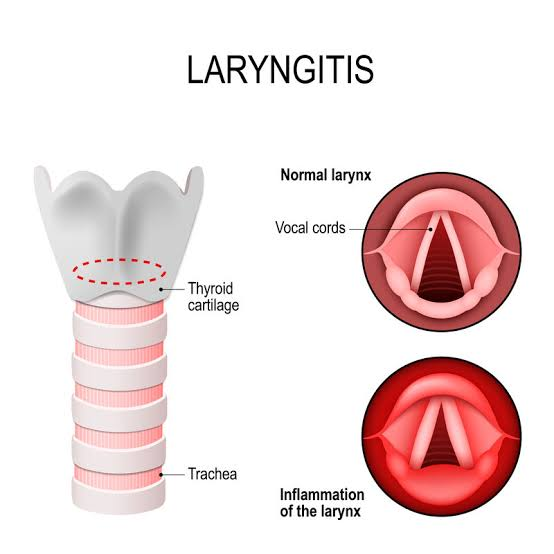
Define Laryngitis
Infection and inflammation of the larynx (voice box) is known as laryngitis.
Write etiological factor of laryngitis (Write etiological factor of laryngitis)
Bacterial infection: Laryngitis is caused by bacteria such as streptococcus.
Viral infections: Viruses responsible for the common cold and flu can also cause laryngitis.
Excessive train: Excessive train of the vocal cords (prolonged loud speaking) can lead to laryngitis.
Irritants: Exposure to irritants like smoke, strong fumes and chemicals can cause laryngitis.
Acid reflex
Allergies
Respiratory infection
Inhalation of toxic substances
Explain sign & symptoms seen in laryngitis
Horseness
Dry cough
Sore throat
Throat pain
Dysphagia (difficulty in swallowing)
Aphonia (loss of voice)
Fever
Fatig
Malays
Discomfort
Write medical management of laryngitis
Using antibiotic medicine to treat bacterial infections. Like Penicillin, Azithromycin
Antiviral: Using antiviral medicine to treat viral infections. such as acyclovir
Corticosteroids: Using corticosteroid drugs to control inflammation.
Pain relievers: Use over-the-counter drugs such as acetaminophen and ibuprofen to relieve pain. Which relieves pain and reduces body temperature.
Throat Lozenges : Throat lozenges relieve throat irritation.
Hydration: Intake plenty of fluids to maintain hydration.
Warm Salt Water Gargle: Gargle with warm salt water. So throat discomfort is removed.
Avoid Irritants: Avoid irritants like smoking, pollutants etc.
Resting the Voice : Do not give advice or talk too much to the patient, speak only when necessary.
Voice therapy: Voice therapy is provided in some cases to make the voice more effective.
Hydration: Ask the patient to ingest fluids to keep the vocal cords hydrated.
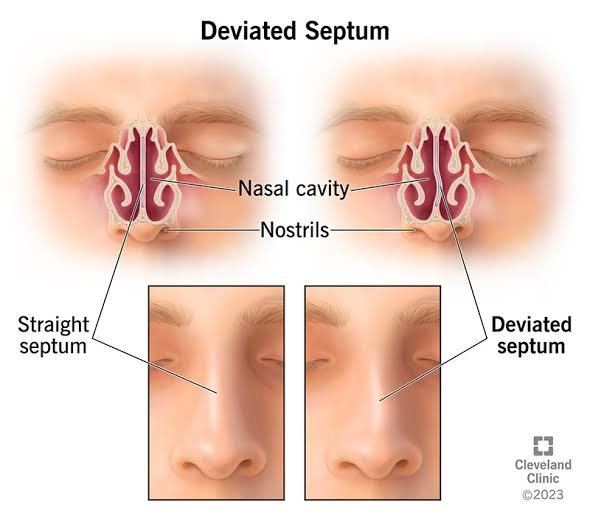
Define deviated nasal septum
The septum between the nostrils, which is normally thin and straight, deviates and protrudes from the midline, causing nasal obstruction and breathing difficulty.
Write causes of deviated nasal septum
A deviated nasal septum is congenital and acquired.
Congenital factor occurs due to birth defect or genetic predisposition.
Deviated nasal septum due to nasal trauma in accrual factor.
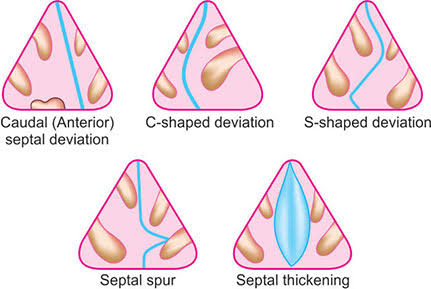
Types of deviated nasal septum (Types of deviated nasal septum)
Anterior or caudal dislocation: In anterior dislocation, the front portion of the septum is deviated. which can be visualized by external examination.
‘C’ Shape Deviation :
In ‘C’ shape deviation, the septum is deviated convexly to one side like the letter ‘c’.
‘S’ Shape Deviation :
In ‘S’ shape deviation, the septum is convexly deviated like the letter ‘s’.
Septal spur:
A spur is a shelf-like projection located near the junction of bone and cartilage. This spur dislocates towards the lateral wall.
Septal thickening: In some cases with nasal trauma, the nasal septum is thickened due to hematoma and access fibrosis.
Write sign and symptoms of deviated nasal septum
Difficulty in breathing
Noisy breathing
Nasal congestion
Recurrent sinus infections
Head one
Post nasal drip
Nose bleed
snoring
Wirte medical management of deviated nasal septum
Nasal decongestants: Use nasal decongestant sprays and drops to reduce nasal congestion.
Nasal corticosteroids: Use nasal corticosteroid sprays to reduce inflammation and swelling of the nasal passages.
Antihistamine: If nasal congestion and inflammation is observed due to allergy, antihistamine drug should be provided.
Saline Nasal Irrigation: Using saline nasal irrigation in a regular manner. Which helps clear the nasal passages and relieves congestion.
Nasal Dilators: Using external nasal dilators such as adhesive strips that widen the nasal passages to improve airflow.
Avoiding Allergens: Minimizing contact with allergens. So that the nasal symptoms can be relieved.
Wirte surgical management of deviated nasal septum
Submucous resection-SMR (submucous resection)
Submucous resection is a surgical procedure commonly used to treat a deviated nasal septum. In which the submucous tissue in the nasal septum is removed and repositioned.
Septoplasty
Septoplasty is a surgical procedure. In which the deviated septum, cartilage and bone are reshaped and repositioned. So that nasal air flow can be improved and breathing difficulty can be removed.
Rhinoplasty
Rhinoplasty is a cosmetic surgery. In which reshaping and resizing of nose is done i.e. reconstruction of nose is done. So that the appearance of the nose can be improved and the breathing issue can be solved.
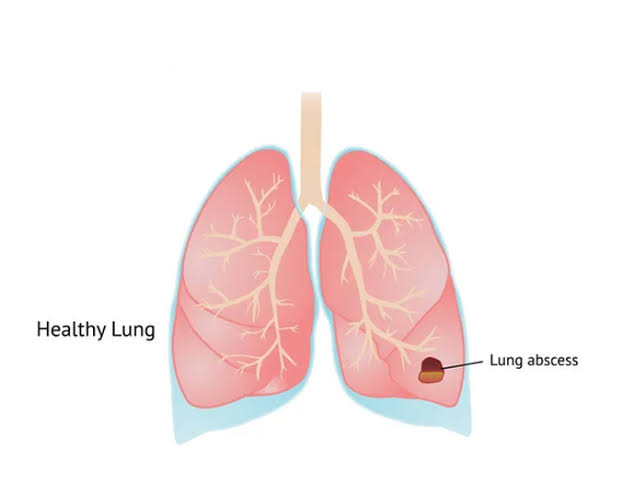
Define lung abscess
A lung abscess is characterized by pus-filled cavities in the lung parenchyma with inflammation and necrosis of the surrounding tissue.
Write causes of lung abscess
Bacterial infection: Lung abscess is most often caused by bacterial infection. Bacterial causes include Streptococcus pneumoniae, Klebsiella pneumoniae, Staphylococcus aureus.
Foreign body inhalation
Foreign body aspiration
trauma
Tuberculosis
COPD
Chronic lung disease Write clinical manifestations of lung abscess
Persistent cough
Blood in sputum
Foul smelling in sputum
Chest pain
Dyspnea
Shortness of breath
Fever
Chills
Wickness
diaphoresis
Cyanosis Write diagnostic evaluation of lung abscess
History Collection
Physical Examination
x ray
CT scan
like this. R. I
Sputum culture
Complete blood count
C reactive protein
Erythrocytes sedimentation rate
Biopsy Write management of lung abscess
Antibiotic therapy: Use of broad-spectrum antibiotics (amoxicillin, clindamycin) to treat bacterial infections.
Oxygen therapy: Provide supplemental oxygen if required.
Percutaneous drainage: If the abscess is large and antibiotics fail to treat it, drainage is necessary. Perform percutaneous drainage under CT scan.
Supportive care: Supportive care includes pain management, oxygen therapy, hydration level etc.
Treat underlying conditions: Treat underlying conditions associated with lung abscess.
Surgery: Perform pulmonary resection (lobectomy) in severe cases.
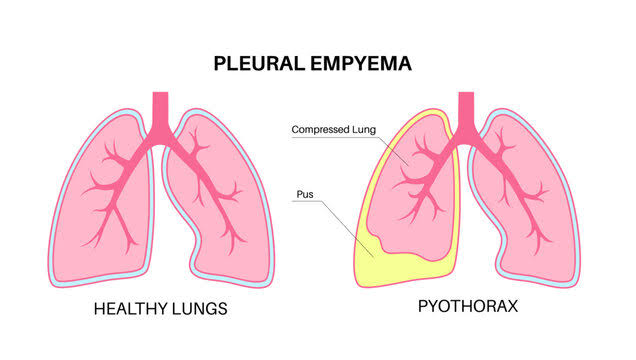
Define Empyema
Abnormal pus collection seen in the pleural cavity is known as empyema. Empyema is also known as ‘pyothorax’ and ‘purulent pleuritis’.
Empyema is mainly seen as a complication of pneumonia and lung abscess. Stage of Empyema
i) Exudative stage: Exudative stage is the early stage of empyema. In which sterile serous fluid accumulates in the pleural space.
ii) Fibropurulent stage : In this stage pleural fluid becomes purulent (pus like) and fibrous septa form pockets with localized pus.
iii) Organizing stage : This is the last stage of empyema. In which fibrin and pus are organized in the pleural space and form a thick pleural peel.
Write causes of empyema
Bacterial infection (Streptococcus pneumoniae)
Viral infection
Fungal infection
Pneumonia
Tuberculosis
Lung abscess
trauma
Chest Wound
Chest Surgery Risk Factor
smoking
Alcoholism
Immunosuppression Write clinical manifestations of Empyema
Shortness of breath
Chest tightness
Chest pain
Persistent cough
Fever
Chills
weakness
Fatig
Night sweats
Anorexia
Weight loss Write diagnostic evaluation of Empyema
History Collection
Physical Examination
x ray
CT scan
Ultra sound
Sputum Analysis
Thoracocentesis
Blood test
Write management of Empyema
Antibiotics: Providing antibiotics to treat bacterial infections.
Pain relievers: Provide analgesic drugs to relieve pain.
Antipyretic: Provide antipyretic drug to reduce fever.
Mucolytic: Provide mucolytic drugs to break up and clear mucus.
Thoracocentesis: In thoracocentesis, pus or fluid is aspirated by direct needle insertion into the pleural cavity.
Chest tube drainage: In chest tube drainage, a chest tube (thoracostomy tube) is placed in the pleural space and the pus is drained.
Fibrinolytic therapy: In cases with fibropurulent empyema, a fibrinolytic agent such as plasminogen activator is instilled into the pleural space. which breaks down the fibrin and helps in drainage.
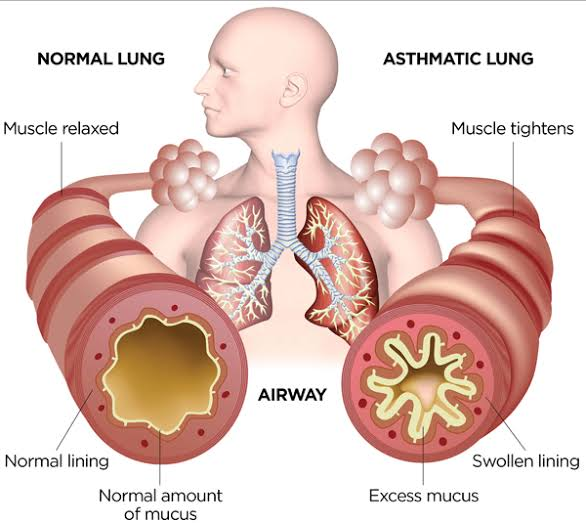
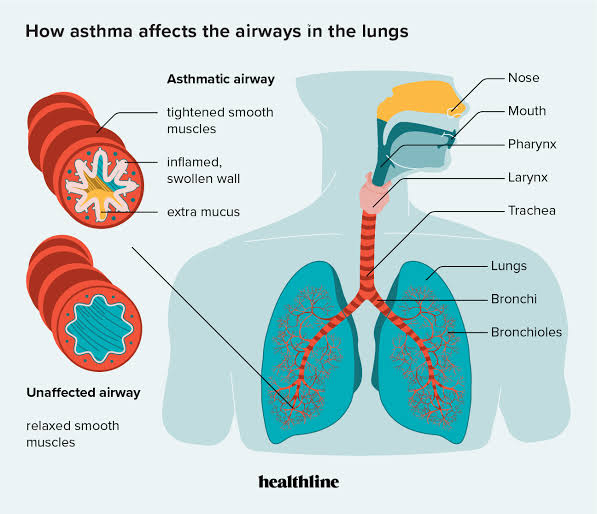
Bronchial asthma
Asthma is a chronic inflammatory respiratory disorder. In which the airways become hyper-responsive to certain stimuli, the airways become inflamed and narrowing, and the airways become obstructed due to mucus production.
Asthma differs from COPD in being a reversible process.
Write causes of asthma
Genetic factor
Family history
Respiratory infection
Environmental Factors: Exposure to Allergens, Air Pollutants (Dust, Chemicals)
Occupational factor
Chronic smoking
Explain pathophysiology of asthma
Due to etiological factors
|
Airway becomes hyperresponsive.
|
This causes inflammation in the airways.
|
Due to which there is hypersecretion of mucus, contraction of airway muscles and swelling of bronchial membrane.
|
Due to which airway narrowing occurs.
|
So cough, chest tightness, shortness of breath and wheezing sound are seen.
Write diagnostic evaluation of asthma
History Collection
Physical Examination
Pulmonary function test
Spirometer
Peak expiratory flow measurement
Fractional exhaled nitric oxide test
Pulse oximetry
Chest x-ray
CT scan
Sputum Analysis
Blood test
Complete blood count
ABGs Analysis
Allergy testing
Write medical management of asthma
Controller Medication: Controller medication is used to control symptoms.
Inhaled corticosteroids: This medication is most effective for long-term control of asthma. It reduces airway inflammation and decreases mucus production. For example budesonide, beclomethasone. In addition, a long-acting beta agonist is also inhaled.
Long Acting Beta Agonists: These bronchodilators drugs are used to dilate the bronchi. For example salmeterol
Leukotriene modifiers: Leukotriene modifiers block the action of leukotriene as an inflammatory molecule in asthma. which reduces airway inflammation and prevents symptoms. For example montelukast,
Mast Cell Stabilizers: Mast cell stabilizers inhibit inflammatory chemicals released from mast cells in the airways to relieve asthma symptoms. For example Nedocromil
Biological therapy: Biologic medications are used in severe asthma cases. For example monoclonal antibodies targeting IgE quick relief medication:
Quick relief medication is used to relieve symptoms quickly. In which short acting beta agonist and oral corticosteroid drugs are used.
Short Acting Beta Agonists: Short acting beta agonists are used to quickly relieve the condition of bronchospasm and improve airflow during an asthma attack. For example
Salbutamol and Levalbuterol
Oral corticosteroids: In severe conditions, oral corticosteroids such as prednisolone, methylprednisolone are given to quickly reduce airway inflammation.
Spacer device: This device is used with a metered dose inhaler. So that the medicine delivered to the lung can be improved.
Write nursing management of asthma
Impaired gas exchange related to altered oxygen supply, obstruction of airway
Improve gas exchange
To monitor vital signs.
Assess respiratory rate, rhythm and breathing pattern.
Assessing breath sound and chest movement.
Monitor pulse oximetry and arterial blood gas values.
Provide Fowler position to the patient and restrict his activities.
Explain and anchor the patient about deepbreathing and cuffing exercises.
To provide knowledge to patients about pursed lip breathing and diaphragmatic breathing.
Anchoring the patient to cough expectorate if secretions are present.
Provide oxygen therapy if spo2 level is low.
Providing nebulization to the patient.
Administer the medicine (bronchodilator) prescribed by the doctor.
To maintain records and reports.
Ineffective airway clearance related to obstruction from narrowed lumen Maintain patent airway
To monitor vital signs.
Assess respiratory rate, rhythm and breathing pattern.
Assessing breath sound and chest movement.
Monitor pulse oximetry and arterial blood gas values.
Provide Fowler position to the patient and restrict his activities.
Explain and anchor the patient about deepbreathing and cuffing exercises.
To provide knowledge to patients about pursed lip breathing and diaphragmatic breathing.
Anchoring the patient to cough expectorate if secretions are present.
Provide oxygen therapy if spo2 level is low.
Providing nebulization to the patient.
Administer the medicine (bronchodilator) prescribed by the doctor.
To maintain records and reports.
Ineffective breathing pattern related to bronchospasm Improving breathing pattern
To monitor vital signs.
Assess respiratory rate, rhythm and breathing pattern.
Assessing breath sound and chest movement.
Monitor pulse oximetry and arterial blood gas values.
Provide Fowler position to the patient and restrict his activities.
Explain and anchor the patient about deepbreathing and cuffing exercises.
To provide knowledge to patients about pursed lip breathing and diaphragmatic breathing.
Anchoring the patient to cough expectorate if secretions are present.
Provide oxygen therapy if spo2 level is low.
Providing nebulization to the patient.
Administer the medicine (bronchodilator) prescribed by the doctor.
To maintain records and reports.
Anxiety related to disease condition, hospitalization Reduce anxiety
Assess the patient’s condition.
Paying attention to the psychological needs of the patient and listening carefully to the patient.
Encouraging the patient to express his feelings, discomfort and anxiety.
To solve all doubts and queries of patients.
Providing knowledge to the patient about his condition and treatment so that his anxiety is removed and the patient becomes confident.
Providing psychological support to the patient.
Providing mind diversion therapy and recreational therapy to patients.
Activity intolerance related to fatigue, dyspnea increases activity level (increasing activity level)
Assess the patient’s condition.
Checking the patient’s activity level.
Provide bed rest to the patient initially.
Then gradually anchor the patient to range of motion exercises.
Assisting the patient with his activities.
2 Provide rest to the patient between activities.
To check if the patient has any breathing difficulty during the activity.
If breathing difficulty is found, stop the patient’s activity and provide rest.
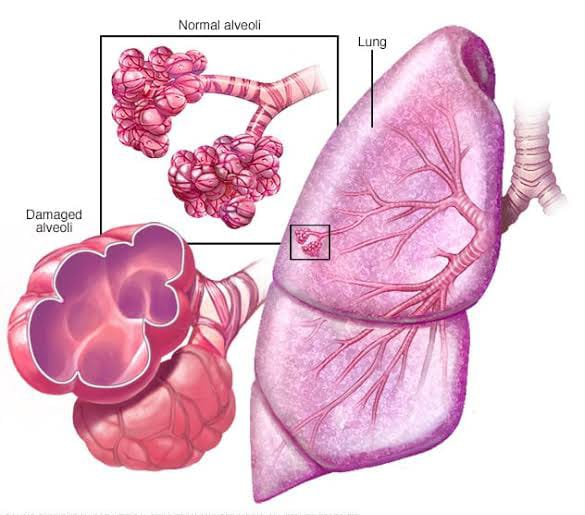
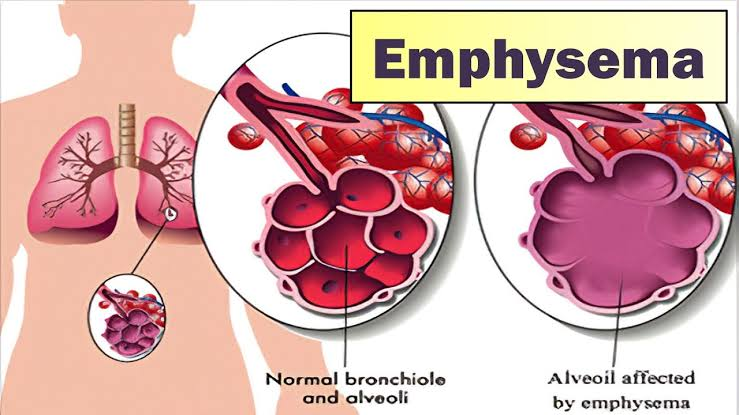
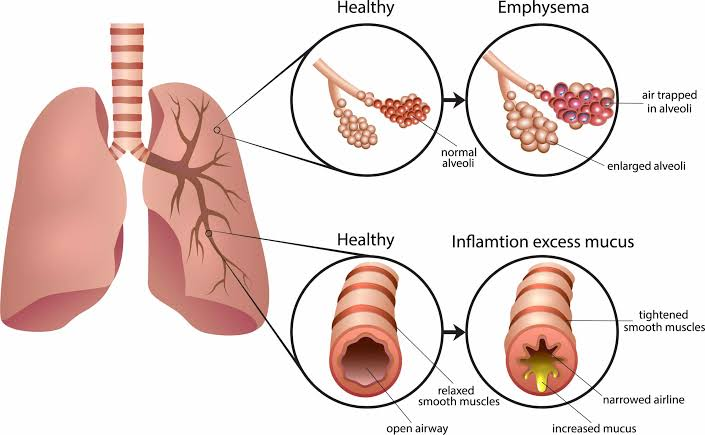
Define Emphysema
Emphysema is a Greek word meaning ‘inflation’.
Emphysema is a chronic lung disease. In which over distension and over inflation of the air sac (alveoli) of the terminal bronchioles in the lung are seen and the air sac is gradually damaged. Due to which shortness of breath is seen.
Emphysema is also known as ‘pink puffer’. Write causes of emphysema
Tobacco smoke
A second hand smoker
Air pollution
Exposure to dust, chemicals, fumes
Alpha one antitrypsin deficiency
Genetic factors Explain pathophysiology of emphysema
Due to etiological factors
|
Hyperinflation is seen in the LV.
|
Because of which, the wall of the alveoli capillary is seen to be distended.
|
Hence, the elasticity of the alveoli is lost and the gas exchange capacity of the alveoli is also lost.
|
Air traps in the LVOly.
|
A condition of emphysema is seen.
Write sign & symptoms seen in emphysema
Shortness of breath
Chronic cough
Wheezing sound
Chest tightness
Barrel chest
Decreases exercise tolerance
hypoxia
Hypercapnia
Cyanosis
Frequent respiratory infections
Fatig
Dia pheresis
Weight loss Write diagnostic evaluation of emphysema
History Collection
Physical Examination
Pulmonary function test
x ray
CT scan
M.R.I
Alpha antitrypsin test
Electrocardiogram
Complete blood count
Exercise tolerance test Write medical management of emphysema
Bronchodilators: Administer bronchodilators to relieve bronchial spasm and relax the muscles surrounding the airways. Bronchodilators relax the muscles around the airways and relieve spasm.
Inhaled corticosteroids: Inhaled corticosteroid drugs to reduce airway inflammation.
Mucolytics: Provide mucolytic drugs to thin mucus and expel it from the lungs.
Antibiotics: Providing antibiotic drugs to prevent bacterial infections.
Oxygen therapy: Providing supplemental oxygen to improve blood oxygen levels.
Write surgical management of emphysema
Bullectomy: In bullectomy, the affected bulla (air field space) is removed. So that compression on healthy lung tissue can be removed.
Lung Volume Reduction Surgery (LVRS): In LVRS, the damaged lung portion is removed. So that the patient can perform lung function well.
Lung Transplantation: In severe cases in which the lung function is significantly compromised, lung transplantation is the treatment. In which the lungs provided by the donor are replaced with the affected lung. Write nursing management of emphysema
To monitor vital signs.
Assess respiratory rate, rhythm and breathing pattern.
Assessing breath sound and chest movement.
Monitor pulse oximetry and arterial blood gas values.
Provide Fowler position to the patient and restrict his activities.
Explain and anchor the patient about deepbreathing and cuffing exercises.
To provide knowledge to patients about pursed lip breathing and diaphragmatic breathing.
Anchoring the patient to cough expectorate if secretions are present.
Provide oxygen therapy if spo2 level is low.
Providing nebulization to the patient.
Administer the medicine (bronchodilator) prescribed by the doctor.
To maintain records and reports. Write complications of emphysema
Chronic obstructive pulmonary disease
Pneumonia
Pneumothorax
Atelectasis
Recurrent respiratory tract infection
Respiratory failure
Respiratory acidosis
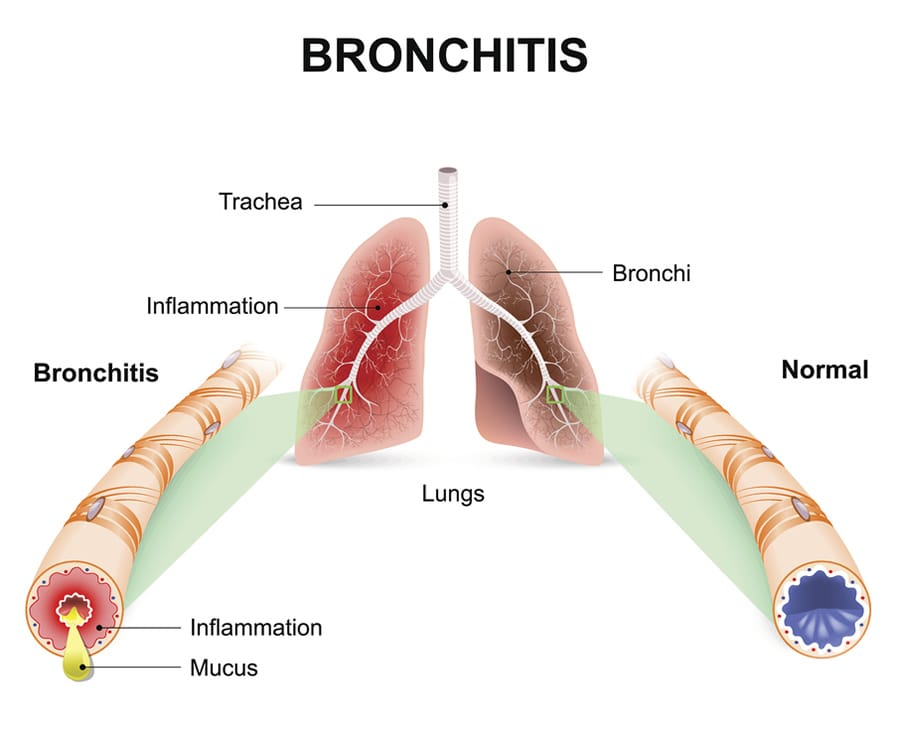
Define bronchitis
Inflammation of the bronchi and bronchial tubes is known as bronchitis. Bronchitis is also known as ‘blue blotter’.
Write causes of bronchitis
Viruses: Rhinovirus, influenza virus, parainfluenza virus
Bacteria : Mycoplasma pneumoniae, Bordetella pertussis
smoking
Air pollution
Exposure to Chemical Fumes
Contact to allergens
Weak immune system Explain pathophysiology of bronchitis
due to etiological factors
|
Hyperplasia is seen in the mucus gland.
|
Due to which goblet cells increase and mucus production increases.
|
Cilia function
|
So the bronchial lumen becomes narrow and there is limitation in air flow.
|
A condition of bronchitis is seen.
Write clinical manifestations of bronchitis
Shortness of breath
Runny and stuffy nose
Chest congestion
Wheezing sound
Yellow or green mucus production is seen
Chest tightness
diaphoresis
Low grade fever
Fatigue
Clubbing Write diagnostic evaluation of bronchitis
History Collection
Physical Examination
x ray
CT scan
Sputum culture
Blood test Write management of bronchitis
Bronchodilators: Administer bronchodilators drugs to relax the respiratory muscles and dilate the bronchi.
Antibiotic: Providing antibiotic drugs to treat bacterial infections.
Cough expectorant: Cough expectorant drug should be provided to expel the phlegm.
Nasal decongestants: Provide nasal decongestants to relieve congestion.
Rest and Hydration: Adequate rest and plenty of fluid intake.
Avoid irritants: Avoid contact with irritants.
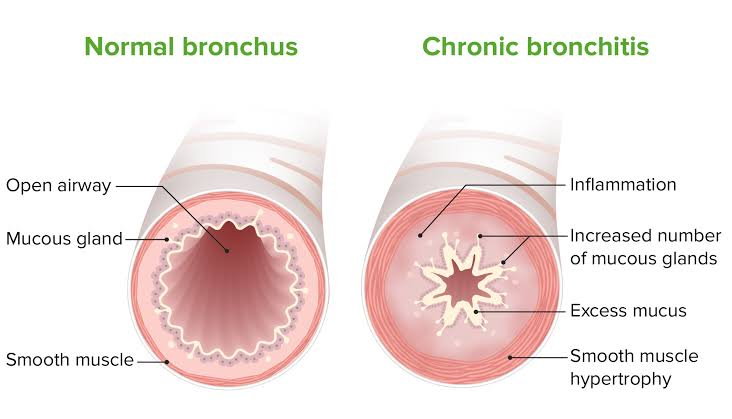
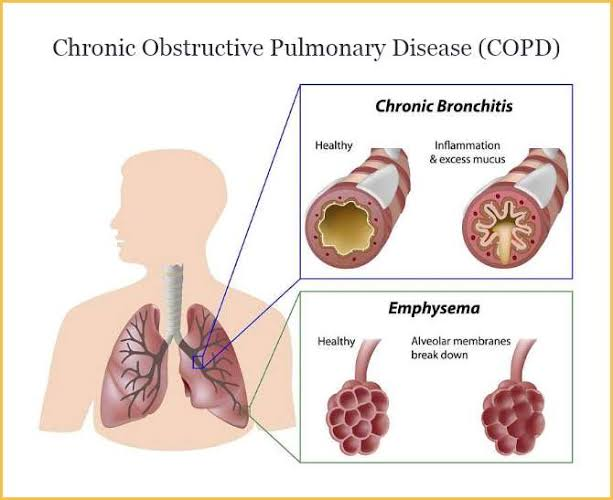
Define chronic obstructive pulmonary disease
Chronic obstructive pulmonary disease is a respiratory disease. In which airflow is obstructed due to chronic bronchitis and emphysema.
Write causes of chronic obstructive pulmonary disease
smoking
A second hand smoker
Environmental Factors
Occupational factor
Genetic factor (deficiency of alpha one antitypsin)
Exposure to pollutants Write clinical manifestations of chronic obstructive pulmonary disease
Chronic cough
Shortness of breath
Wheezing
Chest tightness
Chest pain
Barrel chest
Excessive mucus production
Frequent respiratory infections
Cyanosis
Clubbing
Fatigue
Weight loss
Write diagnostic evaluation of chronic obstructive pulmonary disease (Write diagnostic evaluation of chronic obstructive pulmonary disease)
History Collection
Physical Examination
x ray
CT scan
Spirometry
Pulmonary function test
Arterial blood gas analysis
Sputum Analysis
Blood test Write management of chronic obstructive pulmonary disease (Write management of chronic obstructive pulmonary disease)
Smoking Cessation: The most important intervention for the management of COPD is smoking cessation. which slows the progression of the disease and reduces its frequency and severity.
Medication:
Bronchodilators: Use short-acting bronchodilators (albuterol) and long-acting bronchodilators (salmeterol) to relax the muscles around the airways and improve airflow.
Inhaled corticosteroids: Administer inhaled corticosteroids to reduce airway inflammation. For example budesonide, fluticasone
Phosphodiesterase 4 inhibitors: Use of phosphodiesterase 4 inhibitors in patients with severe COPD and chronic bronchitis. Which reduces inflammation and prevents exacerbation.
Mucolytic drug: Use of mucolytic drug to thin the mucus and clear it from the airways.
Pulmonary Rehabilitation: This comprehensive program includes exercise training, education, nutritional and psychological support. So that the quality of life can be improved.
Oxygen Therapy: Providing supplemental oxygen to improve oxygen levels.
Lifestyle Modification: Lifestyle modification should include regular exercise, healthy diet, avoiding environmental pollutants and respiratory irritants.
Write nursing management of chronic obstructive pulmonary disease
Impaired gas exchange related to pulmonary obstruction as evidenced by hypoxia, hypercapnia, cynosis, abnormal ABG
Improve Gas Exchange
To monitor vital signs.
Assess respiratory rate, rhythm and breathing pattern.
Assessing breath sound and chest movement.
Monitor pulse oximetry and arterial blood gas values.
Provide Fowler position to the patient and restrict his activities.
Explain and anchor the patient about deepbreathing and cuffing exercises.
To provide knowledge to patients about pursed lip breathing and diaphragmatic breathing.
Anchoring the patient to cough expectorate if secretions are present.
Provide oxygen therapy if spo2 level is low.
Providing nebulization to the patient.
Administer the medicine (bronchodilator) prescribed by the doctor.
To maintain records and reports.
Ineffective airway clearance related to bronchoconstriction, increase mucus production Maintain patent airway
To monitor vital signs.
Assess respiratory rate, rhythm and breathing pattern.
Assessing breath sound and chest movement.
Monitor pulse oximetry and arterial blood gas values.
Provide Fowler position to the patient and restrict his activities.
Explain and anchor the patient about deepbreathing and cuffing exercises.
To provide knowledge to patients about pursed lip breathing and diaphragmatic breathing.
Anchoring the patient to cough expectorate if secretions are present.
Provide oxygen therapy if spo2 level is low.
Providing nebulization to the patient.
Administer the medicine (bronchodilator) prescribed by the doctor.
To maintain records and reports.
Ineffective breathing patterns related to shortness of breath, mucous production Improve breathing pattern
To monitor vital signs.
Assess respiratory rate, rhythm and breathing pattern.
Assessing breath sound and chest movement.
Monitor pulse oximetry and arterial blood gas values.
Provide Fowler position to the patient and restrict his activities.
Explain and anchor the patient about deepbreathing and cuffing exercises.
To provide knowledge to patients about pursed lip breathing and diaphragmatic breathing.
Anchoring the patient to cough expectorate if secretions are present.
Provide oxygen therapy if spo2 level is low.
Providing nebulization to the patient.
Administer the medicine (bronchodilator) prescribed by the doctor.
To maintain records and reports.
Knowledge deficit related to disease condition and it’s prognosis Improve knowledge level
Assess the patient’s condition.
Assessing the patient’s knowledge of the disease condition and its treatment.
To provide knowledge to the patient about the disease condition and its prognosis.
Providing knowledge in a language the patient can understand.
To resolve patient’s doubts and queries.
Anxiety related to disease condition, hospitalization Reduce anxiety
Assess the patient’s condition.
Paying attention to the psychological needs of the patient and listening carefully to the patient.
Encouraging the patient to express his feelings, discomfort and anxiety.
To solve all doubts and queries of patients.
Providing knowledge to the patient about his condition and treatment so that his anxiety is removed and the patient becomes confident.
Providing psychological support to the patient.
Providing mind diversion therapy and recreational therapy to patients.
Activity intolerance related to fatigue, dyspnea increases activity level (increasing activity level)
Assess the patient’s condition.
Checking the patient’s activity level.
Provide bed rest to the patient initially.
Then gradually anchor the patient to range of motion exercises.
Assisting the patient with his activities.
2 Provide rest to the patient between activities.
To check if the patient has any breathing difficulty during the activity.
If breathing difficulty is found, stop the patient’s activity and provide rest.
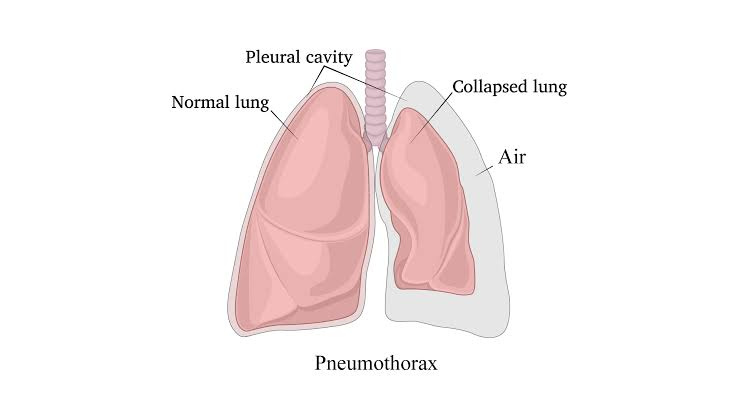
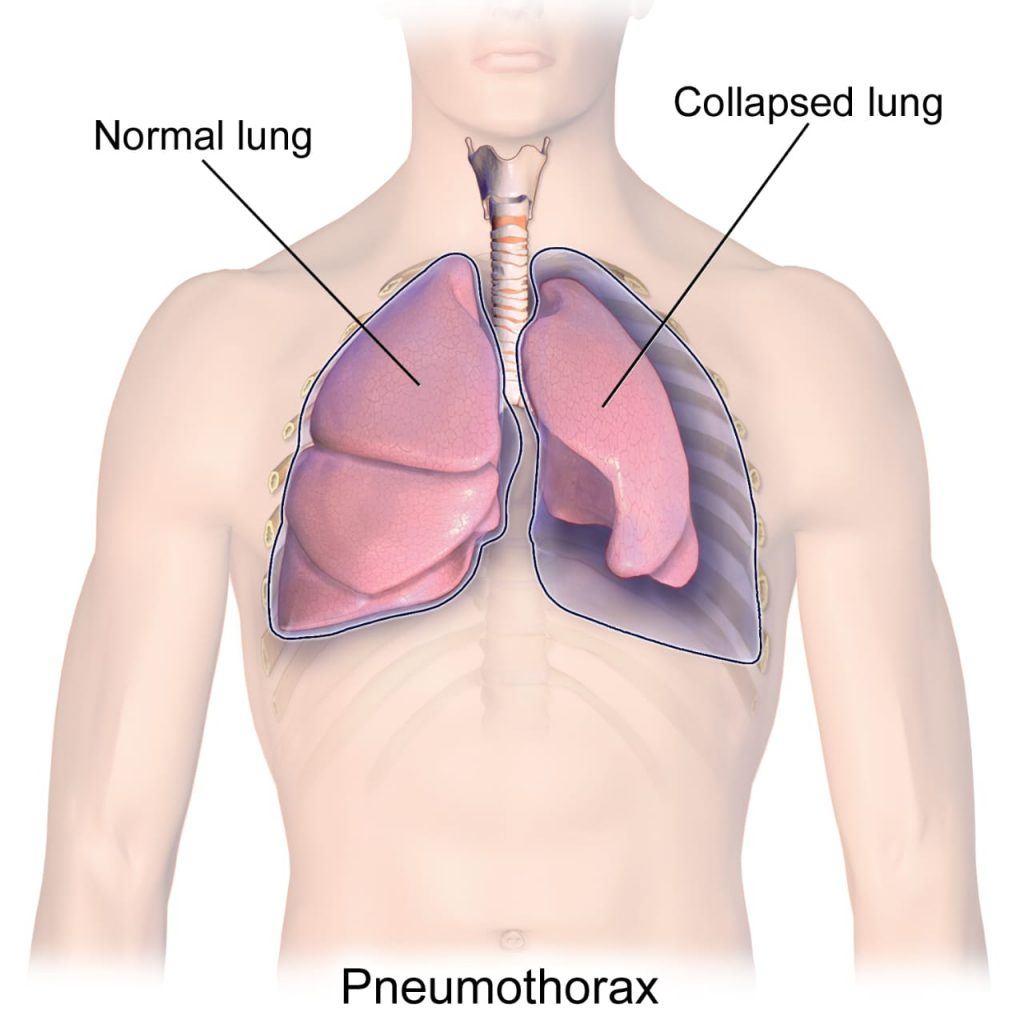
Pneumothorax is a medical condition. In which air or gas leakage is seen in the pleural cavity due to which the lung is seen collapsed.
Write causes of pneumothorax
Chest trauma (ribus fracture)
Lung Disease (COPD, Cystic Fibrosis)
Medical Procedures
Spontaneous Write clinical manifestations of Pneumothorax
Sudden sharp chest pain
Shortness of breath
Rapid breathing
Chest tightness
Cyanosis
Rapid heart rate Write diagnostic evaluation of Pneumothorax
History Collection
Physical Examination
x ray
CT scan
Ultrasound
ABG Analysis Write management of Pneumothorax
Needle Insurance:
In needle insertion, a hollow needle that is connected to a flexible tube (catheter) is inserted into the air filled space. The needle is then removed, the syringe is attached to the catheter and the air is removed.
Chest Tube Insurance:
In chest tube insertion, a flexible chest tube is inserted into the air filled space and has a one way valve attached to it that removes continuous air from the chest cavity.
Surgery: Some cases require surgery. In which a small incision is made and all the air is removed
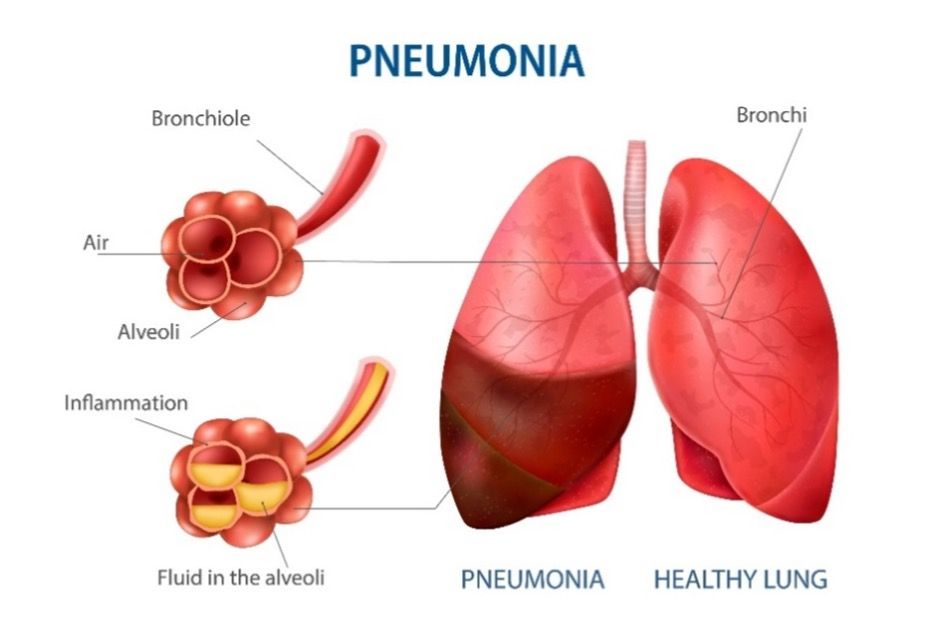
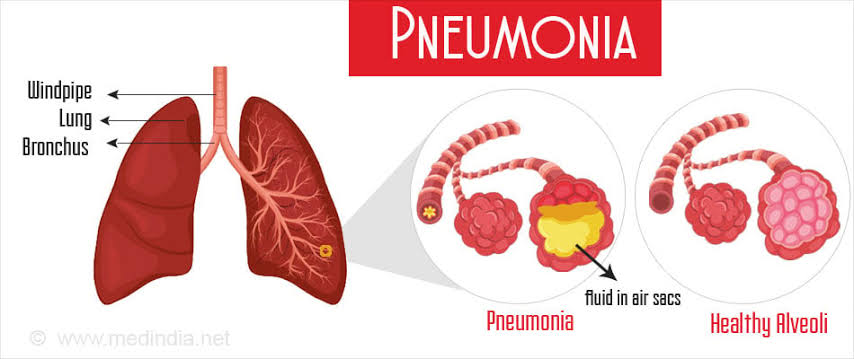
Define Pneumonia
Inflammation of the lung parenchyma (alveoli) known as pneumonia occurs due to bacterial, viral or fungal infection. In which the air sac fills with fluid or pus and becomes solid.
- Write classification of pneumonia
Pneumonia is classified based on its cause, anatomical structure and severity.
On the Basis of Etiological Factors
Bacterial Pneumonia:
Pneumonia caused by bacterial infection is known as bacterial pneumonia. Pneumonia is caused by the bacteria Streptococcus pneumoniae, Mycoplasma pneumoniae and Haemophilus influenzae.
Viral Pneumonia:
Pneumonia caused by a viral infection is known as viral pneumonia. Viruses such as influenza, corona virus, adeno virus and respiratory syncytial virus are responsible for causing pneumonia.
Fungal Pneumonia:
Pneumonia caused by fungal infection is known as fungal pneumonia.
On the Basis of Anatomical Structure
Based on the anatomical structure pneumonia is classified as follows:
Lobar Pneumonia:
Lobar pneumonia is an infection in one or more lobes of the lung.
Broncho pneumonia:
Bronchopneumonia involves infection of the bronchi in addition to multiple lobes.
Interstitial Pneumonia:
In interstitial pneumonia, the interstitial tissue and alveolar septa are infected.
On the Basis of Broad Classification
Community Acquired Pneumonia:
Pneumonia occurring in the community is called Community Acquired Pneumonia.
Hospital Acquired Pneumonia:
Pneumonia occurring after 48 hours of hospitalization is called hospital acquired pneumonia.
Ventilator Associated Pneumonia:
Pneumonia caused by endotracheal incubating or mechanical ventilation is called ventilator-associated pneumonia.
Aspiration Pneumonia:
Pneumonia due to endogenous or exogenous subtense aspirate is called aspiration pneumonia.
Write causes of Pneumonia
Bacterial infection
Viral infection
Fungal infection
Aspiration of gastric contents
Inhalation of chemical substances and fumes Write clinical manifestations of pneumonia
Productive Cough (Green and Yellow Color)
Blood in sputum
Shortness of breath
Chest pain
Cyanosis
Orthopnea
tachypnea
Fever
Dehydration
Malay
Confusion
Sweating
Nozia
Vomiting
Diarrhea
Anorexia Write diagnostic evaluation of pneumonia
History Collection
Physical Examination
Pulmonary function test
x ray
CT scan
Sputum culture
Complete blood count
C reactive protein
Blood culture
Pulse oximetry
Arterial blood gas analysis Write management of pneumonia
Antibiotic therapy: Providing antibiotic drugs to treat bacterial pneumonia.
Antiviral drug: Antiviral drug administration to treat viral pneumonia.
Fever Management: Provide the over-the-counter medicine acetaminophen to relieve fever.
Pain relievers: Provide analgesic drugs to reduce chest pain.
Oxygen Therapy: Provide supplemental oxygen to maintain oxygen levels.
Cough expectorant: Provide cough expectorant to thin and expel cough.
Rest and Fluid: Provide adequate rest to the patient. Also maintaining hydration levels. Write nursing management of pneumonia
Ineffective airway clearance related to bronchoconstriction and increased mucus production
To monitor vital signs.
Assess respiratory rate, rhythm and breathing pattern.
Assessing breath sound and chest movement.
Monitor pulse oximetry and arterial blood gas values.
Provide Fowler position to the patient and restrict his activities.
Explain and anchor the patient about deepbreathing and cuffing exercises.
To provide knowledge to patients about pursed lip breathing and diaphragmatic breathing.
Anchoring the patient to cough expectorate if secretions are present.
Provide oxygen therapy if spo2 level is low.
Providing nebulization to the patient.
Administer the medicine (bronchodilator) prescribed by the doctor.
To maintain records and reports.
Impaired gas exchange related to decreased ventilation
To monitor vital signs.
Assess respiratory rate, rhythm and breathing pattern.
Assessing breath sound and chest movement.
Monitor pulse oximetry and arterial blood gas values.
Provide Fowler position to the patient and restrict his activities.
Explain and anchor the patient about deepbreathing and cuffing exercises.
To provide knowledge to patients about pursed lip breathing and diaphragmatic breathing.
Anchoring the patient to cough expectorate if secretions are present.
Provide oxygen therapy if spo2 level is low.
Providing nebulization to the patient.
Administer the medicine (bronchodilator) prescribed by the doctor.
To maintain records and reports.
Infective breathing pattern related to chest pain to monitor vital signs.
Assess respiratory rate, rhythm and breathing pattern.
Assessing breath sound and chest movement.
Monitor pulse oximetry and arterial blood gas values.
Provide Fowler position to the patient and restrict his activities.
Explain and anchor the patient about deepbreathing and cuffing exercises.
To provide knowledge to patients about pursed lip breathing and diaphragmatic breathing.
Anchoring the patient to cough expectorate if secretions are present.
Provide oxygen therapy if spo2 level is low.
Providing nebulization to the patient.
Administer the medicine (bronchodilator) prescribed by the doctor.
To maintain records and reports. Write complication of pneumonia
Respiratory failure
Sepsis
Lung abscess
Pleural effusion
Atelectasis
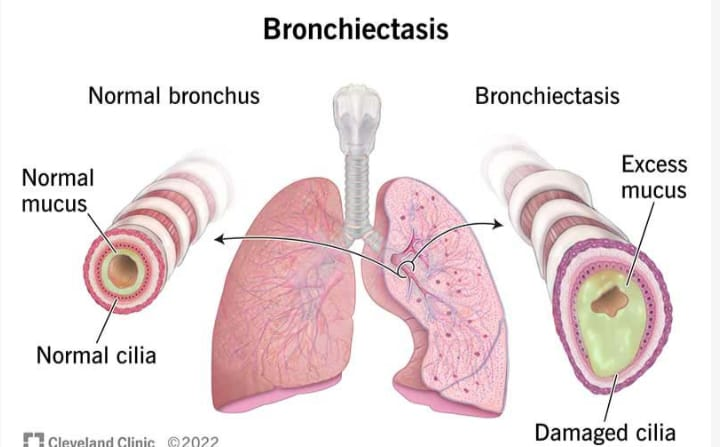
Define bronchiectasis
Bronchiectasis is a chronic respiratory condition characterized by abnormal and irreversible dilation, inflammation and thickening of the bronchi and bronchioles. As a result of which there is accumulation of mucus and the mucus is not cleared properly from the airways due to which recurrent respiratory infections are seen.
Write causes of bronchiectasis
Infection (previous respiratory infection such as pneumonia, tuberculosis
Genetic disorder (cystic fibrosis)
Immune system disorders (rheumatoid arthritis, inflammatory bowel disease)
Auto immune conditions
Allergic bronchopulmonary aspergillosis
Environmental factors Write clinical manifestations of bronchiectasis (Write clinical manifestations of bronchiectasis)
Chronic cough
Excessive sputum production
Blood in cough
Shortness of breath
Wheezing
Chest pain
Recurrent respiratory infection
Clubbing of fingers
Weight loss
Fatig
Weakness Write diagnostic evaluation of bronchiectasis
History Collection
Physical Examination
x ray
CT scan
Pulmonary function test
Sputum culture
Bronchoscopy Write medical management of bronchiectasis
Bronchodilators: Administer bronchodilators drugs to relax the airway muscles and dilate the bronchi.
Antibiotic: Providing antibiotic drugs to treat bacterial infections.
Expectorant and mucolytics: Provide expectorant and mucolytic drugs to thin and expel mucus.
Airway clearance techniques : Airway clearance techniques like chest physiotherapy, postural drainage Write surgical management of bronchiectasis (Write surgical management of bronchiectasis)
In severe cases, severely damaged lung tissue is surgically removed.
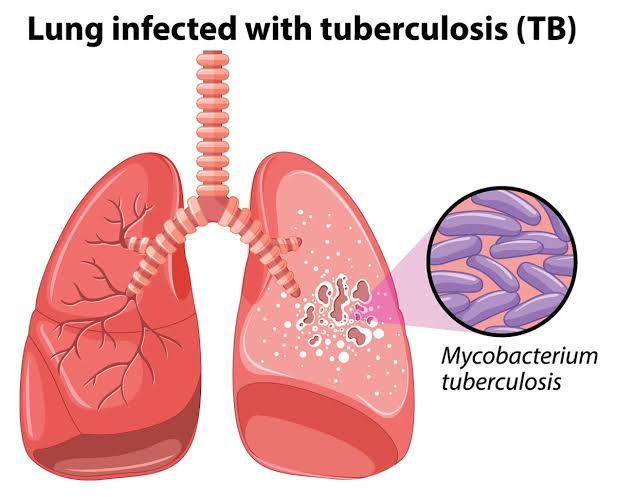
Define pulmonary tuberculosis
Pulmonary tuberculosis is a serious infection caused by the bacterium Mycobacterium tuberculosis that primarily affects the lungs but can also spread to other areas of the body. Pulmonary tuberculosis is spread through air i.e. by coming into contact with coughing or sneezing of an infected person.
Write risk factor of pulmonary tuberculosis
Close contact with active tuberculosis patients
Weak immune system (HIV, organ transplantation, cancer, corticosteroid therapy)
Edge
Subtons abuse
Living in over crowded area
Malnutrition
Chronic health conditions
Write clinical manifestations of pulmonary tuberculosis
Persistent Cough (Cough present for more than three weeks)
Blood in sputum
Chest pain
Fever
Fatigue
Night sweats
Loss of appetite
Weight loss
Shortness of breath Write diagnostic evaluation of pulmonary tuberculosis
History Collection
Physical Examination
Tuberculin skin test
x ray
Sputum test
Blood test
Write management of pulmonary tuberculosis
Antibiotic therapy: A combination of antibiotics is given as a treatment for pulmonary tuberculosis. In which isoniazid, rifampin, ethambutol and pyrazinamide medications are given. A course of this medicine is done for six to nine months.
Directly Observed Treatment Short Course (DOTs): DOTs therapy involves supervision of TB patients by a health care provider. The patient takes exactly the regular medicine and its effectiveness is observed. So it can be known whether the patient has completed the full course of treatment or not.
Isolation: TB positive patients are isolated. Because TB is a contagious disease and it is spread through air to each other. Hence the patient is isolated to prevent it from spreading.
Nutritional Support: Provide adequate nutrition to the patient with TB to improve his immune system and gain weight.
Education and Counselling: Provide education and counseling to patients about tuberculosis. Explain infection control measures to the patient and his family members.
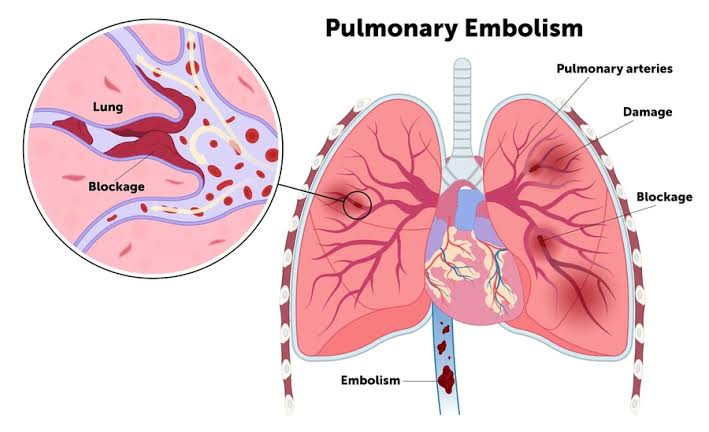
Define pulmonary embolisms
Pulmonary embolism occurs when one or more pulmonary arteries become obstructed or blocked by a thrombus (blood clot). This thrombus originates from the vascular system or right heart and travels to the pulmonary artery.
Write cause of pulmonary embolism
Deep vein thrombosis
Hypercoagulation
Venous Status Risk Factor
Trauma and Injury
Surgery
Prolonged immobilization
Heart failure
Heart disease
Hormonal factor
Advanced Edge
Obesity Write sign & symptoms seen in pulmonary embolism
Rapid onset of dyspnoea
Shortness of breath
Pleuritic chest pain
Tachycardia
diaphoresis
Blood in cough (haemoptysis)
Cyanosis
Fever
Fanting
Calf & Thy Pain Write diagnostic evaluation of pulmonary embolism (Write diagnostic evaluation of pulmonary embolism)
History Collection
Physical Examination
Chest x-ray
Ultra sound
Magnetic resonance imaging
Pulmonary angiography
Ventilation perfusion scan
D dimer test
Electrocardiogram Write management of pulmonary embolisms
Anticoagulant therapy:
Providing anticoagulant drugs for the treatment of pulmonary embolism. Which prevents the formation of blood clot and helps dissolve the clot. Giving heparin, low molecular weight heparin medicine as anticoagulant drug.
Thrombolytic Therapy: Provide thrombolytic therapy to rapidly dissolve the clot in life threatening and emergency conditions. which breaks down clots. For example tissue plasminogen activator (tPA)
Inferior vena cava filter: Inferior vena cava filter is used when anticoagulant therapy is contraindicated or ineffective. In which an inferior vena cava filter is placed which prevents the clot in the lower area of the body from traveling to the lungs and depositing in the filter there.
Supplemental Oxygen: Provide supplemental oxygen to maintain adequate oxygen levels.
Embalectomy: Embalectomy involves the surgical removal of a clot (embolism).
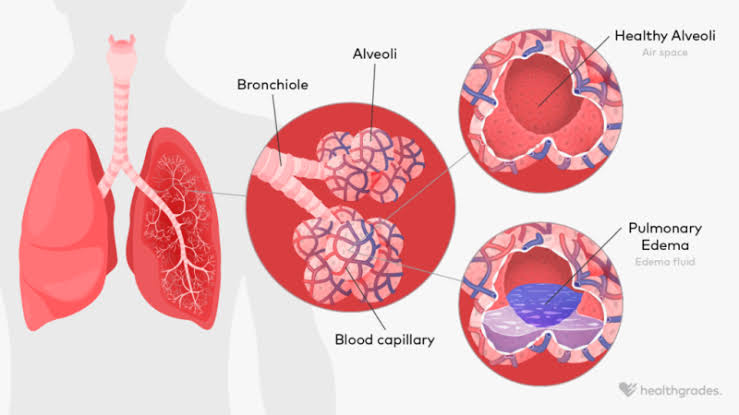
Define pulmonary edema
Pulmonary edema is a condition in which fluid accumulates or builds up around the lungs and this fluid collects in the air sacs, causing breathing difficulties.
Write causes of pulmonary edema
Congestive heart failure
Renal failure
Acute kidney injury
Exposure to certain toxins and drugs
Heart disease
Acute respiratory distress syndrome
Near drowning Explain sign & symptoms seen in pulmonary edema
Shortness of breath
Rapid breathing
Persistent cough and frothy mucus
Blood in cough
Whizzing
Feeling like suffocation
Chest tightness and pain
Fatigue
Restlessness
Increase heart rate
Swelling in leg Write diagnostic evaluation of pulmonary edema
History Collection
Physical Examination
Chest x-ray
Echocardiogram
Electrocardiogram
Complete blood count
Arterial blood gas analysis
Brain natriuretic peptide
Basic metabolic panel Write management of pulmonary edema
Oxygen therapy: Providing supplemental oxygen to improve oxygen levels.
Diuretic: Provide diuretic medicine like frusemide. which prevents fluid overload and reduces pulmonary congestion. Diuretics increase urine output and remove excess fluid from the body.
Vaso dilator: Administer a vasodilator drug such as nitroglycerin or nitroprusside to reduce heart load and decrease cardiac output load. which dilates blood vessels and improves cardiac output.
Inotropic agent: Administration of inotropic agent to improve myocardial contractility. such as dobutamine
Positioning: Elevating the patient’s head off the bed and providing the patient with an upright sitting position. So that lung expansion and venous return can be improved.
Fluid retraction: Fluid retraction in conditions of fluid overload to prevent pulmonary congestion.
Treat underlying causes: Identify and treat the underlying cause of pulmonary edema.
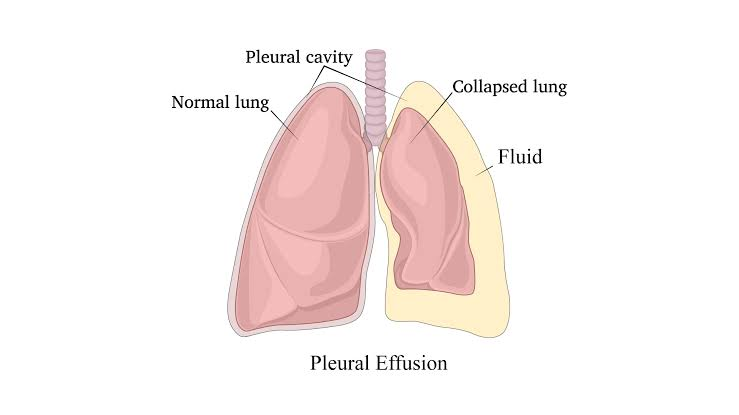
Define pleural effusion Define pleural effusion
Abnormal fluid collection seen in the pleural cavity is known as pleural effusion.
Write causes of pleural effusion
Congestive heart failure
Pneumonia
Pulmonary embolism
Cancer
Liver disease
Kidney disease
Tuberculosis
Auto immune diseases Write clinical manifestations of pleural effusion
Shortness of breath
Chest pain
Dry cough
Reduce chest expansion
Dullness to percussion
Decrease Breathe Sound
Pleuritic pain
Fever
Fatig Write diagnostic evaluation of pleural effusion (Write diagnostic evaluation of pleural effusion)
History Collection
Physical Examination
x ray
CT scan
Ultra sound
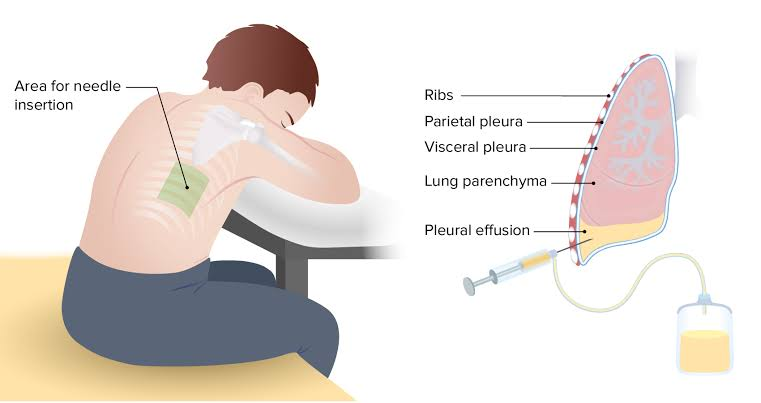
Thoracocentesis
Pleurodesis
Pleural fluid analysis
Pleural biopsy Write medical management of pleural effusion
Diuretic: If pleural effusion is due to congestive heart failure or fluid overload, give diuretic drug to treat it.
Antibiotic: Providing antibiotic drugs to treat bacterial infections.
Anti-inflammatory medication: Provide anti-inflammatory medication or corticosteroid drug to treat pleural effusion due to autoimmune disease or inflammatory condition.
Chemotherapy & Radiation Therapy: If the pleural effusion is due to cancer, chemotherapy and radiation therapy should be provided to treat the cancer.
Pain relievers: Providing pain relievers to relieve pain. such as ibuprofen
Anti-pyretic: Provide anti-pyretic drug to reduce fever.
Oxygen Therapy: Providing supplemental oxygen to improve oxygen levels. Write surgical management of pleural effusion
Video Assisted Thoracic Surgery (VATS): This is a minimally invasive procedure. In which a small incision is made on the chest wall and a thoracoscope is inserted and the fluid is drained and a biopsy is collected from the abnormal tissue.
Pleurodesis: Pleurodesis is a procedure in which adhesion is created between the two layers of the pleura to prevent fluid accumulation due to inflation. In which a sclerosing agent is instilled into the pleural space during thoracoscopy which induces adhesion formation.
Pleurectomy: In a pleurectomy procedure, the parietal pleura and visceral pleura are surgically removed. So that fluid accumulation between them can be prevented.
Pleural catheter placement: In pleural catheter placement, a small tube is inserted through the chest wall into the pleural space through which fluid is continuously drained. Write complications of pleural effusion
Pneumothorax
empyema
Plural thickening
Atelectasis
Respiratory failure
Pulmonary hypertension
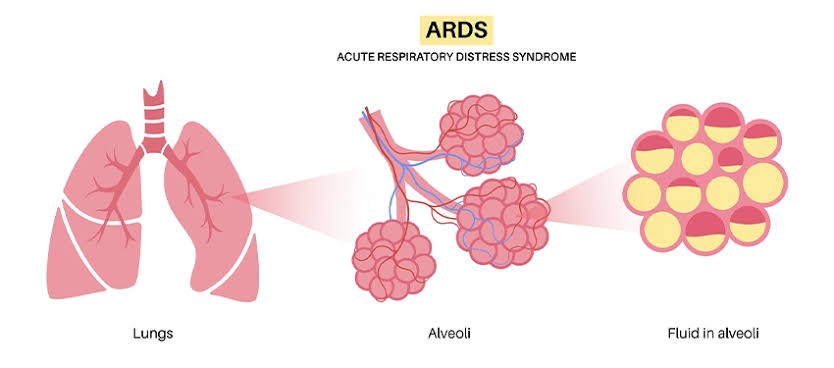
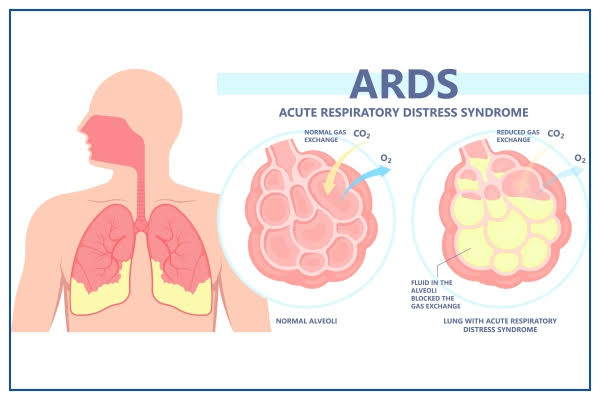
Define acute respiratory distress syndrome
This is a life threatening, severe lung condition. In which there is a fluid buildup in the tiny and elastic air sacs in the color so that the air sacs cannot transport oxygen and the oxygen level in the blood decreases.
Write causes of acute respiratory distress syndrome
infection
Pneumonia
Tuberculosis
Sepsis
Covid 19
Inhalation of Harm Full Subtance
Trauma – direct injury to the lungs
Pancreatitis
Drug overdose (cocaine, opioids)
Draunig Write clinical manifestations of acute respiratory distress syndrome
Difficulty in breathing
Rapid breathing
Hypoxemia
hypoxia
Cyanosis
Cough
Frothy secretion
Fatigue and weakness
Confusion
Altered mental status
Write diagnostic evaluation of acute respiratory distress syndrome
History Collection
Physical Examination
x ray
CT scan
Echocardiogram
Electrocardiogram
Pulse oximeter Write management of acute respiratory distress syndrome
Mechanical ventilation: Provide mechanical ventilation to support breathing.
Oxygen therapy: Provide supplemental oxygen to maintain oxygen levels.
Fluid Management: Administer fluid management to prevent fluid overload and pulmonary edema from developing in patients with ARDS.
Pharmacotherapy: Administration of antibiotics to treat infection. Also providing corticosteroids and neuromuscular blocking agents in some cases.
Positioning: Provide prone position to the patient. So that lung perfusion and ventilation can be improved.
Nutritional support: Provide adequate nutrition to patients with ARDS to promote healing and recovery.
Treatment of underlying causes: Identify and treat the underlying cause of ARDS.
Supportive Care: Close monitoring of vital signs, electrolytes and organ function. Pain management, sedation and stress relief. Write complications of acute respiratory distress syndrome
Blood clot
Deep vein thrombosis
Collapsed lung
Confusion
Multiple organ failure
Muscle weakness
Lung fibrosis
Define SARS
SARS Means Severe Acute Respiratory Syndrome. It is a viral respiratory illness caused by the SARS-related corona virus (SARS-CoV).
Write clinical manifestations of SARS
Fever
Cough
Shortness of breath
Chills
A muscle
Head one
Loss of appetite
Sore throat
Fatigue
Malays
In severe cases, pneumonia and respiratory failure can also occur. Write diagnostic evaluation of SARS
History Collection
Physical Examination
RT-PCR
Serology (ELISA)
x ray
CT scan
Complete blood count
Blood culture
Sputum culture Write management of SARS
Supportive Care: Use supplemental oxygen or mechanical ventilation if needed. In addition to providing adequate hydration and nutrition of the patient.
Infection Control Measure : Isolate SARS my patient to prevent it from spreading to other people. Use of personal protective equipment when dealing with patients with SARS.
Antiviral therapy: Since SARS is caused by a virus, antiviral drugs are used to treat it.
Corticosteroids: Use of corticosteroid drugs in selected cases.