ENGLISH EMERGENCY DRUGS-GNM-SY-VIVA TABLE
EMERGENCY DRUGS-VIVA TABLE
💖 Adrenaline (Epinephrine)


Form:
Epinephrine injection: These are available in various concentrations and forms, including pre-filled syringes, ampoules and auto-injectors.
Indication
- Anaphylaxis (Anaphylaxis)
Severe allergic reactions
Primary treatment (first line treatment) such as due to insect bites (sting bites), food or medicine allergies.
- Cardiac Arrest
It is used during cardiopulmonary resuscitation (CPR) to support heart function
- Severe asthma or respiratory distress:*
In some cases, adrenaline may be used to relieve severe trachea constriction and improve breathing.
Dosage:
The dose of adrenaline depends on the specific indication, the patient’s weight and the way of administration of the medicine.
- In anaphylaxis, the typical adult dose is 0.3 to 0.5 mg (0.3 to 0.5 ml of a 1:1000 solution) given intramuscularly (Im) in the flank thigh. The dose of this medicine in children depends on the weight of the child.
- In cardiac arrest, higher doses may be used, and are usually given intravenously.
Route of Administration
Intramuscular (IM): Treatment of anaphylaxis involves intramuscular (IM) injection into the thigh.
Intravenous (IV): In cardiac arrest or other emergency (critical) situations, adrenaline can be given directly into a vein (vein). This is usually done by a healthcare professional (health care provider).
(Auto-injector) Auto-injectors:
- Adrenaline auto-injectors are pre-filled devices designed for easy and quick administration by individuals or caregivers in critical situations.
- These devices come with specific instructions, and dosages are usually standardized.
Sometimes it is also given directly into the heart which is called intracardiac
Contra Indication Contra Indication-
- Adrenaline should be used with caution in patients with certain medical conditions such as heart disease, hypertension and hyperthyroidism.
- Do not take this medicine if you have an allergy to sulphites or other components of the medicine.
Side effects
- After administration, the patient should be closely monitored for any improvement in symptoms or worsening of the condition.
- Adrenaline side effects may include increased heart rate, increased blood pressure, anxiety, tremors, and possible cardiac arrhythmias.
Nursing Intervention
Assessment of lung sounds, blood pressure, and pulse during continuous therapy
Check for chest pain and blood glucose level as it increases. Monitor for bronchospasm.
The correct administration of adrenaline should be trained and the given protocol should be followed.
In emergency situations, the immediate administration of adrenaline can save lives, but it should be part of a comprehensive emergency response plan.
Warning:
Great care is needed when calculating and preparing the dose of epinephrine. Because epinephrine is a highly potent drug.
If there is even a small error in calculating the dose or in preparing it, it leads to serious Edwards effect.
Double checking and verifying when calculating pediatric doses.
Use only small doses for a short period of time. Epinephrine fastness (which is a form of drug tolerance) occurs if it is used for a long time.
Protect the drug solution from light, excessive heat and freezing (extremely cold temperatures).
Do not use if the solution is brown or pink in color.
The drug solution should be clear and colorless.
Shake well before withdrawing the solution.
to do
Rotate the subcutaneous injection site after injection to prevent necrosis.
Monitor the injection site frequently.
In case of excessive hypertensive reaction, keep a rapid acting alpha adrenergic blocker (phentolamine) or a vasodilator (nitrate) ready (keep available).
Keep an alpha adrenergic blocker and intermittent positive pressure breathing ready in cases with pulmonary edema.
Keep a beta adrenergic blocker ready in case of cardiac arrhythmia. (Propanolol, cardiac selective beta adrenergic blockers such as atenolol used in patients with respiratory distress)
Be careful not to exceed the prescribed dosage of the inhalation product.
Administer pressurized inhalation drug during second half inspiration. Because the airways become wider and the airway distribution becomes wider.
If a second inhalation drug is required, the previously given dose should be given at peak level (three to five minutes).
Give second dose when available.
Use topical nasal solution only for acute condition. Do not use it for more than three to five days and do not give more than the prescribed dose.
After the vasoconstriction subsides, rebound nasal congestion occurs i.e. severe stuffy nose.
💖 Atropine:


Atropine reduces the amount of secretions from the mouth and respiratory passages and relieves spasm and constriction of the respiratory passages and reduces the effect of paralysis in the respiratory muscles. All this is caused by a toxic nerve agent. This toxic nerve agent increases the activity of anticholinesterase in the central nervous system.
Atropine is a drug commonly used in medical settings, and the antimuscarinics
(Antimuscurinics)
belongs to a class of drugs known as Here are some details about atropine, especially when given as an injection:
1. Purpose and mechanism of action:
Note: Stimulation of beta1-adrenergic receptors in the heart is positive inotropic (increases contraction), chronotropic (increases heart rate), dromotropic (increases conduction rate through the AV node) and lusitropic (increases diastole). (while increasing relaxation of the myocardium) results in effects.
*2. indication
(specific indication), the dose varies depending on the patient’s age and weight. Atropine is usually given intravenously (IV) for a faster onset of action. It can also be given intramuscularly (IM) in certain situations. *4. *Contradiction:
Contraindications:
Known hypersensitivity to the drug Atropine
(Hypersensitivity)
Contraindicated in patients with
(Contraindicated)
Can be used with caution in patients with glaucoma, as it may increase intraocular pressure.
can increase.*5. *Side effects:
Side effects: Common side effects include dry mouth
(Dry mouth), blurred vision
Urinary incontinence
and constipation. Higher doses may cause more serious side effects such as hallucinations
(hallucinations),
Confusion and tachycardia.*6. *Observations and interactions:
Monitoring and interaction: Heart rate and rhythm should be closely monitored during atropine administration. Atropine may interact with other drugs, especially those that affect heart rate and rhythm.*7. *Special Considerations:
Special considerations: Elderly patients may be more sensitive to the side effects of atropine. Care should be taken when administering atropine to patients with pre-existing cardiac conditions.*8. *Duration of Action:
Duration of action: The duration of the effects of atropine is relatively short, and depending on the clinical response, repeat doses may be required.*9. *Storage:
Storage: Atropine should be stored according to the manufacturer’s recommendations, usually at room temperature, protected from light.*10. *Emergency Situations:
Emergency situation: Atropine is often used in critical situations, such as cardiac arrest or severe bradycardia, to temporarily increase heart rate and improve cardiac output. It is important to note that the information provided here is general in nature. are, and specific details about atropine administration should always be based on the instructions of the prescribed healthcare provider. Dosage and administration may vary depending on individual patient characteristics and clinical context. Always consult a healthcare professional for specific and individualized information regarding medications before taking medications.
💖 Hydrocortisone
Hydrocortisone is a medicine of the corticosteroid group and has the same action as cortisol. Cortisol is a natural hormone produced by the adrenal gland.
Hydrocortisone has anti-inflammatory and immunosuppressive properties and is useful in many different conditions.
Let’s know about hydrocortisone in detail. 1) Uses: Inflammation
Hydrocortisone is commonly used to treat many conditions such as skin disorders, allergic reactions, and inflammatory joint disorders.
Allergies
Hydrocortisone is used to relieve symptoms of an allergic reaction such as itching, redness, swelling.
Autoimmune condition
Hydrocortisone is also prescribed for autoimmune disorders such as rheumatoid arthritis and lupus. Hydrocortisone suppresses the immune response.
Adrenal insufficiency
Hydrocortisone is used as hormone replacement therapy in cases with adrenal insufficiency such as Addison’s disease.
2) Forms
Hydrocortisone is available in various forms such as cream, ointment, lotion, oral tablet, injection.
Topical forms are used in skin conditions while oral tablets or injections are used in systemic conditions.
3) Mechanism of action
Hydrocortisone inhibits the activity of certain immune cells and reduces the production of inflammatory substances in the body, which helps suppress inflammation and modulate the immune response.
4) Side effects
Common side effects of the topical form of hydrocortisone include skin irritation, burning, itching, and dryness.
When using it as a systemic drug, side effects like weight gain, increase in blood pressure, mood changes, changes in blood glucose etc. are seen.
5) Precaution & Contraindication
- Hydrocortisone should be used under the supervision of a health care professional. Because its prolonged and excessive use can cause complications.
Hydrocortisone should be avoided without medical advice if the patient has other conditions such as systemic fungal infection. 6) Dosage
The dose and duration (how long to give) of hydrocortisone depends on the condition being treated. To follow the regimen prescribed by the health care provider. Do not stop medication suddenly without consulting a health care provider.
7) Interactions
Hydrocortisone interacts with other medications so the health care provider should provide knowledge to the patient about all medications the patient is taking. Including over counter drugs and supplements.
If another medicine is being used and hydrocortisone medicine has been prescribed by a health care professional, follow the dosage and duration instructions given by them. Regular monitoring and follow up by health care provider. Because the effectiveness of the medicine can be known and potential side effects can be managed.
Hydrocortisone is a medicine of the corticosteroid group. which is used to reduce inflammation and relieve symptoms associated with conditions such as skin disorders, allergic reactions, and inflammation. As a nurse, when administering hydrocortisone to a patient or a patient receiving hydrocortisone Many interventions are required while caring.
These interventions vary by specific patient and health care setting. Always follow health care provider’s orders and institute policy.
Here are some general nursing interventions.
1) Assessment
Assess the patient properly before administering hydrocortisone. Knowing the patient’s medical history, allergies and current medications.
Monitor vital signs and especially blood pressure as corticosteroids affect fluid and electrolyte balance.
2) Patient education
Educate the patient about the purpose of administering hydrocortisone and its therapeutic effect.
Explain the importance of the medication the patient is taking and educate them not to stop it suddenly.
3) Dosage administration
Administer medicine as per orders of health care provider and as per institute policy.
Ensure accurate calculation and administer as per prescribed route. Like topical, oral, injection
4) Nursing Responsibility / Monitoring adverse effects
To observe whether adverse effects are present or not. Like increase in blood glucose level, fluid retention, weight gain, mood changes etc
Monitor for signs of an allergic reaction such as rash, itching, swelling
Blood glucose monitoring
Monitor glucose levels in a regular manner in diabetic patients and patients at risk of steroid induced hyperglycemia. 6) Fluid & electrolyte balance Monitoring fluid and electrolyte balance as corticosteroids may cause fluid retention and electrolyte imbalance.
Infection prevention
Explain to the patient that the chance of infection increases while receiving corticosteroid therapy, encourage the patient to maintain proper hygiene, and tell the patient to notify the health care provider if any signs of infection occur.
Skin assessment
Perform a skin assessment if hydrocortisone is administered topically. Assess skin for irritation, atrophy or any other reaction.
Psychological support
Consider the patient’s emotional well-being because corticosteroids can cause mood swings and psychological effects.
Follow up:
Schedule follow-up appointments to monitor the patient’s response to corticosteroid therapy.
Evaluating the need for dose adjustment or discontinuation based on the patient’s condition and response to treatment.
💖 dexamethasone (Dexamethasone)

Group-Dose : Corticosteroid
Dose -Dose: 8 mg
► Indication
Inflammation – Inflammation
Allergic reaction – Allergic reaction
Arthritis – Arthritis
Respiratory disorder – respiratory disorder
Auto immune disorders – Auto immune disorders
All So Uses in covid 19 to Reduce Inflammation. – All so use in Kovid 19 to reduce inflammation.
otitis media – otitis media
Gastro industrial infection. – Gastro industrial infection.
► CONTRACT INDICATION
Hypersensitivity – Hyper sensitivity
At the time when receive live vaccine. – At the time when live vaccine has been taken.
Use causally with hypertension and diabetes. – Use causally with hyper tension and diabetes.
► Mechanism of action
Cotyledons decrease vascular dilation and capillary permeability and decrease migration of leukocides to the site of inflammation.
Corticosteroids help lower levels of prostaglandins and reduce the interaction between certain white blood cells (T-cells and B-cells) involved in the immune response. Corticosteroids stimulate this effect to lessen the inflammatory response.
Side effects Vision Change – Vision Change
Swelling– Swelling
Rapid weight gain- Rapid weight gain
Sleep problem – sleep problem
Mood changes– Mood change
Dry skin – Dry skin
Thinning skin– Thinning skin
Bruising- Bruising
Slow wound healing – Slow wound healing
Head ache- Head one
Disneyness
Stomach pain- Stomach pain
► Nursing Interventions
Checking regular blood pressure, heart rate and temperature.
Monitor fluid intake and output to detect fluid regurgitation and electrolyte imbalance early.
Dexamethasone affects glucose levels so regular glucose level monitoring should be done especially in diabetic patients.
Dexamethasone causes low immunity so observe closely for signs of infection.
To resolve bone den CT related issues and provide calcium and vitamins if required.
This medicine impacts mood and behavior thus providing emotional support.
Ocular complications can occur due to long-acting corticosteroid use, so regular eye check-ups are recommended.
Live vaccine should be avoided if long therapy is started.
💖 calcium gluconate
Group: Mineral supplement
Dosage: 500mg -2gm
►Indication -Indication
Hypo calcium – hypo calcium
Calcium deficiency- Calcium deficiency
Hyperkalemia- Hyperkalemia
Cardiac arrest -cardiac arrest
Cardio Toxicity Due to Hypo Calciumia. Cardio toxic CT DDU hypo calcium.
Hypermagnesemia. Hypermagnesemia.
Anti dot of magnesium sulfate.- Anti dot of magnesium sulfate.
Contra indication- Contra indication
Hyper calcium. Hyper calcium.
Renal impairment Renal impairment
History of Kidney Stone. History of Kidney Stone.
Atrio ventricular block. Atrio ventricular block.
Ventricular fibrillation. Ventricular fibrillation.
Mechanism of Action – Mechanism of Action
Blood calcium level increases by binding with magnesium and potassium. Calcium maintains the function of the nervous, muscular and system.
► Side effect – Side effect
Skin race– Skin race
Etching- Etching
Hives
Swallowing of face, lip, tongue – Swallowing of face, lip, tongue
Fast or regular heart beat – Fast or regular heart beat
High calcium levels – High calcium levels
Nosea
Vomiting Vomiting
Constipation Constipation
Nursing Intervention-Nursing Intervention/Responsibility
Monitor the patient’s calcium level and renal function.
Monitor vital sign
Administer calcium gluconate at a proper dilute and infusion rate to minimize adverse effects.
Educate the patient about the side effects and purpose of calcium gluconate.
Regular monitoring for signs of hypercalcemia like arrhythmia, allergic response etc.
Take proper care of the IV site because leakage of calcium gluconate causes damage to the surrounding tissue so that infiltration can be prevented.
Avoid high calcium rich food including dairy product, green leaf, salmon fish etc.
💖 sodium bicarbonate
Group: Alkalizing agent
Dosage-: 650 mg
indication
Metabolic acidosis Metabolic acidosis
Severe diarrhea-severe diarrhea
Acidity -acidity
poisoning -poisoning
Cardiac arrest -cardiac arrest
Hyperkalemia – hyperkalemia
Topical application – Topical application
Drug in toxicity- Drug in toxicity
►Contract Indication
Hypersensitivity – Hypersensitivity
Underline metabolic or respiratory alkalosis
The patient is losing chloride by vomiting
Heart disease – heart disease
In Edema-ed
Cardiac decompression
Primary or secondary aldosterone – Primary or secondary aldosterone
Hypo calcium- Hypo calcium
Hyper tension- Hyper tension
Severe recipe retary conditions – severe recipe retary condition
Pregnancy and breast feeding. -Pregnancy and breast feeding.
Mechanism of action – Mechanism of action
The body accepts the hydrogen and bicarbonate ions present in sodium bicarbonate which increases the pH and maintains buffer regulation.
Reacts with Hcl in the stomach to neutralize the condition.
Urinary alkanization
Improves pH by increasing excretion of bicarbonate ions from urine.
► Side effects
Nosea
Fluid retention – fluid retention
Metabolic alkalosis – Metabolic alkalosis
Electrolyte imbalance
High blood pressure
Gas and Bloating -Gas and Bloating
Alter blood pH -Alter blood pH
Hypocalcemia- Hypocalcemia.
►Nursing Intervention
Take patient’s heart related history before use.
Monitor vital sign
Monitor calcium bicarbonate and other electrolytes.
Explain to the patient about the side effect, no purpose of the medicine.
Regular blood ph check.
Observe for signs of fluid retention and metabolic alkalosis.
Maintaining the patient’s fluid balance. There is a risk of special fluid retention.
Sodium cycling affects calcium balance so monitor for symptoms such as muscle twitching, numbness, tickling.
Proper positioning when administering sodium bicarbonate IV can prevent complications.
Making accurate documentation.
Recording of intake and output.
Monitoring the level of consciousness.
💖 HEPARIN (Heparin)

►Group (Group)– Anticoagulant (blood clot means)
Heparin is a powerful and fast-acting anticoagulant that is effective both in vivo and in vitro.
►Mode of action
It works indirectly by activating plasma anti-thrombin III and other similar cofactors and rapidly inhibits coagulant factors IXa, Xa, XIa, XIIa, plasmin, kallikrein and thrombin, which prevents the conversion of fibrinogen to fibrin. High doses of heparin cause platelet aggregation. (aggregation) and increases bleeding time. Heparin is a large, ionized molecule that is not orally absorbed. Heparin shows immediate effect if given IV but after 60 minutes if given subcutaneously.
It cannot cross the placental barrier. It is metabolized in the liver by heparinase and excreted in the urine.
► Dosage
This dose is in I.U i.e. International Unit
Adult: 10,000 to 12,500 iu (iv stat)
Maintenance dose: 5000 iu 4-6 hr.
10000- 20000 iv / Ltr in 5% glucose and saline drip.
10,000-12,500 iu , 8-12 hrly.deep im inj.
Child: initially 50 iu / kg iv /kg iv direct
Maintenance dose: 100 iu /kg / dose iv drip 4 hrly.
►Indication
Heparin is used for rapid and short live action. It is discontinued after 4 – 7 days of therapy and oral anticoagulants are given in maintenance therapy unless contraindicated.
Given as prophylaxis in major surgery such as deep vein thrombosis.
It is given in prophylaxis and treatment in venous thrombosis, pulmonary embolism.
Also used in MI, Unstable angina and Disseminated intravascular coagulation (DIC).
► Contraindications
_ Bleeding disorder
Hypersensitivity thrombocytopenia
_ Severe hypertension
Sub acute bacterial endocarditis ocular neurosurgery
Lumbar puncture chronic alcoholic
_GI ulcer
Aspirin and other antiplatelet drugs should be used cautiously with heparin therapy. Heparin should not be used during pregnancy.
► Adverse drug reaction
Bleeding can be the most serious complication of heparin therapy overdose. Its first sign is Hematuria (blood in urine).
Hypersensitivity– (fever, rigor, anaphylaxis)
Bleeding from gums
Thrombocytopenia- Thrombocytopenia
Hyperkalemia- Hyperkalemia
Elevation of serum transaminase level
osteoporosis -osteoporosis
► NURSING RESPONSIBILITY OF HEPARIN INJECTION – (Nursing responsibility of heparin injection)
5R’s to keep in mind (Right Patient, Right Time, Right Route, Right Dose, Right Medicine).
Obtain the patient’s medical history, allergies, and baseline coagulation status and monitor for contraindications and any conditions that would affect the administration of heparin.
Giving the patient a comfortable position while giving the injection. Answer any questions he has and explain the procedure.
To wash hands.
Select the administration side, clean it and give the injection.
Monitor for its adverse reactions.
Recording and reporting.
Monitoring coagulation levels.
Providing health education to patients about side effects and complications.
► INR ratio INR (ratio)
INR – International Normalized Ratio
INR is a standard measurement of blood clotting time. It is used to monitor and adjust the dose of anticoagulant medicine in the patient. like ; Heparin, Warfarin etc.
Formula to calculate INR ratio:
INR=Patient’s PT
——————-❌ISI
Normal PT
Patient’s PT : Patient’s current prothrombin time.
Normal PT : Prothrombin time laboratory value in a healthy individual.
ISI : International Sensitivity Index; ISI accounts for the variation in thromboplastin reagents used by different laboratories.
► Normal blood clotting time – 1.0 INR
If the value of INR increases that means the clotting time decreases.
The target INR range depends on the disease condition being treated, such as atrial fibrillation or deep vein thrombosis.
Regular monitoring of INR levels is necessary to check the range of anticoagulant therapy to prevent blood clotting without increasing the risk of bleeding.
💖 PROPRANOLOL
Group – Beta blocker
Route – oral, iv
Duration of action – 8 to 12 hr
►Dosage
Adult : 40 mg twice daily 80 mg once daily.
Children : 1 mg / kg / 24hr initially every 6 hours.
5 mg / kg / 24hr every 6 hours if needed and progress.
►Mode of action
Propranolol exerts an antagonistic action on adrenergic receptors due to which the heart rate and the force of cardiac contraction also decrease and also inhibits renin secretion.
► INDICATION
Hyper tension Hyper tension
Cardiac arrhythmia Cardiac arrhythmia
Long-term management of hypertrophic subaortic MI
►CONTRAINDICATIONS
Cardiogenic shock, heart block (2nd and 3rd degree)
CCF (Congestive Cardiac Failure)
Bradycardia Bradycardia
chronic obstructive pulmonary disease (COPD)
Raynaud’s Phenomenon
►SIDE EFFECTS
Fatigue, tiredness, fever, skin rash, depression, sexual dysfunction, nightmares, nosia, cold extremities, hypoglycemia, epigastric distress.
►SPECIAL PRECAUTIONS
Adequate precautions should be taken in hepatic dysfunction, renal dysfunction, peripheral artery disease etc.
►NURSING RESPONSIBILITY
Conducting regular vital sign assessments (especially measuring heart rate and blood pressure before and after administration)
Providing education about side effects, benefits, purpose of medicine.
Watch for any side effects such as bradycardia, hypertension, respiratory distress and changes in mental status.
To monitor signs such as bronchospasm and heart block.
Checking correct dose, time, route, person etc.
💖 epsoline
Or
Phenytoin

Group: Antiepileptic drug
Dosage: 250-500mg
indication
Management and Treatment of AP Lepsy.-Management and Treatment of AP Lepsy.
Generalized tonic clonic seizures-Generalized tonic clonic seizures.
Complex parcel Caesar.
Status ap lepticus.-Status ap lepticus.
Contra indication-Contra indication
Hypersensitivity-hyper sensitivity
Sinus bradycardia.-Sinus bradycardia.
Second and third degree atrioventricular block.-Second and third degree atrio ventricular block.
Heart block – heart block
Porphyria.
►Mechanism of Action
By interacting with the neurotransmitter receptor, it reduces the excitability of the membrane, it stops the seizure by slowing down the electrical signal.
► Side effect
Drowsiness.
Gum hyperplasia.-Gum hyperplasia.
Nosea
Vomiting
Skin race-skin race
Engagement of facial features-engagement of facial features
Elevated liver enzymes.-Elevated liver enzymes.
Elevated liver enzymes. Change in blood count
►Nursing Intervention
Assess frequency, duration and characteristics of seizures regularly.
Evaluating the effect of medication.
Administer specifically during dose to monitor vital signs.
Monitoring side effects of medications.
Conducting neurological assessment to identify drug toxicity early.
Educating the patient about proper oral hygiene to minimize the risk of gum hyperplasia.
Regular serum phenytoin levels are monitored to avoid drug toxicity and the dose is adjusted accordingly.
Inform the patient about the common side effects of phenytoin but advise the patient to inform a health care worker if severe side effects occur.
Continue taking the drug without skipping.
Due to the risk of congenital abnormalities during pregnancy, the drug should not be used without a doctor’s prescription.
💖 Dobutamine
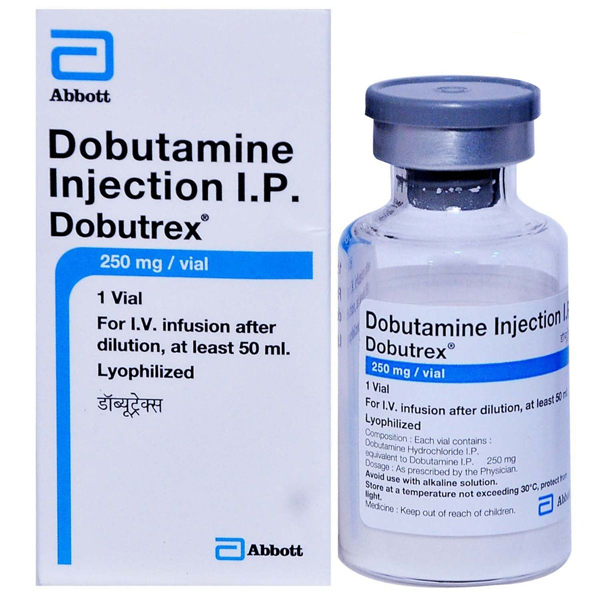

►Group
Eye tropic agent-Heart decongestant
►Route
I. V , I. V infusion
►Dosage
►Adult :- I.v 2.5-10 micrograms/kg/min
I.V infusions in 5% dextrose or normal saline above 40 micrograms/kg/min can be used.
►Onset of action
Immediately immediately.
►Duration of action
Half Life, 2min.
►Mode of action
Dobutamine is primarily a B1 adrenoceptor agonist.
Its inotropic effect on the heart is greater than its chronotopic effect.
It also exhibits alpha agonist action.
Dobutamine is derived from dopamine but is not a D1 and D2 receptor agonist.
It acts on both alpha and beta adrenergic receptors.
Dobutamine causes an increase in cardiac contraction and output.
►Indication
For short treatment of acute cardiac failure after surgery.-For short treatment of acute cardiac failure after surgery.
Congestive heart failure.-Congestive heart failure.
Post acute mi.-Post acute mi.
Cardio myopathy.-Cardio myopathy.
Septic shock.
Pharmacological stress testing.-Pharmacological stress testing.
► Contraindication
Hypersensitivity.
Idiopathic hypertrophic
Subaortic stenosis.-Subaortic stenosis.
►Side effects
Blood pressure and heart rate increase.- Blood pressure and heart rate increase.
Nosea, headache,
Chest pain, palpitation,
Shortness of breathing
hypotension
Tachycardia, dyspnoea.
►Special precaution
Continuous monitoring of ECG electrocardiogram and blood pressure while giving dobutamine.
Treat hypovolemia if there is hypovolemia while giving dobutamine injection.
Dobutamine causes a slight increase in heart rate and BP (including systolic BP).
Hence BP monitoring.
Use this medicine with caution during pregnancy.
Also, use the injection with proper care during lactation.
Use with proper care even in old age.
► Nursing responsibility
Monitor ECG for dysrhythmias and ischemia during treatment.
Treat hypovolemia before giving the infusion.
Continuous monitoring during infusion in patients with atrial fibrillation, hypertension and valvular heart disease.
💖 Dopamine

►Group
Catecholamine neurotransmitter, eye tropic agent.
►Route
I. V infusion, orally has no effect.
►Onset of action
immediate immediately.
►Duration of action
2 min.
►Dosage
Adult :-Adult
2-5 micrograms/kg/min.
Gradually increase the dose by 20-50 micrograms/kg/min by IV infusion based on response.
Child:-Child
Give 2-20 micrograms/kg/min according to individual needs.
Do not give dopamine with sodium bicarbonate in children.
►Mode of action
Dopamine is an agonist for alpha and beta one adrenergic receptors.
It is also an agonist for dopamine receptors in the CNS (Central Nervous System), renal and other vessels.
This leads to stimulation of alpha adrenergic receptors leading to vasoconstriction and increase in cardiac output, systolic BP and diastolic BP.
When given in low doses in IV infusion, it causes blood vessels to dilate and renal blood flow increases.
So there is an increase in gfr and sodium excretion.
►Indication-To whom can it be given?
Signs of grief are visible due to Mi.
Trauma, septicemia,
Heart Surgery, Renal Failure,
Chronic Cardiac Fairlier
Acute cardiac failure,
septic soak
Severe congestive heart failure with oliguria.-Severe congestive heart failure with oliguria.
►Contraindication
Hypersensitivity
hyperthyroidism
In pheochromocytes,
Atrial or ventricular tachycardia.-Atrial or ventricular tachycardia.
►Side effects
Nosea
Vomiting
anginal pain
tachycardia,
Atopic beats.-Atopic beats.
►Special precaution
Obstructive vascular disease,
Do not give in case of hypovolemia.
Use with due care during pregnancy.
Use with due care during lactation.
Nursing responsibility
Administer by IV infusion only.
Do not give Iv bolus or Im.
Dilute the drug before use.
Administer this drug through a central line or big vein.
Discontinue after a small increase in this drug.
This medicine is stable for 24 hours in solution.
Protect it from light.
Continuous BP and ECG monitoring till drug administration.
Monitor intake and output chart.
Monitoring the patient for side effects.
Checking the ivy site to see if there is an extra yzason.
Administering the drug through an electronic infusion device.
►Nursing responsibility of dobutamine
To monitor vital signs.
Checking cardiac output.-Checking cardiac output.
To observe side effects like erythemia etc.
The nurse should educate the patient about the medication and report any other abnormalities to the health care team immediately.
Nurse monitoring infusion site because tissue damage may occur if extravasation occurs.
Monitor fluid balance.-To monitor fluid balance.
Closely monitor hemodynamics of the patient including BP, central venous pressure, pulmonary artery occlusion etc.
💖 Noradrenaline injection

►Group
Alpha and beta adrenergic agonists.
inotropic agent.-inotropic agent.
►Route
Ivy and ivy infusion.
Oral is ineffective. Subcutaneous puerperal is effective.
Onset of action
IV infusion shows immediate effect.
Duration of action
1-2min
Dosage
Hypo tension/Hobbies :-
Administer continuous IV infusion.
8 – 12 micrograms/min.
Titrate to medicine (slowly increase the dose of the medicine by small increments over days, weeks or months until the patient responds well to it).
Based on weight
1) Post cardiac arrest care :-
Administer continuation IV infusion.
0.1-0.5 micrograms/kg/min. (7-38 micrograms/min given in 70 kg patient).
Titrate the medicine according to the patient’s response.
2)Cardio genetic shock:-
Continuous IV infusion.
0.05 -0.4 micrograms/kg/min.
3) Sepsis and septic hobby :-
continuous iv infusion.
0.01 – 3 micrograms /kg/min (giving 0.7 – 210 micrograms/min in a 70 kg patient.
Pediatric Dose
1) Hypo tension and shock :-
Continuous IV infusion.-Continuous IV infusion.
0.05- 0.1 microgram/kg/min.
Usual dose 2 micrograms/kg/min.
Titration of medicine according to patient’s response.
Mode of action
Acts as a powerful peripheral vasoconstrictor on both arteries and veins and acts as an isotopic for the heart.
►Indication
cardiogenic shock
septic soak
grief
Certain hypotensive state (caused by another cause eg mi, blood
restores blood pressure in transfusion reactions etc.
In Profound Hypotension in the Treatment of Cardiac Arrest.
► Contraindications
Do not give in case of hypotension due to hypovolemia.
Not to be given until volume has been replenished but as an exception may be given in emergency conditions to maintain coronary and cerebral perfusion.
► Side effects
Bradycardia-Bradycardia
arrhythmia
head ache
Hyper tension, anxiety,
Respiratory difficulty.-Respiratory difficulty.
► Special precaution
Do not give into hyper tension.
Infusing into a large vein.
Extravasation causes necrosis in the superior vein, which should be taken care of.
In pregnancy and old age, give with care only if needed otherwise not.
► Nursing responsibility
Nurse to follow 5R before giving injection.-Nurse to follow 5R before giving injection.
Administration of such inotropic drug through central line.-Giving such inotropic drug through central line.
Do not stop the infusion suddenly.
Atherosclerosis, mesenteric and peripheral vascular thrombosis or other obstructive diseases such as
Should be used with caution in patients with metabolic acidosis, hypoxia or hyperthyroidism.
Do not administer this injection to patients with hypersensitivity to sodium metaby sulfide, which is a preservative in the solution.
Discard the diluted solution of this injection after 24 hours and discard if there is a change in color.
Monitor for side effects.
To check vital signs.
Connecting the patient to an ECG monitor and monitoring the ECG and pulse rate.
Following standard dilutions.-Following standard dilutions.
Monitor urine output.-To monitor urine output.
Label the infusion series with injection name and dose etc. and set the dose in the infusion device as directed by the doctor.
💖 frusemide (Frusemide)
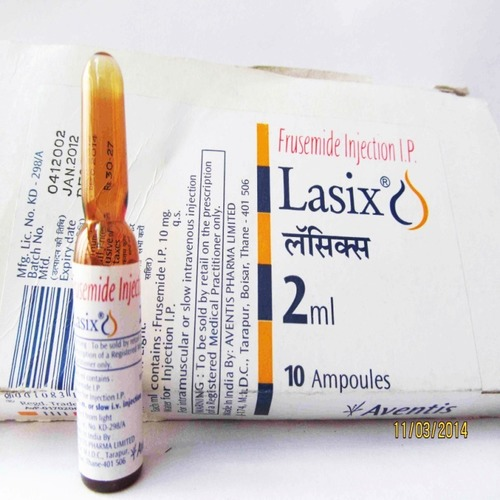
Also called Lasix or Furosemite.
► group
Loop diuretics
► Dosage
20mg iv or I’m per day
Adult Dose: 40 mg twice a day orally.
► Mode of Action
Inhibits the luminal Na-k-cl counterporter. by the Na-k-2cl transporter in the ascending limb of the loop of Henle. This leads to excessive excretion of sodium chloride and potassium in the urine and decreases reabsorption of sodium chloride and potassium in the tubule.
► Indication
Pulmonary edema Treatment of barbiturate poisoning
Mannitol resistance Acute oligouria Advanced renal failure
Prostectomy hypertension
Congestive heart failure Liver disease
► Contra indication
Hypersensitivity,
Anuria
Electrolyte im balance -Electrolyte Imbalance
Pre-Coma State-Pre-Comastate
Pregnancy & Breast Feeding Hypotension
Liver Disease – Liver Disease
Diabetes-Diabetes
Addison’s Disease – Additions Disease
Gout
► Side effects
Dehydration electrolyte im balance
Hypotension Dysness
Lightheadedness
Blood sugar level increases
Gastrointestinal issues (nausea vomiting)
Hearing Loss-Hearing Loss
► Nursing Responsibility
Monitor vital signs and fluid balance and electrolytes. Tell the family and the patient the intended side effects and benefits of the medicine.
Check daily route, time etc. while giving. Monitor for any allergic signs.
Monitor potassium levels. Check for signs of dehydration, electrolyte imbalance and hypotension.
💖 midazolam

It is also used as an anesthetic.
►Group
Benzodiazepine
►Dose
Pre operative sedation:0.07-0.08mg/kg h.im for surgery.
Conscious sedation: 1mg/ml iv
Anesthesia: 0.3 – 0.35mg/kg
Seizure: Loading dose: 0.2mg/kg
Maintenance dose: 0.1 to 2 mg/kg/hr.
►Mode of action
It acts on the central nervous system through the effect of (GABA) GABA amino butyric acid. and neurotransmitter inhibitory.
This increases inhibition of the neuron resulting in sedative anxiolytic and muscle relaxant effects. Which is commonly used in anesthesia, sedation.
►Side effects
Drowsiness _dizziness Respiratory depression
Apnea rarely nosia, vomiting etc.
►Indication (to whom it can be given?)
Preoperative Sedation Conscious Sedation
In general anesthesia induction. Control Prolong Caesar
Insomnia treats anxiety and agitation.
►Contra indication
Hypersensitivity _Narrow Angle Glaucoma
Respiratory depression Myasthenia gravis
_Pregnancy and breast feeding.
►Nursing Responsibility
Assessing the patient’s medical history, allergies, current health status, etc. Taking the patient’s consent, explaining the purpose, risks, and benefits etc.
Calculate the dose according to the weight of the patient. Monitor vital sign, respiratory status, consciousness, etc. while administering medicine.
Giving instructions about side effects etc. Closely monitor in recovery phase.
💖 LMWH (low molecular weight heparin) LMWH (low molecular weight heparin)
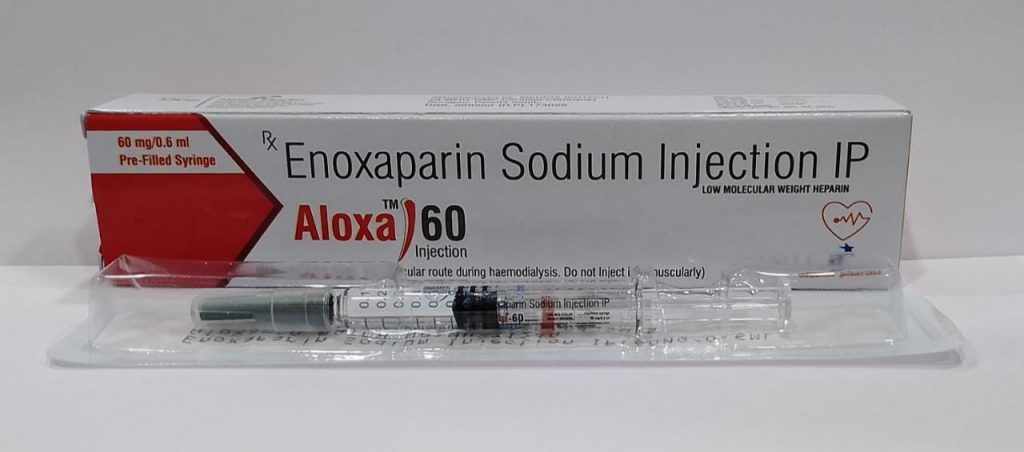
It contains less pentasaccharide sequence and higher anti-thrombin III.
►Gruop (group)
Anti-coagulant
►Dose
General surgery: 3500 iu two hours before surgery followed by 3500 iu once daily for 7-10 days.
►Route
Subcutaneous-sub cutaneous
100 iu/kg initially-100 iu/kg initially
SC. Inj. Every 12- 24 hours.-SC. Inj. Every 12- 24 hours.
►Indication
To prevent deep vein thrombosis, pulmonary embolism in surgical patients. Unstable angina as treatment in DVT To maintain the patency of fissures and sutures created in dialysis patients. Extracorporeal Circulation ►Contraindication Bleeding disorder
Hypersensitivity thrombocytopenia
_ Severe hypertension
Sub acute bacterial endocarditis ocular neurosurgery
Lumbar puncture chronic alcoholic
_GI ulcer
Aspirin and other antiplatelet drugs should be used cautiously with heparin therapy. Heparin should not be used during pregnancy.
►Mode of action
LMWHs act mostly through antithrombin-mediated inhibition of factor Xa. But some thrombin is inhibited by LMWH and is important for the antithrombin effect.
LMWH has higher bioavailability than heparin after subcutaneous injection. LMWH binds to less plasma proteins than heparin because clearance of LMWH is primarily renal which is independent of dose and slower than metabolic clearance of heparin.
► Adverse drug reaction
Bleeding can be the most serious complication of LMWH therapy overdose. Its first sign is Hematuria (blood in urine).
Hypersensitivity (fever, rigor, anaphylaxis)
Bleeding from gums
Thrombocytopenia
Hyperkalemia
Elevation of serum transaminase level
osteoporosis
►Nursing Responsibility
Assess the patient’s regular bleeding risk, renal function and weight. Keep the dose based on weight. Subcutaneous administration with proper technique taking care to minimize bleeding.
Monitor bleeding, petechiae, haematomas etc. and monitor any other symptoms. _Monitor laboratory value of APTT. Educating the patient about signs of bleeding, regular follow-up, complications etc.
Rotating the injection site prevents local irritation or hematoma. Ask him to take regular follow up for correct dosage.
_History taking for any allergy or contraindication to LMWH.
💖 LIGNOCAINE HYDROCHLORIDE (LIDOCAINE)
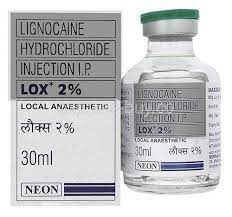
It is a local anesthetic drug given by topical application or local injection. It causes loss of sensory perception. Especially ; There is no pain in that area of the body.
Lignocaine is manufactured under the trademark Xylocard 2%.
Each ml contains – 20 mg lignocaine anhydrous
Lignocaine is a multiple amide linked local anesthetic agent that is good for topical application and injection and is available in several forms.
► INDICATION
As local anesthesia in a specific area of the body during medical procedures, dental procedures or minor surgery.
During diagnostic procedures or cardiac surgery. For example; Cardiac catheterization and angiocardiography.
pain management
Topical sprays are used during cytoscopy, bronchoscopy and ENT surgery.
Topical eye drop is used in eye surgery.
Used as local application in ointment or jelly form in rectal, vaginal, otological examination and urethral catheterization.
As topical anesthesia in patients with painful haemorrhoids, fissure, minor burns.
Also used for infiltration, nerve block, epidural, spinal and intravenous regional block anesthesia.
► DOSE
Dosage depends on clinical condition, age, weight, height, site and purpose of use.
► CONTRAINDICATIONS
To collect history regarding allergy from the patient.
Hypersensitivity (allergy to local anesthesia or any drug of amide group)
Atrioventricular block and conduction disturbance
Bradycardia Bradycardia
Severe heart block-severe heart block
Hypovolemic shock-hypovolemic shock
Myasthenia Gravis Myasthenia Gravis
porphyria
ADVERSE REACTION
Local reaction (irritation redness or swelling)
Systemic effect (dizziness, light headaches)
Central nervous system effect (confusion, tremors or seizures may occur due to high doses)
rarely, respiratory distress
Prolonged use of eye drops can cause corneal damage.
►NURSING RESPONSIBILITY
To check vital signs before, after and during administration of local anesthesia.
Assess for decreased BP, chest pain, loss of consciousness, oxygenation or perfusion deficit. Auscultation of crackles in the lungs in a patient with advanced congestive heart failure.
Assess for urinary retention, check for pain, palpate the bladder, check for benign prostatic hypertrophy in men.
Administer with caution in patients with hepatic (liver) renal dysfunction and epilepsy.
Resuscitation facility should be available when local anesthesia is to be administered.
Avoid feeding for 4 hours before administration of local anesthesia.
Advise the patient not to rub the eye after administering lignocaine eye drop.