ENGLISH-GNM MIDWIFERY UNIT 2 FEMALE REPRODUCTIVE SYSTEM-UPLOAD
FEMALE REPRODUCTIVE SYSTEM:-
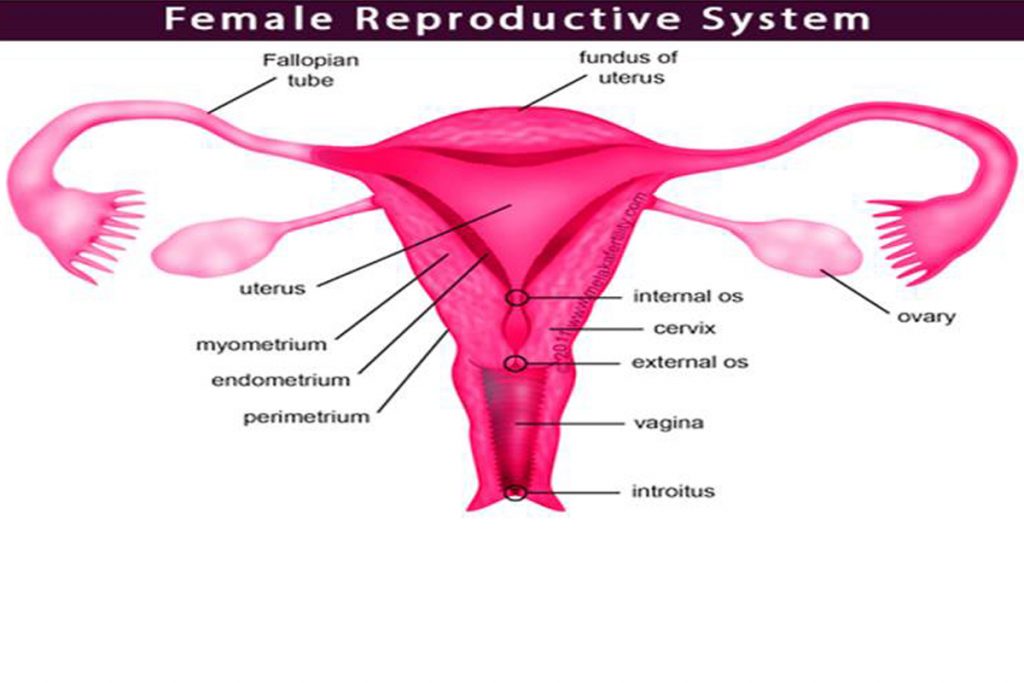
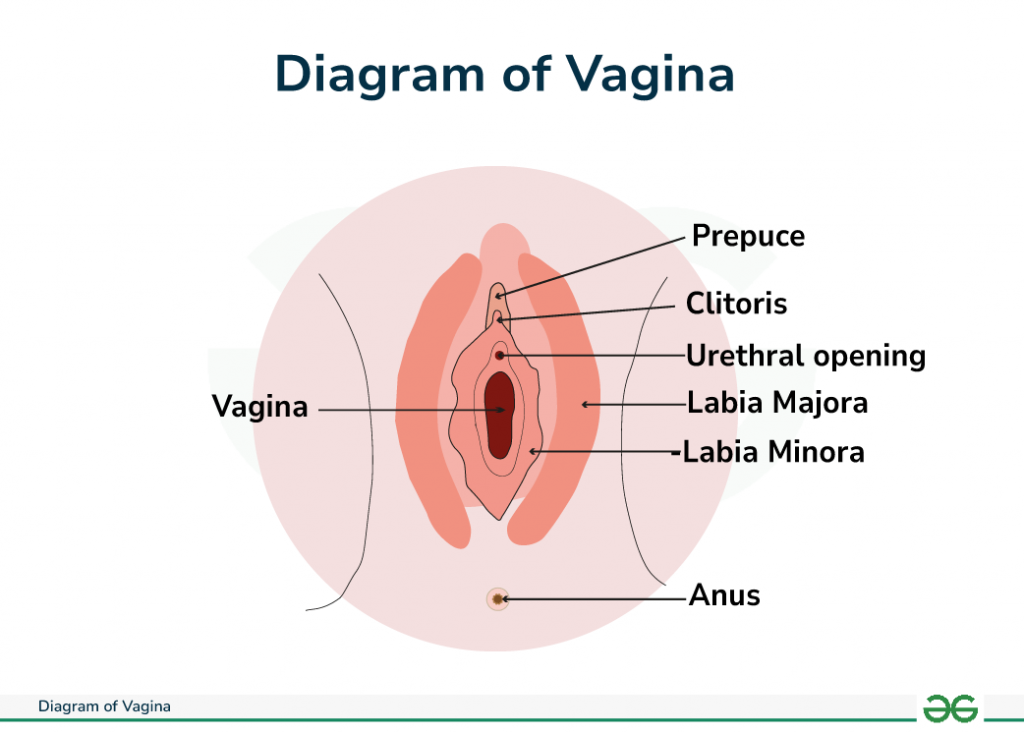
1.EXTERNAL GENITALIA (vulva)
2.INTERNAL GENITALIA
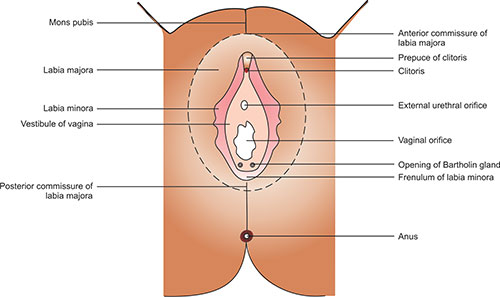
1. VULVA
External genital organs that we can see with the naked eye and are located outwards.
1.mons pubis
2.labia majora
3.labia minora
4.vestibule
5.hymen
6.greater vestibular gland
- external urethral opening
- External vaginal opening
1. MONS PUBIS:-
-The pad of fatty tissue located on the symphysis pubis
2. LABIA MAJORA:-
These are two large skin folds that come together to form the vulva.
Inside these are fat, fibrous tissue, and sebaceous glands.
It is connected to the symphysis pubis in front and to the perineum in back.
It grows hair during puberty.
3. LABIA MINORA:-
The inner part of the labia majora has small folds.
It contains many sebaceous glands.
It forms the clitoris in the front part and joins at the back to form the foreskin.
4. CLITORIS:-
This is a small penis type organ. Its structure is similar to the male penis.
It is very sensitive and has a rich blood supply.
Which acts as a stimulus during sexual intercourse.
5. VESTIBULE:-
The labia minora have a pit-like area inside, which contains the vaginal opening, urethral opening, and vestibular duct.
6.HYMEN:-
This is a thin layer of mucus membrane.
Which is located inside the vaginal opening.
It becomes a hole during puberty.
It ruptures during menstruation.
7.GREATER VESTIBULAR GLAND (Bartholin gland):-
There is one on each side of the Labia MAJORA. These open next to the vaginal opening.
Mucus is secreted in these which keeps the vulva moist.
8.EXTERNAL URETHRAL OPENING:-
It is located 2.5 cm posterior to the clitoris. On either side of it are the Skene’s glands.
9. EXTERNAL VAGINAL OPENING:-
It is located below and behind the external urethral opening.
BLOOD SUPPLY:-
Blood supply is via the internal and external pudendal arteries and venous return occurs via the corresponding vein.
LYMPHATIC DRAINAGE:-
Lymphatic drainage occurs through the inguinal gland.
VAGINA:-
FUNCTIONS:
This acts as a passage for the menstrual flow to exit.
During sexual intercourse, sperm enters through the penis.
Forms a passage for the fetus to exit during delivery.
POSITION:
This extends from the vestibule to the cervix.
RELATION:
Knowledge of the vagina is as important as any other organ.
It is essential for accurate examination of pregnant women and safe delivery.
ANTERIOR:
The bladder and urethra are in contact in the anterior wall.
POSTERIOR:
The pouch of Douglas, rectum and perineum are present.
LATERAL:
On either side are parts of the pelvic fascia, ureter, and pelvic floor muscles.
SUPERIOR:
The uterus is located.
INFERIOR:
External genital organs are present.
STRUCTURE:
This is a fibro muscular tube-like structure.
It is made up of stratified epithelial tissue.
Due to this, it is connected to the external organ.
Its anterior wall is 7.5 CM long and posterior wall is 9 CM long. This distance between the two walls is seen because the cervix is tilted forward.
LAYERS:
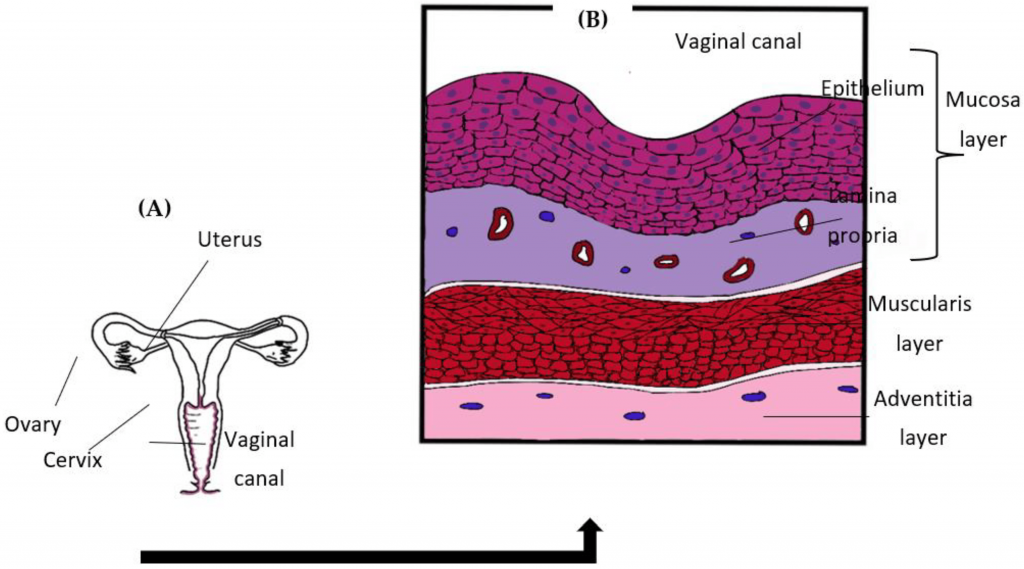
The outer layer is made of Areolar tissue.
The middle layer is made of smooth muscles.
It is divided into two parts, circular muscles are present on the inside and longitudinal muscles are present on the outside. Which are strong.
The inner layer is made of stratified squamous epithelium.
It does not contain any kind of secretory gland, only cervical secretion is secreted to the vagina.
This secretion is acidic. Its ph value is 3.5 to 4.9. Which prevents pathogenic organisms from entering. Normal mucous is alkaline. But doderlein’s bacilli take glycogen from the squamous wall and make it acidic.
BLOOD SUPPLY:
Occurs through the uterine and vaginal arteries. Venous return occurs through the internal iliac.
NERVE SUPPLY:
It is caused by the parasympathetic and sympathetic nerves that originate from the pudendal nerve.
UTERUS:-
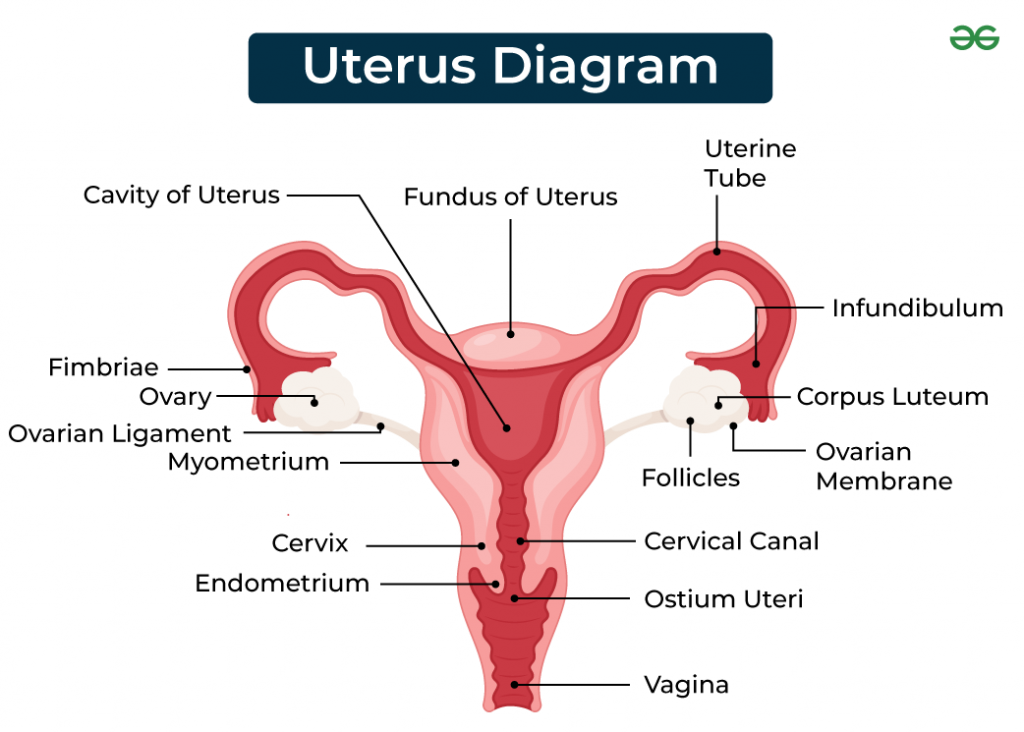
FUNCTION:
The uterus helps in the development of the fetus during pregnancy and works to expel the fetus after its full growth.
POSITION:
It is located behind the bladder and in front of the rectum and is slightly bent forward, which is called anteversion. It is slightly bent forward, which is called antiflexion. When women stand, the fundus of the uterus is resting horizontal.
ANTERIOR:
- Bladder and uterocervical pouch
POSTERIOR:
- Rectum and rectouterine or pouch of Douglas
LATERAL:
Broad ligament, uterine tube and ovaries on both sides
UPERIOR:
- Intestine
INFERIOR:
- Vagina
SUPPORT:
Menstrual support is provided by the pelvic floor, which contains ligaments that support the uterus.
LIGAMENTS:

- TRANSVERSE CERVICAL LIGAMENT:
This ligament is attached to both sides of the cervix and on the other side is attached to the side wall of the pelvis.
- UTEROSACRAL LIGAMENT:
This is located from the back of the cervix to the sacrum.
- PUBOCERVICAL LIGAMENT:
This is attached to the pubic bone from below the bladder in front of the cervix.
- BROAD LIGAMENT:
This is made of peritoneum which hangs like a curtain on both sides of the uterus and is attached to the pelvic side wall.
- OVARIAN LIGAMENT:-
This also starts from the cornua, passes behind the uterine tube, passes through the fold of the broad ligament and is attached to the ovary.
- ROUND LIGAMENT:-
Round ligament and ovarian ligament look similar so care should be taken while identifying the tube.
STRUCTURE:
- Non pregnant uterus hollo, muscular, pear shape organ
- Length: 7.5 CM
- Width: 5 cm
- Depth: 2.5 CM
- Wall thickness: 1.25 CM
- Cervix: 2.5 CM
- Weight: 50 to 60 grams
PARTS OF UTERUS:
- Body or corpus:
-Greater part which makes up 2/3 of the uterus.
- Fundus:
-Upper wall is the dome shaped part of the uterus. In which the fallopian tube is inserted.
- Cornue:
-Cornue is the part of the uterus where the fallopian tube comes and joins.
- cavity:
-The space between the anterior and posterior wall is called the cavity.
- isthmus:
-The narrow area between the cavity and the cervix which is 7mm long.
- cervix or neck:
-Protrudes into the vagina. The upper part is called the supra vaginal portion and the lower part is called the intra vaginal portion.
- Internal os:
-The narrow opening between the isthmus and the cervix is called the internal os.
- External os:
-Near the lower end of the cervix is a small round opening called the external os
-Between these two os is the cervical canal which is continuous with the uterine cavity.
LAYERS:-
1. Perimetrium
2. Myometrium
3. Endometrium
1.PERIMETRIUM:-
It is a layer of double serous membrane. It is an extension of the peritoneum that covers the entire uterus.
The anterior part covers the fundus and passes over the body to form a space called the urinary pouch.
Posteriorly, it passes over the fundus and passes up to the cervix and extends from the rectum to form the rectouterine pouch.
It is attached to the uterus and pelvis from both sides.
2. MYOMETRIUM:
The upper part of the uterus is thick. The isthmus and cervix are narrow. It has three layers.
Outer: longitudinal
Middle layer: interlacting
Inner: circular
3. ENDOMETRIUM:-
It is made of columnar epithelium. In which mucous is secreted. The upper 2/3 part is covered with mucus in the cervical canal. The lower 2/3 part extends to the vagina.
Blood supply:
- 1.uterine artery
- 2. ovarian artery
Nerve supply:
Sympathetic T12 and L1 branches parasympathetic S2,S3,S4.
This supplies the ovarian and hypogastric plexus
FALLOPIAN TUBE:-
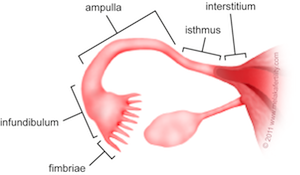
FUNCTION
Carries the ovum from the ovary to the uterus.
Receives sperm and provides space for fertilization.
Provides nutrition until the fertilized ovum embeds in the uterus.
POSITION:
The cornue of the uterus extends forward towards the pelvis. Its fimbrial end connects to the ovary.
RELATION:
- Anterior, posterior and superior: peritoneal cavity and intestines
- Lateral: side wall of pelvis
- Inferior: ovaries and broad ligament
- Medial: uterus
STRUCTURE:
Each tube is 10 cm long. Its lumen is open with the peritoneal cavity. It is divided into four parts.
1.Interstitial portion:
This is a 1.25 cm long part starting from the wall of the uterus. Its lumen is 1 mm wide.
2.Isthmus:
This is the narrow part after the interstitial. It is 2.5 cm away from the uterus.
3.Ampulla:
This is the wide part. In which fertilization takes place. This part is 5 cm long.
- Infundibulum:
This part is funnel shaped. At its end there are many raised parts. Which are known as fimbria. Which are connected to the ovarian fimbria. In this way the fallopian tube is attached.
Layers:
The inner lining is made of ciliated cubical epithelium. In which there are folds. Which slows down the momentum of the ovum. So that the ovum slowly moves towards the uterus. In this there are global self goblet cells. Which contain glycogen in their cells. They nourish the ovum.
Muscle coat:
These are made up of two layers. In our liver there is a circular layer and the outer layer is made up of longitudinal muscles. Both are smooth muscles. This helps in the peristalsis movement of the fallopian tube. It pushes the ovum towards the uterus.
Outer coat:
The outer layer is covered by the peritoneum. The infundibulum has an opening in front that connects to the peritoneal cavity.
Blood supply
Blood supply is via the ovarian and uterine arteries.
Venous return from the ovarian to the uterine vein does not occur.
Lymphatic drainage
It occurs through the lumbar gland.
Nerve supply
- Ovarian
OVARIES:-
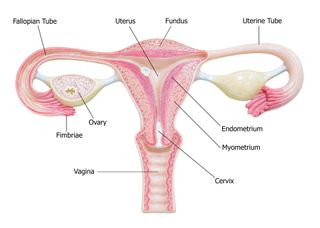
Female gonads are located on both sides of the lateral pelvic wall
Color: Grayish pink
Structure: Almond shape
3 to 4 centimeters long
1.5 to 2 centimeters wide
1 to 1.25 centimeters thick
One end of the ovary is attached to the wall of the uterus by the ovarian ligament. The other end of the ovary is attached to the pelvic wall by the suspensory ligament.
The ovary is in contact with the fimbria layer in the fallopian tube. The ovary is divided into two parts.
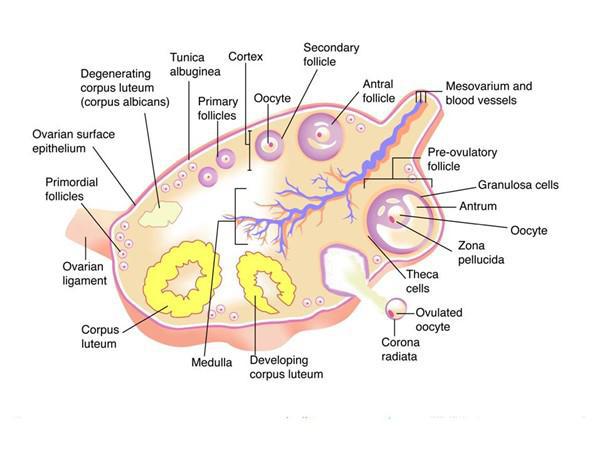
1.CORTEX:
2.MEDULLA:
The medulla is a connective tissue supporting framework.
The cortex is the covering which is the important functional part which is made up of germinal epithelium, stoma cells and Graafian follicles
The germinal epithelium lies on the tunica albuginea and forms the surface of the ovary and is the primary tissue in the ovary.
Which is present in the number of one lakh at the time of birth. When puberty is reached, premature follicles start to mature but do not ripen till puberty. At that time, they come to the surface and mature and produce ovum. Before ovulation, the surface of the ovary is smooth, then it becomes rough due to degeneration of the corpus luteum.
Mature Graafian follicles are about 10mm in diameter and are composed of two layers: an outer layer called the thica external and an inner layer called the thica interna.
The thica interna is lined with a clear fluid called the granulosa membrane, which is a layer of granulosa cells that surround the follicle’s end.
Functions of Overy:
- Ovulation
- endocrine action (oestrogen, progesterone)
Ovulation:
The mature Graafian follicle ruptures and expels the ovum. This is a process that occurs once a month in every healthy woman. This process starts from puberty and occurs on the 12th to 16th day of menstruation until menopause.
This mature follicle ruptures on the surface of the ovary and enters the fallopian tube through the fimbria.
The corpus luteum is formed from the ruptured Graafian follicle. If the egg is not fertilized, it is destroyed and replaced by hyaline tissue called the corpus albicans, which allows it to heal without forming scar tissue.
Endocrine Action:
Production of hormones
Progesterone
Estrogen
Oestrogen:
Estrogen is produced by the follicle stimulating hormone of the anterior pituitary gland and this hormone develops secondary sex characteristics in females and has metabolic effects.
It causes proliferative changes in the endometrium and helps in breast growth. It also helps in vaginal and cervical growth.
During pregnancy, it plays a role in placental growth and helps the endometrium of the uterus to grow during pregnancy.
The amount of estrogen excreted in the urine during pregnancy is dependent on the well-being of the fetus.
Progesterone
This hormone is produced by the corpus luteum of the anterior pituitary gland under the influence of LH, which is responsible for the second to week of the secretory phase of the menstrual cycle. Progesterone affects the same tissues as estrogen.
In early pregnancy, progesterone is produced by the corpus luteum, then by the placenta, and the adrenal cortex is also involved.
Due to this hormone:-
Proliferation of decidua occurs.
Provides the nutritional needs of the embryo.
Helps maintain the LV olear balance of the breast. Helps in knowing the fluid and electrolyte balance.
In fertility, it can be known whether ovulation occurs or not.
There is no need for a late pregnancy.
𝗠𝗘𝗡𝗦𝗧𝗥𝗨𝗔𝗧𝗜𝗢𝗡 𝗖𝗬𝗖𝗟𝗘 :-
The endometrium of the uterus is the reproductive tissue. Approximately 400 eggs are produced and regenerated during a woman’s entire life. Total menstrual blood loss during life is 10 to 20 liters.
The average menstrual cycle is 28 days long, which continues from regular puberty to menopause.
The first day of menstruation is considered the cycle, which has four phases during which the endometrial tissue is affected.
Indirectly, the gonadal trophin hormone of ante puberty is secreted directly, and the ovarian hormones estrogen and progesterone are secreted directly.
The phases are as follows:-
Reproductive Phage
This process begins on the third day after menstruation stops or occurs, in which new endometrium is formed in place of the shed endometrium, blood vessels reform, blood supply to the uterus increases, and new endometrium is formed.
Proliferative Phage
It starts from the fifth day after the cessation of menstruation and lasts until ovulation, i.e. 14 days before the next menstruation. Due to this, the blood supply to the endometrium increases. The endometrium tubule gland is found 2.5 mm thick. Three layers are found in the endometrium.
a. basal layer: – which is found 1 mm thick.
b. functional layer: – in which the glands are located which become thick
c. spongy layer: – in which a layer of cuboidal epithelium is located. This layer covers the functional layer.
Secretary Phage
It is related to the luteal phase of the ovarian cycle. It is related to ovulation. The corpus luteum develops under the influence of estrogen and progesterone. In this phase, the endometrium or fallopian tube is distended with blood and the soft vascular membrane is prepared to receive and fertilized egg. If fertilization does not occur during this time, the ovum dies and the endometrium undergoes degenerative changes and is shed.
Menstrual Phage
If the egg is not fertilized, the corpus luteum degenerates and due to this, the progesterone level keeps going down, due to which the blood supply to the endometrium stops, due to which the endometrium sheds and vaginal bleeding is observed which lasts for 3 to 5 days.
BREAST:-
The breast is an accessory organ of the female reproductive system. The breast is composed of compound secretory glands and is made up of glandular tissue.
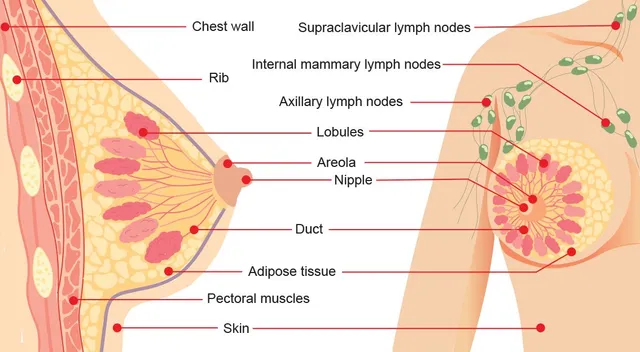
Structure:-
If you look at the breast section, you will see 20 lobes and they are divided into small parts. Inside these are the secretory cells that produce milk.
The breast is made up of fatty tissue, a layer of fatty tissue, covered with skin, in the center of which is the nipple. Around the nipple are black areola. The nipple is made up of erectile tissue.
Each lobe contains lactiferous ducts which join together to form lactiferous ducts which open in the centre of the breast. The lobes are made up of alveoli which produce milk. Around them are myoepithelium which contracts the ducts and helps in ejecting milk. Oxytocin hormone plays an important role in milk secretion. Its secretion widens the tubules which act as temporary milk reservoirs. The areola contains the Montgomery glands which secrete a sticky substance. It develops during pregnancy and the cells of the glands grow. After delivery, milk is secreted in it. The sucking of the baby produces the lactogens which helps in ejecting milk.
MALE REPRODUCTIVE SYSTEM:-
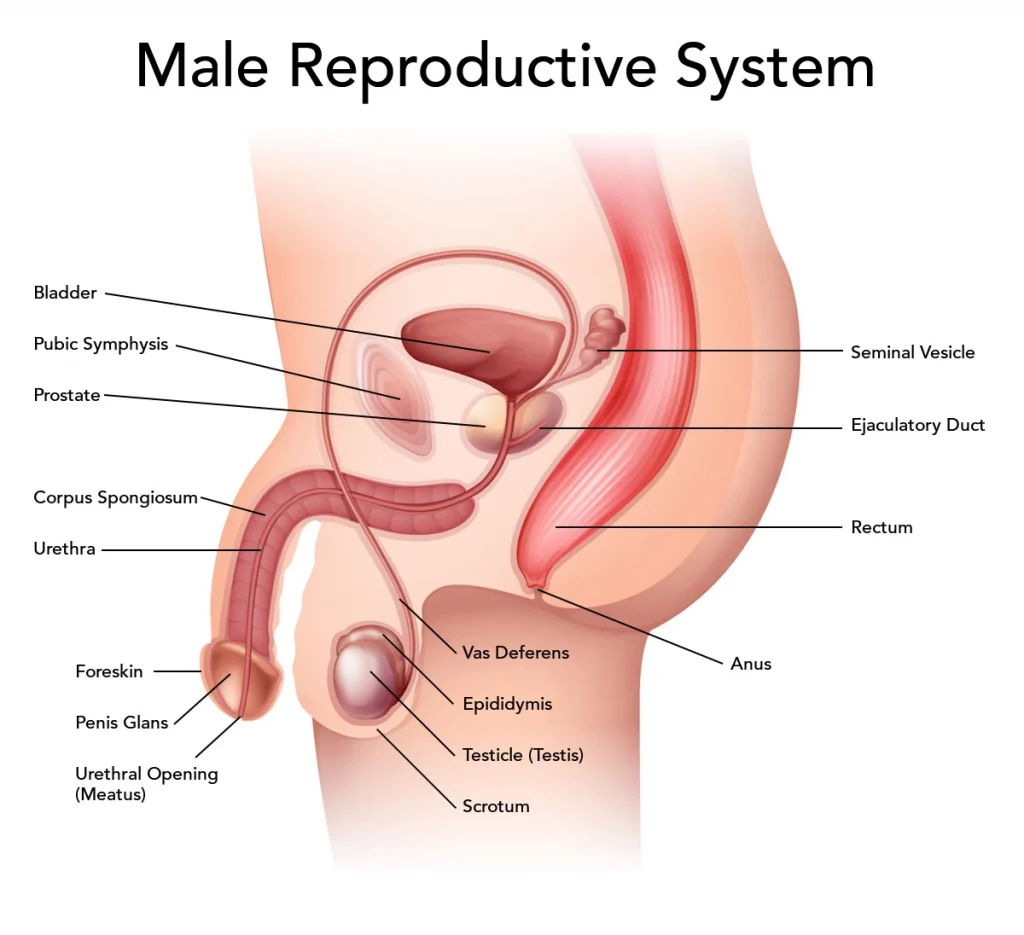
Scrotum:-
Function:-
This forms a pouch for the testicles. Below this body, the outside symphysis UBC is divided into two compartments by the upper part of the testicle, which is behind the penis.
Testes
Function:-
These male gonads produce spermatozoa and help develop the characteristic hormone testosterone, which is stimulated by follicle stimulating hormone and promotes the production of spermatozoa.
Position:-
This is stimulated in the scrotum, requires a low body temperature for its proper function, and is situated on the outside of the body.
Structure:-
- 4.5 cm long
- 2.5 cm wide
- 3 cm thick
Layers:-
Tunica Vasculosa is the inner layer made of connective tissue in which the network is located.
Tunica Albuginea is the cover of fiber tissue which divides 200 to 500 times during development.
Tunica Vaginitis is the outer layer made of peritoneum which in fetal life is located in the lumbar region and descends towards the scrotum along with the peritoneum.
Duct:-
Seminiferous Tubules: These produce spermatozoa. They are divided into three lobes, with interstitial cells located between them.
Which secrete testosterone and the tubes join to form a channel called the Epididymis.
Epididymis:-
This is a coma-shaped structure that lies on the testicles. It is transformed into a small structure in the form of a vessel and enters the inguinal canal from there it descends through the posterior part of the peritoneum and comes forward to the neck of the bladder and forms a pouch called the seminal vesicle in which the testicular secretion is deposited and enters the ejector duct. After passing through the prostate gland, it enters the urethra.
Glandular Function:-
The two functions of the testis gland are to produce spermatozoa and testosterone.
The prostate gland helps in facilitating the passage of spermatozoa through the prostate gland.
The corpus cavernosum is a gland located below the prostate gland, whose secretion acts as a lubricant.
The penis is responsible for ejaculation and urination.
Female pelvis:-
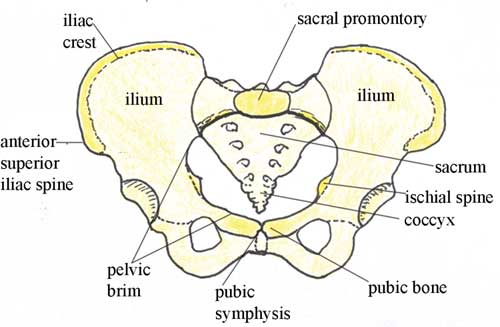
Pelvis bone ( 4 Bone ):-
1. Two innominate bone
2. One scrum
3. One coccyx
1. Innominate Bone:-
- Ilium
- Ischium
- Pubis
1. Ilium.
The upper part of the innominate bone is called the ilium.
The upper edge is called the iliac crest.
The front edge is called the anterior superior iliac spine.
The back edge is called the posterior inferior iliac spine.
Behind the iliac bone is a rough surface where the sacrum bone joins to form the sacroiliac joint.
The anterior concave surface is called the iliac fossa.
2.Ischium.
The thick lower part is called the large prominent part of the ischial tuberosity.
Which is in the resting position while sitting.
The inwardly projected part of the tuberosity can be estimated from its relation to the ischial spine.
3. Public Bone.
It forms the anterior part of the pelvis.
The second big bone is called the symbiosis of pubis when joined.
The middle part is called the body.
The ascending ramus or superior ramus that goes upwards is called the inferior ramus.
The two inferior rami join to form the pubic area.
The body of pubic ramus forms the space between the ischial and the ischial.
It is called the obturator foramen.
-The deep cap shape cavity in the innominate bone is called the acetabulum cavity. In which the head of the femur bone is located.
-This cavity is made up of 2/3 of the ilium, 2/5 of the steam and 1/5 of the pubic bone.
-Two curves are seen in the lower border of the innominate bone. The posterior inferior iliac spine starts from the iliac spine and reaches the iliac spine. This is called the sciatic notch. The ischial spine is located between the ischial tuberosity and the ischial tuberosity.
-These three bones become fused by the age of 24.
-The line that passes through the lower part of the iliac fossa is called the iliopectineal line.
-In the front part of this line, there is a small hill-like part, called the iliopectineal eminence.
-There is a raised part near the lumbosacral joint. It is called the sacral prominantary.
-The pubic bone, on the other hand, forms an arch towards the upper part, called the superior pubic arch.
-The part above the iliopectineal line is called the false pelvis, where the abdominal organs are located.
-The part starting below the iliopectineal line is called the true pelvis. In which the female reproductive organs are located.
-This part plays an important part in terms of midwifery.
• scrum:-
5 Vertebrae fuse to form one bone.
The edge that protrudes from the first sacral vertebra is called sacrum promontory.
The anterior surface of the sacrum is concave, called the hollow of the sacrum.
The two parts of the sacrum extending from the front are called wings or alla.
Inside the sacrum, 4 pairs of holes or foramen are seen intersecting the sacrum.
The sacral nerve passes through them and supplies the pelvic organs with nerves.
•coccyx.:-
4 Vertebra fuses to form a small triangular bone.
Which looks like a tail.
Connected to the sacrum above. It provides space for the fetus during delivery. Part of the tail moves backwards.
Pelvis joint:-
-Total 4 joints are formed.
symphysis of pubis -1
sacroiliac joint-2
sacrococcygeal joint-1
Symphysis of pubis.
This is a cartilaginous joint. It is formed by the union of two pubic bones. There is a pad of cartilage between the two bones.
Sacroiliac joint.
Strongest joint of the body. Slightly movable. Connects the sacrum to the iliac on both sides. This joint connects the spine to the pelvis.
Sacro coccygeal joint.
The base of the coccyx joins the tip of the sacrum to form a hinge joint. In the non-pregnant state, there is little movement in this joint, but during pregnancy, due to endocrine activity and ligament softening, the moment increases, which helps the fetal head pass through the pelvis.
PELVIC LIGAMENTS:-
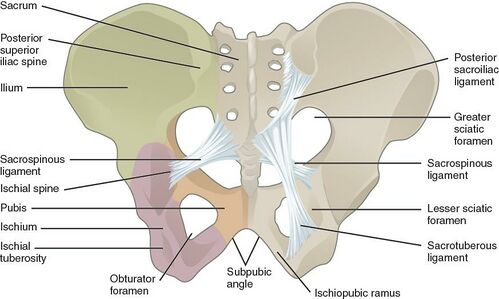
It works to hold the pelvic joint in its position and provide support to the pelvic girdle in a way that provides great strength and stability.
Interpublic ligament. It lies in front of the symphysis of pubis.
sacroiliac ligament
sacrococcygeal ligament
sacrospinous ligament
Important in midwifery Sacro tuberous ligament This lies in front of the sacrum to the ischial tuberosity.
It lies from the sacrum to the ischial spine. This ligament extends to the ischial spine. And both these ligaments cross in front of the sciatic notch. And it firm the pelvic outlet and the posterior ovum.
Due to the brim of the pelvis, the pelvic cavity is divided into two-part:-
1. True pelvis.
2. False pelvis
1. True pelvis.
This bony canal through which the fetus has to pass during birth is divided into 3 parts.
- Brim
- Cavity
- Outlet
1.Pelvic brim.
Except for the sacral promontory, the part of the brim is round in shape.
Prominantary and wing of sacral from posterior border of iliac bone to lateral border pubic bone to anterior border also formed by pubic bone.
The fixed points of pelvic brim are called land marks which start from posterior.
LANDMARKS OF PELVIS:-
sacral prominantary
sacral ala and wing
sacroiliac joint
The iliopectineal line is formed on the edge of the inner aspect of the ilium.
iliopectineal eminance
This is the rough area where the pubic meets the superior ramus of the ilium, where it forms.
Superior remous of the pubic bone
Internal border of the body of the pubic bone
Upper inner border of the symphysis of pubis.
Diameter of the brim:-
1. Anterior posterior brim diameter
2. Oblique diameter
3. Transverse diameter
Anterior posterior brim diameter:
The upper border of the symphysis of pubis starting from the sacral promentary is called the anatomical conjugate. Its length is 12 cm.
When taken below the upper surface of the posterior border, it is called the obstetrical conjugate and its length is 12 cm. Both these are called true image.
Diagonal conjugate:– The anterior posterior measurement from the lower border of the symphysis of pubis to the sacral promentary is 12 to 13 cm.
Oblique diameter.
It is a measurement from the Sacro Iliac joint of a bone to the iliopectineal line eminence of the opposite side. Its length is 12 cm. It is taken in this way on the right and left side.
Transverse diameter.
Pelvic is the length between the two iliopectineal line points. Which is 13 cm.
Sacro Cataloid diameter.:-Starting from the sacral promentary, the iliopectineal eminence on both sides is 9 to 9.5 cm long up to the occipital. The significance of this is that the fetal head gets trapped when the parietal eminence is in the posterior position of the occipital, which is related to it.
Pelvic outlet.:-
There are two outlets:-
- Anatomical outlet:
- Obstetrical outlet:
Anatomical outlet.
The lower border of each bone meets the sacrotuberous ligament.
Obstetrical outlet.
It has great practical significance because it is the narrow part of the pelvis through which the fetus has to pass.
Pelvic outlet Sacro coccygeal joint lies between the lower border of the two ischial spines and the symphysis pubis. Its shape is diamond shape and it has three diameters.
Interior posterior diameter. The lower border of the symphysis of the pubis is taken up to the middle line of the sacro coccygeal, which is usually 13 cm. During labor, the space increases due to the coccyx moving backward.
Oblique diameter. It is the line between the obturator foramen and the sacro spinus ligament, but it is not a fixed point, its length is 12 cm.
Transverse diameter: It is the line between the ischial spine and its length is 10 to 11 cm. This is the smallest diameter of the pubis.
External diameter of pelvis:-
External measurement can provide some information about the shape and size of the pelvis. A pelvinometer is used to measure this.
Internal spinus. In which the diameter between the left and right anterior superior iliac spine is measured, its measurement is 23 to 24 cm or 9 inch to 10 inch.
Inter Cristal. In this, the measurement is taken between the two Iliac crests, which is normally 26 to 27 cm, or 10.5 ” to 11.5 “.
External conjugate. This is the anterior posterior diameter of the pelvis, which is measured from the outside.
This measurement can be known by placing it on the midpoint of the pubis bone and placing it on the spine of the fifth lumbar vertebrae behind, which is 7.5″ to 8″ or 19 to 20 cm.
To know the spine of the 5th lumbar vertebrae, in the back part of the waist where the superior iliac spine of the iliac bone is located. There is a pit-like part, in its middle part the 5th lumbar vertebrae is present.
If the above measurements are small, the pelvis is small. It can be known that. Normally the difference between these measurements is 2.5 cm. Through this measurement, the internal condition of the pelvis can be known.
Pelvic cavity:-
This cavity is the part starting from the breem and ending at the outlet.
Anteriorly: Made up of the pubic bone which is the joint of two bones and forms the symphysis pubis. Which is 4 cm deep.
Posterior wall: Made up of the sacrum curve which is 12 cm long.
Lateral wall: Made up of the pelvic side wall. Especially covered by the obturator internal muscle. This cavity is circular in shape so its diameter cannot be measured exactly. All three diameters are 12 cm.
diameters Ap_ oblique_ trasverse
Brim_ 11 12 13
Cavity_ 12 12 12
Outlet_ 13 12 11
False pelvic
The part above the pelvic brim is called false pelvis. It is made up of the broad part above the iliac bone. It protects the abdominal organs. It has no specific importance in obstetrics.
TYPES OF PELVIC
The categories fall into the shape of the bream, the fetal head is the best pelvinoneter:-
- Gynecoid pelvis
- android pelvis
- Android pelvis
- Platy pelloid pelvic.
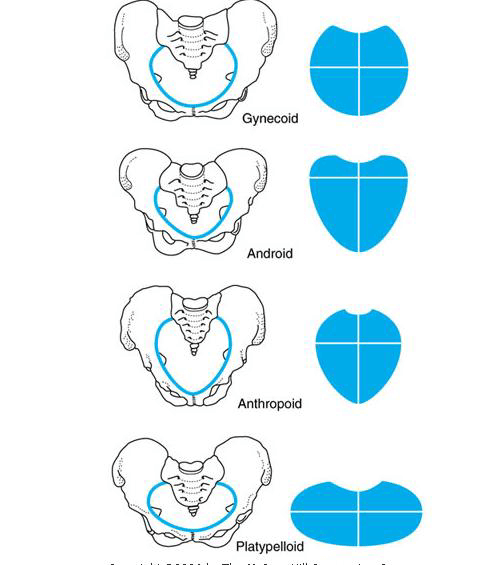
(1) Gynacoid pelvic:
A deal pelvic for child birth
Main feature (wide sciatic notch)
Round brim
Enerous fer pelvic
Straight side wall
Shallow cavity with broad wall
Curved sacrum
Blunt ischial spine
Pubic arc at 90′ angle
Average ladies’ shoulders are wider than their shoe sizes 4 and 5.3 in height.
(2) Android pelvic:
Can be compared with male pelvis.
Brim is heart shaped with narrow fer.
Transverse diameter is back. Side wall is curved inwards.
Cavity is funnel shaped.
Sacrum is straight. Ischial spine is prominent and sciatic notch is narrow.
Angle of pubic area is less than 90 degrees.
Short and fat women have more hair all over their body.
Occipito posterior position is usually seen.
Child bearing is less common.
(3) Anthropoid pelvic:
Large oval shaped brim.
Transverse diameter is greater than anterior posterior diameter.
Side walls are curved outward.
Sacrum is long and deeply concave.
Sciatic notch and subpubic angle are very wide.
This type of pelvis is seen in tall women with narrow shoulders.
Labor is usually not difficult. It is seen in anterior or posterior position.
(4) platy palloid pelvic:
Flat kidney shaped brim is seen.
In which anterior posterior diameter and transverse diameter are seen more.
Side wall is seen outward.
Sacrum flat cavity is seen shallow.
Ischial spine is seen blunt.
Sciatic notch and subpubic angle are wide.
Fetal head is engaged with transverse diameter.
Body comes out of cavity without difficulty usually.
Pelvic floor:-
It is made up of soft tissue that fills the pelvic outlet. It has strong muscles. This urethra extends from the vagina to the anal canal.
Function:-
Supports the abdominal and pelvic organs.
There is voluntary control over micturition and defecation.
Plays an important role in sexual intercourse.
Helps in passive movement of the fetus during childbirth. And helps the fetus to come out.
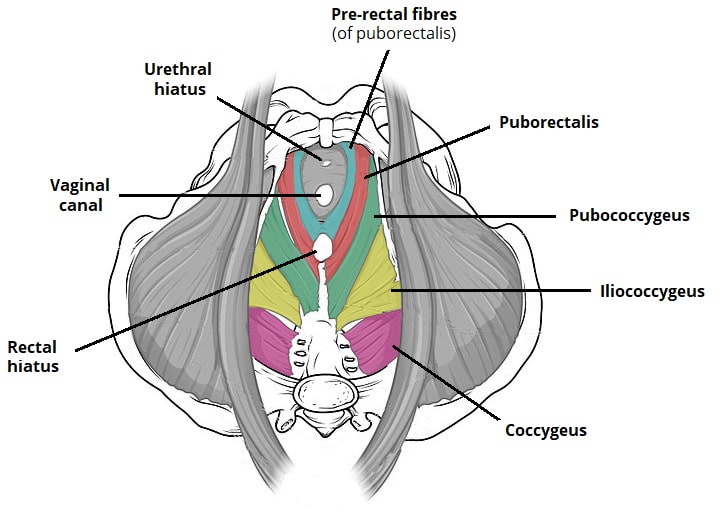
Muscle Of Pelvic Floor:-
Superficial Layer:-
Five main muscles participate.
- External anus sphincter
- Transverse perineal muscle
- Bulbo covernosus muscle
- Ischio covernosus muscle
- Membranous sphincter of the urethra.
Deep layer:-
It is made up of three pairs of muscles. Which are called levoter ani muscle
These are arranged left & right.
Pubo coccygeal muscle
Ilio coccygeal muscle
Ischio coccygeal muscle
Perineal Body
This pyramid shape is made of fibrous tissue.
It is located between the vagina and rectum.
Appex: Deepest part is made of coccygeal muscle fibers.
Base: Made of transverse perineal muscle. Which is found near the perineum. It joins the bulbo coverniea or in front & the external anus sphincter behind.
The perineal body is 4 cm long in each direction.